Clevidipine Phase III Studies Perioperative Hypertension ESCAPE1 Preoperative


- Slides: 65
Clevidipine Phase III Studies: Perioperative Hypertension ESCAPE-1: Pre-operative ESCAPE-2: Post-operative Levy JH et al. Anesth Analg. 2007; 105: 918 -925 Singla N et al. Anesth Analg. 2008; 107: 59 -67
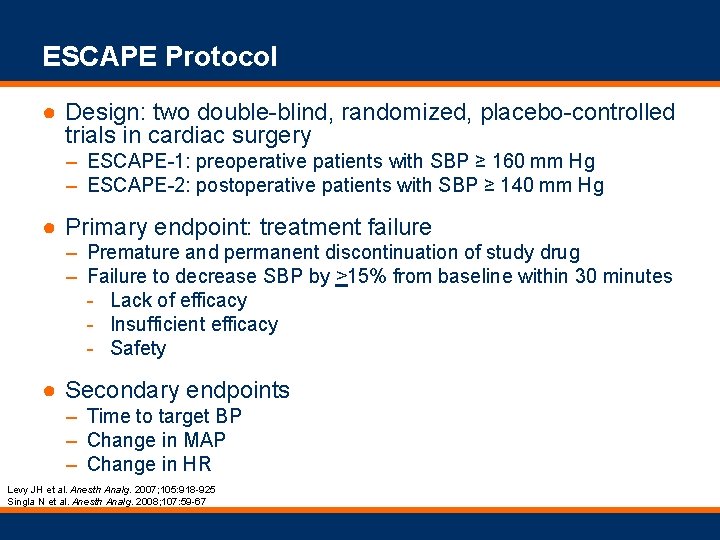
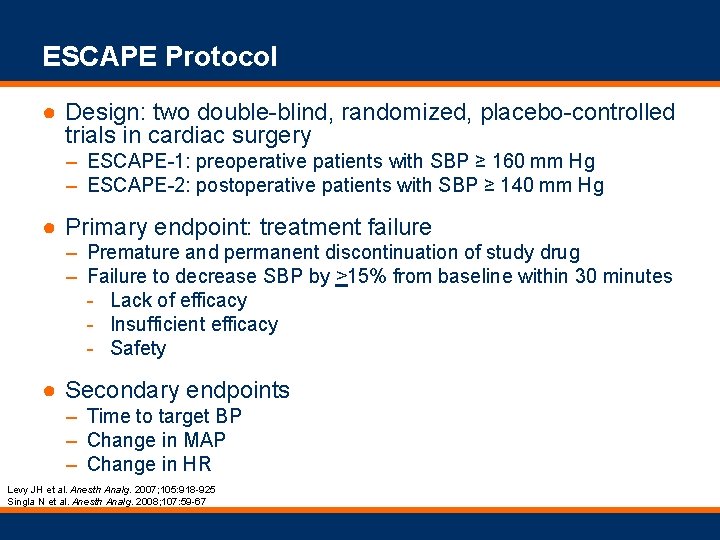
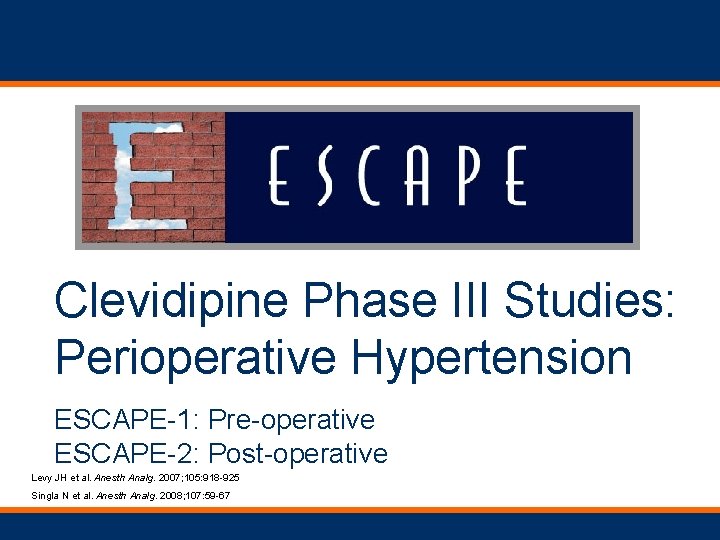
ESCAPE Protocol ● Design: two double-blind, randomized, placebo-controlled trials in cardiac surgery – ESCAPE-1: preoperative patients with SBP ≥ 160 mm Hg – ESCAPE-2: postoperative patients with SBP ≥ 140 mm Hg ● Primary endpoint: treatment failure – Premature and permanent discontinuation of study drug – Failure to decrease SBP by >15% from baseline within 30 minutes - Lack of efficacy - Insufficient efficacy - Safety ● Secondary endpoints – Time to target BP – Change in MAP – Change in HR Levy JH et al. Anesth Analg. 2007; 105: 918 -925 Singla N et al. Anesth Analg. 2008; 107: 59 -67
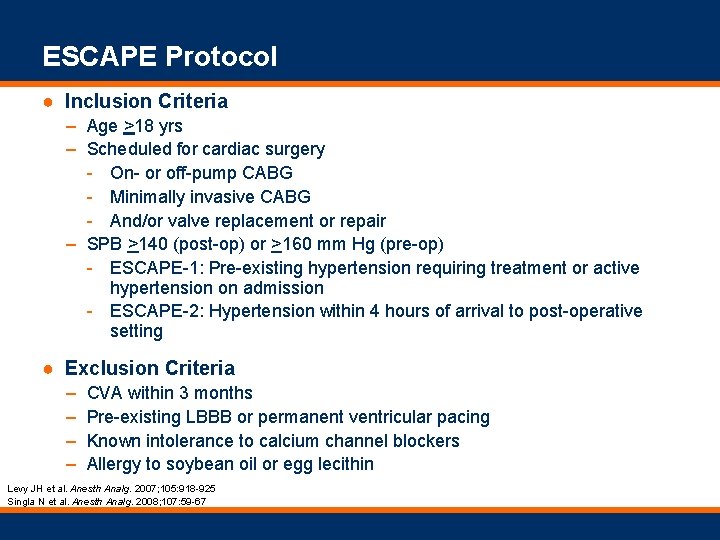
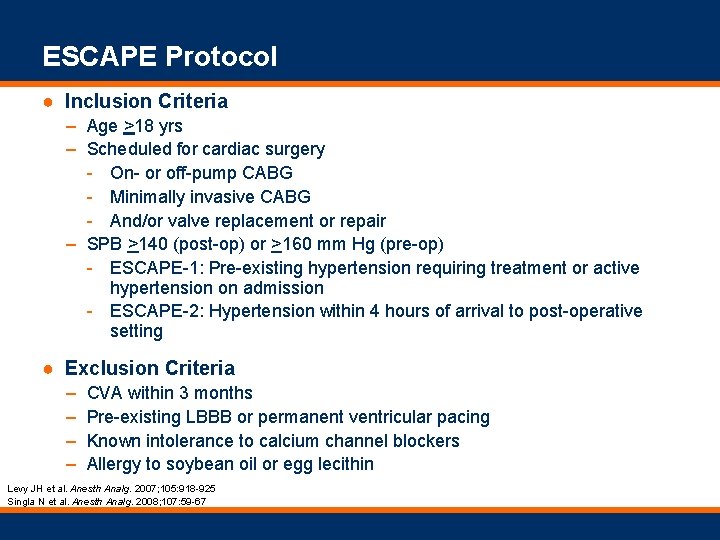
ESCAPE Protocol ● Inclusion Criteria – Age >18 yrs – Scheduled for cardiac surgery - On- or off-pump CABG - Minimally invasive CABG - And/or valve replacement or repair – SPB >140 (post-op) or >160 mm Hg (pre-op) - ESCAPE-1: Pre-existing hypertension requiring treatment or active hypertension on admission - ESCAPE-2: Hypertension within 4 hours of arrival to post-operative setting ● Exclusion Criteria – – CVA within 3 months Pre-existing LBBB or permanent ventricular pacing Known intolerance to calcium channel blockers Allergy to soybean oil or egg lecithin Levy JH et al. Anesth Analg. 2007; 105: 918 -925 Singla N et al. Anesth Analg. 2008; 107: 59 -67
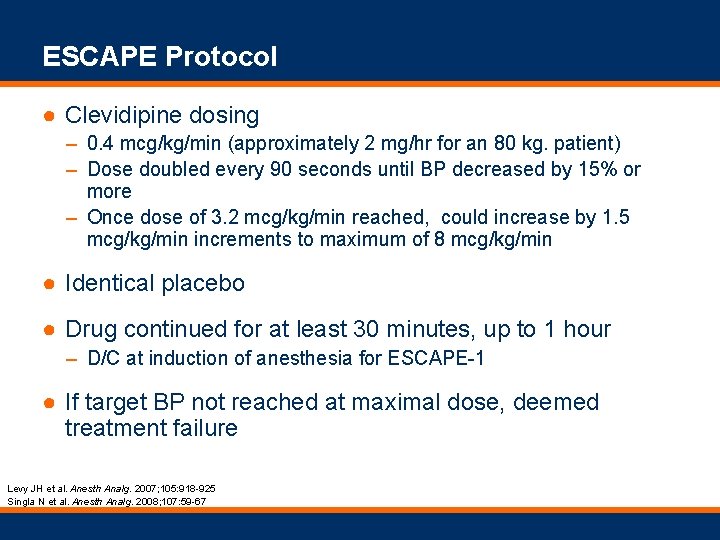
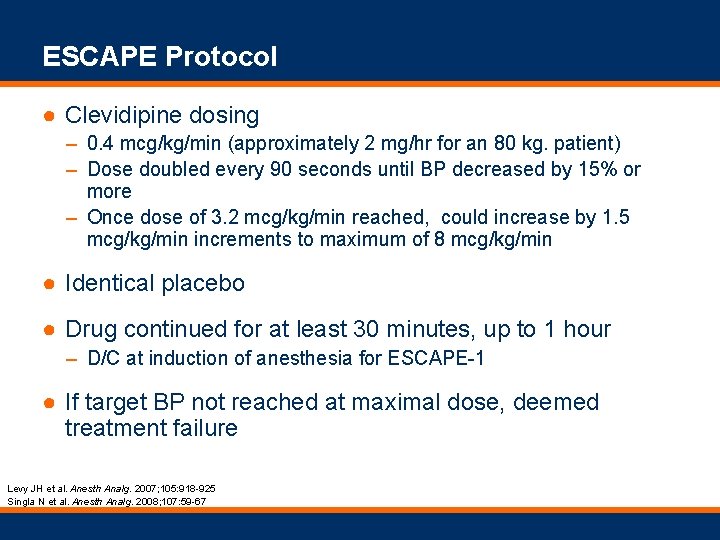
ESCAPE Protocol ● Clevidipine dosing – 0. 4 mcg/kg/min (approximately 2 mg/hr for an 80 kg. patient) – Dose doubled every 90 seconds until BP decreased by 15% or more – Once dose of 3. 2 mcg/kg/min reached, could increase by 1. 5 mcg/kg/min increments to maximum of 8 mcg/kg/min ● Identical placebo ● Drug continued for at least 30 minutes, up to 1 hour – D/C at induction of anesthesia for ESCAPE-1 ● If target BP not reached at maximal dose, deemed treatment failure Levy JH et al. Anesth Analg. 2007; 105: 918 -925 Singla N et al. Anesth Analg. 2008; 107: 59 -67
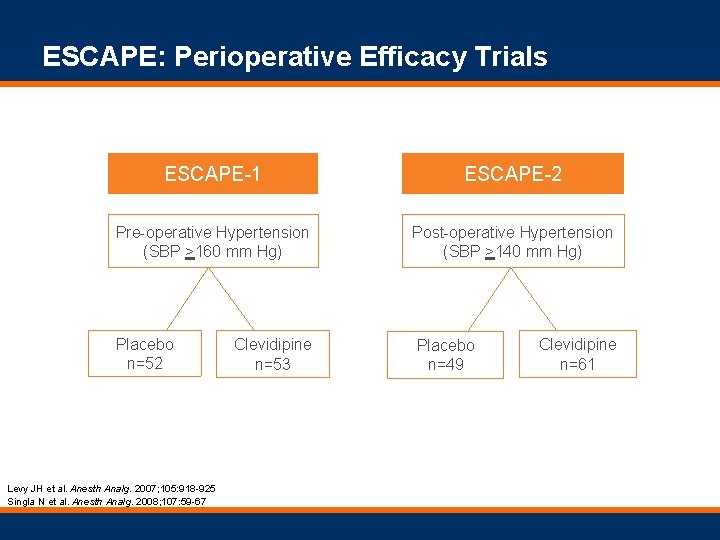
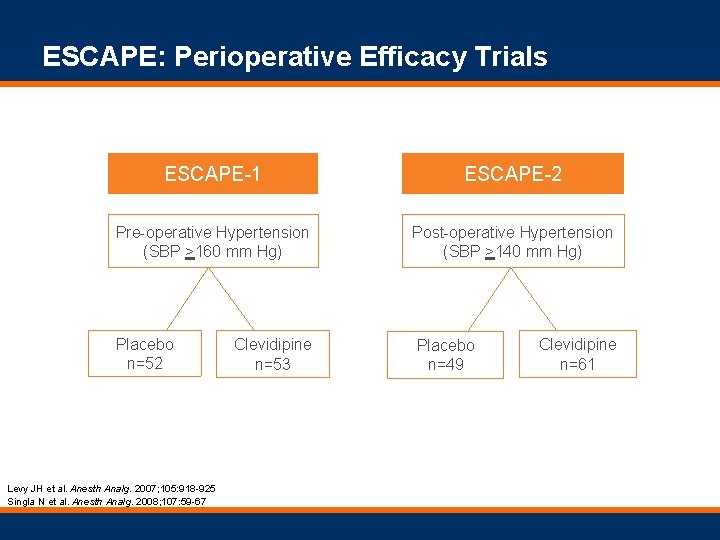
ESCAPE: Perioperative Efficacy Trials ESCAPE-1 ESCAPE-2 Pre-operative Hypertension (SBP >160 mm Hg) Post-operative Hypertension (SBP >140 mm Hg) Placebo n=52 Placebo n=49 Levy JH et al. Anesth Analg. 2007; 105: 918 -925 Singla N et al. Anesth Analg. 2008; 107: 59 -67 Clevidipine n=53 Clevidipine n=61
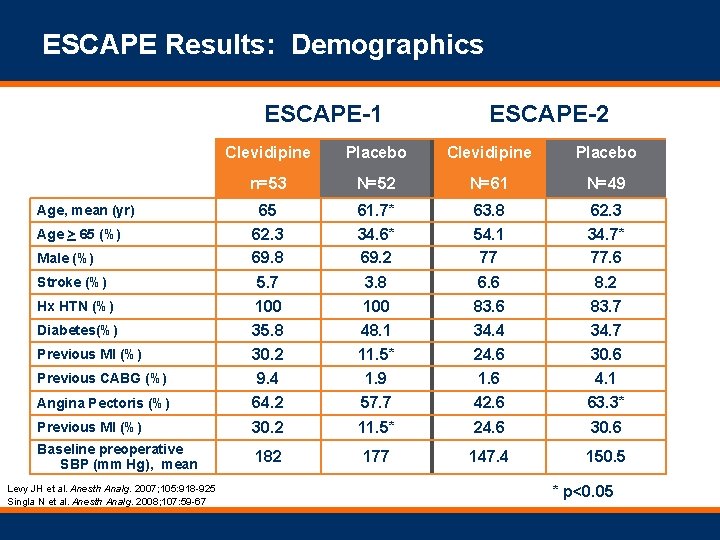
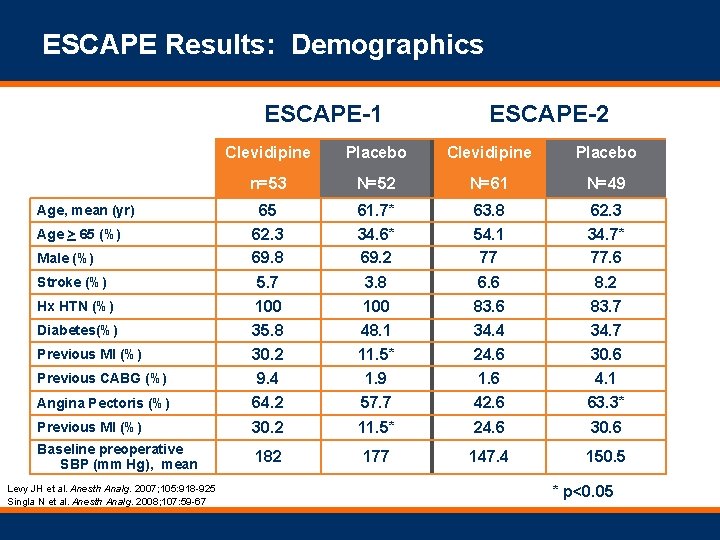
ESCAPE Results: Demographics ESCAPE-1 ESCAPE-2 Clevidipine Placebo n=53 N=52 N=61 N=49 65 62. 3 69. 8 61. 7* 34. 6* 69. 2 63. 8 54. 1 77 62. 3 34. 7* 77. 6 Stroke (%) 5. 7 3. 8 6. 6 8. 2 Hx HTN (%) 100 35. 8 30. 2 100 48. 1 11. 5* 83. 6 34. 4 24. 6 83. 7 34. 7 30. 6 Previous CABG (%) 9. 4 1. 9 1. 6 4. 1 Angina Pectoris (%) 64. 2 57. 7 42. 6 63. 3* Previous MI (%) 30. 2 11. 5* 24. 6 30. 6 Baseline preoperative SBP (mm Hg), mean 182 177 147. 4 150. 5 Age, mean (yr) Age > 65 (%) Male (%) Diabetes(%) Previous MI (%) Levy JH et al. Anesth Analg. 2007; 105: 918 -925 Singla N et al. Anesth Analg. 2008; 107: 59 -67 * p<0. 05
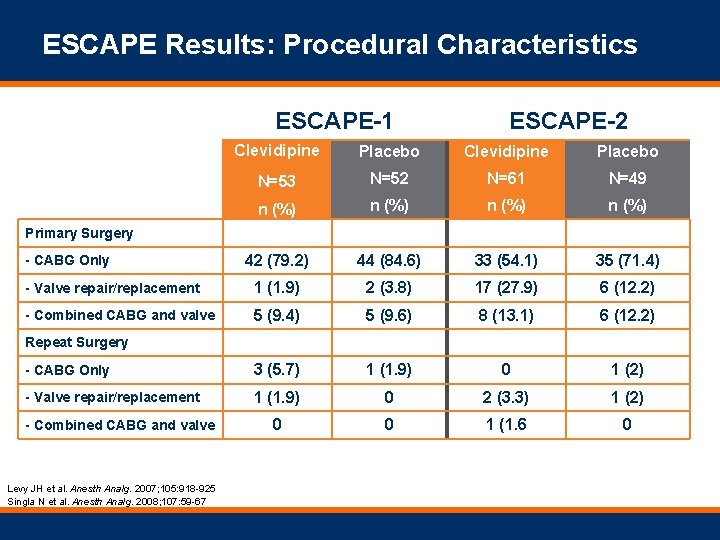
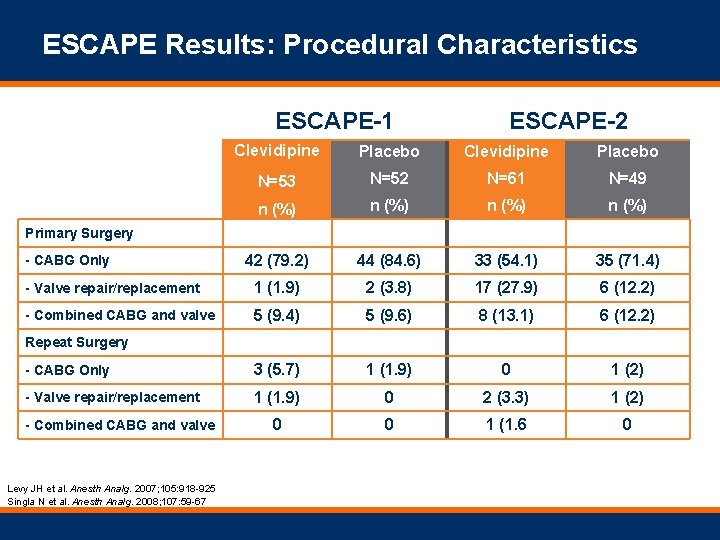
ESCAPE Results: Procedural Characteristics ESCAPE-1 ESCAPE-2 Clevidipine Placebo N=53 N=52 N=61 N=49 n (%) 42 (79. 2) 44 (84. 6) 33 (54. 1) 35 (71. 4) - Valve repair/replacement 1 (1. 9) 2 (3. 8) 17 (27. 9) 6 (12. 2) - Combined CABG and valve 5 (9. 4) 5 (9. 6) 8 (13. 1) 6 (12. 2) - CABG Only 3 (5. 7) 1 (1. 9) 0 1 (2) - Valve repair/replacement 1 (1. 9) 0 2 (3. 3) 1 (2) 0 0 1 (1. 6 0 Primary Surgery - CABG Only Repeat Surgery - Combined CABG and valve Levy JH et al. Anesth Analg. 2007; 105: 918 -925 Singla N et al. Anesth Analg. 2008; 107: 59 -67
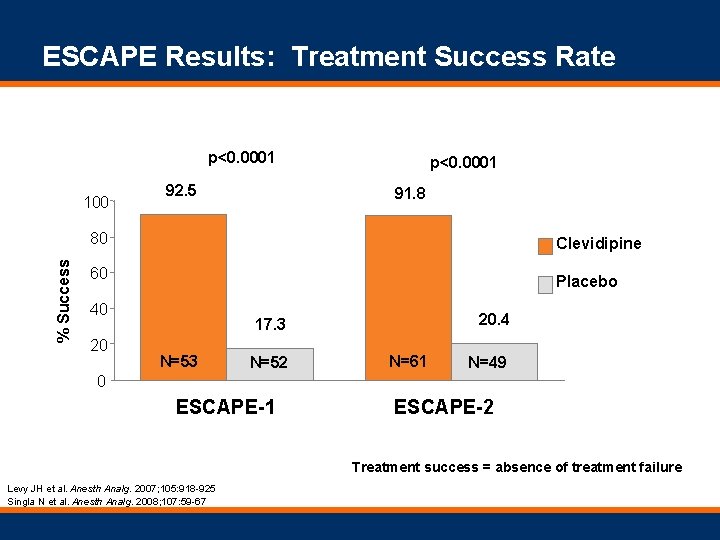
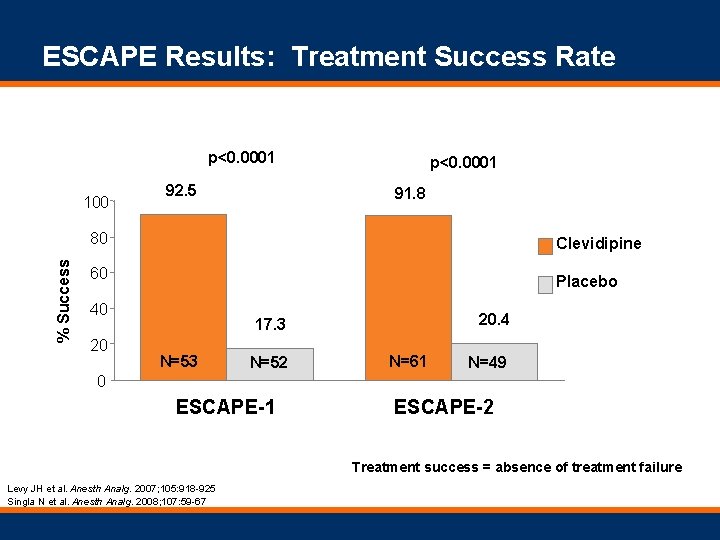
ESCAPE Results: Treatment Success Rate p<0. 0001 % Success 100 92. 5 p<0. 0001 91. 8 80 Clevidipine 60 Placebo 40 20 20. 4 17. 3 N=52 N=61 N=49 0 ESCAPE-1 ESCAPE-2 Treatment success = absence of treatment failure Levy JH et al. Anesth Analg. 2007; 105: 918 -925 Singla N et al. Anesth Analg. 2008; 107: 59 -67
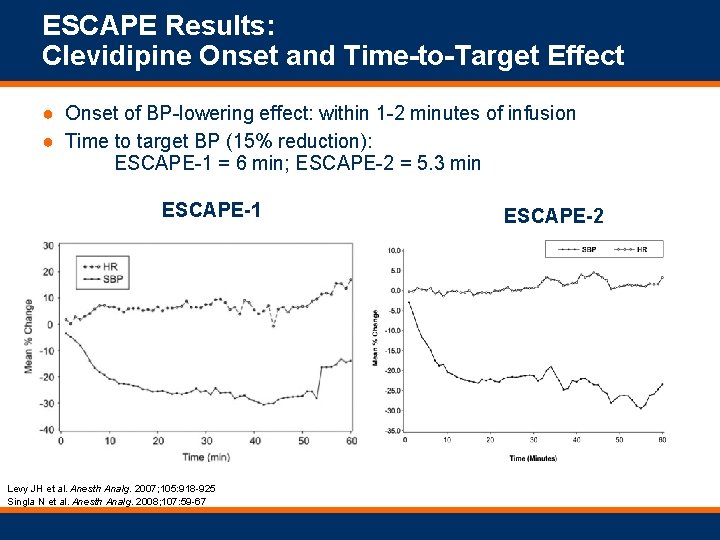
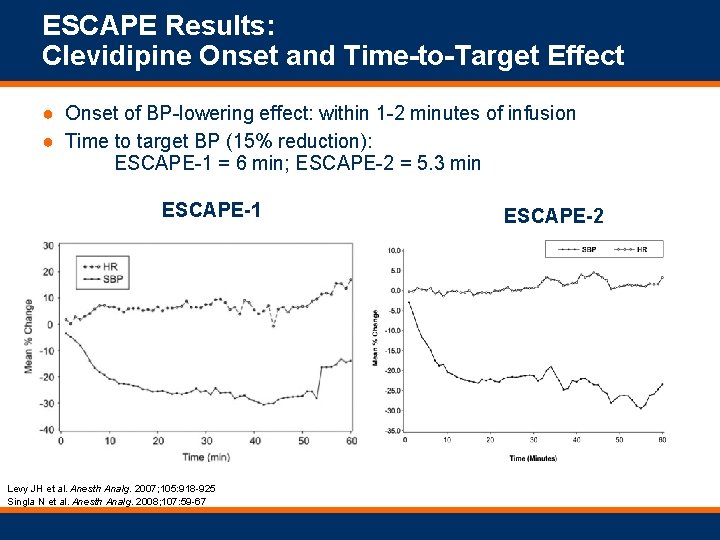
ESCAPE Results: Clevidipine Onset and Time-to-Target Effect ● Onset of BP-lowering effect: within 1 -2 minutes of infusion ● Time to target BP (15% reduction): ESCAPE-1 = 6 min; ESCAPE-2 = 5. 3 min ESCAPE-1 Levy JH et al. Anesth Analg. 2007; 105: 918 -925 Singla N et al. Anesth Analg. 2008; 107: 59 -67 ESCAPE-2
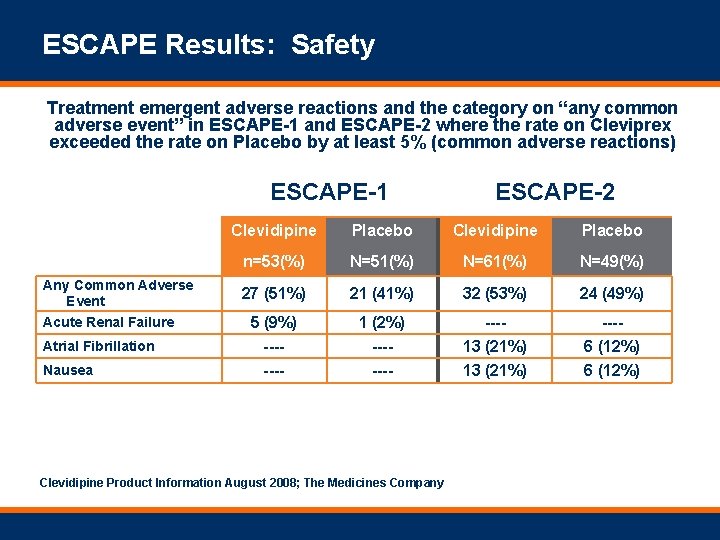
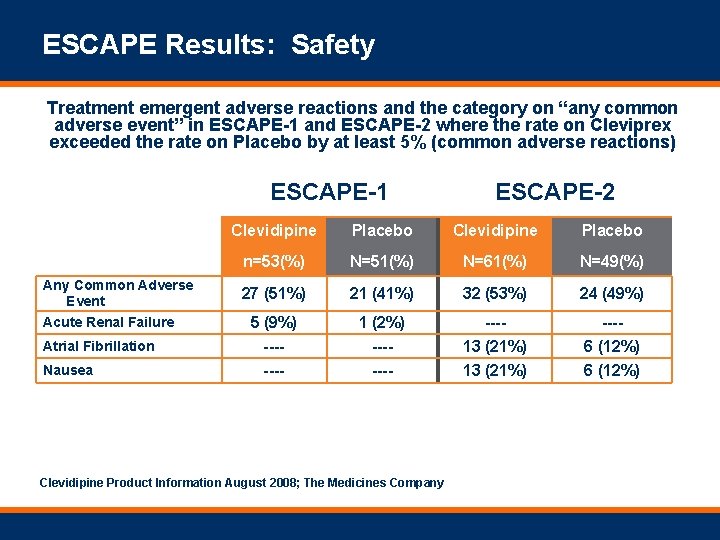
ESCAPE Results: Safety Treatment emergent adverse reactions and the category on “any common adverse event” in ESCAPE-1 and ESCAPE-2 where the rate on Cleviprex exceeded the rate on Placebo by at least 5% (common adverse reactions) ESCAPE-1 Any Common Adverse Event Acute Renal Failure Atrial Fibrillation Nausea ESCAPE-2 Clevidipine Placebo n=53(%) N=51(%) N=61(%) N=49(%) 27 (51%) 21 (41%) 32 (53%) 24 (49%) 5 (9%) ---- 1 (2%) ---- ---13 (21%) ---6 (12%) ---- 13 (21%) 6 (12%) Clevidipine Product Information August 2008; The Medicines Company
ESCAPE Results: Safety ● Clevidipine was well tolerated ● AEs were similar between clevidipine- and placebo-treated patients ● AEs were as expected for a cardiac surgery population ● Three AEs considered related to clevidipine treatment: atrial fibrillation, thrombophlebitis, and insomnia (1 patient each) ● No clinically relevant reflex tachycardia Levy JH et al. Anesth Analg. 2007; 105: 918 -925 Singla N et al. Anesth Analg. 2008; 107: 59 -67
Blood Pressure Control with Clevidipine Compared with Nitroglycerin, Sodium Nitroprusside, or Nicardipine in the Treatment of Perioperative Hypertension: Results of the Three Randomized ECLIPSE Trials Aronson S et al. Anesth Analg 2008 (in press)
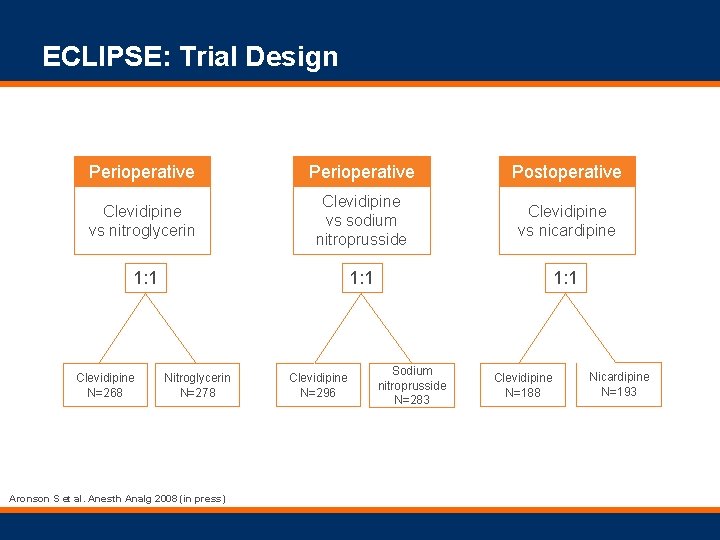
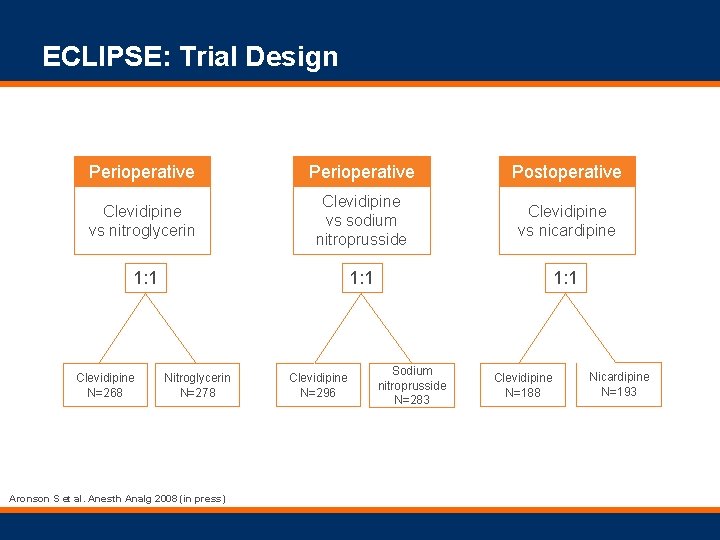
ECLIPSE: Trial Design Perioperative Postoperative Clevidipine vs nitroglycerin Clevidipine vs sodium nitroprusside Clevidipine vs nicardipine 1: 1 Clevidipine N=268 Nitroglycerin N=278 Aronson S et al. Anesth Analg 2008 (in press) Clevidipine N=296 Sodium nitroprusside N=283 Clevidipine N=188 Nicardipine N=193
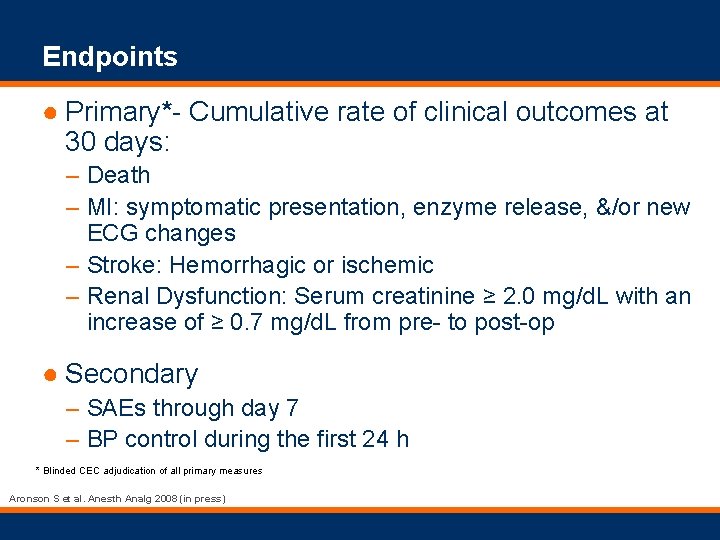
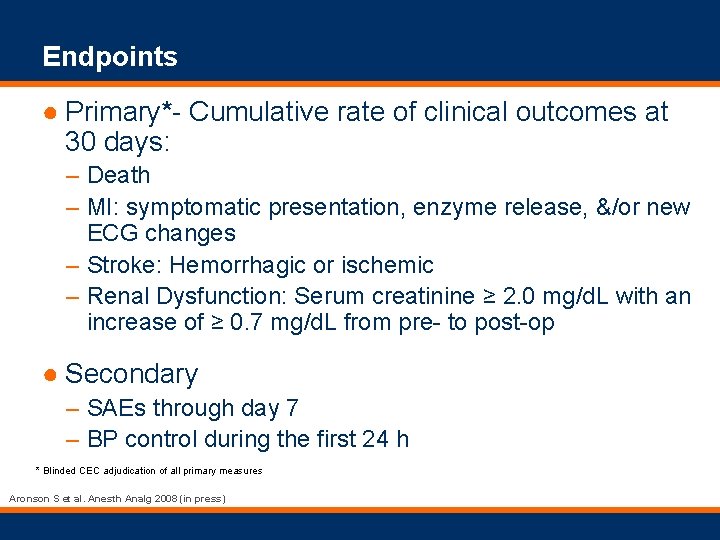
Endpoints ● Primary*- Cumulative rate of clinical outcomes at 30 days: – Death – MI: symptomatic presentation, enzyme release, &/or new ECG changes – Stroke: Hemorrhagic or ischemic – Renal Dysfunction: Serum creatinine ≥ 2. 0 mg/d. L with an increase of ≥ 0. 7 mg/d. L from pre- to post-op ● Secondary – SAEs through day 7 – BP control during the first 24 h * Blinded CEC adjudication of all primary measures Aronson S et al. Anesth Analg 2008 (in press)
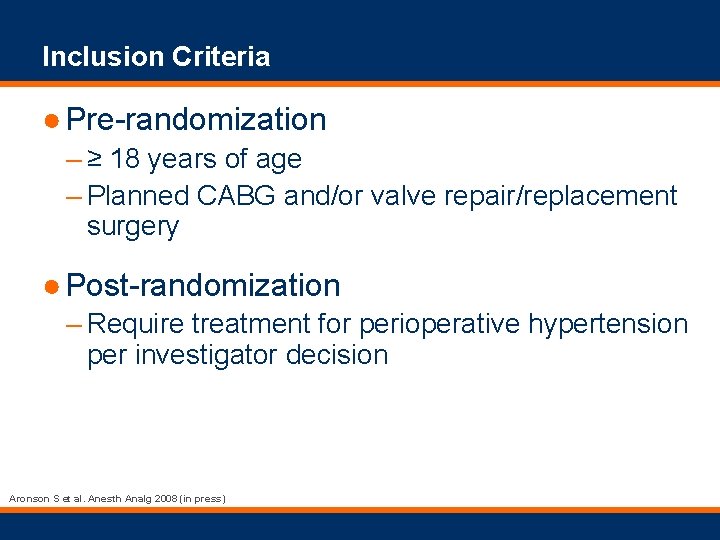
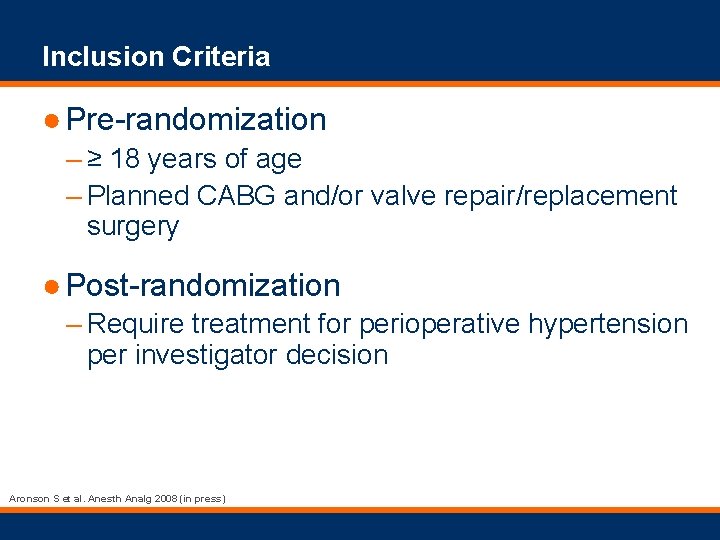
Inclusion Criteria ● Pre-randomization – ≥ 18 years of age – Planned CABG and/or valve repair/replacement surgery ● Post-randomization – Require treatment for perioperative hypertension per investigator decision Aronson S et al. Anesth Analg 2008 (in press)
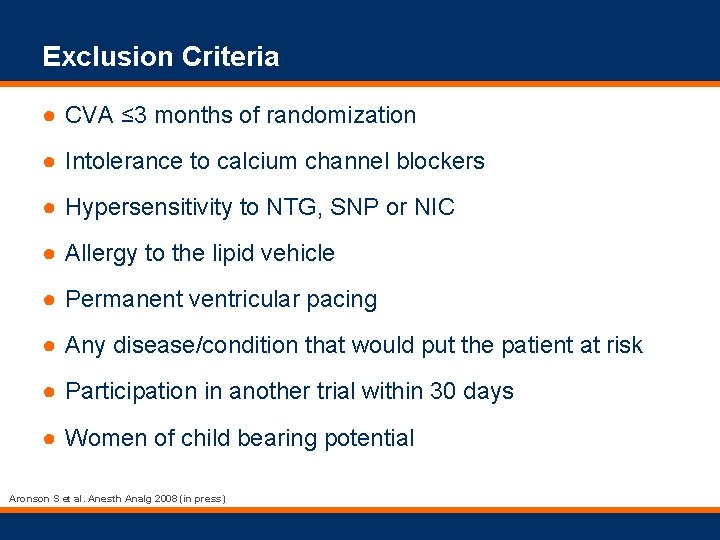
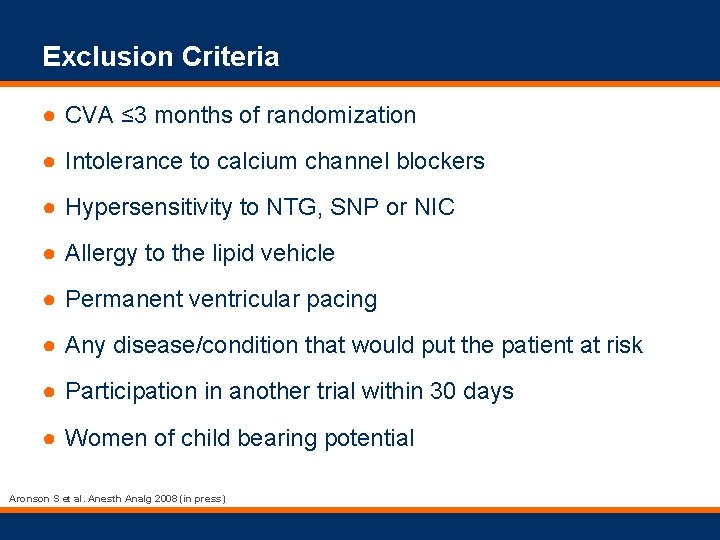
Exclusion Criteria ● CVA ≤ 3 months of randomization ● Intolerance to calcium channel blockers ● Hypersensitivity to NTG, SNP or NIC ● Allergy to the lipid vehicle ● Permanent ventricular pacing ● Any disease/condition that would put the patient at risk ● Participation in another trial within 30 days ● Women of child bearing potential Aronson S et al. Anesth Analg 2008 (in press)
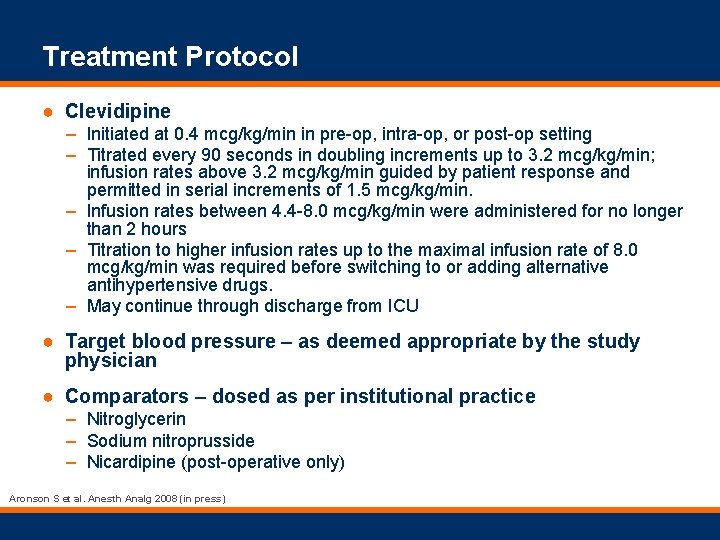
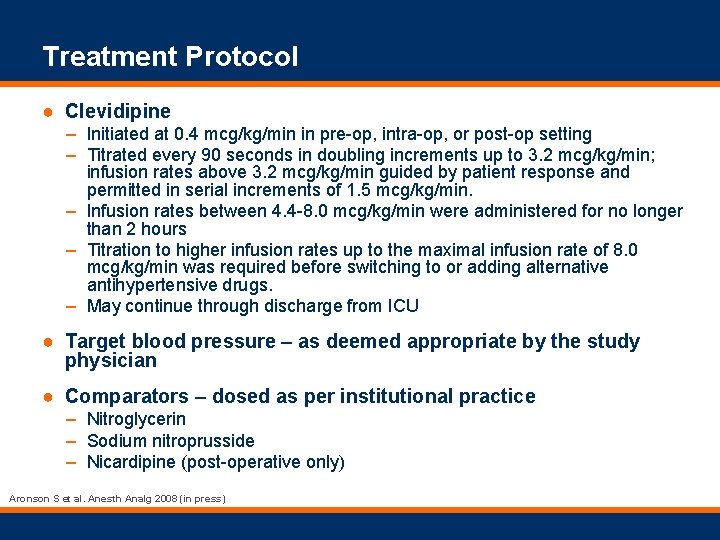
Treatment Protocol ● Clevidipine – Initiated at 0. 4 mcg/kg/min in pre-op, intra-op, or post-op setting – Titrated every 90 seconds in doubling increments up to 3. 2 mcg/kg/min; infusion rates above 3. 2 mcg/kg/min guided by patient response and permitted in serial increments of 1. 5 mcg/kg/min. – Infusion rates between 4. 4 -8. 0 mcg/kg/min were administered for no longer than 2 hours – Titration to higher infusion rates up to the maximal infusion rate of 8. 0 mcg/kg/min was required before switching to or adding alternative antihypertensive drugs. – May continue through discharge from ICU ● Target blood pressure – as deemed appropriate by the study physician ● Comparators – dosed as per institutional practice – Nitroglycerin – Sodium nitroprusside – Nicardipine (post-operative only) Aronson S et al. Anesth Analg 2008 (in press)
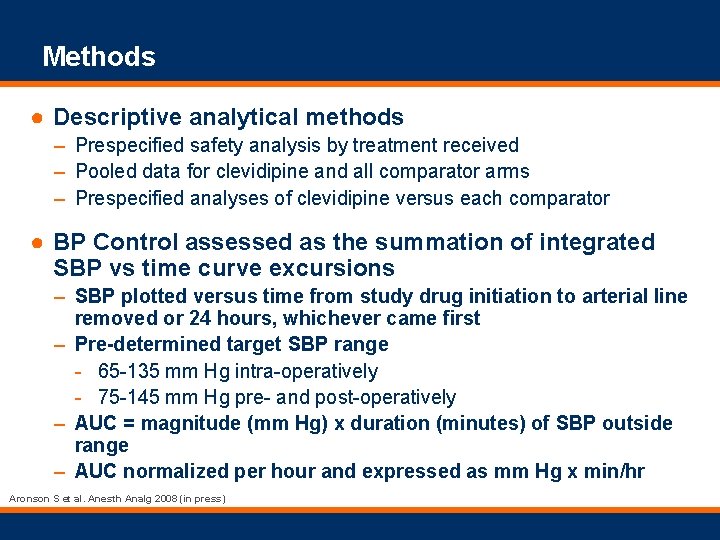
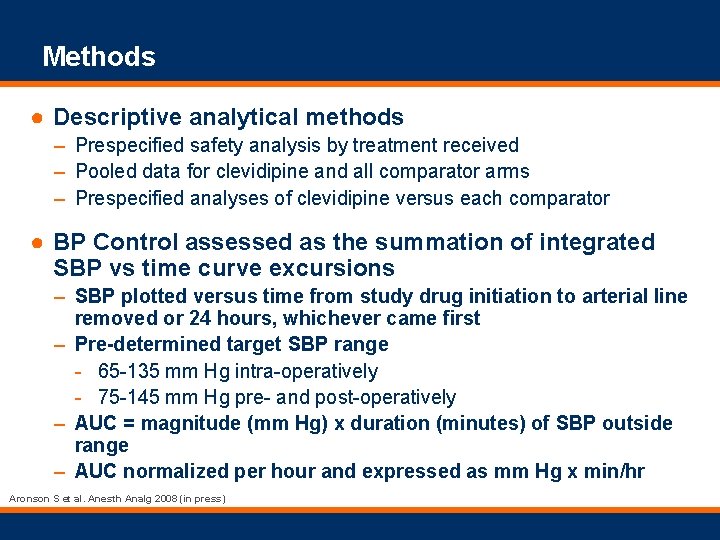
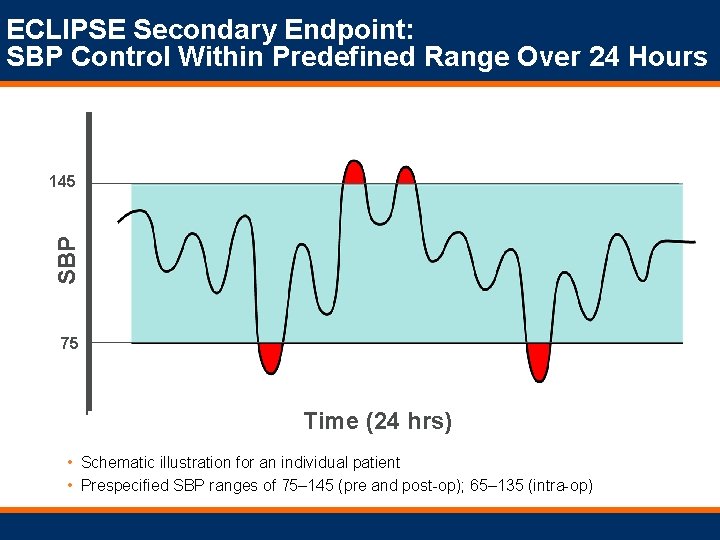
Methods ● Descriptive analytical methods – Prespecified safety analysis by treatment received – Pooled data for clevidipine and all comparator arms – Prespecified analyses of clevidipine versus each comparator ● BP Control assessed as the summation of integrated SBP vs time curve excursions – SBP plotted versus time from study drug initiation to arterial line removed or 24 hours, whichever came first – Pre-determined target SBP range - 65 -135 mm Hg intra-operatively - 75 -145 mm Hg pre- and post-operatively – AUC = magnitude (mm Hg) x duration (minutes) of SBP outside range – AUC normalized per hour and expressed as mm Hg x min/hr Aronson S et al. Anesth Analg 2008 (in press)
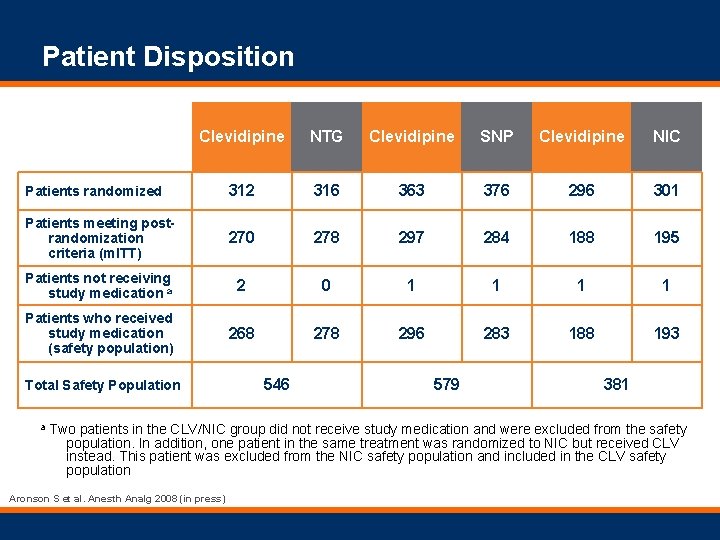
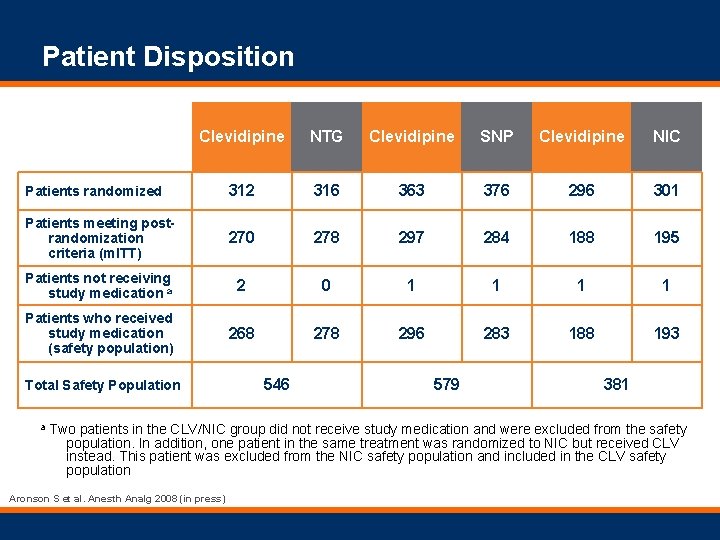
Patient Disposition Clevidipine NTG Clevidipine SNP Clevidipine NIC Patients randomized 312 316 363 376 296 301 Patients meeting postrandomization criteria (m. ITT) 270 278 297 284 188 195 Patients not receiving study medication a 2 0 1 1 Patients who received study medication (safety population) 268 278 296 283 188 193 Total Safety Population 546 579 381 a Two patients in the CLV/NIC group did not receive study medication and were excluded from the safety population. In addition, one patient in the same treatment was randomized to NIC but received CLV instead. This patient was excluded from the NIC safety population and included in the CLV safety population Aronson S et al. Anesth Analg 2008 (in press)
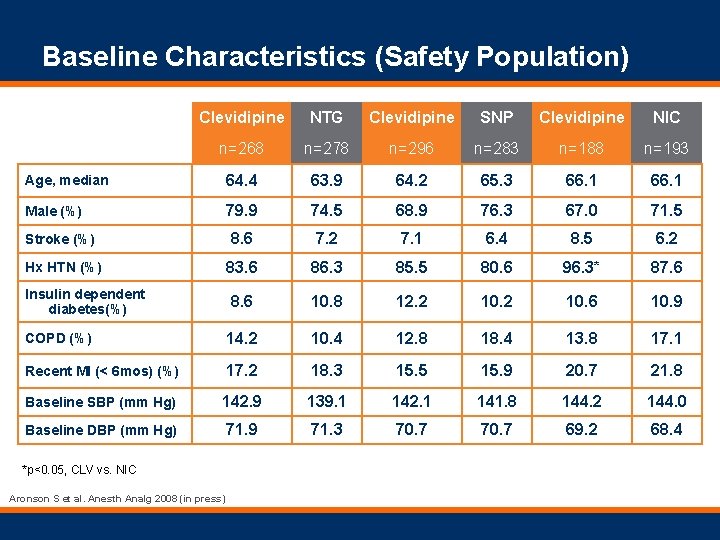
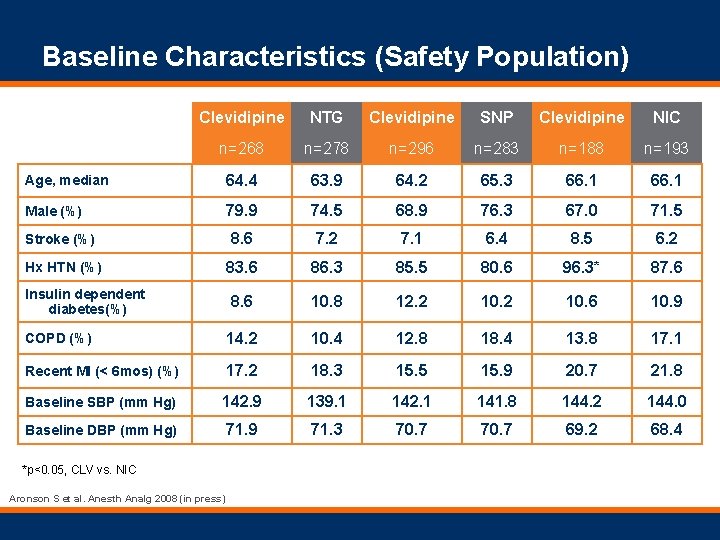
Baseline Characteristics (Safety Population) Clevidipine NTG Clevidipine SNP Clevidipine NIC n=268 n=278 n=296 n=283 n=188 n=193 Age, median 64. 4 63. 9 64. 2 65. 3 66. 1 Male (%) 79. 9 74. 5 68. 9 76. 3 67. 0 71. 5 Stroke (%) 8. 6 7. 2 7. 1 6. 4 8. 5 6. 2 Hx HTN (%) 83. 6 86. 3 85. 5 80. 6 96. 3* 87. 6 8. 6 10. 8 12. 2 10. 6 10. 9 COPD (%) 14. 2 10. 4 12. 8 18. 4 13. 8 17. 1 Recent MI (< 6 mos) (%) 17. 2 18. 3 15. 5 15. 9 20. 7 21. 8 Baseline SBP (mm Hg) 142. 9 139. 1 142. 1 141. 8 144. 2 144. 0 Baseline DBP (mm Hg) 71. 9 71. 3 70. 7 69. 2 68. 4 Insulin dependent diabetes(%) *p<0. 05, CLV vs. NIC Aronson S et al. Anesth Analg 2008 (in press)
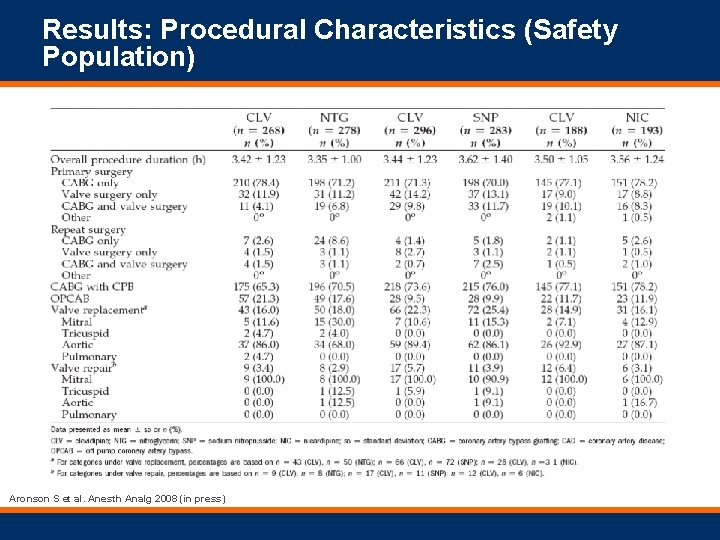
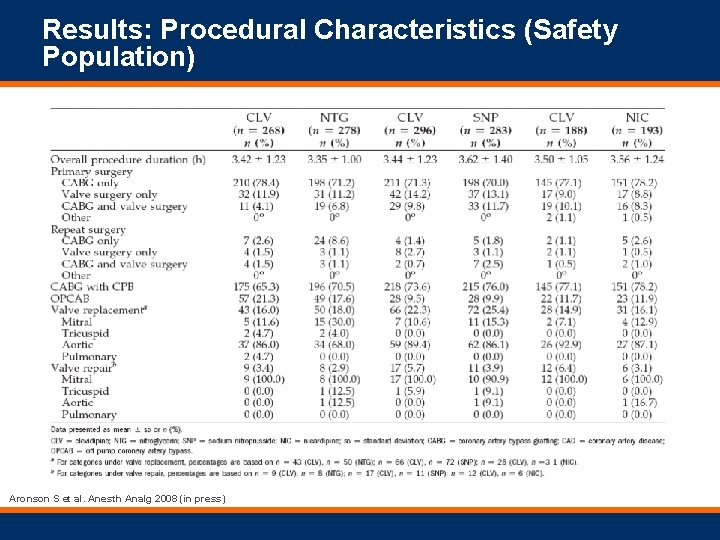
Results: Procedural Characteristics (Safety Population) Aronson S et al. Anesth Analg 2008 (in press)
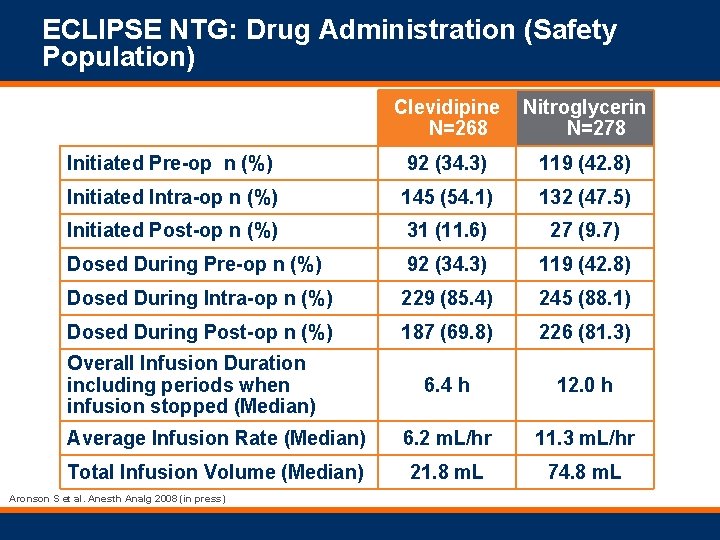
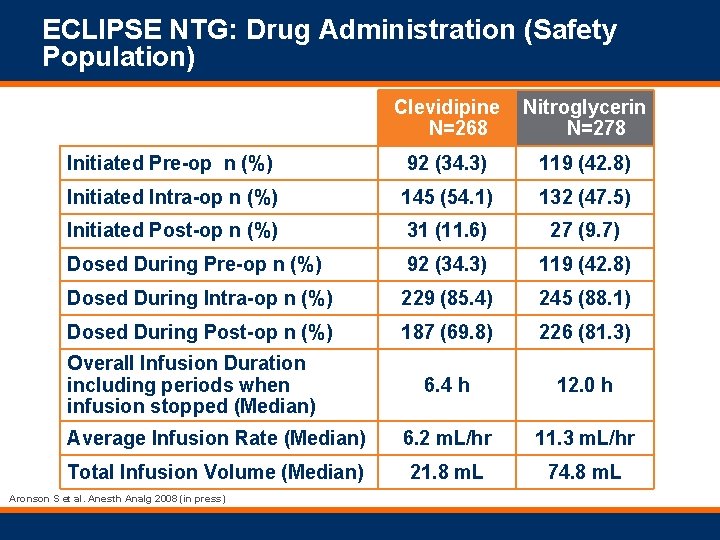
ECLIPSE NTG: Drug Administration (Safety Population) Clevidipine N=268 Nitroglycerin N=278 Initiated Pre-op n (%) 92 (34. 3) 119 (42. 8) Initiated Intra-op n (%) 145 (54. 1) 132 (47. 5) Initiated Post-op n (%) 31 (11. 6) 27 (9. 7) Dosed During Pre-op n (%) 92 (34. 3) 119 (42. 8) Dosed During Intra-op n (%) 229 (85. 4) 245 (88. 1) Dosed During Post-op n (%) 187 (69. 8) 226 (81. 3) 6. 4 h 12. 0 h Average Infusion Rate (Median) 6. 2 m. L/hr 11. 3 m. L/hr Total Infusion Volume (Median) 21. 8 m. L 74. 8 m. L Overall Infusion Duration including periods when infusion stopped (Median) Aronson S et al. Anesth Analg 2008 (in press)
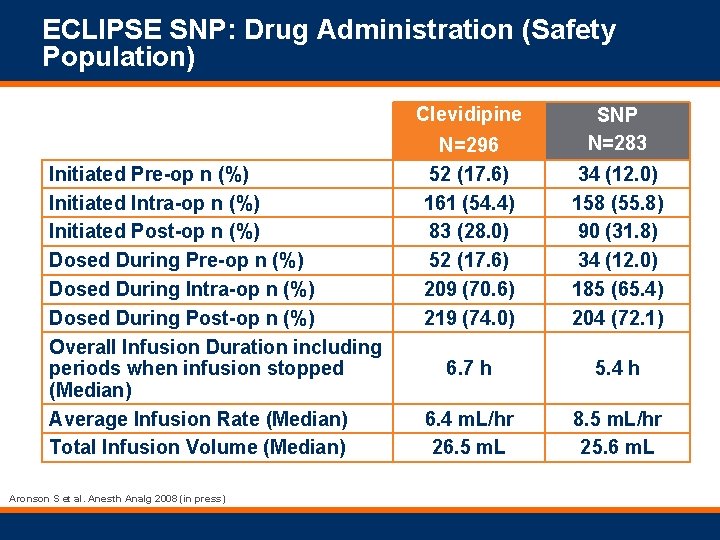
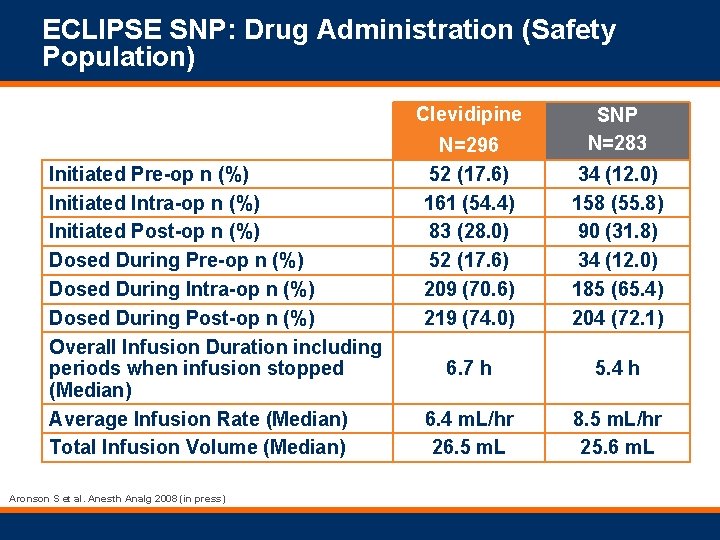
ECLIPSE SNP: Drug Administration (Safety Population) Clevidipine Initiated Pre-op n (%) Initiated Intra-op n (%) Initiated Post-op n (%) Dosed During Pre-op n (%) Dosed During Intra-op n (%) Dosed During Post-op n (%) Overall Infusion Duration including periods when infusion stopped (Median) Average Infusion Rate (Median) Total Infusion Volume (Median) Aronson S et al. Anesth Analg 2008 (in press) SNP N=283 N=296 52 (17. 6) 161 (54. 4) 83 (28. 0) 52 (17. 6) 209 (70. 6) 219 (74. 0) 34 (12. 0) 158 (55. 8) 90 (31. 8) 34 (12. 0) 185 (65. 4) 204 (72. 1) 6. 7 h 5. 4 h 6. 4 m. L/hr 26. 5 m. L 8. 5 m. L/hr 25. 6 m. L
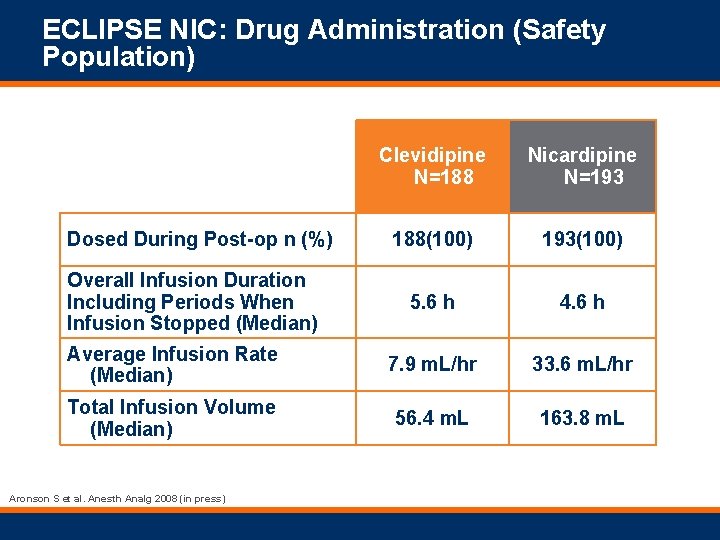
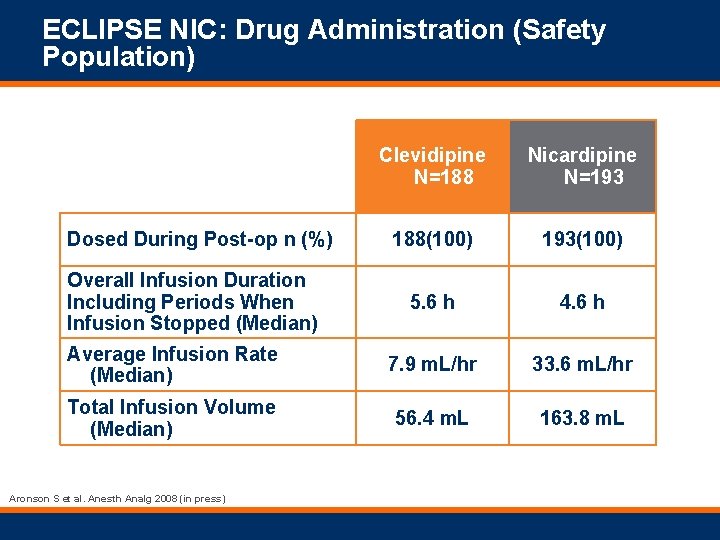
ECLIPSE NIC: Drug Administration (Safety Population) Clevidipine N=188 Nicardipine N=193 188(100) 193(100) 5. 6 h 4. 6 h Average Infusion Rate (Median) 7. 9 m. L/hr 33. 6 m. L/hr Total Infusion Volume (Median) 56. 4 m. L 163. 8 m. L Dosed During Post-op n (%) Overall Infusion Duration Including Periods When Infusion Stopped (Median) Aronson S et al. Anesth Analg 2008 (in press)
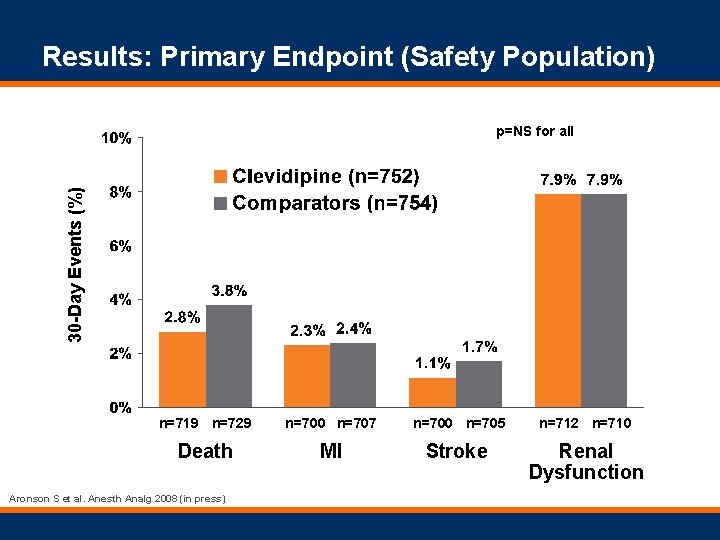
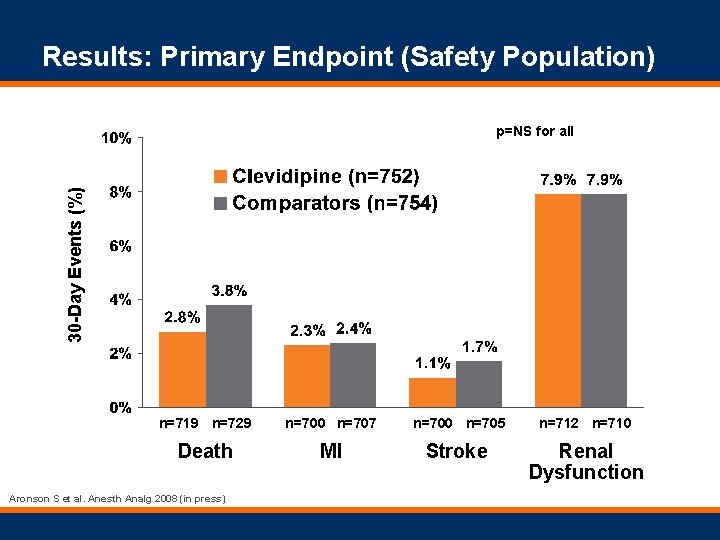
Results: Primary Endpoint (Safety Population) 30 -Day Events (%) p=NS for all n=719 n=729 n=700 n=707 n=700 n=705 n=712 n=710 Death MI Stroke Renal Dysfunction Aronson S et al. Anesth Analg 2008 (in press)
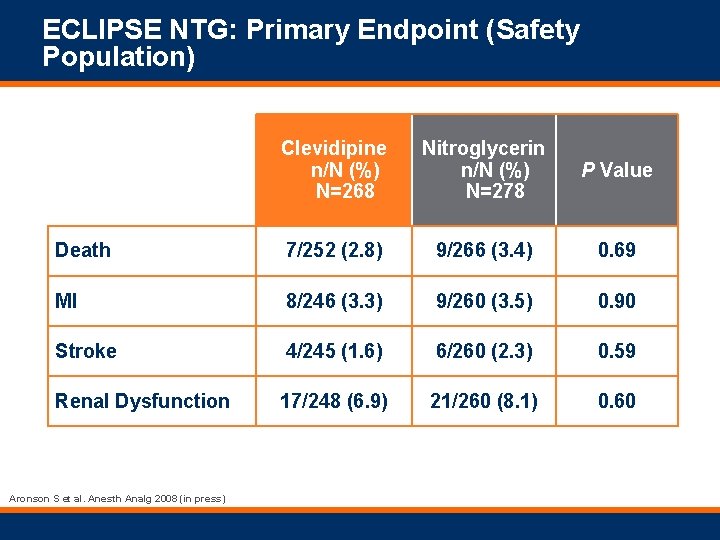
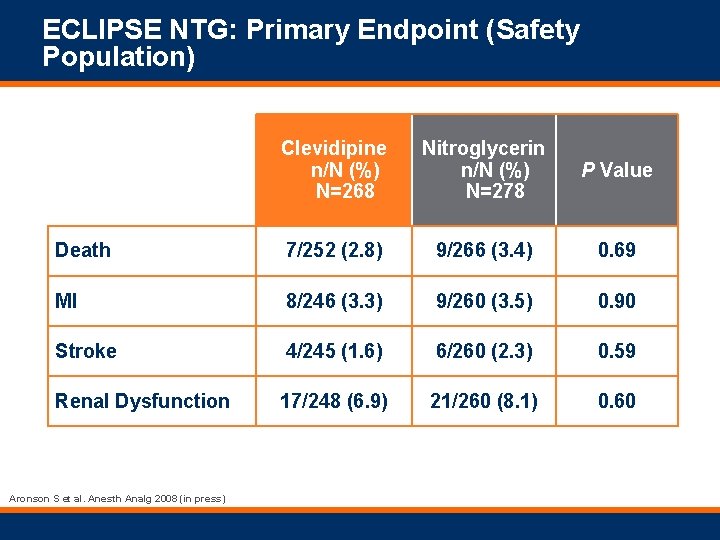
ECLIPSE NTG: Primary Endpoint (Safety Population) Clevidipine n/N (%) N=268 Nitroglycerin n/N (%) N=278 P Value Death 7/252 (2. 8) 9/266 (3. 4) 0. 69 MI 8/246 (3. 3) 9/260 (3. 5) 0. 90 Stroke 4/245 (1. 6) 6/260 (2. 3) 0. 59 Renal Dysfunction 17/248 (6. 9) 21/260 (8. 1) 0. 60 Aronson S et al. Anesth Analg 2008 (in press)
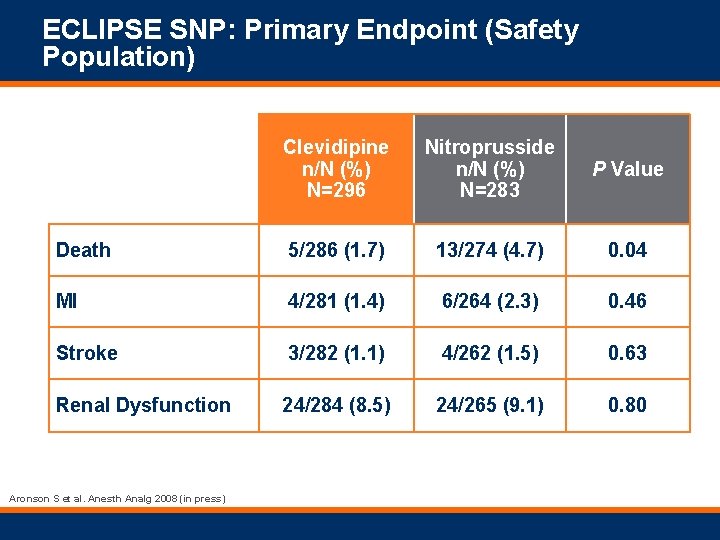
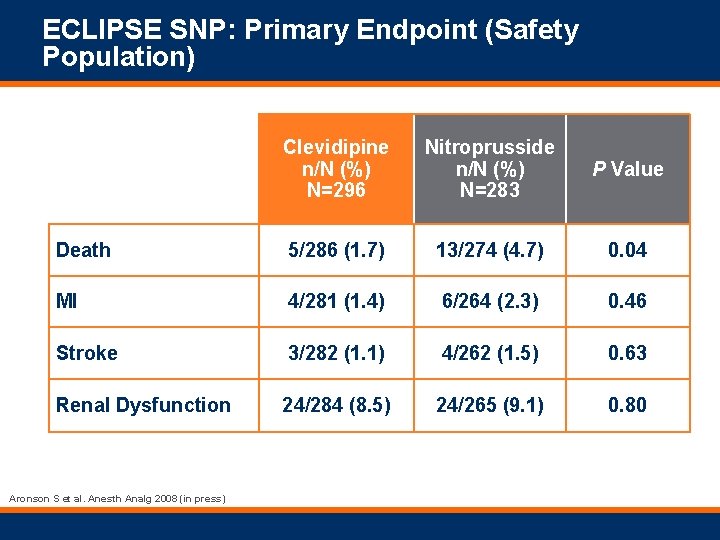
ECLIPSE SNP: Primary Endpoint (Safety Population) Clevidipine n/N (%) N=296 Nitroprusside n/N (%) N=283 P Value Death 5/286 (1. 7) 13/274 (4. 7) 0. 04 MI 4/281 (1. 4) 6/264 (2. 3) 0. 46 Stroke 3/282 (1. 1) 4/262 (1. 5) 0. 63 Renal Dysfunction 24/284 (8. 5) 24/265 (9. 1) 0. 80 Aronson S et al. Anesth Analg 2008 (in press)
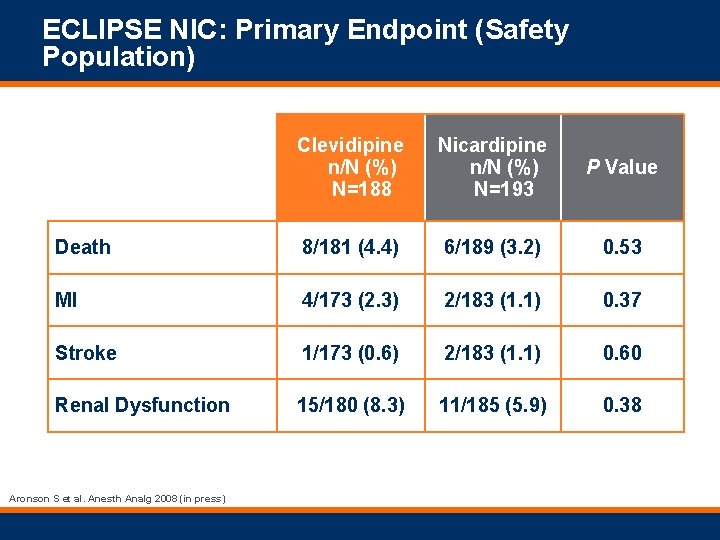
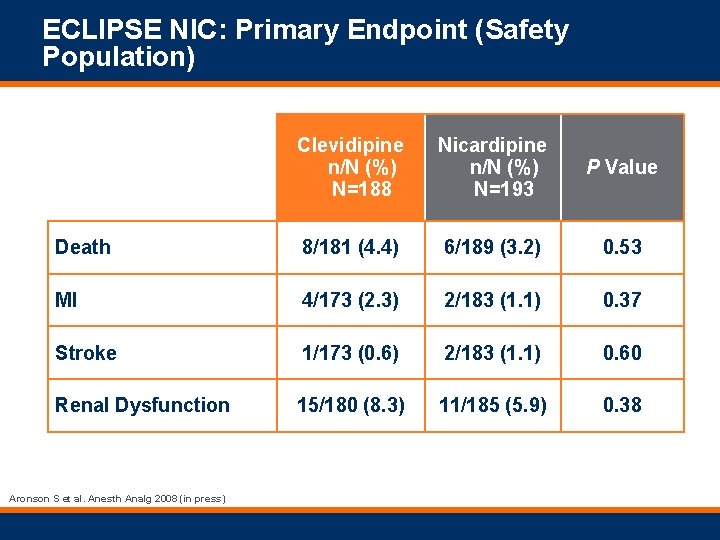
ECLIPSE NIC: Primary Endpoint (Safety Population) Clevidipine n/N (%) N=188 Nicardipine n/N (%) N=193 P Value Death 8/181 (4. 4) 6/189 (3. 2) 0. 53 MI 4/173 (2. 3) 2/183 (1. 1) 0. 37 Stroke 1/173 (0. 6) 2/183 (1. 1) 0. 60 Renal Dysfunction 15/180 (8. 3) 11/185 (5. 9) 0. 38 Aronson S et al. Anesth Analg 2008 (in press)
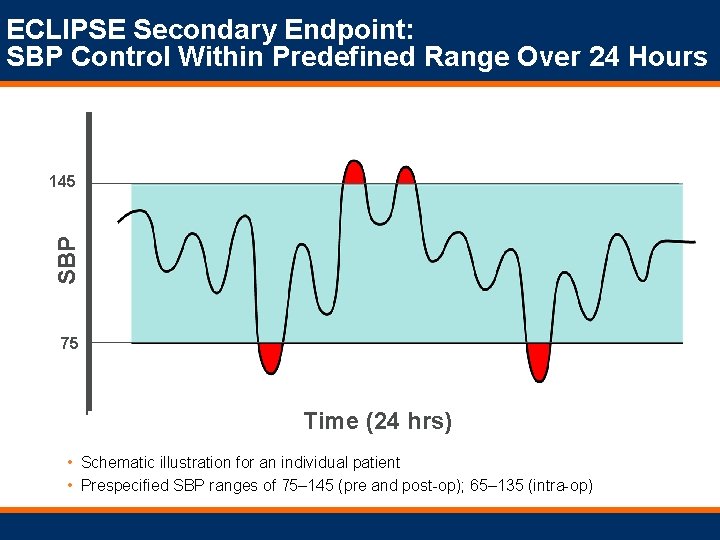
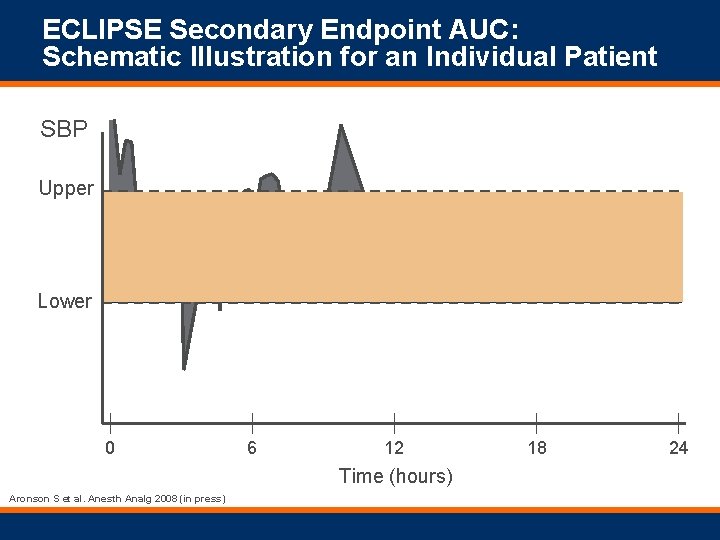
ECLIPSE Secondary Endpoint: SBP Control Within Predefined Range Over 24 Hours SBP 145 75 Time (24 hrs) • Schematic illustration for an individual patient • Prespecified SBP ranges of 75– 145 (pre and post-op); 65– 135 (intra-op)
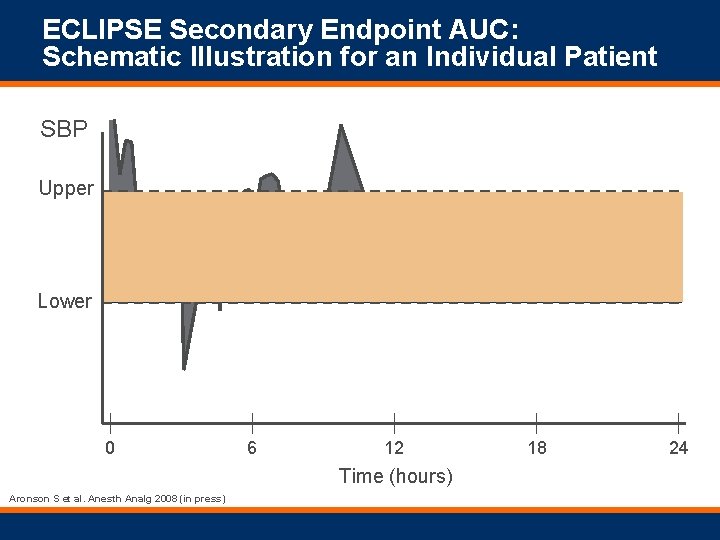
ECLIPSE Secondary Endpoint AUC: Schematic Illustration for an Individual Patient SBP Upper Lower 0 6 12 Time (hours) Aronson S et al. Anesth Analg 2008 (in press) 18 24
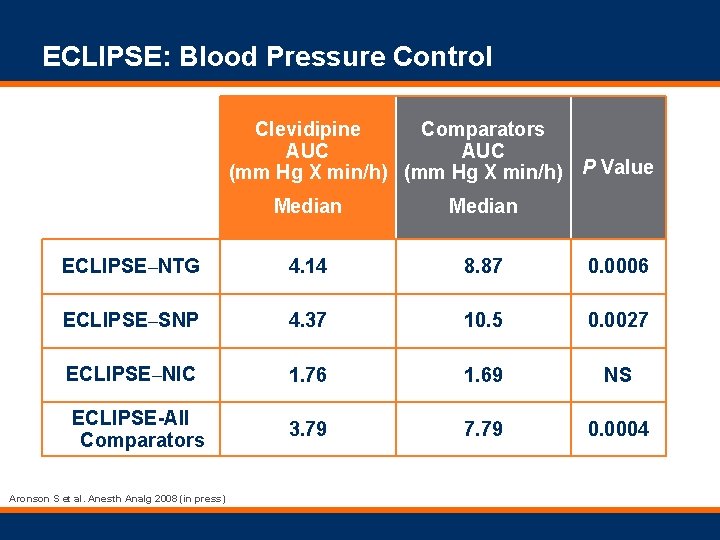
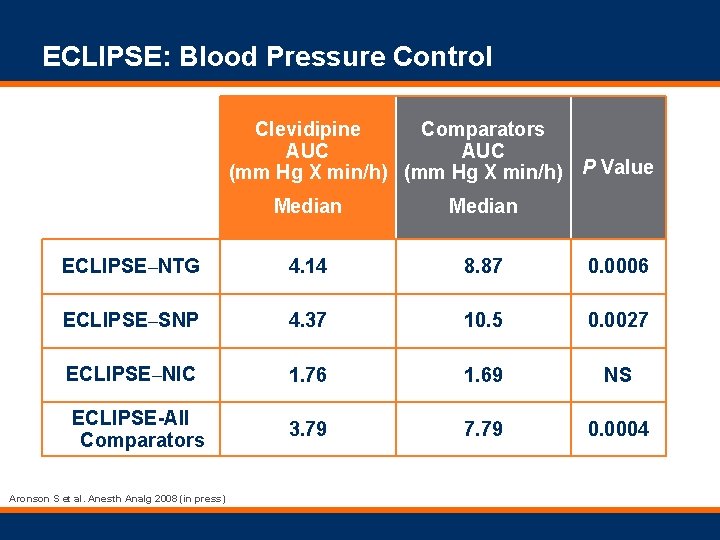
ECLIPSE: Blood Pressure Control Clevidipine Comparators AUC (mm Hg X min/h) P Value Median ECLIPSE–NTG 4. 14 8. 87 0. 0006 ECLIPSE–SNP 4. 37 10. 5 0. 0027 ECLIPSE–NIC 1. 76 1. 69 NS 3. 79 7. 79 0. 0004 ECLIPSE-All Comparators Aronson S et al. Anesth Analg 2008 (in press)
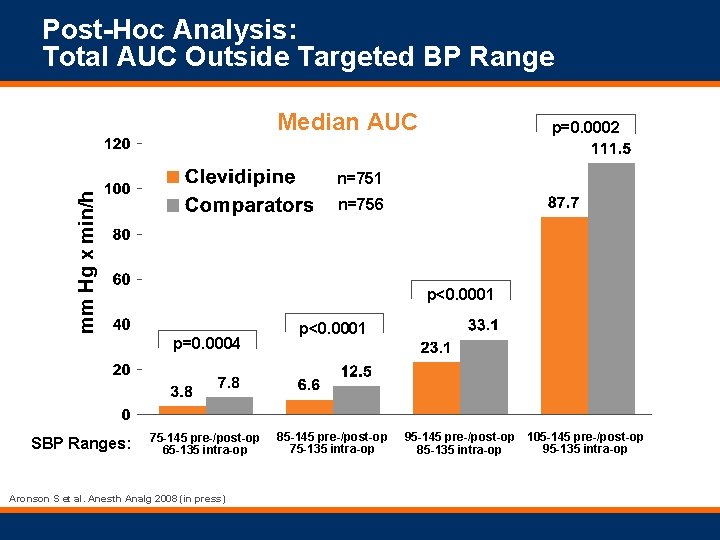
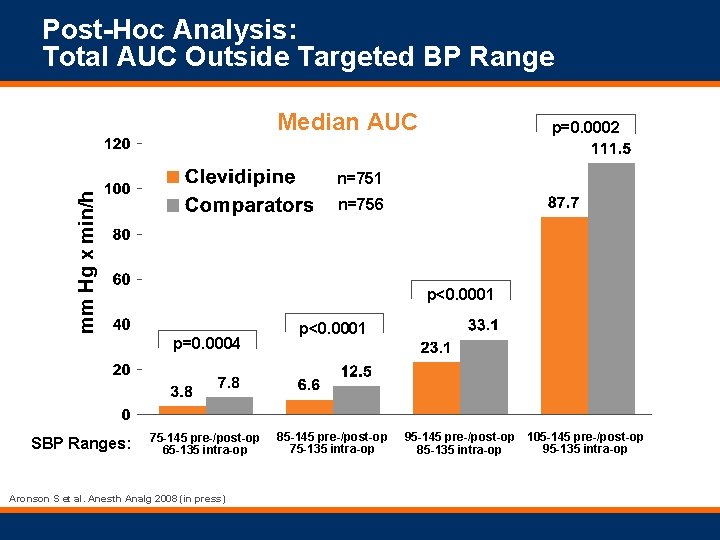
Post-Hoc Analysis: Total AUC Outside Targeted BP Range Median AUC p=0. 0002 mm Hg x min/h n=751 n=756 p<0. 0001 p=0. 0004 SBP Ranges: 75 -145 pre-/post-op 65 -135 intra-op Aronson S et al. Anesth Analg 2008 (in press) p<0. 0001 85 -145 pre-/post-op 75 -135 intra-op 95 -145 pre-/post-op 105 -145 pre-/post-op 95 -135 intra-op 85 -135 intra-op
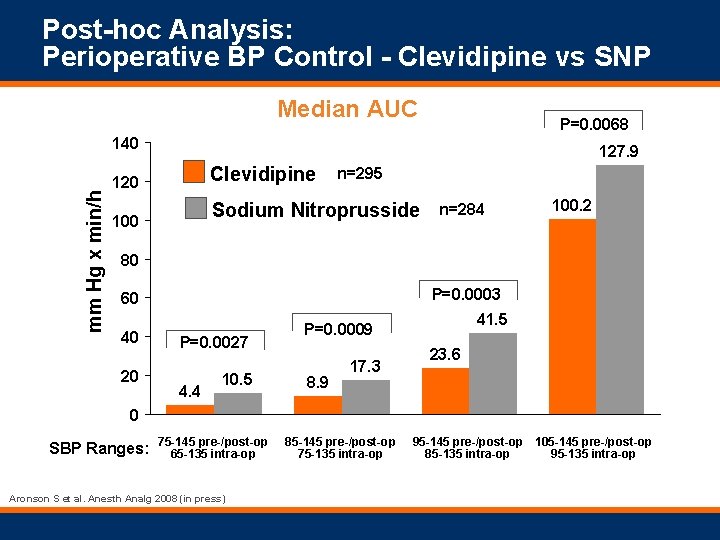
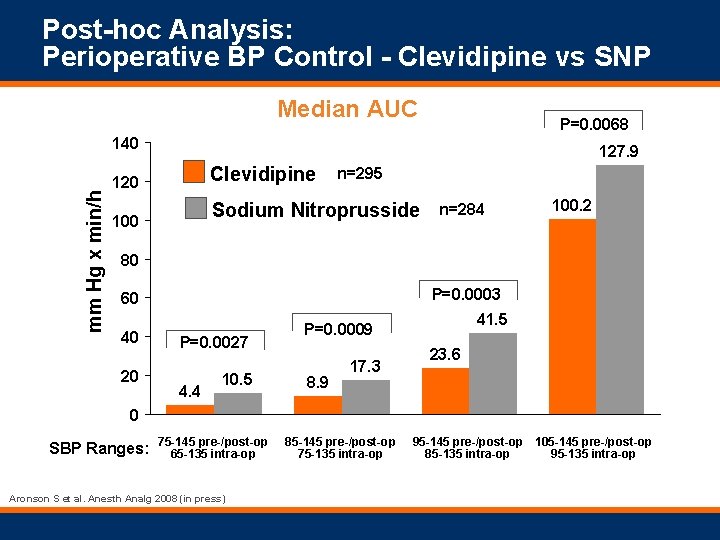
Post-hoc Analysis: Perioperative BP Control - Clevidipine vs SNP Median AUC P=0. 0068 mm Hg x min/h 140 127. 9 Clevidipine 120 n=295 Sodium Nitroprusside 100 n=284 100. 2 80 P=0. 0003 60 40 20 P=0. 0027 4. 4 10. 5 41. 5 P=0. 0009 8. 9 17. 3 23. 6 0 SBP Ranges: 75 -145 pre-/post-op 65 -135 intra-op Aronson S et al. Anesth Analg 2008 (in press) 85 -145 pre-/post-op 75 -135 intra-op 95 -145 pre-/post-op 105 -145 pre-/post-op 95 -135 intra-op 85 -135 intra-op

Post-hoc Analysis: Perioperative BP Control - Clevidipine vs NTG Median AUC mm Hg x min/h 120 P=0. 0556 108. 6 Clevidipine Nitroglycerin 100 n=269 n=278 83. 7 80 60 40 P=0. 0016 P=0. 0006 20 4. 1 8. 9 34. 2 P=0. 0002 23. 4 14. 9 6. 0 0 SBP Ranges: 75 -145 pre-/post-op 65 -135 intra-op Aronson S et al. Anesth Analg 2008 (in press) 85 -145 pre-/post-op 75 -135 intra-op 95 -145 pre-/post-op 105 -145 pre-/post-op 95 -135 intra-op 85 -135 intra-op
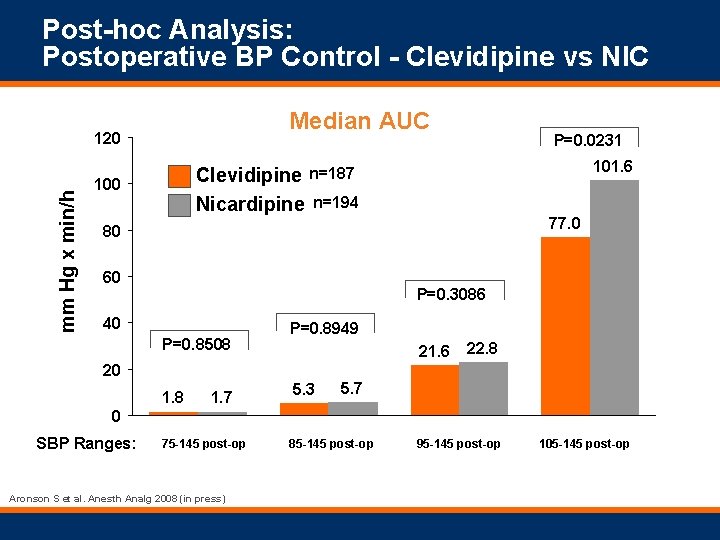
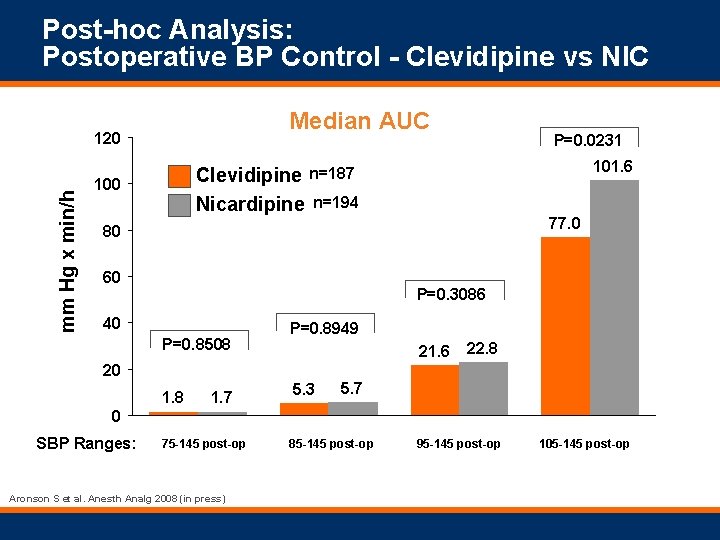
Post-hoc Analysis: Postoperative BP Control - Clevidipine vs NIC Median AUC mm Hg x min/h 120 P=0. 0231 101. 6 Clevidipine n=187 Nicardipine n=194 100 77. 0 80 60 P=0. 3086 40 P=0. 8508 P=0. 8949 21. 6 20 1. 8 1. 7 5. 3 22. 8 5. 7 0 SBP Ranges: 75 -145 post-op Aronson S et al. Anesth Analg 2008 (in press) 85 -145 post-op 95 -145 post-op 105 -145 post-op
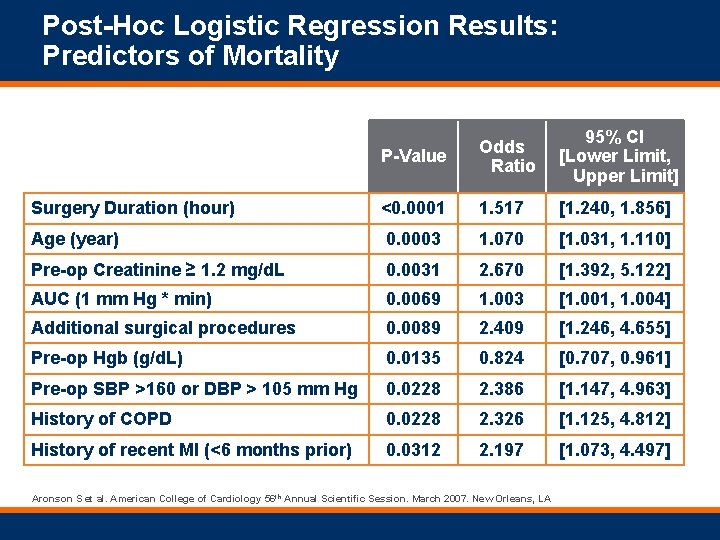
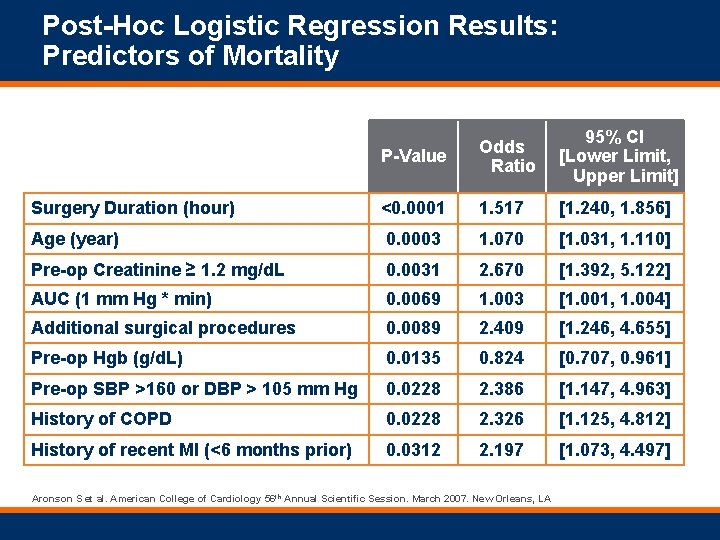
Post-Hoc Logistic Regression Results: Predictors of Mortality P-Value Odds Ratio 95% CI [Lower Limit, Upper Limit] Surgery Duration (hour) <0. 0001 1. 517 [1. 240, 1. 856] Age (year) 0. 0003 1. 070 [1. 031, 1. 110] Pre-op Creatinine ≥ 1. 2 mg/d. L 0. 0031 2. 670 [1. 392, 5. 122] AUC (1 mm Hg * min) 0. 0069 1. 003 [1. 001, 1. 004] Additional surgical procedures 0. 0089 2. 409 [1. 246, 4. 655] Pre-op Hgb (g/d. L) 0. 0135 0. 824 [0. 707, 0. 961] Pre-op SBP >160 or DBP > 105 mm Hg 0. 0228 2. 386 [1. 147, 4. 963] History of COPD 0. 0228 2. 326 [1. 125, 4. 812] History of recent MI (<6 months prior) 0. 0312 2. 197 [1. 073, 4. 497] Aronson S et al. American College of Cardiology 56 th Annual Scientific Session. March 2007. New Orleans, LA
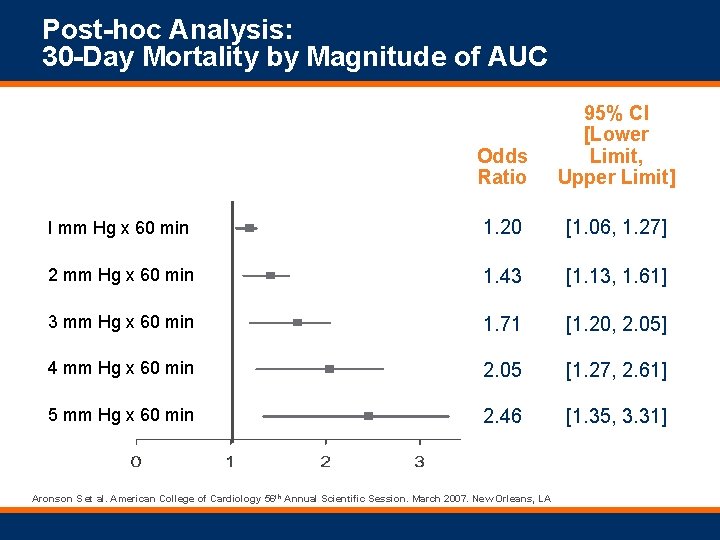
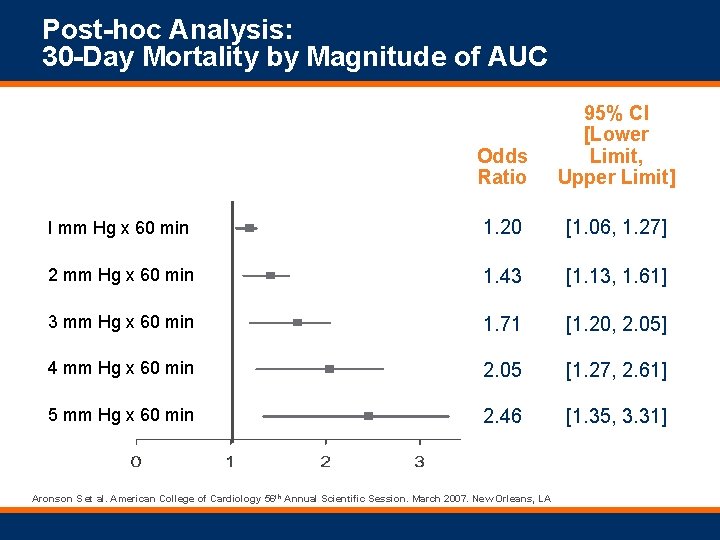
Post-hoc Analysis: 30 -Day Mortality by Magnitude of AUC Odds Ratio 95% CI [Lower Limit, Upper Limit] I mm Hg x 60 min 1. 20 [1. 06, 1. 27] 2 mm Hg x 60 min 1. 43 [1. 13, 1. 61] 3 mm Hg x 60 min 1. 71 [1. 20, 2. 05] 4 mm Hg x 60 min 2. 05 [1. 27, 2. 61] 5 mm Hg x 60 min 2. 46 [1. 35, 3. 31] Aronson S et al. American College of Cardiology 56 th Annual Scientific Session. March 2007. New Orleans, LA
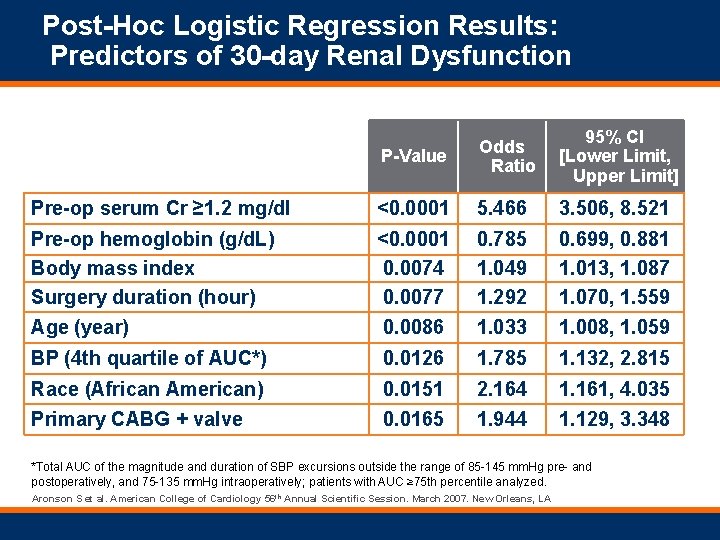
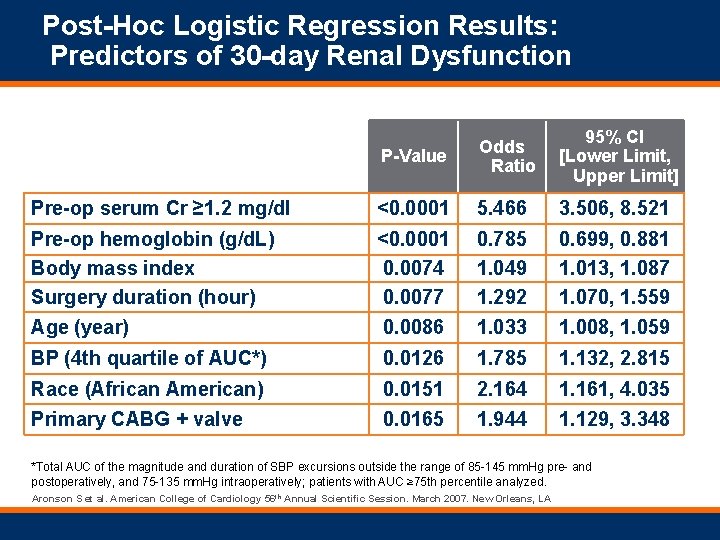
Post-Hoc Logistic Regression Results: Predictors of 30 -day Renal Dysfunction P-Value Odds Ratio 95% CI [Lower Limit, Upper Limit] Pre-op serum Cr ≥ 1. 2 mg/dl <0. 0001 5. 466 3. 506, 8. 521 Pre-op hemoglobin (g/d. L) Body mass index Surgery duration (hour) <0. 0001 0. 0074 0. 0077 0. 785 1. 049 1. 292 0. 699, 0. 881 1. 013, 1. 087 1. 070, 1. 559 Age (year) 0. 0086 1. 033 1. 008, 1. 059 BP (4 th quartile of AUC*) 0. 0126 1. 785 1. 132, 2. 815 Race (African American) 0. 0151 2. 164 1. 161, 4. 035 Primary CABG + valve 0. 0165 1. 944 1. 129, 3. 348 *Total AUC of the magnitude and duration of SBP excursions outside the range of 85 -145 mm. Hg pre- and postoperatively, and 75 -135 mm. Hg intraoperatively; patients with AUC ≥ 75 th percentile analyzed. Aronson S et al. American College of Cardiology 56 th Annual Scientific Session. March 2007. New Orleans, LA
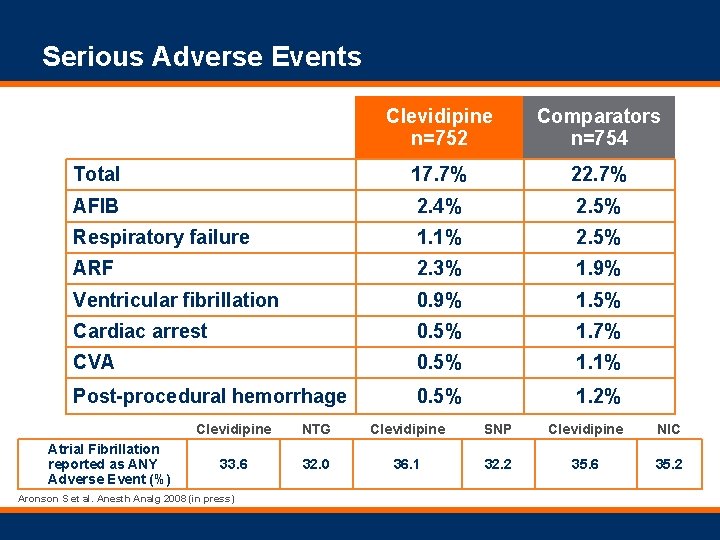
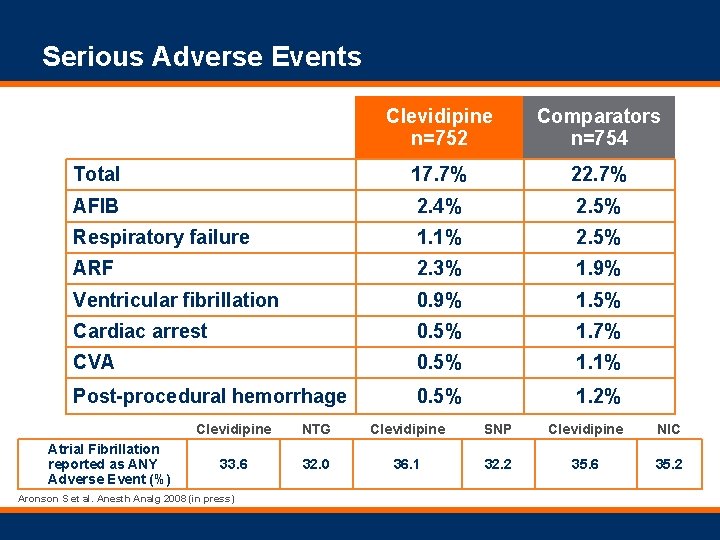
Serious Adverse Events Clevidipine n=752 Comparators n=754 Total 17. 7% 22. 7% AFIB 2. 4% 2. 5% Respiratory failure 1. 1% 2. 5% ARF 2. 3% 1. 9% Ventricular fibrillation 0. 9% 1. 5% Cardiac arrest 0. 5% 1. 7% CVA 0. 5% 1. 1% Post-procedural hemorrhage 0. 5% 1. 2% Atrial Fibrillation reported as ANY Adverse Event (%) Clevidipine NTG Clevidipine SNP Clevidipine NIC 33. 6 32. 0 36. 1 32. 2 35. 6 35. 2 Aronson S et al. Anesth Analg 2008 (in press)
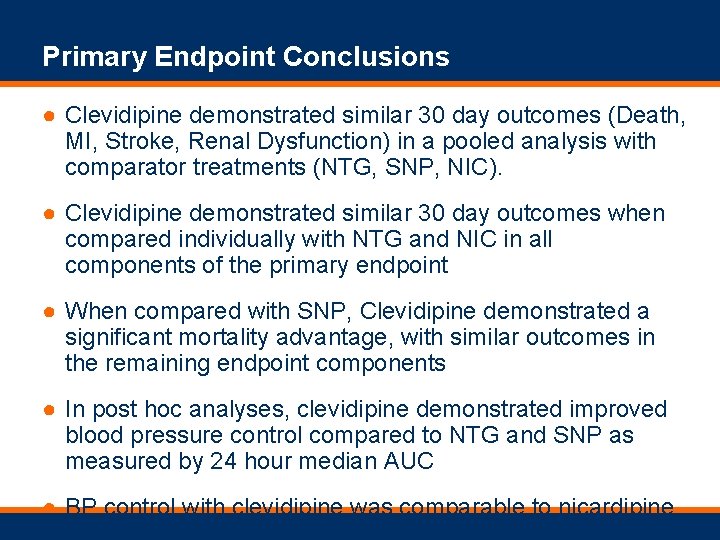
Primary Endpoint Conclusions ● Clevidipine demonstrated similar 30 day outcomes (Death, MI, Stroke, Renal Dysfunction) in a pooled analysis with comparator treatments (NTG, SNP, NIC). ● Clevidipine demonstrated similar 30 day outcomes when compared individually with NTG and NIC in all components of the primary endpoint ● When compared with SNP, Clevidipine demonstrated a significant mortality advantage, with similar outcomes in the remaining endpoint components ● In post hoc analyses, clevidipine demonstrated improved blood pressure control compared to NTG and SNP as measured by 24 hour median AUC ● BP control with clevidipine was comparable to nicardipine
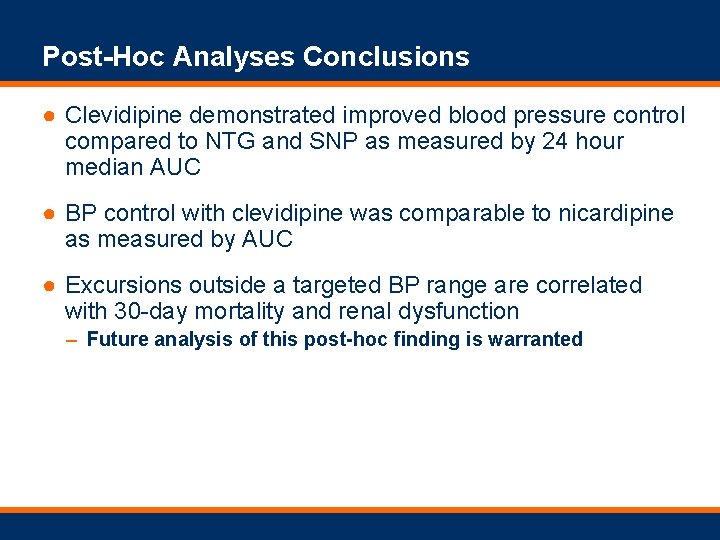
Post-Hoc Analyses Conclusions ● Clevidipine demonstrated improved blood pressure control compared to NTG and SNP as measured by 24 hour median AUC ● BP control with clevidipine was comparable to nicardipine as measured by AUC ● Excursions outside a targeted BP range are correlated with 30 -day mortality and renal dysfunction – Future analysis of this post-hoc finding is warranted
Annals of Emergency Medicine - 06 June 2008 (10. 1016/j. annemergmed. 2008. 04. 025)
VELOCITY: Rationale Common Hypertensive Emergencies 1, 2 ● Acute coronary syndromes ● Heart failure, pulmonary edema ● Acute cerebrovascular syndromes (Stroke) – subarachnoid hemorrhage – cerebral bleeding – cerebral infarction ● Hypertensive encephalopathy and retinopathy ● Renal Crisis 1. Varon J, Marik PE. Chest. 2000; 118: 214 -227. 2. Mansoor GA, Frishman WH. Heart Dis. 2002; 4: 358 -371.
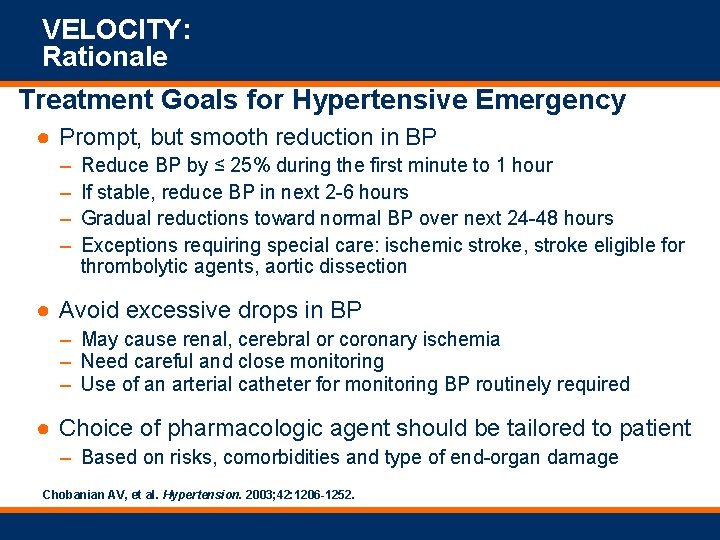
VELOCITY: Rationale Treatment Goals for Hypertensive Emergency ● Prompt, but smooth reduction in BP – – Reduce BP by ≤ 25% during the first minute to 1 hour If stable, reduce BP in next 2 -6 hours Gradual reductions toward normal BP over next 24 -48 hours Exceptions requiring special care: ischemic stroke, stroke eligible for thrombolytic agents, aortic dissection ● Avoid excessive drops in BP – May cause renal, cerebral or coronary ischemia – Need careful and close monitoring – Use of an arterial catheter for monitoring BP routinely required ● Choice of pharmacologic agent should be tailored to patient – Based on risks, comorbidities and type of end-organ damage Chobanian AV, et al. Hypertension. 2003; 42: 1206 -1252.
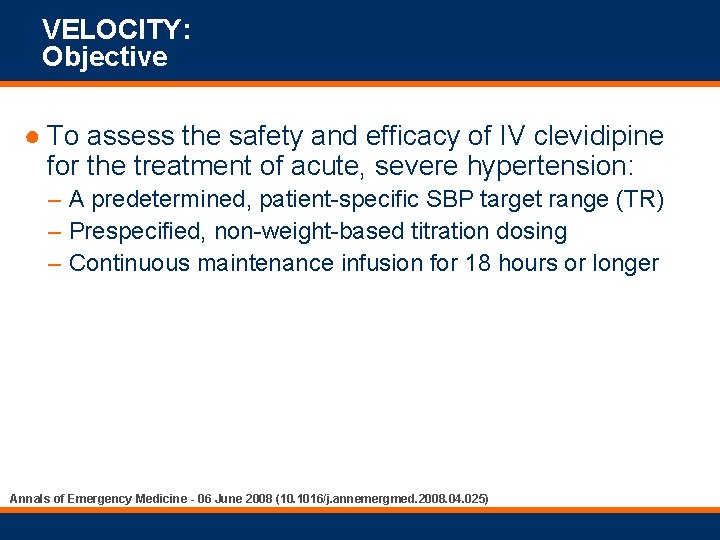
VELOCITY: Objective ● To assess the safety and efficacy of IV clevidipine for the treatment of acute, severe hypertension: – A predetermined, patient-specific SBP target range (TR) – Prespecified, non-weight-based titration dosing – Continuous maintenance infusion for 18 hours or longer Annals of Emergency Medicine - 06 June 2008 (10. 1016/j. annemergmed. 2008. 04. 025)
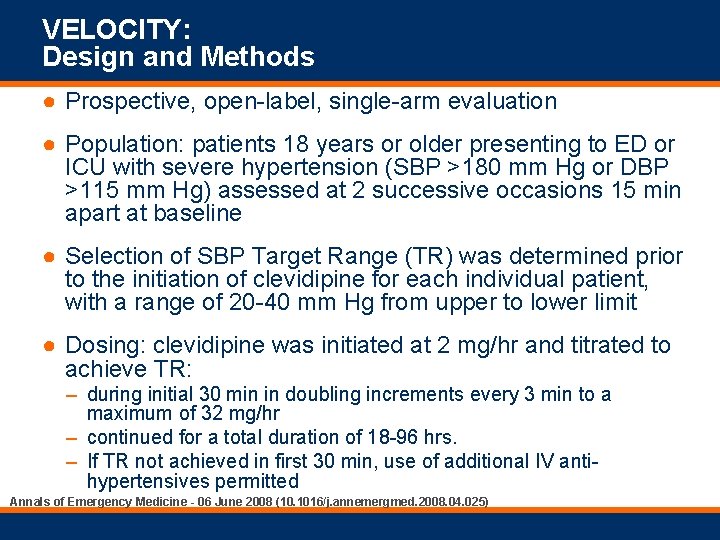
VELOCITY: Design and Methods ● Prospective, open-label, single-arm evaluation ● Population: patients 18 years or older presenting to ED or ICU with severe hypertension (SBP >180 mm Hg or DBP >115 mm Hg) assessed at 2 successive occasions 15 min apart at baseline ● Selection of SBP Target Range (TR) was determined prior to the initiation of clevidipine for each individual patient, with a range of 20 -40 mm Hg from upper to lower limit ● Dosing: clevidipine was initiated at 2 mg/hr and titrated to achieve TR: – during initial 30 min in doubling increments every 3 min to a maximum of 32 mg/hr – continued for a total duration of 18 -96 hrs. – If TR not achieved in first 30 min, use of additional IV antihypertensives permitted Annals of Emergency Medicine - 06 June 2008 (10. 1016/j. annemergmed. 2008. 04. 025)
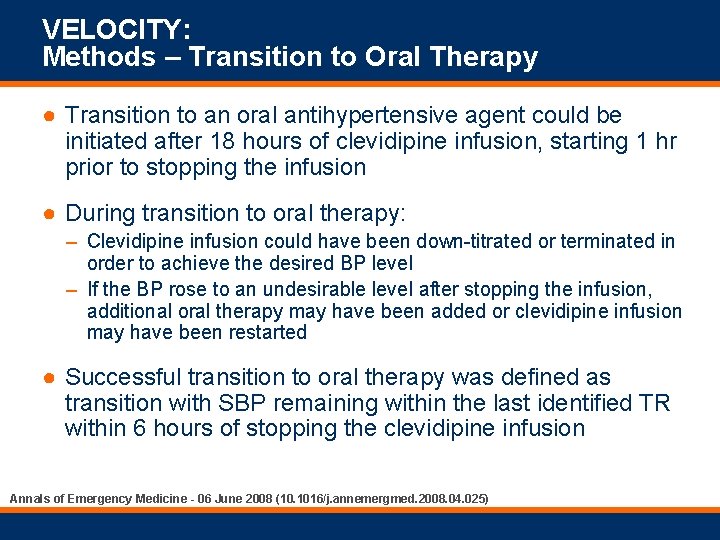
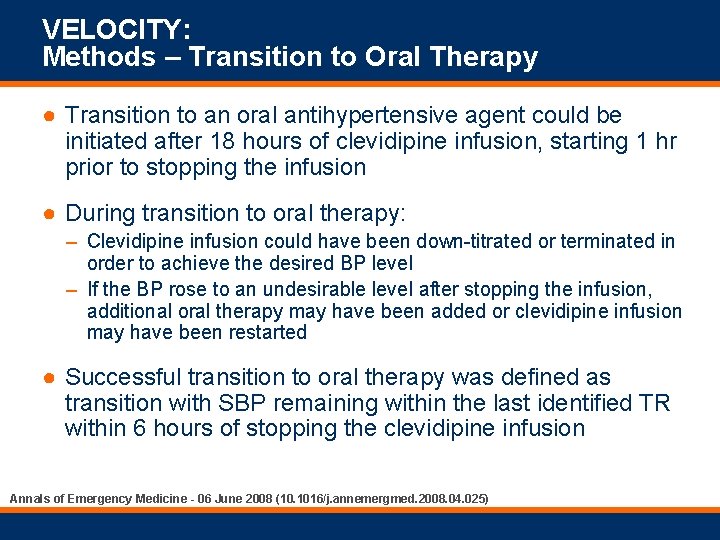
VELOCITY: Methods – Transition to Oral Therapy ● Transition to an oral antihypertensive agent could be initiated after 18 hours of clevidipine infusion, starting 1 hr prior to stopping the infusion ● During transition to oral therapy: – Clevidipine infusion could have been down-titrated or terminated in order to achieve the desired BP level – If the BP rose to an undesirable level after stopping the infusion, additional oral therapy may have been added or clevidipine infusion may have been restarted ● Successful transition to oral therapy was defined as transition with SBP remaining within the last identified TR within 6 hours of stopping the clevidipine infusion Annals of Emergency Medicine - 06 June 2008 (10. 1016/j. annemergmed. 2008. 04. 025)
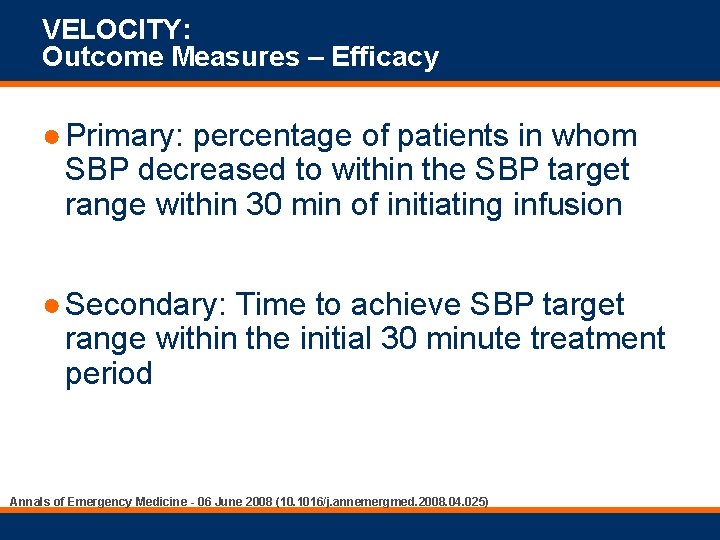
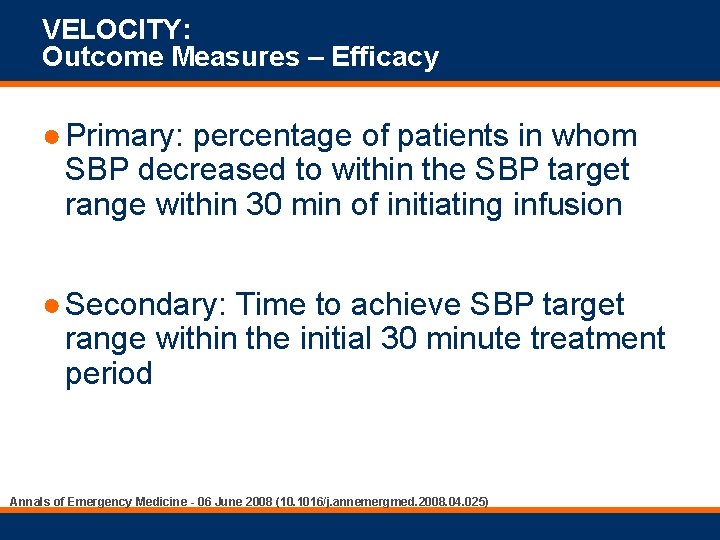
VELOCITY: Outcome Measures – Efficacy ● Primary: percentage of patients in whom SBP decreased to within the SBP target range within 30 min of initiating infusion ● Secondary: Time to achieve SBP target range within the initial 30 minute treatment period Annals of Emergency Medicine - 06 June 2008 (10. 1016/j. annemergmed. 2008. 04. 025)
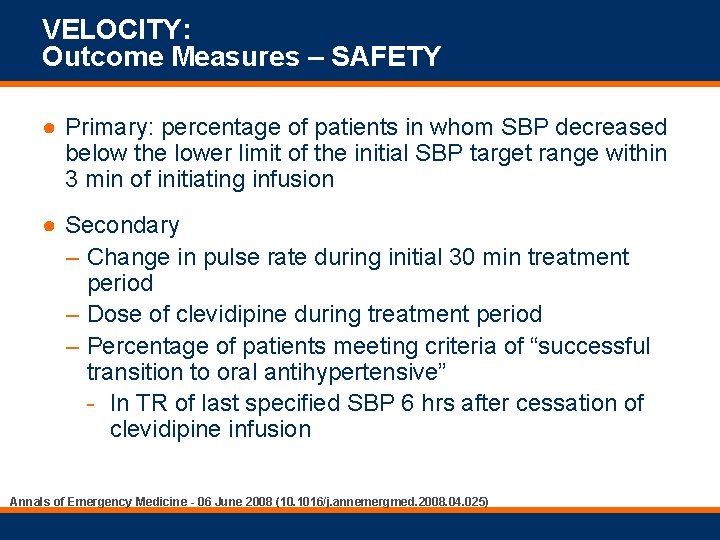
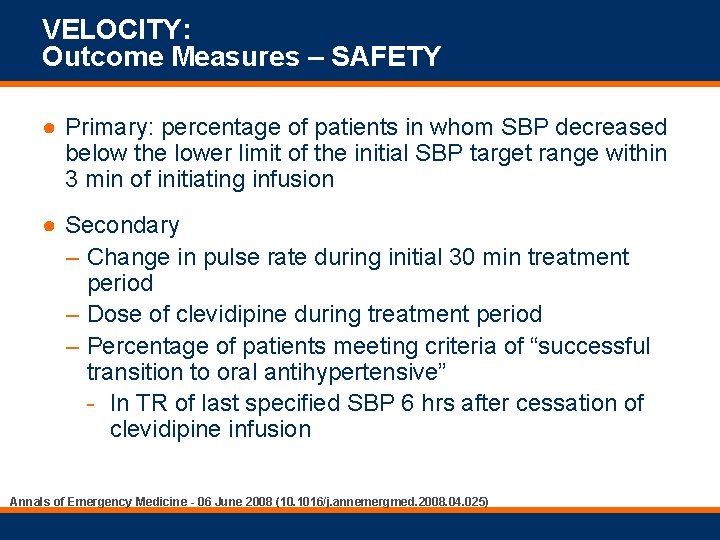
VELOCITY: Outcome Measures – SAFETY ● Primary: percentage of patients in whom SBP decreased below the lower limit of the initial SBP target range within 3 min of initiating infusion ● Secondary – Change in pulse rate during initial 30 min treatment period – Dose of clevidipine during treatment period – Percentage of patients meeting criteria of “successful transition to oral antihypertensive” - In TR of last specified SBP 6 hrs after cessation of clevidipine infusion Annals of Emergency Medicine - 06 June 2008 (10. 1016/j. annemergmed. 2008. 04. 025)
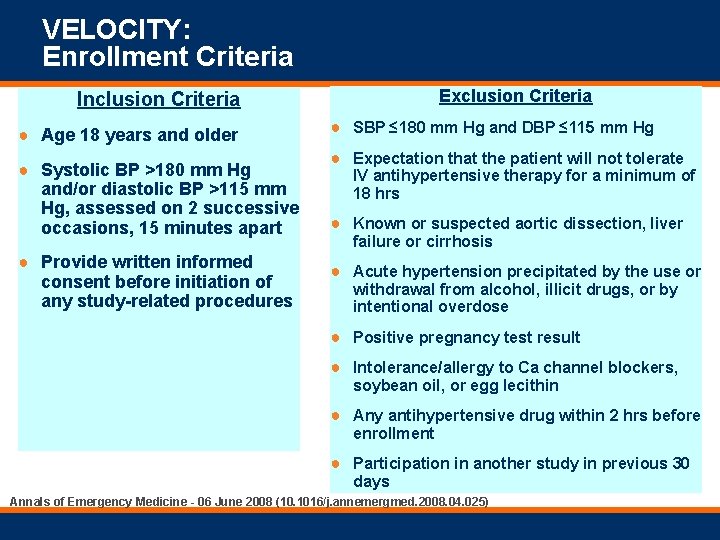
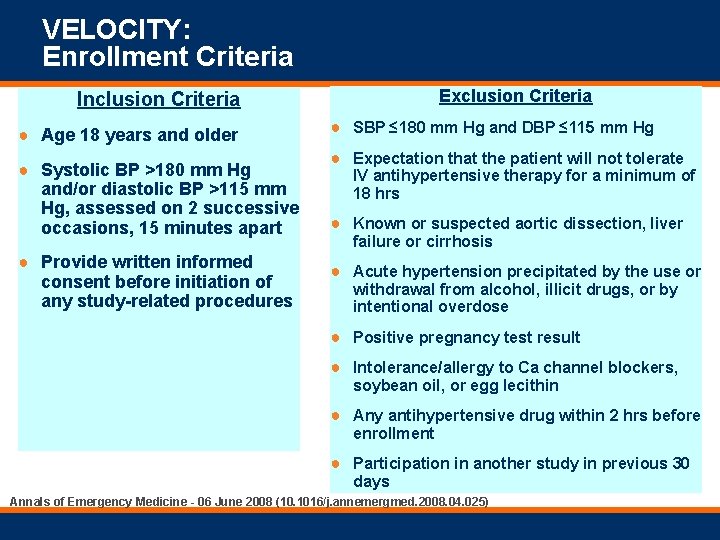
VELOCITY: Enrollment Criteria Exclusion Criteria Inclusion Criteria ● Age 18 years and older ● Systolic BP >180 mm Hg and/or diastolic BP >115 mm Hg, assessed on 2 successive occasions, 15 minutes apart ● Provide written informed consent before initiation of any study-related procedures ● SBP ≤ 180 mm Hg and DBP ≤ 115 mm Hg ● Expectation that the patient will not tolerate IV antihypertensive therapy for a minimum of 18 hrs ● Known or suspected aortic dissection, liver failure or cirrhosis ● Acute hypertension precipitated by the use or withdrawal from alcohol, illicit drugs, or by intentional overdose ● Positive pregnancy test result ● Intolerance/allergy to Ca channel blockers, soybean oil, or egg lecithin ● Any antihypertensive drug within 2 hrs before enrollment ● Participation in another study in previous 30 days Annals of Emergency Medicine - 06 June 2008 (10. 1016/j. annemergmed. 2008. 04. 025)
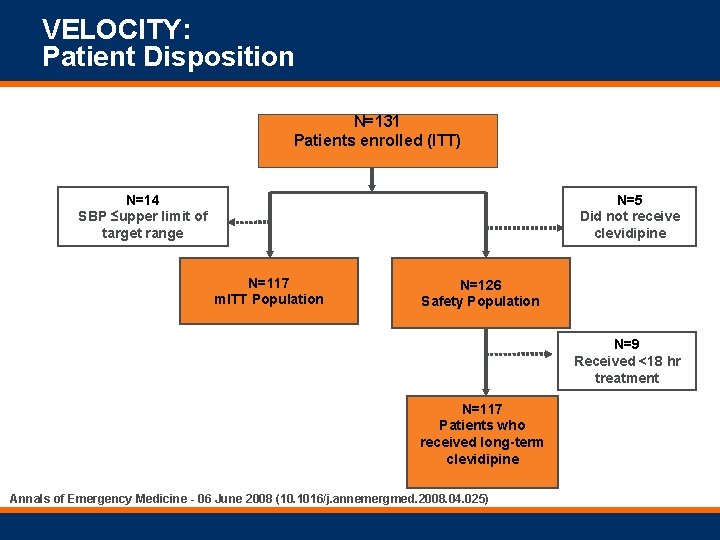
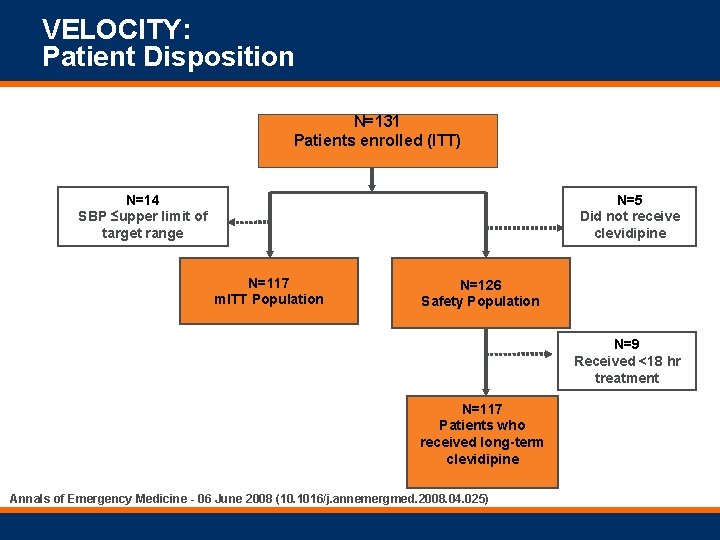
VELOCITY: Patient Disposition N=131 Patients enrolled (ITT) N=14 SBP ≤upper limit of target range N=5 Did not receive clevidipine N=117 m. ITT Population N=126 Safety Population N=9 Received <18 hr treatment N=117 Patients who received long-term clevidipine Annals of Emergency Medicine - 06 June 2008 (10. 1016/j. annemergmed. 2008. 04. 025)
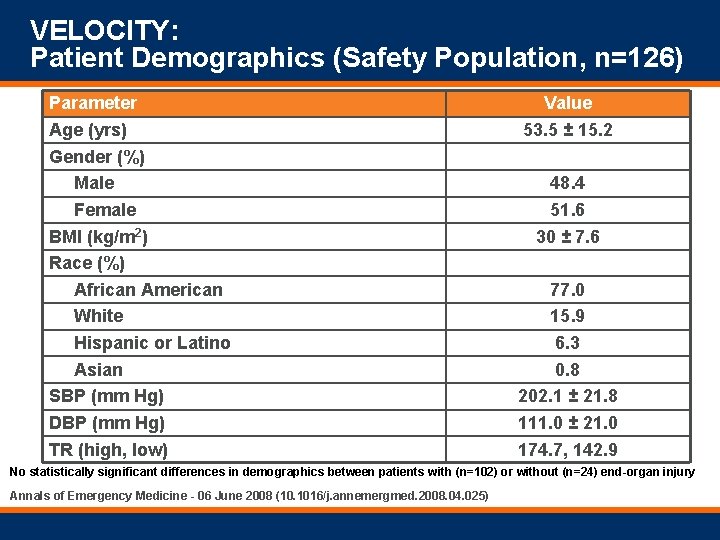
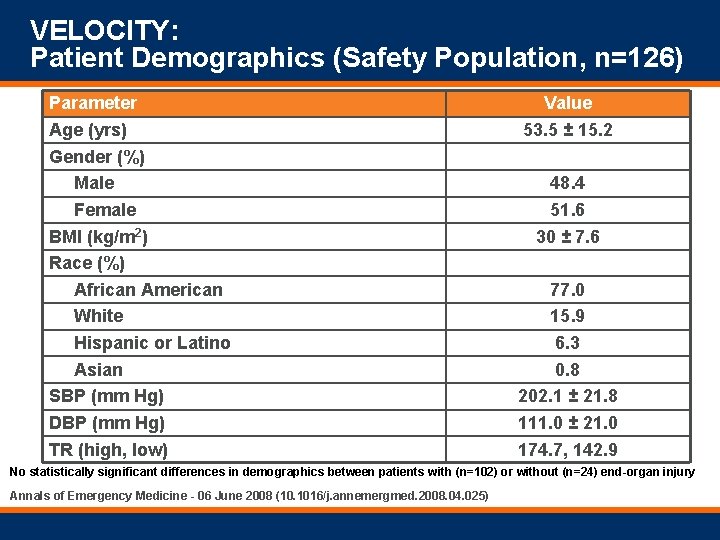
VELOCITY: Patient Demographics (Safety Population, n=126) Parameter Age (yrs) Gender (%) Male Female BMI (kg/m 2) Race (%) African American White Hispanic or Latino Asian SBP (mm Hg) DBP (mm Hg) TR (high, low) Value 53. 5 ± 15. 2 48. 4 51. 6 30 ± 7. 6 77. 0 15. 9 6. 3 0. 8 202. 1 ± 21. 8 111. 0 ± 21. 0 174. 7, 142. 9 No statistically significant differences in demographics between patients with (n=102) or without (n=24) end-organ injury Annals of Emergency Medicine - 06 June 2008 (10. 1016/j. annemergmed. 2008. 04. 025)
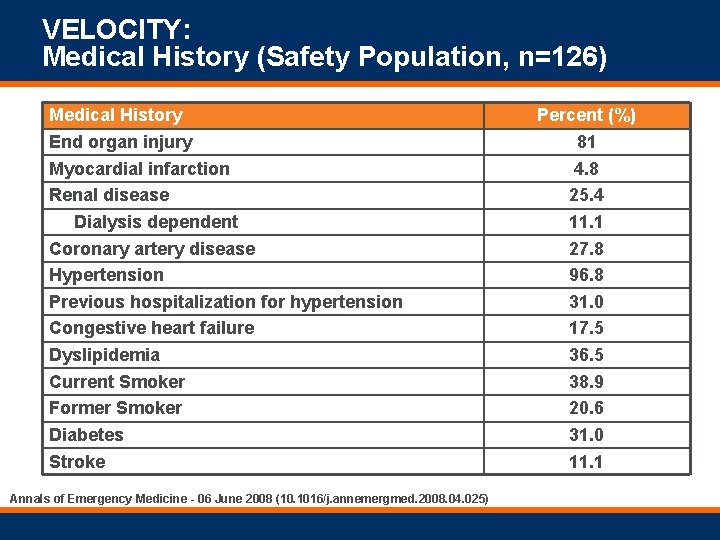
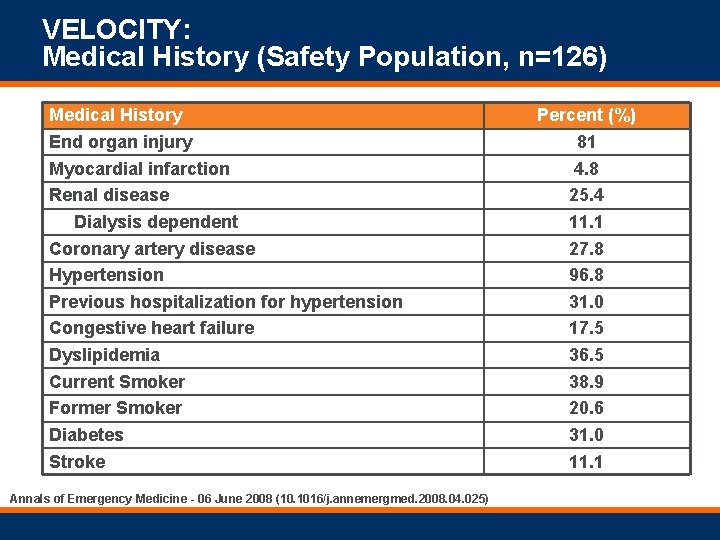
VELOCITY: Medical History (Safety Population, n=126) Medical History End organ injury Myocardial infarction Renal disease Dialysis dependent Coronary artery disease Hypertension Previous hospitalization for hypertension Congestive heart failure Dyslipidemia Current Smoker Former Smoker Diabetes Stroke Annals of Emergency Medicine - 06 June 2008 (10. 1016/j. annemergmed. 2008. 04. 025) Percent (%) 81 4. 8 25. 4 11. 1 27. 8 96. 8 31. 0 17. 5 36. 5 38. 9 20. 6 31. 0 11. 1
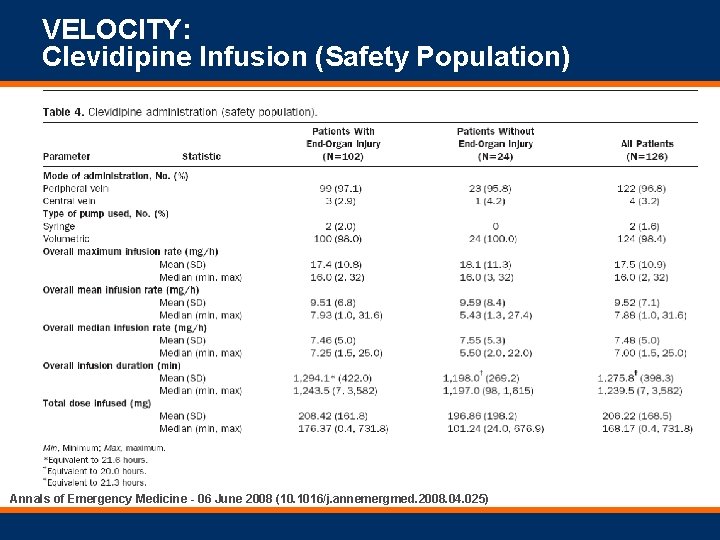
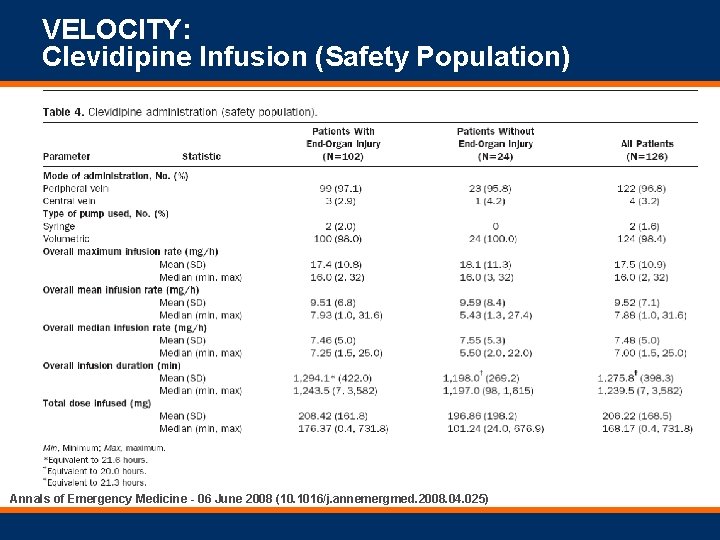
VELOCITY: Clevidipine Infusion (Safety Population) Annals of Emergency Medicine - 06 June 2008 (10. 1016/j. annemergmed. 2008. 04. 025)
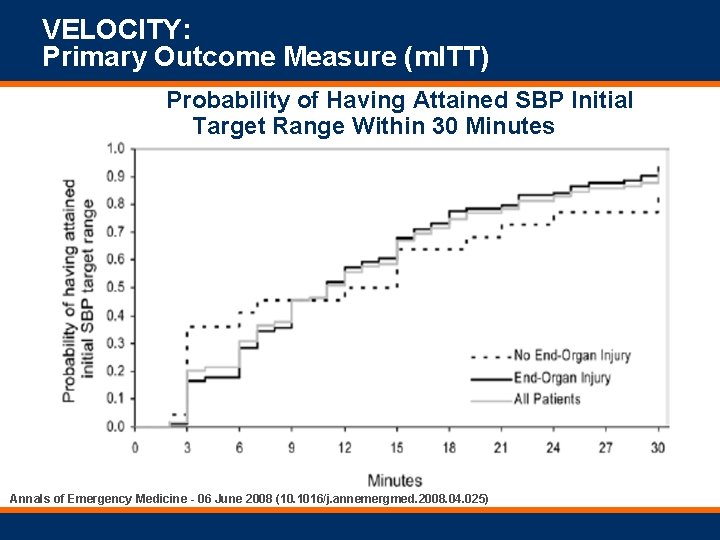
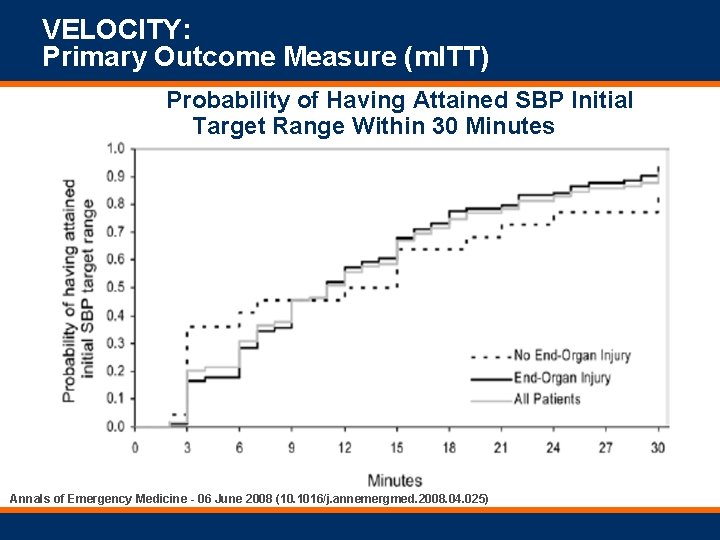
VELOCITY: Primary Outcome Measure (m. ITT) Probability of Having Attained SBP Initial Target Range Within 30 Minutes Annals of Emergency Medicine - 06 June 2008 (10. 1016/j. annemergmed. 2008. 04. 025)
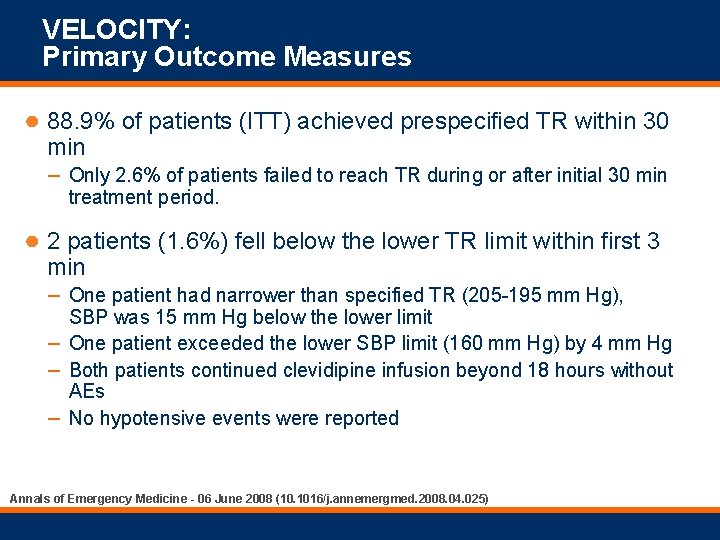
VELOCITY: Primary Outcome Measures ● 88. 9% of patients (ITT) achieved prespecified TR within 30 min – Only 2. 6% of patients failed to reach TR during or after initial 30 min treatment period. ● 2 patients (1. 6%) fell below the lower TR limit within first 3 min – One patient had narrower than specified TR (205 -195 mm Hg), SBP was 15 mm Hg below the lower limit – One patient exceeded the lower SBP limit (160 mm Hg) by 4 mm Hg – Both patients continued clevidipine infusion beyond 18 hours without AEs – No hypotensive events were reported Annals of Emergency Medicine - 06 June 2008 (10. 1016/j. annemergmed. 2008. 04. 025)
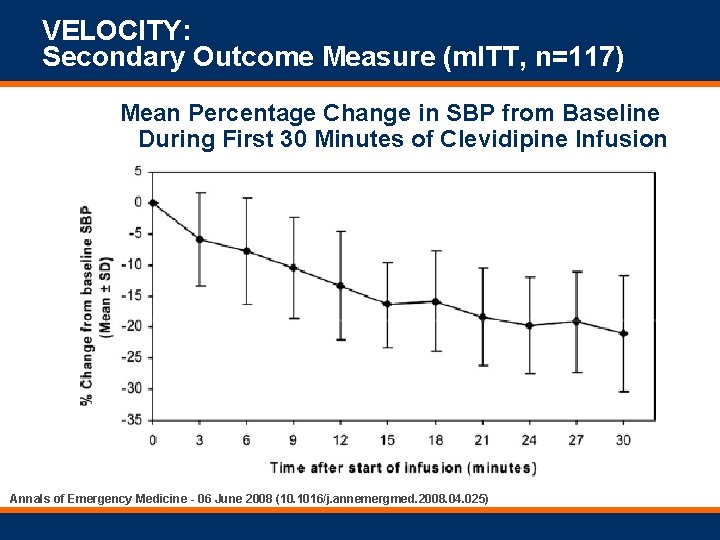
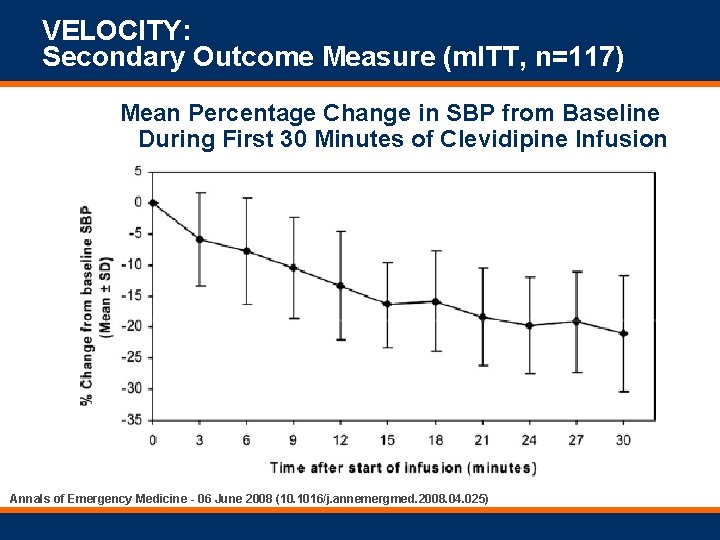
VELOCITY: Secondary Outcome Measure (m. ITT, n=117) Mean Percentage Change in SBP from Baseline During First 30 Minutes of Clevidipine Infusion Annals of Emergency Medicine - 06 June 2008 (10. 1016/j. annemergmed. 2008. 04. 025)
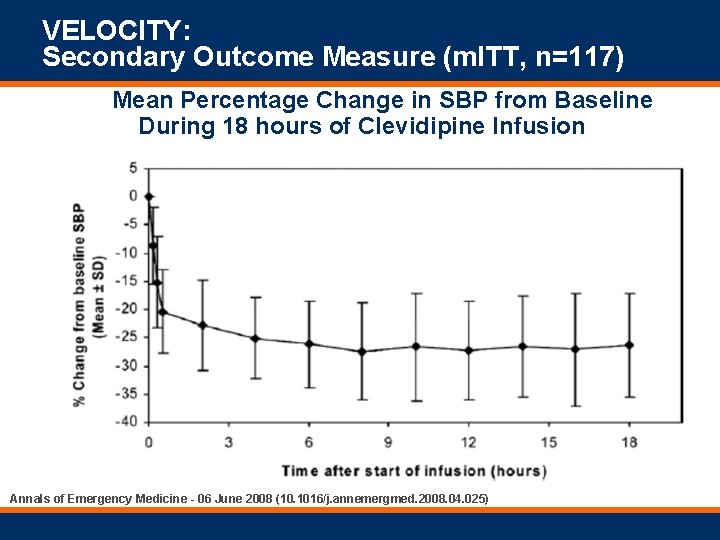
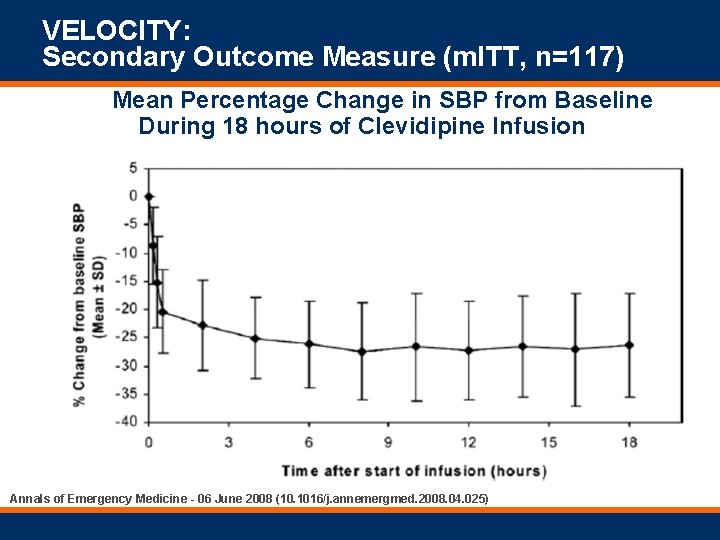
VELOCITY: Secondary Outcome Measure (m. ITT, n=117) Mean Percentage Change in SBP from Baseline During 18 hours of Clevidipine Infusion Annals of Emergency Medicine - 06 June 2008 (10. 1016/j. annemergmed. 2008. 04. 025)
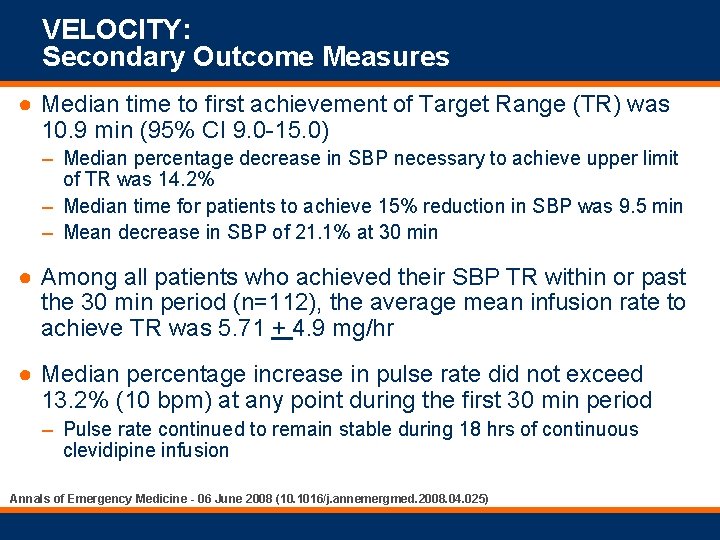
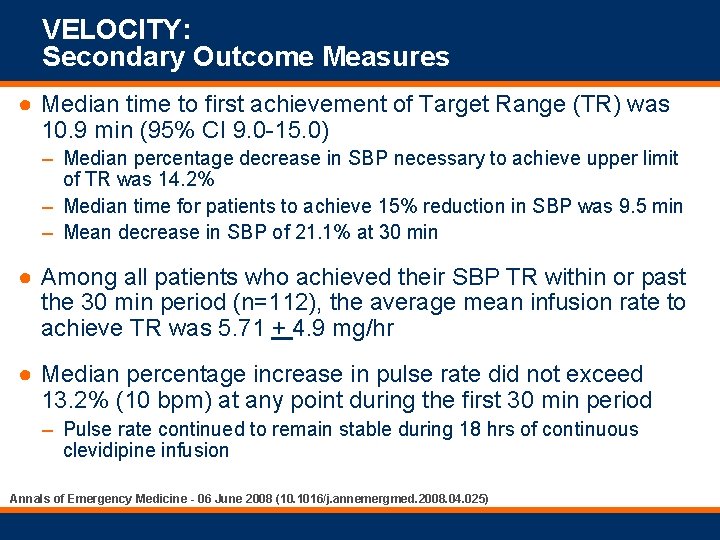
VELOCITY: Secondary Outcome Measures ● Median time to first achievement of Target Range (TR) was 10. 9 min (95% CI 9. 0 -15. 0) – Median percentage decrease in SBP necessary to achieve upper limit of TR was 14. 2% – Median time for patients to achieve 15% reduction in SBP was 9. 5 min – Mean decrease in SBP of 21. 1% at 30 min ● Among all patients who achieved their SBP TR within or past the 30 min period (n=112), the average mean infusion rate to achieve TR was 5. 71 + 4. 9 mg/hr ● Median percentage increase in pulse rate did not exceed 13. 2% (10 bpm) at any point during the first 30 min period – Pulse rate continued to remain stable during 18 hrs of continuous clevidipine infusion Annals of Emergency Medicine - 06 June 2008 (10. 1016/j. annemergmed. 2008. 04. 025)
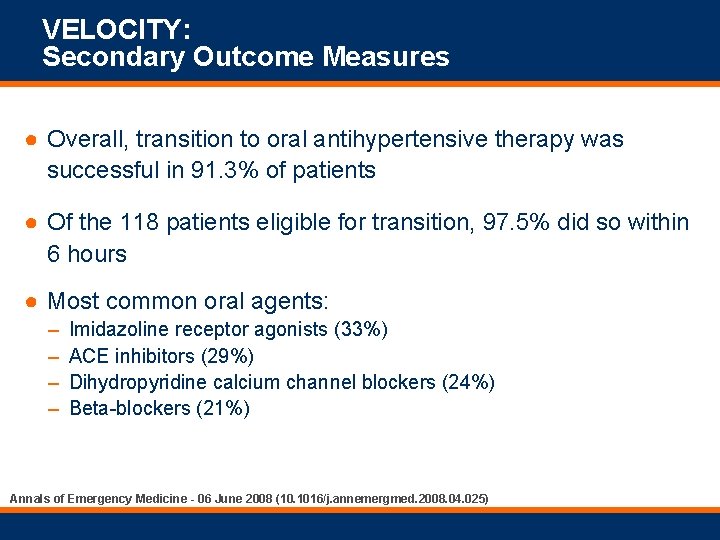
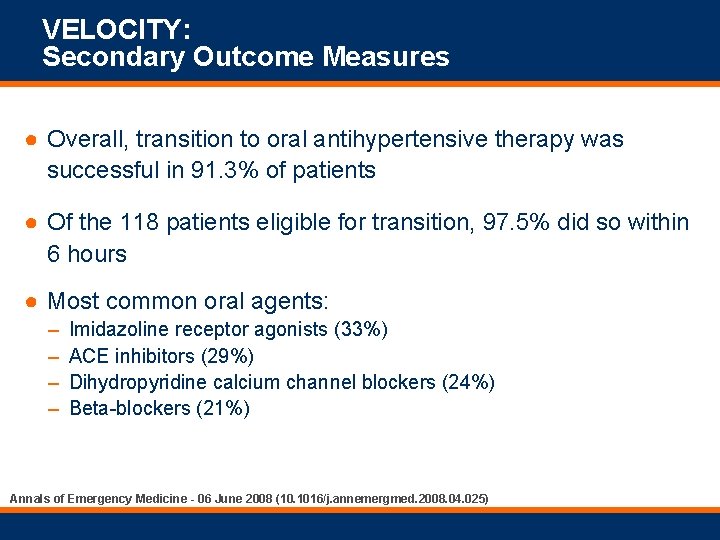
VELOCITY: Secondary Outcome Measures ● Overall, transition to oral antihypertensive therapy was successful in 91. 3% of patients ● Of the 118 patients eligible for transition, 97. 5% did so within 6 hours ● Most common oral agents: – – Imidazoline receptor agonists (33%) ACE inhibitors (29%) Dihydropyridine calcium channel blockers (24%) Beta-blockers (21%) Annals of Emergency Medicine - 06 June 2008 (10. 1016/j. annemergmed. 2008. 04. 025)
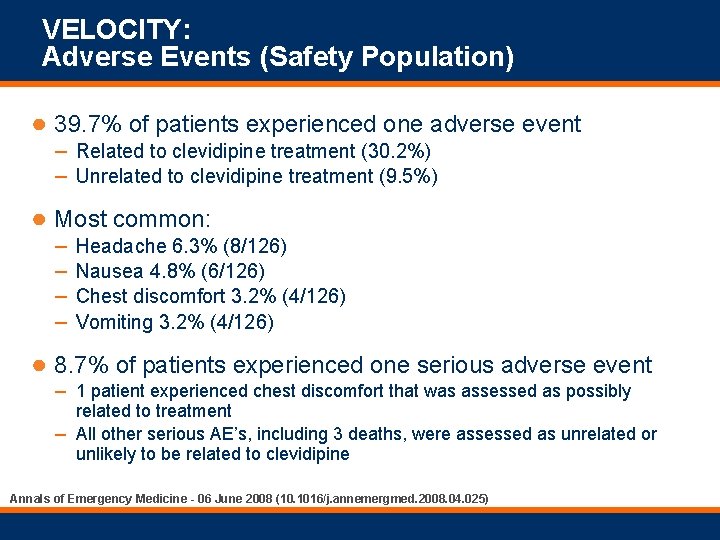
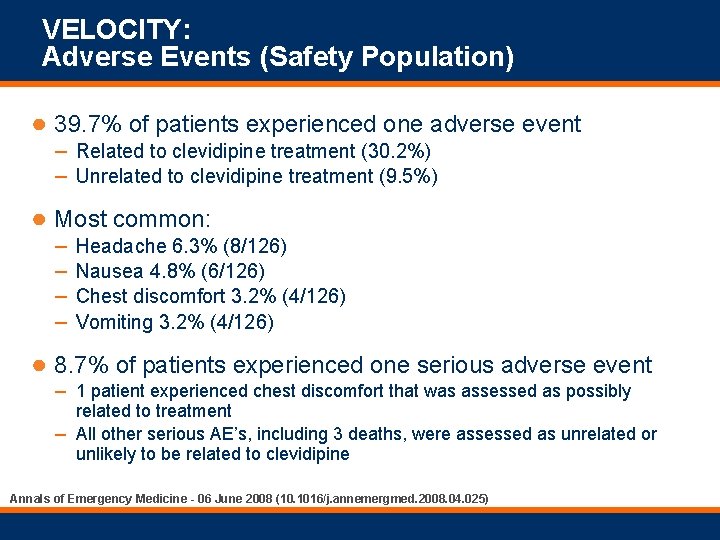
VELOCITY: Adverse Events (Safety Population) ● 39. 7% of patients experienced one adverse event – Related to clevidipine treatment (30. 2%) – Unrelated to clevidipine treatment (9. 5%) ● Most common: – – Headache 6. 3% (8/126) Nausea 4. 8% (6/126) Chest discomfort 3. 2% (4/126) Vomiting 3. 2% (4/126) ● 8. 7% of patients experienced one serious adverse event – 1 patient experienced chest discomfort that was assessed as possibly related to treatment – All other serious AE’s, including 3 deaths, were assessed as unrelated or unlikely to be related to clevidipine Annals of Emergency Medicine - 06 June 2008 (10. 1016/j. annemergmed. 2008. 04. 025)
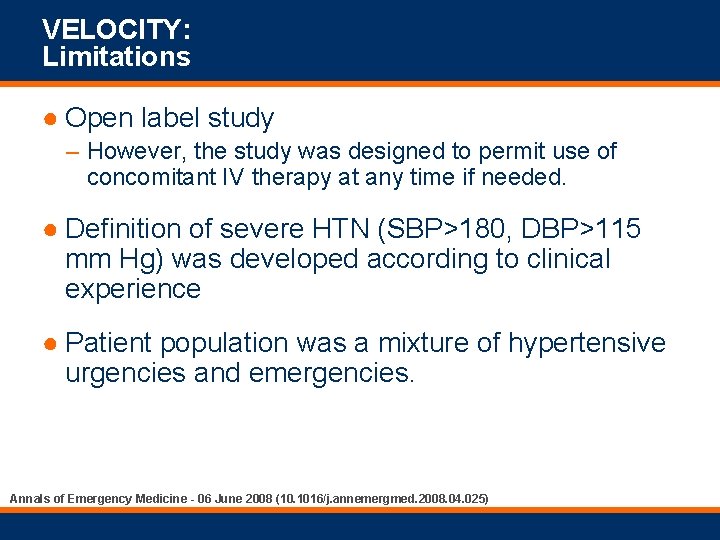
VELOCITY: Limitations ● Open label study – However, the study was designed to permit use of concomitant IV therapy at any time if needed. ● Definition of severe HTN (SBP>180, DBP>115 mm Hg) was developed according to clinical experience ● Patient population was a mixture of hypertensive urgencies and emergencies. Annals of Emergency Medicine - 06 June 2008 (10. 1016/j. annemergmed. 2008. 04. 025)

VELOCITY: Conclusions ● Initial non-weight-based dose of 2 mg/hr of clevidipine is appropriate in the ED setting ● Reliably lowered BP to pre-specified target range in 90% of patients within 30 min ● Predictably reached target BP without overshoot in a median 10. 9 min ● Transition from clevidipine to oral antihypertensive therapy was successful Annals of Emergency Medicine - 06 June 2008 (10. 1016/j. annemergmed. 2008. 04. 025)
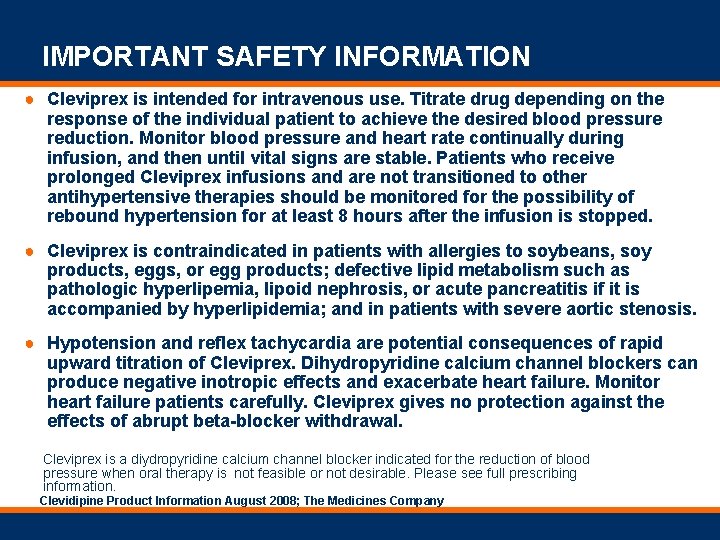
IMPORTANT SAFETY INFORMATION ● Cleviprex is intended for intravenous use. Titrate drug depending on the response of the individual patient to achieve the desired blood pressure reduction. Monitor blood pressure and heart rate continually during infusion, and then until vital signs are stable. Patients who receive prolonged Cleviprex infusions and are not transitioned to other antihypertensive therapies should be monitored for the possibility of rebound hypertension for at least 8 hours after the infusion is stopped. ● Cleviprex is contraindicated in patients with allergies to soybeans, soy products, eggs, or egg products; defective lipid metabolism such as pathologic hyperlipemia, lipoid nephrosis, or acute pancreatitis if it is accompanied by hyperlipidemia; and in patients with severe aortic stenosis. ● Hypotension and reflex tachycardia are potential consequences of rapid upward titration of Cleviprex. Dihydropyridine calcium channel blockers can produce negative inotropic effects and exacerbate heart failure. Monitor heart failure patients carefully. Cleviprex gives no protection against the effects of abrupt beta-blocker withdrawal. Cleviprex is a diydropyridine calcium channel blocker indicated for the reduction of blood pressure when oral therapy is not feasible or not desirable. Please see full prescribing information. Clevidipine Product Information August 2008; The Medicines Company
IMPORTANT SAFETY INFORMATION: continued ● Most common adverse reactions (> 2%) are headache, nausea, and vomiting. ● Cleviprex should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. ● Maintain aseptic technique while handling Cleviprex contains phospholipids and can support microbial growth. Do not use if contamination is suspected. Once the stopper is punctured, use and discard within 4 hours. Cleviprex is a diydropyridine calcium channel blocker indicated for the reduction of blood pressure when oral therapy is not feasible or not desirable. Please see full prescribing information. Clevidipine Product Information August 2008; The Medicines Company
 Perioperative vs intraoperative
Perioperative vs intraoperative Hamlet act iii scene iii
Hamlet act iii scene iii Ipfp phase iii
Ipfp phase iii Paradigm shift from women studies to gender studies
Paradigm shift from women studies to gender studies Canadian perioperative guidelines
Canadian perioperative guidelines Site:slidetodoc.com
Site:slidetodoc.com Perioperative nursing meaning
Perioperative nursing meaning Perioperative case study
Perioperative case study Pre operative care
Pre operative care Preoperative care ppt
Preoperative care ppt Cushing's triad
Cushing's triad Nursing management for glaucoma
Nursing management for glaucoma Nursing management of patient with cataract
Nursing management of patient with cataract Preoperative medical evaluation of the healthy patient
Preoperative medical evaluation of the healthy patient Chapter 17 preoperative nursing management
Chapter 17 preoperative nursing management What is mobile and stationary phase
What is mobile and stationary phase In a triangle connected source feeding a y connected load
In a triangle connected source feeding a y connected load Normal phase vs reverse phase chromatography
Normal phase vs reverse phase chromatography Normal phase vs reverse phase chromatography
Normal phase vs reverse phase chromatography Broad phase vs narrow phase
Broad phase vs narrow phase Tswett pronunciation
Tswett pronunciation Power formula three phase
Power formula three phase Mobile phase and stationary phase
Mobile phase and stationary phase Which detector used in hplc
Which detector used in hplc Pulmonary hypertension differential diagnosis
Pulmonary hypertension differential diagnosis Ttp disease
Ttp disease Causes of secondary hypertension
Causes of secondary hypertension Hypertensive urgency
Hypertensive urgency Hypertension
Hypertension Varices cardio tubérositaires
Varices cardio tubérositaires Talipes equinovarus in varicose veins
Talipes equinovarus in varicose veins 6 vital signs first aid
6 vital signs first aid Faa hypertension worksheet
Faa hypertension worksheet Mitral stenosis pulmonary hypertension
Mitral stenosis pulmonary hypertension Antihypertensive drugs classification
Antihypertensive drugs classification Nursing blood pressure assessment
Nursing blood pressure assessment Malignant hypertension management
Malignant hypertension management Stages of pulmonary hypertension
Stages of pulmonary hypertension Definition of hypertension
Definition of hypertension Med
Med Non pharmacological management of hypertension
Non pharmacological management of hypertension Portal hypertension
Portal hypertension Conclusion of hypertension
Conclusion of hypertension Conclusion of hypertension
Conclusion of hypertension Conclusion of hypertension
Conclusion of hypertension Stigmata of chronic liver disease
Stigmata of chronic liver disease Signs of portal hypertension
Signs of portal hypertension Hypertension
Hypertension Non pharmacological management of hypertension
Non pharmacological management of hypertension Intimal hyperplasia
Intimal hyperplasia Pneumotrieste
Pneumotrieste Intracranial hypertension
Intracranial hypertension Hypertension
Hypertension Hypertensive encephalopathy
Hypertensive encephalopathy Hypertensive emergency
Hypertensive emergency Urapidil rcp
Urapidil rcp Hypertensive emergency vs urgency
Hypertensive emergency vs urgency Ascites veins
Ascites veins Presinusoidal portal hypertension
Presinusoidal portal hypertension Masked hypertension
Masked hypertension Hypertensive urgency vs emergency
Hypertensive urgency vs emergency Health coaches for hypertension control
Health coaches for hypertension control Medical nutrition therapy for hypertension
Medical nutrition therapy for hypertension Pathophysiology of pulmonary hypertension
Pathophysiology of pulmonary hypertension Pulmonary hypertension definition
Pulmonary hypertension definition Hypertension vs hypotension
Hypertension vs hypotension