Child Maltreatment Outcomes Integrate the evaluation of child











- Slides: 39

Child Maltreatment
Outcomes �Integrate the evaluation of child maltreatment into daily nursing practice �Identify risk factors, key indicators, common physical injuries, and long term consequences of child maltreatment �Recognize that screening, evaluation, and appropriate nursing interventions are extremely important for victims of child treatment �Appreciate the value of documentation, evidence collection, and the importance of reporting suspected child maltreatment to appropriate local authorities
Introduction �Physical abuse an important cause for pediatric morbidity and mortality �Associated with major physical and mental health problems that extends into adulthood �Child Abuse Prevention and Treatment Act �“any recent act or failure to act on the part of a parent or caregiver, which results in death, serious physical or emotional harm, sexual abuse or exploitation…or an act or failure to act which prevents an imminent risk of serious harm. ”
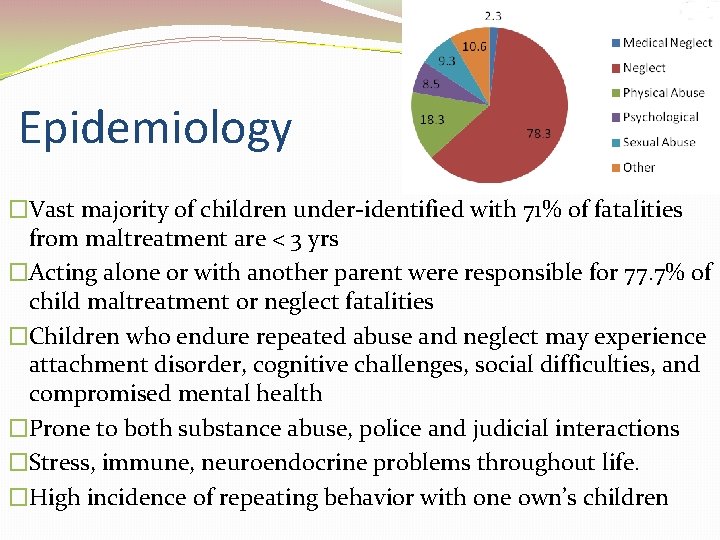
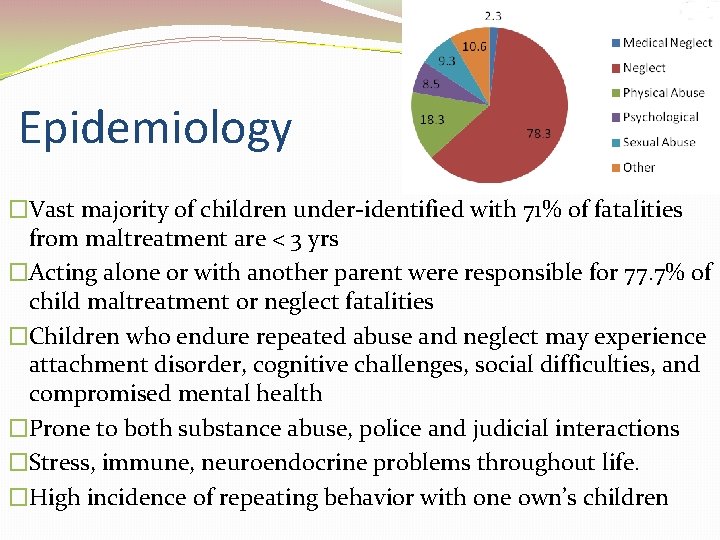
Epidemiology �Vast majority of children under-identified with 71% of fatalities from maltreatment are < 3 yrs �Acting alone or with another parent were responsible for 77. 7% of child maltreatment or neglect fatalities �Children who endure repeated abuse and neglect may experience attachment disorder, cognitive challenges, social difficulties, and compromised mental health �Prone to both substance abuse, police and judicial interactions �Stress, immune, neuroendocrine problems throughout life. �High incidence of repeating behavior with one own’s children
Long Term Consequences �Those who endure repeated abuse and neglect �attachment disorder �Cognitive challenges �Social difficulties �Compromised mental health �More prone to substance abuse �Increased negative contact with law enforcement and the judicial system �Emerging recognition that adverse childhood experiences including physical abuse, influence biological adaptations associated with how the brain, neuroendocrine stress response, and immune system function
Neglect �Most common �Failure to provide for child’s basic physical, emotional, or educational needs or to protect a child from harm or potential harm �Neglected children do not learn how to develop coping abilities and tend to be overly dependent and unhappy �Tend to develop criminal behavior, personality disorders, substance abuse, and stressful life events



Physical Abuse �Physical abuse make direction much more objective than other forms of abuse �Unintentional and intentional injuries �Past medical history / “story” VERY important to build evidence �Monitor for signs of discrepancies
Psychological Abuse �Intentional behavior on the part of the caregiver that conveys to a child that they are worthless, flawed, unloved, unwanted, endangered, or valued only in meeting another’s needs �Emotionally abused children do not learn how to regulate and control emotional expression, nor do they learn to manage the subtleties of emotional life. �Difficult for nurse to pinpoint with limited exposure (like ED). Might take several exposures.
Sexual Abuse �Any completed or attempted sexual act, sexual contact with, or exploitation of a child by a caregiver �Those who have experienced sexual abuse require consistent, objective, and immediate medical care, with forensic evidence collected by ED (SANE) nurses and medical providers trained in jurisdictional guidelines and protocols �Goes unreported into adulthood �Many children fearful of “breaking the rules” �Does not want to upset or disappoint alleged abuser �Manipulate and silence children creating opportunity for offenders �Child’s dependence on caregivers �Child’s developmental age �Cognitive ability
Medical Child Maltreatment �AKA Munchhausen Syndrome by Proxy AKA Pediatric Condition Falsification AKA Factitious Disorder by Proxy AKA Factitious Disorder AKA Medicinal Abuse �A child receives unnecessary and harmful or potentially harmful medical care at the instigation of a caretaker �Factitious disorder; factitious disorder by proxy, medicinal abuse, and pediatric condition falsification �Perpetrators tend to “doctor shop” choosing physicians who recommend repeat testing and invasive procedures, and remove their children from the care of physicians who refuse to escalate treatment �Motivation usually need for attention or to covertly manipulate or deceive authority figures �Often leads to disability or death
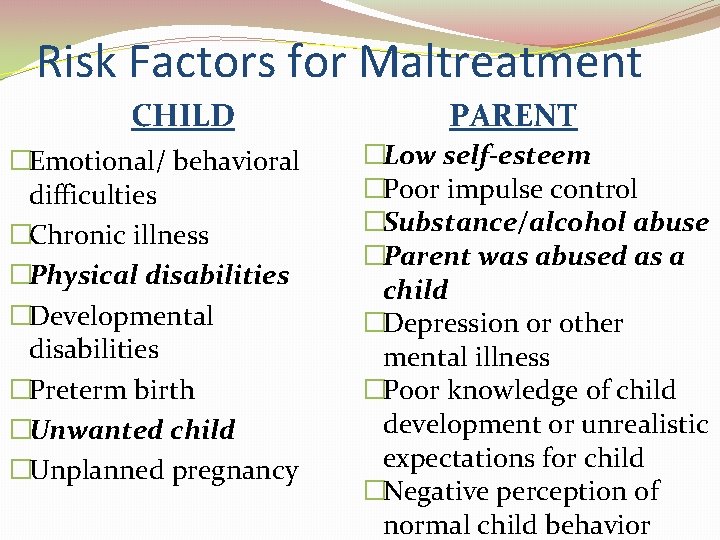
Risk Factors for Maltreatment CHILD �Emotional/ behavioral difficulties �Chronic illness �Physical disabilities �Developmental disabilities �Preterm birth �Unwanted child �Unplanned pregnancy PARENT �Low self-esteem �Poor impulse control �Substance/alcohol abuse �Parent was abused as a child �Depression or other mental illness �Poor knowledge of child development or unrealistic expectations for child �Negative perception of normal child behavior
Risk Factors for Maltreatment �Environment �Social isolation �Poverty �Unemployment �Low educational achievement �Single parent �Non-biologically related male living in household �Family or intimate partner violence �Immigrant families
Intentional Trauma Screening �RED Flag history of present illness �No history or inconsistent history �Changing history �Unwitnessed injury �Delay in seeking care �Prior ED visit �Domestic violence in home �Premature infant (<37 weeks) �LBW �Chronic medical conditions
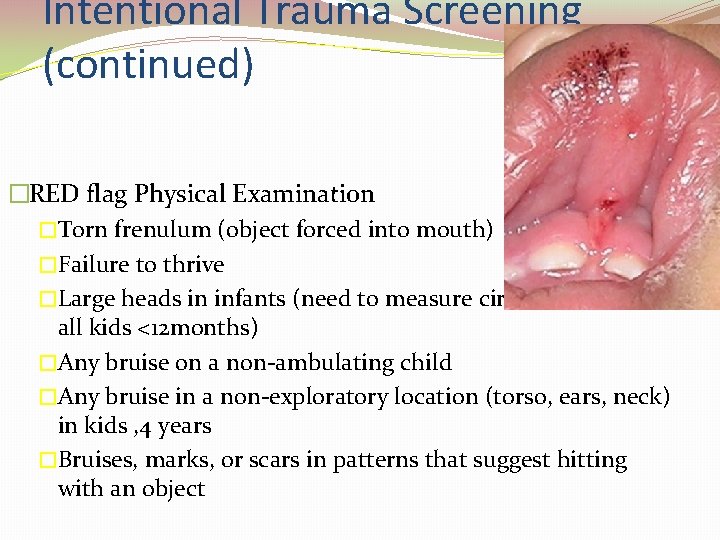
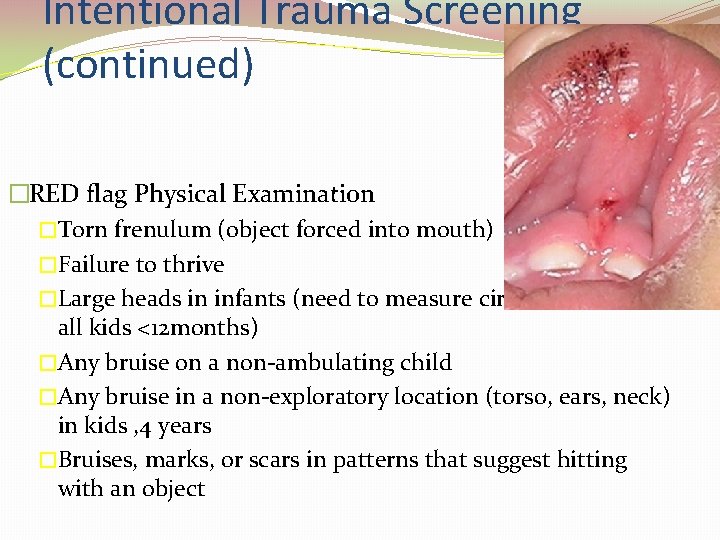
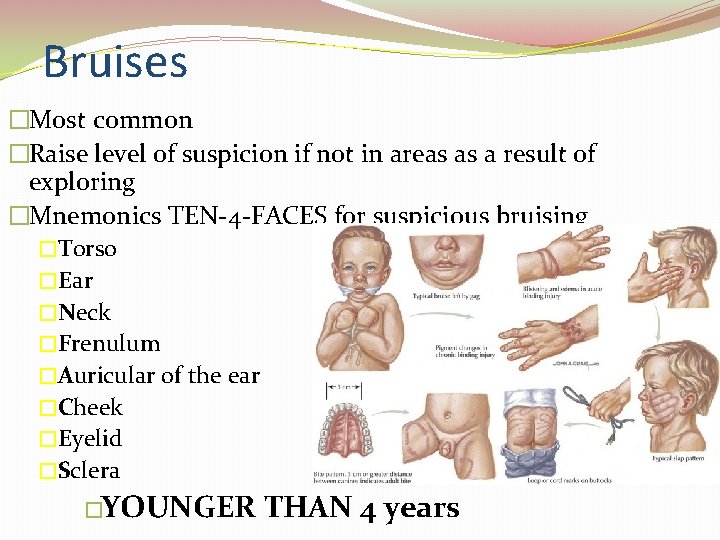
Intentional Trauma Screening (continued) �RED flag Physical Examination �Torn frenulum (object forced into mouth) �Failure to thrive �Large heads in infants (need to measure circumference on all kids <12 months) �Any bruise on a non-ambulating child �Any bruise in a non-exploratory location (torso, ears, neck) in kids , 4 years �Bruises, marks, or scars in patterns that suggest hitting with an object
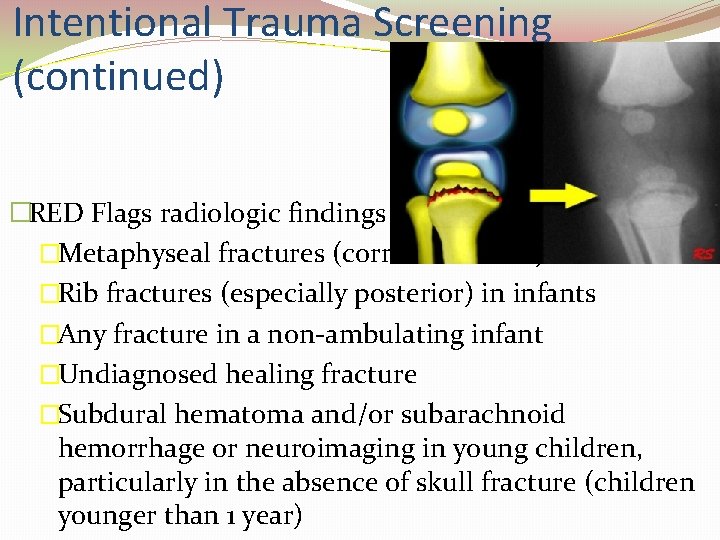
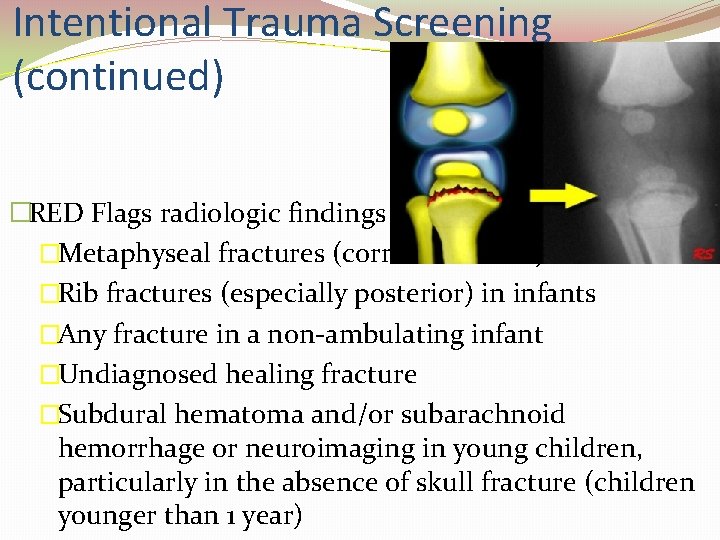
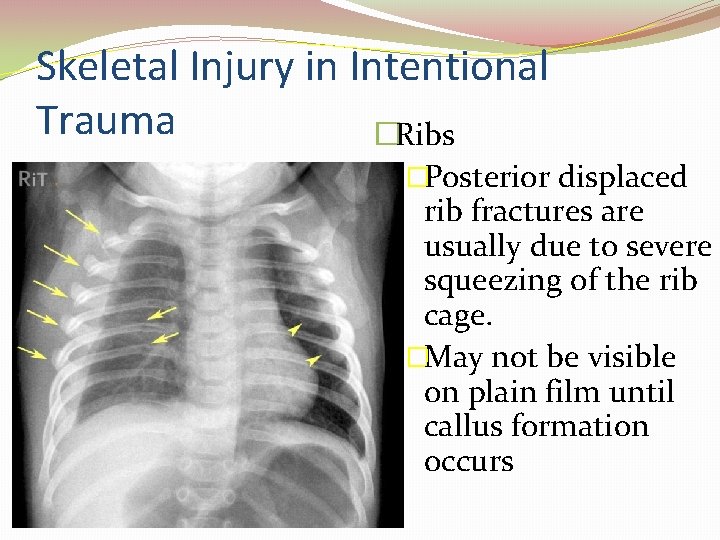
Intentional Trauma Screening (continued) �RED Flags radiologic findings �Metaphyseal fractures (corner fractures) �Rib fractures (especially posterior) in infants �Any fracture in a non-ambulating infant �Undiagnosed healing fracture �Subdural hematoma and/or subarachnoid hemorrhage or neuroimaging in young children, particularly in the absence of skull fracture (children younger than 1 year)
“What happened here” �Asking the verbal child – looking for body language and facial expressions along with speech pattern �Children more apt to describe story behind injury when it is not a result of abuse �Compare explanations with pattern of injury, and caregiver
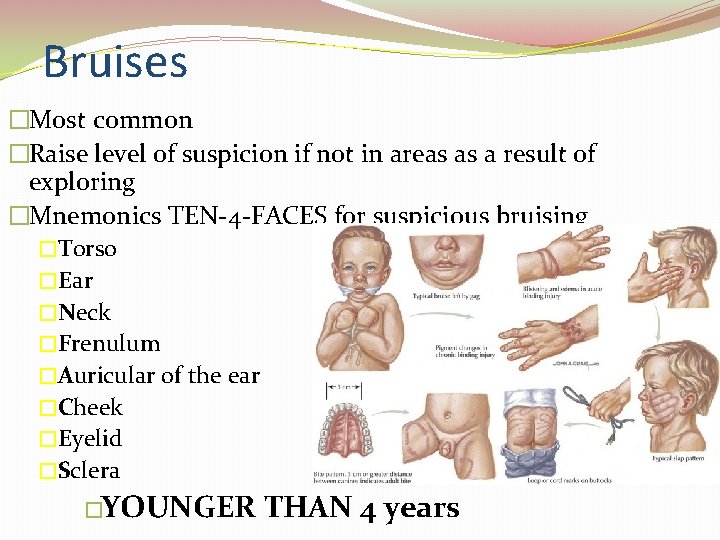
Bruises �Most common �Raise level of suspicion if not in areas as a result of exploring �Mnemonics TEN-4 -FACES for suspicious bruising �Torso �Ear �Neck �Frenulum �Auricular of the ear �Cheek �Eyelid �Sclera �YOUNGER THAN 4 years

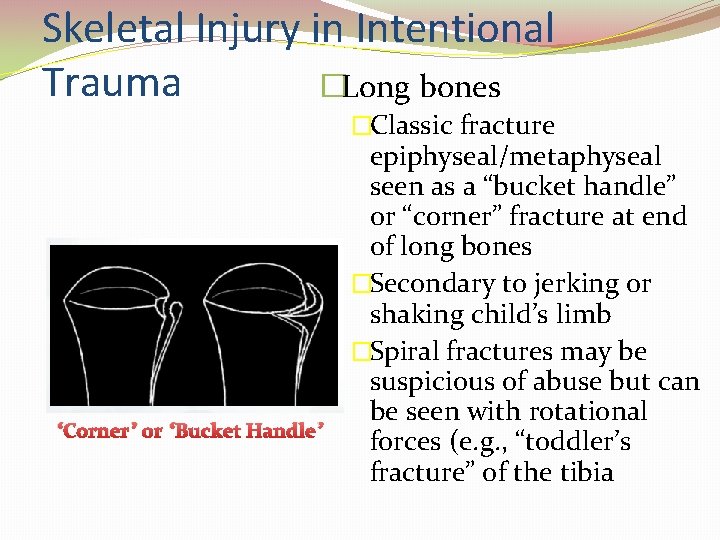
Fractures �Very common in ambulating children �Second most common presentation in maltreatment �Raise concern of physical abuse in non-ambulatory children with fractures and no clear history of how the injury occurred �Certain particular skeletal injuries might raise concern especially for <2 years
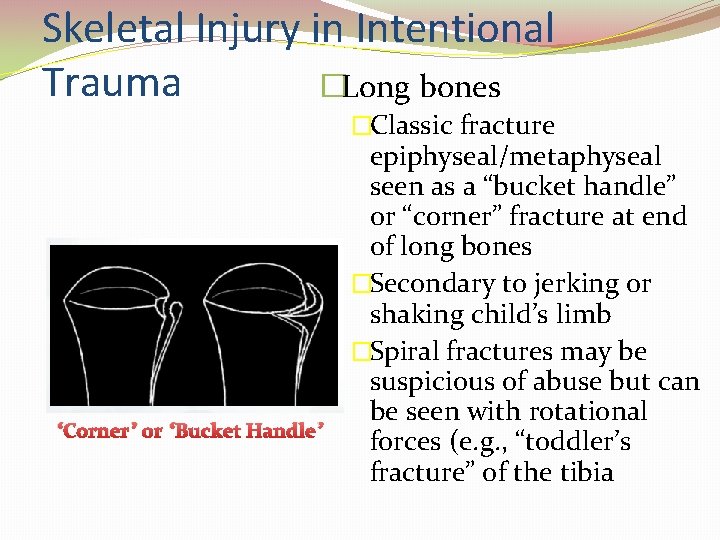
Skeletal Injury in Intentional Trauma �Long bones �Classic fracture “Corner” or “Bucket Handle” epiphyseal/metaphyseal seen as a “bucket handle” or “corner” fracture at end of long bones �Secondary to jerking or shaking child’s limb �Spiral fractures may be suspicious of abuse but can be seen with rotational forces (e. g. , “toddler’s fracture” of the tibia
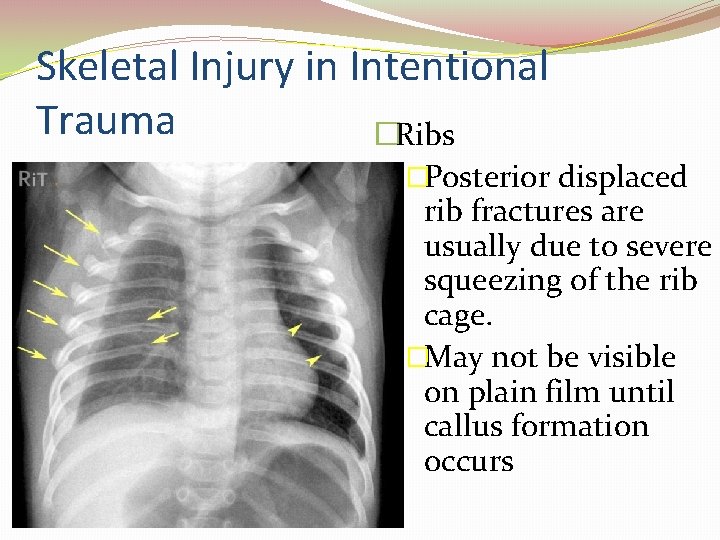
Skeletal Injury in Intentional Trauma �Ribs �Posterior displaced rib fractures are usually due to severe squeezing of the rib cage. �May not be visible on plain film until callus formation occurs
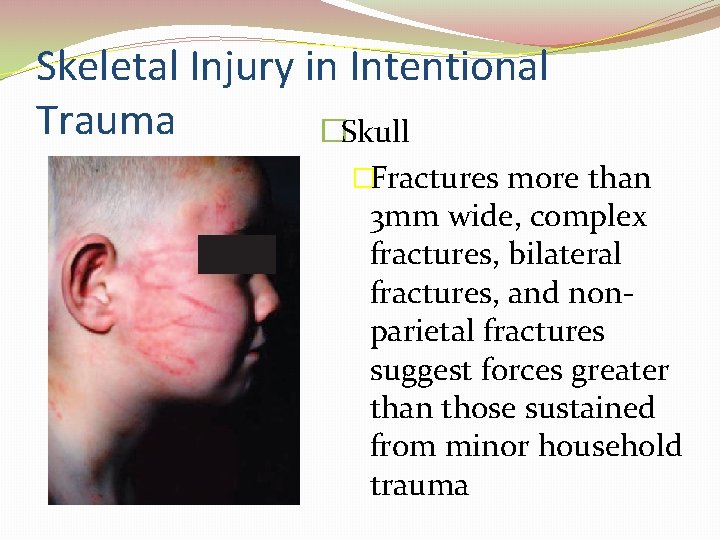
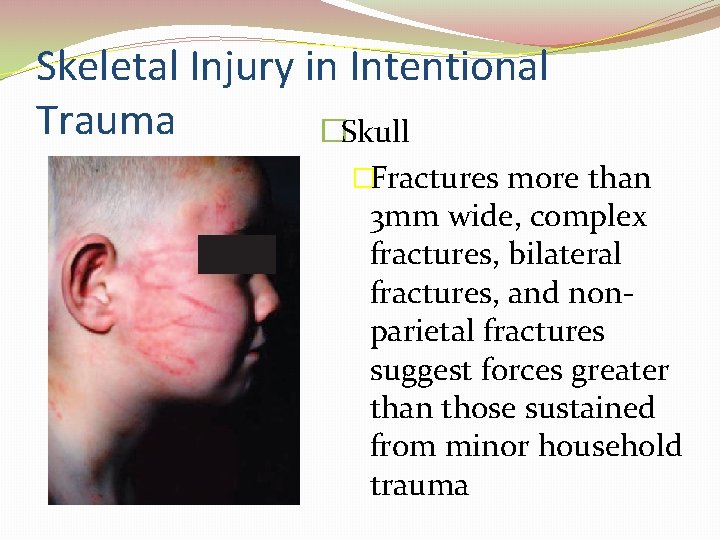
Skeletal Injury in Intentional Trauma �Skull �Fractures more than 3 mm wide, complex fractures, bilateral fractures, and nonparietal fractures suggest forces greater than those sustained from minor household trauma
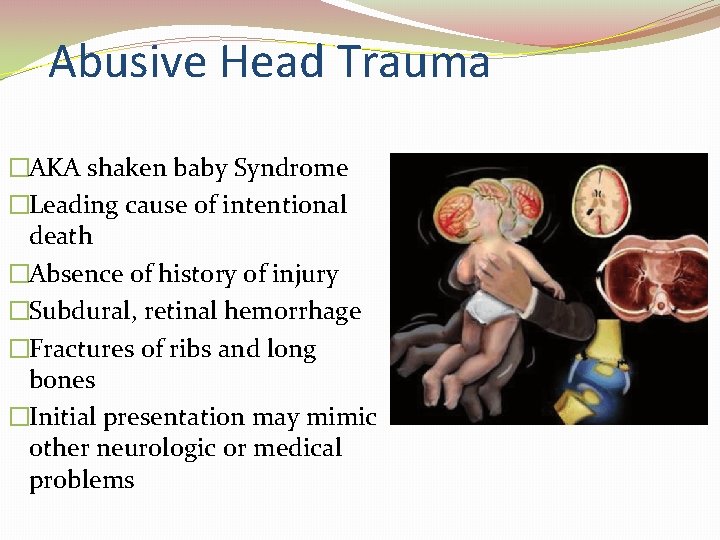
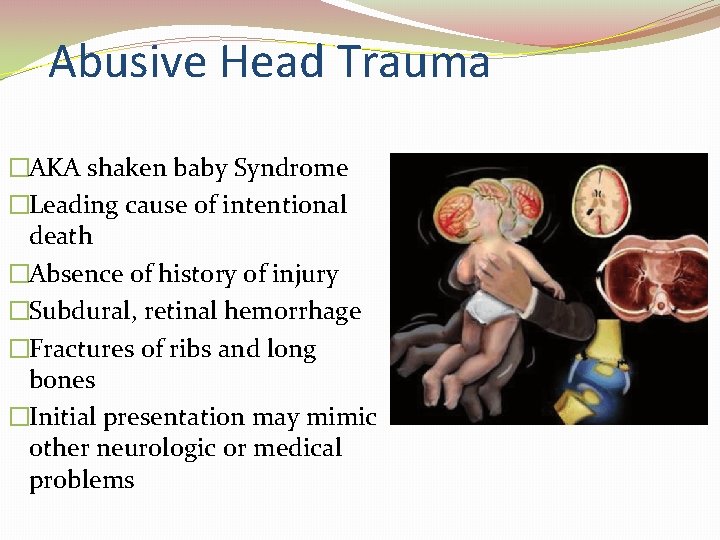
Abusive Head Trauma �AKA shaken baby Syndrome �Leading cause of intentional death �Absence of history of injury �Subdural, retinal hemorrhage �Fractures of ribs and long bones �Initial presentation may mimic other neurologic or medical problems
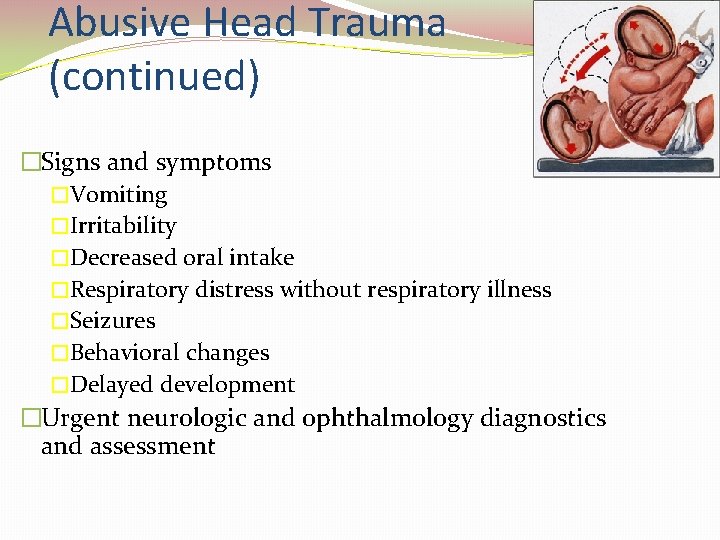
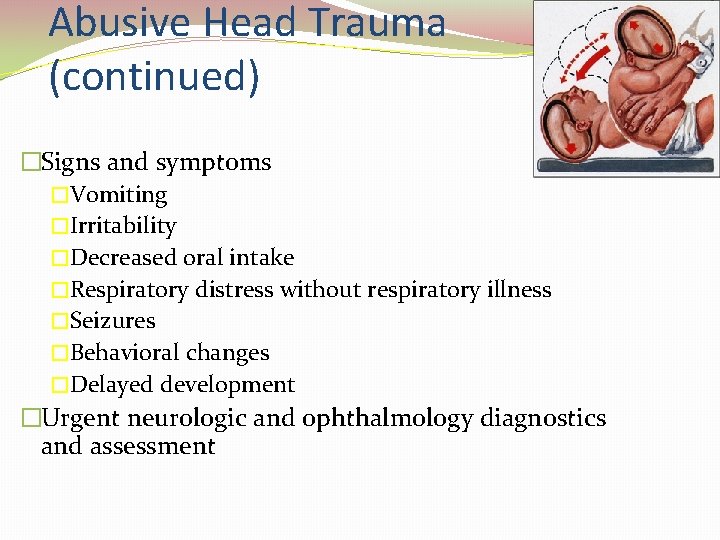
Abusive Head Trauma (continued) �Signs and symptoms �Vomiting �Irritability �Decreased oral intake �Respiratory distress without respiratory illness �Seizures �Behavioral changes �Delayed development �Urgent neurologic and ophthalmology diagnostics and assessment
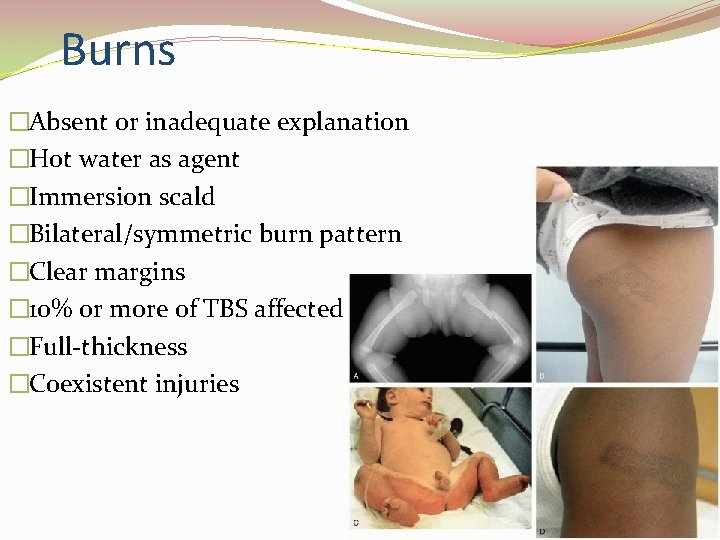
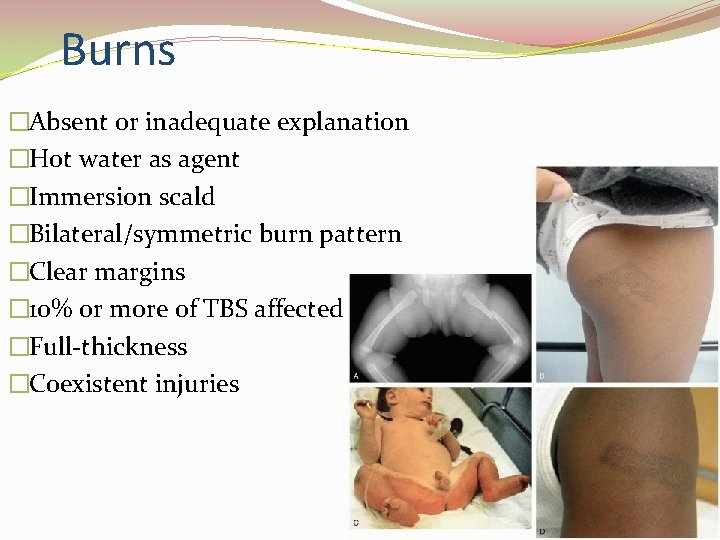
Burns �Absent or inadequate explanation �Hot water as agent �Immersion scald �Bilateral/symmetric burn pattern �Clear margins � 10% or more of TBS affected �Full-thickness �Coexistent injuries
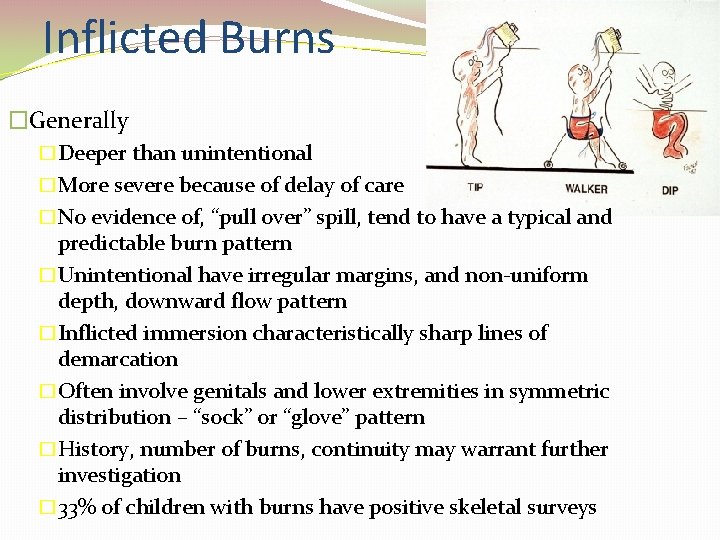
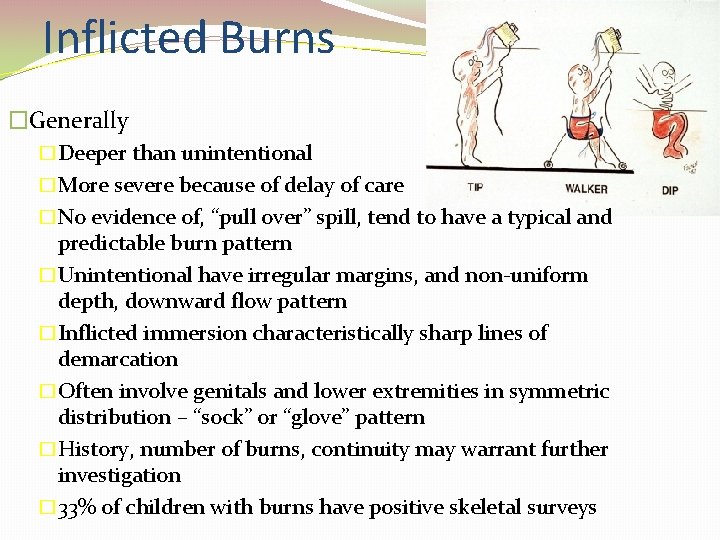
Inflicted Burns �Generally �Deeper than unintentional �More severe because of delay of care �No evidence of, “pull over” spill, tend to have a typical and predictable burn pattern �Unintentional have irregular margins, and non-uniform depth, downward flow pattern �Inflicted immersion characteristically sharp lines of demarcation �Often involve genitals and lower extremities in symmetric distribution – “sock” or “glove” pattern �History, number of burns, continuity may warrant further investigation � 33% of children with burns have positive skeletal surveys

Unintentional vs Intentional Pull over spill Burn Stocking / Glove Burn
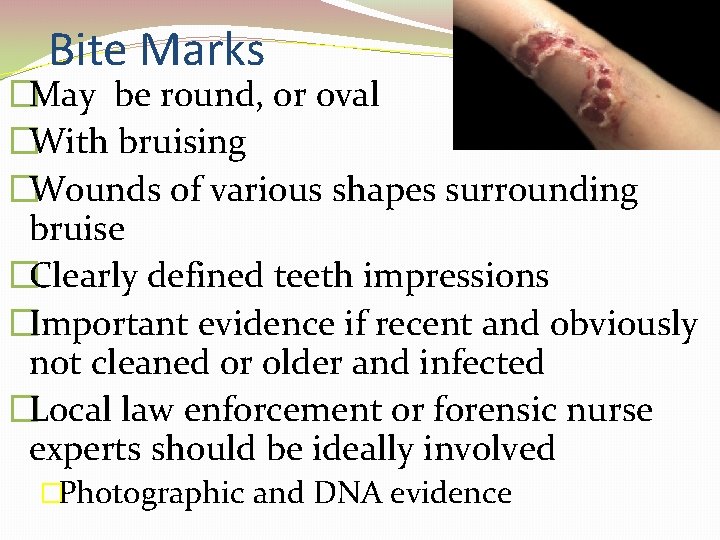
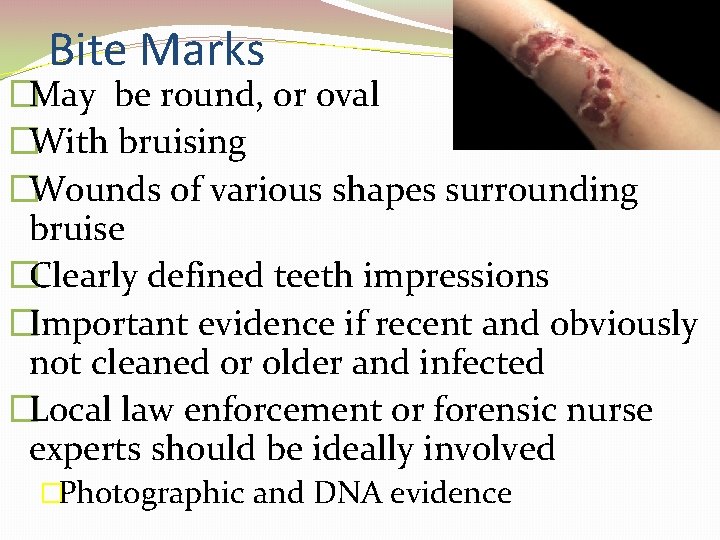
Bite Marks �May be round, or oval �With bruising �Wounds of various shapes surrounding bruise �Clearly defined teeth impressions �Important evidence if recent and obviously not cleaned or older and infected �Local law enforcement or forensic nurse experts should be ideally involved �Photographic and DNA evidence

Evaluation of Child Maltreatment �Screening is systematic process �AAP – The evaluation of Suspected Child Physical Abuse helps guide a facility in developing such a protocol �Provide relaxed environment to obtain history from children and caregivers – open ended questions �Comprehensive and accurate documentation- using exact quotes - photographs
Nursing Interventions �Document for Court �provide the facts- avoid personal opinions �Descriptive documentation gives reader most accurate picture of what is observed �Exact words of patient and caregivers in quotes, even in slang, violent terms, or vulgar terms �Evidence �Defined as data presented to a court or jury to prove or disapprove a claim (physical, words spoken, observations) �Safeguard evidentiary materials �Avoid cutting through blood, stains, splatter, or holes made by projectiles; cut along seams �Know jurisdictional laws regarding evidence collection and chain of custody �REMEMBER: The well-being of a patient takes precedence over forensic evidence collection
Mandated Reporting �All involved in child care (physicians, nurses, teachers, daycare workers, police) are mandated reporters required by law in all states – report suspected abuse or neglect �Fear of over-reporting in an already overburdened system may be a deterrent �Confidence and self-efficacy in ability to recognize child maltreatment may assist healthcare providers to take appropriate action and report suspicions




Summary �Nurses crucial position to identify children at risk for maltreatment �Performing a more comprehensive evaluation to determine whether they are in a safe situation �Those educated related to this issue more likely to recognize & report their findings �Healthcare providers at every point of care must effectively identify and intervene on behalf of children who deserve a life free from abuse
 Rules for integration
Rules for integration Integrating quotes
Integrating quotes Nursing intervention examples
Nursing intervention examples Sisteme informatice integrate erp
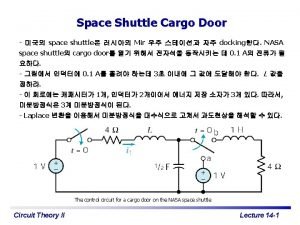
Sisteme informatice integrate erp Unit step function convolution
Unit step function convolution Haidlmair jobs
Haidlmair jobs Express definition
Express definition Sa-sd
Sa-sd Integration quotes
Integration quotes Kentico infor integrate
Kentico infor integrate How to successfully integrate new employees
How to successfully integrate new employees Activitati integrate grupa mare
Activitati integrate grupa mare Product rule integration
Product rule integration 6fc5800-0ap67-0yb0
6fc5800-0ap67-0yb0 Globalization collocation
Globalization collocation Lời thề hippocrates
Lời thề hippocrates Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Phản ứng thế ankan
Phản ứng thế ankan Các môn thể thao bắt đầu bằng tiếng đua
Các môn thể thao bắt đầu bằng tiếng đua Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Dot
Dot điện thế nghỉ
điện thế nghỉ Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Fecboak
Fecboak Một số thể thơ truyền thống
Một số thể thơ truyền thống Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Slidetodoc
Slidetodoc Sơ đồ cơ thể người
Sơ đồ cơ thể người Số nguyên là gì
Số nguyên là gì Tư thế ngồi viết
Tư thế ngồi viết đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Chụp phim tư thế worms-breton
Chụp phim tư thế worms-breton ưu thế lai là gì
ưu thế lai là gì