CHALLENGES IN MANAGEMENT OF UTERINE PROLAPSE IN PREGNANCY


- Slides: 45
CHALLENGES IN MANAGEMENT OF UTERINE PROLAPSE IN PREGNANCY Presented by Dr Moses Mwei Dr Benjamin Shayo Dr Bariki Mchome 8 th June 2017
CASE REPORT
DEMOGRAPHIC INFO. • • Patient Name: S. M Age: 26 Sex: Female Adress: Nyumba ya mungu- Moshi
PRESENTING COMPLAINT • Patient came in as a referral from Mawenzi regional hospital • Complaints of slight abdominal pains and progressive protrusion of a mass per vagina
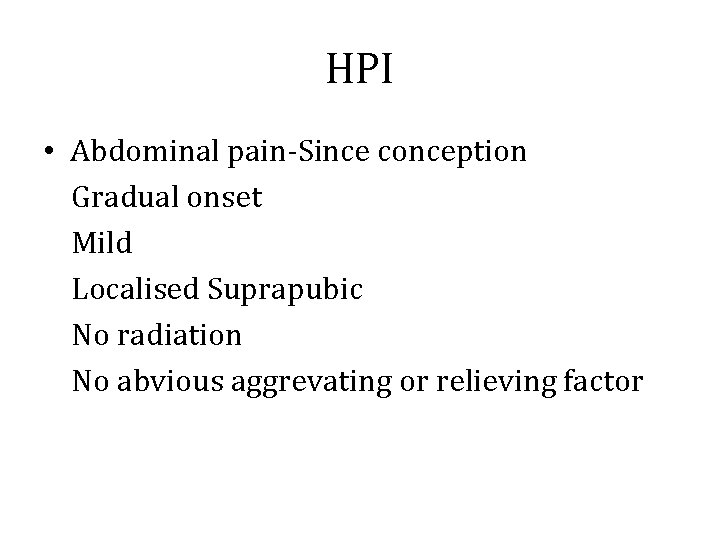
HPI • Abdominal pain-Since conception Gradual onset Mild Localised Suprapubic No radiation No abvious aggrevating or relieving factor
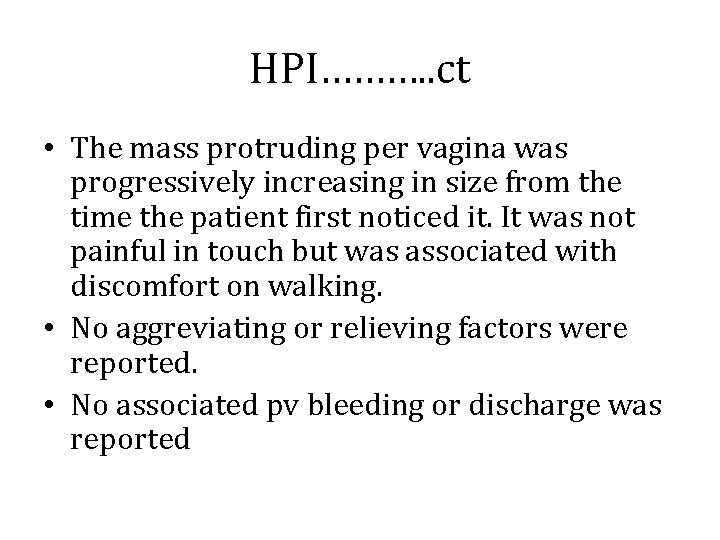
HPI………. . ct • The mass protruding per vagina was progressively increasing in size from the time the patient first noticed it. It was not painful in touch but was associated with discomfort on walking. • No aggreviating or relieving factors were reported. • No associated pv bleeding or discharge was reported
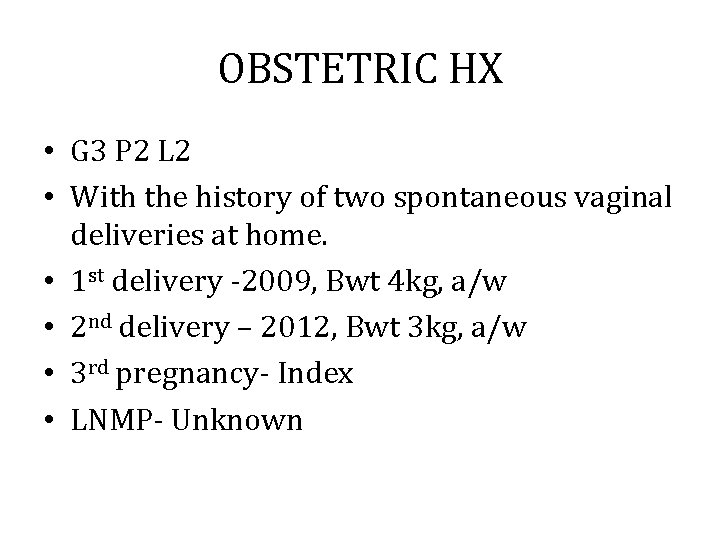
OBSTETRIC HX • G 3 P 2 L 2 • With the history of two spontaneous vaginal deliveries at home. • 1 st delivery -2009, Bwt 4 kg, a/w • 2 nd delivery – 2012, Bwt 3 kg, a/w • 3 rd pregnancy- Index • LNMP- Unknown
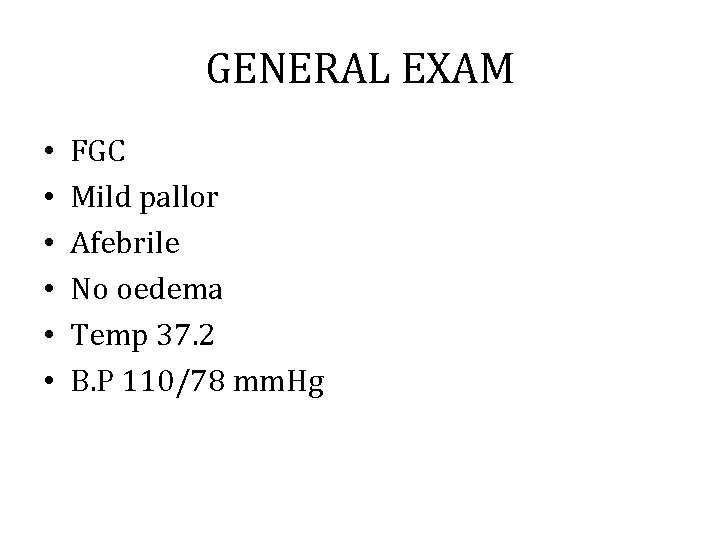
GENERAL EXAM • • • FGC Mild pallor Afebrile No oedema Temp 37. 2 B. P 110/78 mm. Hg
PV EXAM • FGM done • Cervix prolapsed past introitus, normal anterior and posterior walls • Smooth surface with no decubitus ulcer • Pelvic assessment couldn’t be performed due to obstruction by the mass • Baden walker classification grade 3

Per abdomen examination • • Fundal height – 27 cm Estimated fetal size- 2 kg Lie- longitudinal Presentation – Breech
Initial plan • • Admit Obstetric ward Hb- 6. 6 g/dl, BTX- 2 units -given IM Dexamethasone 6 mg 12 hourly- 24 hrs IM Mg. SO 4 6 G STAT Nifedipine 10 mg OD for 3 days Obstetric u/sound Haematinics
Obstetric u/sound • • BPP- 8/8 GA- 32 Weeks EFW- 1. 8 KG Placenta- fundal
Subsequent management • Patient stayed in the ward for two weeks and an elective c/section + BTL was done at GA (LUSS) of 34 weeks. • INTRA OP- LFI, 2 KG, Scored 8 in 1 st minute and 10 in 5 th minute • BTL was done
Follow up plan • Discharge plan -Kegel exercise -Avoid risk activities(Carrying heavy objects etc) -Follow up after 6 month for reevaluation and definitive treatment
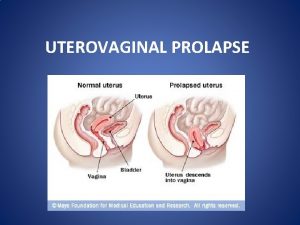
INTRODUCTION • The herniation of genital organs into or beyond the vaginal walls • Symptoms can impact – Daily activities – Sexual dysfunction – Exercise – Body image and sexuality
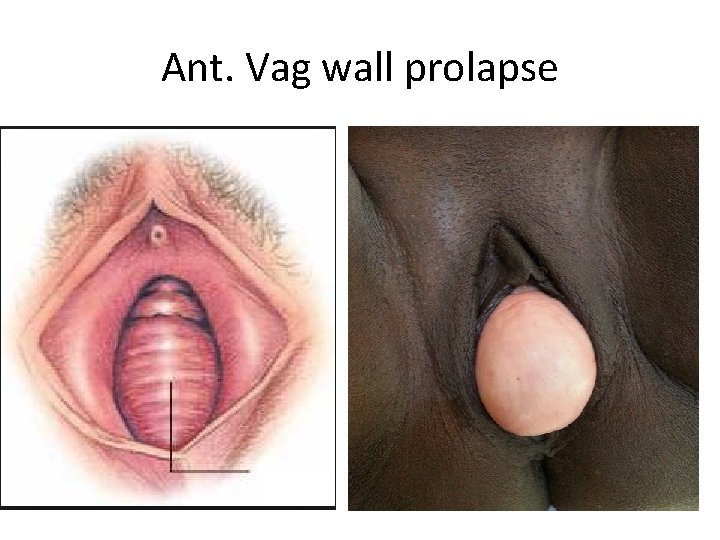
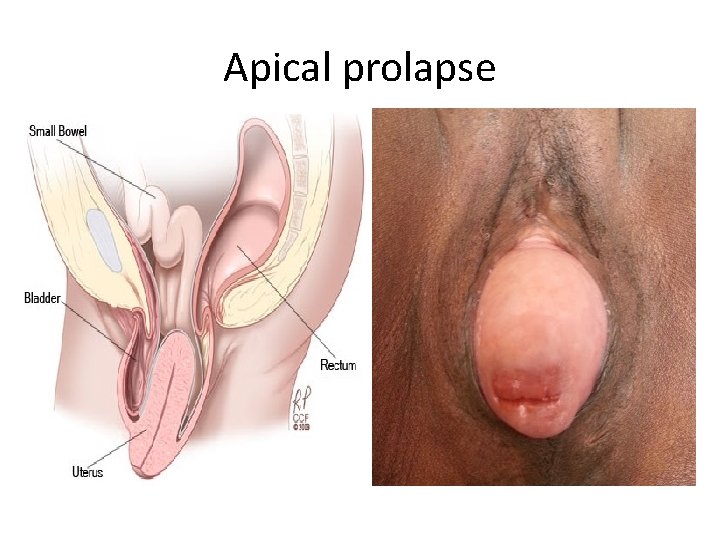
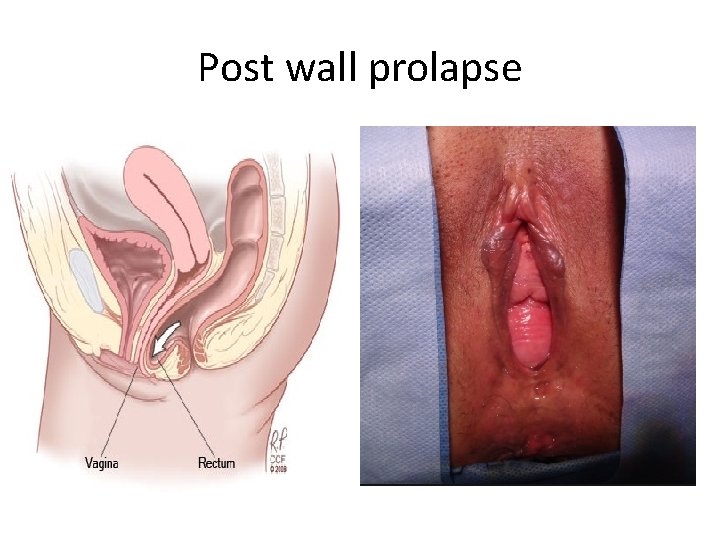
Types • POP is arbitrary divided into; § Anterior vaginal compartment prolapse eg cystocele § Apical compartment prolapse eg uterine, vaginal vault, enterocele § Posterior compartment prolapse eg rectocele • Uterine procidentia § Hernia of all three compartments through the vaginal introitus
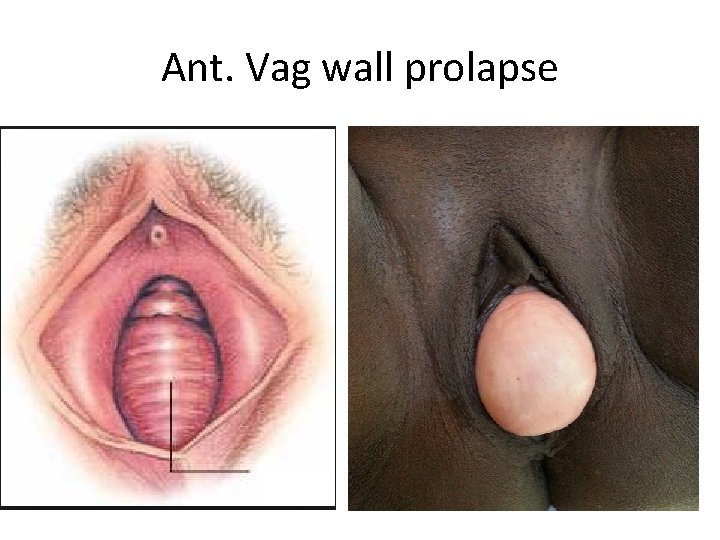
Ant. Vag wall prolapse
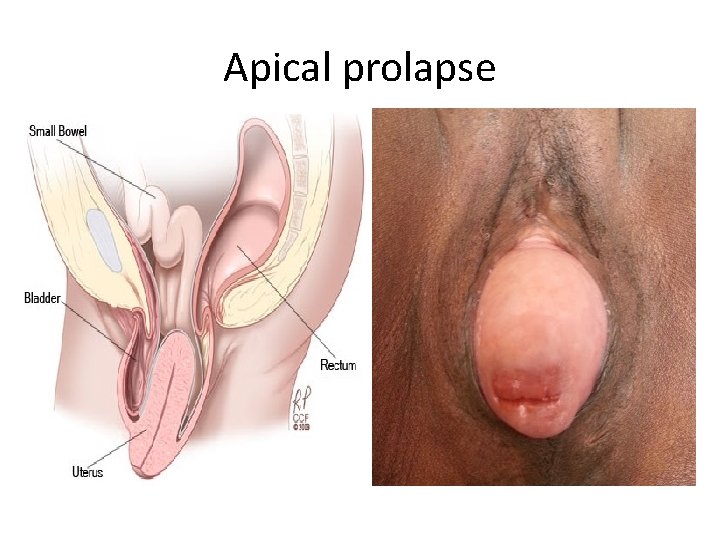
Apical prolapse
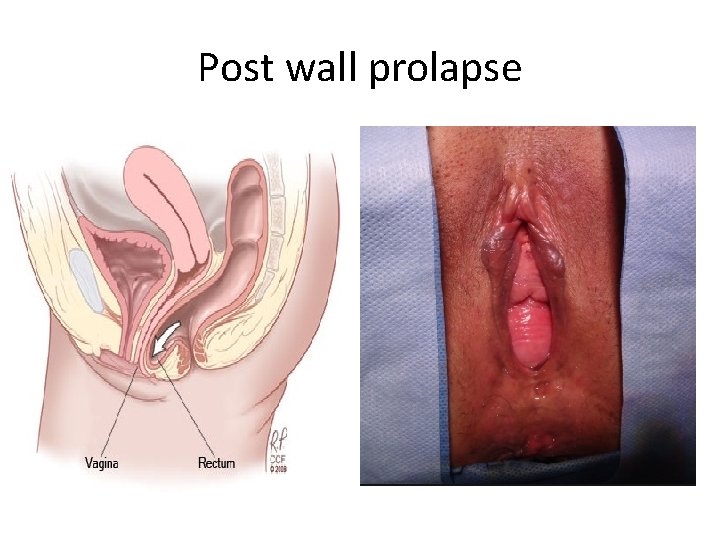
Post wall prolapse
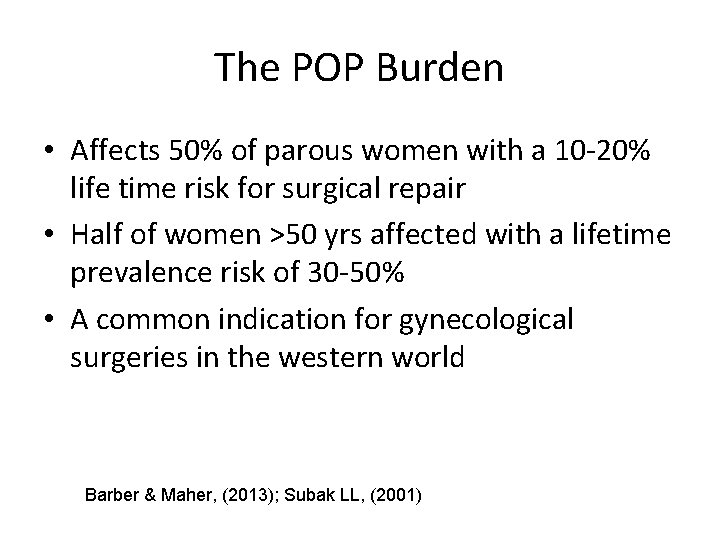
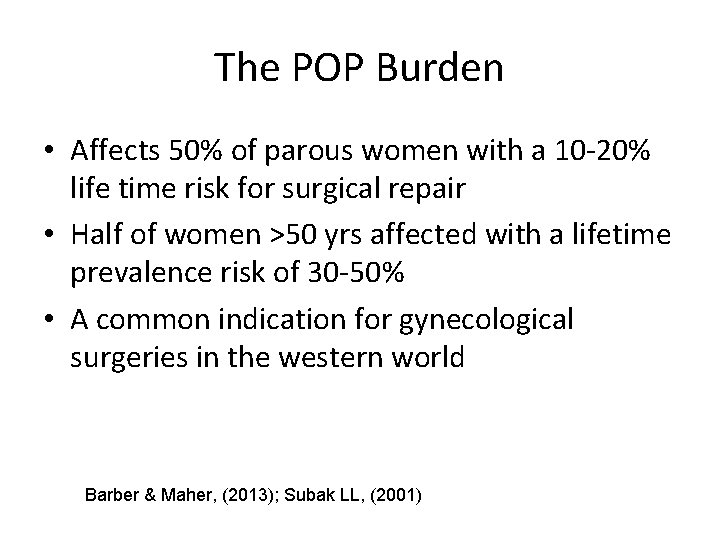
The POP Burden • Affects 50% of parous women with a 10 -20% life time risk for surgical repair • Half of women >50 yrs affected with a lifetime prevalence risk of 30 -50% • A common indication for gynecological surgeries in the western world Barber & Maher, (2013); Subak LL, (2001)
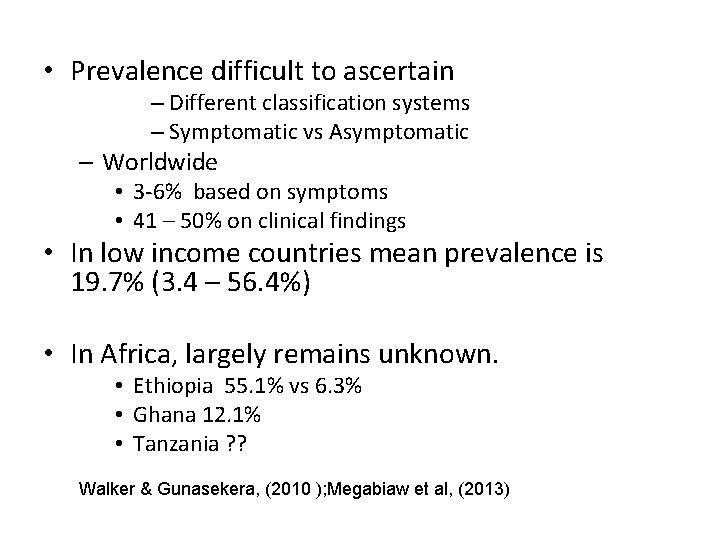
• Prevalence difficult to ascertain – Different classification systems – Symptomatic vs Asymptomatic – Worldwide • 3 -6% based on symptoms • 41 – 50% on clinical findings • In low income countries mean prevalence is 19. 7% (3. 4 – 56. 4%) • In Africa, largely remains unknown. • Ethiopia 55. 1% vs 6. 3% • Ghana 12. 1% • Tanzania ? ? Walker & Gunasekera, (2010 ); Megabiaw et al, (2013)
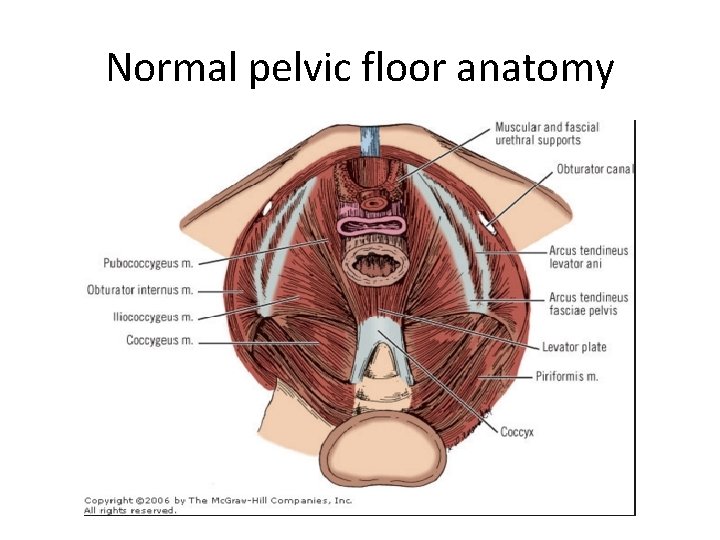
. . relevant anatomy • Pelvic support is provided by pelvic floor muscles and connective tissues in bony pelvis • Levator ani (pubococcygeus, puborectalis, iliococcygeus) → firm, elastic base for support. • Endopelvic fascia condensations eg uterosaccral, cardinal ligaments and arcus tendineus fascia →correct positioning of pelvic organs
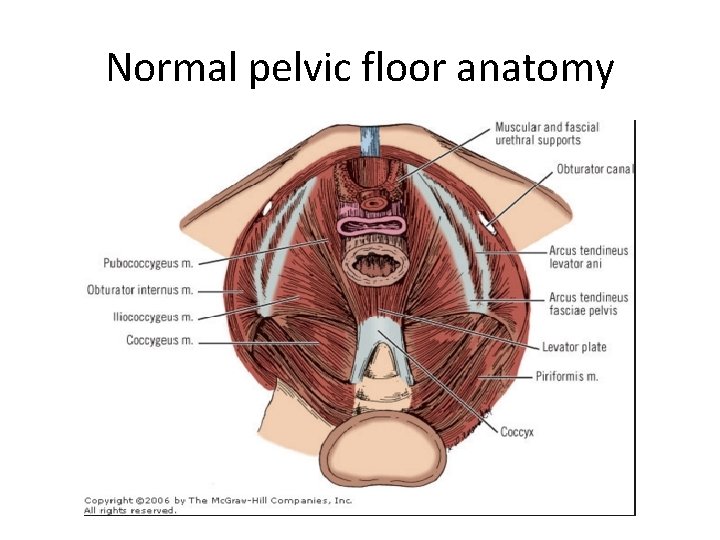
Normal pelvic floor anatomy
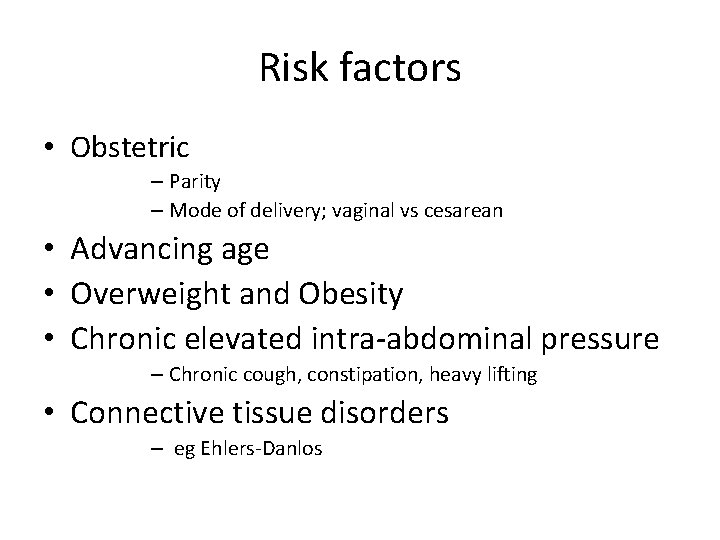
Risk factors • Obstetric – Parity – Mode of delivery; vaginal vs cesarean • Advancing age • Overweight and Obesity • Chronic elevated intra-abdominal pressure – Chronic cough, constipation, heavy lifting • Connective tissue disorders – eg Ehlers-Danlos
Clinical Manifestations • Specific symptoms – Vaginal bulge/something falling out of vagina – Vaginal or pelvic pressure • Associated symptoms – Urinary e. g. incontinence in early stages vs. obstructive in late stages – Defecatory e. g. constipation, fecal urgency/incontinence – Sexual dysfunction (fear, discomfort, embarrassment)
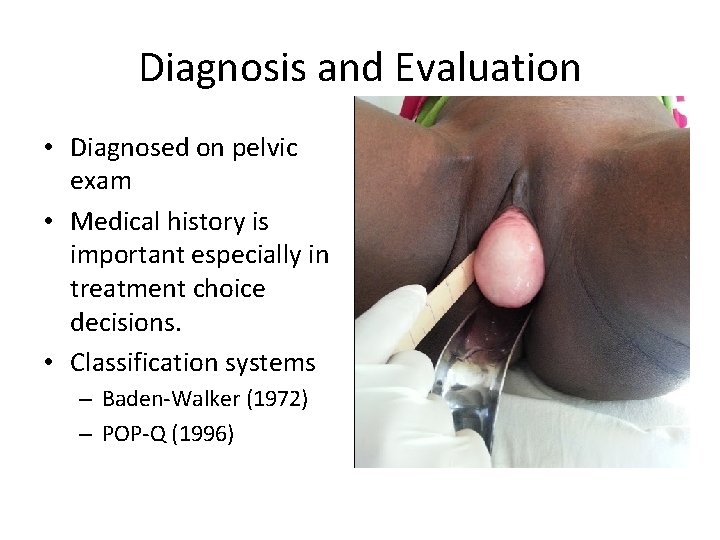
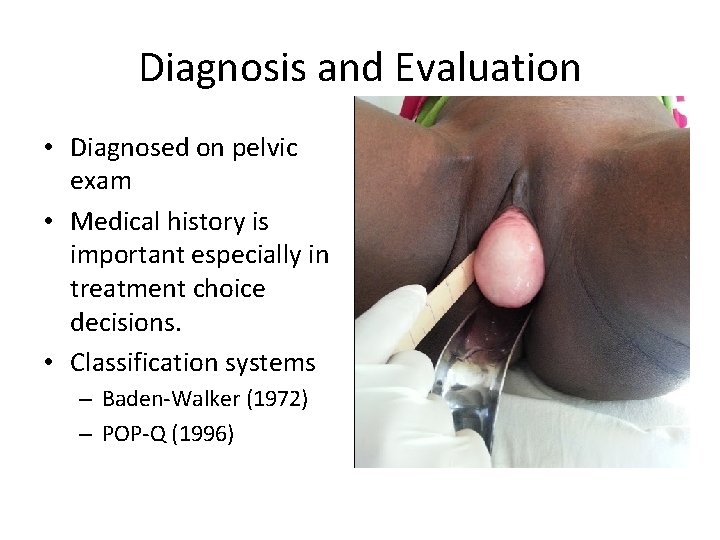
Diagnosis and Evaluation • Diagnosed on pelvic exam • Medical history is important especially in treatment choice decisions. • Classification systems – Baden-Walker (1972) – POP-Q (1996)
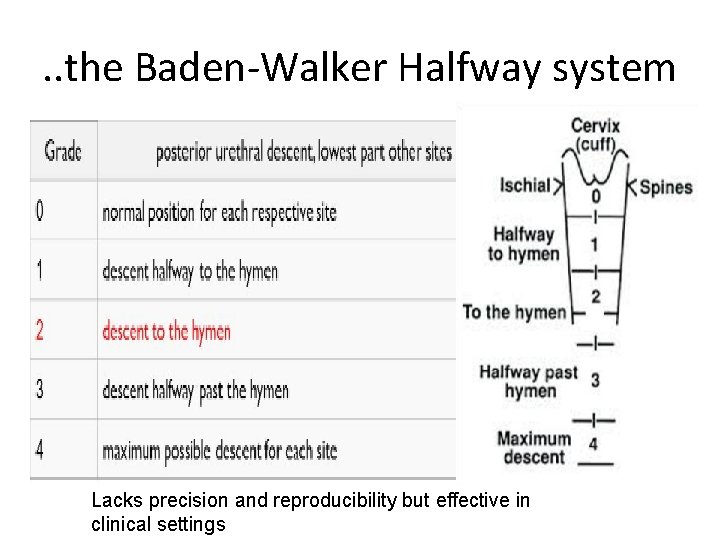
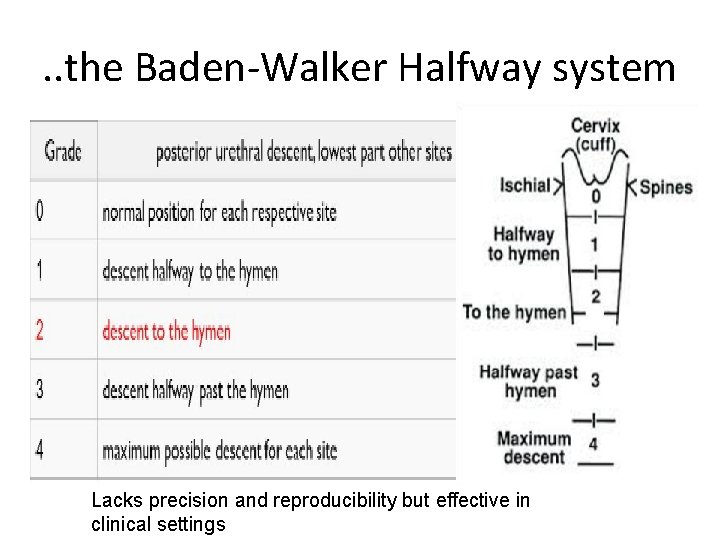
. . the Baden-Walker Halfway system Lacks precision and reproducibility but effective in clinical settings
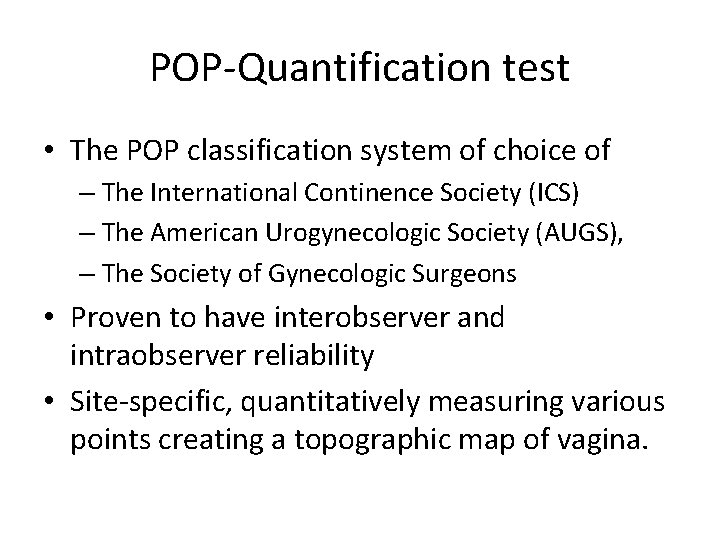
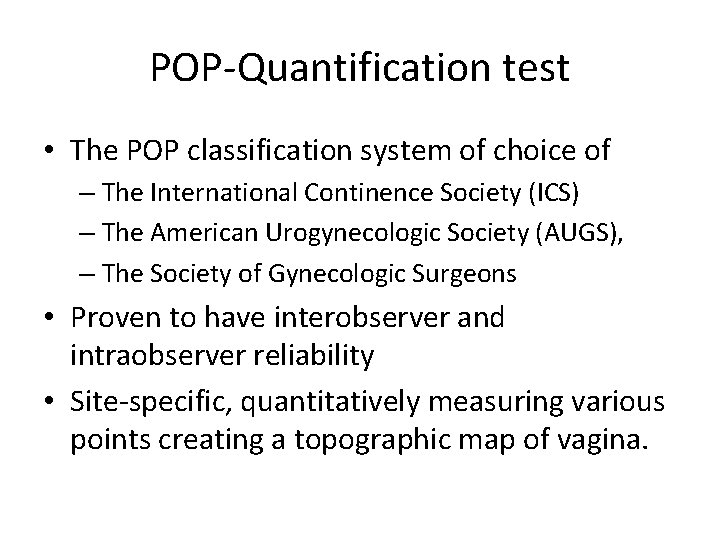
POP-Quantification test • The POP classification system of choice of – The International Continence Society (ICS) – The American Urogynecologic Society (AUGS), – The Society of Gynecologic Surgeons • Proven to have interobserver and intraobserver reliability • Site-specific, quantitatively measuring various points creating a topographic map of vagina.
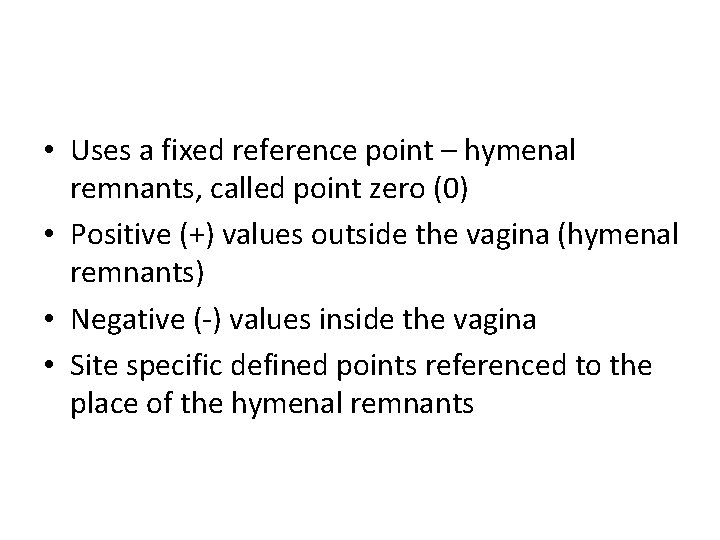
• Uses a fixed reference point – hymenal remnants, called point zero (0) • Positive (+) values outside the vagina (hymenal remnants) • Negative (-) values inside the vagina • Site specific defined points referenced to the place of the hymenal remnants

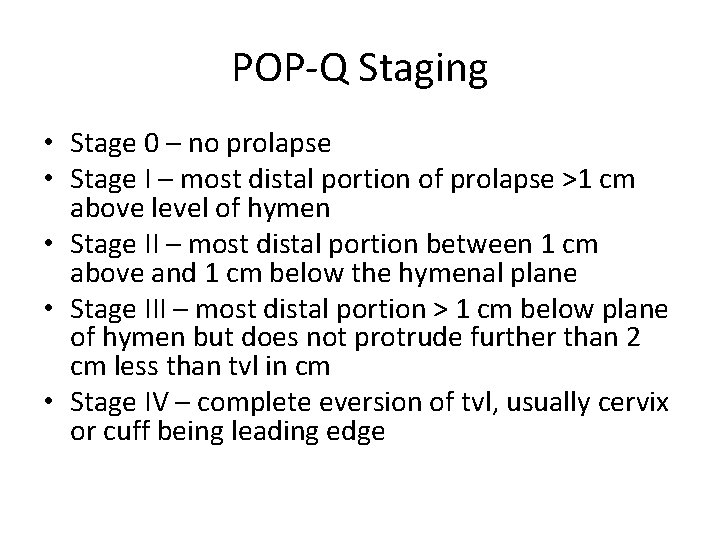
POP-Q Staging • Stage 0 – no prolapse • Stage I – most distal portion of prolapse >1 cm above level of hymen • Stage II – most distal portion between 1 cm above and 1 cm below the hymenal plane • Stage III – most distal portion > 1 cm below plane of hymen but does not protrude further than 2 cm less than tvl in cm • Stage IV – complete eversion of tvl, usually cervix or cuff being leading edge
MANAGEMENT OF UTERINE PROLAPSE • Goal of treatment -Alleviate symptoms -Restore anatomical structure -Restore/Preserve sexual function • Choice of treatment depends on -Symptoms severity -Prolapse severity -Fertility desire
MNGT OF UTERINE PROLAPSE • Conservative management -Asymptomatic patient -Grade I & II -Patient desire -Address risky condition( Heavy weight lifting, coughing, constipation, Obesity etc) -Employ use of Kegel exercise
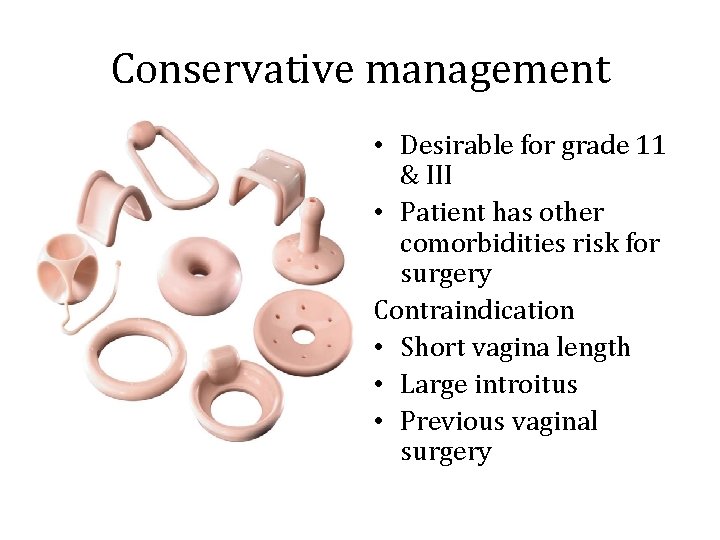
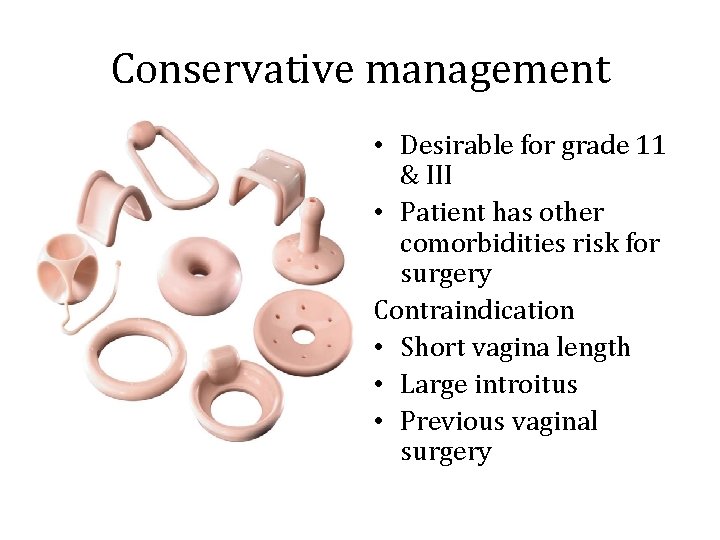
Conservative management • Desirable for grade 11 & III • Patient has other comorbidities risk for surgery Contraindication • Short vagina length • Large introitus • Previous vaginal surgery
Surgery • Goals -Provide mechanical support -Suspension -Obliterative -Surgical excision-NOT VERY EFFECTIVE!!!
Suspension procedures • Material used Synthetic material-Mesh (Polyprolene mesh) -Graft Xenograft Allograft-Harvested rectus fascia
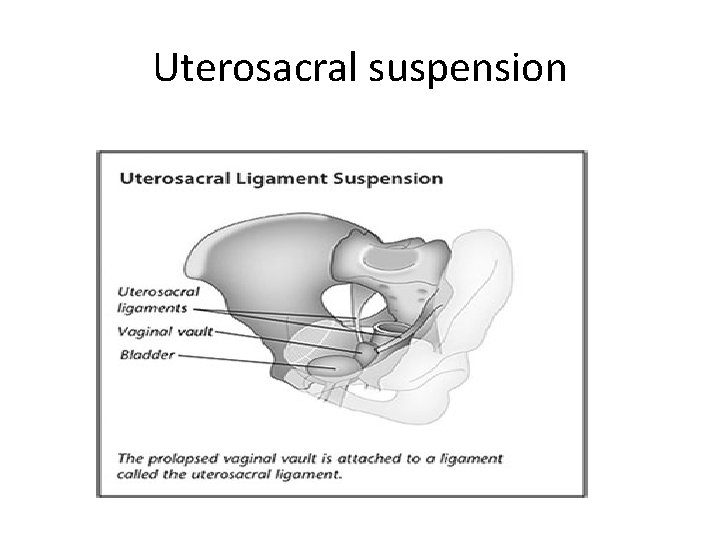
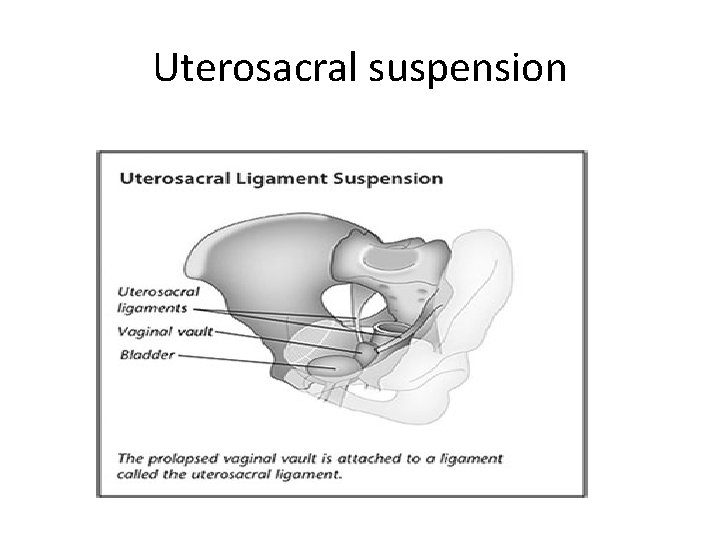
Uterosacral suspension
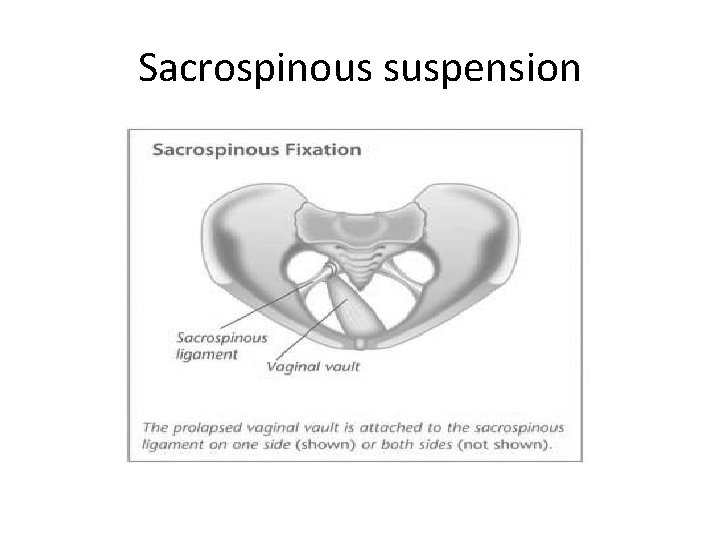
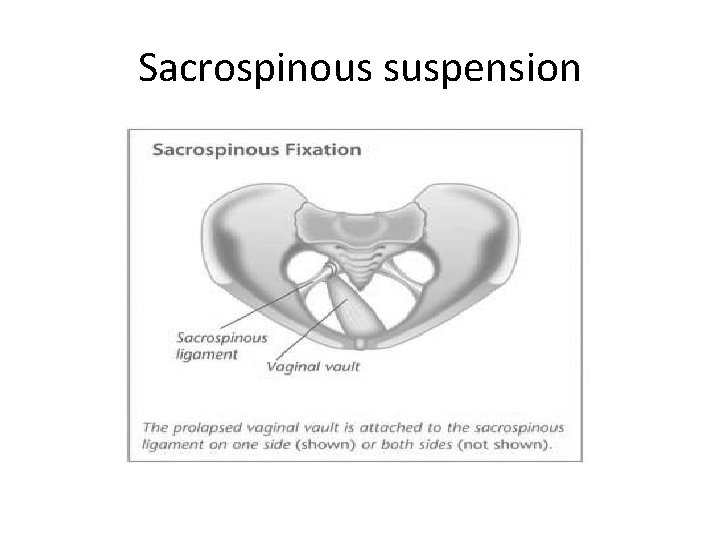
Sacrospinous suspension
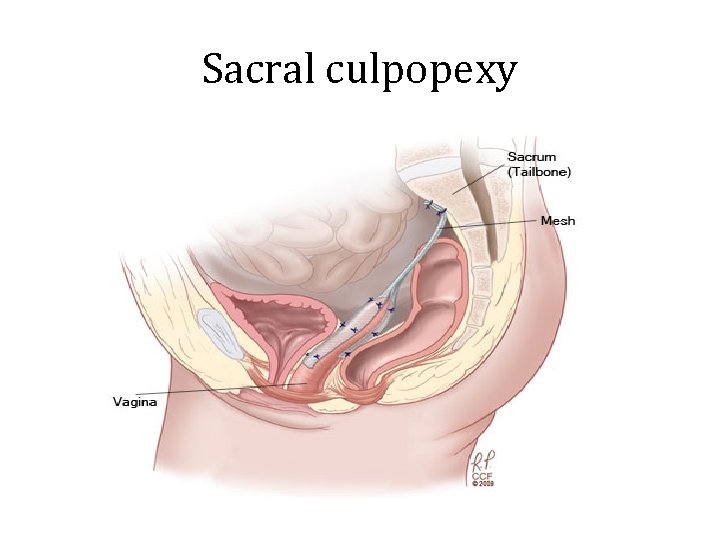
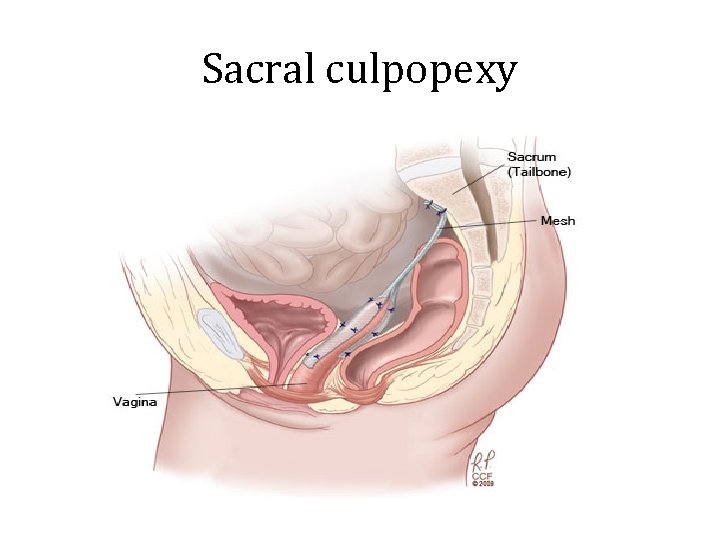
Sacral culpopexy
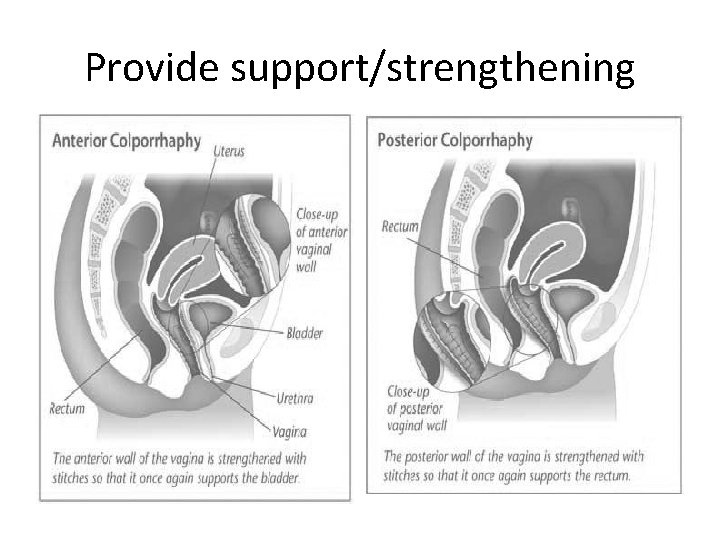
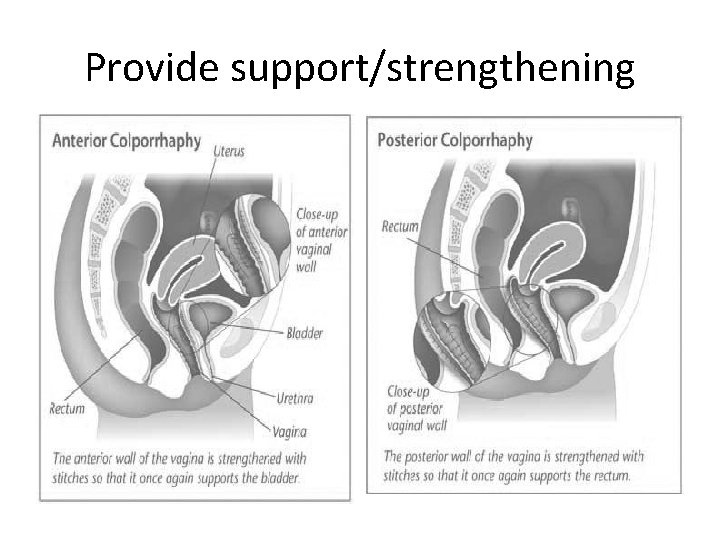
Provide support/strengthening
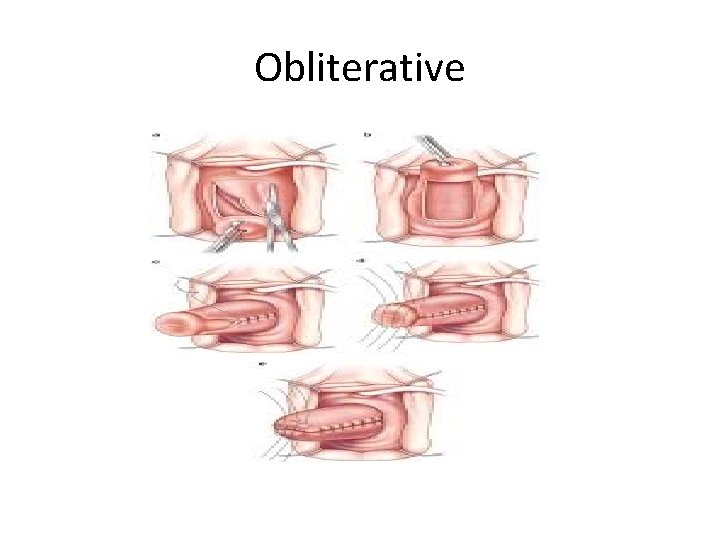
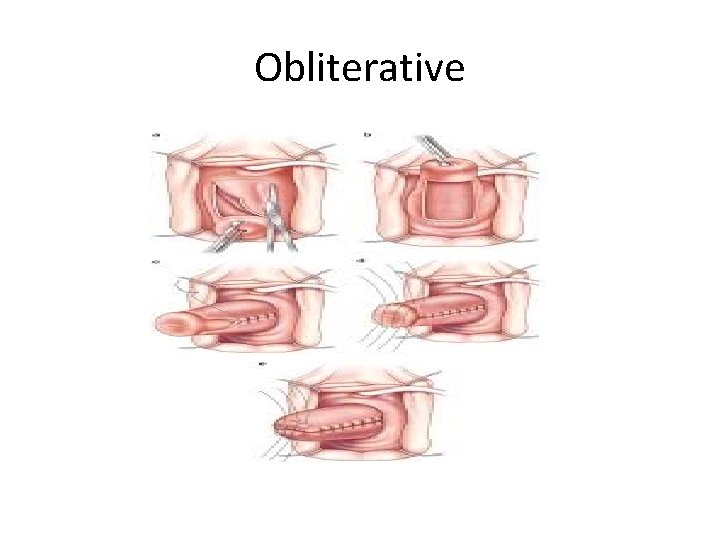
Obliterative
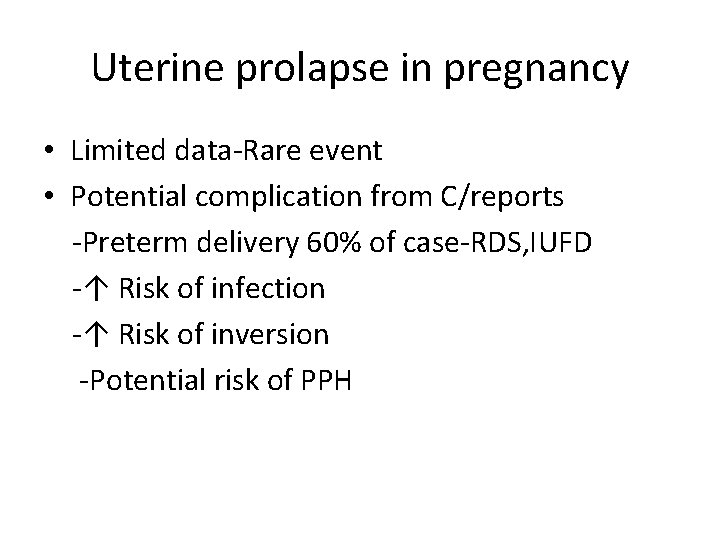
Uterine prolapse in pregnancy • Limited data-Rare event • Potential complication from C/reports -Preterm delivery 60% of case-RDS, IUFD -↑ Risk of infection -↑ Risk of inversion -Potential risk of PPH
Uterine prolapse in pregnancy • Management -Reduce risk of complication Enhance fetal lung maturation Tocolytic until viability attained Bed rest Pessaries if presents early
THE END
 Anterflexio
Anterflexio Left uterine displacement
Left uterine displacement Uterine prolapse treatment non surgical
Uterine prolapse treatment non surgical Uterine prolapse stages pictures
Uterine prolapse stages pictures Types of uterine prolapse
Types of uterine prolapse Pictures of spotting during pregnancy
Pictures of spotting during pregnancy Uterotonics
Uterotonics Nursing diagnosis for cord prolapse
Nursing diagnosis for cord prolapse Vaginak prolapse
Vaginak prolapse Vagina prolapse
Vagina prolapse Vaginal vault prolapse
Vaginal vault prolapse Spinal cord extends from
Spinal cord extends from Child abuse
Child abuse Prolapsed umbilical cord
Prolapsed umbilical cord Ampulla uterus
Ampulla uterus Uterus reaches the level of umbilicus at
Uterus reaches the level of umbilicus at Uterine volume by age
Uterine volume by age Dr mabel marotta
Dr mabel marotta Dr khani
Dr khani What does infected lochia look like
What does infected lochia look like Bimanual compression
Bimanual compression Expulsion
Expulsion Hydroceplus
Hydroceplus Hauteur utérine
Hauteur utérine Abnormal uterine bleeding definition figo
Abnormal uterine bleeding definition figo Hypertonic vs hypotonic uterine dysfunction
Hypertonic vs hypotonic uterine dysfunction Uterus seal
Uterus seal Uterine bleeding
Uterine bleeding Perdarahan post partum
Perdarahan post partum Uterine orifice
Uterine orifice Abnormal uterine bleeding definition figo
Abnormal uterine bleeding definition figo Tphandrl
Tphandrl Tortuous basilar artery symptoms
Tortuous basilar artery symptoms Uterus
Uterus Pph
Pph Phase 2 of parturition
Phase 2 of parturition Biohelminthes
Biohelminthes Female genitalia labeled
Female genitalia labeled Active labor contraction
Active labor contraction Uterine stimulants and relaxants
Uterine stimulants and relaxants Palm coein classification
Palm coein classification Normal endometrial thickness postmenopausal
Normal endometrial thickness postmenopausal Thickening of uterine lining
Thickening of uterine lining Uterine compression sutures
Uterine compression sutures Abnormal uterine bleeding
Abnormal uterine bleeding Uterine inversion
Uterine inversion