RECTAL PROLAPSE Rectal Prolapse Prolapse of the rectum




- Slides: 47
RECTAL PROLAPSE
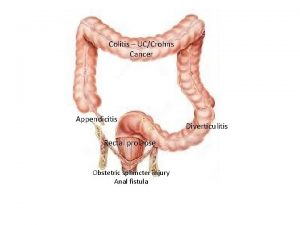
Rectal Prolapse: Prolapse of the rectum mainly two types: Partial or incomplete prolapse (procidentia) when the mucous membrane lining the anal canal protrudes through the anus only. Complete prolapse in which the whole thickness of the bowel protudes through the anus. Rectal prolapse occurs most often at extremes of life e. g, in children between 1 -5 years of age and elderly people. More
In children: Aetiology the predisposing causes are: - The vertical straight course of the rectum. Reduction of supporting fat in the ischiorectal fossa. Straining at stool. Chronic cough.
In adult: the predisposing causes depend on type of the prolapse. Partial prolapse Advance degree of prolapsing piles. Loss of sphincteric tone. Straining from urethral obstruction. Operations for fistula. Complete prolapse is generally regarded as sliding hernia of the recto vesical or recto vaginal pouch due to stretching of the levator from pregnancy, obesity.
Prolapse is first noted during defaecation. Discomfort during defaecation. Bleeding. Mucous discharge. Bowel habit irregular and may lead to incontinence.
Examining for rectal prolapse w Most NOT evident in lying position as rest w Ask patient to bear down – most still not evident w Need to examine after straining on the toilet for 1 -2 minutes – lean forward – observe from behind – estimate in centimetres - ? full thickness circumferential, or partial mucosal only?
Examining for rectal prolapse
Ano-rectal digital examination w Resting tone (low = IAS problem) w Squeeze pressure (low = EAS problem) w Co-ordination w Sensation (? Neurological dysfunction) w Assessment stops here for MOST patients
Radiologic examination
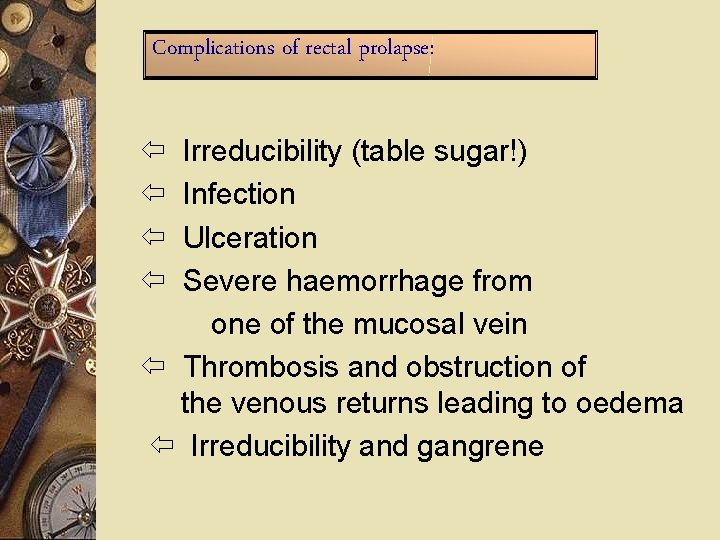
Complications of rectal prolapse: Irreducibility (table sugar!) Infection Ulceration Severe haemorrhage from one of the mucosal vein Thrombosis and obstruction of the venous returns leading to oedema Irreducibility and gangrene
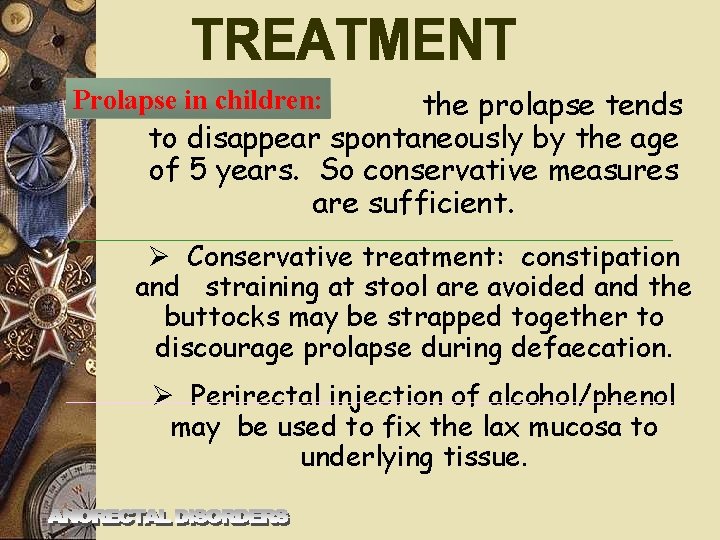
the prolapse tends to disappear spontaneously by the age of 5 years. So conservative measures are sufficient. Prolapse in children: Conservative treatment: constipation and straining at stool are avoided and the buttocks may be strapped together to discourage prolapse during defaecation. Perirectal injection of alcohol/phenol may be used to fix the lax mucosa to underlying tissue.
Partial prolapse: Injections of 5% phenol in oil in submucosa. 10 -15 ml total. Electrical stimulation with sphincteric exercises.
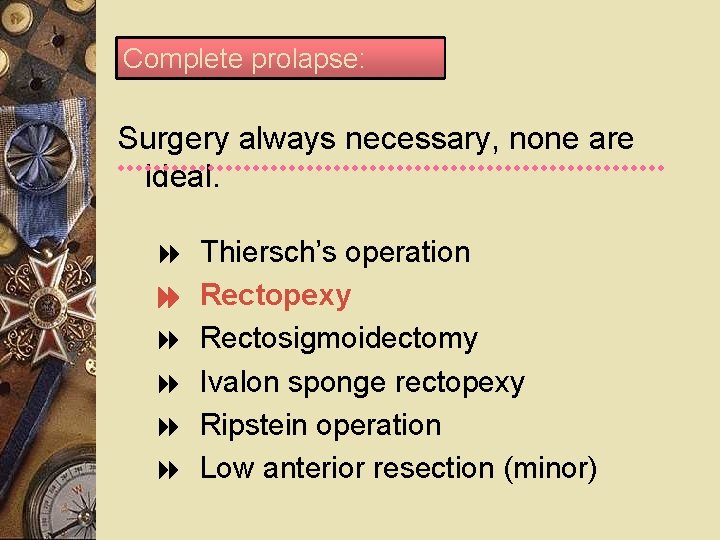
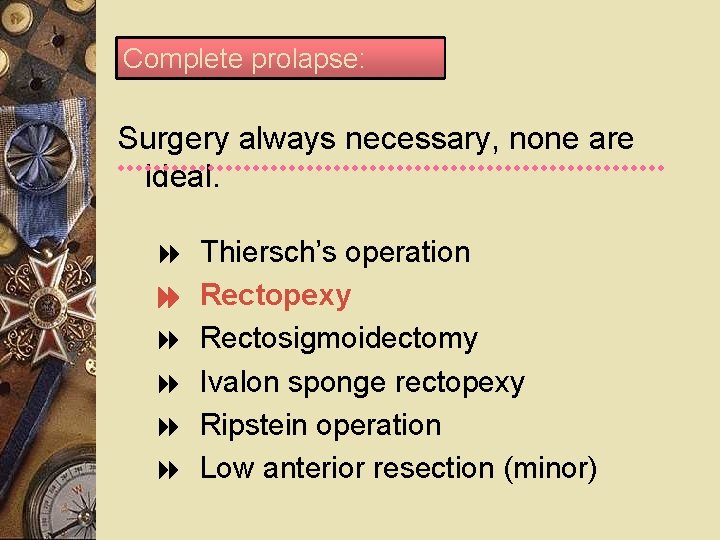
Complete prolapse: Surgery always necessary, none are ideal. Thiersch’s operation Rectopexy Rectosigmoidectomy Ivalon sponge rectopexy Ripstein operation Low anterior resection (minor)

Rectal cancer
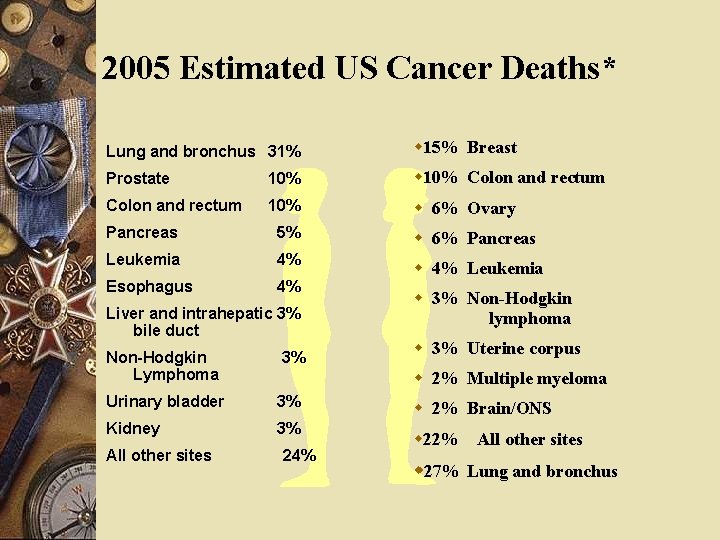
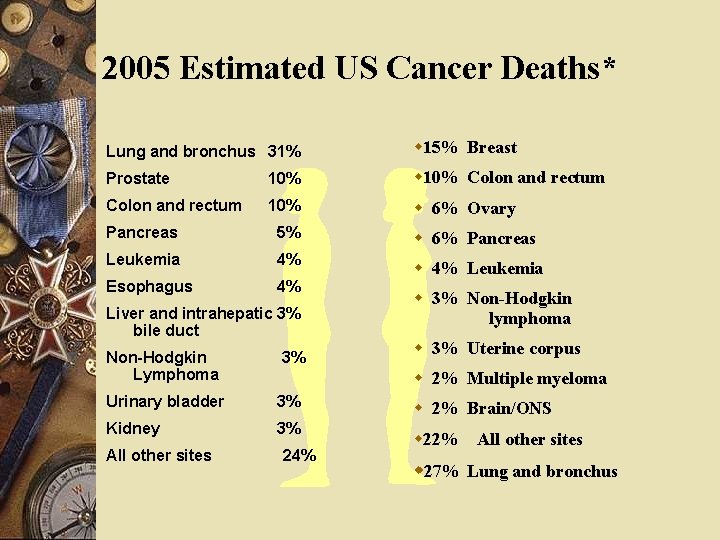
2005 Estimated US Cancer Deaths* Lung and bronchus 31% w 15% Breast Prostate 10% w 10% Colon and rectum 10% w 6% Ovary Pancreas 5% w 6% Pancreas Leukemia 4% Esophagus 4% w 4% Leukemia Liver and intrahepatic 3% bile duct Non-Hodgkin Lymphoma 3% w 3% Uterine corpus w 2% Multiple myeloma Urinary bladder 3% Kidney 3% All other sites w 3% Non-Hodgkin lymphoma 24% w 2% Brain/ONS w 22% All other sites w 27% Lung and bronchus
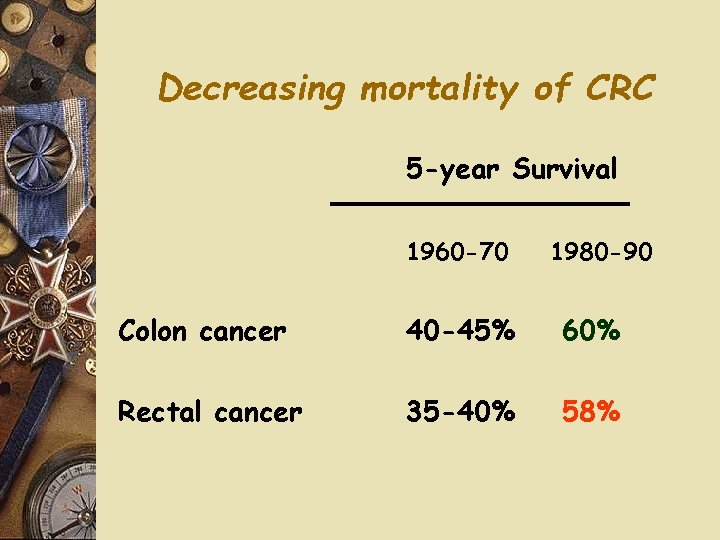
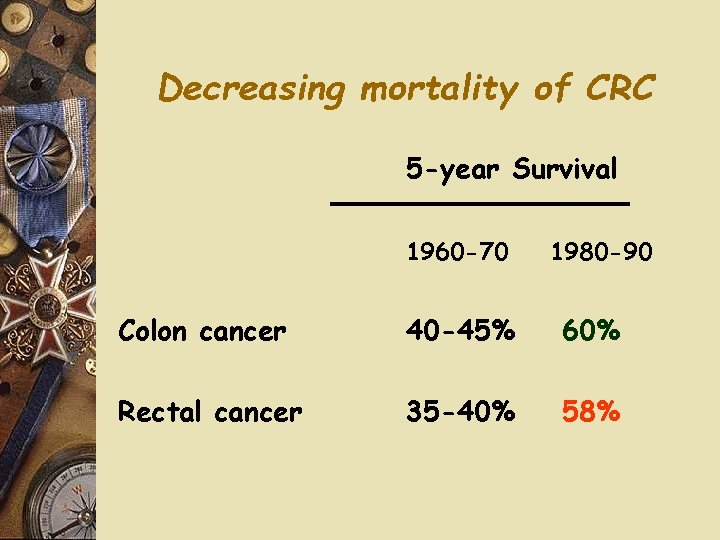
Decreasing mortality of CRC 5 -year Survival 1960 -70 1980 -90 Colon cancer 40 -45% 60% Rectal cancer 35 -40% 58%

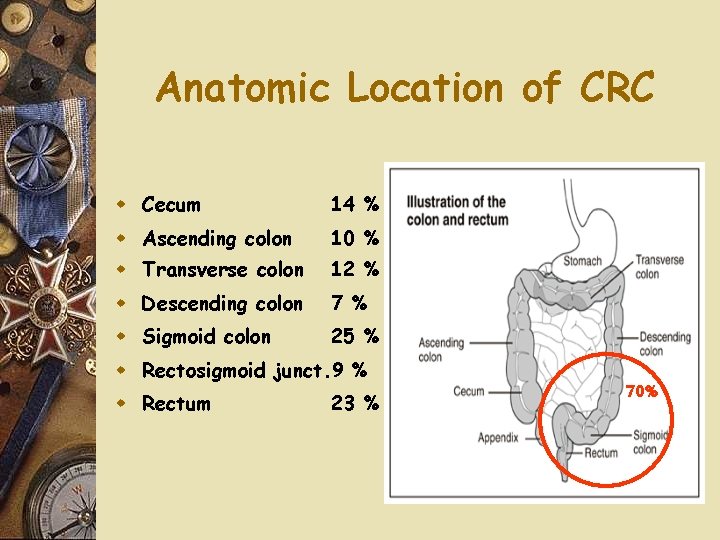
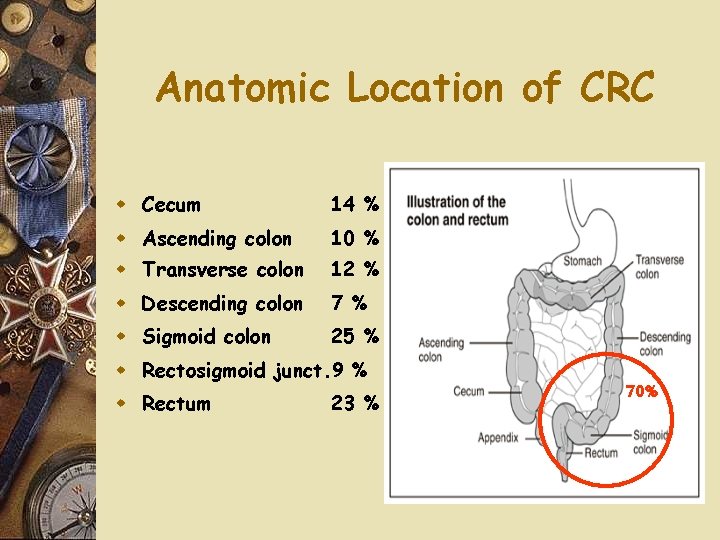
Anatomic Location of CRC w Cecum 14 % w Ascending colon 10 % w Transverse colon 12 % w Descending colon 7 % w Sigmoid colon 25 % w Rectosigmoid junct. 9 % w Rectum 23 % 70%
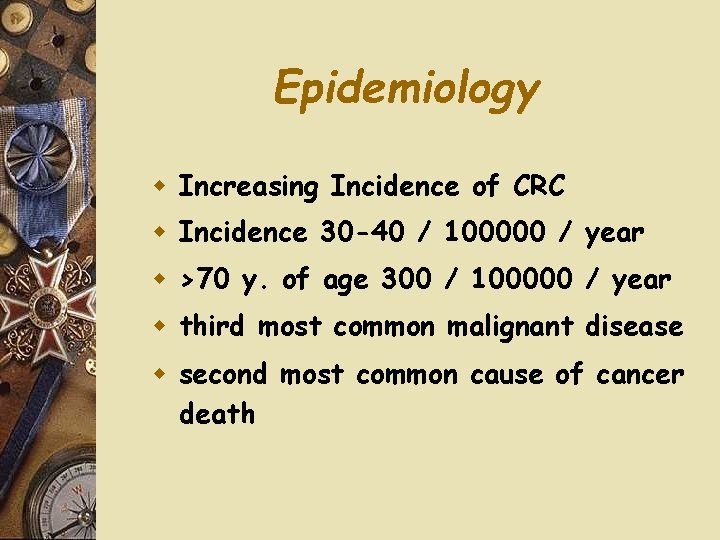
Epidemiology w Increasing Incidence of CRC w Incidence 30 -40 / 100000 / year w >70 y. of age 300 / 100000 / year w third most common malignant disease w second most common cause of cancer death
Epidemiology w 70% of CRC are resectable at diagnosis w Mortality has decreased
Ethiology w Diet: fibers, vit E, vit C w Polips (adenomatous) w IBD – more then 10 years of progression w Smoking w Cyclooxigenase inhibitors w Genetic cancer
WHO Classification of CRC w w w w w Adenocarcinoma in situ / severe dysplasia Adenocarcinoma Mucinous (colloid) adenocarcinoma (>50% mucinous) Signet ring cell carcinoma (>50% signet ring cells) Squamous cell (epidermoid) carcinoma Adenosquamous carcinoma Small-cell (oat cell) carcinoma Medullary carcinoma Undifferentiated Carcinoma
Symptoms Bleeding per anum Sensation of incomplete bladder empting Tenesmus Abdominal pain Palpable rectal tumor w Pacienţi în stadii avansate: pierdere ponderală, hepatomegalie, icter, anemie. w Examenul fizic include: aprecierea stării generale, a prezenţei adenopatiilor periferice şi a hepatomegaliei. !!! RECTAL EXAMINATION
Investigations w Staging: - Recto- and colonoscopy - Barium enema - CT - MRI - EUS
w RECTOSCOPY w COLONOSCOPY + BIOPSY Indications - Suggestive images on barium enema - Suggestive symptoms of colonic cancer - Screening -After polipectomy
COMPUTER-TOMOGRAFIA (aspecte CR)
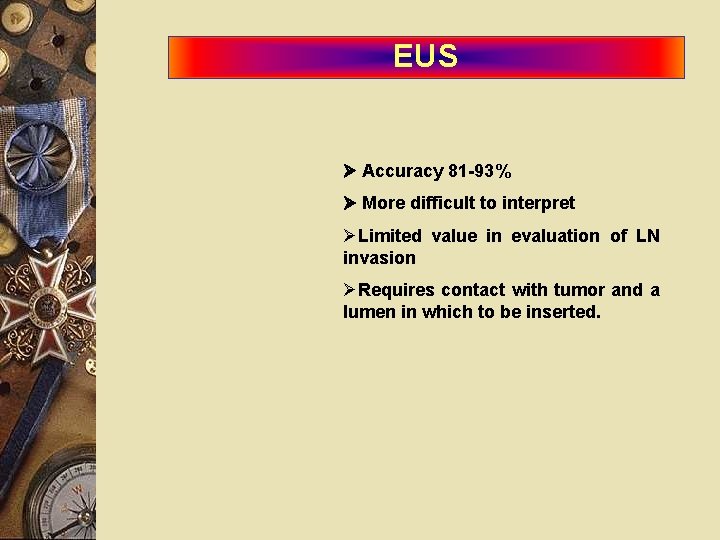
EUS Accuracy 81 -93% More difficult to interpret Limited value in evaluation of LN invasion Requires contact with tumor and a lumen in which to be inserted.

MRI – standard of care
Tumor markers w CEA w CA 19 -9 – Dynamic may be significant for recurrence
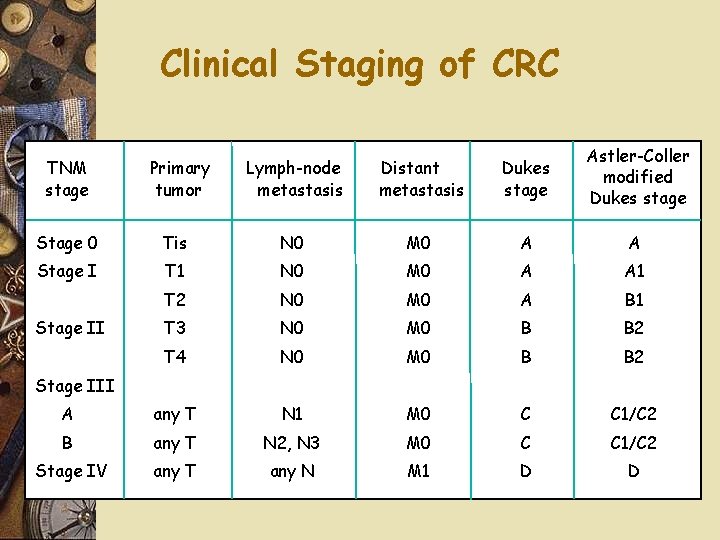
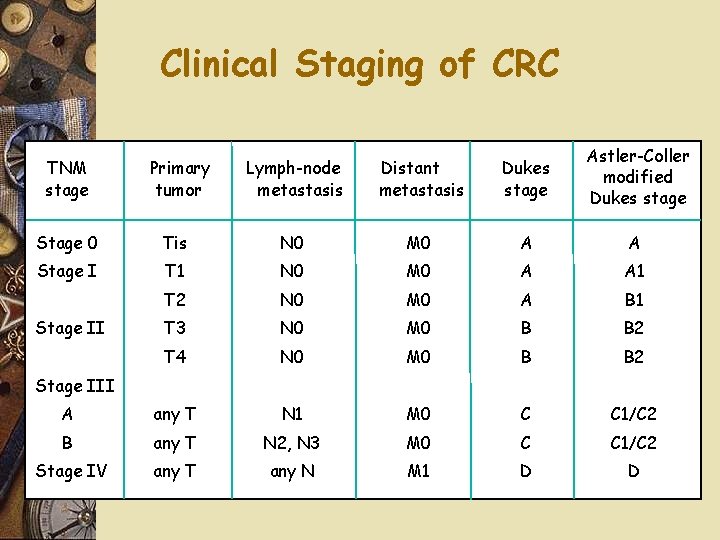
Clinical Staging of CRC TNM stage Primary tumor Lymph-node metastasis Distant metastasis Dukes stage Astler-Coller modified Dukes stage Stage 0 Tis N 0 M 0 A A Stage I T 1 N 0 M 0 A A 1 T 2 N 0 M 0 A B 1 T 3 N 0 M 0 B B 2 T 4 N 0 M 0 B B 2 A any T N 1 M 0 C C 1/C 2 B any T N 2, N 3 M 0 C C 1/C 2 Stage IV any T any N M 1 D D Stage III
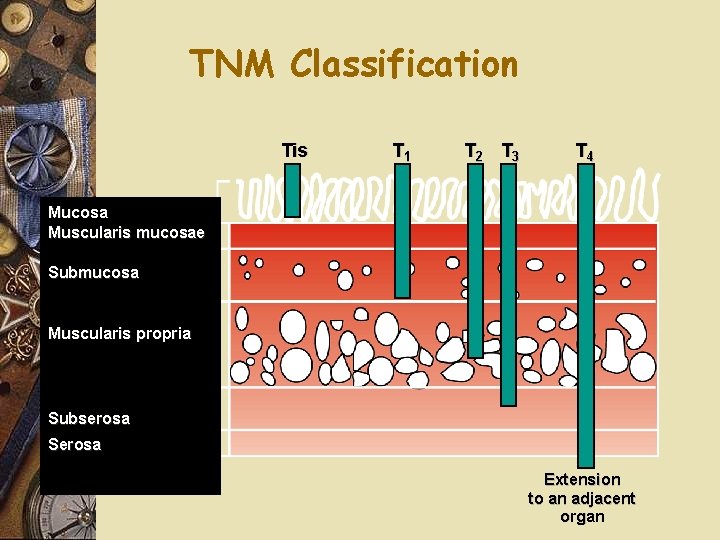
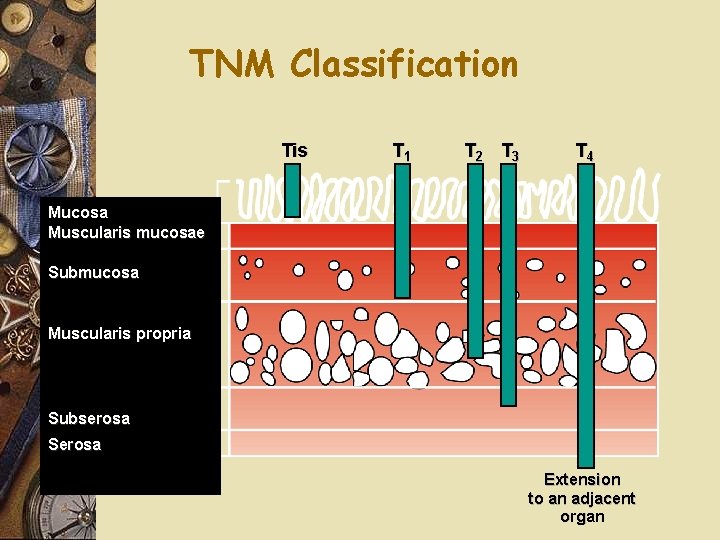
TNM Classification Tis T 1 T 2 T 3 T 4 Mucosa Muscularis mucosae Submucosa Muscularis propria Subserosa Serosa Extension to an adjacent organ
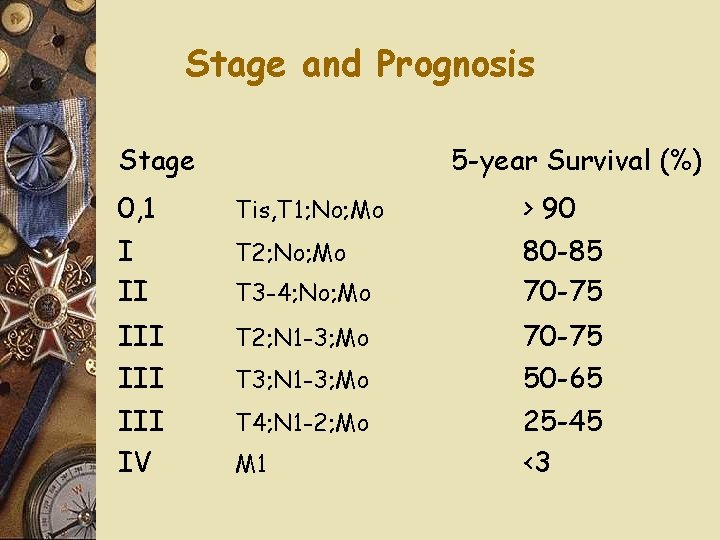
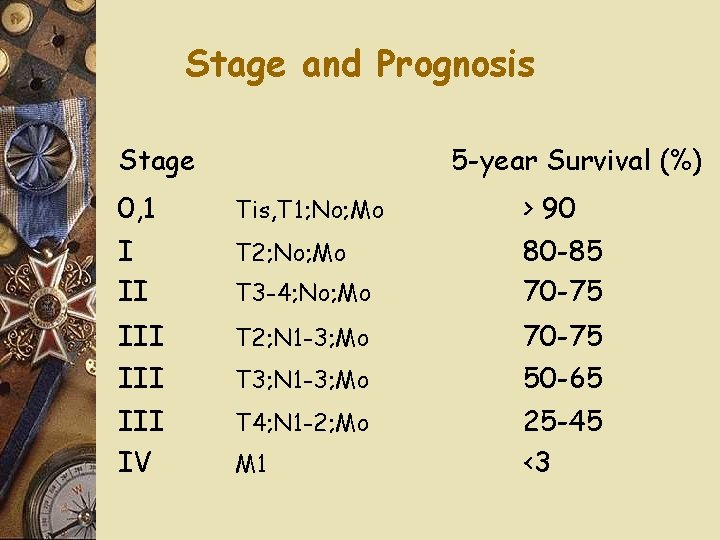
Stage and Prognosis Stage 5 -year Survival (%) 0, 1 Tis, T 1; No; Mo > 90 I II T 2; No; Mo 80 -85 70 -75 III T 2; N 1 -3; Mo III IV T 4; N 1 -2; Mo T 3 -4; No; Mo T 3; N 1 -3; Mo M 1 70 -75 50 -65 25 -45 <3
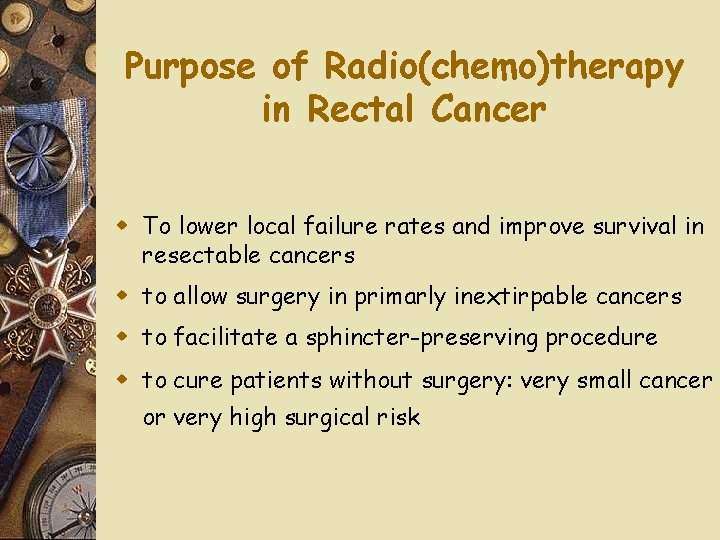
Purpose of Radio(chemo)therapy in Rectal Cancer w To lower local failure rates and improve survival in resectable cancers w to allow surgery in primarly inextirpable cancers w to facilitate a sphincter-preserving procedure w to cure patients without surgery: very small cancer or very high surgical risk
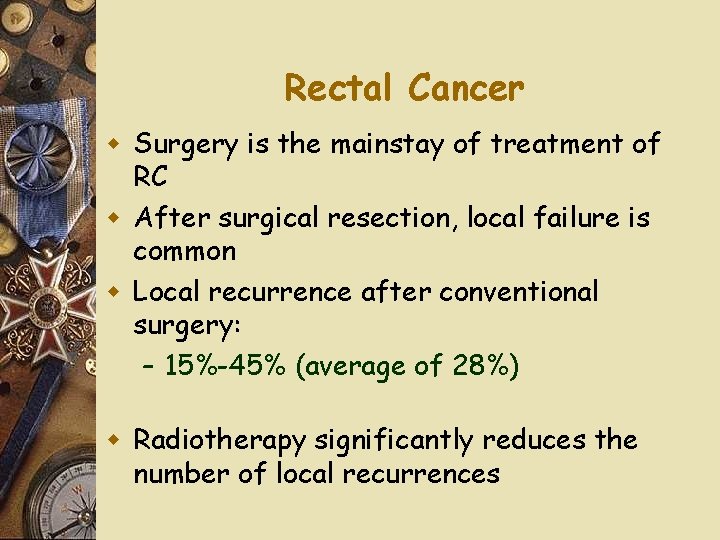
Rectal Cancer w Surgery is the mainstay of treatment of RC w After surgical resection, local failure is common w Local recurrence after conventional surgery: – 15%-45% (average of 28%) w Radiotherapy significantly reduces the number of local recurrences
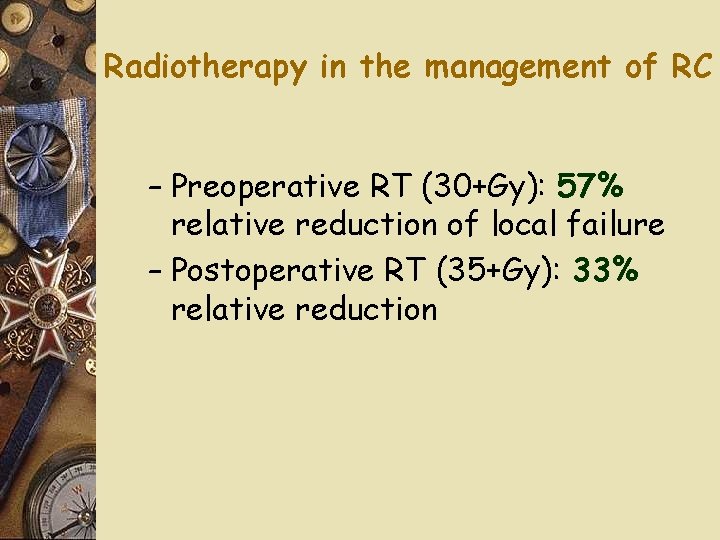
Radiotherapy in the management of RC – Preoperative RT (30+Gy): 57% relative reduction of local failure – Postoperative RT (35+Gy): 33% relative reduction
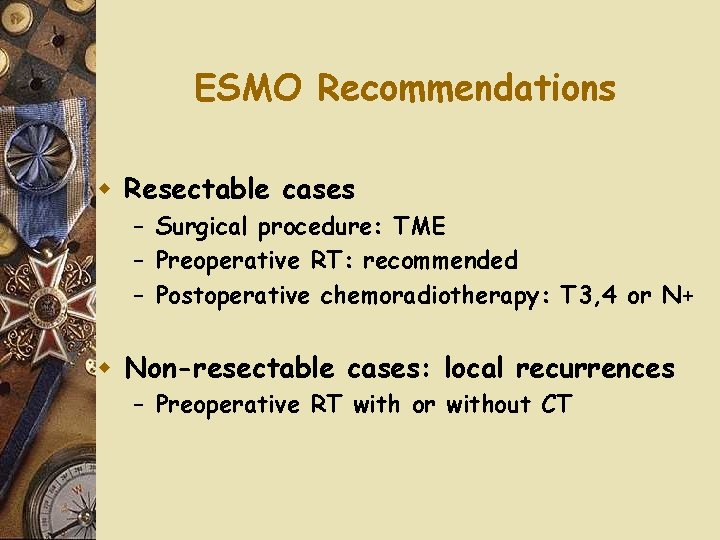
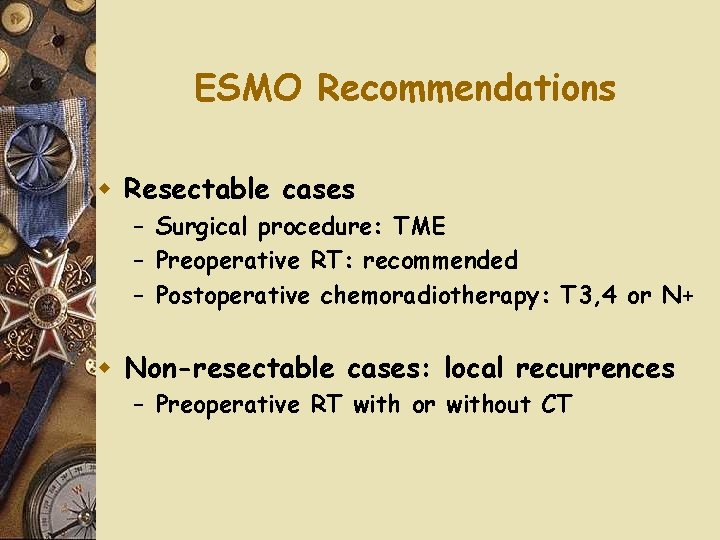
ESMO Recommendations w Resectable cases – Surgical procedure: TME – Preoperative RT: recommended – Postoperative chemoradiotherapy: T 3, 4 or N+ w Non-resectable cases: local recurrences – Preoperative RT with or without CT
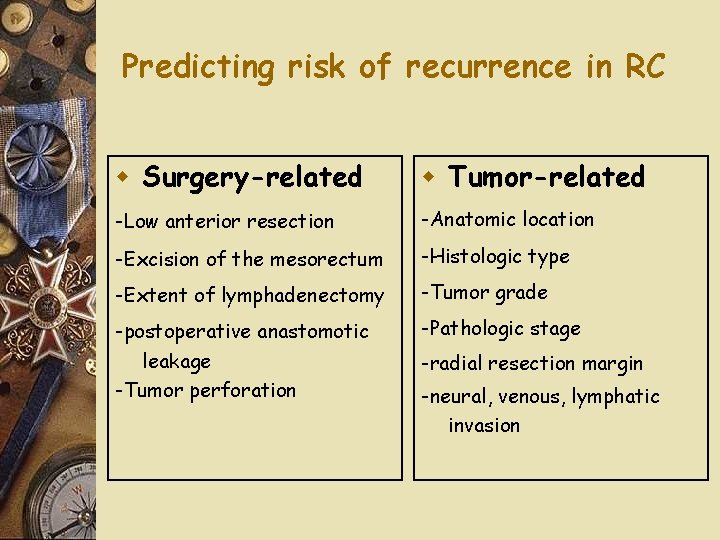
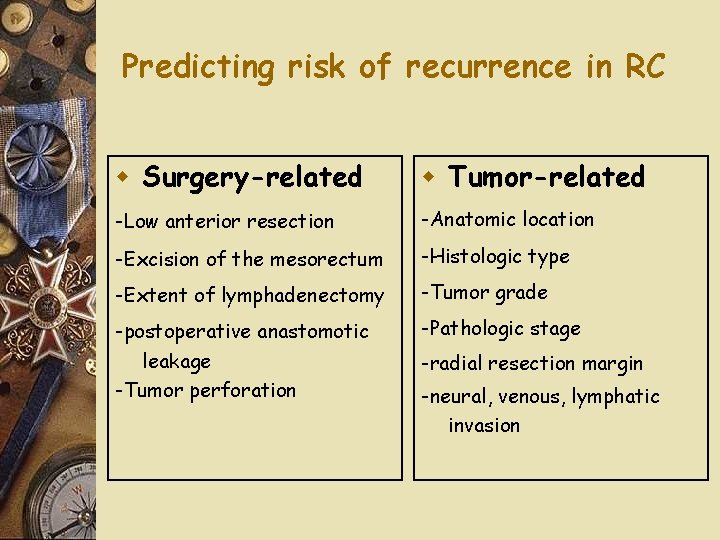
Predicting risk of recurrence in RC w Surgery-related w Tumor-related -Low anterior resection -Anatomic location -Excision of the mesorectum -Histologic type -Extent of lymphadenectomy -Tumor grade -postoperative anastomotic -Pathologic stage leakage -Tumor perforation -radial resection margin -neural, venous, lymphatic invasion
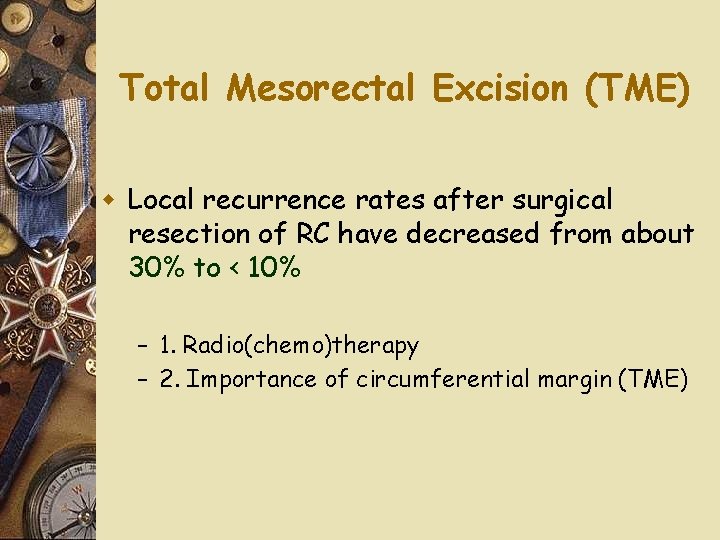
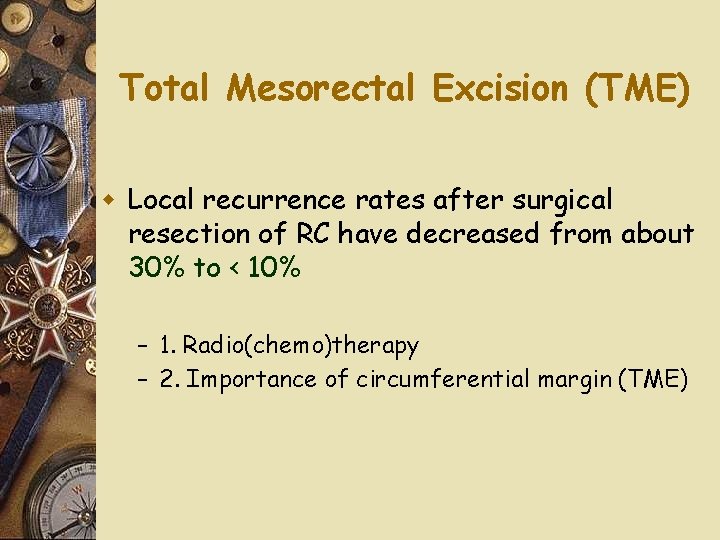
Total Mesorectal Excision (TME) w Local recurrence rates after surgical resection of RC have decreased from about 30% to < 10% – 1. Radio(chemo)therapy – 2. Importance of circumferential margin (TME)
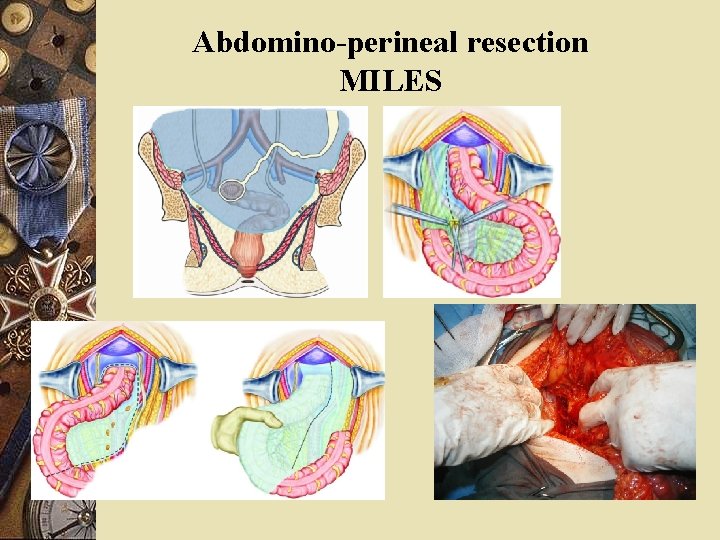
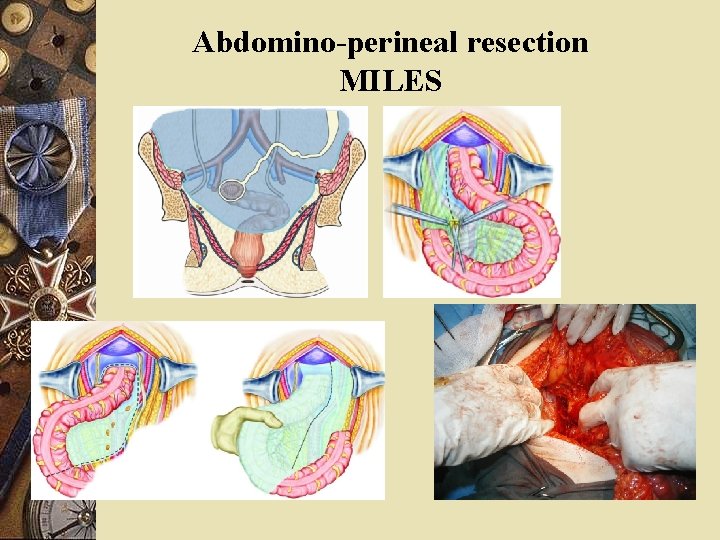
Abdomino-perineal resection MILES
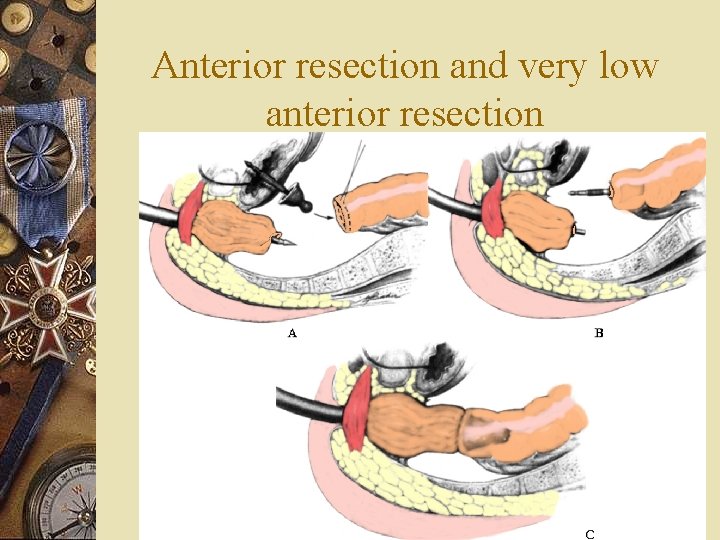
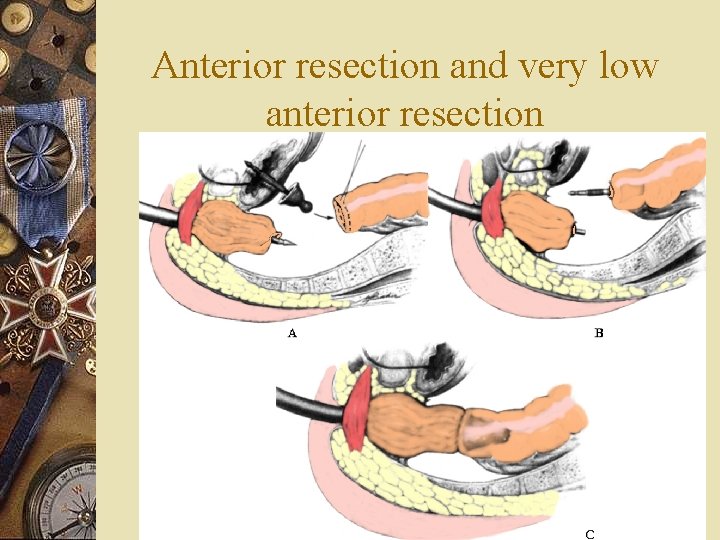
Anterior resection and very low anterior resection

Follow up!!
Epidermoid carcinoma w 75% of all malignancies of the area – Early: verucous, nodular lesion – Late: ulcerated, indurated, nodular nmass w Palpable inguinal nodes w May invade the rectum: false impression of rectal carcinoma w Lymphatic spread: like rectal + inguinal nodes
Treatment w External radiation + concomitant chemotherapy w Radical surgery in case of failure
Malignant melanoma w Horrible prognosis w Dark mass protruding from the anus w 50% pigmented w Lymph node MTS early w Treatment - not clear advantage of any alternative
Bowen’s disease: Squamous cell carcinoma in situ w Like all other places of skin w Plaque-like eczematoid lesion + pruritus w Biopsy-carcioma in situ + hyperkeratosis and giant cells w Therapy: local excision with safety margins
Basal cell carcinoma w Ulcerating tumor (uncommon) w “Rodent ulcer” like every other place of skin exposed w Doesn’t spread distantly w Local excision
Paget’s disease w Rare condition w Pale plaquelike condition with induration + nodular mass (not always) w Nodular mass= coloid carcinoma from glands or other skin appendages w Local excision (without mass) w Radical surgery + chemo + RT for coloid carcinoma
 Histology of large intestine
Histology of large intestine How to find latus rectum of parabola
How to find latus rectum of parabola Distensie
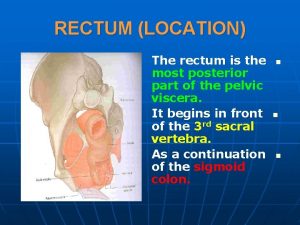
Distensie Rectum and anal canal
Rectum and anal canal Rectum
Rectum Squid classification
Squid classification Latus rectum
Latus rectum Rectum extraperitoneal
Rectum extraperitoneal Rectum in men
Rectum in men Proctitis adalah
Proctitis adalah Rectum
Rectum Anatomy of a rectum
Anatomy of a rectum Sfi in suppository
Sfi in suppository Via de administracion rectal
Via de administracion rectal Lana rhoos
Lana rhoos Vena rectal superior
Vena rectal superior Similar
Similar Ipss
Ipss Normolineo brevilíneo, longilineo
Normolineo brevilíneo, longilineo Syndrome rectal de bensaude
Syndrome rectal de bensaude Proctalgia fugax
Proctalgia fugax Cul de sac para rectal
Cul de sac para rectal Rectal rocket compound
Rectal rocket compound Groin temperature
Groin temperature Inferior pancreaticoduodenal artery
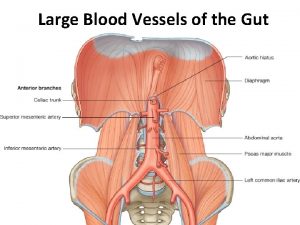
Inferior pancreaticoduodenal artery Colon rectal
Colon rectal Valores normales de la temperatura oral axilar y rectal
Valores normales de la temperatura oral axilar y rectal Zonas de puncion
Zonas de puncion Bowel wash nursing responsibility
Bowel wash nursing responsibility Spirit dosage form
Spirit dosage form Where are your pulse points
Where are your pulse points Sma origin
Sma origin Aural temp
Aural temp Rectal catheter hospice
Rectal catheter hospice Rectal fluids images
Rectal fluids images Via rectal
Via rectal Dr. rolando estrada
Dr. rolando estrada Syndrome rectal de bensaude
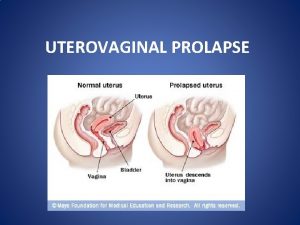
Syndrome rectal de bensaude Types of uterine prolapse
Types of uterine prolapse N
N Colporrhaphy
Colporrhaphy Cystocele with incomplete uterine prolapse
Cystocele with incomplete uterine prolapse Umbilical cord prolapse
Umbilical cord prolapse Vaginak prolapse
Vaginak prolapse Intervertebral disc prolapse
Intervertebral disc prolapse Uterine prolapse treatment non surgical
Uterine prolapse treatment non surgical Uterine prolapse
Uterine prolapse Metaphyseal
Metaphyseal