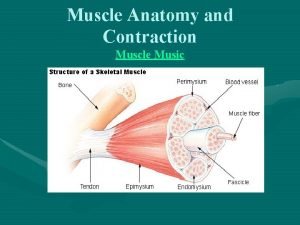
INTRAPARTUM SURVEILLANCE OF UTERINE ACTIVITY O Uterine muscle

- Slides: 19
INTRAPARTUM SURVEILLANCE OF UTERINE ACTIVITY
O Uterine muscle efficiency to effect delivery varies greatly. O To use an analogy, 100 -meter sprinters all have the same muscle groups yet cross the finish line at different times.
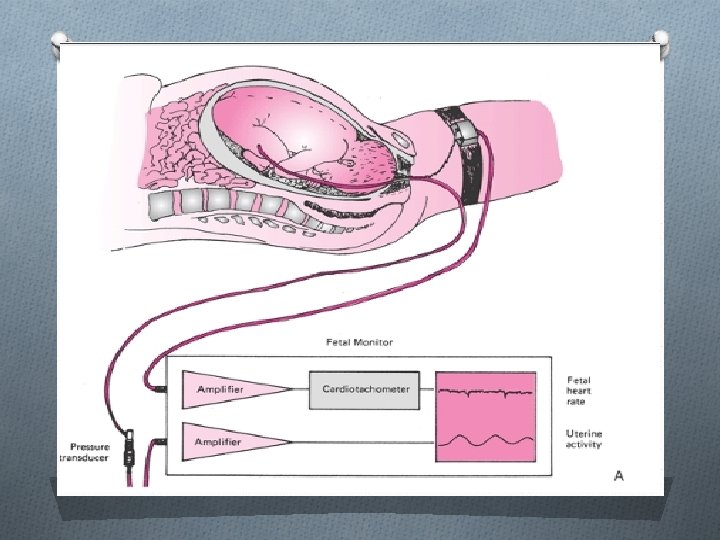
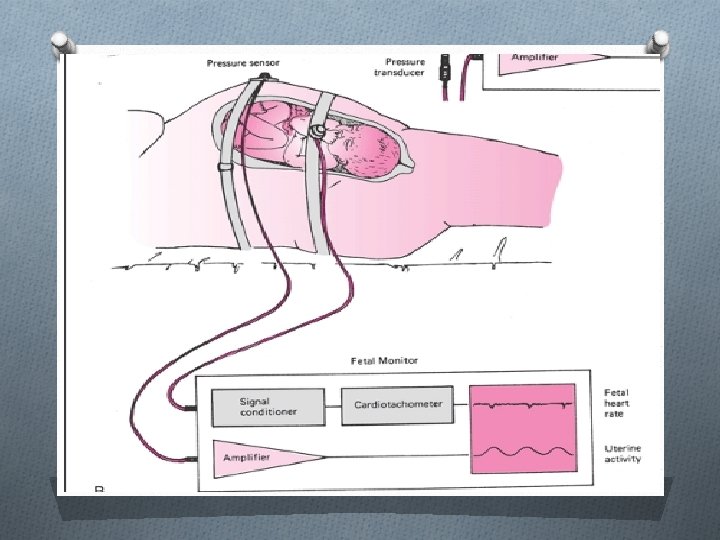
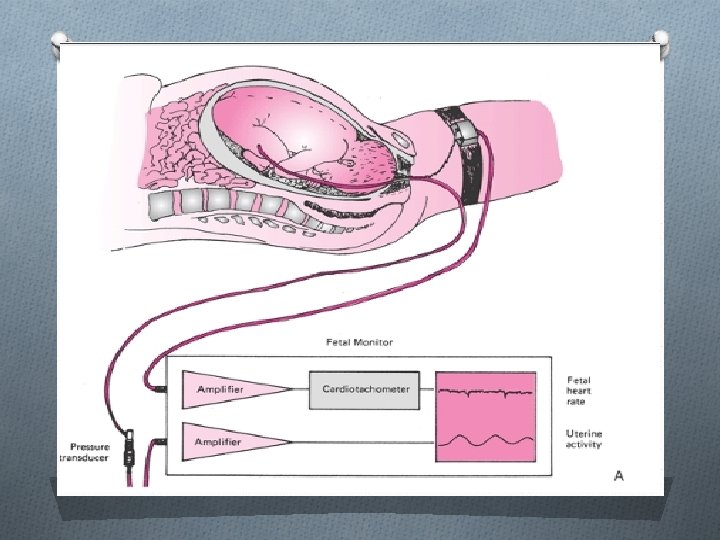
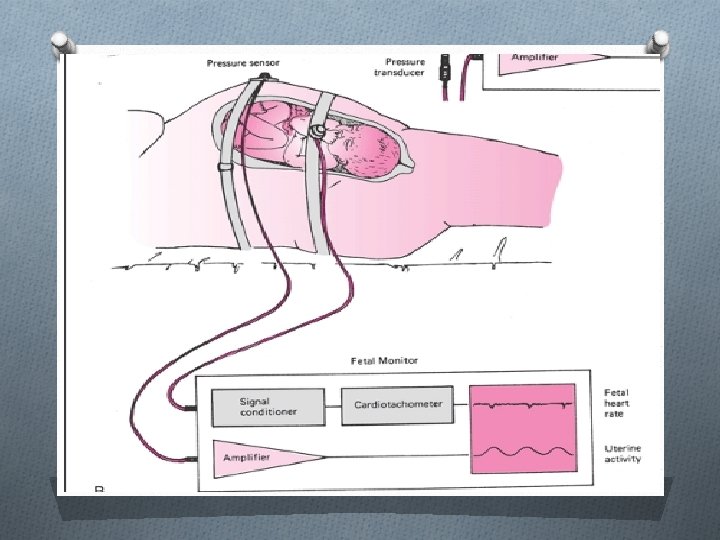
Internal Uterine Pressure Monitoring O Amnionic fluid pressure is measured between and during contractions by a fluid-filled plastic catheter with its distal tip located above the presenting part. O The catheter is connected to a strain-gauge pressure sensor adjusted to the same level as the catheter tip in the uterus. O The amplified electrical signal produced in the strain gauge by variation in pressure within the fluid system is recorded on a calibrated moving paper strip simultaneously with the fetal heart rate recording O Intrauterine pressure catheters are now available that have the pressure sensor in the catheter tip, which obviates the need for the fluid column

External Monitoring O Uterine contractions canbemeasured by a displacement transducer in which the transducer button, or“plunger, ” is held against the abdominal wall. O As the uterus contracts, the button moves in proportion to the strength of the contraction. This movement is converted into a measurable electrical signal that indicates the relative intensity of the contraction. O It has generally been accepted to not give an accurate measure of intensity.
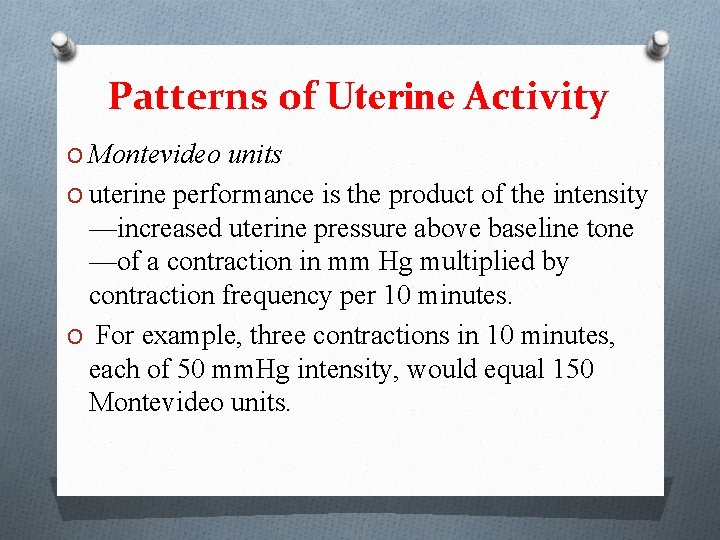
Patterns of Uterine Activity O Montevideo units O uterine performance is the product of the intensity —increased uterine pressure above baseline tone —of a contraction in mm Hg multiplied by contraction frequency per 10 minutes. O For example, three contractions in 10 minutes, each of 50 mm. Hg intensity, would equal 150 Montevideo units.
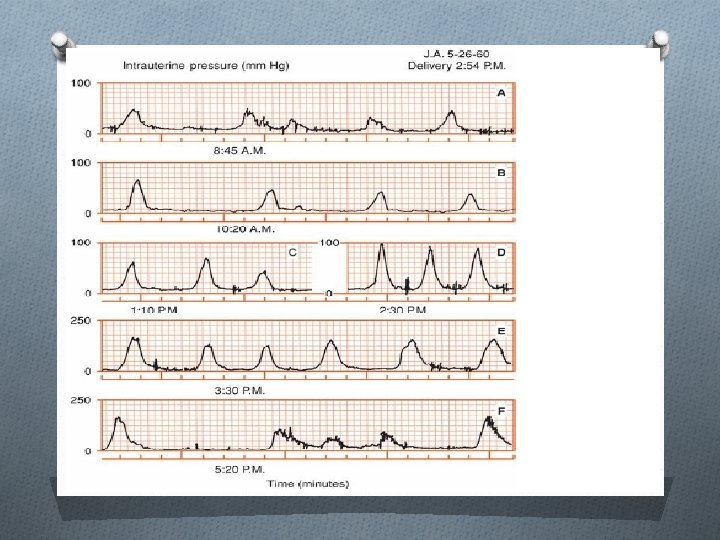
Patterns of Uterine Activity O During the first 30 weeks of pregnancy, uterine activity is comparatively quiescent. O Contractions are seldom greater than 20 mm Hg, and these have been equated with those first described in 1872 by John Braxton Hicks. O Uterine activity increases gradually after 30 weeks, and it is noteworthy that these Braxton Hicks contractions also increase in intensity and frequency O Further increases in uterine activity are typical of the last weeks of pregnancy, termed prelabor. During this phase, the cervix ripens
Patterns of Uterine Activity O clinical labor usually commences when uterine activity reaches values between 80 and 120 Montevideo units. O This translates into approximately three contractions of 40 mm Hg every 10 minutes. O Importantly, there is no clear-cut division between prelabor and labor, but rather a gradual and progressive transition.
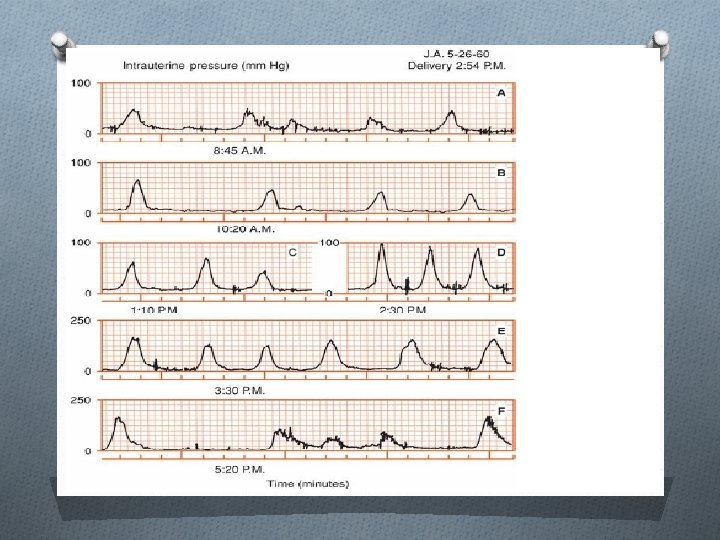
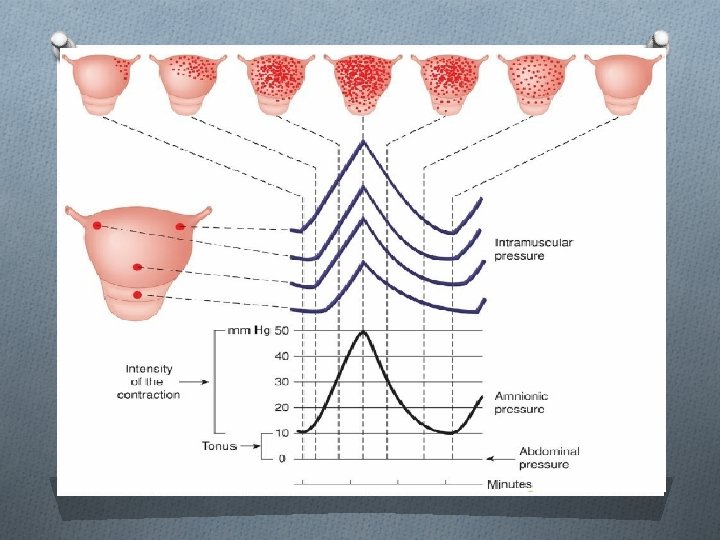
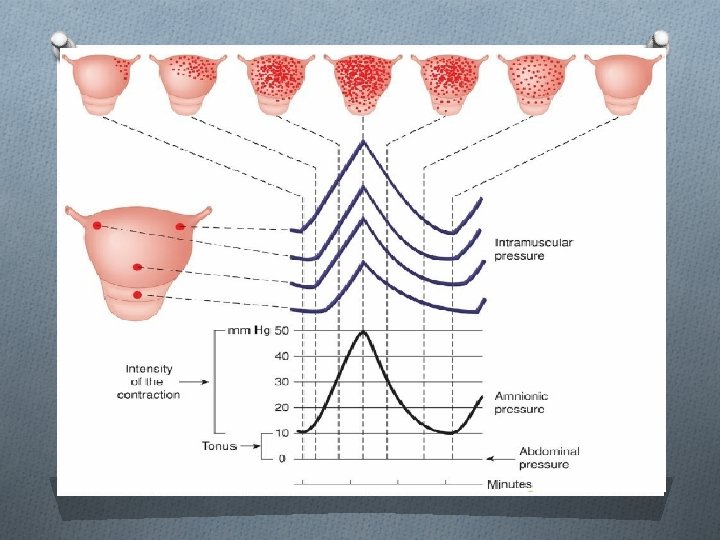
Patterns of Uterine Activity O During first-stage labor, uterine contractions increase progressively in intensity from approximately 25 mm Hg at commencement of labor to 50 mm Hg at the end. O At the same time, frequency increases from three to five contractions per 10 minutes, and uterine baseline tone from 8 to 12 mm Hg. O Uterine activity further increases during second-stage labor, aided by maternal pushing. O Indeed, contractions of 80 to 100 mm Hg are typical and occur as frequently as five to six per 10 minutes. O the duration of uterine contractions— 60 to 80 seconds— does not increase appreciably from early active labor through the second stage.
O Presumably, this duration constancy serves fetal respiratory gas exchange. During a uterine contraction, as the intrauterine pressure exceeds that of the intervillous space O uterine contractions are clinically palpable only after their intensity exceeds 10 mm Hg. Moreover, until the intensity of contractions reaches 40 mm Hg, the uterine wall can readily be depressed by the finger. O Uterine contractions usually are not associated with pain until their intensity exceeds 15 mm Hg, presumably because this is the minimum pressure required for distending the lower uterine segment and cervix. O It follows that Braxton Hicks contractions exceeding 15 mm Hg may be perceived as uncomfortable because distention of the uterus, cervix, and birth canal is generally thought to produce discomfort.
O The uterus is expected to remain well relaxed during pregnancy, to contract effectively but intermittently during labor, and then to remain in a state of almost constant contraction for several hours postpartum. O Uterine activity progressively and gradually increases from prelabor through late labor. O uterine contractions after birth are identical to those resulting in delivery of the infant. O It is therefore not surprising that the uterus that performs poorly before delivery is also prone to atony and puerperal hemorrhage.
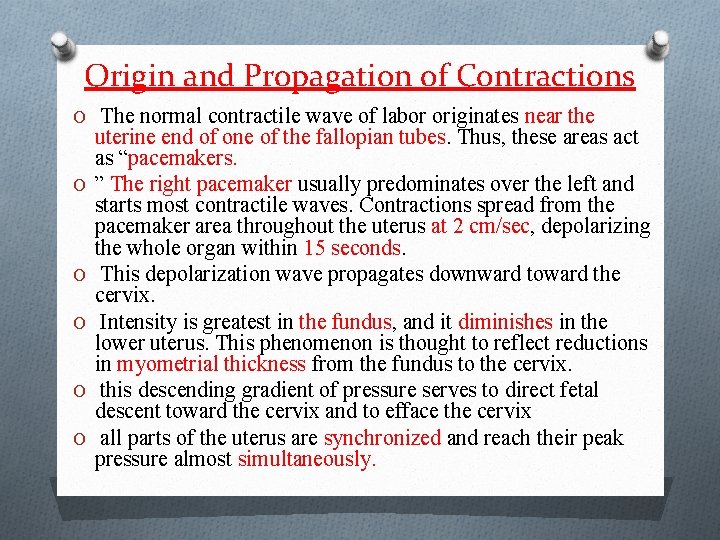
Origin and Propagation of Contractions O The normal contractile wave of labor originates near the O O O uterine end of one of the fallopian tubes. Thus, these areas act as “pacemakers. ” The right pacemaker usually predominates over the left and starts most contractile waves. Contractions spread from the pacemaker area throughout the uterus at 2 cm/sec, depolarizing the whole organ within 15 seconds. This depolarization wave propagates downward toward the cervix. Intensity is greatest in the fundus, and it diminishes in the lower uterus. This phenomenon is thought to reflect reductions in myometrial thickness from the fundus to the cervix. this descending gradient of pressure serves to direct fetal descent toward the cervix and to efface the cervix all parts of the uterus are synchronized and reach their peak pressure almost simultaneously.
O A contractile wave begins in one cornual-region pacemaker, but does not synchronously depolarize the entire uterus. O As a result, another contraction begins in the contralateral pacemaker and produces the second contractile wave of the couplet. These small contractions alternating with larger ones appear to be typical of early labor. O Indeed, labor may progress with such uterine activity, albeit at a slower pace. O labor would progress slowly if regular contractions were hypotonic—that is, contractions with intensity less than 25 mm Hg or frequency less than 2 per 10 minutes. O The authors suggested that these levels of uterine activity should be sought before consideration of cesarean delivery for presumed dystocia.
New Terminology for Uterine Contractions O This has been recommended by the American College of Obstetricians and Gynecologists (2013 b), for the description and quantification of uterine contractions. O Normal uterine activity is defined as five or fewer contractions in 10 minutes, averaged over a 30 -minute window. O Tachysystole was defined as more than five contractions in 10 minutes, averaged over 30 minutes. Tachysystole can be applied to spontaneous or induced labor. O The term hyperstimulation was abandoned.
Complications of Electronic Fetal Monitoring O Electrodes for fetal heart rate evaluation and catheters for uterine O O O contraction measurement an intrauterine pressure catheter during placement may lacerate a fetal vessel in the placenta. Also with insertion, placental and possibly uterine perforation cause hemorrhage, serious morbidity, . Severe cord compression has been described from entanglement with the pressure catheter. Injury to the fetal scalp or breech by a heart rate electrode is rarely severe Both the fetus and the mother may be at increased risk of infection from internal monitoring Scalp wounds from the electrode may become infected, and subsequent cranial osteomyelitis has been reported (Brook. The American Academy of Pediatrics and the American College of Obstetricians and Gynecologists (2012) have recommended that certain maternal infections, including human immunodeficiency virus (HIV), herpes simplex virus, and hepatitis B and C virus, are relative contraindications to internal fetal monitoring.
 Define breech presentation
Define breech presentation Antenatal intrapartum and postnatal
Antenatal intrapartum and postnatal Wandering baseline fhr
Wandering baseline fhr Intrapartum meaning
Intrapartum meaning Class diagram for safe home security system
Class diagram for safe home security system Powerful shoulder abductor used to raise the arm overhead
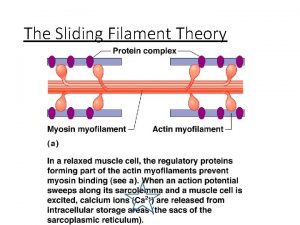
Powerful shoulder abductor used to raise the arm overhead Gap junctions in smooth muscle
Gap junctions in smooth muscle Muscle activity during gait cycle ppt
Muscle activity during gait cycle ppt 5 golden rules of skeletal muscle
5 golden rules of skeletal muscle 5 golden rules of skeletal muscle activity
5 golden rules of skeletal muscle activity Activity 1 introductory activity
Activity 1 introductory activity Activity 3 a lot of square
Activity 3 a lot of square Reactants, products, and leftovers
Reactants, products, and leftovers Activity 2 finding the sequence
Activity 2 finding the sequence Activity 1 activity 2
Activity 1 activity 2 Activity corrections
Activity corrections Draw aoa diagram
Draw aoa diagram Risque thromboembolique surveillance
Risque thromboembolique surveillance Sentinel surveillance is for
Sentinel surveillance is for Texas brfss
Texas brfss