INTRA PARTUM FETAL MONITORING Diagnosis It consists of


- Slides: 14
INTRA PARTUM FETAL MONITORING
Diagnosis: It consists of continuous FHR uterine contraction with intermittent complementary & supplementary fetal micro blood sampling F PH and respiratory gases to clarify clinical situation. 2
Aim: To detect hypoxia and so prevent asphyxia which may cause either death or permanent neurological damage as cerebral palsy, mental deficiency or both.
How to Record: There are 2 methods of recording FHR A → External B → Internal
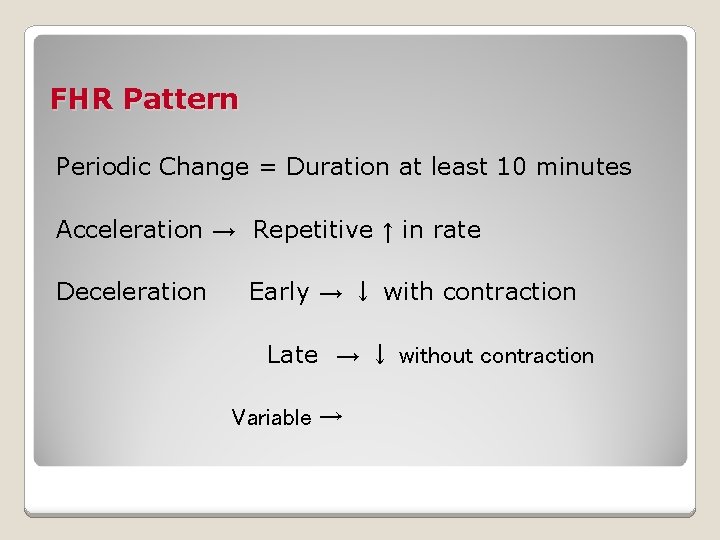
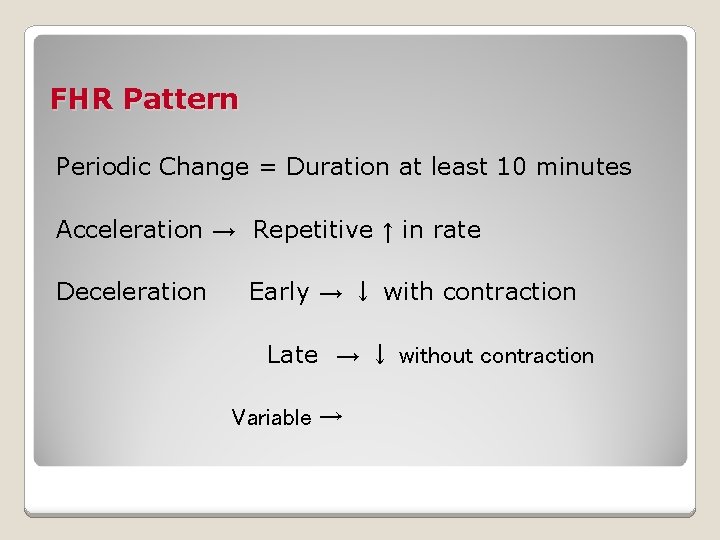
FHR Pattern Periodic Change = Duration at least 10 minutes Acceleration → Repetitive ↑ in rate Deceleration Early → ↓ with contraction Late → ↓ without contraction Variable →
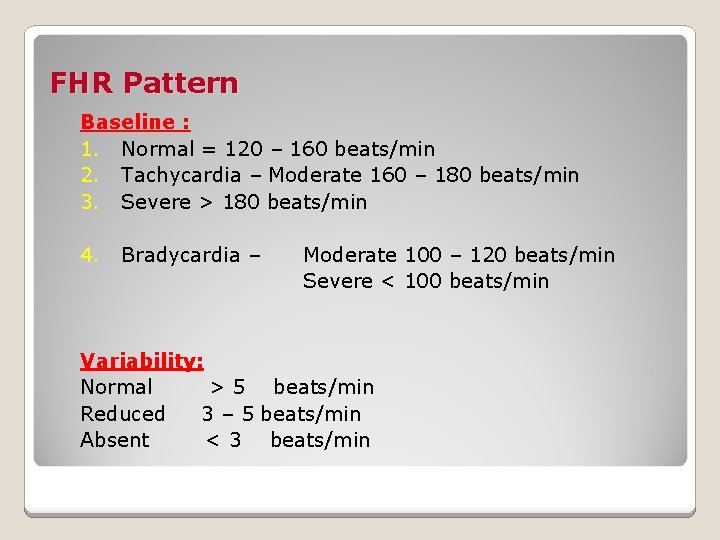
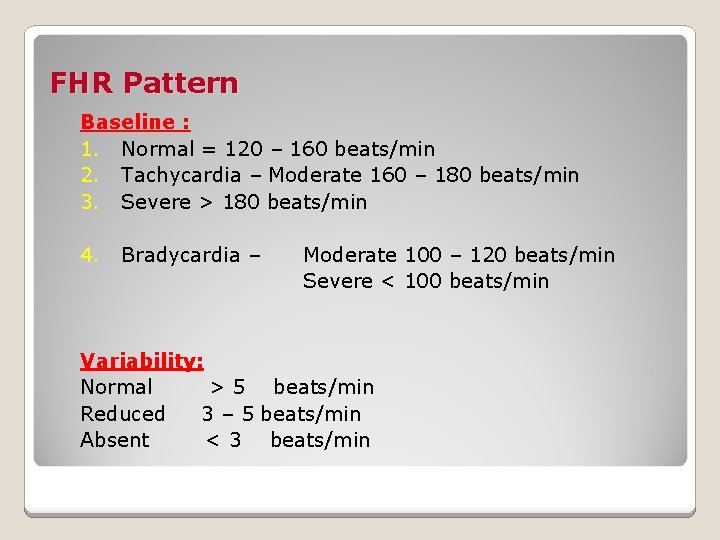
FHR Pattern Baseline : 1. Normal = 120 – 160 beats/min 2. Tachycardia – Moderate 160 – 180 beats/min 3. Severe > 180 beats/min 4. Bradycardia – Moderate 100 – 120 beats/min Severe < 100 beats/min Variability: Normal > 5 beats/min Reduced 3 – 5 beats/min Absent < 3 beats/min
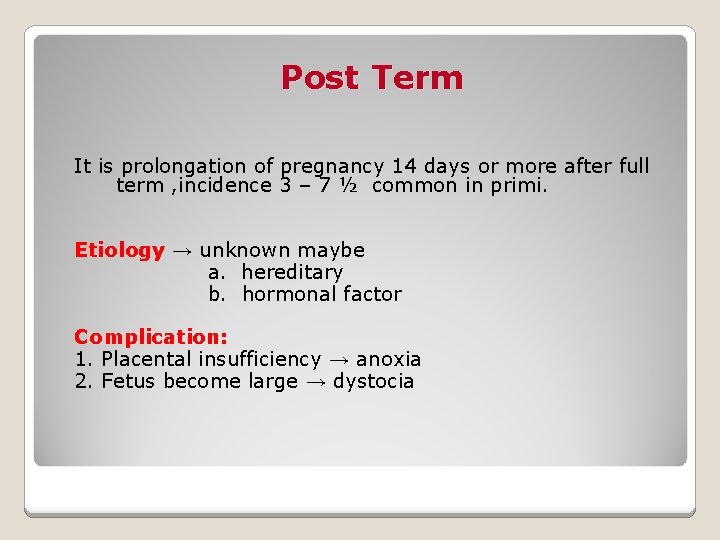
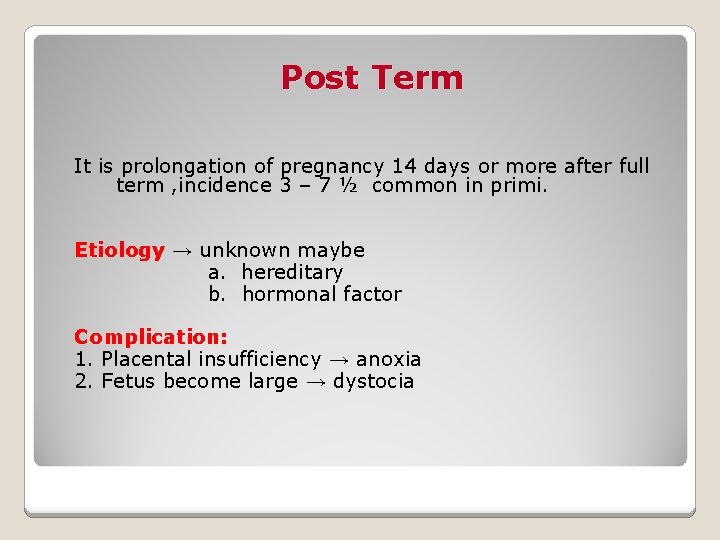
Post Term It is prolongation of pregnancy 14 days or more after full term , incidence 3 – 7 ½ common in primi. Etiology → unknown maybe a. hereditary b. hormonal factor Complication: 1. Placental insufficiency → anoxia 2. Fetus become large → dystocia
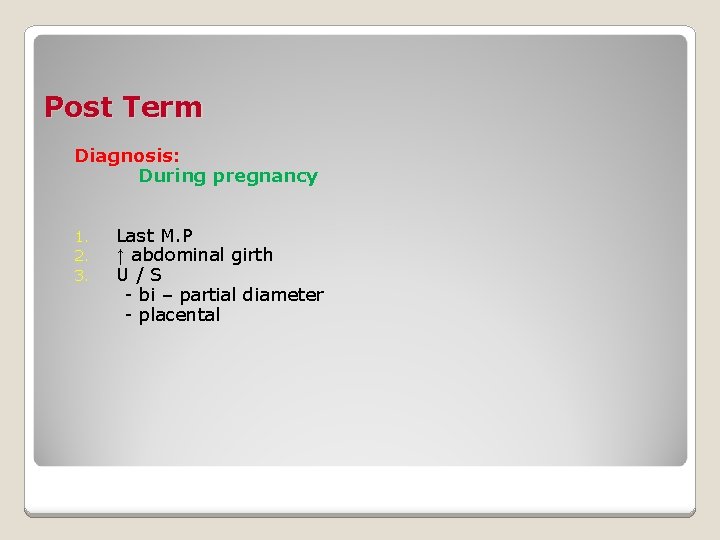
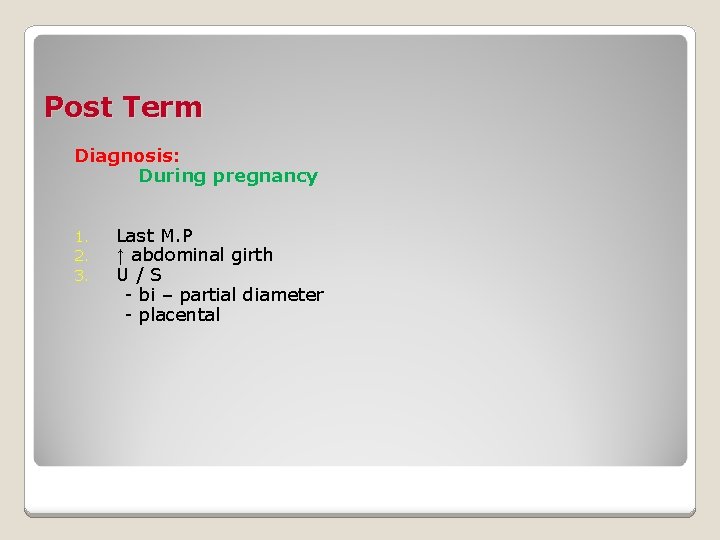
Post Term Diagnosis: During pregnancy 1. 2. 3. Last M. P ↑ abdominal girth U/S - bi – partial diameter - placental
After birth 1. 2. 3. : Long more than 45 cm. & weight more than 4. 3 Well ossified skull with small fontanels Fingernails are unduly long Management : Termination of pregnancy is advisable (if there is placental insufficiency either by: ) 1. 2. Induction of labor Cesarean section in primi & any other obstetrical complications.

Intra Uterine Fetal Death (IUFD) Etiology Hypertensive - PET - Eclampsia - Essential Nephritis - Chronic Nephritis 2. Diabetic Mellitus 3. Erythroblastosis → due to destructive effect, maternal antibodies on fetal red blood cells 4. Syphilis → due to endarteritis obliterans of the vessels & the villi 5. Placental insufficiency - Accidental He - Multiple infarction - Small Placenta 1.
6. Congenital anomalies of the fetus 7. Knots of the cord 8. Acute infectious diseases of the mother 9. Chemical poisoning 10. Idiopathic - Severe anemia - Malnutrition

Intra Uterine Fetal Death (IUFD) Pathology Changes: 1. Pealing of the skin starts 12 hours after death. 2. The brain undergoes softening and CST is absored so the cranial bones override. This is shown in x-ray → Spalding sign. Diagnosis: A. Symptoms 1. Cessation of fetal movements 2. Regression of breast changes B. Signs 1. The uterus is smaller than date 2. The fetus feels like homogenous mass 3. No fetal heart
Intra Uterine Fetal Death (IUFD) Investigations: 1. Pregnancy test negative 2. No fetal heart 3. X-ray - Spalding sign - Hyperflexia of the spine - Collapse of the thorax Complications: 1. 2. 3. Intra uterine infection Hypofibrinogenmia Amnionitic fluid embolism
Intra Uterine Fetal Death (IUFD) Management: 1. Await spontaneous evacuation of the uterus in 4 weeks. 2. If the dead fetus is retained more than 4 weeks or : - the mother is very anxious - if the hypofibrinogenmia is detected - sign of intra uterine infection developed a) Give pitocin drip b) Prostaglandin c) Cytotec or Nalidor