Post partum complication Dr Sahar Anwar Rizk Post
- Slides: 29
Post partum complication Dr: Sahar Anwar Rizk
Post partum complication Types of post partum complications: 1 - post partum hemorrhage 2 - puerperal sepsis
post partum hemorrhage l Postpartum hemorrhage is a significant cause of maternal morbidity and mortality. l Postpartum hemorrhage, the loss of more than 500 m. L of blood after delivery, occurs in up to 18 percent of births and is the most common maternal morbidity in developed countries. Although risk factors and preventive strategies are clearly documented, not all cases are expected or avoidable.
l l l l Risk Factors for Postpartum Hemorrhage Prolonged third stage of labor Preeclampsia Mediolateral episiotomy Previous postpartum hemorrhage Twin pregnancy Arrest of descent Soft-tissue lacerations Asian ethnicity Augmented labor Forceps or vacuum delivery Midline episiotomy Nulliparity& high parity Systemic diseases
Type of post partum hemorrhage: 1 -Primary post partum hemorrhage: occur during the first 24 hrs after delivery 2 -Secondary post partum hemorrhage: occurring more than 24 hrs after delivery. It can occur along 6 weeks after delivery
1 -Primary post partum hemorrhage l Major cause: l A tonic uterus: It is the most common cause of post partum hemorrhage with separation of the placenta , the uterine sinuses cannot compressed effectively.
: 2 -Trumatic l Hemorrhage occurs due to trauma of the uterus, cervix, vagina following vaginal or operative delivery l Delay during episiotomy 3 -Mixed 4 -Blood coagulating disorder: A acquired or congenital blood coagulation disorder.
Factors affecting efficient uterine contraction &retraction l 1. 2. 3. l l l Placental : Incomplete separation of placenta Retained cotyledon &membrane Placenta previa Prolonged labor Multiple pregnancy General anesthesia Full bladder Manipulation of the uterus during third stage
Clinical manifestation of PPH l If blood loss more than 750 -1, 250 l BP normal or decrease l Pulse normal or elevated l Mild vasoconstriction l Normal urinary out put l Aware , alert, oriented
l Atonic uterus (1, 250 -1, 750) l Systolic BP<90 to 100 mm/hg l Moderate tachycardia 100 -120 b/m l Moderate vasoconstriction, skin pallor , cold, moist l Decrease urinary out put l Increase restlessness
l Atonic uterus (1. 800 -2. 500) l Systolic BP <60 mm/Hg l Sever bradycardia >120 b/m l Pronounced vasoconstriction ( extreme pallor, cold , clammy cyanotic lips and finger) l Urinary output ceases (anurea) l Mental stupor , lethargy, semi-comatose *Uterus is flabby and become hard on massaging in a tonic PPH *Uterus is well contracted in traumatic PPH
l l l l l How is postpartum hemorrhage diagnosed? In addition to a complete medical history and physical examination, diagnosis is usually based on symptoms, with laboratory tests often helping with the diagnosis. Tests used to diagnose postpartum hemorrhage may include: estimation of blood loss (this may be done by counting the number of saturated pads, or by weighing of packs and sponges used to absorb blood; 1 milliliter of blood weighs approximately one gram) pulse rate and blood pressure measurement hematocrit (red blood cell count) clotting factors in the blood
Prevention of PPH l Ante partum l Complete history-----to identify high risk pt who are likely to develop PPH l Improve health status especially to rise hg l Hospital delivery of high risk pt who develop polyhydramnios, multiple pregnancy, sever anemia l Routine blood grouping
Intrapartum PPH l Careful administration of sedatives l Avoid hasty delivery of the infant l Prophylactic administration of oxytocin l Avoid massaging the uterus before separation of placenta l Examine the utero –vaginal canal for trauma l Effective management of the fourth stage of labor
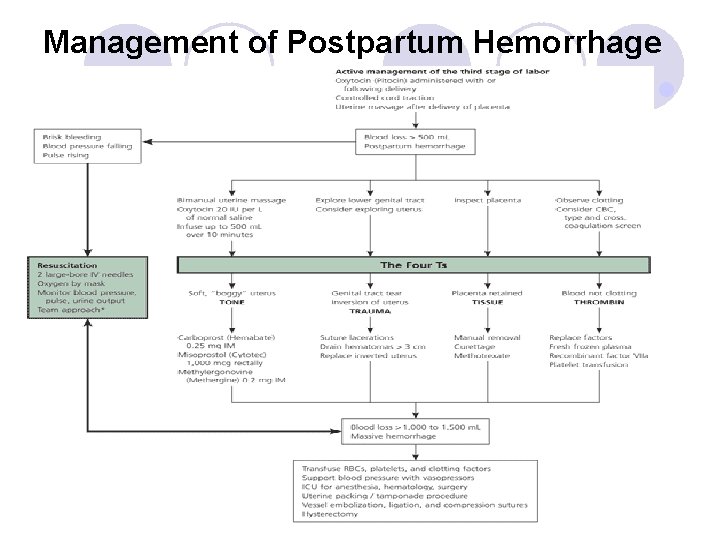
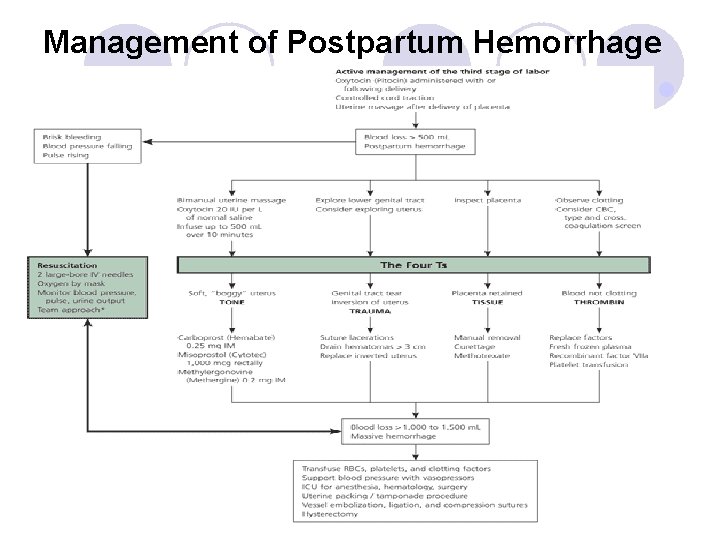
Management of Postpartum Hemorrhage l
l The aim of treatment of postpartum hemorrhage is to find and stop the cause of the bleeding as quickly as possible. Treatment for postpartum hemorrhage may include: medication (to stimulate uterine contractions) manual massage of the uterus (to stimulate contractions) removal of placental pieces that remain in the uterus examination of the uterus and other pelvic tissues packing the uterus with sponges and sterile materials (to compress the bleeding area in the uterus) l tying-off of bleeding blood vessels l laparotomy - surgery to open the abdomen to find the cause of the bleeding. l hysterectomy - surgical removal of the uterus; in most cases, this is a last re l l l
Observation of the mother l l l l l Record pulse, BP, every 15 min Palpate uterus every 15 min ----contraction Check temp /4 hrs Examine lochia for amount & consistency Examine IV infusion Hourly urine output Intake &output chart Relive anxiety Administer prophylactic antibiotic
l Uterotonic Agents. l Uterotonic agents include oxytocin, ergot alkaloids (Methergine ), and prostaglandins. l Oxytocin stimulates the upper segment of the myometrium to contract rhythmically, which constricts spiral arteries and decreases blood flow through the uterus 30. Oxytocin is an effective first-line treatment for post
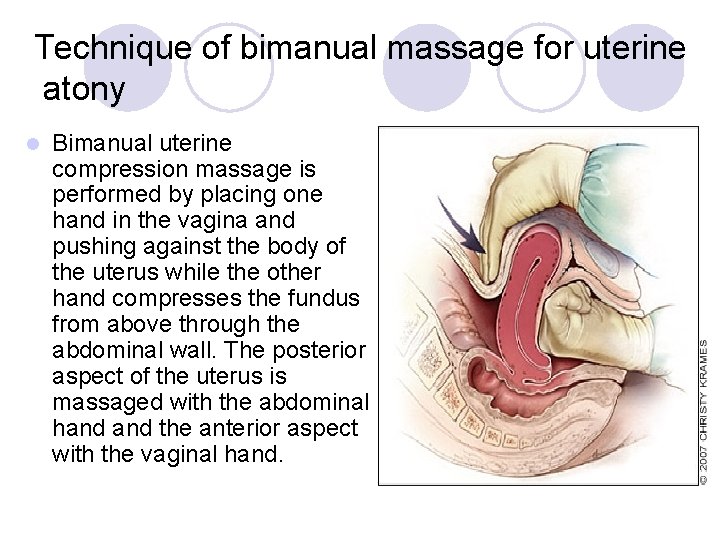
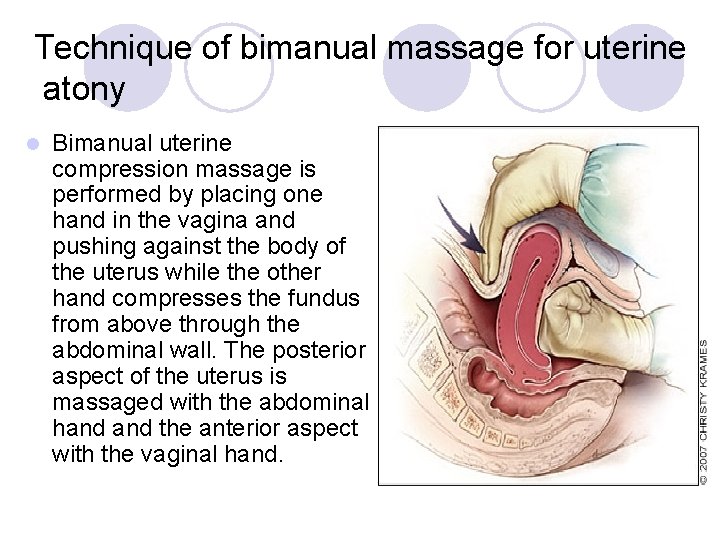
Technique of bimanual massage for uterine atony l Bimanual uterine compression massage is performed by placing one hand in the vagina and pushing against the body of the uterus while the other hand compresses the fundus from above through the abdominal wall. The posterior aspect of the uterus is massaged with the abdominal hand the anterior aspect with the vaginal hand.
Nursing management l Assess pt l Identify risk group: l Vital sign l State of the uterus l Natural of bleeding l S&S of blood loss l compare laboratory report
: Nursing intervention l If atonic l Inform obst Feel the consistency of the uterus Massage the uterus Assess the physical condition Monitor TPR &BP Put the infant on breast Prepare the instrument l l l
l Administer oxytocin l Start IV infusion l Empty bladder l Examine placenta l Reassure the mother l In trumatic: l press on the tear or laceration l Prepare the equipment
Secondary post partum hg l Commonly occur 10 -14 day PP l Common cause: l retained bit of cotyledon l Separation of slough exposing a blood vessels l Sub involution at the placental sit
S&S l Sudden episode of bleeding l Sub involution l Sepsis l Anemia l Management: l Reassurance l Monitor TPR l IV, empty bladder, give medication
: Puerperal sepsis l It is an infection of the genital tract that occur at any time between the onset of rupture of the membrane or labor & the 42 ed day post partum or abortion : l The following are present: l Pelvic pain l Fever 38. 5 l Abnormal vaginal discharge l Foul odor &sub involution
Microorganisms commonly involved in PPGTI l Gram positive l Gram negative l Microorganism that sexually transmitted
Risk factors for PP infection l Related to general infection risk l Related to labor and delivery l Related to operative risk factors
Principle clinical feature l Elevated temp l Suprapubic pain l Foul smell lochia l Uterine involution l General symptoms l Laboratory investigation
Preventive measures l Ante partum l Intrapartum l Post partum l Nursing management