POSTPARTUM HEMORRHAGE Dr Nahal Nasehi Post partum hemorrhage
















- Slides: 48
POSTPARTUM HEMORRHAGE Dr. Nahal Nasehi

Post partum hemorrhage: Definition: Estimated blood loss≥ 500 ml after vaginal birth or ≥ 1000 ml after C/S. � � The mean blood loss after NVD and C/S is 400600 ml and 1000 ml respectively and clinicians were more likely to underestimate than overestimate the volume of blood loss.
Etiopathogenesis � � -tone( most common) -trauma -tissue(placenta) -thrombin(DIC)
Post partum hemorrhage: PRIMARY OR EARLY(DURING FIRST 24 H) SECONDARY OR LATE(AFTER 24 H TO 12 WEEKS)
� � � PPH happens in 1 -5% of deliveries with death rate of 1 in 100, 000 to 1000 birth in high VS low income countries. One of the leading causes of M. M world wide. Most deaths are due to lack of anticipation of excessive bleeding or gross underestimation of blood loss
� � EBL is usually ½ of actual blood loss. VS After 1000 ml blood loss there is only 3% reduced HCT during 1 st hour. In very acute bleeding HCT is at maximum level during bleeding . � Urinary output is the most vital sign in Ob. hemorrhage, that should be 30 -60 cc/ h. So, indwelling catheter is mandatory in potentially dangerous bleeding and diuretics is not accepted.
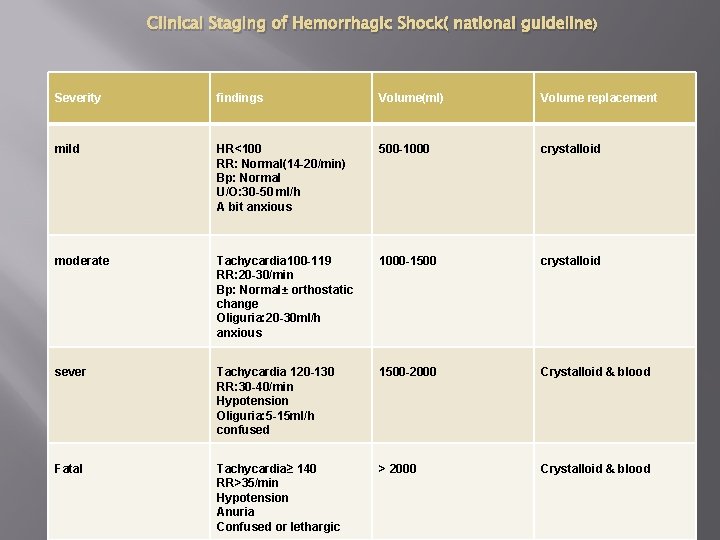
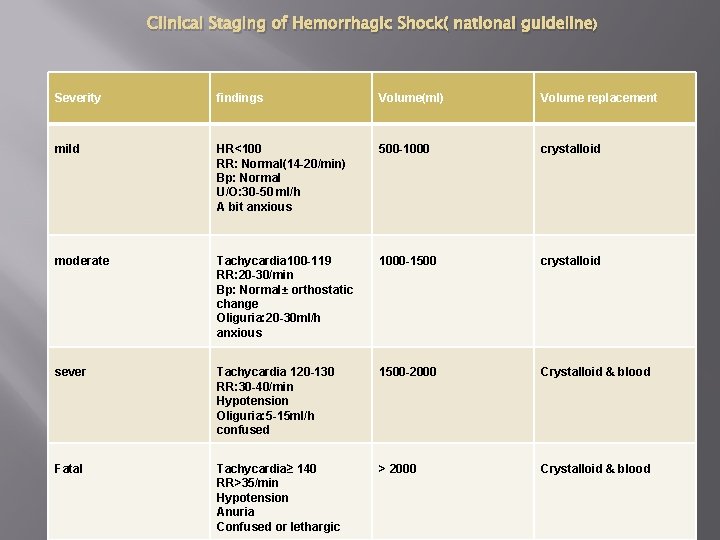
Clinical Staging of Hemorrhagic Shock( national guideline) Severity findings Volume(ml) Volume replacement mild HR<100 RR: Normal(14 -20/min) Bp: Normal U/O: 30 -50 ml/h A bit anxious 500 -1000 crystalloid moderate Tachycardia 100 -119 RR: 20 -30/min Bp: Normal± orthostatic change Oliguria: 20 -30 ml/h anxious 1000 -1500 crystalloid sever Tachycardia 120 -130 RR: 30 -40/min Hypotension Oliguria: 5 -15 ml/h confused 1500 -2000 Crystalloid & blood Fatal Tachycardia≥ 140 RR>35/min Hypotension Anuria Confused or lethargic > 2000 Crystalloid & blood
Caution � � Risk assessment for every delivery(induced labor, previous PPH, over distention, precipitated labor, …). Determine placental position in repeat c/s by US Scan Use Color Doppler or MRI in suspicious cases Prepare multidisciplinary care if needed

Prevention � � � 5 -10 u oxytocin im or 10 u in 500 ml serum with 10 cc/min or 200 mu/min after birth( 5 u slowly iv after C/S? ) Clamp the umbilical cord during 30 -120 sec. after birth Controlled traction of placenta
Communication Call experienced midwife (in addition to midwife in charge). ● Call obstetric middle grade and alert consultant. ● Call anaesthetic middle grade and alert consultant. ● Alert consultant clinical haematologist on call. ● Alert blood transfusion laboratory. ● Call porters for delivery of specimens/blood. ● Alert one member of the team to record events, fluids, drugs and vital signs.

Management two basic goals � Restoration of blood volume and oxygen carrying capacity( One or two main IV line) � Definitive treatment of the underlying disorder It is ideal to stabilize patient before definitive therapy is begun, but this is frequently impossible in obstetric hemorrhage so; operation theater, surgeon and anesthesiologist should be informed immediately. �
nonpharmacologic management � � � Ask help: midwife obstetrician, anesthesiologist Lie down, keep warm Etiology? Two main iv line Blood test& # match
nonpharmacologic management � � IV volume Supplemental oxygen by face mask 10 -15 L/min. Pulse oximetry and V/S EKC if needed

nonpharmacologic management � � � Uterine massage Folly catheter CV line? Arrange ICU care or delivery ward after PPH management Fill the flow chart and document I/O
� Definitive therapy for individual circumstances Immediate postpartum hemorrhage � Uterine massage � Direct compression � Cleaning uterine cavity � Pharmacologic agents � Surgical approach
Volume replacement therapy � � The best agent is blood, if not available, large IV line and rapid crystalloid( 2 -3 ml per 1 ml blood loss) up to 3/5 L if the blood is not ready(or colloid fluid 1 -2 L or hartmann/lactate ringer). FFP should not be used for replacement alone( expensive, needed for specific factors, risk of infection)
Dilutional coagulopathy: happens with 5 -10 or more RBCU � � � If platelet is<50, 000 with active bleeding and surgery, use platelet( every unit of 50 cc, increases platelet up to 5000/ml), no need for ABO compatibility but D Ag must be compatible. Without surgery 5000 -10000 platelet rarely leads to bleeding. If PT>16" or PTT>60" or fibrinogen level is under 100 mg/dl; FFP( ABO matched)10 -15 ml/kg but needs 30 minute for defreezing. (250 cc/unit) Cryoprecipitate( ABO matched) is needed when we have limitation for volume and need all factors at the same time(Hemophilia A, Von Willebrand, decreased fibrinogen or factor XIII). 15 cc/unit. 10 u cryo (2 pack) results in fibrinogen>1 gr/L
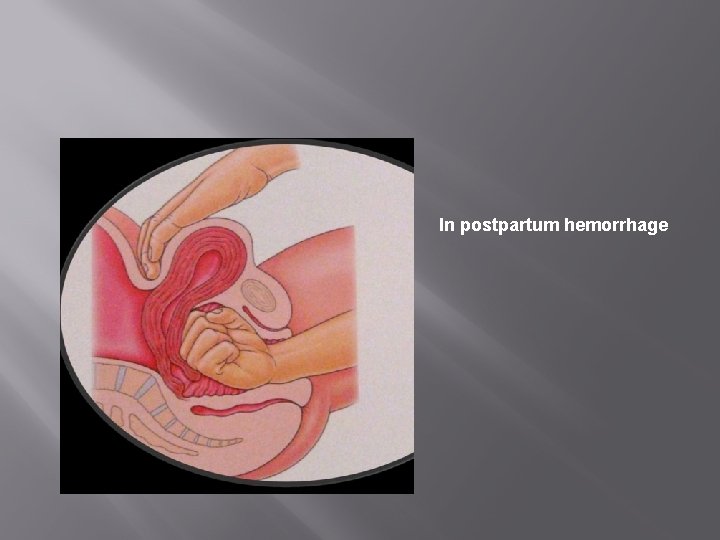
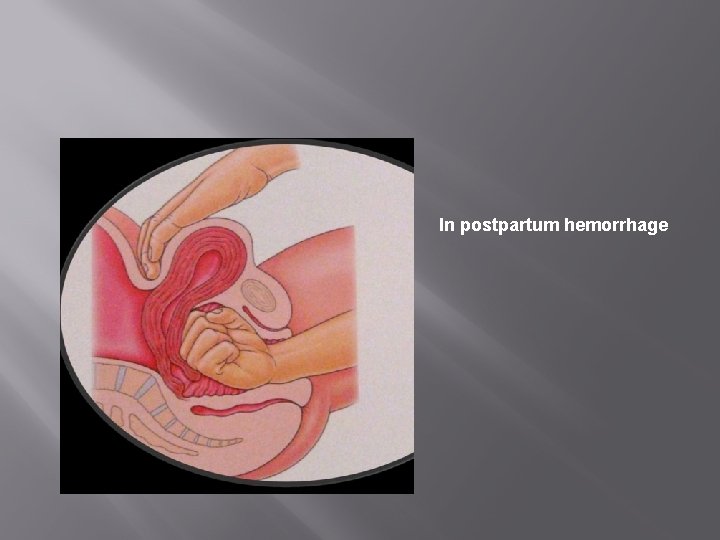
In postpartum hemorrhage

Placental remove

Trauma repair

Agent Dose Contraindication Oxytocin* 5 u IV 60 drip/min up to 3 Lor 10 u im No bolos iv Methyl ergonovin** 0. 2 mg IM(q 15 min to 2 -4 h up to 5 doses) HTN Cardiac dis. PET PG 15 Methyl F 2α 0. 25 mg IM(q 15 -90 min up to 2 mg No iv Asthma, Active cardiac, pulmonary and liver disease Prostaglandin. E 2 20 mg PR or Vag. Misoprostol*** (PGE 1) 800 -1000 micgr rectal Single dose Recombinant Factor. VIIα RFVIIα 90 micgr/kg Tranexamic Acid? Plate<50000 Fibrinogen<1 gr/L Abnormal PT Ph<7. 2 BT<35

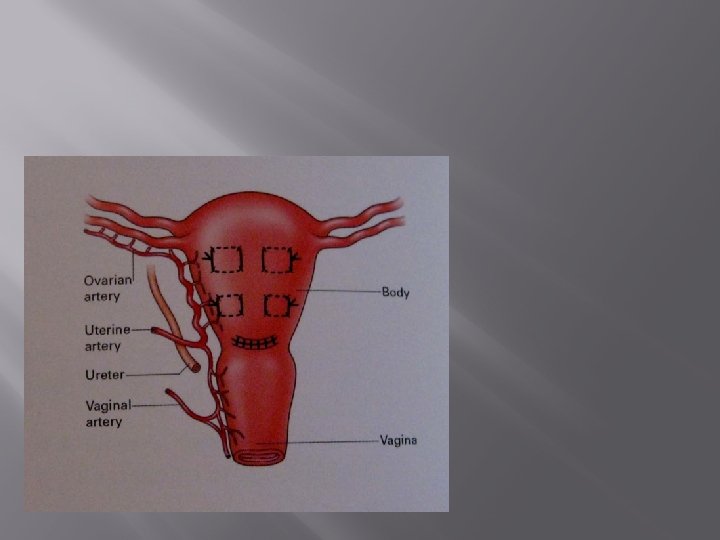
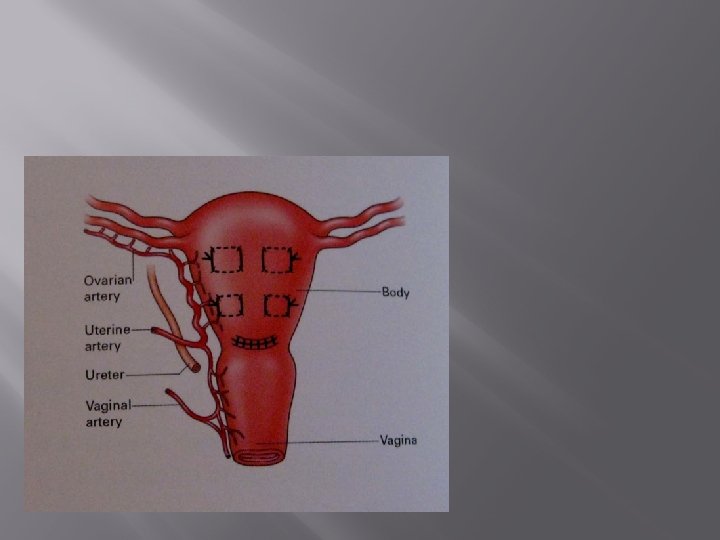
� � Uterine artery embolization if possible Bilateral uterine and utero-ovarian artery ligation Hypogastric artery ligation? Total or subtotal hysterectomy
Basic measures for MINOR PPH (blood loss 500– 1000 ml, no clinical shock ● Intravenous access (14 -gauge cannula x 1). ● Commence crystalloid infusion
> 1000 ml and continuing to bleed OR clinical shock ● Assess airway. ● Assess breathing. ● Evaluate circulation ● Oxygen by mask at 10– 15 litres/minute. ● Intravenous access (14 -gauge cannula x 2, orange cannulae). ● Position flat. ● Keep the woman warm using appropriate available measures. ● Transfuse blood as soon as possible
goals of management of massive blood loss is to maintain ● haemoglobin > 8 g/dl ● platelet count > 75 x 109/l ● prothrombin < 1. 5 x mean control ● activated prothrombin times < 1. 5 x mean control ● fibrinogen > 1. 0 g/l.
is arrested any coagulopathy is corrected, thrombo- prophylaxis is administered, as there is a high risk of thrombosis. Alternatively, pneumatic compression devices can be used, if thromboprophylaxis is contraindicated in cases of thrombocytopenia.
Anaesthetic management The anaesthetist needs to able to assess the woman quickly, to initiate or continue resuscitation to restore intravascular volume and provide adequate anaesthesia
The presence of cardiovascular instability is a relative contraindication to regional anaesthesia. Blockage of the sympathetic system can potentially lead to worsening hypotension due to haemorrhage. If cardiovascular stability has been achieved and there is no evidence of coagulation failure, regional anaesthesia can be used
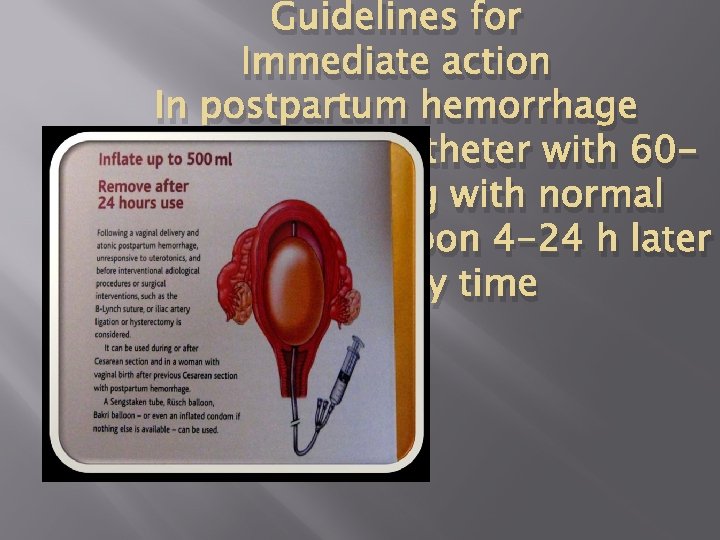
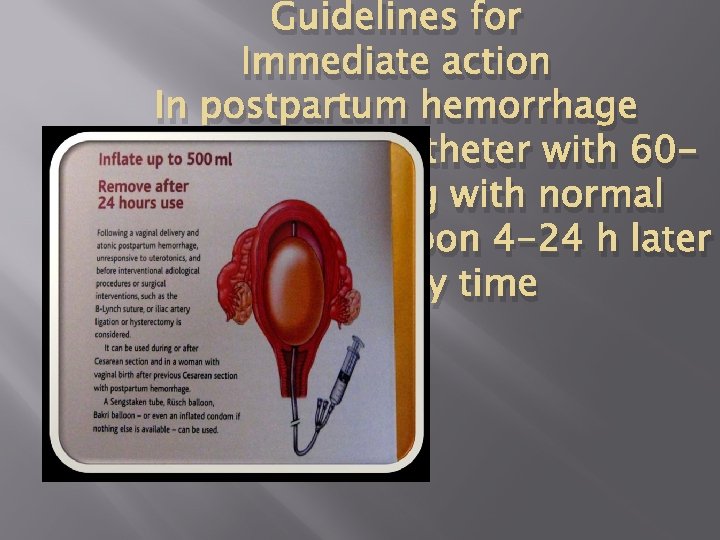
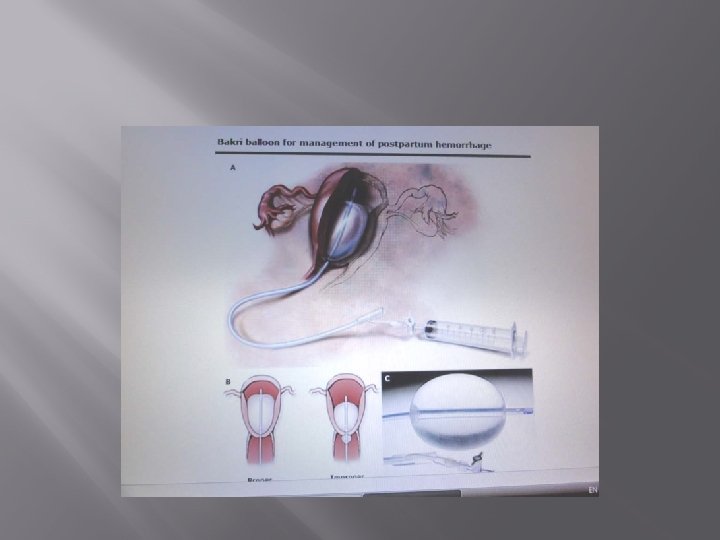
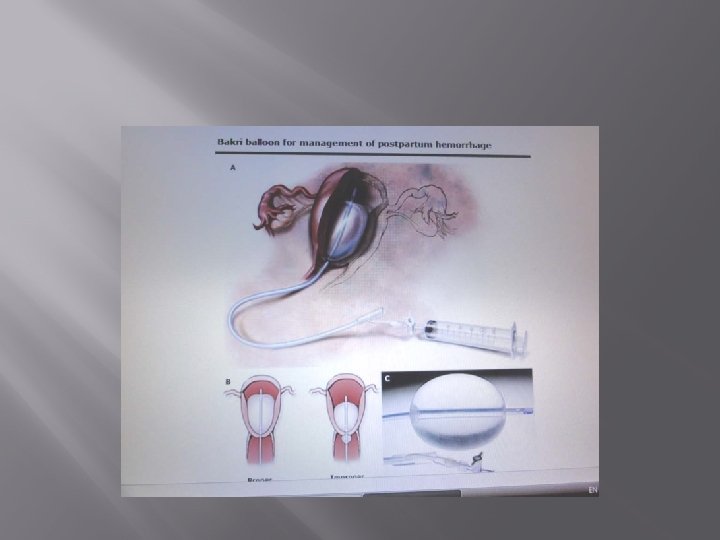
Guidelines for Immediate action In postpartum hemorrhage 3 -4 no: 16 Folly catheter with 6080 cc inflated bag with normal saline. Deflate balloon 4 -24 h later during day time
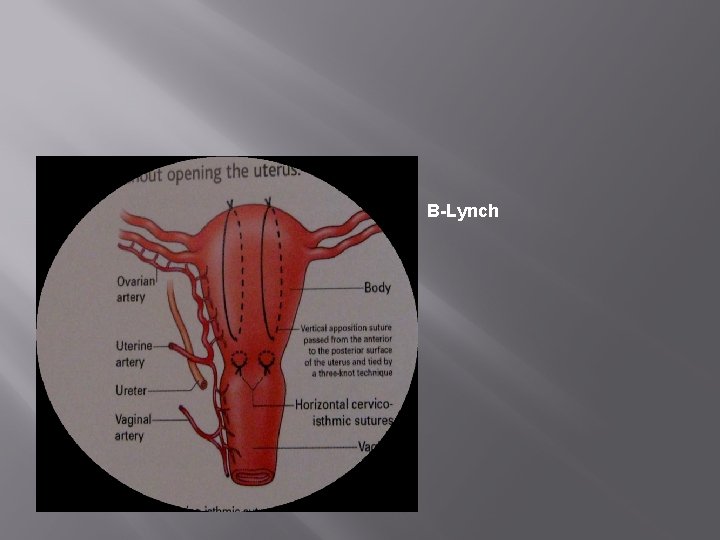
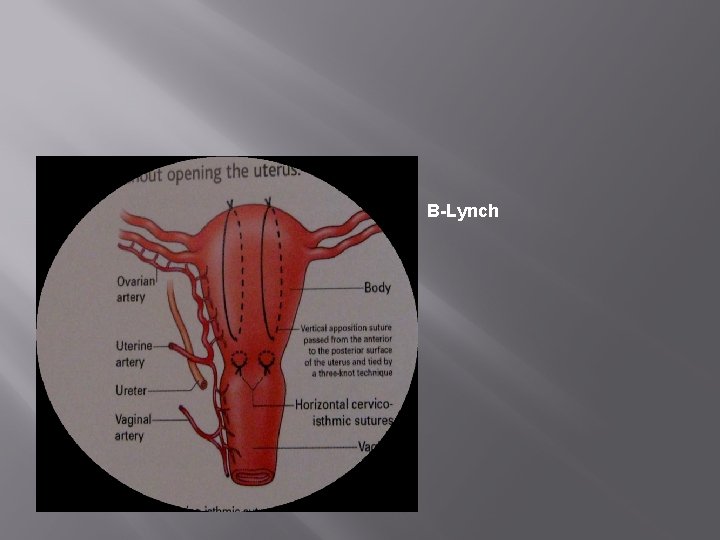
B-Lynch
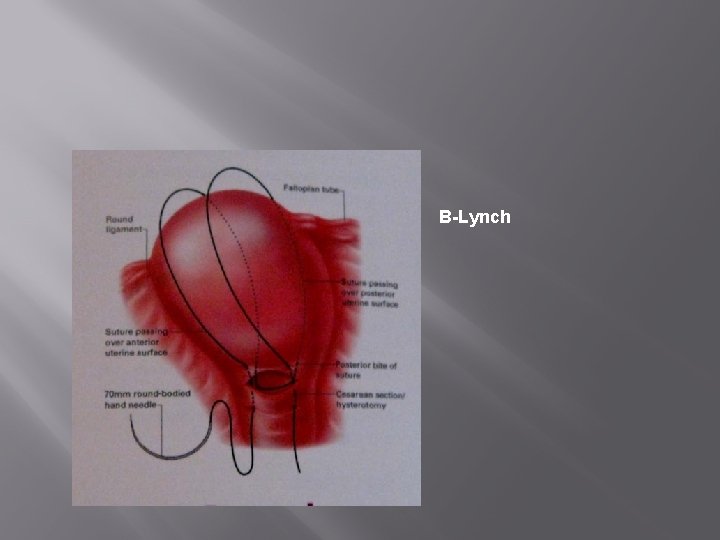
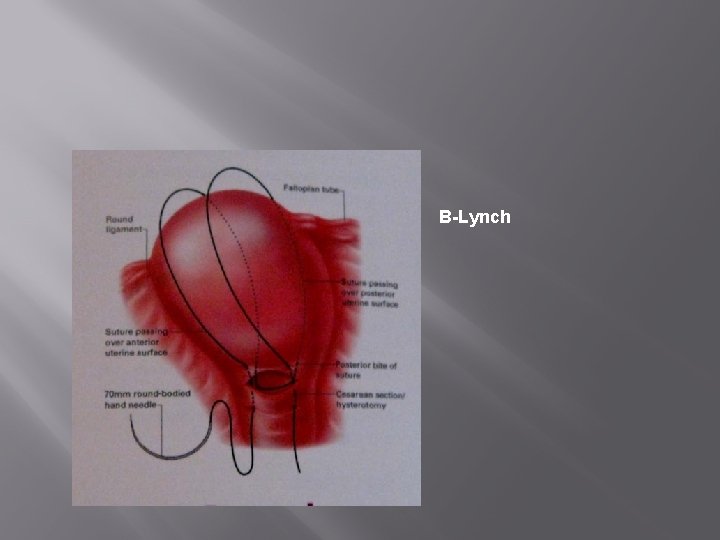
B-Lynch




Secondary PPH is often associated with endometritis. When antibiotics are clinically indicated, a combination of ampicillin (clindamycin if penicillin allergic) and metronidazole is appropriate. In cases of endomyometritis (tender uterus) or overt sepsis, then the addition of “ gentamicin is recommended. ”
Late PPH � � � Incision infection: 500 mg ampicillin Po q 6 h+500 mg metronidazol Po q 8 h In renal failure use clindamycin instead of gentamycin Remove retained placenta if needed after US Scan
that secondary PPH is often associated with infection and conventional treatment involves antibiotics and uterotonics. In continuing haemorrhage, insertion of balloon catheter may be effective. “ ”
summery � � � � One of the leading causes of M. M. EBL is usually ½ of real loss. Never forget indwelling catheter. Remember H. R. , B. P, urinary output and consciousness for staging shock. The best agent for replacement is blood, if not accessible, crystalloid( 3/1). Definitive therapy for individual conditions. Other components in specific conditions.
“ thanks ”

THA NK Y OU F OR Y ATT OUR ENT ION
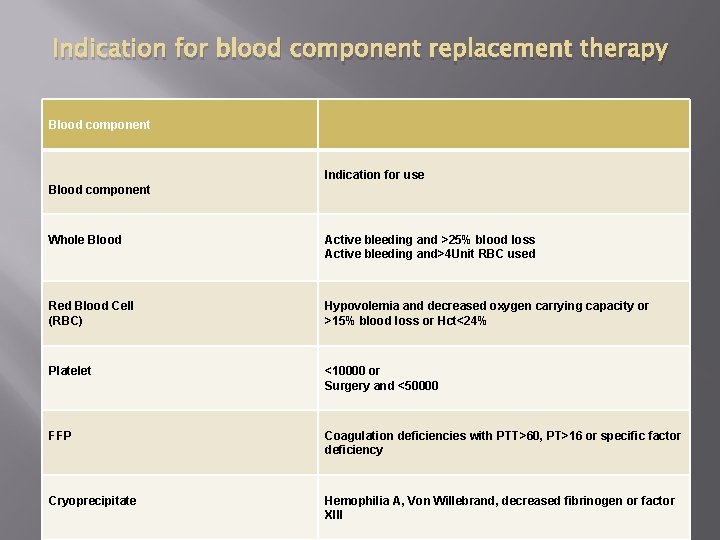
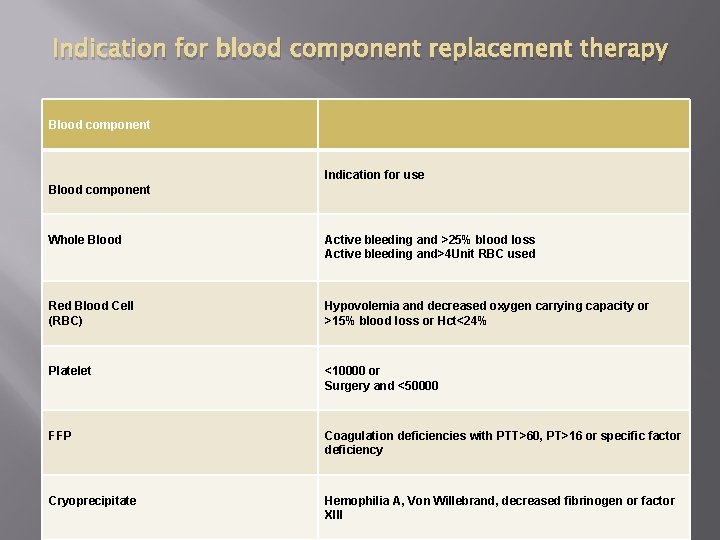
Indication for blood component replacement therapy Blood component Indication for use Blood component Whole Blood Active bleeding and >25% blood loss Active bleeding and>4 Unit RBC used Red Blood Cell (RBC) Hypovolemia and decreased oxygen carrying capacity or >15% blood loss or Hct<24% Platelet <10000 or Surgery and <50000 FFP Coagulation deficiencies with PTT>60, PT>16 or specific factor deficiency Cryoprecipitate Hemophilia A, Von Willebrand, decreased fibrinogen or factor XIII

� � Misoprostol is not as effective as oxytocin but it may be used when the latter is not available, such as A the home-birth setting.

have been given, there will be clotting factor defects and blood components should be given to 1 litre of fresh frozen plasma (FFP) and 10 units of cryoprecipitate (two packs) may be given empirically in the face of relentless bleeding, while awaiting the results of coagulation studies
Surgical measures should be undertaken if there is excessive or continuing bleeding, irrespective of ultrasound findings. “ ”

A multidisciplinary approach to treatment should ensure that everyone knows how to work together to ensure prompt and efficient treatment in such an emergency. “ ”
 Seronox
Seronox Anti shock trousers
Anti shock trousers Uterine atony
Uterine atony Nursing care plan for postpartum hemorrhage slideshare
Nursing care plan for postpartum hemorrhage slideshare Nursing management of pph
Nursing management of pph Pph management
Pph management Postpartum hemorrhage
Postpartum hemorrhage Defination of pph
Defination of pph Rncob
Rncob What does infected lochia look like
What does infected lochia look like Post tonsillectomy hemorrhage
Post tonsillectomy hemorrhage Post tonsillectomy hemorrhage
Post tonsillectomy hemorrhage Fluxus postpartum
Fluxus postpartum Secondary postpartum haemorrhage
Secondary postpartum haemorrhage Wolff chaikoff effect
Wolff chaikoff effect Fundus fiddling
Fundus fiddling Root word medical terminology examples
Root word medical terminology examples Bubble postpartum
Bubble postpartum Rubin's phases of postpartum
Rubin's phases of postpartum Postpartum infections
Postpartum infections Postpartum infection
Postpartum infection Chapter 20 postpartum adaptations
Chapter 20 postpartum adaptations Postpartum thyroiditis
Postpartum thyroiditis Postpartum stomach pain
Postpartum stomach pain Lochia assessment
Lochia assessment Postpartum thyroiditis
Postpartum thyroiditis Bubble he assessment
Bubble he assessment Osmotherapy
Osmotherapy Brain hemorrhage
Brain hemorrhage Hemorrhage assessment
Hemorrhage assessment Hemorrhage
Hemorrhage Gastroesophageal sphincter
Gastroesophageal sphincter Antipartum hemorrhage
Antipartum hemorrhage Triad of death
Triad of death Raina flores
Raina flores Hunt and hess scale
Hunt and hess scale Hemorrhage
Hemorrhage Stamca
Stamca Pulmonary toilet
Pulmonary toilet Antipartum
Antipartum Lateral venous lacunae
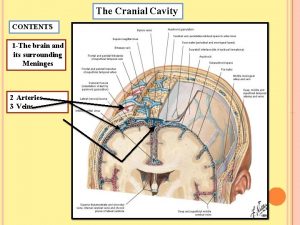
Lateral venous lacunae Hemorrhage
Hemorrhage Rubeosis of iris
Rubeosis of iris Management of hemorrhage
Management of hemorrhage Fetomaternal hemorrhage
Fetomaternal hemorrhage Brain hemorrhage
Brain hemorrhage Subconjunctival hemorrhage
Subconjunctival hemorrhage Waiter's tip deformity
Waiter's tip deformity Blood loss classification
Blood loss classification