Chapter 20 Post partum Assessment and Care Post

- Slides: 22
Chapter 20 Post partum Assessment and Care
Post partum assessment Initial assessment : Include q -Vital signs q -Skin color q -Fundus, lochia and perineum q -Pain q -IV(type, rate, medication, site) q -Urinary output q -Abdominal incision if present q -Feeling level and ability to move if regional anesthesia was administered
Chart review: Relevant information q -Gravida para q-Type of delivery q-Degree of episiotomy and laceration q-Anesthesia or medication during labor q-Significant medical or surgical history q-Medication routinely taken q-Food and drug allergies q-Method chosen for infant feeding q-Condition of baby
q. Laboratory data: Hb, Hct, blood group and Hepatitis B, rubella titer, syphills and group B streptococci q Assess for the need for RH(D) immunoglobulin q. Assess need for Rubella Vaccine q Risk factors for postpartum hemorrhage and infection
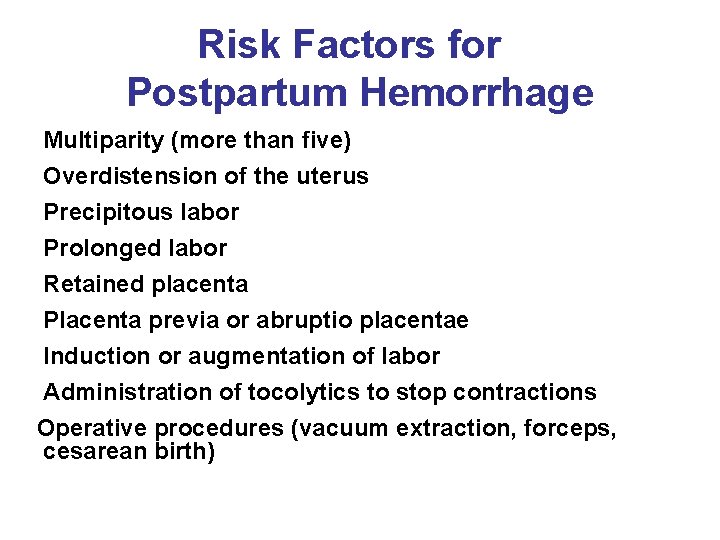
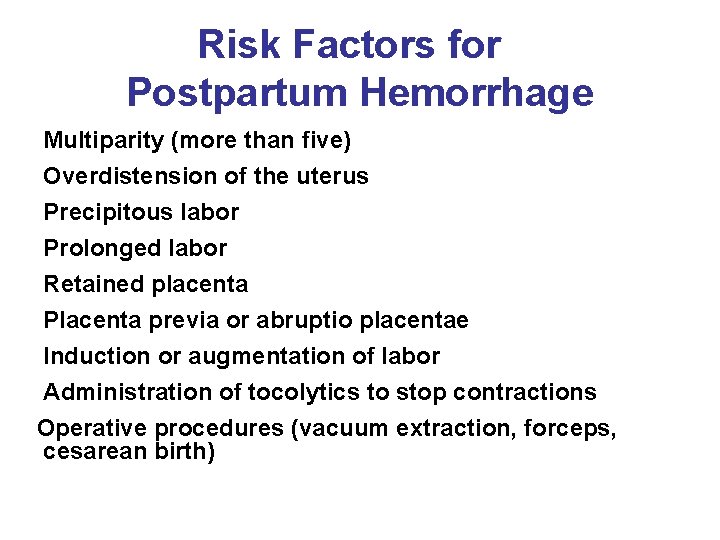
Risk Factors for Postpartum Hemorrhage Multiparity (more than five) Overdistension of the uterus Precipitous labor Prolonged labor Retained placenta Placenta previa or abruptio placentae Induction or augmentation of labor Administration of tocolytics to stop contractions Operative procedures (vacuum extraction, forceps, cesarean birth)
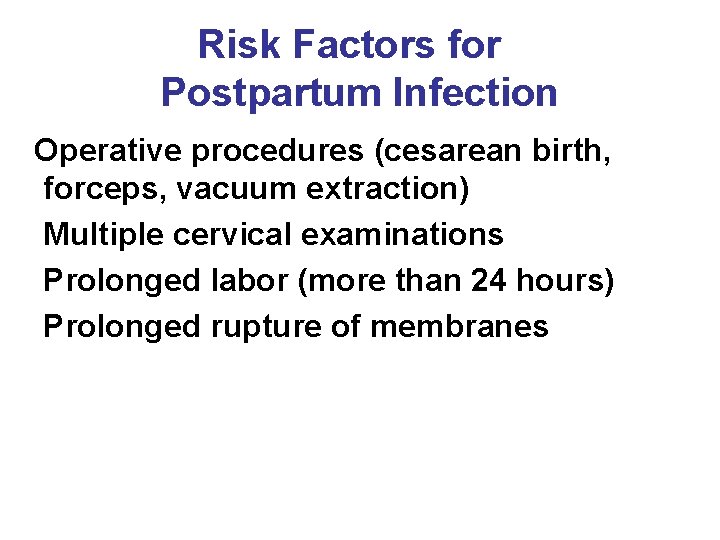
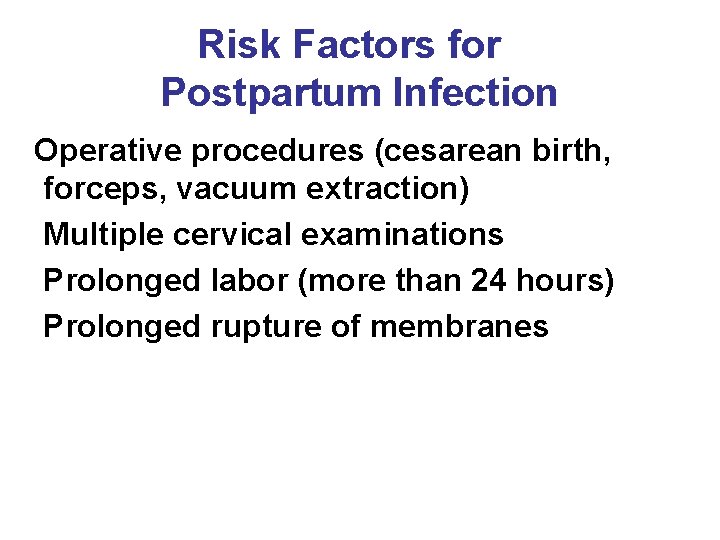
Risk Factors for Postpartum Infection Operative procedures (cesarean birth, forceps, vacuum extraction) Multiple cervical examinations Prolonged labor (more than 24 hours) Prolonged rupture of membranes
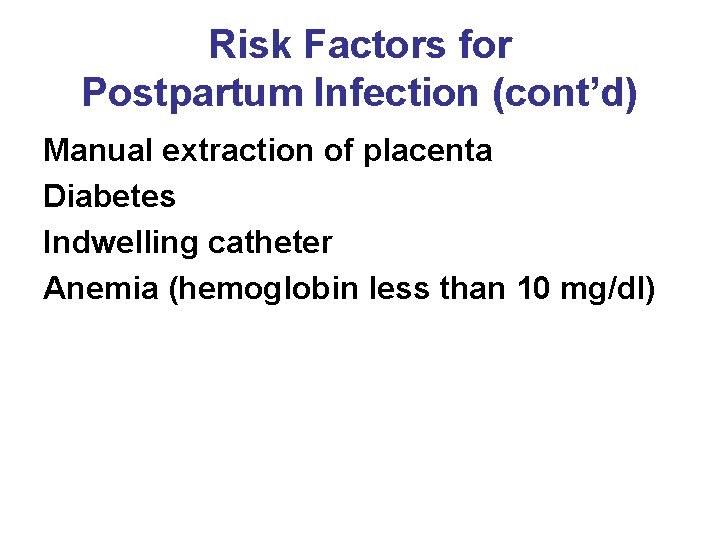
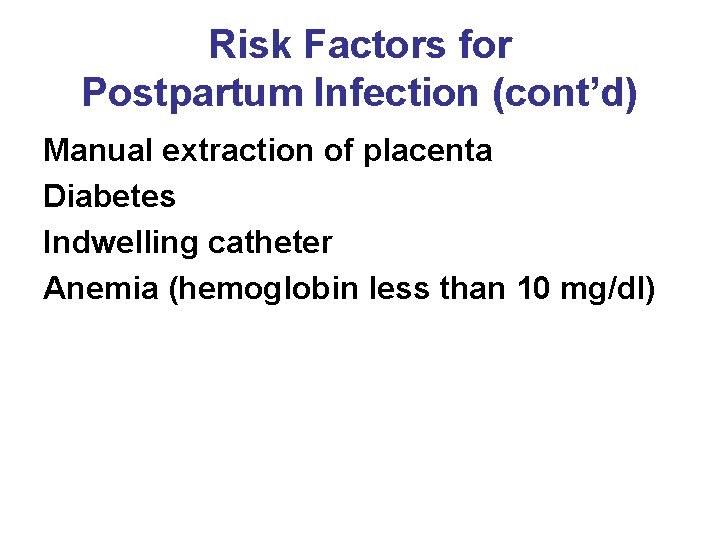
Risk Factors for Postpartum Infection (cont’d) Manual extraction of placenta Diabetes Indwelling catheter Anemia (hemoglobin less than 10 mg/dl)
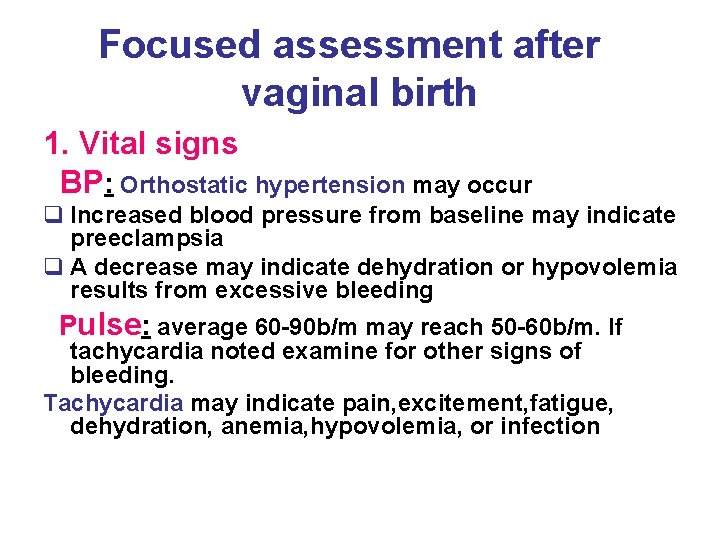
Focused assessment after vaginal birth 1. Vital signs BP: Orthostatic hypertension may occur q Increased blood pressure from baseline may indicate preeclampsia q A decrease may indicate dehydration or hypovolemia results from excessive bleeding Pulse: average 60 -90 b/m may reach 50 -60 b/m. If tachycardia noted examine for other signs of bleeding. Tachycardia may indicate pain, excitement, fatigue, dehydration, anemia, hypovolemia, or infection
Respiration: 12 -20 breath /m Auscultation of breath sound is necessary in some situation such as C/S, smoking , asthma, upper respiratory tract infection and those receiving Magnesium Sulfate Temp: Up to 38 is normal for 24 hour may be caused by dehydration or normal leukocytosis but if more than 38 after 24 hour is considered abnormal Pain: type, location and severity
2. Fundus: consistency and location § If the uterus is above the expected level or shifted from midline the bladder may be distended § If the fundus is difficult to locate or is soft(boggy), stimulate it by gentle massage 3. Lochia: amount , color and odor § A constant trickle or dribble of lochia indicates excessive bleeding and requires immediate interventions § Excessive lochia in the presence of contracted uterus suggest laceration of birth canal § The odor of lochia is usually described as fleshy or earthy , a foul odor suggest infection § Absence of lochia may also suggest infection § If the birth is C/S lochia may be scant
4. Perineum : REEDA R: Redness E: Edema E: Ecchymosis D: Discharge A: Approximation 5. Bladder elimination: q 1. 2. 3. 4. 5. 6. Examine signs of distended bladder which include: Location of fundus above baseline level Fundus displaced from midline Excessive lochia Bladder discomfort Bulge of bladder above symphysis pubis Frequent voiding of less than 150 ml of urine , which may indicate retention q voiding at least 300 -400 ml indicate that bladder is empty q urgency, frequency and dysuria suggest infection
6. Breast: Inspection(size, shape, symmetry, nipple and skin) q The first two days the breast is soft and nontender q The areola should be inspected for retraction or flatness which affects breast feeding q Signs of nipple trauma such as redness and fissures q palpation: for firmness and tenderness, the breast may feel lumpy 7. lower extremities; signs of DVT, Homan’s sign and edema 8. Edema and DTR q Pedal or peritibial edema may be present for the first few days q Diuresis is highest between day 2 -5 and is complete day 21 q Deep tendon reflexes should be +1 0 r +2
Care in the post partum period • Postpartum period is often divided into three periods • 1. Immediate postpartum period: the first 24 hours • 2. Early postpartum period; the first week • 3. late postpartum period: 2 -6 weeks
Care in The Immediate Post partum Period(first 24 hour) 1. Providing Comfort measures q -Ice packs: during first 12 -24 hours It should be wrapped with washcloth before it applied to the perineum and should left in place until ice is melt, then removed for 10 minute before another pack is applied q -Perinael care: squirting warm water over perinuim after voiding or bowel elimination q -Topical medication: Anesthetic spray to decrease discomfort , should be used after perineal care and before new pad is applied
q Sitting measures: advise the mother to squeeze her buttocks together before sitting and to lower her weight slowly onto her buttocks Sitting slightly in the side q Sitz baths: warm water if more than 24 hour q Analgesics: encourage mother to take analgesics for perineal pain and after pain Many analgesics contain acetaminophen, so the nurse should be careful that the client receives no more than 4 g of acetaminophen in 24 hour period
2. Promoting baldder elimination - Measure to stimulate voiding q Medicating woman for perineal pain q Running water, place hand in water, pouring water over vulva q. Encourage urination in shower or sitz baths q Hot tea or other fluids q Ask mother to blow abubble through straw
* Mother must be catheterized if: q she is unable to void q the amount voided less than 150 ml q the fundus is elevated or displaced from midline 3. Providing fluid and food q Fluid 2500 ml/day q Encourage healthy food choices 4. Preventing Thrombphlebitis: Encourage ambulation
Teaching after Birth 1. Teaching the process of involution How to assess lochia and palpate fundus 2. Teaching Self care q Hand washing: before touching breasts, after diaper changes and after elimination q Breast care and suppression of lactation if not breast feed q Care of C/S q Perineal care q Kegel’s exercise
3. Promoting rest and sleep Rest measures at the birth facility § Group assessment and care to minimize interruptions § Restricts phone calls and visitors during time of napping Encourage the use of side lying position for breast feeding

§ Rest measures at home § Maintain flexible routine that focuses on care of the mother and infant § Nap or rest whenever the infant is sleeps if possible § Plan simple meals and flexible meal times § Limit visitors § Accept assistance with food preparation and house work § Ask the mother to reduce caffeine for the first few weeks and use relaxation techniques and to share her feeling s and concerns
4. Providing Nutrition counseling § Avoid severe restriction of caloric intake 5. Promoting regular bowel elimination § exercise, fluid and fiber § Walking and drinking at least 8 glasses of fluid daily § A regular schedule of bowel elimination such as after breakfast , this will allows the advantage of gastrocolic reflex stimulation of peristalsis induced in the colon when food is consumed in an empty stomach) 6. Promoting good body mechanics and exercise 7. Counseling about sexual activity 8. Teaching about follow up appointment( usually 2 -6 weeks )
9. Teaching about S/S that should be reported q -Fever q -Localized area of redness, swelling, or pain in either breast q -Persistent abdominal tenderness q -Feeling of pelvic fullness or pressure q -Persistent perineal pain q -Frequency, urgency or burning in urination q -Chang in character of lochia: increased amount, resumption of bright red color or foul odor) q -Localized tenderness , redness or warmth of leg q -Separation or foul drainage from C/S