Capillary rethink time Andrew Magnay University Hospital of


- Slides: 55

Capillary rethink time Andrew Magnay University Hospital of North Staffordshire NHS Trust
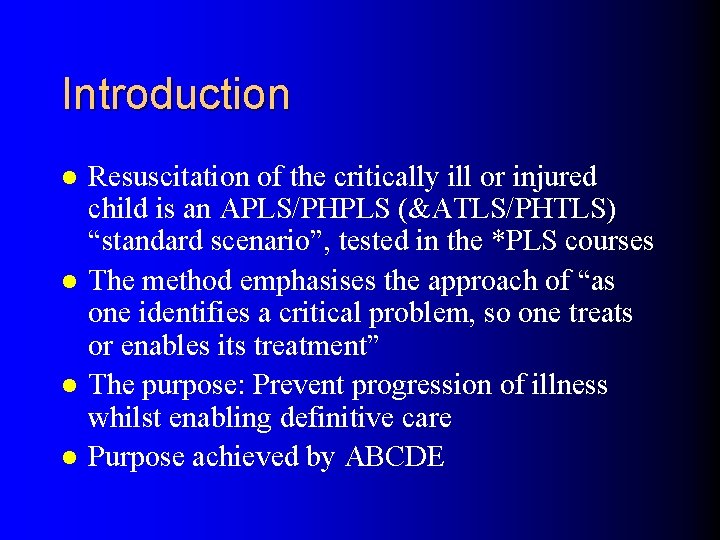
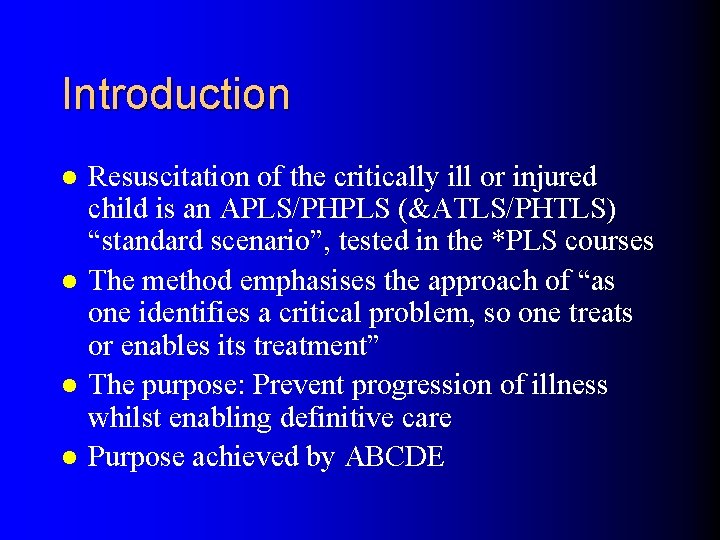
Introduction l l Resuscitation of the critically ill or injured child is an APLS/PHPLS (&ATLS/PHTLS) “standard scenario”, tested in the *PLS courses The method emphasises the approach of “as one identifies a critical problem, so one treats or enables its treatment” The purpose: Prevent progression of illness whilst enabling definitive care Purpose achieved by ABCDE
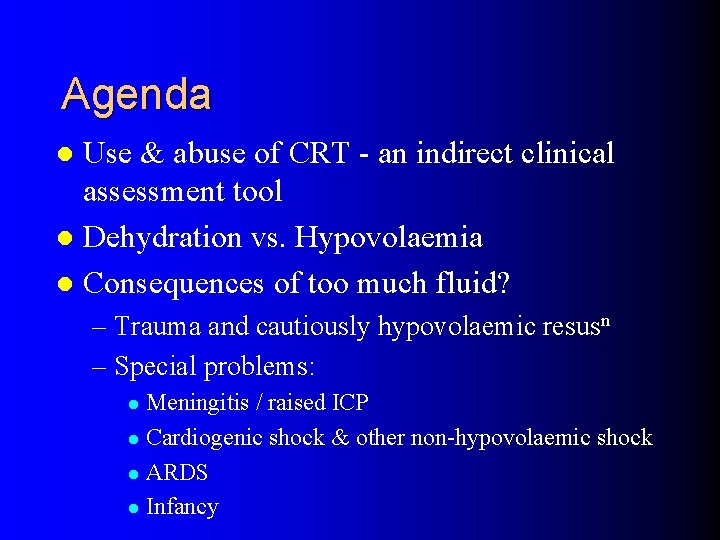
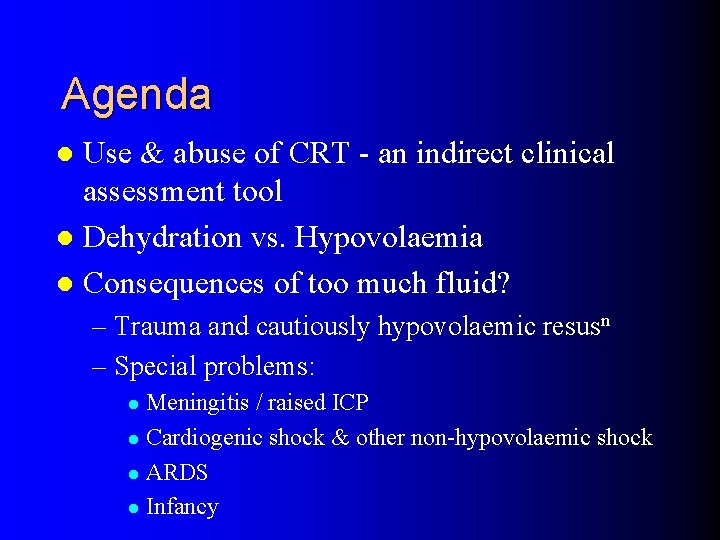
Agenda Use & abuse of CRT - an indirect clinical assessment tool l Dehydration vs. Hypovolaemia l Consequences of too much fluid? l – Trauma and cautiously hypovolaemic resusn – Special problems: Meningitis / raised ICP l Cardiogenic shock & other non-hypovolaemic shock l ARDS l Infancy l
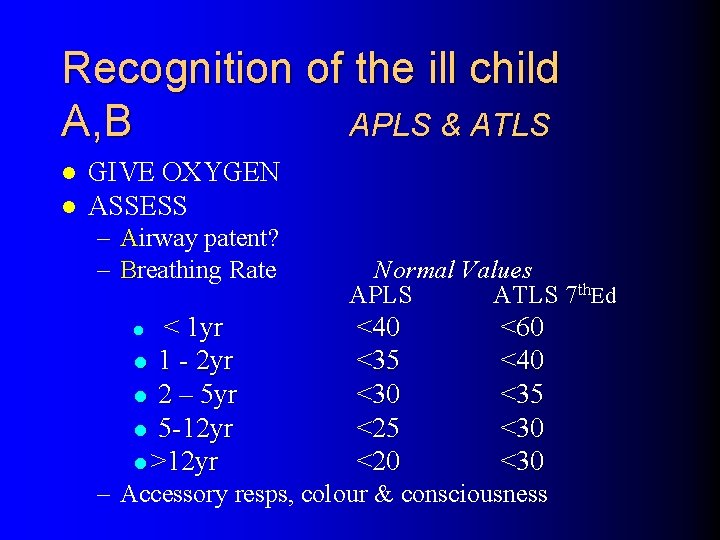
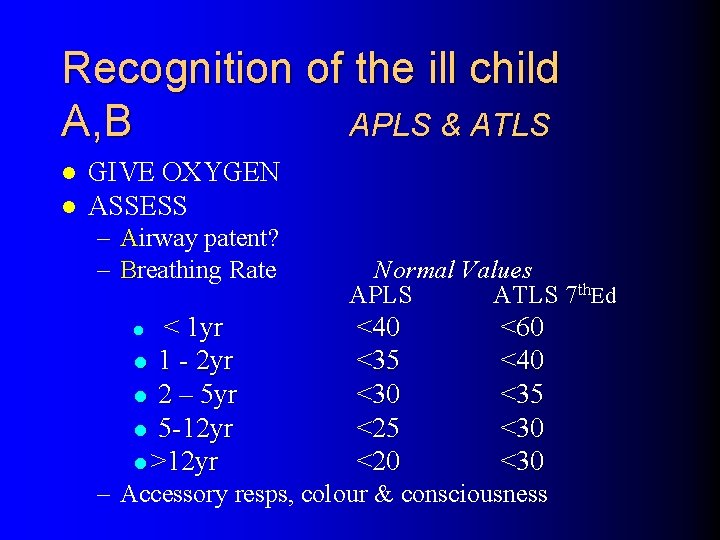
Recognition of the ill child A, B APLS & ATLS l l GIVE OXYGEN ASSESS – Airway patent? – Breathing Rate < 1 yr l 1 - 2 yr l 2 – 5 yr l 5 -12 yr l >12 yr l Normal Values APLS ATLS 7 th. Ed <40 <35 <30 <25 <20 <60 <40 <35 <30 – Accessory resps, colour & consciousness
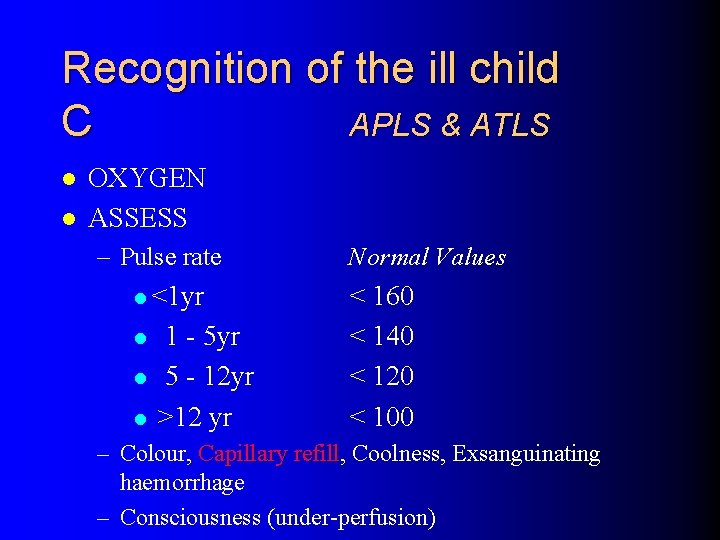
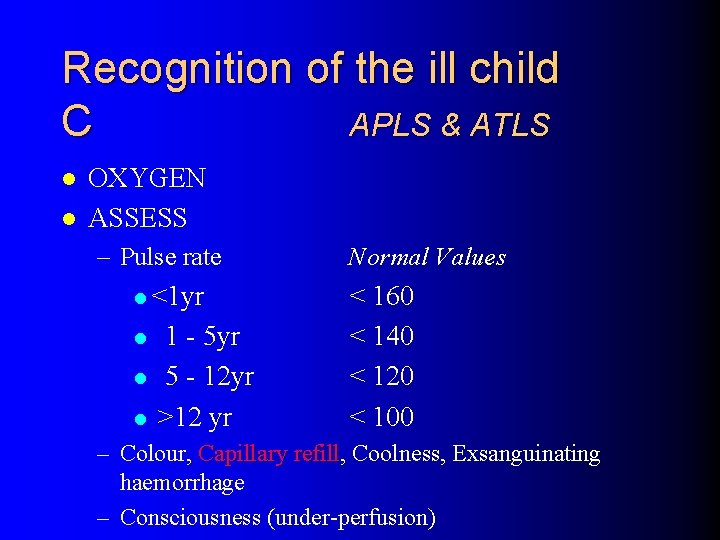
Recognition of the ill child C APLS & ATLS l l OXYGEN ASSESS – Pulse rate l <1 yr l l l 1 - 5 yr 5 - 12 yr >12 yr Normal Values < 160 < 140 < 120 < 100 – Colour, Capillary refill, refill Coolness, Exsanguinating haemorrhage – Consciousness (under-perfusion)
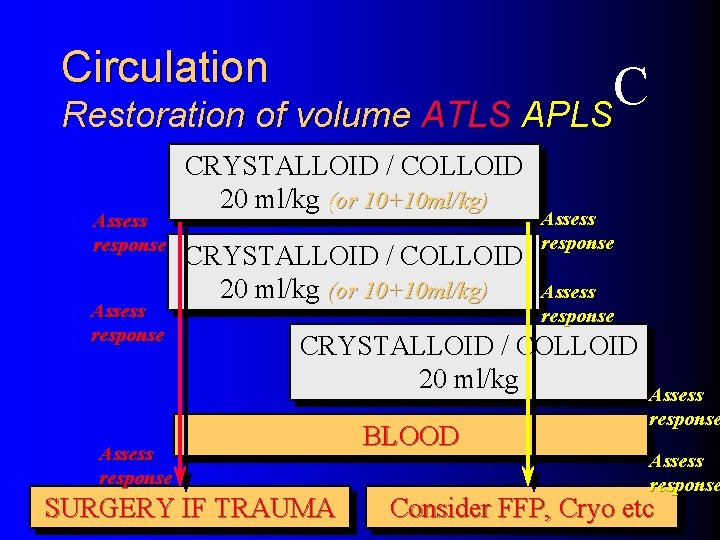
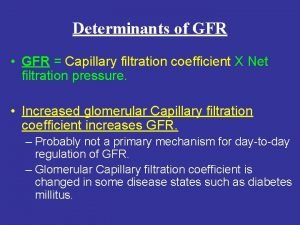
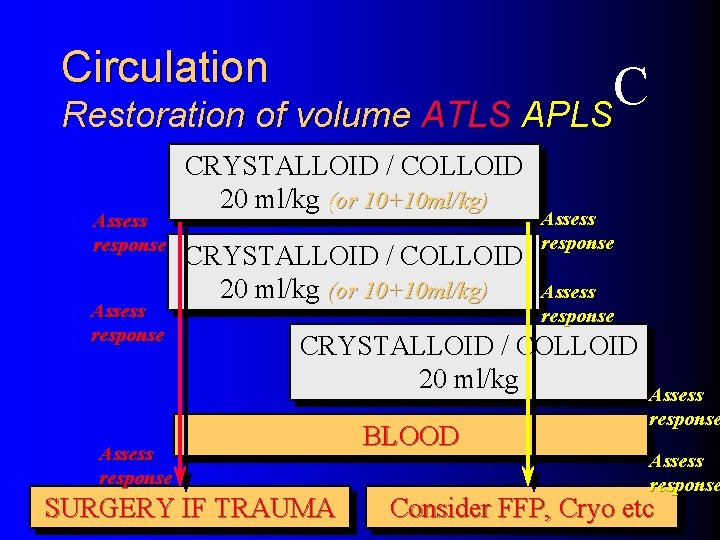
Circulation C Restoration of volume ATLS APLS Assess response CRYSTALLOID / COLLOID 20 ml/kg (or 10+10 ml/kg) Assess response CRYSTALLOID / COLLOID 20 ml/kg Assess response SURGERY IF TRAUMA BLOOD Assess response Consider FFP, Cryo etc
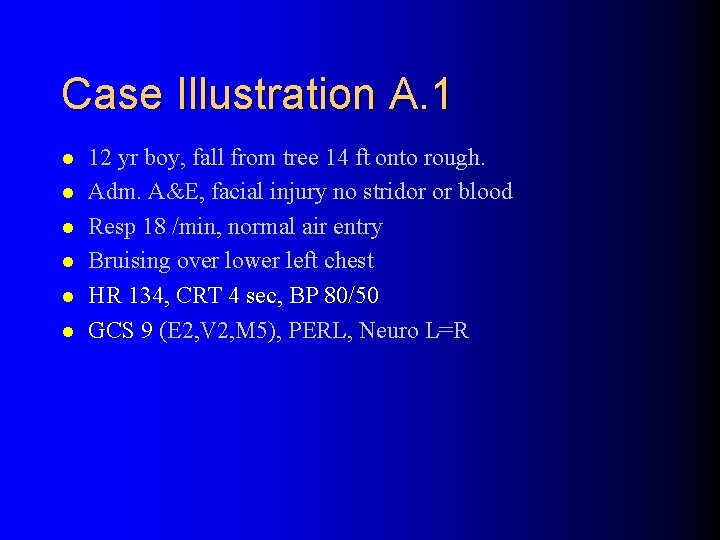
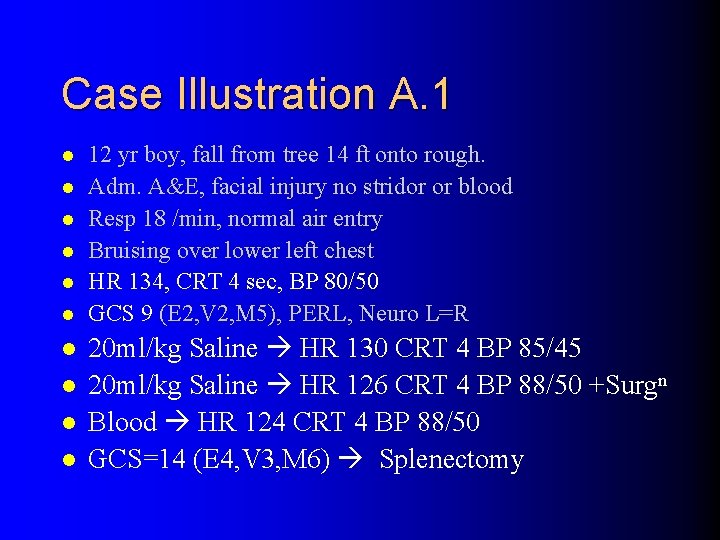
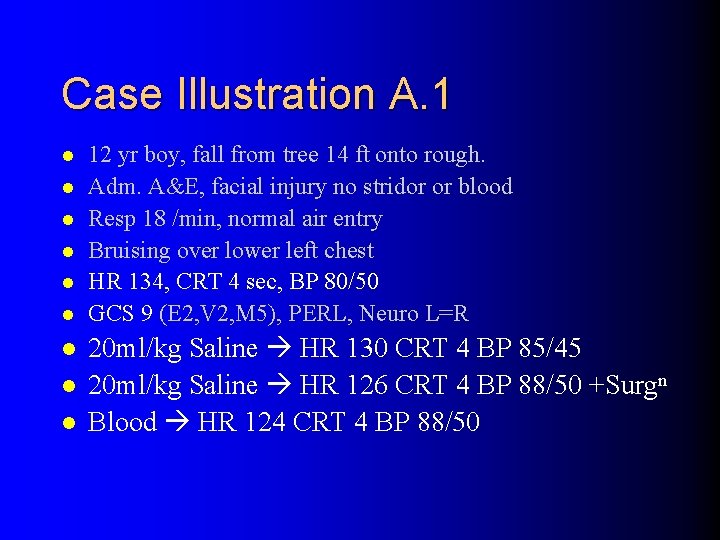
Case Illustration A. 1 l l l 12 yr boy, fall from tree 14 ft onto rough. Adm. A&E, facial injury no stridor or blood Resp 18 /min, normal air entry Bruising over lower left chest HR 134, CRT 4 sec, BP 80/50 GCS 9 (E 2, V 2, M 5), PERL, Neuro L=R
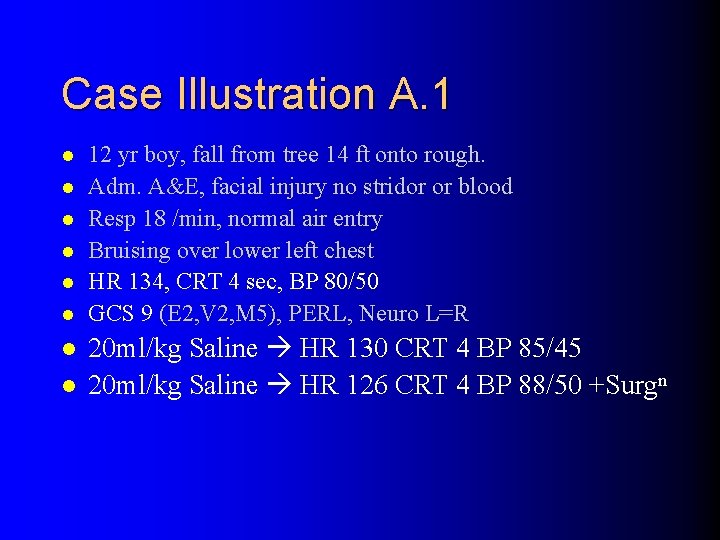
Case Illustration A. 1 l l l l 12 yr boy, fall from tree 14 ft onto rough. Adm. A&E, facial injury no stridor or blood Resp 18 /min, normal air entry Bruising over lower left chest HR 134, CRT 4 sec, BP 80/50 GCS 9 (E 2, V 2, M 5), PERL, Neuro L=R 20 ml/kg Saline HR 130 CRT 4 BP 85/45 20 ml/kg Saline HR 126 CRT 4 BP 88/50 +Surgn
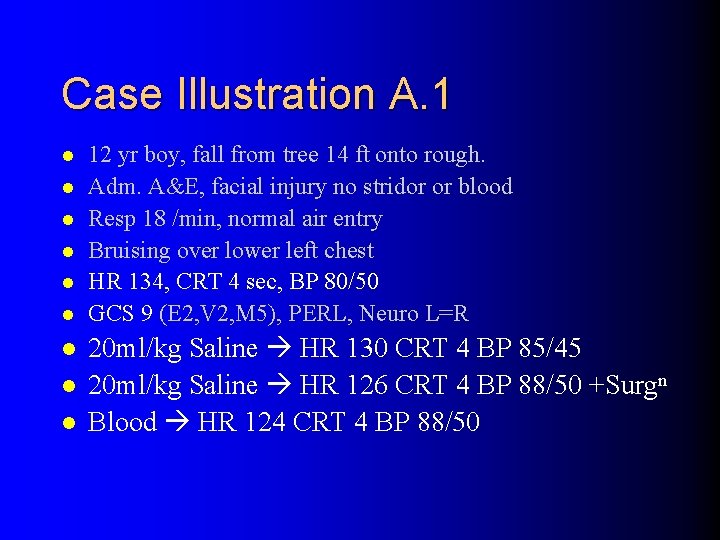
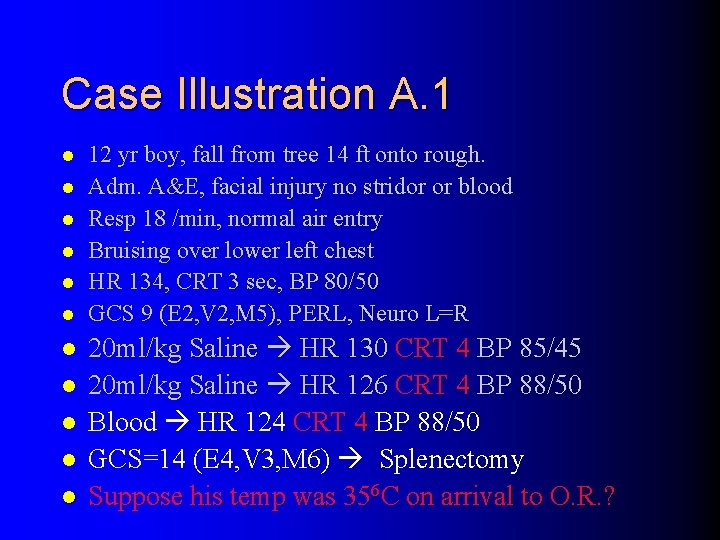
Case Illustration A. 1 l l l l l 12 yr boy, fall from tree 14 ft onto rough. Adm. A&E, facial injury no stridor or blood Resp 18 /min, normal air entry Bruising over lower left chest HR 134, CRT 4 sec, BP 80/50 GCS 9 (E 2, V 2, M 5), PERL, Neuro L=R 20 ml/kg Saline HR 130 CRT 4 BP 85/45 20 ml/kg Saline HR 126 CRT 4 BP 88/50 +Surgn Blood HR 124 CRT 4 BP 88/50
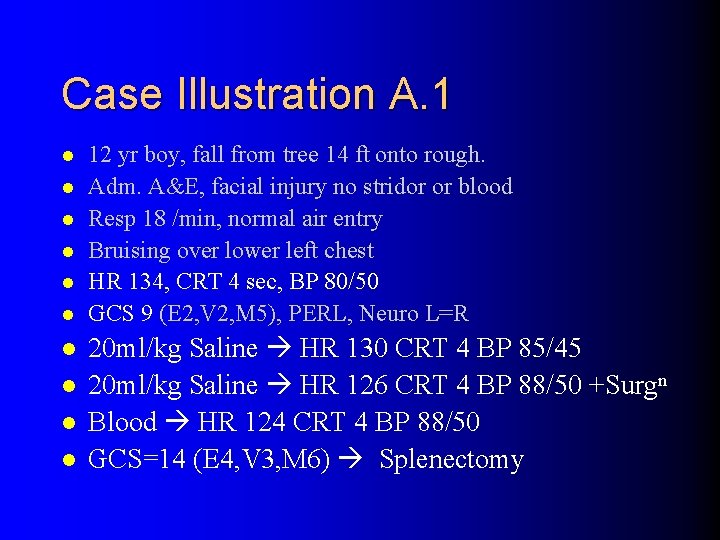
Case Illustration A. 1 l l l l l 12 yr boy, fall from tree 14 ft onto rough. Adm. A&E, facial injury no stridor or blood Resp 18 /min, normal air entry Bruising over lower left chest HR 134, CRT 4 sec, BP 80/50 GCS 9 (E 2, V 2, M 5), PERL, Neuro L=R 20 ml/kg Saline HR 130 CRT 4 BP 85/45 20 ml/kg Saline HR 126 CRT 4 BP 88/50 +Surgn Blood HR 124 CRT 4 BP 88/50 GCS=14 (E 4, V 3, M 6) Splenectomy
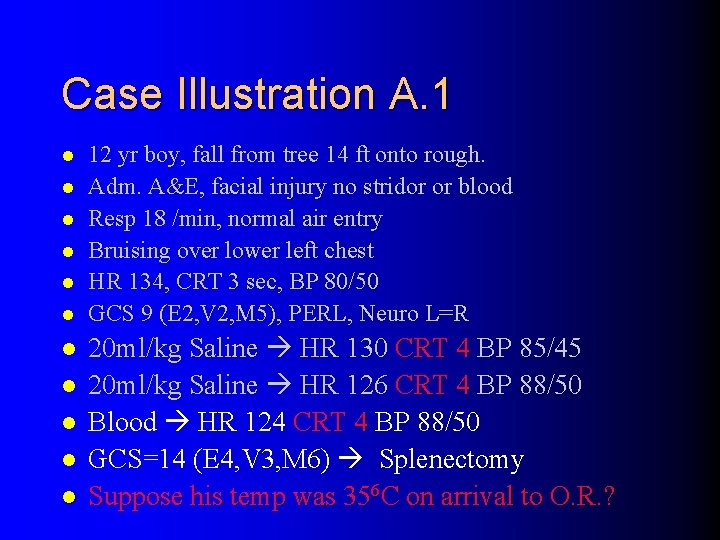
Case Illustration A. 1 l l l 12 yr boy, fall from tree 14 ft onto rough. Adm. A&E, facial injury no stridor or blood Resp 18 /min, normal air entry Bruising over lower left chest HR 134, CRT 3 sec, BP 80/50 GCS 9 (E 2, V 2, M 5), PERL, Neuro L=R 20 ml/kg Saline HR 130 CRT 4 BP 85/45 20 ml/kg Saline HR 126 CRT 4 BP 88/50 Blood HR 124 CRT 4 BP 88/50 GCS=14 (E 4, V 3, M 6) Splenectomy Suppose his temp was 356 C on arrival to O. R. ?
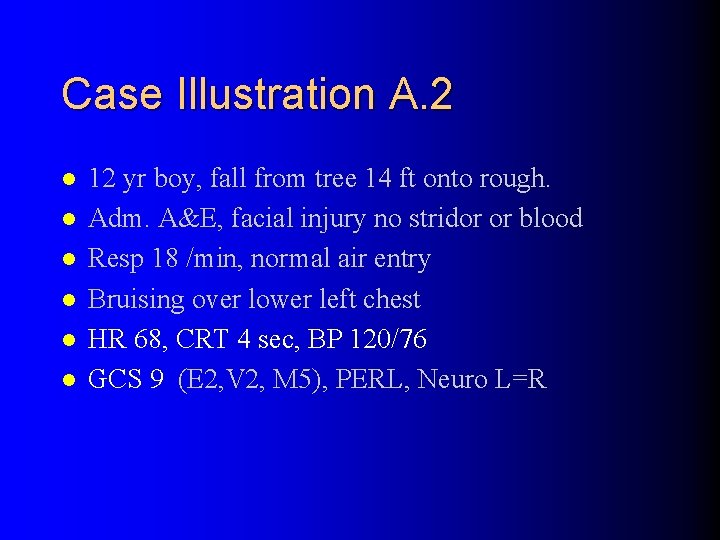
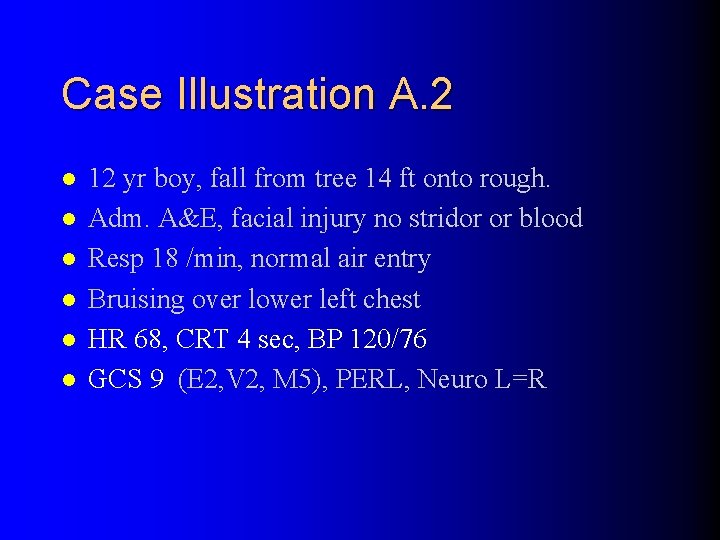
Case Illustration A. 2 l l l 12 yr boy, fall from tree 14 ft onto rough. Adm. A&E, facial injury no stridor or blood Resp 18 /min, normal air entry Bruising over lower left chest HR 68, CRT 4 sec, BP 120/76 GCS 9 (E 2, V 2, M 5), PERL, Neuro L=R
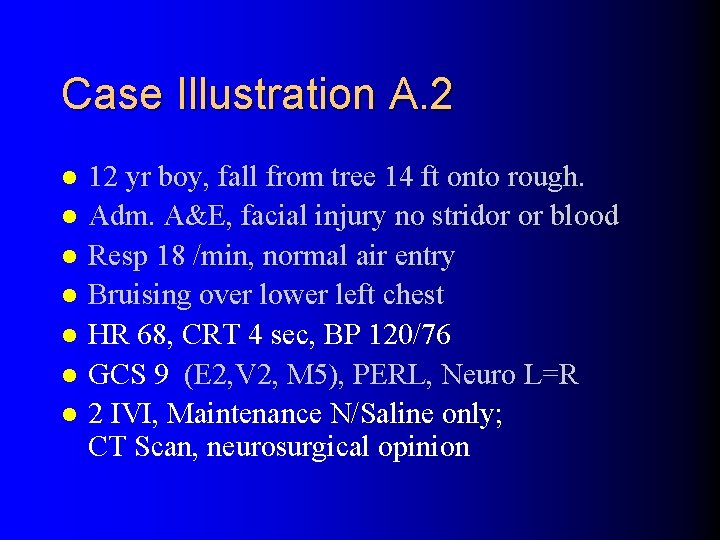
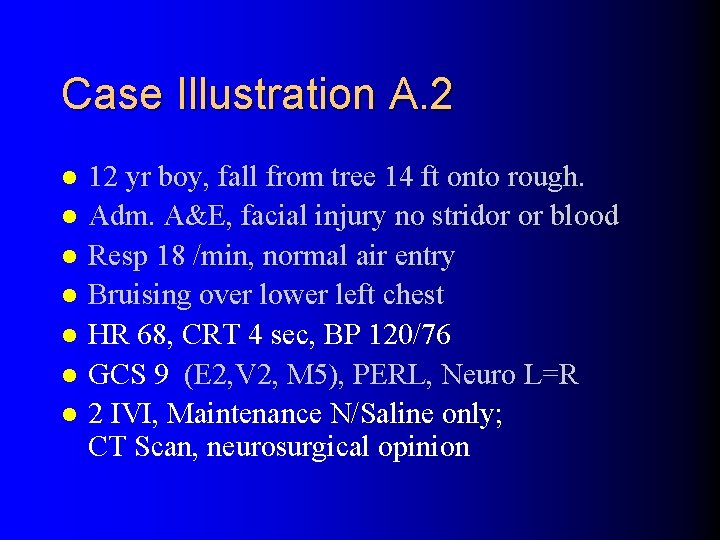
Case Illustration A. 2 l l l l 12 yr boy, fall from tree 14 ft onto rough. Adm. A&E, facial injury no stridor or blood Resp 18 /min, normal air entry Bruising over lower left chest HR 68, CRT 4 sec, BP 120/76 GCS 9 (E 2, V 2, M 5), PERL, Neuro L=R 2 IVI, Maintenance N/Saline only; CT Scan, neurosurgical opinion
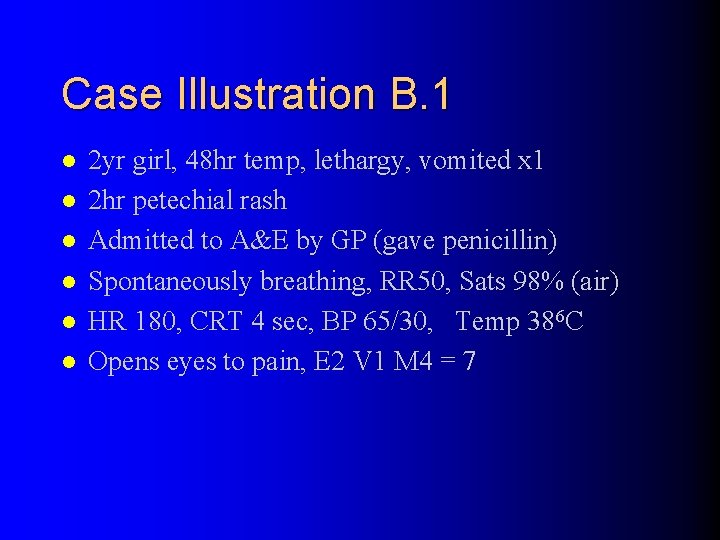
Case Illustration B. 1 l l l 2 yr girl, 48 hr temp, lethargy, vomited x 1 2 hr petechial rash Admitted to A&E by GP (gave penicillin) Spontaneously breathing, RR 50, Sats 98% (air) HR 180, CRT 4 sec, BP 65/30, Temp 386 C Opens eyes to pain, E 2 V 1 M 4 = 7
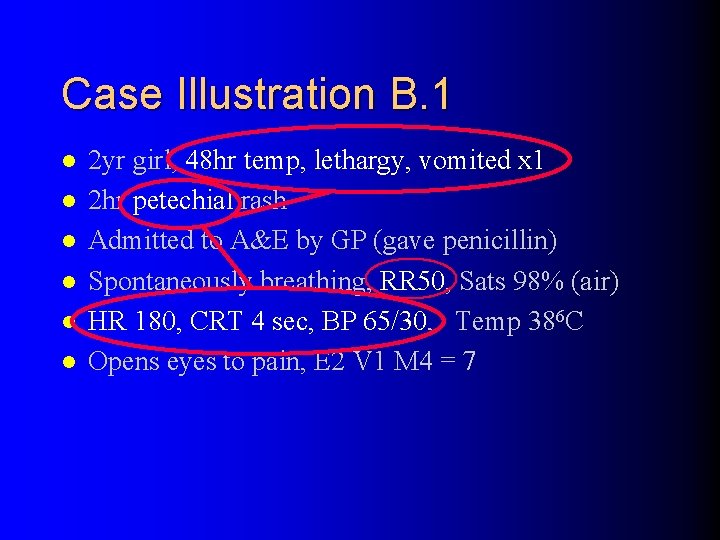
Case Illustration B. 1 l l l 2 yr girl, 48 hr temp, lethargy, vomited x 1 2 hr petechial rash Admitted to A&E by GP (gave penicillin) Spontaneously breathing, RR 50, Sats 98% (air) HR 180, CRT 4 sec, BP 65/30, Temp 386 C Opens eyes to pain, E 2 V 1 M 4 = 7
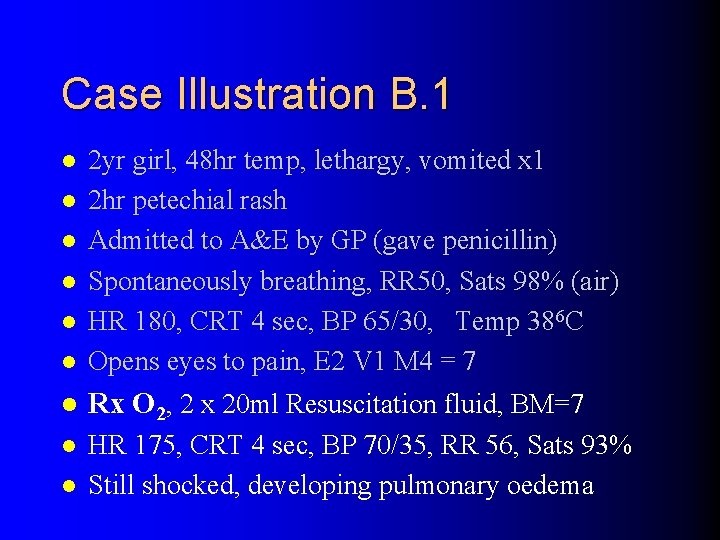
Case Illustration B. 1 l 2 yr girl, 48 hr temp, lethargy, vomited x 1 2 hr petechial rash Admitted to A&E by GP (gave penicillin) Spontaneously breathing, RR 50, Sats 98% (air) HR 180, CRT 4 sec, BP 65/30, Temp 386 C Opens eyes to pain, E 2 V 1 M 4 = 7 l Rx O 2, 2 x 20 ml Resuscitation fluid, BM=7 l HR 175, CRT 4 sec, BP 70/35, RR 56, Sats 93% Still shocked, developing pulmonary oedema l l l
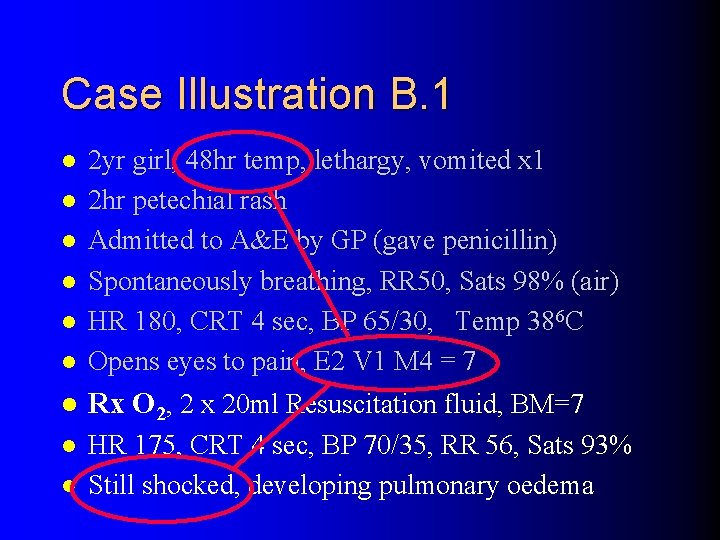
Case Illustration B. 1 l 2 yr girl, 48 hr temp, lethargy, vomited x 1 2 hr petechial rash Admitted to A&E by GP (gave penicillin) Spontaneously breathing, RR 50, Sats 98% (air) HR 180, CRT 4 sec, BP 65/30, Temp 386 C Opens eyes to pain, E 2 V 1 M 4 = 7 l Rx O 2, 2 x 20 ml Resuscitation fluid, BM=7 l HR 175, CRT 4 sec, BP 70/35, RR 56, Sats 93% Still shocked, developing pulmonary oedema l l l
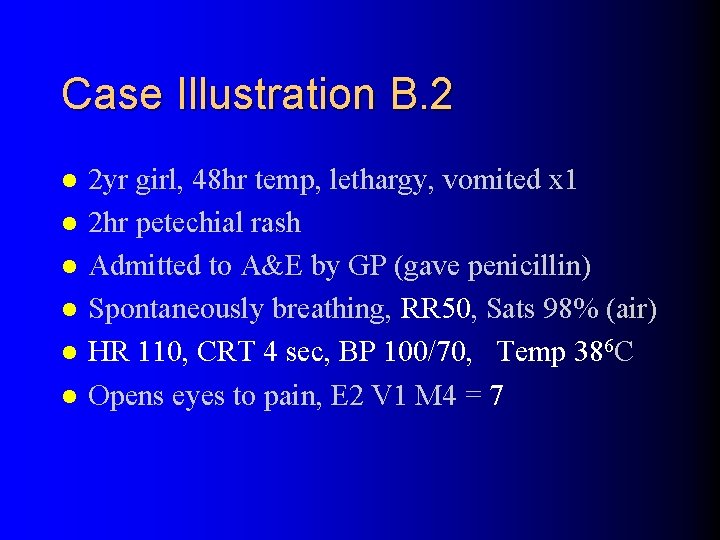
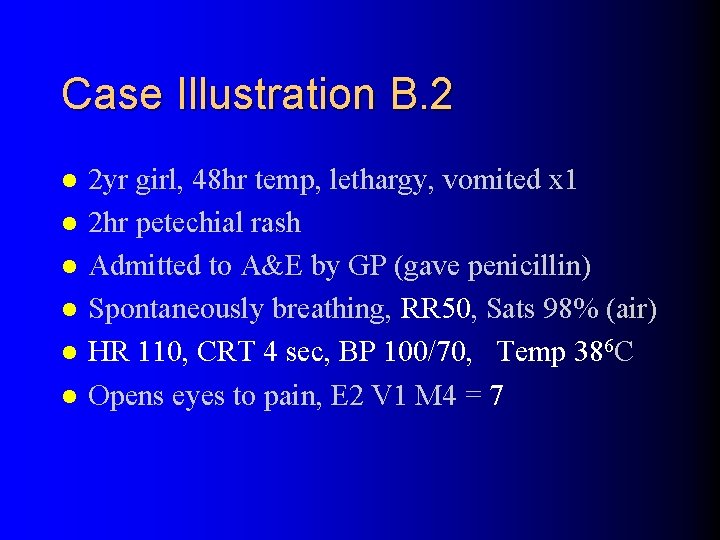
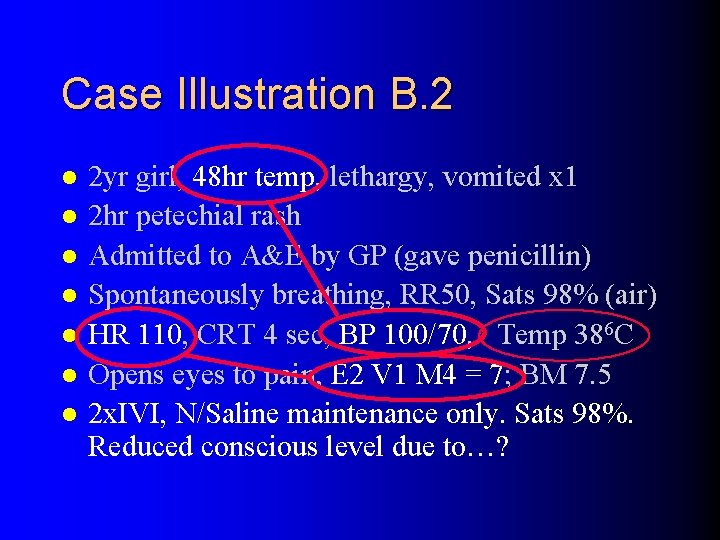
Case Illustration B. 2 l l l 2 yr girl, 48 hr temp, lethargy, vomited x 1 2 hr petechial rash Admitted to A&E by GP (gave penicillin) Spontaneously breathing, RR 50, Sats 98% (air) HR 110, CRT 4 sec, BP 100/70, Temp 386 C Opens eyes to pain, E 2 V 1 M 4 = 7
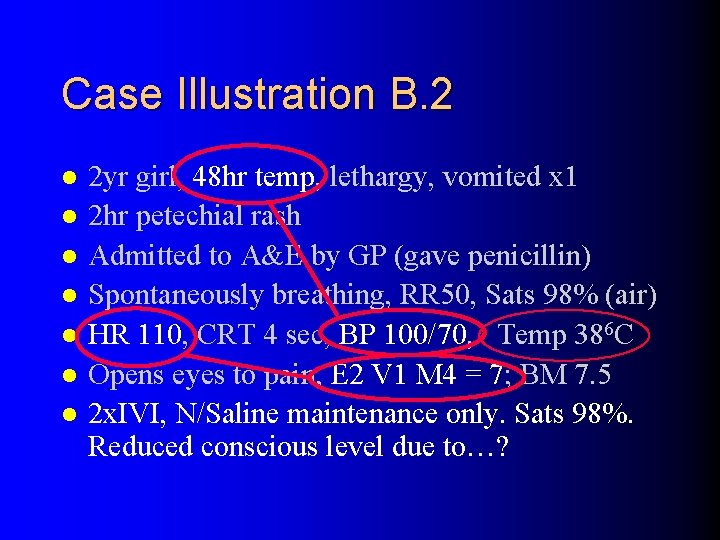
Case Illustration B. 2 l l l l 2 yr girl, 48 hr temp, lethargy, vomited x 1 2 hr petechial rash Admitted to A&E by GP (gave penicillin) Spontaneously breathing, RR 50, Sats 98% (air) HR 110, CRT 4 sec, BP 100/70, Temp 386 C Opens eyes to pain, E 2 V 1 M 4 = 7; BM 7. 5 2 x. IVI, N/Saline maintenance only. Sats 98%. Reduced conscious level due to…?
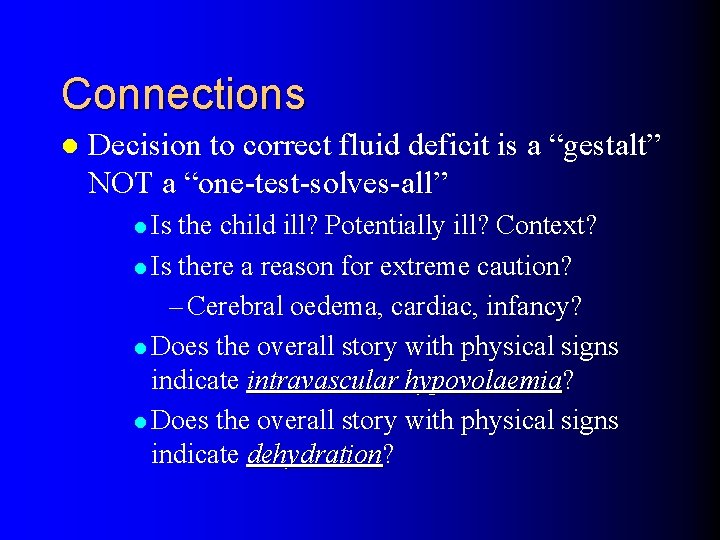
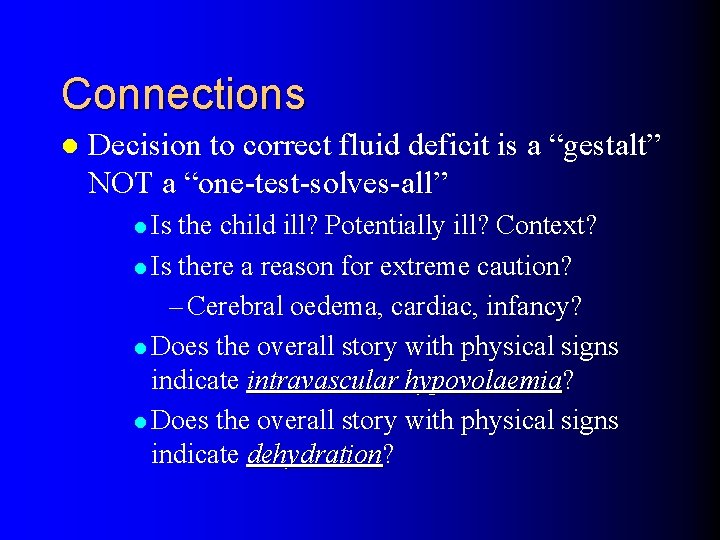
Connections l Decision to correct fluid deficit is a “gestalt” NOT a “one-test-solves-all” l Is the child ill? Potentially ill? Context? l Is there a reason for extreme caution? – Cerebral oedema, cardiac, infancy? l Does the overall story with physical signs indicate intravascular hypovolaemia? hypovolaemia l Does the overall story with physical signs indicate dehydration? dehydration
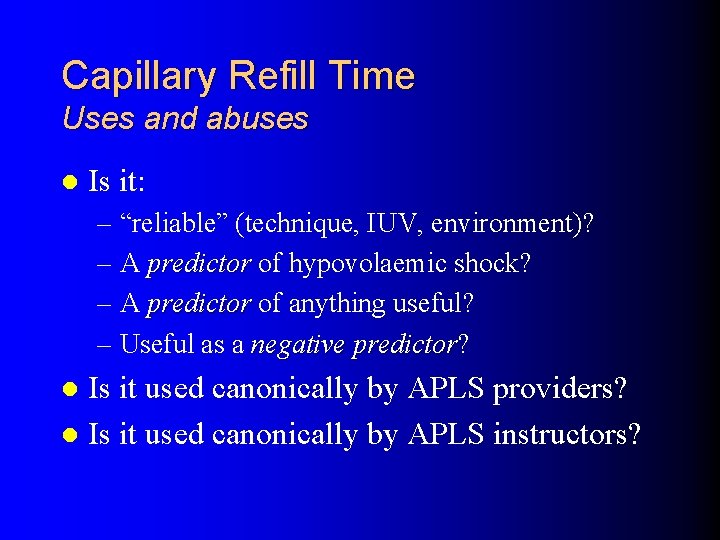
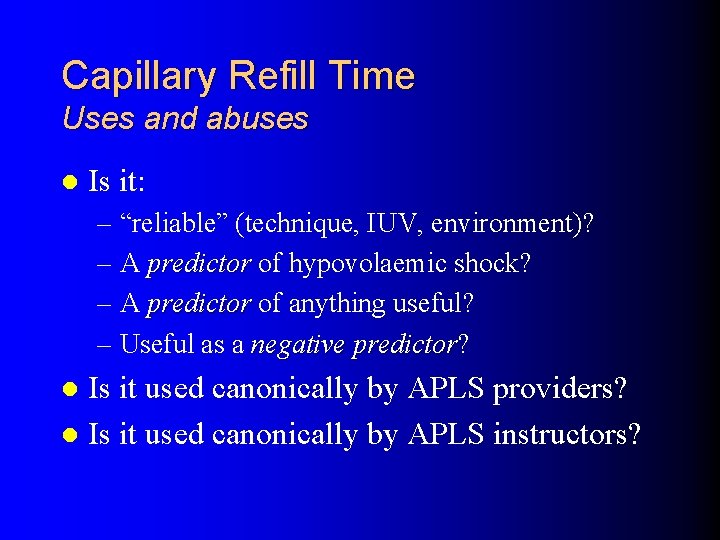
Capillary Refill Time Uses and abuses l Is it: – “reliable” (technique, IUV, environment)? – A predictor of hypovolaemic shock? – A predictor of anything useful? – Useful as a negative predictor? predictor Is it used canonically by APLS providers? l Is it used canonically by APLS instructors? l
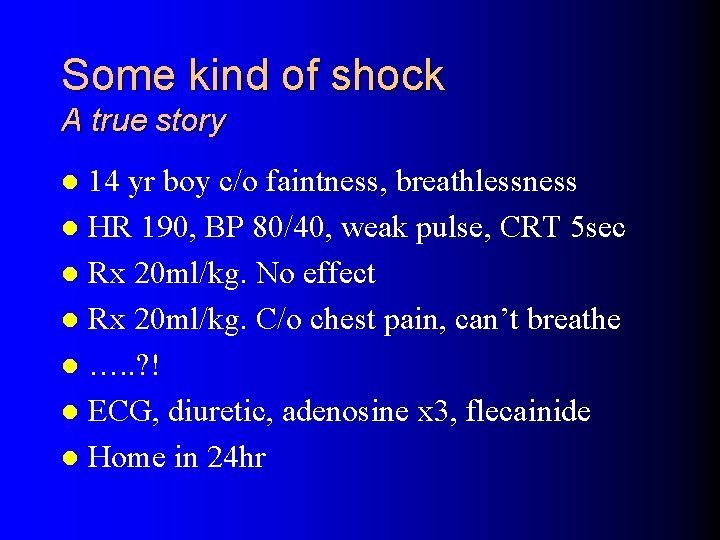
Some kind of shock A true story 14 yr boy c/o faintness, breathlessness l HR 190, BP 80/40, weak pulse, CRT 5 sec l Rx 20 ml/kg. No effect l Rx 20 ml/kg. C/o chest pain, can’t breathe l …. . ? ! l ECG, diuretic, adenosine x 3, flecainide l Home in 24 hr l
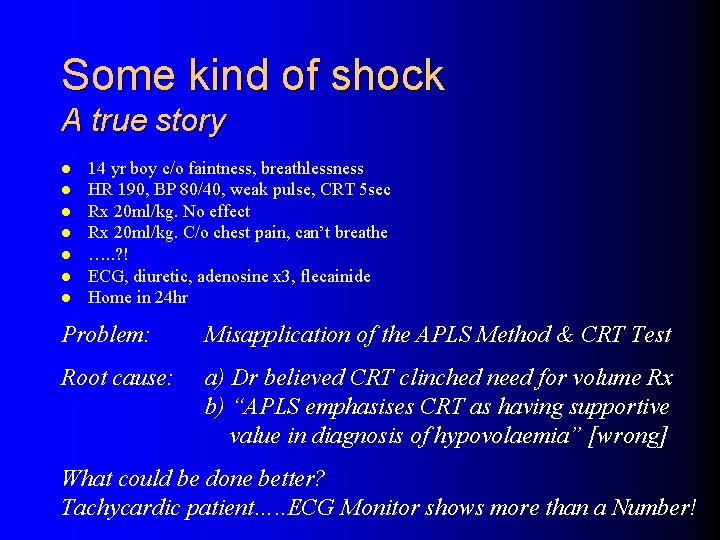
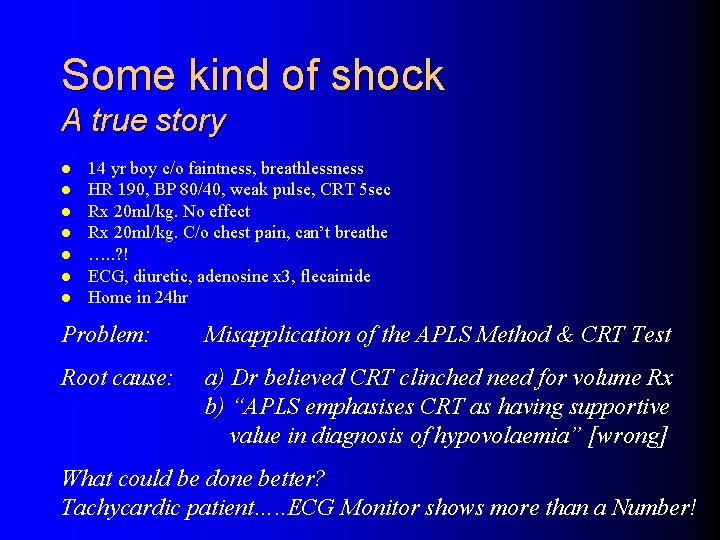
Some kind of shock A true story l l l l 14 yr boy c/o faintness, breathlessness HR 190, BP 80/40, weak pulse, CRT 5 sec Rx 20 ml/kg. No effect Rx 20 ml/kg. C/o chest pain, can’t breathe …. . ? ! ECG, diuretic, adenosine x 3, flecainide Home in 24 hr Problem: Misapplication of the APLS Method & CRT Test Root cause: a) Dr believed CRT clinched need for volume Rx b) “APLS emphasises CRT as having supportive value in diagnosis of hypovolaemia” [wrong] What could be done better? Tachycardic patient…. . ECG Monitor shows more than a Number!
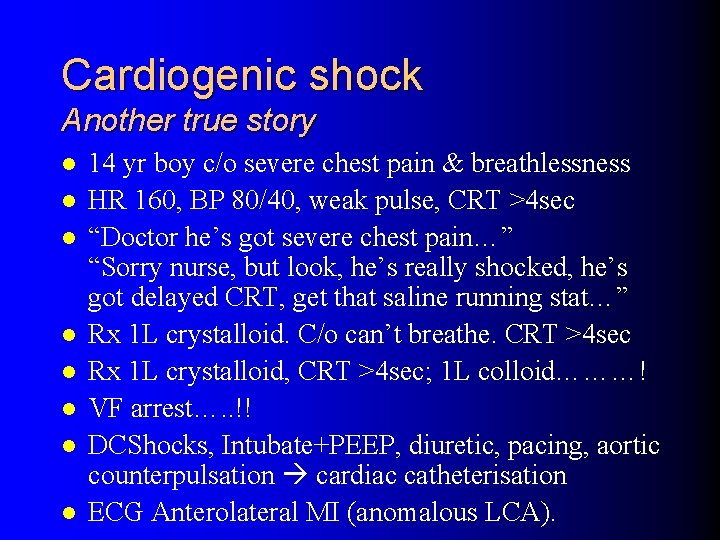
Cardiogenic shock Another true story l l l l 14 yr boy c/o severe chest pain & breathlessness HR 160, BP 80/40, weak pulse, CRT >4 sec “Doctor he’s got severe chest pain…” “Sorry nurse, but look, he’s really shocked, he’s got delayed CRT, get that saline running stat…” Rx 1 L crystalloid. C/o can’t breathe. CRT >4 sec Rx 1 L crystalloid, CRT >4 sec; 1 L colloid………! VF arrest…. . !! DCShocks, Intubate+PEEP, diuretic, pacing, aortic counterpulsation cardiac catheterisation ECG Anterolateral MI (anomalous LCA).
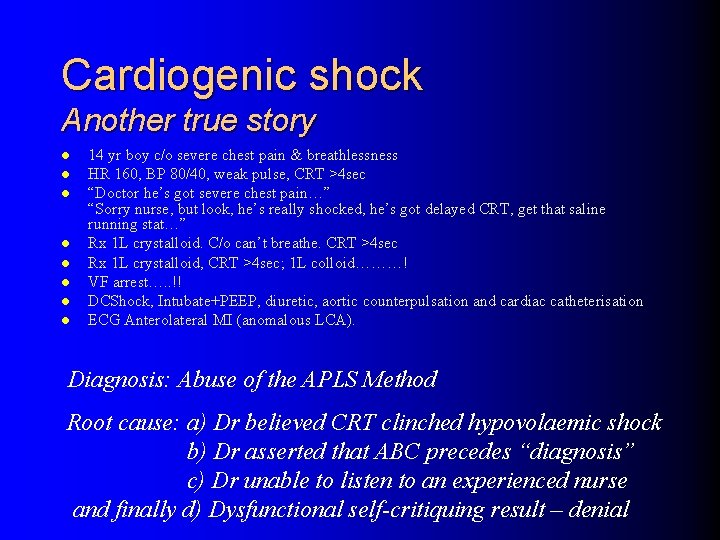
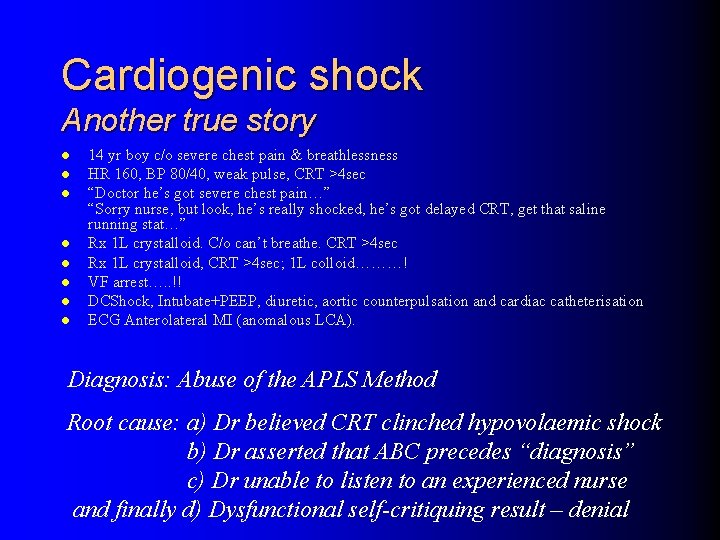
Cardiogenic shock Another true story l l l l 14 yr boy c/o severe chest pain & breathlessness HR 160, BP 80/40, weak pulse, CRT >4 sec “Doctor he’s got severe chest pain…” “Sorry nurse, but look, he’s really shocked, he’s got delayed CRT, get that saline running stat…” Rx 1 L crystalloid. C/o can’t breathe. CRT >4 sec Rx 1 L crystalloid, CRT >4 sec; 1 L colloid………! VF arrest…. . !! DCShock, Intubate+PEEP, diuretic, aortic counterpulsation and cardiac catheterisation ECG Anterolateral MI (anomalous LCA). Diagnosis: Abuse of the APLS Method Root cause: a) Dr believed CRT clinched hypovolaemic shock b) Dr asserted that ABC precedes “diagnosis” c) Dr unable to listen to an experienced nurse and finally d) Dysfunctional self-critiquing result – denial
Capillary Refill Time How useful is it really?
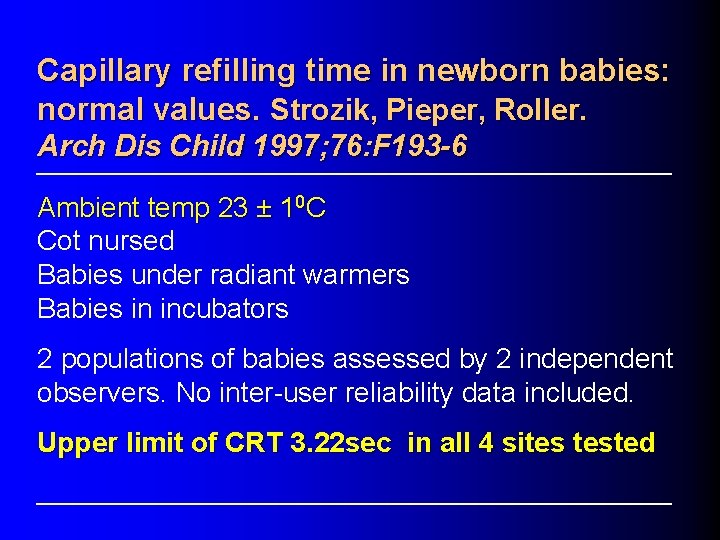
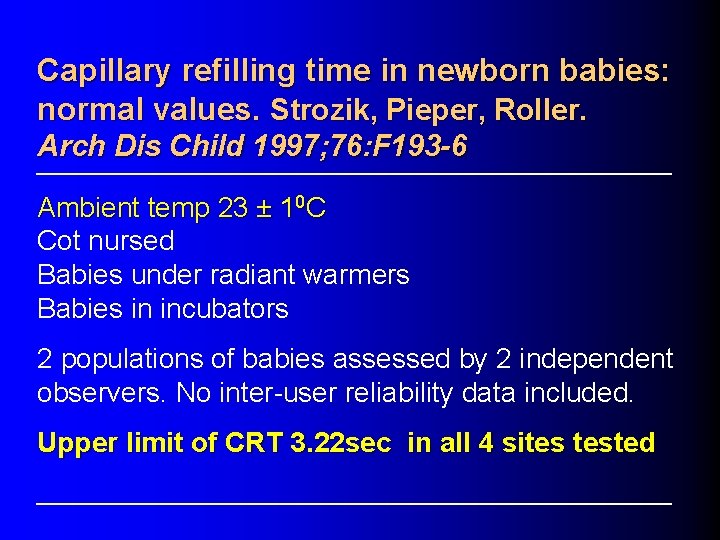
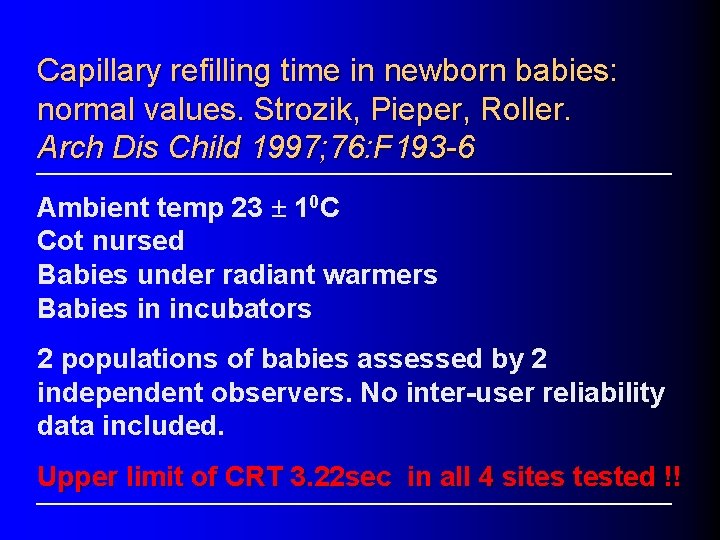
Capillary refilling time in newborn babies: normal values. Strozik, Pieper, Roller. Arch Dis Child 1997; 76: F 193 -6 Ambient temp 23 ± 10 C Cot nursed Babies under radiant warmers Babies in incubators 2 populations of babies assessed by 2 independent observers. No inter-user reliability data included. Upper limit of CRT 3. 22 sec in all 4 sites tested
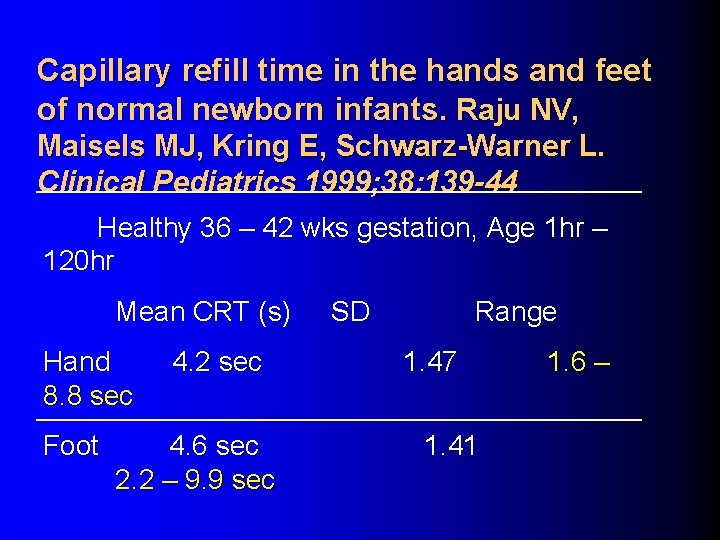
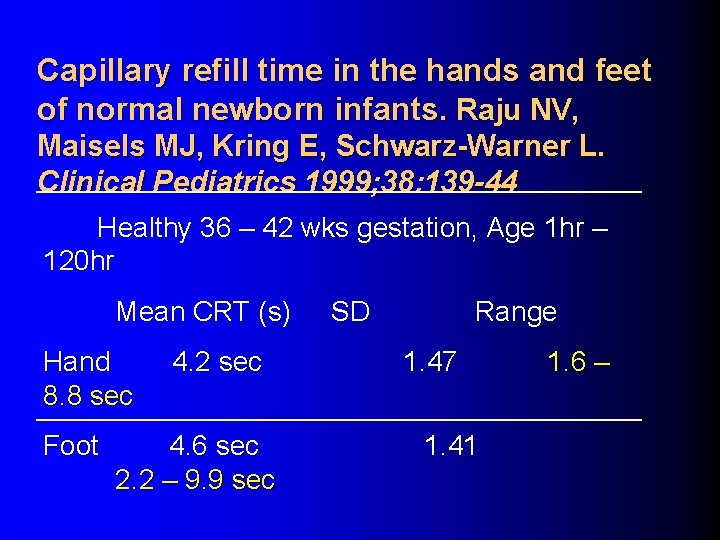
Capillary refill time in the hands and feet of normal newborn infants. Raju NV, Maisels MJ, Kring E, Schwarz-Warner L. Clinical Pediatrics 1999; 38: 139 -44 Healthy 36 – 42 wks gestation, Age 1 hr – 120 hr Mean CRT (s) Hand 8. 8 sec Foot 4. 2 sec 4. 6 sec 2. 2 – 9. 9 sec SD Range 1. 47 1. 41 1. 6 –
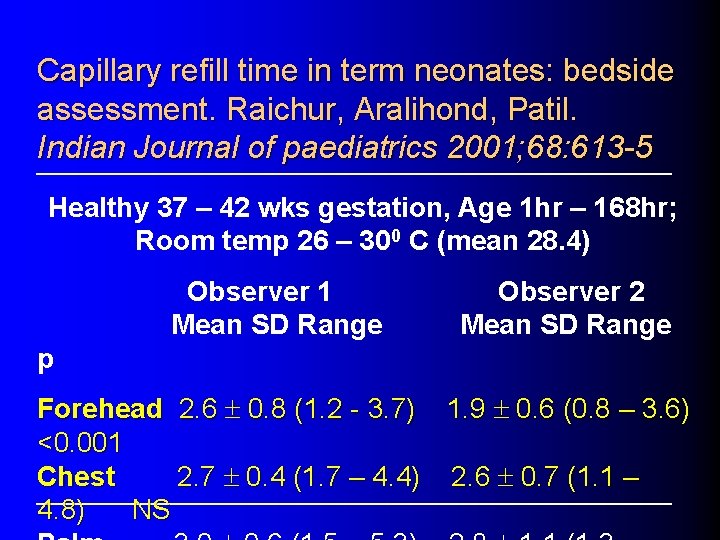
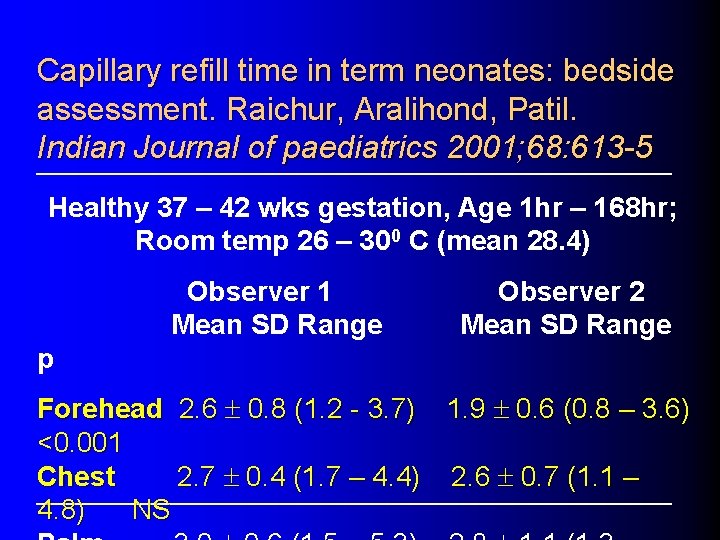
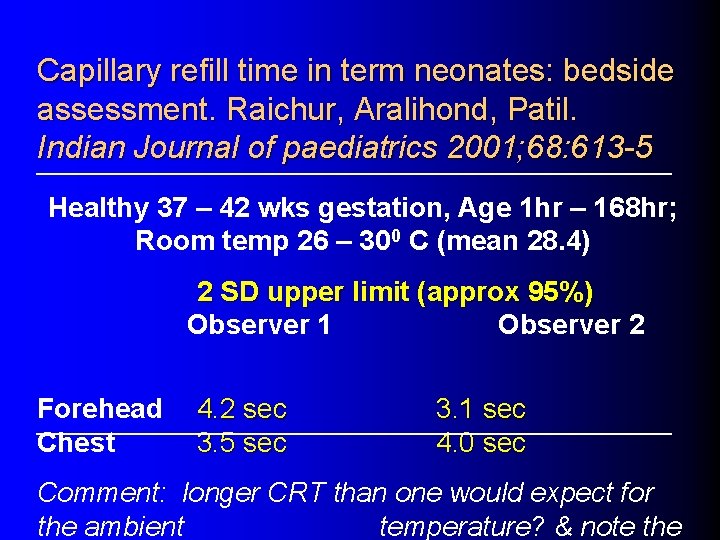
Capillary refill time in term neonates: bedside assessment. Raichur, Aralihond, Patil. Indian Journal of paediatrics 2001; 68: 613 -5 Healthy 37 – 42 wks gestation, Age 1 hr – 168 hr; Room temp 26 – 300 C (mean 28. 4) Observer 1 Mean SD Range Observer 2 Mean SD Range p Forehead 2. 6 ± 0. 8 (1. 2 - 3. 7) 1. 9 ± 0. 6 (0. 8 – 3. 6) <0. 001 Chest 2. 7 ± 0. 4 (1. 7 – 4. 4) 2. 6 ± 0. 7 (1. 1 – 4. 8) NS
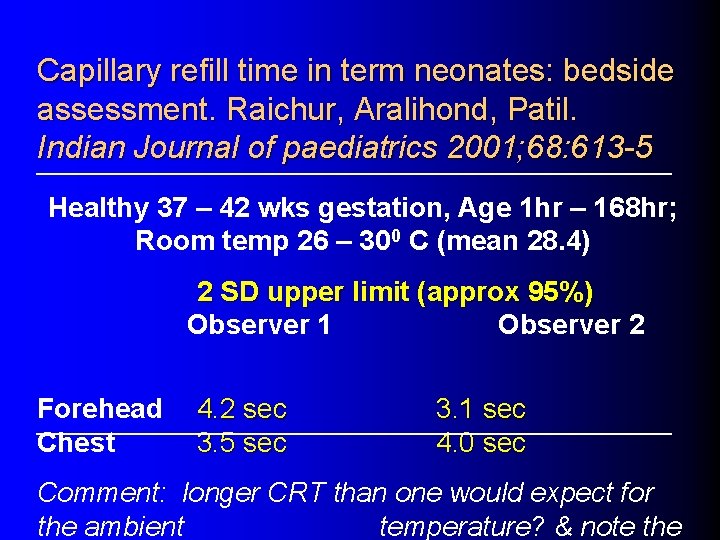
Capillary refill time in term neonates: bedside assessment. Raichur, Aralihond, Patil. Indian Journal of paediatrics 2001; 68: 613 -5 Healthy 37 – 42 wks gestation, Age 1 hr – 168 hr; Room temp 26 – 300 C (mean 28. 4) 2 SD upper limit (approx 95%) Observer 1 Observer 2 Forehead Chest 4. 2 sec 3. 5 sec 3. 1 sec 4. 0 sec Comment: longer CRT than one would expect for the ambient temperature? & note the
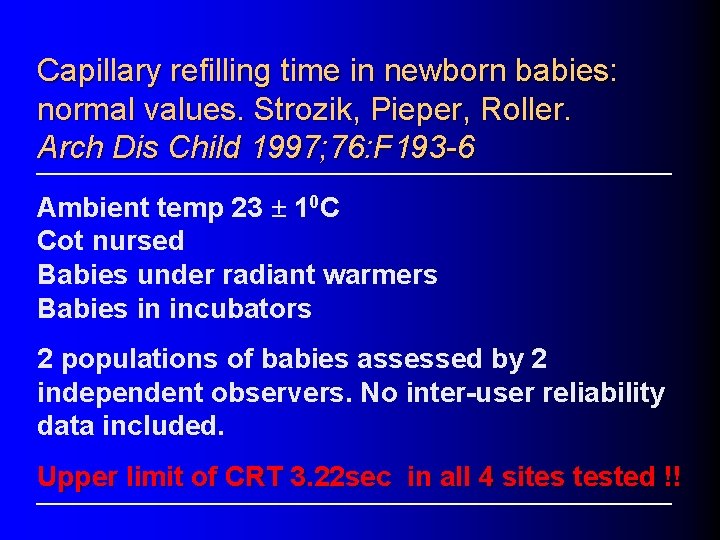
Capillary refilling time in newborn babies: normal values. Strozik, Pieper, Roller. Arch Dis Child 1997; 76: F 193 -6 Ambient temp 23 ± 10 C Cot nursed Babies under radiant warmers Babies in incubators 2 populations of babies assessed by 2 independent observers. No inter-user reliability data included. Upper limit of CRT 3. 22 sec in all 4 sites tested !!
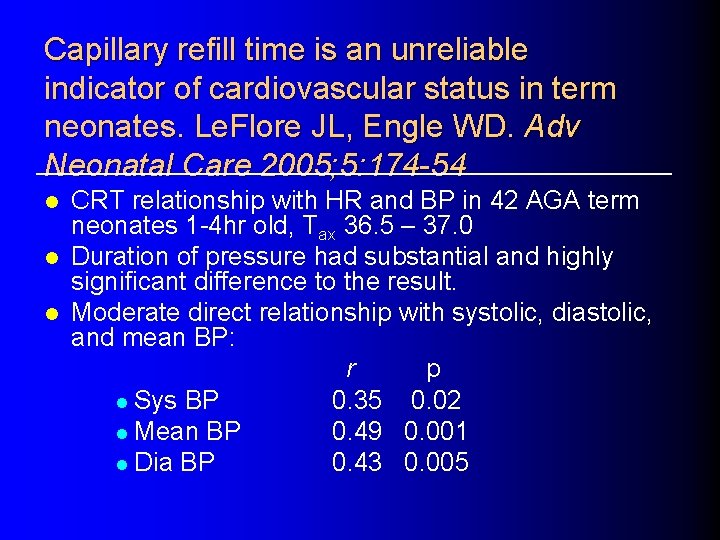
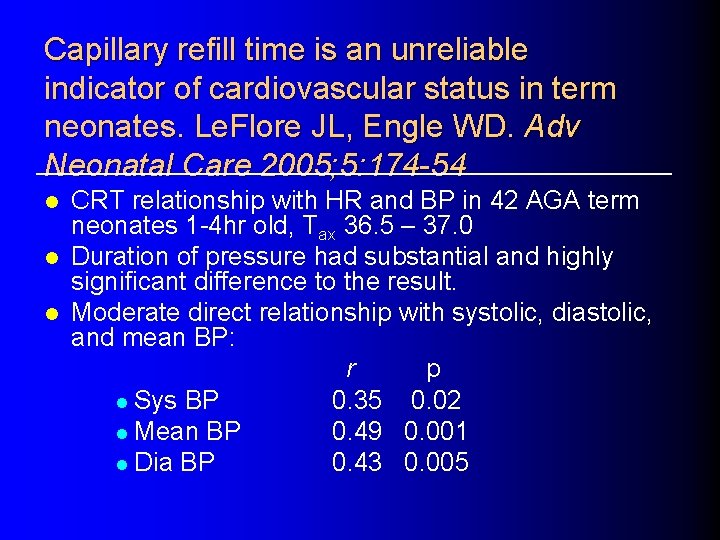
Capillary refill time is an unreliable indicator of cardiovascular status in term neonates. Le. Flore JL, Engle WD. Adv Neonatal Care 2005; 5: 174 -54 l l l CRT relationship with HR and BP in 42 AGA term neonates 1 -4 hr old, Tax 36. 5 – 37. 0 Duration of pressure had substantial and highly significant difference to the result. Moderate direct relationship with systolic, diastolic, and mean BP: r p l Sys BP 0. 35 0. 02 l Mean BP 0. 49 0. 001 l Dia BP 0. 43 0. 005
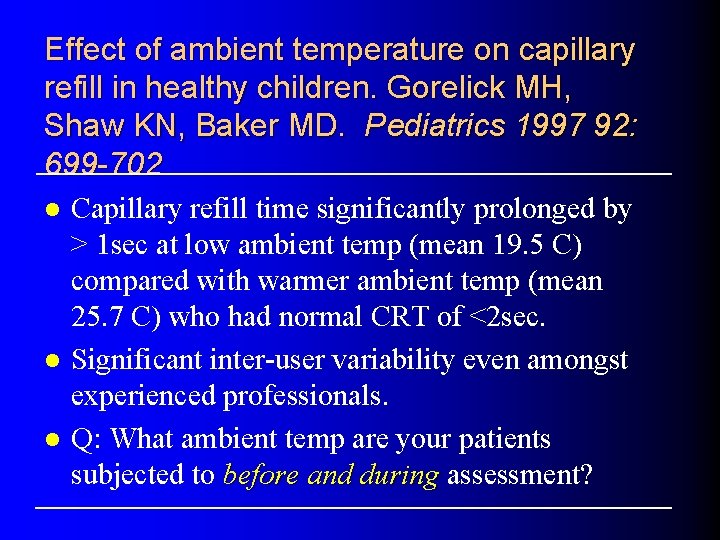
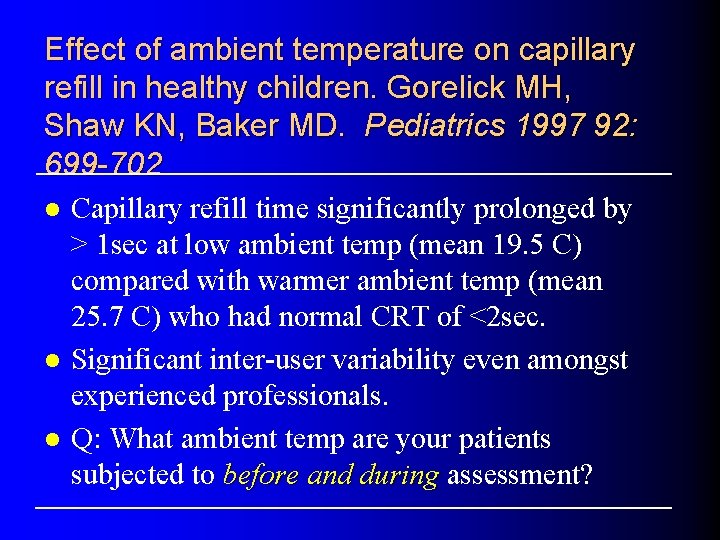
Effect of ambient temperature on capillary refill in healthy children. Gorelick MH, Shaw KN, Baker MD. Pediatrics 1997 92: 699 -702 l l l Capillary refill time significantly prolonged by > 1 sec at low ambient temp (mean 19. 5 C) compared with warmer ambient temp (mean 25. 7 C) who had normal CRT of <2 sec. Significant inter-user variability even amongst experienced professionals. Q: What ambient temp are your patients subjected to before and during assessment?
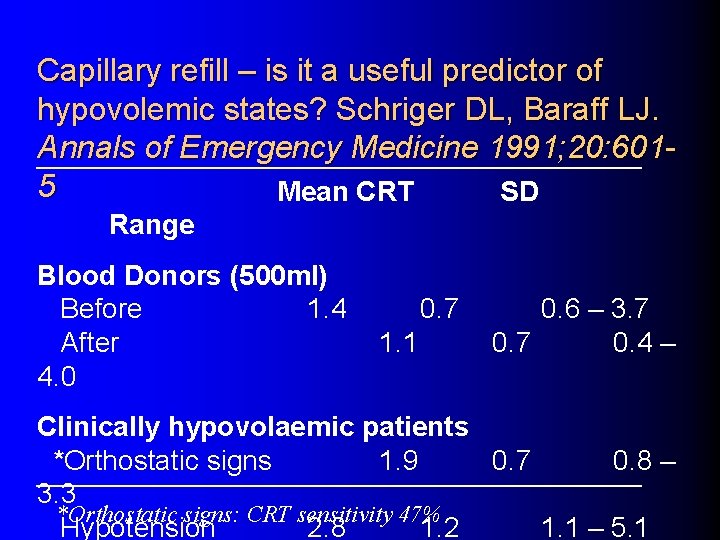
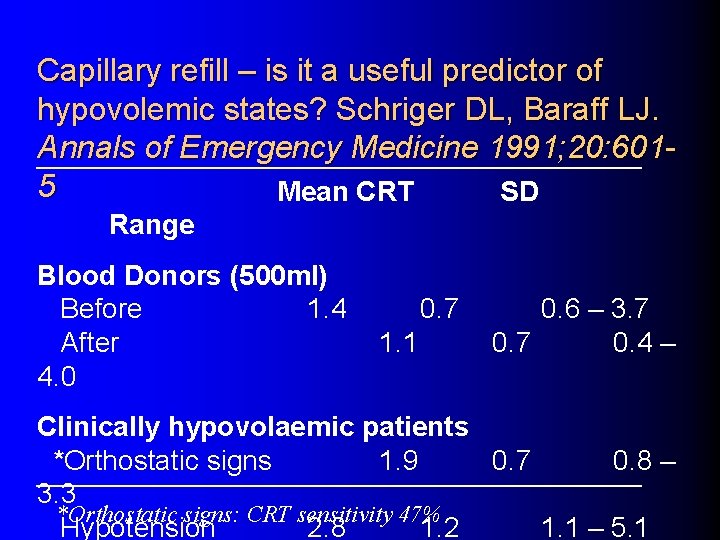
Capillary refill – is it a useful predictor of hypovolemic states? Schriger DL, Baraff LJ. Annals of Emergency Medicine 1991; 20: 6015 Mean CRT SD Range Blood Donors (500 ml) Before 1. 4 After 4. 0 0. 7 1. 1 0. 6 – 3. 7 0. 4 – Clinically hypovolaemic patients *Orthostatic signs 1. 9 0. 7 0. 8 – 3. 3 *Orthostatic signs: CRT sensitivity 47% Hypotension 2. 8 1. 2 1. 1 – 5. 1
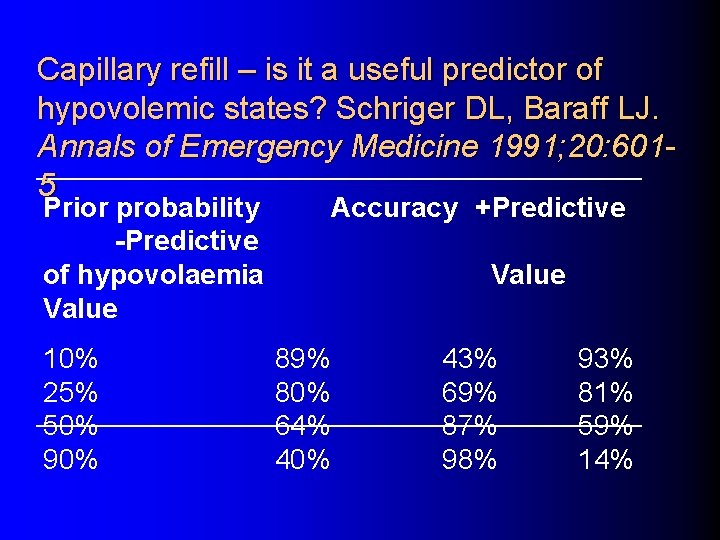
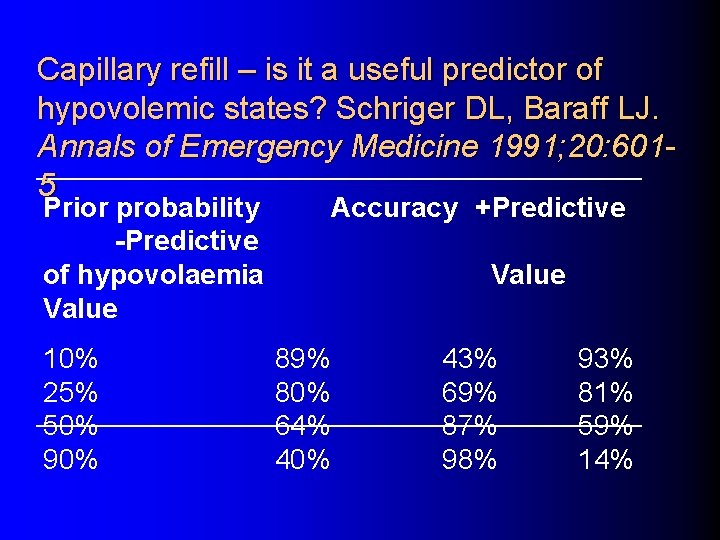
Capillary refill – is it a useful predictor of hypovolemic states? Schriger DL, Baraff LJ. Annals of Emergency Medicine 1991; 20: 6015 Prior probability -Predictive of hypovolaemia Value 10% 25% 50% 90% Accuracy +Predictive Value 89% 80% 64% 40% 43% 69% 87% 98% 93% 81% 59% 14%
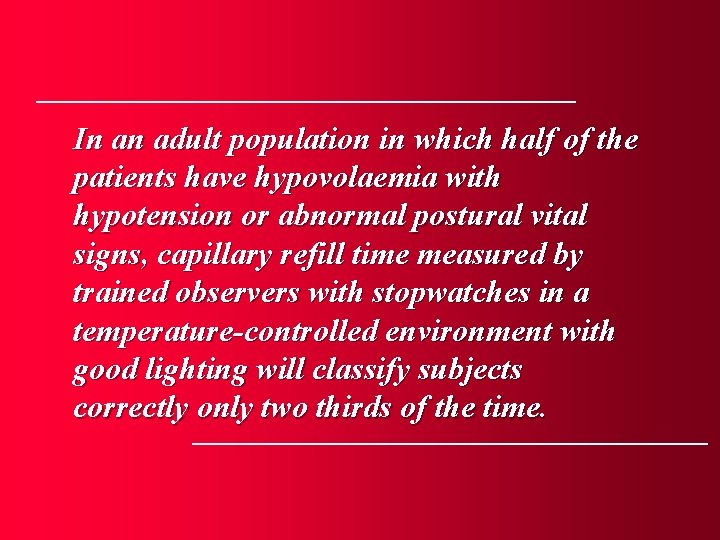
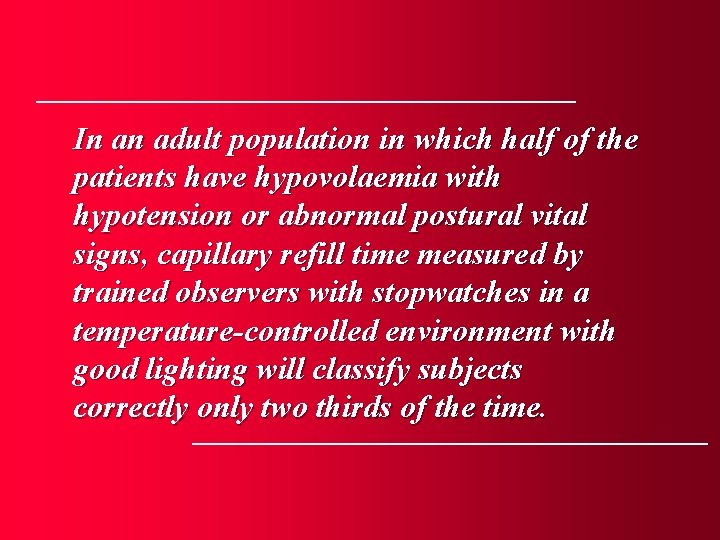
In an adult population in which half of the patients have hypovolaemia with hypotension or abnormal postural vital signs, capillary refill time measured by trained observers with stopwatches in a temperature-controlled environment with good lighting will classify subjects correctly only two thirds of the time.
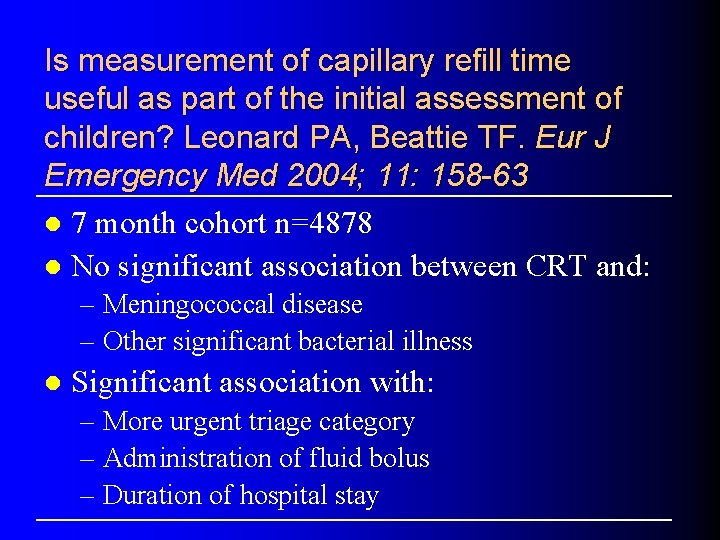
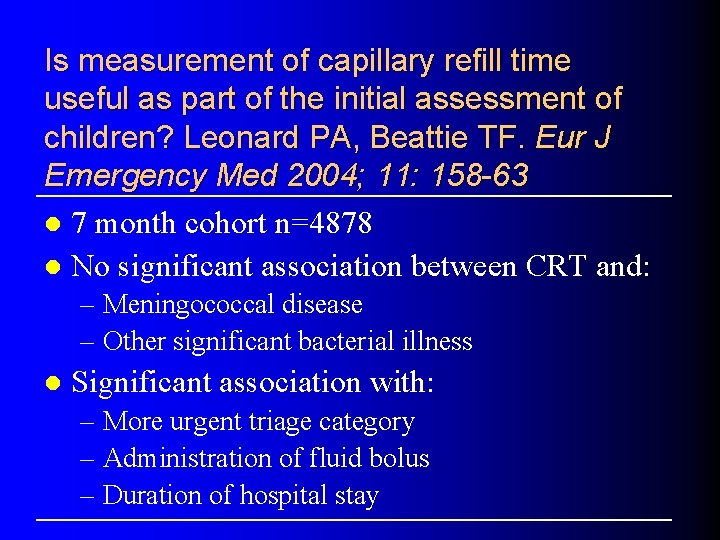
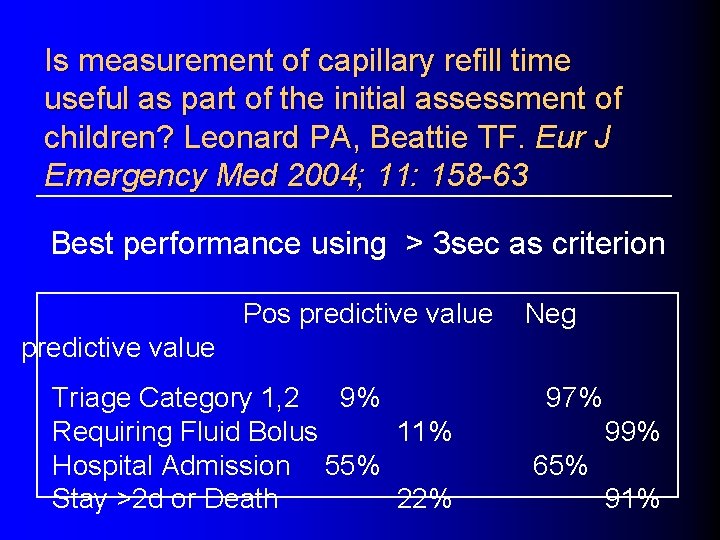
Is measurement of capillary refill time useful as part of the initial assessment of children? Leonard PA, Beattie TF. Eur J Emergency Med 2004; 11: 158 -63 l 7 month cohort n=4878 l No significant association between CRT and: – Meningococcal disease – Other significant bacterial illness l Significant association with: – More urgent triage category – Administration of fluid bolus – Duration of hospital stay
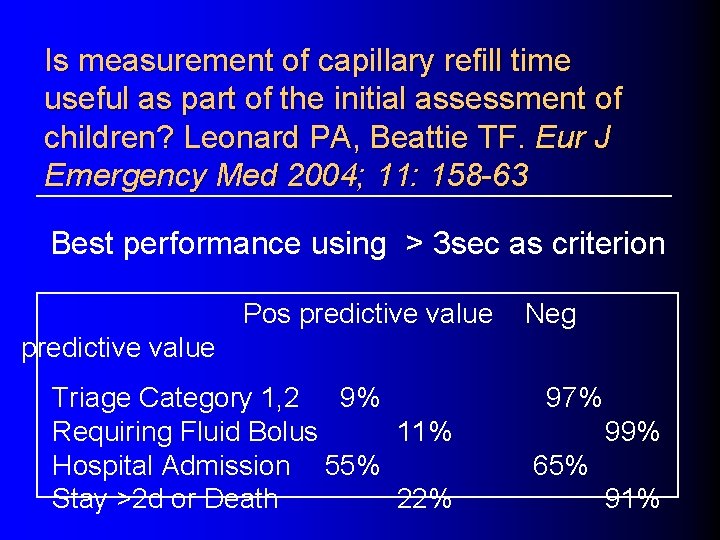
Is measurement of capillary refill time useful as part of the initial assessment of children? Leonard PA, Beattie TF. Eur J Emergency Med 2004; 11: 158 -63 Best performance using > 3 sec as criterion Pos predictive value Neg predictive value Triage Category 1, 2 9% Requiring Fluid Bolus 11% Hospital Admission 55% Stay >2 d or Death 22% 97% 99% 65% 91%
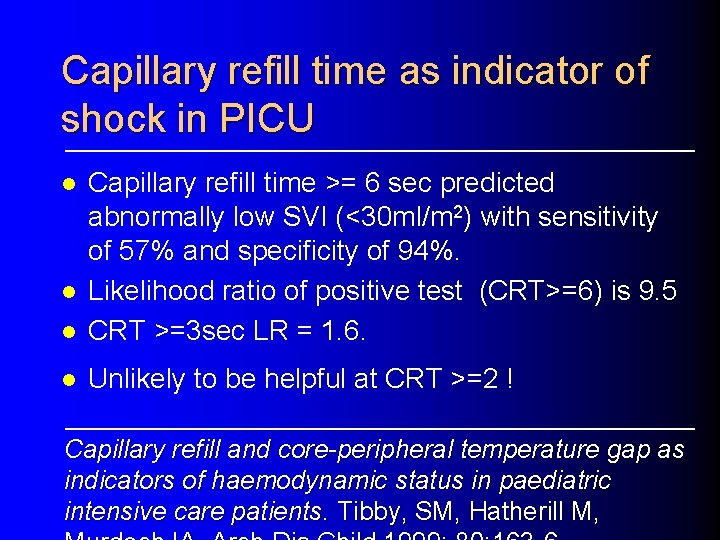
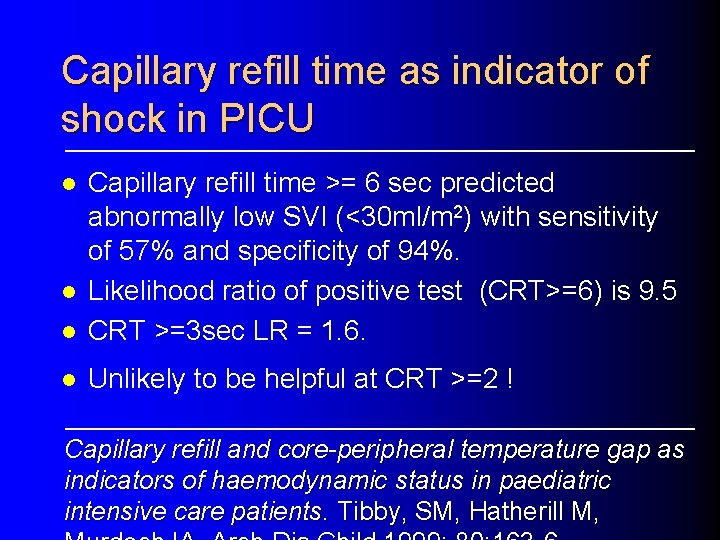
Capillary refill time as indicator of shock in PICU l Capillary refill time >= 6 sec predicted abnormally low SVI (<30 ml/m 2) with sensitivity of 57% and specificity of 94%. Likelihood ratio of positive test (CRT>=6) is 9. 5 CRT >=3 sec LR = 1. 6. l Unlikely to be helpful at CRT >=2 ! l l Capillary refill and core-peripheral temperature gap as indicators of haemodynamic status in paediatric intensive care patients. Tibby, SM, Hatherill M,
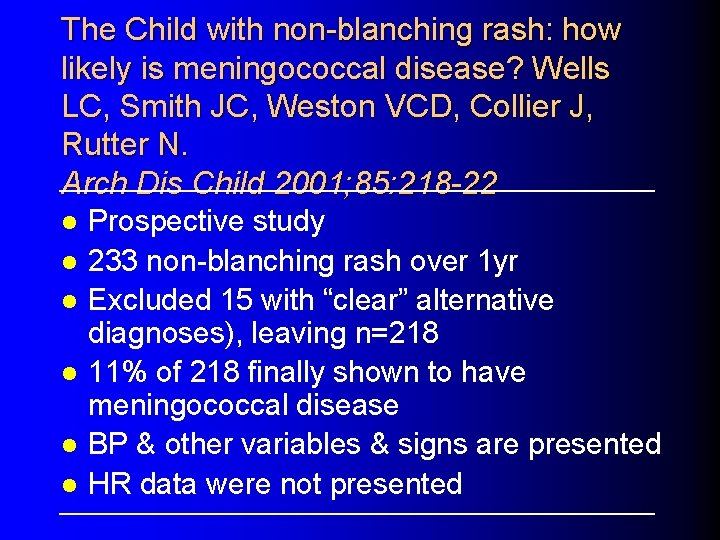
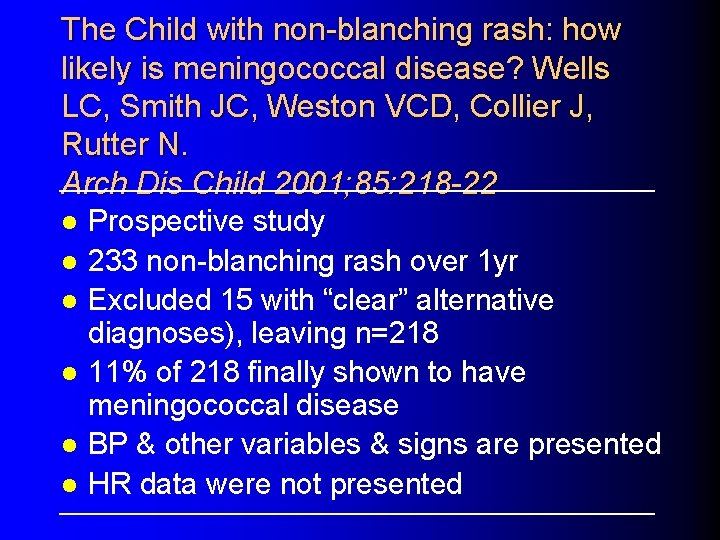
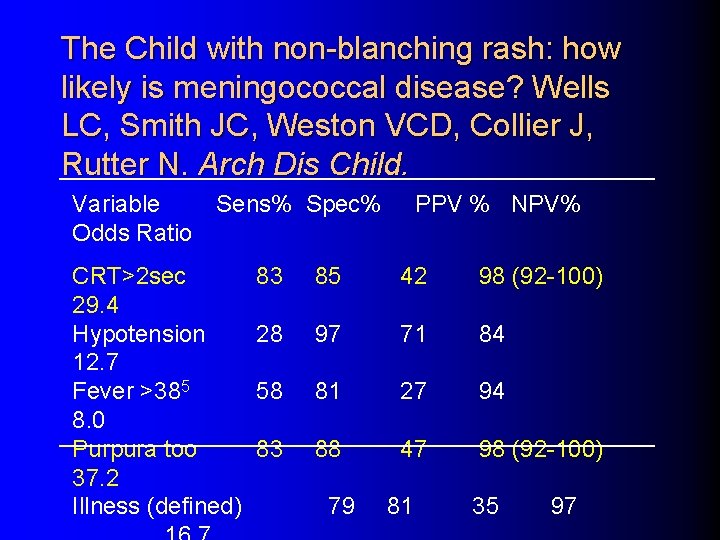
The Child with non-blanching rash: how likely is meningococcal disease? Wells LC, Smith JC, Weston VCD, Collier J, Rutter N. Arch Dis Child 2001; 85: 218 -22 l l l Prospective study 233 non-blanching rash over 1 yr Excluded 15 with “clear” alternative diagnoses), leaving n=218 11% of 218 finally shown to have meningococcal disease BP & other variables & signs are presented HR data were not presented
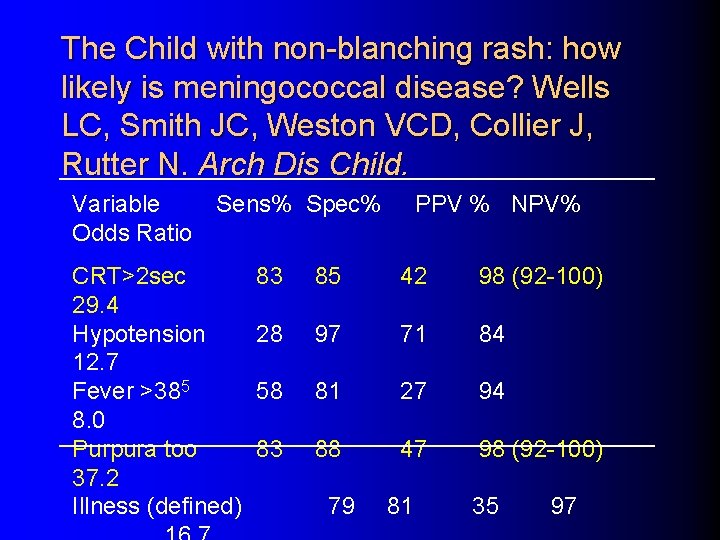
The Child with non-blanching rash: how likely is meningococcal disease? Wells LC, Smith JC, Weston VCD, Collier J, Rutter N. Arch Dis Child. Variable Odds Ratio Sens% Spec% CRT>2 sec 29. 4 Hypotension 12. 7 Fever >385 8. 0 Purpura too 37. 2 Illness (defined) PPV % NPV% 83 85 42 98 (92 -100) 28 97 71 84 58 81 27 94 83 88 47 98 (92 -100) 79 81 35 97
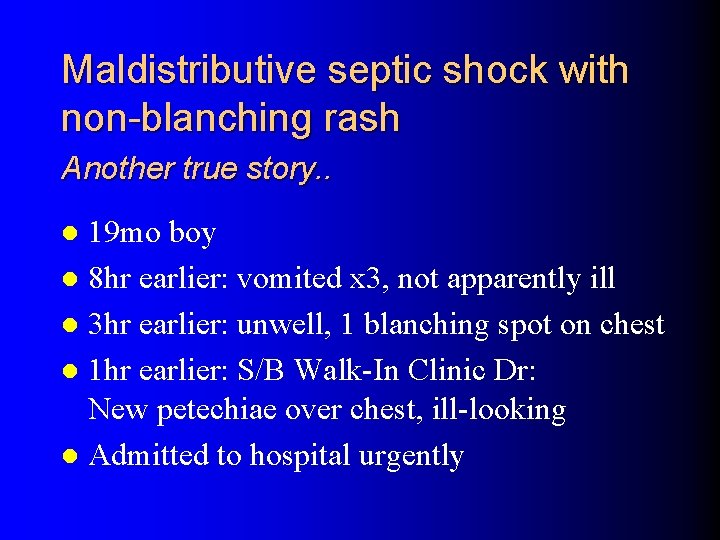
Maldistributive septic shock with non-blanching rash Another true story. . 19 mo boy l 8 hr earlier: vomited x 3, not apparently ill l 3 hr earlier: unwell, 1 blanching spot on chest l 1 hr earlier: S/B Walk-In Clinic Dr: New petechiae over chest, ill-looking l Admitted to hospital urgently l
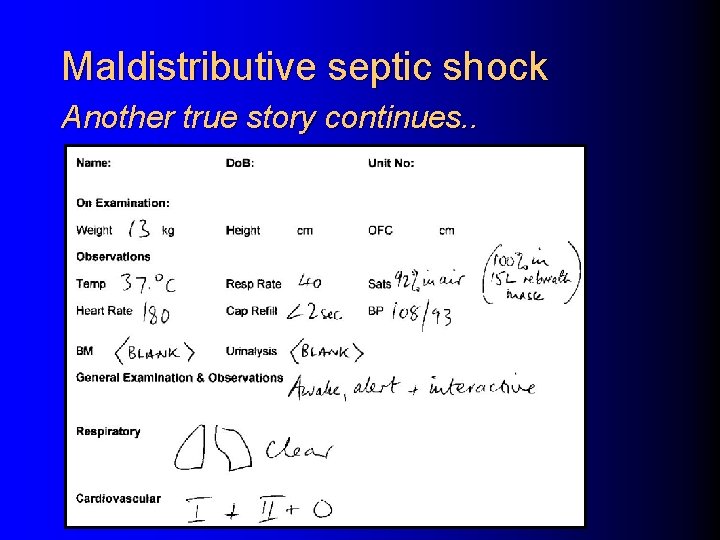
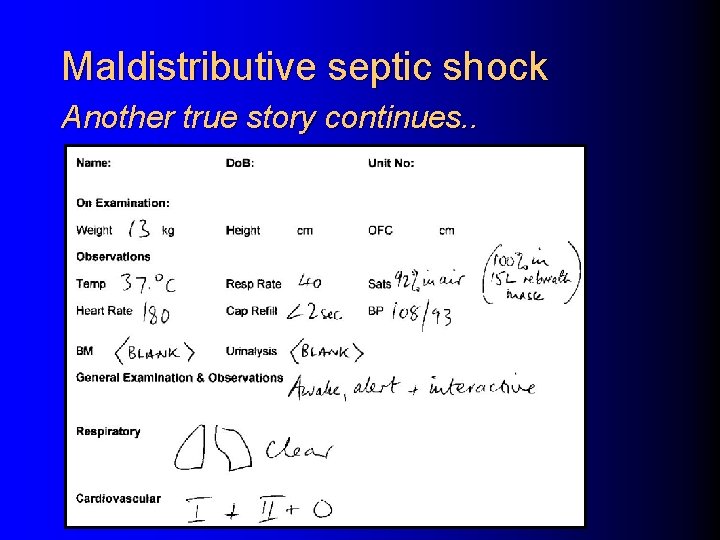
Maldistributive septic shock Another true story continues. .
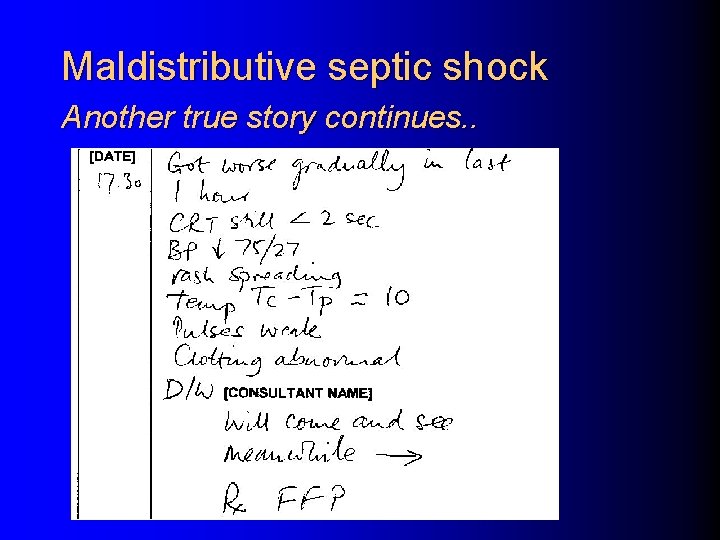
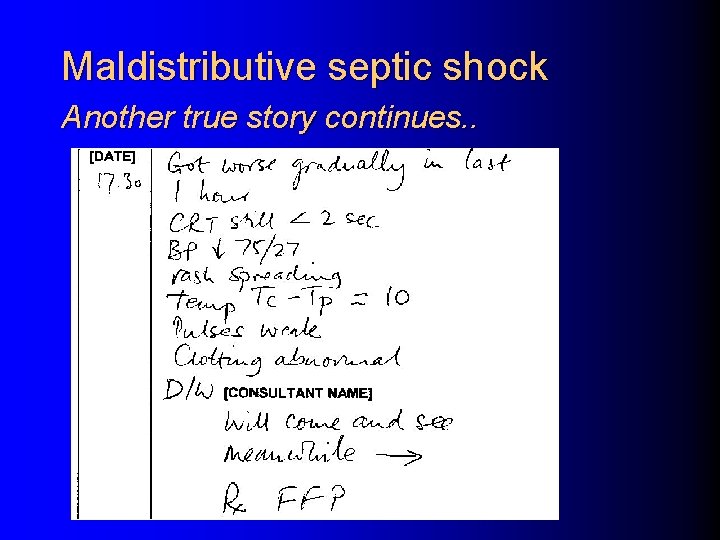
Maldistributive septic shock Another true story continues. .

Maldistributive septic shock Another true story continues. .
Invasive Meningococcal Disease Meningitis without shock l l l Rising ICP and aggressive fluid therapy: a deadly combination. Unconscious, petechiae, minimal- or easily- corrected haemodynamic disturbance: THINK BRAIN Early intubation to protect airway and control ventilation Use cerebral protective drugs at intubation Ensure good perfusion, but don’t overdo volume boluses. Think mannitol 0. 25 – 0. 5 g/kg
“Poor capillary refill and differential pulse volumes are neither sensitive nor specific indicators of shock in infants and children, but are useful clinical signs when used in conjunction with the other signs described. They should not be used as the only indicators of shock, nor as quantitative measures of the response to treatment. ” Advanced Paediatric Life Support, 3 rd Ed. 2001; p 16 Advanced Paediatric Life Support, 4 th Ed.
“Poor capillary refill and differential pulse volumes are neither sensitive nor specific indicators of shock in infants and children, but are useful clinical signs when used in conjunction with the other signs described. They should not be used as the only indicators of shock, nor as quantitative measures of the response to treatment. ” Advanced Paediatric Life Support, 3 rd Ed. 2001; p 16 Advanced Paediatric Life Support, 4 th Ed.
“Poor capillary refill and differential pulse volumes are neither sensitive nor specific indicators of shock in infants and children, but are useful clinical signs when used in conjunction with the other signs described. They should not be used as the only indicators of shock, nor as quantitative measures of the response to treatment. ” Advanced Paediatric Life Support, 3 rd Ed. 2001; p 16 Advanced Paediatric Life Support, 4 th Ed.
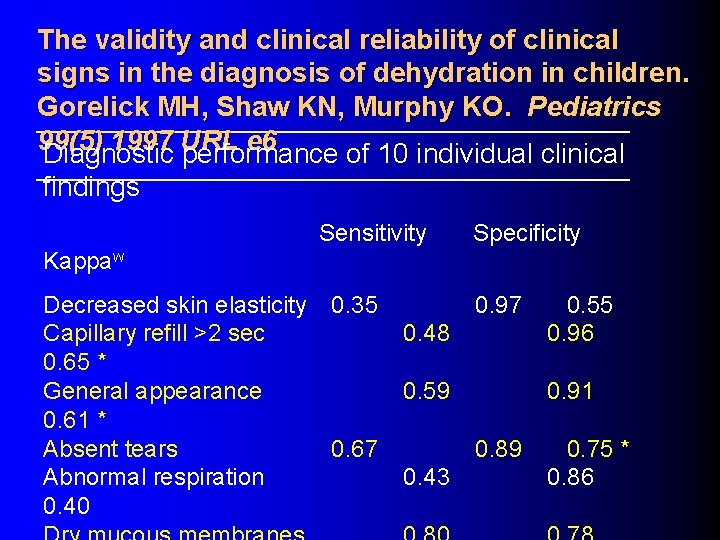
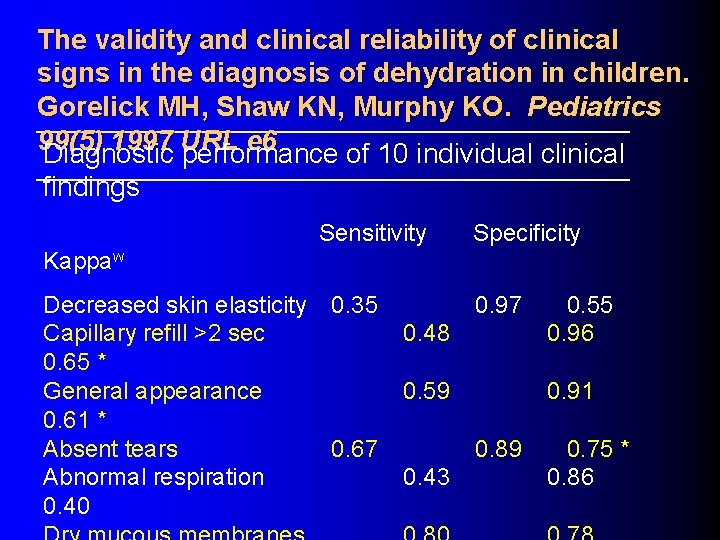
The validity and clinical reliability of clinical signs in the diagnosis of dehydration in children. Gorelick MH, Shaw KN, Murphy KO. Pediatrics 99(5) 1997 URL e 6 Diagnostic performance of 10 individual clinical findings Sensitivity Specificity Kappaw Decreased skin elasticity Capillary refill >2 sec 0. 65 * General appearance 0. 61 * Absent tears Abnormal respiration 0. 40 0. 35 0. 97 0. 48 0. 55 0. 96 0. 59 0. 91 0. 67 0. 89 0. 43 0. 75 * 0. 86
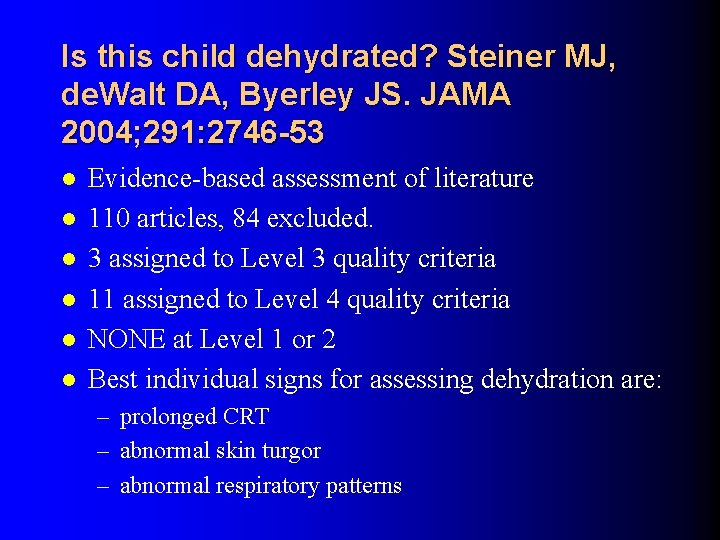
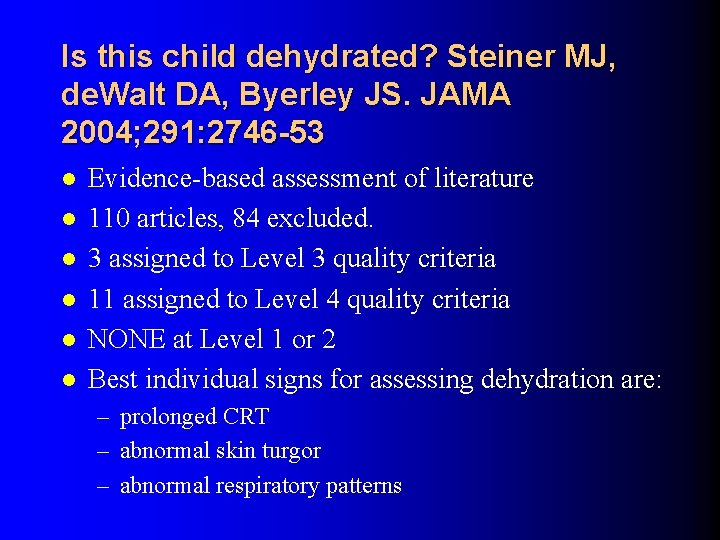
Is this child dehydrated? Steiner MJ, de. Walt DA, Byerley JS. JAMA 2004; 291: 2746 -53 l l l Evidence-based assessment of literature 110 articles, 84 excluded. 3 assigned to Level 3 quality criteria 11 assigned to Level 4 quality criteria NONE at Level 1 or 2 Best individual signs for assessing dehydration are: – prolonged CRT – abnormal skin turgor – abnormal respiratory patterns
APLS Message Dehydration APLS uses CRT as an adjunct for determining the presence of shock. l APLS makes no mention of CRT in the workshop on fluids in connection with dehydration. l
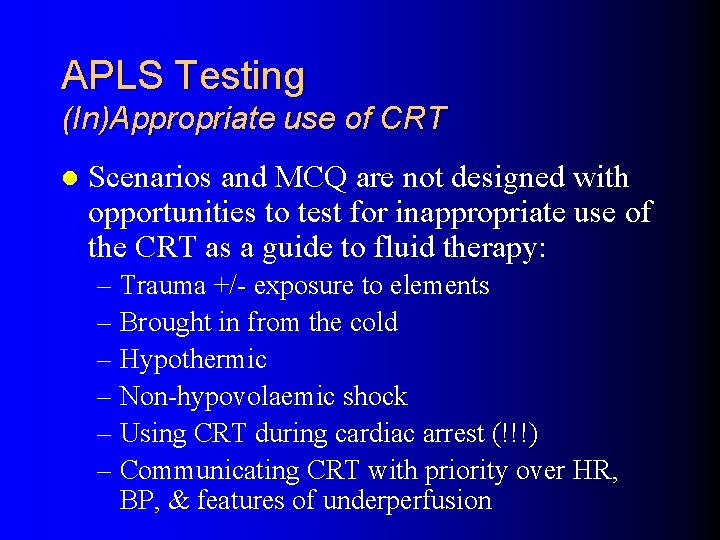
APLS Testing (In)Appropriate use of CRT l Scenarios and MCQ are not designed with opportunities to test for inappropriate use of the CRT as a guide to fluid therapy: – Trauma +/- exposure to elements – Brought in from the cold – Hypothermic – Non-hypovolaemic shock – Using CRT during cardiac arrest (!!!) – Communicating CRT with priority over HR, BP, & features of underperfusion
CRT: Summary A rapid clinical assessment of…something l “Normal” value not especially age-related l But: is the clinical assessment tool reliable? l Consequences of giving too much fluid? l – Special problems l Non-hypovolaemic shock l Meningitis l ARDS l Infancy
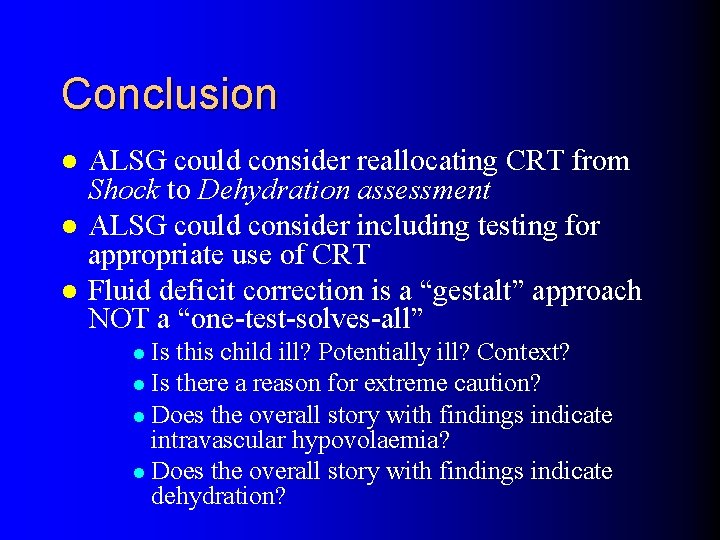
Conclusion l l l ALSG could consider reallocating CRT from Shock to Dehydration assessment ALSG could consider including testing for appropriate use of CRT Fluid deficit correction is a “gestalt” approach NOT a “one-test-solves-all” l Is this child ill? Potentially ill? Context? l Is there a reason for extreme caution? l Does the overall story with findings indicate intravascular hypovolaemia? l Does the overall story with findings indicate dehydration?
 Autism curriculum encyclopedia
Autism curriculum encyclopedia Rethink your drink posters
Rethink your drink posters Rethink your drink science project
Rethink your drink science project Rethink obesity global
Rethink obesity global Rethink your drink project
Rethink your drink project Rethink rubbish at home
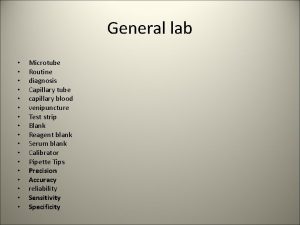
Rethink rubbish at home What is the normal capillary refill time
What is the normal capillary refill time Capillary method of clotting time
Capillary method of clotting time Pulse sites
Pulse sites Clotting time capillary tube method procedure
Clotting time capillary tube method procedure Define hospital
Define hospital Andrew kim mun
Andrew kim mun Start time, end time and elapsed time
Start time, end time and elapsed time University hospital of pisa
University hospital of pisa Brendan rauw
Brendan rauw Benha university hospital
Benha university hospital Kyorin university ranking
Kyorin university ranking University hospital tuebingen
University hospital tuebingen Pisa university hospital
Pisa university hospital Patras university hospital
Patras university hospital Pisa university hospital
Pisa university hospital Hospital university of pennsylvania
Hospital university of pennsylvania Portsmouth university hospital trust values
Portsmouth university hospital trust values Kyung hee university hospital at gangdong
Kyung hee university hospital at gangdong Kaohsiung medical university hospital
Kaohsiung medical university hospital University of iowa hospital and clinics departments
University of iowa hospital and clinics departments King saud university hospital nurse salary
King saud university hospital nurse salary Capillary viscometer
Capillary viscometer Viscosity of liquids
Viscosity of liquids Diagram of juxtaglomerular apparatus
Diagram of juxtaglomerular apparatus Advantages of soldering and brazing
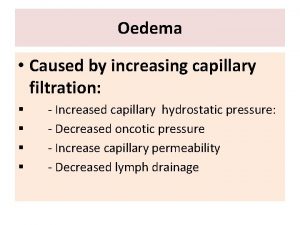
Advantages of soldering and brazing Capillary fluid shift mechanism blood pressure
Capillary fluid shift mechanism blood pressure Hydrostatic pressure in interstitial fluid
Hydrostatic pressure in interstitial fluid Microscopic view of liquid
Microscopic view of liquid Afferent and efferent arterioles
Afferent and efferent arterioles External urethral orifice
External urethral orifice Net filtration pressure definition
Net filtration pressure definition Artery vein capillary structure
Artery vein capillary structure Capillary action intermolecular forces
Capillary action intermolecular forces Capillary viscometer
Capillary viscometer Capillary number
Capillary number Application of capillary
Application of capillary Chapter 20:3 puncturing the skin to obtain capillary blood
Chapter 20:3 puncturing the skin to obtain capillary blood Pulmonary capillary bed
Pulmonary capillary bed Chapter 11 the cardiovascular system figure 11-10 answers
Chapter 11 the cardiovascular system figure 11-10 answers Capillary number
Capillary number Arterial vs venous end of capillary
Arterial vs venous end of capillary Chapter 10 capillary puncture equipment and procedures
Chapter 10 capillary puncture equipment and procedures Capillaries exchange
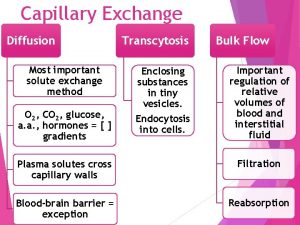
Capillaries exchange Most important method of capillary exchange
Most important method of capillary exchange Arterial vs venous end of capillary
Arterial vs venous end of capillary Whats capillary action
Whats capillary action Hydrosphere facts
Hydrosphere facts Capillary attraction in plumbing
Capillary attraction in plumbing Capillary electrophoresis disadvantages
Capillary electrophoresis disadvantages Whats capillary action
Whats capillary action