General Approach of Haemostasis Lecture 3 Coagulation Time
- Slides: 26
General Approach of Haemostasis Lecture 3: Coagulation Time of whole blood
Coagulation Time ( Clotting Time) CT. q q q Clotting Time is the time required for blood to form a clot in vitro. The basis for the test is that whole blood will form a solid clot when exposed to a foreign surface such as a glass tube. It is a rough measure of all intrinsic clotting factors in the absence of tissue factors. Variations are wide and the test sensitivity is limited. As the test is the least effective test in the diagnosis of actual haemostasis failure, it has been replaced by PTT. Clotting time was used as a screening test to measure all stages in the intrinsic coagulation system and to monitor heparin therapy.
q q q It is however, a time-consuming test, has poor reproducibility, is sensitive only extreme factor deficiencies. It is therefore, of limited use in today’s laboratory. It is a complex process involving over 30 substances Conditions accompanied by increased Clotting Time: q q q Factors V, VIII, IX, XII Deficiencies. Hemorrhagic disease of Newborn Vitamin K deficiency. Heparin Therapy. Presence of Circulating antibodies (inhibitors) Afibinogenemia and Pneumonia.
Methods: q Capillary Method. q Slide Method. q Tube Method.
Tube Method (Lee-White method) q Reagent & equipment q Water bath, 37 O C. q Glass test tube (10 x 75 mm) q Stopwatch. q Plastic syringe and 20 -gauge needle. q Specimen q Fresh whole blood , 4 ml.
Procedure 1. Label 3 glass test tube with patient name and number them, 1, 2, and 3. 2. Perform a clean, Untraumatic venipucture using a 20 -gauge needle and drawn 4 m. L of blood. 3. Remove the needle from the syringe, and fill each of the three tubes with 1 ml blood. v The last 1 ml of blood may be discarded. v Start the stopwatch as soon as the blood enters the syringe. 4. Place three test tubes in a 37°C water bath. 5. At exactly 3 min. , Remove the first tube form water bath and tilt gently to a 45° angle to see whether the blood has clotted. 6. If Blood not clotted return it to the water bath and examine it at 30 second intervals.
5. 6. 7. After the blood in the first tube has clotted, examine the second tube immediately. Then examine the 3 rd one. Record the time it took the blood in the 3 rd test tube to clot. Normal Range: 5 – 12 Minutes***
Discussion 1. 2. 3. 4. Poor venipucture technique, causing hemolysis or tissue thromboplastin to mix with the blood, shortens the clotting time. Bubbles entering the syringe when the blood sample is being obtained increase the rate of coagulation. Always tilt the tube in the same direction and at the same angle so that the blood is moving in the same pathway up the side of the tube each time. Excessive agitation of blood (occur during the transfer of the blood from the syringe to the test tube). The blood should be allowed to flow gently down the inside of the test tube and not forcefully squirted into the test tube.
6. At the completion of the clotting time, one tube should remain in the 37°C water bath to be checked for clot retraction. Also, this same tube may be allowed to remain in the water bath overnight and checked the next day for clot lysis. Dirty Test Tubes will affect the result. q Coagulation will be retarded by the following: 5. q q q Temperature Below 35 O C. Temperature above 45 O C. Diameter of the test tube (the smaller the diameter, the more rapid the clot formation is).
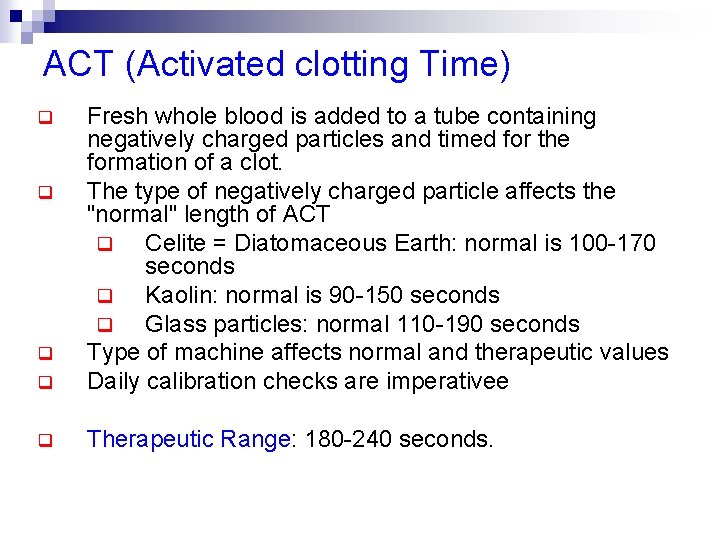
ACT (Activated clotting Time) q Fresh whole blood is added to a tube containing negatively charged particles and timed for the formation of a clot. The type of negatively charged particle affects the "normal" length of ACT q Celite = Diatomaceous Earth: normal is 100 -170 seconds q Kaolin: normal is 90 -150 seconds q Glass particles: normal 110 -190 seconds Type of machine affects normal and therapeutic values Daily calibration checks are imperativee q Therapeutic Range: 180 -240 seconds. q q q
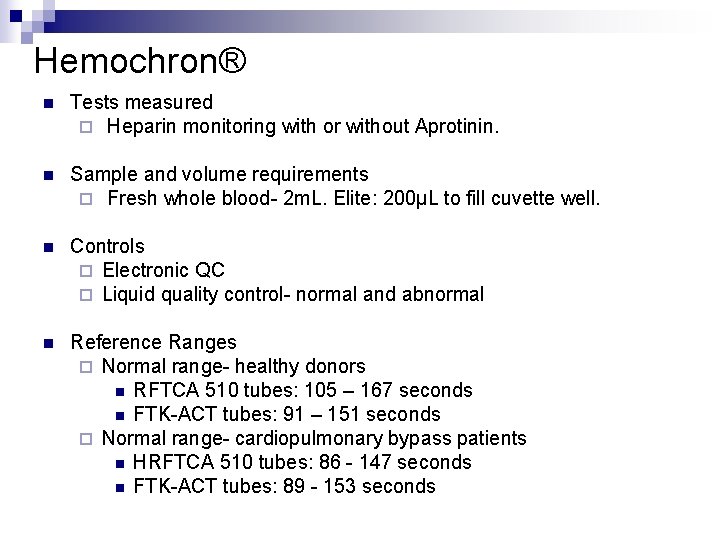
Hemochron® n Tests measured ¨ Heparin monitoring with or without Aprotinin. n Sample and volume requirements ¨ Fresh whole blood- 2 m. L. Elite: 200µL to fill cuvette well. n Controls ¨ Electronic QC ¨ Liquid quality control- normal and abnormal n Reference Ranges ¨ Normal range- healthy donors n RFTCA 510 tubes: 105 – 167 seconds n FTK-ACT tubes: 91 – 151 seconds ¨ Normal range- cardiopulmonary bypass patients n HRFTCA 510 tubes: 86 - 147 seconds n FTK-ACT tubes: 89 - 153 seconds
Clotting Time - Capillary method Material q q q Sterile disposable pricking needle or lancet. Stop watch Dry glass capillary tube (narrow diameter top 2 mm, minimum 10 cm long. ) Cotton Swab of absorbent cotton. Spirit wetted, cotton swab. 70 % v/v ethyl alcohol
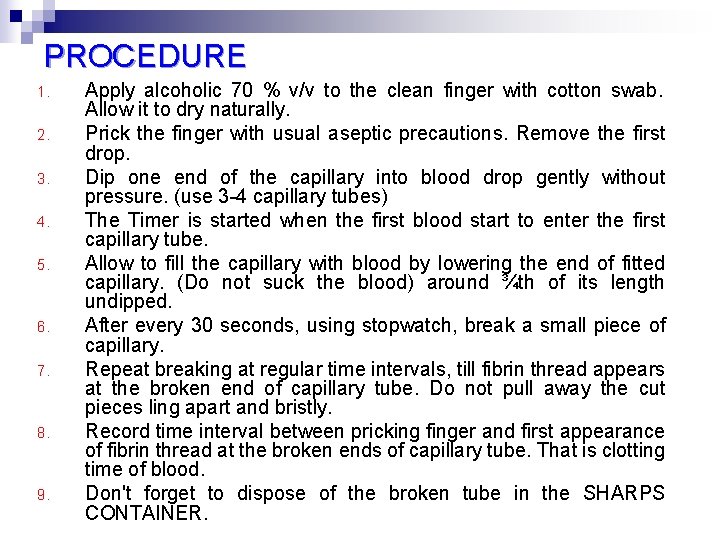
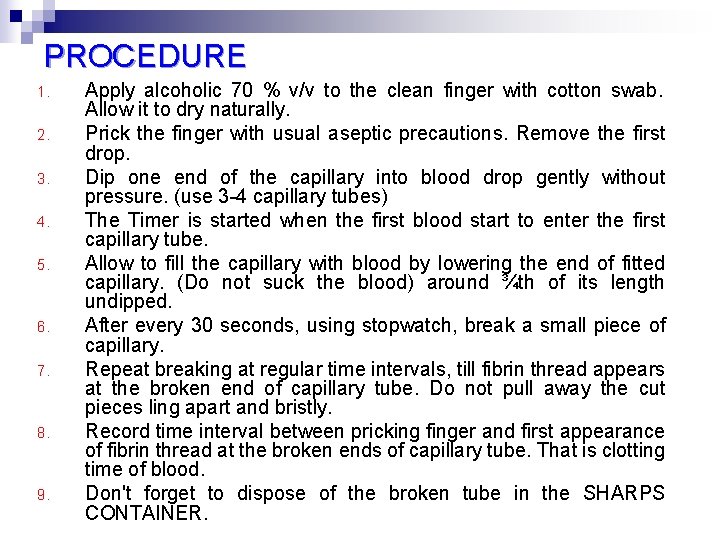
PROCEDURE 1. 2. 3. 4. 5. 6. 7. 8. 9. Apply alcoholic 70 % v/v to the clean finger with cotton swab. Allow it to dry naturally. Prick the finger with usual aseptic precautions. Remove the first drop. Dip one end of the capillary into blood drop gently without pressure. (use 3 -4 capillary tubes) The Timer is started when the first blood start to enter the first capillary tube. Allow to fill the capillary with blood by lowering the end of fitted capillary. (Do not suck the blood) around ¾th of its length undipped. After every 30 seconds, using stopwatch, break a small piece of capillary. Repeat breaking at regular time intervals, till fibrin thread appears at the broken end of capillary tube. Do not pull away the cut pieces ling apart and bristly. Record time interval between pricking finger and first appearance of fibrin thread at the broken ends of capillary tube. That is clotting time of blood. Don't forget to dispose of the broken tube in the SHARPS CONTAINER.
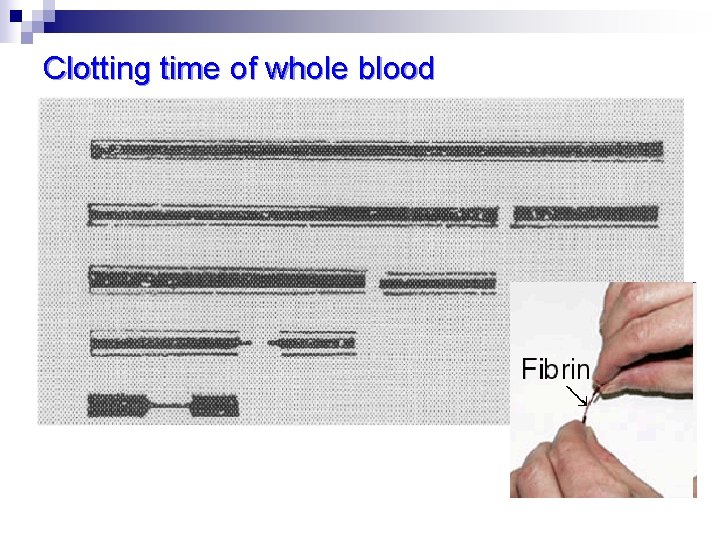
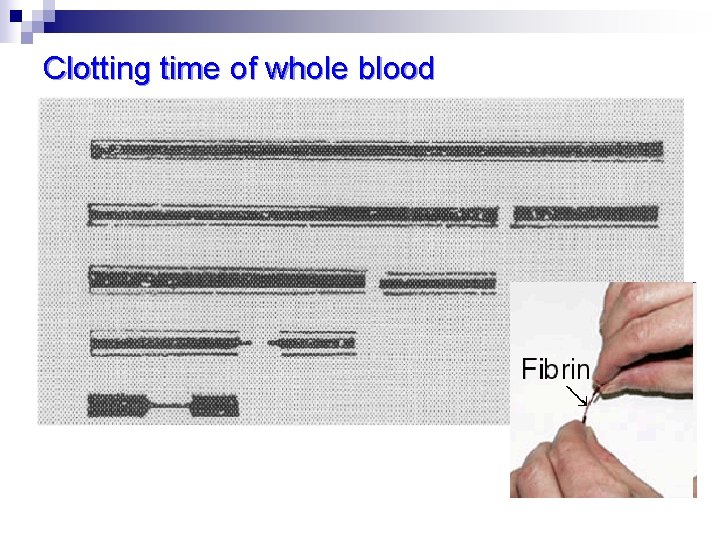
Clotting time of whole blood
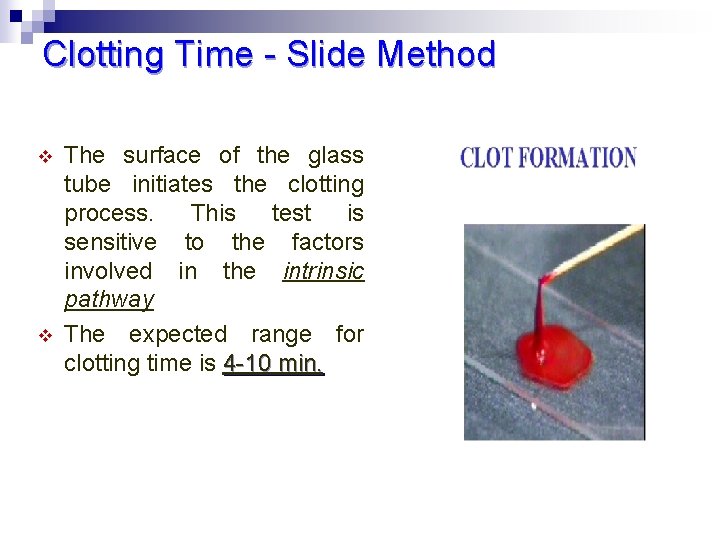
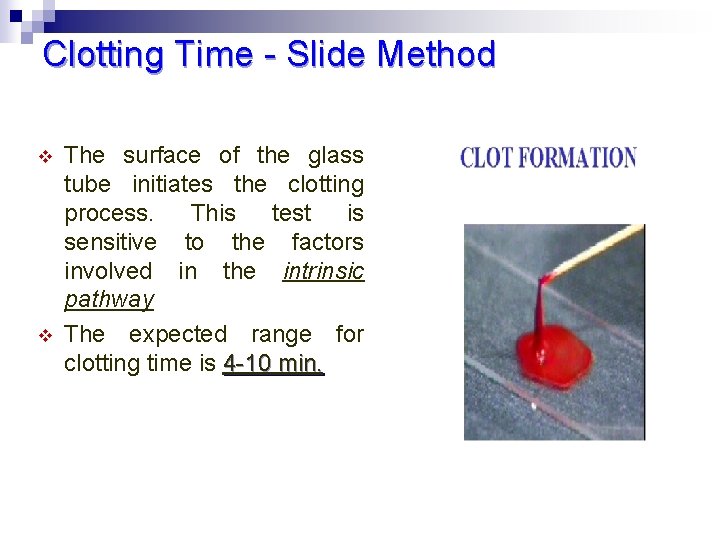
Clotting Time - Slide Method v v The surface of the glass tube initiates the clotting process. This test is sensitive to the factors involved in the intrinsic pathway The expected range for clotting time is 4 -10 min.
Clot retraction (Obsolete test) n n n This test measures the amount of time it takes for a blood clot to pull away from the walls of a test tube (Shrinking). The edges of the blood vessel wall at the point of injury are slowly brought together again to repair the damage. It is used to evaluate and manage blood platelet disorders, including Glanzmann's thrombasthenia So Clot retraction depends primarily on the number and activity of the blood platelets. This test is reliable only when the concentration of fibrinogen within normal limits. Normally a blood clot will begin to retract from the walls of the tube and express serum within one hour.
Glanzmann's thrombasthenia n n n Is an abnormality of the platelets It is an extremely rare coagulopathy in which the platelets lack glycoprotein IIb/IIIa. Reduced glycoprotein IIb/IIIa causes reduced platelet aggregation and clot retraction - no fibrinogen bridging can occur, and bleeding time is significantly prolonged);
Clot retraction test q q This is a measure of platelet function. The test is done in blood to which no anticoagulant has been added and is allowed to clot. Clot retraction is then looked for. Clot retraction becomes abnormal in conditions like q Fibrinogen deficiency (congenital or acquired) q Thrombocytopenia < 1 ooooo q Thrombosthenia q Polycythaemia q Reduced clot formation: Glanzmann thrombasthenia , DIC, hypofibrinogenemia, dysfibrinogenemia (small clot with increased red blood cell “fall-out”)
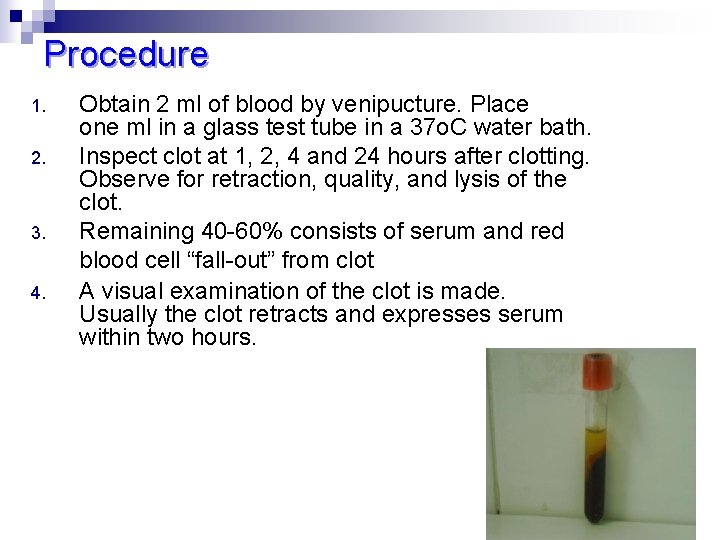
Procedure 1. 2. 3. 4. Obtain 2 ml of blood by venipucture. Place one ml in a glass test tube in a 37 o. C water bath. Inspect clot at 1, 2, 4 and 24 hours after clotting. Observe for retraction, quality, and lysis of the clot. Remaining 40 -60% consists of serum and red blood cell “fall-out” from clot A visual examination of the clot is made. Usually the clot retracts and expresses serum within two hours.
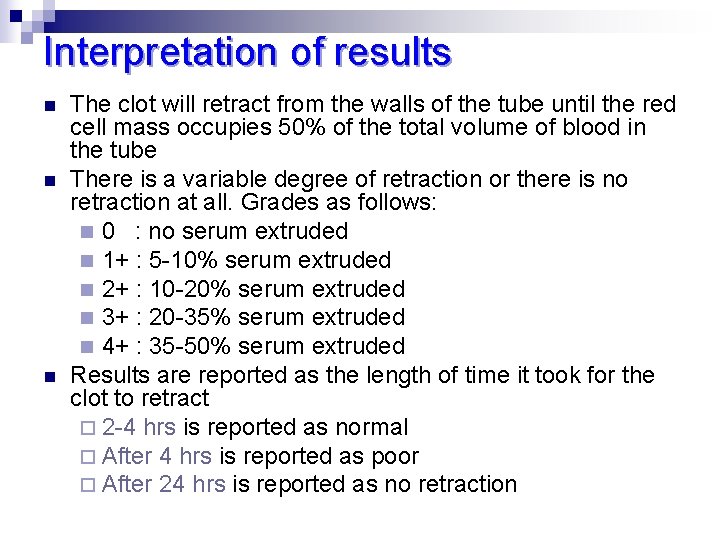
Interpretation of results n n n The clot will retract from the walls of the tube until the red cell mass occupies 50% of the total volume of blood in the tube There is a variable degree of retraction or there is no retraction at all. Grades as follows: n 0 : no serum extruded n 1+ : 5 -10% serum extruded n 2+ : 10 -20% serum extruded n 3+ : 20 -35% serum extruded n 4+ : 35 -50% serum extruded Results are reported as the length of time it took for the clot to retract ¨ 2 -4 hrs is reported as normal ¨ After 4 hrs is reported as poor ¨ After 24 hrs is reported as no retraction
Clot lysis test n n n The whole blood clot lysis time is used to detect increase fibrinolysis This test is only able to detect high increase in fibrinolytic activity Clot lysis testing is a measure of the presence of the clot after 24 hours (blood fibrinolysis).
Procedure 1. 2. 3. 4. At the completion of the clotting time one tube should remain in the 37 water bath A second tube is placed in the refrigerator as soon as clotted as a control The tube is test for the disappearance of clot after 4, 8 and 24 hrs If the sample becomes fluid in less than 48 hrs , the blood is poured out onto a piece of filter paper to be sure for clot disappearance
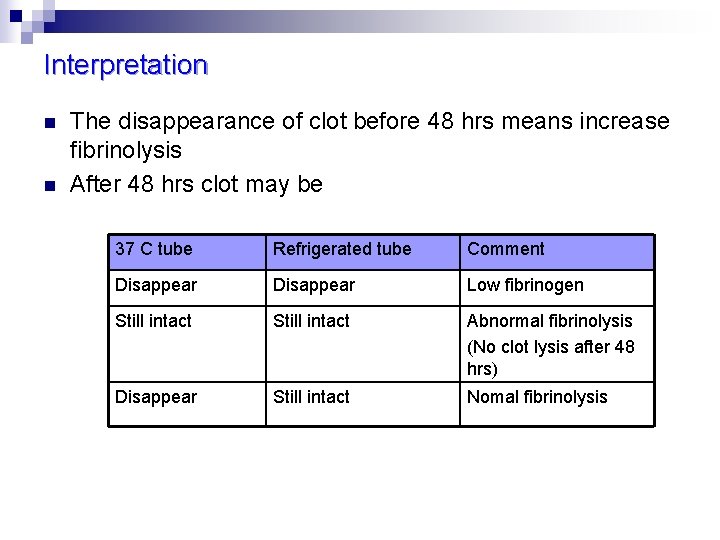
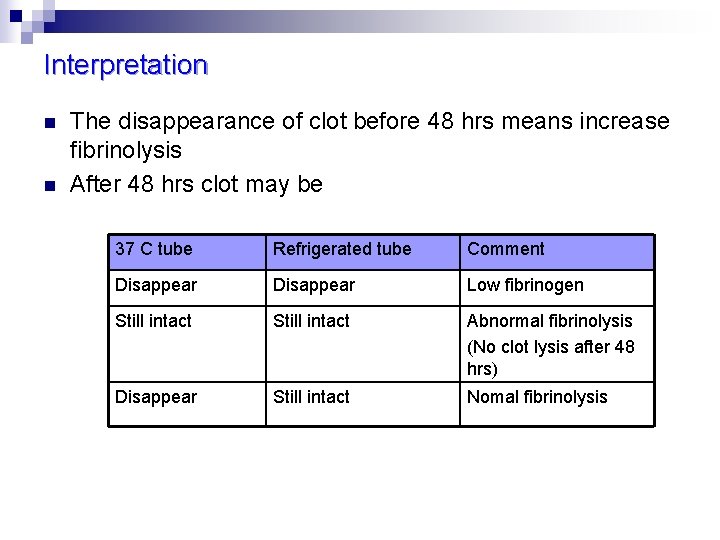
Interpretation n n The disappearance of clot before 48 hrs means increase fibrinolysis After 48 hrs clot may be 37 C tube Refrigerated tube Comment Disappear Low fibrinogen Still intact Abnormal fibrinolysis (No clot lysis after 48 hrs) Disappear Still intact Nomal fibrinolysis
Activity What is the test mentioned below and how w we can do it? . Euglobulin Clot Lysis Time
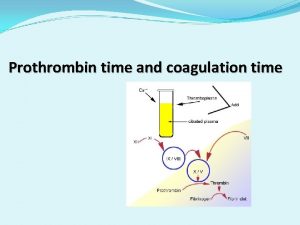
Next Lecture: Prothrombin Time (PT)
 Haemostasis
Haemostasis Clotting factors
Clotting factors Slide method procedure
Slide method procedure 01:640:244 lecture notes - lecture 15: plat, idah, farad
01:640:244 lecture notes - lecture 15: plat, idah, farad Diathermy machine
Diathermy machine Disseminated intravascular coagulation pathophysiology
Disseminated intravascular coagulation pathophysiology Coagulation pathway made easy
Coagulation pathway made easy Coagulation profile test
Coagulation profile test Nécrose de coagulation anapath
Nécrose de coagulation anapath Primary hemostasis
Primary hemostasis Examples of dextrinisation
Examples of dextrinisation Composition of egg
Composition of egg Coagulation profile test
Coagulation profile test Salting out
Salting out Lines of zahn gross
Lines of zahn gross D'alessio
D'alessio Coagulation modifier drugs
Coagulation modifier drugs Coagulation disorders
Coagulation disorders Protein denaturation definition
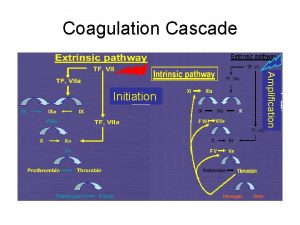
Protein denaturation definition Coagulation cascade
Coagulation cascade Dicoumoral
Dicoumoral Flow chart of blood coagulation
Flow chart of blood coagulation Hus dic
Hus dic General parasitology lecture notes
General parasitology lecture notes Define distinguish
Define distinguish General parasitology lecture notes
General parasitology lecture notes What is elapsed time
What is elapsed time