Brain Abscess 2006 03 14 Definitions Focal pyogenic
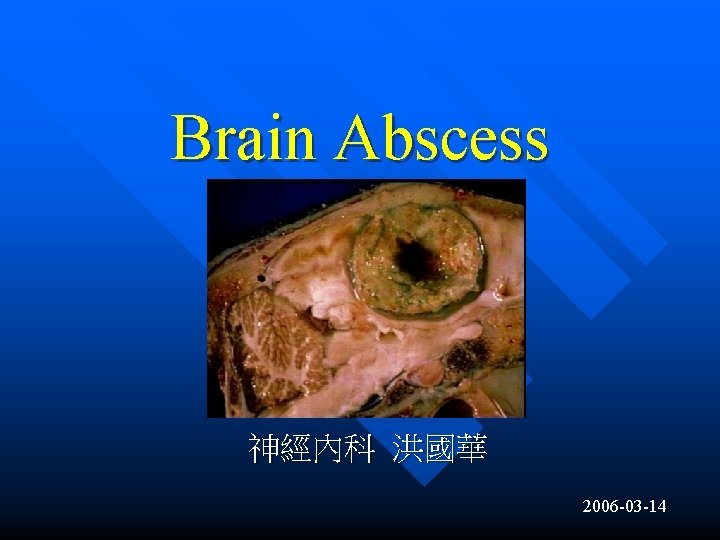
Brain Abscess 神經內科 洪國華 2006 -03 -14

Definitions • • Focal pyogenic infection of the brain parenchyma, typically bacterial; fungal or parasitic less common Four pathologic stages: Early cerebritis, late cerebritis, early capsule, late capsule
Imaging Findings General Features (1) • Best diagnostic clue • Imaging varies with stages of abscess development • Early capsule: Well defined, thin-walled enhancing rim • Ring enhancing lesion with high signal on DWI • T 2 hypointense abscess rim with surrounding edema

Imaging Findings General Features (2) • Location • Typically supratentorial, but may occur infratentorial (up to 14 %) • Frontal and parietal lobes most common, graywhite junction (hematogenous) • Anterior and middle cerebral artery distribution • Size: Variable, 5 mm to several cm
Imaging Findings CT Findings: NECT • • Early cerebritis: Ill-defined hypodense subcortical lesion with mass effect; may be normal early Late cerebritis: Central low density area; peripheral edema, mass effect increase Early capsule: Hypodense mass with moderate vasogenic edema and mass effect Late capsule: Edema, mass effect diminish
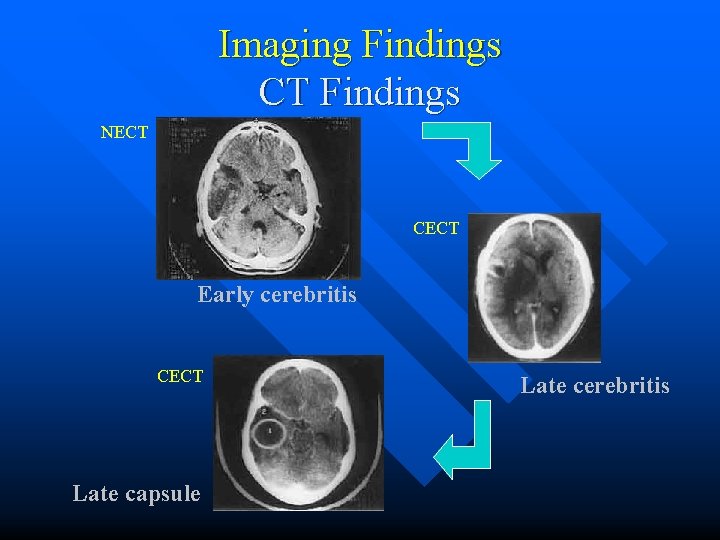
Imaging Findings CT Findings NECT CECT Early cerebritis CECT Late capsule Late cerebritis
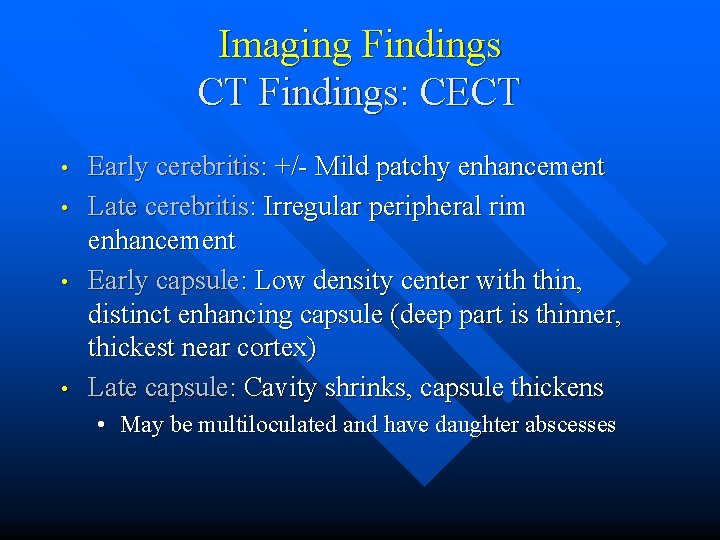
Imaging Findings CT Findings: CECT • • Early cerebritis: +/- Mild patchy enhancement Late cerebritis: Irregular peripheral rim enhancement Early capsule: Low density center with thin, distinct enhancing capsule (deep part is thinner, thickest near cortex) Late capsule: Cavity shrinks, capsule thickens • May be multiloculated and have daughter abscesses

Imaging Findings MR Findings: T 1 WI • • Early cerebritis: Poorly marginated, mixed hypointense/isointense mass Late cerebritis: Hypointense center, isotense /mildly hyperintense rim Early capsule: Rim isointense to hyperintense to white matter; center hyperintense to CSF Late capsule: Cavity shrinks, capsule thickened
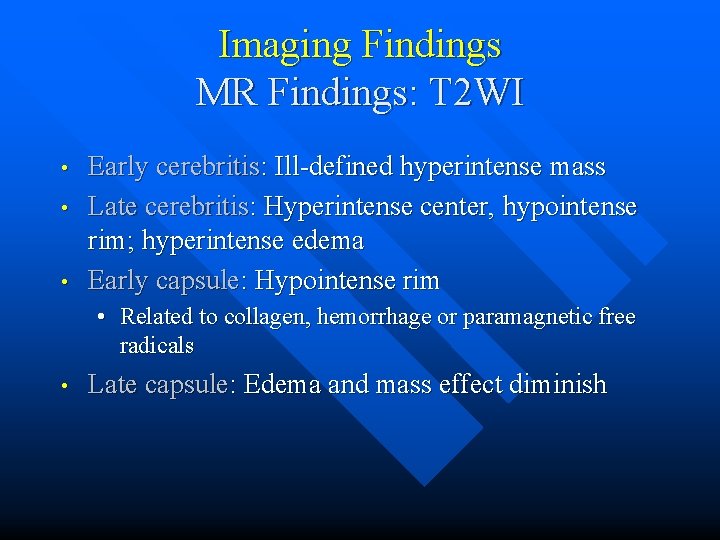
Imaging Findings MR Findings: T 2 WI • • • Early cerebritis: Ill-defined hyperintense mass Late cerebritis: Hyperintense center, hypointense rim; hyperintense edema Early capsule: Hypointense rim • Related to collagen, hemorrhage or paramagnetic free radicals • Late capsule: Edema and mass effect diminish
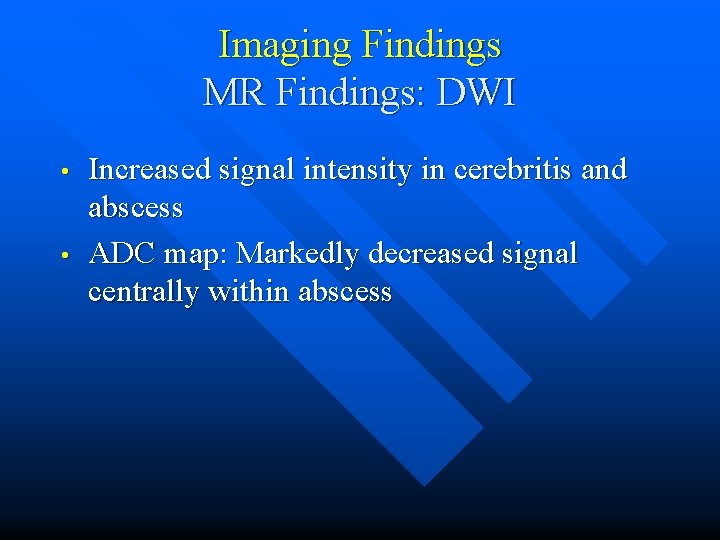
Imaging Findings MR Findings: DWI • • Increased signal intensity in cerebritis and abscess ADC map: Markedly decreased signal centrally within abscess
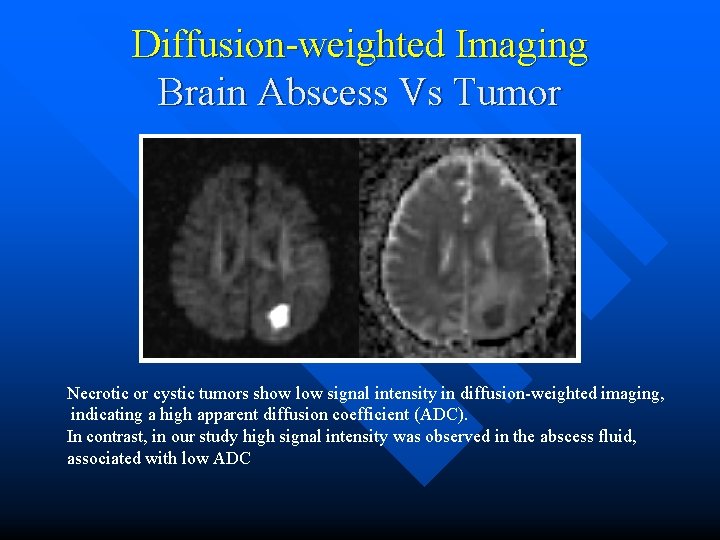
Diffusion-weighted Imaging Brain Abscess Vs Tumor Necrotic or cystic tumors show low signal intensity in diffusion-weighted imaging, indicating a high apparent diffusion coefficient (ADC). In contrast, in our study high signal intensity was observed in the abscess fluid, associated with low ADC
Imaging Findings MR Findings: T 1 C+ • • Early cerebritis: Patchy enhancement Late cerebritis: Intense but irregular rim enhancement Early capsule: Well defined, thin-walled enhancing rim Late capsule: Cavity collapse, thickened enhancement of capsule • Capsule is thinnest on the ventricular side
Imaging Findings MR Findings: MRS • Central necrotic area may show presence of acetate, lactate, alanine, succinate, pyruvate, and amino acids
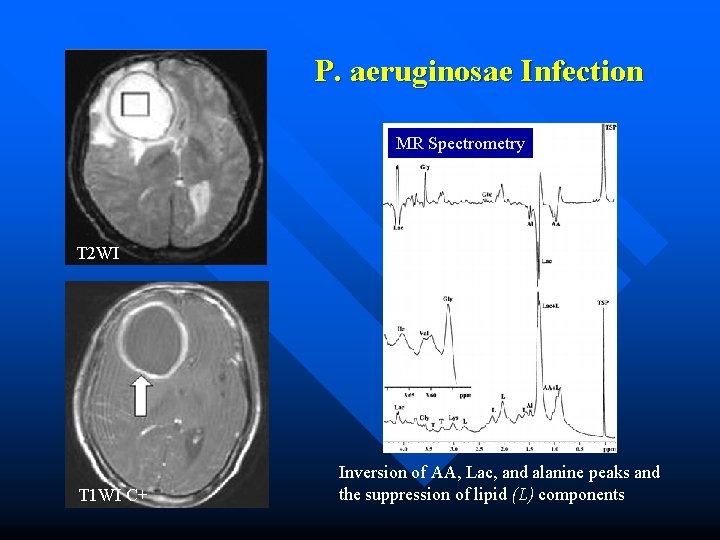
P. aeruginosae Infection MR Spectrometry T 2 WI T 1 WI C+ Inversion of AA, Lac, and alanine peaks and the suppression of lipid (L) components

Imaging Findings Resolving Abscess • • Hyperintense on T 2 WI, FLAIR; hypointense rim resolves Small ring/punctate enhancing focus may persist for month

Imaging Recommendation • • • Best diagnostic tool: Contrast-enhanced MR Protocol advice: Multiplanar MR without and with contrast, DWI MRS may be helpful
Differential Diagnosis • • Primary or metastatic neoplasm Resolving hematoma Demyelination Subacute infarct
Differential Diagnosis Primary or metastatic neoplasm • • Thick, nodular enhancing wall typical Low signal on DWI (occasionally high, can mimic abscess
Differential Diagnosis Resolving hematoma • • History of trauma or vascular lesion Blood products presents
Differential Diagnosis Demyelination • • • Enhancement often incomplete ring Characteristic lesions elsewhere in brain Small amount of mass effect for size of lesion
Differential Diagnosis Subacute infarct • • History of stroke Vascular distribution, gyriform enhancement
Etiology • • • Hematogenous from extracranial location (e. g. pulmonary infection, endocarditis, urinary tract infections) Direct extension from a calvarial or meningeal infection (Paranasal sinus, middle ear, teeth infections) Penetrating trauma Postoperative Right-to-left shunts (congenital cardiac malformations, pulmonary arteriovenous fistulas)
Cryptogenic • • 20~30% have no identifiable source Often polymicrobial (streptococci, staphylococci, anaerobes)

Epidemiology • • • Uncommon, approximately 2500 cases/year in U. S. Bacterial: Staphylococcus, Streptococcus, Pneumococcus Diabetic: Klebsiella pneumoniae Posttransplant: Norcardia, Aspergillus, Candida AIDS: Toxoplasmosis, Mycobacterium Tuberculosis
Pathology Early Cerebritis • • • 3 to 5 days Infection is focal but not localized Unencapsulated mass of PMNs, edema, scattered foci of necrosis and petechial hemorrhages
Pathology Late Cerebritis • • 4 ~ 5 days up to 2 weeks Necrotic foci coalesce Rim of inflammatory cells, macrophages, granulation tissue, fibroblasts surrounds central necrotic core Vascular proliferation, surrounding vasogenic edema
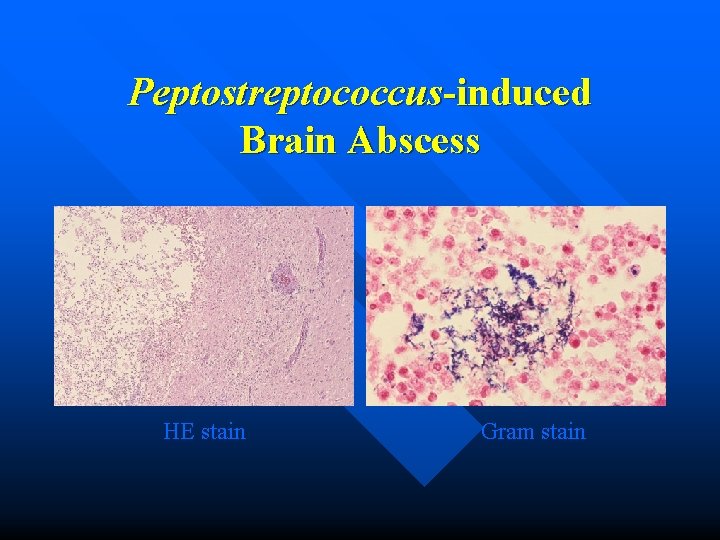
Peptostreptococcus-induced Brain Abscess HE stain Gram stain
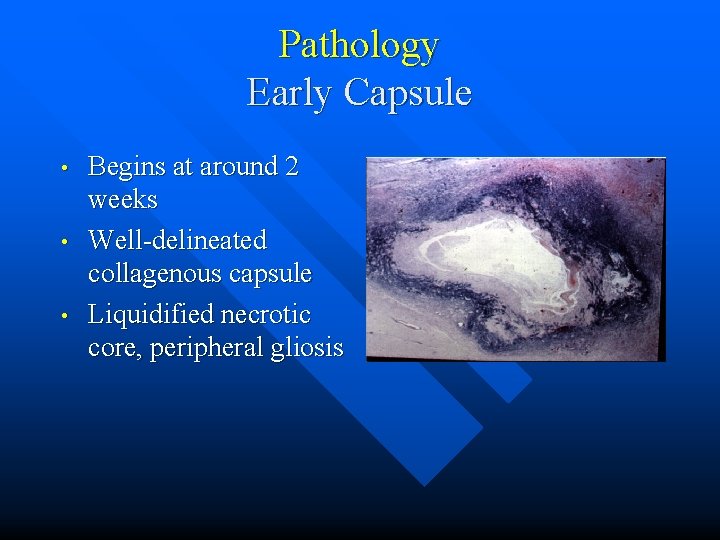
Pathology Early Capsule • • • Begins at around 2 weeks Well-delineated collagenous capsule Liquidified necrotic core, peripheral gliosis
Pathology Late Capsule • • • Weeks to months Central cavity shrinks Thick wall (collagen, granulation tissue, macrophages, gliosis)
Clinical Presentation • • Headache: the most common symptom Fever: 50% Other signs/symptoms: Seizures, altered mental status, focal neurologic deficits Lab: Increased ESR (75%), elevated WBC count (50%)
Demographics • • • May occur at any age Most common during third and fourth decades, but 25% occur in patients < 15 years Gender: M: F = 2: 1
Treatment • • Surgical drainage and/or excision as the primary therapy Antibiotics only if small (< 2. 5 cm) or early phase of cerebritis Steroids to treat edema and mass effect Lumbar puncture hazardous, pathogen often can’t be determined from CSF

Empiric Antibiotic Therapy Primary or Contiguous Source • • • Streptococci (60~70%), bacteroides (20~40%), Enterobacteriaceae (25~33%), S. aureus (10~15%) P Ceph 3 (cefotaxime 2 gm q 4 h IV or ceftriaxone 2 gm q 12 h IV) + metronidazole 7. 5 mg/kg q 6 h or 15 mg/kg q 12 h IV Alternative: Pen G 20~24 m. U IV qd + metronidazole
Empiric Antibiotic Therapy Post-surgical, Post-traumatic • • • S. aureus, Enterobacteriaceae Primary: Oxacillin 2 gm q 4 h IV + P Ceph 3 Alternative: Vancomycin 1 gm q 12 h IV + P Ceph 3
Empiric Antibiotic Therapy HIV-1 Infected (AIDS) • • • Toxoplasma gondii Pyrimethamine + salfadiazine + folinic acid Alternative: TMP/SMX

Complications • Inadequately or untreated abscesses • Intraventricular rupture, ventriculitis (may be fatal) • • • Ventricular debris with irregular fluid level Hydrocephalus Ependymal enhancement typical • Meningitis, “daughter” lesions • Mass effect, herniation
Prognosis • • Stereotactic surgery + medical therapy have greatly reduce mortality Mortality: Variable, 0 ~ 30%
- Slides: 37