Antihypertensive drugs FREQUENCY of arterial hypertension AH AP




![Aldosterone Antagonist Potassium-Sparing Diuretics Spironolactone [ALDACTON] - Hyperaldosteronism - In severe heart failure (NYHA Aldosterone Antagonist Potassium-Sparing Diuretics Spironolactone [ALDACTON] - Hyperaldosteronism - In severe heart failure (NYHA](https://slidetodoc.com/presentation_image_h2/69e6bd8dc7628617460ea294f75ffaba/image-17.jpg)





![ACE Inhibitors ( … pril) Captopril [CAPOTEN] Enalapril [VASOTEC] Lisinopril [PRINIVIL, ZESTRIL] Benazepril [LOTENSIN] ACE Inhibitors ( … pril) Captopril [CAPOTEN] Enalapril [VASOTEC] Lisinopril [PRINIVIL, ZESTRIL] Benazepril [LOTENSIN]](https://slidetodoc.com/presentation_image_h2/69e6bd8dc7628617460ea294f75ffaba/image-34.jpg)

![Angiotensin II Receptor Blockers (. . . sartans) Losartan [COZAAR] Valsartan [DIOVAN] Irbesartan [AVAPRO] Angiotensin II Receptor Blockers (. . . sartans) Losartan [COZAAR] Valsartan [DIOVAN] Irbesartan [AVAPRO]](https://slidetodoc.com/presentation_image_h2/69e6bd8dc7628617460ea294f75ffaba/image-39.jpg)

![Calcium Channel Blockers § Dihydropyridines * § Amlodipine Verapamil § Benzothiazepine Diltiazem [NORVASC] § Calcium Channel Blockers § Dihydropyridines * § Amlodipine Verapamil § Benzothiazepine Diltiazem [NORVASC] §](https://slidetodoc.com/presentation_image_h2/69e6bd8dc7628617460ea294f75ffaba/image-42.jpg)



![Central a 2–Agonists § Clonidine [CATAPRES] § Methyldopa [ALDOMET] § Old drugs: § Guanfacine Central a 2–Agonists § Clonidine [CATAPRES] § Methyldopa [ALDOMET] § Old drugs: § Guanfacine](https://slidetodoc.com/presentation_image_h2/69e6bd8dc7628617460ea294f75ffaba/image-52.jpg)




- Slides: 70

Antihypertensive drugs
FREQUENCY of arterial hypertension (AH) AP > 140/90 mm Hg § 20 -30 % in population § At elderly people - 45 -50 %
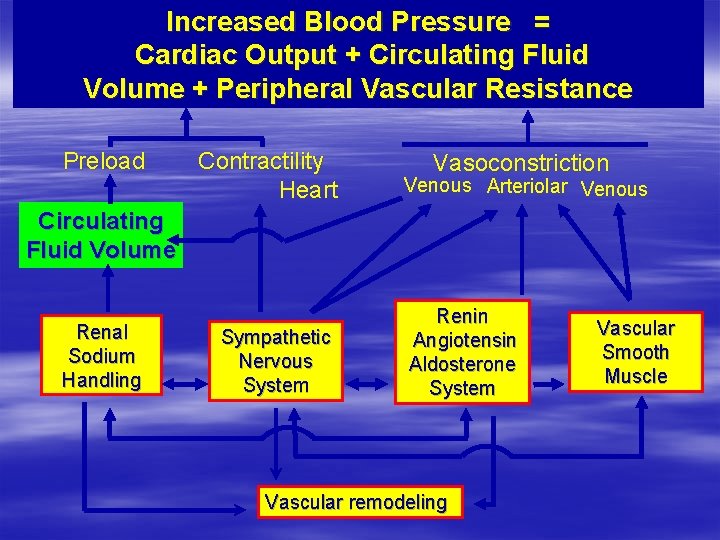
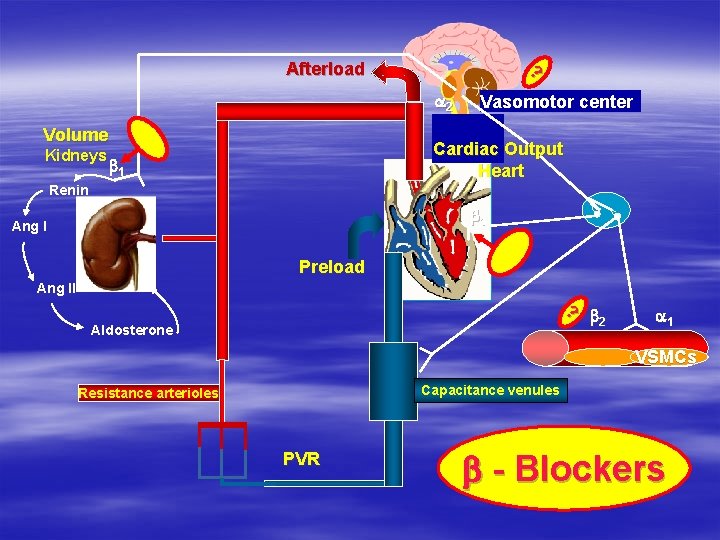
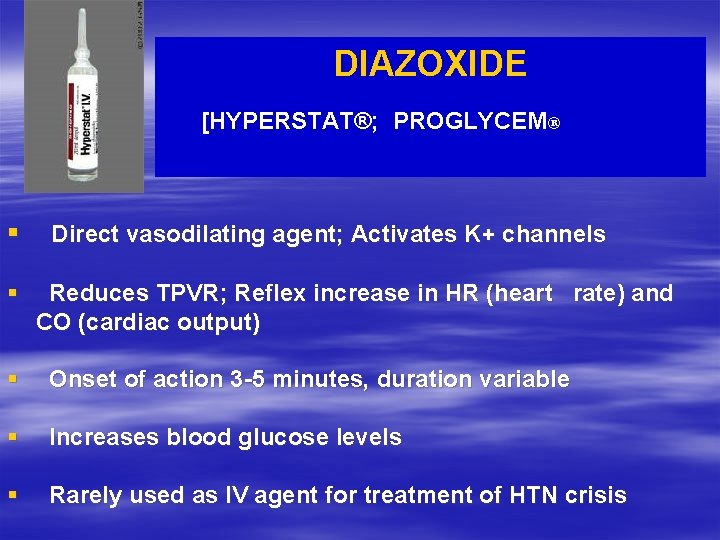
Increased Blood Pressure = Cardiac Output + Circulating Fluid Volume + Peripheral Vascular Resistance Preload Contractility Heart Vasoconstriction Venous Arteriolar Venous Rate Circulating Fluid Volume Renal Sodium Handling Sympathetic Nervous System Renin Angiotensin Aldosterone System Vascular remodeling Vascular Smooth Muscle

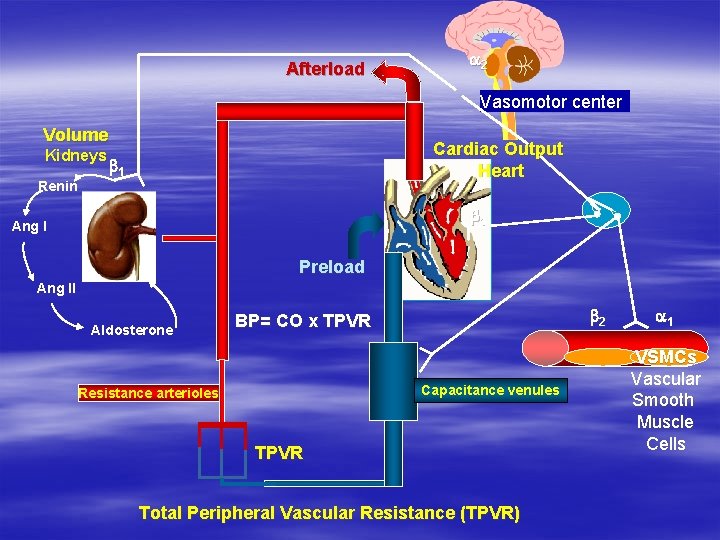
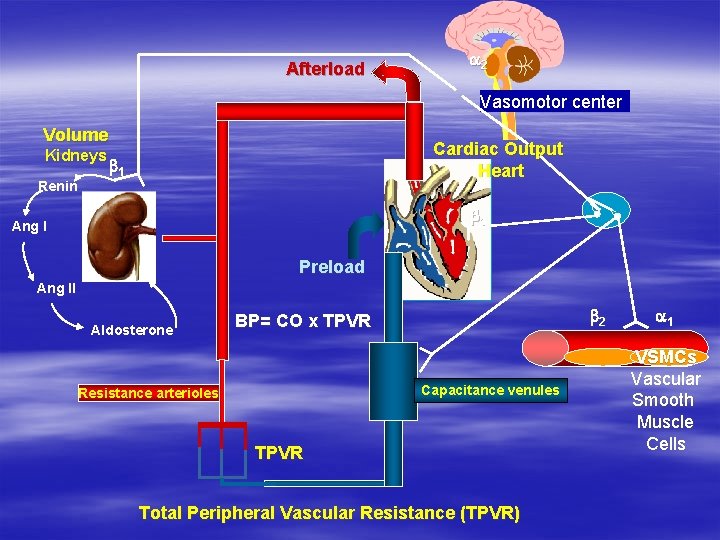
Afterload a 2 Vasomotor center Volume Renin Cardiac Output Heart b 1 V b 1 Ang I V Kidneys Preload Ang II Aldosterone b 2 BP= CO x TPVR Capacitance venules Resistance arterioles TPVR Total Peripheral Vascular Resistance (TPVR) a 1 VSMCs Vascular Smooth Muscle Cells
Factors which provoke AH
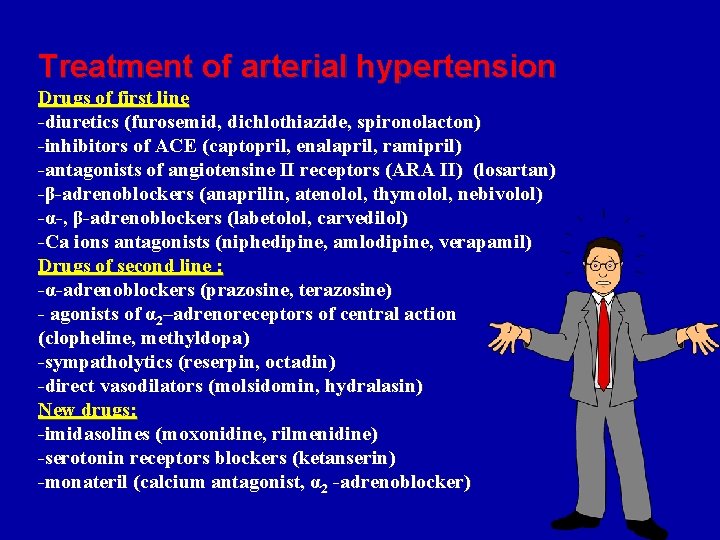
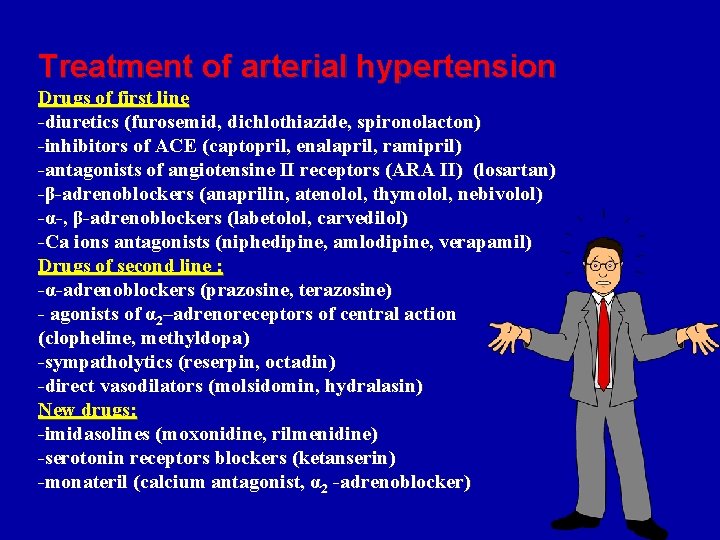
Treatment of arterial hypertension Drugs of first line -diuretics (furosemid, dichlothiazide, spironolacton) -inhibitors of ACE (captopril, enalapril, ramipril) -antagonists of angiotensine II receptors (АRА ІІ) (losartan) -β-adrenoblockers (anaprilin, atenolol, thymolol, nebivolol) -α-, β-adrenoblockers (labetolol, carvedilol) -Ca ions antagonists (niphedipine, amlodipine, verapamil) Drugs of second line : -α-adrenoblockers (prazosine, terazosine) - agonists of α 2–adrenoreceptors of central action (clopheline, methyldopa) -sympatholytics (reserpin, octadin) -direct vasodilators (molsidomin, hydralasin) New drugs: -imidasolines (moxonidine, rilmenidine) -serotonin receptors blockers (ketanserin) -monateril (calcium antagonist, α 2 -adrenoblocker)
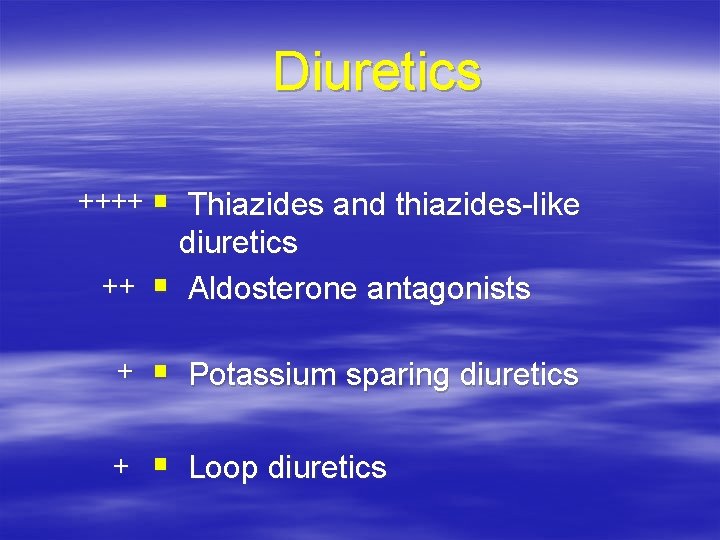
Diuretics
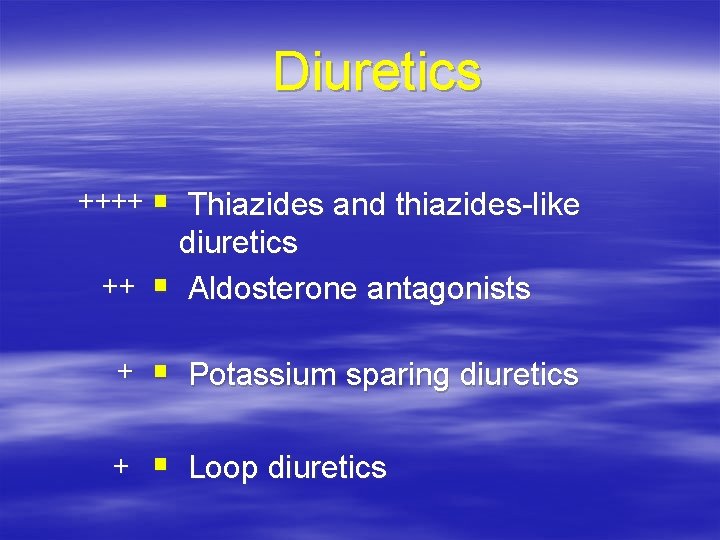
Diuretics ++++ § Thiazides and thiazides-like diuretics ++ § Aldosterone antagonists + § Potassium sparing diuretics + § Loop diuretics
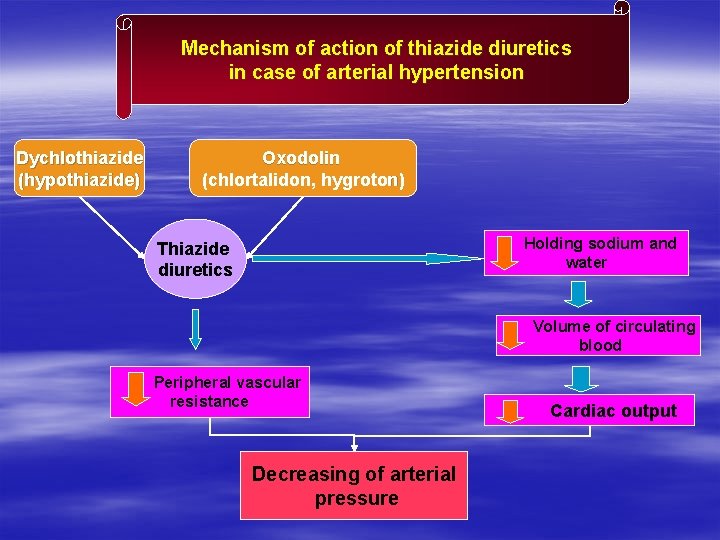
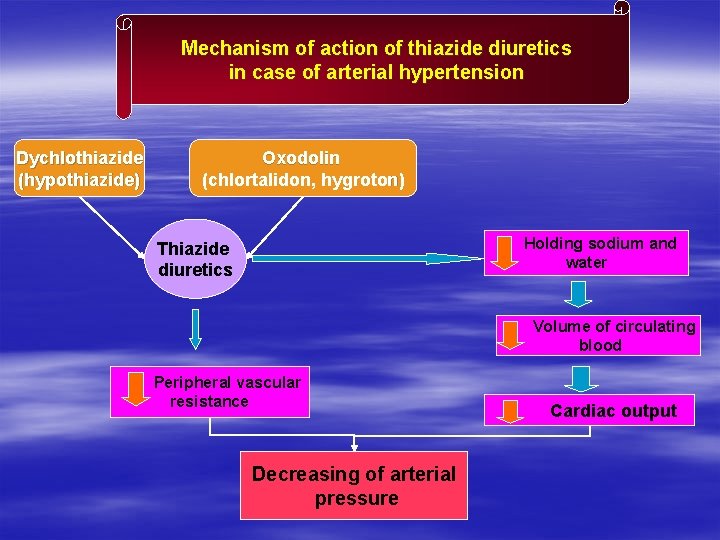
Mechanism of action of thiazide diuretics in case of arterial hypertension Dychlothiazide (hypothiazide) Oxodolin (chlortalidon, hygroton) Holding sodium and water Thiazide diuretics Volume of circulating blood Peripheral vascular resistance Decreasing of arterial pressure Cardiac output
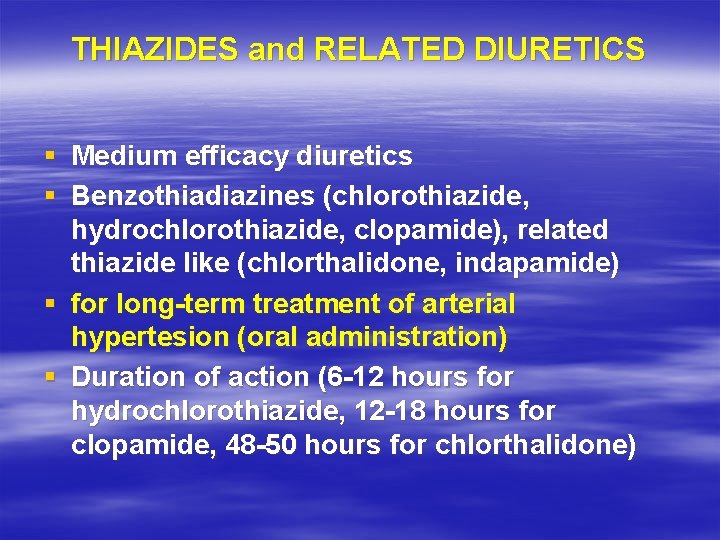
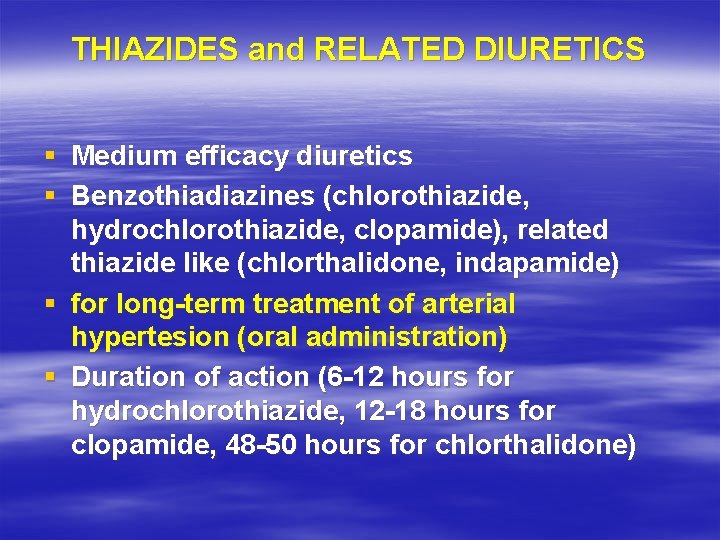
THIAZIDES and RELATED DIURETICS § Medium efficacy diuretics § Benzothiadiazines (chlorothiazide, hydrochlorothiazide, clopamide), related thiazide like (chlorthalidone, indapamide) § for long-term treatment of arterial hypertesion (oral administration) § Duration of action (6 -12 hours for hydrochlorothiazide, 12 -18 hours for clopamide, 48 -50 hours for chlorthalidone)
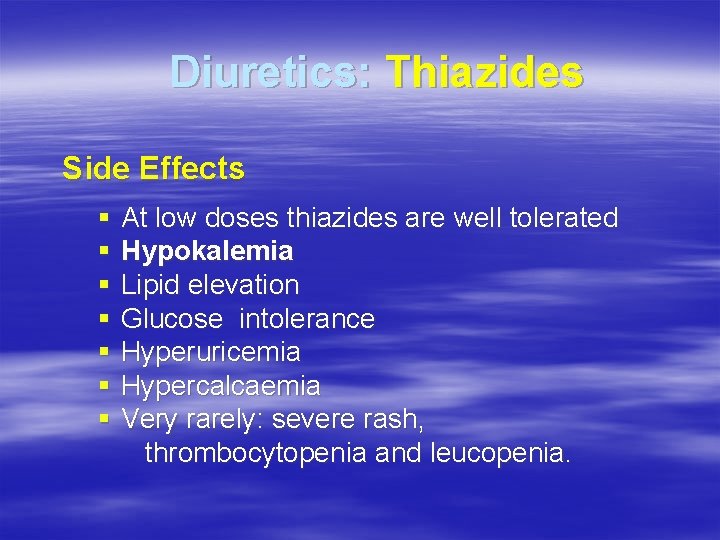
Diuretics: Thiazides Side Effects § At low doses thiazides are well tolerated § Hypokalemia § Lipid elevation § Glucose intolerance § Hyperuricemia § Hypercalcaemia § Very rarely: severe rash, thrombocytopenia and leucopenia.
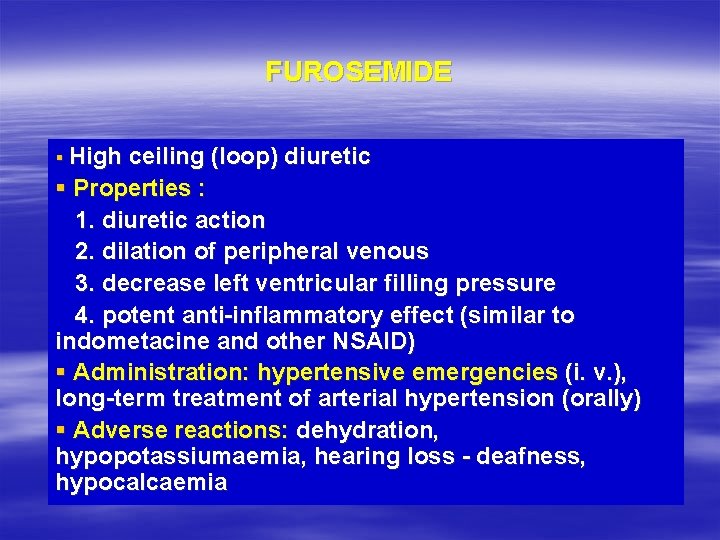
FUROSEMIDE § High ceiling (loop) diuretic § Properties : 1. diuretic action 2. dilation of peripheral venous 3. decrease left ventricular filling pressure 4. potent anti-inflammatory effect (similar to indometacine and other NSAID) § Administration: hypertensive emergencies (i. v. ), long-term treatment of arterial hypertension (orally) § Adverse reactions: dehydration, hypopotassiumaemia, hearing loss - deafness, hypocalcaemia

Furosemid (diuretic)
Furosemid (diuretic)

Triampur (triamteren + hydrochlorthiaside) diuretic
![Aldosterone Antagonist PotassiumSparing Diuretics Spironolactone ALDACTON Hyperaldosteronism In severe heart failure NYHA Aldosterone Antagonist Potassium-Sparing Diuretics Spironolactone [ALDACTON] - Hyperaldosteronism - In severe heart failure (NYHA](https://slidetodoc.com/presentation_image_h2/69e6bd8dc7628617460ea294f75ffaba/image-17.jpg)
Aldosterone Antagonist Potassium-Sparing Diuretics Spironolactone [ALDACTON] - Hyperaldosteronism - In severe heart failure (NYHA Class IV), improves survival and reduces hospitalization (RALES Study) - Hyperkalemia, Gynecomastia
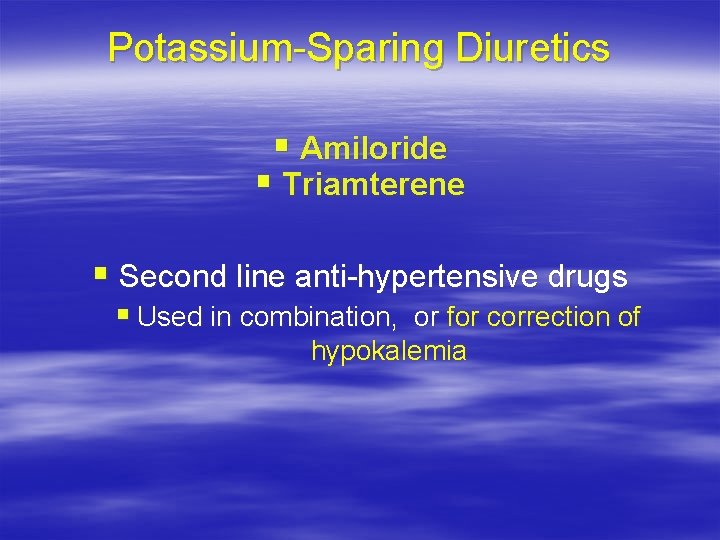
Potassium-Sparing Diuretics § Amiloride § Triamterene § Second line anti-hypertensive drugs § Used in combination, or for correction of hypokalemia

Beta-adrenoblockers

Mechanism of action of beta-adrenoblockers (anaprilin, atenolol, methoprolol etc. ) in case of arterial hypertension βadrenoblockers β 1 -adrenoreceptors of heart NO production Cardiac output Peripheral resistance of vessels Angiotensine Renin Decreasing of blood pressure ΙΙ Aldosterone Holding sodium and water Volume of blood circulation
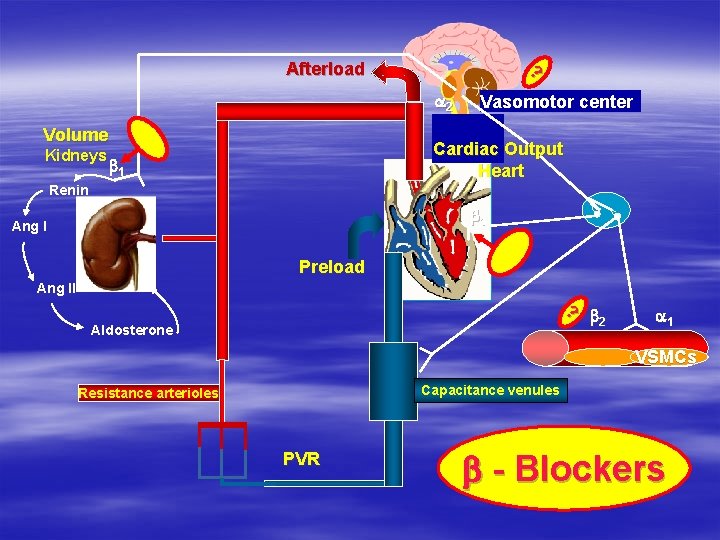
? Afterload a 2 Volume Kidneys Vasomotor center Cardiac Output Heart b 1 Renin V V b 1 Ang I Preload Ang II ? b 2 Aldosterone a 1 VSMCs Capacitance venules Resistance arterioles PVR b - Blockers
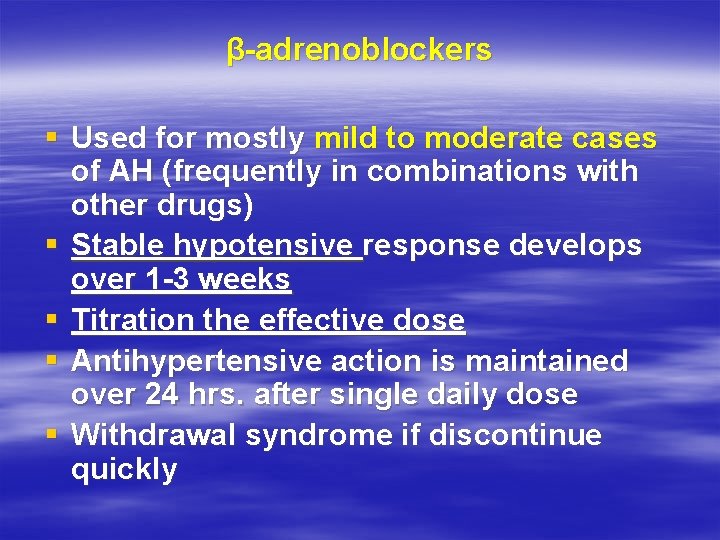
β-adrenoblockers § Used for mostly mild to moderate cases of AH (frequently in combinations with other drugs) § Stable hypotensive response develops over 1 -3 weeks § Titration the effective dose § Antihypertensive action is maintained over 24 hrs. after single daily dose § Withdrawal syndrome if discontinue quickly
Beta Blockers § Side Effects: § Bronchospasm § Bradicardia/heart block § Mask and prolong the symptoms of hypoglycemia § Abrupt withdrawal can precipitate MI § Cold extremities, Raynaud’s phenomenon, intermittent § § § claudication Decreased exercise tolerance; fatigue, depression and impotence CNS: sleep disturbance, vivid dreams, nightmares Effects of plasma lipids
Atenolol β - adrenoblocker
Anaprilin β 1 - β 2 adrenoblocker
Vasocardin 100 mg Methoprolol tartrate
Nadolol ( β 1, β 2 - adrenoblocker )

Tenoretic (atenolol + chlortalidon)

Nebilet (Nebivolol) Betaadrenoblocker with excessive production of NO (nitric oxide)
α, β – adrenoreceptors blockers (labetalol, carvedilol) § Labetalol is used for long-term treatment of AH and for emergencies (i. v. - hypertensive crisis, clonidine withdrawal, cheese reaction) § Carvedilol – produces vasodilatation, antioxidant/free radical scavenging properties, it is used for CHF
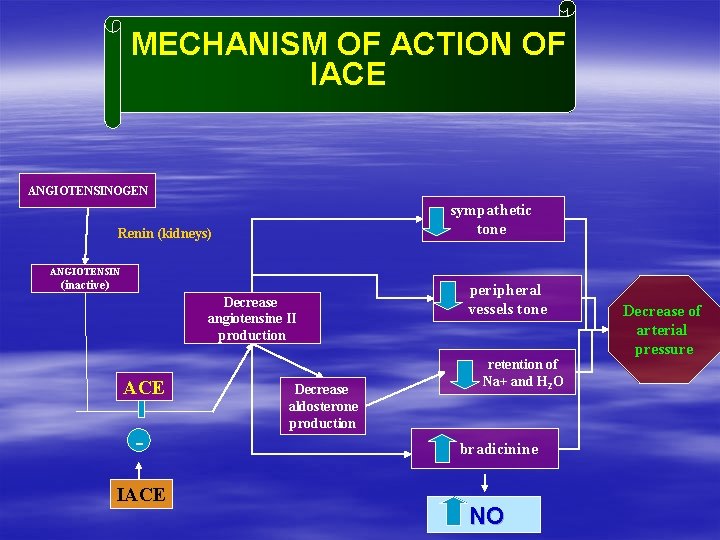
IACE (ANGIOTENSIN CONVERTING ENZYME INHIBITORS)
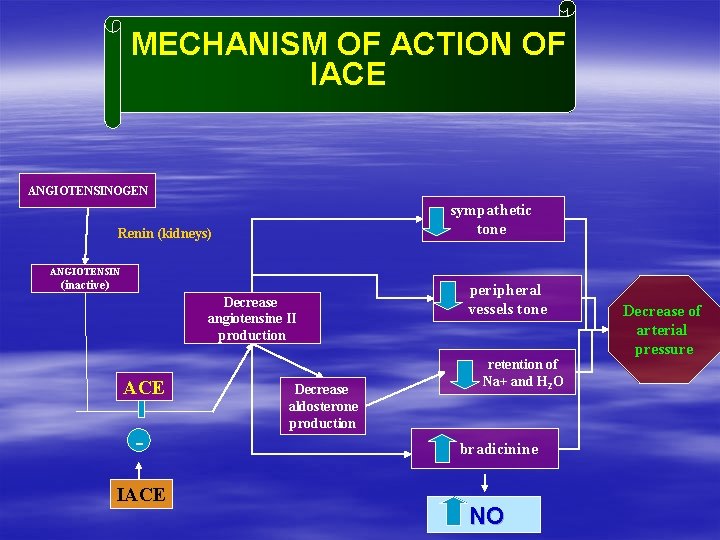
MECHANISM OF ACTION OF IACE ANGIOTENSINOGEN sympathetic tone Renin (kidneys) ANGIOTENSIN (inactive) Decrease angiotensine II production ACE IACE Decrease aldosterone production peripheral vessels tone retention of Na+ and H 2 O bradicinine NO Decrease of arterial pressure

![ACE Inhibitors pril Captopril CAPOTEN Enalapril VASOTEC Lisinopril PRINIVIL ZESTRIL Benazepril LOTENSIN ACE Inhibitors ( … pril) Captopril [CAPOTEN] Enalapril [VASOTEC] Lisinopril [PRINIVIL, ZESTRIL] Benazepril [LOTENSIN]](https://slidetodoc.com/presentation_image_h2/69e6bd8dc7628617460ea294f75ffaba/image-34.jpg)
ACE Inhibitors ( … pril) Captopril [CAPOTEN] Enalapril [VASOTEC] Lisinopril [PRINIVIL, ZESTRIL] Benazepril [LOTENSIN] Fosinopril [MONOPRIL] Quinapril [ACCUPRIL] Ramipril [ALTACE] Spirapril [RENOMAX] Moexipril [UNIVASC] Perindopril [ACEON] Trandolapril [MAVIK]

Captopril (IACE)
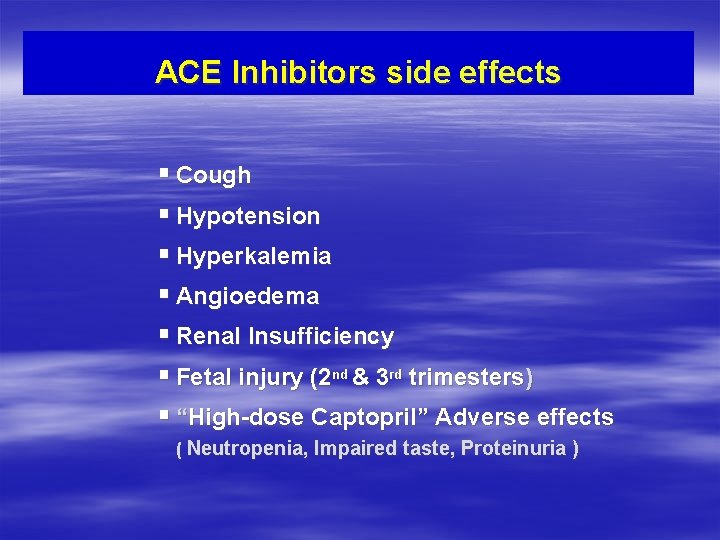
ACE Inhibitors side effects § Cough § Hypotension § Hyperkalemia § Angioedema § Renal Insufficiency § Fetal injury (2 nd & 3 rd trimesters) § “High-dose Captopril” Adverse effects ( Neutropenia, Impaired taste, Proteinuria )
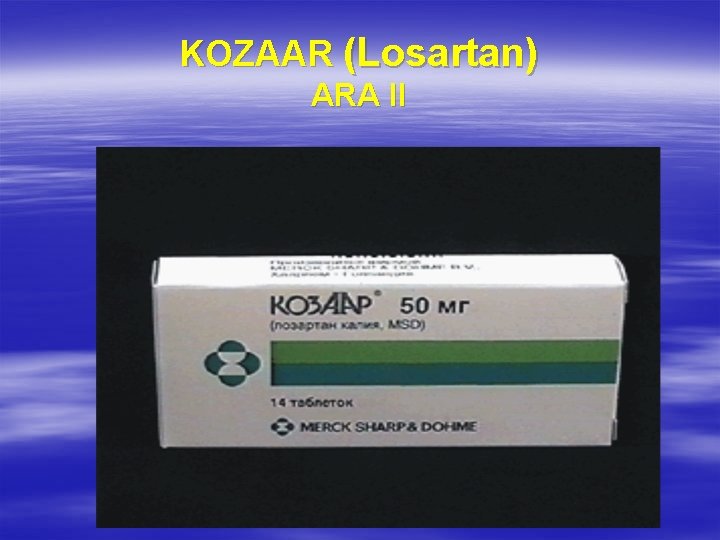
KOZAAR (Losartan) АRА ІІ
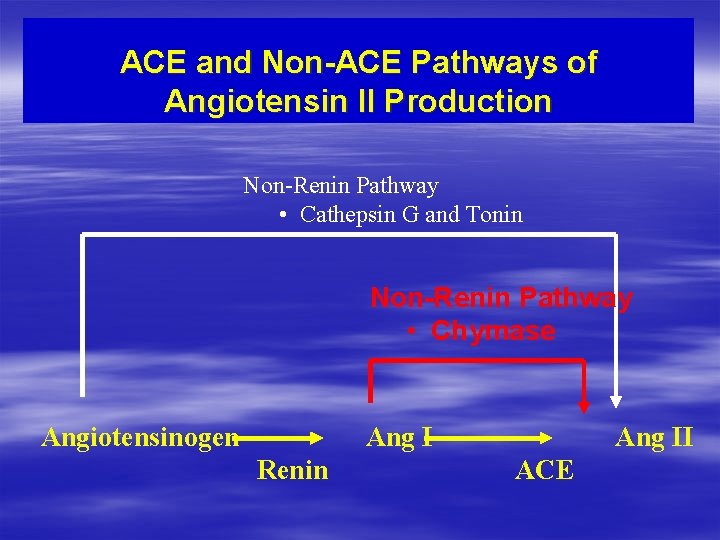
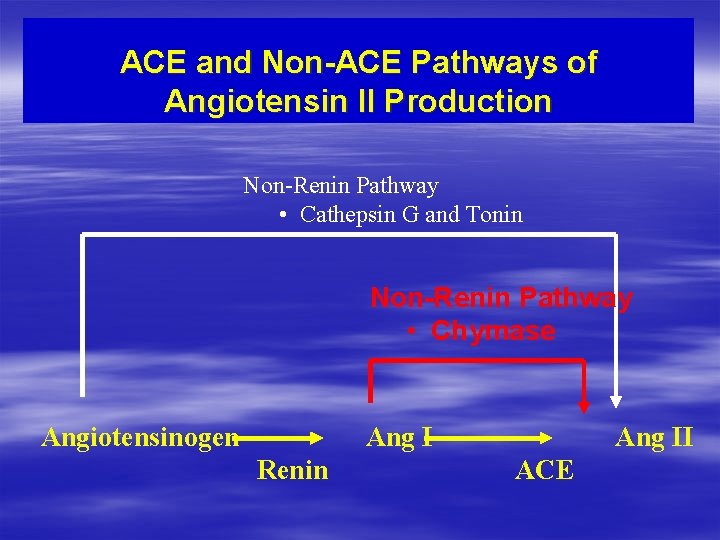
ACE and Non-ACE Pathways of Angiotensin II Production Non-Renin Pathway • Cathepsin G and Tonin Non-Renin Pathway • Chymase Angiotensinogen Ang I Renin Ang II ACE
![Angiotensin II Receptor Blockers sartans Losartan COZAAR Valsartan DIOVAN Irbesartan AVAPRO Angiotensin II Receptor Blockers (. . . sartans) Losartan [COZAAR] Valsartan [DIOVAN] Irbesartan [AVAPRO]](https://slidetodoc.com/presentation_image_h2/69e6bd8dc7628617460ea294f75ffaba/image-39.jpg)
Angiotensin II Receptor Blockers (. . . sartans) Losartan [COZAAR] Valsartan [DIOVAN] Irbesartan [AVAPRO] Candesartan [ATACAND] Eprosartan [TEVETEN] Tasosartan [VERDIA] Telmisartan [MICARDIS]

Calcium Channel Blockers
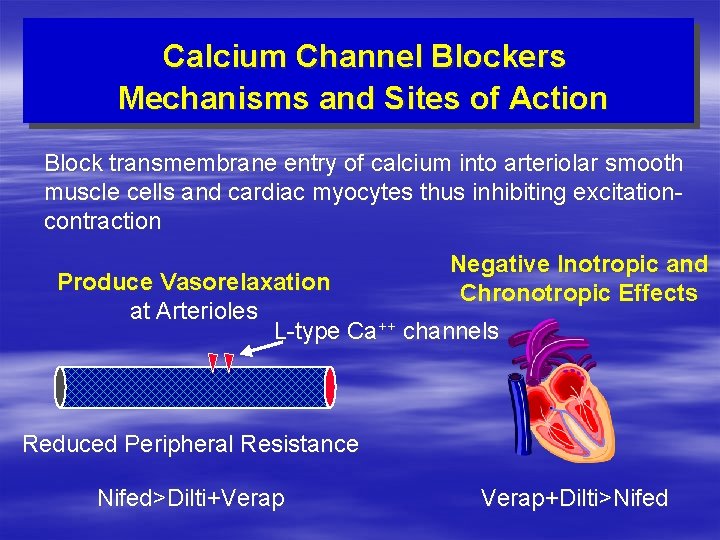
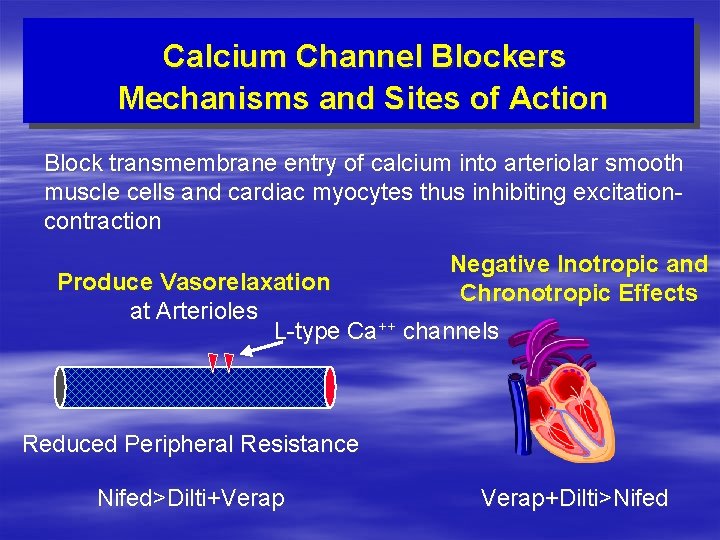
Calcium Channel Blockers Mechanisms and Sites of Action Block transmembrane entry of calcium into arteriolar smooth muscle cells and cardiac myocytes thus inhibiting excitationcontraction Negative Inotropic and Chronotropic Effects Produce Vasorelaxation at Arterioles L-type Ca++ channels Reduced Peripheral Resistance Nifed>Dilti+Verap+Dilti>Nifed
![Calcium Channel Blockers Dihydropyridines Amlodipine Verapamil Benzothiazepine Diltiazem NORVASC Calcium Channel Blockers § Dihydropyridines * § Amlodipine Verapamil § Benzothiazepine Diltiazem [NORVASC] §](https://slidetodoc.com/presentation_image_h2/69e6bd8dc7628617460ea294f75ffaba/image-42.jpg)
Calcium Channel Blockers § Dihydropyridines * § Amlodipine Verapamil § Benzothiazepine Diltiazem [NORVASC] § Felodipine § Isradipine § Nicardipine § Nimodipine * long-acting or slow-released [NIMOTOP] § Nifedipine [PROCARDIA, ADALAT] § Phenylalkylamine * formulations should be used for high blood pressure
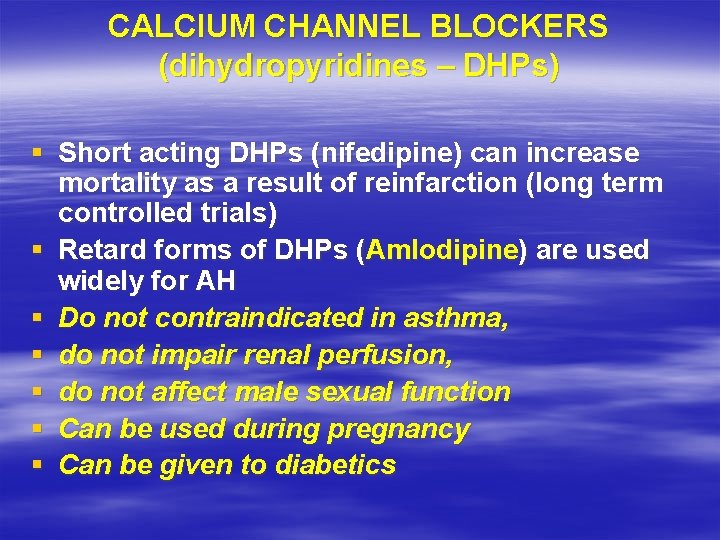
CALCIUM CHANNEL BLOCKERS (dihydropyridines – DHPs) § Short acting DHPs (nifedipine) can increase mortality as a result of reinfarction (long term controlled trials) § Retard forms of DHPs (Amlodipine) are used widely for AH § Do not contraindicated in asthma, § do not impair renal perfusion, § do not affect male sexual function § Can be used during pregnancy § Can be given to diabetics
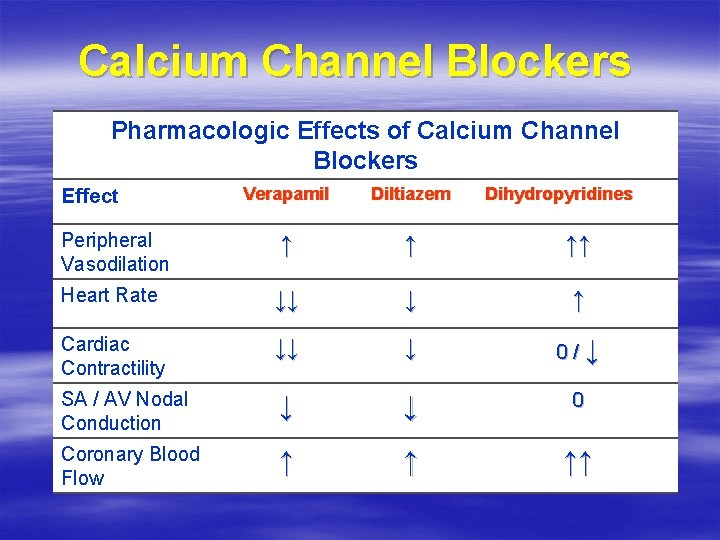
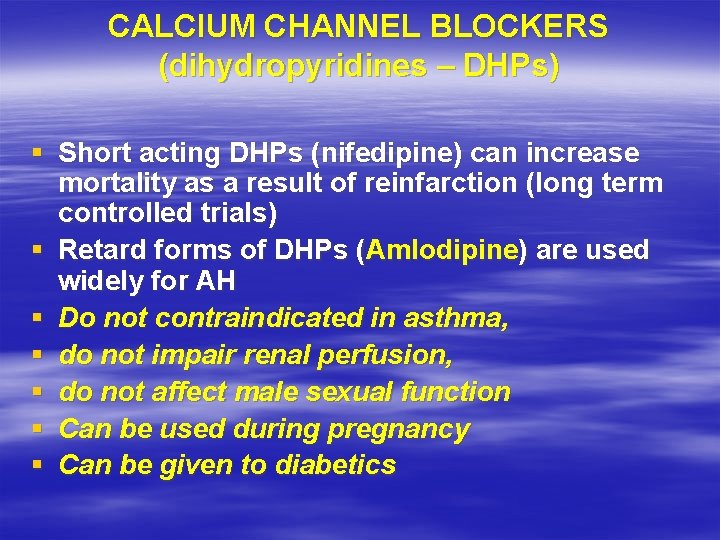
Calcium Channel Blockers Pharmacologic Effects of Calcium Channel Blockers Verapamil Diltiazem ↑ ↑ ↑↑ Heart Rate ↓↓ ↓ ↑ Cardiac Contractility ↓↓ ↓ 0/↓ SA / AV Nodal Conduction ↓ ↓ 0 Coronary Blood Flow ↑ ↑ ↑↑ Effect Peripheral Vasodilation Dihydropyridines
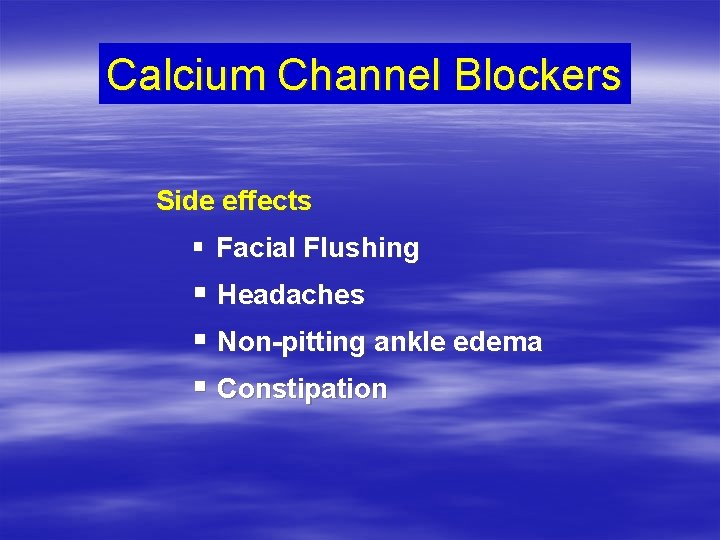
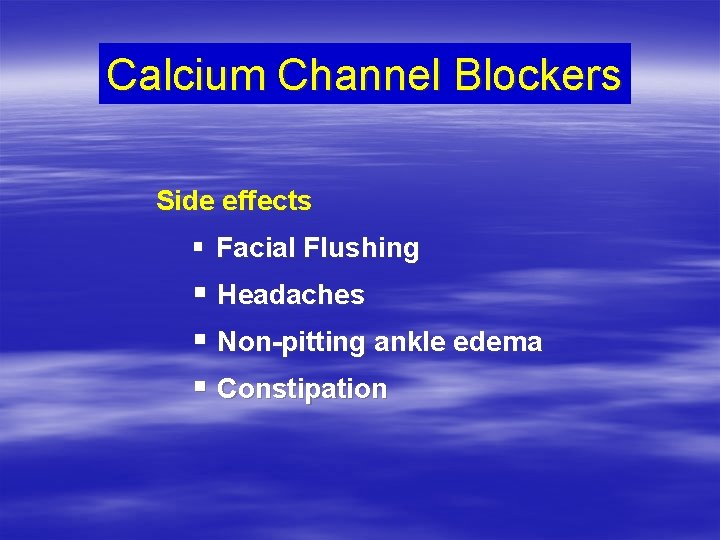
Calcium Channel Blockers Side effects § Facial Flushing § Headaches § Non-pitting ankle edema § Constipation

NIFEDIPINE (calcium channels blocker)

NIFEDIPINE (calcium channels blocker)

NIFEDIPINE (calcium channels blocker)
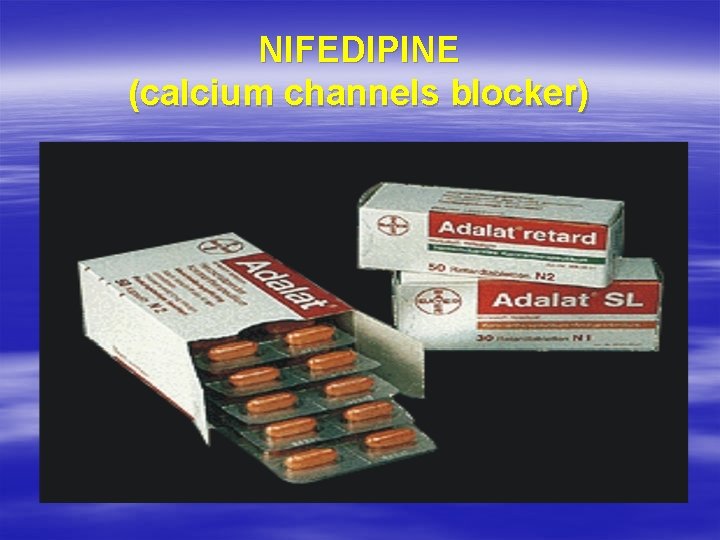
NIFEDIPINE (calcium channels blocker)
NORVASC (AMLODIPINE) (calcium channels blocker)
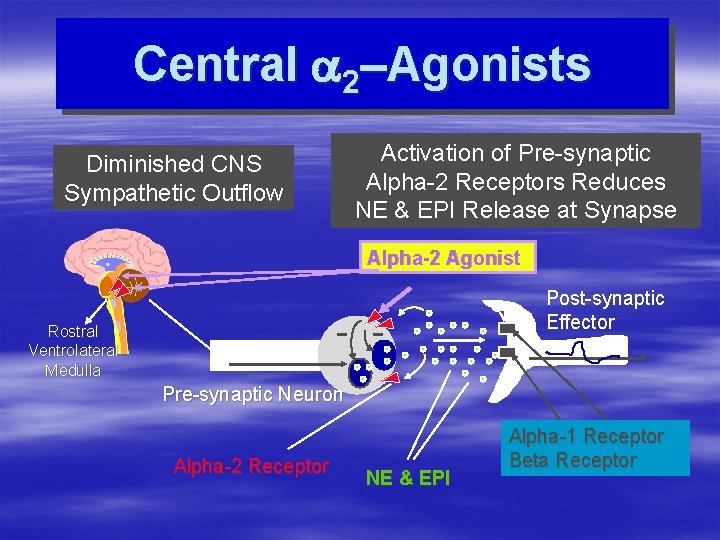
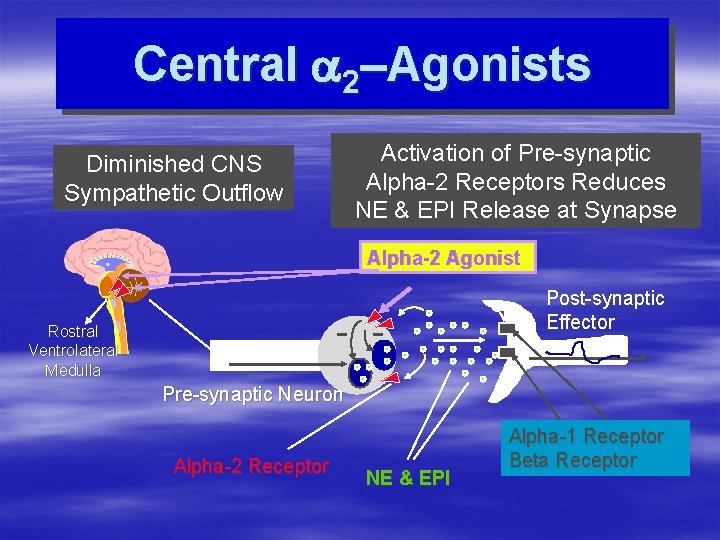
Central a 2–Agonists Diminished CNS Sympathetic Outflow Activation of Pre-synaptic Alpha-2 Receptors Reduces NE & EPI Release at Synapse Alpha-2 Agonist Post-synaptic Effector Rostral Ventrolateral Medulla Pre-synaptic Neuron Alpha-2 Receptor NE & EPI Alpha-1 Receptor Beta Receptor
![Central a 2Agonists Clonidine CATAPRES Methyldopa ALDOMET Old drugs Guanfacine Central a 2–Agonists § Clonidine [CATAPRES] § Methyldopa [ALDOMET] § Old drugs: § Guanfacine](https://slidetodoc.com/presentation_image_h2/69e6bd8dc7628617460ea294f75ffaba/image-52.jpg)
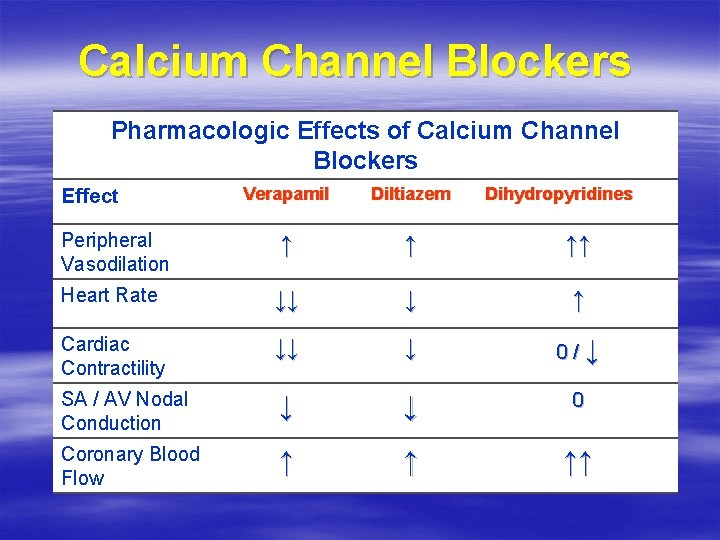
Central a 2–Agonists § Clonidine [CATAPRES] § Methyldopa [ALDOMET] § Old drugs: § Guanfacine § Guanabenz
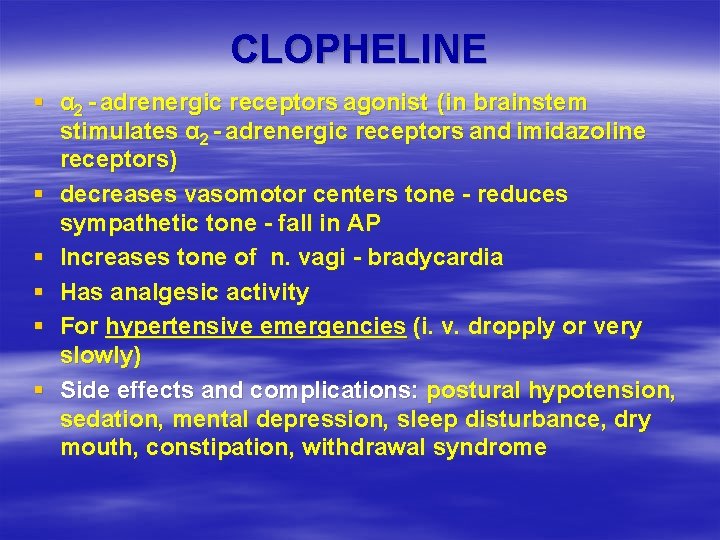
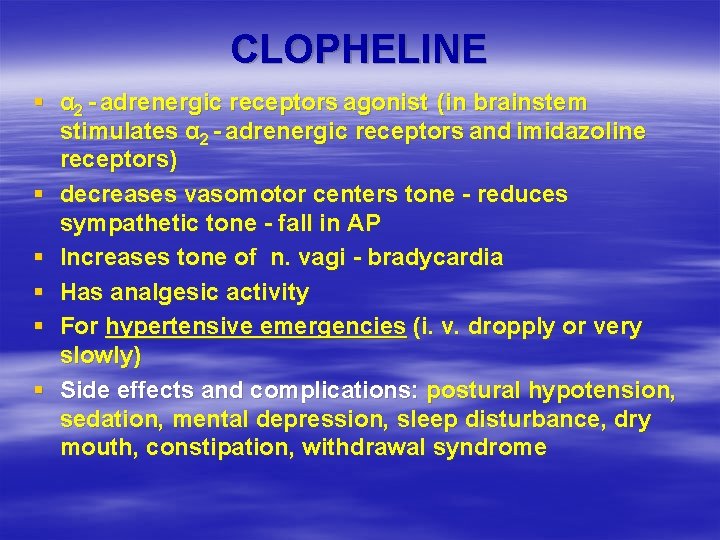
CLOPHELINE § α 2 - adrenergic receptors agonist (in brainstem stimulates α 2 - adrenergic receptors and imidazoline receptors) § decreases vasomotor centers tone - reduces sympathetic tone - fall in AP § Increases tone of n. vagi - bradycardia § Has analgesic activity § For hypertensive emergencies (i. v. dropply or very slowly) § Side effects and complications: postural hypotension, sedation, mental depression, sleep disturbance, dry mouth, constipation, withdrawal syndrome

CLOPHELINE (decreases vasomotor centers tone)
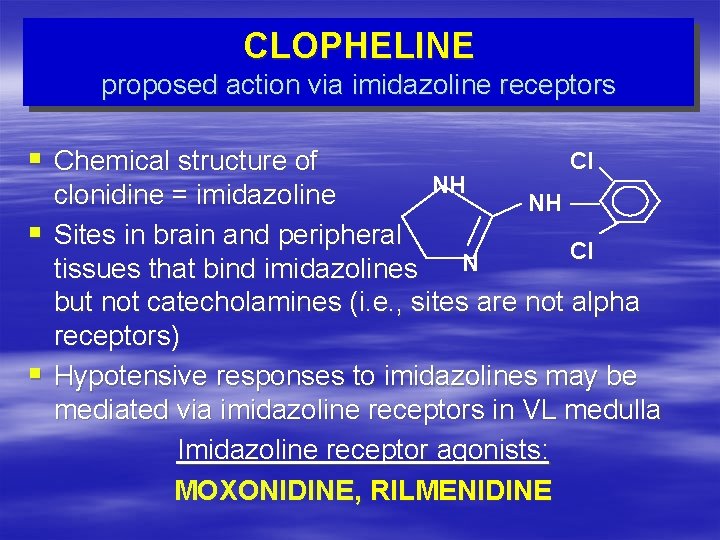
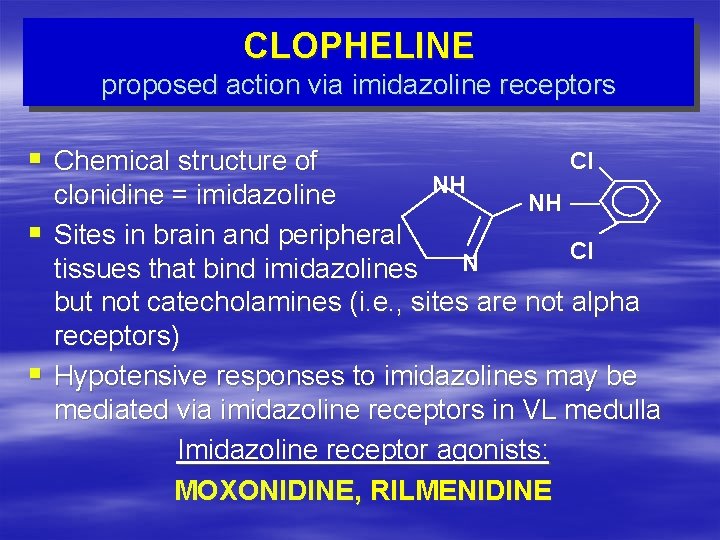
CLOPHELINE proposed action via imidazoline receptors § Chemical structure of § § Cl NH clonidine = imidazoline NH Sites in brain and peripheral Cl N tissues that bind imidazolines but not catecholamines (i. e. , sites are not alpha receptors) Hypotensive responses to imidazolines may be mediated via imidazoline receptors in VL medulla Imidazoline receptor agonists: MOXONIDINE, RILMENIDINE
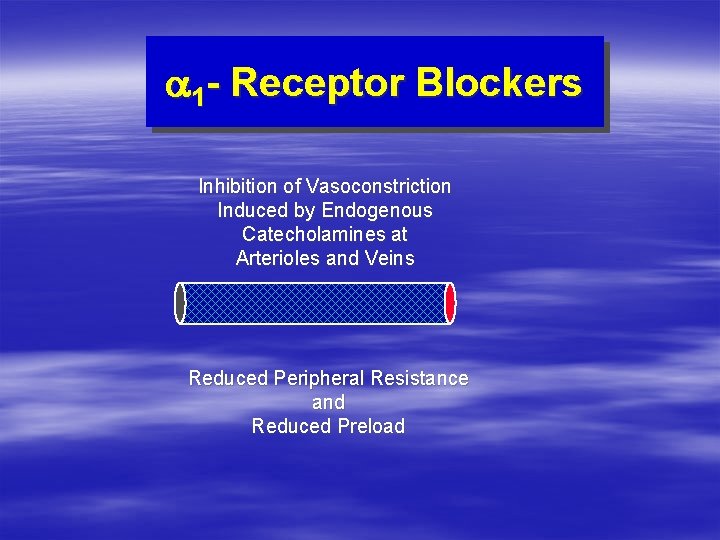
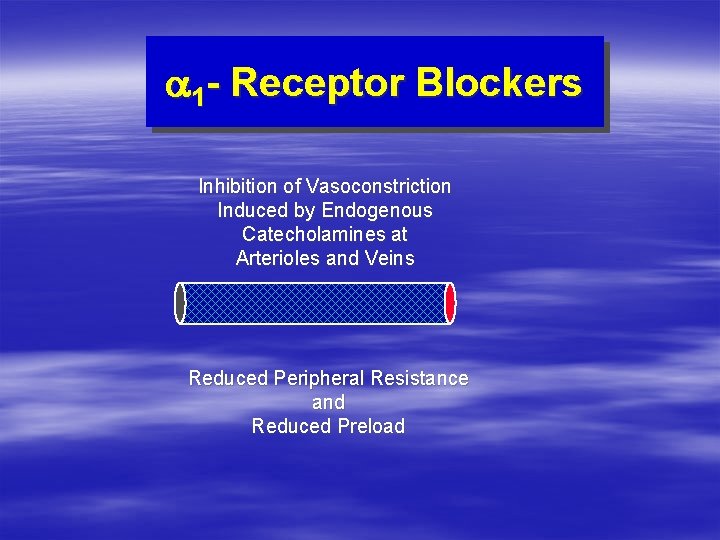
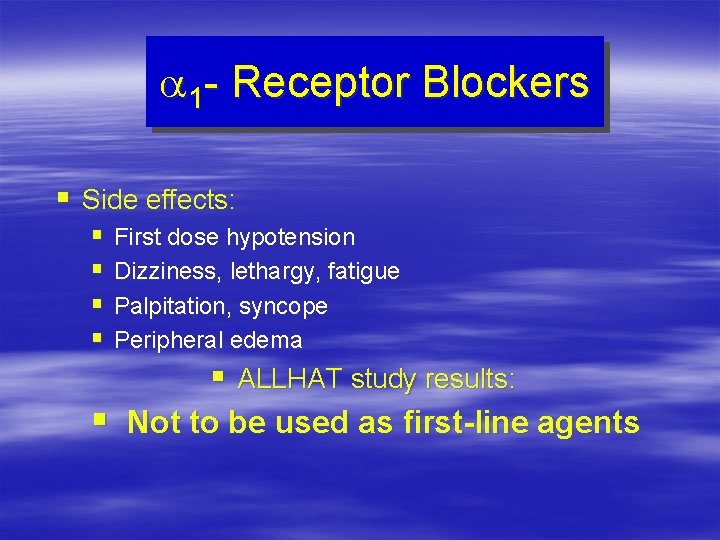
a 1 - Receptor Blockers Inhibition of Vasoconstriction Induced by Endogenous Catecholamines at Arterioles and Veins Reduced Peripheral Resistance and Reduced Preload
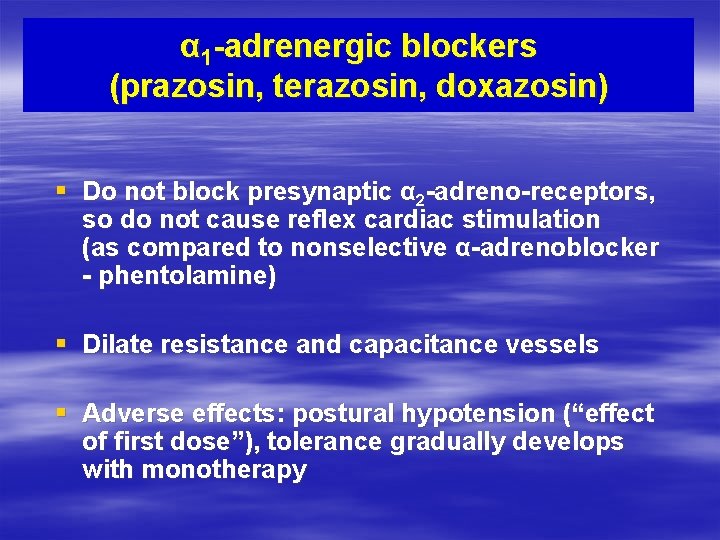
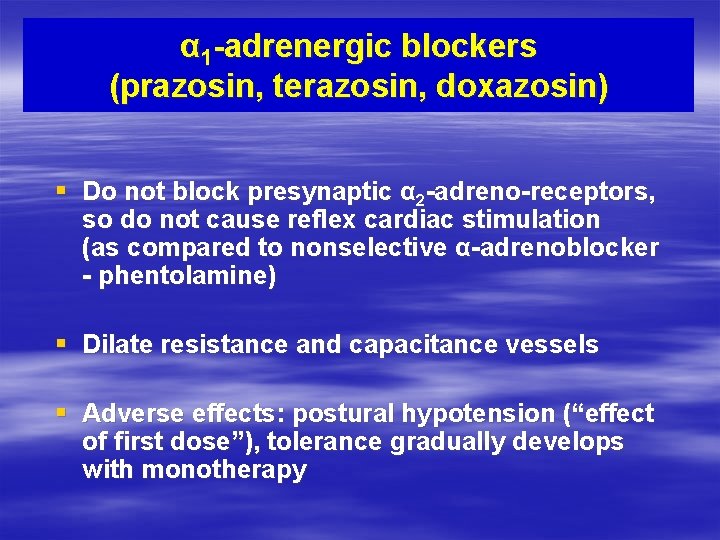
α 1 -adrenergic blockers (prazosin, terazosin, doxazosin) § Do not block presynaptic α 2 -adreno-receptors, so do not cause reflex cardiac stimulation (as compared to nonselective α-adrenoblocker - phentolamine) § Dilate resistance and capacitance vessels § Adverse effects: postural hypotension (“effect of first dose”), tolerance gradually develops with monotherapy

Prazosine (α 1 –adrenoblocker)
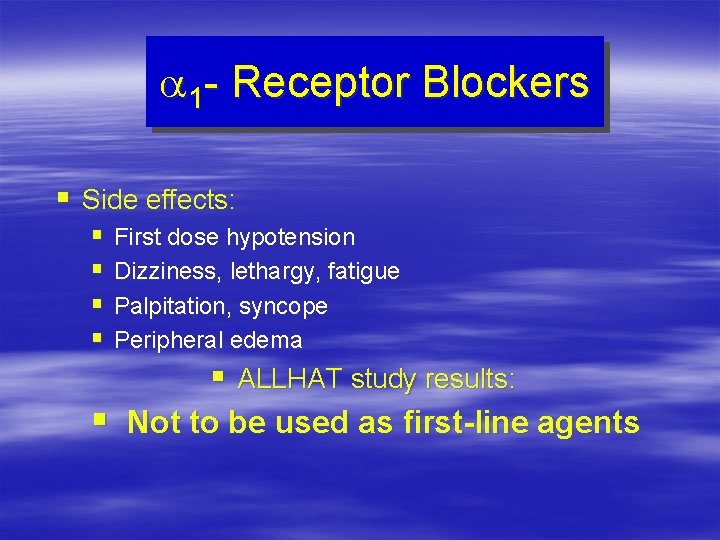
a 1 - Receptor Blockers § Side effects: § First dose hypotension § Dizziness, lethargy, fatigue § Palpitation, syncope § Peripheral edema § ALLHAT study results: § Not to be used as first-line agents
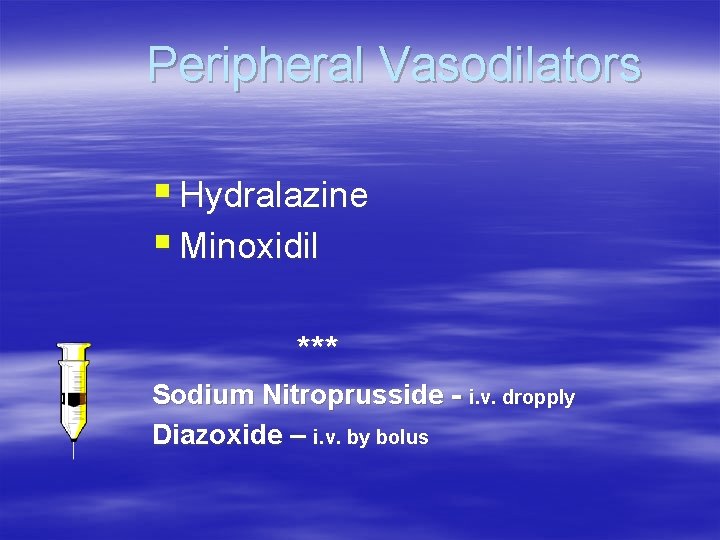
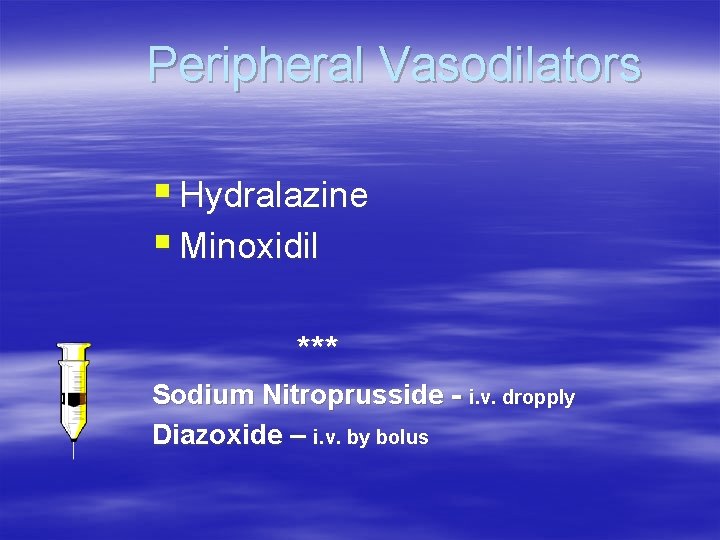
Peripheral Vasodilators § Hydralazine § Minoxidil *** Sodium Nitroprusside - i. v. dropply Diazoxide – i. v. by bolus
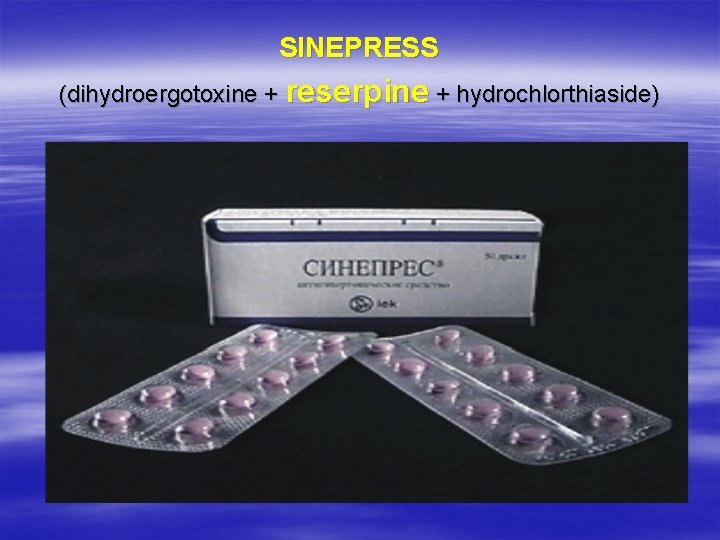
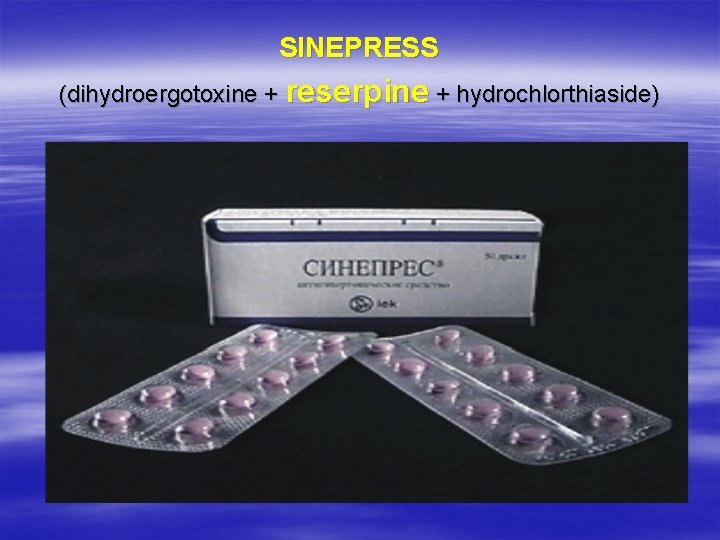
SINEPRESS (dihydroergotoxine + reserpine + hydrochlorthiaside)

TRIRESIDE (reserpine + hydralasine + hydrochlorothiaside)

CRISTEPIN (clopamide + dihydroergocristine + reserpine)
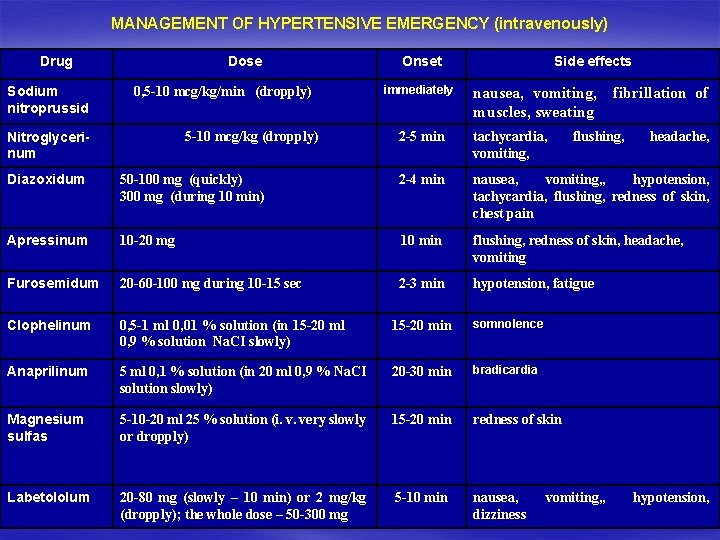
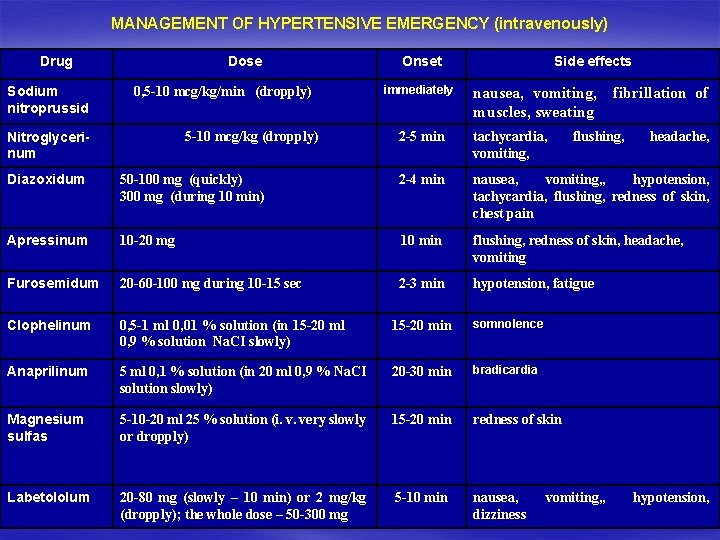
MANAGEMENT OF HYPERTENSIVE EMERGENCY (intravenously) Drug Sodium nitroprussid Dose 0, 5 -10 mcg/kg/min (dropply) Nitroglycerinum 5 -10 mcg/kg (dropply) Onset immediately Side effects nausea, vomiting, muscles, sweating 2 -5 min tachycardia, vomiting, fibrillation of flushing, headache, Diazoxidum 50 -100 mg (quickly) 300 mg (during 10 min) 2 -4 min nausea, vomiting, , hypotension, tachycardia, flushing, redness of skin, chest pain Apressinum 10 -20 mg 10 min flushing, redness of skin, headache, vomiting Furosemidum 20 -60 -100 mg during 10 -15 sec 2 -3 min hypotension, fatigue Clophelinum 0, 5 -1 ml 0, 01 % solution (in 15 -20 ml 0, 9 % solution Na. CI slowly) 15 -20 min somnolence Anaprilinum 5 ml 0, 1 % solution (in 20 ml 0, 9 % Na. CI solution slowly) 20 -30 min bradicardia Magnesium sulfas 5 -10 -20 ml 25 % solution (i. v. very slowly or dropply) 15 -20 min redness of skin Labetololum 20 -80 mg (slowly – 10 min) or 2 mg/kg (dropply); the whole dose – 50 -300 mg 5 -10 min nausea, dizziness vomiting, , hypotension,
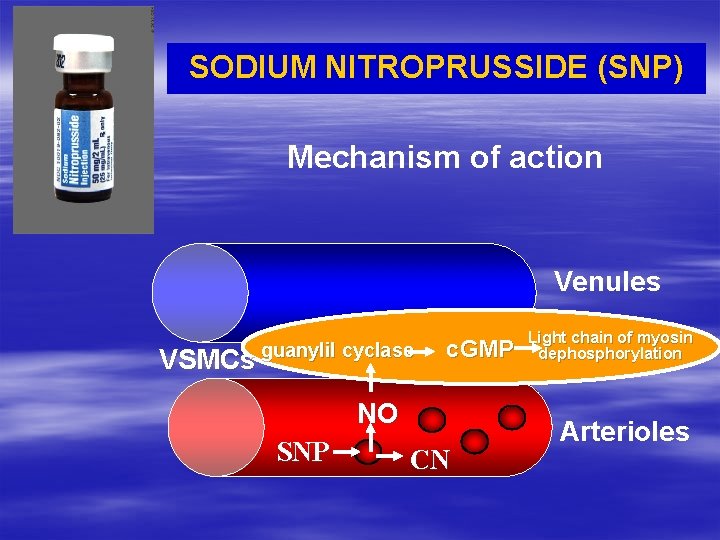
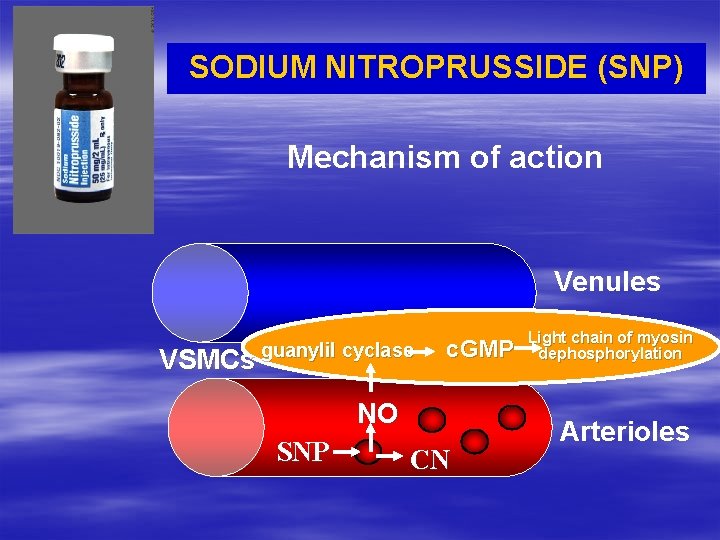
SODIUM NITROPRUSSIDE (SNP) Mechanism of action Venules VSMCs guanylil cyclase c. GMP NO SNP CN Light chain of myosin dephosphorylation Arterioles
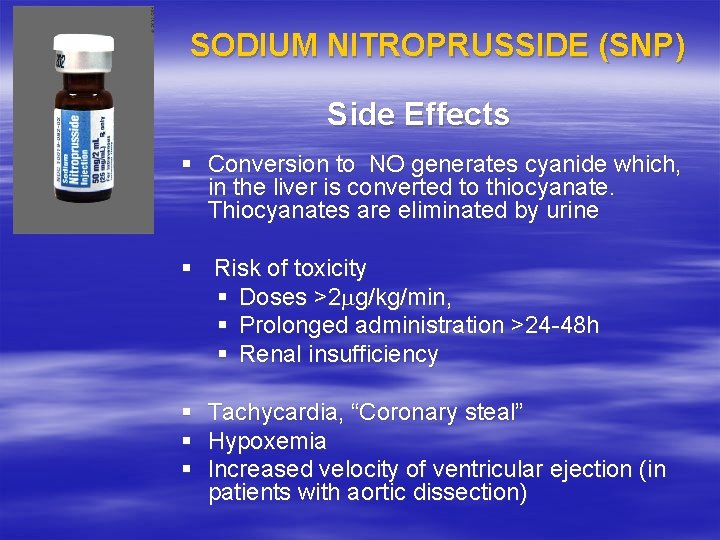
SODIUM NITROPRUSSIDE (SNP) Side Effects § Conversion to NO generates cyanide which, in the liver is converted to thiocyanate. Thiocyanates are eliminated by urine § Risk of toxicity § Doses >2 mg/kg/min, § Prolonged administration >24 -48 h § Renal insufficiency § § § Tachycardia, “Coronary steal” Hypoxemia Increased velocity of ventricular ejection (in patients with aortic dissection)
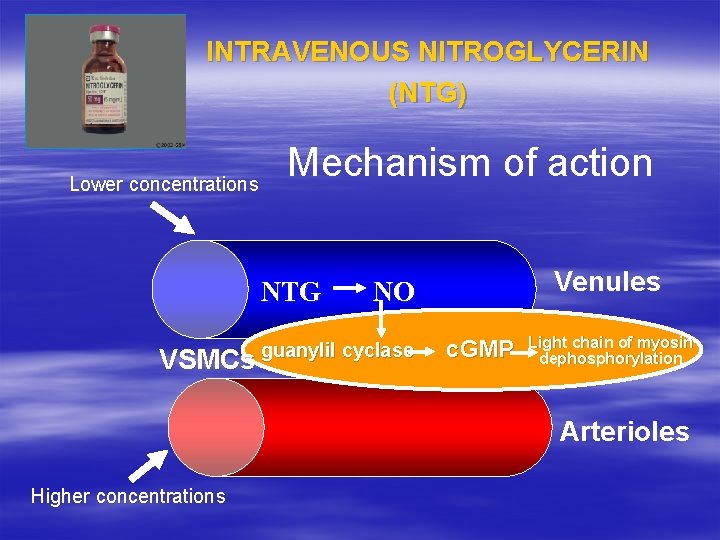
INTRAVENOUS NITROGLYCERIN (NTG) Lower concentrations Mechanism of action NTG VSMCs Venules NO guanylil cyclase c. GMP Light chain of myosin dephosphorylation Arterioles Higher concentrations
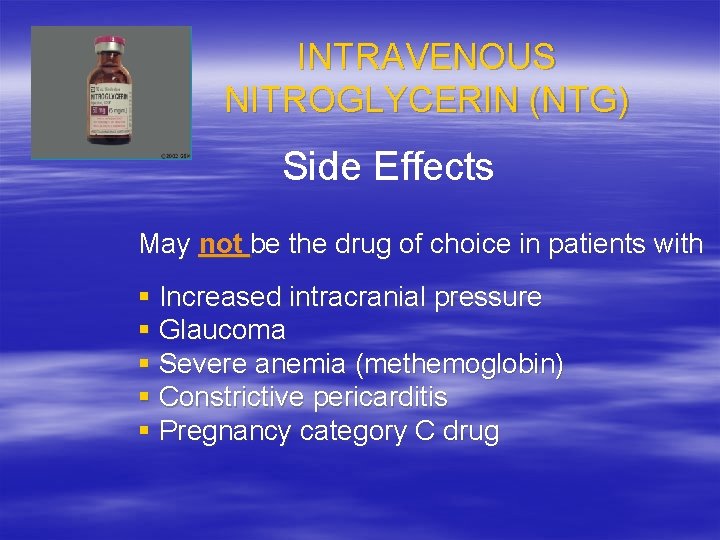
INTRAVENOUS NITROGLYCERIN (NTG) Side Effects May not be the drug of choice in patients with § Increased intracranial pressure § Glaucoma § Severe anemia (methemoglobin) § Constrictive pericarditis § Pregnancy category C drug
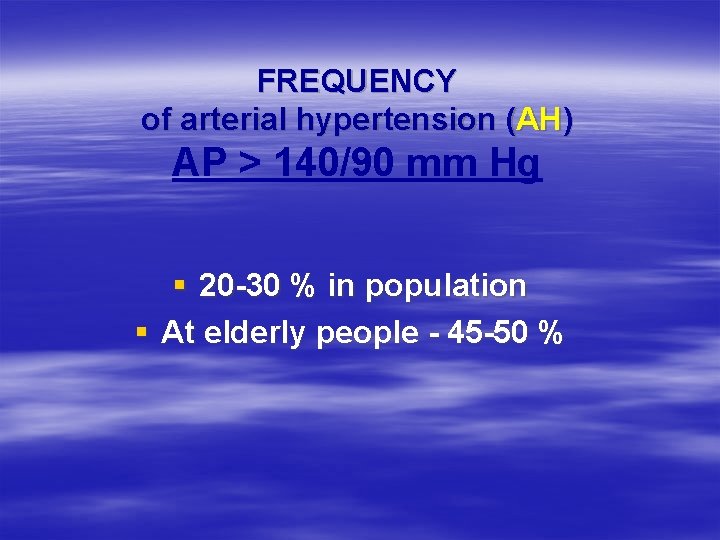
AGENTS GIVEN BY INTERMITTENT IV INJECTION § Labetalol § Enalaprilat § Hydralazine § Diazoxide
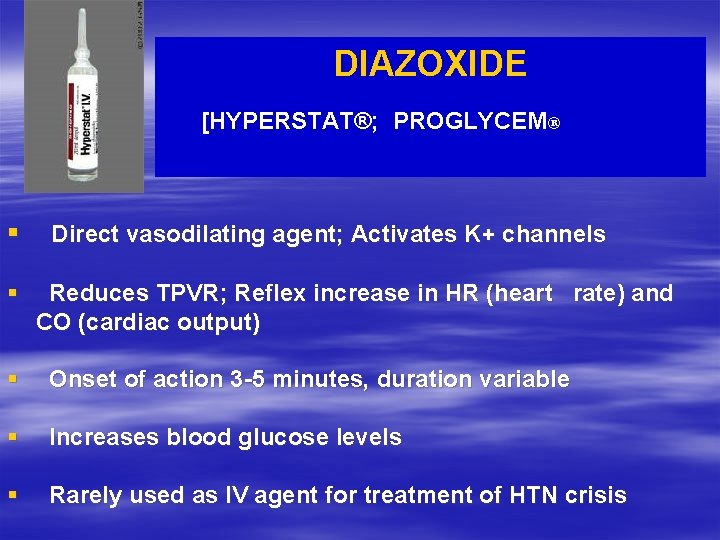
DIAZOXIDE [HYPERSTAT®; PROGLYCEM® § § Direct vasodilating agent; Activates K+ channels Reduces TPVR; Reflex increase in HR (heart rate) and CO (cardiac output) § Onset of action 3 -5 minutes, duration variable § Increases blood glucose levels § Rarely used as IV agent for treatment of HTN crisis
 Blood pressure medication dosage chart
Blood pressure medication dosage chart Antihypertensive drugs classification
Antihypertensive drugs classification Classification of antihypertensive drugs with examples
Classification of antihypertensive drugs with examples Classification of sympatholytic drugs
Classification of sympatholytic drugs Hypertension drugs
Hypertension drugs Antihypertensives classification
Antihypertensives classification Antihypertensive
Antihypertensive Vmax = aw
Vmax = aw Joint relative frequency
Joint relative frequency Relative frequency bar chart
Relative frequency bar chart Probability with relative frequency
Probability with relative frequency Marginal frequency table
Marginal frequency table Form factor and crest factor
Form factor and crest factor Marginal relative frequency
Marginal relative frequency Conclusion of hypertension
Conclusion of hypertension Pulmonary hypertension
Pulmonary hypertension Malignant hypertension management
Malignant hypertension management Definition of hypertension
Definition of hypertension Causes of secondary hypertension
Causes of secondary hypertension Stages of pulmonary hypertension
Stages of pulmonary hypertension Non pharmacological management of hypertension
Non pharmacological management of hypertension Dyslipidemia pathophysiology
Dyslipidemia pathophysiology Vital signs cpr
Vital signs cpr Conclusion of hypertension
Conclusion of hypertension Conclusion of hypertension
Conclusion of hypertension Mitral stenosis pulmonary hypertension
Mitral stenosis pulmonary hypertension Dr douglas simonetto
Dr douglas simonetto Hypertension artérielle
Hypertension artérielle Inokuchi shunt
Inokuchi shunt Hypertension
Hypertension Hypertensive urgency vs emergency
Hypertensive urgency vs emergency Pulmonary hypertension
Pulmonary hypertension Stage 1 hypertension
Stage 1 hypertension Intracranial hypertension
Intracranial hypertension Complications of cirrhosis
Complications of cirrhosis Pah vs pulmonary hypertension
Pah vs pulmonary hypertension Sohil rangwala
Sohil rangwala Diagnosis hypertension
Diagnosis hypertension Definition of hypertension
Definition of hypertension Dcld vs cld
Dcld vs cld Presinusoidal portal hypertension
Presinusoidal portal hypertension Pulmonary hypertension
Pulmonary hypertension Urgency hypertension
Urgency hypertension Hypertension
Hypertension Medical nutrition therapy for hypertension
Medical nutrition therapy for hypertension Pulmonary hypertension definition
Pulmonary hypertension definition Malignant hypertension treatment
Malignant hypertension treatment Amas faa medication
Amas faa medication Missed some points on the visual field test for dvla
Missed some points on the visual field test for dvla Nursing blood pressure assessment
Nursing blood pressure assessment Masked hypertension
Masked hypertension Isolated systolic hypertension
Isolated systolic hypertension Modifiable risk factors for hypertension
Modifiable risk factors for hypertension Nursing management of portal hypertension
Nursing management of portal hypertension Health coaches for hypertension control
Health coaches for hypertension control Hypertension
Hypertension Hypertensive emergency vs urgency
Hypertensive emergency vs urgency Conclusion of hypertension
Conclusion of hypertension Dash diet
Dash diet Jnc 8 classification of hypertension
Jnc 8 classification of hypertension Hematocrit
Hematocrit Hypertension vs hypotension
Hypertension vs hypotension Sachin gupta md
Sachin gupta md Demadex
Demadex Jnc 7 hypertension
Jnc 7 hypertension Case scenario for hypertension
Case scenario for hypertension Pico question examples hypertension
Pico question examples hypertension Ascites veins
Ascites veins Sbp179
Sbp179 Hypertension medical definition
Hypertension medical definition Pulmonary hypertension severity
Pulmonary hypertension severity