Advanced Cardiovascular Life Support American Heart Association Guidelines





















































- Slides: 98

Advanced Cardiovascular Life Support American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care 2015





CPR 1) Basic cardiac life support • compressions • • 2) • • • 3) • • Airway control Breathing Advance cardiac life support Drug and fluids Electrocardiography Fibrillation treatment Prolonged cardiac life support Human mentation Intensive care
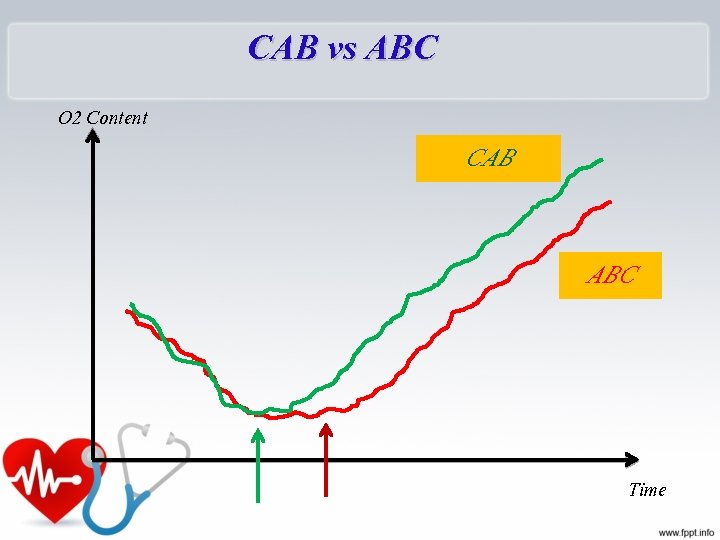
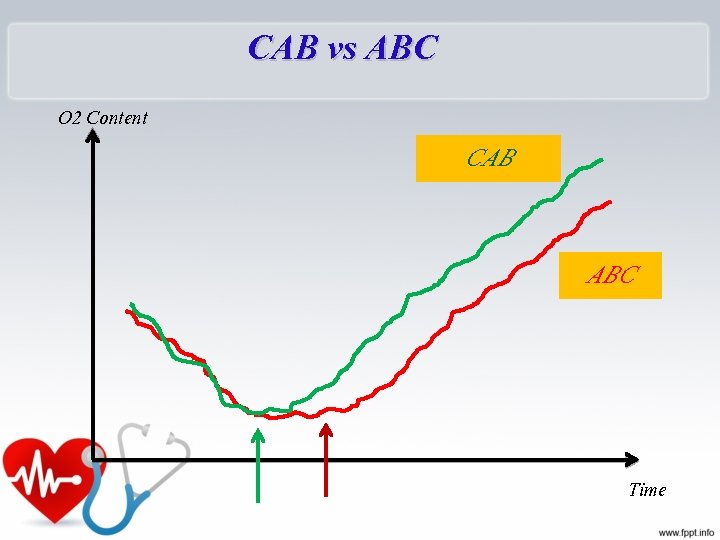
CAB vs ABC O 2 Content CAB ABC Time
Start CPR Immediately • Better chance of survival • Brain damage starts in 4 -6 minutes • Brain damage is certain after 10 minutes without CPR Provides O 2 to the brain until ACLS arrives
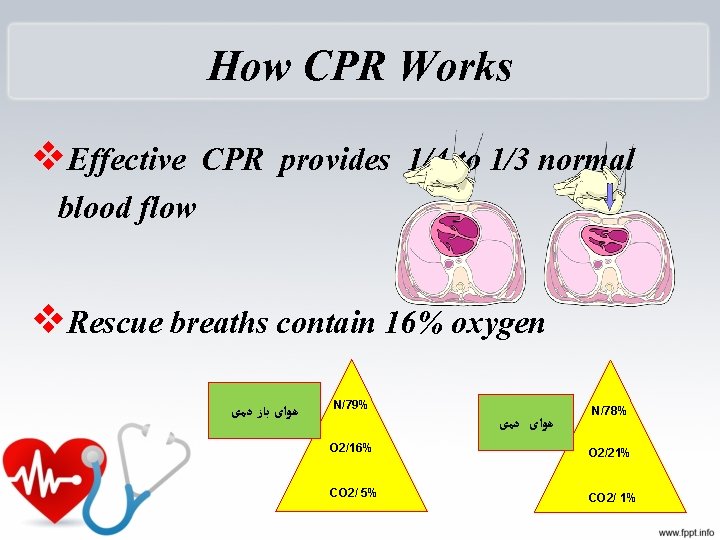
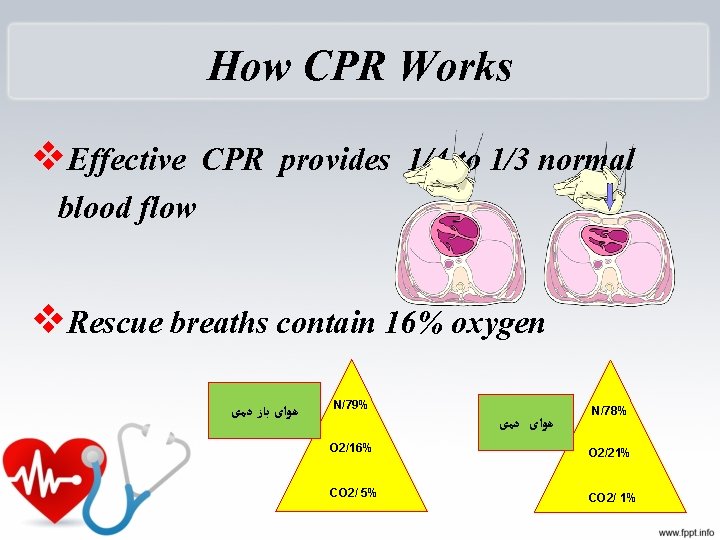
How CPR Works v. Effective CPR provides 1/4 to 1/3 normal blood flow v. Rescue breaths contain 16% oxygen ﻫﻮﺍی ﺑﺎﺯ ﺩﻣی N/79% ﻫﻮﺍی ﺩﻣی N/78% O 2/16% O 2/21% CO 2/ 5% CO 2/ 1%
Do Not Move the Victim Until CPR is Given and Qualified Help Arrives… Ø unless the scene dictates otherwise vthreat of fire or explosion vvictim must be on a hard surface v. Place victim level or head slightly lower than body
Survey The Scene, then: R. A. P • R - Responsiveness – Tap shoulder and shout “Are you ok? ”
R. A. P • A - Activate EMS 115 OR
R. A. P • P - Position on back – All body parts rolled over at the same time • Always be aware of head and spinal cord injuries • Support neck and spinal column
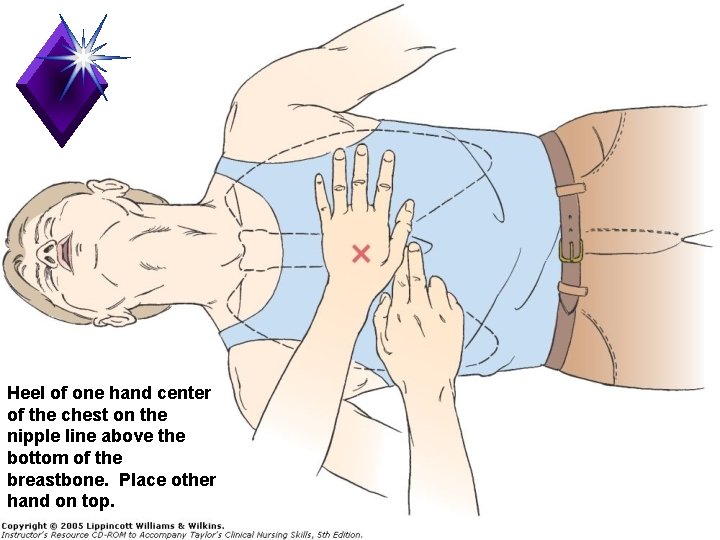
Compressions q. Locate proper hand position for chest compressions q. Place heel of one hand on center of chest between the nipples
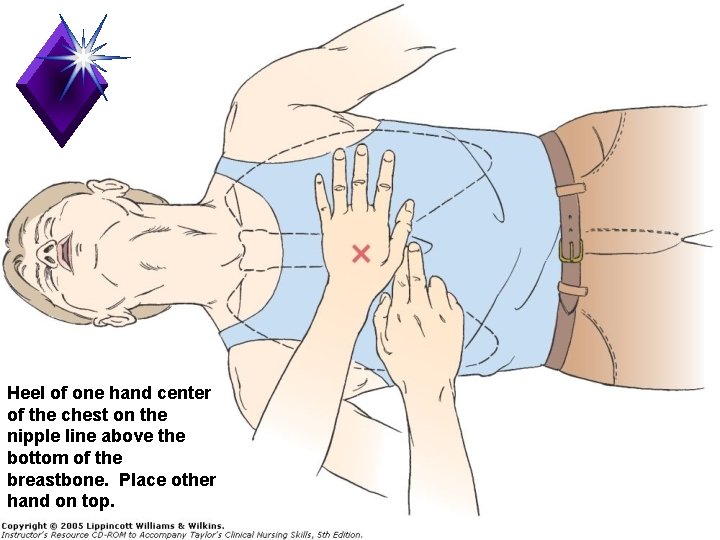
Heel of one hand center of the chest on the nipple line above the bottom of the breastbone. Place other hand on top.



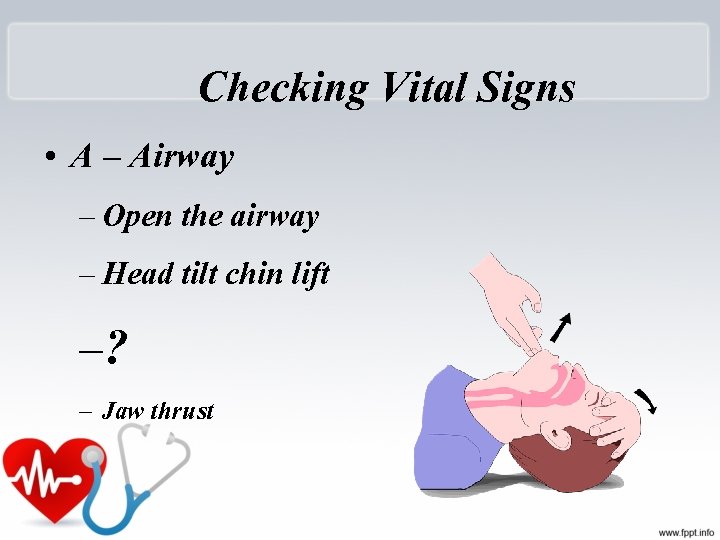
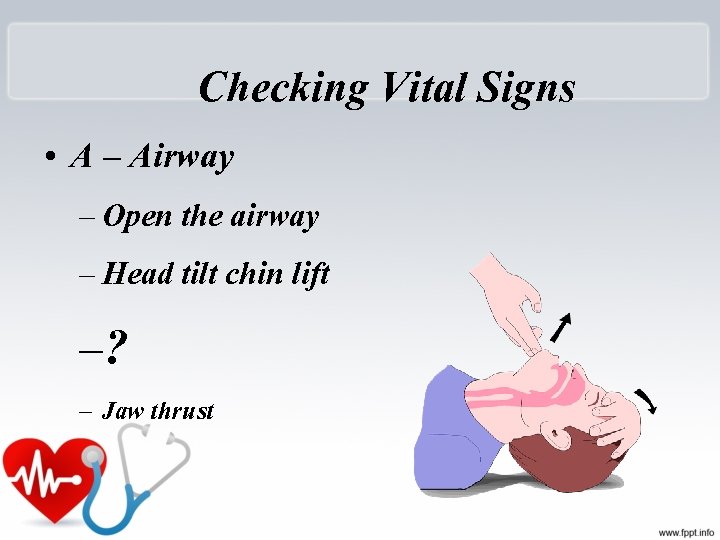
Checking Vital Signs • A – Airway – Open the airway – Head tilt chin lift –? – Jaw thrust

Jaw-thrust maneuver

Head tilt- chin lift maneuver
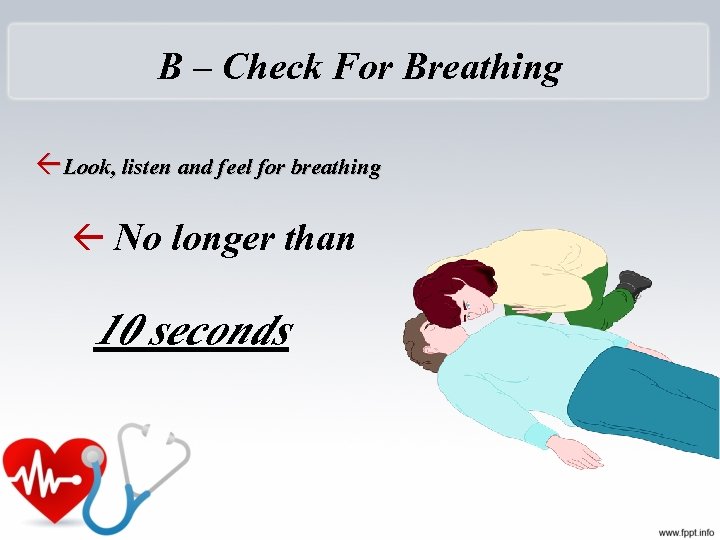
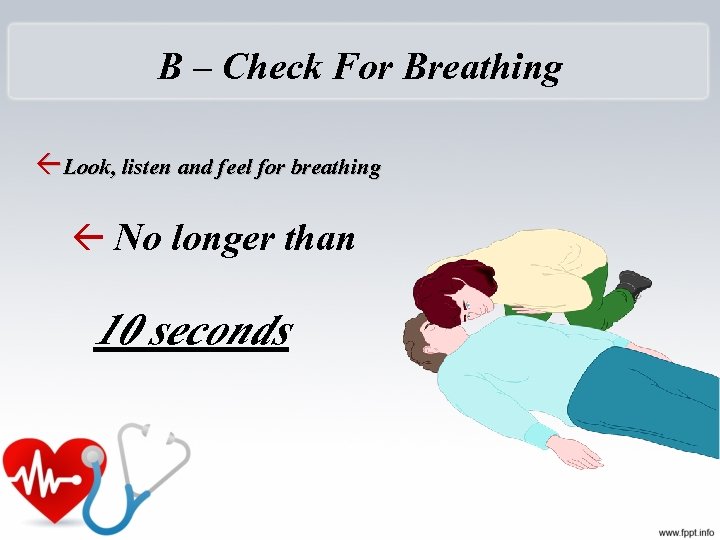
B – Check For Breathing Look, listen and feel for breathing No longer than 10 seconds
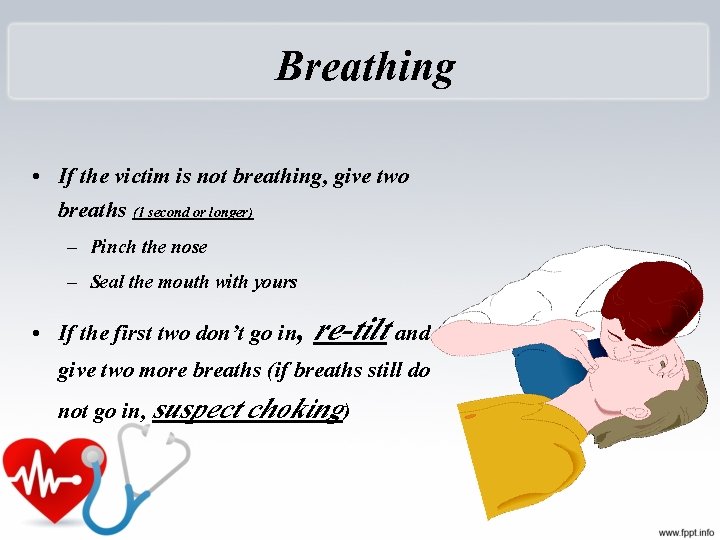
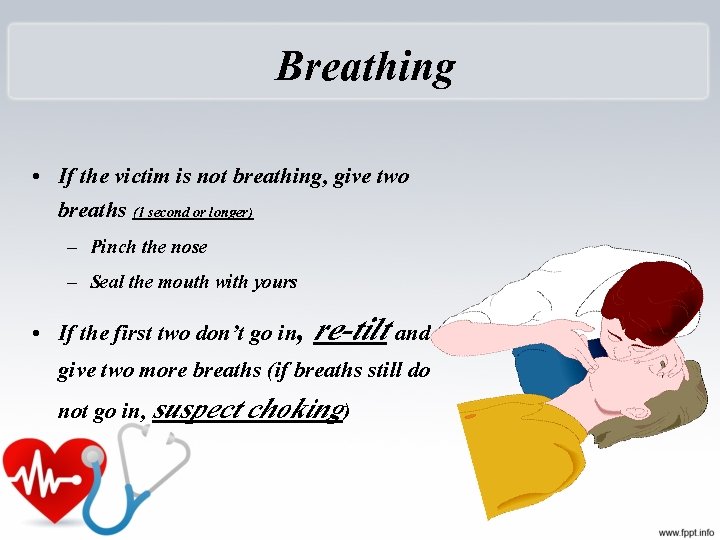
Breathing • If the victim is not breathing, give two breaths (1 second or longer) – Pinch the nose – Seal the mouth with yours • If the first two don’t go in, re-tilt and give two more breaths (if breaths still do not go in, suspect choking)
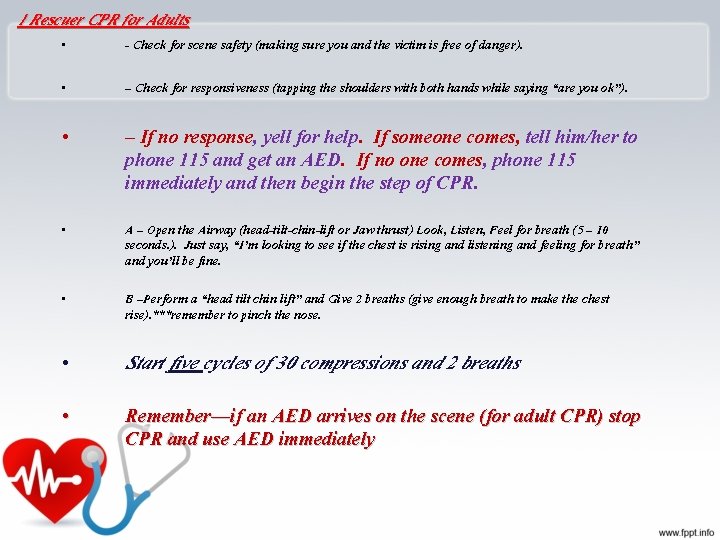
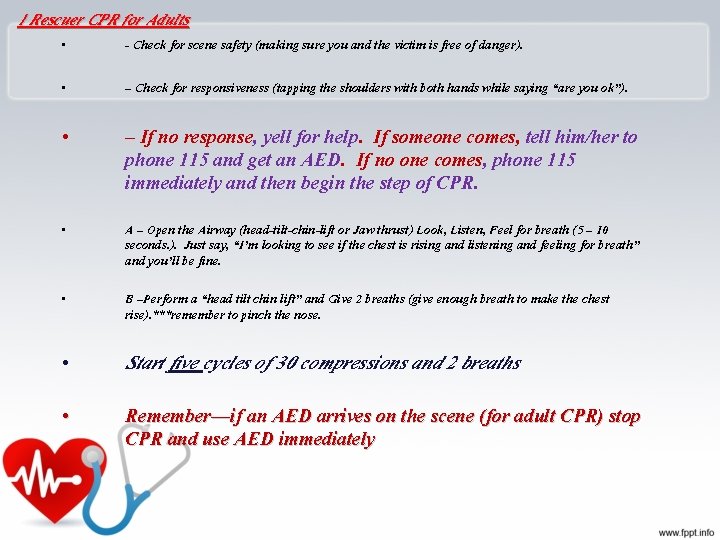
1 Rescuer CPR for Adults • - Check for scene safety (making sure you and the victim is free of danger). • – Check for responsiveness (tapping the shoulders with both hands while saying “are you ok”). • – If no response, yell for help. If someone comes, tell him/her to phone 115 and get an AED. If no one comes, phone 115 immediately and then begin the step of CPR. • A – Open the Airway (head-tilt-chin-lift or Jaw thrust) Look, Listen, Feel for breath (5 – 10 seconds. ). Just say, “I’m looking to see if the chest is rising and listening and feeling for breath” and you’ll be fine. • B –Perform a “head tilt chin lift” and Give 2 breaths (give enough breath to make the chest rise). ***remember to pinch the nose. • Start five cycles of 30 compressions and 2 breaths • Remember—if an AED arrives on the scene (for adult CPR) stop CPR and use AED immediately
Injuries Related to CPR • Rib fractures • Laceration related to the tip of the sternum – Liver, lung, spleen
Stomach Distension




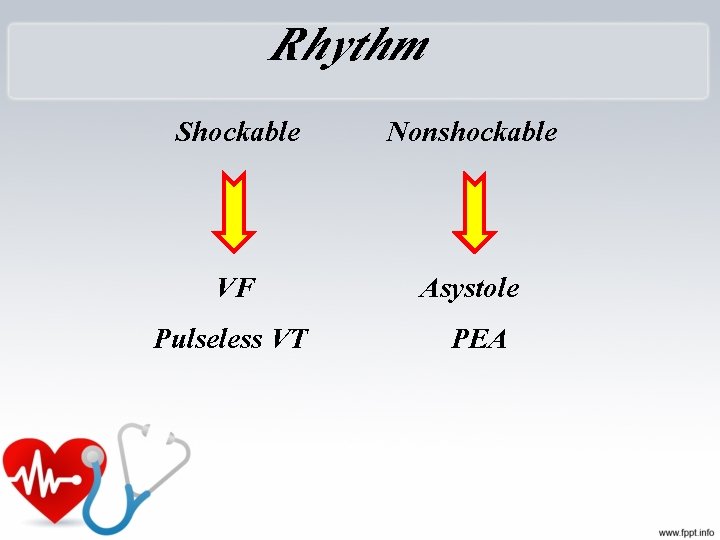
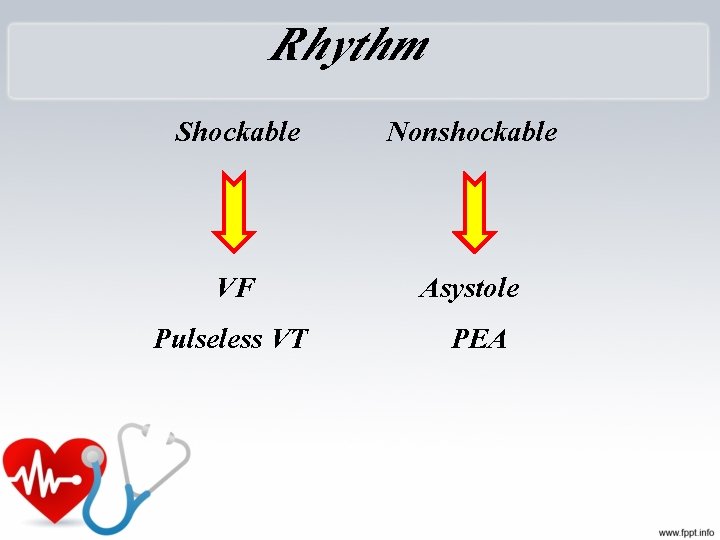
Rhythm Shockable Nonshockable VF Pulseless VT Asystole PEA
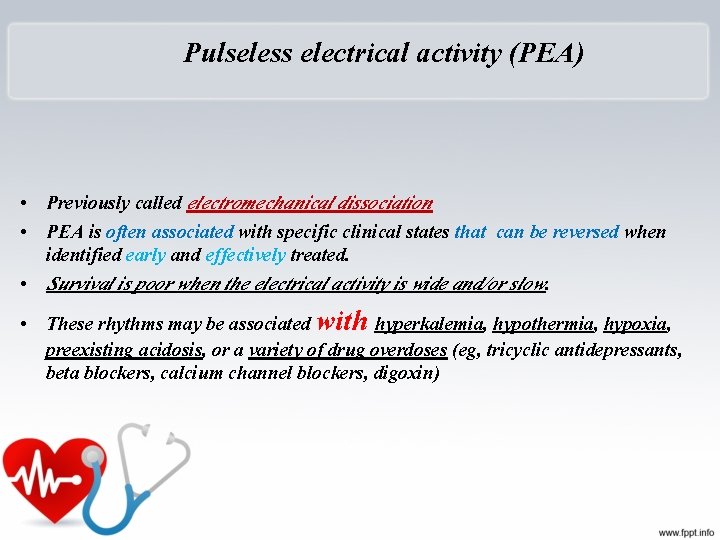
Pulseless electrical activity (PEA) • Previously called electromechanical dissociation • PEA is often associated with specific clinical states that can be reversed when identified early and effectively treated. • Survival is poor when the electrical activity is wide and/or slow. • These rhythms may be associated with hyperkalemia, hypothermia, hypoxia, preexisting acidosis, or a variety of drug overdoses (eg, tricyclic antidepressants, beta blockers, calcium channel blockers, digoxin)
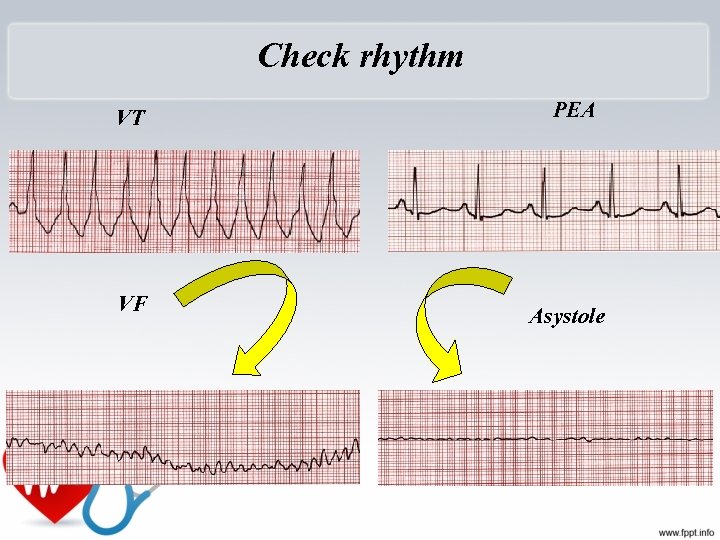
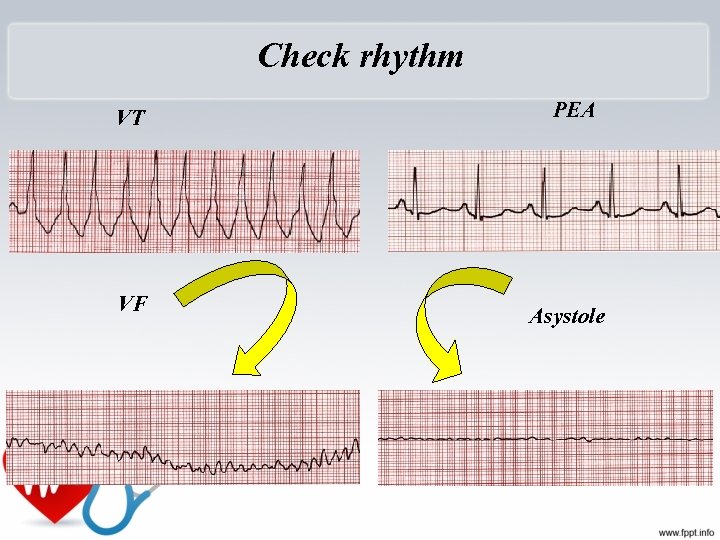
Check rhythm VT PEA VF Asystole
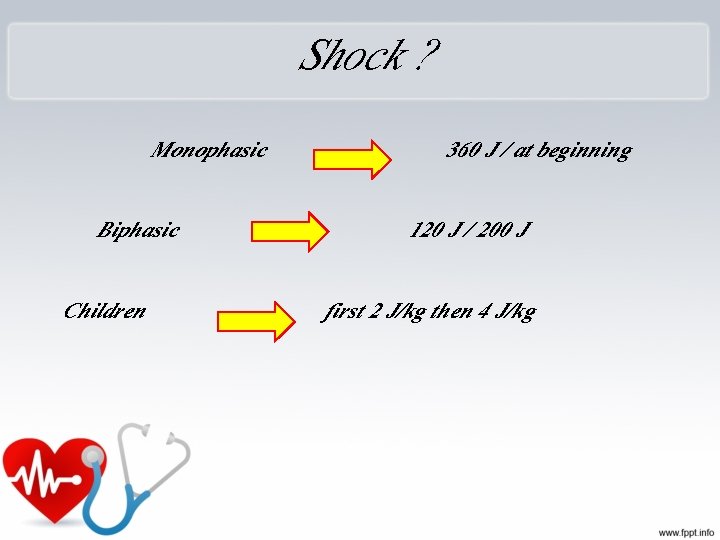
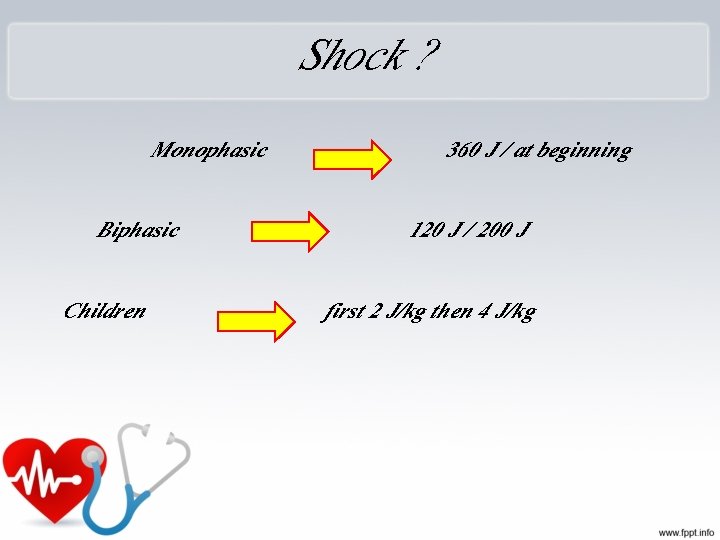
Shock ? Monophasic Biphasic Children 360 J / at beginning 120 J / 200 J first 2 J/kg then 4 J/kg


Do not check pulse until The rhythm changed


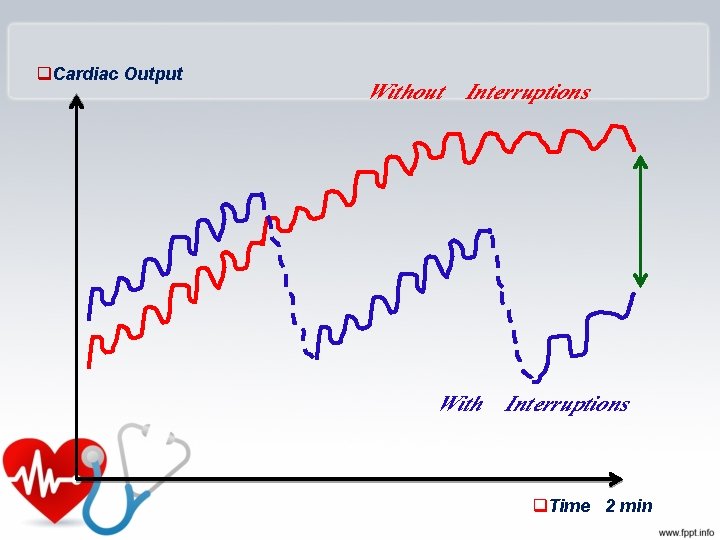
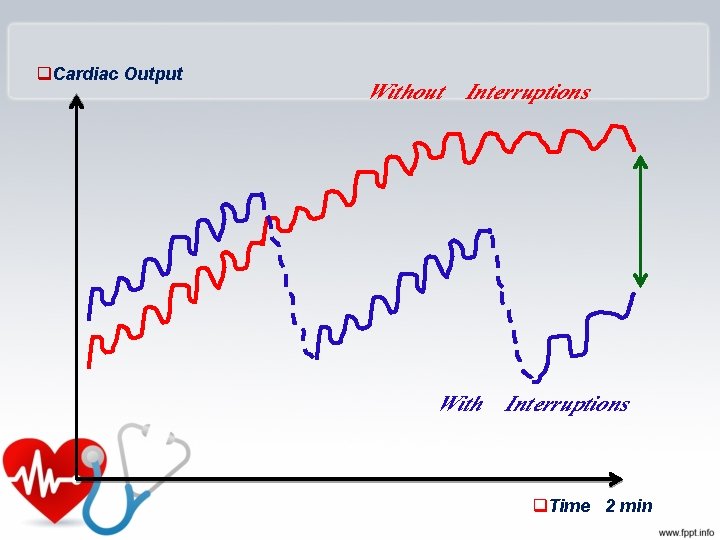
q. Cardiac Output Without Interruptions With Interruptions q. Time 2 min


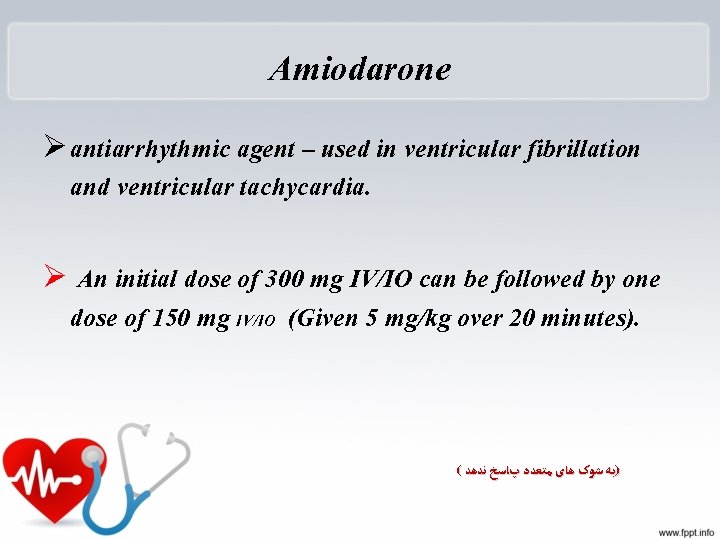
Amiodarone Ø antiarrhythmic agent – used in ventricular fibrillation and ventricular tachycardia. Ø An initial dose of 300 mg IV/IO can be followed by one dose of 150 mg IV/IO (Given 5 mg/kg over 20 minutes). ( )ﺑﻪ ﺷﻮک ﻫﺎی ﻣﺘﻌﺪﺩ پﺎﺳﺦ ﻧﺪﻫﺪ
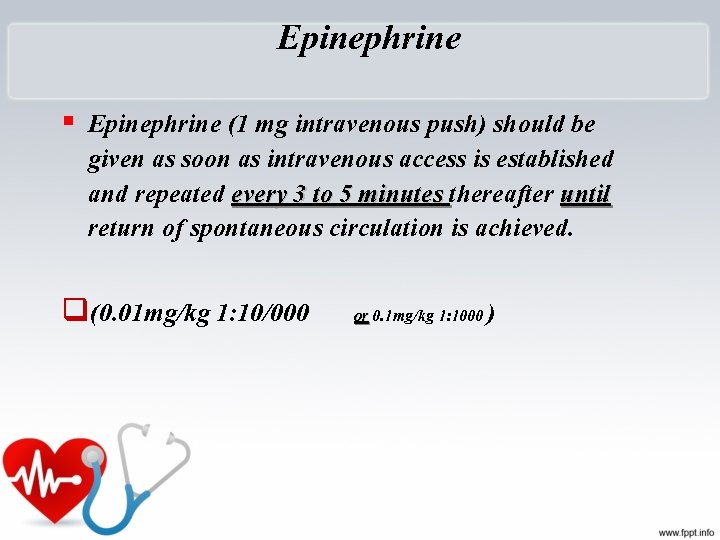
Epinephrine § Epinephrine (1 mg intravenous push) should be given as soon as intravenous access is established and repeated every 3 to 5 minutes thereafter until return of spontaneous circulation is achieved. q(0. 01 mg/kg 1: 10/000 or 0. 1 mg/kg 1: 1000 )

Oxygen Therapy • “Generally speaking”, a patient who is breathing less than 12 and more than 24 times a minute needs oxygen 47
Lidocaine • Lidocaine can be used as an alternative to amiodarone, but should not be administered if amiodarone has already been given. • Lidocaine is administered at a dose of 1 mg/kg as an intravenous push and can be repeated every 3 to 5 minutes; it should not exceed a total dose of 3 mg/kg during the first hour. آﺴﺘﺎﻧﻪ ﻓیﺒﺮیﻼﺳیﻮﻥ ﺩﺭ ﻗﻠﺐ ﺭﺍ ﺑﺎﻻ ﻣی ﺑﺮﺩ. • ﻋﻤﺪﺗ ﺭﻭی ﺑﻄﻦ ﻫﺎ ﻣﻮﺛﺮ ﺍﺳﺖ ﺍﺛﺮ VF ﻭﻟی ﺩﺭ ﺧﻮﺩ. ﺟﻠﻮگیﺮی ﻣی کﻨﺪ VF ﺑﻨﺎﺑﺮﺍیﻦ ﺍﺯ ﺗکﺮﺍﺭ ﺩﻭﺭﻩ ﻫﺎی . ﻧﻤی کﻨﺪ

P. E. A

Sodium bicarbonate • Sodium bicarbonate (1 meq/kg) has a role in the treatment of PEA (or) due to specific causes: • preexisting hyperkalemia • preexisting bicarbonate-responsive acidosis • treatment of tricyclic antidepressant overdose • alkalinize the urine in aspirin or other drug overdoses.
Sodium bicarbonate • It is not routinely used for acute lactic acidosis associated with CPR, but may be considered if the initial interventions (defibrillation, ventilation, cardiac compression, and vasopressor therapy) have been ineffective. • ? ? The use of bicarbonate is acceptable in intubated and ventilated patients with a long arrest interval or upon return of circulation after a long arrest interval; however, there is only fair evidence for its efficacy in these settings. • The use of bicarbonate is harmful and not indicated for respiratory acidosis (hypercapnic).




Drug As a law: Drugs injections in CPR must be: PUSH ETT administration: 2 - 2. 5 times as IV doses plus 5 -10 ml distilled water

E T route: q. Lidocaine q. Epinephrine q Atropine q. Naloxone q Vasopressin VALEN
peripheral venous route: 1. Follow with a 20 ml bolus of IV fluid. 2. Elevate the extremity for 10 to 20 seconds to facilitate drug delivery to the central circulation.




Resuscitation of the Pregnant Patient
Key Points Ø During resuscitation there are two patients, mother & fetus ØThe best hope of fetal survival is maternal survival Ø Consider the physiologic changes due to pregnancy

Manual left uterine displacement by the 1 -handed technique from the right of the patient during adult resuscitation. Farida M. Jeejeebhoy et al. Circulation. 2015; 132: 1747 -1773 Copyright © American Heart Association, Inc. All rights reserved.

automated external defibrillator AED
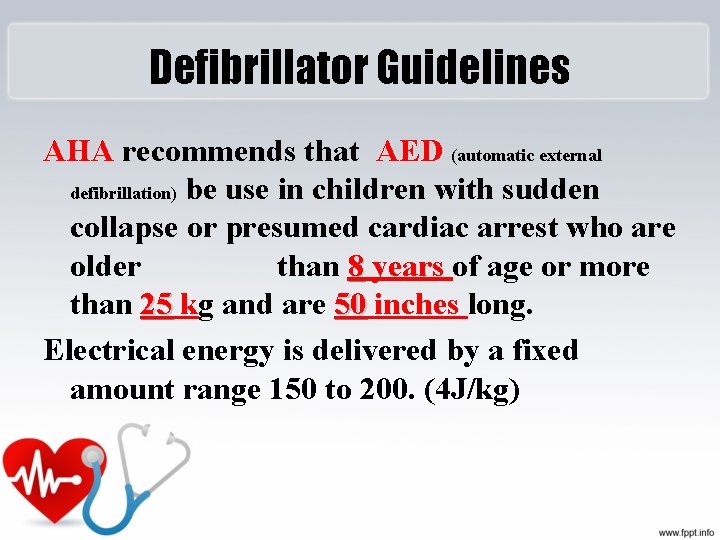
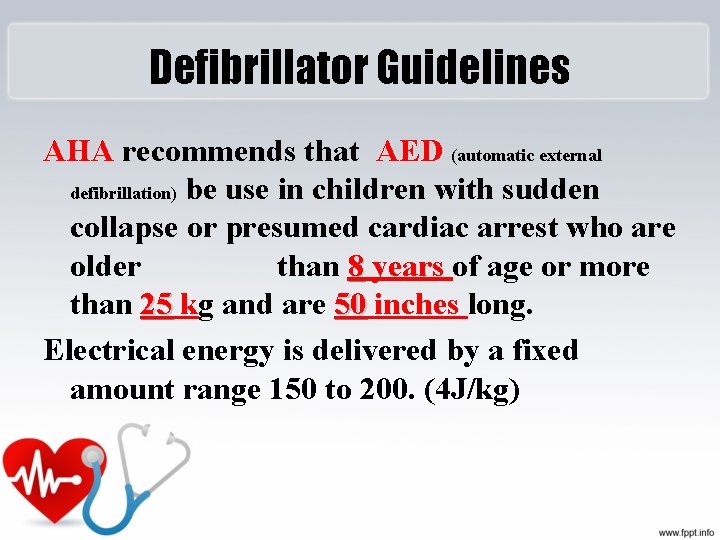
Defibrillator Guidelines AHA recommends that AED (automatic external defibrillation) be use in children with sudden collapse or presumed cardiac arrest who are older than 8 years of age or more than 25 kg and are 50 inches long. Electrical energy is delivered by a fixed amount range 150 to 200. (4 J/kg)
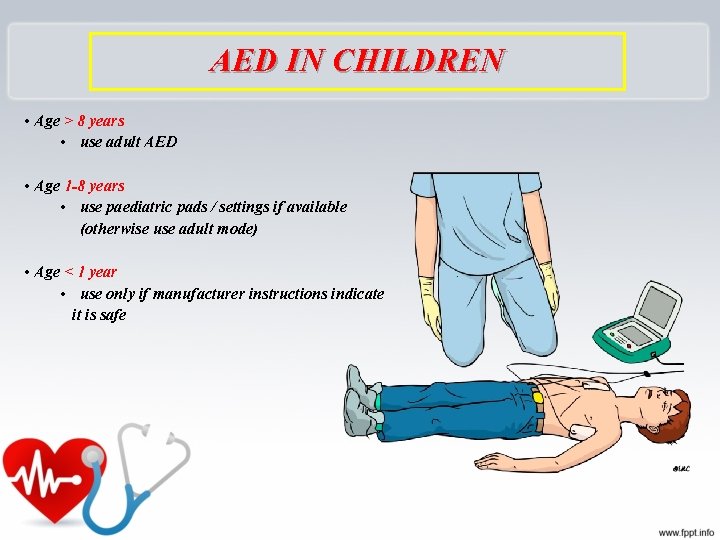
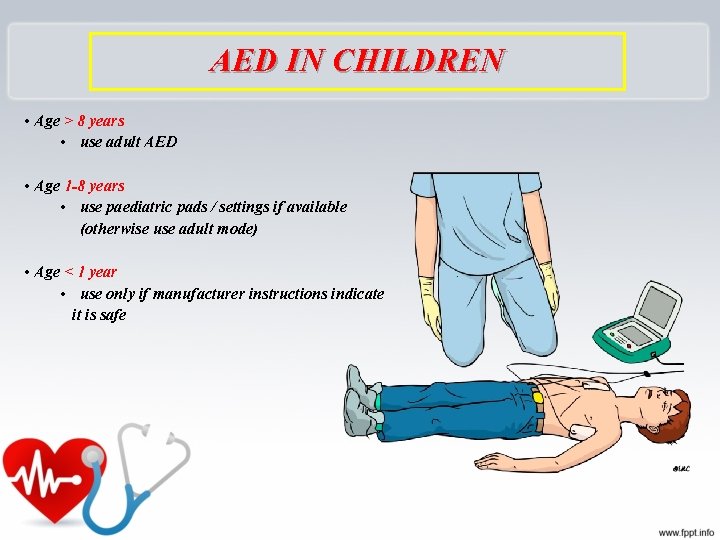
AED IN CHILDREN • Age > 8 years • use adult AED • Age 1 -8 years • use paediatric pads / settings if available (otherwise use adult mode) • Age < 1 year • use only if manufacturer instructions indicate it is safe







Pediatric CPR * child(1 -8 y) CPR * Infant(<1 y) CPR
Cardiac Arrest • Pediatric cardiac arrest is: – Uncommon – Rarely sudden cardiac arrest caused by primary cardiac arrhythmias. – Most often asphyxial, resulting from the progression of respiratory failure or shock or both.
Impending Respiratory Failure • RR <10 or >60 is an ominous sign of impending respiratory failure. Prearrest. s
Circulatory Assessment • HR is the most sensitive parameter for determining perfusion and oxygenation in children. (<3 Y) – Heart rate needs to be at least 60 beats per minute to provide adequate perfusion. NEONATE – HR > 140 beats per minute at rest needs to be evaluated.



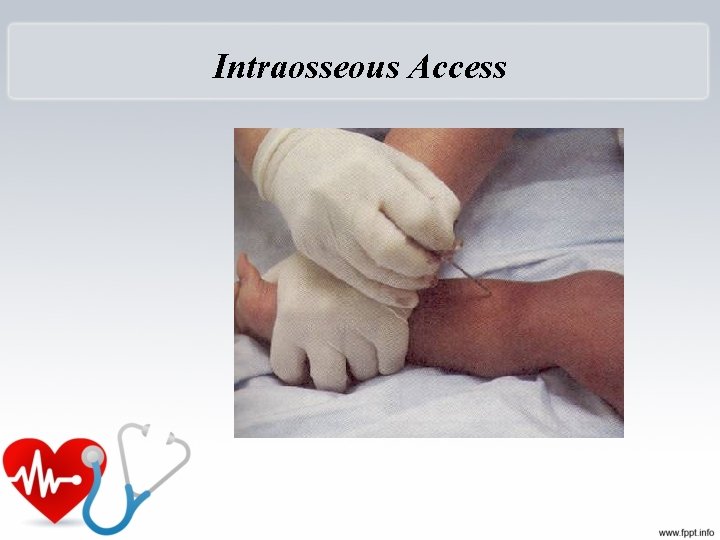
Vascular Access – New Guidelines • New guidelines: in children who are six years or younger after 90 seconds or 3 attempts at peripheral intravenous access – Intraosseous access recommended.
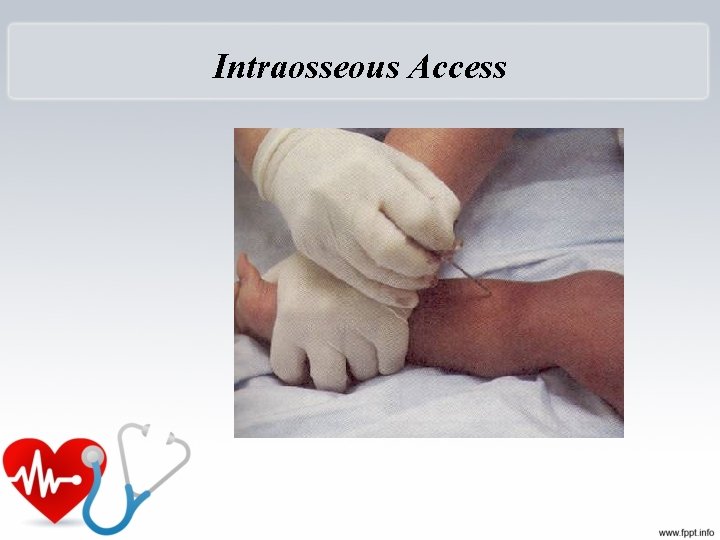
Intraosseous Access
Gastric Decompression • Gastric decompression with a nasogastric or oral gastric tube is necessary to ensure maximum ventilation. – Air trapped in stomach can put pressure on the diaphragm impeding adequate ventilation. – Undigested food can lead to aspiration.

Title • Text
The END







extracorporeal membrane oxygenation (ECMO) or extracorporeal life support (ECLS) In intensive care medicine, extracorporeal membrane oxygenation (ECMO) or extracorporeal life support (ECLS) is an extracorporeal technique of providing both cardiac and respiratory support to persons whose heart and lungs are unable to provide an adequate amount of gas exchange to sustain life. This intervention has mostly been used on children, but it is seeing more use in adults with cardiac and respiratory failure. ECMO works by removing blood from the persons body and artificially removing the carbon dioxide and oxygenating red blood cells. Generally it is only used in the later treatment of a person with heart or lung failure as it is solely a life-sustaining intervention. type There are several forms of ECMO, the two most common of which are the veno-arterial (VA) and veno-venous (VV). In both modalities, blood drained from the venous system is oxygenated outside of the body. In VA ECMO, this blood is returned to the arterial system and in VV ECMO the blood is returned to the venous system. In VV ECMO, no cardiac support is provided. Veno-arterial (VA) In veno-arterial ECMO – a venous cannula is usually placed in the right common femoral vein for extraction and an arterial cannula is usually placed into the right femoral artery for infusion. [2] The tip of the femoral venous cannula should be maintained near the junction of the inferior vena cava and right atrium, while the tip of the femoral arterial cannula is maintained in the iliac artery. [2] In adults accessing the femoral artery is preferred because the insertion is simpler. [2] Central VA ECMO may be used if cardiopulmonary bypass has already been established (with cannulae in the right atrium and ascending aorta)
Synchronized cardioversion • is a LOW ENERGY SHOCK that uses a sensor to deliver electricity that is synchronized with the peak of the QRS complex (the highest point of the R-wave). When the “sync” option is engaged on a defibrillator and the shock button pushed, there will be a delay in the shock. During this delay, the machine reads and synchronizes with the patients ECG rhythm. This occurs so that the shock can be delivered with or just after the peak of the R-wave in the patients QRS complex. Synchronization avoids the delivery of a LOW ENERGY shock during cardiac repolarization (t-wave). If the shock occurs on the t-wave (during repolarization), there is a high likelihood that the shock can precipitate VF (Ventricular Fibrillation). • The most common indications for synchronized cardioversion are unstable atrial fibrillation, atrial flutter, atrial tachycardia, and supraventricular tachycardias. If medications fail in the stable patient with the before mentioned arrhythmias, synchronized cardioversion will most likely be indicated.
Unsynchronized cardioversion (defibrillation) • is a HIGH ENERGY shock which is delivered as soon as the shock button is pushed on a defibrillator. This means that the shock may fall randomly anywhere within the cardiac cycle (QRS complex). Unsynchronized cardioversion (defibrillation) is used when there is no coordinated intrinsic electrical activity in the heart (pulseless VT/VF) or the defibrillator fails to synchronize in an unstable patient. For cases where electrical shock is needed, if the patient is stable and you can see a QRS-t complex use (LOW ENERGY) synchronized cardioversion. If the patient is pulseless, or if the patient is unstable and the defibrillator will not synchronize, use (HIGH ENERGY) unsynchronized cardioversion (defibrillation).
 Battiti ectopici ventricolari forum
Battiti ectopici ventricolari forum American thyroid association guidelines pregnancy 2017
American thyroid association guidelines pregnancy 2017 Unresponsive child cpr
Unresponsive child cpr Aha cpr in schools training kit
Aha cpr in schools training kit American heart association 2020
American heart association 2020 Jnc 8 hypertension classification
Jnc 8 hypertension classification American heart association
American heart association Advanced life support
Advanced life support American board of cardiovascular medicine
American board of cardiovascular medicine Arizona child support guidelines 2020
Arizona child support guidelines 2020 Host nation support guidelines
Host nation support guidelines Association analysis advanced concepts
Association analysis advanced concepts Association analysis advanced concepts
Association analysis advanced concepts Association analysis advanced concepts
Association analysis advanced concepts Association analysis advanced concepts
Association analysis advanced concepts Association analysis advanced concepts
Association analysis advanced concepts Association rules in data mining
Association rules in data mining Association analysis advanced concepts
Association analysis advanced concepts Major and minor supporting details examples
Major and minor supporting details examples Ceds certification salary
Ceds certification salary National tribal child support association
National tribal child support association Cardiac dullness
Cardiac dullness Sheep heart labeled
Sheep heart labeled Heart 2 heart
Heart 2 heart Swedish american heart hospital rockford illinois
Swedish american heart hospital rockford illinois American researcher who involved in getting heart rate
American researcher who involved in getting heart rate Tlups
Tlups Starts new page numbered sequentially
Starts new page numbered sequentially American galvanizers association inc
American galvanizers association inc American marketing association definition brand
American marketing association definition brand American berkshire association
American berkshire association American baking association
American baking association How to do in text citation apa
How to do in text citation apa Style apa adalah
Style apa adalah Apa image caption
Apa image caption American alzheimer's association
American alzheimer's association The miller test
The miller test New york mental health counselors association
New york mental health counselors association North american gaming regulators association
North american gaming regulators association North american association for environmental education
North american association for environmental education American library association
American library association American pyrotechnics association
American pyrotechnics association American psychiatric association annual meeting 2020
American psychiatric association annual meeting 2020 American association on health and disability
American association on health and disability Aaa gestation calculator
Aaa gestation calculator American gas association
American gas association Mobile baptist association
Mobile baptist association American college of private physicians
American college of private physicians Psychiatric nurse conference
Psychiatric nurse conference American association on health and disability
American association on health and disability Cuban american association of civil engineers
Cuban american association of civil engineers American association of caregiving youth
American association of caregiving youth American statistical association salary survey
American statistical association salary survey Donmeg developments
Donmeg developments American association of continuing medical education
American association of continuing medical education Oak schuetz
Oak schuetz Gelbvieh.org
Gelbvieh.org Lcm particle analyser
Lcm particle analyser American marketing association
American marketing association American burn association clasificacion de quemaduras
American burn association clasificacion de quemaduras Pemasaran menurut american marketing association
Pemasaran menurut american marketing association Vancouver bibliography
Vancouver bibliography Journal of american medical informatics association
Journal of american medical informatics association American psichological association
American psichological association American bar association rule of law initiative
American bar association rule of law initiative Venous blood
Venous blood Riesgo cardiovascular por perimetro abdominal
Riesgo cardiovascular por perimetro abdominal Soplo protosistolico
Soplo protosistolico What makes up the circulatory system
What makes up the circulatory system Rias hipertension arterial
Rias hipertension arterial Pithed rat meaning
Pithed rat meaning National cardiovascular partners
National cardiovascular partners Cardiovascular/lymphatic system it's totally tubular
Cardiovascular/lymphatic system it's totally tubular Cardiovascular drift
Cardiovascular drift Blood vessels crash course
Blood vessels crash course Cengage chapter 5
Cengage chapter 5 Chapter 46 the child with a cardiovascular alteration
Chapter 46 the child with a cardiovascular alteration The child with a cardiovascular disorder chapter 26
The child with a cardiovascular disorder chapter 26 Chapter 25 assessment of cardiovascular function
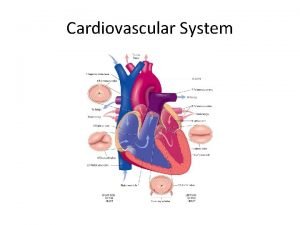
Chapter 25 assessment of cardiovascular function Chapter 11 the cardiovascular system figure 11-3
Chapter 11 the cardiovascular system figure 11-3 Figure 11-12 is a diagram of a capillary bed
Figure 11-12 is a diagram of a capillary bed Chapter 11 the cardiovascular system
Chapter 11 the cardiovascular system Lesson 11 cardiovascular system
Lesson 11 cardiovascular system Centro cardiovascular
Centro cardiovascular The circulatory system includes
The circulatory system includes Hypertensive atherosclerotic cardiovascular disease
Hypertensive atherosclerotic cardiovascular disease Características de los vasos sanguíneos
Características de los vasos sanguíneos Isgemiese hartsiekte
Isgemiese hartsiekte Introduction of heart
Introduction of heart Halimbawa ng cardiovascular endurance
Halimbawa ng cardiovascular endurance Stent placement
Stent placement Salud cardiovascular
Salud cardiovascular Components of physical fitness grade 7
Components of physical fitness grade 7 Salud cardiovascular
Salud cardiovascular Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Cuestionario aha/acsm
Cuestionario aha/acsm Cardiovascular system diseases and disorders chapter 8
Cardiovascular system diseases and disorders chapter 8 Chapter 7 cardiovascular fitness
Chapter 7 cardiovascular fitness Chapter 17 cardiovascular emergencies
Chapter 17 cardiovascular emergencies