American Heart Association Guidelines for CPR 2015 Wanida



- Slides: 49
American Heart Association Guidelines for CPR 2015 Wanida Chongarunngamsang, MD. Faculty of Srinakarinwirot University
American Heart Association Guidelines for CPR 2015 • BLS • ACLS – Pulseless Arrest – Bradycardia – Tachycardia • Post cardiac arrest care
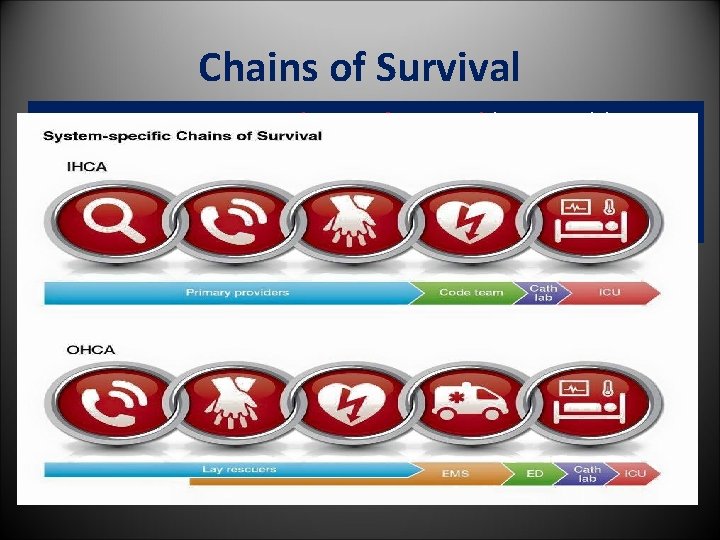
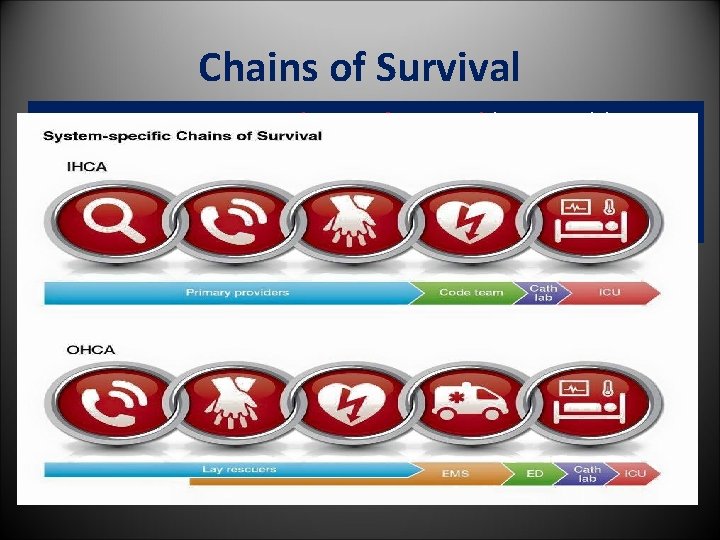
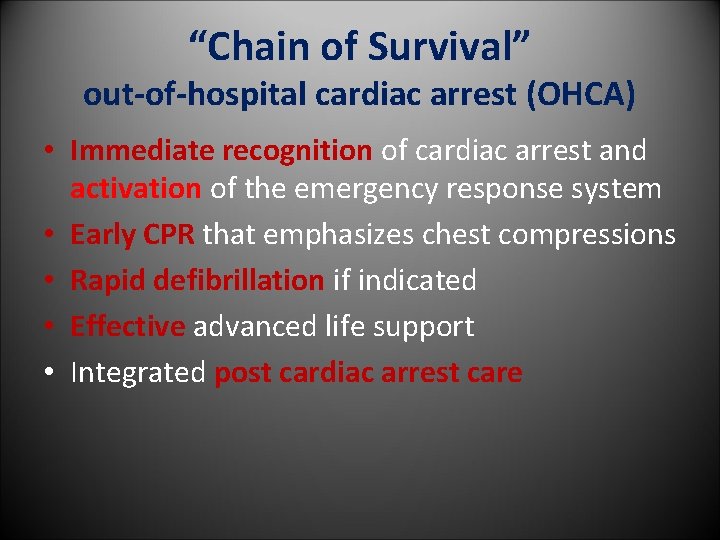
Chains of Survival 2015 (New): Separate Chains of Survival (Figure 4) have been recommended that identify the different pathways of care for patients who experience cardiac arrest in the hospital as distinct from out-of-hospital settings
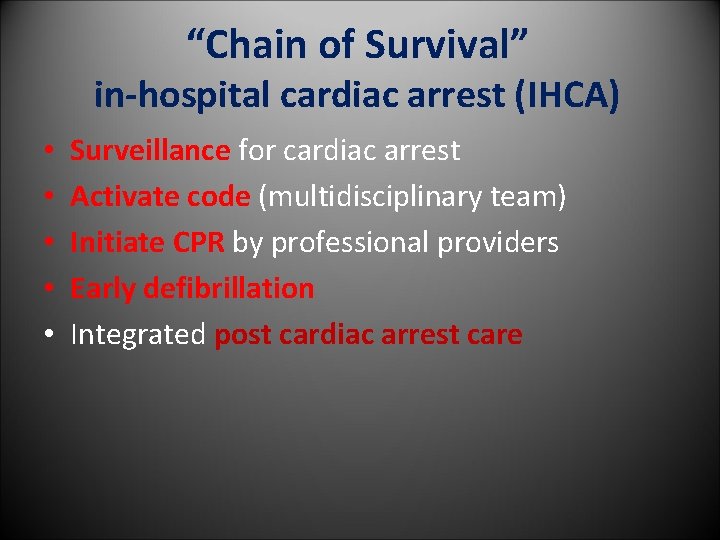
“Chain of Survival” in-hospital cardiac arrest (IHCA) • • • Surveillance for cardiac arrest Activate code (multidisciplinary team) Initiate CPR by professional providers Early defibrillation Integrated post cardiac arrest care
“Chain of Survival” out-of-hospital cardiac arrest (OHCA) • Immediate recognition of cardiac arrest and activation of the emergency response system • Early CPR that emphasizes chest compressions • Rapid defibrillation if indicated • Effective advanced life support • Integrated post cardiac arrest care

Adult Basic Life Support (BLS)
Basic Life Support – Used for patients with life-threatening illness or injury before the patient can be given full medical care. – Generally used in the pre-hospital setting, and can be provided without medical equipment. – Generally does not include the use of drugs or invasive skills. .
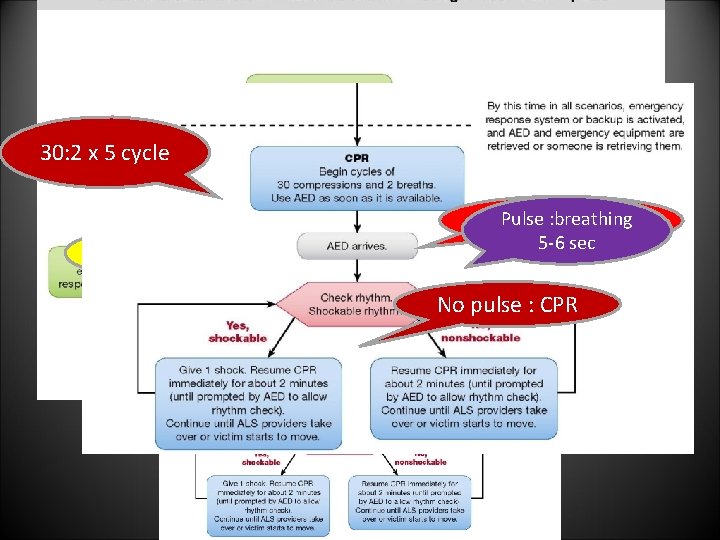
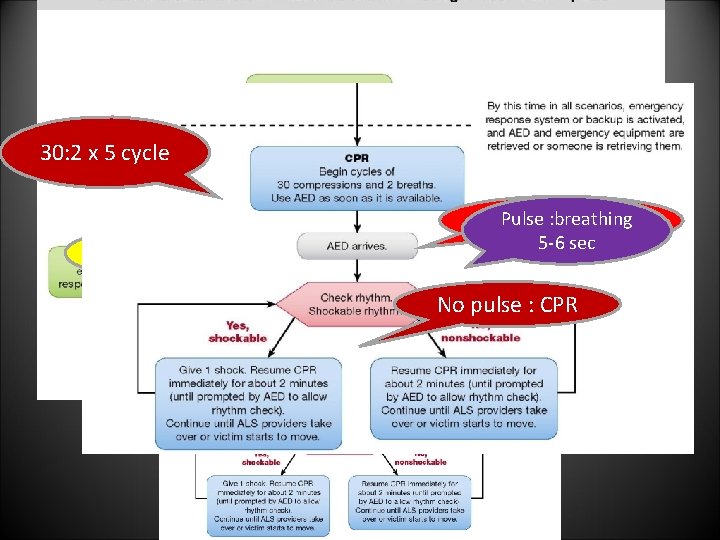
30: 2 x 5 cycle Breathing and pulse unresponsesive Pulse : breathing Call for help and AED 5 -6 sec No pulse : CPR
The BLS Survey includes four steps: • • The BLS survey is the starting point for all ACLS management Check for a response Call for help and to bring an AED Check circulation Check rhythm
The Primary Assessment uses the ABCDE model • Airway – Use the least advanced airway possible to maintain the airway and oxygenation • Breathing – Monitor tube placement and oxygenation using waveform capnography • Circulation – Medications, CPR, fluids and defibrillation • Differential Diagnosis –treat reversible causes • Disability- neurological assessment “AVPU”(Alert, Voice, Painful, Unresponsive) • Exposure - looking for signs of trauma, bleeding, burns, or medical alert bracelets
The Secondary Assessment • The secondary assessment includes a search for underlying causes for the emergency and if possible a focused medical history “SAMPLE’ • (S)Signs and symptoms • (A)Allergies • (M)Medications • (P)Past Illnesses • (L)Last Oral Intake • (E)Events Leading Up To Present Illness
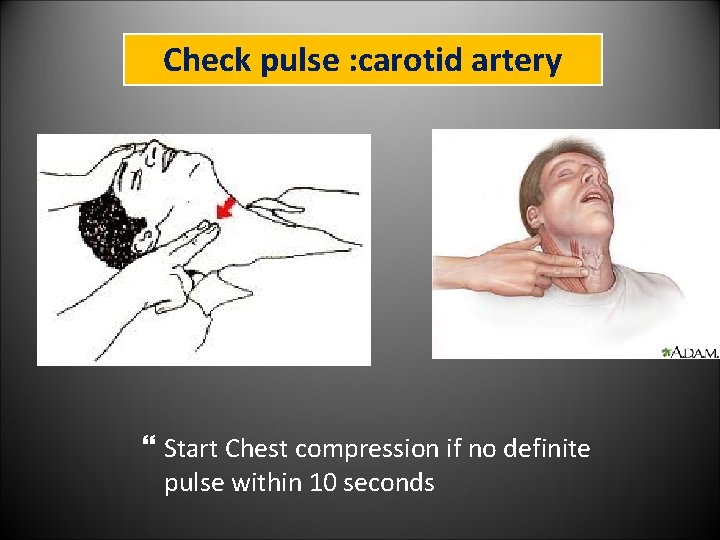
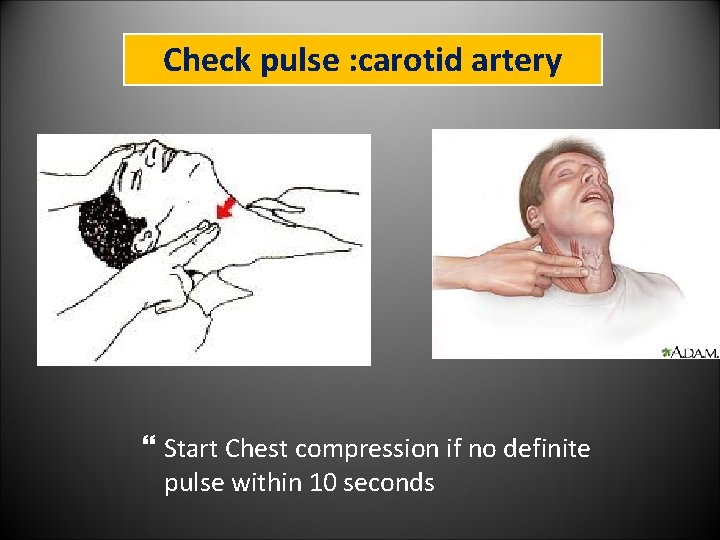
Check pulse : carotid artery Start Chest compression if no definite pulse within 10 seconds
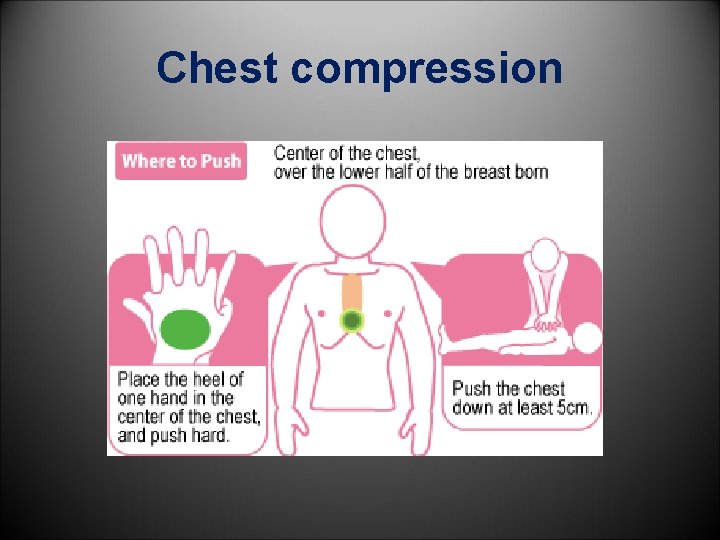
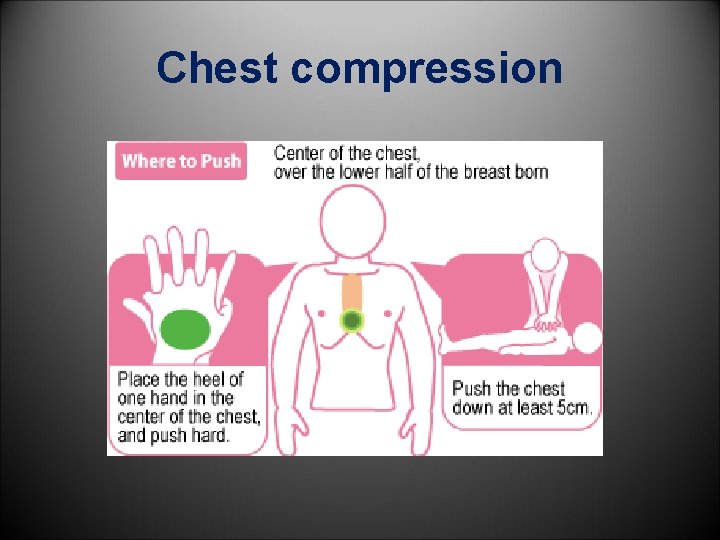
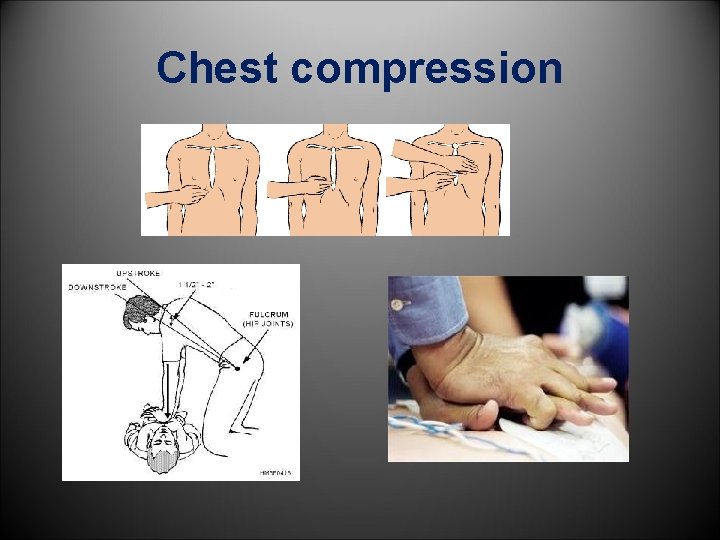
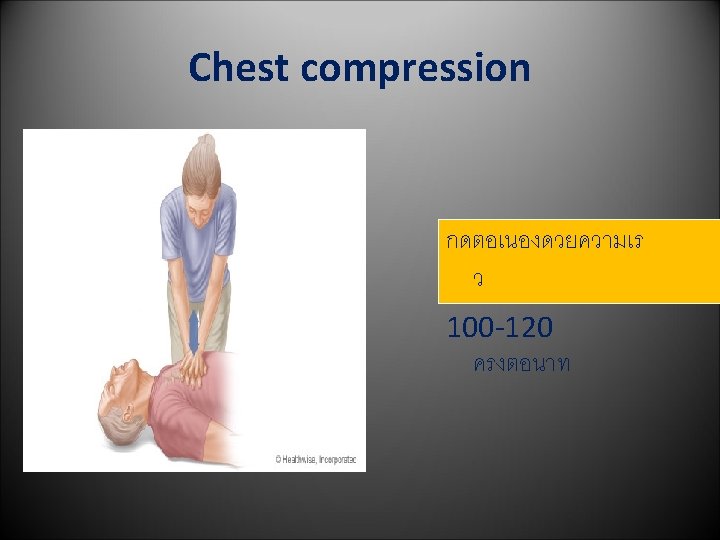
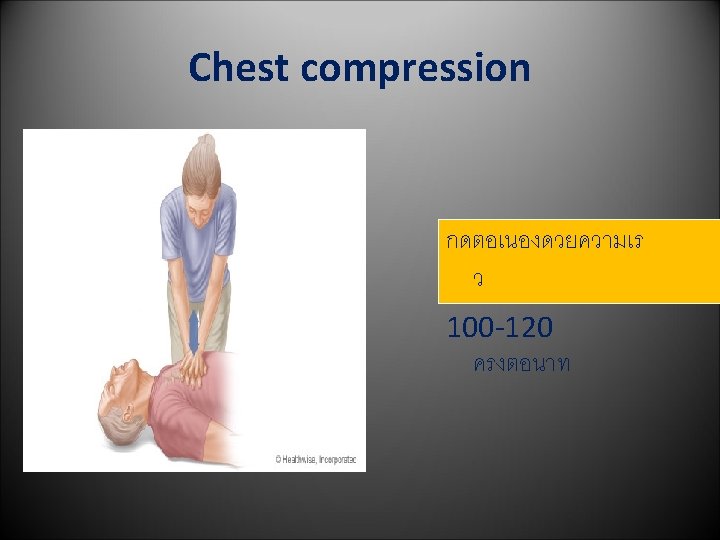
Chest compression
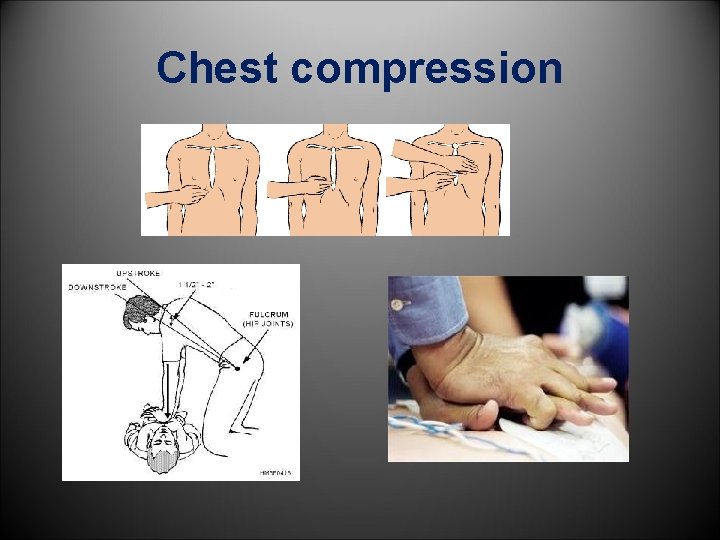
Chest compression
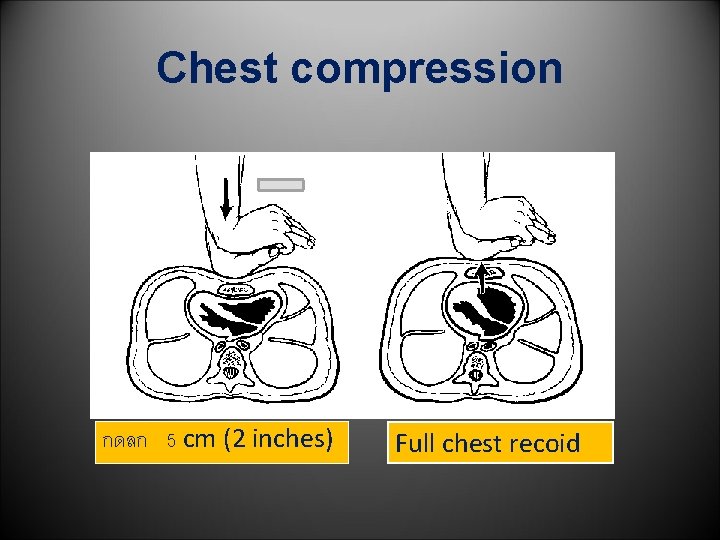
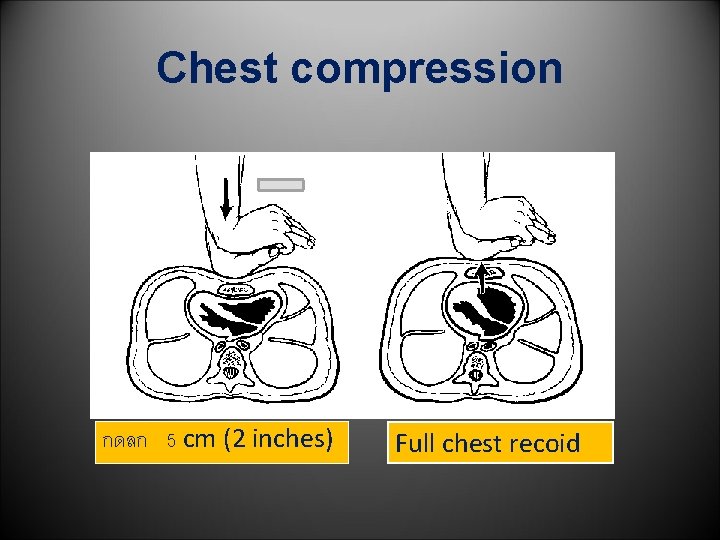
Chest compression กดลก 5 cm (2 inches) Full chest recoid
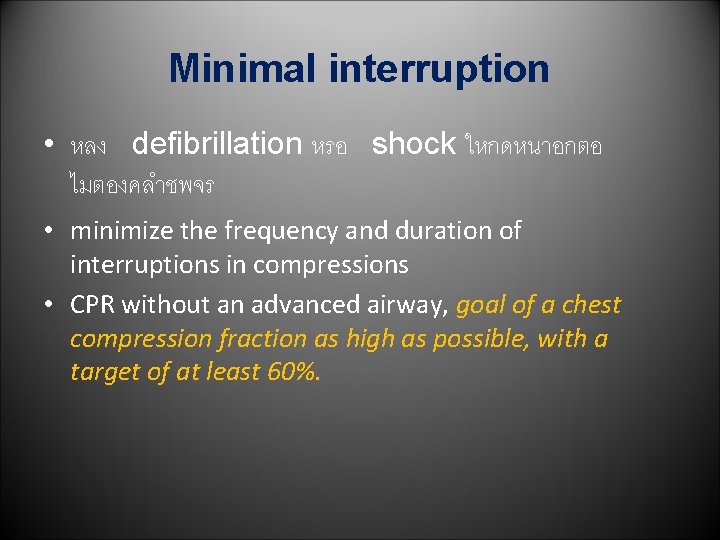
Minimal interruption • หลง defibrillation หรอ shock ใหกดหนาอกตอ ไมตองคลำชพจร • minimize the frequency and duration of interruptions in compressions • CPR without an advanced airway, goal of a chest compression fraction as high as possible, with a target of at least 60%.
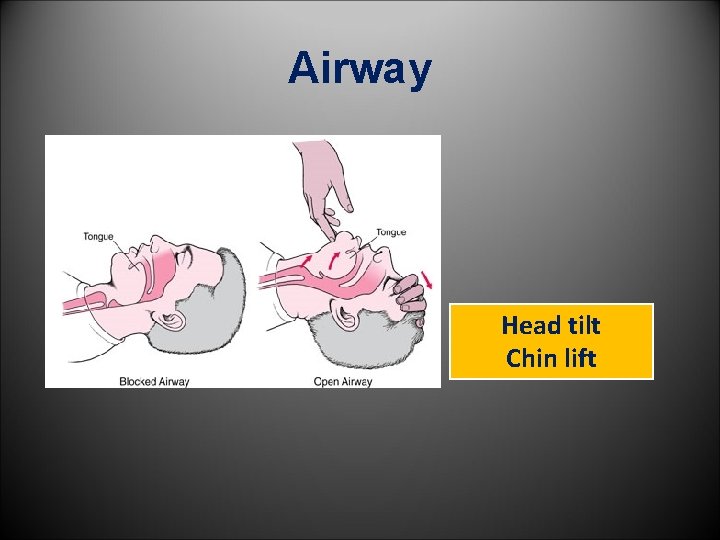
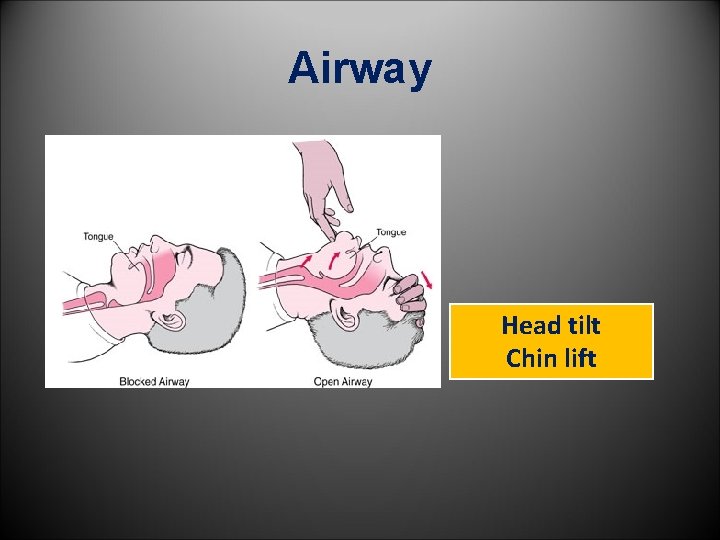
Airway Head tilt Chin lift
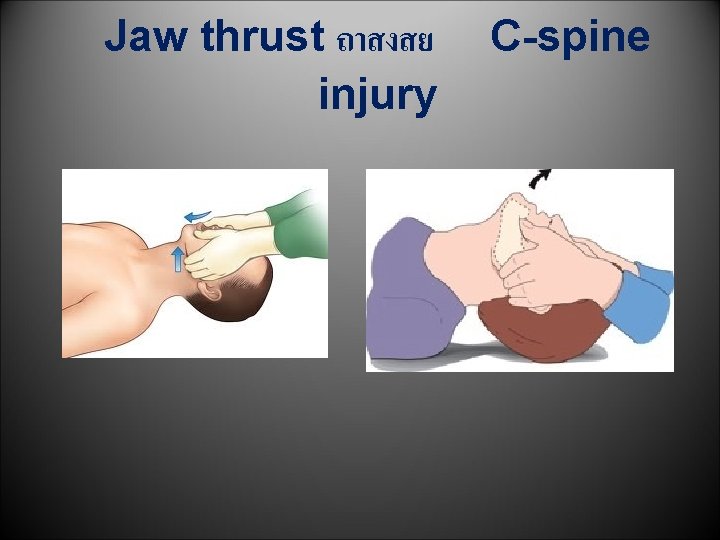
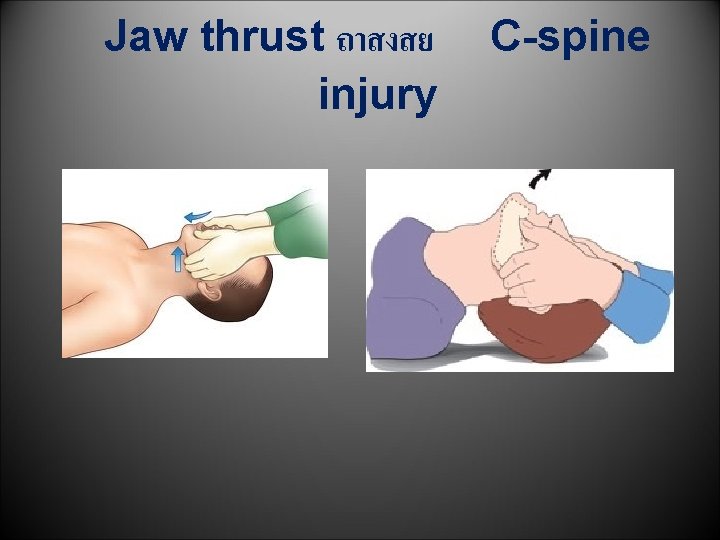
Jaw thrust ถาสงสย injury C-spine

Breathing
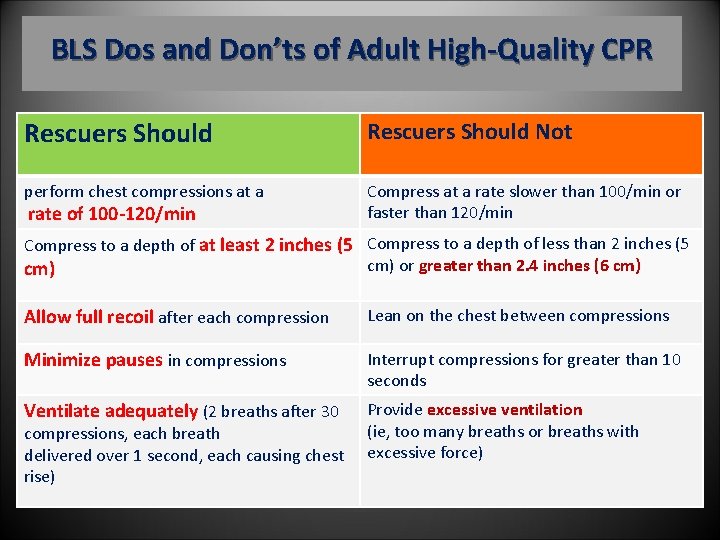
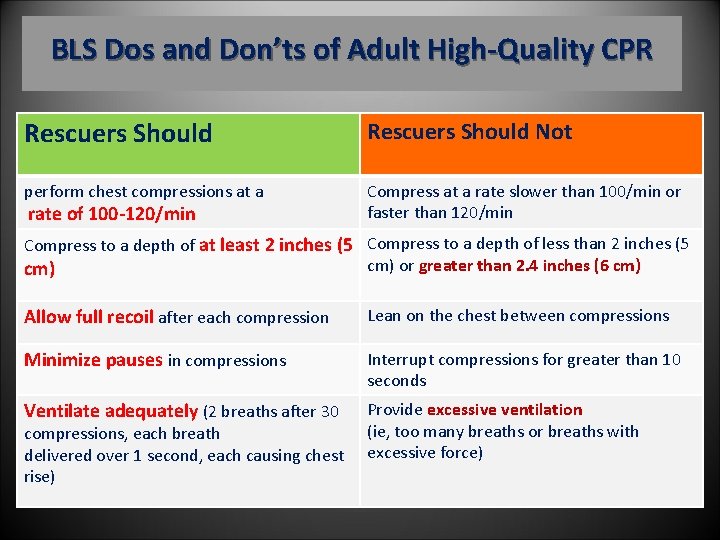
BLS Dos and Don’ts of Adult High-Quality CPR Rescuers Should Not perform chest compressions at a rate of 100 -120/min Compress at a rate slower than 100/min or faster than 120/min Compress to a depth of at least 2 inches (5 Compress to a depth of less than 2 inches (5 cm) or greater than 2. 4 inches (6 cm) Allow full recoil after each compression Lean on the chest between compressions Minimize pauses in compressions Interrupt compressions for greater than 10 seconds Ventilate adequately (2 breaths after 30 Provide excessive ventilation (ie, too many breaths or breaths with excessive force) compressions, each breath delivered over 1 second, each causing chest rise)
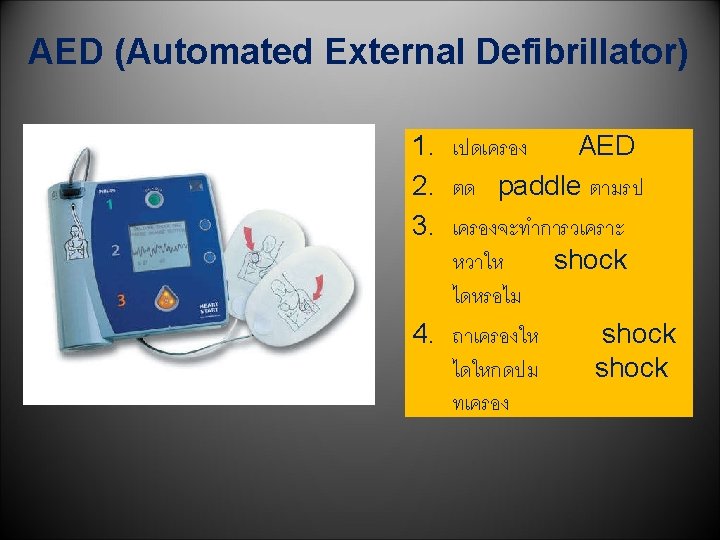
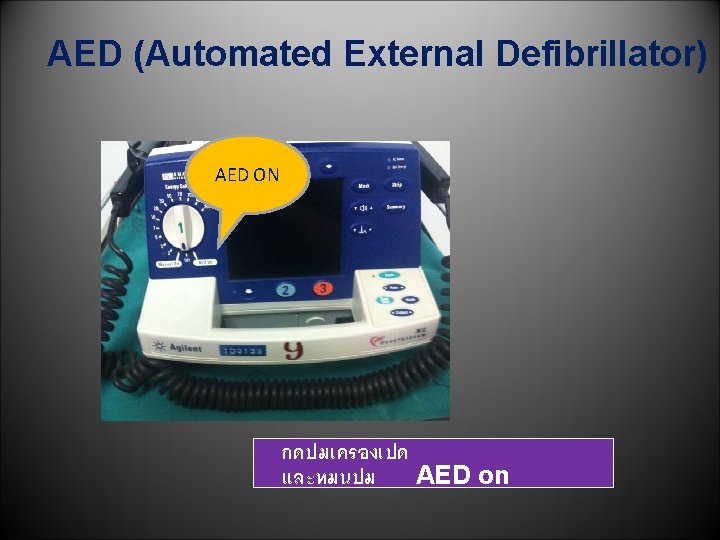
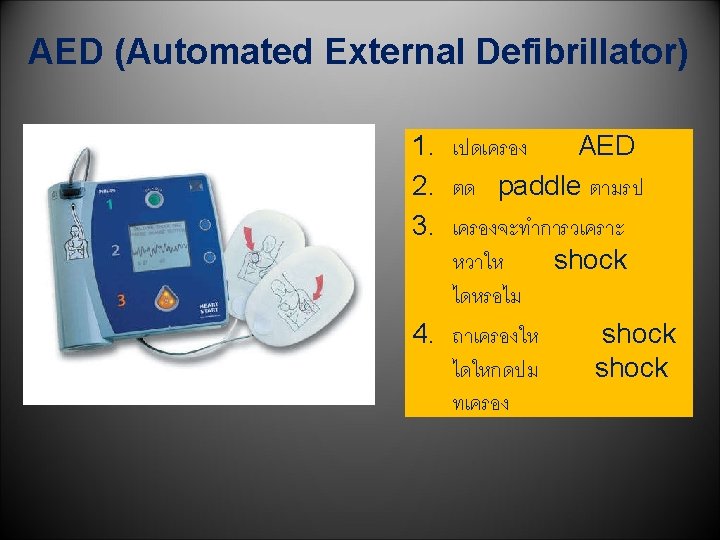
AED (Automated External Defibrillator) AED ON กดปมเครองเปด และหมนปม AED on
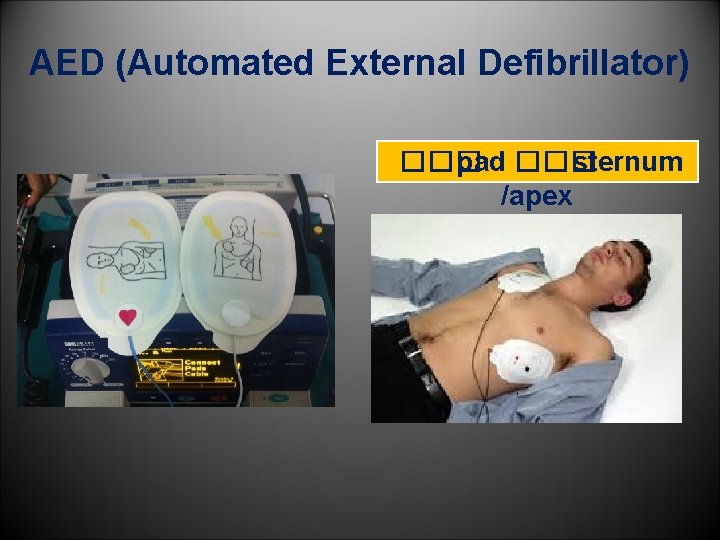
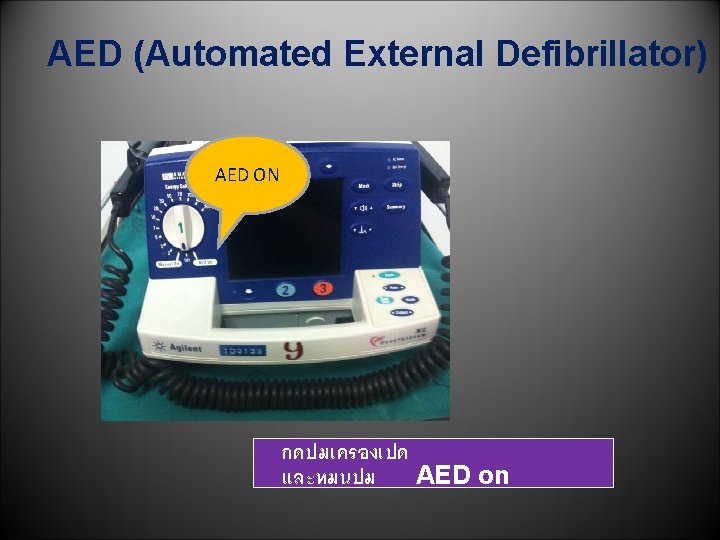
AED (Automated External Defibrillator) ��� pad ��� sternum /apex
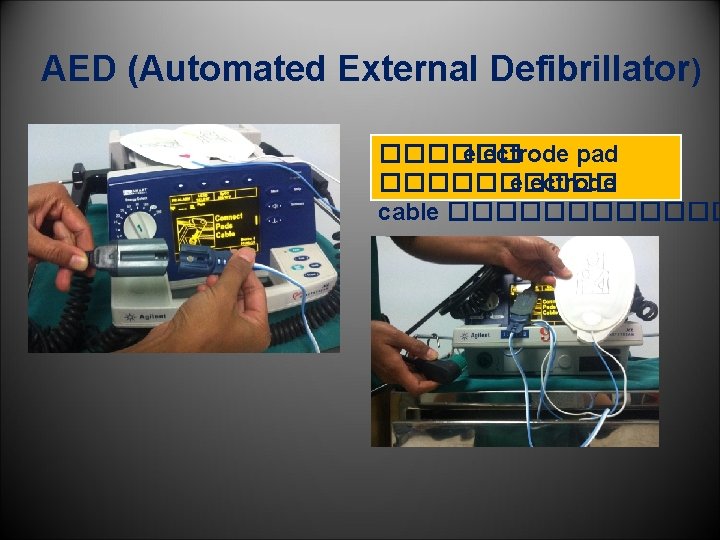
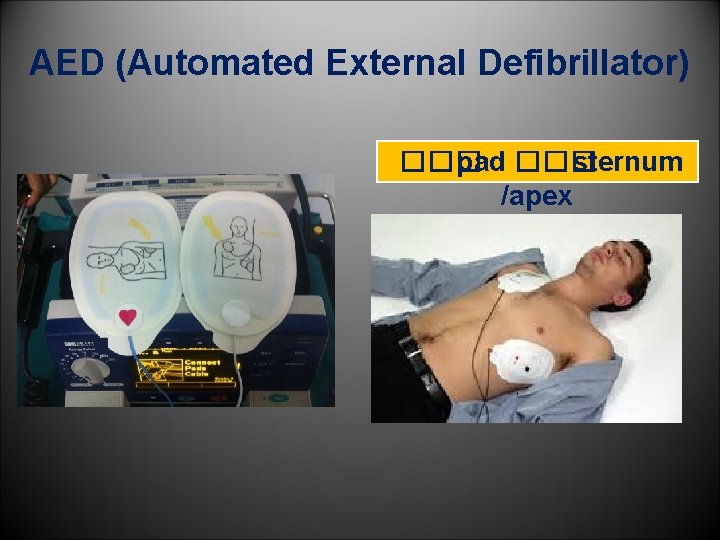
AED (Automated External Defibrillator) ������ electrode pad ����� electrode cable ������
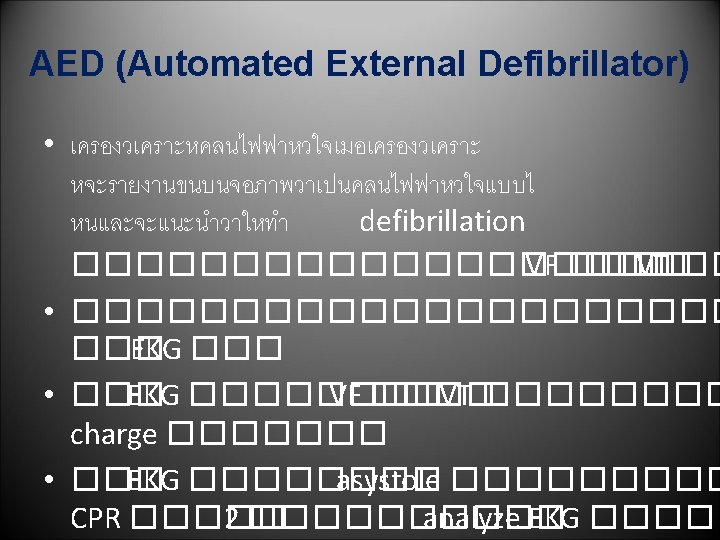
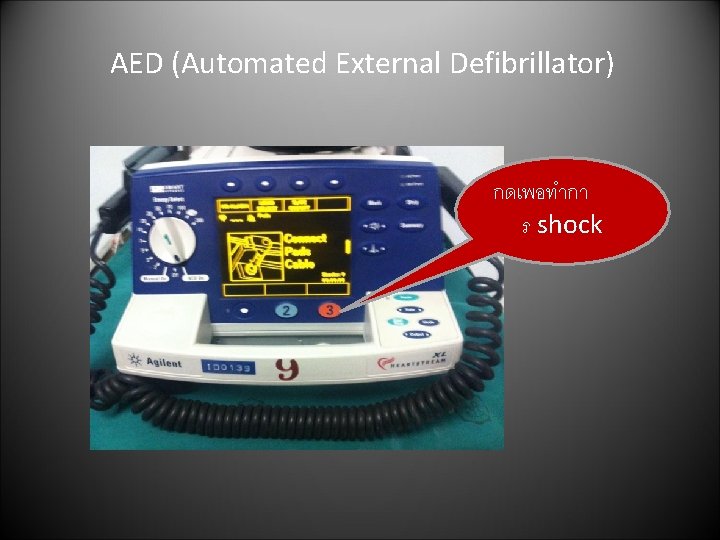
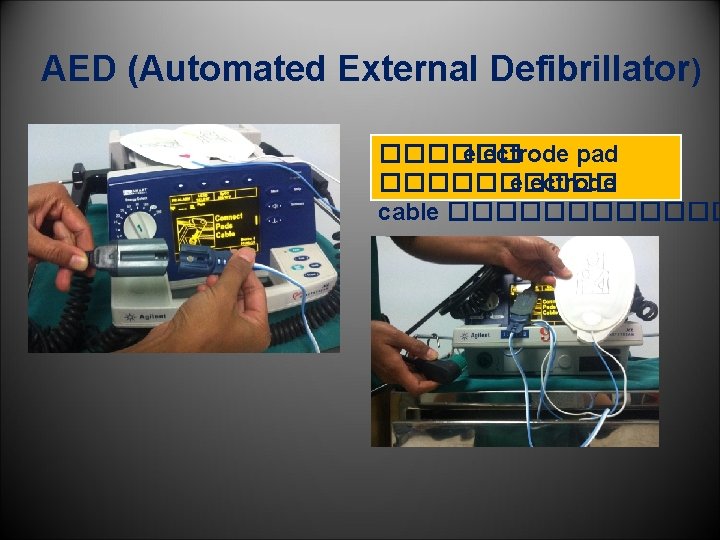
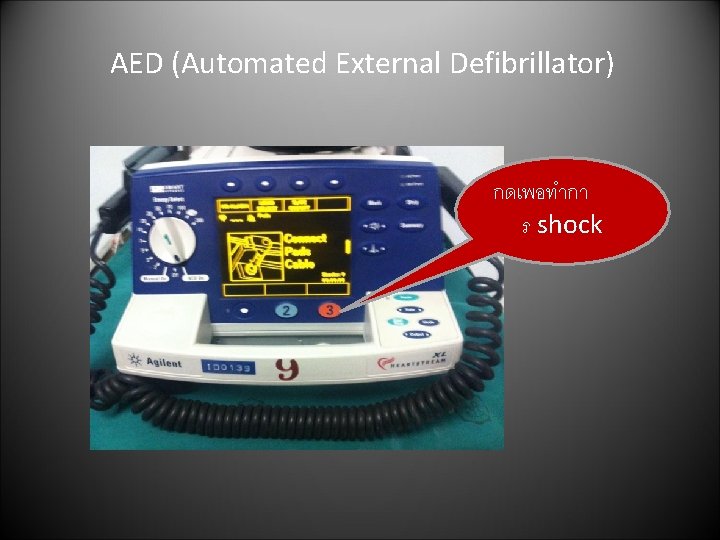
AED (Automated External Defibrillator) กดเพอทำกา ร shock
Advanced Cardiovascular Life Support: ACLS
Advanced Cardiovascular Life Support: ACLS • Pulseless Arrest • Bradycardia with Pulse • Tachycardia with Pulse

Pulseless Arrest
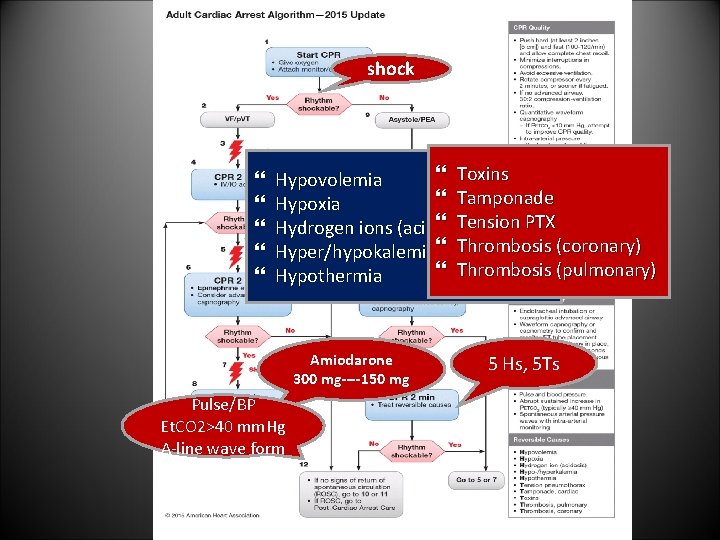
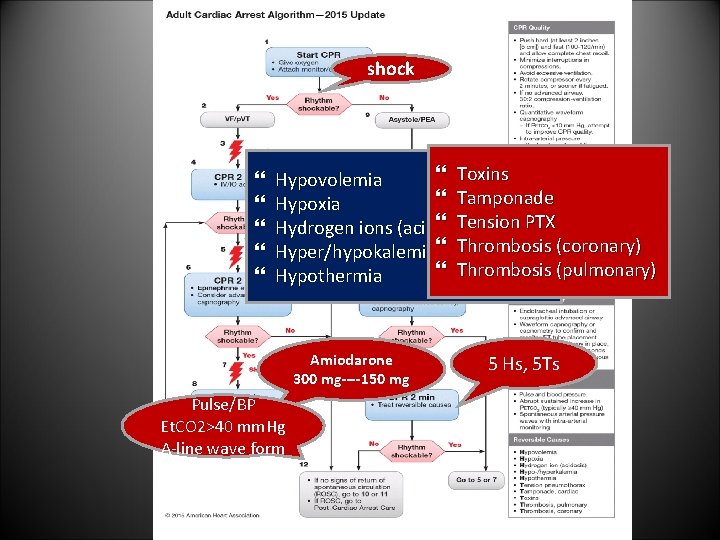
shock Toxins Hypovolemia Tamponade Hypoxia Tension PTX Hydrogen ions (acidosis) Hyper/hypokalemia Thrombosis (coronary) Thrombosis (pulmonary) Hypothermia Amiodarone 300 mg----150 mg Pulse/BP Et. CO 2>40 mm. Hg A-line wave form 5 Hs, 5 Ts
Bradycardia with Pulse
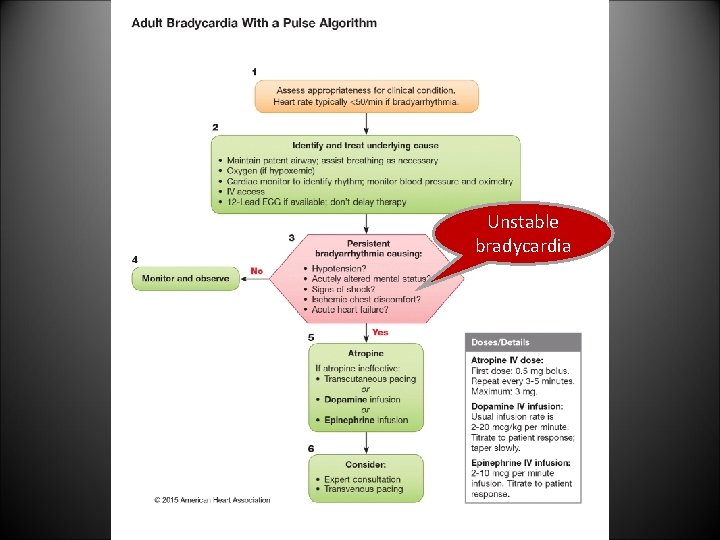
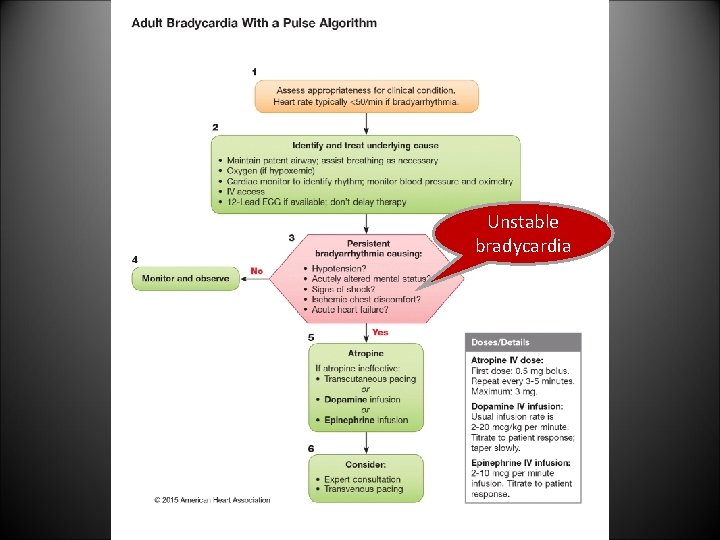
Unstable bradycardia
Tachycardia with Pulse
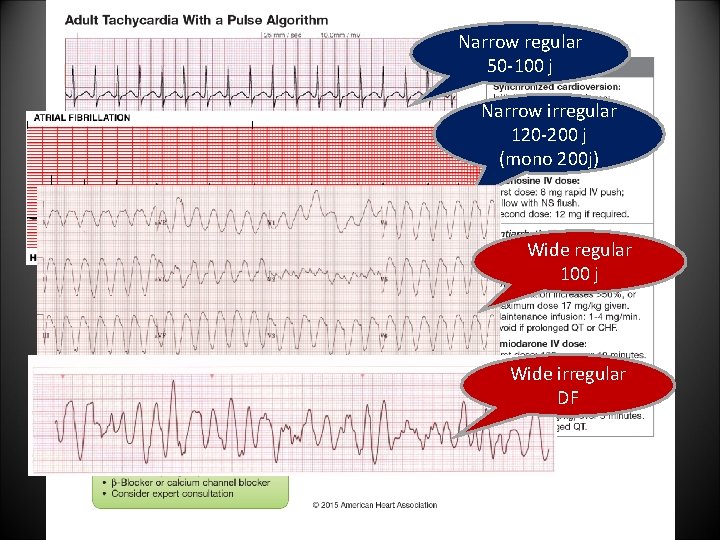
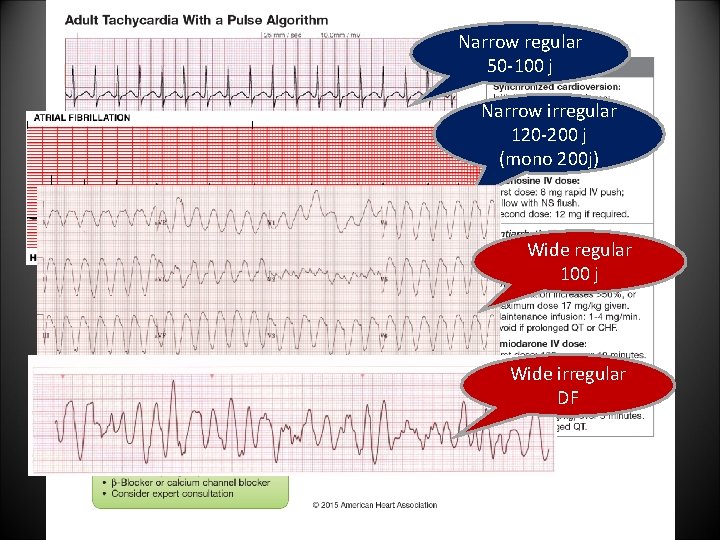
Narrow regular 50 -100 j Narrow irregular 120 -200 j (mono 200 j) Unstable Tachycardia Wide regular 100 j Wide irregular DF
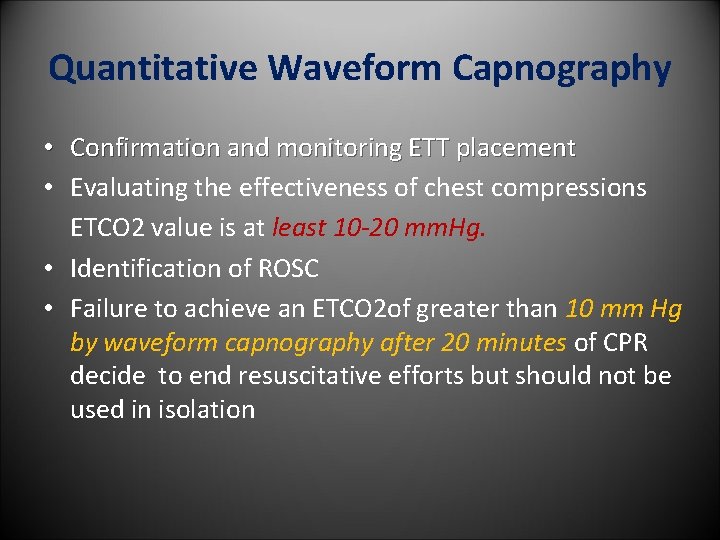
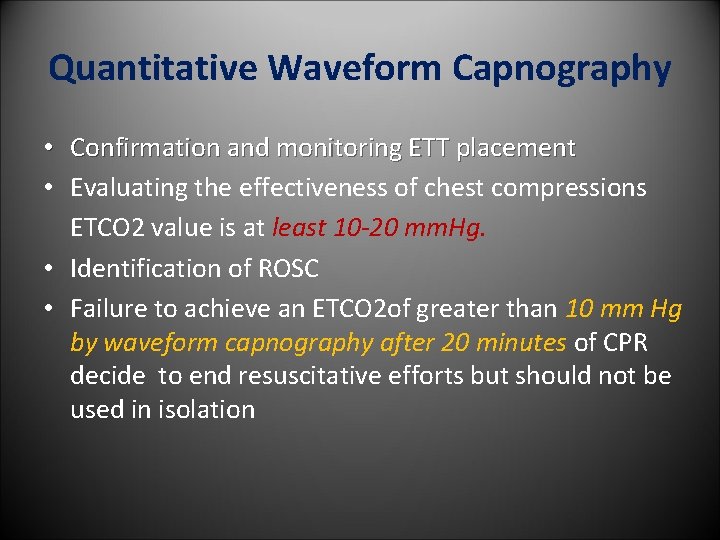
Quantitative Waveform Capnography • Confirmation and monitoring ETT placement • Evaluating the effectiveness of chest compressions ETCO 2 value is at least 10 -20 mm. Hg. • Identification of ROSC • Failure to achieve an ETCO 2 of greater than 10 mm Hg by waveform capnography after 20 minutes of CPR decide to end resuscitative efforts but should not be used in isolation
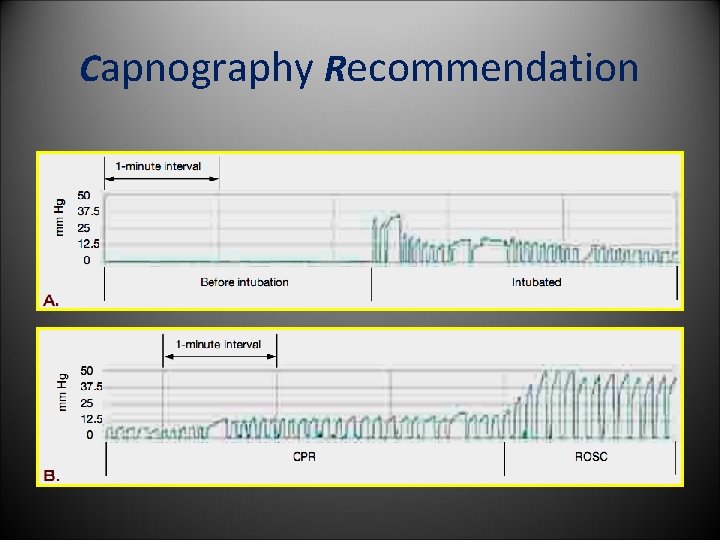
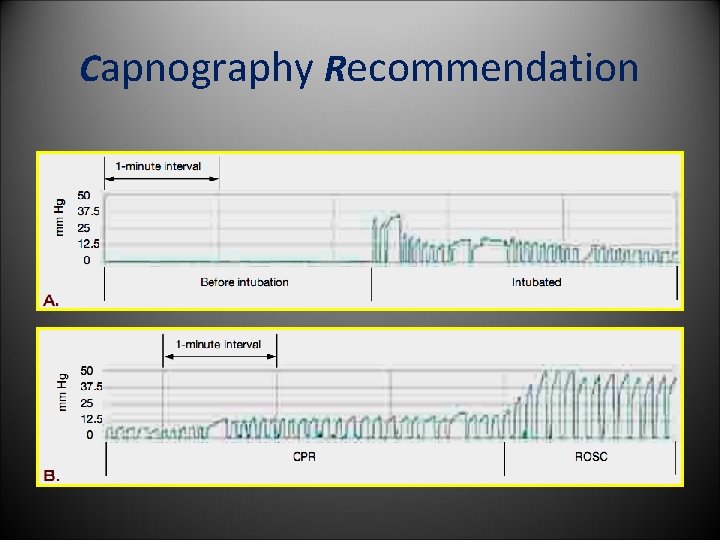
Capnography Recommendation
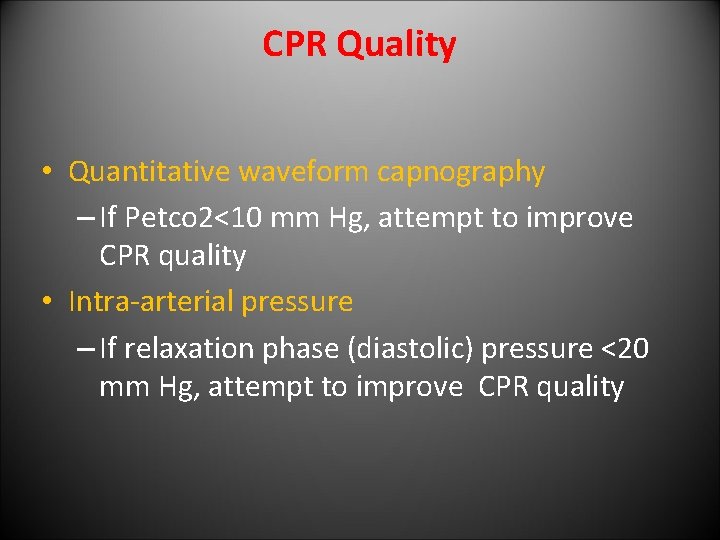
CPR Quality • Quantitative waveform capnography – If Petco 2<10 mm Hg, attempt to improve CPR quality • Intra-arterial pressure – If relaxation phase (diastolic) pressure <20 mm Hg, attempt to improve CPR quality
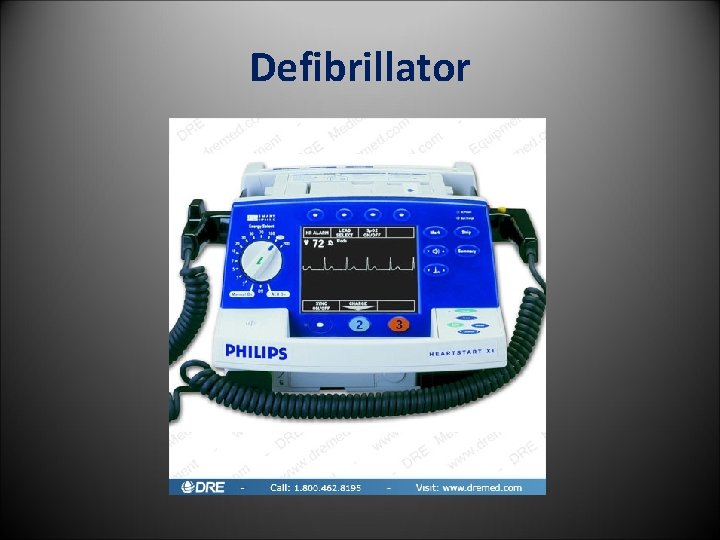
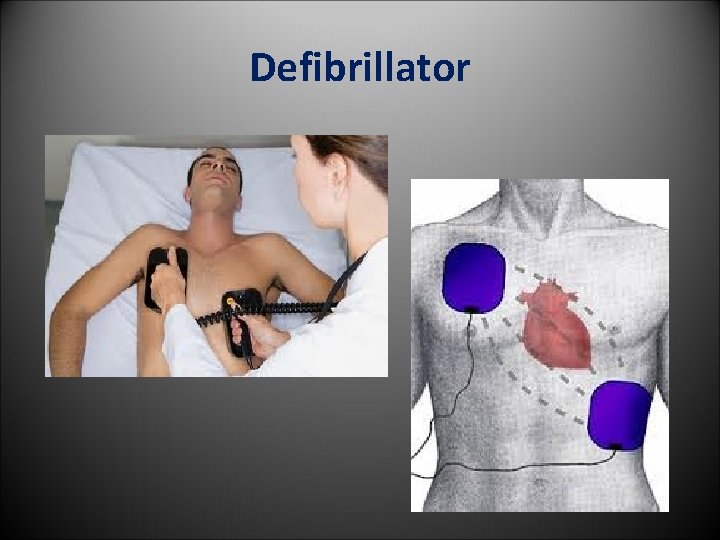
Defibrillator
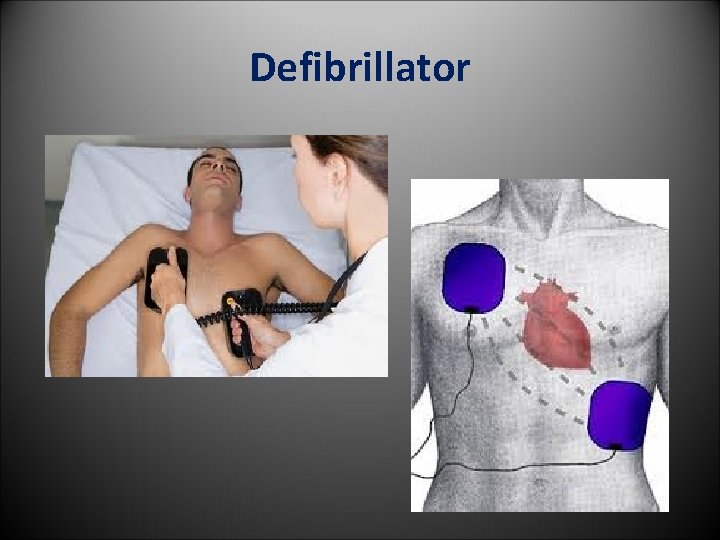
Defibrillator
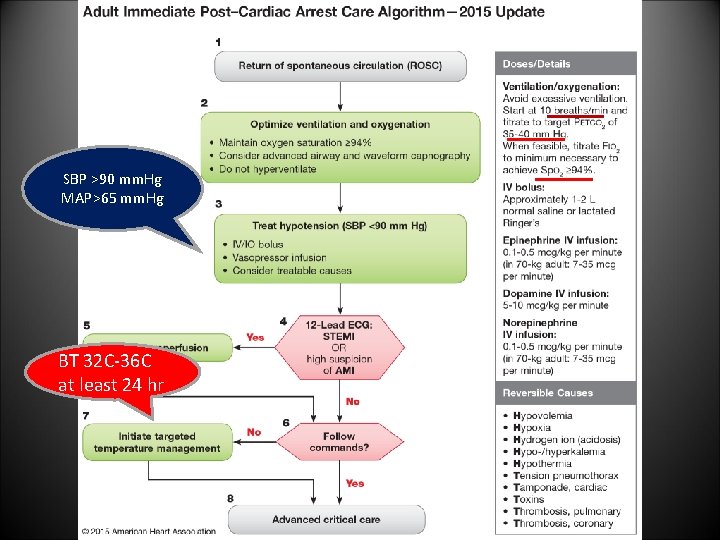
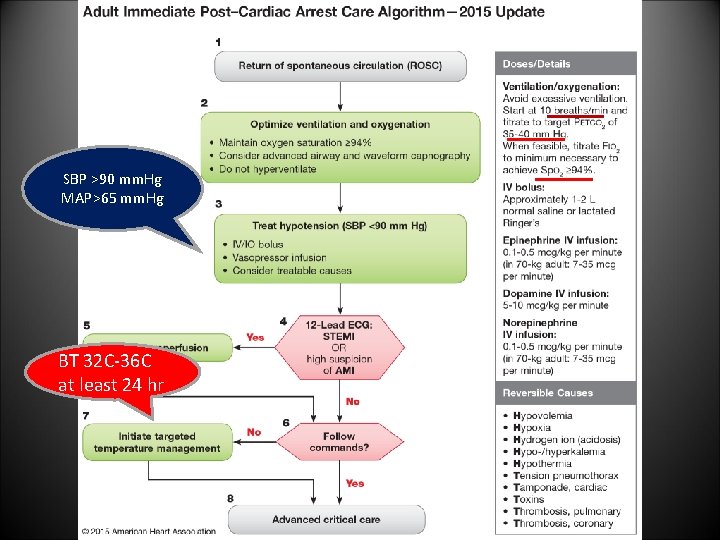
SBP >90 mm. Hg MAP>65 mm. Hg BT 32 C-36 C at least 24 hr
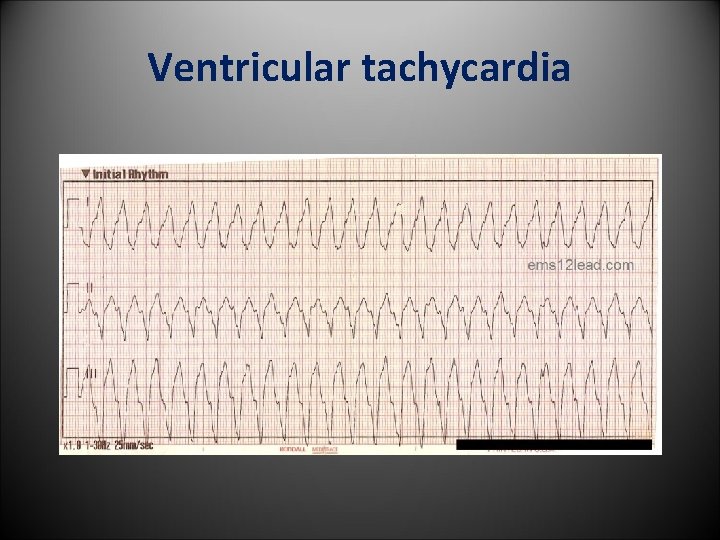
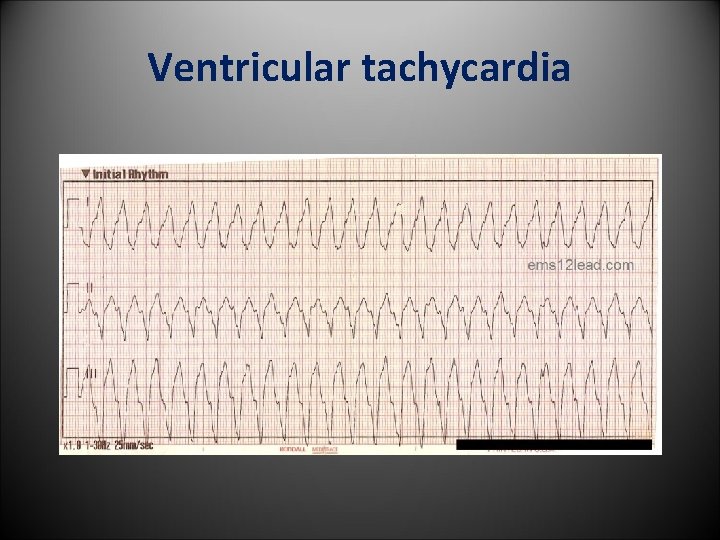
Ventricular tachycardia
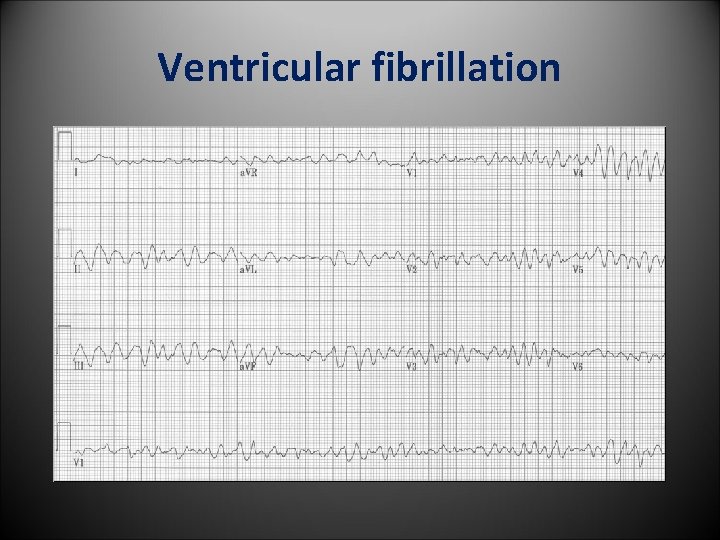
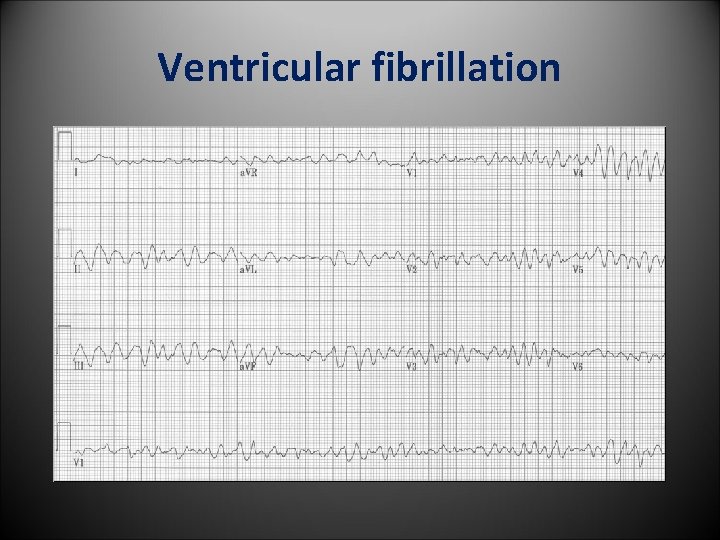
Ventricular fibrillation
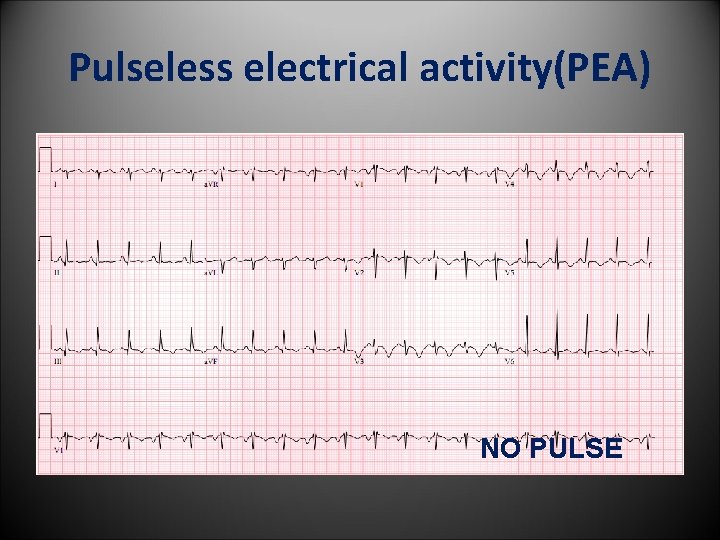
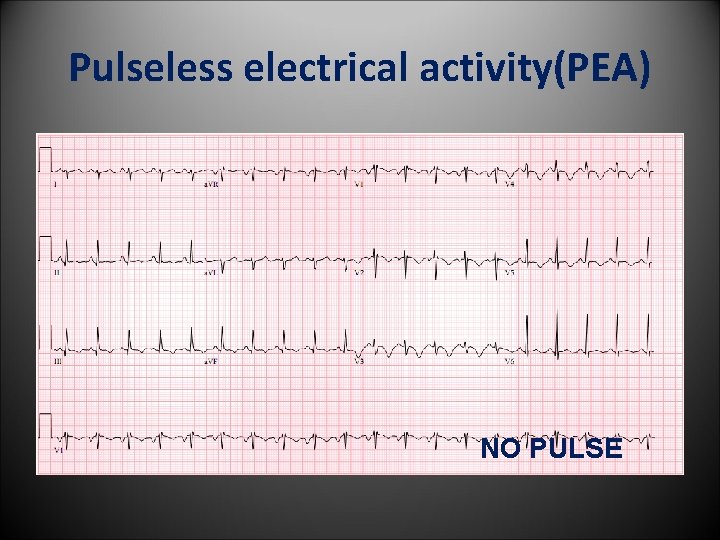
Pulseless electrical activity(PEA) NO PULSE
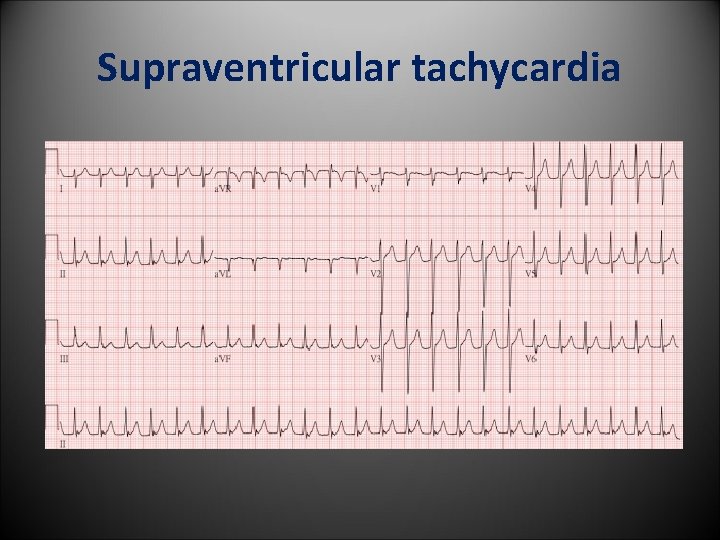
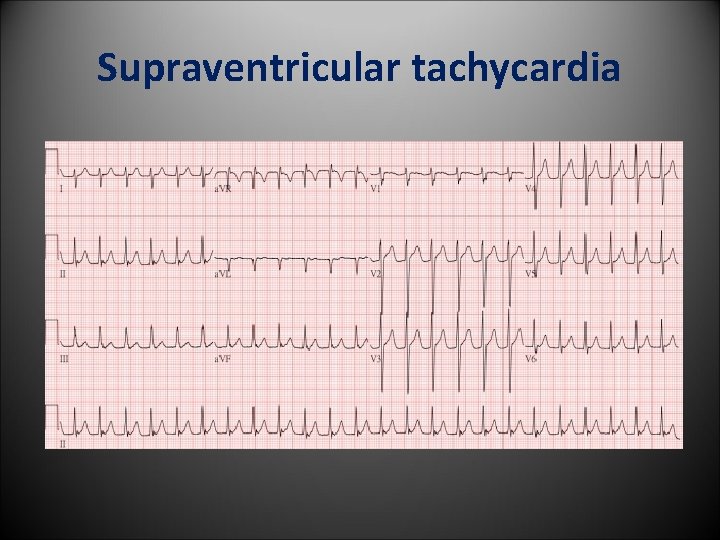
Supraventricular tachycardia
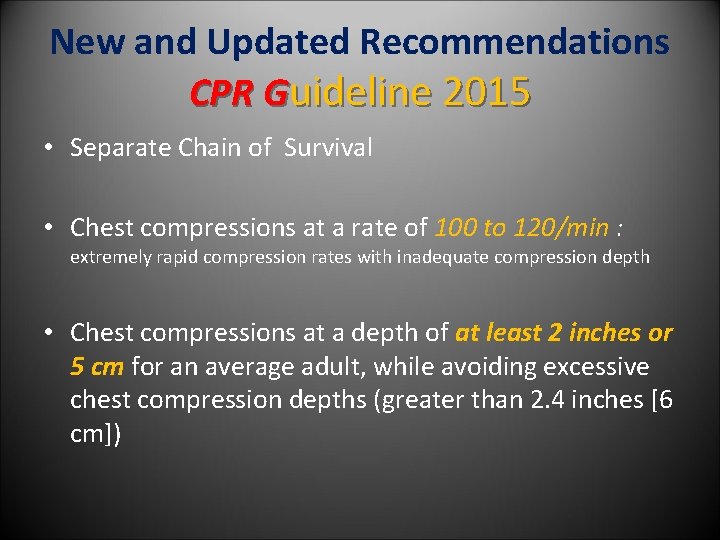
New and Updated Recommendations CPR Guideline 2015 • Separate Chain of Survival • Chest compressions at a rate of 100 to 120/min : extremely rapid compression rates with inadequate compression depth • Chest compressions at a depth of at least 2 inches or 5 cm for an average adult, while avoiding excessive chest compression depths (greater than 2. 4 inches [6 cm])
New and Updated Recommendations CPR Guideline 2015 • Delivery 1 breath every 6 seconds (10 /min) while continuous chest compression with advance airway • Vasopressin was removed from the ACLS Cardiac Arrest Algorithm • Nonshockable rhythm , administer epinephrine as soon as feasible (IV/IO/ET) • Targeted temperature management 32 C to 36 C in 24 hr • The routine prehospital cooling of patients with rapid infusion of cold IV fluids after ROSC is not recommended
Thank you