84 yearold male Crushing injury paper skin n












- Slides: 81


84 year-old male Crushing injury paper skin


n 7 months follow up
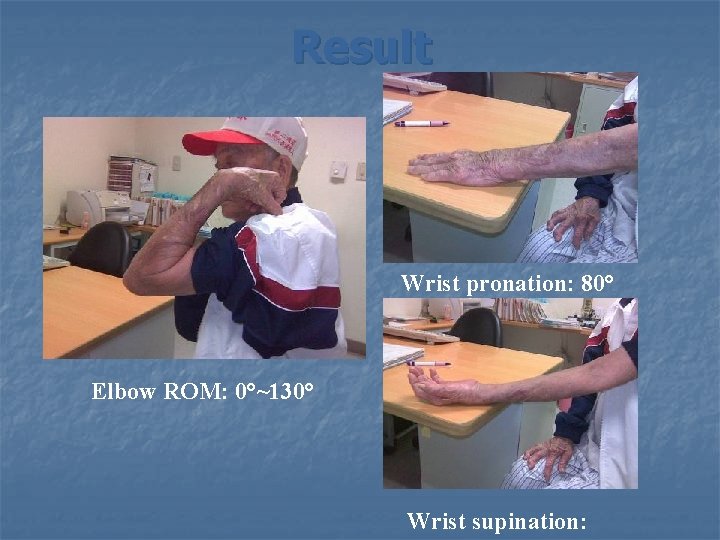
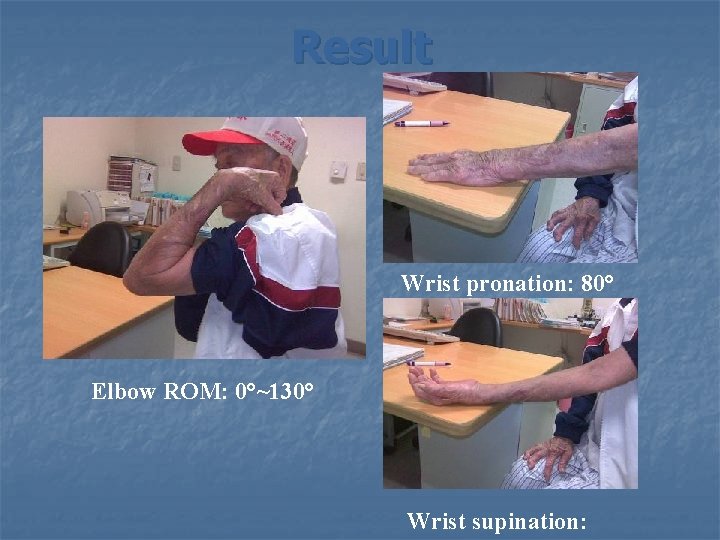
Result Wrist pronation: 80° Elbow ROM: 0°~130° Wrist supination:
Learning objectives n. The principles of management n. The surgical and applied anatomy n. The treatment options Fractures of the shaft Galeazzi fracture Monteggia fracture Essex-Lopresti injury n The complications and the outcomes
Introduction PRUJ and DRUJ pronation and Supination Muscle origin inserting to the hand the daily activity
Principles of Management Mechanisms of injury n n n A fall from standing height A direct blow– fight isolated fracture of the ulna- nightstick fr. more stable, esp < 50% displacement a road traffic accident
Principles of Management History and Physical Examination n n 1. 2. 3. Often displaced the diagnosis can easily be made from the S/S PE: neurologic evaluation of the motor and sensory functions Compartment syndrome The soft tissue injury of the elbow and wrist Galeazzi fracture, Monteggia fracture, Essex. Lopresti injury
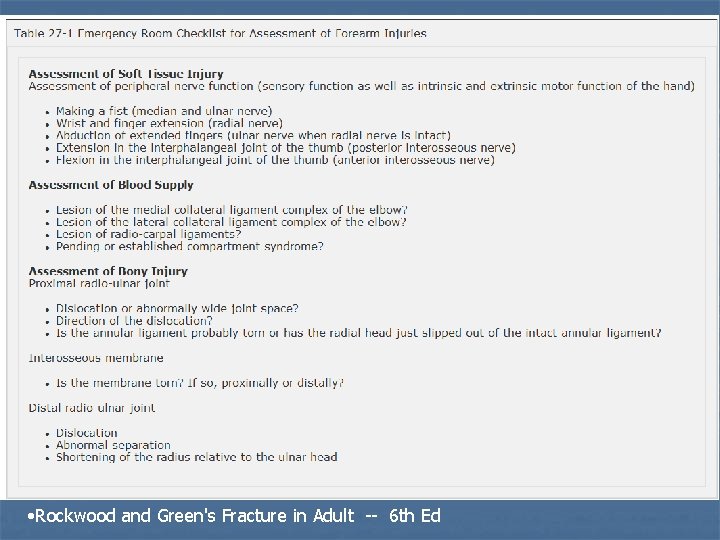
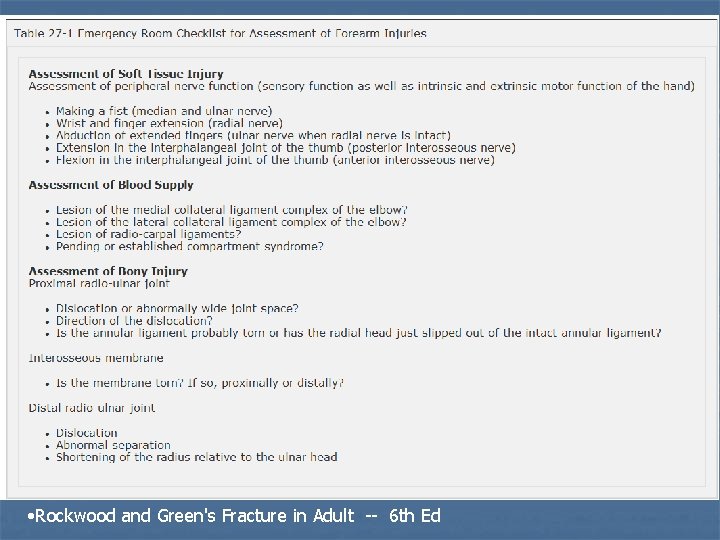
• Rockwood and Green's Fracture in Adult -- 6 th Ed
Monteggia Fracture- Dislocation Fracture of the proximal ulna with a concomitant dislocation of the radial head n 5% - 10% of all forearm fractures n First described by Monteggia in 1814 n Radial head may be palpable at anterior or posterior aspect of the elbow n PIN injury: 17% -- stretch-- recover spontaneously -- entrapment-- irreducble Monteggia lesion n
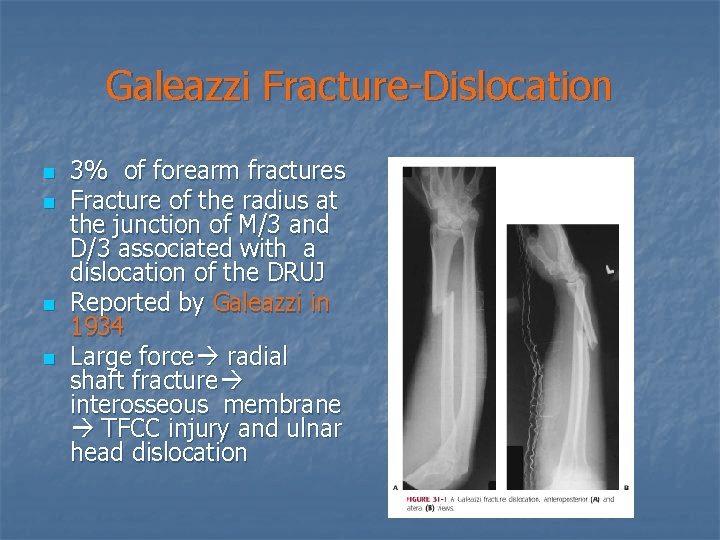
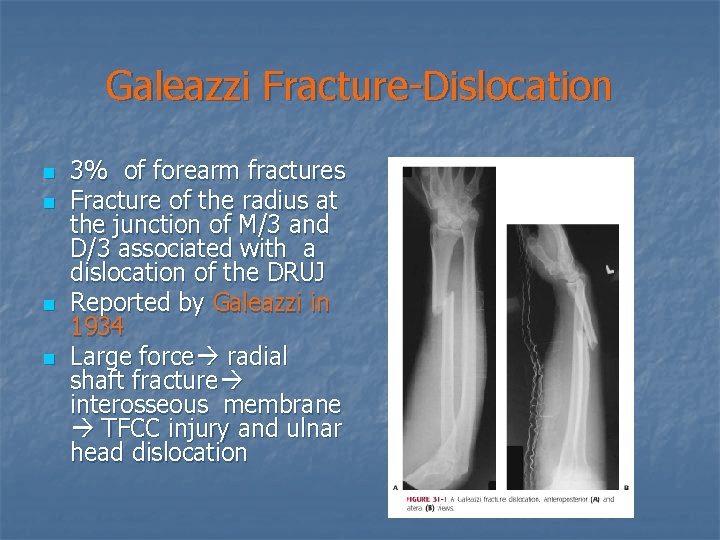
Galeazzi Fracture-Dislocation n n 3% of forearm fractures Fracture of the radius at the junction of M/3 and D/3 associated with a dislocation of the DRUJ Reported by Galeazzi in 1934 Large force radial shaft fracture interosseous membrane TFCC injury and ulnar head dislocation
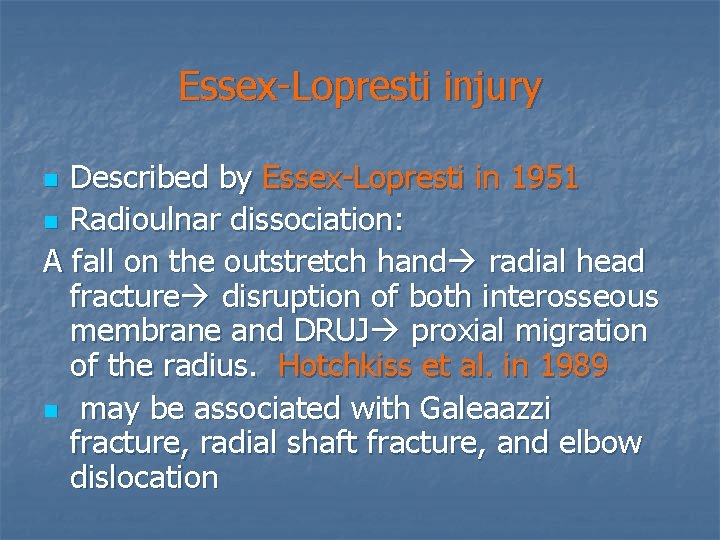
Essex-Lopresti injury Described by Essex-Lopresti in 1951 n Radioulnar dissociation: A fall on the outstretch hand radial head fracture disruption of both interosseous membrane and DRUJ proxial migration of the radius. Hotchkiss et al. in 1989 n may be associated with Galeaazzi fracture, radial shaft fracture, and elbow dislocation n
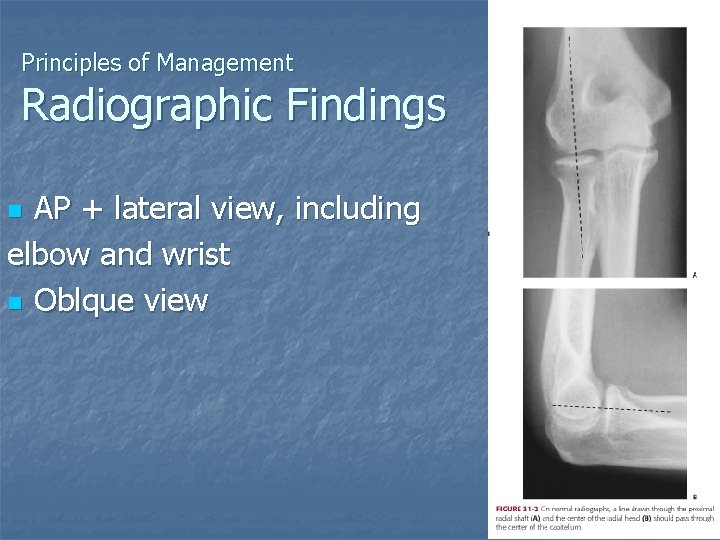
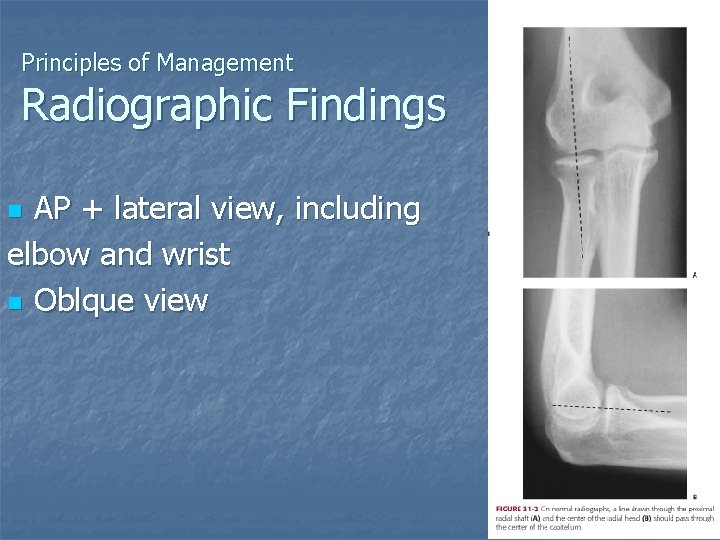
Principles of Management Radiographic Findings AP + lateral view, including elbow and wrist n Oblque view n
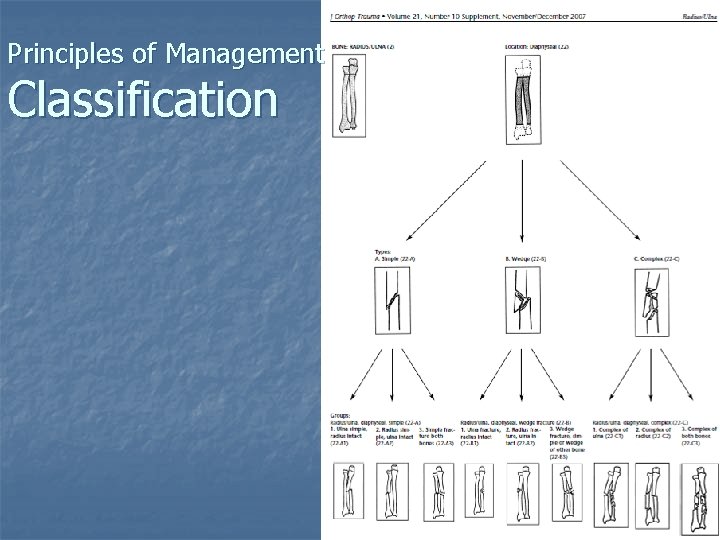
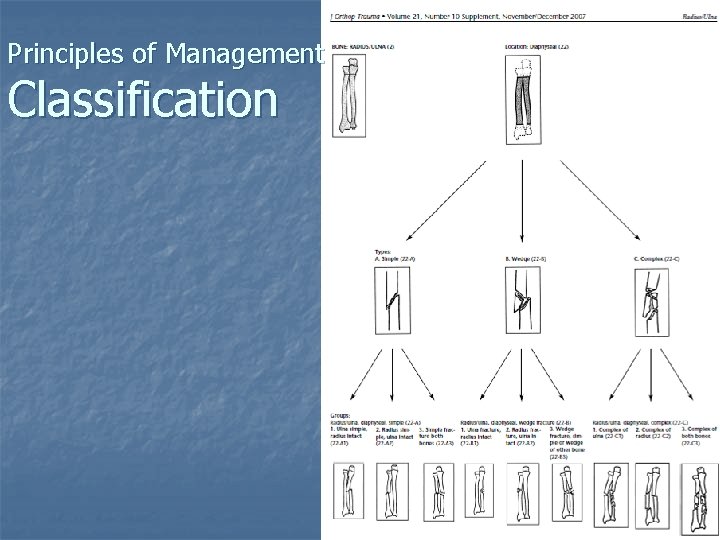
Principles of Management Classification

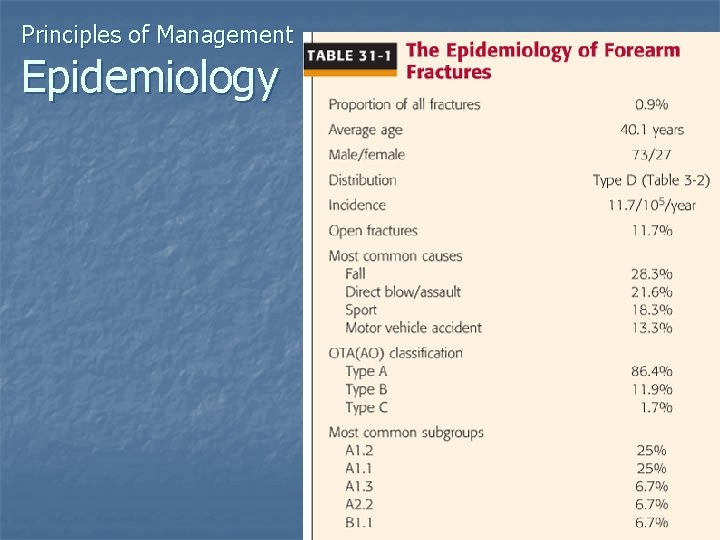
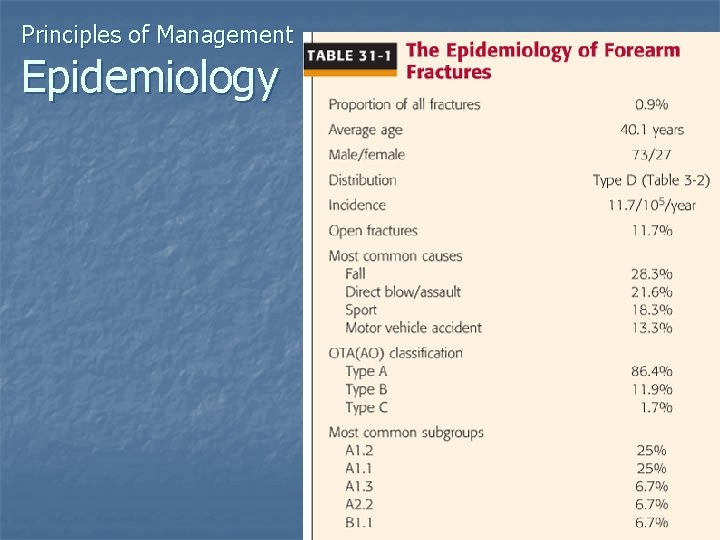
Principles of Management Epidemiology
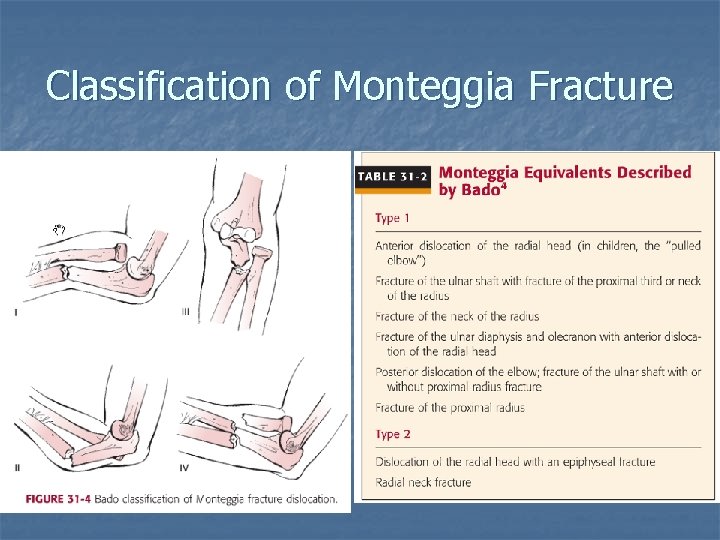
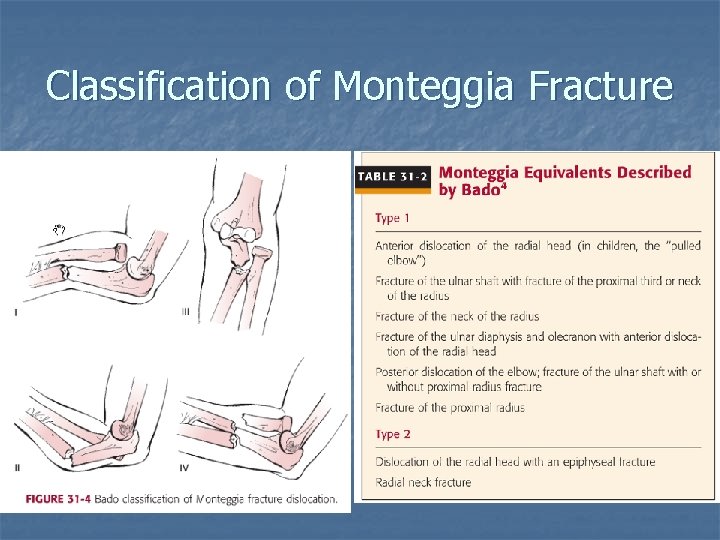
Classification of Monteggia Fracture 15 -30% 59 -79%
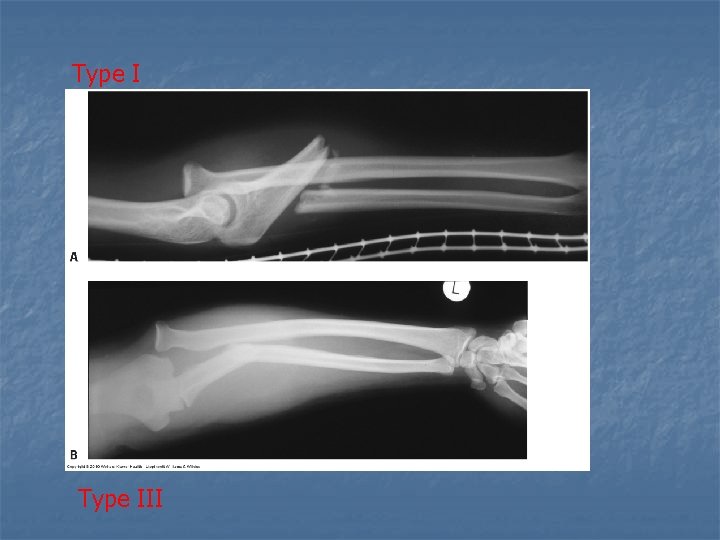
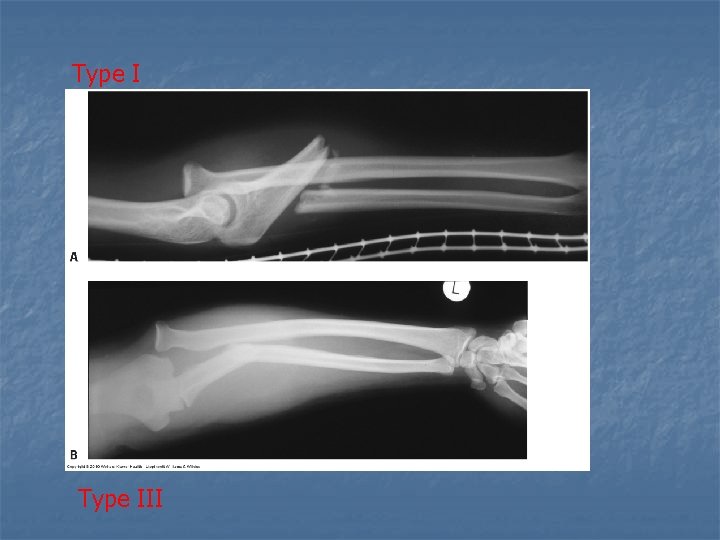
Type III
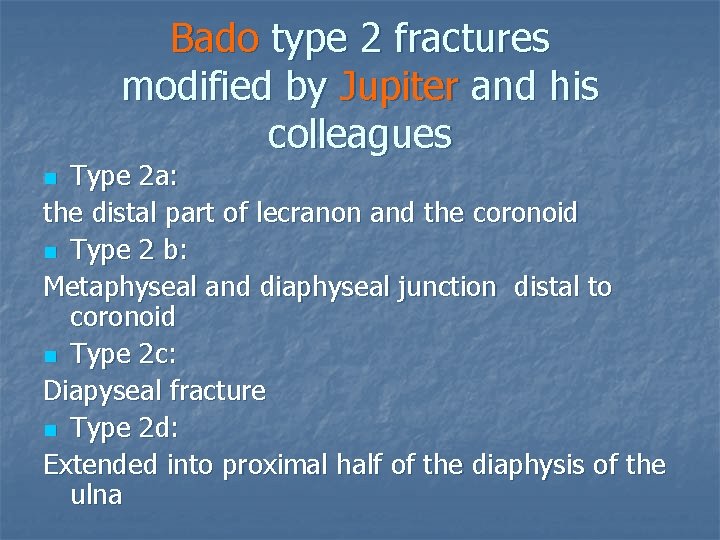
Bado type 2 fractures modified by Jupiter and his colleagues Type 2 a: the distal part of lecranon and the coronoid n Type 2 b: Metaphyseal and diaphyseal junction distal to coronoid n Type 2 c: Diapyseal fracture n Type 2 d: Extended into proximal half of the diaphysis of the ulna n
Classification of Galeazzi Fracture Type I: the distal radial fracture < 7. 5 cm distal radial articular surface, 6% DRUJ instability n Type II: > 7. 5 cm, 55% DRUJ instability n
Classification of Essex-Lopresti injury n Edwards and Jupiter’s Classification Depends on the type of radial head fracture Type 1: large displaced Type 2: severely comminuted Type 3: old injuries with irreducible proximal migration of the radius

Surgical and Applied Anatomy Bone and joint n n 5 articular surface Rotational movement: Radial bow: sage, 1959 Proximal: n Apex medial: 13. 10 , Apex anerior: 13. 10 Distal Apex lateral: 9. 30 , Apex posterior: 6. 40 n Ulnar bow : relative straight Apex posterior
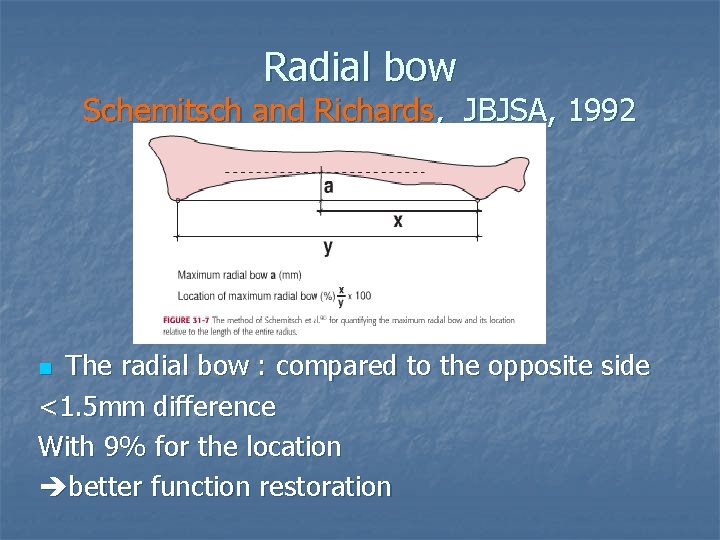
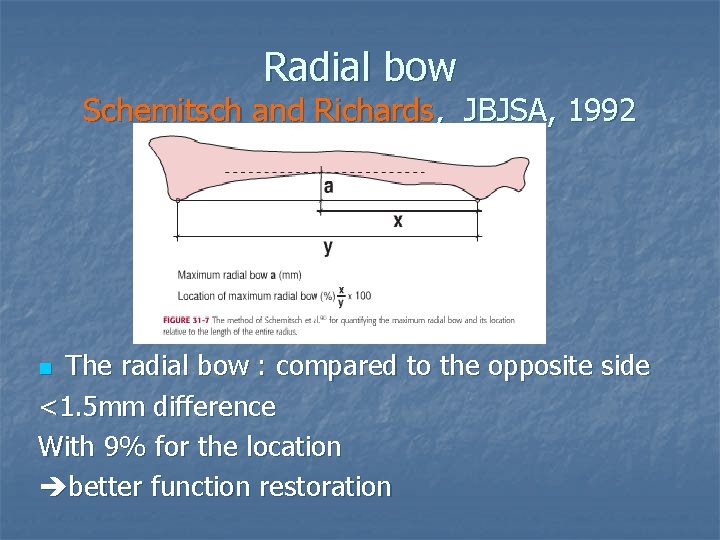
Radial bow Schemitsch and Richards, JBJSA, 1992 The radial bow : compared to the opposite side <1. 5 mm difference With 9% for the location better function restoration n
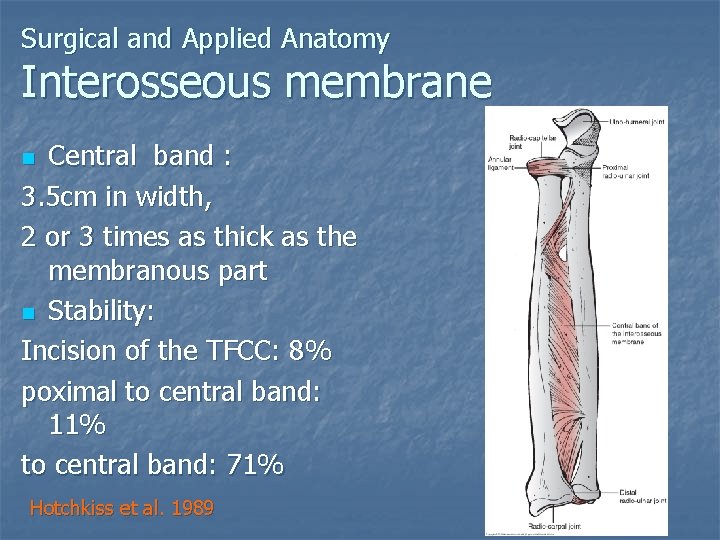
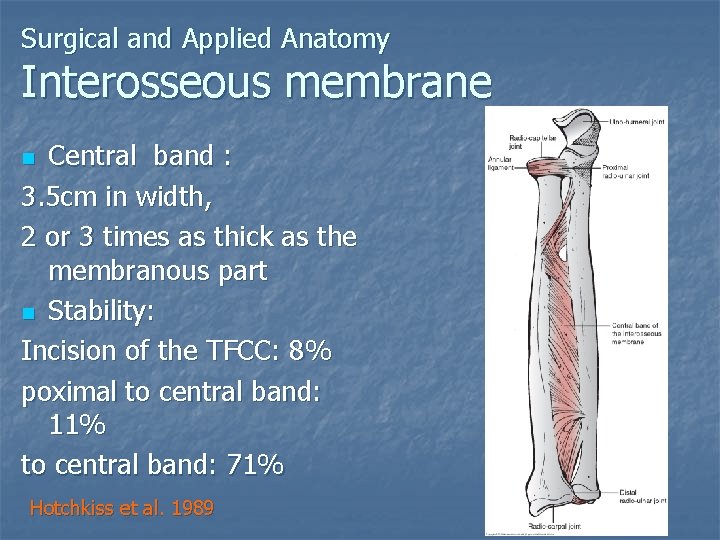
Surgical and Applied Anatomy Interosseous membrane Central band : 3. 5 cm in width, 2 or 3 times as thick as the membranous part n Stability: Incision of the TFCC: 8% poximal to central band: 11% to central band: 71% n Hotchkiss et al. 1989
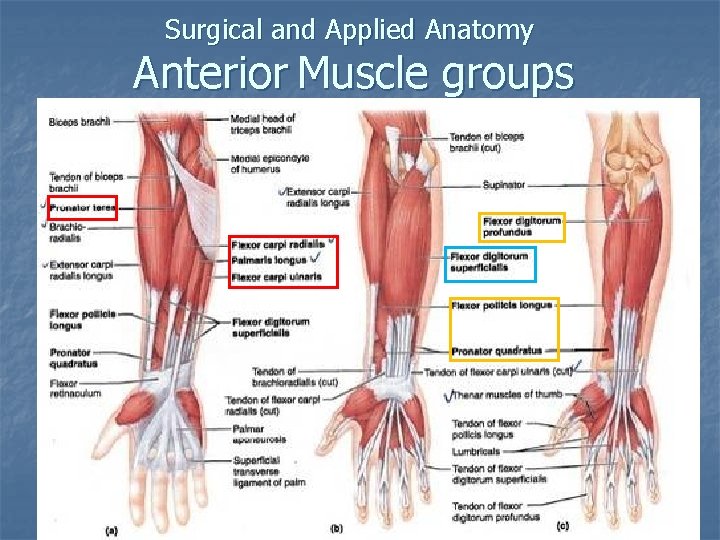
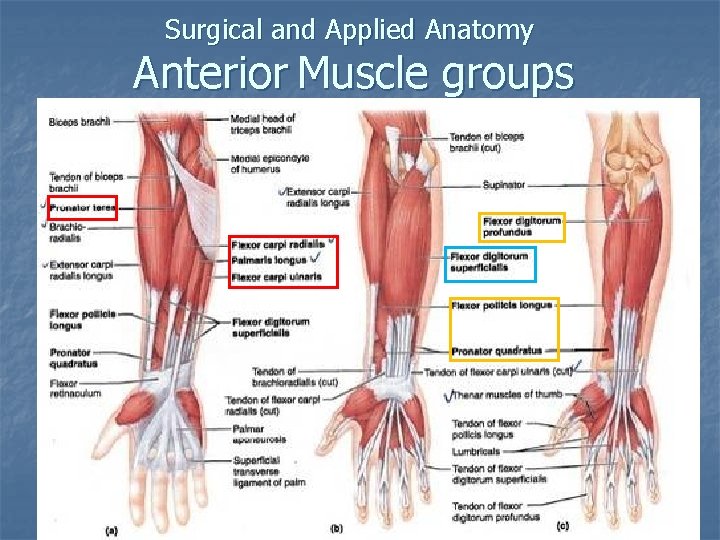
Surgical and Applied Anatomy Anterior Muscle groups
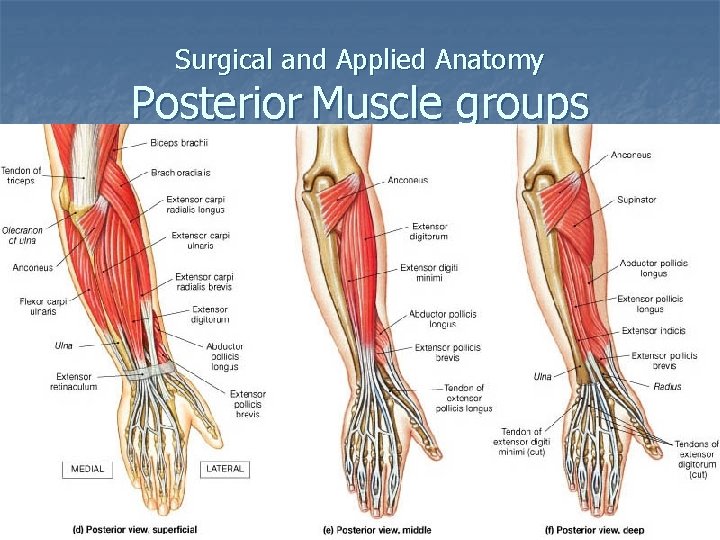
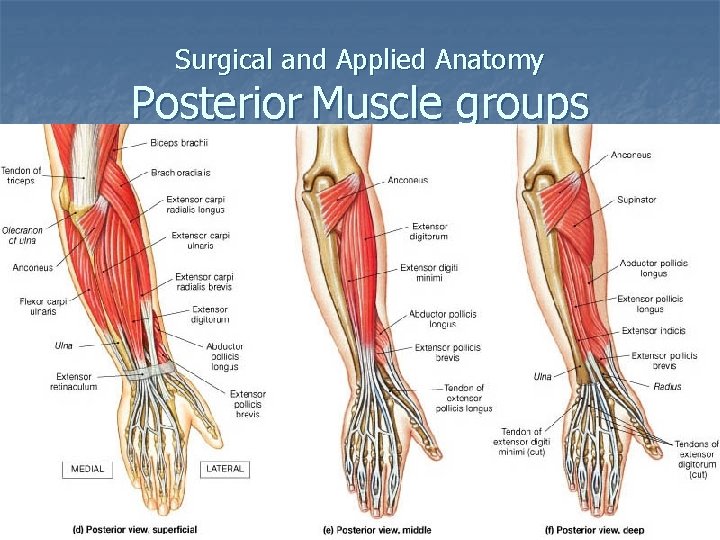
Surgical and Applied Anatomy Posterior Muscle groups
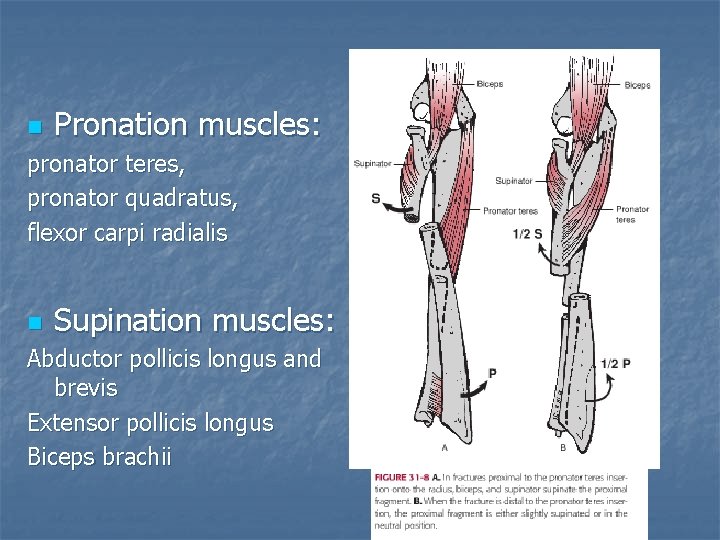
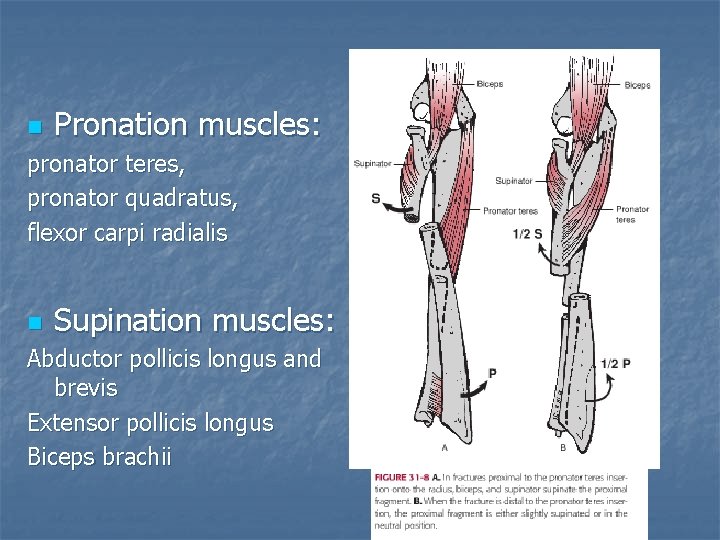
n Pronation muscles: pronator teres, pronator quadratus, flexor carpi radialis n Supination muscles: Abductor pollicis longus and brevis Extensor pollicis longus Biceps brachii
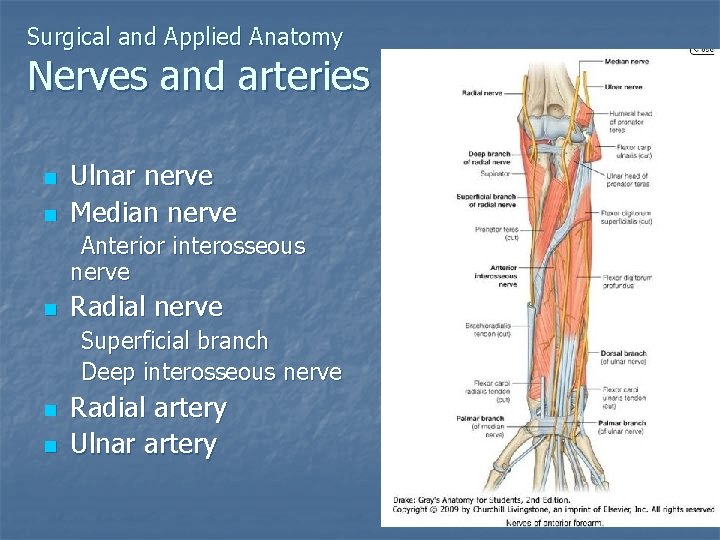
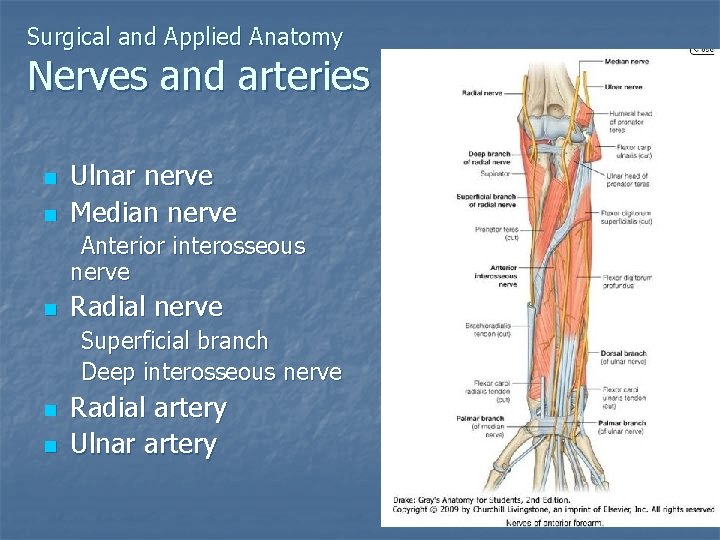
Surgical and Applied Anatomy Nerves and arteries n n Ulnar nerve Median nerve Anterior interosseous nerve n Radial nerve Superficial branch Deep interosseous nerve n n Radial artery Ulnar artery


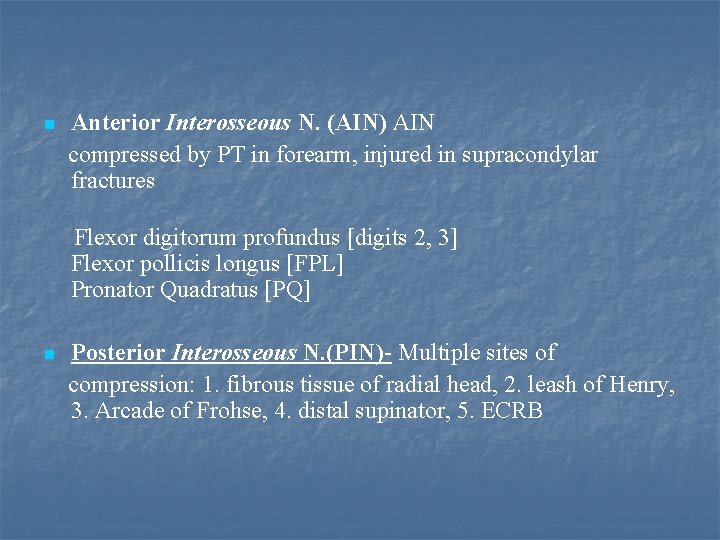
n Anterior Interosseous N. (AIN) AIN compressed by PT in forearm, injured in supracondylar fractures Flexor digitorum profundus [digits 2, 3] Flexor pollicis longus [FPL] Pronator Quadratus [PQ] n Posterior Interosseous N. (PIN)- Multiple sites of compression: 1. fibrous tissue of radial head, 2. leash of Henry, 3. Arcade of Frohse, 4. distal supinator, 5. ECRB
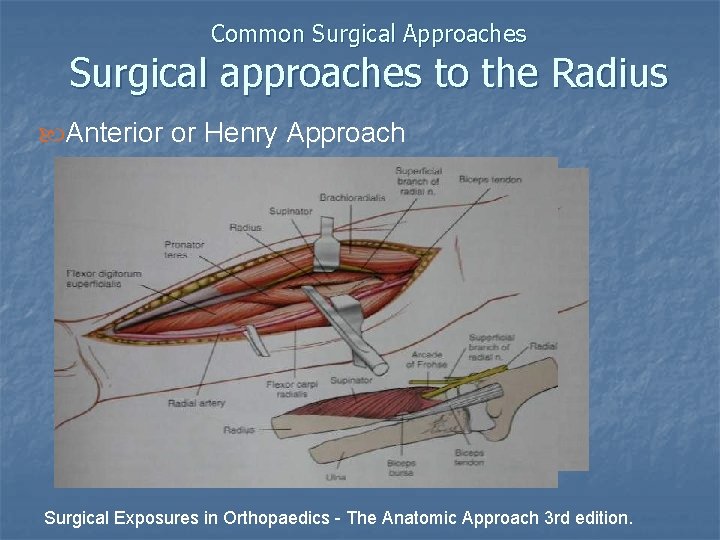
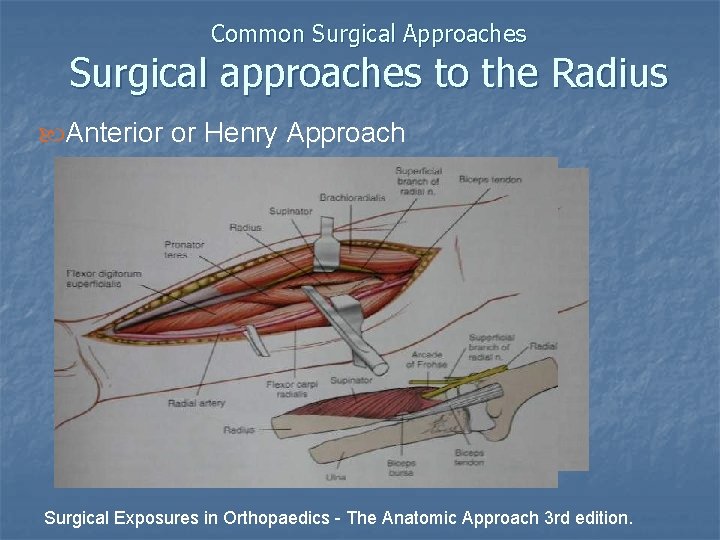
Common Surgical Approaches Surgical approaches to the Radius Anterior or Henry Approach Surgical Exposures in Orthopaedics - The Anatomic Approach 3 rd edition.
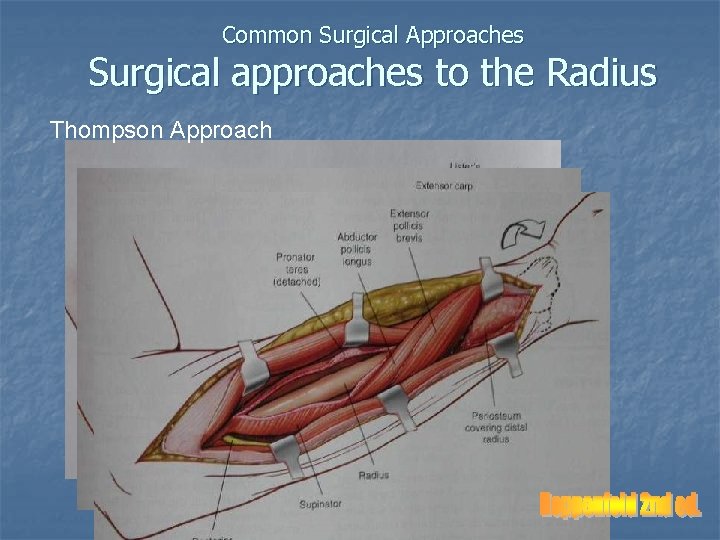
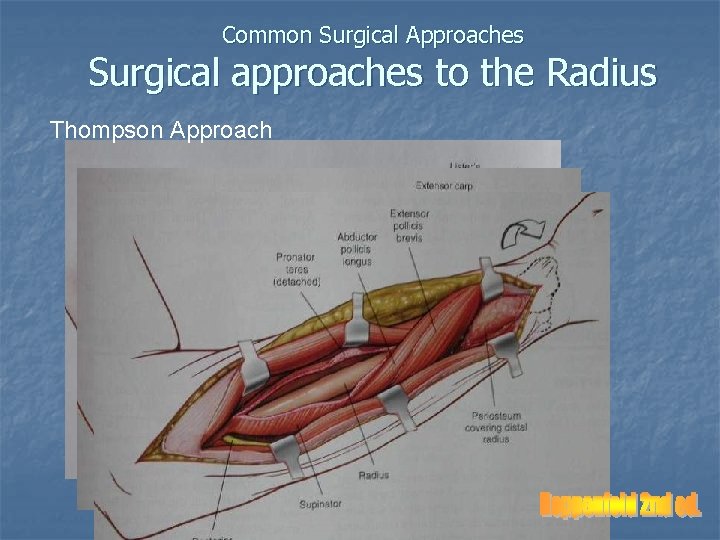
Common Surgical Approaches Surgical approaches to the Radius Thompson Approach
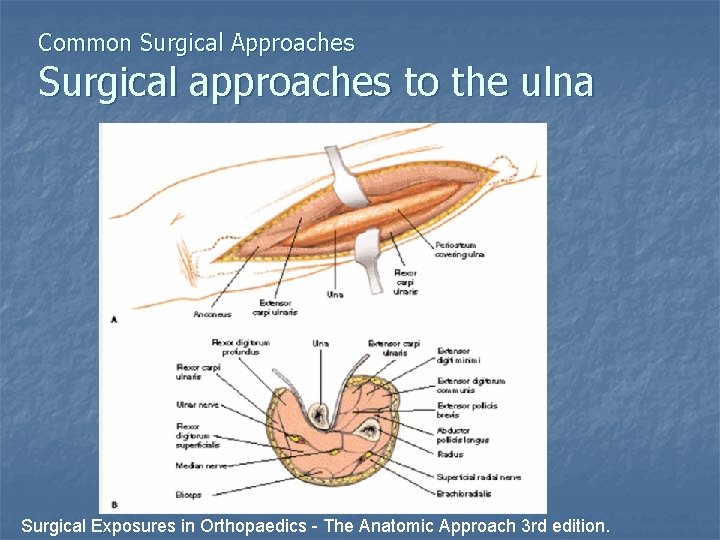
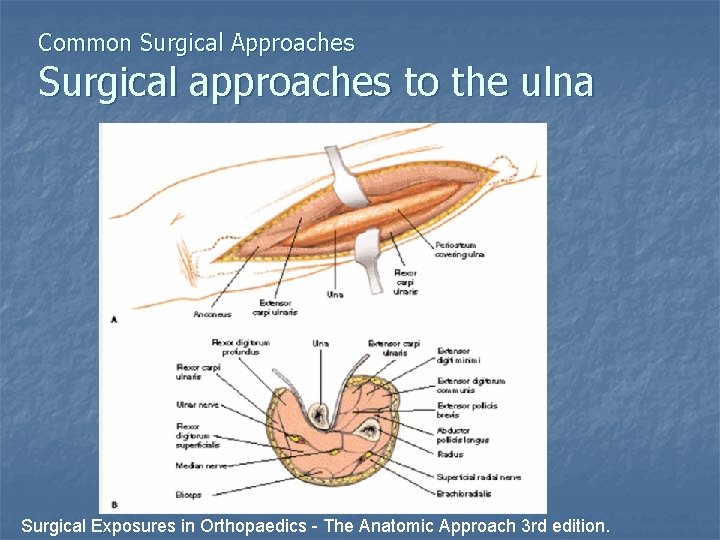
Common Surgical Approaches Surgical approaches to the ulna Surgical Exposures in Orthopaedics - The Anatomic Approach 3 rd edition.
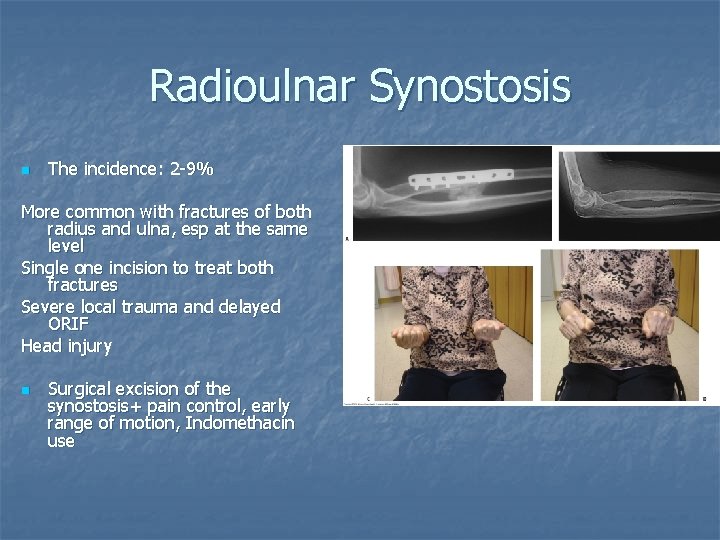
n n Regarding implant position and surgical approach, radioulnar synostosis is associated with a single incision approach. A double-incision approach is preferred by the authors for ORIF of both-bone forearm fractures. (OKU— 11)
Current Treatment Options Fractures of the forearm Anatomic reduction, rigid fixation n PRUJ and DRUJ Anatomic reduction n Early range of motion
Nonoperative treatment n n Conservative treatment of displaced forearm shaft fracture poor functional outcome, 92% Isolated ulnar shaft fracture (<50% displacement, angulation <100) => good satisfactory results, by cast immobilization or functional bracing
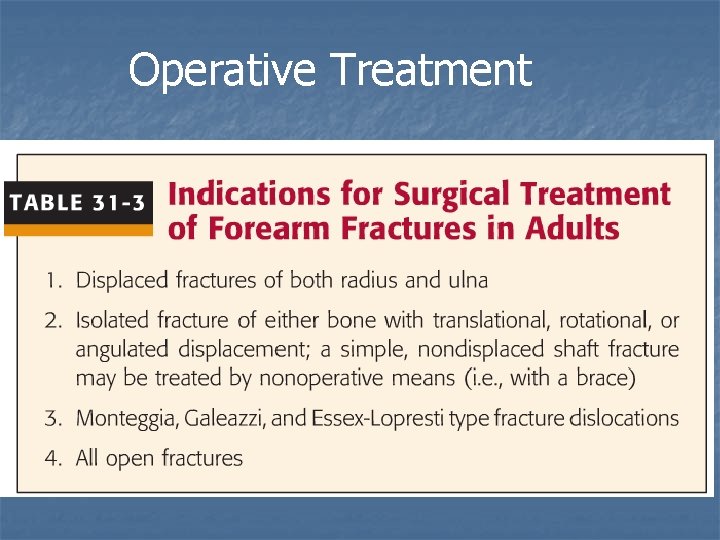
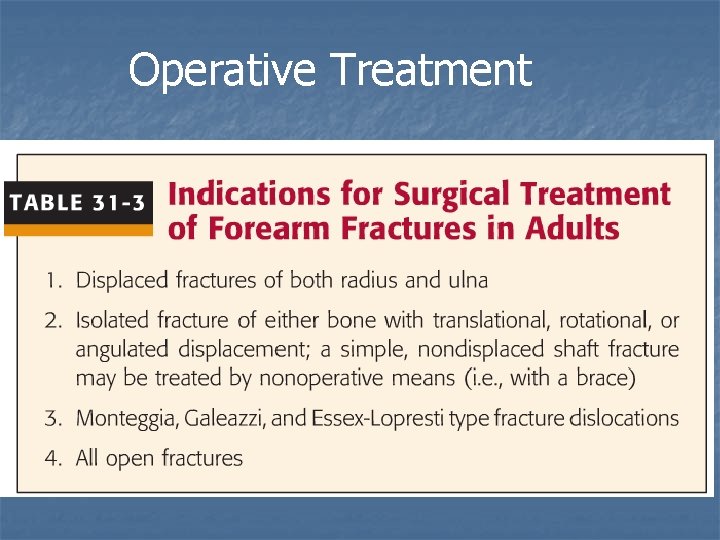
Operative Treatment
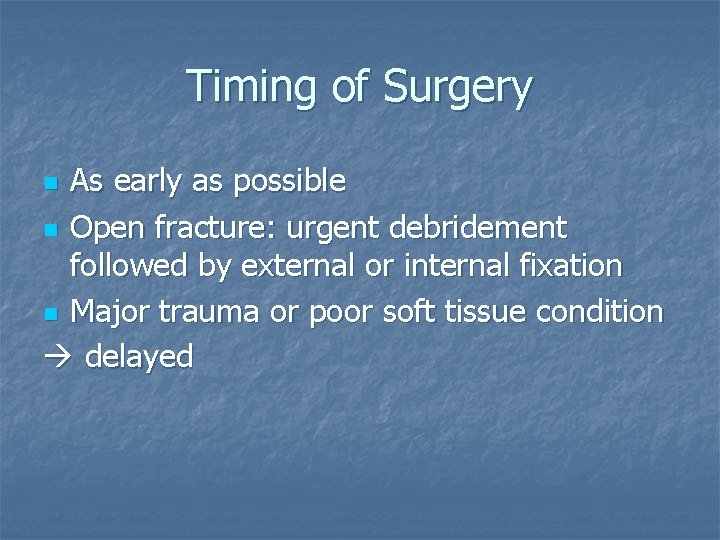
Timing of Surgery As early as possible n Open fracture: urgent debridement followed by external or internal fixation n Major trauma or poor soft tissue condition delayed n
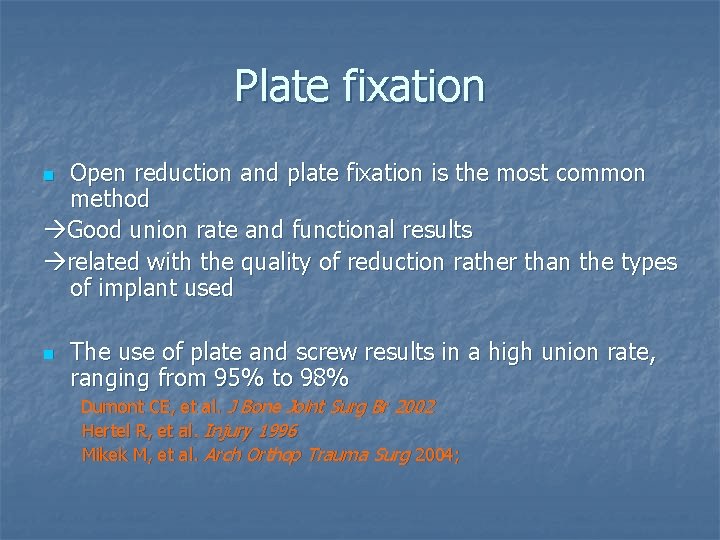
Plate fixation Open reduction and plate fixation is the most common method Good union rate and functional results related with the quality of reduction rather than the types of implant used n n The use of plate and screw results in a high union rate, ranging from 95% to 98% Dumont CE, et al. J Bone Joint Surg Br 2002 Hertel R, et al. Injury 1996 Mikek M, et al. Arch Orthop Trauma Surg 2004;
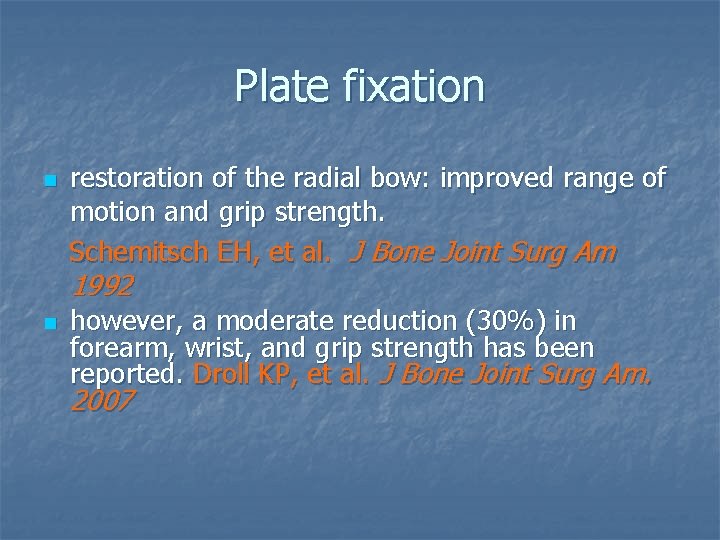
Plate fixation n restoration of the radial bow: improved range of motion and grip strength. Schemitsch EH, et al. J Bone Joint Surg Am 1992 n however, a moderate reduction (30%) in forearm, wrist, and grip strength has been reported. Droll KP, et al. J Bone Joint Surg Am. 2007
Plate fixation n The results are not related with the implants used Limited contact dynamic compression plate (LC-DCP), the point contact fixator (PCFix), locking compression plate (LCP) The current literature lacks good evidence to support one plating technique over another. (OKU-11)
Intramedullary Nailing n n Kirschner wires, steinman pins, Rush pins 20% nonunion rate, poor range of motion, Smith H, Sage FP, 1957 Sage nail 11% delayed or nonunion, Sage FP, 1959 Fore. Sight nail 32 degree loss of rotation, 12. 5% infection rate, Gao et al. 2005 8%, Nonunion rate; 12%, loss of rotation Weckbach, 2006 Treat Nonunion: 47%, unsatisfactory or poor results
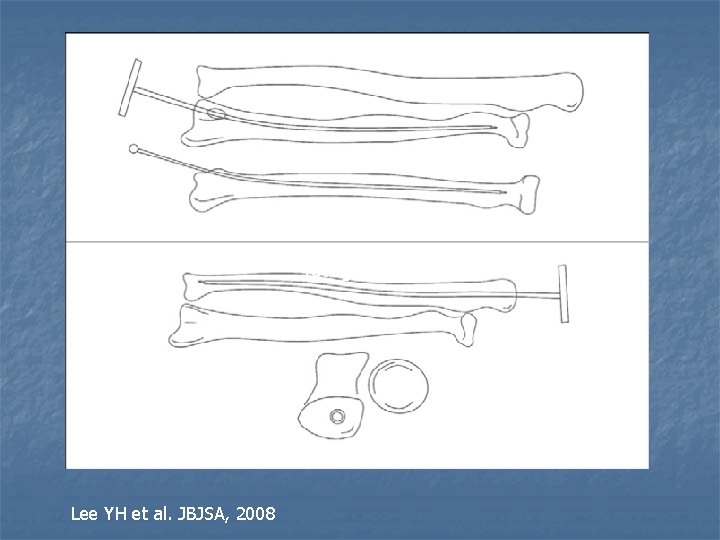
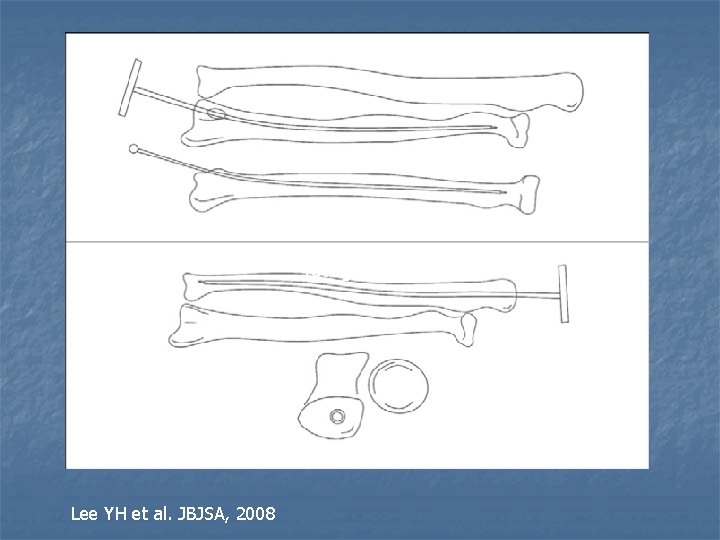
Young Ho Lee, Lee YH et al. JBJSA, 2008
Intramedullary Nailing n n Surgical technique demanding Can not fulfill the surgical goal of restoration of normal bowing, adequate rotational stability, and early mobilization
Intramedullary Nailing n Lee YH, et al. JBJSA, 2008 a high rate of osseous consolidation for simple (noncomminuted) diaphyseal fractures. 81% excellent and 11% good results. the need for a brace and longer periods of immobilization n n The indications : pathologic fractures, segmental fractures, and fractures with poor soft tissue conditions. (Trauma OKU 4) Intramedually device should not be used for fixation of adult Monteggia fractures
External Fixation n n An alternative management of open fracture In severely injured patient for damage control 16. 5% malunion rate, 8. 5% delayed or nonunion rate, Schuind et al, 1991 For temporary fixation : the pins placed at ulna, seldom necessary at the radius Caution not to injury the nerve and artery
Management of Monteggia Fracture Dislocation n n Goal: anatomic relocation of the radial head, with reduction and fixation of the ulna The radial head does not reduce after accurate reduction of the ulna interposition of the annular ligament retract and repair
Management of Monteggia Fracture Dislocation n Historically, poor results : 95% permanent disability, Watson-Jones, 1943 Modern methods of fixation improved the outcomes: 83% excellent or good results. Ring D. et al. 1998 The poor prognostic factors: Bado type 2 fractures, Jupiter type 2 a fractures, radial head fracture, coronoid fracture, ulnohumeral instability
Management of Galeazzi Fracture Dislocation n n Goal: relocation of the DRUJ, anatomic reduction and rigid fixation of the radial fracture reduction of the DRUJ: confirmed by images, 2 planes, and by passive rotation of the forearm
Indications of Possible DRUJ Instability n n n Requirement of forceful reduction A “ mushy” feel of the reduction Fracture at the base of the ulnar styloid Persistent incongruity of the distal ulna on a true lateral view Shortening (> 5 mm) of the radius (Ring et al. 2006) Widening of the DRUJ on an AP view 2 Kirschner wires transfixation, with the forearm in supinatioon Long arm splint For 6 weeks
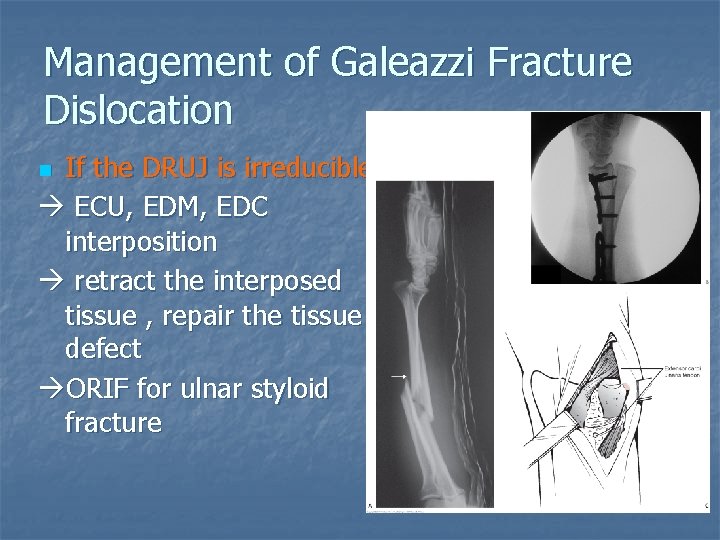
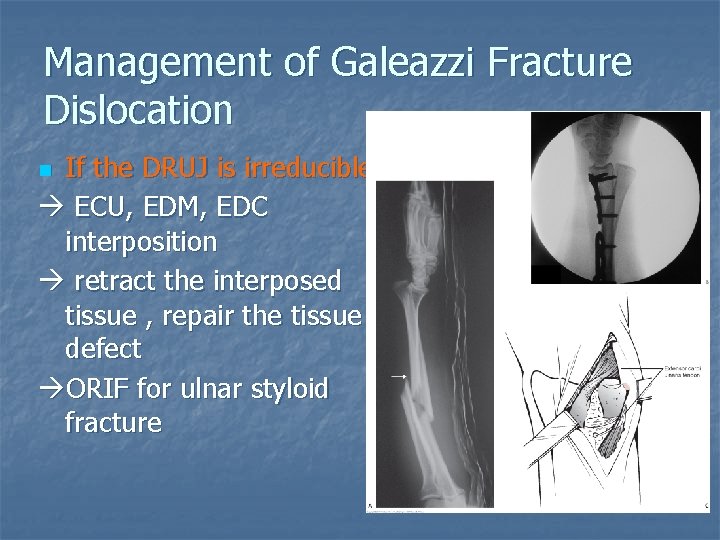
Management of Galeazzi Fracture Dislocation If the DRUJ is irreducible ECU, EDM, EDC interposition retract the interposed tissue , repair the tissue defect ORIF for ulnar styloid fracture n
Management of Galeazzi Fracture Dislocation Results: Moore et al. 1985 averaged restoration of finger grip strength was 71% Complication rate: 39% , Nonunion, malunion, infection, refracture and instability of DRUJ, nerve injury n
Management of Essex-Lopresti Injury n Goals: restoration of the length of the radius and stabilization of the DRUJ Radial head fracture Type 1 : ORIF, Type 2: prosthesis inserted n All concomitant injuries should be dealt n

Management of Essex-Lopresti Injury Early detection and treatment improves the outcome n Late diagnosis: accurate realignment of the radius and ulna, radial head replacement Distal ulnar shortening or Sauve-Kapandji procedure reconstruction of the central band? ? Chloros et al. 2008 n
Management of Open Fractures of the Forearm n n Ø Ø Thorough irrigation and debridement Immediate internal fixation is considered Moed et al. 1986: 4% deep infection, 12@ nounion 85% good to excellent functional outcome Chapman et al. 1989: 2% infection Duncan et al. 1992: recommended immediate plating in grade I, IIIA open fracutre ……

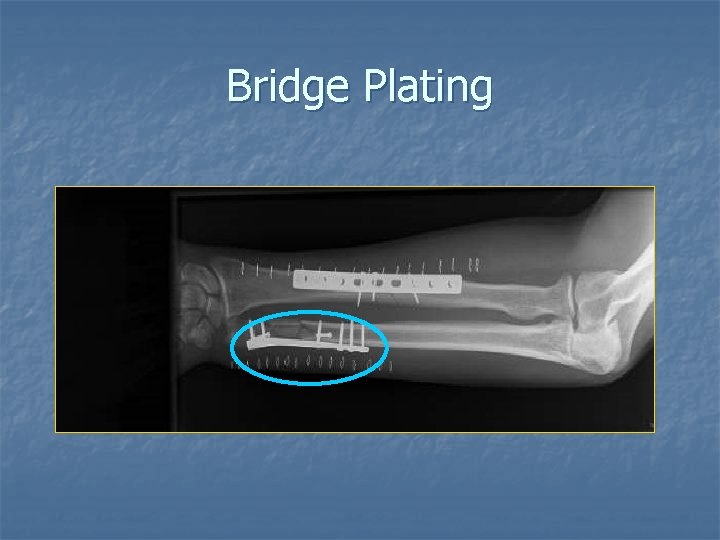
Management of Open Fractures of the Forearm n Severe comminution: bridging plating n Bone graft : a secondary procedure n Soft tissue coverage for the implants
Author’s Preferred Treatment--Open Reduction and Plate Fixation Preoperative Planning: Checklist n n n Properly taken radiographs Correct diagnosis of the fracture including classification Patient positioning Use of tourniquet Reduction tools: pointed reduction clips and bone clamps Which implant and set: 3. 5 mm implant and 2. 7 mm screws n n n Length of the plate and number of screws Need for lag screw or prebent plate Kind of approach Need of bone graft Closure technique Plan of postoperative rehabilitation
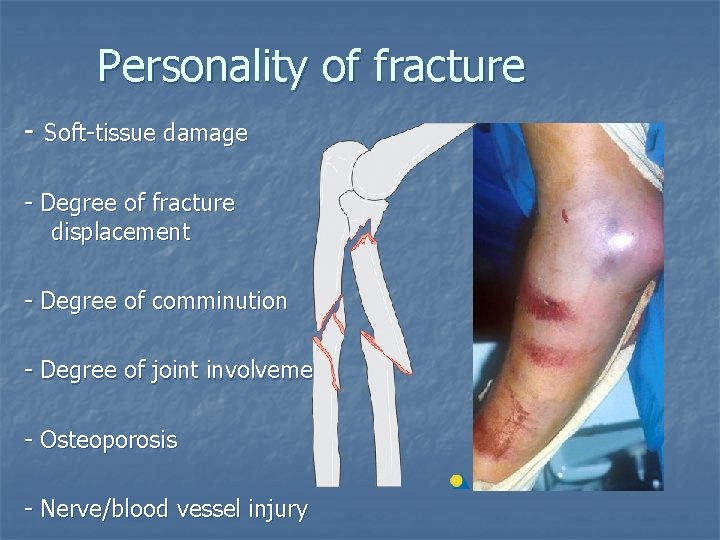
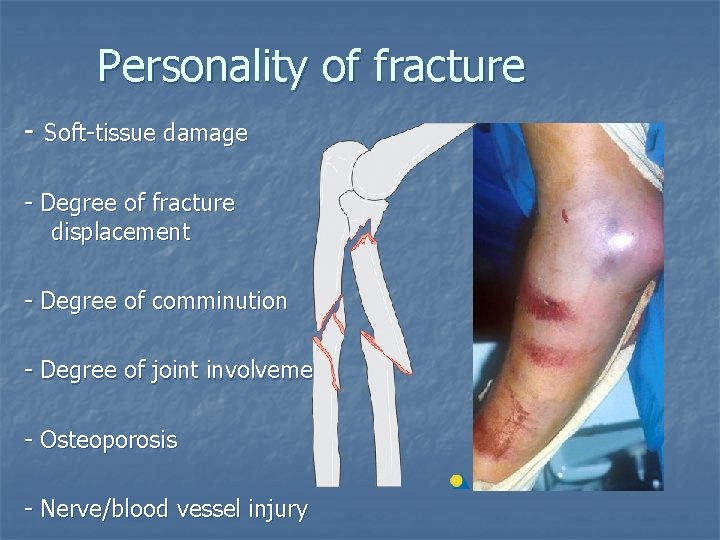
Personality of fracture - Soft-tissue damage - Degree of fracture displacement - Degree of comminution - Degree of joint involvement - Osteoporosis - Nerve/blood vessel injury
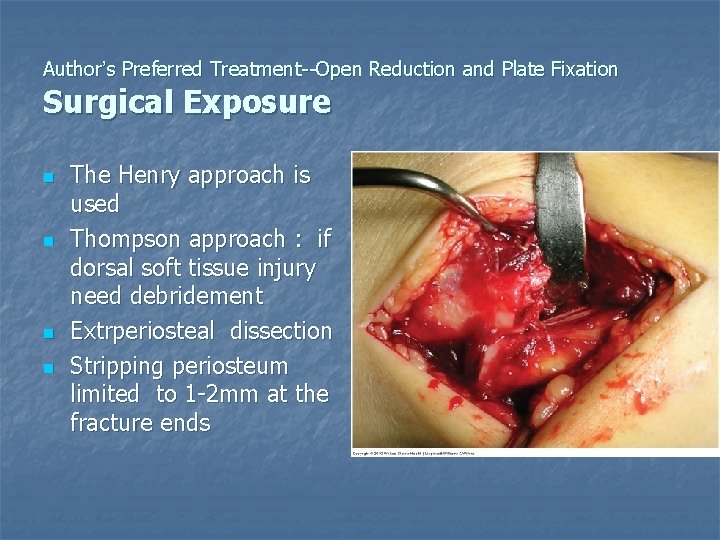
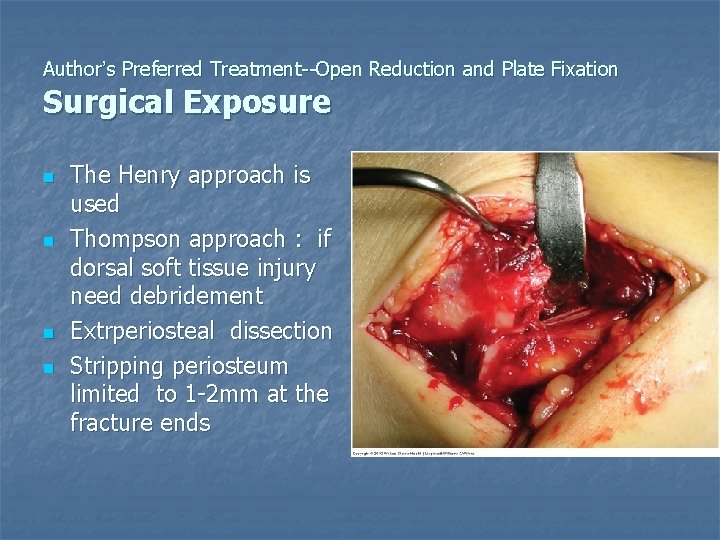
Author’s Preferred Treatment--Open Reduction and Plate Fixation Surgical Exposure n n The Henry approach is used Thompson approach : if dorsal soft tissue injury need debridement Extrperiosteal dissection Stripping periosteum limited to 1 -2 mm at the fracture ends
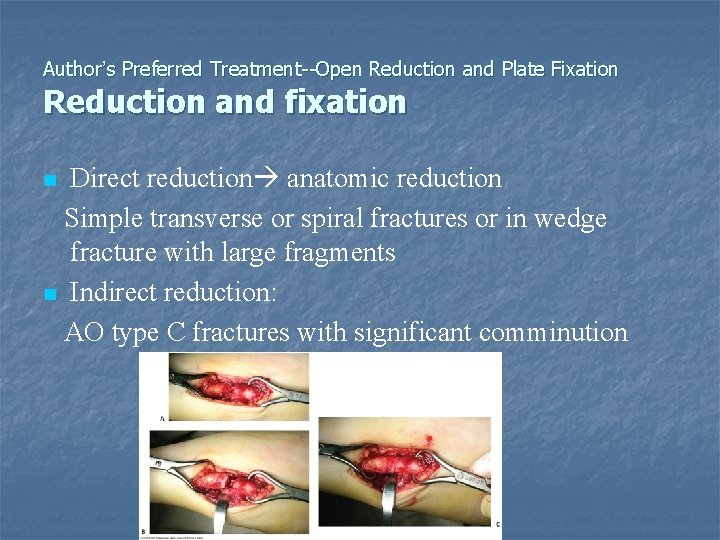
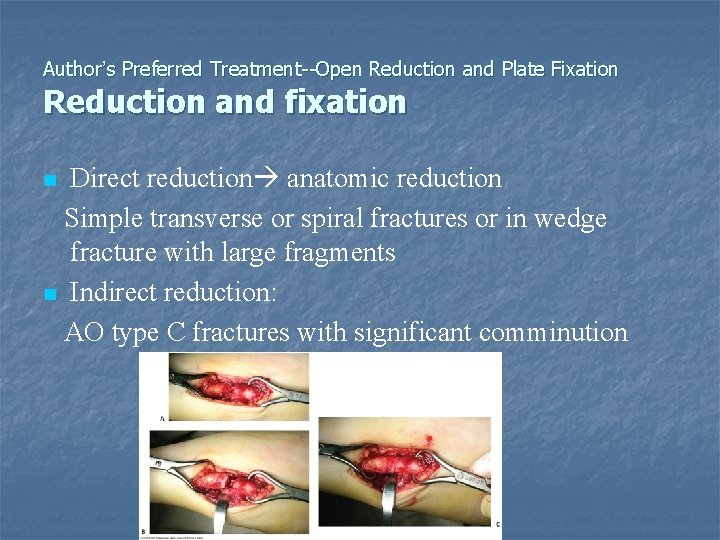
Author’s Preferred Treatment--Open Reduction and Plate Fixation Reduction and fixation Direct reduction anatomic reduction Simple transverse or spiral fractures or in wedge fracture with large fragments n Indirect reduction: AO type C fractures with significant comminution n
Author’s Preferred Treatment--Open Reduction and Plate Fixation Choice of Implant Conventional plating: 6 -7 cortices in each main fragments n Locking plate: at least 4 cortices in each main fragments 2 bicortical screws or 1 bicortical screw with 2 mono cortical screws n
Locked Plating n n Highly comminuted ulna as a “Bridge plate” Helpful in osteoporotic bone, non-unions Increased stiffness…. . Long term effect not known Routine use not appropriate
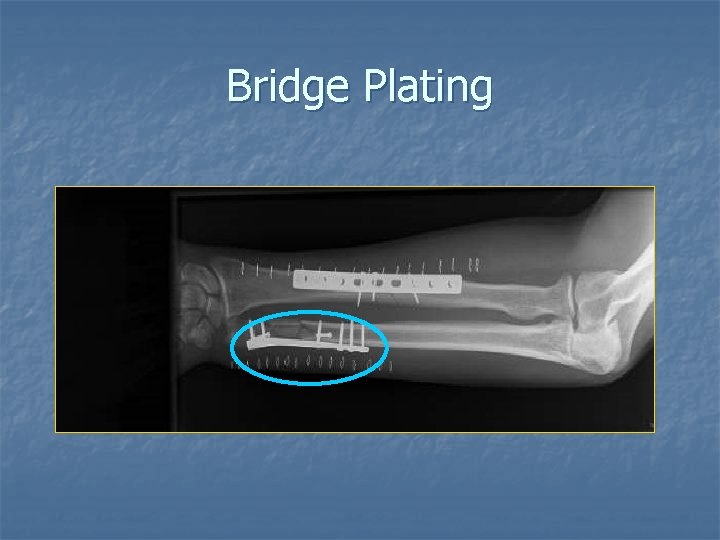
Bridge Plating
Author’s Preferred Treatment--Open Reduction and Plate Fixation Closure and aftercare u • • • u • • Wound closure: avoiding undue tension at edge No need to suture the fascial layer The bone and implant should be covered Aftercare: No splint if the stability is achieved Keep the arm elevated and early active movement of the elbow and wrist
Author’s Preferred Treatment--Open Reduction and Plate Fixation Pearls and Pifalls--- Which bone first? n The less comminution first n The same comminution radius first
Author’s Preferred Treatment--Open Reduction and Plate Fixation Pearls and Pifalls--- Need for Bone Graft n Indications controversial n “Comminution with > 1/3 rd cortical circumference” Anderson et al. , JBJS 1975 n Comminution when interfragmentary screw fixation cannot be achieved n Bone loss or defect with open fracture n Necessity for routine bone grafting recently questioned
Role of Bone Grafting n n Autogenous bone graft did not increase the union rates— Anderson , 1975 Wright et al. (1997) and Wei et al. (1999) “. . Acute bone grafting did not affect the union rate or the time to union” n “. . Routine use of bone graft in comminuted forearm fractures is not indicated” n
Complications of Forearm Fractures n n n n Compartment syndrome Neurovascular injury Infection Nonunion Malunion Refracture Radioulnar Synostosis

Compartment syndrome Relatively uncommon n 10%, Moed and Fakouri, 1991 n Fracture location is the only significantly risk factor In gunshot, proximal third Young man, distal end of the radius n Fasciotomy, volar decompression, single curvilinear incision n Median nerve compression is common n
Neurovascular injury Revascularization is usually unnecessary in a single artery injury n Nerve injury ü The PIN is most common ü most neurapraxias wait for 2 -4 months ü Iatrogenic injury n
Infection Immediate plate fixation of open fracture acceptable risk of infection n If infection does occur, adequate debridement, copious irrigation Antibiotics use Implant removal is not advised if the fixation is stable and the bone is vascularized n
Nonunion n n Inadequate stability or devascularized bone IM nail higher nonunion rate Inappropriate implants ( one third tubular plate), plates of inadequate length, failure of precise reduction, open fracture Nonunion rate < 2% in plate fixation nonunion bone grafting
Malunion Significant loss of function, especially in forearm rotation n IM nailing or closed reduction and cast fixation n Malunion osteotomy and rigid plate fixation good results n
Refracture n n n Remove implant 30% refaracture rate The original fracture site or through an old screw tract Higher risk: Excessively large screws, early removal < 1 year
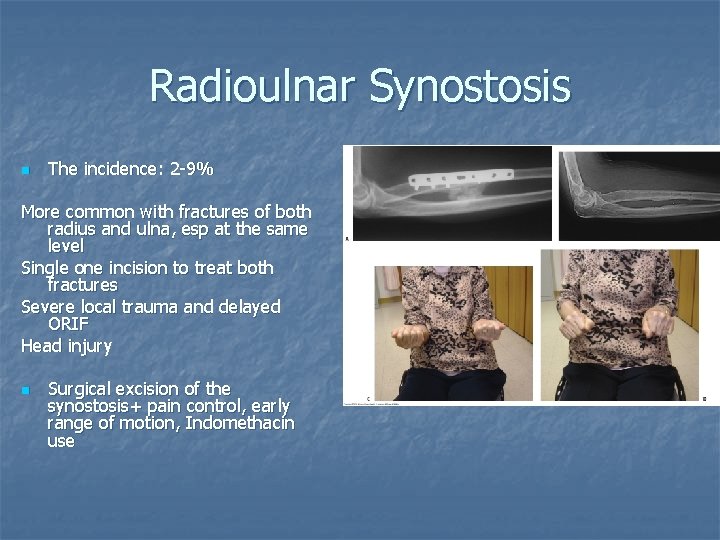
Radioulnar Synostosis n The incidence: 2 -9% More common with fractures of both radius and ulna, esp at the same level Single one incision to treat both fractures Severe local trauma and delayed ORIF Head injury n Surgical excision of the synostosis+ pain control, early range of motion, Indomethacin use
Conclusions n Analysis of fracture mechanism and associated soft- tissue lesions are vital to allow adequate treatment planning n n Complete reconstruction of anatomy is essential to restore normal function Stable fixation with long plates and early movement are the keys to success n Plate fixation gives good results

Further directions n n n Locking implants Interlocking nail Minimal invasive plate osteosynthesis
Reference • • Rockwood and Green's Fracture in Adult -- 7 th Ed OKU 9 OKU 10 OKU 11 Trauma OKU 4 Master technique in orthopaedics surgery, 2 nd Surgical Exposures in Orthopaedics - The Anatomic Approach 3 rd edition. Netter's Concise Atlas of Orthopaedic Anatomy, 1 st ed
 Examples of intentional injury
Examples of intentional injury Tyne and wear crushing contractor
Tyne and wear crushing contractor Crushing a can physical or chemical change
Crushing a can physical or chemical change Connie carter
Connie carter Knee crushing torture devices
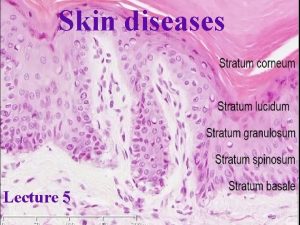
Knee crushing torture devices Stratum lucidum
Stratum lucidum Thin skin vs thick skin
Thin skin vs thick skin Milady facial steps
Milady facial steps English general paper paper 2 comprehension
English general paper paper 2 comprehension Aice general paper practice test
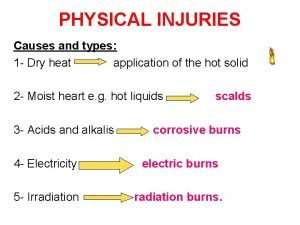
Aice general paper practice test Types of cell injury
Types of cell injury Cellular adaptation
Cellular adaptation Mitochondrial swelling
Mitochondrial swelling Metabolic response to injury
Metabolic response to injury Lifting injury
Lifting injury When a serious customer injury occurs
When a serious customer injury occurs The ability to bend without injury or breakage
The ability to bend without injury or breakage Copyright
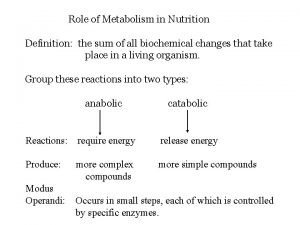
Copyright Metabolism nutrition definition
Metabolism nutrition definition Recurrent laryngeal nerve palsy
Recurrent laryngeal nerve palsy Injury prevention safety and first aid
Injury prevention safety and first aid Low voltage electrical injury
Low voltage electrical injury Intentional injury
Intentional injury Wiki commons
Wiki commons Strained
Strained Biesiedin injury
Biesiedin injury Careless neglect often resulting in injury
Careless neglect often resulting in injury Eat well live well
Eat well live well Equine injury database
Equine injury database Fall astride injury
Fall astride injury Troy injury management
Troy injury management Needle stick injury
Needle stick injury New mexico brain injury resource center
New mexico brain injury resource center Serious injury
Serious injury Which microorganism
Which microorganism Makenzie milton injury
Makenzie milton injury Signet ring sign scaphoid
Signet ring sign scaphoid Pengertian buku register
Pengertian buku register Ebb phase of metabolic response to injury
Ebb phase of metabolic response to injury Facial nerve injury
Facial nerve injury Hops athletic performance
Hops athletic performance Dartos tissue
Dartos tissue Spinal cord injury shoulder exercises
Spinal cord injury shoulder exercises Weinert and kulenkampff sign
Weinert and kulenkampff sign Serious injury
Serious injury Jsp539
Jsp539 Skt aki
Skt aki Thermal injury classification
Thermal injury classification Beveling phenomenon
Beveling phenomenon Enjambment
Enjambment Nrl head injury recognition and referral form
Nrl head injury recognition and referral form Perbedaan rumus mifflin dan harris
Perbedaan rumus mifflin dan harris Myelin figures in reversible cell injury
Myelin figures in reversible cell injury Serious injury and fatality prevention
Serious injury and fatality prevention Unilateral superior laryngeal nerve injury
Unilateral superior laryngeal nerve injury Chapter 5 emergency preparedness injury game plan
Chapter 5 emergency preparedness injury game plan Kavi bhalla
Kavi bhalla Wendy dean moral injury
Wendy dean moral injury Employment injury
Employment injury Injury certificate
Injury certificate Steps in employment based green card
Steps in employment based green card Foosh injury
Foosh injury Most common site of ureteric injury during hysterectomy
Most common site of ureteric injury during hysterectomy Sports injury definition
Sports injury definition Chainsaw injury statistics
Chainsaw injury statistics Soap injury evaluation
Soap injury evaluation St jude brain injury network
St jude brain injury network Subsequent report of injury
Subsequent report of injury Sports injury definition
Sports injury definition Brachial plexus injury classification
Brachial plexus injury classification Endothelial injury
Endothelial injury Restoration of health leave nyc doe
Restoration of health leave nyc doe Poikilothermism and spinal cord injury
Poikilothermism and spinal cord injury Neck injury zone
Neck injury zone Battle's sign
Battle's sign Intentional tort examples
Intentional tort examples Cell injury and inflammation
Cell injury and inflammation What is hops in sports medicine
What is hops in sports medicine Sunset baseball field
Sunset baseball field Cell injury and inflammation
Cell injury and inflammation Magnanimous noun form
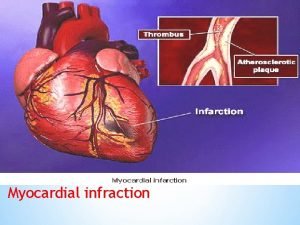
Magnanimous noun form Myocardial infarction
Myocardial infarction