Case Report 39 yearold white male diagnosed with



























- Slides: 91
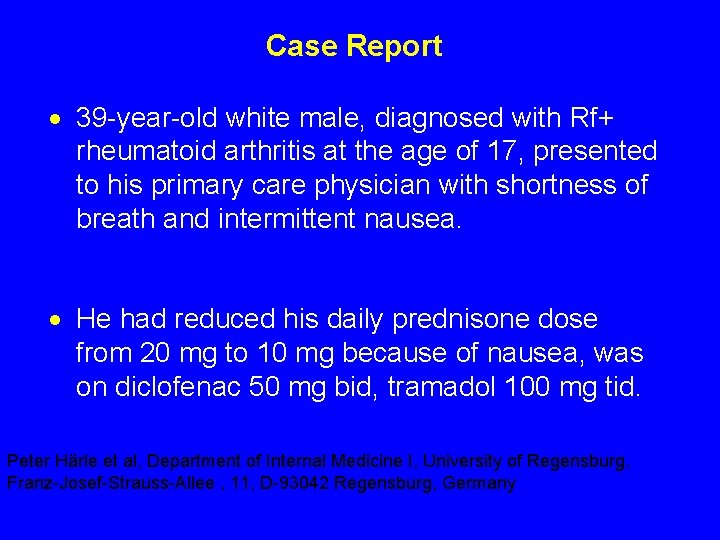
Case Report · 39 -year-old white male, diagnosed with Rf+ rheumatoid arthritis at the age of 17, presented to his primary care physician with shortness of breath and intermittent nausea. · He had reduced his daily prednisone dose from 20 mg to 10 mg because of nausea, was on diclofenac 50 mg bid, tramadol 100 mg tid. Peter Härle et al, Department of Internal Medicine I, University of Regensburg, Franz-Josef-Strauss-Allee , 11, D-93042 Regensburg, Germany
· In addition to steroid therapy, several different disease-modifying drugs were given over the years since diagnosis, including sulfasalazine, oral gold, chloroquine, methotrexate, and TNFinhibitors. · A total of 16 orthopedic operations had been performed including excision of rheumatic nodules, tendon repair, and bilateral knee- and unilateral hip-replacement.
· On exam, he showed signs of extensive rheumatoid arthritis, most marked on hand, foot, and shoulder joints as well as rheumatic nodules on both elbows. · HR regular at 105/min · BP 130/90 mm Hg · ESR 82 mm/h
· A CT-scan and echo revealed a pericardial effusion (1. 5 cm), a thickened pericardium (5 mm), and basal bilateral low-grade lung fibrosis. · Diuretic therapy and increased prednisone dose controlled his symptoms - The pericardial effusion was almost undetectable 4 weeks later.
· Four months later, he was admitted to the hospital because of a sudden onset of abdominal pain. - A perforated NSAID/steroid-induced ulcer was diagnosed and the patient required emergency surgery. · During anesthesia, severe cardiovascular problems developed including low blood pressure, tachycardia, and pre-renal kidney failure. - A left and right heart catheterization was performed subsequently which showed a cardiac index of 2. 4 l/min/m 2, equalization of elevated left and right ventricular diastolic pressures.
· Coronary angiography revealed a 75% obstruction of the diagonal branch. · An MRI-scan showed a thickened pericardium (5 mm), a small pericardial effusion, enlarged right atrium, and bilateral pleural effusions.
· Patient was diagnosed with constrictive pericarditis without a hemodynamic relevant pericardial effusion. · He was referred to CT Surgery - Pericardectomy was suggested. · The patient was informed about the prognosis of this RA-associated complication but declined surgery and was discharged in improved physical condition.
· Repeated hospitalizations were necessary because of clinically dominant right heart failure. · On his last admission, p/w cachexia, extensive edema, tachycardia of 122/min, blood pressure of 105/55 mm Hg, orthopnea, and ascites. · Follow-up heart catheterization revealed a reduced ventricular function with a cardiac index of 1. 46 l/min/m 2.
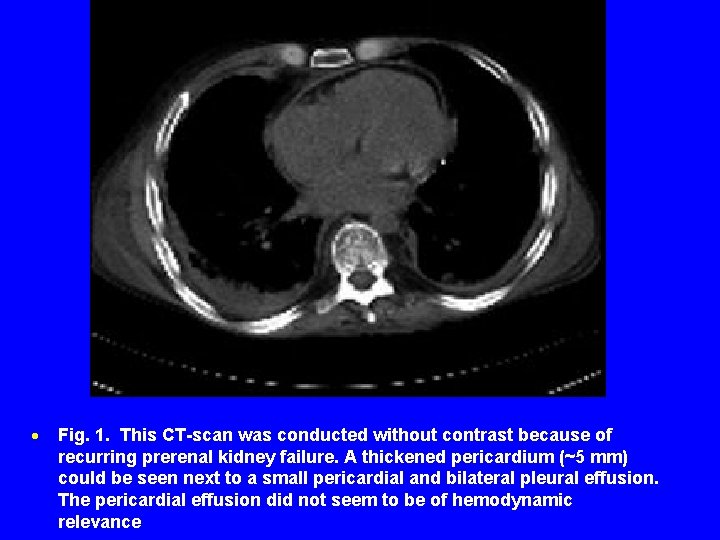
· Surgical intervention was recommended repeatedly but the patient still declined any further procedures. · In the following weeks, the patient had three episodes of renal failure attributable to low median blood pressure (40– 60 mm Hg) together with diuretic therapy - Intermittently required vasopressor medication. · The CT-scan of the chest did not show a hemodynamically relevant pericardial effusion.
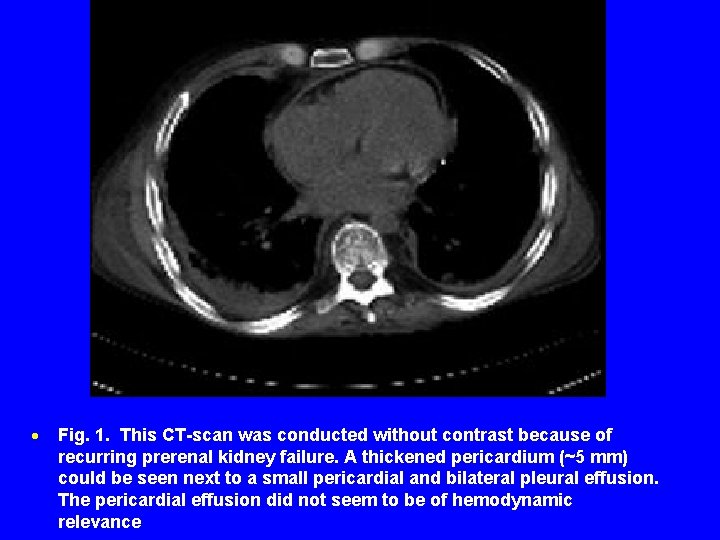
· Fig. 1. This CT-scan was conducted without contrast because of recurring prerenal kidney failure. A thickened pericardium (~5 mm) could be seen next to a small pericardial and bilateral pleural effusion. The pericardial effusion did not seem to be of hemodynamic relevance
· Pt was noted to be adrenally insufficient and have pancreatic insufficiency · In the following weeks, cardiovascular and renal functions were increasingly difficult to stabilize and intermittent dialysis was necessary. · He developed a DVT despite the use of prophylactic heparin and a bilateral pneumonia despite broad-spectrum antibiotic therapy. · The patient died in septic shock combined with multi-organ failure.
· The patient died 2 years after the onset of extra-articular cardiac symptoms. · Pericarditis is a frequent extra-articular manifestation of rheumatoid arthritis showing a post-mortem prevalence of 30%– 50%. - These findings correlate well with echocardiographic diagnosis in living patients. However, clinically relevant symptoms are rare with a prevalence of 0. 06%– 3% of all RA patients · This case demonstrates the devastating course of progressive constrictive pericarditis under sole medical therapy and emphasizes the importance of early radical pericardectomy to avoid progression of disease and secondary complications with fatal outcome.
Rheumatoid Arthritis Julie Schwartzman, MD
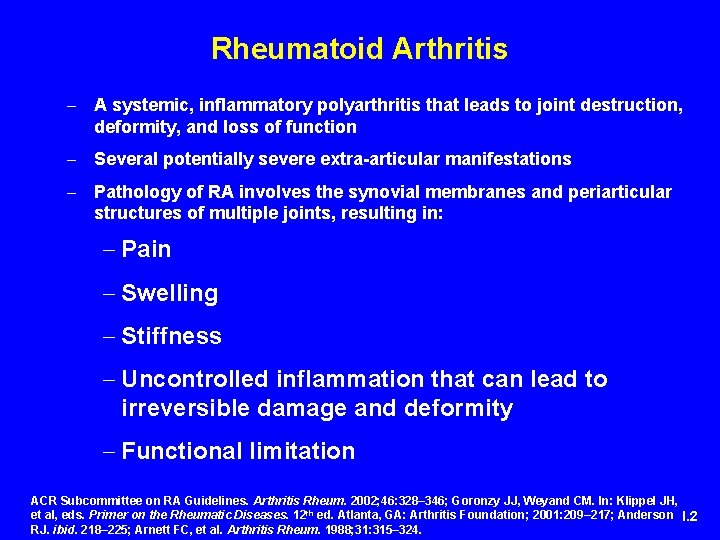
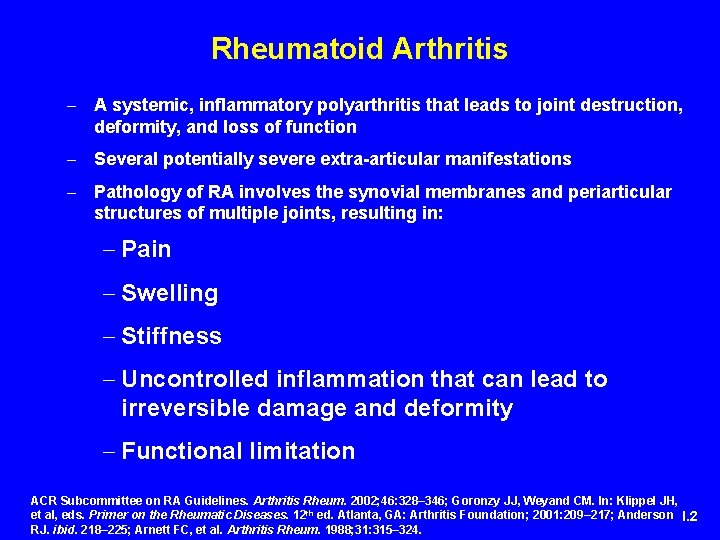
Rheumatoid Arthritis - A systemic, inflammatory polyarthritis that leads to joint destruction, deformity, and loss of function - Several potentially severe extra-articular manifestations - Pathology of RA involves the synovial membranes and periarticular structures of multiple joints, resulting in: - Pain - Swelling - Stiffness - Uncontrolled inflammation that can lead to irreversible damage and deformity - Functional limitation ACR Subcommittee on RA Guidelines. Arthritis Rheum. 2002; 46: 328– 346; Goronzy JJ, Weyand CM. In: Klippel JH, et al, eds. Primer on the Rheumatic Diseases. 12 th ed. Atlanta, GA: Arthritis Foundation; 2001: 209– 217; Anderson I. 2 RJ. ibid. 218– 225; Arnett FC, et al. Arthritis Rheum. 1988; 31: 315– 324.
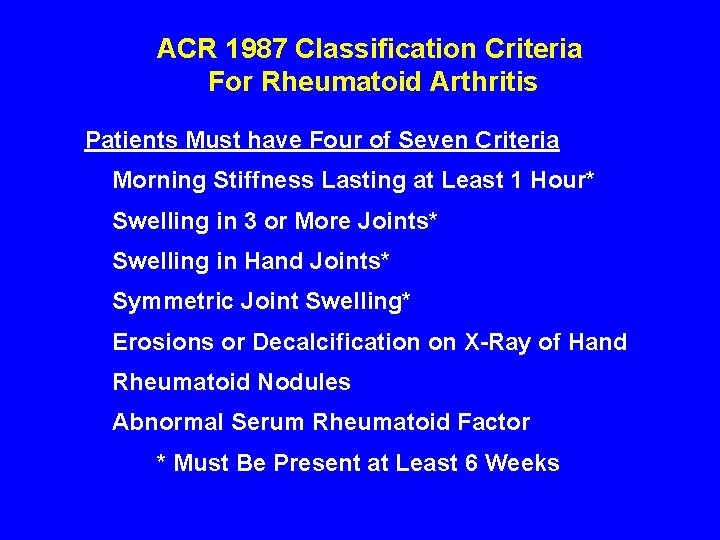
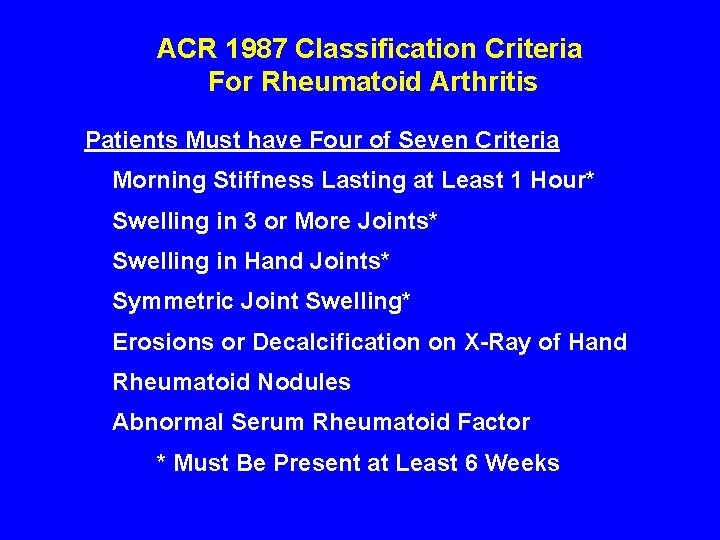
ACR 1987 Classification Criteria For Rheumatoid Arthritis Patients Must have Four of Seven Criteria Morning Stiffness Lasting at Least 1 Hour* Swelling in 3 or More Joints* Swelling in Hand Joints* Symmetric Joint Swelling* Erosions or Decalcification on X-Ray of Hand Rheumatoid Nodules Abnormal Serum Rheumatoid Factor * Must Be Present at Least 6 Weeks
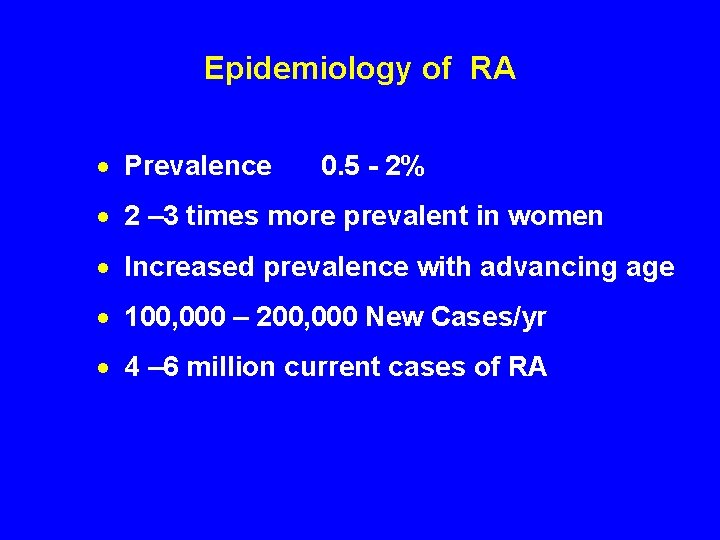
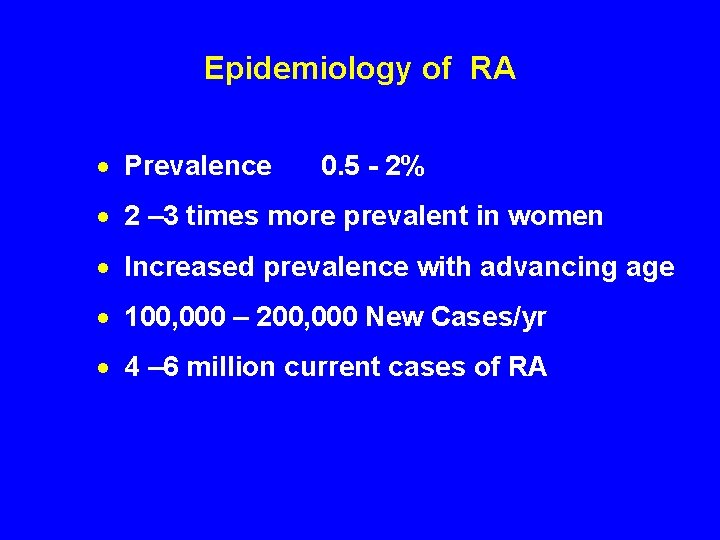
Epidemiology of RA · Prevalence 0. 5 - 2% · 2 – 3 times more prevalent in women · Increased prevalence with advancing age · 100, 000 – 200, 000 New Cases/yr · 4 – 6 million current cases of RA
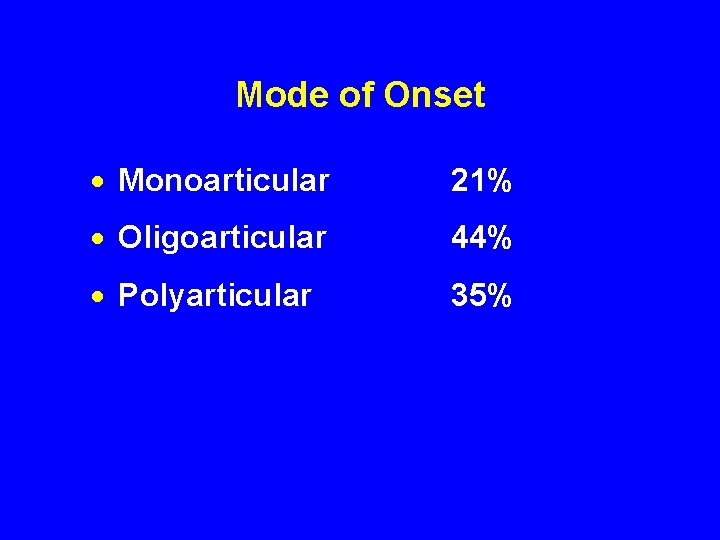
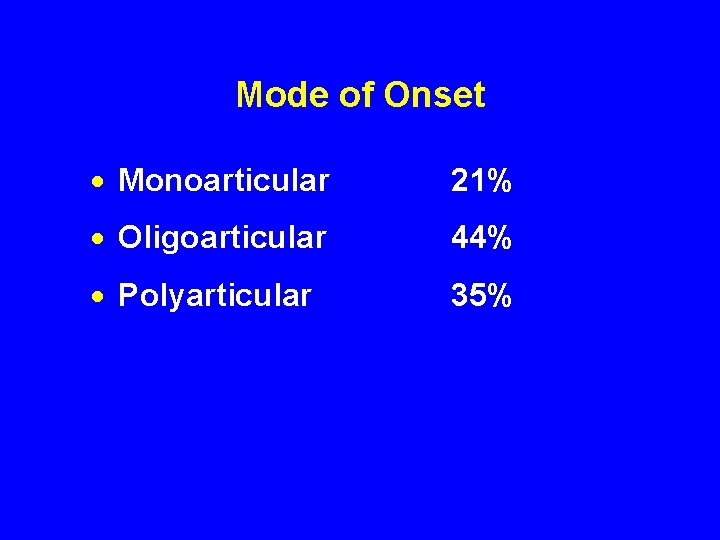
Mode of Onset · Monoarticular 21% · Oligoarticular 44% · Polyarticular 35%
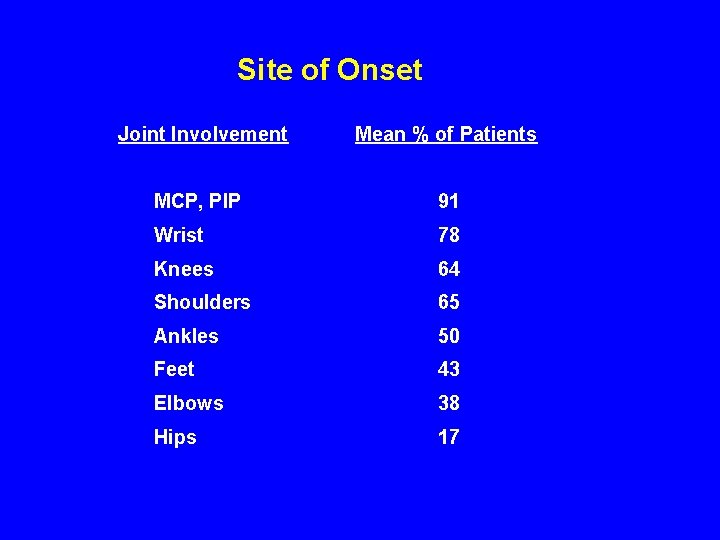
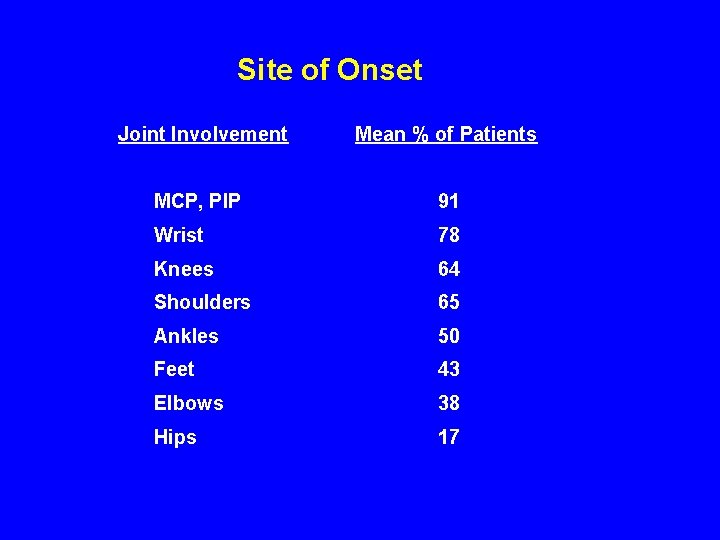
Site of Onset Joint Involvement Mean % of Patients MCP, PIP 91 Wrist 78 Knees 64 Shoulders 65 Ankles 50 Feet 43 Elbows 38 Hips 17
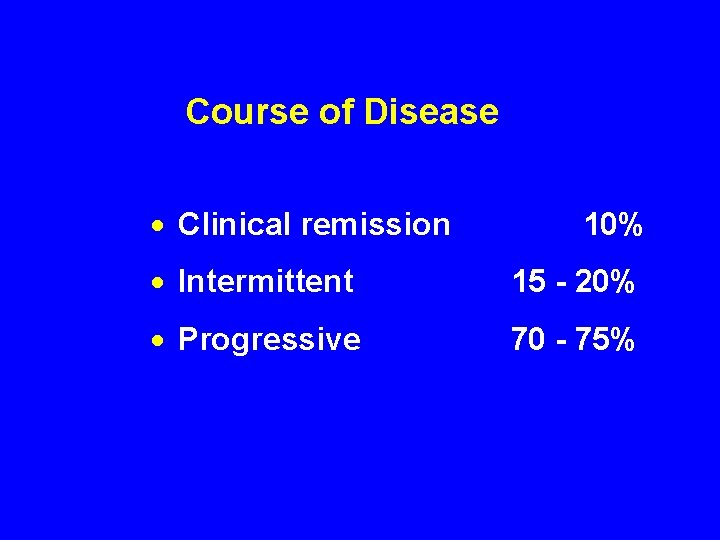
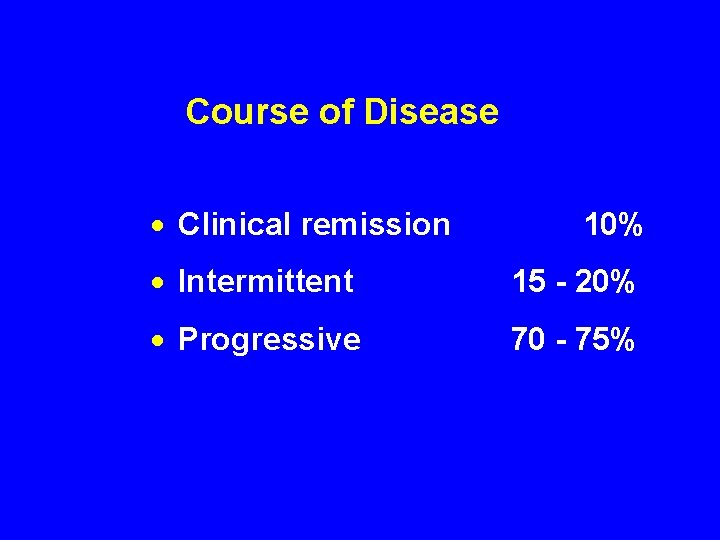
Course of Disease · Clinical remission 10% · Intermittent 15 - 20% · Progressive 70 - 75%












Extra-articular Manifestations of Rheumatoid Arthritis



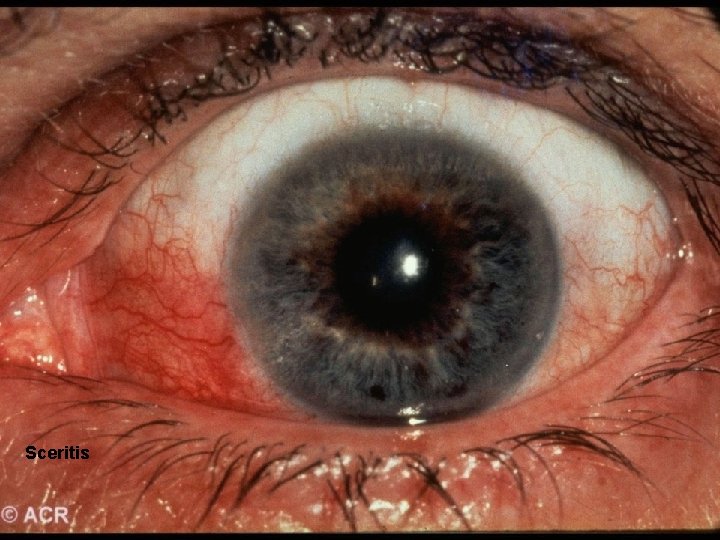
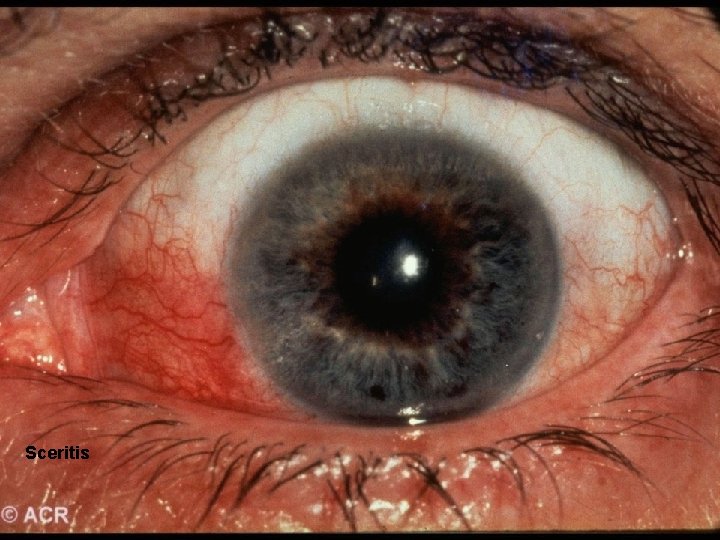
Sceritis
Secondary Sjögren’s Syndrome · SICCA · Pleuritis/ Pericarditis · Ro/La positive · Hypergammaglobulinemia


Vasculitis · Digital vasculitis · Cutaneous ulceration · Peripheral neuropathy · Mononeuritis multiplex


Pulmonary Involvement · Pleural Disease · Interstitial fibrosis · Nodules · Pneumonitis

Cardiac Involvement · Pericarditis · Myositis · Endocardial Inflammation · Conduction Defects
Articular Manifestations: Synovial Fluid Analysis · Straw colored to slightly cloudy · WBC 5000 – 25, 000/ mm 3 · Rheumatoid Factor · Elevated protein · Decreased glucose
Laboratory Presentation · Leukocytosis · Eosinophilia · Thrombocytosis · Mild Anemia · ESR > 30 mm/hr · Normal renal and hepatic function · Negative ANA · Rheumatoid Factor
Anti-Cyclic Citrullinated Peptide (CCP) Antibodies · High diagnostic specificity (>98%) and sensitivity · Presence in 65% of early RA, with the same specificity · Prognosis value linked to the most erosive forms
Differential Diagnosis · Seronegative polyarthritis - Psoriatic Arthritis - Reiter’s Syndrome · Chondrocalcinosis · Gout · Behcet’s Syndrome · Infectious Arthritis · Thyroid Disease · Malignancies · Polymyalgia Rheumatica · Hemochromatosis
Baseline Evaluation · 43 yo AAF came to PMD, reports 4 mo. h/o bilateral wrist and knee pain. · Occasional swelling in wrists and “knuckles” · No PMH · Takes tylenol for pain w/o relief · BASELINE EVALUATION: Important questions
Baseline Evaluation of Patients · Subjective/History - Degree of joint pain/swelling symmetry? # joints involved? - Presence/Duration of morning stiffness - Presence of fatigue - Limitation of function - H/o SICCA symptoms? Recent GI/GU infection? Sexual Activity?
Baseline Evaluation of Patients · Physical Exam · Essential Assessments
Baseline Evaluation of Patients · Physical Examination - Documentation of actively inflamed joints - Documentation of mechanical joint problems: loss of motion, crepitus, instability, deformity - Documentation of extra-articular manifestations - Optho, cardiac, pulmonary, rash, LAD
Baseline Evaluation of Patients · LABS/STUDIES
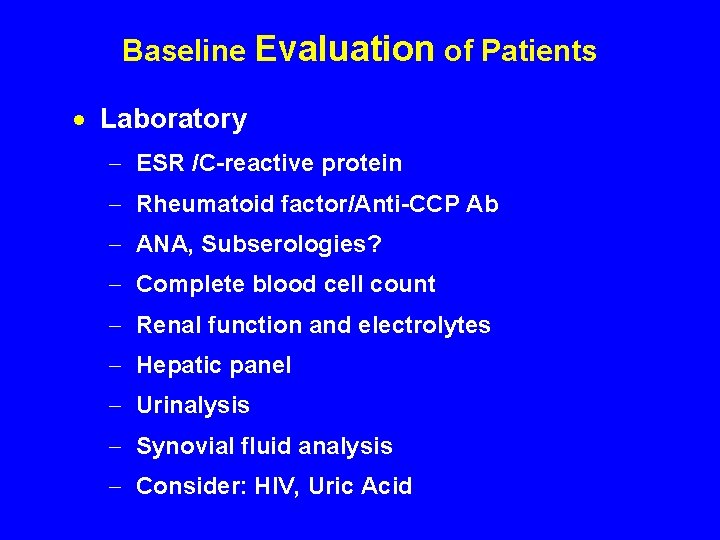
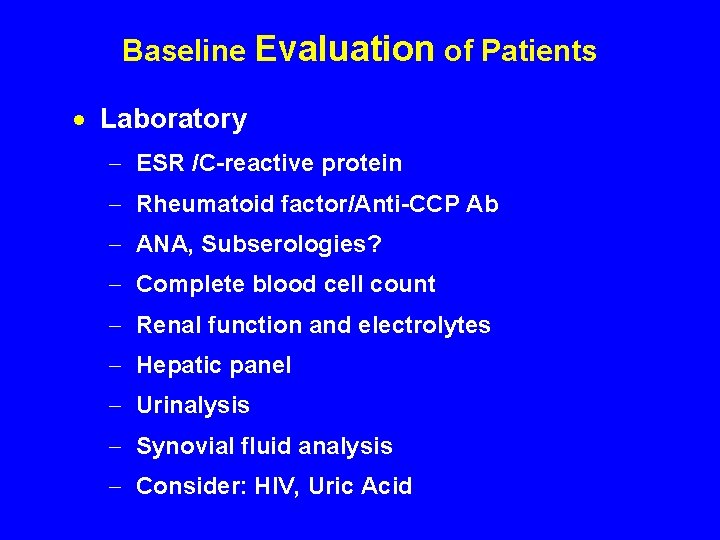
Baseline Evaluation of Patients · Laboratory - ESR /C-reactive protein - Rheumatoid factor/Anti-CCP Ab - ANA, Subserologies? - Complete blood cell count - Renal function and electrolytes - Hepatic panel - Urinalysis - Synovial fluid analysis - Consider: HIV, Uric Acid
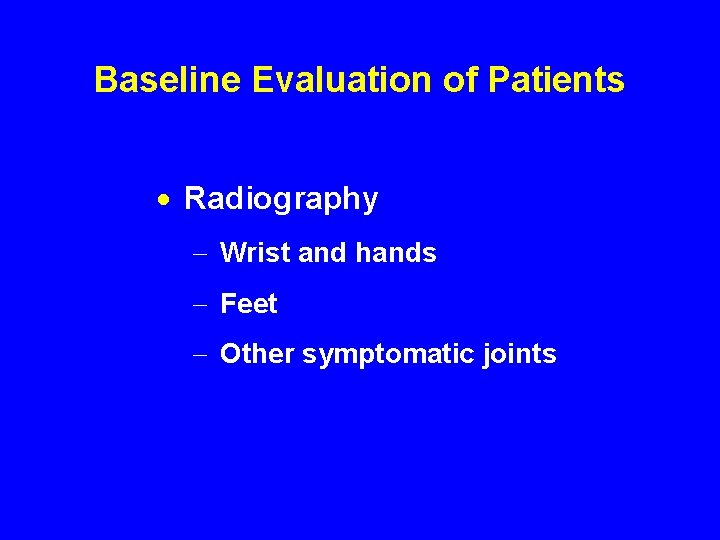
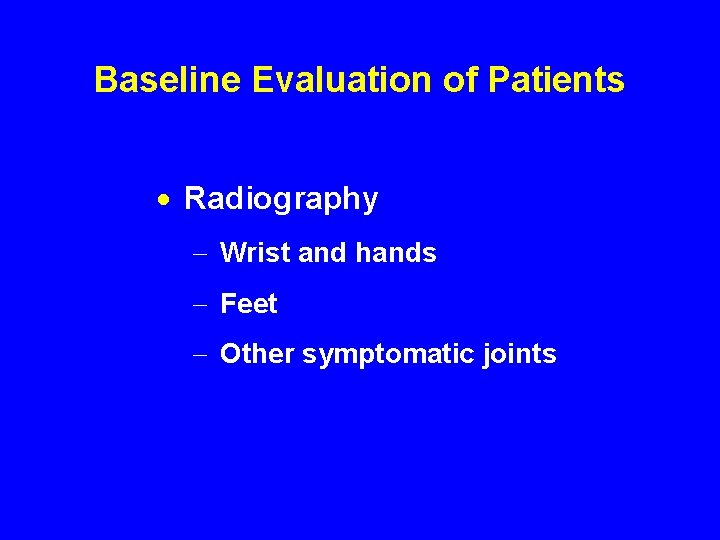
Baseline Evaluation of Patients · Radiography - Wrist and hands - Feet - Other symptomatic joints
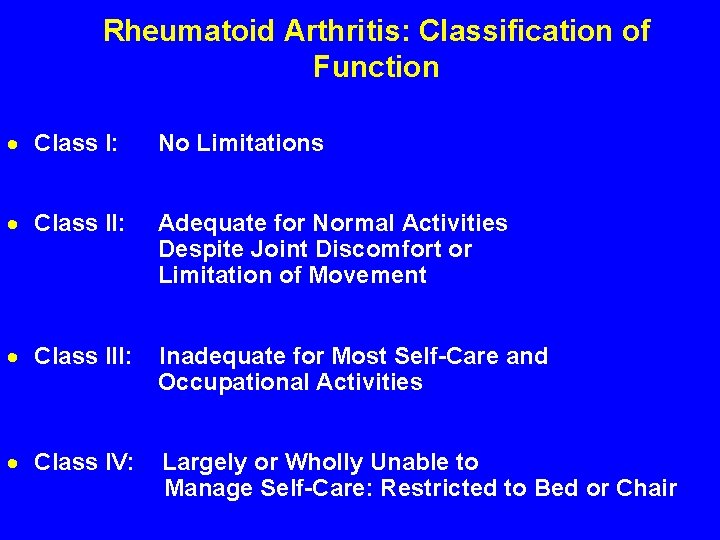
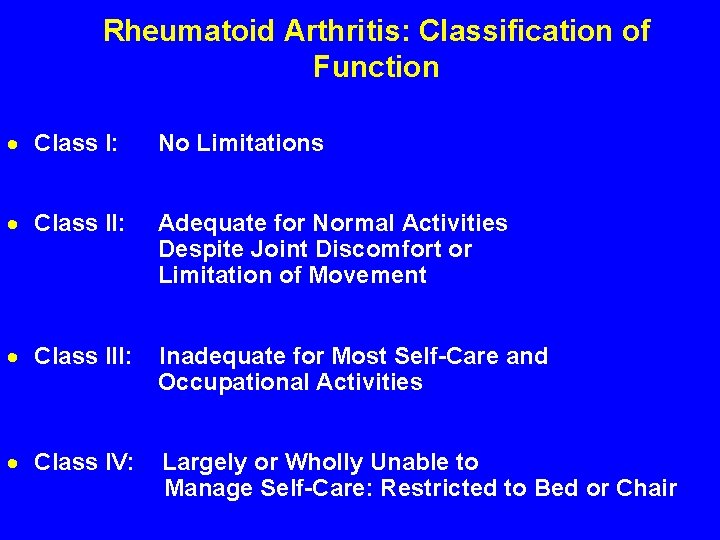
Rheumatoid Arthritis: Classification of Function · Class I: No Limitations · Class II: Adequate for Normal Activities Despite Joint Discomfort or Limitation of Movement · Class III: Inadequate for Most Self-Care and Occupational Activities · Class IV: Largely or Wholly Unable to Manage Self-Care: Restricted to Bed or Chair
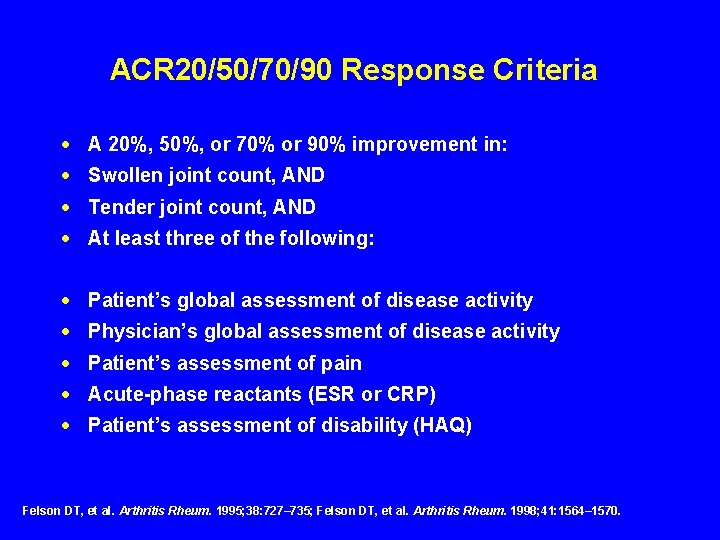
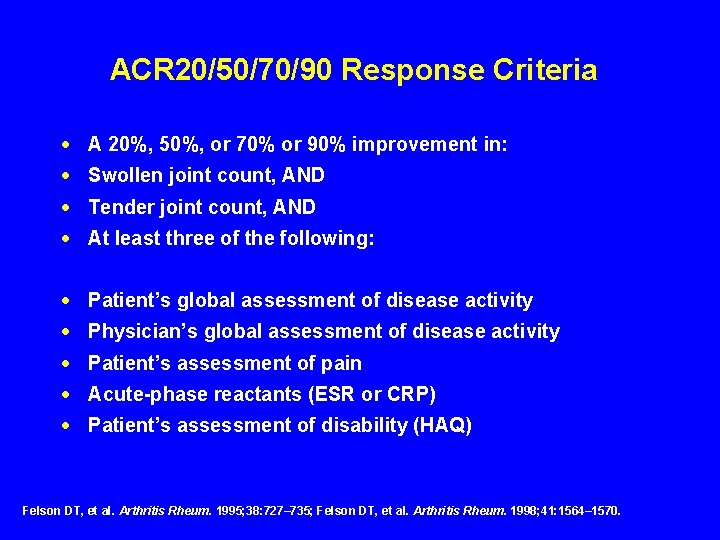
ACR 20/50/70/90 Response Criteria · A 20%, 50%, or 70% or 90% improvement in: · Swollen joint count, AND · Tender joint count, AND · At least three of the following: · Patient’s global assessment of disease activity · Physician’s global assessment of disease activity · Patient’s assessment of pain · Acute-phase reactants (ESR or CRP) · Patient’s assessment of disability (HAQ) Felson DT, et al. Arthritis Rheum. 1995; 38: 727– 735; Felson DT, et al. Arthritis Rheum. 1998; 41: 1564– 1570.
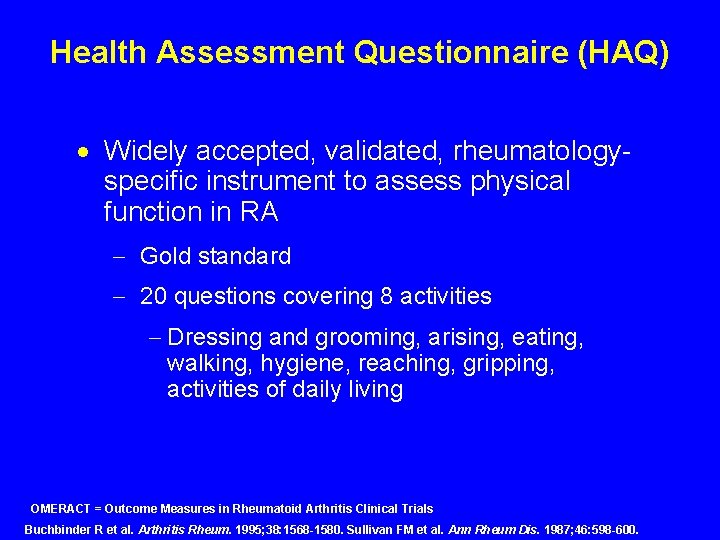
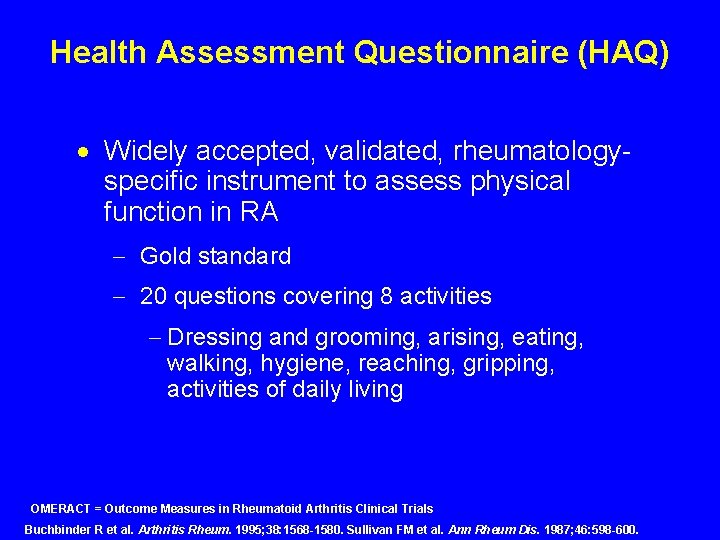
Health Assessment Questionnaire (HAQ) · Widely accepted, validated, rheumatologyspecific instrument to assess physical function in RA - Gold standard - 20 questions covering 8 activities - Dressing and grooming, arising, eating, walking, hygiene, reaching, gripping, activities of daily living OMERACT = Outcome Measures in Rheumatoid Arthritis Clinical Trials Buchbinder R et al. Arthritis Rheum. 1995; 38: 1568 -1580. Sullivan FM et al. Ann Rheum Dis. 1987; 46: 598 -600.
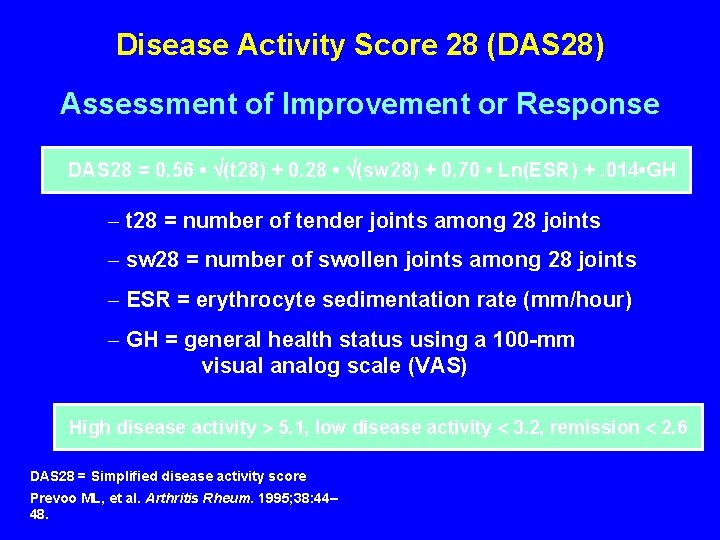
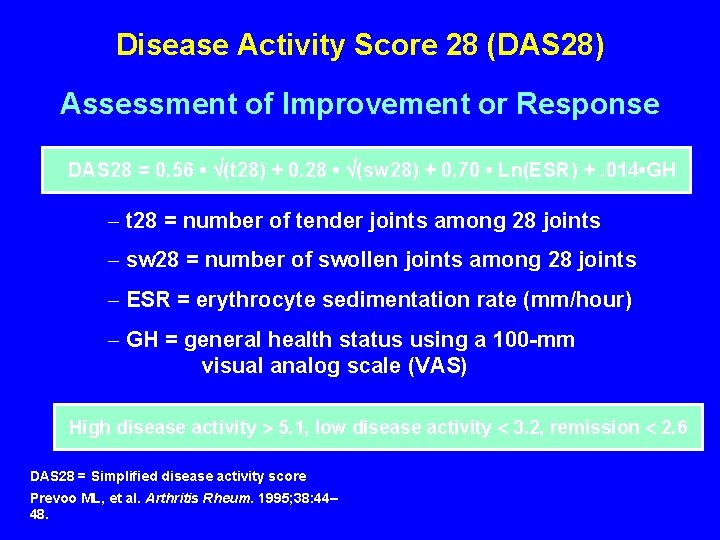
Disease Activity Score 28 (DAS 28) Assessment of Improvement or Response DAS 28 = 0. 56 • (t 28) + 0. 28 • (sw 28) + 0. 70 • Ln(ESR) +. 014 • GH - t 28 = number of tender joints among 28 joints - sw 28 = number of swollen joints among 28 joints - ESR = erythrocyte sedimentation rate (mm/hour) - GH = general health status using a 100 -mm visual analog scale (VAS) High disease activity 5. 1, low disease activity 3. 2, remission 2. 6 DAS 28 = Simplified disease activity score Prevoo ML, et al. Arthritis Rheum. 1995; 38: 44– 48.
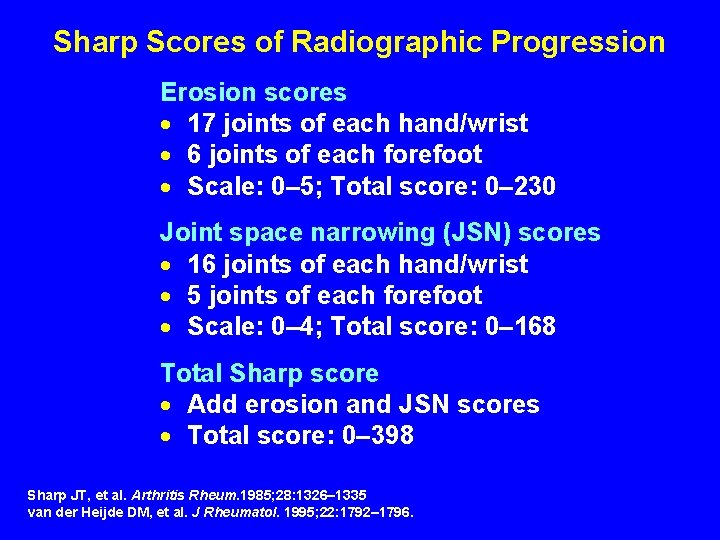
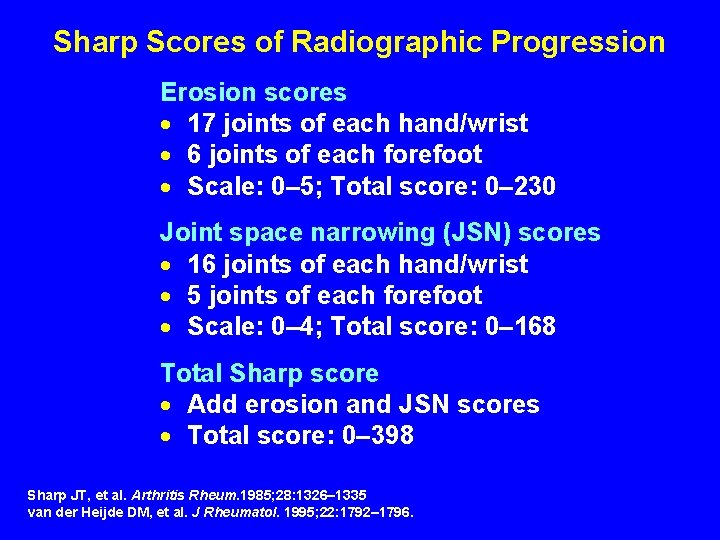
Sharp Scores of Radiographic Progression Erosion scores · 17 joints of each hand/wrist · 6 joints of each forefoot · Scale: 0– 5; Total score: 0– 230 Joint space narrowing (JSN) scores · 16 joints of each hand/wrist · 5 joints of each forefoot · Scale: 0– 4; Total score: 0– 168 Total Sharp score · Add erosion and JSN scores · Total score: 0– 398 Sharp JT, et al. Arthritis Rheum. 1985; 28: 1326– 1335 van der Heijde DM, et al. J Rheumatol. 1995; 22: 1792– 1796.
Prognostic Markers in RA · Early Markers - Generalized onset with numerous joints involved - Systemic involvement including fatigue, fever, weight loss, morning stiffness - Elevated CRP or ESR - Positive test for rheumatoid factor/Anti. CCP - Early erosions, JSN - HLA-DR 4 genetic marker
Prognostic Markers in RA · Later Markers - Involvement of more joints - Increased morning stiffness - Rheumatoid factor 1: 160 or greater - Anemia and thrombocytosis
Prognostic Markers in RA · Definitive Markers - Subcutaneous nodules - Detection of erosions on x-ray
The Importance of Early Diagnosis · RA is progressive, not benign · Structural damage and disability occurs within first two to three years of disease · Slower progression of disease is linked to early treatment with DMARDs, Biologic Agents
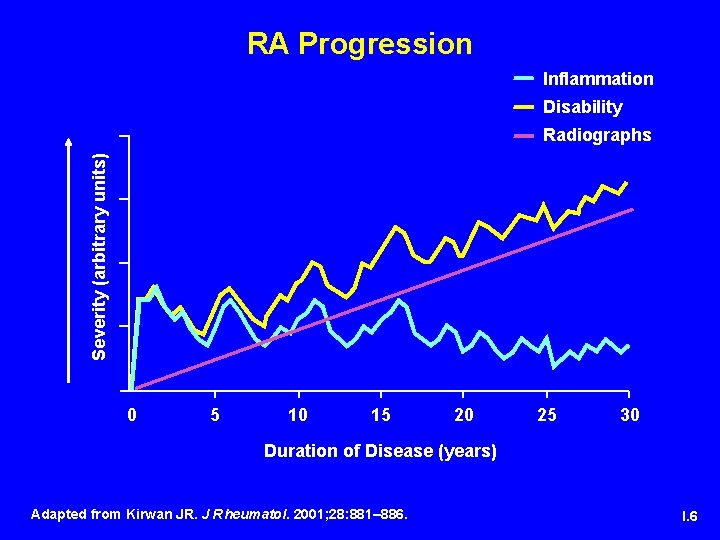
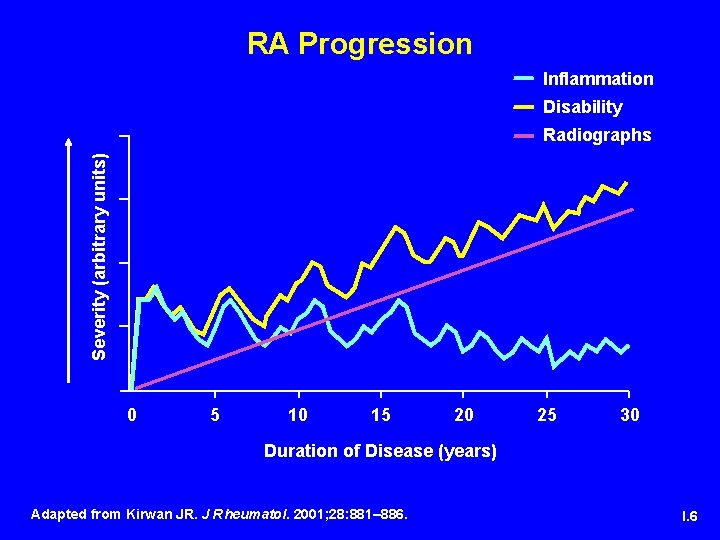
RA Progression Inflammation Disability Severity (arbitrary units) Radiographs 0 5 10 15 20 25 30 Duration of Disease (years) Adapted from Kirwan JR. J Rheumatol. 2001; 28: 881– 886. I. 6
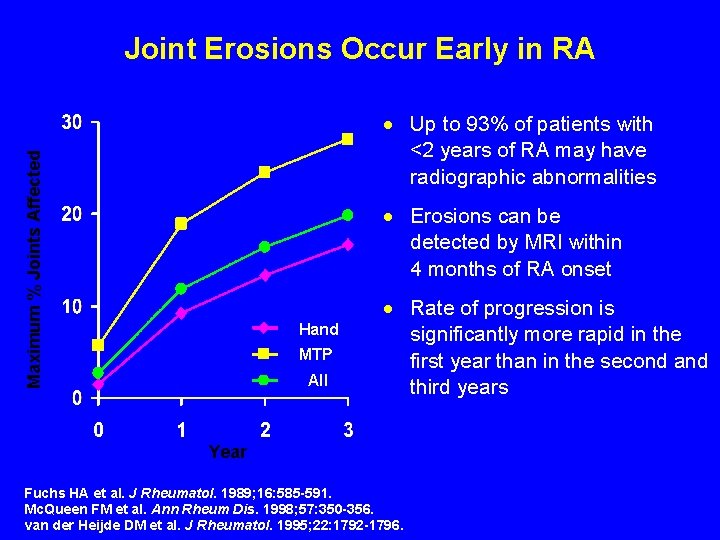
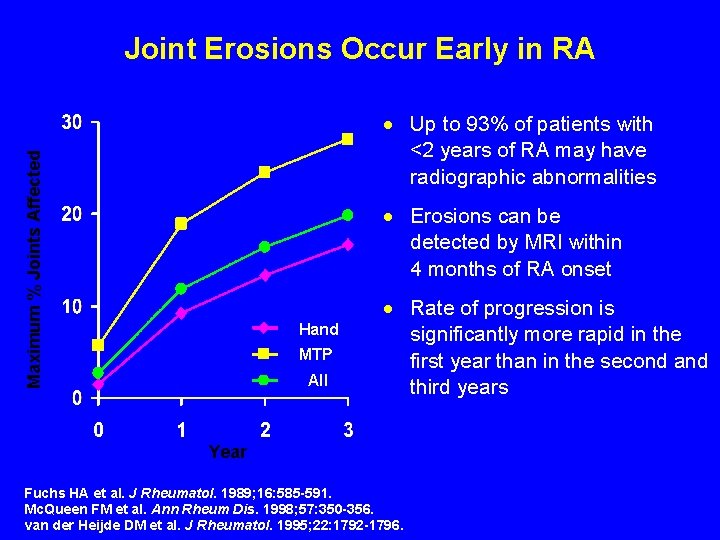
Joint Erosions Occur Early in RA Maximum % Joints Affected · Up to 93% of patients with <2 years of RA may have radiographic abnormalities · Erosions can be detected by MRI within 4 months of RA onset Hand MTP All · Rate of progression is significantly more rapid in the first year than in the second and third years Year Fuchs HA et al. J Rheumatol. 1989; 16: 585 -591. Mc. Queen FM et al. Ann Rheum Dis. 1998; 57: 350 -356. van der Heijde DM et al. J Rheumatol. 1995; 22: 1792 -1796.
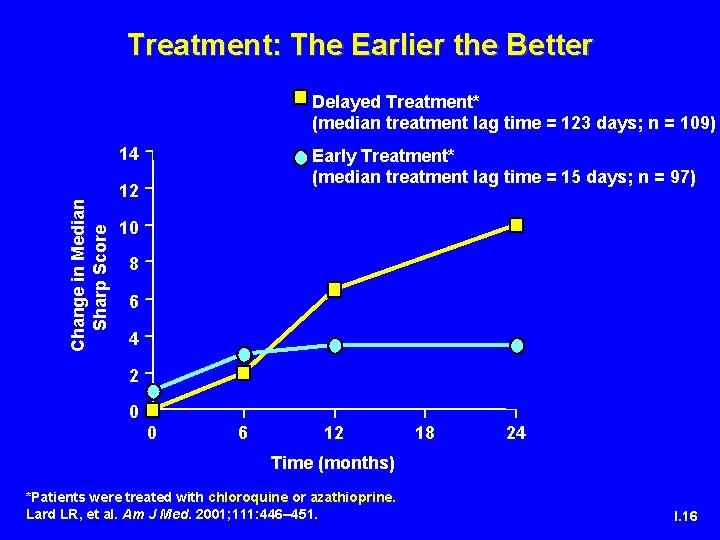
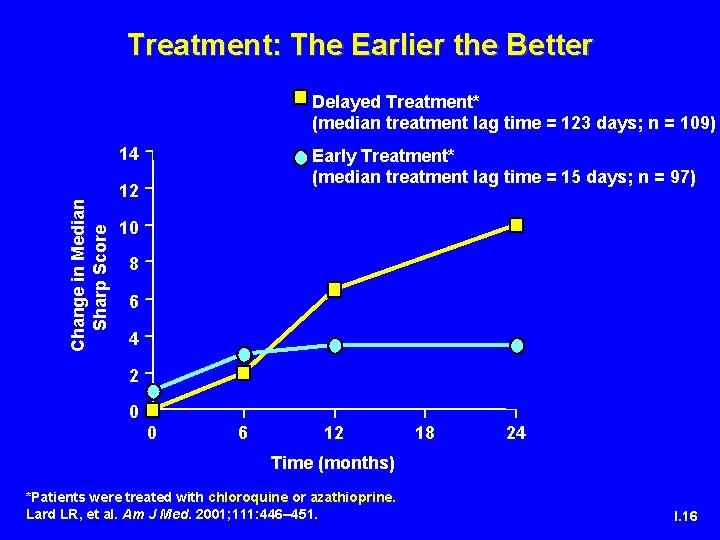
Treatment: The Earlier the Better Delayed Treatment* (median treatment lag time = 123 days; n = 109) Change in Median Sharp Score 14 Early Treatment* (median treatment lag time = 15 days; n = 97) 12 10 8 6 4 2 0 0 6 12 18 24 Time (months) *Patients were treated with chloroquine or azathioprine. Lard LR, et al. Am J Med. 2001; 111: 446– 451. I. 16

The Goals of Treatment · Eliminate synovitis and disease activity · Improve symptoms · Prevent joint damage · Prevent or reduce disability · Prevent or reduce other adverse outcomes Adapted from Wolfe F et al. J Rheumatol. 2001; 28: 1423.

Current Treatment Options · Nonsteroidal Anti-inflammatory Drugs (NSAIDs) · Corticosteroids · Disease Modifying Anti-rheumatic Drugs (DMARDs) · Biologic Agents
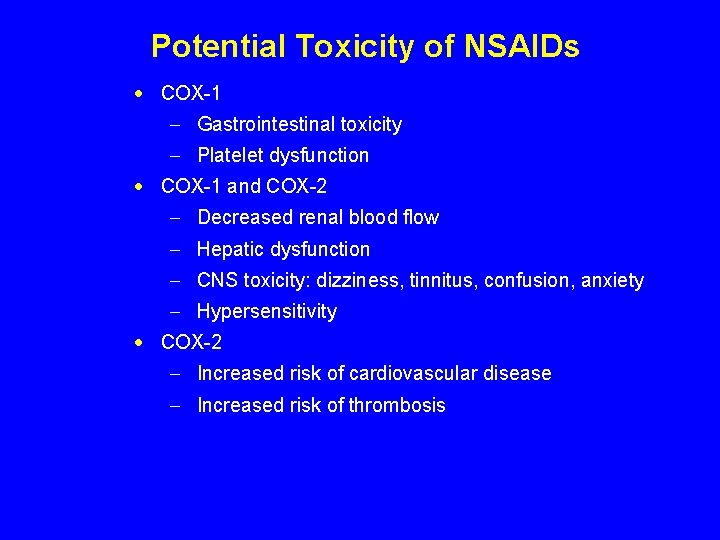
Potential Toxicity of NSAIDs · COX-1 - Gastrointestinal toxicity - Platelet dysfunction · COX-1 and COX-2 - Decreased renal blood flow - Hepatic dysfunction - CNS toxicity: dizziness, tinnitus, confusion, anxiety - Hypersensitivity · COX-2 - Increased risk of cardiovascular disease - Increased risk of thrombosis
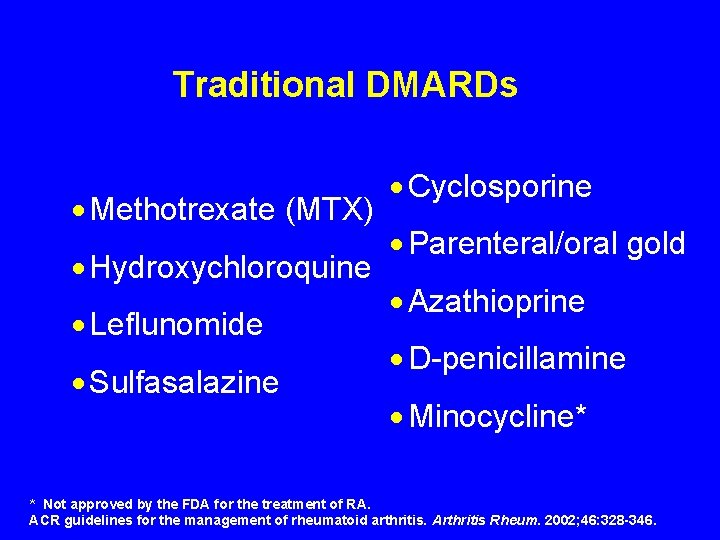
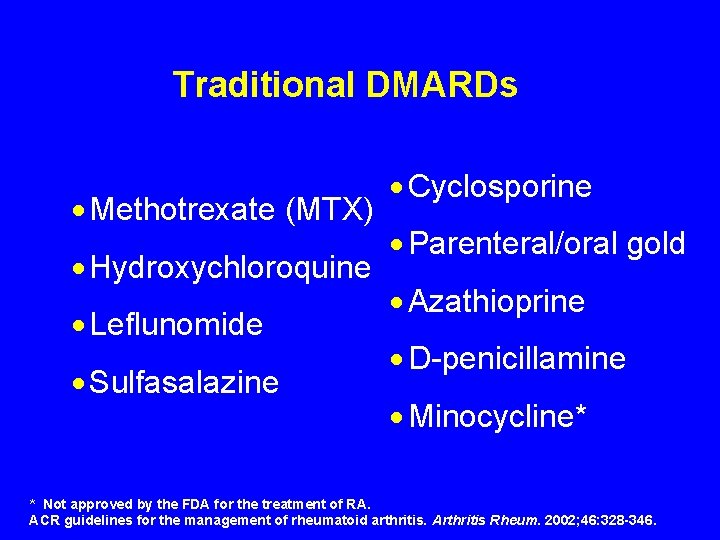
Traditional DMARDs · Methotrexate (MTX) · Hydroxychloroquine · Leflunomide · Sulfasalazine · Cyclosporine · Parenteral/oral gold · Azathioprine · D-penicillamine · Minocycline* * Not approved by the FDA for the treatment of RA. ACR guidelines for the management of rheumatoid arthritis. Arthritis Rheum. 2002; 46: 328 -346.
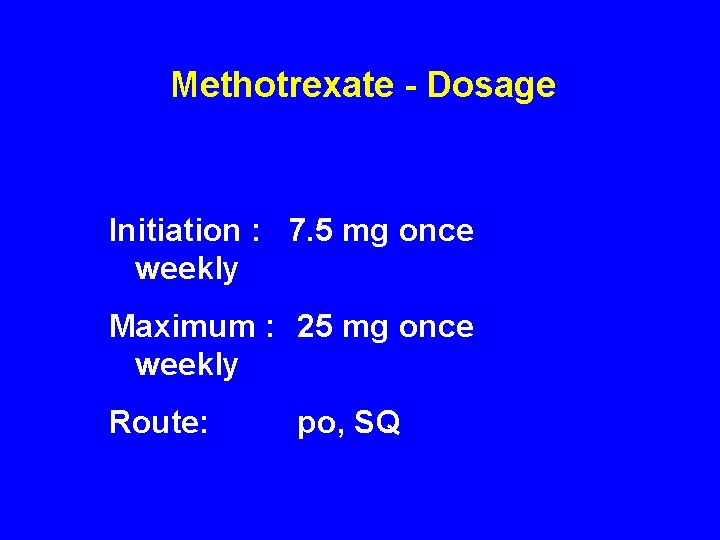
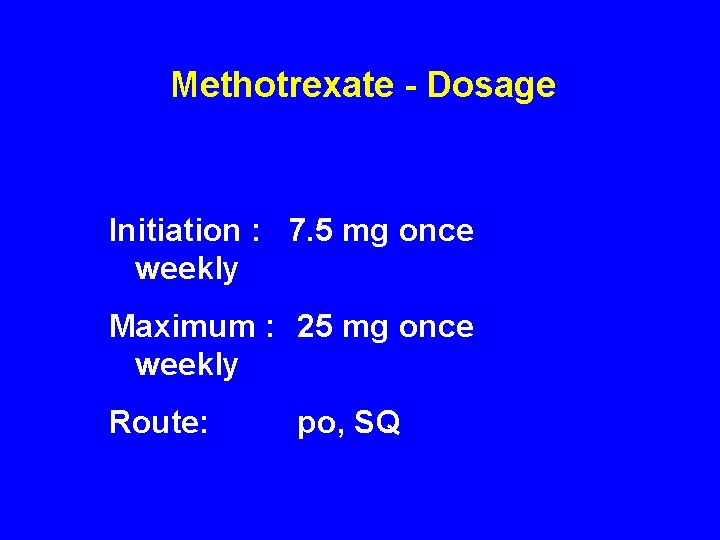
Methotrexate - Dosage Initiation : 7. 5 mg once weekly Maximum : 25 mg once weekly Route: po, SQ
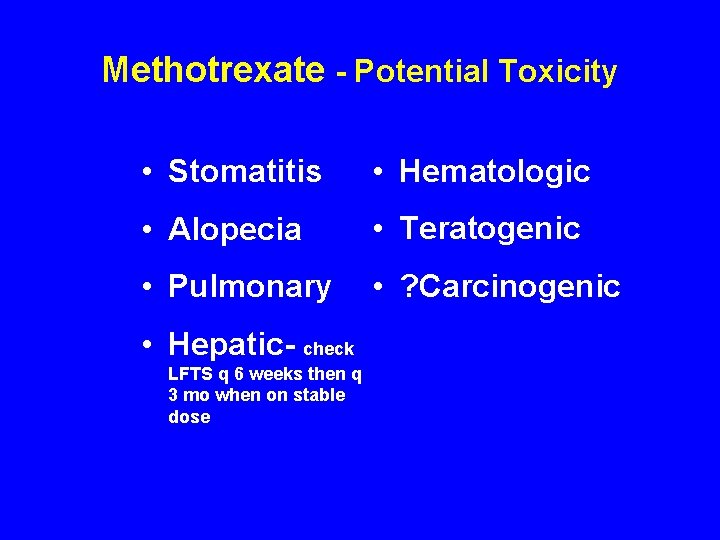
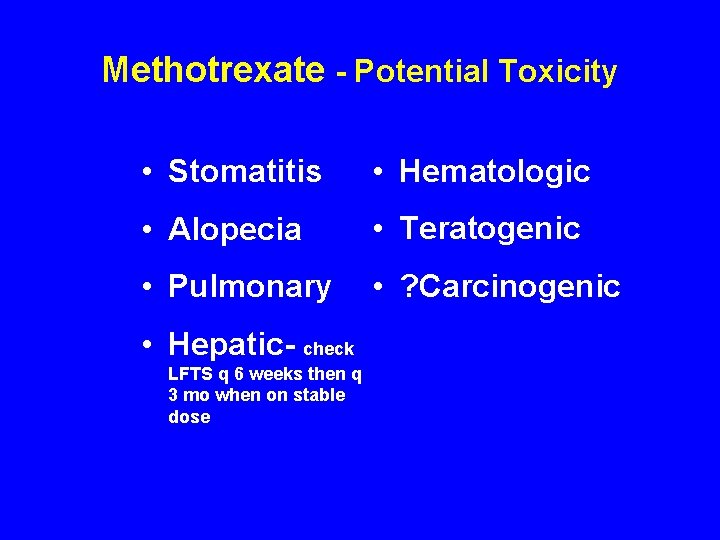
Methotrexate - Potential Toxicity • Stomatitis • Hematologic • Alopecia • Teratogenic • Pulmonary • ? Carcinogenic • Hepatic- check LFTS q 6 weeks then q 3 mo when on stable dose
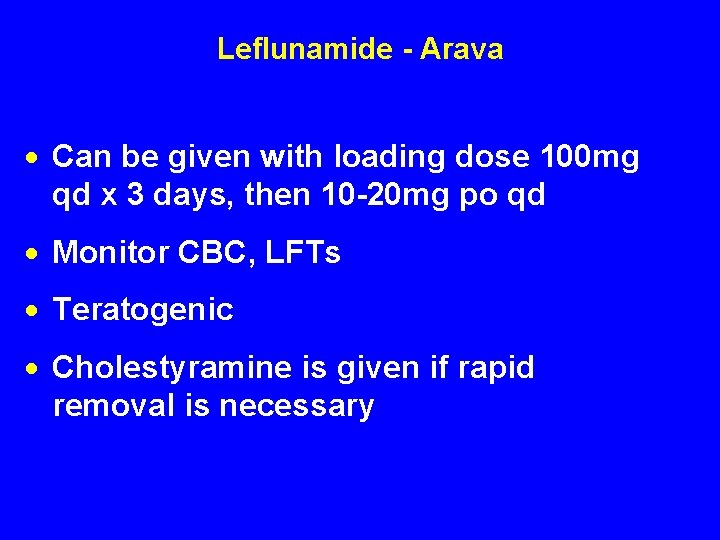
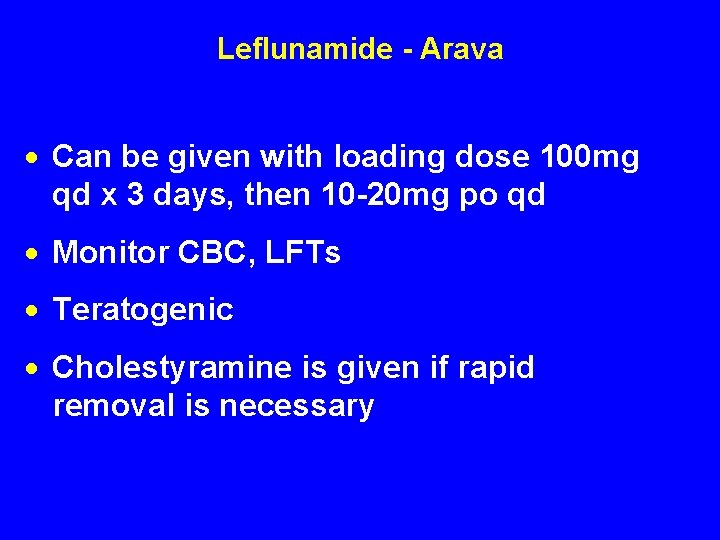
Leflunamide - Arava · Can be given with loading dose 100 mg qd x 3 days, then 10 -20 mg po qd · Monitor CBC, LFTs · Teratogenic · Cholestyramine is given if rapid removal is necessary
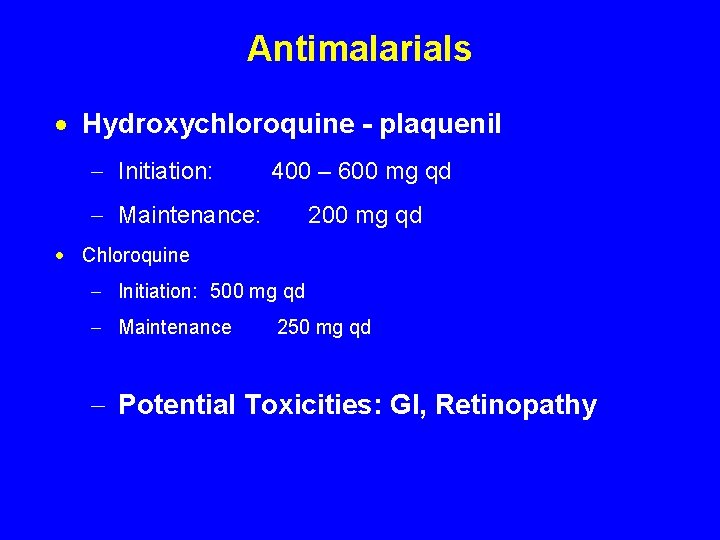
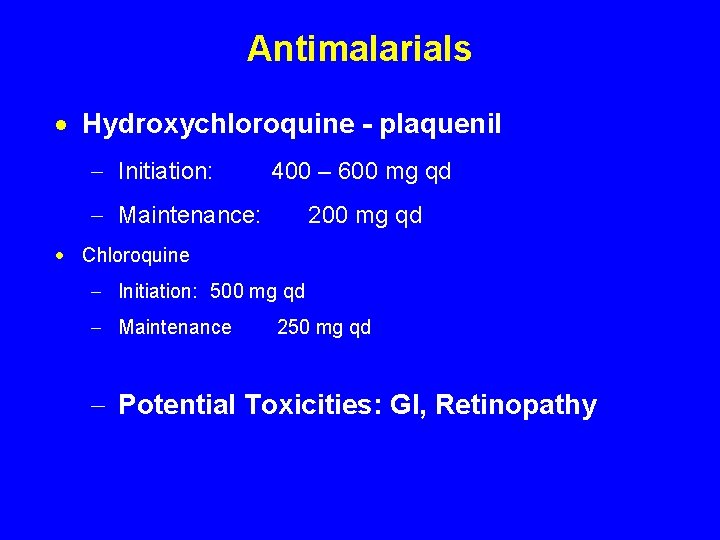
Antimalarials · Hydroxychloroquine - plaquenil - Initiation: 400 – 600 mg qd - Maintenance: 200 mg qd · Chloroquine - Initiation: 500 mg qd - Maintenance 250 mg qd - Potential Toxicities: GI, Retinopathy
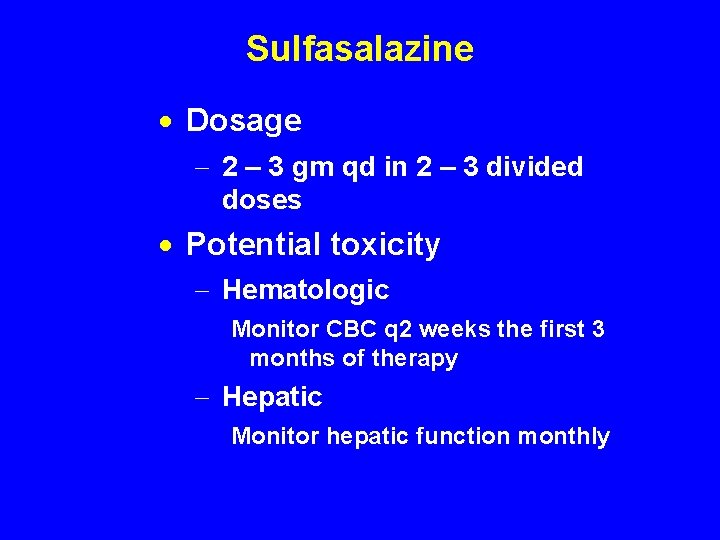
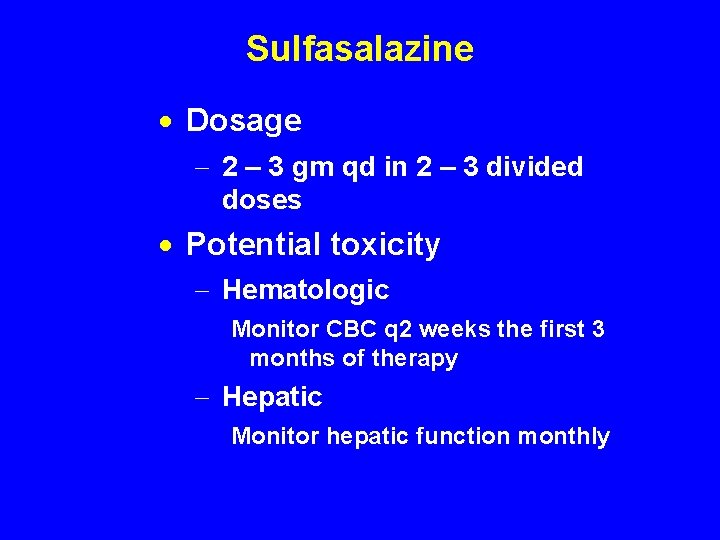
Sulfasalazine · Dosage - 2 – 3 gm qd in 2 – 3 divided doses · Potential toxicity - Hematologic Monitor CBC q 2 weeks the first 3 months of therapy - Hepatic Monitor hepatic function monthly
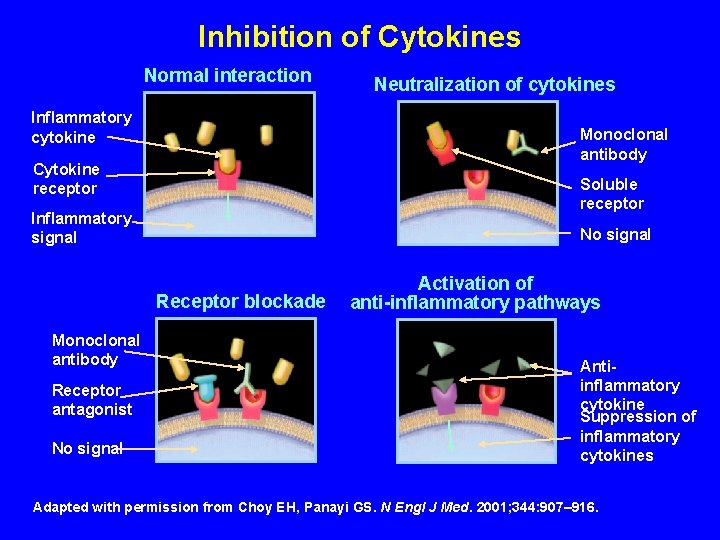
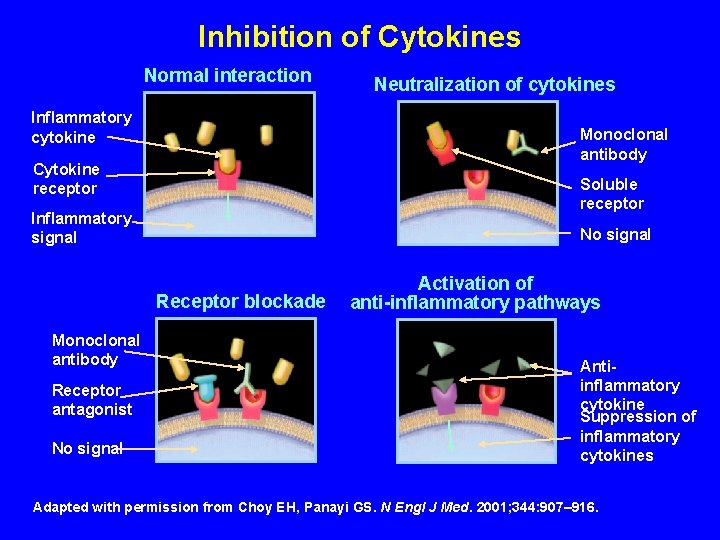
Inhibition of Cytokines Normal interaction Inflammatory cytokine Monoclonal antibody Cytokine receptor Soluble receptor Inflammatory signal No signal Receptor blockade Monoclonal antibody Receptor antagonist No signal Neutralization of cytokines Activation of anti-inflammatory pathways Antiinflammatory cytokine Suppression of inflammatory cytokines Adapted with permission from Choy EH, Panayi GS. N Engl J Med. 2001; 344: 907– 916.
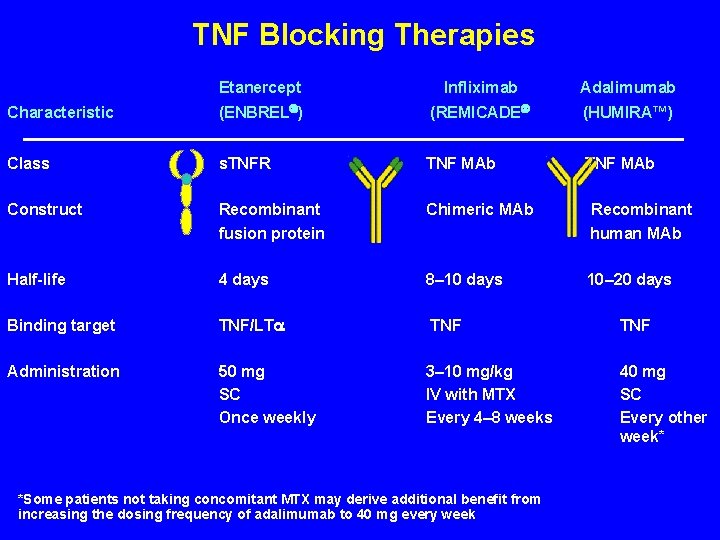
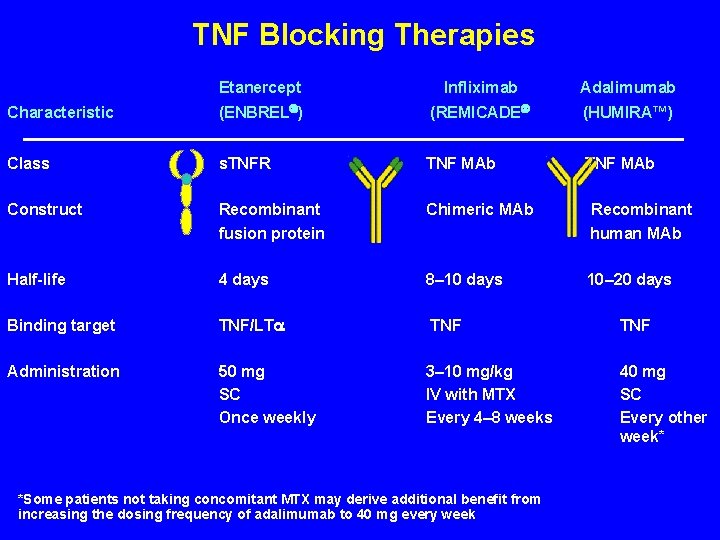
TNF Blocking Therapies Etanercept Infliximab Adalimumab Characteristic (ENBREL ) (REMICADE (HUMIRA™) Class s. TNFR TNF MAb TNF MAb Construct Recombinant fusion protein Chimeric MAb Recombinant human MAb Half-life 4 days 8– 10 days 10– 20 days Binding target TNF/LT TNF Administration 50 mg SC Once weekly 3– 10 mg/kg IV with MTX Every 4– 8 weeks 40 mg SC Every other week* *Some patients not taking concomitant MTX may derive additional benefit from increasing the dosing frequency of adalimumab to 40 mg every week

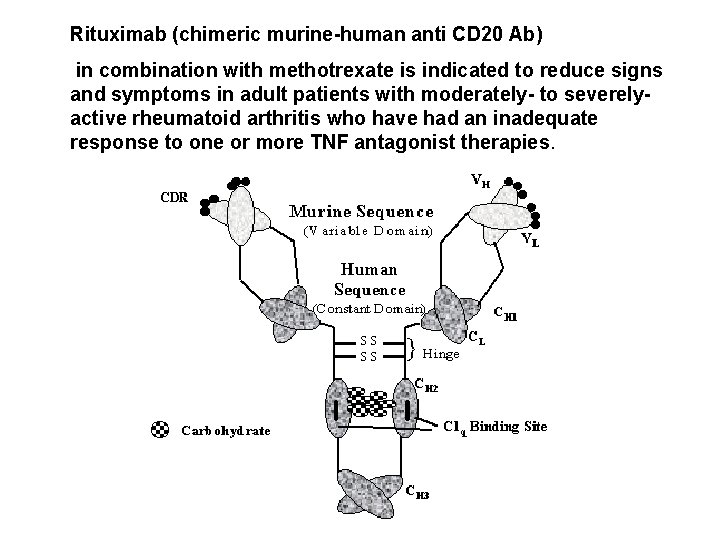
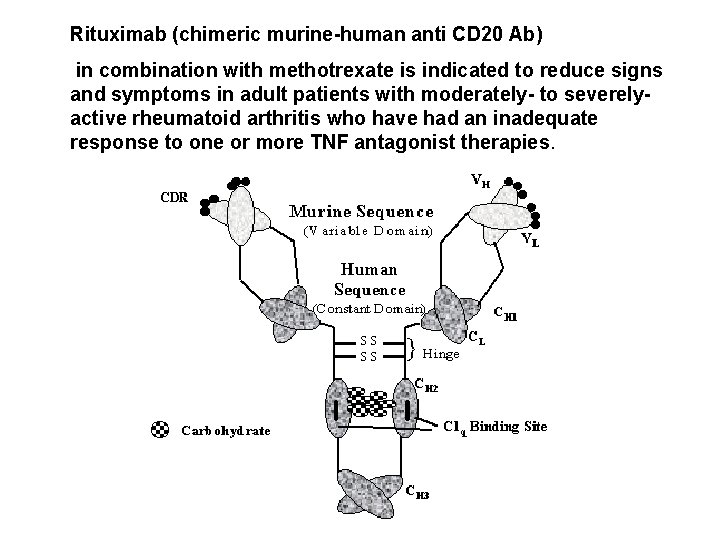
Rituximab (chimeric murine-human anti CD 20 Ab) in combination with methotrexate is indicated to reduce signs and symptoms in adult patients with moderately- to severely- active rheumatoid arthritis who have had an inadequate response to one or more TNF antagonist therapies.
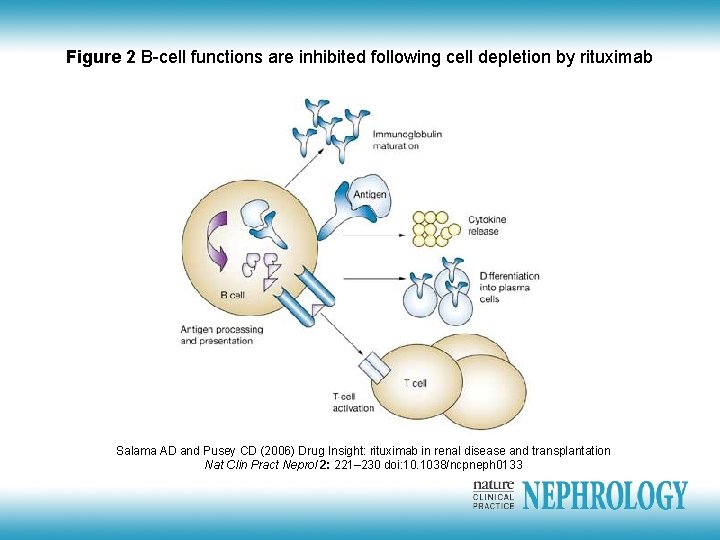
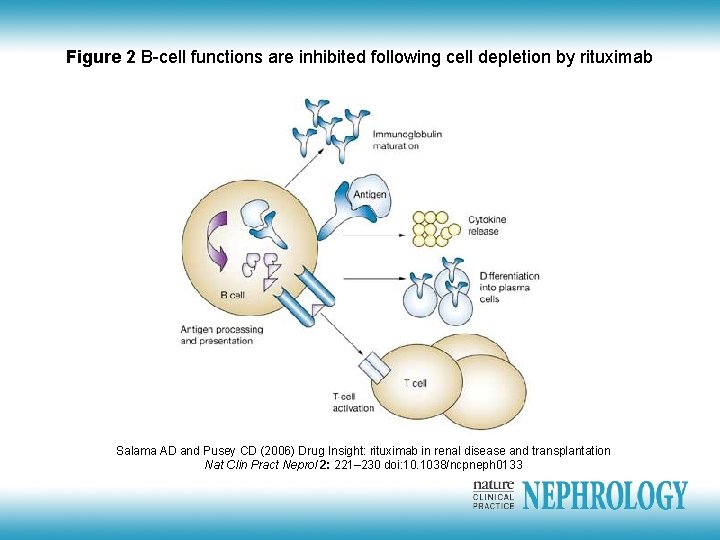
Figure 2 B-cell functions are inhibited following cell depletion by rituximab Salama AD and Pusey CD (2006) Drug Insight: rituximab in renal disease and transplantation Nat Clin Pract Neprol 2: 221– 230 doi: 10. 1038/ncpneph 0133
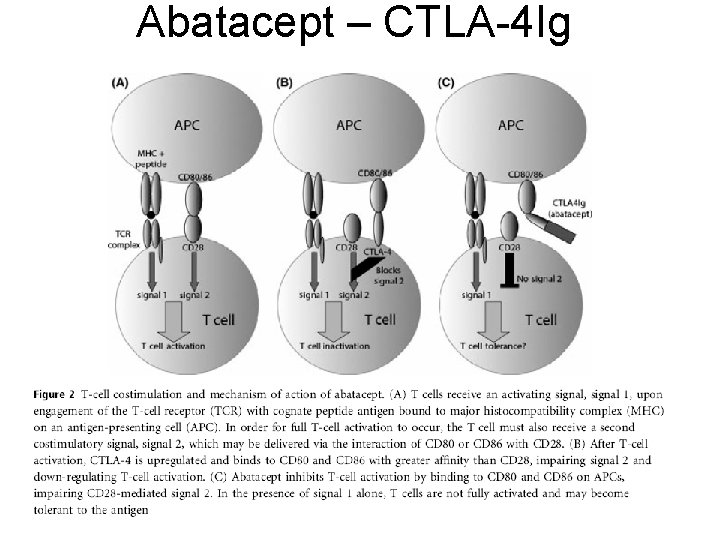
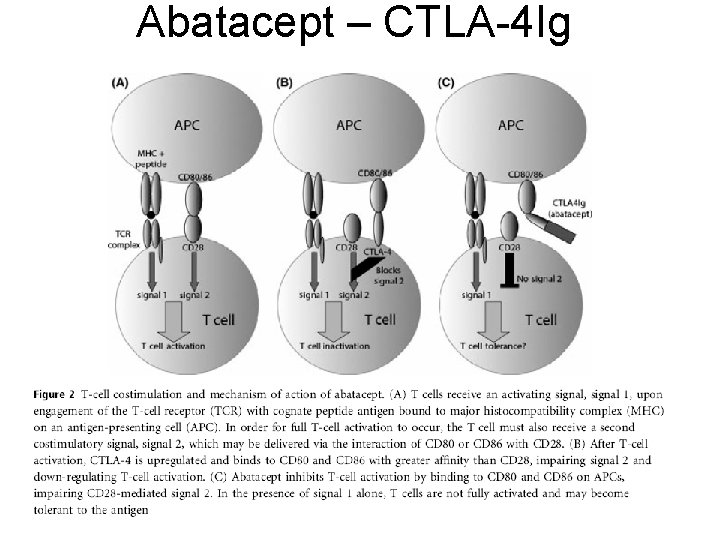
Abatacept – CTLA-4 Ig
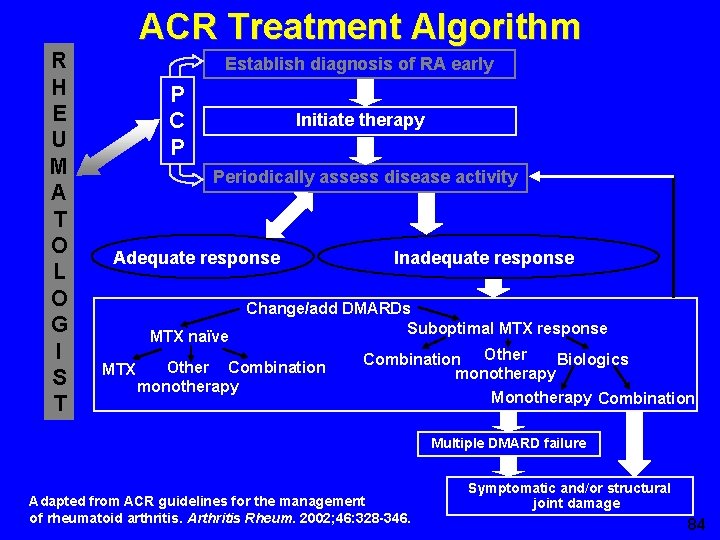
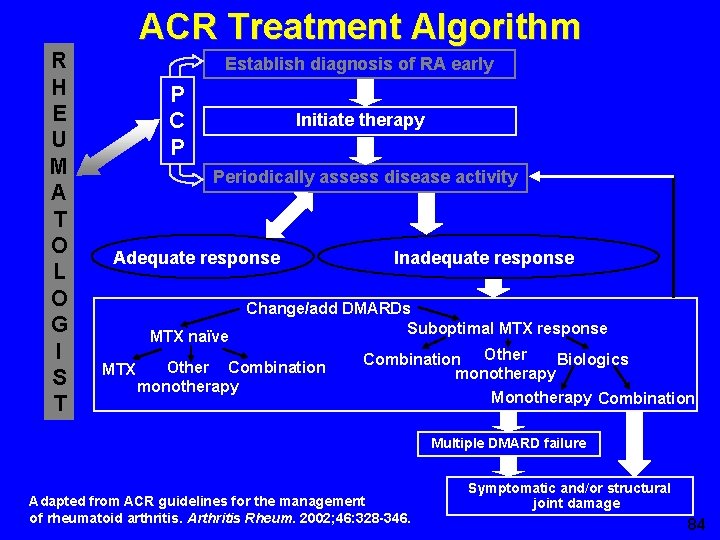
ACR Treatment Algorithm R H E U M A T O L O G I S T Establish diagnosis of RA early P C P Initiate therapy Periodically assess disease activity Adequate response MTX naïve MTX Inadequate response Change/add DMARDs Suboptimal MTX response Other Combination monotherapy Combination Other Biologics monotherapy Monotherapy Combination Multiple DMARD failure Adapted from ACR guidelines for the management of rheumatoid arthritis. Arthritis Rheum. 2002; 46: 328 -346. Symptomatic and/or structural joint damage 84
· Questions · Case report
Case Report · 57 -year-old man was admitted to a hospital affiliated with dyspnea and dry cough lasting 2 weeks. · He had previously been diagnosed with rheumatoid arthritis, manifested by painful swelling of the joints 2 years prior to admission. · The patient was being treated with prednisone and gold. · Patient with diffuse pulmonary rheumatoid nodules and interstitial fibrosis throughout both lungs, is described. · The patient, with articular symptoms and seropositivity, exhibited a rapid clinical course and died of respiratory failure 3 months after the appearance of dyspnea.




· Chest radiography indicated interstitial pneumonitis with bilateral diffuse peripheral shadows. · At autopsy, numerous rheumatoid nodules and interstitial fibrosis had destroyed both lungs, such that no residual normal pulmonary tissue remained. · It is believed that this was an extremely rare case exhibiting large numbers of rheumatoid nodules throughout the lungs. · Findings with this patient indicate that, in patients with rheumatoid arthritis, clinical interstitial pneumonitis confirmed radiographically does not exclude the existence of rheumatoid lung nodules.
 Lisa has a diagnosed learning disability
Lisa has a diagnosed learning disability How is progeria diagnosed
How is progeria diagnosed How is progeria diagnosed
How is progeria diagnosed Crohn's disease test
Crohn's disease test Two years ago jenny was diagnosed with schizophrenia
Two years ago jenny was diagnosed with schizophrenia Best case worst case average case
Best case worst case average case Snow white and the seven dwarfs gender roles
Snow white and the seven dwarfs gender roles Unknown white male
Unknown white male Codominance
Codominance What is a nonsense poem
What is a nonsense poem Biography of ellen g white
Biography of ellen g white Joseph brazil white and case
Joseph brazil white and case Jonathan feng white & case
Jonathan feng white & case Jonathan feng white & case
Jonathan feng white & case Project progress status
Project progress status Partial report technique
Partial report technique Catarahh
Catarahh Structure of a case report
Structure of a case report Slidetodoc
Slidetodoc Case report example
Case report example Consent form for case report
Consent form for case report Difference between short case and long case
Difference between short case and long case Average case complexity of binary search
Average case complexity of binary search Glennan building cwru
Glennan building cwru Bubble sort best case and worst case
Bubble sort best case and worst case Crm failure case study
Crm failure case study Bubble sort best case and worst case
Bubble sort best case and worst case Bubble sort best case and worst case
Bubble sort best case and worst case The ambiguous case for the law of sines
The ambiguous case for the law of sines Dislocatio ad peripheriam
Dislocatio ad peripheriam Whats a male sheep called
Whats a male sheep called Methods of karyotyping
Methods of karyotyping Male fat distribution
Male fat distribution An aquarium contains 6 male goldfish
An aquarium contains 6 male goldfish Brow ridge male vs female
Brow ridge male vs female Length of male urethra
Length of male urethra Function of cervix
Function of cervix Navy hair regulations female 2019
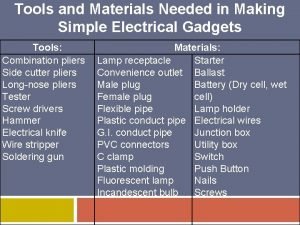
Navy hair regulations female 2019 Simple electrical gadgets and their uses
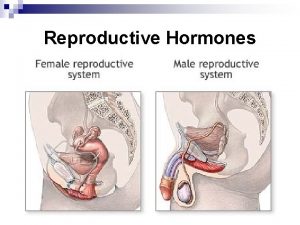
Simple electrical gadgets and their uses Function of male reproductive system
Function of male reproductive system Female testes
Female testes Anatomy of the reproductive system exercise 42
Anatomy of the reproductive system exercise 42 Wiregrass
Wiregrass What is the proper use of the ffa jacket
What is the proper use of the ffa jacket Oogenesis process
Oogenesis process Major endocrine glands male and female
Major endocrine glands male and female Major endocrine glands male and female
Major endocrine glands male and female Primary sexual characteristics
Primary sexual characteristics Std from oral
Std from oral Minkspor
Minkspor Gabriele cilia pensare male
Gabriele cilia pensare male Male genital variation
Male genital variation Cos'è il male per sant'agostino
Cos'è il male per sant'agostino Female sex organ diagram
Female sex organ diagram Female and male reproductive system
Female and male reproductive system Pearson education
Pearson education Luteinizing hormone in male reproductive system
Luteinizing hormone in male reproductive system Male gonad
Male gonad From where sperm is produced
From where sperm is produced Male reproductive system in plant
Male reproductive system in plant What part of the plant produces pollen
What part of the plant produces pollen Rectum in men
Rectum in men Tanner staging boys
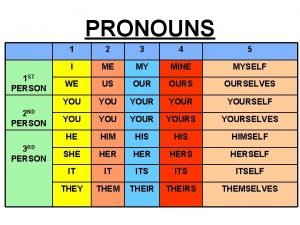
Tanner staging boys I st person
I st person Art-labeling activity: the male reproductive system, part 1
Art-labeling activity: the male reproductive system, part 1 Bmi 22 female pictures
Bmi 22 female pictures Navy prt standards
Navy prt standards What is the perineum and where is it located
What is the perineum and where is it located Hiatus of schwalbe
Hiatus of schwalbe Bulbospongiosus
Bulbospongiosus Pedigree affected male symbol
Pedigree affected male symbol Functions of pistil
Functions of pistil Kiwibann
Kiwibann Malé kotě noty
Malé kotě noty Male reproductive system information
Male reproductive system information Noirmle
Noirmle Chapter 7 extending mendelian genetics
Chapter 7 extending mendelian genetics Reproductive organ
Reproductive organ Epidisymis
Epidisymis Male cow reproductive system diagram
Male cow reproductive system diagram Prostate
Prostate How to create sperm in male body
How to create sperm in male body Racconto fantasy
Racconto fantasy The cleaner you are the dirtier you get
The cleaner you are the dirtier you get Corniculate cartilage
Corniculate cartilage Gabriele cilia pensare male
Gabriele cilia pensare male Whats a karyotype
Whats a karyotype Karta male azije
Karta male azije Karta male azije
Karta male azije Male reproductive system plants
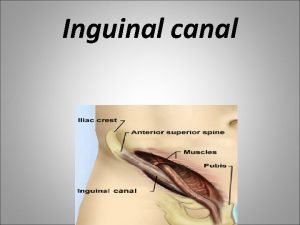
Male reproductive system plants Inguinal region
Inguinal region Cupping points
Cupping points