WHAT IS OXYGEN WHAT IS OXYGEN A colourless






- Slides: 55

WHAT IS OXYGEN ?
WHAT IS OXYGEN ? A colourless, odourless reactive gas, The chemical element of atomic number 8 and the lifesupporting component of the air. “If breathing stops, there is no oxygen getting to the brain and the cells begin to die"

IMPORTANCE OF OXYGEN ? 34% of ambulance patients receive oxygen during transit and 15– 17% of hospital inpatients will be receiving oxygen at any given time. Yet prior to 2008, there was no national or international guidance available for the safe use of oxygen.
WHAT IS OXYGEN ? It is widely believed that supplemental oxygen relieves dyspnoea in the absence of hypoxaemia (low arterial oxygen levels). No evidence of benefit exists for administering oxygen in patients who are normoxaemic (normal arterial oxygen levels) or very mildly hypoxaemic. Dyspnoea can occur for many reasons other than cardiorespiratory disease, including metabolic acidosis, anxiety and pain, and treatment with oxygen is not indicated in these cases.
OVERVIEW Introduction Indications Oxygen delivery systems Complications of oxygen therapy
GOAL OF OXYGEN THERAPY To maintain adequate tissue oxygenation while minimizing cardiopulmonary work To correct potentially harmful hypoxaemia Oxygen has not been proven to have any consistent effect To alleviate breathlessness (only if hypoxemic) Benefit has been found with use of a hand-held fan and consider on the sensation of breathlessness in non-hypoxaemic patients. use of opioids for patients with malignancy or other causes of chronic severe breathlessness
CLINICAL OBJECTIVES 1. 1. Correct documented or suspected hypoxemia Decrease the symptoms associated with chronic hypoxemia Decrease the workload hypoxemia imposes on the cardiopulmonary system
INDICATIONS Documented hypoxemia as evidenced by Pa. O 2 < 60 mm. Hg or Sa. O 2 < 90% on room air Pa. O 2 or Sa. O 2 below desirable range for a specific clinical situation Acute care situations in which hypoxemia is suspected Severe trauma Acute myocardial infarction Short term therapy (Post anaesthesia recovery)
INDICATIONS High-dose oxygen Severe Pneumonia Severe LVF Major Trauma Sepsis and Shock Lung collapse Pulmonary Embolism Lung Fibrosis
ASSESSMENT The need for oxygen therapy should be assessed by 1. Monitoring of ABGs - Pa. O 2, Sp. O 2 2. Clinical assessment findings.
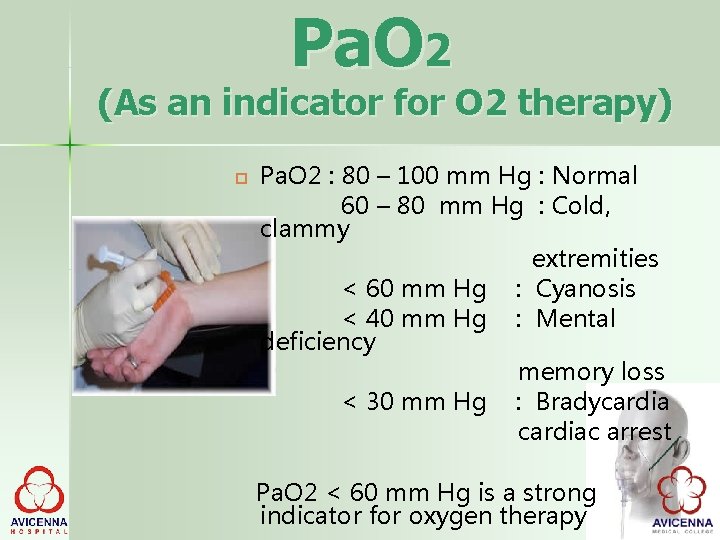
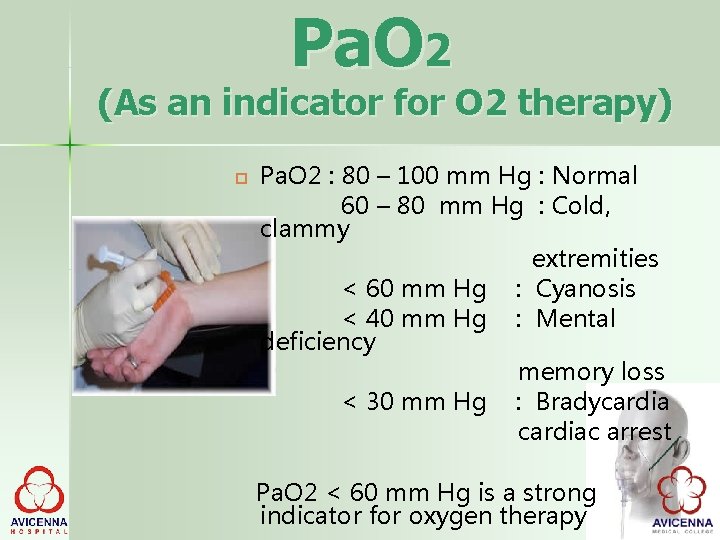
Pa. O 2 (As an indicator for O 2 therapy) Pa. O 2 : 80 – 100 mm Hg : Normal 60 – 80 mm Hg : Cold, clammy extremities < 60 mm Hg : Cyanosis < 40 mm Hg : Mental deficiency memory loss < 30 mm Hg : Bradycardiac arrest Pa. O 2 < 60 mm Hg is a strong indicator for oxygen therapy
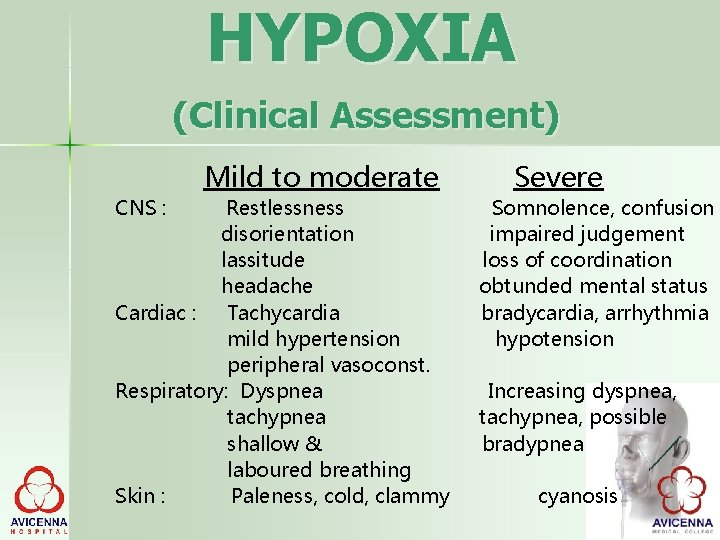
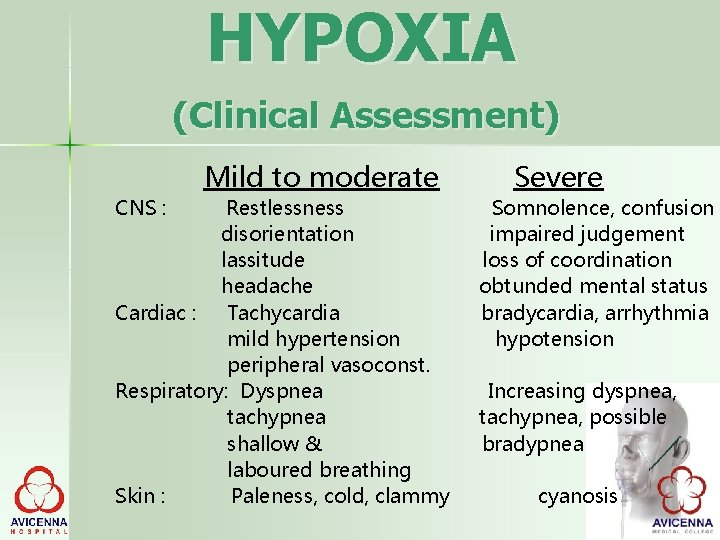
HYPOXIA (Clinical Assessment) CNS : Mild to moderate Restlessness disorientation lassitude headache Cardiac : Tachycardia mild hypertension peripheral vasoconst. Respiratory: Dyspnea tachypnea shallow & laboured breathing Skin : Paleness, cold, clammy Severe Somnolence, confusion impaired judgement loss of coordination obtunded mental status bradycardia, arrhythmia hypotension Increasing dyspnea, tachypnea, possible bradypnea cyanosis
MONITORING Physical examination for C/F of hypoxemia Pulse oximetry ABGs analysis p. H p. O 2 p. CO 2 Mixed venous blood oxygenation

OXYGEN THERAPY DEVICES o o Low flow (Variable performance devices ) Nasal cannula Simple face mask Partial rebreathing mask Non rebreathing mask Tracheostomy mask High flow (Fixed performance devices) Ventimask (HAFOE) Aerosol mask and T-piece with nebulizers
COMLICATIONS 2. Depression of ventilation 3. Retinopathy of Prematurity 4. Absorption atelectasis 5. Fire hazard
HOW MUCH OXYGEN IS SAFE 100% - not more than 12 hrs 80% - not more than 24 hrs 60% - not more than 36 hrs Goal should be to use lowest possible Fi. O 2 compatible with adequate tissue oxygenation
IMPORTANT POINTS 1 Oxygen is a life saving drug for hypoxemic patients. (Patients whose oxygen levels are low) 2 Giving too much oxygen is unnecessary as oxygen cannot be store in the body 3 COPD patients (and some other patients) may be harmed by too much oxygen as this can lead to increased carbon dioxide (C 02) levels 4 Other patients (e. g. myocardial infarction) may also be harmed by too much oxygen 5 Only give as much as needed– no need for extra!
WHAT'S THE PROBLEM Published audits have shown: Doctors and nurses have a poor understanding of how oxygen should be used Oxygen is often given without a prescription (In the 2015 BTS audit, 42% of hospital patients using oxygen had no prescription ) If there is a prescription, patients do not always receive what is specified on the prescription Where there is a prescription with target range, almost one third of patients are outside the range (9. 5% of Sp. O 2 results below target range and 21. 5% above target range in 2015 BTS audit)
OXYGEN IS A DRUG Oxygen should be regarded as a drug (BNF 2016) Oxygen must be prescribed in all situations (except for the immediate management of critical illness in accordance with BTS guidelines) (NPSA Oct 2009) Oxygen should be prescribed to achieve a target saturation ( Sp 02) which should be written on the drug chart or electronic prescription
Normal Oxygen saturation range in healthy adults Sp. O 2 Saturation of O 2 (measured by pulse oximetry) HEALTHY ADULTS Daytime Sp 02 96 -98% *Transient dips in saturation are common during sleep (~84%)
OXYGEN THERAPY BY FIRST RESPONDER • Patients must not go without oxygen while waiting for a medical review • Initial 02 therapy is reservoir mask at 15 litres/minute (RM 15) • Once stable aim for Sp. O 2 94 -98% or patient-specific target range • COPD patients who are critically ill should have the same oxygen therapy until blood gases have been obtained and may then need controlled oxygen therapy or non-invasive or invasive ventilation
Prescribing to a Target Saturation range • Oxygen will be prescribed in order to keep Sp 02 within a specified range for individual patients • Target oxygen saturation prescription is integrated into the patient’s drug chart and bedside monitoring • Oxygen delivery device and/or flow should be changed if necessary to keep the Sp. O 2 in the target range
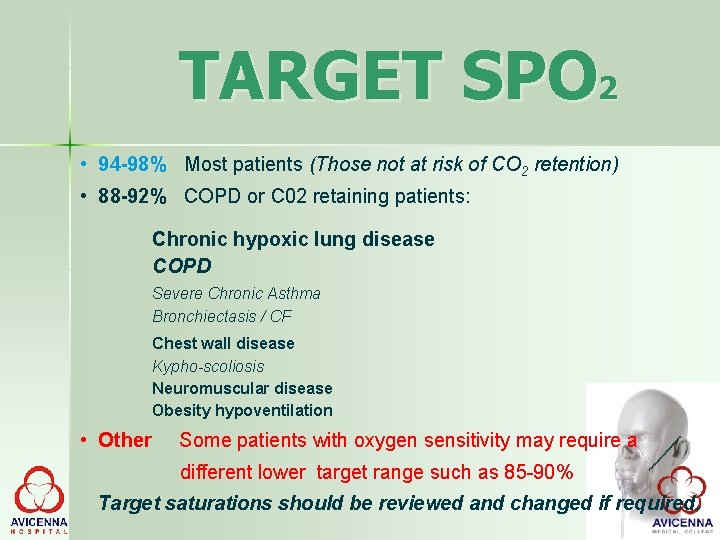
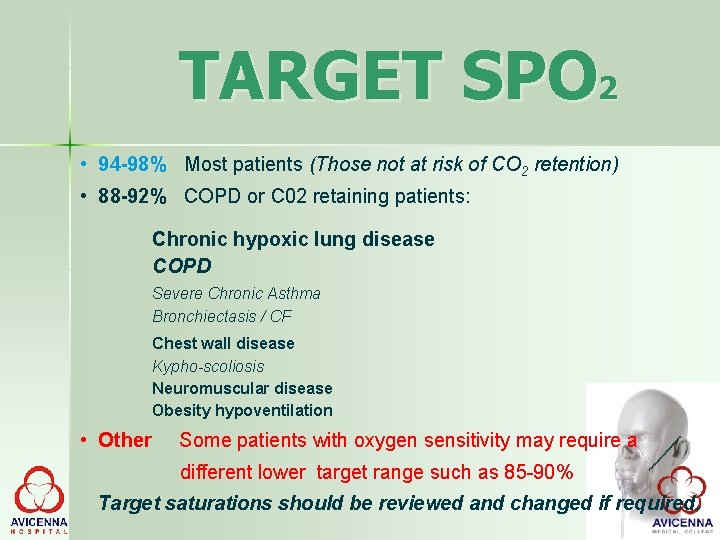
TARGET SPO 2 • 94 -98% Most patients (Those not at risk of CO 2 retention) • 88 -92% COPD or C 02 retaining patients: Chronic hypoxic lung disease COPD Severe Chronic Asthma Bronchiectasis / CF Chest wall disease Kypho-scoliosis Neuromuscular disease Obesity hypoventilation • Other Some patients with oxygen sensitivity may require a different lower target range such as 85 -90% Target saturations should be reviewed and changed if required.
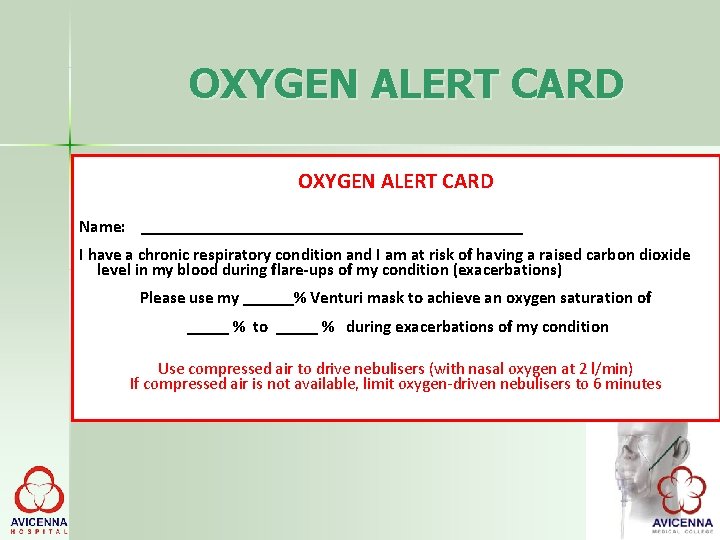
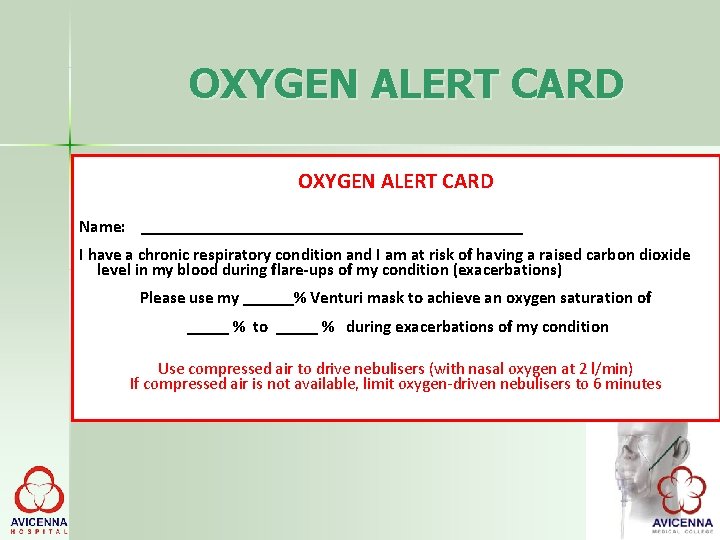
OXYGEN ALERT CARD Name: _______________________ I have a chronic respiratory condition and I am at risk of having a raised carbon dioxide level in my blood during flare-ups of my condition (exacerbations) Please use my ______% Venturi mask to achieve an oxygen saturation of _____ % to _____ % during exacerbations of my condition Use compressed air to drive nebulisers (with nasal oxygen at 2 l/min) If compressed air is not available, limit oxygen-driven nebulisers to 6 minutes
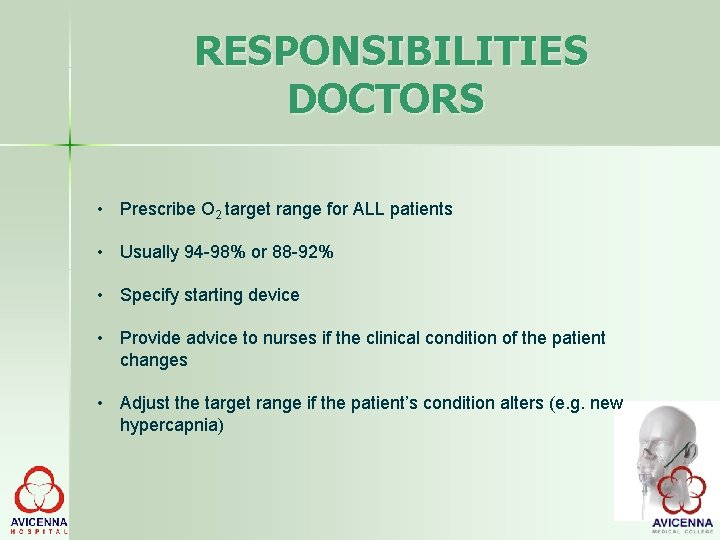
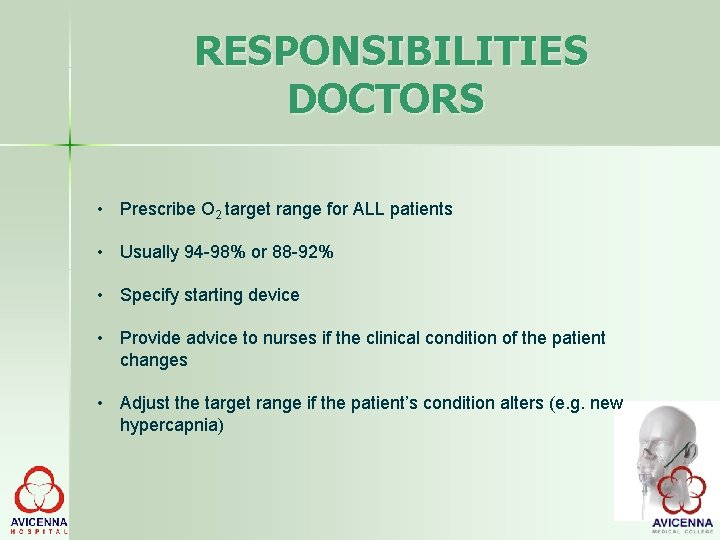
RESPONSIBILITIES DOCTORS • Prescribe O 2 target range for ALL patients • Usually 94 -98% or 88 -92% • Specify starting device • Provide advice to nurses if the clinical condition of the patient changes • Adjust the target range if the patient’s condition alters (e. g. new hypercapnia)
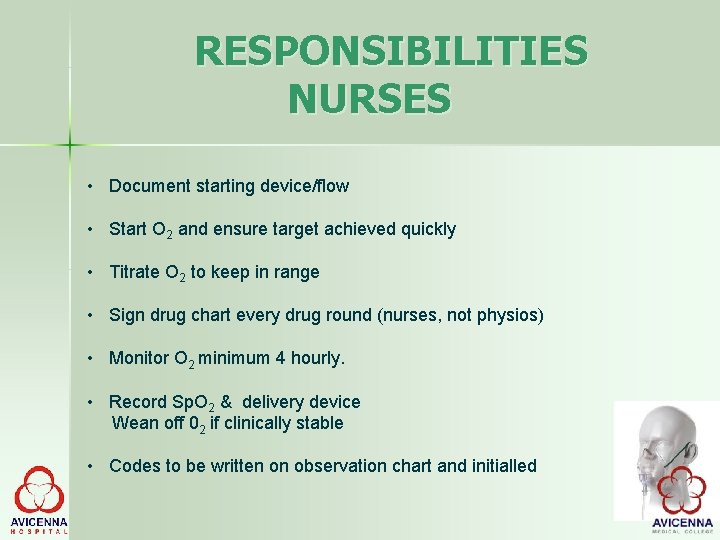
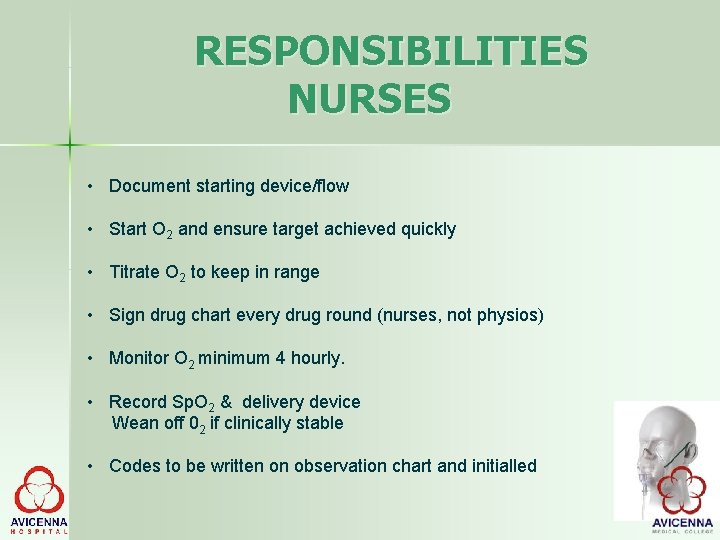
RESPONSIBILITIES NURSES • Document starting device/flow • Start O 2 and ensure target achieved quickly • Titrate O 2 to keep in range • Sign drug chart every drug round (nurses, not physios) • Monitor O 2 minimum 4 hourly. • Record Sp. O 2 & delivery device Wean off 02 if clinically stable • Codes to be written on observation chart and initialled
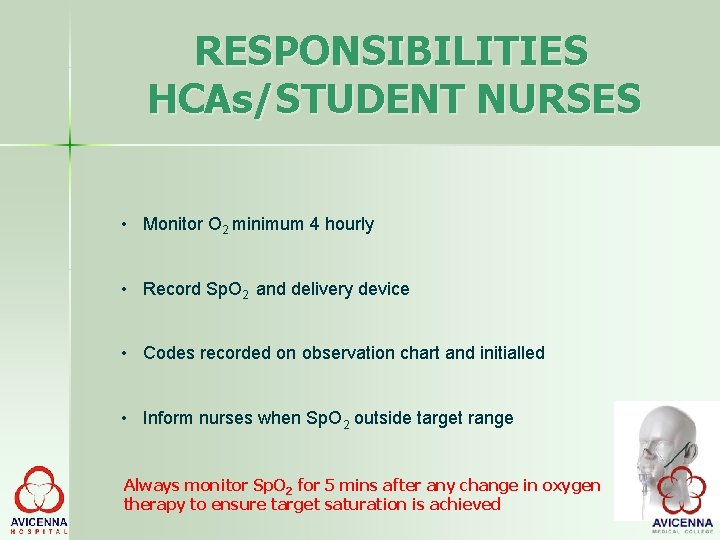
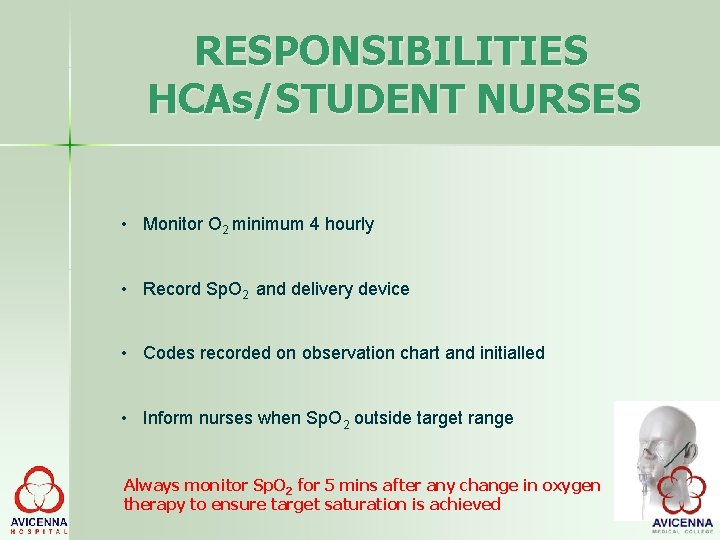
RESPONSIBILITIES HCAs/STUDENT NURSES • Monitor O 2 minimum 4 hourly • Record Sp. O 2 and delivery device • Codes recorded on observation chart and initialled • Inform nurses when Sp. O 2 outside target range Always monitor Sp. O 2 for 5 mins after any change in oxygen therapy to ensure target saturation is achieved
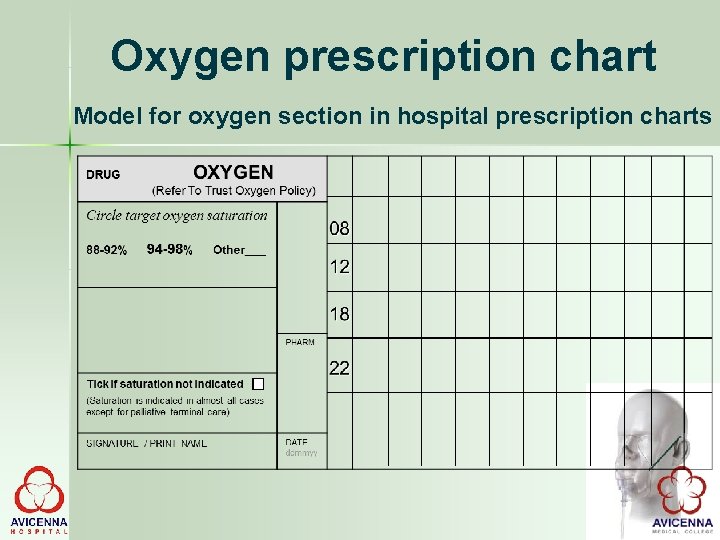
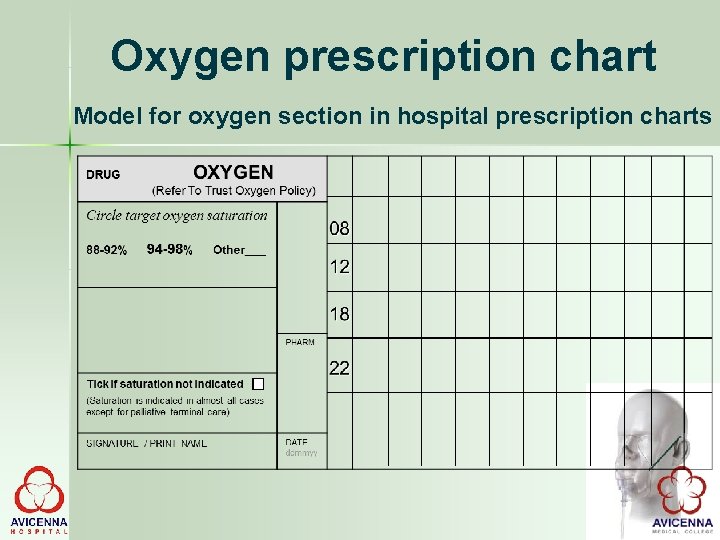
Oxygen prescription chart Model for oxygen section in hospital prescription charts
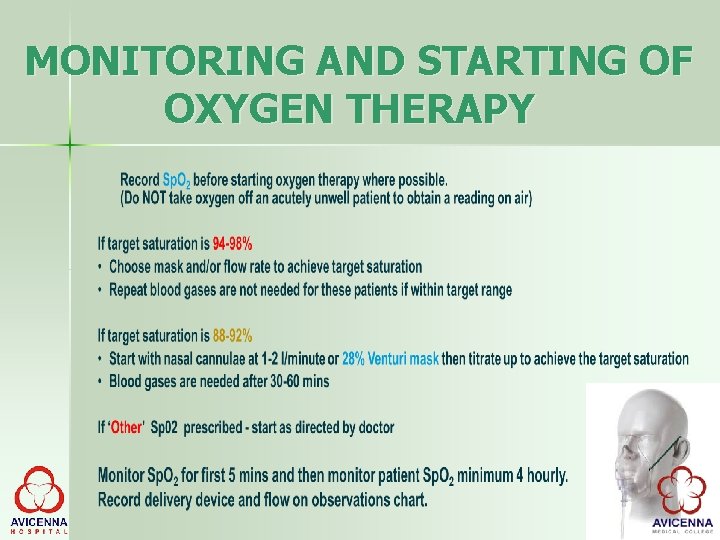
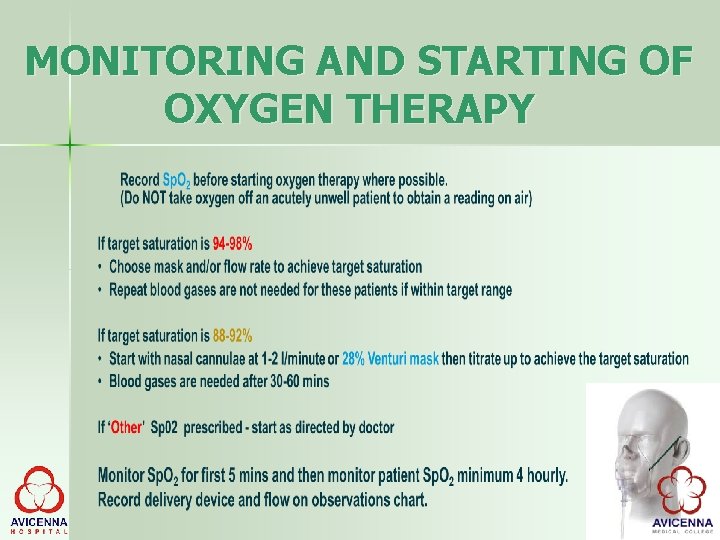
MONITORING AND STARTING OF OXYGEN THERAPY
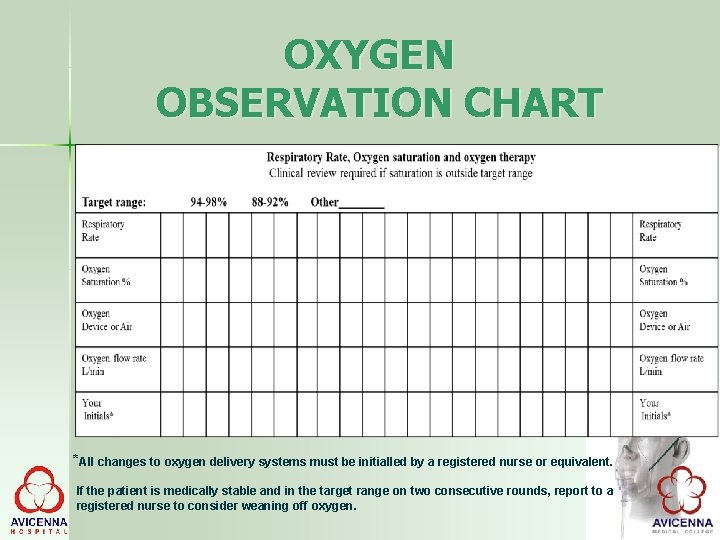
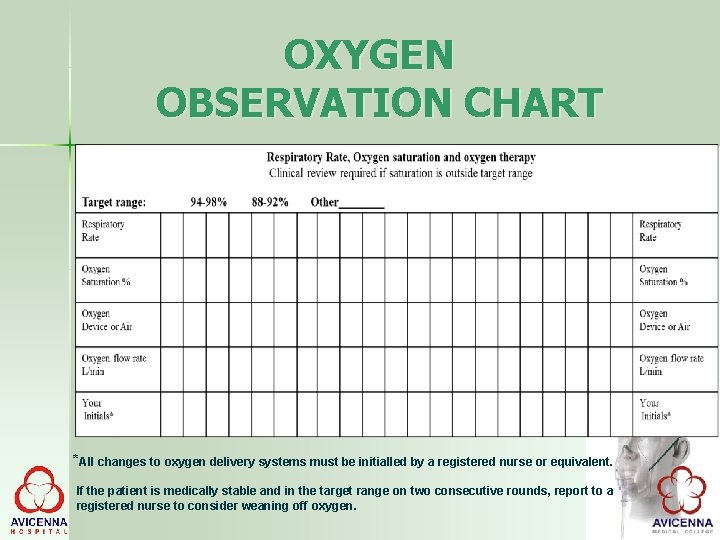
OXYGEN OBSERVATION CHART *All changes to oxygen delivery systems must be initialled by a registered nurse or equivalent. If the patient is medically stable and in the target range on two consecutive rounds, report to a registered nurse to consider weaning off oxygen.
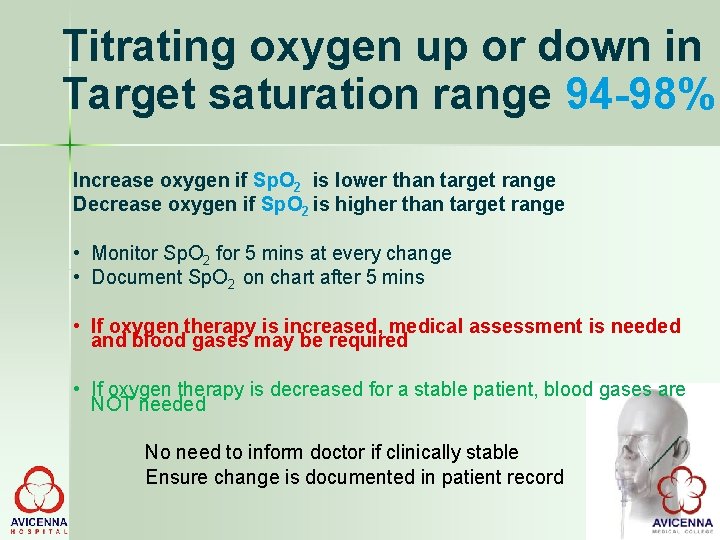
Titrating oxygen up or down in Target saturation range 94 -98% Increase oxygen if Sp. O 2 is lower than target range Decrease oxygen if Sp. O 2 is higher than target range • Monitor Sp. O 2 for 5 mins at every change • Document Sp. O 2 on chart after 5 mins • If oxygen therapy is increased, medical assessment is needed and blood gases may be required • If oxygen therapy is decreased for a stable patient, blood gases are NOT needed No need to inform doctor if clinically stable Ensure change is documented in patient record
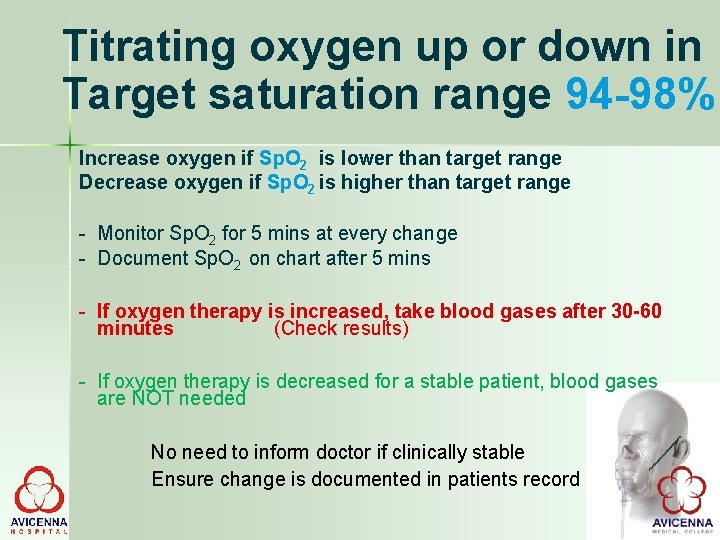
Titrating oxygen up or down in Target saturation range 94 -98% Increase oxygen if Sp. O 2 is lower than target range Decrease oxygen if Sp. O 2 is higher than target range - Monitor Sp. O 2 for 5 mins at every change - Document Sp. O 2 on chart after 5 mins - If oxygen therapy is increased, take blood gases after 30 -60 minutes (Check results) - If oxygen therapy is decreased for a stable patient, blood gases are NOT needed No need to inform doctor if clinically stable Ensure change is documented in patients record
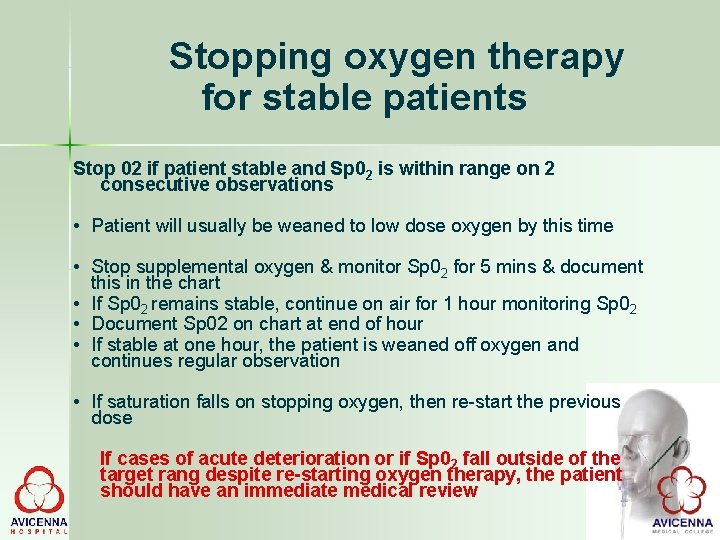
Stopping oxygen therapy for stable patients Stop 02 if patient stable and Sp 02 is within range on 2 consecutive observations • Patient will usually be weaned to low dose oxygen by this time • Stop supplemental oxygen & monitor Sp 02 for 5 mins & document this in the chart • If Sp 02 remains stable, continue on air for 1 hour monitoring Sp 02 • Document Sp 02 on chart at end of hour • If stable at one hour, the patient is weaned off oxygen and continues regular observation • If saturation falls on stopping oxygen, then re-start the previous dose If cases of acute deterioration or if Sp 02 fall outside of the target rang despite re-starting oxygen therapy, the patient should have an immediate medical review
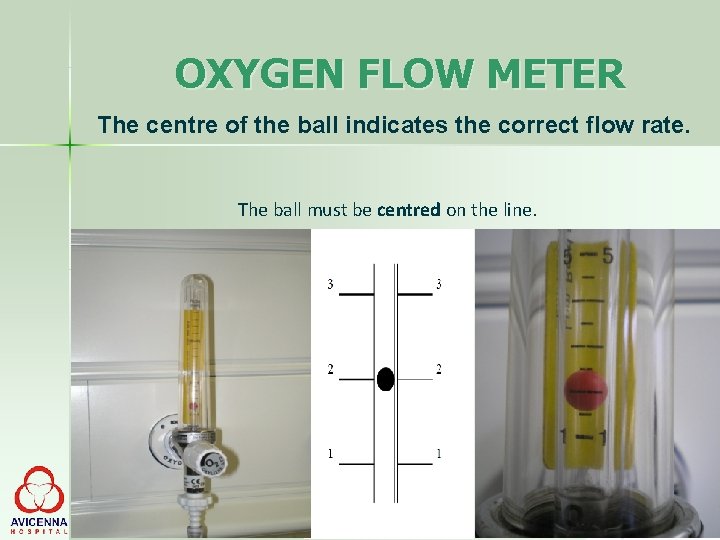
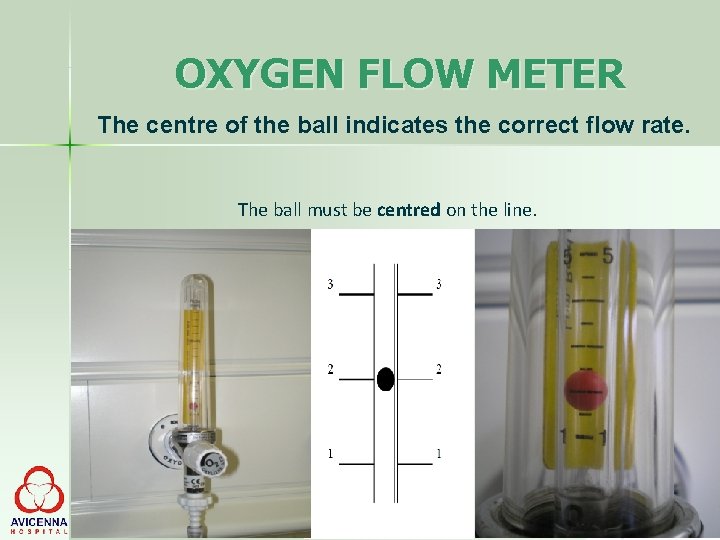
OXYGEN FLOW METER The centre of the ball indicates the correct flow rate. The ball must be centred on the line.
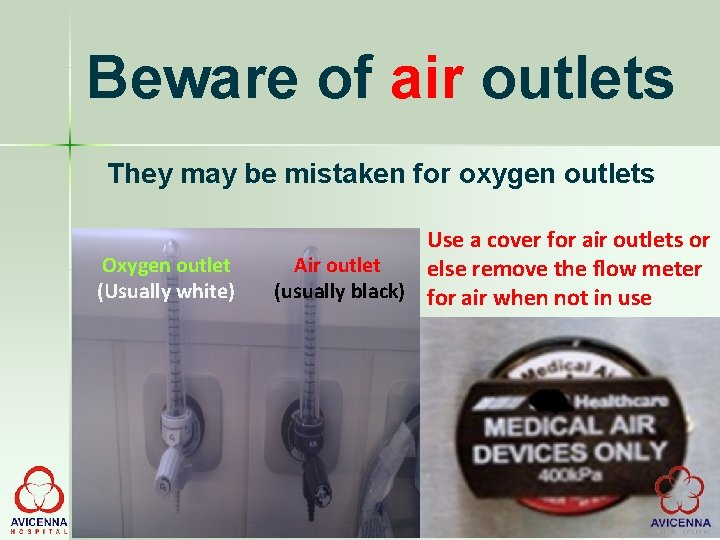
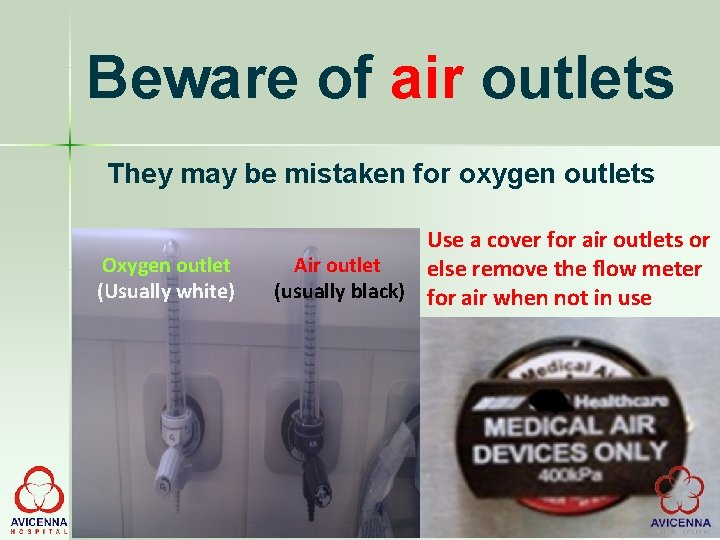
Beware of air outlets They may be mistaken for oxygen outlets Oxygen outlet (Usually white) Use a cover for air outlets or Air outlet else remove the flow meter (usually black) for air when not in use
PROCEDURE • Determine need for oxygen therapy. • Check physician order for rate and device used for concentration. • Perform an assessment of vital signs, level of consciousness , lab values etc, and record. • Assess risk factors of oxygen therapy in patients and environment such as patient with hypoxia drive, faulty electrical connections
PROCEDURE • Explain procedure to the patient and relative and inform them how to cooperate. • Post “no smoking” sign on the patient’s door in view of patient and visitors and explain to them the dangers of smoking when oxygen is on flow. • Wash hands • Set up oxygen equipment and humidifier • Fill humidifier upto the level marked on it with sterile wate
PROCEDURE • Attach flow meter to the source, set flow meter in off position • Attach humidifier to base of flow meter • Attach tubing and nasal cannula/ face mask to humidifier( if venture mask is used attach the colour coded ventruri adapter to mask as appropriate. • Regulate flowmeter to prescribed level • Ensure proper functioning by checking for bubbles in humidifier or feeling oxygen at the outlet.
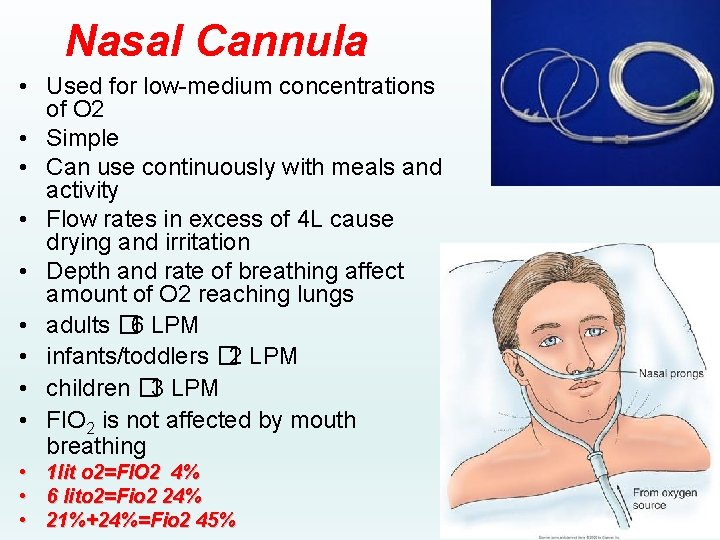
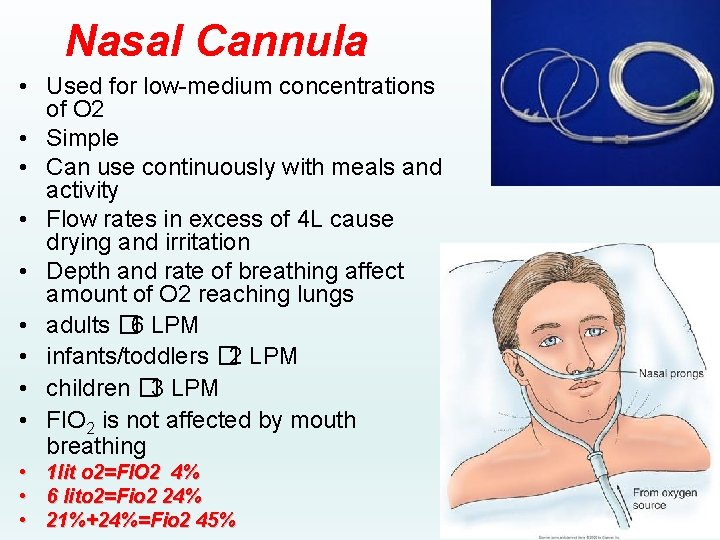
Nasal Cannula • Used for low-medium concentrations of O 2 • Simple • Can use continuously with meals and activity • Flow rates in excess of 4 L cause drying and irritation • Depth and rate of breathing affect amount of O 2 reaching lungs • adults � 6 LPM • infants/toddlers � 2 LPM • children � 3 LPM • FIO 2 is not affected by mouth breathing • 1 lit o 2=FIO 2 4% • 6 lito 2=Fio 2 24% • 21%+24%=Fio 2 45%
NASAL CANNULA • Place tips of nasal cannula to patient’s nares and adjust straps around ear for snug fit it. • The elastic band may be fixed behind head or under chin. • Pad tubing with gauze pads over ear and inpect skin behind ear periodically for irritation and breakdown. • Inspect patient and equipment frequently for flow rate, clinical condition , level of water in humidifier.
NASAL CANNULA • Ensure that safety precautions are followed. • Wash hands • Document time, flow rate and observations made on patient. • Encourage patient to breath through his/her nose with mouth closed. • Remove and clean the cannula with soap and water, dry and replace every 8 hours. • Assess nares at least every 8 hrs.
NASAL CANNULA • Never deliver more than 2 -3 litres of oxygen to patients with chronic lung disease • Maximum delivery with nasal cannula should be 4 -5 L/min • Check frequent that both prongs are in patients nares. • Do not start oxygen therapy with NP if patient is mouth breather
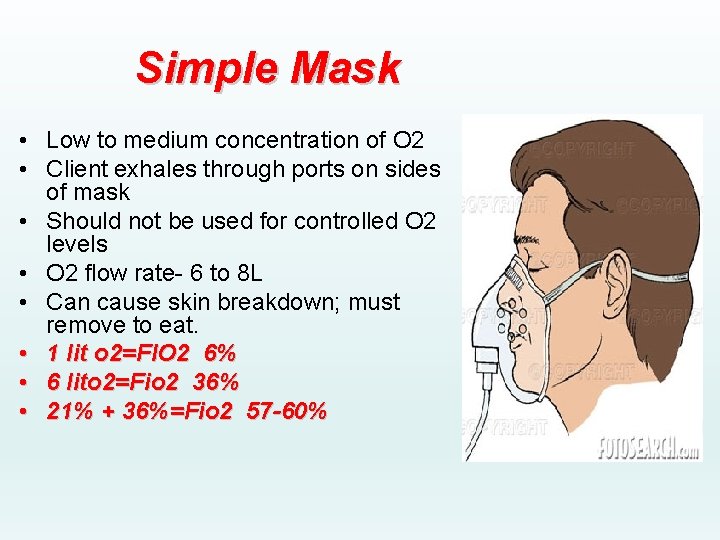
Simple Mask • Low to medium concentration of O 2 • Client exhales through ports on sides of mask • Should not be used for controlled O 2 levels • O 2 flow rate- 6 to 8 L • Can cause skin breakdown; must remove to eat. • 1 lit o 2=FIO 2 6% • 6 lito 2=Fio 2 36% • 21% + 36%=Fio 2 57 -60%
MASK METHOD • Guide mask to patient’s face and apply it from nose downward. • Fit the metal piece of mask to conform to shape of nose. • Secure elastic band around patient’s head • Apply padding behind ears as well as scalp where elastic band passes.
MASK METHOD • Ensure that safety precautions are followed • Inspect patient and equipment frequently for flow rate, clinical condition , level of water in humidifier • Wash hands • Remove the mask and dry the skin every 2 -3 hrs if oxygen is administered continuously.
MASK METHOD • Ensure that safety precautions are followed • Inspect patient and equipment frequently for flow rate, clinical condition , level of water in humidifier • Wash hands • Remove the mask and dry the skin every 2 -3 hrs if oxygen is administered continuously. • Document relevant data in patients record.
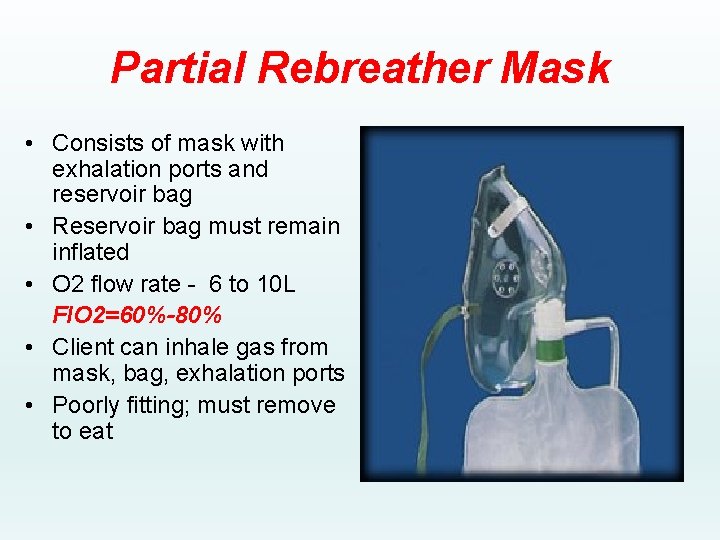
Partial Rebreather Mask • Consists of mask with exhalation ports and reservoir bag • Reservoir bag must remain inflated • O 2 flow rate - 6 to 10 L FIO 2=60%-80% • Client can inhale gas from mask, bag, exhalation ports • Poorly fitting; must remove to eat
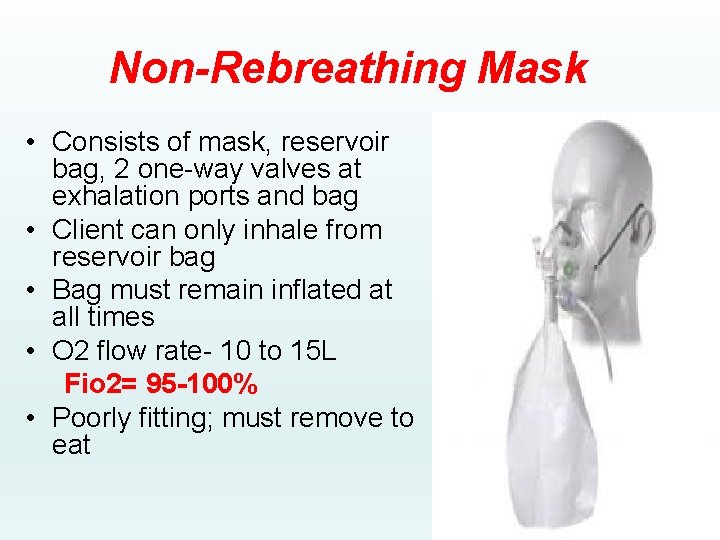
Non-Rebreathing Mask • Consists of mask, reservoir bag, 2 one-way valves at exhalation ports and bag • Client can only inhale from reservoir bag • Bag must remain inflated at all times • O 2 flow rate- 10 to 15 L Fio 2= 95 -100% • Poorly fitting; must remove to eat
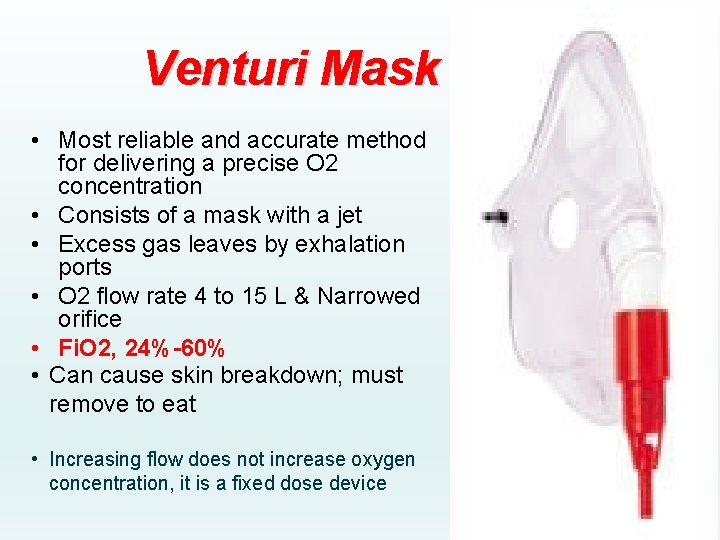
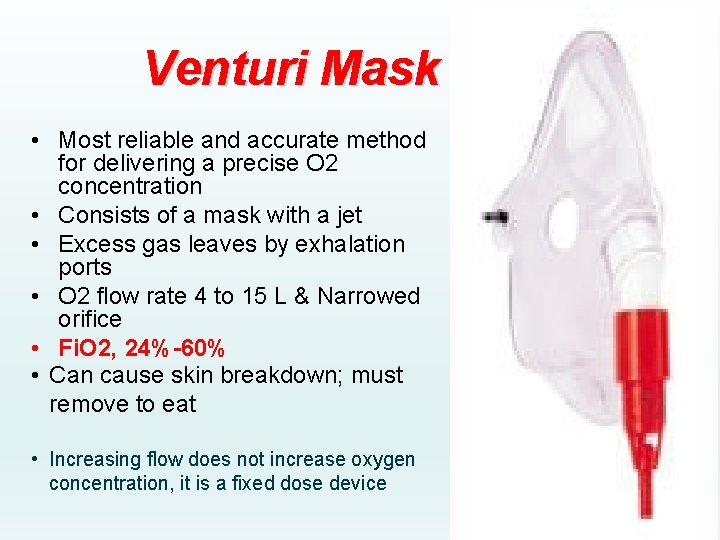
Venturi Mask • Most reliable and accurate method for delivering a precise O 2 concentration • Consists of a mask with a jet • Excess gas leaves by exhalation ports • O 2 flow rate 4 to 15 L & Narrowed orifice • Fi. O 2, 24%-60% • Can cause skin breakdown; must remove to eat • Increasing flow does not increase oxygen concentration, it is a fixed dose device

VENTURI MASK
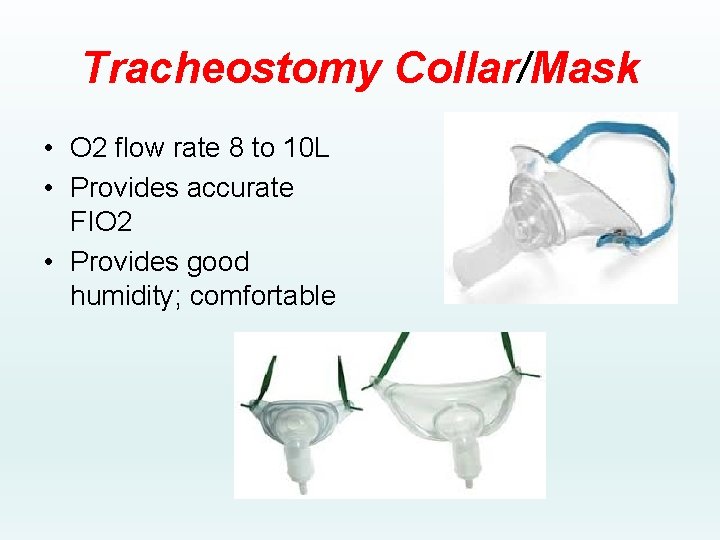
Tracheostomy Collar/Mask • O 2 flow rate 8 to 10 L • Provides accurate FIO 2 • Provides good humidity; comfortable

OXYGEN Oxygen is a drug. When appropriately used, it is extremely beneficial When misused or abused, it is potentially harmful
