Oxygen Delivery vs Oxygen Consumption K Allen Eddington












![DO 2= [O 2 content in blood] x CO [(1. 34 x Hb x DO 2= [O 2 content in blood] x CO [(1. 34 x Hb x](https://slidetodoc.com/presentation_image_h/e65522c2f62c60e355f253ca8dee35ac/image-63.jpg)


- Slides: 76
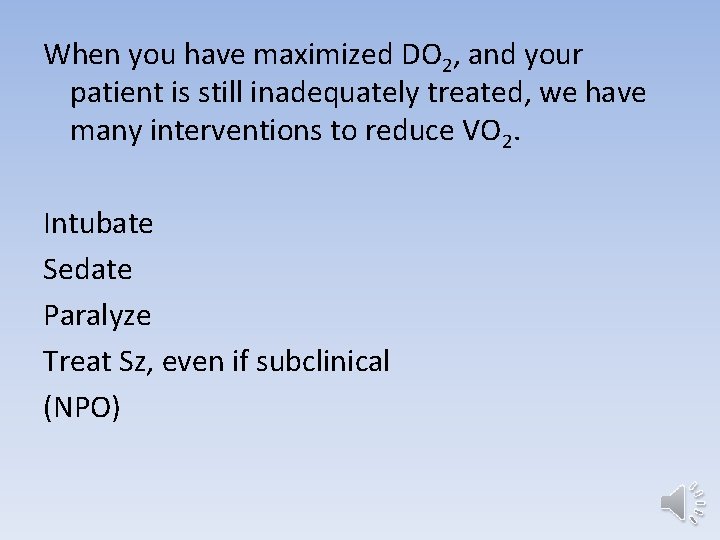
Oxygen Delivery vs Oxygen Consumption K. Allen Eddington, MD, MSc Assistant Professor Pediatric Critical Care Medicine Albert Einstein College of Medicine
Objective: • Demonstrate a framework for the assessment, initial resuscitation, and ongoing reassessment and management of critically ill children, based on physiologic principles of tissue oxygen delivery and oxygen consumption.
• There are several physiologic principles and formulas which are introduced in the second year of medical school…and then often forgotten. • Reviewing these principles and formulas--without necessarily re-memorizing them--can help us prioritize and interpret the patient data we gather when a child is critically ill, and can help guide and prioritize our management. • In my experience, reviewing these principles after a few years of clinical experience, turns them into helpful tools.
• Let’s make this interactive! (I usually do this talk sitting at a table with a pen and paper. )

Oxygen Delivery > Oxygen Consumption (DO 2 > VO 2) If this relationship is not maintained… • Tissue damage begins within minutes • If not corrected, organ damage and death ensue…rather rapidly

Oxygen Delivery > Oxygen Consumption (DO 2 > VO 2) • There a lot of disease entities out there with a lot of treatments we all have to know, but they tend to take time to work. • In critically ill patients, the focus is on maintaining DO 2 > VO 2, while we wait for other treatments to work.
In simplistic terms, what are the steps a molecule of oxygen has to take to get from the outside environment to the mitochondria of a cell in your baby toe? If you need help reading my mind, I’m thinking of 4 major steps.
• Air (including oxygen) is drawn in from the environment to the alveoli • Oxygen diffuses across the alveolar and capillary membranes into the blood • Oxygen is carried in the blood to a capillary near a cell in your baby toe. • Oxygen diffuses across the capillary and cellular membranes into the mitochondria (where it is used in oxidative phosphorylation to generate ATP, which the cell uses to fill its energy requirements)

Let’s look at the physiology of each of these steps more closely, to see • how patients (especially children) compensate when something doesn’t work well • what clinical data is most critical to gather • what interventions will most directly address maintaining DO 2 > VO 2 at each step
• Air (including oxygen) is drawn in from the environment to the alveoli • Oxygen diffuses across the alveolar and capillary membranes into the blood • Oxygen is carried in the blood to a capillary near a cell in your baby toe. • Oxygen diffuses across the capillary and cellular membranes into the mitochondria (where it is used in oxidative phosphorylation to generate ATP, which the cell uses to fill its energy requirements)
Air is drawn in from the environment to the alveoli What parameters determine the content of oxygen transferred in this step? • Respiratory rate (RR) • Tidal Volume (Vt) • Fraction of inhaled oxygen (Fi. O 2)

Vt (ml) x RR (bpm) x Fi. O 2 (%) = volume of inspired oxygen per minute (l/min) Examples; Healthy, 1 month-old, 4 kg 30 ml air x 35 bpm x 0. 21 oxygen/volume air = 220 ml of oxygen/min Healthy, 16 year-old, 60 kg 450 ml air x 14 bpm x 0. 21 oxygen/volume air = 1300 ml of oxygen/min
In infants, the ability to accelerate RR > the ability to increase Vt (When RR increases greatly, Vt decreases) In teens and adults, the ability to increase Vt > the ability to accelerate RR

Examples; Stressed, 1 month-old, 4 kg 25 ml x 90 bpm x 0. 21 = 475 ml O 2 /min (475 -220)/220 x 100% = 115% increase Stressed 16 y/o, 60 kg 900 ml x 30 bpm x 0. 21 = 5600 ml O 2 /min (5600 -1300)/1300 x 100% = 330% increase
How is this clinically meaningful? Children of all ages have the capacity to significantly compensate for increased oxygen requirement by increasing RR and Vt.
How is this clinically meaningful? Take home point: If a patient’s compensatory mechanism is intact, but not in use, respiratory failure is not imminent.
How is this clinically meaningful? It is usually obvious when the compensatory mechanism is NOT intact. • Severe neurological impairment • Tiring after prolonged compensation Check if the baby accelerates when you approach or when you stick him, then calms back down. • Of note, most infants can breathe in the 70 -90’s for several DAYS before “getting tired”.
How is this clinically meaningful? When you communicate with the PICU about respiratory patients, we are AXIOUSLY awaiting a current and accurate respiratory rate! Right before you call, clock the kid yourself, and tell me EARLY in the presentation.

How is this clinically meaningful? Other tidbits you might be tempted to tell me first • how impressive the stridor is • how deep the retractions are • or what poor air entry you hear on ausultation. … are all more meaningful in the context of a current RR.
How is this clinically meaningful? I only barely care about the RR on initial presentation, so please tell me where we are now, then tell me about the journey to get there. (Telling the punchline and then the set-up makes for bad joke telling, but great critical care communication!)
When you identify patients in respiratory distress, what fundemental treatments most directly address and maximize this step in oxygen transport? • 100% Fi. O 2 • Mechanical assistance to optimize Vt and RR • (Various specific treatments for obstructive and restrictive airway and lung disease)
• Air (including oxygen) is drawn in from the environment to the alveoli • Oxygen diffuses across the alveolar and capillary membranes into the blood • Oxygen is carried in the blood to a capillary near a cell in your baby toe. • Oxygen diffuses across the capillary and cellular membranes into the mitochondria (where it is used in oxidative phosphorylation to generate ATP, which the cell uses to fill its energy requirements)
Oxygen diffuses across the alveolar and capillary membranes into the blood What parameters determine the content of oxygen transferred in this step? • Permeability of the membranes to oxygen • Functional surface area of the membranes • Concentration gradient
How do we assess the ability of oxygen to diffuse in a particular patient? A-a gradient…. the classic answer PAO 2 –Pa. O 2 = Fi. O 2 (Patm-PH 2 O) – Pa. CO 2/0. 8 Doable, but not handy.
How do we assess the ability of oxygen to diffuse in a particular patient? Other estimates include : • Pa. O 2/Fi. O 2 ratio • SPO 2/Fi. O 2 ratio • Oxygenation Index, when mechanically ventilated – (Mean Airway Pressure x Fi. O 2)/Pa. O 2

How do we assess the ability of oxygen to diffuse in a particular patient? Other estimates include : • Pa. O 2/Fi. O 2 ratio • SPO 2/Fi. O 2 ratio These are intuitive, simple to remember, and simple to calculate.
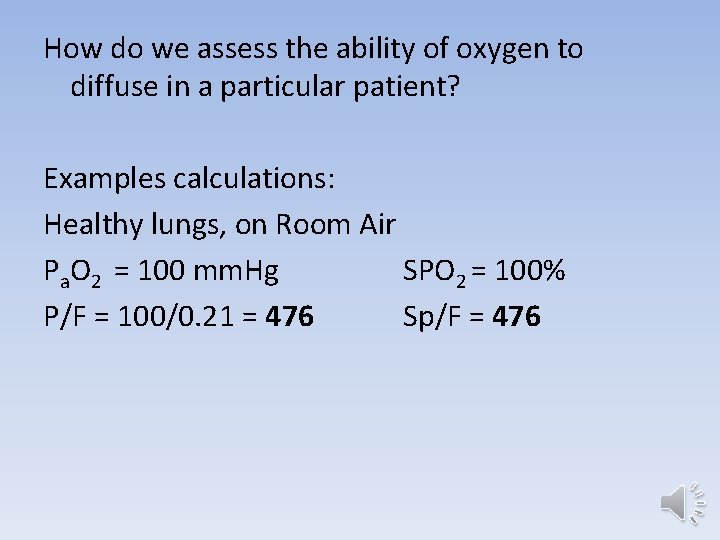
How do we assess the ability of oxygen to diffuse in a particular patient? Examples calculations: Healthy lungs, on Room Air Pa. O 2 = 100 mm. Hg SPO 2 = 100% P/F = 100/0. 21 = 476 Sp/F = 476
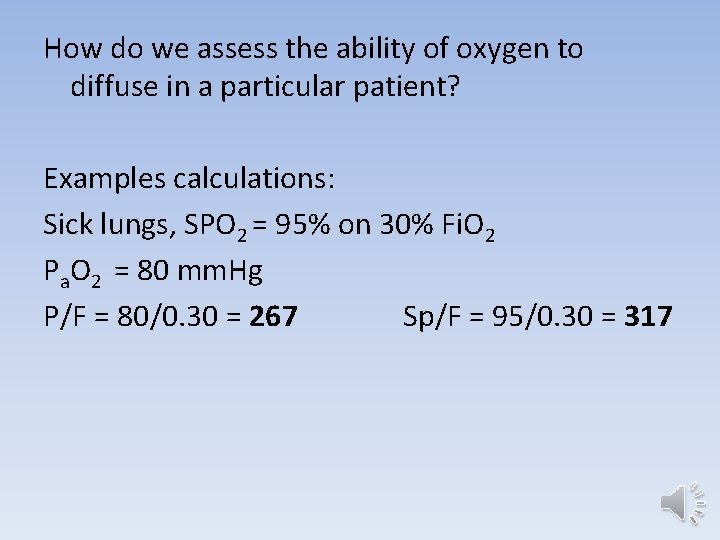
How do we assess the ability of oxygen to diffuse in a particular patient? Examples calculations: Sick lungs, SPO 2 = 95% on 30% Fi. O 2 Pa. O 2 = 80 mm. Hg P/F = 80/0. 30 = 267 Sp/F = 95/0. 30 = 317
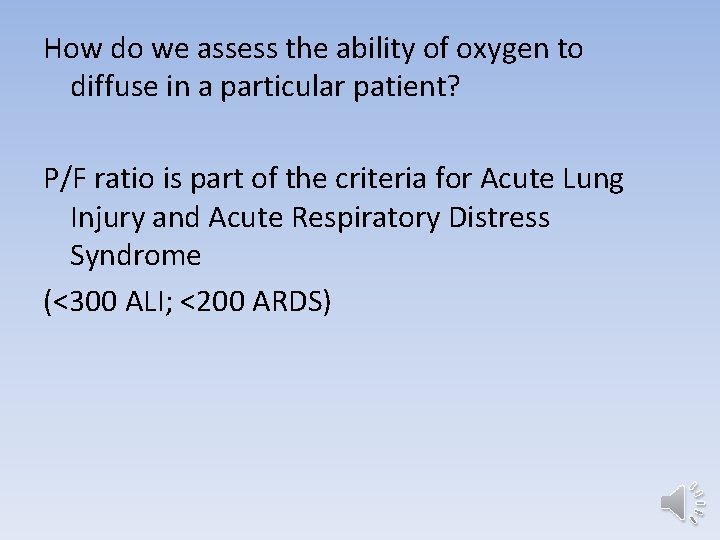
How do we assess the ability of oxygen to diffuse in a particular patient? P/F ratio is part of the criteria for Acute Lung Injury and Acute Respiratory Distress Syndrome (<300 ALI; <200 ARDS)
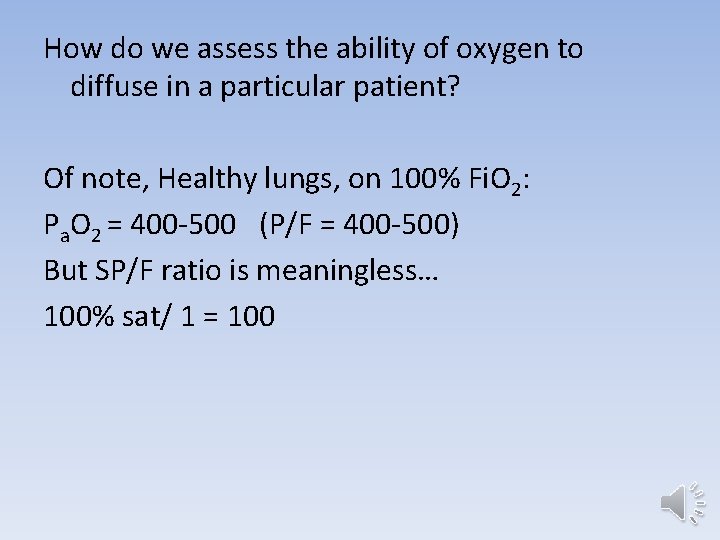
How do we assess the ability of oxygen to diffuse in a particular patient? Of note, Healthy lungs, on 100% Fi. O 2: Pa. O 2 = 400 -500 (P/F = 400 -500) But SP/F ratio is meaningless… 100% sat/ 1 = 100
How do we assess the ability of oxygen to diffuse in a particular patient? Take home point: To non-invasively assess oxygen requirement with SP/F ratio, patients on supplemental oxygen need to saturate 99% or less. You may still want to increase the Fi. O 2 to 100% in the early stages of care, but be aware of the distinction between your assessment and your treatment.
Oxygen moves slowly across the membrane in healthy patients, and even more slowly when lung disease is present, so the functional surface area of the alveolar/capillary membrane is paramount to oxygen movement.
Carbon dioxide moves across the alveolar/capillary membrane rapidly. Functional alveolar surface area is rarely if ever a limiting factor to CO 2 removal.
Membrane diffusion is the rate limiting step in oxygen delivery to the blood, while movement from the alveoli to the outside environment is the rate limiting step for CO 2 removal. In respiratory failure, it’s important to distinguish between oxygenation failure and failure of CO 2 removal.
How does this help me take better care of my patients? • Mechanical ventilator settings predominately address one or the other. • Settings that directly affect the minute ventilation will predominately affect CO 2 removal. – RR – Vt or positive inspiratory pressure (PIP)
How does this help me take better care of my patients? • Mean airway pressure (MAP) is the primary determinant of the lung’s volume. • With increased lung volume is increased functional alveolar surface volume
How does this help me take better care of my patients? • MAP is determined by positive end-exipratory pressure (PEEP)>>Vt/PIP, RR, Inspiratory Time, slope of breath delivery. • And obviously, Fi. O 2 influences O 2 delivery without effecting CO 2 removal
• Air (including oxygen) is drawn in from the environment to the alveoli • Oxygen diffuses across the alveolar and capillary membranes into the blood • Oxygen is carried in the blood to a capillary near a cell in your baby toe. • Oxygen diffuses across the capillary and cellular membranes into the mitochondria (where it is used in oxidative phosphorylation to generate ATP, which the cell uses to fill its energy requirements)
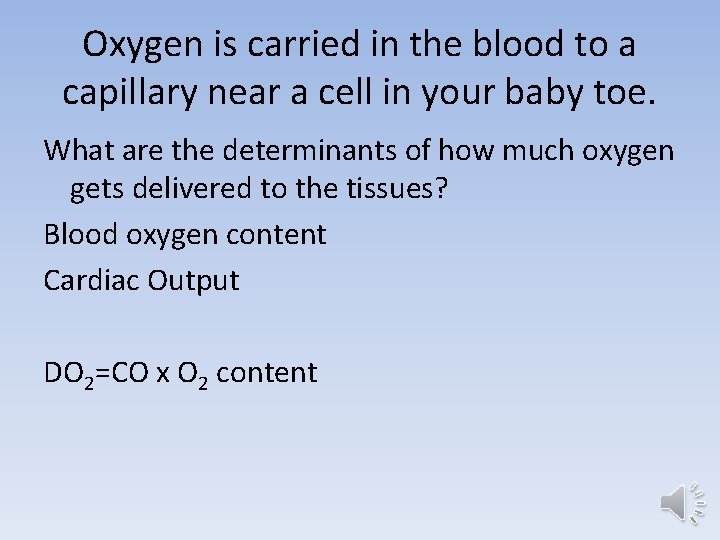
Oxygen is carried in the blood to a capillary near a cell in your baby toe. What are the determinants of how much oxygen gets delivered to the tissues? Blood oxygen content Cardiac Output DO 2=CO x O 2 content

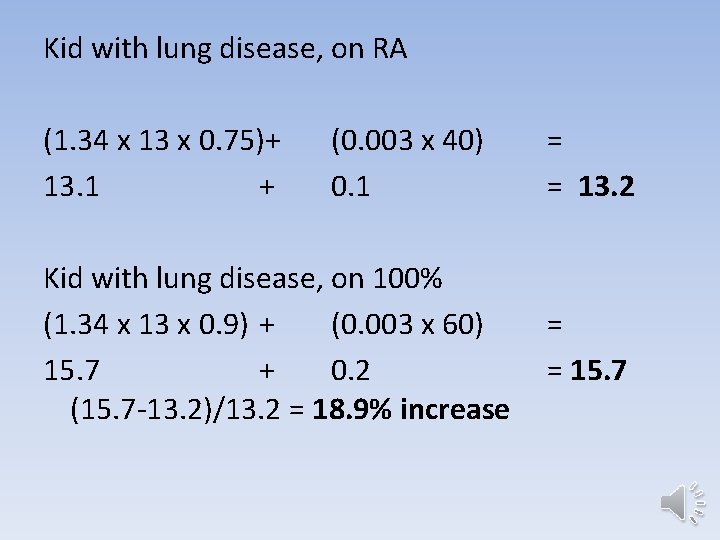
What are the determinants of blood oxygen content? Hb bound O 2 + 1. 34 x Hb x sat (as integer) + Dissolved O 2 0. 003 x Pa. O 2 To get familiar with the norms and implications of different derangements, we’ll do some example calculations.

Normal kid, on room air Hb bound Dissolved (1. 34 x 13 x 1) + (0. 003 x 90) 17. 4 + 0. 3 Normal kid, on 100% Fi. O 2 17. 4 + (0. 003 x 500) 17. 4 + 1. 5 (18. 9 -17. 7)/17. 7 = 6. 7% increase = = 17. 7 = = 18. 9
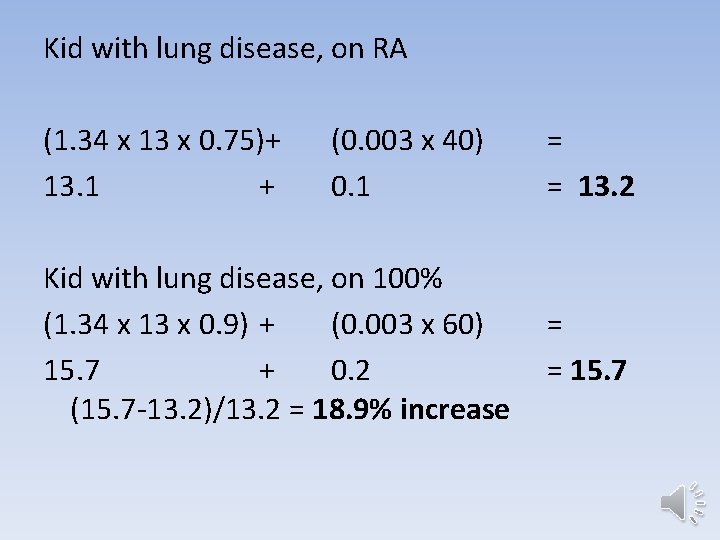
Kid with lung disease, on RA (1. 34 x 13 x 0. 75)+ (0. 003 x 40) 13. 1 + 0. 1 Kid with lung disease, on 100% (1. 34 x 13 x 0. 9) + (0. 003 x 60) 15. 7 + 0. 2 (15. 7 -13. 2)/13. 2 = 18. 9% increase = = 13. 2 = = 15. 7
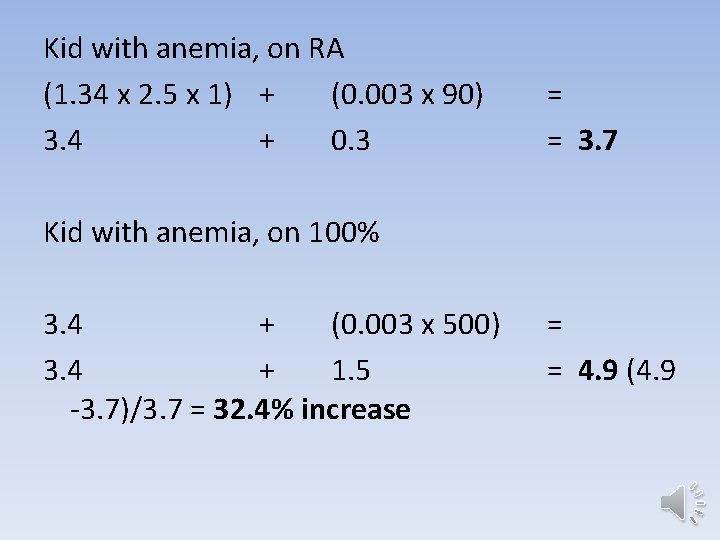
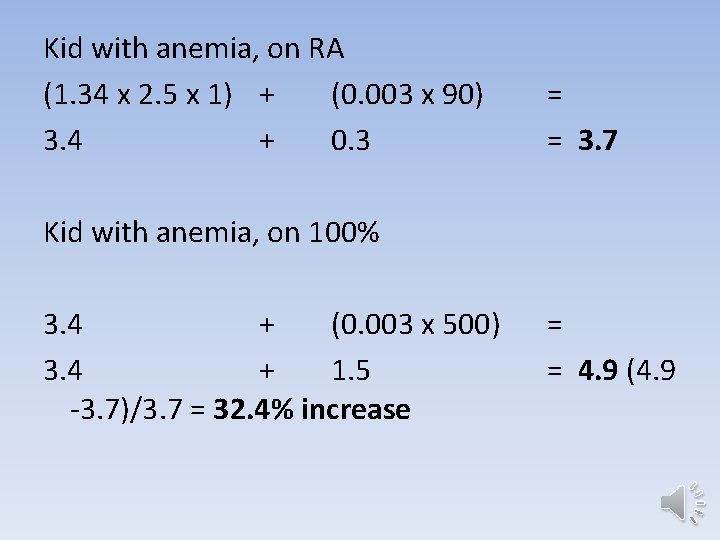
Kid with anemia, on RA (1. 34 x 2. 5 x 1) + (0. 003 x 90) 3. 4 + 0. 3 Kid with anemia, on 100% 3. 4 + (0. 003 x 500) 3. 4 + 1. 5 -3. 7)/3. 7 = 32. 4% increase = = 3. 7 = = 4. 9 (4. 9

Kid with cyanotic heart disease, on RA (1. 34 x 16 x 0. 75) + (0. 003 x 40) = 16. 1 + 0. 1 = 16. 2 Kid with cyanotic heart disease, on 100% (Don’t try this at home!!) (1. 34 x 16 x 0. 9) + (0. 003 x 60) = 19. 3 + 0. 2 = 19. 5 (19. 5 -16. 2)/16. 2 = 20. 4 % increase
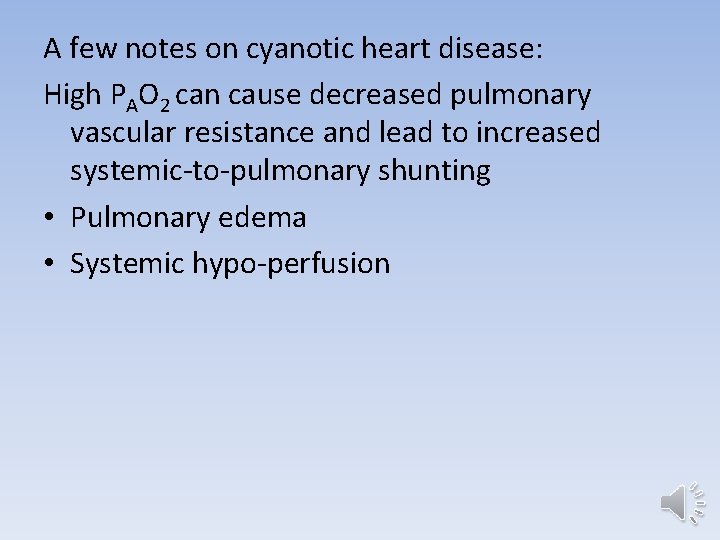
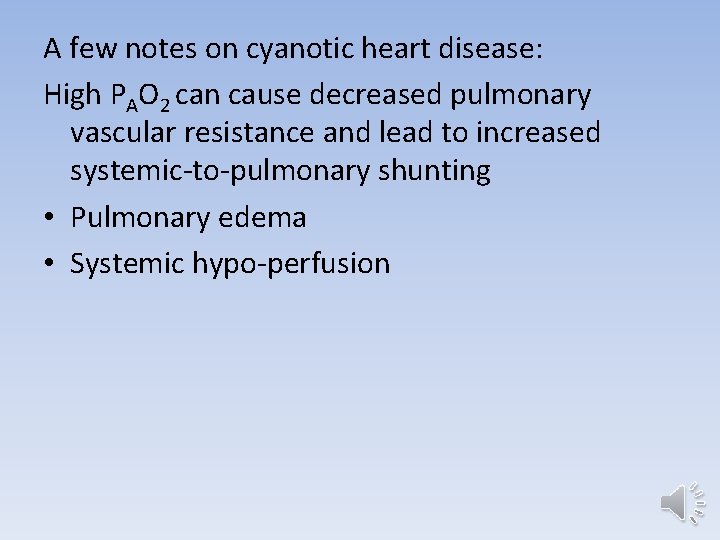
A few notes on cyanotic heart disease: High PAO 2 can cause decreased pulmonary vascular resistance and lead to increased systemic-to-pulmonary shunting • Pulmonary edema • Systemic hypo-perfusion
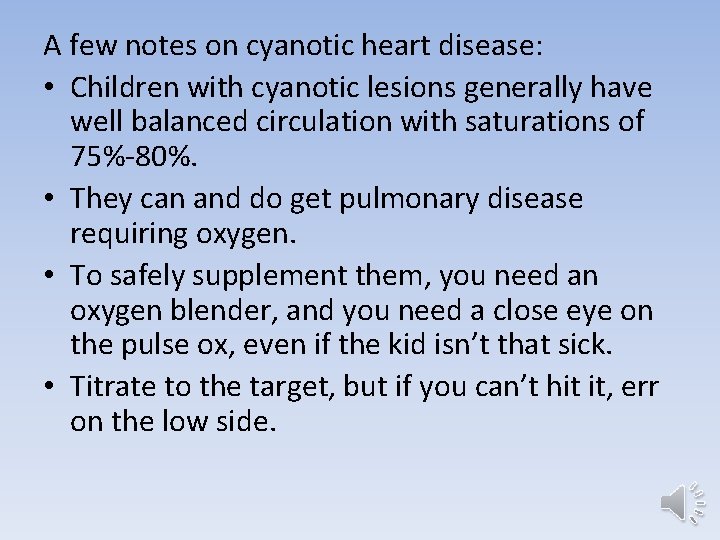
A few notes on cyanotic heart disease: • Children with cyanotic lesions generally have well balanced circulation with saturations of 75%-80%. • They can and do get pulmonary disease requiring oxygen. • To safely supplement them, you need an oxygen blender, and you need a close eye on the pulse ox, even if the kid isn’t that sick. • Titrate to the target, but if you can’t hit it, err on the low side.
Take home points on blood oxygen content: • Children in distress should (almost) ALL get supplemental oxygen via non-rebreather in the initial phase of resuscitation. • The roll of dissolved oxygen is usually negligible, but not always. In cases of severe anemia, supplemental oxygen significantly increases DO 2 until a transfusion can be given, even if the patient sats 100% on RA at presentation.
Take home points on blood oxygen content: • Children with cyanotic lesions are polycythemic to compensate for their persistently desaturated state, so don’t let the low sats scare you. Don’t over-think them; unless peds cardio tells you differently for a particular child, a saturation as close to 75% as you can get should be the goal.
Enough about blood oxygen content! On to Cardiac Output!
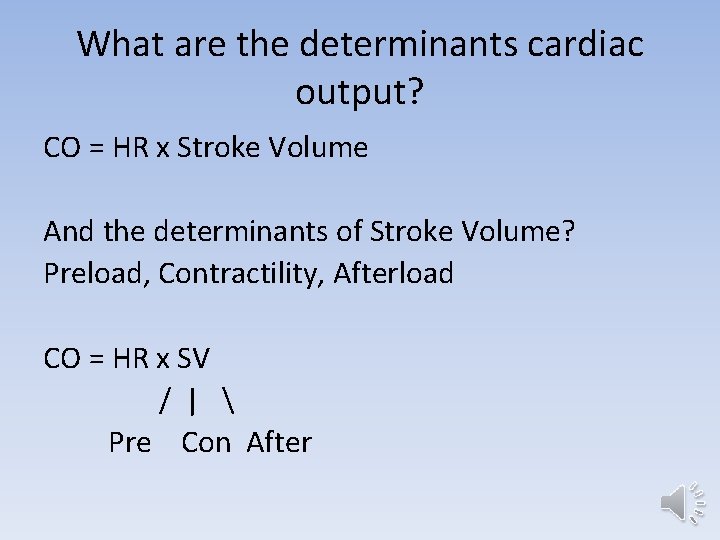
What are the determinants cardiac output? CO = HR x Stroke Volume And the determinants of Stroke Volume? Preload, Contractility, Afterload CO = HR x SV / | Pre Con After
What is a child’s primary compensatory mechanism when DO 2 is insufficient for VO 2? Tachycardia, Tachycardia (Also brought on by fever, pain, anxiety, etc. )
What is a child’s primary compensatory mechanism when DO 2 is insufficient for VO 2? • In the first months of life, tachycardia to the 180 s is common and not impressive. • Breastfeeding may be enough to induce it. • Intermittent tachycardia to 200 s or 220 s should raise a red flag, but isn’t particularly rare, either.
So how do I know what HR is worrisome? • Watch for variability. • A baby who works his way up to 220 for a few seconds and calms back down to 180 is not in SVT (which usually starts around 240), and is less worrisome than a baby stuck at 180 or stuck at 220.

So how do I know what HR is worrisome? • Watch the response to your interventions. • Giving oxygen and giving fluid boluses should result in significant improvements in tachycardia.
Take home point: A patient who has shown the capacity for tachycardia, who has a normal HR now, has adequate DO 2 for his needs.
As we look at the our initial interventions for critically ill patients —even without a diagnosis—they fall clearly within the paradigm of DO 2 vs VO 2. • Deliver 100% Fi. O 2 • Assess perfusion, assist if necessary • Secure airway, assist breathing if necessary
• Continuous monitoring for HR, RR, Sat (and frequent BP) • Maximize preload (bolus, bolus) • Augment contractility (inotropes) • Augment HR (chronotropes)
When a baby is brought back to the resuscitation room grey and lifeless, the initial decisions are easy. Children not quite as sick, or those who respond well to initial interventions, but have persistant derangements in labs, vitals, or physical exam are more anxiety provoking for providers.
What are the best objective measures to assess the relationship of DO 2 and VO 2 in your patient? (IE, What can tell you that your patient is good enough for now versus that you need to continue active interventions? )
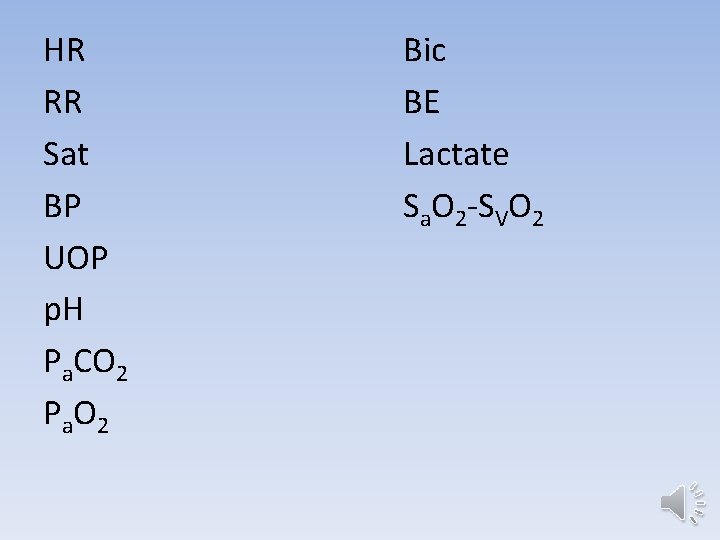
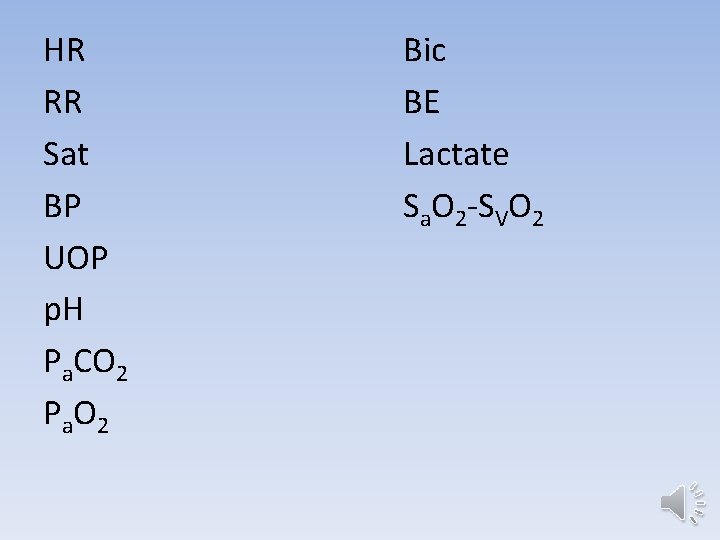
HR RR Sat BP UOP p. H Pa. CO 2 P a. O 2 Bic BE Lactate Sa. O 2 -SVO 2
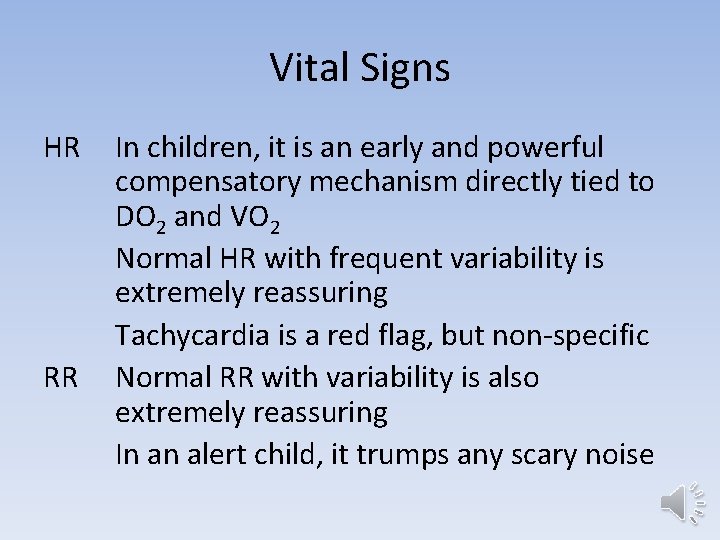
Vital Signs HR RR In children, it is an early and powerful compensatory mechanism directly tied to DO 2 and VO 2 Normal HR with frequent variability is extremely reassuring Tachycardia is a red flag, but non-specific Normal RR with variability is also extremely reassuring In an alert child, it trumps any scary noise

Vital Signs Sat Important and telling, but doesn’t directly address DO 2 at the tissue level BP The VS which impresses me the least and tells me the least. If you don’t have one, you die, but unless it is a very extreme value, it’s not very telling in children (Where is BP in the DO 2 formula? )
![DO 2 O 2 content in blood x CO 1 34 x Hb x DO 2= [O 2 content in blood] x CO [(1. 34 x Hb x](https://slidetodoc.com/presentation_image_h/e65522c2f62c60e355f253ca8dee35ac/image-63.jpg)
DO 2= [O 2 content in blood] x CO [(1. 34 x Hb x Sat) + (0. 003 x. Pa. O 2)] x HR x SV / | Pre Con After ↑ BP

Tools to assess DO 2 vs VO 2 UOP Tells me about perfusion, a big chunk of the equation, but doesn’t exactly answer the question. p. H Tells me if my pt acidemic…Insufficient DO 2 can cause acidemia Pa. CO 2 Good info…helps me interpret my p. H, but doesn’t address my question. BIC doesn’t directly address the question
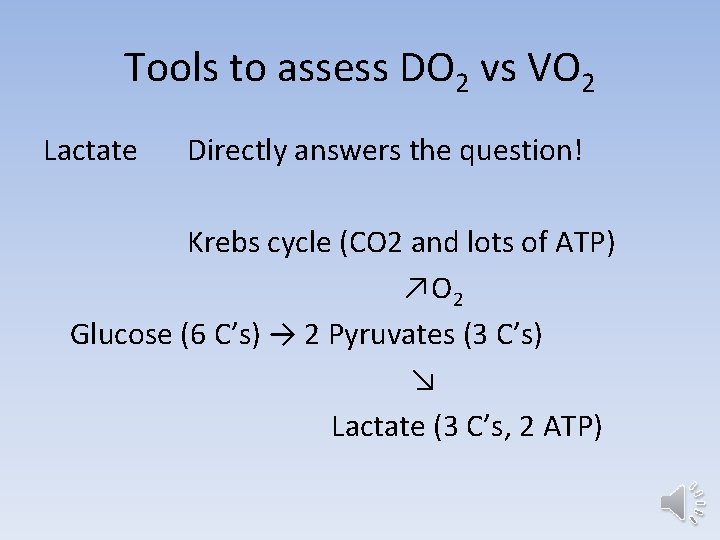
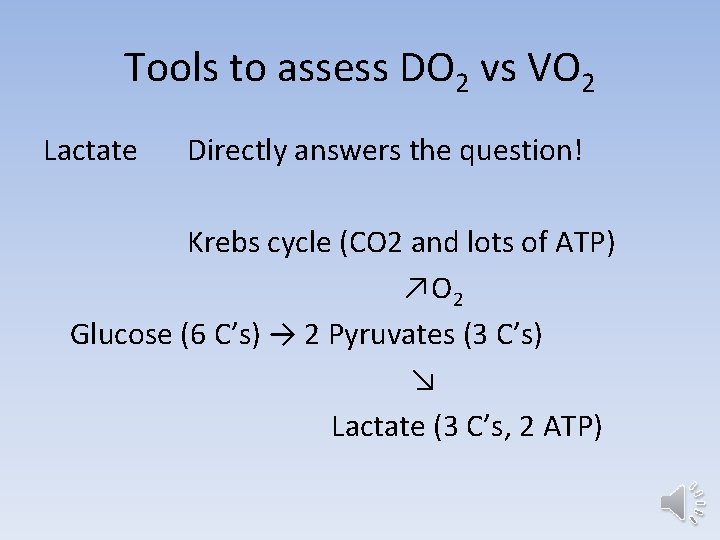
Tools to assess DO 2 vs VO 2 Lactate Directly answers the question! Krebs cycle (CO 2 and lots of ATP) ↗O 2 Glucose (6 C’s) → 2 Pyruvates (3 C’s) ↘ Lactate (3 C’s, 2 ATP)
Tools to assess DO 2 vs VO 2 Lactate Directly answers the question! Accumulates in minutes Clears in minutes to hours Easy to trend Can be elevated in certain metabolic diseases

Tools to assess DO 2 vs VO 2 Sa. O 2 -SVO 2 Directly answers the question! Measures oxygen extraction (Don’t confuse Sa. O 2 with Pa. O 2) Normal 25 ish, above 40 is worrisome in Maybe falsely reassuring in mitochondrial dysfunction (like some cases of sepsis)
Case #1 5 y/o, 20 kg boy presents with RR 40 -50’s and labored breathing, peri-oral cyanosis, and ill appearance, after 3 days of “a bad cold”. He has no significant PMH. The pt remains cyanotic, though mildly improved, after non-rebreather, then a brief trial of Bi. PAP. Ultimately, he is intubated in the ED for saturations in the low 80’s and persistent distress.
Case #1 (PICU attending is coming, but is stuck on a bridge…He predicts he will another 2 hours, at least. ) Post intubation CXR shows a tube in good position and diffuse bilateral infiltrates with areas of atelectasis.
Case #1 The patient has only stirred occasionally since intubation. Current vent settings are 150 ml/5 peep x 22, Fi. O 2 100% Sats 85% RR 22 Peak Pressure 28 ABG 7. 25/60/50
Case #1 How do you assess this patient’s DO 2 vs VO 2? If you determine it is necessary, how can you improve his oxygen balance?
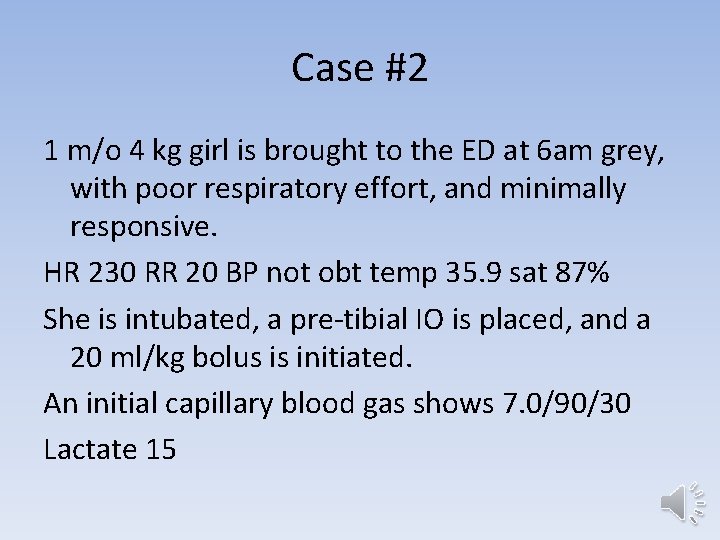
Case #2 1 m/o 4 kg girl is brought to the ED at 6 am grey, with poor respiratory effort, and minimally responsive. HR 230 RR 20 BP not obt temp 35. 9 sat 87% She is intubated, a pre-tibial IO is placed, and a 20 ml/kg bolus is initiated. An initial capillary blood gas shows 7. 0/90/30 Lactate 15
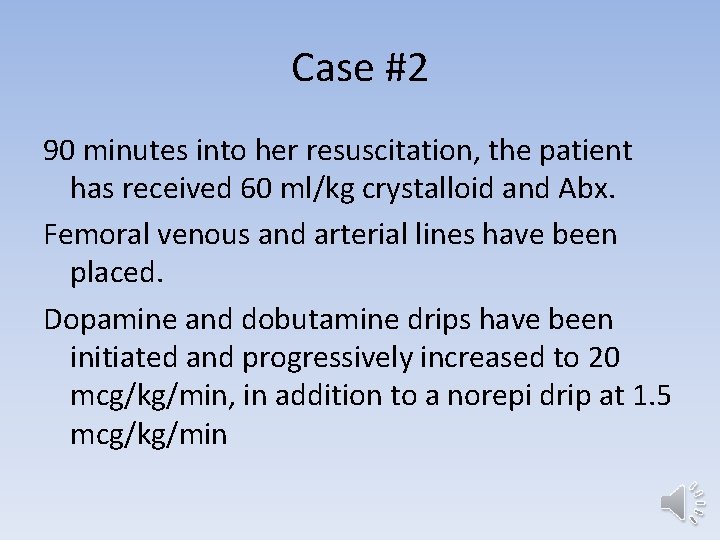
Case #2 90 minutes into her resuscitation, the patient has received 60 ml/kg crystalloid and Abx. Femoral venous and arterial lines have been placed. Dopamine and dobutamine drips have been initiated and progressively increased to 20 mcg/kg/min, in addition to a norepi drip at 1. 5 mcg/kg/min
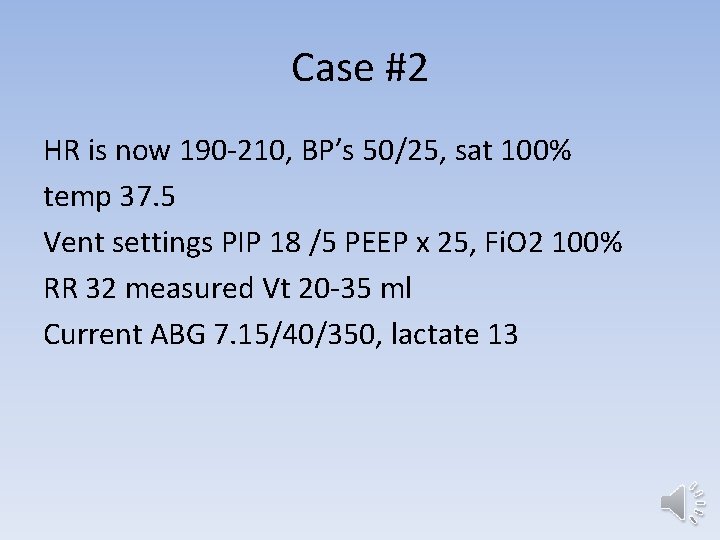
Case #2 HR is now 190 -210, BP’s 50/25, sat 100% temp 37. 5 Vent settings PIP 18 /5 PEEP x 25, Fi. O 2 100% RR 32 measured Vt 20 -35 ml Current ABG 7. 15/40/350, lactate 13
Case #2 How do you assess this patient’s DO 2 vs VO 2? If you determine it is necessary, how can you improve her oxygen balance?
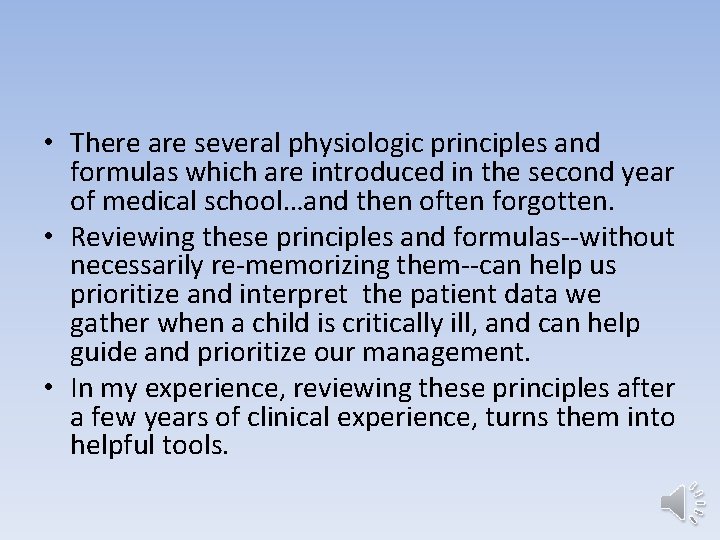
When you have maximized DO 2, and your patient is still inadequately treated, we have many interventions to reduce VO 2. Intubate Sedate Paralyze Treat Sz, even if subclinical (NPO)
 Postulates of special theory of relativity
Postulates of special theory of relativity Eddington approximation grey atmosphere
Eddington approximation grey atmosphere Blockreim
Blockreim Tracheostomy oxygen delivery
Tracheostomy oxygen delivery Indications of oxygen therapy
Indications of oxygen therapy Non rebreather mask nursing considerations
Non rebreather mask nursing considerations Venturi mask oxygen flow rate
Venturi mask oxygen flow rate Accenture delivery tools list
Accenture delivery tools list Intermediate consumption
Intermediate consumption Objectives of personality
Objectives of personality Milk consumption and height
Milk consumption and height Definition of food preparation
Definition of food preparation Difference between investment and consumption
Difference between investment and consumption The life-cycle model of consumption and saving
The life-cycle model of consumption and saving Fuel consumption
Fuel consumption Autonomous investment
Autonomous investment Functional tea market share
Functional tea market share Polysynchronous classroom
Polysynchronous classroom Daily cigarette consumption
Daily cigarette consumption Food consumption score interpretation
Food consumption score interpretation Keynesian consumption function
Keynesian consumption function Consumer behavior in a service context
Consumer behavior in a service context Subculture of consumption examples
Subculture of consumption examples Dr sait uysal
Dr sait uysal Mean effective pressure
Mean effective pressure Keynes psychological law of consumption
Keynes psychological law of consumption Hpe green lake
Hpe green lake Chapter 7 consumer behavior
Chapter 7 consumer behavior Essential consumption
Essential consumption Consumption expenditures formula
Consumption expenditures formula Meat consumption
Meat consumption Freud personality types
Freud personality types Consumption diary example
Consumption diary example Determinants of consumption
Determinants of consumption Cad theory of personality
Cad theory of personality Sustainable clothing consumption
Sustainable clothing consumption Drinking fountain
Drinking fountain Consumption in science
Consumption in science Autonomous consumption
Autonomous consumption Consumption function formula
Consumption function formula Consequences of underage drinking
Consequences of underage drinking Rationalization of water consumption
Rationalization of water consumption A small, hard, dry seed harvested for human consumption.
A small, hard, dry seed harvested for human consumption. Fan in cmos
Fan in cmos Flat indifference curve
Flat indifference curve World tea consumption
World tea consumption Pluralization of consumption
Pluralization of consumption What is dynamic resolution scaling
What is dynamic resolution scaling Ethics of food production and consumption
Ethics of food production and consumption Gross capital formation formula
Gross capital formation formula Consumption in science
Consumption in science Consumption choice set
Consumption choice set Nexus 5010 layer 3
Nexus 5010 layer 3 Lack of carbohydrates
Lack of carbohydrates Dell finacial
Dell finacial Efsa comprehensive european food consumption database
Efsa comprehensive european food consumption database Alcohol consumption causes blood vessels to contract
Alcohol consumption causes blood vessels to contract Consumption in science
Consumption in science Sacred consumption
Sacred consumption Consumption meaning
Consumption meaning Maryam kamgarpour
Maryam kamgarpour The equilibrium level of real gdp
The equilibrium level of real gdp Total consumption burner
Total consumption burner Consumption in science
Consumption in science Keynesian consumption function
Keynesian consumption function Server power consumption
Server power consumption Merit goods vs public goods
Merit goods vs public goods Japan rice consumption
Japan rice consumption Mri energy consumption
Mri energy consumption Cisco ucs bios
Cisco ucs bios Exercise may alcohol consumption
Exercise may alcohol consumption Subcultures of consumption
Subcultures of consumption How exercise affect our consumption
How exercise affect our consumption History of milk consumption
History of milk consumption Government spending multiplier
Government spending multiplier Sacred and profane consumption
Sacred and profane consumption Fuel consumption
Fuel consumption