Oxygen Therapy Mark Carpenter ICU Consultant CHS Jan









- Slides: 56
Oxygen Therapy Mark Carpenter ICU Consultant CHS Jan 2016
Quiz 1. 2. 3. 4. 5. High-flow oxygen (non-rebreathe mask) Controlled oxygen therapy (24% etc) NIV on respiratory ward Call ICU for consideration of ventilation No need for Oxygen therapy
Lifelong smoker admitted with cough: Sp. O 2 82%, p. H 7. 4, p. CO 2 8. 0 p. O 2 5. 4 1. 2. 3. 4. 5. High-flow oxygen (nonrebreathe mask) Controlled oxygen therapy (24% etc) NIV on respiratory ward Call ICU for consideration of ventilation No need for Oxygen therapy
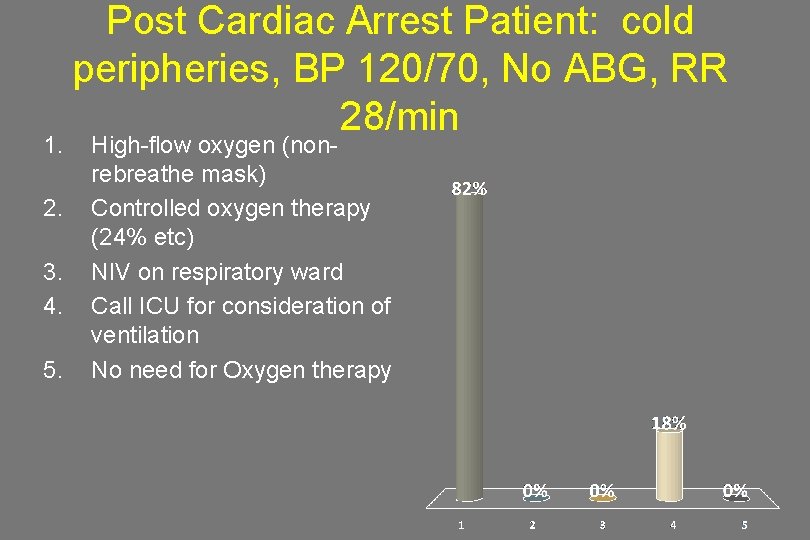
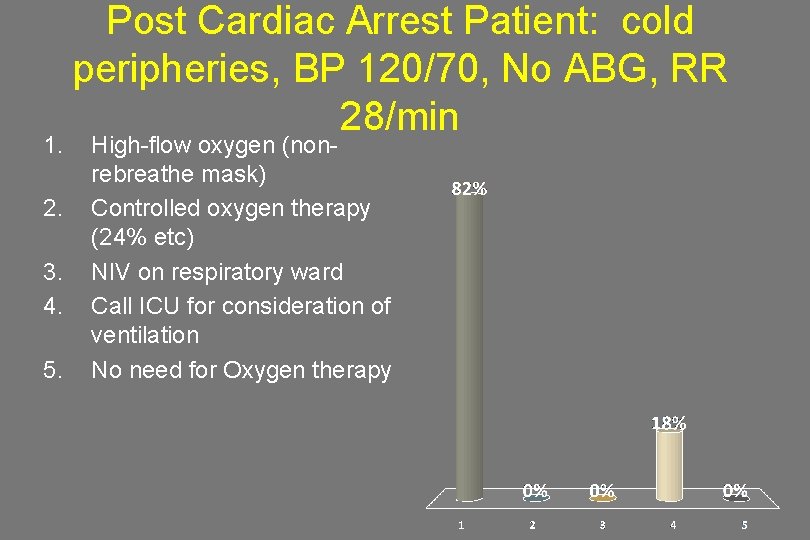
1. 2. 3. 4. 5. Post Cardiac Arrest Patient: cold peripheries, BP 120/70, No ABG, RR 28/min High-flow oxygen (nonrebreathe mask) Controlled oxygen therapy (24% etc) NIV on respiratory ward Call ICU for consideration of ventilation No need for Oxygen therapy
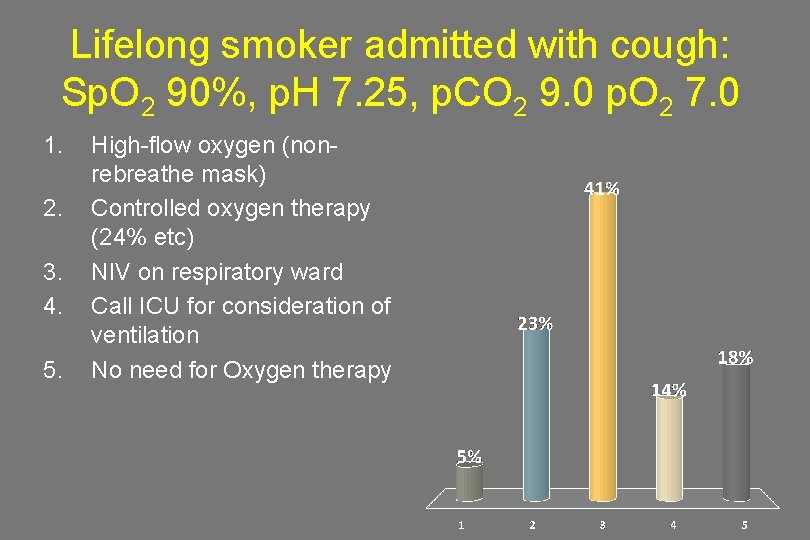
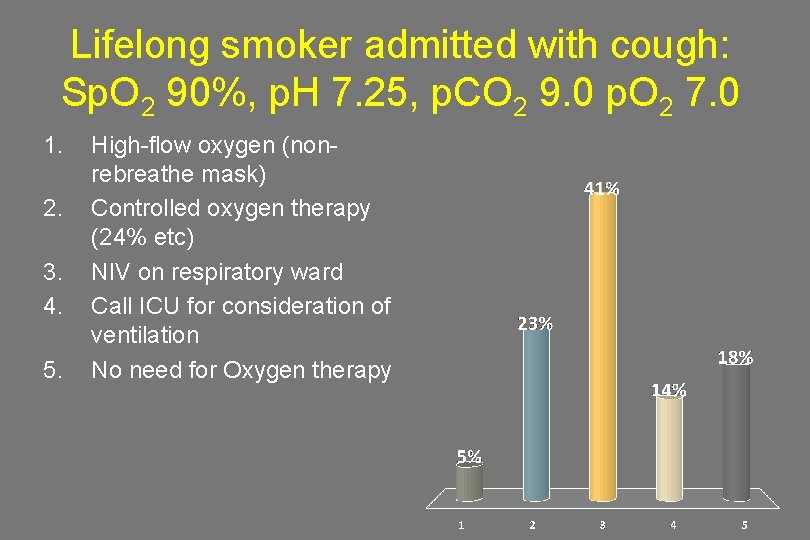
Lifelong smoker admitted with cough: Sp. O 2 90%, p. H 7. 25, p. CO 2 9. 0 p. O 2 7. 0 1. 2. 3. 4. 5. High-flow oxygen (nonrebreathe mask) Controlled oxygen therapy (24% etc) NIV on respiratory ward Call ICU for consideration of ventilation No need for Oxygen therapy
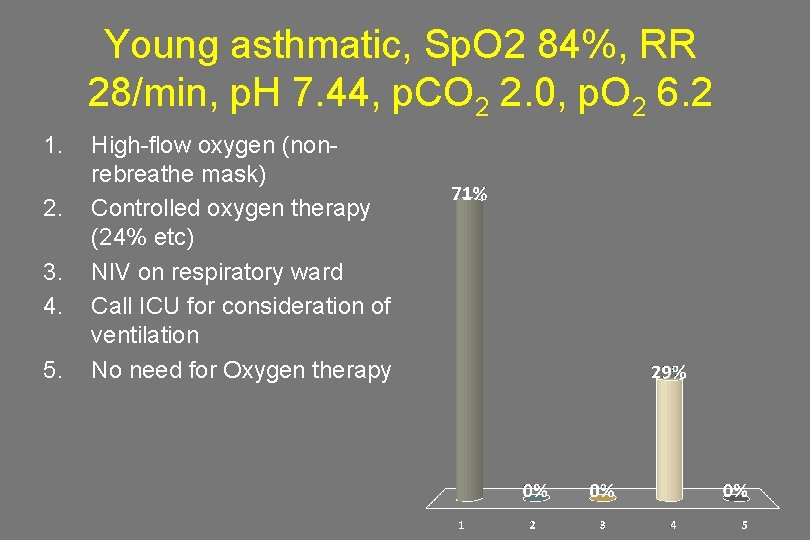
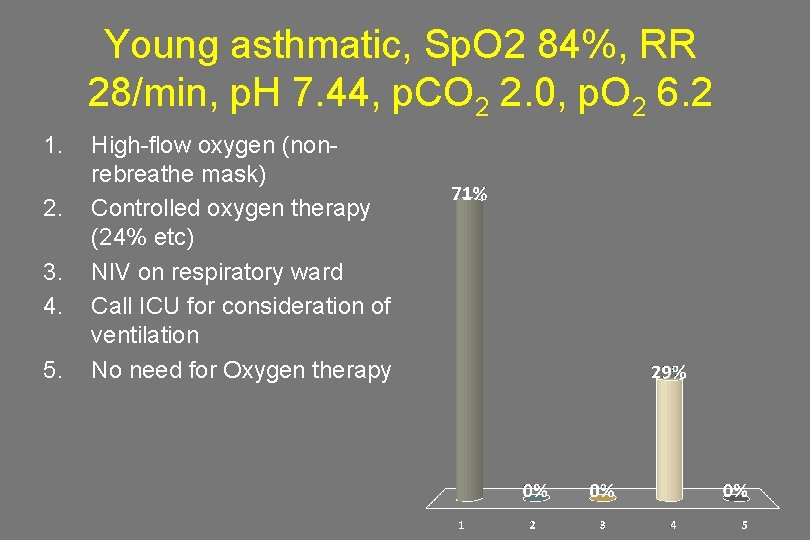
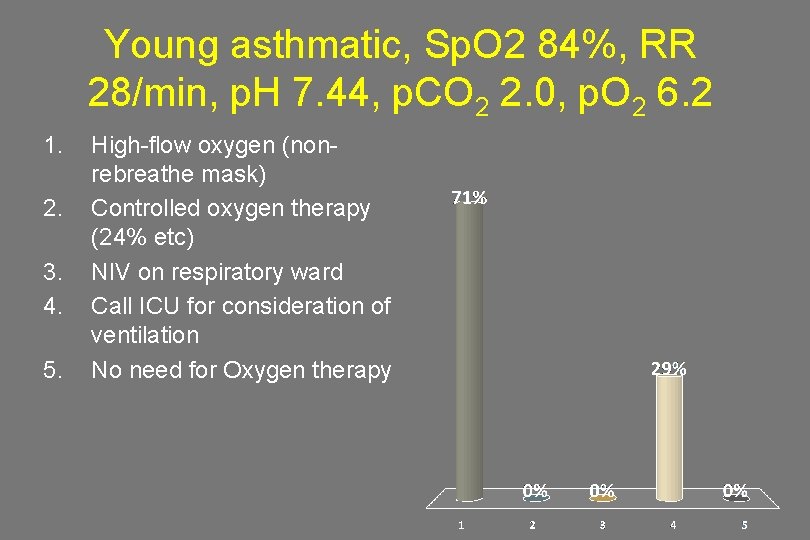
Young asthmatic, Sp. O 2 84%, RR 28/min, p. H 7. 44, p. CO 2 2. 0, p. O 2 6. 2 1. 2. 3. 4. 5. High-flow oxygen (nonrebreathe mask) Controlled oxygen therapy (24% etc) NIV on respiratory ward Call ICU for consideration of ventilation No need for Oxygen therapy

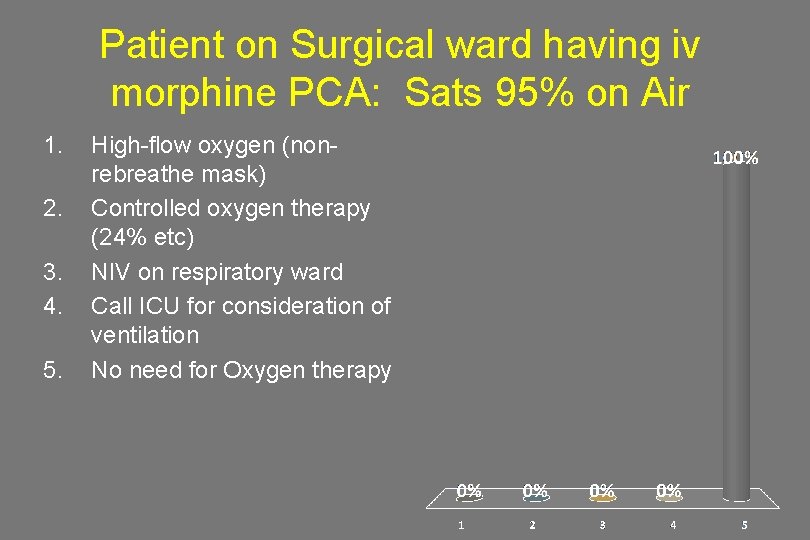
Patient on Surgical ward having iv morphine PCA: Sats 95% on Air 1. 2. 3. 4. 5. High-flow oxygen (nonrebreathe mask) Controlled oxygen therapy (24% etc) NIV on respiratory ward Call ICU for consideration of ventilation No need for Oxygen therapy
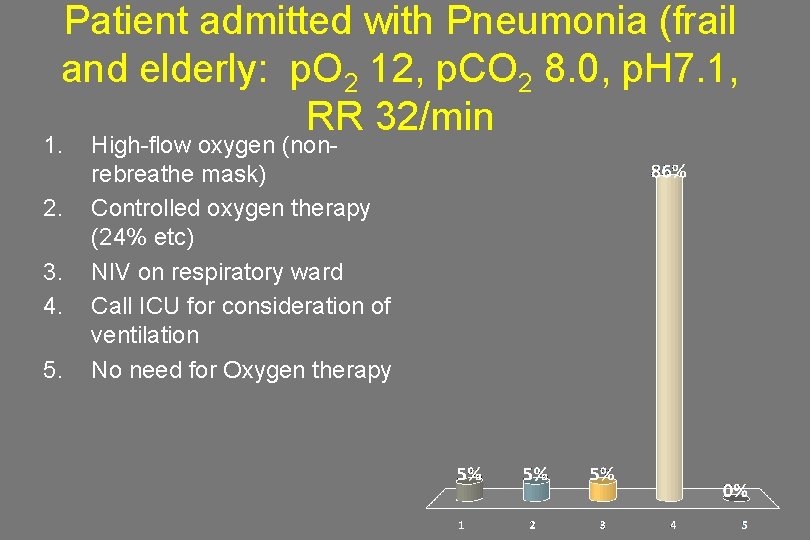
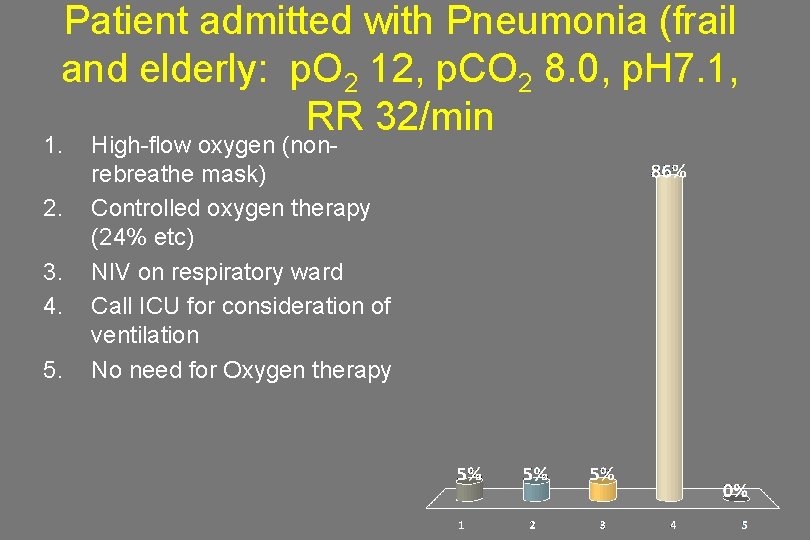
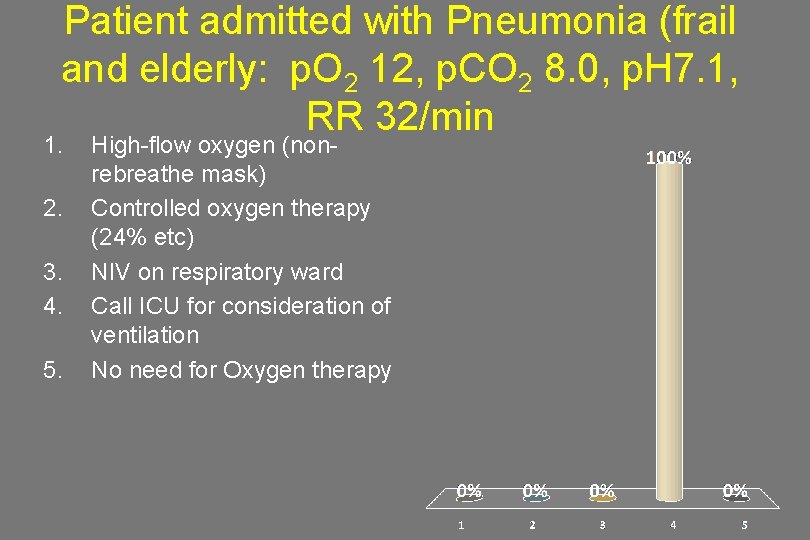
Patient admitted with Pneumonia (frail and elderly: p. O 2 12, p. CO 2 8. 0, p. H 7. 1, RR 32/min 1. 2. 3. 4. 5. High-flow oxygen (nonrebreathe mask) Controlled oxygen therapy (24% etc) NIV on respiratory ward Call ICU for consideration of ventilation No need for Oxygen therapy
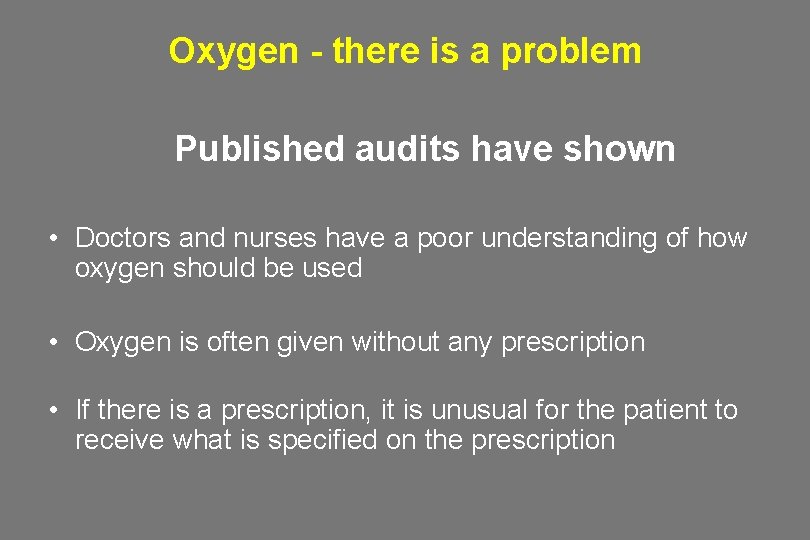
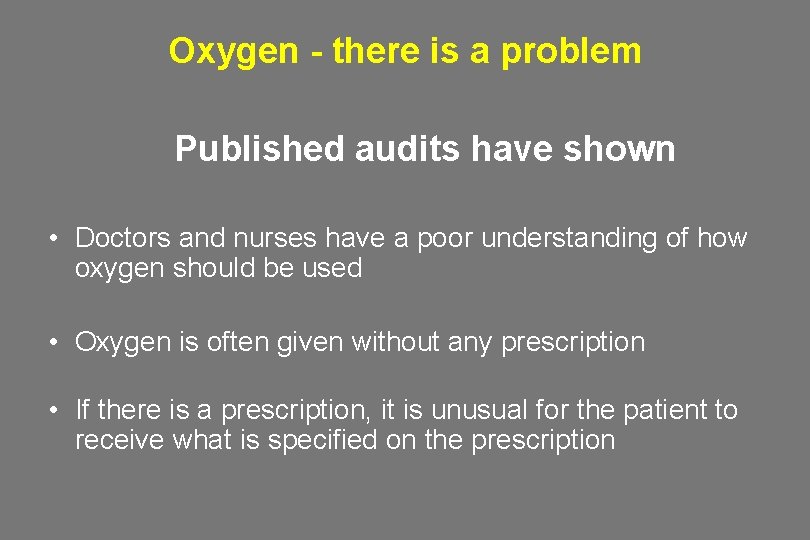
Oxygen - there is a problem Published audits have shown • Doctors and nurses have a poor understanding of how oxygen should be used • Oxygen is often given without any prescription • If there is a prescription, it is unusual for the patient to receive what is specified on the prescription

Oxygen - there was a disagreement • Chest Physicians • Intensivists • Emergency Medicine / A&E clinicians • Ambulance teams
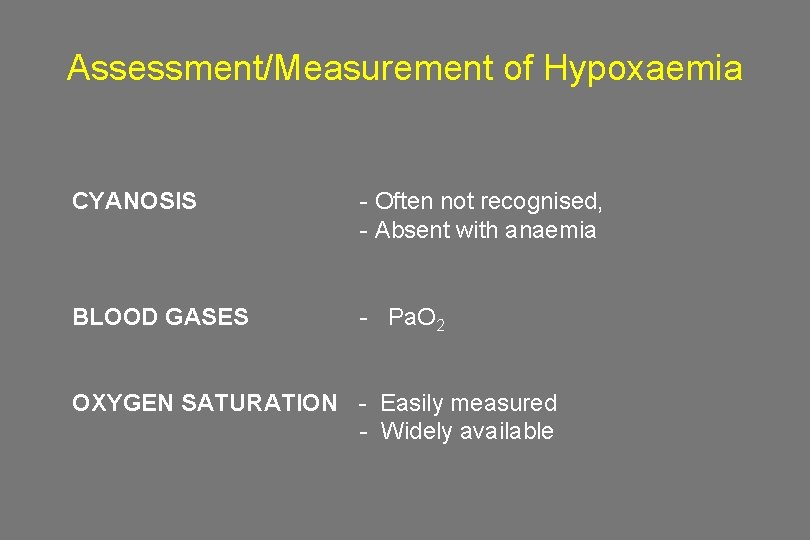
Assessment/Measurement of Hypoxaemia CYANOSIS BLOOD GASES - Often not recognised, - Absent with anaemia - Pa. O 2 OXYGEN SATURATION - Easily measured - Widely available
Prescribing by target oxygen saturation Basis of the BTS guideline Keep it normal/near-normal for all patients except pre-defined groups who are at risk from hypercapnic respiratory failure
What is normal and what is dangerous?
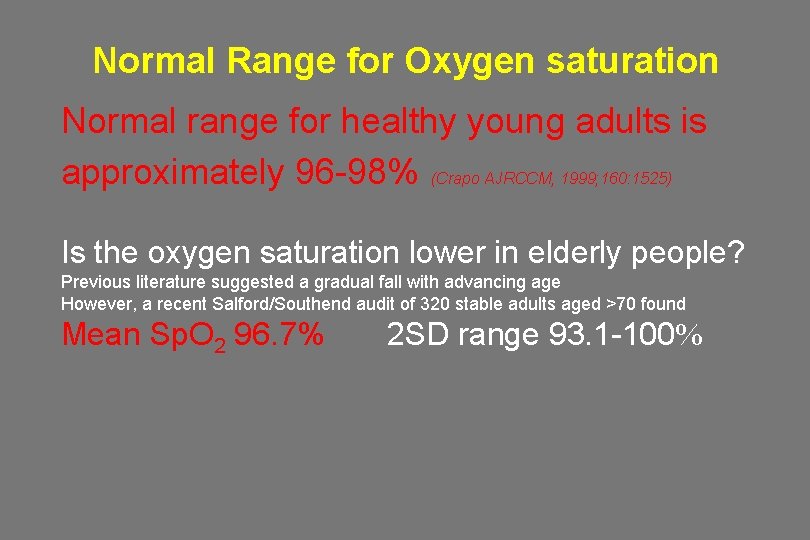
Normal Range for Oxygen saturation Normal range for healthy young adults is approximately 96 -98% (Crapo AJRCCM, 1999; 160: 1525) Is the oxygen saturation lower in elderly people? Previous literature suggested a gradual fall with advancing age However, a recent Salford/Southend audit of 320 stable adults aged >70 found Mean Sp. O 2 96. 7% 2 SD range 93. 1 -100%
What is a “normal” nocturnal oxygen saturation? • Healthy subjects in all age groups routinely desaturate to an average nadir of 90. 4% during the night (SD 3. 1%) Gries RE et al Chest 1996; 110: 1489 -92 *Therefore, be cautious in interpreting a single oximetry measurement from a sleeping patient. Watch the oximeter for a few minutes if in any doubt (if the patient is othewise stable) as normal overnight dips are of short duration.
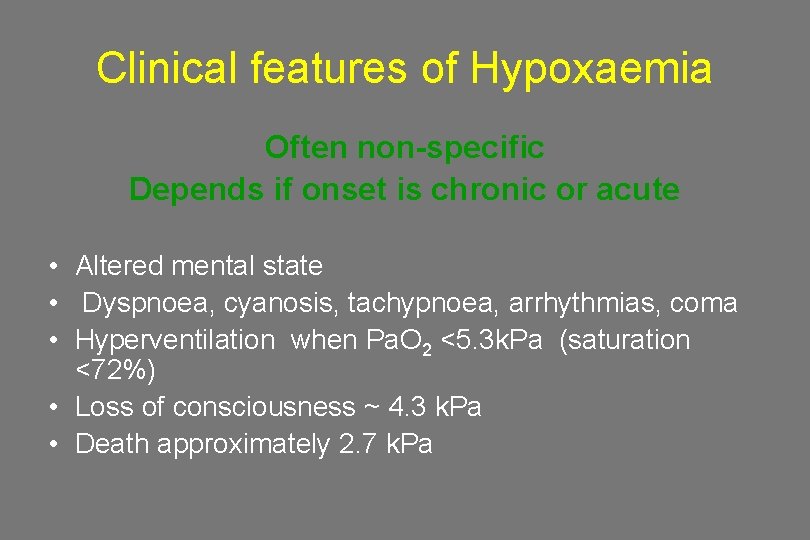
Clinical features of Hypoxaemia Often non-specific Depends if onset is chronic or acute • Altered mental state • Dyspnoea, cyanosis, tachypnoea, arrhythmias, coma • Hyperventilation when Pa. O 2 <5. 3 k. Pa (saturation <72%) • Loss of consciousness ~ 4. 3 k. Pa • Death approximately 2. 7 k. Pa
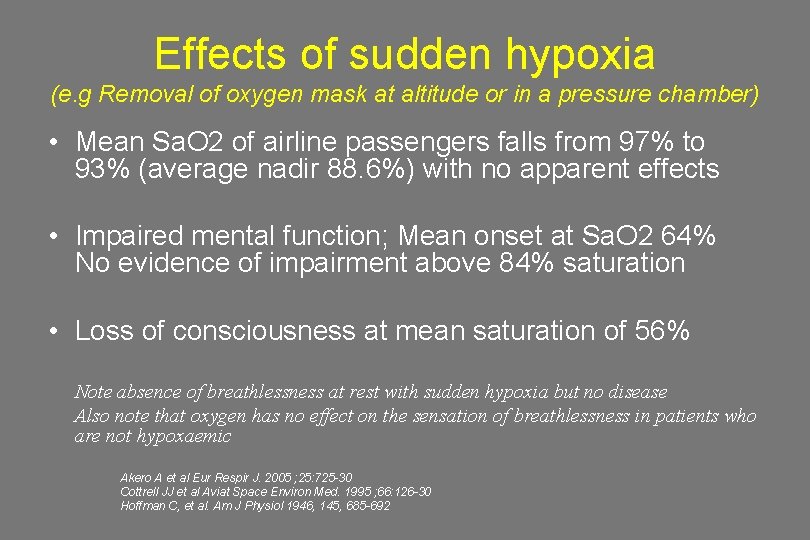
Effects of sudden hypoxia (e. g Removal of oxygen mask at altitude or in a pressure chamber) • Mean Sa. O 2 of airline passengers falls from 97% to 93% (average nadir 88. 6%) with no apparent effects • Impaired mental function; Mean onset at Sa. O 2 64% No evidence of impairment above 84% saturation • Loss of consciousness at mean saturation of 56% Note absence of breathlessness at rest with sudden hypoxia but no disease Also note that oxygen has no effect on the sensation of breathlessness in patients who are not hypoxaemic Akero A et al Eur Respir J. 2005 ; 25: 725 -30 Cottrell JJ et al Aviat Space Environ Med. 1995 ; 66: 126 -30 Hoffman C, et al. Am J Physiol 1946, 145, 685 -692
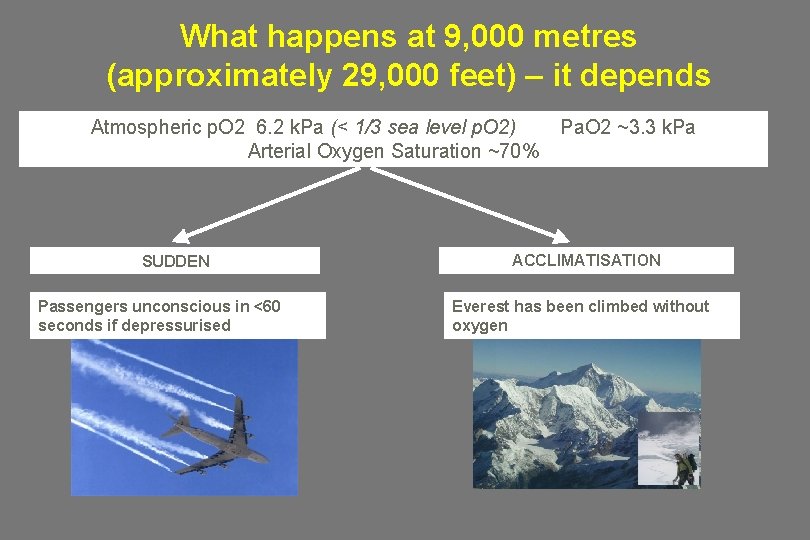
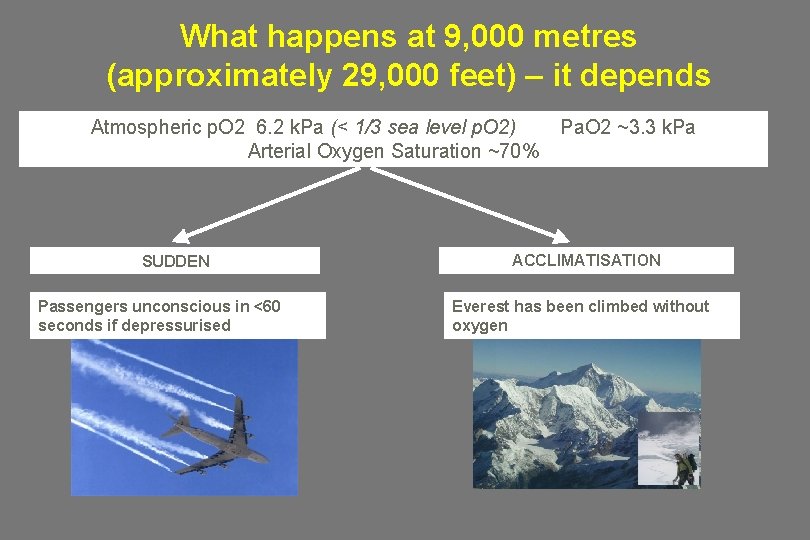
What happens at 9, 000 metres (approximately 29, 000 feet) – it depends Atmospheric p. O 2 6. 2 k. Pa (< 1/3 sea level p. O 2) Arterial Oxygen Saturation ~70% SUDDEN Passengers unconscious in <60 seconds if depressurised Pa. O 2 ~3. 3 k. Pa ACCLIMATISATION Everest has been climbed without oxygen

Why is oxygen used?
Aims of emergency oxygen therapy • To correct or prevent potentially harmful hypoxaemia • To alleviate breathlessness (only if hypoxaemic) • Oxygen has no effect on breathlessness if the oxygen saturation is normal

But some patients are at risk of CO 2 retention and acidosis if given high dose oxygen • Chronic hypoxic lung disease – COPD – Severe Chronic Asthma – Bronchiectasis / CF • Chest wall disease – Kyphoscoliosis – Thoracoplasty • Neuromuscular disease • Obesity hypoventilation
Oxygen therapy is only one element of resuscitation of a critically ill patient The oxygen carrying power of blood may be increased by • Enhancing circulating volume • Correcting severe anaemia • Enhancing cardiac output • Safeguarding the airway • Avoiding/Reversing Respiratory Depressants • Increasing Fraction of Inspired Oxygen (FIO 2) • Establish the reason for Hypoxia and treat the underlying cause (e. g Bronchospasm, LVF etc) • Patient may need, CPAP or NIV or Invasive ventilation
Exposure to high concentrations of oxygen may be harmful • • • Absorption Atelectasis even at FIO 2 30 -50% Intrapulmonary shunting Post-operative hypoxaemia Risk to COPD patients Coronary vasoconstriction Increased Systemic Vascular Resistance Reduced Cardiac Index Possible reperfusion injury post MI Worsens systolic myocardial performance Oxygen therapy INCREASED mortality in non-hypoxic patients with mildmoderate stroke RECOMMENDATION – This guideline recommends an upper limit of 98% for most patients. This is a combination of what is normal and safe Harten JM et al J Cardiothoracic Vasc Anaesth 2005; 19: 173 -5 Kaneda T et al. Jpn Circ J 2001; 213 -8 Frobert O et al. Cardiovasc Ultrasound 2004; 2: 22 Haque WA et al. J Am Coll Cardiol 1996; 2: 353 -7 Thomaon aj ET AL. BMJ 2002; 1406 -7 Ronning OM et al. Stroke 1999; 30
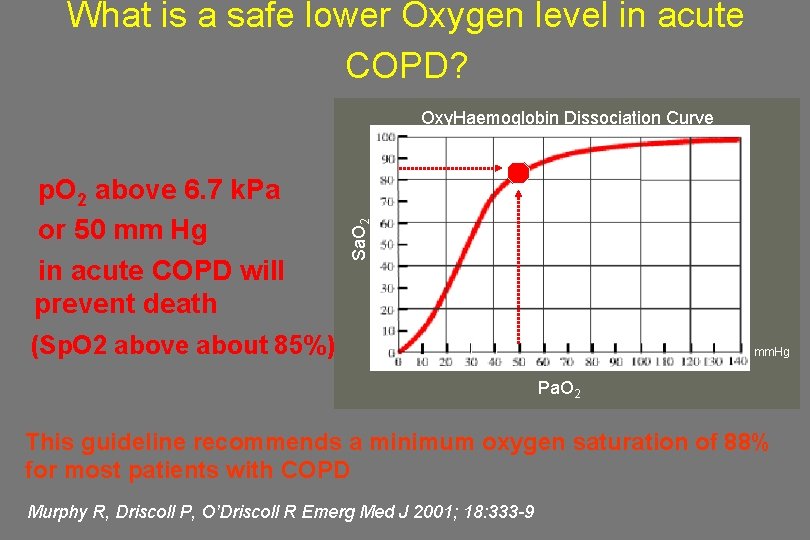
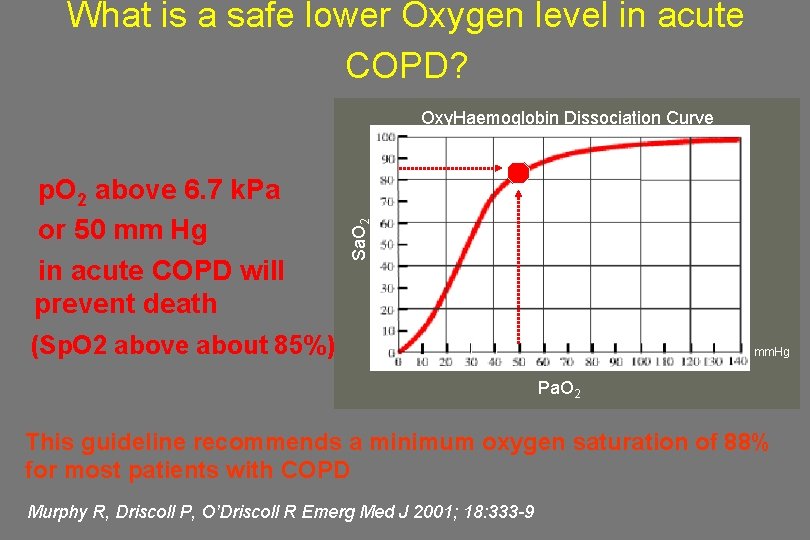
What is a safe lower Oxygen level in acute COPD? p. O 2 above 6. 7 k. Pa or 50 mm Hg in acute COPD will prevent death Sa. O 2 Oxy. Haemoglobin Dissociation Curve (Sp. O 2 above about 85%) mm. Hg Pa. O 2 This guideline recommends a minimum oxygen saturation of 88% for most patients with COPD Murphy R, Driscoll P, O’Driscoll R Emerg Med J 2001; 18: 333 -9
What is a safe higher oxygen level in acute COPD • 47% of 982 patients with exacerbation of COPD were hypercapnic on arrival in hospital • 20% had Respiratory Acidosis (p. H < 7. 35) • 5% had p. H < 7. 25 (and were likely to need ICU care) • Most hypercapnic patients with p. O 2 > 10 k. Pa were acidotic (equivalent to oxygen saturation of above ~ 92%) i. e. had been given too much oxygen RECOMMENDATION: Keep Pa. O 2 below 10 k. Pa and Sp. O 2 < 92% in acute COPD Plant et al Thorax 2000; 55: 550
Fallacies regarding Oxygen Therapy “Routine administration of supplemental oxygen is useful, harmless and clinically indicated” • Renders pulse oximetry worthless as a measure of ventilation • May prevent early diagnosis and specific treatment of hypoventilation This guideline only recommends supplemental oxygen when the patients oximetry is below the target range John B Downs MD Respiratory care 2003; 48: 611 -20
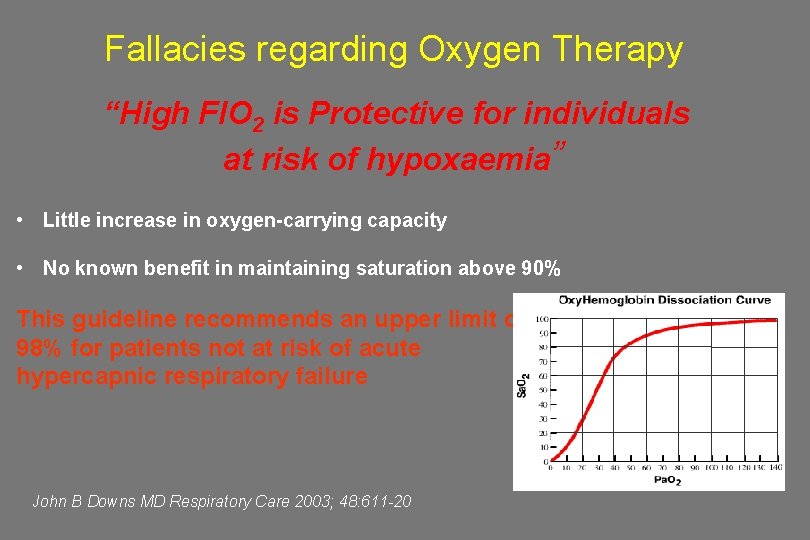
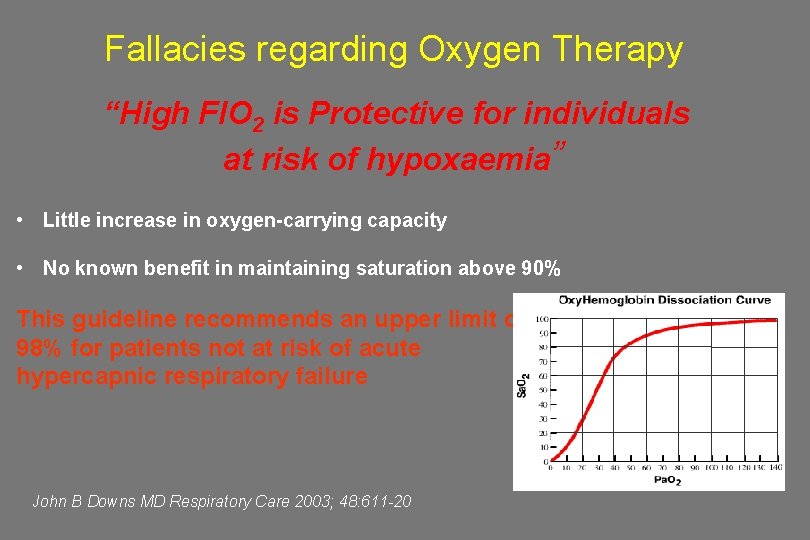
Fallacies regarding Oxygen Therapy “High FIO 2 is Protective for individuals at risk of hypoxaemia” • Little increase in oxygen-carrying capacity • No known benefit in maintaining saturation above 90% This guideline recommends an upper limit of 98% for patients not at risk of acute hypercapnic respiratory failure John B Downs MD Respiratory Care 2003; 48: 611 -20
Use of target ranges
Target Saturation Scheme • O 2 prescribed by target saturation (like an Insulin “BM sliding-scale chart”) • Oxygen delivery device and flow administered and changed if necessary to keep the Sp. O 2 in the target range • Target oxygen saturation prescription integrated into patient drug chart and monitoring
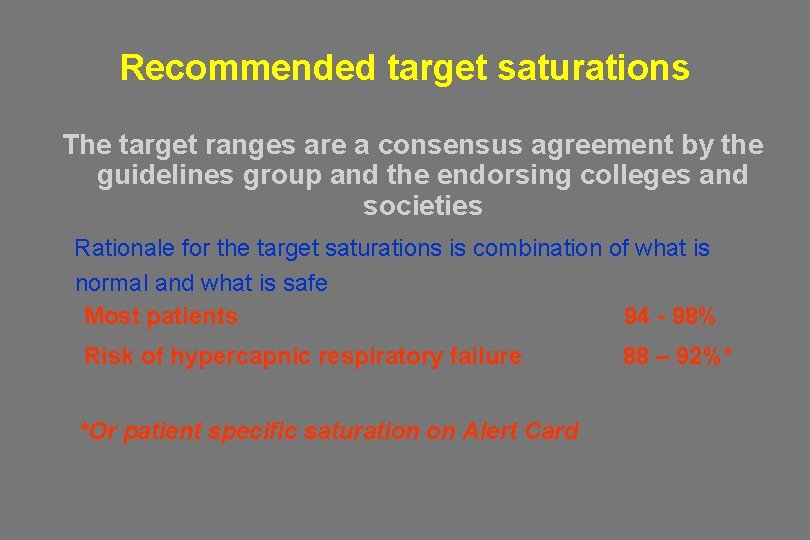
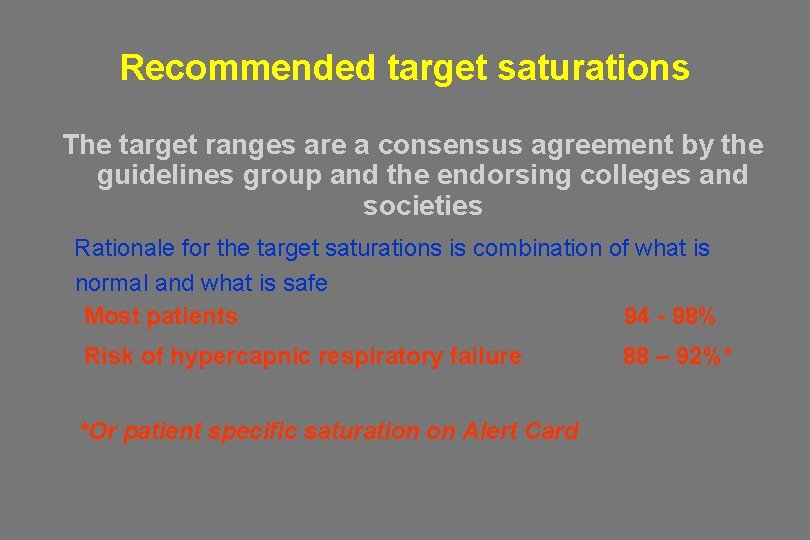
Recommended target saturations The target ranges are a consensus agreement by the guidelines group and the endorsing colleges and societies Rationale for the target saturations is combination of what is normal and what is safe Most patients Risk of hypercapnic respiratory failure *Or patient specific saturation on Alert Card 94 - 98% 88 – 92%*
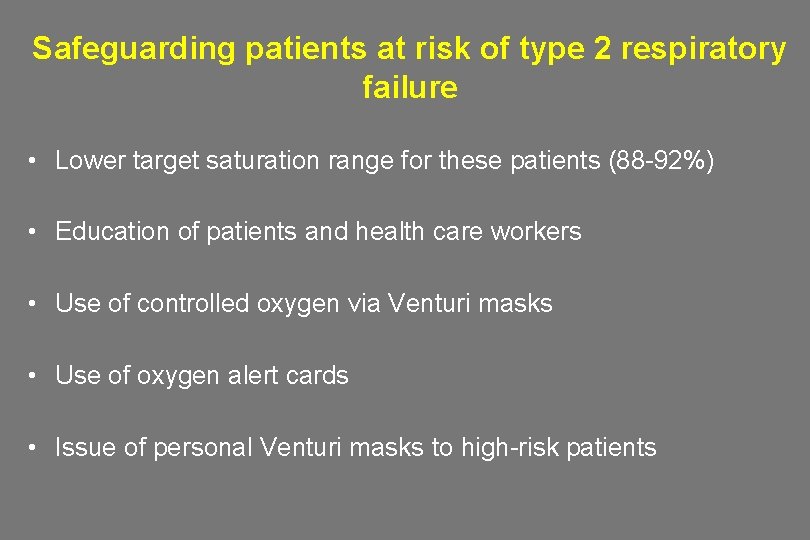
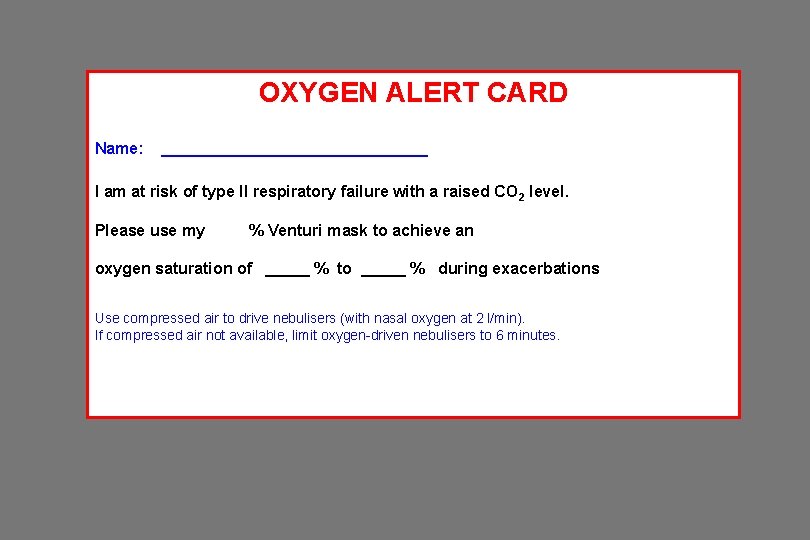
Safeguarding patients at risk of type 2 respiratory failure • Lower target saturation range for these patients (88 -92%) • Education of patients and health care workers • Use of controlled oxygen via Venturi masks • Use of oxygen alert cards • Issue of personal Venturi masks to high-risk patients
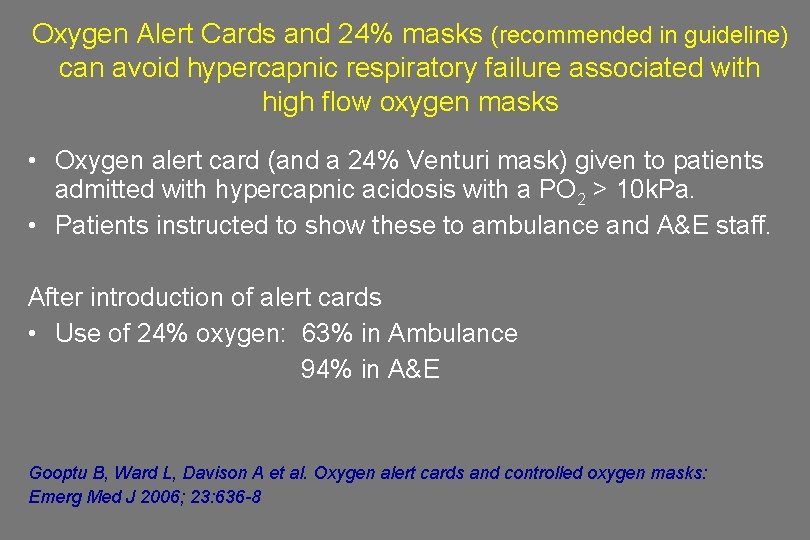
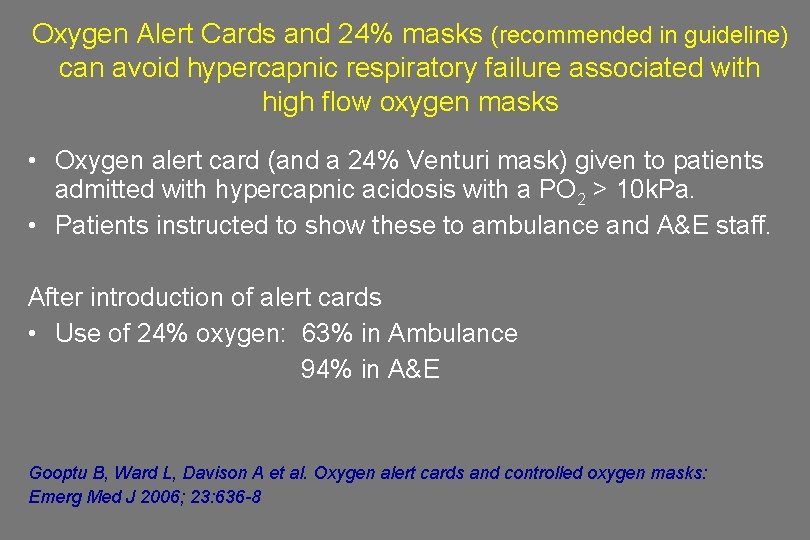
Oxygen Alert Cards and 24% masks (recommended in guideline) can avoid hypercapnic respiratory failure associated with high flow oxygen masks • Oxygen alert card (and a 24% Venturi mask) given to patients admitted with hypercapnic acidosis with a PO 2 > 10 k. Pa. • Patients instructed to show these to ambulance and A&E staff. After introduction of alert cards • Use of 24% oxygen: 63% in Ambulance 94% in A&E Gooptu B, Ward L, Davison A et al. Oxygen alert cards and controlled oxygen masks: Emerg Med J 2006; 23: 636 -8
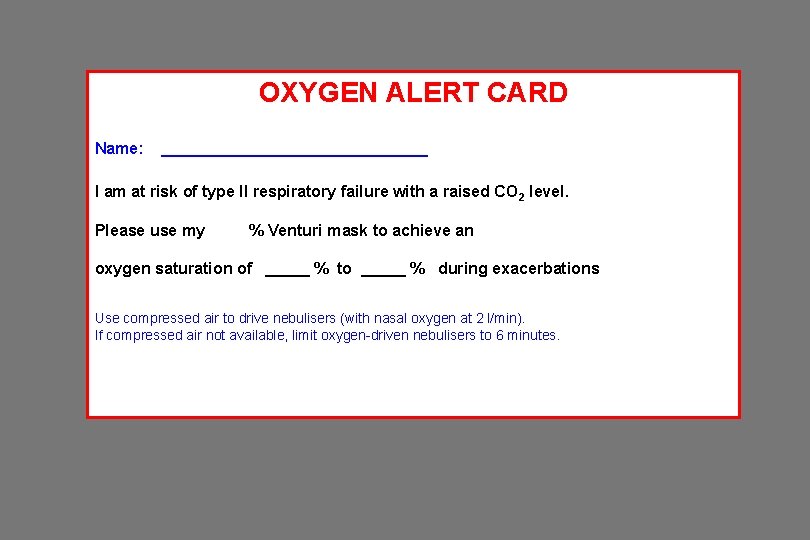
OXYGEN ALERT CARD Name: _______________ I am at risk of type II respiratory failure with a raised CO 2 level. Please use my % Venturi mask to achieve an oxygen saturation of _____ % to _____ % during exacerbations Use compressed air to drive nebulisers (with nasal oxygen at 2 l/min). If compressed air not available, limit oxygen-driven nebulisers to 6 minutes.

Devices
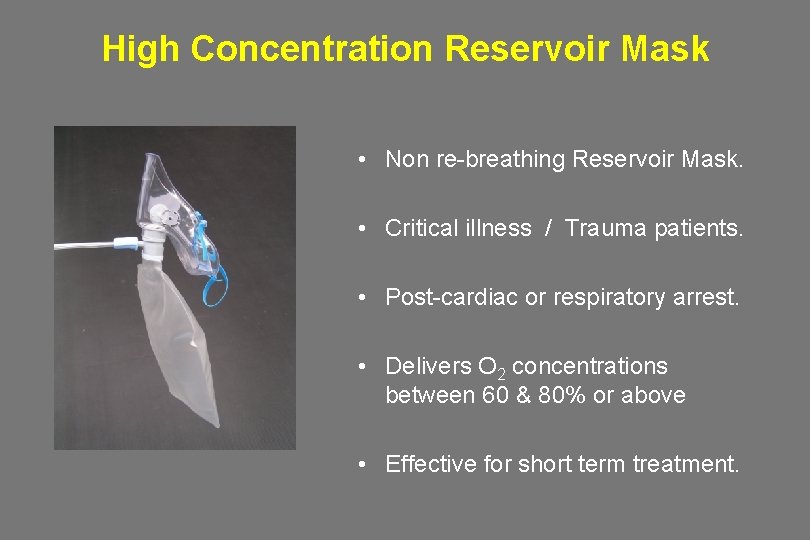
High Concentration Reservoir Mask • Non re-breathing Reservoir Mask. • Critical illness / Trauma patients. • Post-cardiac or respiratory arrest. • Delivers O 2 concentrations between 60 & 80% or above • Effective for short term treatment.
Nasal Cannulae • Recommended in the Guideline as suitable for most patients with both type I and II respiratory failure. • 2 -6 L/min gives approx 24 -50% FIO 2 • FIO 2 depends on oxygen flow rate and patient’s minute volume and inspiratory flow and pattern of breathing. • Comfortable and easily tolerated • No re-breathing • Low cost product • Preferred by patients (Vs simple mask)
Simple face mask (Medium concentration, variable performance) • Used for patients with type I respiratory failure. • Delivers variable O 2 concentration between 35% & 60%. • Low cost product. • Flow 5 -10 L/min Flow must be at least 5 L/min to avoid CO 2 build up and resistance to breathing (although packaging says 2 -10 L)
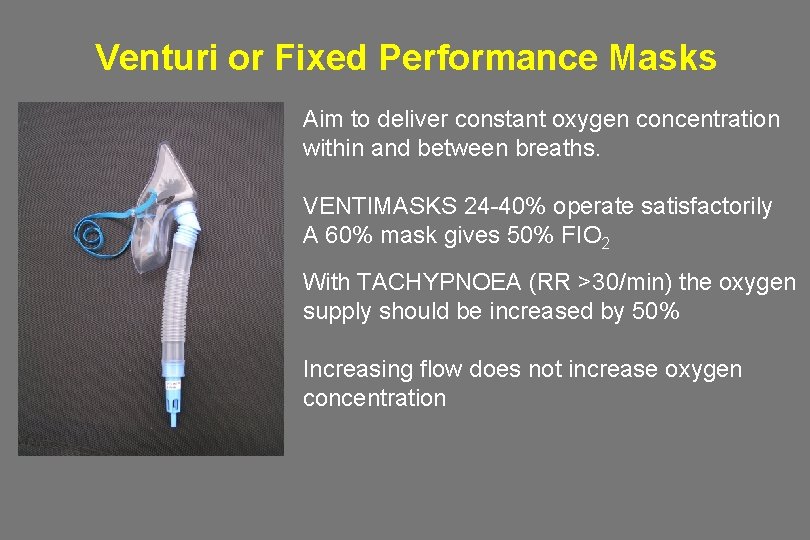
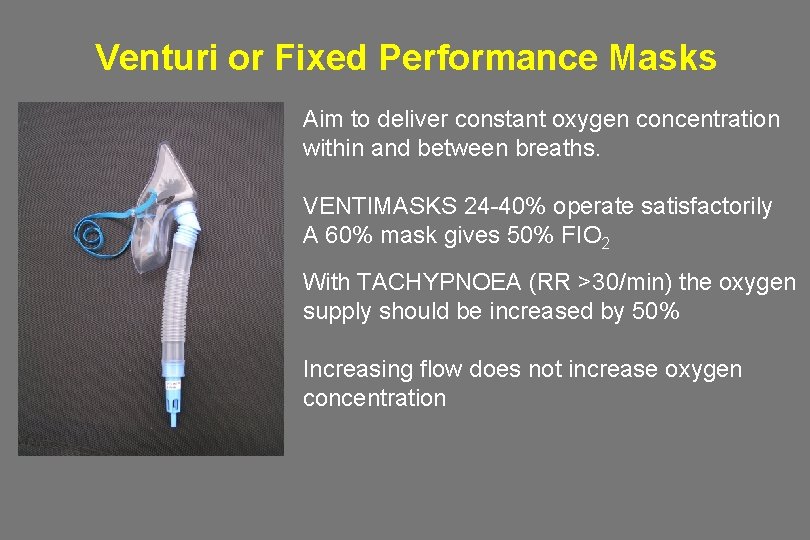
Venturi or Fixed Performance Masks Aim to deliver constant oxygen concentration within and between breaths. VENTIMASKS 24 -40% operate satisfactorily A 60% mask gives 50% FIO 2 With TACHYPNOEA (RR >30/min) the oxygen supply should be increased by 50% Increasing flow does not increase oxygen concentration

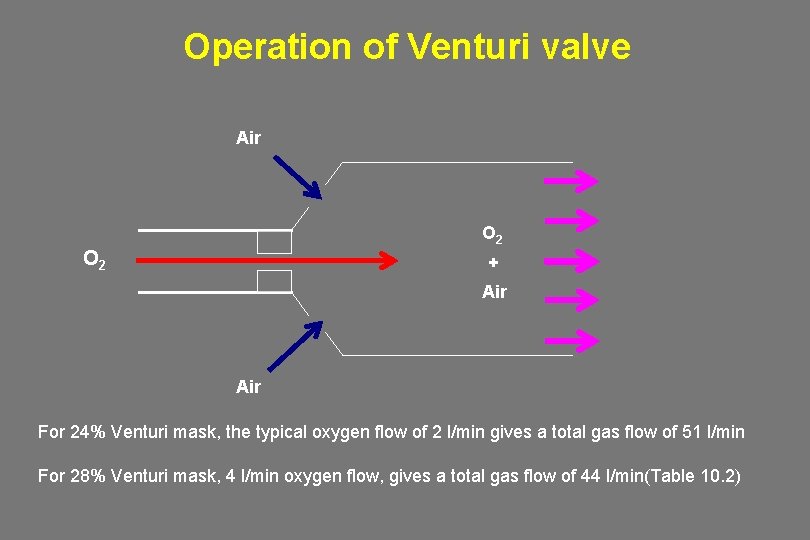
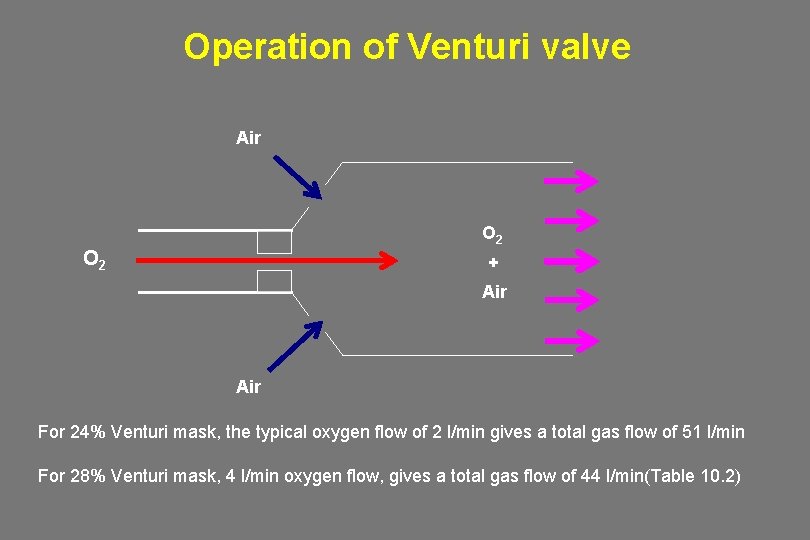
Operation of Venturi valve Air O 2 + Air For 24% Venturi mask, the typical oxygen flow of 2 l/min gives a total gas flow of 51 l/min For 28% Venturi mask, 4 l/min oxygen flow, gives a total gas flow of 44 l/min(Table 10. 2)
What device and flow rate should you use in each situation?
Many patients need high-dose oxygen to normalize saturation • • Severe Pneumonia Severe LVF Major Trauma Sepsis and Shock Major atelectasis Pulmonary Embolism Lung Fibrosis Etc etc

Oxygen prescription for acutely hypoxaemic patients in hospital Yes Is the patient critically ill or in a peri-arrest condition? Commence treatment with reservoir mask or bag-valve mask No Is this patient at risk of hypercapnic respiratory failure (Type 2 Respiratory Failure)? YES Target saturation is 88 -92 % (or level on alert card) whilst awaiting blood gas results. NO Aim for Sp. O 2 94 -98%
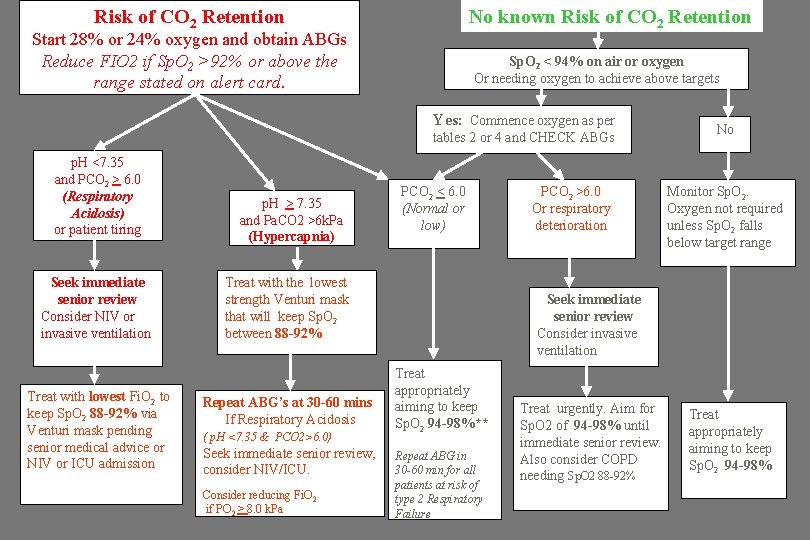
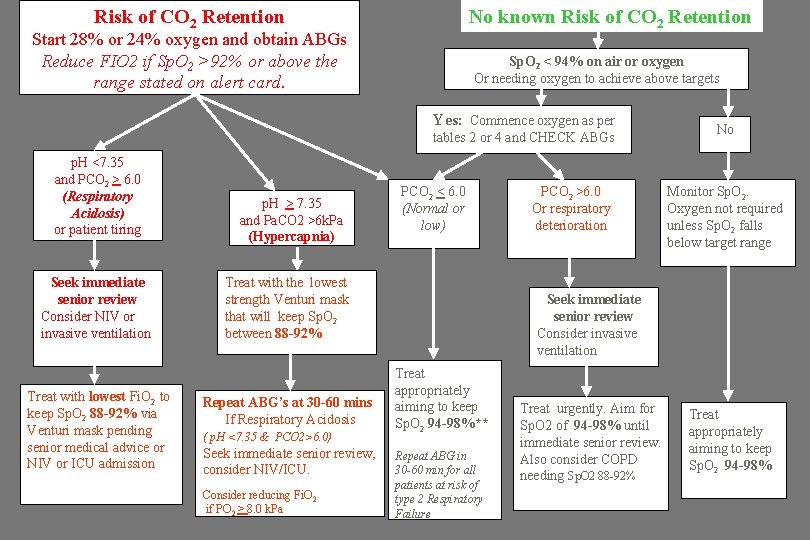
Risk of CO 2 Retention No known Risk of CO 2 Retention Start 28% or 24% oxygen and obtain ABGs Reduce FIO 2 if Sp. O 2 >92% or above the range stated on alert card. Sp. O 2 < 94% on air or oxygen Or needing oxygen to achieve above targets Yes: Commence oxygen as per tables 2 or 4 and CHECK ABGs p. H <7. 35 and PCO 2 > 6. 0 (Respiratory Acidosis) or patient tiring Seek immediate senior review Consider NIV or invasive ventilation Treat with lowest Fi. O 2 to keep Sp. O 2 88 -92% via Venturi mask pending senior medical advice or NIV or ICU admission p. H > 7. 35 and Pa. CO 2 >6 k. Pa (Hypercapnia) PCO 2 < 6. 0 (Normal or low) (see box in chart 2) Treat with the lowest strength Venturi mask that will keep Sp. O 2 between 88 -92% Repeat ABG’s at 30 -60 mins If Respiratory Acidosis ( p. H <7. 35 & PCO 2>6. 0) Seek immediate senior review, consider NIV/ICU. Consider reducing Fi. O 2 if PO 2 > 8. 0 k. Pa PCO 2 >6. 0 Or respiratory deterioration No Monitor Sp. O 2. Oxygen not required unless Sp. O 2 falls below target range Seek immediate senior review Consider invasive ventilation Treat appropriately aiming to keep Sp. O 2 94 -98%** Repeat ABG in 30 -60 min for all patients at risk of type 2 Respiratory Failure Treat urgently. Aim for Sp. O 2 of 94 -98% until immediate senior review. Also consider COPD needing Sp. O 2 88 -92% Treat appropriately aiming to keep Sp. O 2 94 -98%

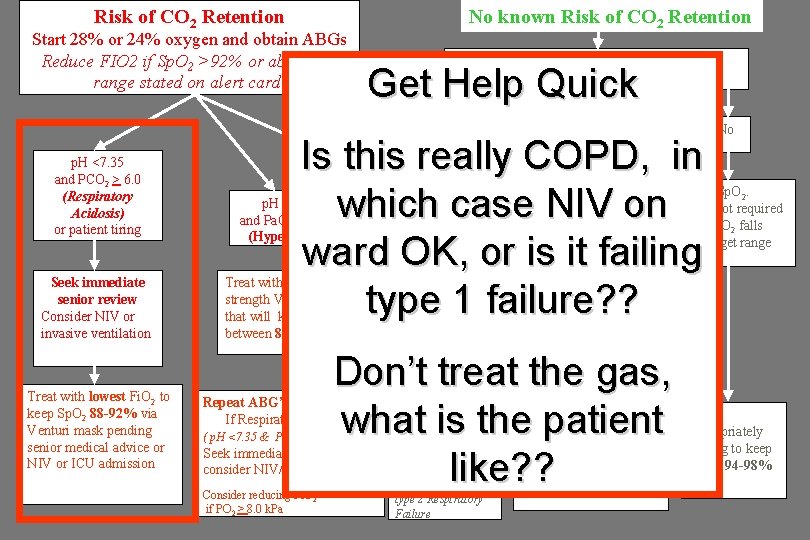
Risk of CO 2 Retention No known Risk of CO 2 Retention Start 28% or 24% oxygen and obtain ABGs Reduce FIO 2 if Sp. O 2 >92% or above the range stated on alert card. Get Help Quick p. H <7. 35 and PCO 2 > 6. 0 (Respiratory Acidosis) or patient tiring About to arrest p. H > 7. 35 and Pa. CO 2 >6 k. Pa (Hypercapnia) Sp. O 2 < 94% on air or oxygen Or needing oxygen to achieve above targets Yes: Commence oxygen as per tables 2 or 4 and CHECK ABGs PCO 2 < 6. 0 (Normal or low) (see box in chart 2) Don’t treat the gas, what is the patient like? ? Seek immediate senior review Consider NIV or invasive ventilation Treat with lowest Fi. O 2 to keep Sp. O 2 88 -92% via Venturi mask pending senior medical advice or NIV or ICU admission Treat with the lowest strength Venturi mask that will keep Sp. O 2 between 88 -92% Repeat ABG’s at 30 -60 mins If Respiratory Acidosis ( p. H <7. 35 & PCO 2>6. 0) Seek immediate senior review, consider NIV/ICU. Consider reducing Fi. O 2 if PO 2 > 8. 0 k. Pa PCO 2 >6. 0 Or respiratory deterioration Treat appropriately aiming to keep Sp. O 2 94 -98%** Repeat ABG in 30 -60 min for all patients at risk of type 2 Respiratory Failure No Monitor Sp. O 2. Oxygen not required unless Sp. O 2 falls below target range Seek immediate senior review Consider invasive ventilation Treat urgently. Aim for Sp. O 2 of 94 -98% until immediate senior review. Also consider COPD needing Sp. O 2 88 -92% Treat appropriately aiming to keep Sp. O 2 94 -98%
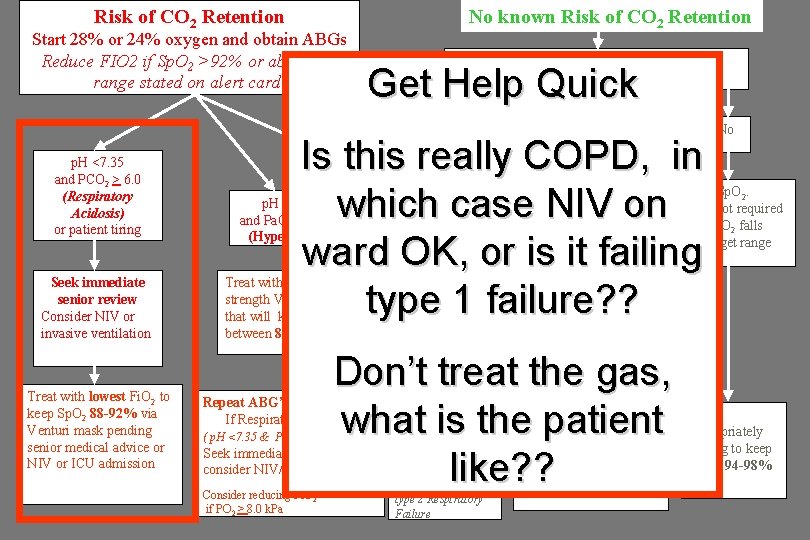
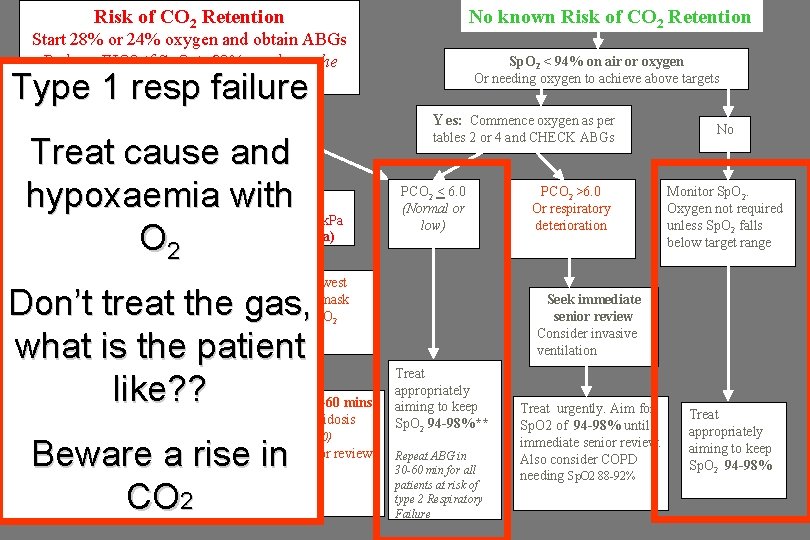
Risk of CO 2 Retention Start 28% or 24% oxygen and obtain ABGs Reduce FIO 2 if Sp. O 2 >92% or above the range stated on alert card. No known Risk of CO 2 Retention Sp. O 2 < 94% on air or oxygen Or needing oxygen to achieve above targets Get Help Quick Yes: Commence oxygen as per tables 2 or 4 and CHECK ABGs p. H <7. 35 and PCO 2 > 6. 0 (Respiratory Acidosis) or patient tiring Seek immediate senior review Consider NIV or invasive ventilation Treat with lowest Fi. O 2 to keep Sp. O 2 88 -92% via Venturi mask pending senior medical advice or NIV or ICU admission Is this really COPD, in which case NIV on ward OK, or is it failing type 1 failure? ? p. H > 7. 35 and Pa. CO 2 >6 k. Pa (Hypercapnia) PCO 2 < 6. 0 (Normal or low) (see box in chart 2) Treat with the lowest strength Venturi mask that will keep Sp. O 2 between 88 -92% Monitor Sp. O 2. Oxygen not required unless Sp. O 2 falls below target range Seek immediate senior review Consider invasive ventilation Don’t treat the gas, what is the patient like? ? Repeat ABG’s at 30 -60 mins If Respiratory Acidosis ( p. H <7. 35 & PCO 2>6. 0) Seek immediate senior review, consider NIV/ICU. Consider reducing Fi. O 2 if PO 2 > 8. 0 k. Pa PCO 2 >6. 0 Or respiratory deterioration No Treat appropriately aiming to keep Sp. O 2 94 -98%** Repeat ABG in 30 -60 min for all patients at risk of type 2 Respiratory Failure Treat urgently. Aim for Sp. O 2 of 94 -98% until immediate senior review. Also consider COPD needing Sp. O 2 88 -92% Treat appropriately aiming to keep Sp. O 2 94 -98%
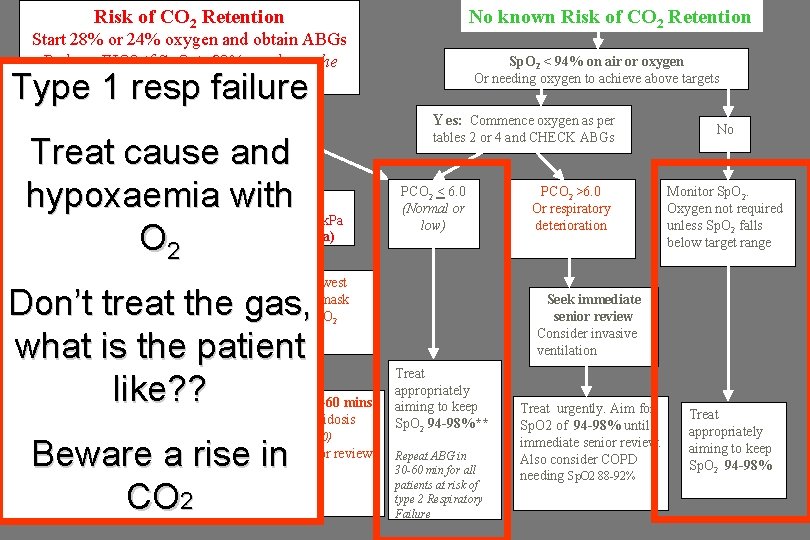
Risk of CO 2 Retention No known Risk of CO 2 Retention Start 28% or 24% oxygen and obtain ABGs Reduce FIO 2 if Sp. O 2 >92% or above the range stated on alert card. Sp. O 2 < 94% on air or oxygen Or needing oxygen to achieve above targets Type 1 resp failure Yes: Commence oxygen as per Treat cause and hypoxaemia with O 2 p. H <7. 35 and PCO 2 > 6. 0 (Respiratory Acidosis) or patient tiring Seek immediate senior review Consider NIV or invasive ventilation p. H > 7. 35 and Pa. CO 2 >6 k. Pa (Hypercapnia) PCO 2 < 6. 0 (Normal or low) Repeat ABG’s at 30 -60 mins If Respiratory Acidosis ( p. H <7. 35 & PCO 2>6. 0) Seek immediate senior review, consider NIV/ICU. Beware a rise in CO 2 Consider reducing Fi. O 2 if PO 2 > 8. 0 k. Pa PCO 2 >6. 0 Or respiratory deterioration (see box in chart 2) Treat with the lowest strength Venturi mask that will keep Sp. O 2 between 88 -92% Don’t treat the gas, what is the patient like? ? Treat with lowest Fi. O 2 to keep Sp. O 2 88 -92% via Venturi mask pending senior medical advice or NIV or ICU admission tables 2 or 4 and CHECK ABGs No Monitor Sp. O 2. Oxygen not required unless Sp. O 2 falls below target range Seek immediate senior review Consider invasive ventilation Treat appropriately aiming to keep Sp. O 2 94 -98%** Repeat ABG in 30 -60 min for all patients at risk of type 2 Respiratory Failure Treat urgently. Aim for Sp. O 2 of 94 -98% until immediate senior review. Also consider COPD needing Sp. O 2 88 -92% Treat appropriately aiming to keep Sp. O 2 94 -98%
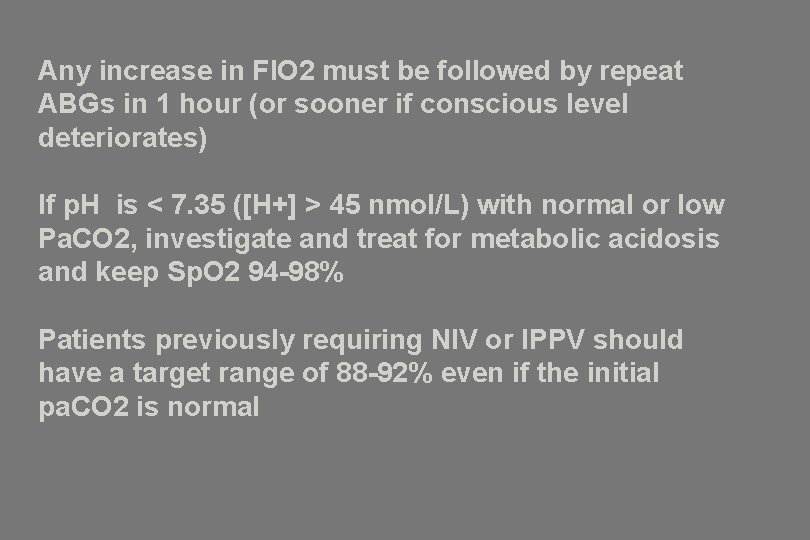
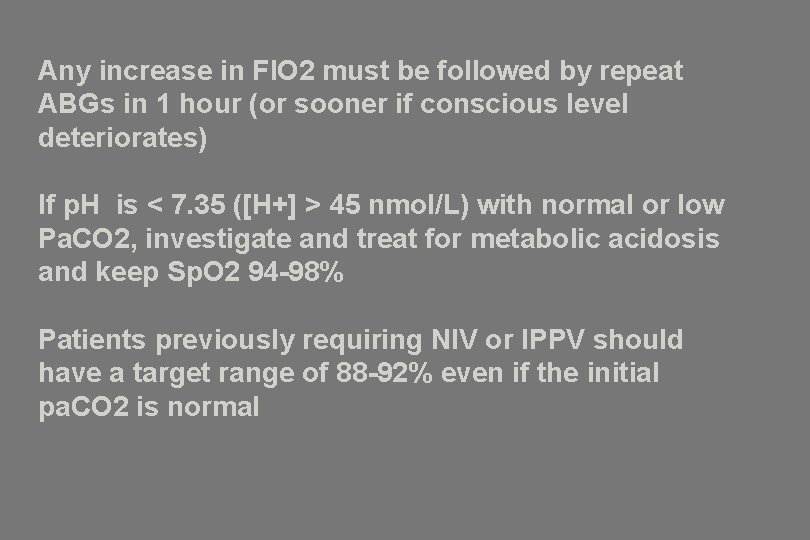
Any increase in FIO 2 must be followed by repeat ABGs in 1 hour (or sooner if conscious level deteriorates) If p. H is < 7. 35 ([H+] > 45 nmol/L) with normal or low Pa. CO 2, investigate and treat for metabolic acidosis and keep Sp. O 2 94 -98% Patients previously requiring NIV or IPPV should have a target range of 88 -92% even if the initial pa. CO 2 is normal
Quiz…. you might recognise some of the questions
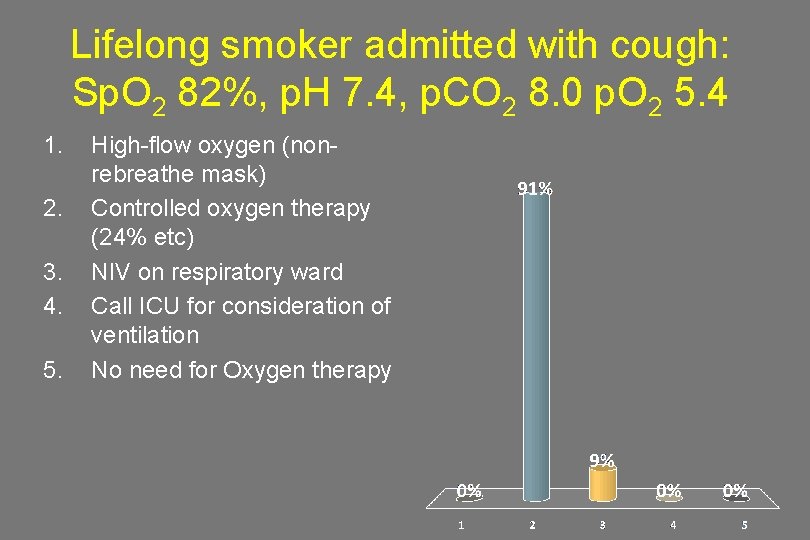
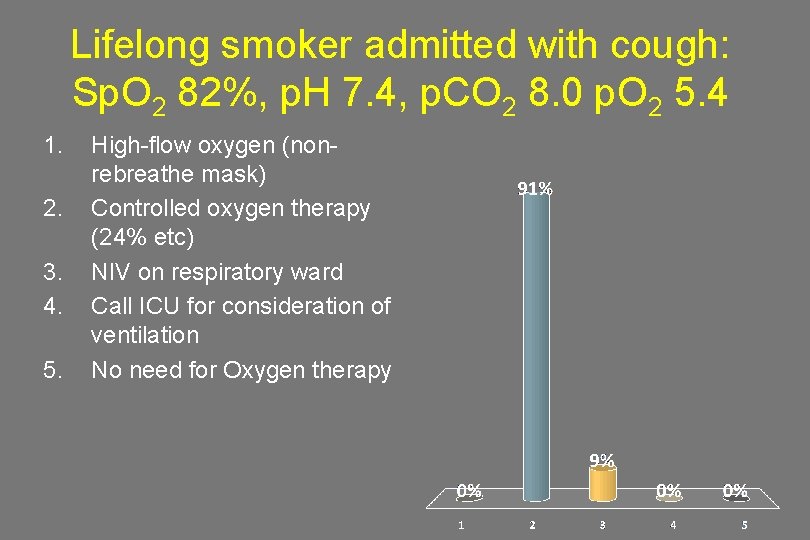
Lifelong smoker admitted with cough: Sp. O 2 82%, p. H 7. 4, p. CO 2 8. 0 p. O 2 5. 4 1. 2. 3. 4. 5. High-flow oxygen (nonrebreathe mask) Controlled oxygen therapy (24% etc) NIV on respiratory ward Call ICU for consideration of ventilation No need for Oxygen therapy
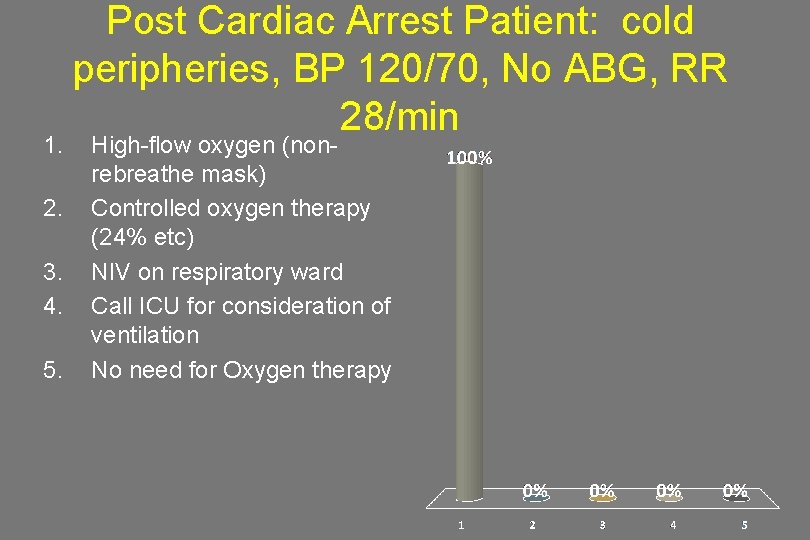
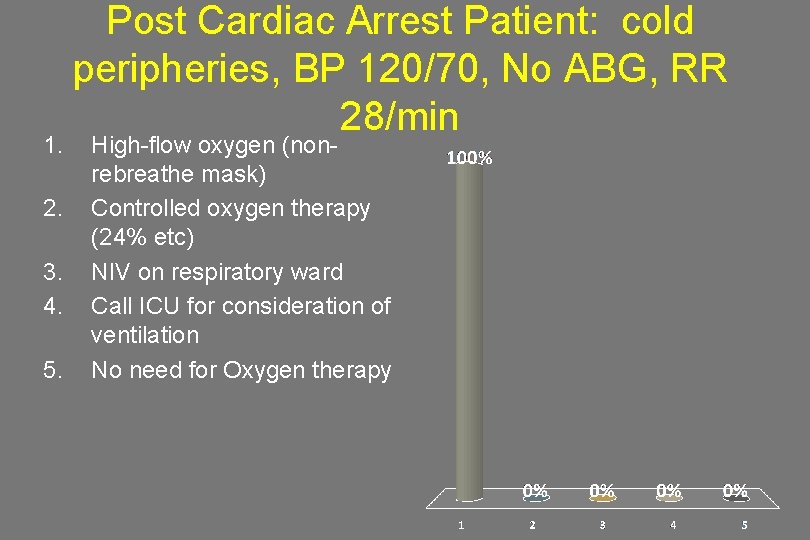
1. 2. 3. 4. 5. Post Cardiac Arrest Patient: cold peripheries, BP 120/70, No ABG, RR 28/min High-flow oxygen (nonrebreathe mask) Controlled oxygen therapy (24% etc) NIV on respiratory ward Call ICU for consideration of ventilation No need for Oxygen therapy
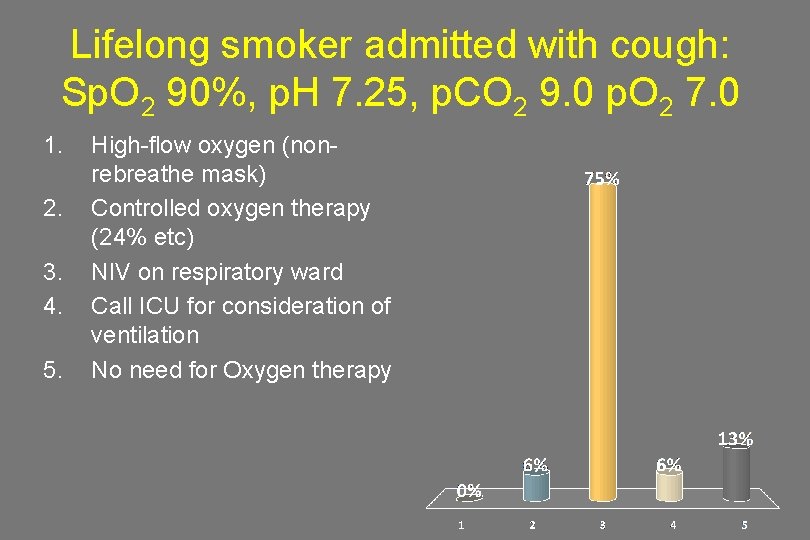
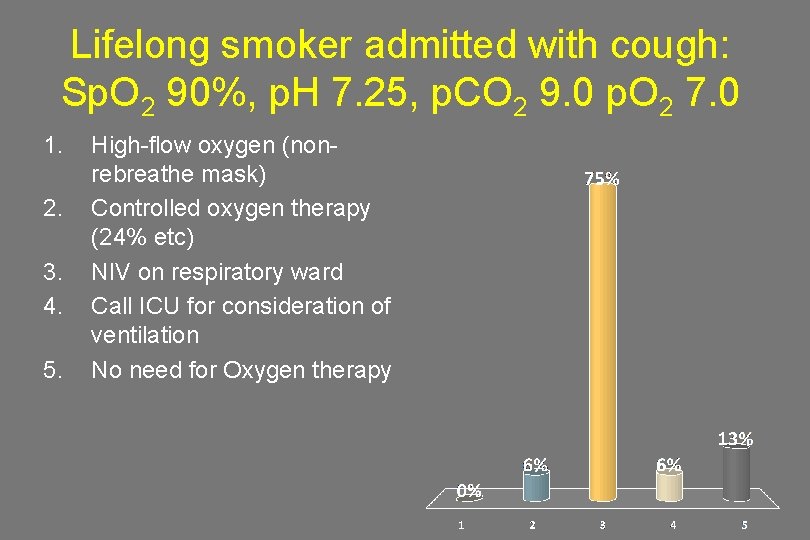
Lifelong smoker admitted with cough: Sp. O 2 90%, p. H 7. 25, p. CO 2 9. 0 p. O 2 7. 0 1. 2. 3. 4. 5. High-flow oxygen (nonrebreathe mask) Controlled oxygen therapy (24% etc) NIV on respiratory ward Call ICU for consideration of ventilation No need for Oxygen therapy
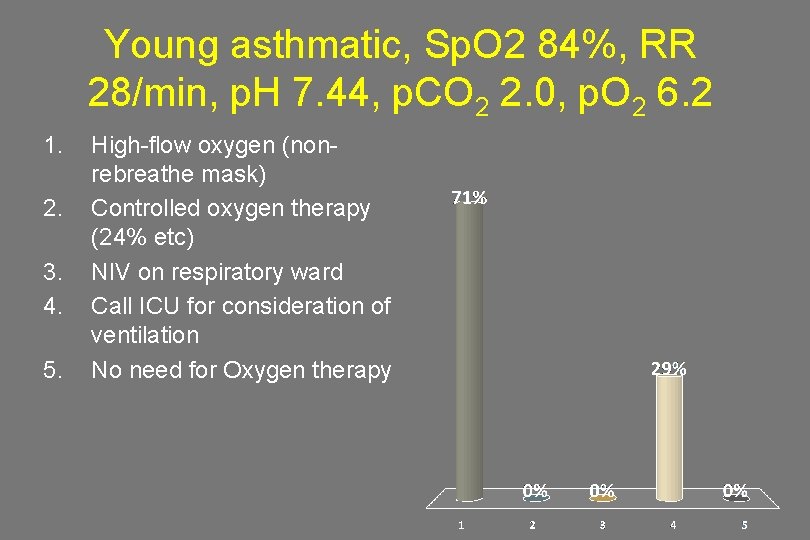
Young asthmatic, Sp. O 2 84%, RR 28/min, p. H 7. 44, p. CO 2 2. 0, p. O 2 6. 2 1. 2. 3. 4. 5. High-flow oxygen (nonrebreathe mask) Controlled oxygen therapy (24% etc) NIV on respiratory ward Call ICU for consideration of ventilation No need for Oxygen therapy
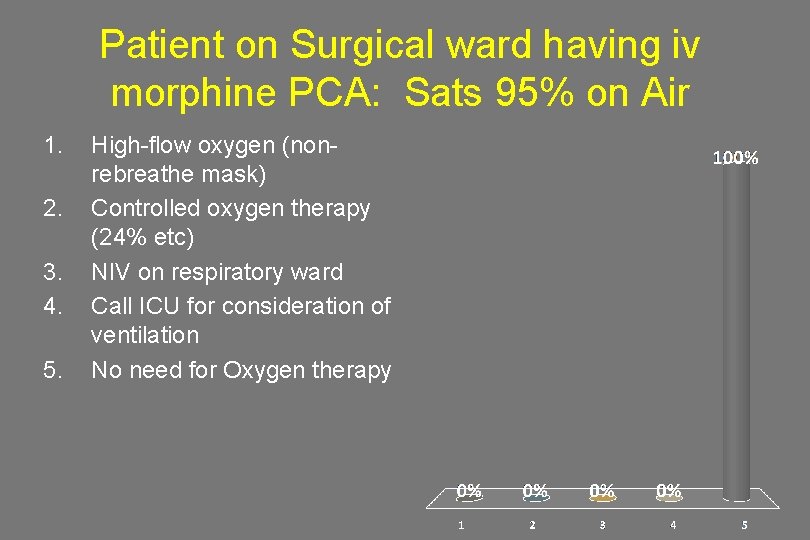
Patient on Surgical ward having iv morphine PCA: Sats 95% on Air 1. 2. 3. 4. 5. High-flow oxygen (nonrebreathe mask) Controlled oxygen therapy (24% etc) NIV on respiratory ward Call ICU for consideration of ventilation No need for Oxygen therapy
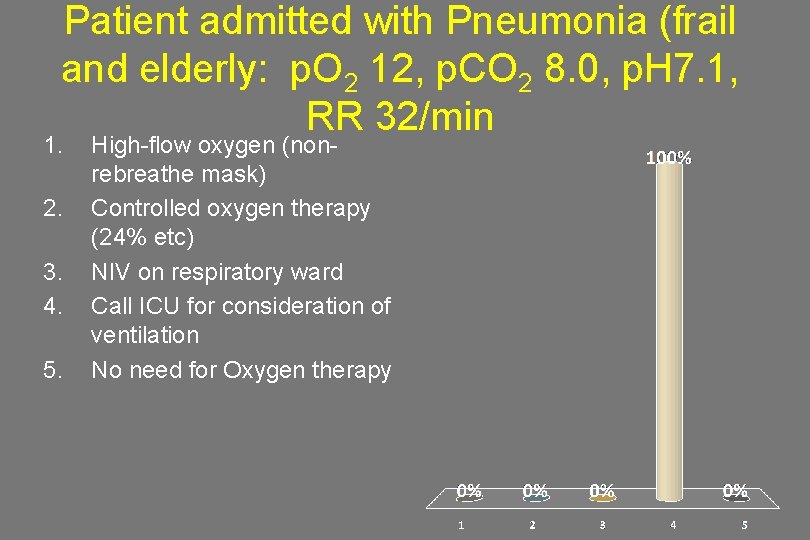
Patient admitted with Pneumonia (frail and elderly: p. O 2 12, p. CO 2 8. 0, p. H 7. 1, RR 32/min 1. 2. 3. 4. 5. High-flow oxygen (nonrebreathe mask) Controlled oxygen therapy (24% etc) NIV on respiratory ward Call ICU for consideration of ventilation No need for Oxygen therapy

Summary 1. Treat the patient not the gas 2. Prescribe oxygen to a target saturation for each group of patients • 94 - 98% for most adult patients • 88 - 92% if risk of hypercapnia (or patient-specific target on alert card) 3. Administer oxygen to achieve target saturation 4. Monitor oxygen saturation and keep in target range 5. Taper oxygen dose and stop when stable 6. Beware Hypercapnoea