Waldemar Machaa Principles of fluid therapy in a
![Crystalloids vs. colloids … volume effect Transfused volume [m. L] Type of infusion fluid Crystalloids vs. colloids … volume effect Transfused volume [m. L] Type of infusion fluid](https://slidetodoc.com/presentation_image_h2/8fb3ae4808abe9ce56aabae6d07ffda6/image-26.jpg)

- Slides: 37
Waldemar Machała Principles of fluid therapy in a massive trauma and hemorrhage. Ghazni, Afghanistan, September 2012 Department of Anesthesiology and Intensive Care The Military Teaching Hospital-CSW The gen. bryg. Stefan Hubicki Military Center of Medical Education
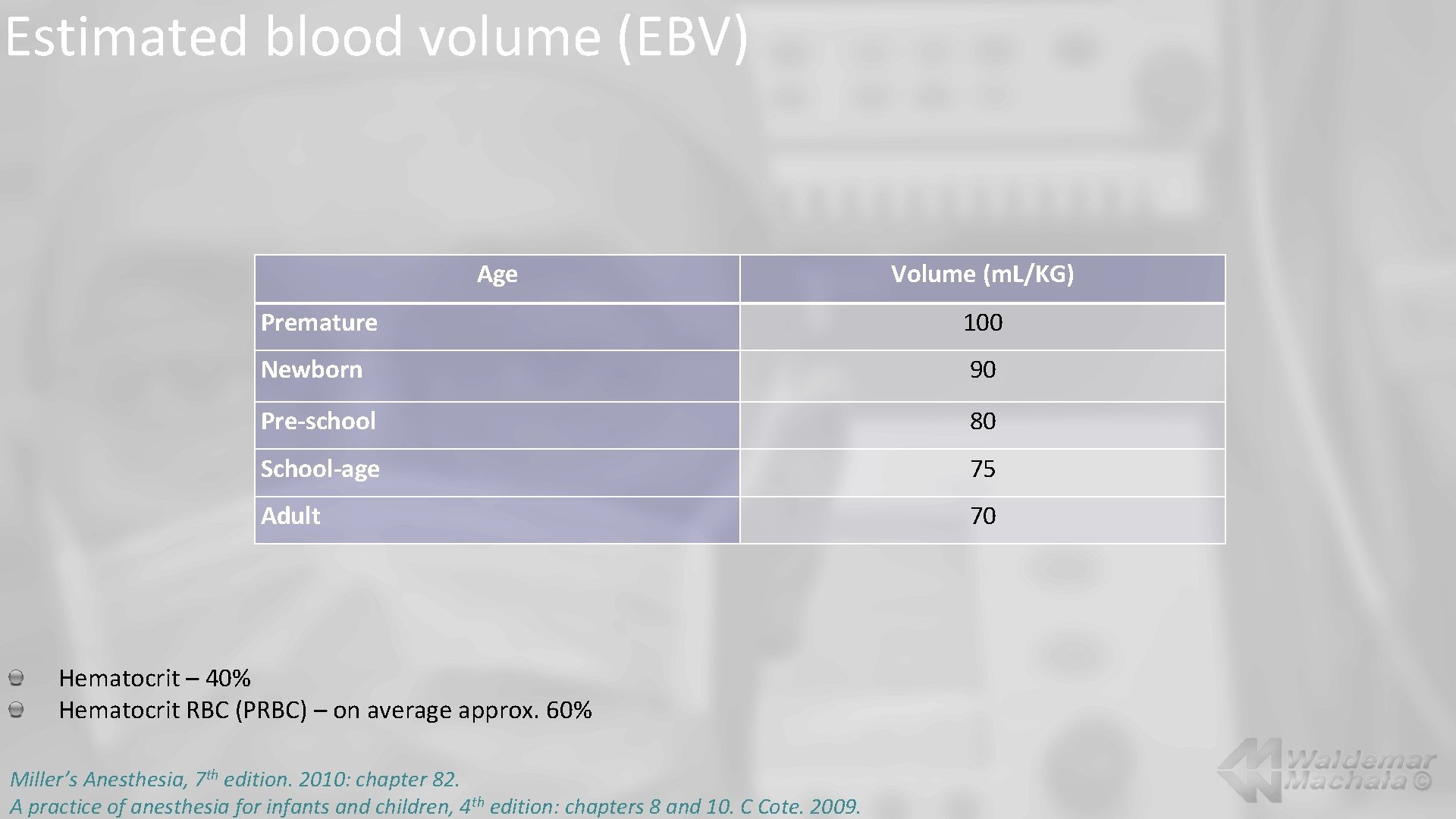
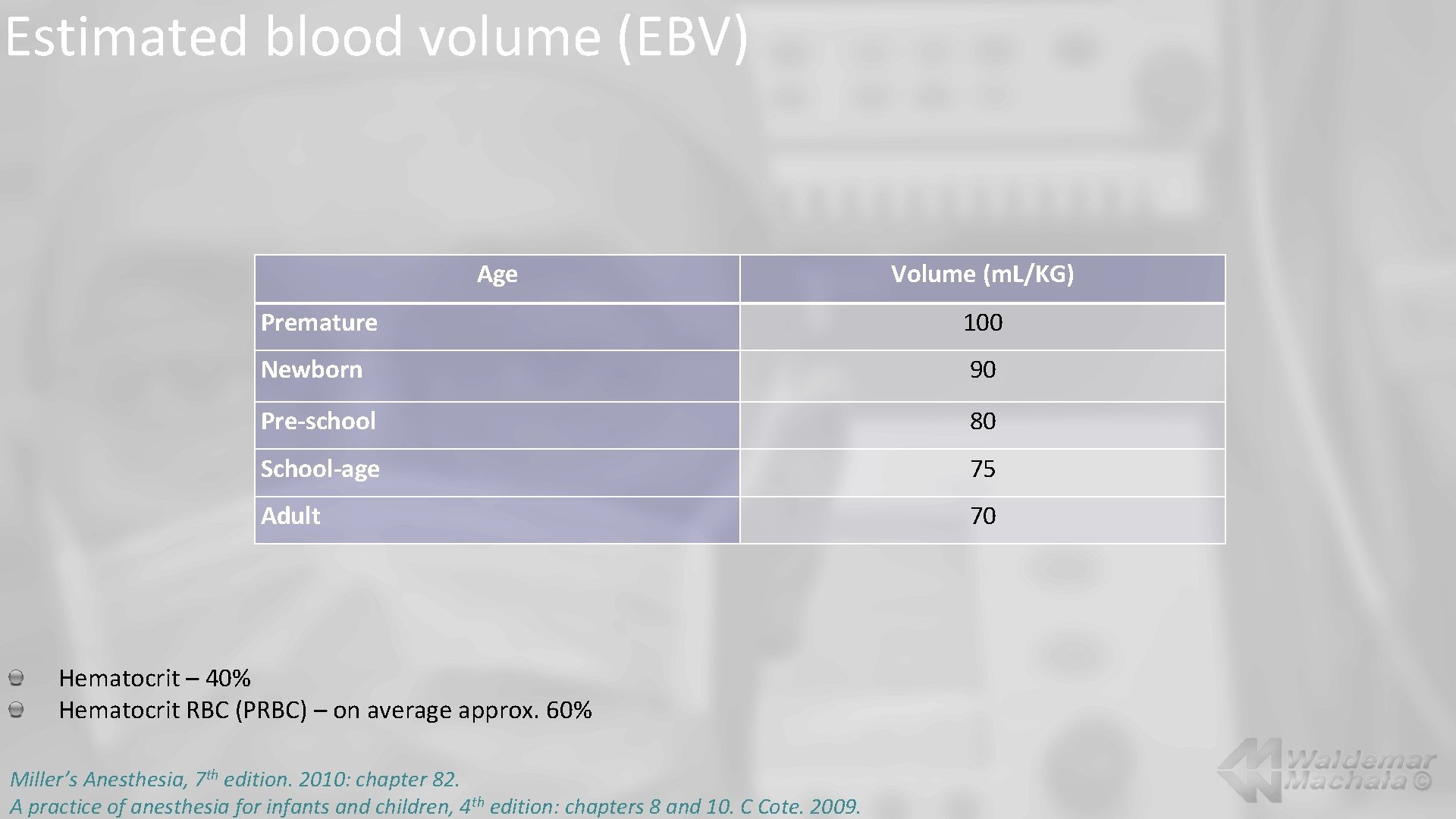
Estimated blood volume (EBV) Age Volume (m. L/KG) Premature 100 Newborn 90 Pre-school 80 School-age 75 Adult 70 Hematocrit – 40% Hematocrit RBC (PRBC) – on average approx. 60% Miller’s Anesthesia, 7 th edition. 2010: chapter 82. A practice of anesthesia for infants and children, 4 th edition: chapters 8 and 10. C Cote. 2009.
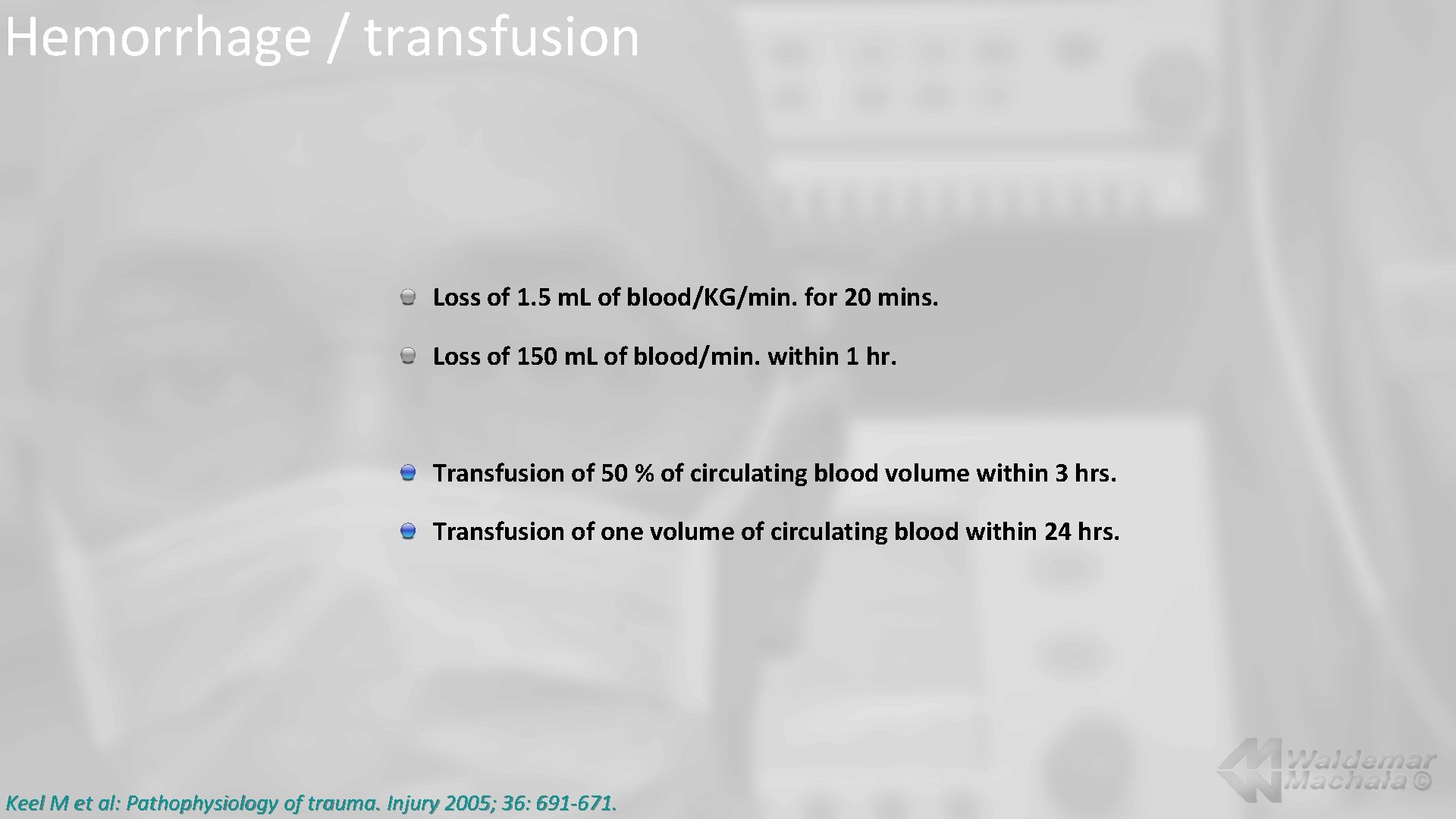
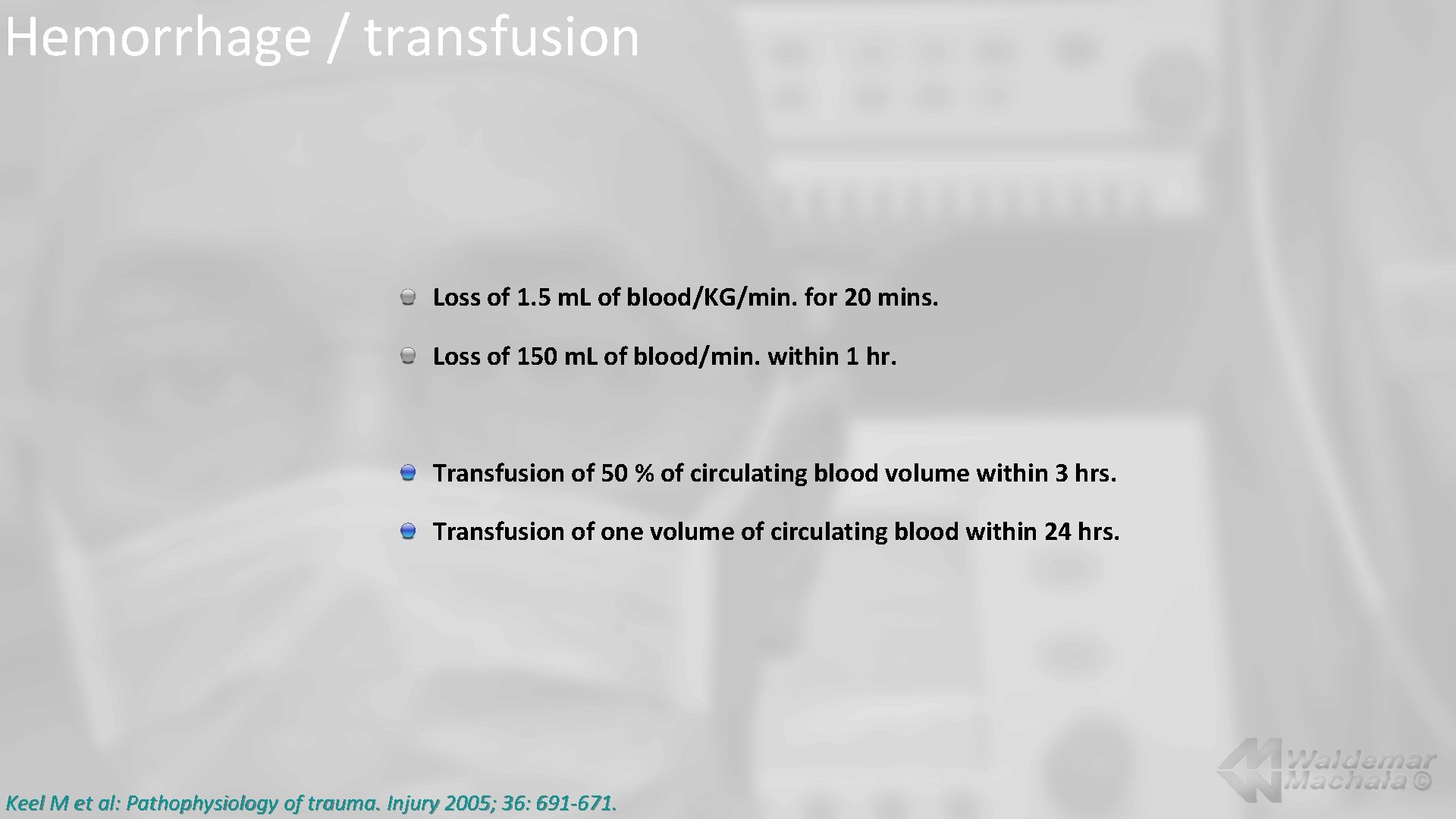
Hemorrhage / transfusion Loss of 1. 5 m. L of blood/KG/min. for 20 mins. Loss of 150 m. L of blood/min. within 1 hr. Transfusion of 50 % of circulating blood volume within 3 hrs. Transfusion of one volume of circulating blood within 24 hrs. Keel M et al: Pathophysiology of trauma. Injury 2005; 36: 691 -671.
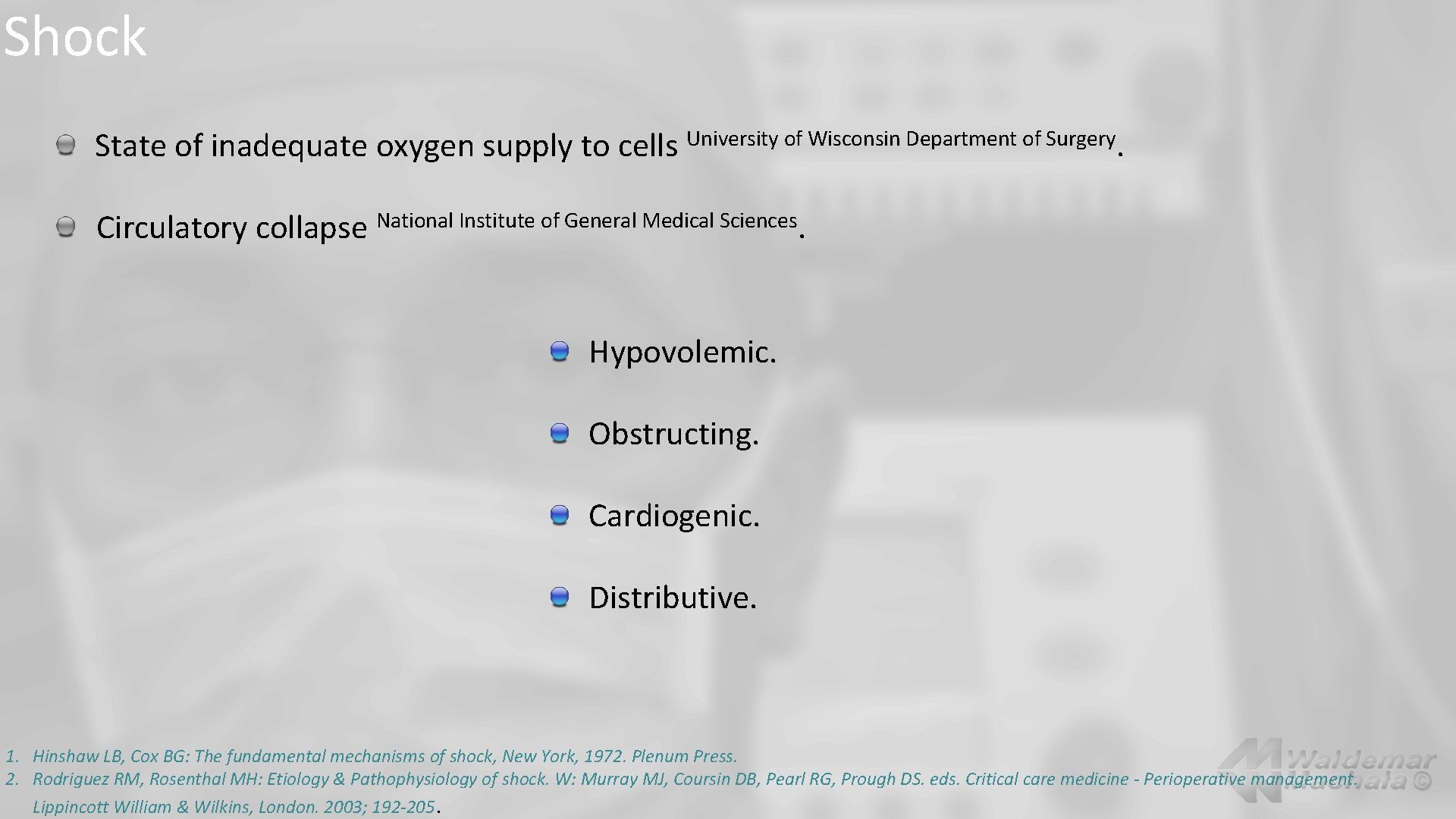
Shock State of inadequate oxygen supply to cells University of Wisconsin Department of Surgery. Circulatory collapse National Institute of General Medical Sciences. Hypovolemic. Obstructing. Cardiogenic. Distributive. 1. Hinshaw LB, Cox BG: The fundamental mechanisms of shock, New York, 1972. Plenum Press. 2. Rodriguez RM, Rosenthal MH: Etiology & Pathophysiology of shock. W: Murray MJ, Coursin DB, Pearl RG, Prough DS. eds. Critical care medicine - Perioperative management. Lippincott William & Wilkins, London. 2003; 192 -205.
Hinshaw, Cox 1972 Hypovelemic shock Hemorrhagic. Visible. Invisible. Non-hemorrhagic. 1. Hinshaw LB, Cox BG: The fundamental mechanisms of shock, New York, 1972. Plenum Press. 2. Rodriguez RM, Rosenthal MH: Etiology & Pathophysiology of shock. W: Murray MJ, Coursin DB, Pearl RG, Prough DS. eds. Critical care medicine - Perioperative management. Lippincott William & Wilkins, London. 2003; 192 -205.
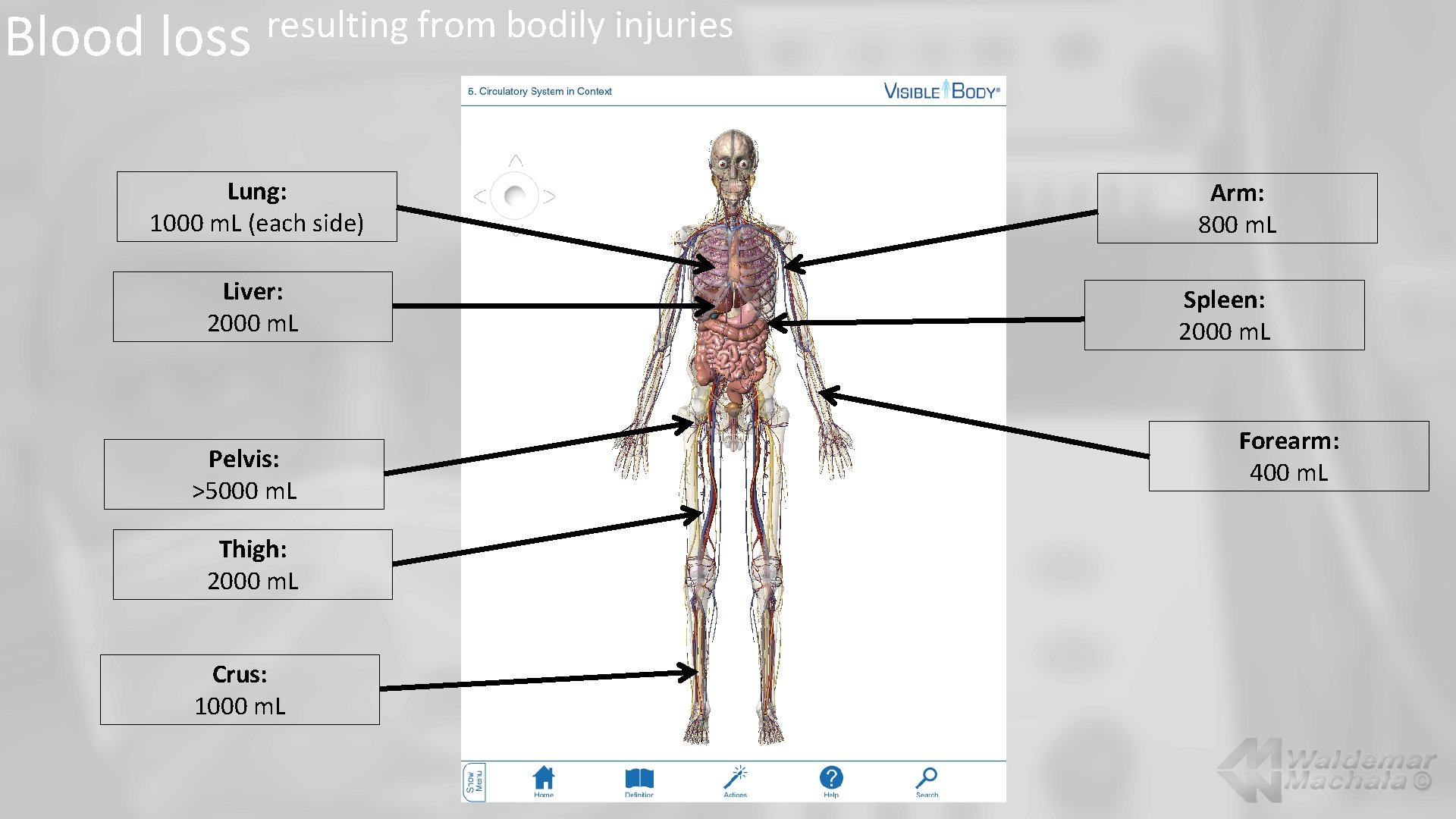
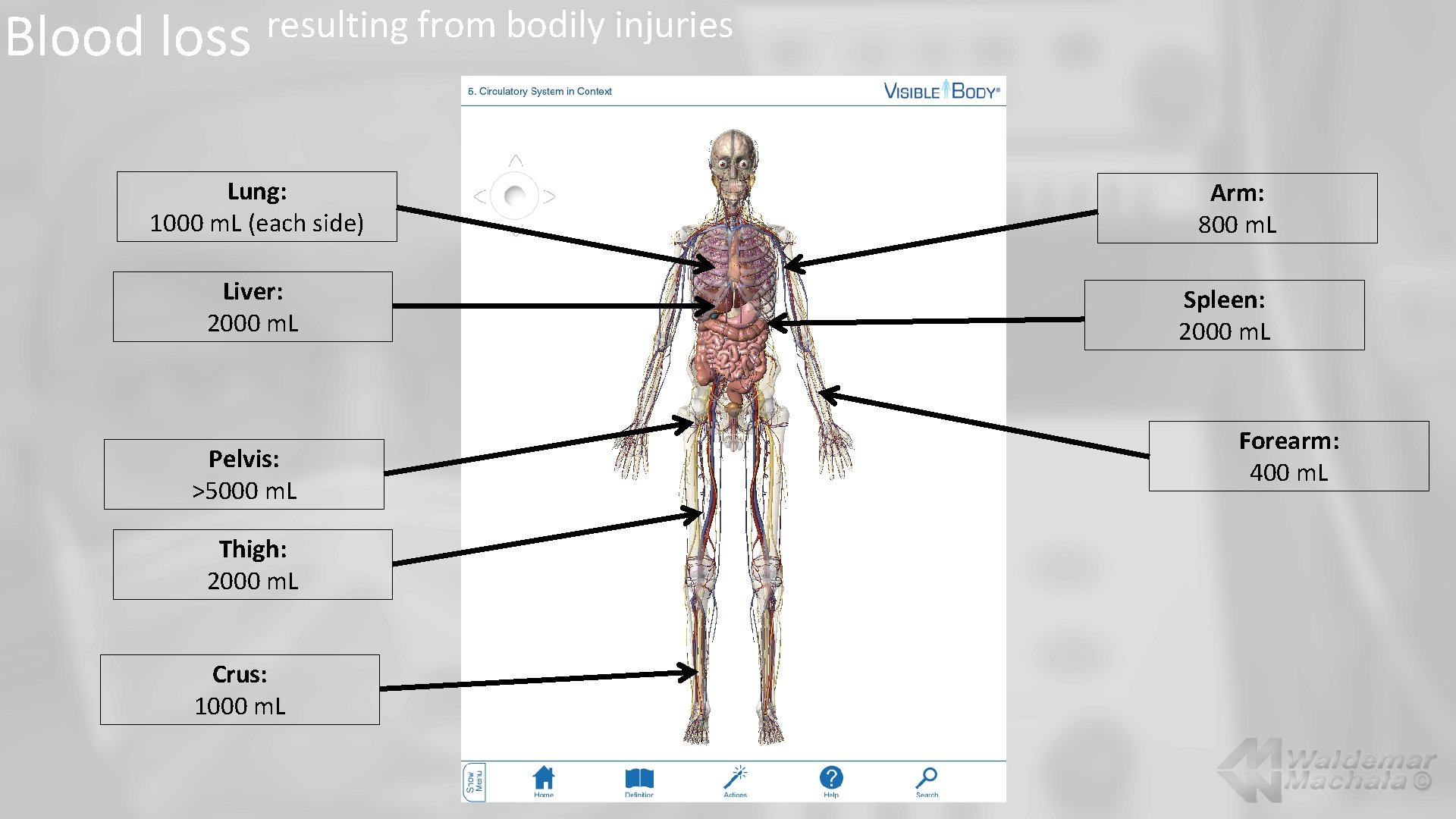
Blood loss resulting from bodily injuries Lung: 1000 m. L (each side) Liver: 2000 m. L Pelvis: >5000 m. L Thigh: 2000 m. L Crus: 1000 m. L Arm: 800 m. L Spleen: 2000 m. L Forearm: 400 m. L
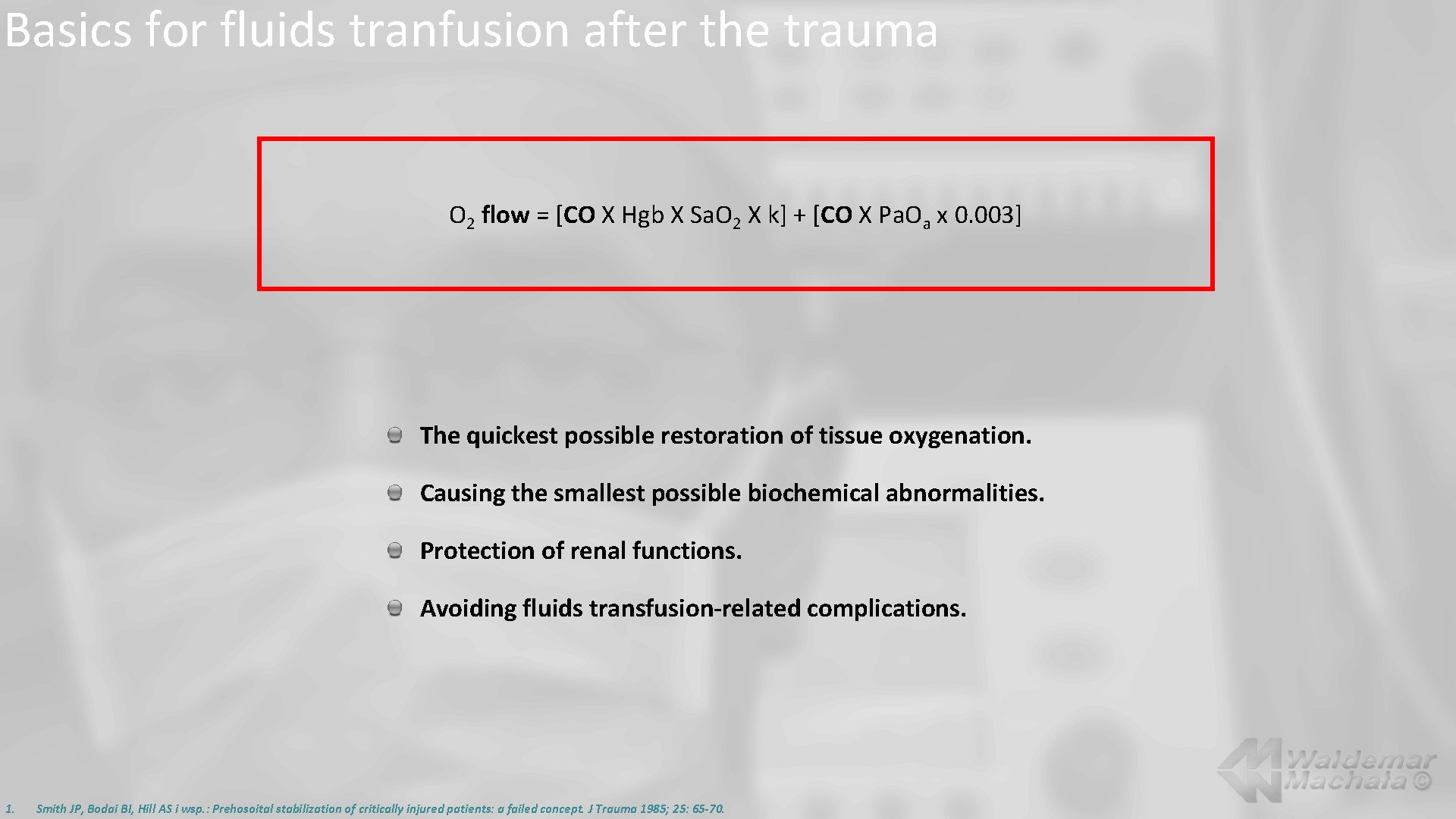
Basics for fluids tranfusion after the trauma O 2 flow = [CO X Hgb X Sa. O 2 X k] + [CO X Pa. Oa x 0. 003] The quickest possible restoration of tissue oxygenation. Causing the smallest possible biochemical abnormalities. Protection of renal functions. Avoiding fluids transfusion-related complications. 1. Smith JP, Bodai BI, Hill AS i wsp. : Prehosoital stabilization of critically injured patients: a failed concept. J Trauma 1985; 25: 65 -70.
Time for fluid therapy onset Pre-hospital. Hospital emergency ward. During emergency operations. In ICU. 1. Smith JP, Bodai BI, Hill AS i wsp. : Prehosoital stabilization of critically injured patients: a failed concept. J Trauma 1985; 25: 65 -70.
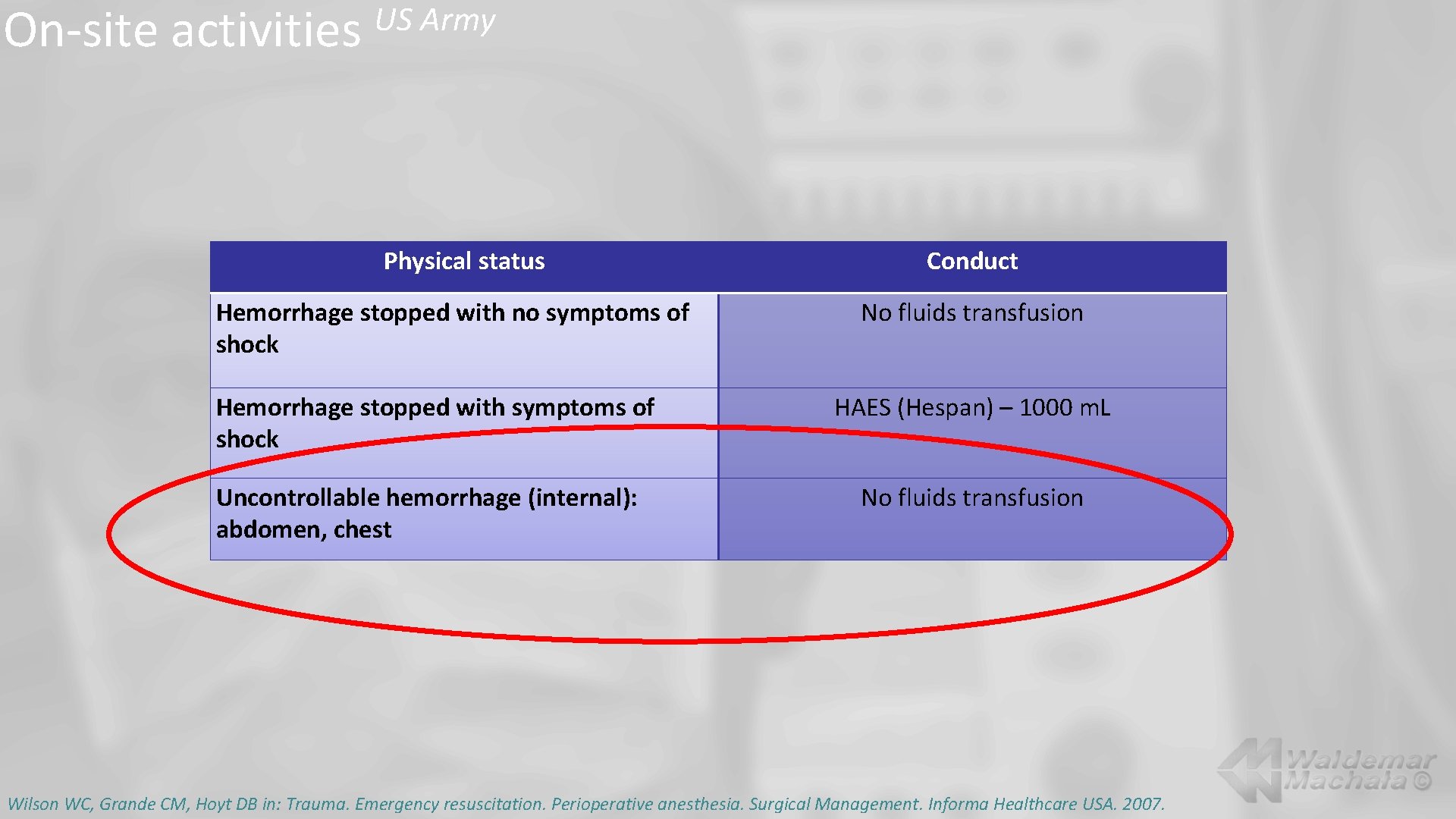
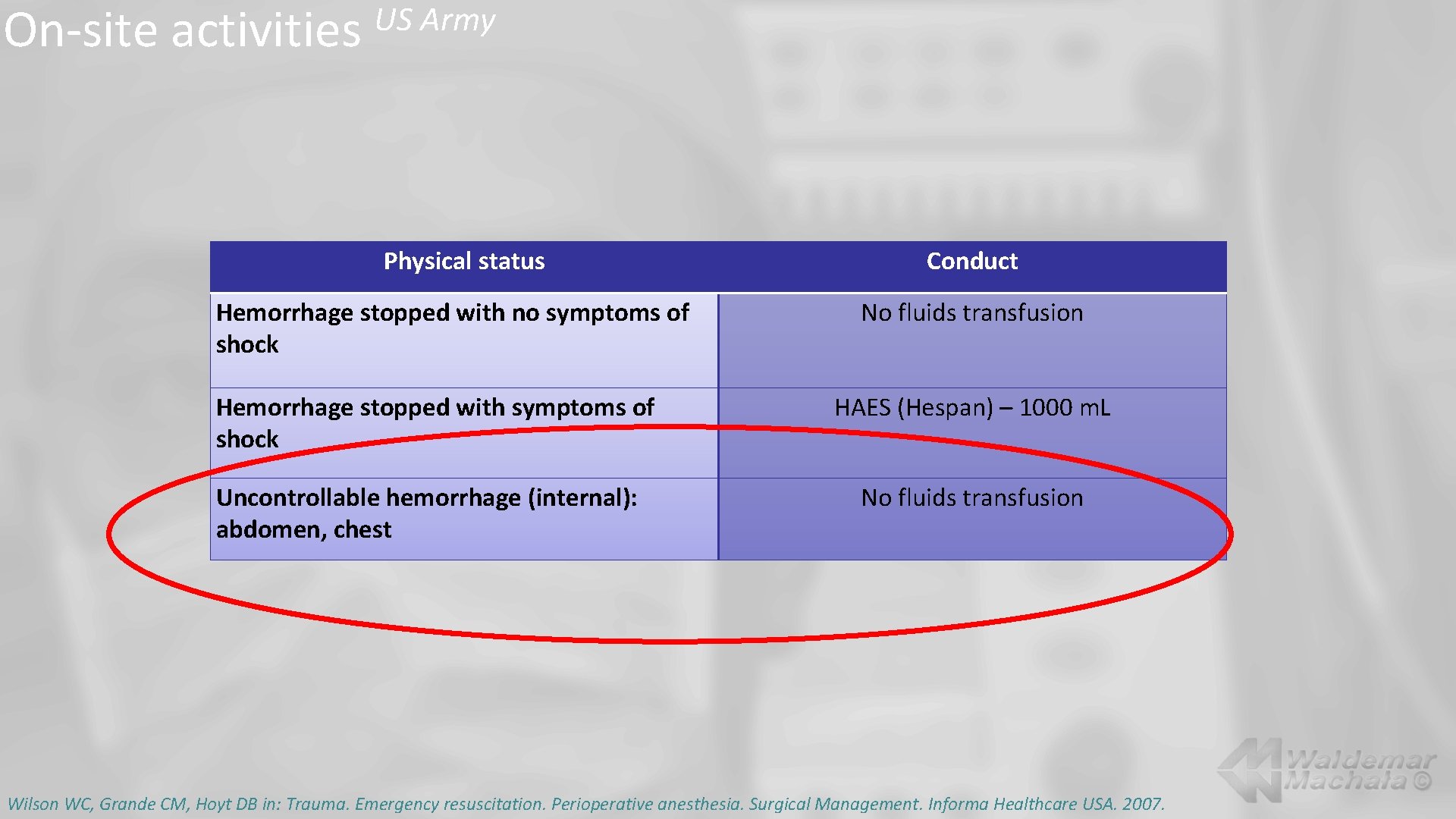
On-site activities US Army Physical status Hemorrhage stopped with no symptoms of shock Hemorrhage stopped with symptoms of shock Uncontrollable hemorrhage (internal): abdomen, chest Conduct No fluids transfusion HAES (Hespan) – 1000 m. L No fluids transfusion Wilson WC, Grande CM, Hoyt DB in: Trauma. Emergency resuscitation. Perioperative anesthesia. Surgical Management. Informa Healthcare USA. 2007.
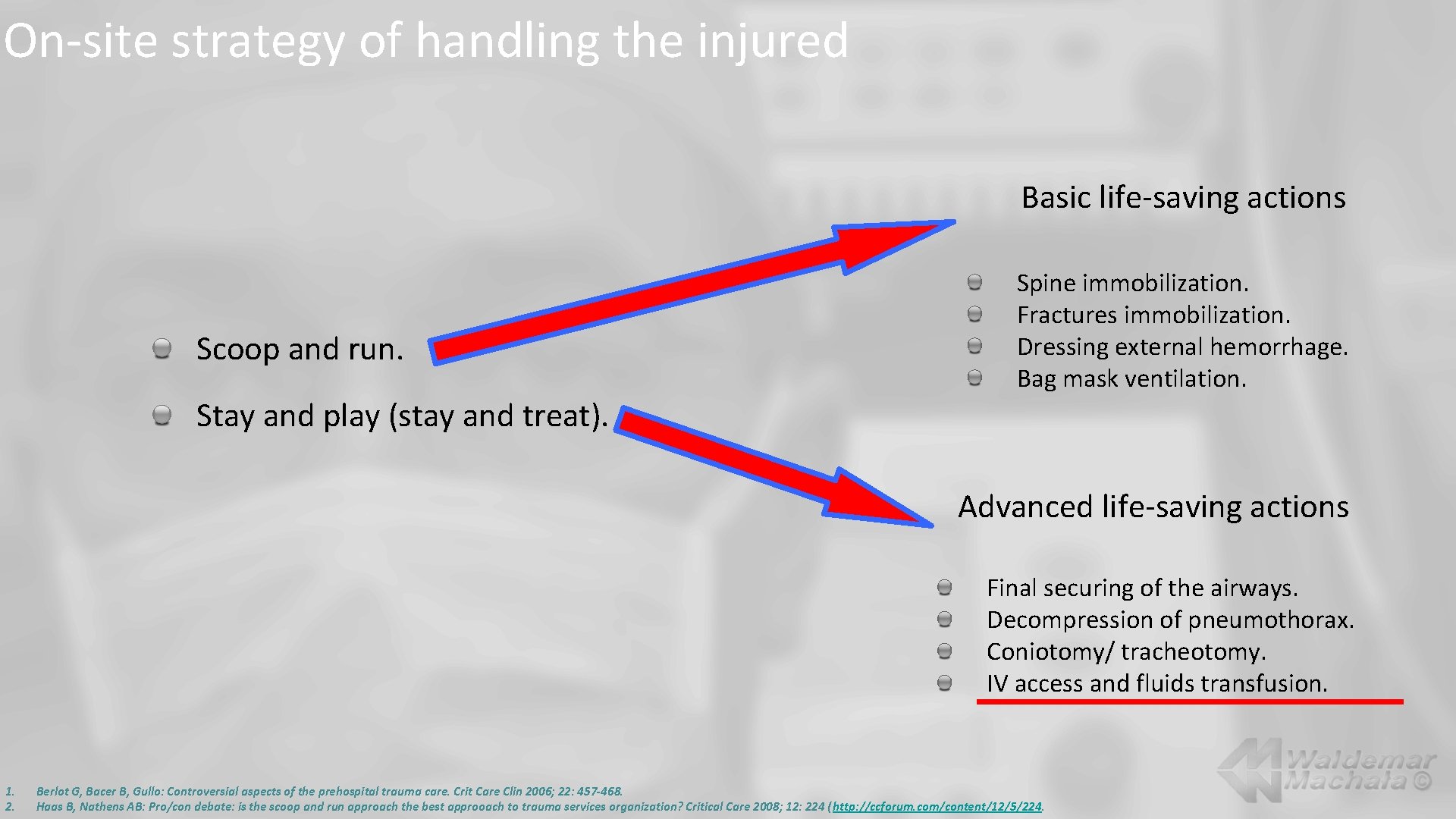
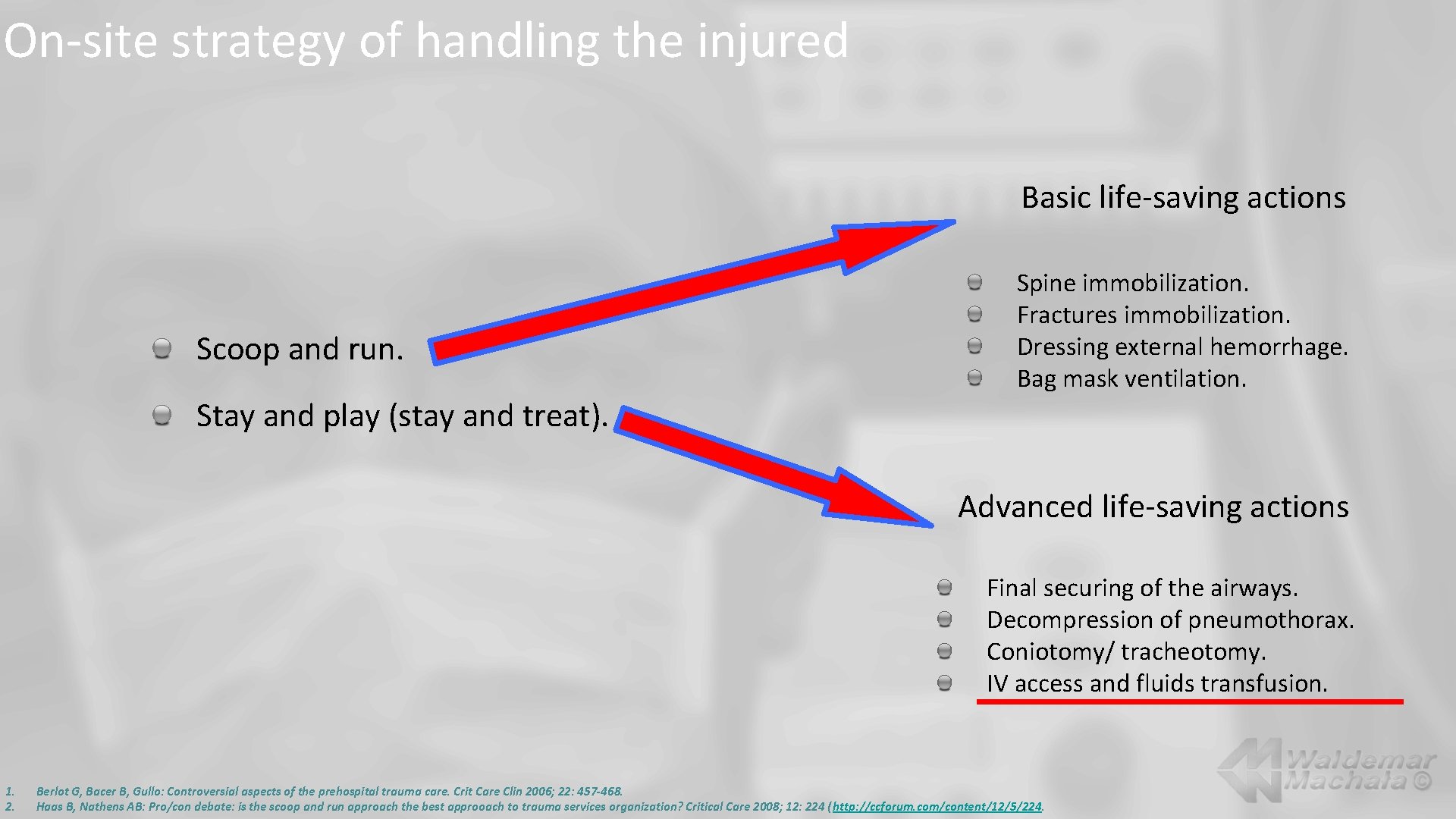
On-site strategy of handling the injured Basic life-saving actions Scoop and run. Spine immobilization. Fractures immobilization. Dressing external hemorrhage. Bag mask ventilation. Stay and play (stay and treat). Advanced life-saving actions Final securing of the airways. Decompression of pneumothorax. Coniotomy/ tracheotomy. IV access and fluids transfusion. 1. 2. Berlot G, Bacer B, Gullo: Controversial aspects of the prehospital trauma care. Crit Care Clin 2006; 22: 457 -468. Haas B, Nathens AB: Pro/con debate: is the scoop and run approach the best approoach to trauma services organization? Critical Care 2008; 12: 224 (http: //ccforum. com/content/12/5/224.
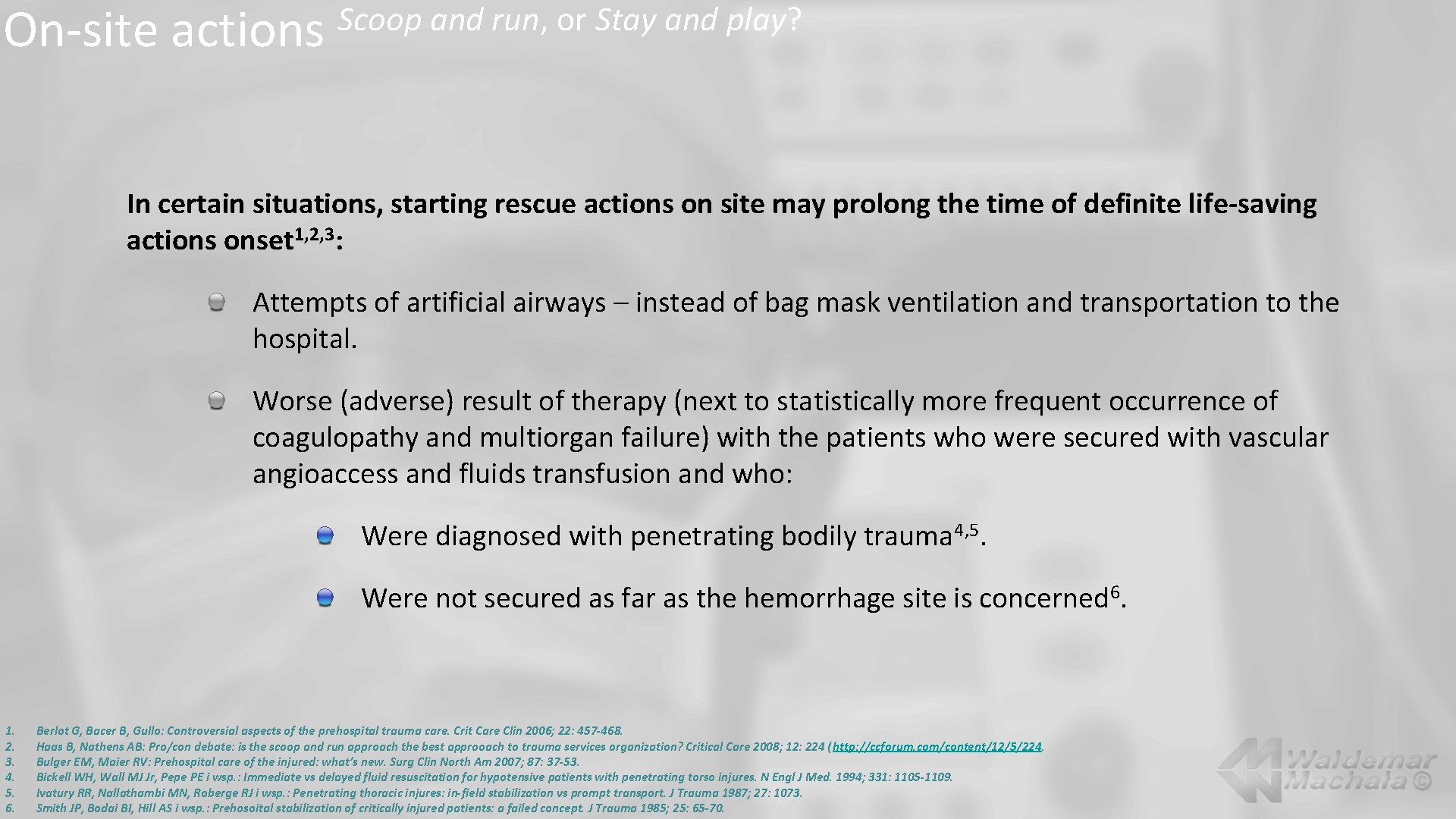
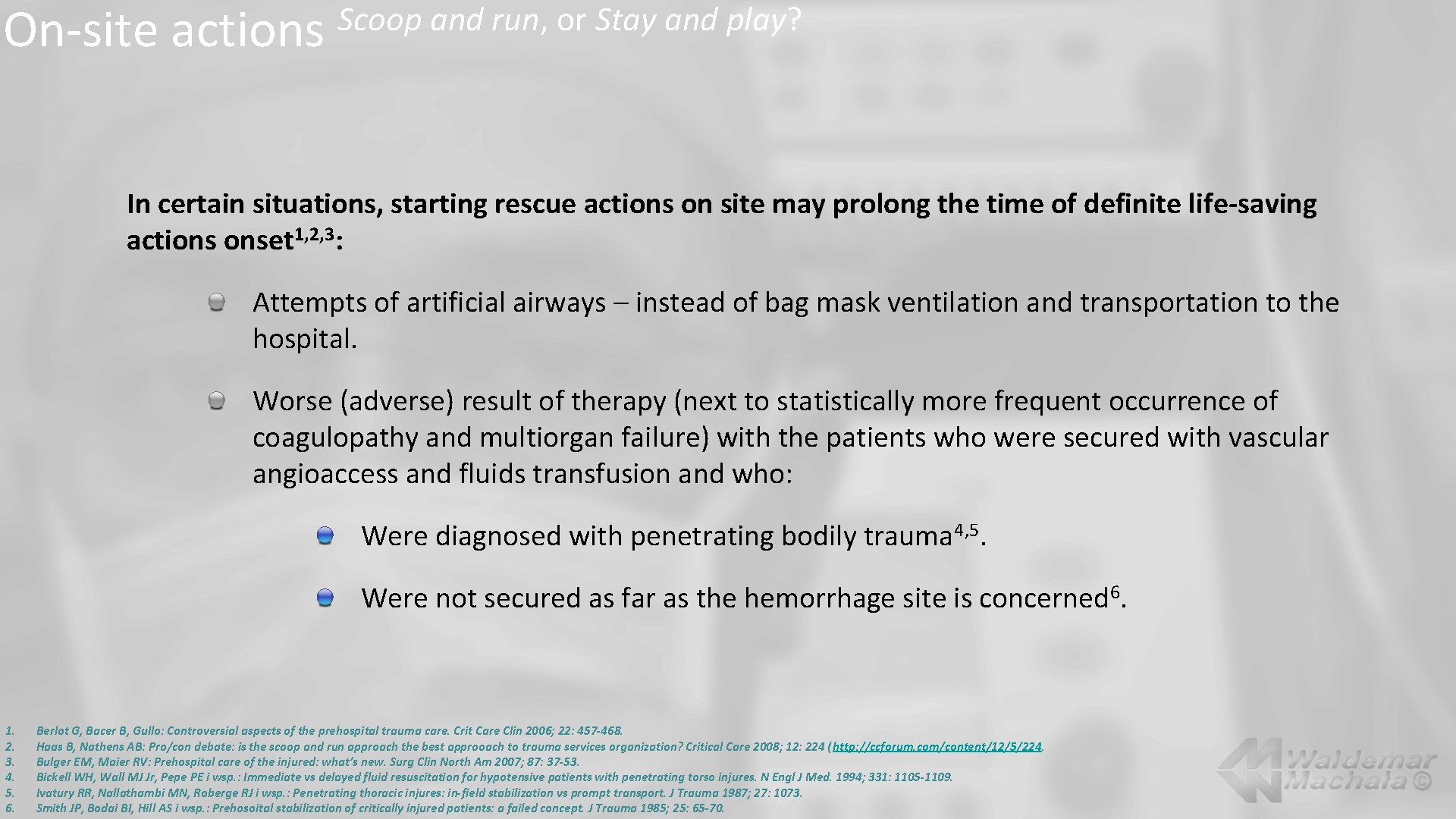
On-site actions Scoop and run, or Stay and play? In certain situations, starting rescue actions on site may prolong the time of definite life-saving actions onset 1, 2, 3: Attempts of artificial airways – instead of bag mask ventilation and transportation to the hospital. Worse (adverse) result of therapy (next to statistically more frequent occurrence of coagulopathy and multiorgan failure) with the patients who were secured with vascular angioaccess and fluids transfusion and who: Were diagnosed with penetrating bodily trauma 4, 5. Were not secured as far as the hemorrhage site is concerned 6. 1. 2. 3. 4. 5. 6. Berlot G, Bacer B, Gullo: Controversial aspects of the prehospital trauma care. Crit Care Clin 2006; 22: 457 -468. Haas B, Nathens AB: Pro/con debate: is the scoop and run approach the best approoach to trauma services organization? Critical Care 2008; 12: 224 (http: //ccforum. com/content/12/5/224. Bulger EM, Maier RV: Prehospital care of the injured: what’s new. Surg Clin North Am 2007; 87: 37 -53. Bickell WH, Wall MJ Jr, Pepe PE i wsp. : Immediate vs delayed fluid resuscitation for hypotensive patients with penetrating torso injures. N Engl J Med. 1994; 331: 1105 -1109. Ivatury RR, Nallathambi MN, Roberge RJ i wsp. : Penetrating thoracic injures: in-field stabilization vs prompt transport. J Trauma 1987; 27: 1073. Smith JP, Bodai BI, Hill AS i wsp. : Prehosoital stabilization of critically injured patients: a failed concept. J Trauma 1985; 25: 65 -70.
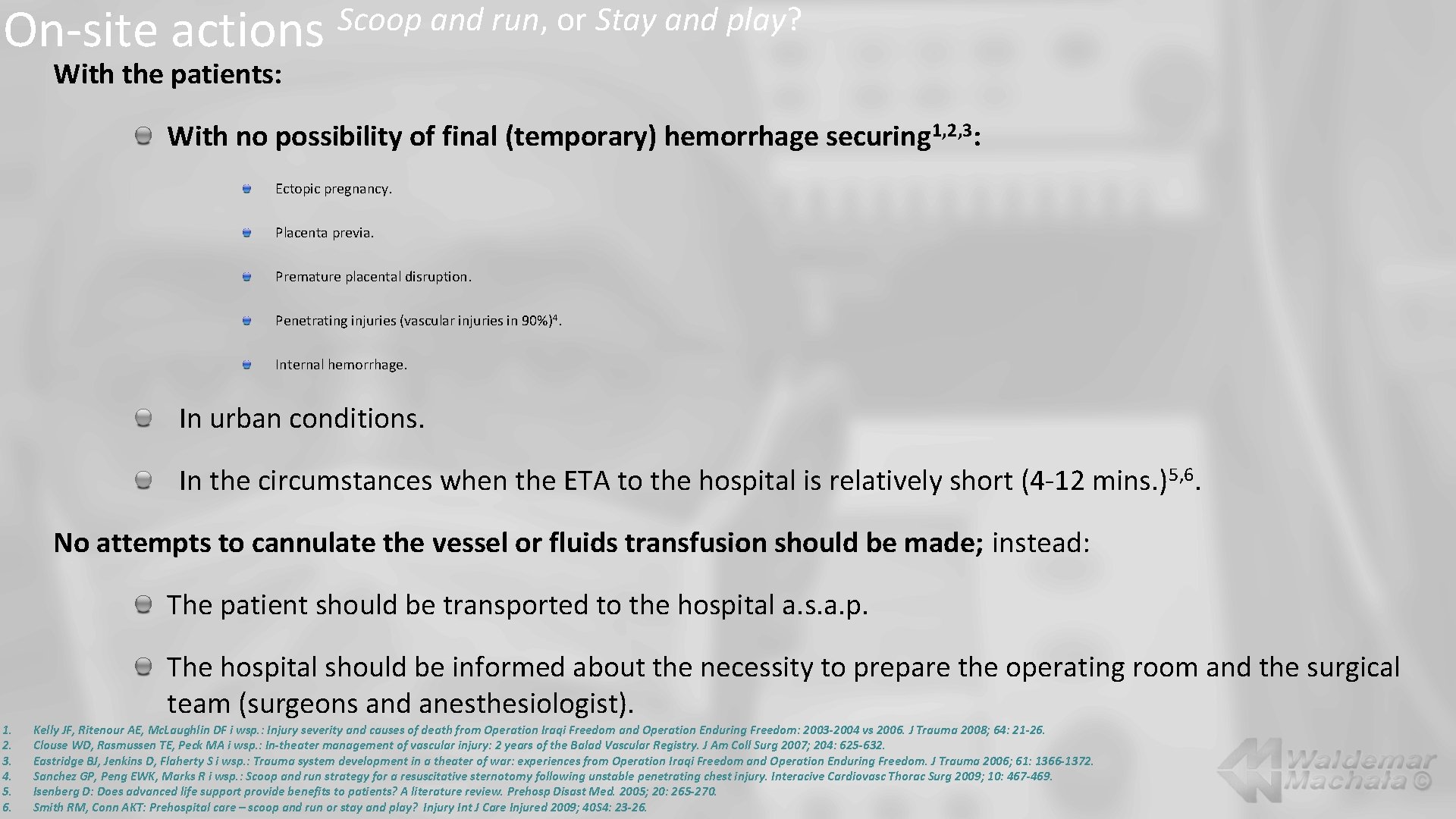
On-site actions Scoop and run, or Stay and play? With the patients: With no possibility of final (temporary) hemorrhage securing 1, 2, 3: Ectopic pregnancy. Placenta previa. Premature placental disruption. Penetrating injuries (vascular injuries in 90%)4. Internal hemorrhage. In urban conditions. In the circumstances when the ETA to the hospital is relatively short (4 -12 mins. ) 5, 6. No attempts to cannulate the vessel or fluids transfusion should be made; instead: The patient should be transported to the hospital a. s. a. p. The hospital should be informed about the necessity to prepare the operating room and the surgical team (surgeons and anesthesiologist). 1. 2. 3. 4. 5. 6. Kelly JF, Ritenour AE, Mc. Laughlin DF i wsp. : Injury severity and causes of death from Operation Iraqi Freedom and Operation Enduring Freedom: 2003 -2004 vs 2006. J Trauma 2008; 64: 21 -26. Clouse WD, Rasmussen TE, Peck MA i wsp. : In-theater management of vascular injury: 2 years of the Balad Vascular Registry. J Am Coll Surg 2007; 204: 625 -632. Eastridge BJ, Jenkins D, Flaherty S i wsp. : Trauma system development in a theater of war: experiences from Operation Iraqi Freedom and Operation Enduring Freedom. J Trauma 2006; 61: 1366 -1372. Sanchez GP, Peng EWK, Marks R i wsp. : Scoop and run strategy for a resuscitative sternotomy following unstable penetrating chest injury. Interacive Cardiovasc Thorac Surg 2009; 10: 467 -469. Isenberg D: Does advanced life support provide benefits to patients? A literature review. Prehosp Disast Med. 2005; 20: 265 -270. Smith RM, Conn AKT: Prehospital care – scoop and run or stay and play? Injury Int J Care Injured 2009; 40 S 4: 23 -26.
On-site actions Scoop and run, or Stay and play? With the patients with no possibility of final (temporary) hemorrhage securing 1, 2, 3 no attempts to cannulate the vessel or fluids transfusion should be made, instead: The patient should be transported to the hospital a. s. a. p. . The hospital should be informed about the necessity to prepare the operating room and the surgical team (surgeons and anesthesiologist). Adverse effects of fluids transfusion with the lack of securing the hemorrhage site: Increased bleeding from damaged vessels. Smaller clot-forming abilities in the site where the vessels are damaged. Increase in the hematocrit and the hemoglobin levels. Lowering of the clotting factors levels. Risk of hypothermia. 1. 2. 3. Kelly JF, Ritenour AE, Mc. Laughlin DF i wsp. : Injury severity and causes of death from Operation Iraqi Freedom and Operation Enduring Freedom: 2003 -2004 vs 2006. J Trauma 2008; 64: 21 -26. Clouse WD, Rasmussen TE, Peck MA i wsp. : In-theater management of vascular injury: 2 years of the Balad Vascular Registry. J Am Coll Surg 2007; 204: 625 -632. Eastridge BJ, Jenkins D, Flaherty S i wsp. : Trauma system development in a theater of war: experiences from Operation Iraqi Freedom and Operation Enduring Freedom. J Trauma 2006; 61: 1366 -1372.
On-site actions 1. 2. 3. Scoop and run, or Stay and play? Kelly JF, Ritenour AE, Mc. Laughlin DF i wsp. : Injury severity and causes of death from Operation Iraqi Freedom and Operation Enduring Freedom: 2003 -2004 vs 2006. J Trauma 2008; 64: 21 -26. Clouse WD, Rasmussen TE, Peck MA i wsp. : In-theater management of vascular injury: 2 years of the Balad Vascular Registry. J Am Coll Surg 2007; 204: 625 -632. Eastridge BJ, Jenkins D, Flaherty S i wsp. : Trauma system development in a theater of war: experiences from Operation Iraqi Freedom and Operation Enduring Freedom. J Trauma 2006; 61: 1366 -1372.
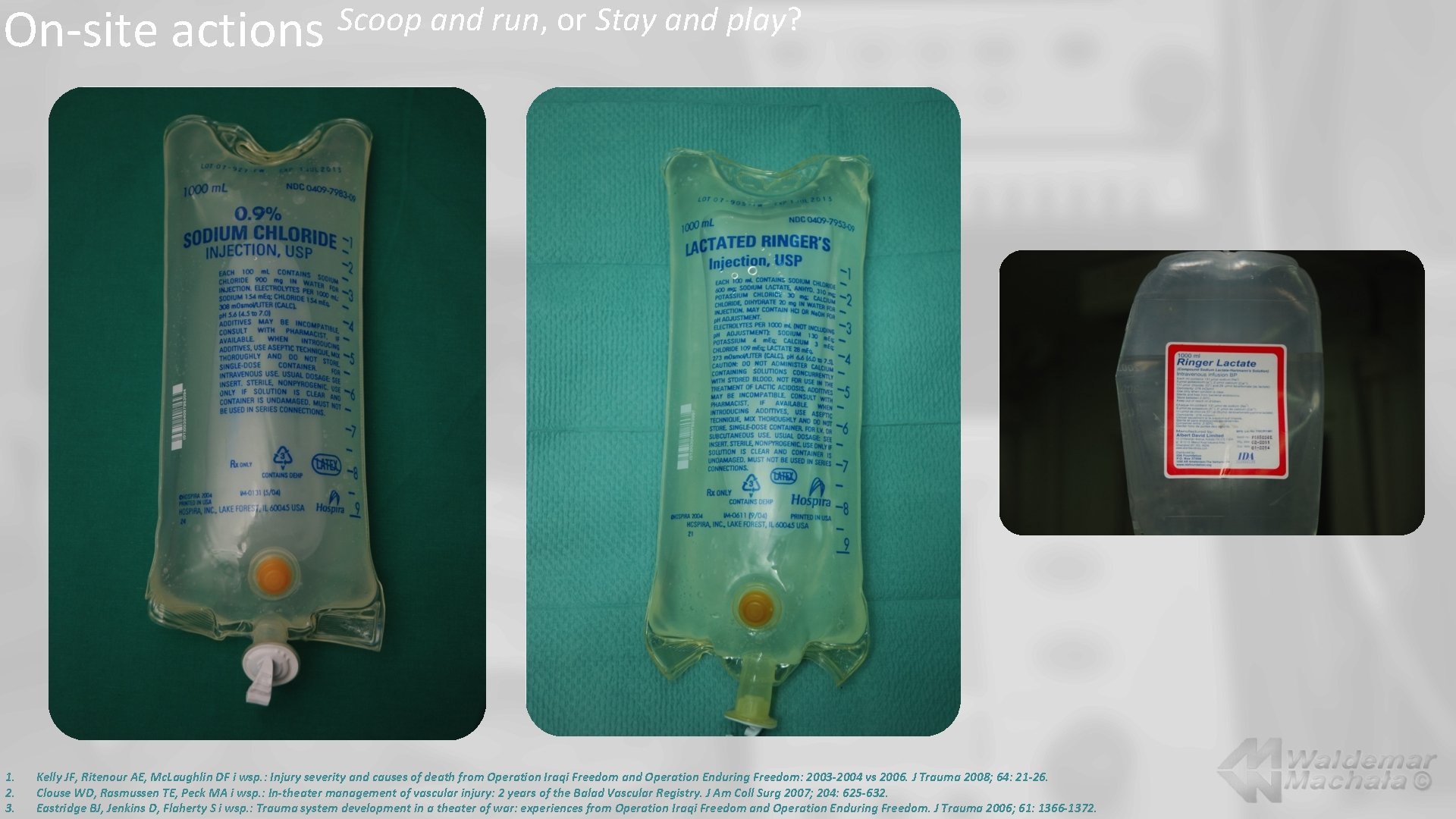
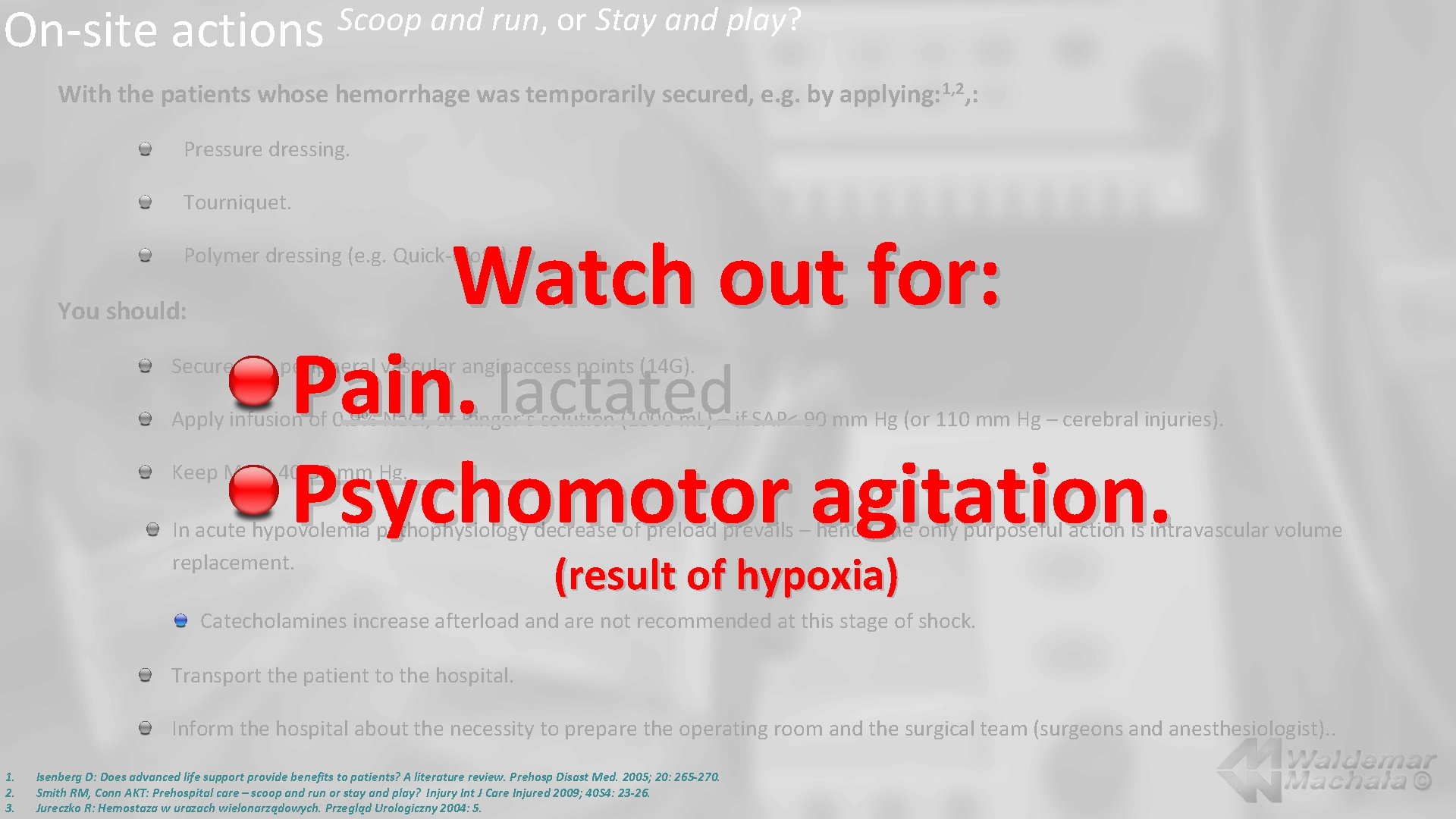
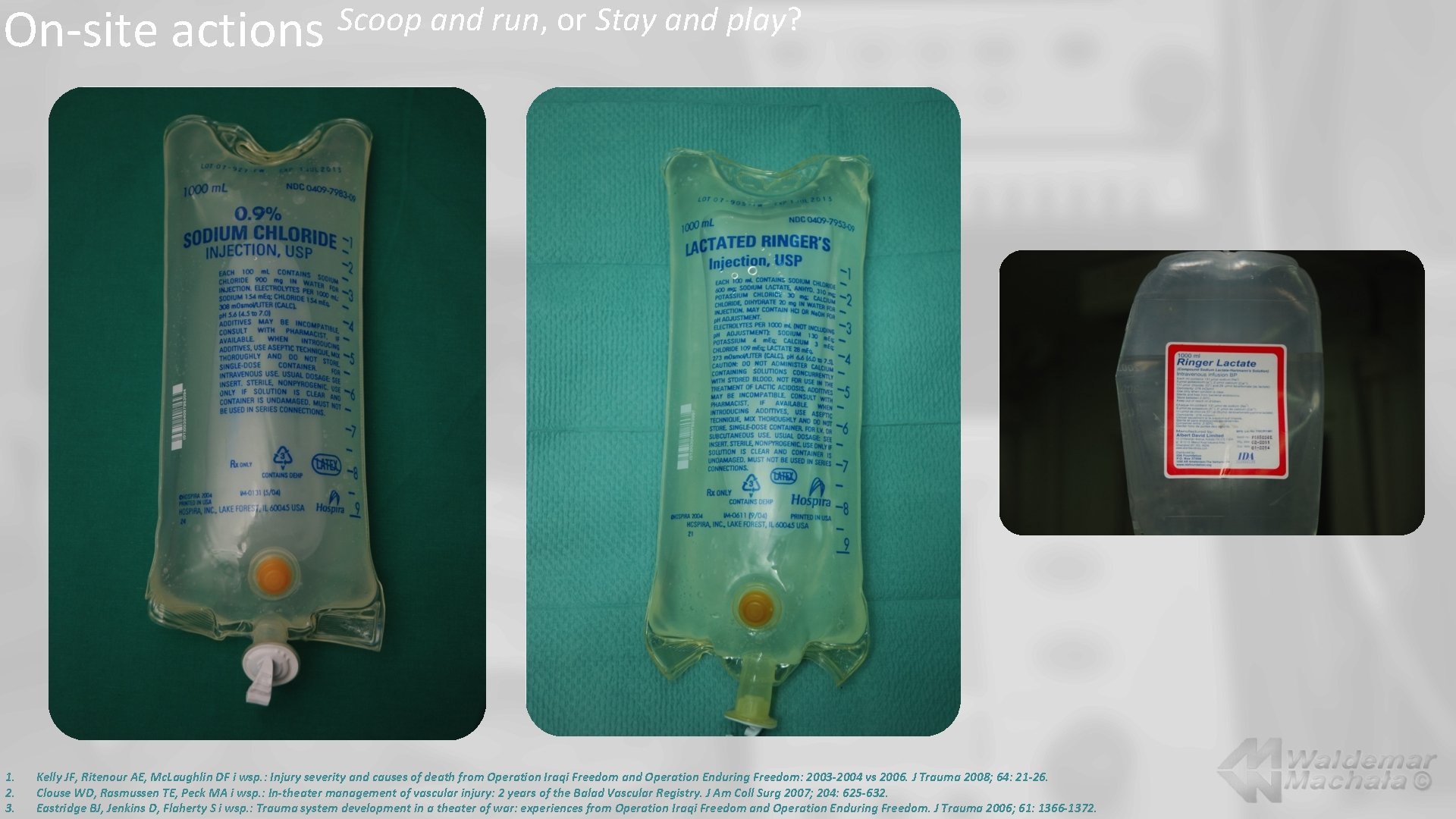
On-site actions Scoop and run, or Stay and play? With the patients whose hemorrhage was temporarily secured, e. g. by applying: 1, 2, : Pressure dressing. Tourniquet. Polymer dressing (e. g. Quick-Cloth). you should: Secure two peripheral vascular angioaccess points (14 G). Apply infusion of 0. 9% Na. Cl, or lactatad Ringer’s solution (1000 m. L) – if SAP< 90 mm Hg (or 110 mm Hg – cerebral injuries). Maintain MAP: 40 -50 mm Hg. In acute hypovolemia pathophysiology, decrease in preload prevails – hence, the only purposeful action is intravascular volume replacement. Catecholamines increase afterload and are not recommended at this stage of shock. Transport the patient to the hospital. Inform the hospital about the necessity to prepare the operating room and the surgical team (surgeons and anesthesiologist). 1. 2. 3. Isenberg D: Does advanced life support provide benefits to patients? A literature review. Prehosp Disast Med. 2005; 20: 265 -270. Smith RM, Conn AKT: Prehospital care – scoop and run or stay and play? Injury Int J Care Injured 2009; 40 S 4: 23 -26. Jureczko R: Hemostaza w urazach wielonarządowych. Przegląd Urologiczny 2004: 5.
On-site actions Scoop and run, or Stay and play? With the patients whose hemorrhage was temporarily secured, e. g. by applying: 1, 2, : Pressure dressing. Tourniquet. Watch out for: Pain. lactated Psychomotor agitation. Polymer dressing (e. g. Quick-Cloth). You should: Secure two peripheral vascular angioaccess points (14 G). Apply infusion of 0. 9% Na. Cl, or Ringer’s solution (1000 m. L) – if SAP< 90 mm Hg (or 110 mm Hg – cerebral injuries). Keep MAP: 40 -50 mm Hg. In acute hypovolemia pathophysiology decrease of preload prevails – hence, the only purposeful action is intravascular volume replacement. (result of hypoxia) Catecholamines increase afterload and are not recommended at this stage of shock. Transport the patient to the hospital. Inform the hospital about the necessity to prepare the operating room and the surgical team (surgeons and anesthesiologist). . 1. 2. 3. Isenberg D: Does advanced life support provide benefits to patients? A literature review. Prehosp Disast Med. 2005; 20: 265 -270. Smith RM, Conn AKT: Prehospital care – scoop and run or stay and play? Injury Int J Care Injured 2009; 40 S 4: 23 -26. Jureczko R: Hemostaza w urazach wielonarządowych. Przegląd Urologiczny 2004: 5.
On-site actions 1. 2. 3. Scoop and run, or Stay and play? Isenberg D: Does advanced life support provide benefits to patients? A literature review. Prehosp Disast Med. 2005; 20: 265 -270. Smith RM, Conn AKT: Prehospital care – scoop and run or stay and play? Injury Int J Care Injured 2009; 40 S 4: 23 -26. Jureczko R: Hemostaza w urazach wielonarządowych. Przegląd Urologiczny 2004: 5.
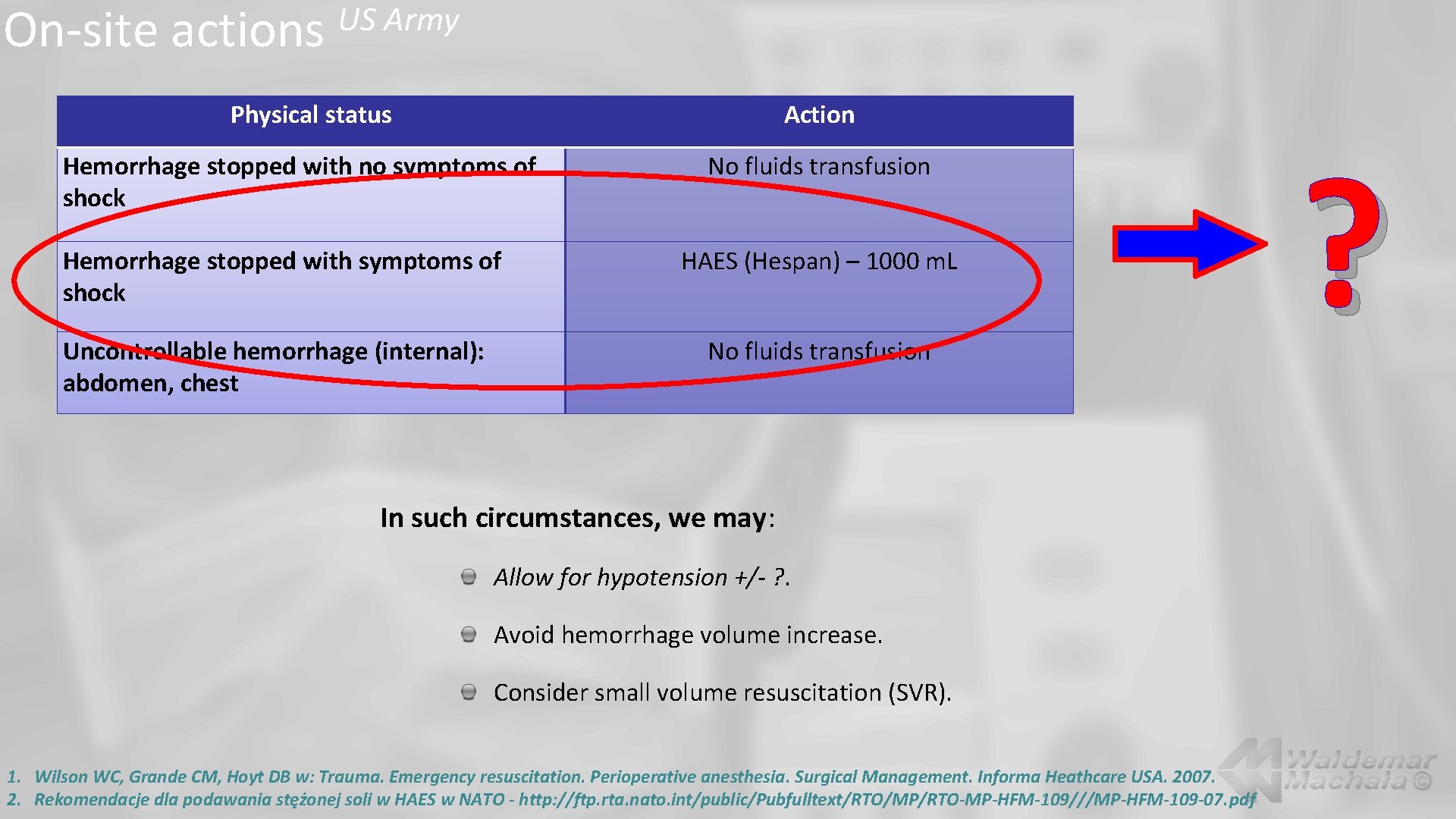
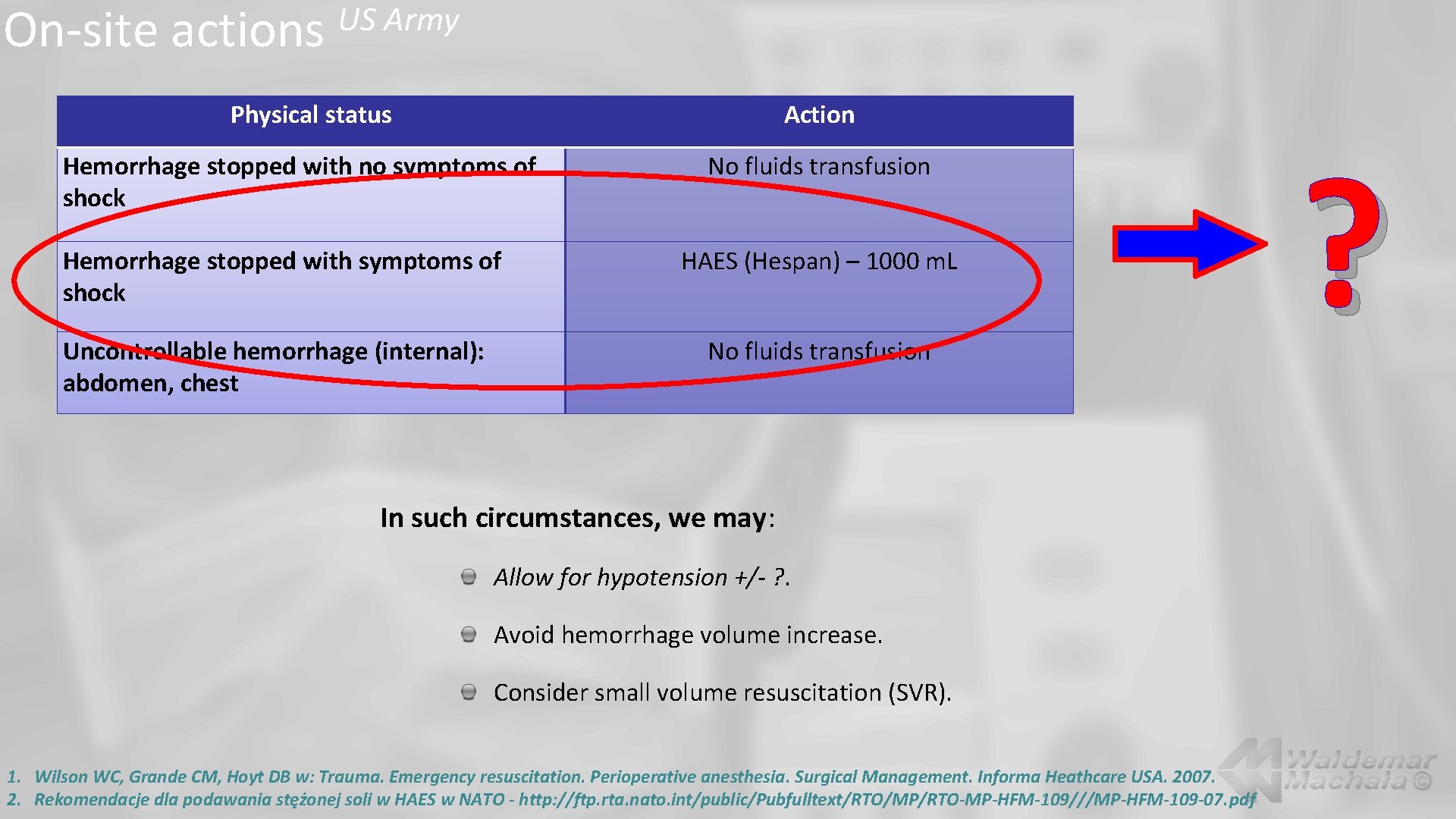
On-site actions US Army Physical status Action Hemorrhage stopped with no symptoms of shock Hemorrhage stopped with symptoms of shock Uncontrollable hemorrhage (internal): abdomen, chest No fluids transfusion HAES (Hespan) – 1000 m. L No fluids transfusion In such circumstances, we may: Allow for hypotension +/- ? . Avoid hemorrhage volume increase. Consider small volume resuscitation (SVR). 1. Wilson WC, Grande CM, Hoyt DB w: Trauma. Emergency resuscitation. Perioperative anesthesia. Surgical Management. Informa Heathcare USA. 2007. 2. Rekomendacje dla podawania stężonej soli w HAES w NATO - http: //ftp. rta. nato. int/public/Pubfulltext/RTO/MP/RTO-MP-HFM-109///MP-HFM-109 -07. pdf ?
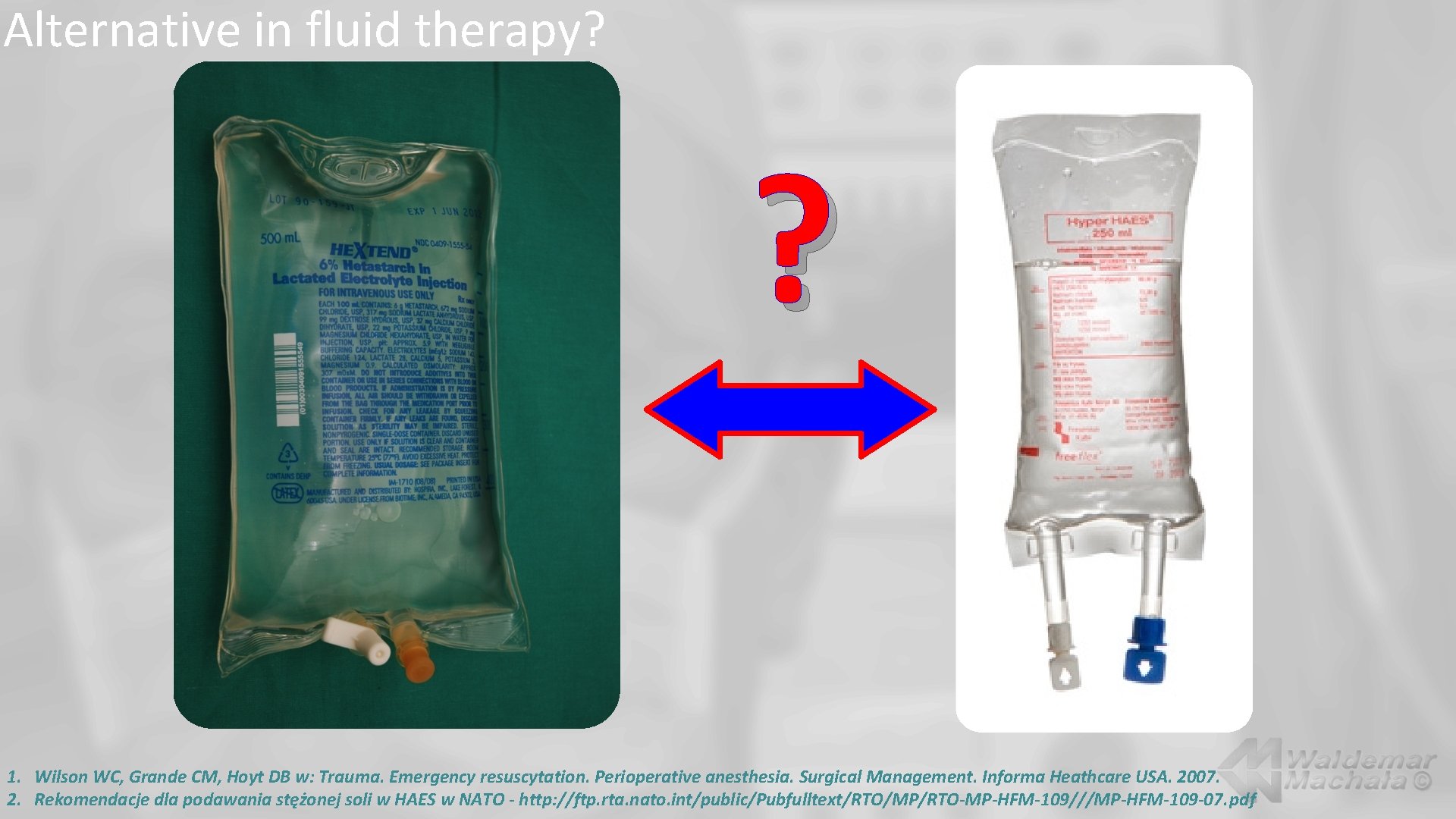
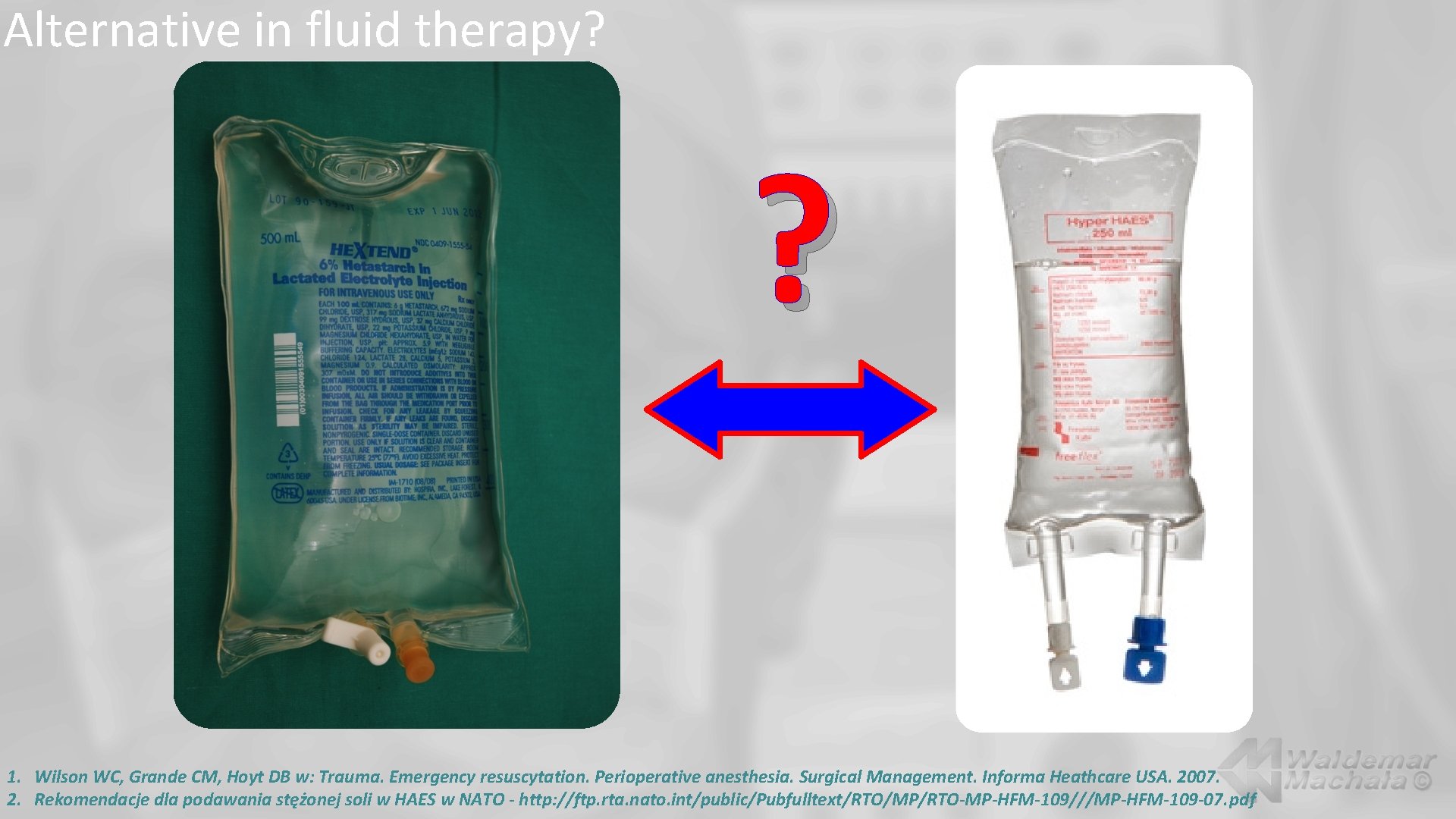
Alternative in fluid therapy? ? 1. Wilson WC, Grande CM, Hoyt DB w: Trauma. Emergency resuscytation. Perioperative anesthesia. Surgical Management. Informa Heathcare USA. 2007. 2. Rekomendacje dla podawania stężonej soli w HAES w NATO - http: //ftp. rta. nato. int/public/Pubfulltext/RTO/MP/RTO-MP-HFM-109///MP-HFM-109 -07. pdf
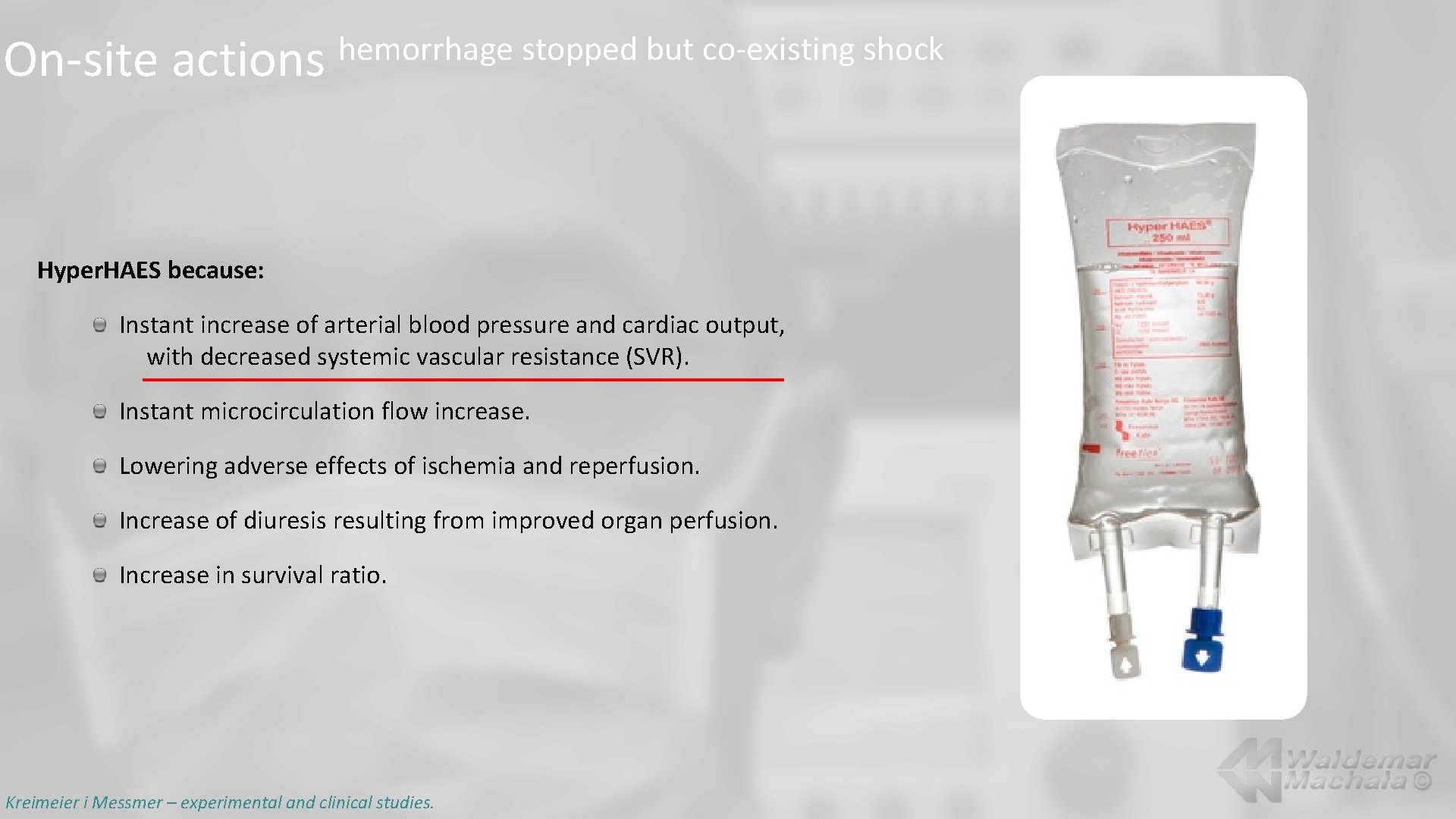
On-site actions hemorrhage stopped but co-existing shock Hyper. HAES because: Instant increase of arterial blood pressure and cardiac output, with decreased systemic vascular resistance (SVR). Instant microcirculation flow increase. Lowering adverse effects of ischemia and reperfusion. Increase of diuresis resulting from improved organ perfusion. Increase in survival ratio. Kreimeier i Messmer – experimental and clinical studies.
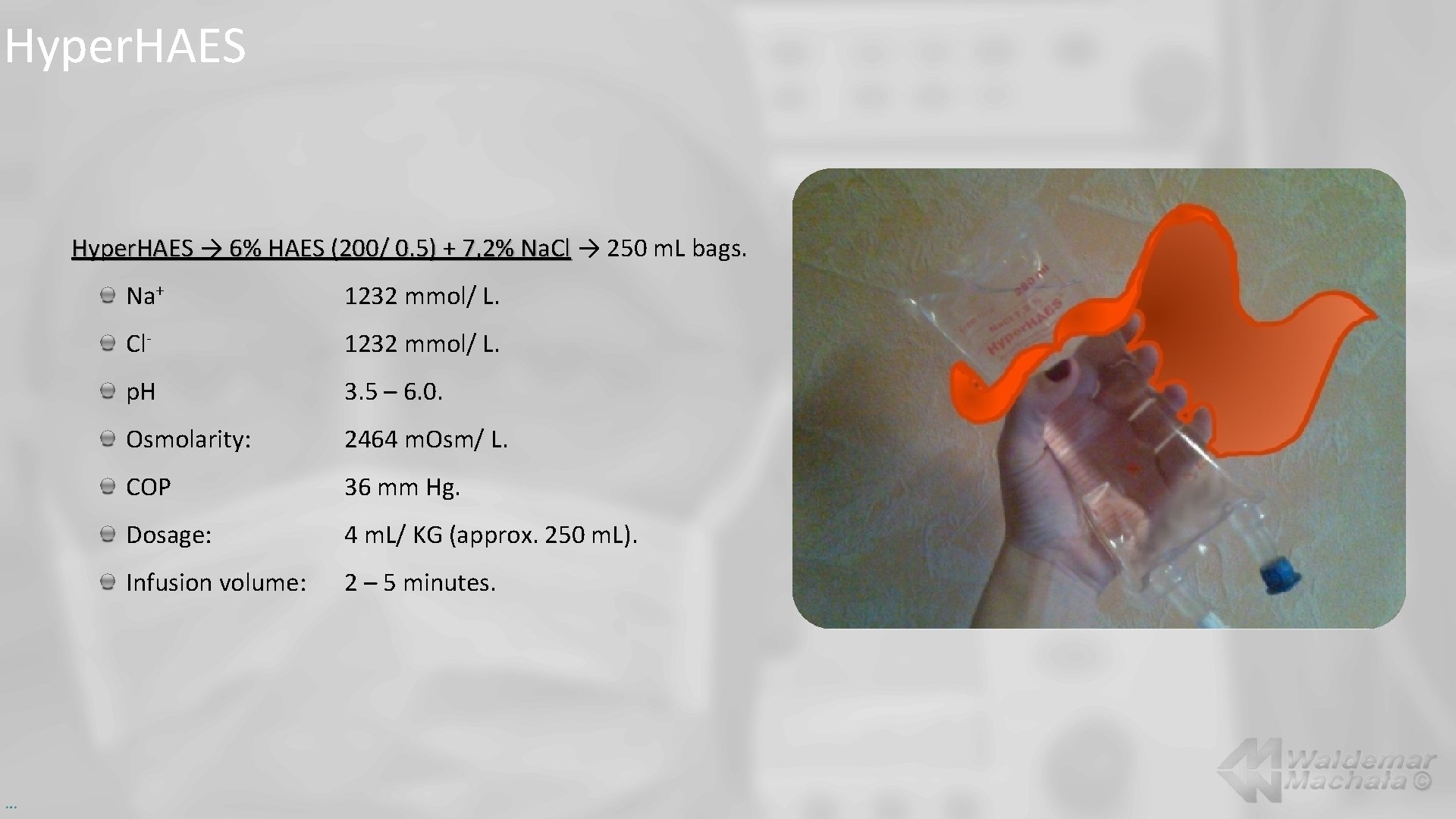
Hyper. HAES → 6% HAES (200/ 0. 5) + 7, 2% Na. Cl → 250 m. L bags. … Na+ 1232 mmol/ L. Cl- 1232 mmol/ L. p. H 3. 5 – 6. 0. Osmolarity: 2464 m. Osm/ L. COP 36 mm Hg. Dosage: 4 m. L/ KG (approx. 250 m. L). Infusion volume: 2 – 5 minutes.
Hyper. HAES - effects Hypertonic solution of Na. Cl quickly increases circulating blood volume through transferring the fluid from extravascular to intravascular space. 7. 2% Na. Cl included in the Hyper. HAES solution is responsible for inducing the mechanism of quick endogenous fluid transfer. Colloid present in the solution binds water which ensures long-lasting volume effect. Endogenous water is mobilized mainly from the area of erythrocytes and vascular endothelial cells: Circulating blood volume is rapidly increased (3 – 4 x of the transfused volume). Microcirculation flow appears through endothelial cells dehydration thus increasing oxygen supply to tissues. …
Ideal solution for fluid resuscitation: Transfusion of small volume improves perfusion. Beneficial effect on oxygen extraction in tissues: Oxygen supply. Oxygen use. Proper composition taking into account p. H measure and electrolyte composition. Sterility. Suitably long effects. Stability. Ready to use. Inexpensive. …
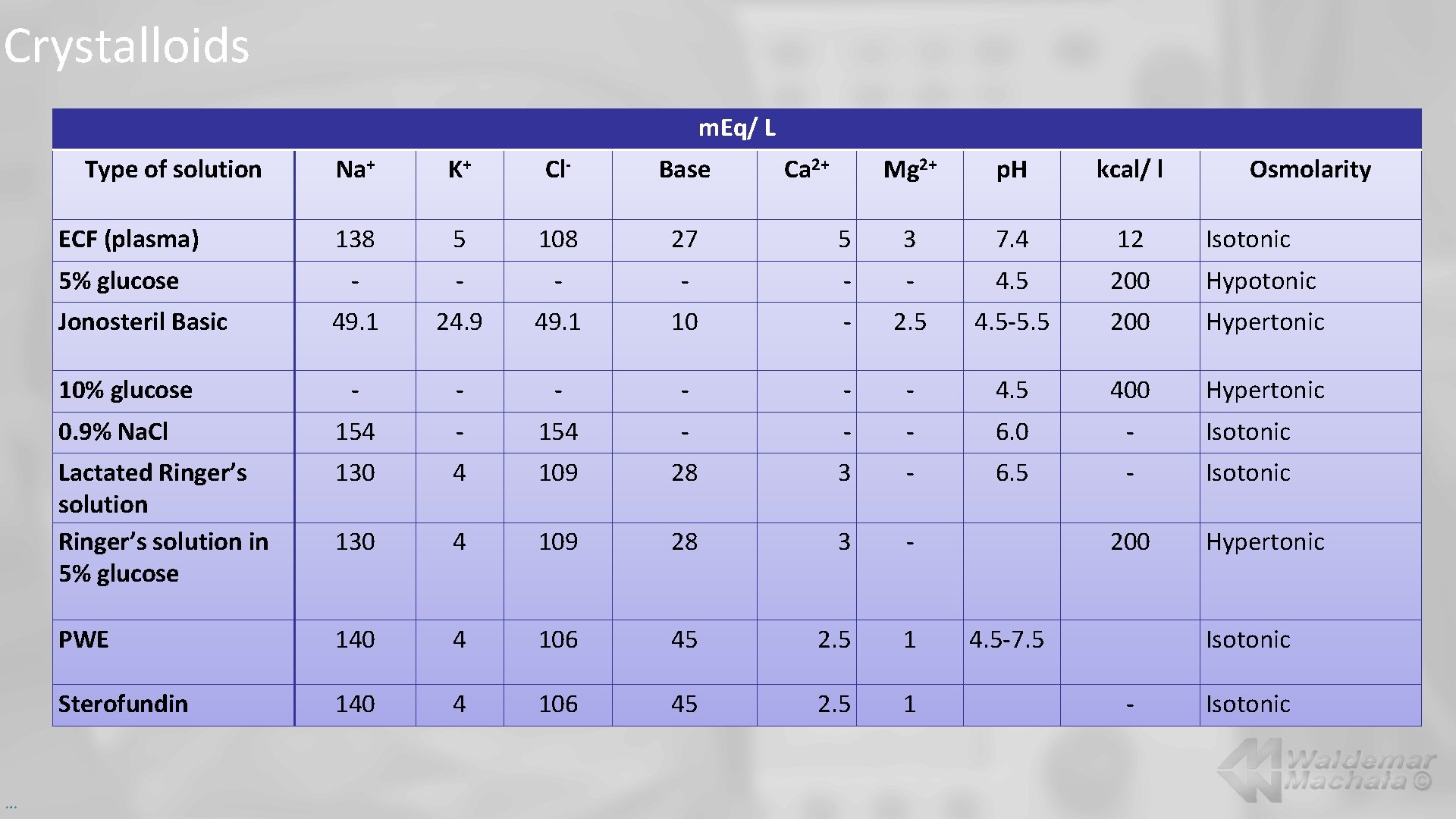
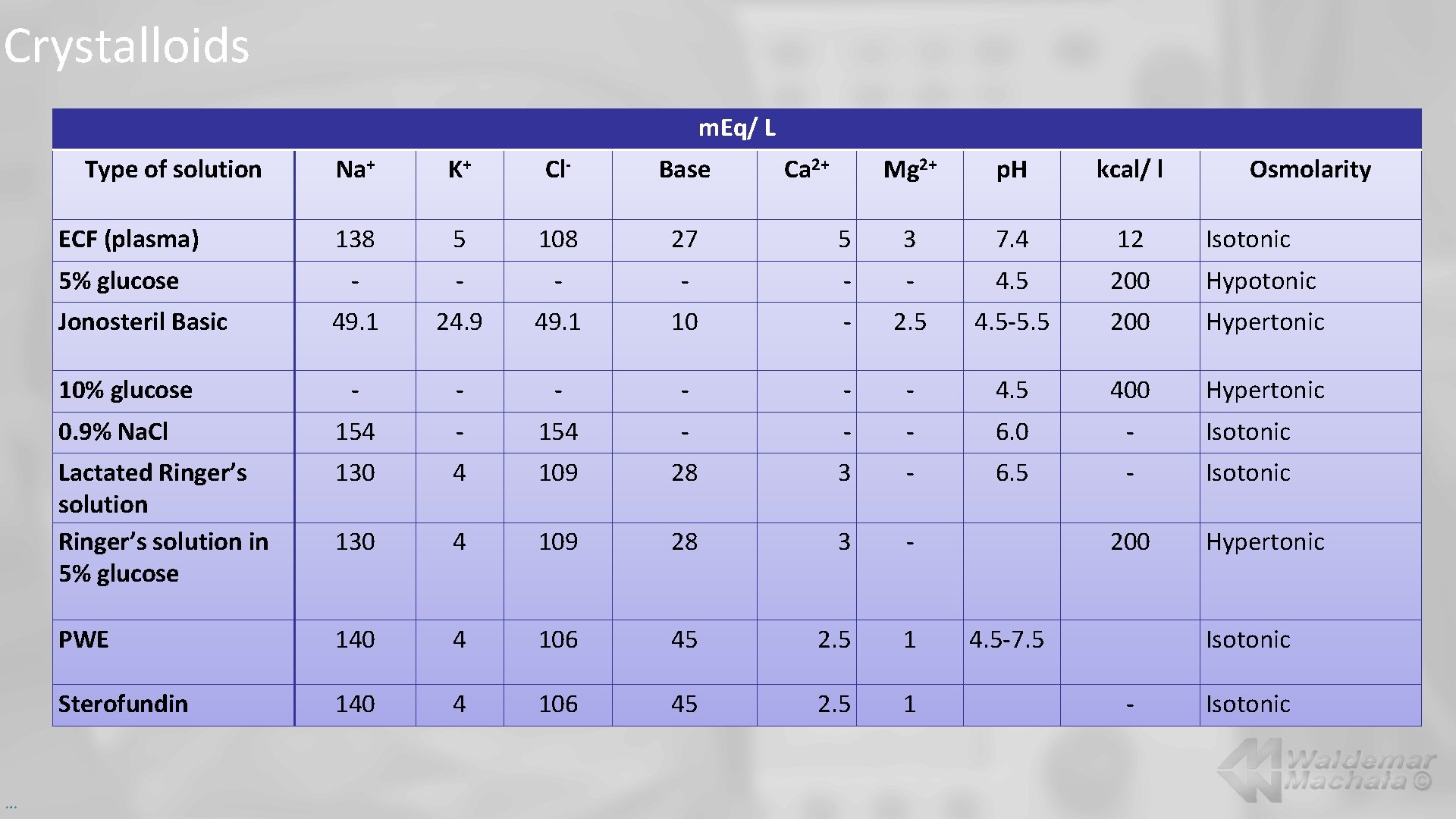
Crystalloids m. Eq/ L Type of solution Na+ K+ Cl- Base Mg 2+ p. H kcal/ l 138 5 108 27 5 3 7. 4 12 Isotonic - - - 4. 5 200 Hypotonic 49. 1 24. 9 49. 1 10 - 2. 5 4. 5 -5. 5 200 Hypertonic - - - 4. 5 400 Hypertonic 0. 9% Na. Cl 154 - - - 6. 0 - Isotonic Lactated Ringer’s solution in 5% glucose 130 4 109 28 3 - 6. 5 - Isotonic 130 4 109 28 3 - PWE 140 4 106 45 2. 5 1 Sterofundin 140 4 106 45 2. 5 1 ECF (plasma) 5% glucose Jonosteril Basic 10% glucose … Ca 2+ 200 4. 5 -7. 5 Osmolarity Hypertonic Isotonic - Isotonic
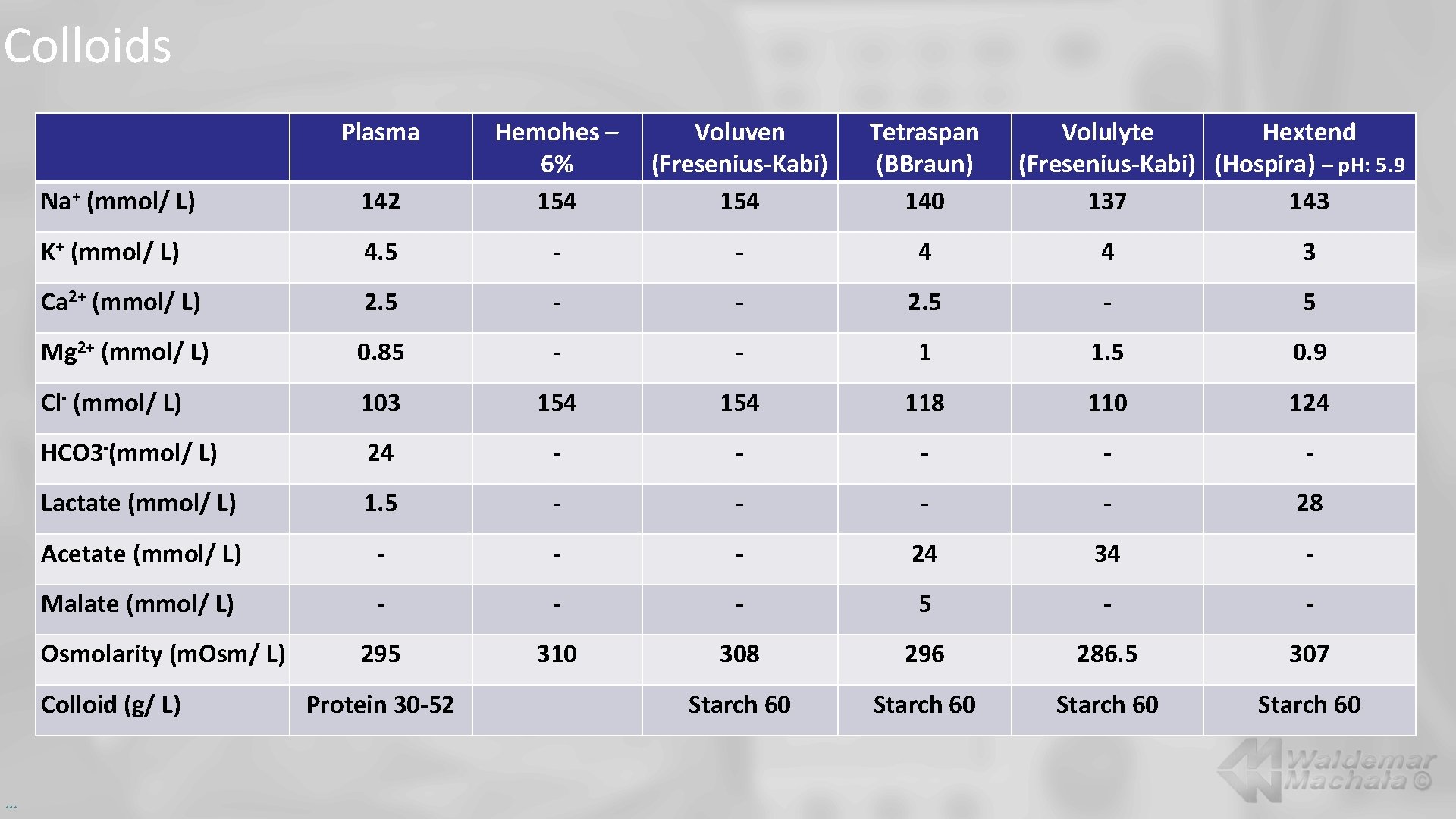
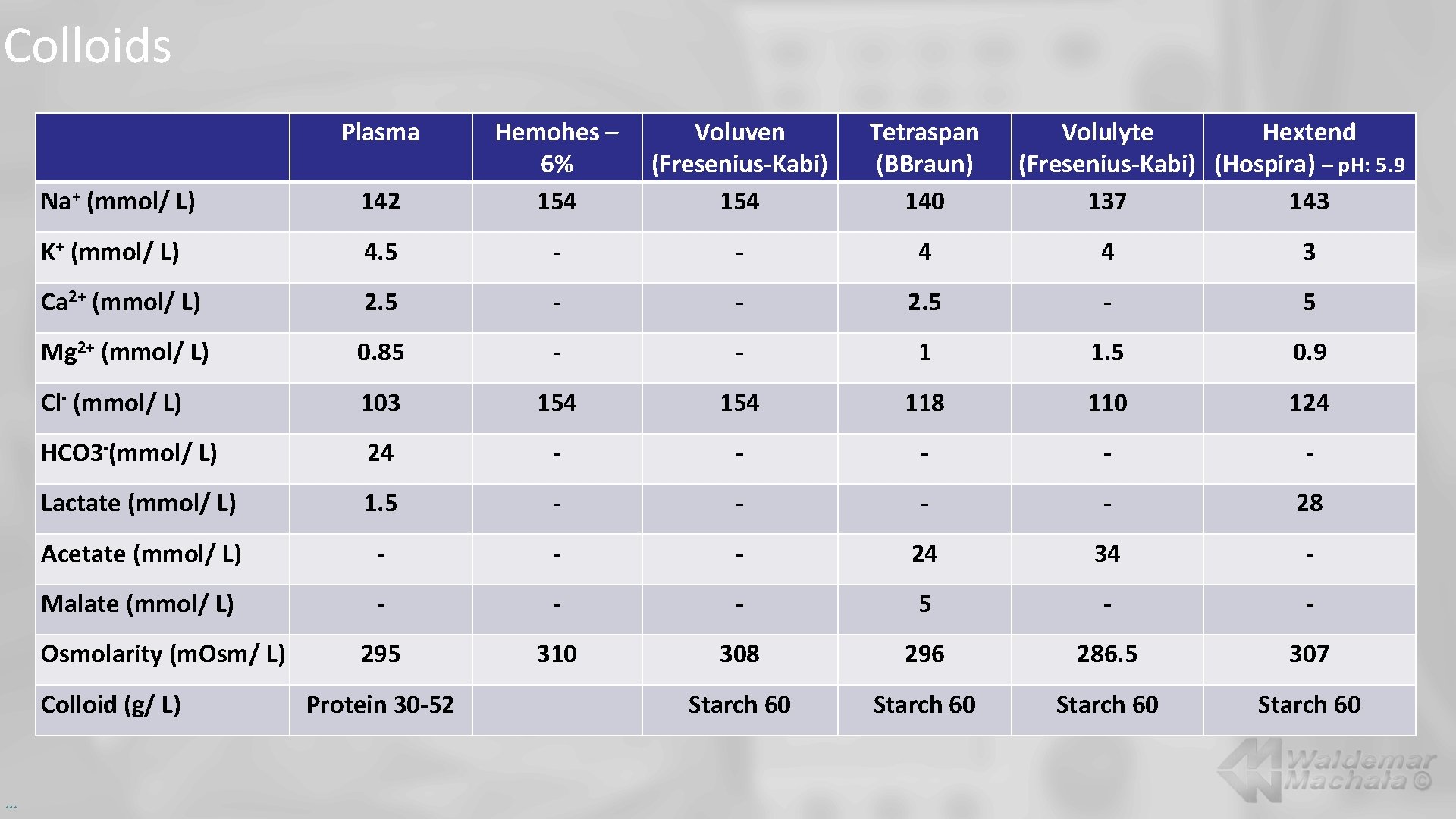
Colloids Plasma Na+ (mmol/ L) 142 Hemohes – 6% 154 K+ (mmol/ L) 4. 5 - - 4 4 3 Ca 2+ (mmol/ L) 2. 5 - - 2. 5 - 5 Mg 2+ (mmol/ L) 0. 85 - - 1 1. 5 0. 9 Cl- (mmol/ L) 103 154 118 110 124 HCO 3 -(mmol/ L) 24 - - - Lactate (mmol/ L) 1. 5 - - 28 Acetate (mmol/ L) - - - 24 34 - Malate (mmol/ L) - - - 5 - - 295 310 308 296 286. 5 307 Starch 60 Osmolarity (m. Osm/ L) Colloid (g/ L) … Protein 30 -52 Voluven (Fresenius-Kabi) 154 Tetraspan (BBraun) 140 Volulyte Hextend (Fresenius-Kabi) (Hospira) – p. H: 5. 9 137 143
![Crystalloids vs colloids volume effect Transfused volume m L Type of infusion fluid Crystalloids vs. colloids … volume effect Transfused volume [m. L] Type of infusion fluid](https://slidetodoc.com/presentation_image_h2/8fb3ae4808abe9ce56aabae6d07ffda6/image-26.jpg)
Crystalloids vs. colloids … volume effect Transfused volume [m. L] Type of infusion fluid Increase in plasma volume [m. L] 1000 5% glucose 1000 250 Lactated Ringer’s solution 7, 5% Na. Cl 1000 5% Albumins 375 100 25% Albumins 450 500 Volulyte 500
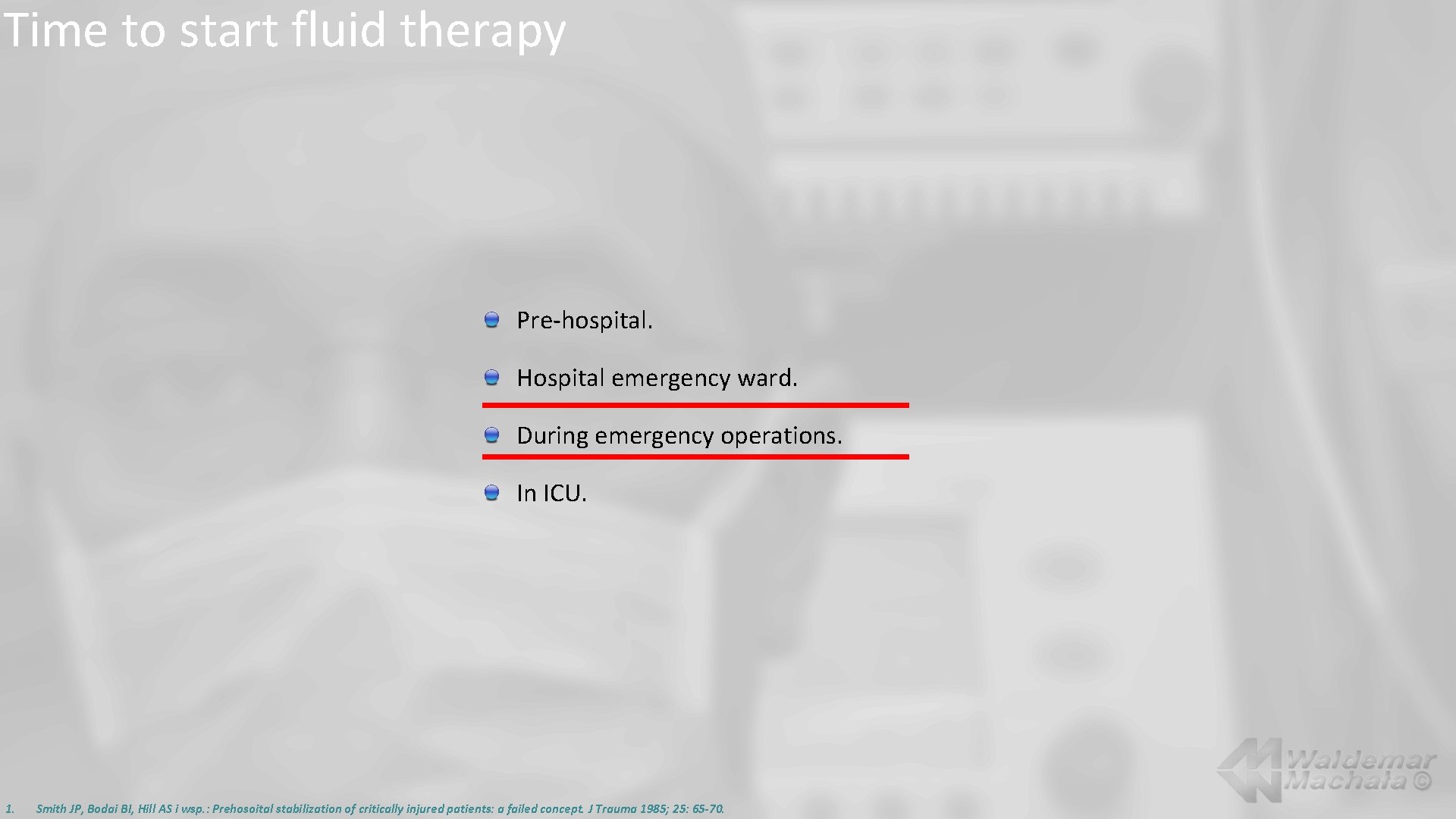
Time to start fluid therapy Pre-hospital. Hospital emergency ward. During emergency operations. In ICU. 1. Smith JP, Bodai BI, Hill AS i wsp. : Prehosoital stabilization of critically injured patients: a failed concept. J Trauma 1985; 25: 65 -70.
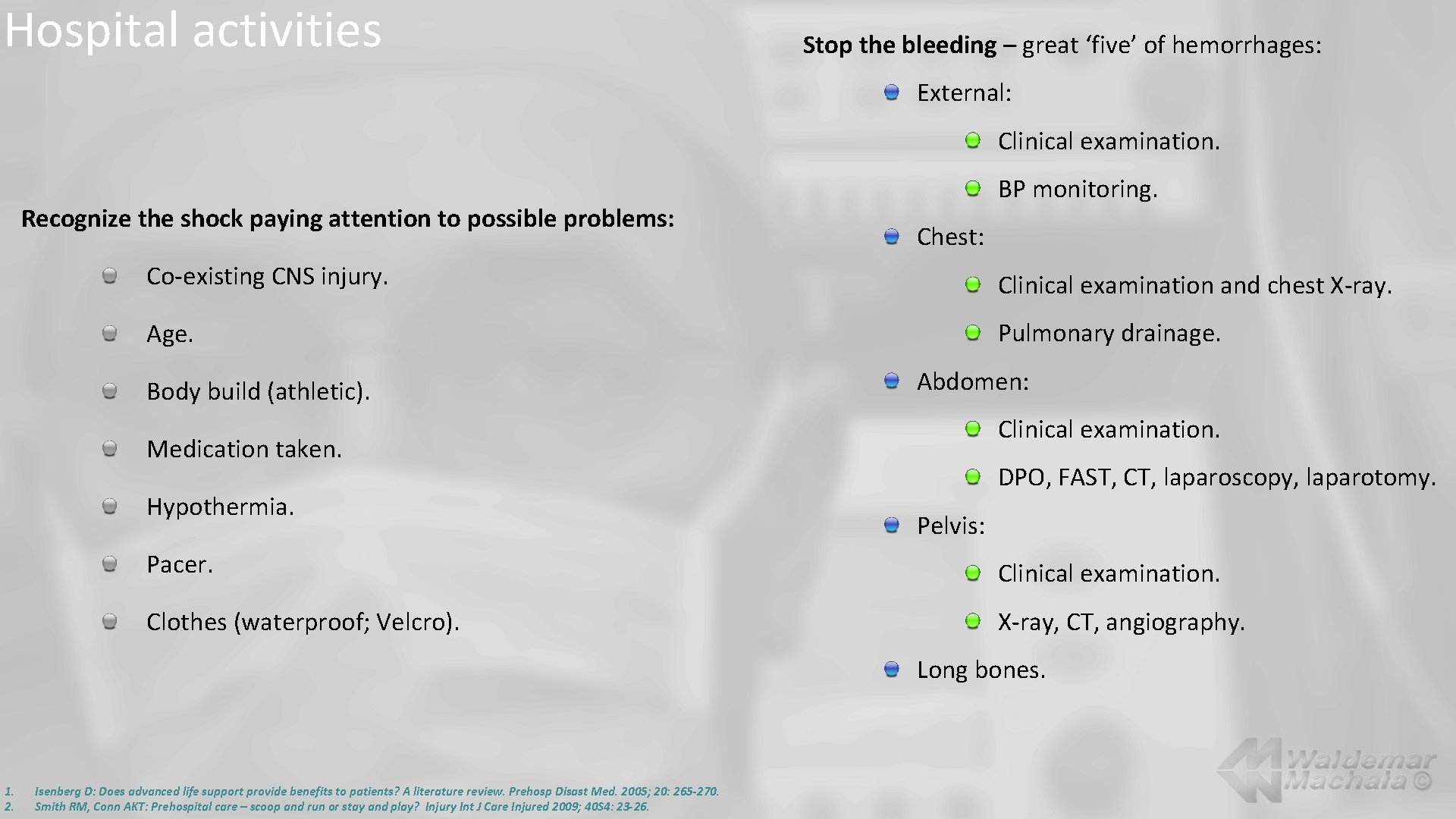
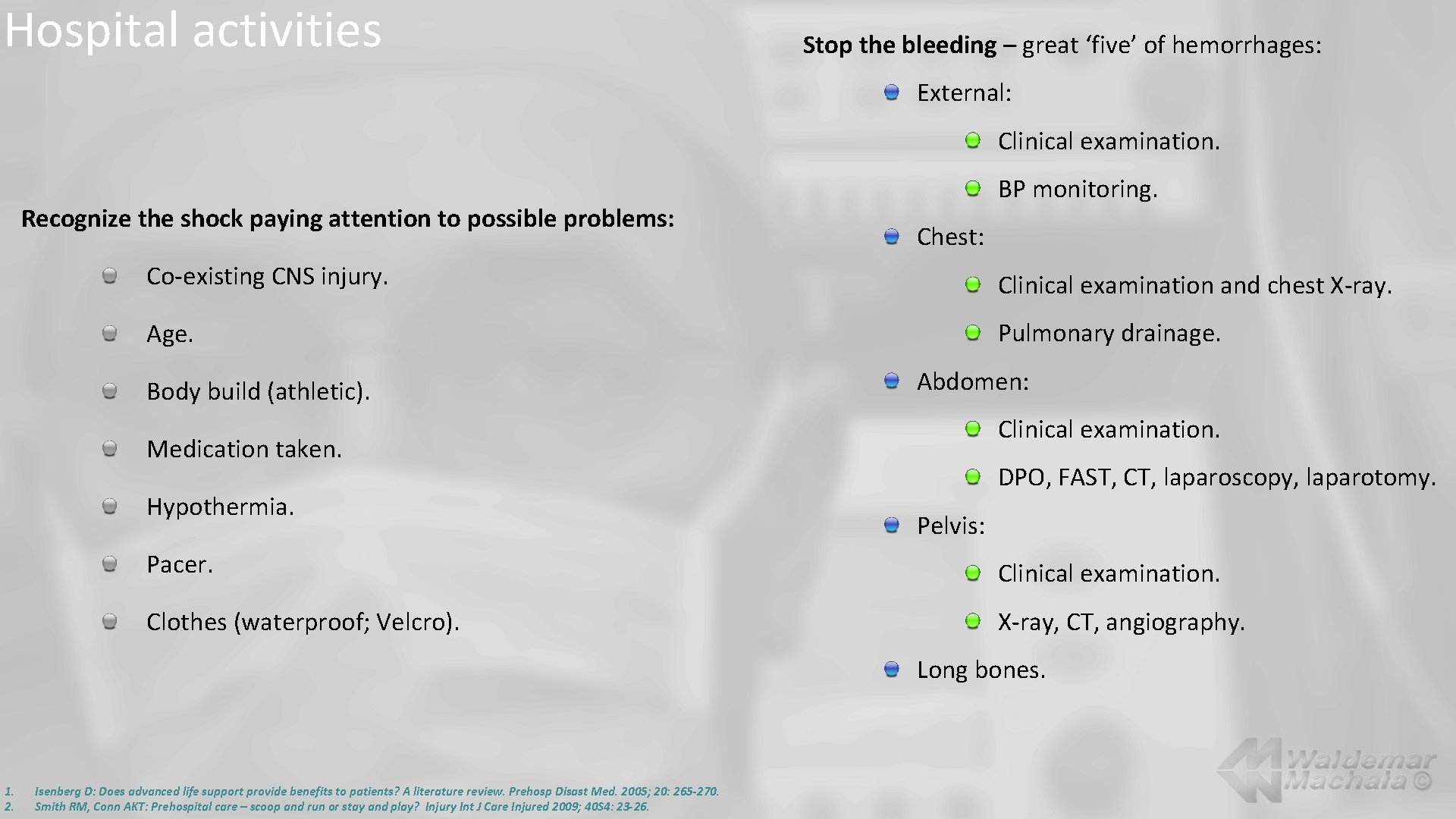
Hospital activities Stop the bleeding – great ‘five’ of hemorrhages: External: Clinical examination. Recognize the shock paying attention to possible problems: BP monitoring. Chest: Co-existing CNS injury. Clinical examination and chest X-ray. Age. Pulmonary drainage. Body build (athletic). Abdomen: Clinical examination. Medication taken. Hypothermia. DPO, FAST, CT, laparoscopy, laparotomy. Pelvis: Pacer. Clinical examination. Clothes (waterproof; Velcro). X-ray, CT, angiography. Long bones. 1. 2. Isenberg D: Does advanced life support provide benefits to patients? A literature review. Prehosp Disast Med. 2005; 20: 265 -270. Smith RM, Conn AKT: Prehospital care – scoop and run or stay and play? Injury Int J Care Injured 2009; 40 S 4: 23 -26.
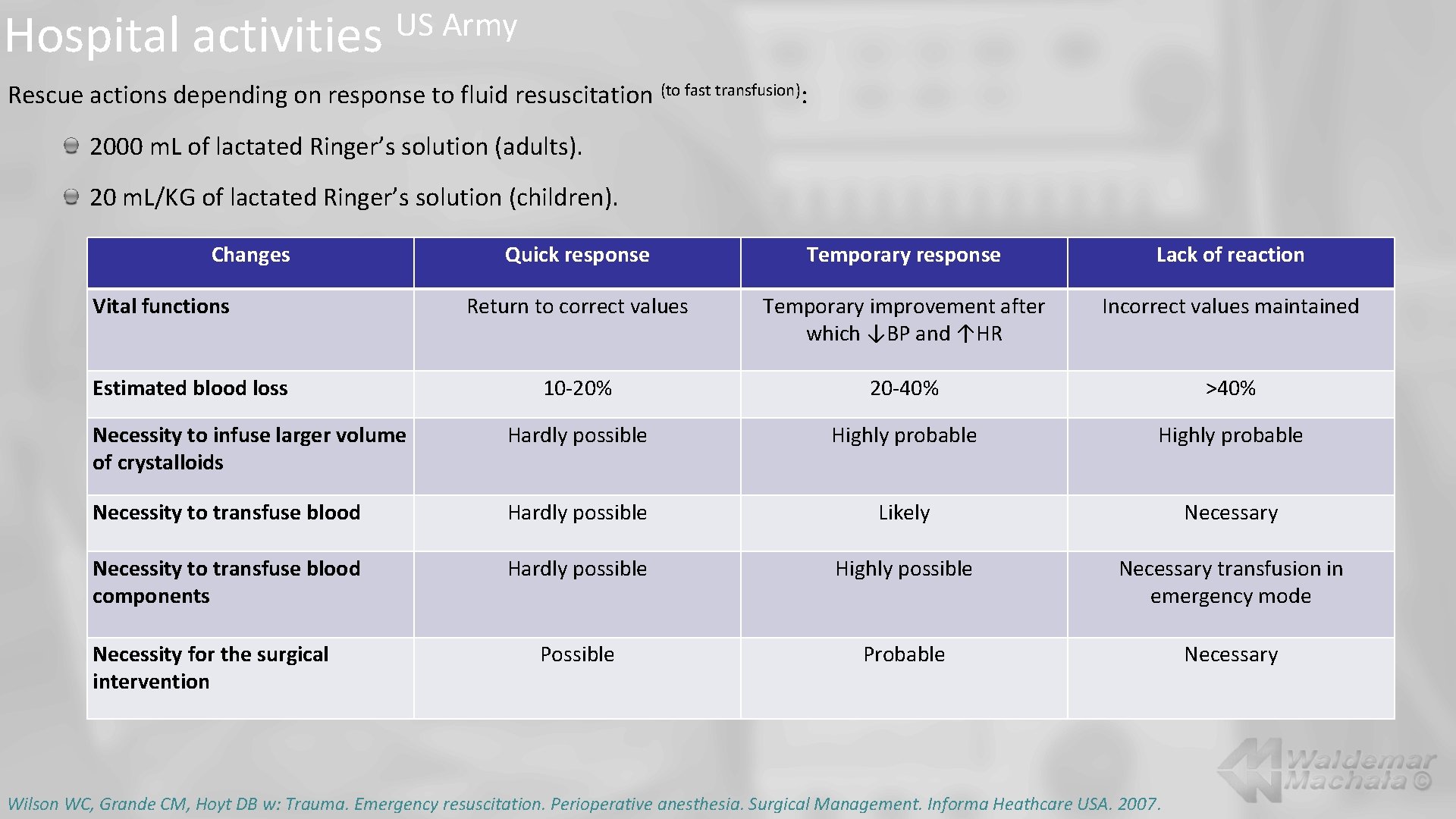
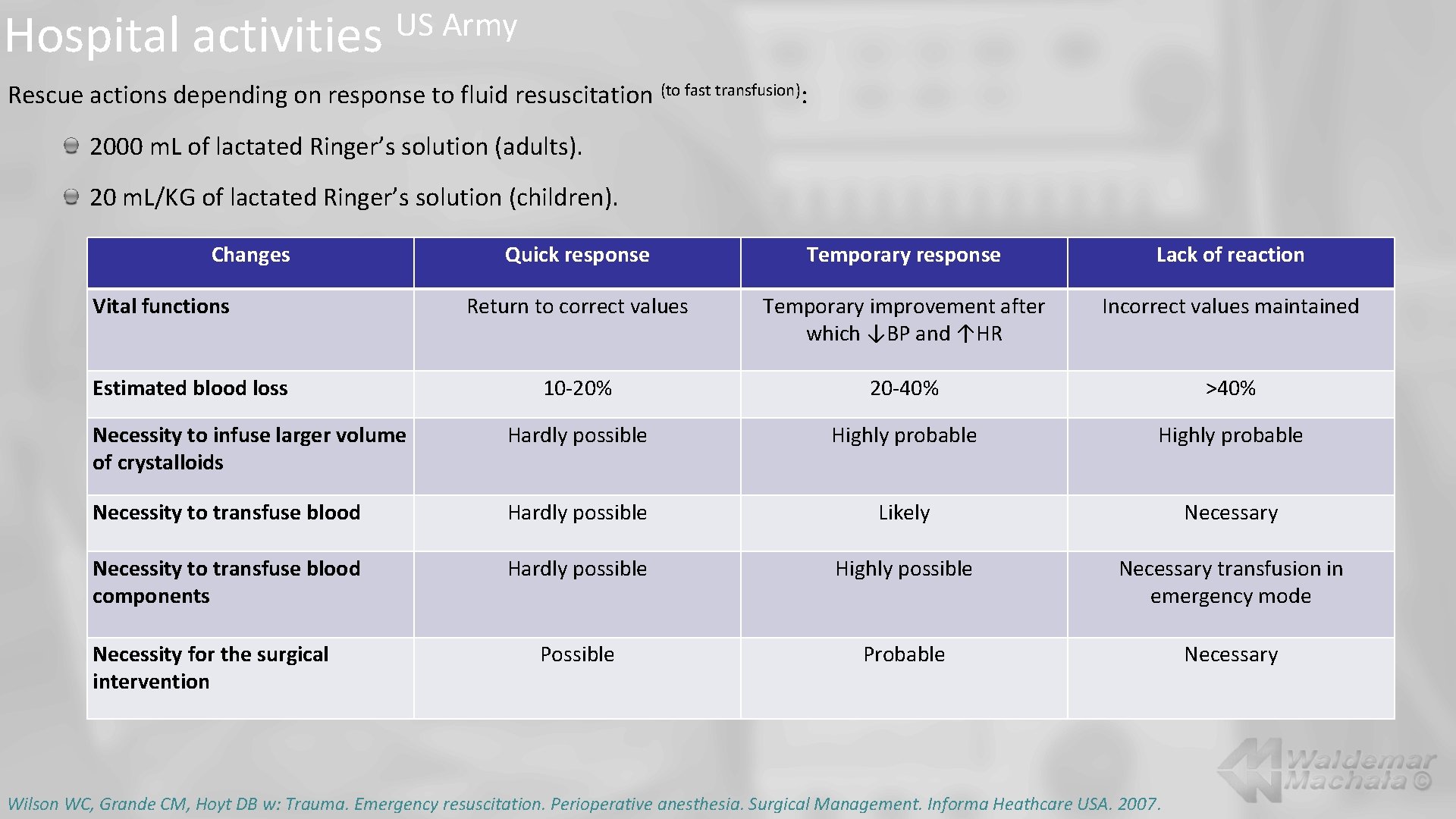
Hospital activities US Army Rescue actions depending on response to fluid resuscitation (to fast transfusion): 2000 m. L of lactated Ringer’s solution (adults). 20 m. L/KG of lactated Ringer’s solution (children). Changes Quick response Temporary response Lack of reaction Return to correct values Temporary improvement after which ↓BP and ↑HR Incorrect values maintained 10 -20% 20 -40% >40% Necessity to infuse larger volume of crystalloids Hardly possible Highly probable Necessity to transfuse blood Hardly possible Likely Necessary Necessity to transfuse blood components Hardly possible Highly possible Necessary transfusion in emergency mode Possible Probable Necessary Vital functions Estimated blood loss Necessity for the surgical intervention Wilson WC, Grande CM, Hoyt DB w: Trauma. Emergency resuscitation. Perioperative anesthesia. Surgical Management. Informa Heathcare USA. 2007.
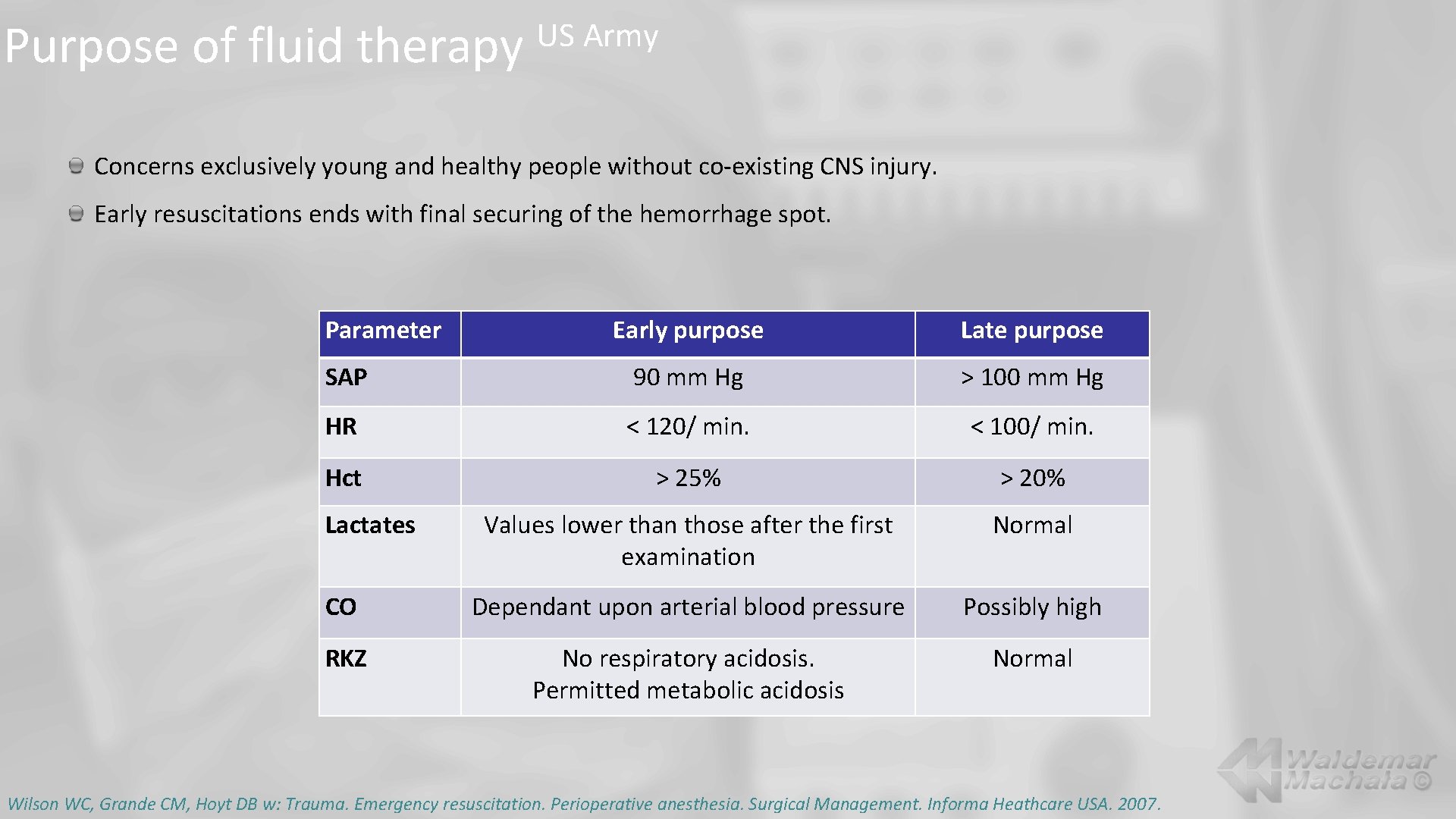
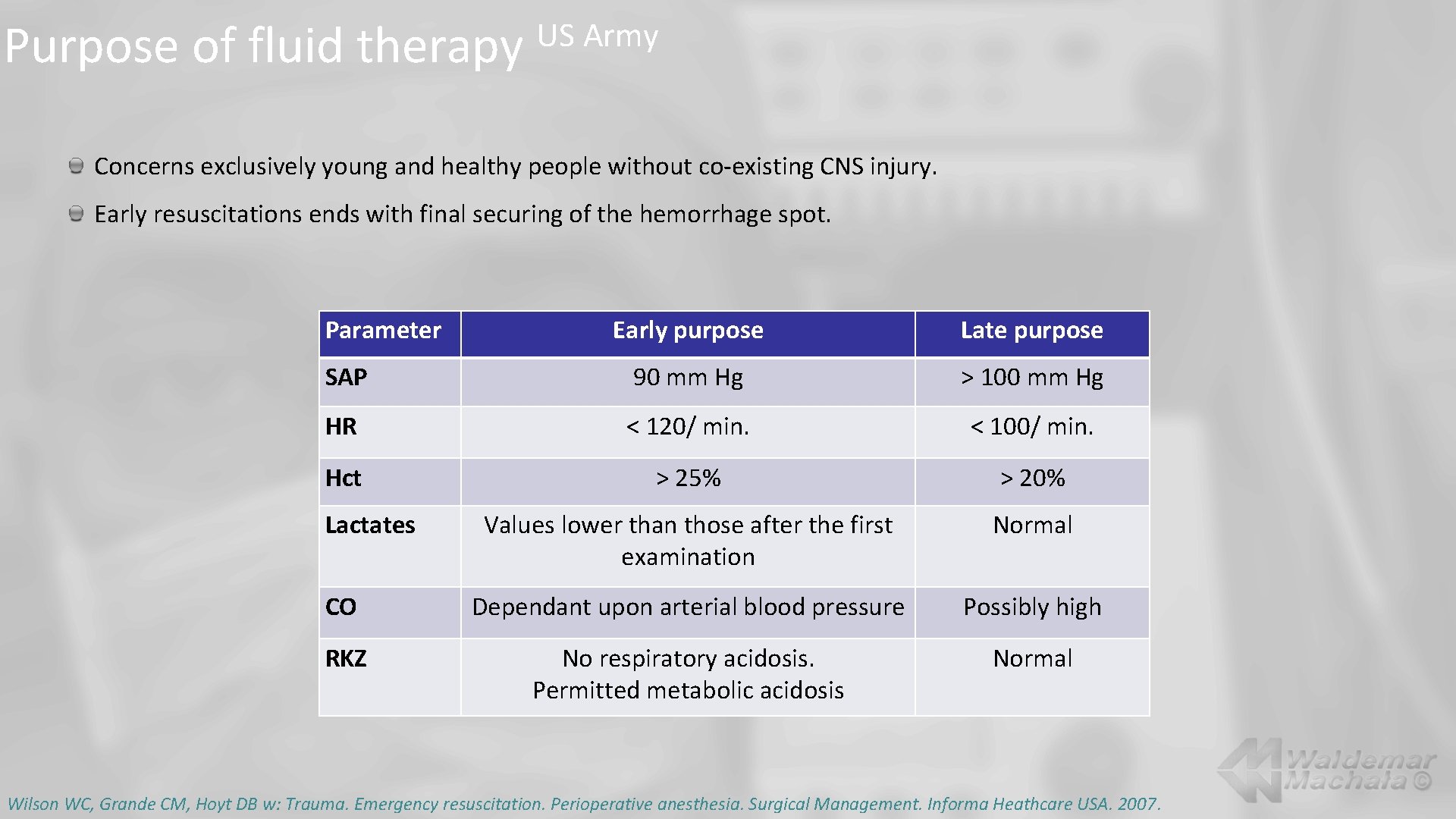
Purpose of fluid therapy US Army Concerns exclusively young and healthy people without co-existing CNS injury. Early resuscitations ends with final securing of the hemorrhage spot. Parameter Early purpose Late purpose SAP 90 mm Hg > 100 mm Hg HR < 120/ min. < 100/ min. Hct > 25% > 20% Values lower than those after the first examination Normal CO Dependant upon arterial blood pressure Possibly high RKZ No respiratory acidosis. Permitted metabolic acidosis Normal Lactates Wilson WC, Grande CM, Hoyt DB w: Trauma. Emergency resuscitation. Perioperative anesthesia. Surgical Management. Informa Heathcare USA. 2007.
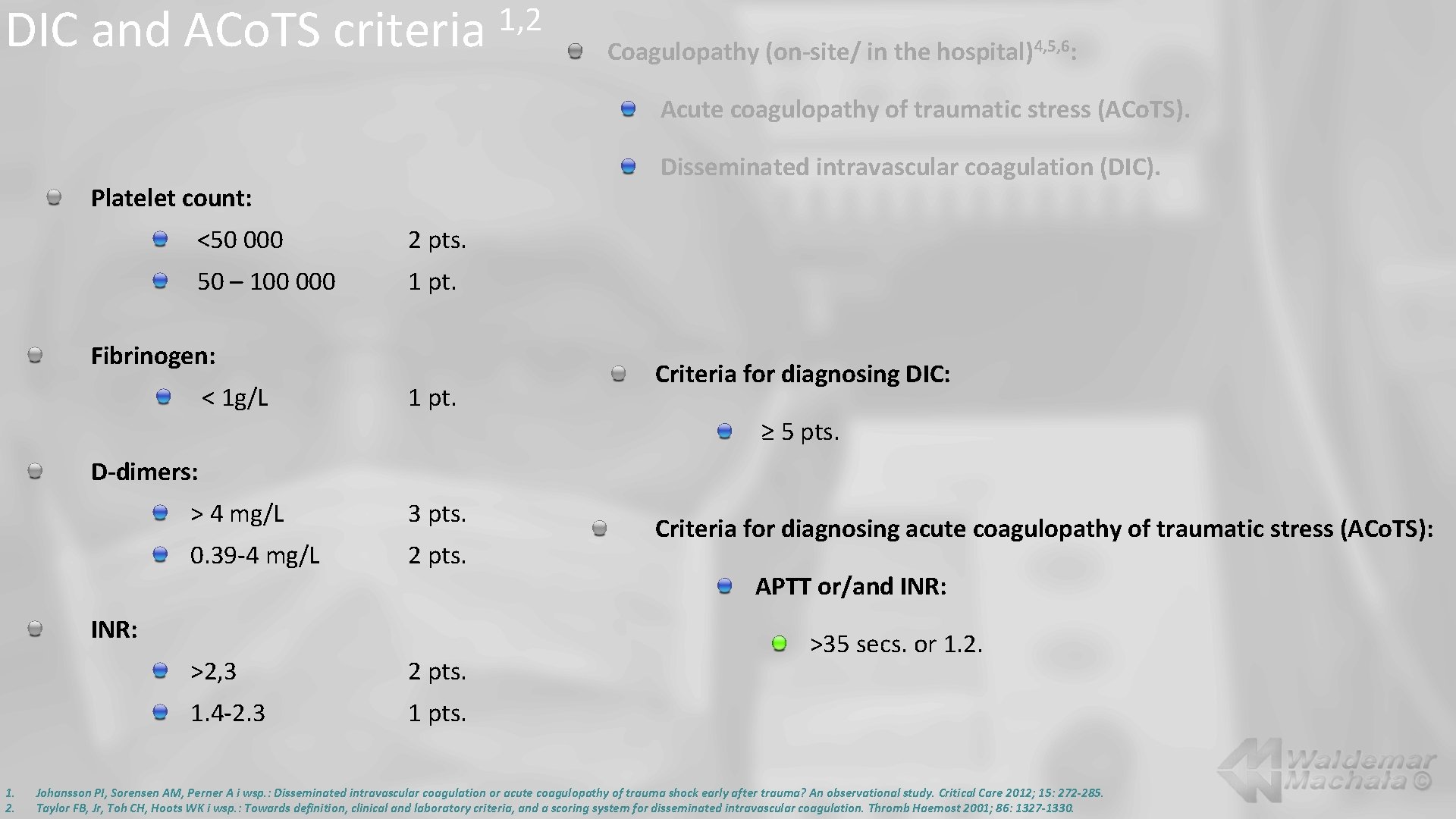
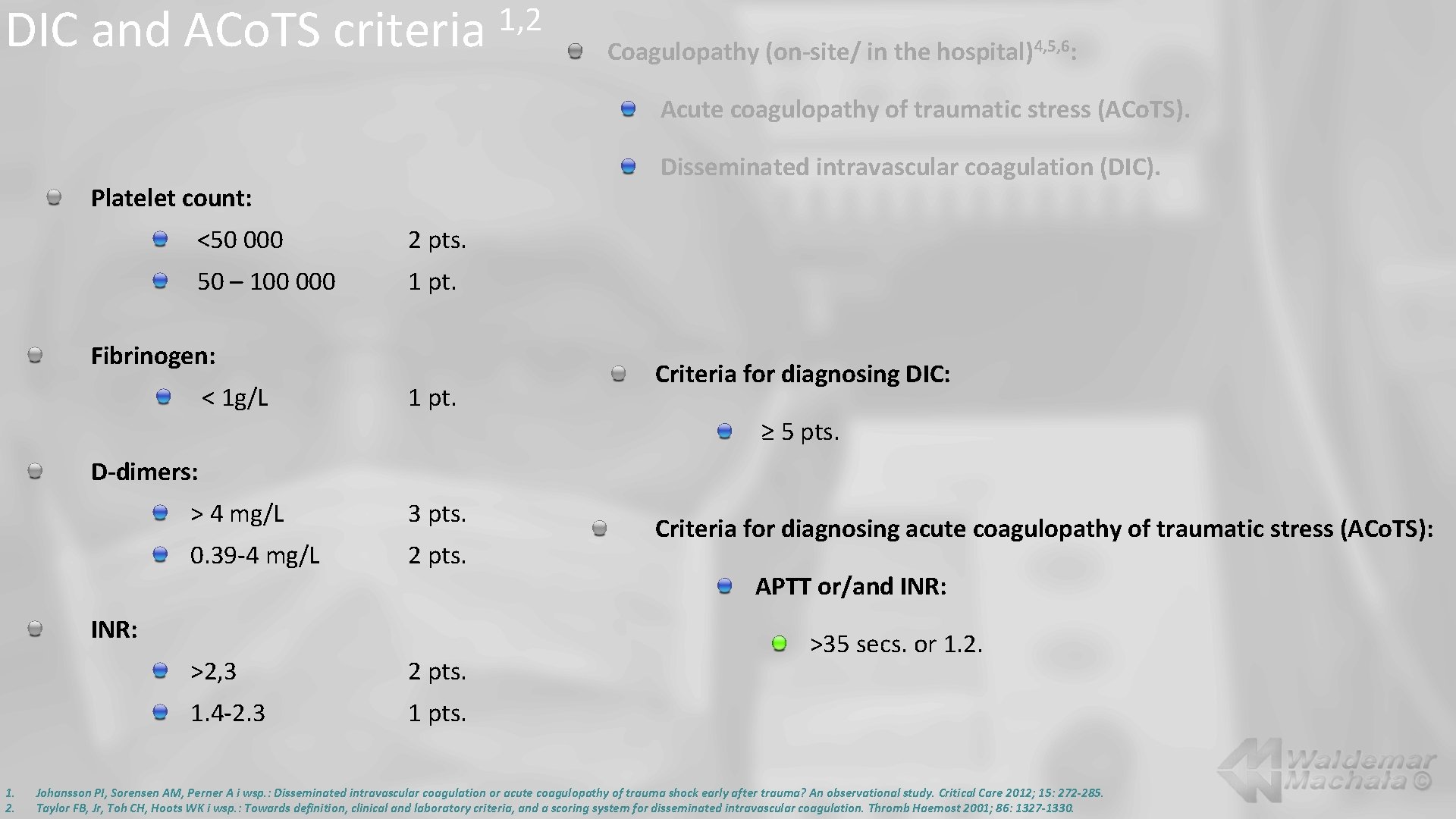
DIC and ACo. TS criteria 1, 2 Coagulopathy (on-site/ in the hospital)4, 5, 6: Acute coagulopathy of traumatic stress (ACo. TS). Disseminated intravascular coagulation (DIC). Platelet count: <50 000 2 pts. 50 – 100 000 1 pt. Fibrinogen: < 1 g/L 1 pt. Criteria for diagnosing DIC: ≥ 5 pts. D-dimers: > 4 mg/L 3 pts. 0. 39 -4 mg/L 2 pts. INR: 1. 2. >2, 3 2 pts. 1. 4 -2. 3 1 pts. Criteria for diagnosing acute coagulopathy of traumatic stress (ACo. TS): APTT or/and INR: >35 secs. or 1. 2. Johansson PI, Sorensen AM, Perner A i wsp. : Disseminated intravascular coagulation or acute coagulopathy of trauma shock early after trauma? An observational study. Critical Care 2012; 15: 272 -285. Taylor FB, Jr, Toh CH, Hoots WK i wsp. : Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost 2001; 86: 1327 -1330.
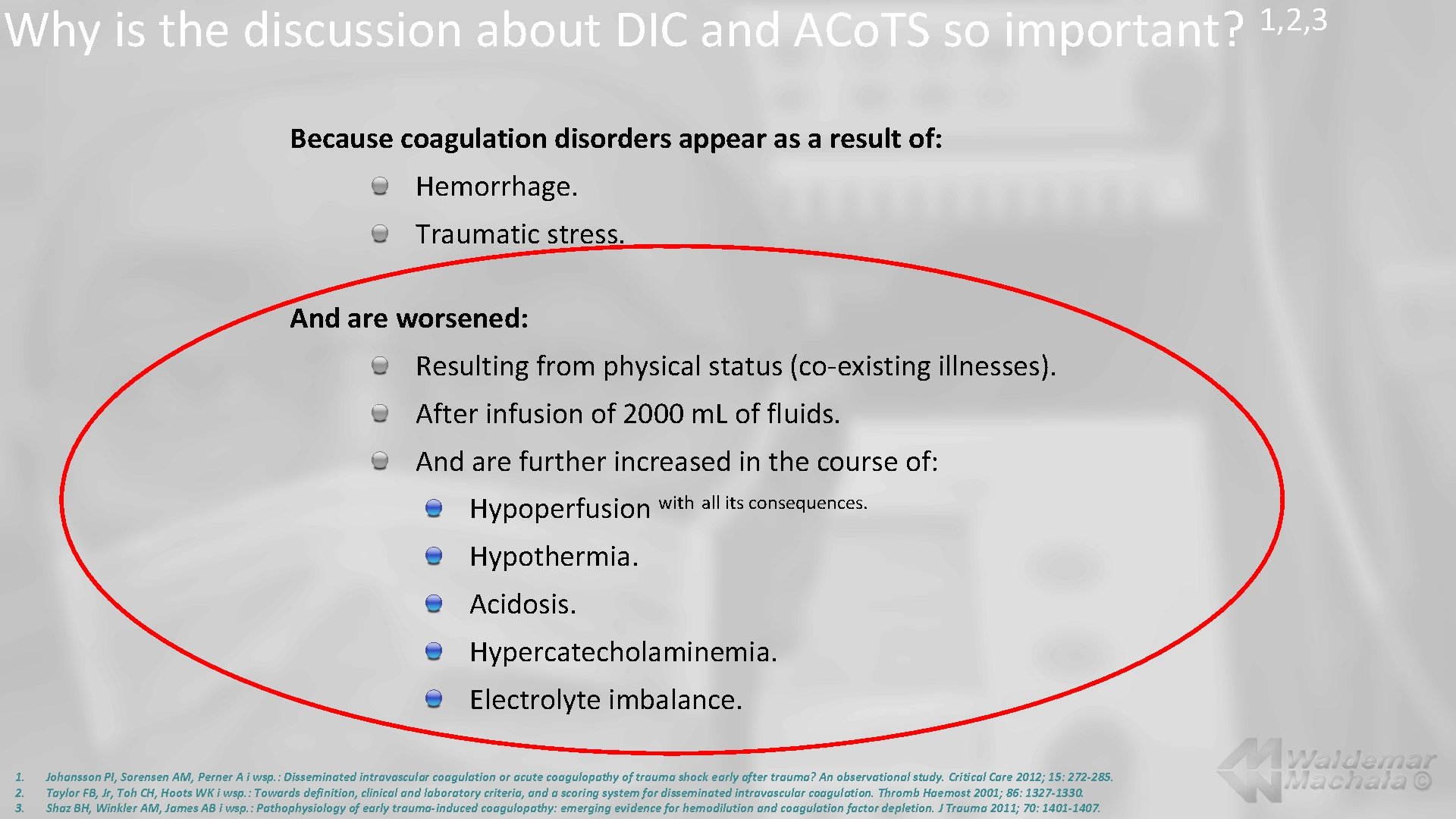
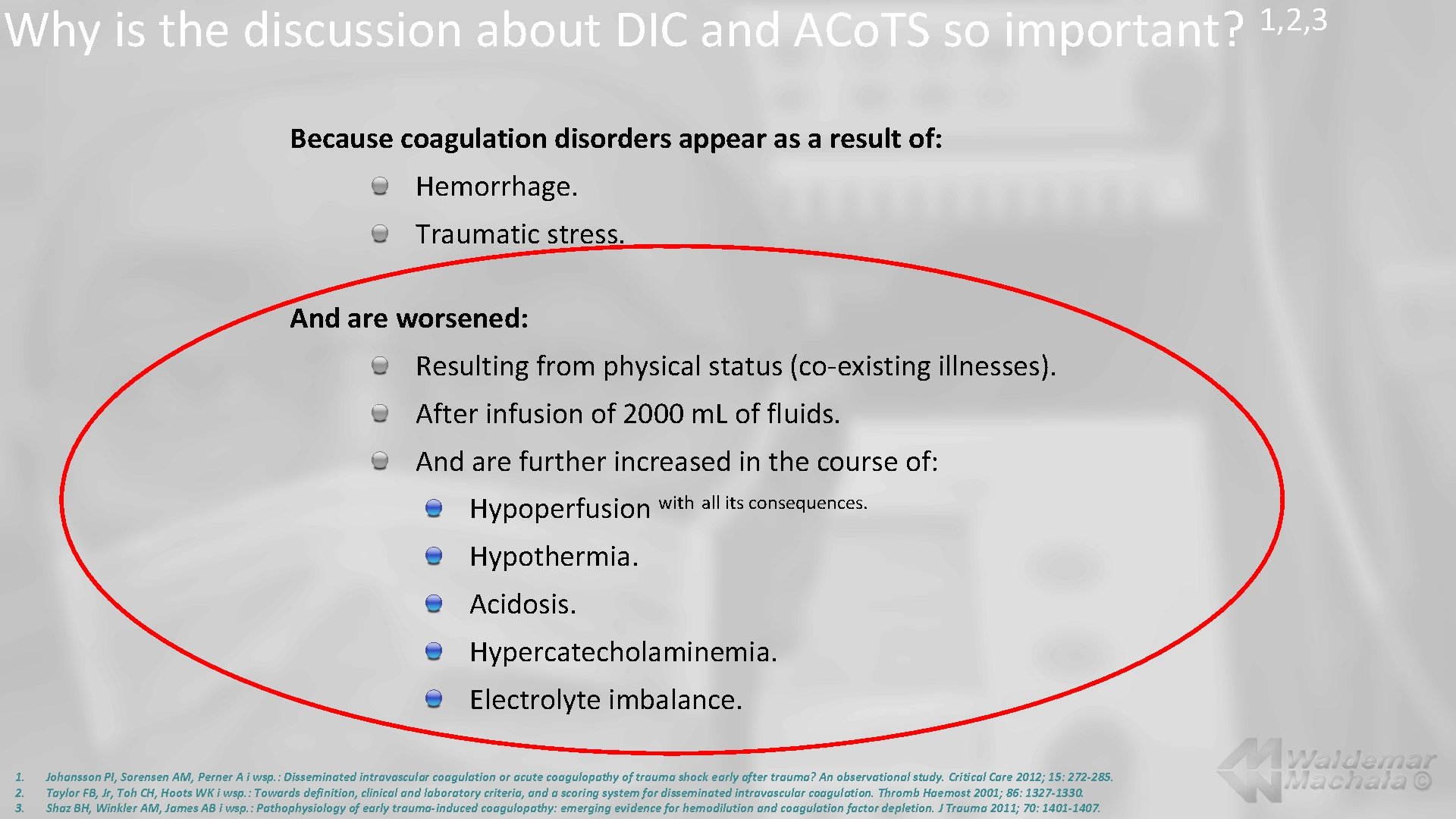
Why is the discussion about DIC and ACo. TS so important? Because coagulation disorders appear as a result of: Hemorrhage. Traumatic stress. And are worsened: Resulting from physical status (co-existing illnesses). After infusion of 2000 m. L of fluids. And are further increased in the course of: Hypoperfusion with all its consequences. Hypothermia. Acidosis. Hypercatecholaminemia. Electrolyte imbalance. 1. 2. 3. Johansson PI, Sorensen AM, Perner A i wsp. : Disseminated intravascular coagulation or acute coagulopathy of trauma shock early after trauma? An observational study. Critical Care 2012; 15: 272 -285. Taylor FB, Jr, Toh CH, Hoots WK i wsp. : Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost 2001; 86: 1327 -1330. Shaz BH, Winkler AM, James AB i wsp. : Pathophysiology of early trauma-induced coagulopathy: emerging evidence for hemodilution and coagulation factor depletion. J Trauma 2011; 70: 1401 -1407. 1, 2, 3
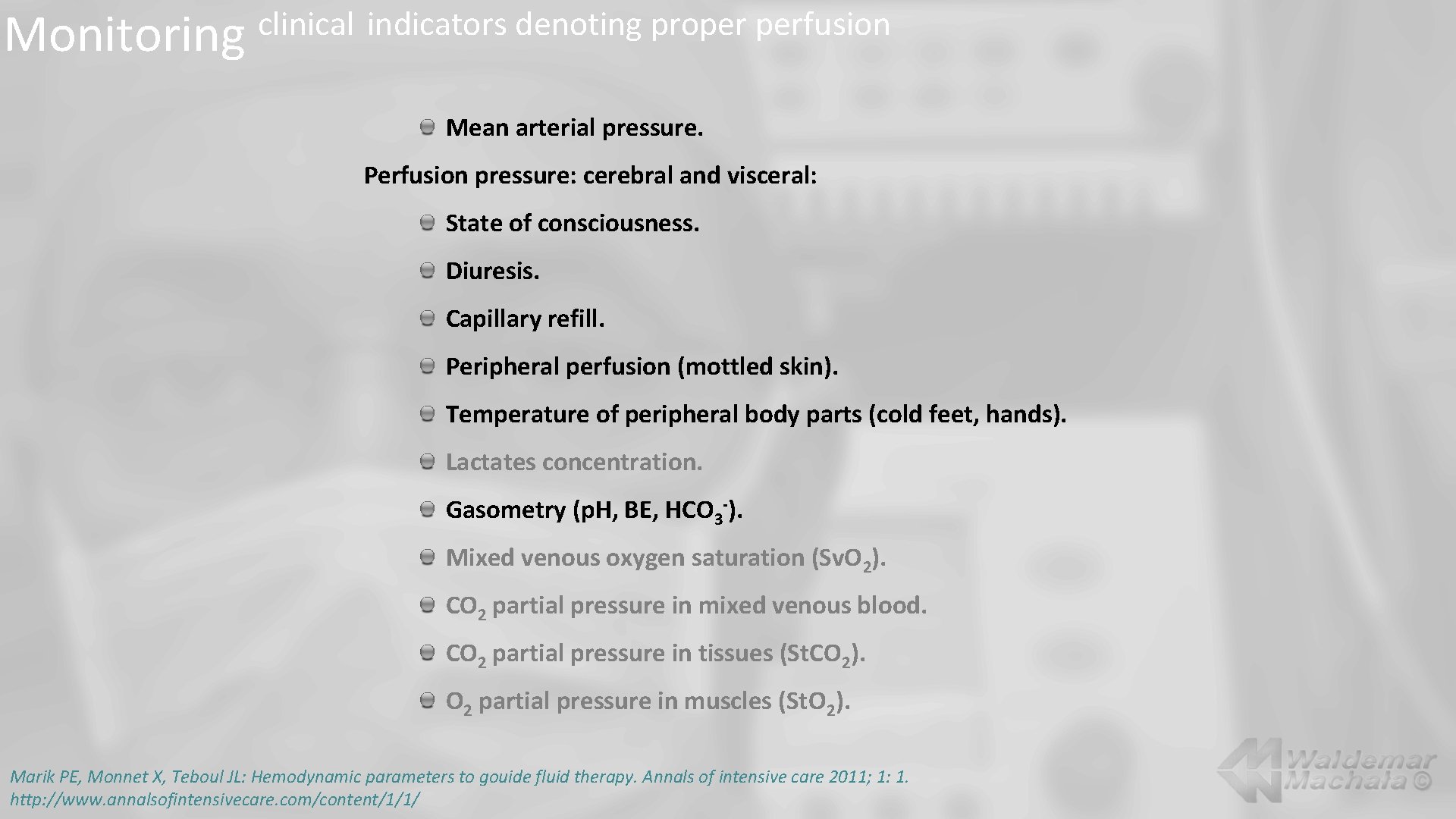
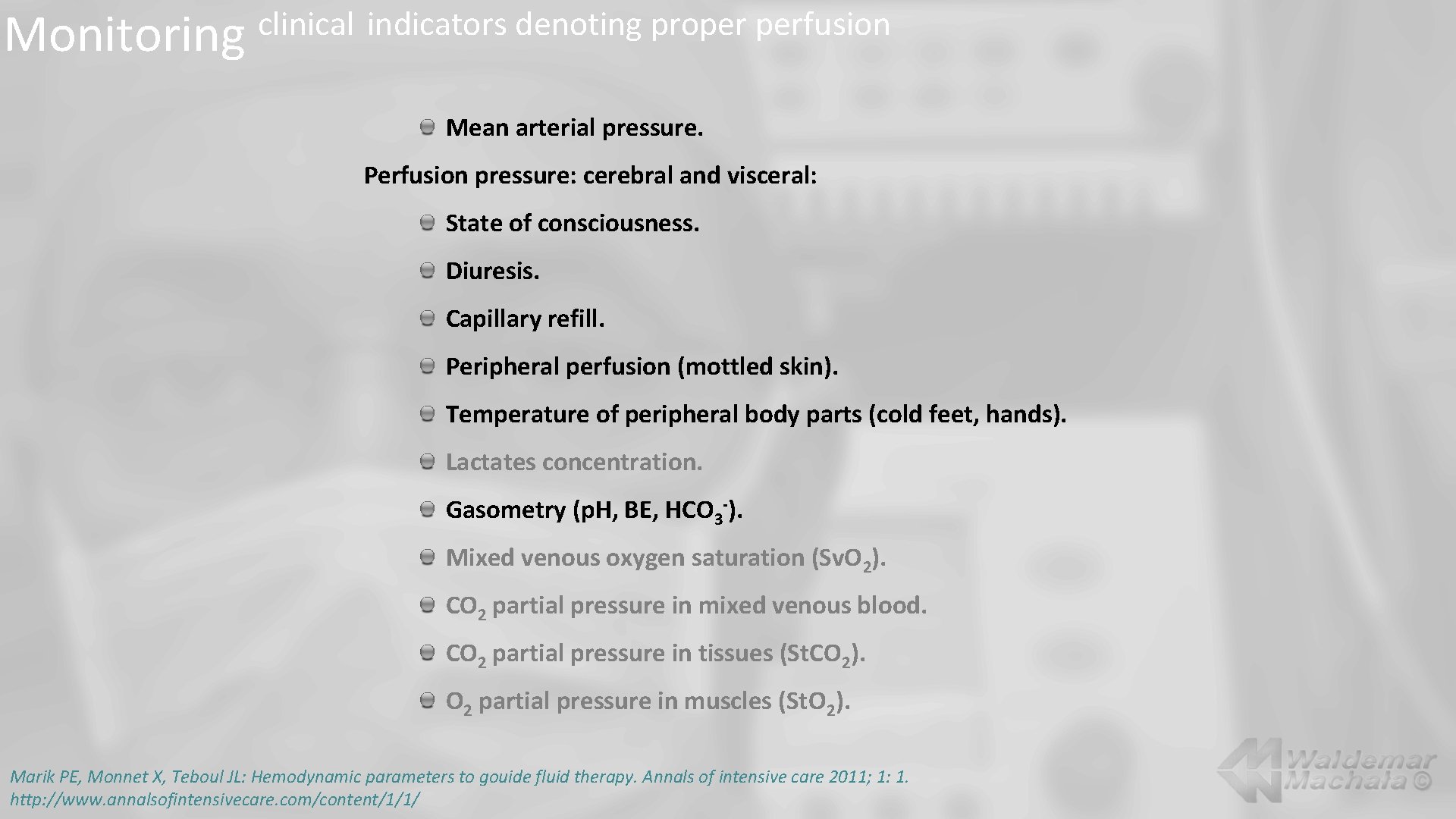
Monitoring clinical indicators denoting proper perfusion Mean arterial pressure. Perfusion pressure: cerebral and visceral: State of consciousness. Diuresis. Capillary refill. Peripheral perfusion (mottled skin). Temperature of peripheral body parts (cold feet, hands). Lactates concentration. Gasometry (p. H, BE, HCO 3 -). Mixed venous oxygen saturation (Sv. O 2). CO 2 partial pressure in mixed venous blood. CO 2 partial pressure in tissues (St. CO 2). O 2 partial pressure in muscles (St. O 2). Marik PE, Monnet X, Teboul JL: Hemodynamic parameters to gouide fluid therapy. Annals of intensive care 2011; 1: 1. http: //www. annalsofintensivecare. com/content/1/1/
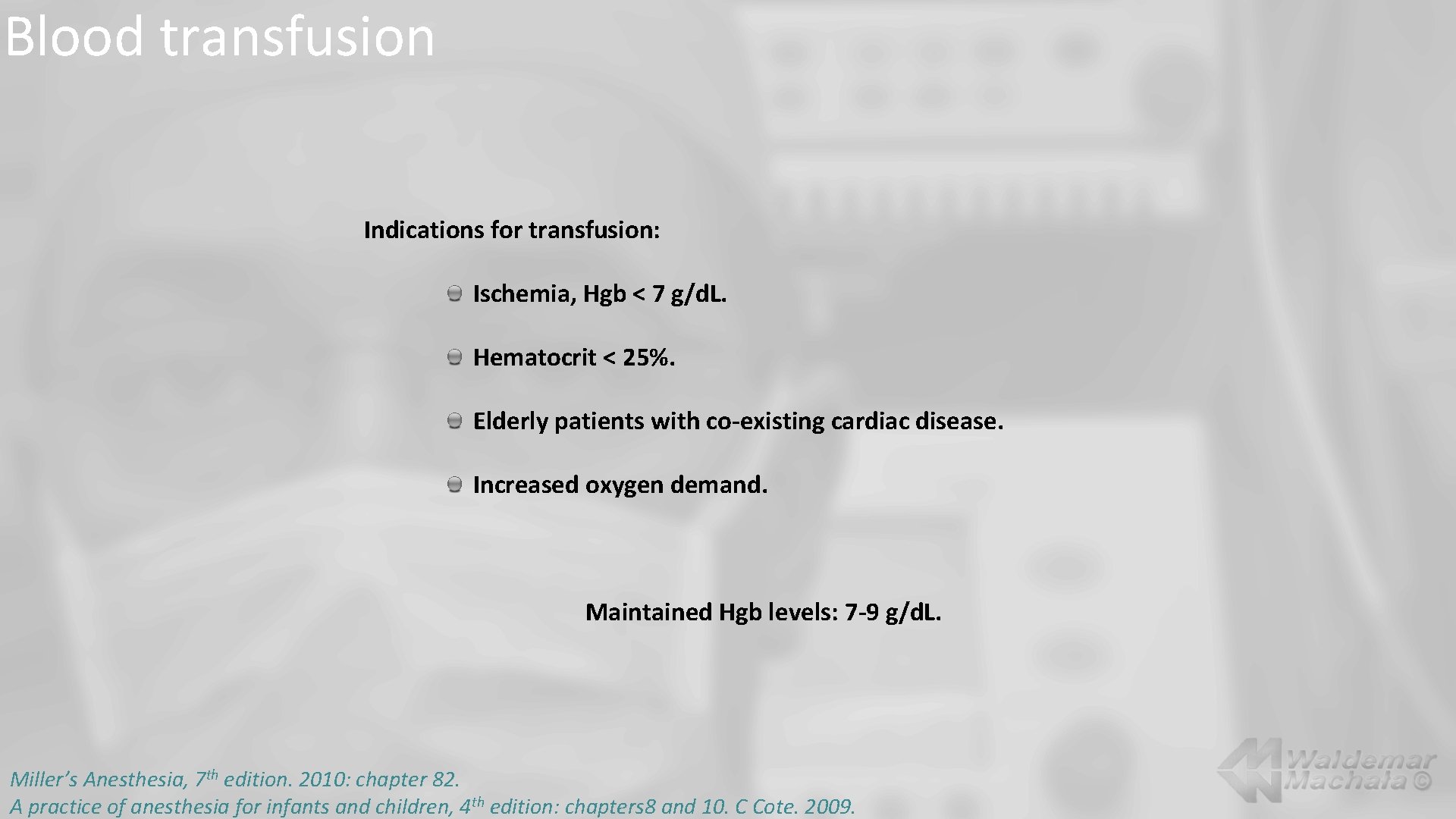
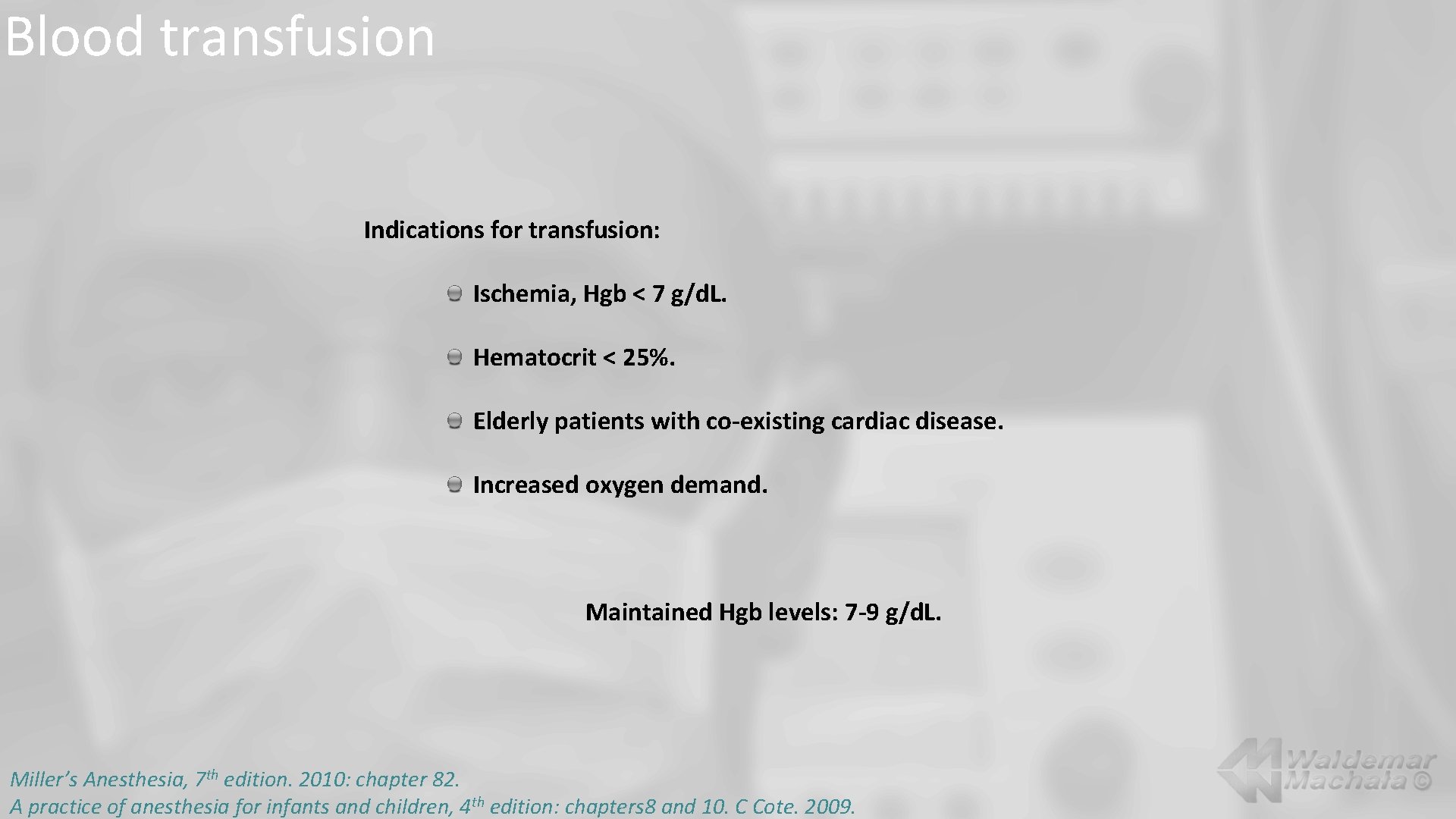
Blood transfusion Indications for transfusion: Ischemia, Hgb < 7 g/d. L. Hematocrit < 25%. Elderly patients with co-existing cardiac disease. Increased oxygen demand. Maintained Hgb levels: 7 -9 g/d. L. Miller’s Anesthesia, 7 th edition. 2010: chapter 82. A practice of anesthesia for infants and children, 4 th edition: chapters 8 and 10. C Cote. 2009.
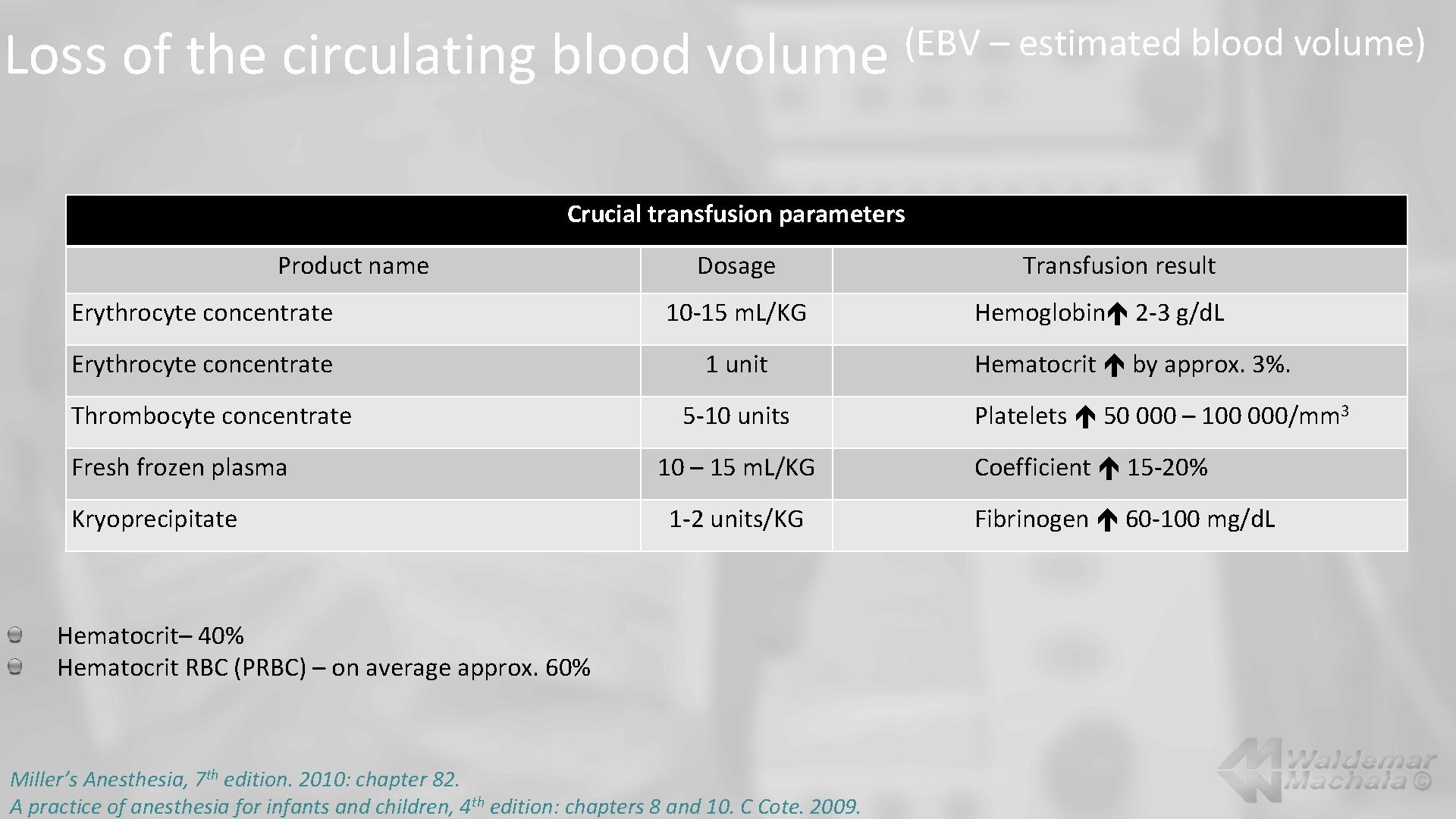
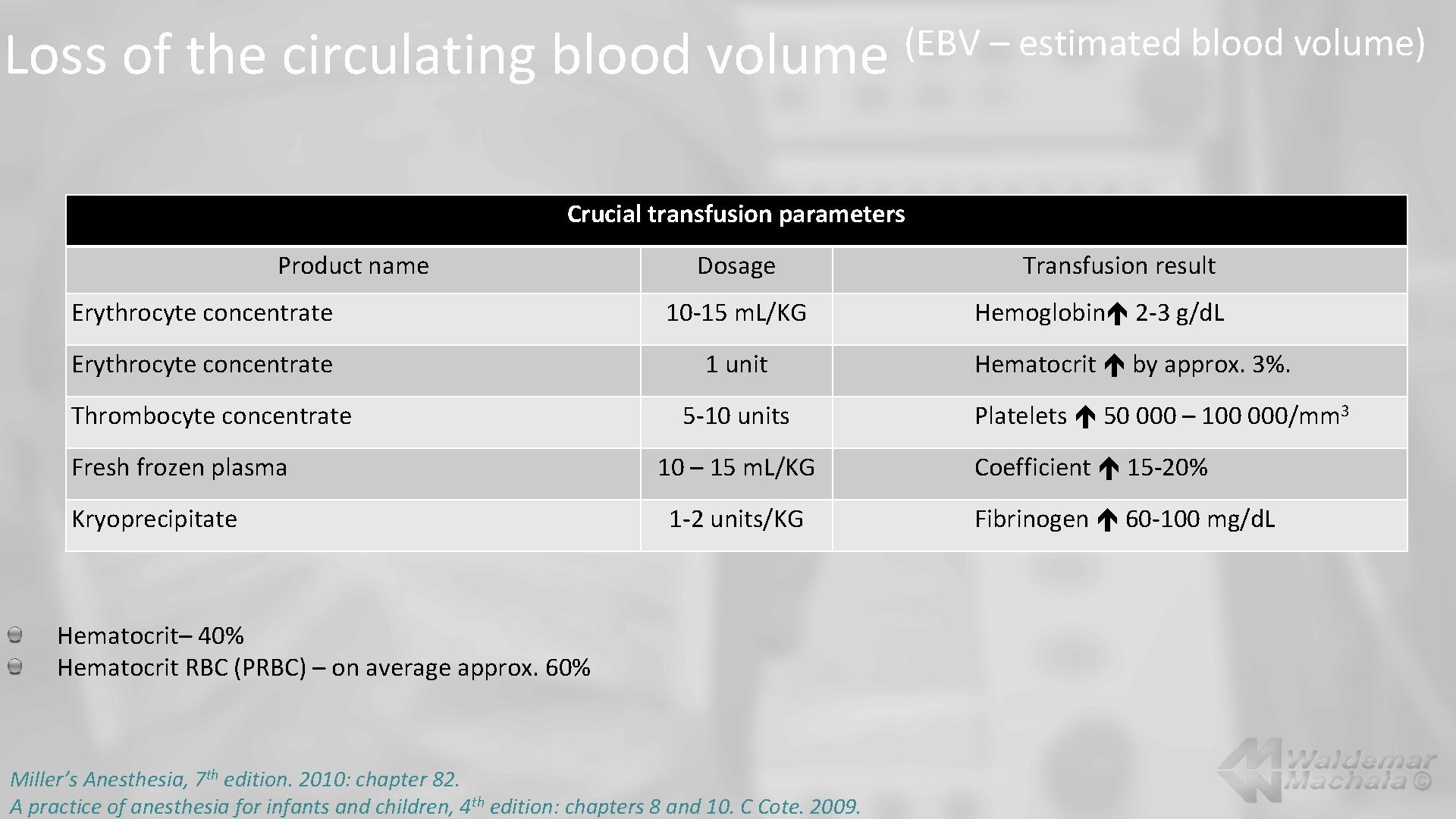
Loss of the circulating blood volume (EBV – estimated blood volume) Crucial transfusion parameters Product name Dosage Erythrocyte concentrate 10 -15 m. L/KG Erythrocyte concentrate 1 unit Thrombocyte concentrate Fresh frozen plasma Kryoprecipitate 5 -10 units 10 – 15 m. L/KG 1 -2 units/KG Hematocrit– 40% Hematocrit RBC (PRBC) – on average approx. 60% Miller’s Anesthesia, 7 th edition. 2010: chapter 82. A practice of anesthesia for infants and children, 4 th edition: chapters 8 and 10. C Cote. 2009. Transfusion result Hemoglobin 2 -3 g/d. L Hematocrit by approx. 3%. Platelets 50 000 – 100 000/mm 3 Coefficient 15 -20% Fibrinogen 60 -100 mg/d. L
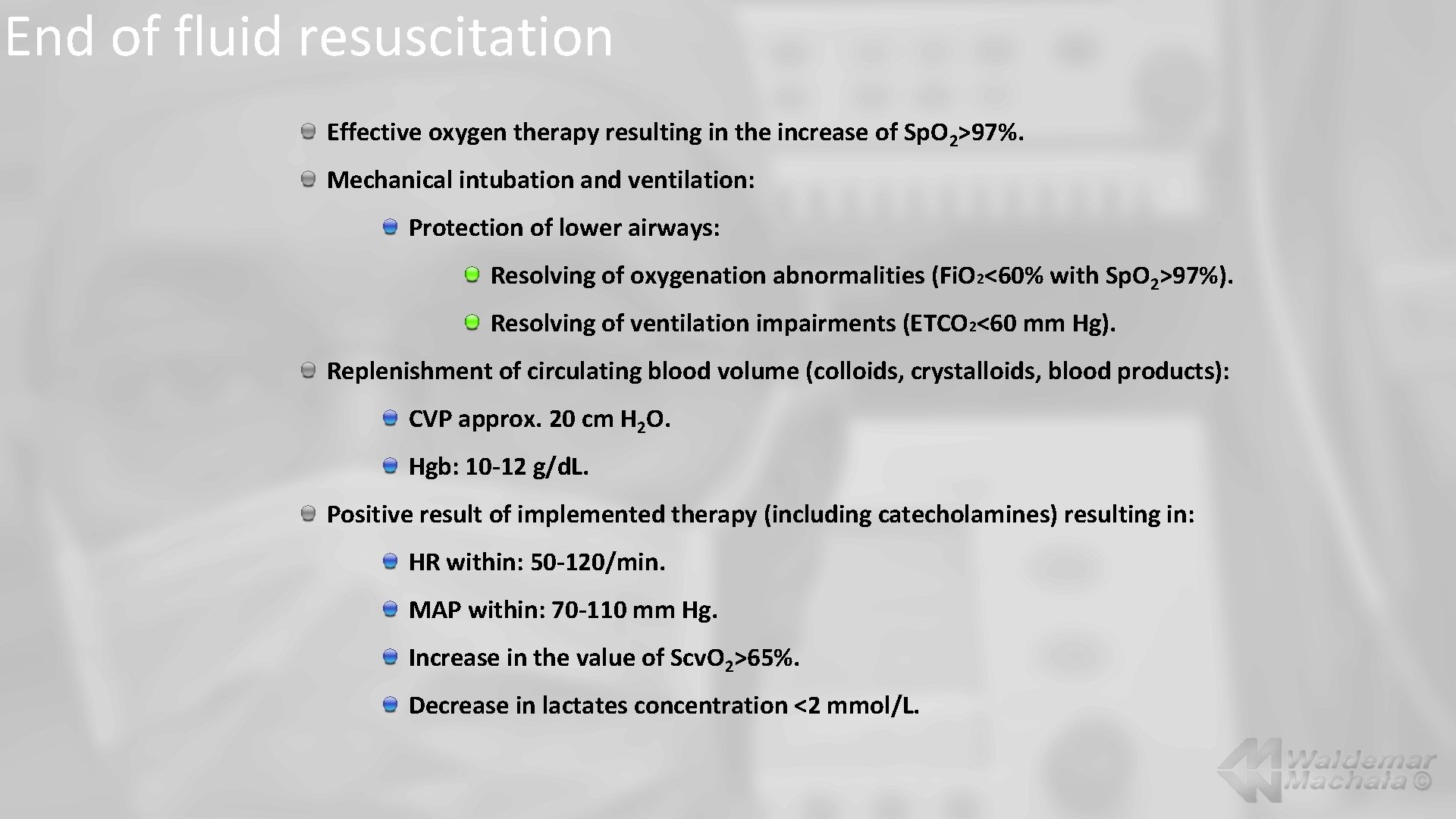
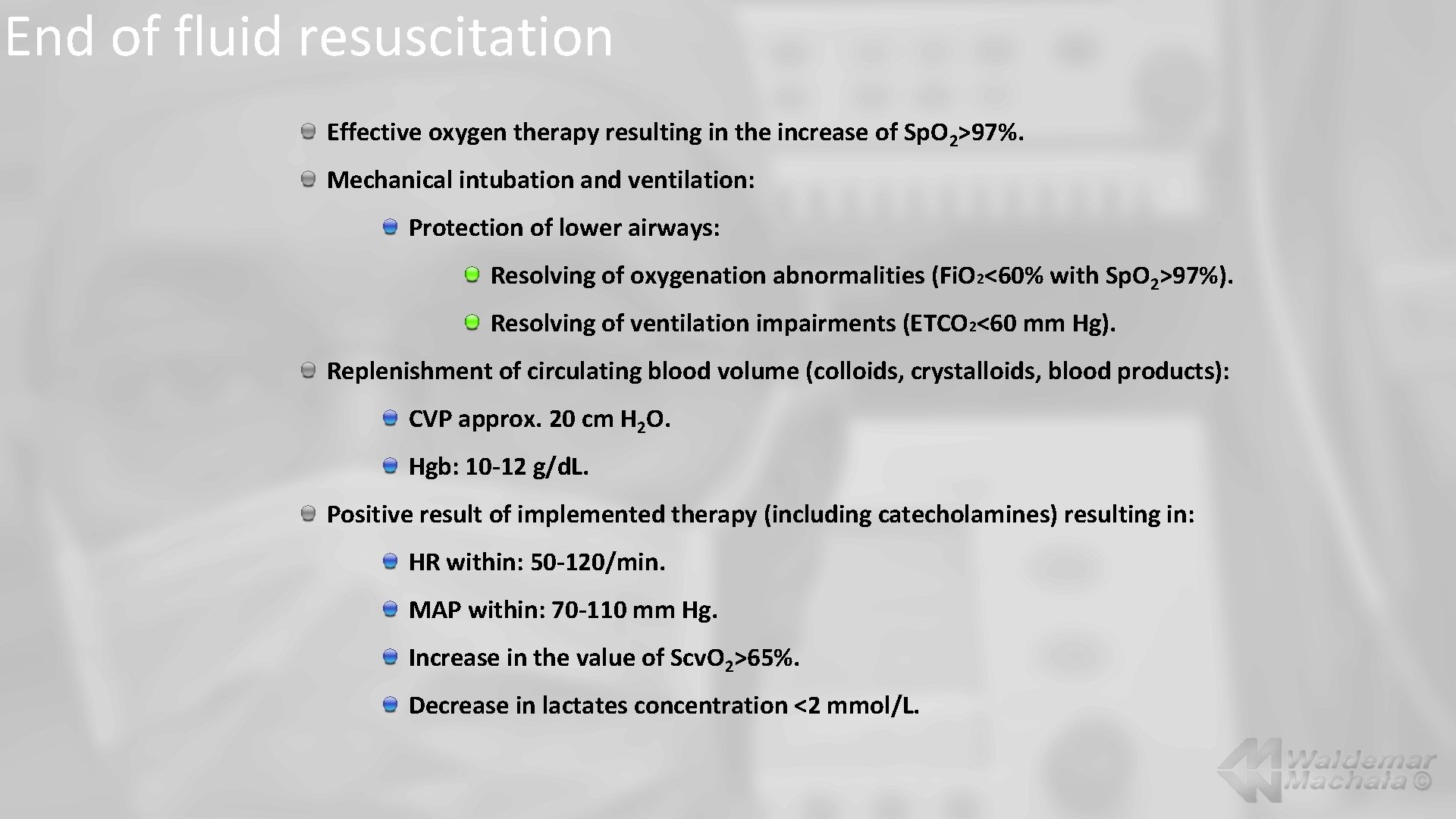
End of fluid resuscitation Effective oxygen therapy resulting in the increase of Sp. O 2>97%. Mechanical intubation and ventilation: Protection of lower airways: Resolving of oxygenation abnormalities (Fi. O 2<60% with Sp. O 2>97%). Resolving of ventilation impairments (ETCO 2<60 mm Hg). Replenishment of circulating blood volume (colloids, crystalloids, blood products): CVP approx. 20 cm H 2 O. Hgb: 10 -12 g/d. L. Positive result of implemented therapy (including catecholamines) resulting in: HR within: 50 -120/min. MAP within: 70 -110 mm Hg. Increase in the value of Scv. O 2>65%. Decrease in lactates concentration <2 mmol/L.

http: //www. machala. info
 Waldemar giza
Waldemar giza Her dufter lysegrønt af græs tekst
Her dufter lysegrønt af græs tekst Waldemar fortuna
Waldemar fortuna Waldemar mercado
Waldemar mercado Waldemar giza
Waldemar giza Arthur ernest guedel
Arthur ernest guedel Adam gessler wikipedia
Adam gessler wikipedia Synovial membrane
Synovial membrane Fluid statics deals with fluid at rest
Fluid statics deals with fluid at rest Fluid statics deals with fluid at rest
Fluid statics deals with fluid at rest Fluid compartments in the body
Fluid compartments in the body Intracellular extracellular fluid
Intracellular extracellular fluid Interstitial fluid vs extracellular fluid
Interstitial fluid vs extracellular fluid Fluid mechanics chapter
Fluid mechanics chapter Extracellular fluid and interstitial fluid
Extracellular fluid and interstitial fluid Fluid thrill volume
Fluid thrill volume Both psychoanalysis and humanistic therapy stress
Both psychoanalysis and humanistic therapy stress Bioness integrated therapy system price
Bioness integrated therapy system price Humanistic therapies aim to boost
Humanistic therapies aim to boost Wubbolding
Wubbolding Suspension therapy
Suspension therapy Robyn smith therapist
Robyn smith therapist Principles of topical therapy in dermatology
Principles of topical therapy in dermatology Difference between crystalized and fluid intelligence
Difference between crystalized and fluid intelligence Fixed layout website example
Fixed layout website example Sprittles
Sprittles Serous fluid
Serous fluid Colloids fluids examples
Colloids fluids examples Hydraulic fluid conditioning
Hydraulic fluid conditioning Fluid vs crystallized intelligence
Fluid vs crystallized intelligence Types pf friction
Types pf friction Difference between laminar and turbulent flow
Difference between laminar and turbulent flow Clear liquid diet
Clear liquid diet Thar supercritical fluid extraction
Thar supercritical fluid extraction Cerebrospinal fluid flow
Cerebrospinal fluid flow Bernoulli
Bernoulli Synovial fluid composition
Synovial fluid composition String test synovial fluid
String test synovial fluid