VTE during pregnancy and the puerperium DR MONA





![�The two most common modalities for imaging are lung scintigraphy [V/Q] and (CTPA). �although �The two most common modalities for imaging are lung scintigraphy [V/Q] and (CTPA). �although](https://slidetodoc.com/presentation_image_h2/a881e46718640e0477ce52b2a57e9bb2/image-28.jpg)








- Slides: 62
VTE during pregnancy and the puerperium DR MONA YADOLLAHI CARDIOLOGIST FACULTY MEMBER OF RAJAEI HEART CENTER
�VTE (PTE&DVT) represents a significant cause of pregnancy-related morbidity and mortality. �Pregnancy and the puerperium increase incidence of VTE, occurring in 0. 05– 0. 20% of all pregnancies. (1 in 1600 )
�The risk of VTE is highest in the immediate post- partum period, particularly after C/S, and returns to the non-pregnant level after the sixth week post-partum.
�Case fatality rate is 3. 5%. � In the United States, PE is the sixth leading cause of maternal mortality, responsible for 20 to 30% of maternal deaths.
�There are NO clinical signs or symptoms that are specific for PE. � NO symptoms to shock or sudden death.
� overlap symptoms, dyspnea occurs in up to 70% of normal pregnancies. � Thus, identifying a clinically important PE during pregnancy is challenging, both over diagnosing and under diagnosing PE during pregnancy.
� in a study of 38 pregnant women with confirmed PE: dyspnea 62% pleuritic chest pain 55% cough 24% sweating 18% were the four most common presenting features.
�DYSPNEA of normal pregnancy starts during the first or second trimester, the frequency rises during the second trimester, and then is reasonably stable during the third trimester. � worse when the pregnant woman is in the sitting position, and is not associated with exercise.
�Is dyspnea of acute or gradual onset? � Other common findings suggesting pulmonary embolism are tachypnea, pleuritic chest pain, and hemoptysis, which do not occur with normal dyspnea of pregnancy. � Heart rate may increase above the elevated baseline rate of normal pregnancy.
�Is cough or wheezing present? �Acute cough is most commonly due to an acute respiratory tract infection. � Other considerations include an acute exacerbation of underlying chronic pulmonary disease, pneumonia, and pulmonary embolism.
�Is the chest clear on auscultation? �Crackles (rales) are indicative of abnormalities affecting the distal lung parenchyma(interstitial pulmonary edema or ILD)
�Are other symptoms present? � Physiologic dyspnea is not accompanied by pain or other symptoms. �Thoracic tumors and pulmonary emboli may present with dyspnea and chest pain, hemoptysis, cough, or wheezing.
�Is onset early in gestation or near term? � Women with PPCMP commonly complain of dyspnea, but onset is rarely before 36 weeks of gestation, and affected patients usually present during the first four to five months postpartum.
� Any one or combination of the symptoms should always raise alarm and increase the clinical suspicion for a PE during pregnancy.
�The most significant risk factors for VTE in pregnancy are a prior history of unprovoked DVT or pulmonary embolism and thrombophilias.
�From 15% to 25% of VTEs are recurrent events. �Half of the women who develop a thrombotic event during pregnancy have either a thrombophilic disorder or a previous idiopathic VTE.
�On the basis of the type and the total number of risk factors present in the individual patient, three risk groups can be identified (high, intermediate, and low risk groups) and preventive measures applied accordingly. �Previous recurrent VTEs and previous VTE— unprovoked or estrogen related—are considered high risk factors. �The exact influence of the other single risk factors or the summation of several risk factors on total VTE risk is not known according to ROYAL college.




LABORATORY STUDIES � ABG, D-dimer levels, and echocardiography are often performed but are neither sensitive nor specific as diagnostic or pretest probability tools for the evaluation of suspected PE during pregnancy.
ABG: neither sensitive nor specific A respiratory alkalosis is a very common. presence of hypoxemia with normal CXR should raise the clinical suspicion for PE in pregnancy and prompt further evaluation.
D-dimer �Increase during the course of a normal pregnancy and slowly decline postpartum. � Interpretation of D-dimer levels during pregnancy and the puerperium is complicated by a lack of normal reference ranges in this setting. �Thus, D-dimer levels have limited utility for the diagnosis of VTE.
�Considering the low sensitivity (high false negative rate) and specificity (high false positive rate) of D-dimer in this setting, a high D-dimer is not diagnostic of PE, and a low D-dimer (even <500 ng/m. L) only modestly lowers the suspicion but does not effectively eliminate PE from the differential diagnosis.

Echocardiography � NOT routinely performed in the diagnostic evaluation of a pregnant patient suspected of having a PE. � excludes CMP or to evaluate the size of the RV in a patient with confirmed PE. �However, the prognostic value of RV dilation by echocardiogram has not been formally evaluated in pregnancy.
�PE cannot be definitively diagnosed without confirmatory imaging.
![The two most common modalities for imaging are lung scintigraphy VQ and CTPA although �The two most common modalities for imaging are lung scintigraphy [V/Q] and (CTPA). �although](https://slidetodoc.com/presentation_image_h2/a881e46718640e0477ce52b2a57e9bb2/image-28.jpg)
�The two most common modalities for imaging are lung scintigraphy [V/Q] and (CTPA). �although contrast-enhanced pulmonary angiography was the gold standard, neither test is commonly used in the pregnant population. �Employing strategies that use compressive ultrasound (CUS) to avoid the radiation exposure of V/Q and CTPA have been described, but CUS is not definitively diagnostic of PE.
� The evidence to support choosing one imaging modality over another is weak in the pregnant population

CXR �Despite its poor diagnostic accuracy, a CXR should be performed in every pregnant patient in whom a PE is suspected. This both evaluates for alternative diagnoses and allows the accurate interpretation of V/Q scan results.
�For those with a normal CXR, V/Q scanning remains the test of choice for the diagnosis of PE in pregnancy. �A positive V/Q scan demonstrates a definitive pattern of mismatch between the ventilation and perfusion images of the lung. �In general, only normal or very low probability scans and high probability scans are considered diagnostic.
�Unlike the general population, pregnant women have a relatively low likelihood of indeterminate V/Q scans and a high likelihood of diagnostic V/Q scans.
�CTPA has a high negative predictive value for ruling out the diagnosis of PE in pregnancy. �However, compared to that reported in the general population, it may have a slightly higher rate of nondiagnostic studies during pregnancy, particularly when the chest radiograph is abnormal. � CTPA is diagnostically useful when V/Q scanning is not available or is indeterminate (eg, when the chest radiograph is abnormal) or when an alternate pathology is being considered.
Contrast-enhanced pulmonary angiography it is rarely performed in this population. it is less sensitive than CTPA for the detection of emboli. Most of the thrombi missed on contrast angiography were sub segmental.
�The Wells score has limited value in the pregnant population, probably due to the high prevalence of baseline tachycardia and the low likelihood of certain risk factors (eg, malignancy or recent surgery) that are listed on the scoring system.
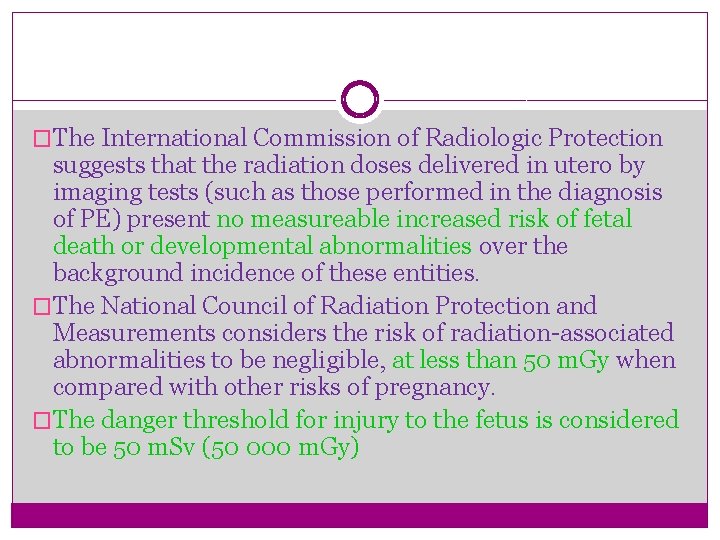
�The International Commission of Radiologic Protection suggests that the radiation doses delivered in utero by imaging tests (such as those performed in the diagnosis of PE) present no measureable increased risk of fetal death or developmental abnormalities over the background incidence of these entities. �The National Council of Radiation Protection and Measurements considers the risk of radiation-associated abnormalities to be negligible, at less than 50 m. Gy when compared with other risks of pregnancy. �The danger threshold for injury to the fetus is considered to be 50 m. Sv (50 000 m. Gy)


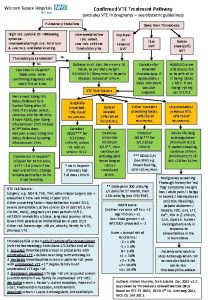
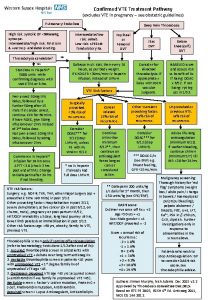
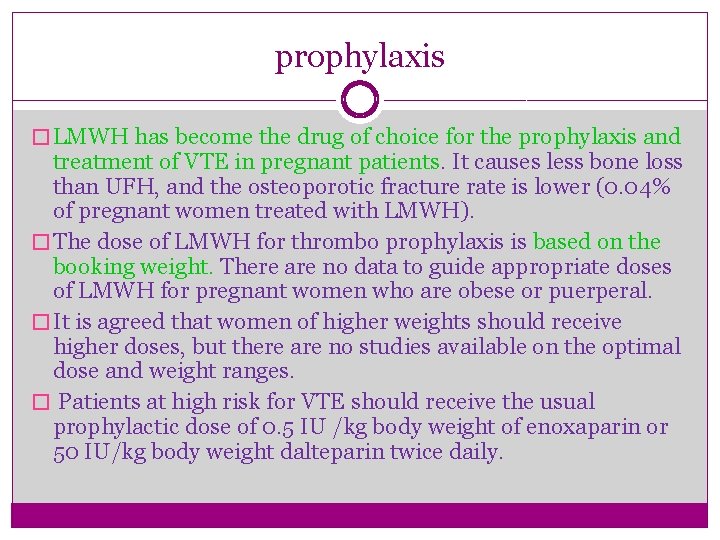
prophylaxis � LMWH has become the drug of choice for the prophylaxis and treatment of VTE in pregnant patients. It causes less bone loss than UFH, and the osteoporotic fracture rate is lower (0. 04% of pregnant women treated with LMWH). � The dose of LMWH for thrombo prophylaxis is based on the booking weight. There are no data to guide appropriate doses of LMWH for pregnant women who are obese or puerperal. � It is agreed that women of higher weights should receive higher doses, but there are no studies available on the optimal dose and weight ranges. � Patients at high risk for VTE should receive the usual prophylactic dose of 0. 5 IU /kg body weight of enoxaparin or 50 IU/kg body weight dalteparin twice daily.




�LMWH has also become the drug of choice for the treatment of VTE in pregnancy and puerperium.
Treatment � recurrent VTE 1. 15%. � major bleeding 1. 98%. �HIT 0. 04%. � In clinically suspected DVT or pulmonary embolism, treatment with LMWH should be given until the diagnosis is excluded by objective testing.
Dosage �The recommended therapeutic dose is calculated on body weight (e. g. enoxaparin 1 mg/kg body weight twice daily, Dalteparin 100 IU/kg body weight twice daily) aiming for 4– 6 h peak anti-Xa values of 0. 6– 1. 2 IU/m. L
Monitoring �The necessity to monitor anti-Xa values regularly in patients with VTE is still controversial. �Given the need for dose increase as pregnancy progresses to maintain a certain therapeutic anti-Xa level, it seems reasonable to determine anti-Xa levels also during pregnancy in patients with VTE.
�A simple guide is dose adjustment according to increasing weight during pregnancy.

�No LMWH when the patient thinks that she is in labour �LMWH should be discontinued 24 hours prior to planned delivery �Regional anaesthetic should not be used until at least 24 h after last dose of therapeutic LMWH �LMWH should not be given for 4 h after spinal anaesthesia � Epidural catheter should not be removed within 12 hours of the most recent injection
UFH �It is favored in patients with renal failure and when urgent reversal of anticoagulation by protamine is needed, as well as in the acute treatment of massive pulmonary emboli. �In patients with acute pulmonary embolism with hemodynamic compromise, i. v. administration of UFH is recommended (loading dose of 80 U/kg, followed by a continuous i. v infusion of 18 U/kg/h). �The dose is then titrated to achieve a therapeutic a. PTT, defined as the a. PTT that corresponds to an anti-Xa level of 0. 3– 0. 7 IU/m. L.
�When hemodynamic are improved and the patient is stabilized, UFH can be switched to LMWH in therapeutic doses and maintained during pregnancy. �LMWH should be switched to i. v. UFH at least 36 h before the induction of labor or caesarean delivery. � UFH should be discontinued 4– 6 h before anticipated delivery, and restarted 6 h after delivery if there are no bleeding complications. �Neither UFH nor LWMH is found in breast milk in any significant amount and they do not represent a contraindication to breastfeeding.
Thrombolysis �Thrombolytics are considered to be relatively contraindicated during pregnancy and peripartum and should only be used in high risk patients with severe hypotension or shock. � The risk of haemorrhage, mostly from the genital tract, is 8%. � Fetal loss of 6% and 6% pre-term delivery were reported.
�Both thrombolytics do not cross the placenta in significant amounts. �When thrombolysis has been given, the loading dose of UFH should be omitted an infusion started at a rate of 18 U/kg/h. � After stabilization of the patient, UFH can be switched to LMWH for the residual duration of pregnancy.
Fondaparinux � There are very few studies on fondaparinux in pregnancy. � one has shown minor transplacental passage of fondaparinux. � Because of the scarce data, the drug should not be used in pregnancy.
Rivaroxaban � Rivaroxaban crosses the placental barrier and has therefore not been evaluated, and is not recommended in pregnant patients.
Vena cava filters � Indications for vena cava filters are the same as in non-pregnant patients. However, the risk associated with the procedure may be increased.
�In patients with recent PTE, pre-partum heparin treatment should be restarted 6 h after a vaginal birth and 12 h after a caesarean delivery, if no significant bleeding has occurred, with subsequent overlap with vitamin K antagonists for at least 5 days.
Post-partum management �Vitamin K antagonists may be started on the second day after delivery and continued for at least 3 months or for 6 months if pulmonary embolism occurred late in pregnancy. �The INR should be between 2 and 3 and needs regular monitoring, ideally once every 1– 2 weeks. Vitamin K antagonists do not enter the breast milk in active forms and are safe for nursing mothers.
Thanks for your tolerance & attention
 Icd 10 code for twin pregnancy
Icd 10 code for twin pregnancy Spotting differential diagnosis
Spotting differential diagnosis Vte protocol
Vte protocol Prevention of vte in nonorthopedic surgical patients
Prevention of vte in nonorthopedic surgical patients Secondary prevention vte
Secondary prevention vte Vte safety zone
Vte safety zone L
L Lactating women meaning
Lactating women meaning Galactokinesis definition
Galactokinesis definition Define puerperium
Define puerperium Stages of implantation
Stages of implantation Hormones during pregnancy
Hormones during pregnancy Dexamethasone action in pregnancy
Dexamethasone action in pregnancy Role of nurse in reproductive health ppt
Role of nurse in reproductive health ppt Components of weight gain during pregnancy
Components of weight gain during pregnancy Sajda during pregnancy
Sajda during pregnancy Are sore breasts and cramps a sign of pregnancy
Are sore breasts and cramps a sign of pregnancy Fluticasone furoate pregnancy
Fluticasone furoate pregnancy Robert longo
Robert longo Pictures of garbage: the gipsy (magna)
Pictures of garbage: the gipsy (magna) Facts about mona lisa
Facts about mona lisa Pregnancy and infant cohort monitoring and evaluation
Pregnancy and infant cohort monitoring and evaluation Mona walia
Mona walia The dinner party by mona gardner plot diagram
The dinner party by mona gardner plot diagram Mohammed mona md
Mohammed mona md In other words mona baker
In other words mona baker Joconde nombre d'or
Joconde nombre d'or Last supper golden ratio
Last supper golden ratio Mona lisa golden ratio
Mona lisa golden ratio Mona lisa allusion
Mona lisa allusion Mona lisa also known as
Mona lisa also known as Color vectors and viewpoint in still and moving images
Color vectors and viewpoint in still and moving images Allusion meaning
Allusion meaning Petra van brabandt
Petra van brabandt Semantička (ikonološka) perspektiva
Semantička (ikonološka) perspektiva Mona pozitif
Mona pozitif Mona lisa 1503
Mona lisa 1503 Dr mona soliman
Dr mona soliman Burj khalifa project management
Burj khalifa project management Allusion kid definition
Allusion kid definition Mona lisa agile
Mona lisa agile Mona lisa rule of thirds
Mona lisa rule of thirds Louvre, mona lisa
Louvre, mona lisa Thomson reuters cto
Thomson reuters cto Mona lisa effect matthew savage
Mona lisa effect matthew savage Cn tower golden ratio
Cn tower golden ratio A obra great coffee
A obra great coffee Mona badr
Mona badr Mona grover
Mona grover Mona minus8
Mona minus8 Mona lisa symmetry
Mona lisa symmetry Mona lisa individualism
Mona lisa individualism Dr mona idris
Dr mona idris Paul giovanopoulos mona lisa
Paul giovanopoulos mona lisa Allusions meaning
Allusions meaning Allusion in freak the mighty
Allusion in freak the mighty Mona mawari
Mona mawari Komodo dragon names
Komodo dragon names Co mona
Co mona Mona berciu
Mona berciu Mona lisa goldener schnitt
Mona lisa goldener schnitt Co mona
Co mona Mona lisa
Mona lisa