Purpose and Outcome Mona Grover A good plan






- Slides: 27
Purpose and Outcome Mona Grover
“A good plan is like a road map: it shows the final destination and usually the best way to get there. ” H. Stanley Judd
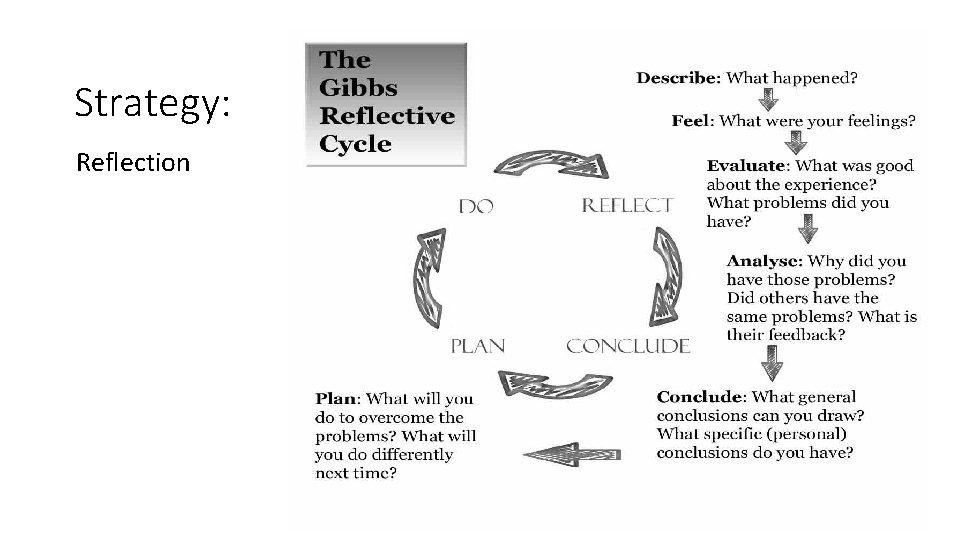
Reflection is not only utilized for learning from experiences but also to identify what lies ahead and how to plan for it.
Reflection Through reflection I want to plan for what lies ahead with what I have learned so far …. .
How do I do it?
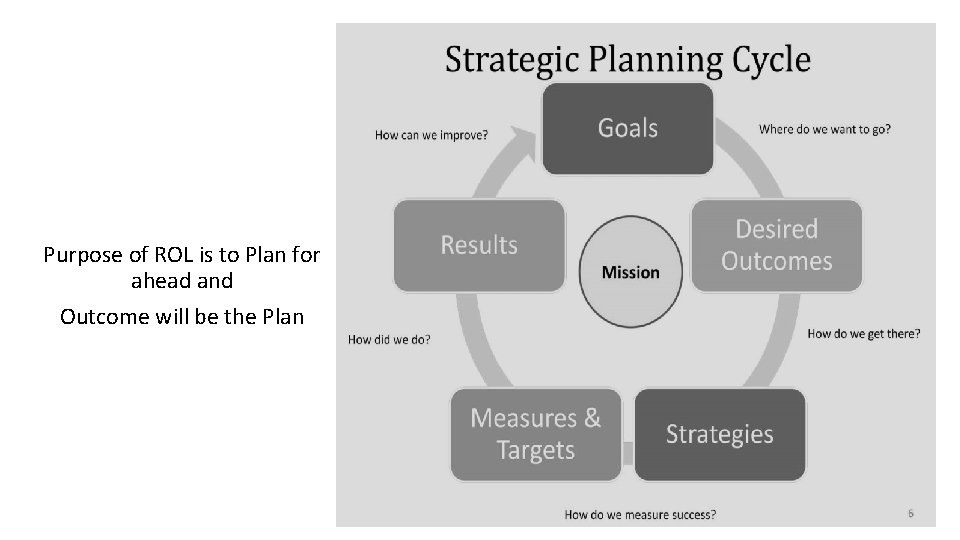
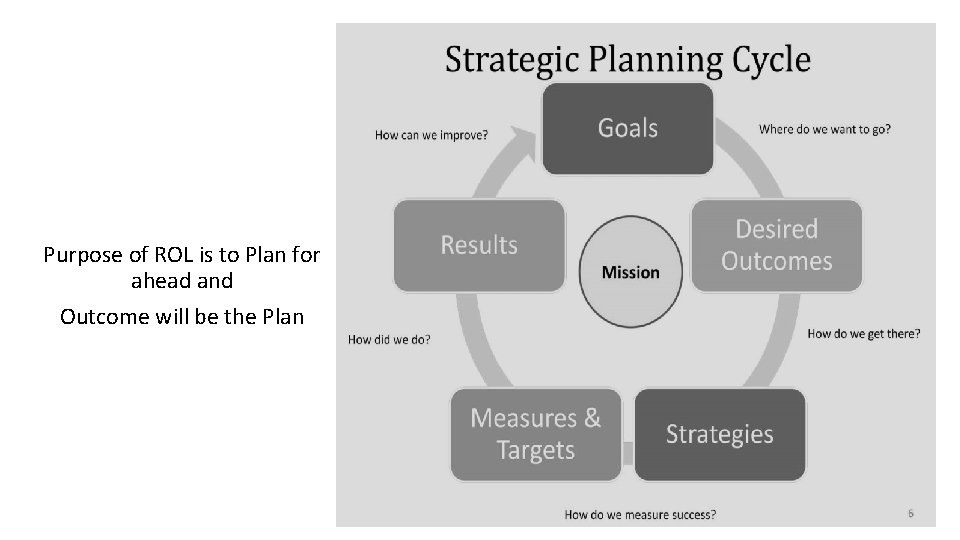
Purpose of ROL is to Plan for ahead and Outcome will be the Plan
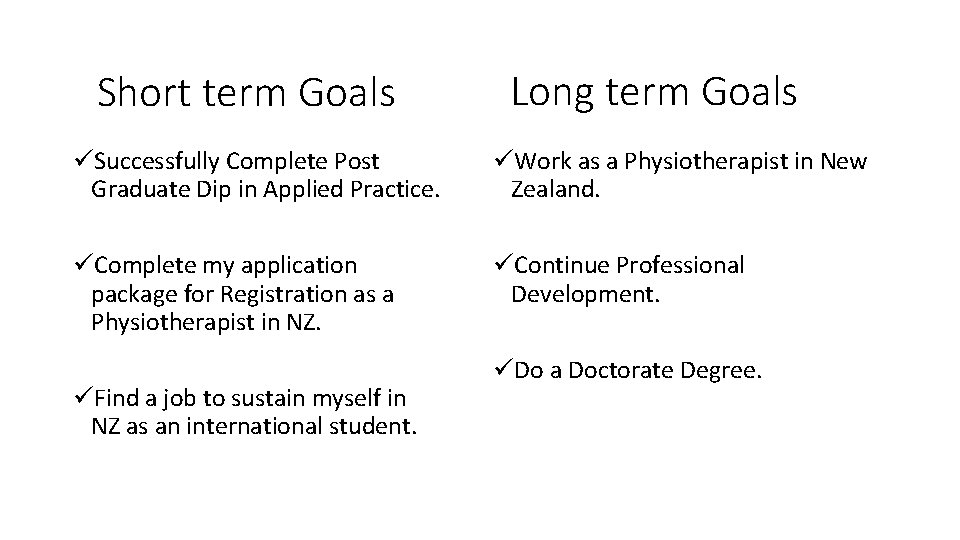
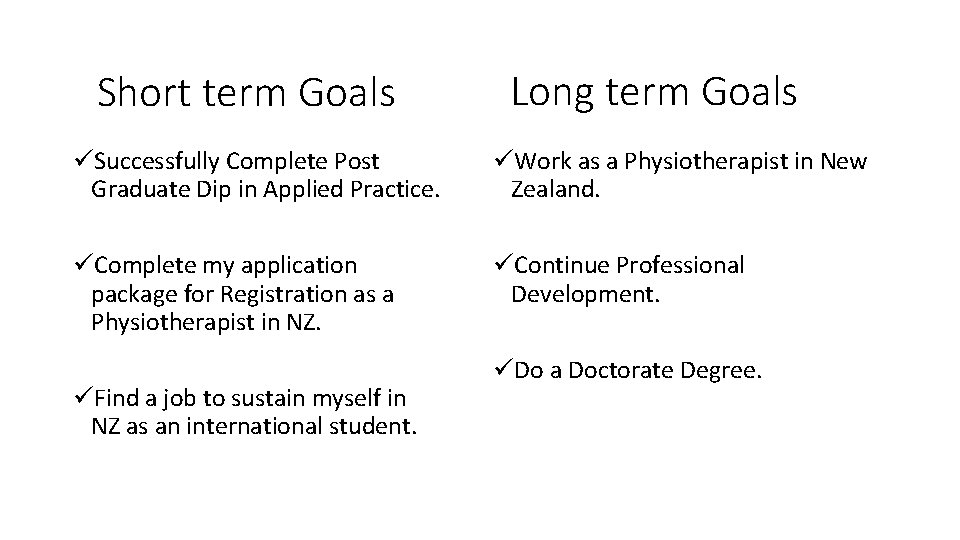
Short term Goals Long term Goals üSuccessfully Complete Post Graduate Dip in Applied Practice. üWork as a Physiotherapist in New Zealand. üComplete my application package for Registration as a Physiotherapist in NZ. üContinue Professional Development. üFind a job to sustain myself in NZ as an international student. üDo a Doctorate Degree.

Desired Outcomes Complete Application Pack as Overseas Qualified Physiotherapist in New Zealand including: i. Referenced Report on the Treaty of Waitangi. ii. Reflective Statement on a chosen topic from the list identified by the Board. iii. Statement of Cultural Competency. iv. Additional Evidence of Competency as a Physiotherapist- Published Article
How do I do it?
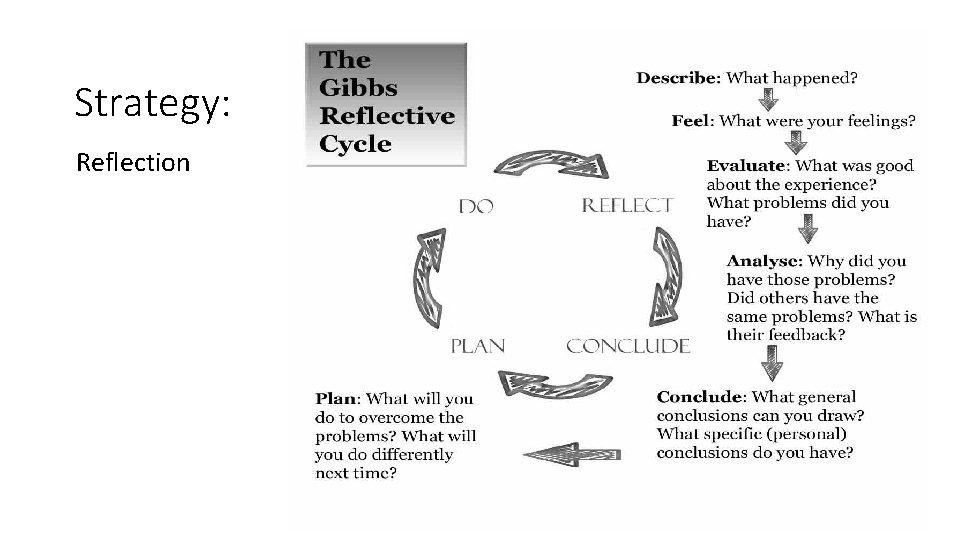
Strategy: Reflection
References Culture and Physiotherapy Practice in New Zealand
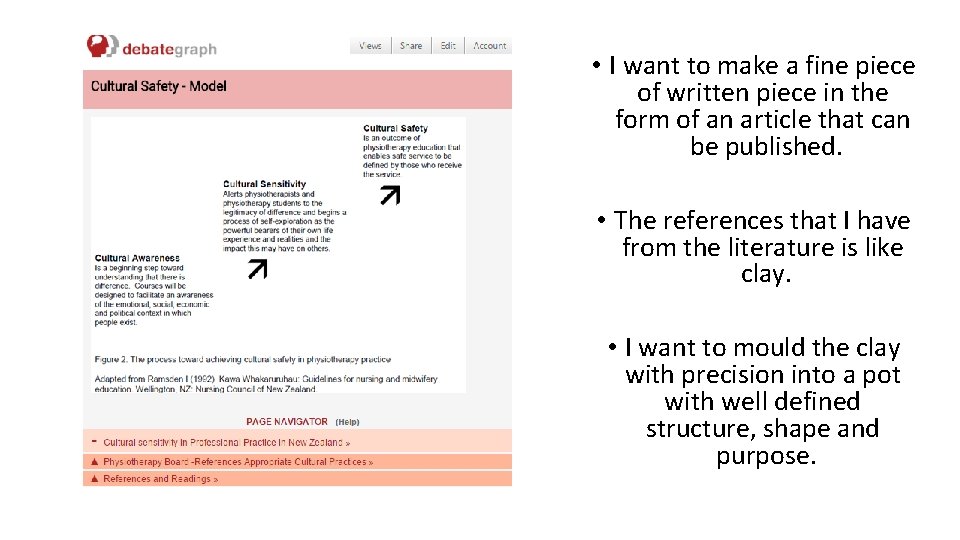
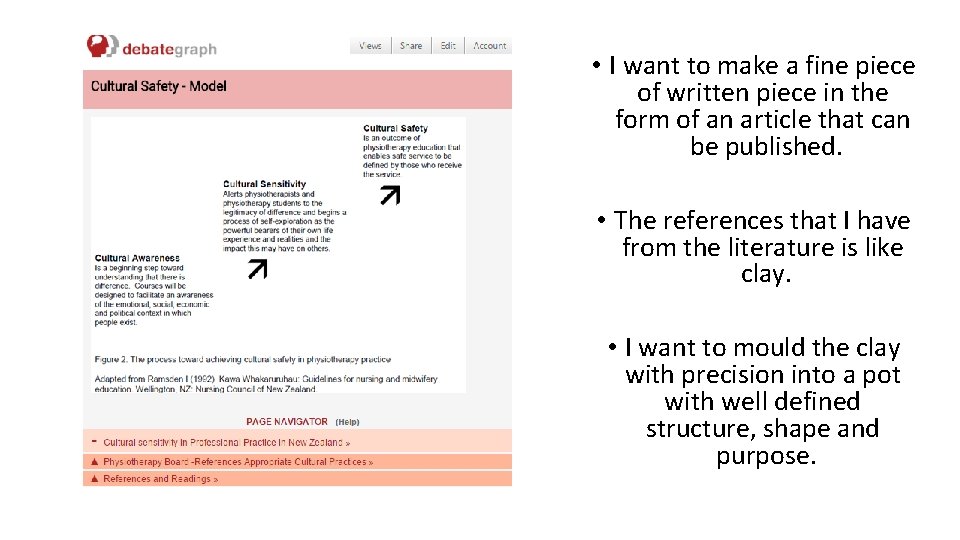
• I want to make a fine piece of written piece in the form of an article that can be published. • The references that I have from the literature is like clay. • I want to mould the clay with precision into a pot with well defined structure, shape and purpose.
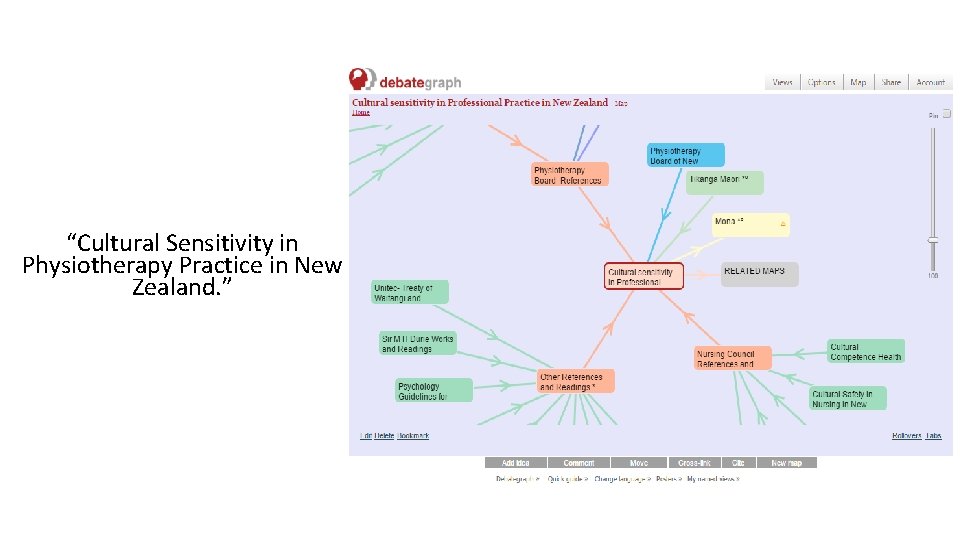
“Cultural Sensitivity in Physiotherapy Practice in New Zealand. ”



Shape of the Pot • After refining literature and selecting articles for defining the shape of article. • The shape will be the structure of my article. • Will include relevant research articles for defining cultural sensitivity in Health care in New Zealand in Physiotherapy Practice.
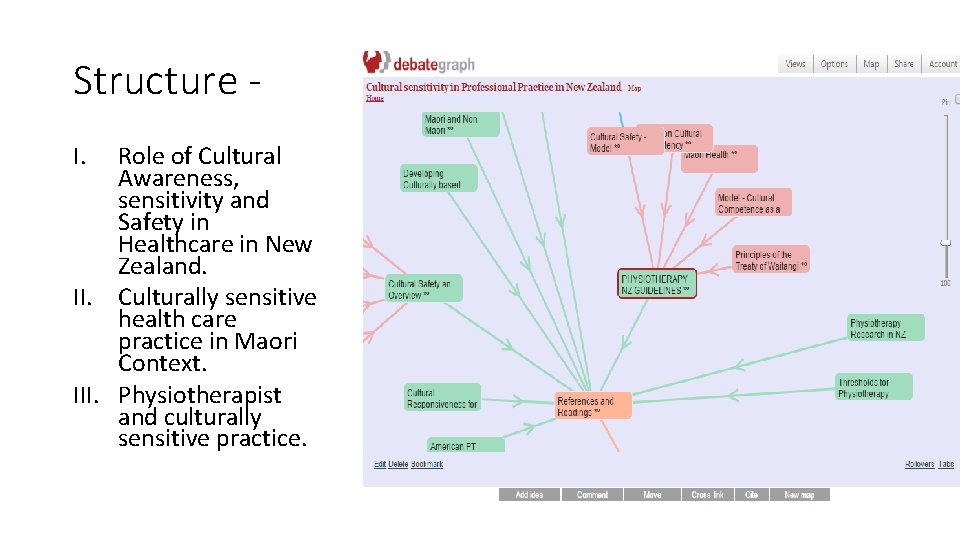
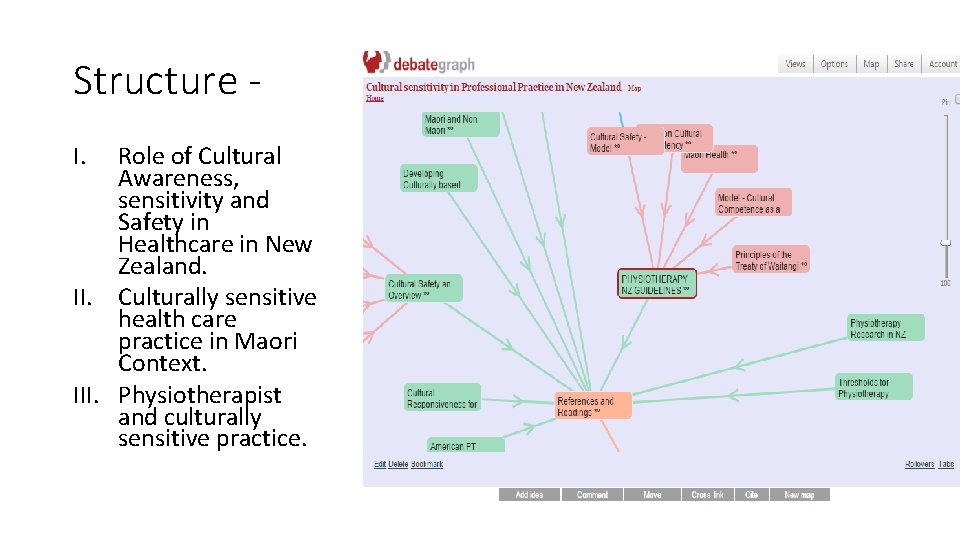
Structure I. Role of Cultural Awareness, sensitivity and Safety in Healthcare in New Zealand. II. Culturally sensitive health care practice in Maori Context. III. Physiotherapist and culturally sensitive practice.

I. Role of Cultural Awareness, sensitivity and Safety in Healthcare in New Zealand. • New Zealand- Biculturalism and Treaty of Waitangi. • Culture and Health care. • Culturally appropriate in Health care in New Zealand.

II. Culturally sensitive health care practice in Maori Context. • Developing Cultural Sensitivity – Maori Indigenous Knowledge and culture in New Zealand. • Treaty of Waitangi and Health care. • Tikanga Maori- Guidelines for cultural awareness and sensitivity.
III. Physiotherapist and culturally sensitive practice • Culturally sensitive Physiotherapy practice in New Zealand. • Guidelines for Physiotherapist. • Cultural safety and Education. • Cultural Safety and Clinical Practice and Competence.
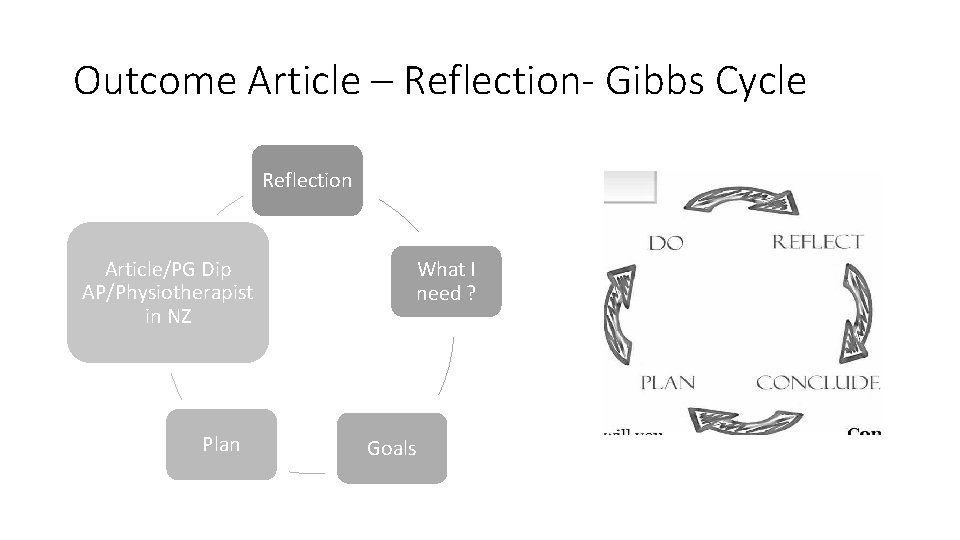
Outcome Article – Reflection- Gibbs Cycle Reflection Article/PG Dip AP/Physiotherapist in NZ Plan What I need ? Goals
What remains? • Contacting the Journals • Preparing the Manuscript • Applying for the Physiotherapy Board Registration as an Overseas Qualified Physiotherapist.
The Process of Reflection … • The process of Reflection and • To continue the progress of reflection Reflective Learning has taught me to I plan to practice reflection on a day to be organized and focussed on what I day basis even in tasks that are not want and my approach for achieving it. part of my professional life. • I can now confidently set targets and • As a full time practicing plan to meet those targets within the physiotherapist I want to continue to time frame. be a part of a research in what ever way possible using the process of • Organized and Confident are the two Reflection. objective qualities that I have surely developed in me after doing ROL. • Continue my professional development by developing qualities like leadership and mentoring in a clinical role using reflection and reflective learning
References • Ajwani, S and others. Decades of disparity: Ethnic mortality trends in New Zealand 1980– 1999. Wellington: Ministry of Health and University of Otago; 2003 • ACC (Te Kaporeihana Awhina Hunga Whara). Summary guidelines on Maori cultural competencies for providers. Wellington: ACC; 2004. • Agency of Health Research and Quality (AHRQ). Strategies for improving minority health care quality: Evidence Report/Tech-nology Assessment #90. Washington DC: US Agency of Health Research and Quality (AHRQ); 2004. • Arroll B, Goodyear-Smith F, Lloyd T. Depression in patients in an Auckland general practice. N Z Med J 2002 Apr 26; 115(1152): 176 -9. • Baxter J. Barriers to health care for Maori with known diabetes. NZ National Working Group on Diabetes and Te Roopu Rangahau Hauora a Ngai Tahu; 2002. • Carr J, Robson B, Reid P, Purdie G, Workman P. Heart failure: ethnic disparities in morbidity and mortality in New Zealand. N Z Med J 2002; 115(1146): 15– 7. • Counties Manukau chronic care manage-ment plan (unpublished report); 2001. Ministry of Health. Reducing inequalities in health. Ministry of Health; 2002. • Crengle S, Lay-Yee R Davis P Pearson J. A Comparison of Maori and non-Maori patient visits to doctors, Nat. Med. Ca. Report 6. 2002. • Crengle S. The development of Maori primary care services. Pac Health Dialog 2000; 7: 48– 53. • Ellison-Loschmann L, Cheng S, Pearce N. Time trends and sea-sonal patterns of asthma deaths and hospitalisations among Maori and non-Maori. N Z Med J. 2002; 115(1146): 6– 9. • Gribben B. Ethnicity and resource use in general practice in West Auckland. Experience in Practice TM. Healthcare Review – Online March 1999; 1(1). http//www. enigma. co. nz/eip_articles/ 9903. vol 1 no 1_001. htm. • Levinson W et al. A study of patient clues and physician responses in primary care and surgical settings. JAMA 2000; 284: 1021– 7.
• Lo HT, Fung KP. Culturally competent psychotherapy. Can J Psychiatry. 2003; 48(3): 161 -70. • Lockyear P. Physician-patient communication: Enhancing skills to improve patient satisfaction. Medscape CME 2004. • Ministry of Health. Maori providers: Primary health care deliv-ered by doctors and nurses: The National Primary Medical Care Survey (Nat. Med. Ca): 2001/02 Report 3. Wellington: Ministry of Health; 2004. • Ministry of Health. New Zealand Medical Practitioners 2000. Wellington: New Zealand Health Information Service; 2001. • Neuwirth ZE. An essential understanding of physician-patient com-munication Part 2. J Med Pract Management 1999; 15: 68 -72. • Reid P et al. Disparities in health: common myths and uncom-mon truths. Pacific Health Dialog 2000; 7: 38– 47. • Scott K, Marwick J, Crampton P. Utilization of general practi-tioner services in New Zealand its relationship with income, ethnicity and government subsidy. Health Services Management Research, 2003; 16(1): 45 -55. • Skegg D, Mc. Credie MR. Comparison of cancer mortality and incidence in New Zealand Australia. N Z Med J 2002; 115(1153): 205 -8. • Smith RC et al. The effectiveness of intensive training for resi-dents in interviewing. Ann Int Med 1998; 128: 118– 26. • Sporle A, Pearce N, Davis P. Social class mortality differences in Maori and non-Maori men aged 15– 64 during the last two dec-ades. N Z Med J 2002; 22; 115(1150): 127 -31. • Travaline JM, Ruchinskas R, D’Alonzo GE Jr. Patient-physician communication: why and how. J Am Osteopath Assoc. 2005; 105(1): 13– 8. • Wear D. Insurgent multiculturalism: Rethinking how and why we teach culture in medical education. Academic Medicine 2003; 78: 549– 54. • Westbrooke I, Baxter J, Hogan J. Are Maori under-served for cardiac interventions? N Z Med J 2001; 114(1143): 484 -7. • Yedidia MJ et al. Effect of communications training on medical student performance. JAMA 2003; 290: 1157– 65.
Thank You