Fits Faints and Funny Turns Anne Grover CN




- Slides: 28
Fits, Faints and Funny Turns Anne Grover CN 1 Neurology
Objectives l To appreciate the wide range of disorders that present with ‘clinical events’ l To discuss epileptic ‘lookalikes’ l To outline history taking
Seizures Are characterized by a sudden change in movement, behaviour, sensation or consciousness produced by a sudden burst of excessive electrical activity in brain cells causing a chemical (neurotransmitter) imbalance.
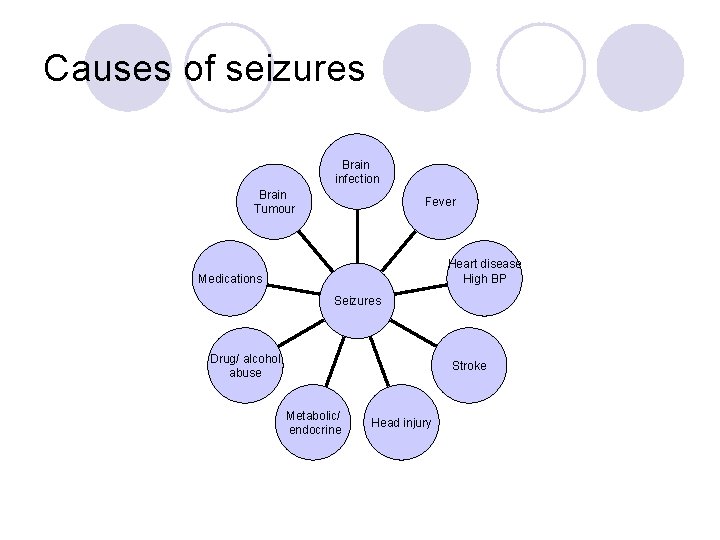
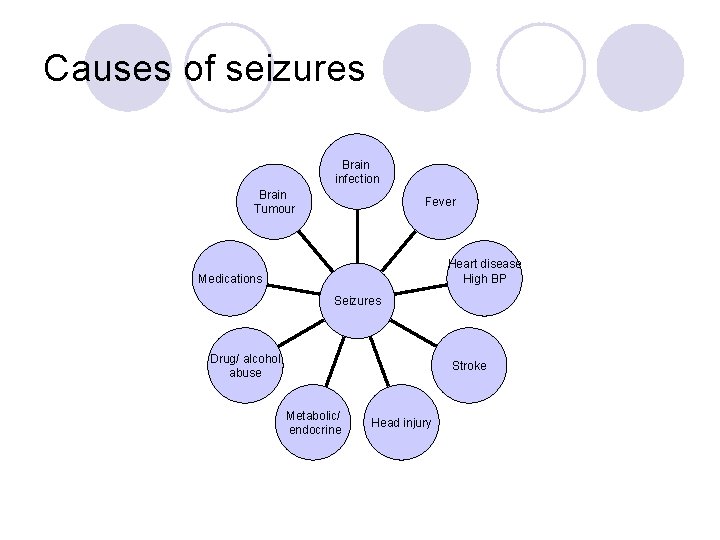
Causes of seizures Brain infection Brain Tumour Fever Heart disease High BP Medications Seizures Drug/ alcohol abuse Stroke Metabolic/ endocrine Head injury
Epilepsy l Epilepsy – refers to a group of different neurological conditions characterised by recurrent, unprovoked epileptic seizures l A manifestation(s) of epileptic excessive usually self-limiting activity of neurons in the brain
Epilepsy l Affects 1 in 115 people l Prevalence in Ireland <42 000 people with epilepsy l Approximately 50 million worldwide l One of the most common serious chronic neurological conditions 1. Joint Epilepsy Council. Epilepsy prevalence, incidence and other statistics. 2011; 2. Brainwave 2009



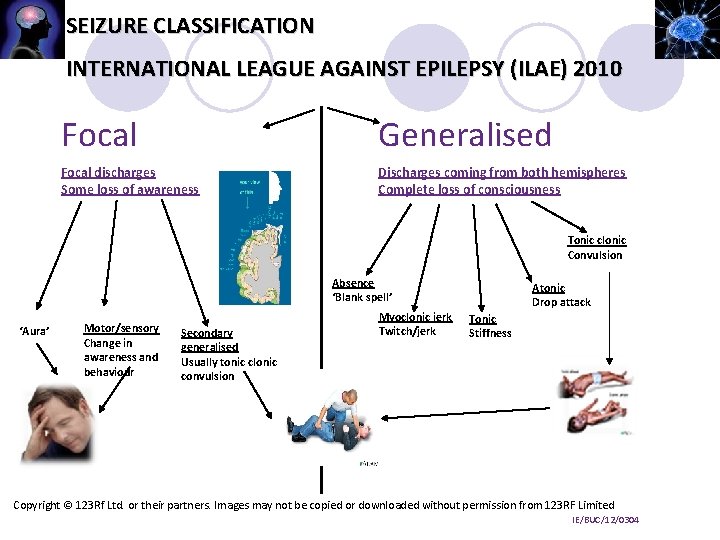
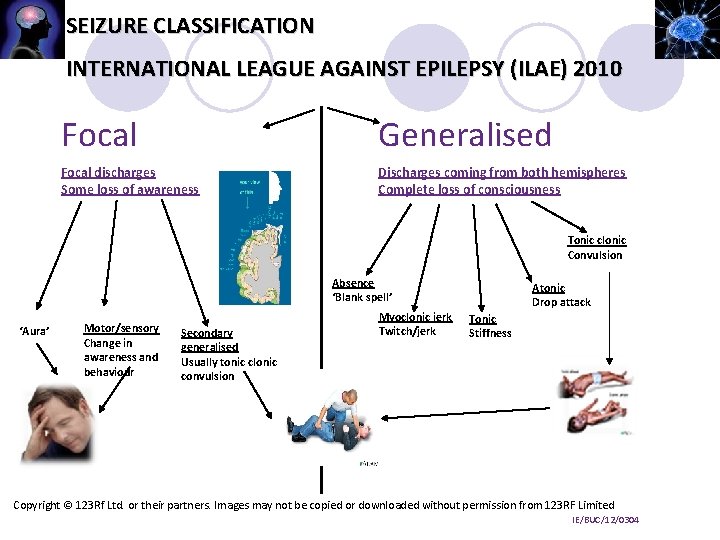
SEIZURE CLASSIFICATION INTERNATIONAL LEAGUE AGAINST EPILEPSY (ILAE) 2010 Focal Generalised Focal discharges Some loss of awareness Discharges coming from both hemispheres Complete loss of consciousness Tonic clonic Convulsion Absence ‘Blank spell’ ‘Aura’ Motor/sensory Change in awareness and behaviour Secondary generalised Usually tonic clonic convulsion Myoclonic jerk Twitch/jerk Atonic Drop attack Tonic Stiffness Copyright © 123 Rf Ltd. or their partners. Images may not be copied or downloaded without permission from 123 RF Limited IE/BUC/12/0304
Electroclinical syndromes l Defined as an ‘electroclinical’ pattern of clinical features and investigation findings may have different aetiologies. l Common electroclinical syndromes l eg- Childhood absence epilepsy l - Juvenile myoclonic epilepsy l - Lennox Gastaut
Generalised Tonic Clonic Seizure l Prodromes – non-epileptic clinical alteration prior to onset of an epileptic seizure l Aura – “warning sign” – epileptic seizure experienced prior to GTCS l Initial tonic phase l -Epileptic cry, eyes open, roll upwards, jaw clamps shut l Limbs stiff & extended, arms may flex, cyanosis
Clonic Phase l Rhythmic jerking of all 4 limbs, jaw & facial muscles l May froth at the mouth, bite tongue, urinary incontinence l Jerking gradually slows before stopping
Itcal phase l Followed by flaccidity of muscles l Consciousness slowly regained, may lapse into deep sleep minutes to hours after l GTCS generally self-limiting, last 1 -2 minutes
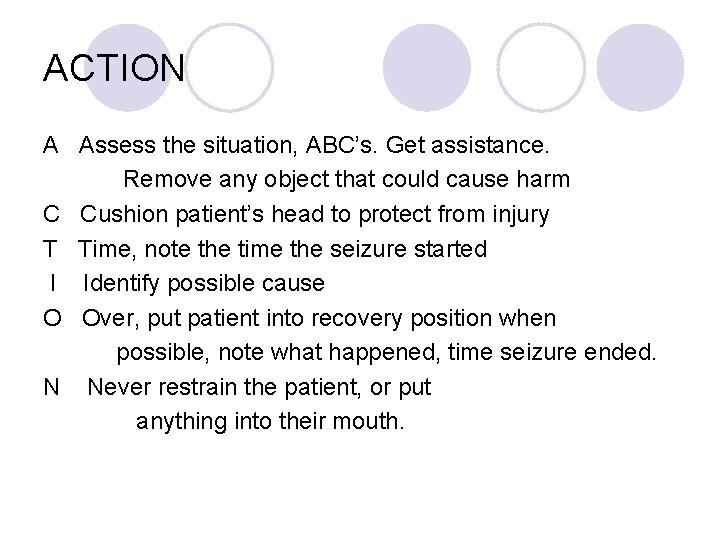
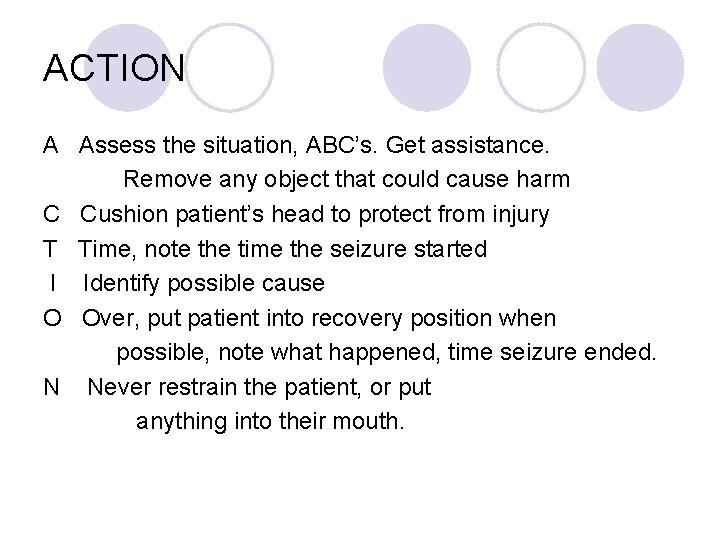
ACTION A Assess the situation, ABC’s. Get assistance. Remove any object that could cause harm C Cushion patient’s head to protect from injury T Time, note the time the seizure started I Identify possible cause O Over, put patient into recovery position when possible, note what happened, time seizure ended. N Never restrain the patient, or put anything into their mouth.
Provoking factors l Illness or fever l Sleep deprivation l Missing doses AED’s l Alcohol l Stress
Prolonged acute epileptic seizures l Definition of status epilepticus: l A seizure lasting >5 minutes, or l Two or more seizures without a return of consciousness between seizures 1 l Immediate treatment is recommended for: l Prolonged seizures ≥ 5 minutes, or l Repeated convulsive seizures (≥ 3 in an hour)2 l Treatment delay lessens the chance of successful response to a single medication 3
Women’s issues l Menstrual cycle l Fertility l Contraception l Pregnancy
Lifestyle implications • • Social issues Driving Working Personal safety Good nutrition, special diets Memory problems Mood changes
Seizure imitators l l l l Syncope Psychogenic non-epileptic seizures (PNES) Transient ischaemic attack Narcolepsy/cataplexy/sleep apnea Sleep-walking, night terrors Panic attack Complex migraines. Cardiac arrhythmias.
Syncope l LOC & postural tone l Brief stiffening or spasms & irregular jerks of the limbs l Eyes open, roll upwards l Urinary incontinence & trauma l Generally less than 10 seconds l Convulsive syncope - 70 -90%
Psychogenic non-epileptic seizures l Appear to lose consciousness & fall l Eyes closed l Often lack stereotypical characteristics l Jerking may be asymmetric, asynchronous, wax and wane l Pelvic thrust, flailing & tremors l Vocalise throughout l Consciousness may be retained

Diagnosis l History
History l Obtain a detailed account of the event from the patient and a witness l Where, when, what happened? l Any warning sign? Any triggers? l First event? Other events? l Progression- How did it start? l After the event? l Useful features
Conclusion l Epilepsy is one of the most serious, chronic neurological conditions l Can be difficult to distinguish between imitators l 20 -30% of patients misdiagnosed l A detailed history can assist with diagnosis
References l Brainwave The Irish Epilepsy Association. Shedding Light on Epilepsy. A nurses information pack. l Epilepsy Ireland. (2009). The prevalence of Epilepsy in Ireland Study. www. epilepsy. ie l Murphy, S. , Epilepsy-definitions, diagnosis and treatment. Nursing in General Practice. l Nizam, S. , Spencer, S. S. (2004). An approach to the evaluation of a patient for seizures and epilepsy. Wisconsin Medical Journal. 103: 1. l British Paediatric Neurology Association. (2013). Paediatric Epilepsy Training Level One Handbook. United Kingdom.
l Thank you
 Lightning thief chapter 2
Lightning thief chapter 2 Limits fits and tolerances lecture notes
Limits fits and tolerances lecture notes Unilateral tolerance definition
Unilateral tolerance definition 50h8 tolerance
50h8 tolerance Percy jackson chapter 12 pdf
Percy jackson chapter 12 pdf Grover's algorithm multiple solutions
Grover's algorithm multiple solutions Why does percy feel ashamed that poseidon saved him
Why does percy feel ashamed that poseidon saved him Christen brun
Christen brun How does grover lose his pants
How does grover lose his pants Percy jackson lightning thief chapter 11
Percy jackson lightning thief chapter 11 Grover underwood
Grover underwood Why does grover say he retrieved the minotaur horn?
Why does grover say he retrieved the minotaur horn? Mona grover
Mona grover Anil kumar nmr
Anil kumar nmr Grover
Grover Robert grover dds
Robert grover dds Political bosses apush
Political bosses apush Goals of the populist party
Goals of the populist party Which fits best in the empty box above?
Which fits best in the empty box above? Strange fits of passion text
Strange fits of passion text Security that fits everywhere
Security that fits everywhere Find the value of
Find the value of Judicial restraint clipart
Judicial restraint clipart Practice 11-1 tangent lines
Practice 11-1 tangent lines Most common blood type in europe
Most common blood type in europe Two signal words used on whmis 2015 labels
Two signal words used on whmis 2015 labels One size fits all
One size fits all Difference between inductive and analytical learning
Difference between inductive and analytical learning A belt fits tightly around two pulleys
A belt fits tightly around two pulleys