Syncope Faints Funny Turns When to reassure or




- Slides: 28

Syncope: Faints & Funny Turns. When to reassure or refer Dr Peter Lillitos Paediatric Cardiology Registrar Leeds Children’s Hospital
House keeping QUESTIONS AT THE END MICROPHONES ON MUTE NO RECORDING PLEASE
Objectives • Understand the range of presentations of syncope from infancy to young person • Appreciate the physiology behind syncope • Understand the diagnostic usefulness of taking a good history, clinical examination and 12 lead-ECG • Know the Red-Flags in history • When to reassure; When to refer
Resources: Harris M, Bu’Lock F. Arch Dis Child Educ Pract Ed 2016; 101: 26– 30. doi: 10. 1136/archdischild-2015 -308422 - https: //www. networks. nhs. uk/nhs-networks/yorkshire-andhumber-congenital-cardiac-network STARS. org


Pre-syncope - definition • Feeling one is about to pass out, transient loss of postural tone
Syncope - definition • Syncope is a transient, but complete, loss of consciousness (with associated loss of muscle tone) due to global cerebral hypoperfusion By definition: ▸ rapid onset ▸ short duration (<1 min) ▸ Recovery is – quick – spontaneous – complete
What is not syncope: This excludes: • Falls, without loss of consciousness • States of altered consciousness • Prolonged LOC • Epileptic seizures • Psychogenic collapse/movements
Prevalence • 15 -20% children & YP have syncopal event between 8 -18 yrs • Before 6 yrs syncope is unusual – unless breath holds, reflex anoxic faints
Johnson, E. R. , Etheridge, S. P. , Minich, L. L. et al. Pediatr Cardiol (2014) 35: 753. https: //doi. org/10. 1007/s 00246 -013 -0848 -4 • Referrals for tertiary opinions occupy a lot of time in paediatric cardiology and neurology clinics (5. 8% of paediatric cardiology clinic referrals in a 1 year period in a US Centre) • Sudden cardiac death is rare (0. 6– 8. 5 deaths/100 000 patient years) • Sensitivity of screening using history, examination and 12 -lead ECG findings can be 100% sensitive for the cardiac causes of syncope
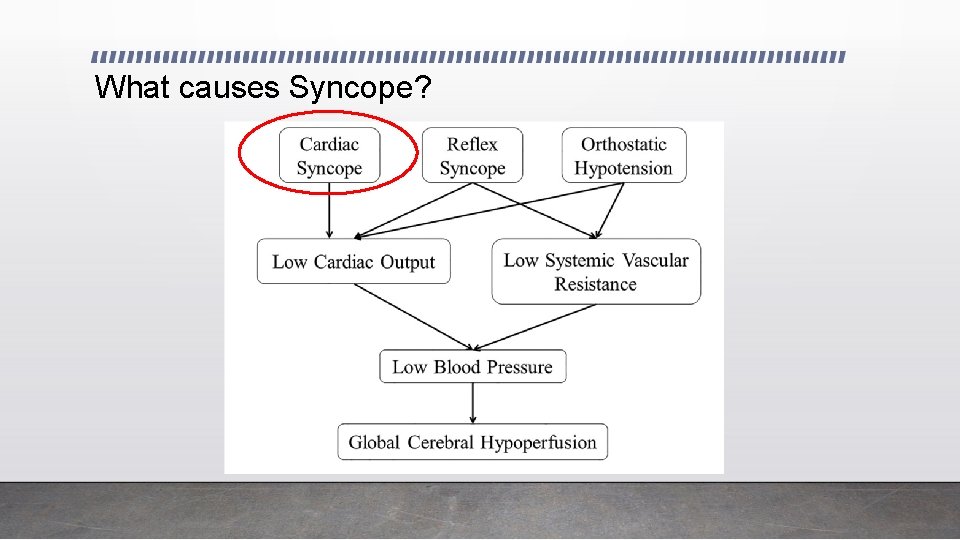
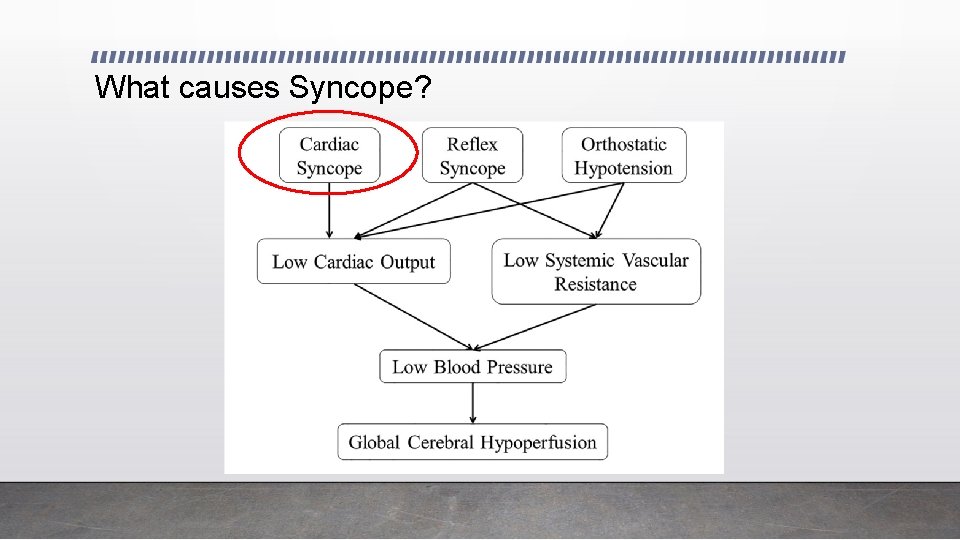
What causes Syncope?
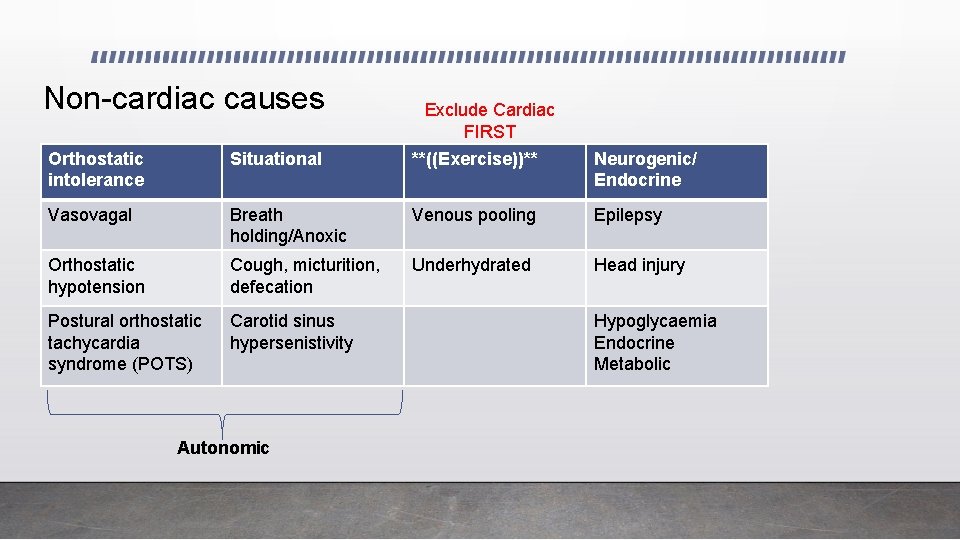
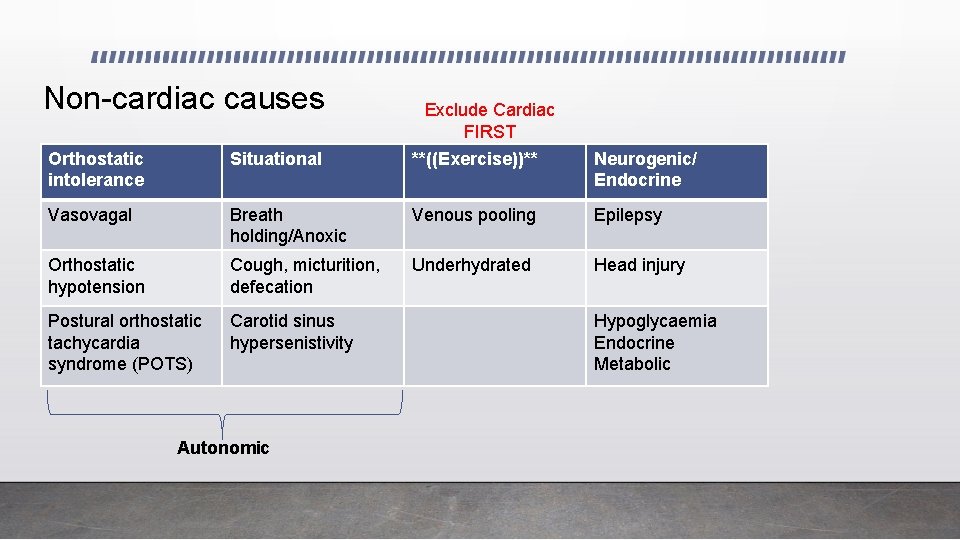
Non-cardiac causes Exclude Cardiac FIRST Orthostatic intolerance Situational **((Exercise))** Neurogenic/ Endocrine Vasovagal Breath holding/Anoxic Venous pooling Epilepsy Orthostatic hypotension Cough, micturition, defecation Underhydrated Head injury Postural orthostatic tachycardia syndrome (POTS) Carotid sinus hypersenistivity Autonomic Hypoglycaemia Endocrine Metabolic
Cardiac syncope Electrical Structural/ Functional
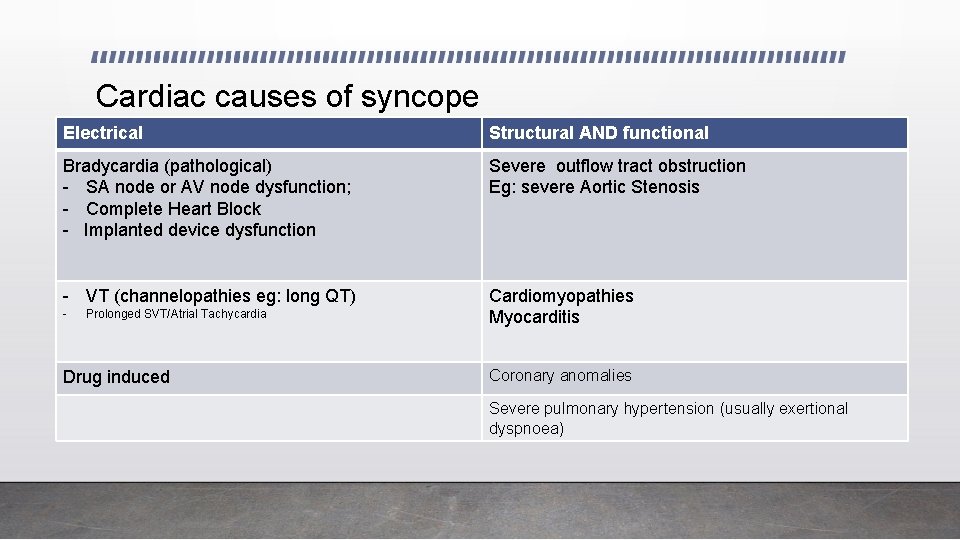
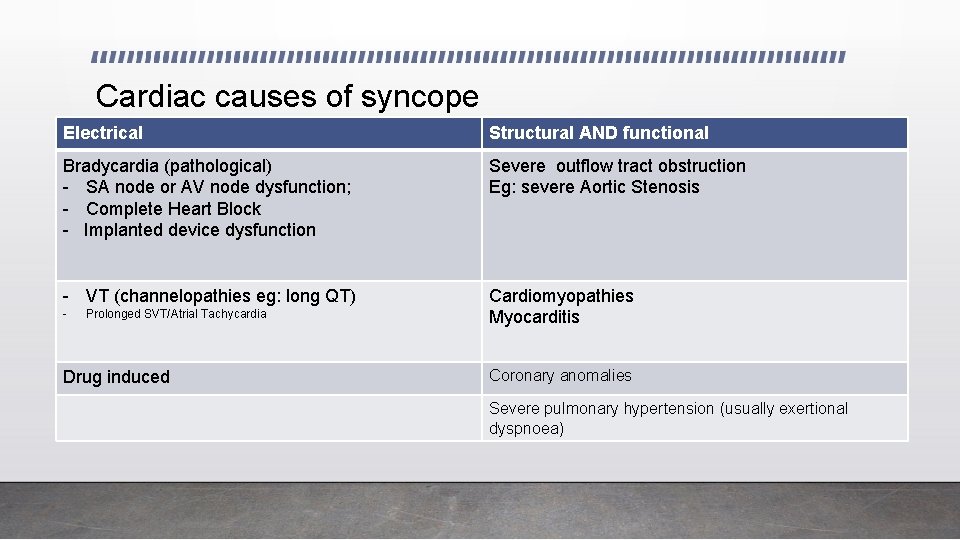
Cardiac causes of syncope Electrical Structural AND functional Bradycardia (pathological) - SA node or AV node dysfunction; - Complete Heart Block - Implanted device dysfunction Severe outflow tract obstruction Eg: severe Aortic Stenosis - VT (channelopathies eg: long QT) Cardiomyopathies Myocarditis - Prolonged SVT/Atrial Tachycardia Drug induced Coronary anomalies Severe pulmonary hypertension (usually exertional dyspnoea)
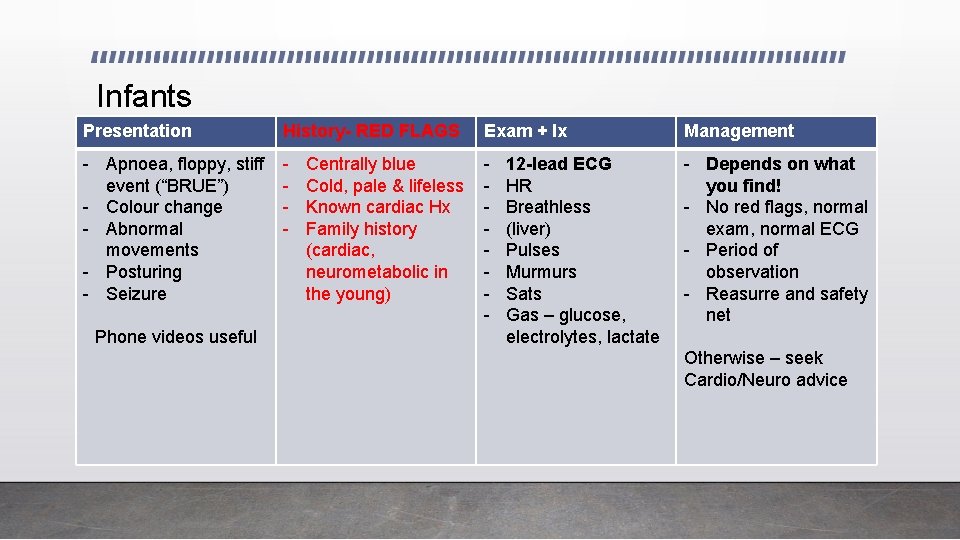
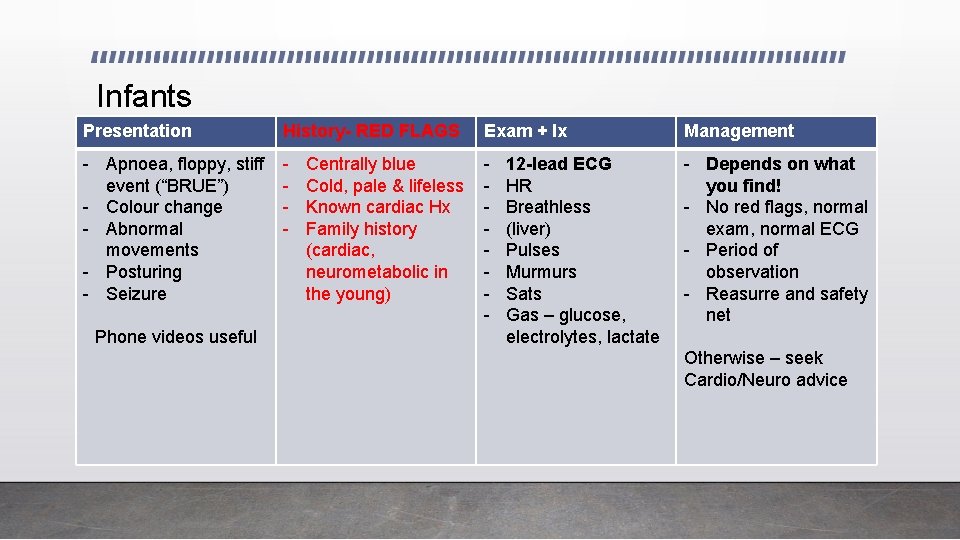
Infants Presentation History- RED FLAGS Exam + Ix Management - Apnoea, floppy, stiff event (“BRUE”) - Colour change - Abnormal movements - Posturing - Seizure - - - Depends on what you find! - No red flags, normal exam, normal ECG - Period of observation - Reasurre and safety net Phone videos useful Centrally blue Cold, pale & lifeless Known cardiac Hx Family history (cardiac, neurometabolic in the young) 12 -lead ECG HR Breathless (liver) Pulses Murmurs Sats Gas – glucose, electrolytes, lactate Otherwise – seek Cardio/Neuro advice
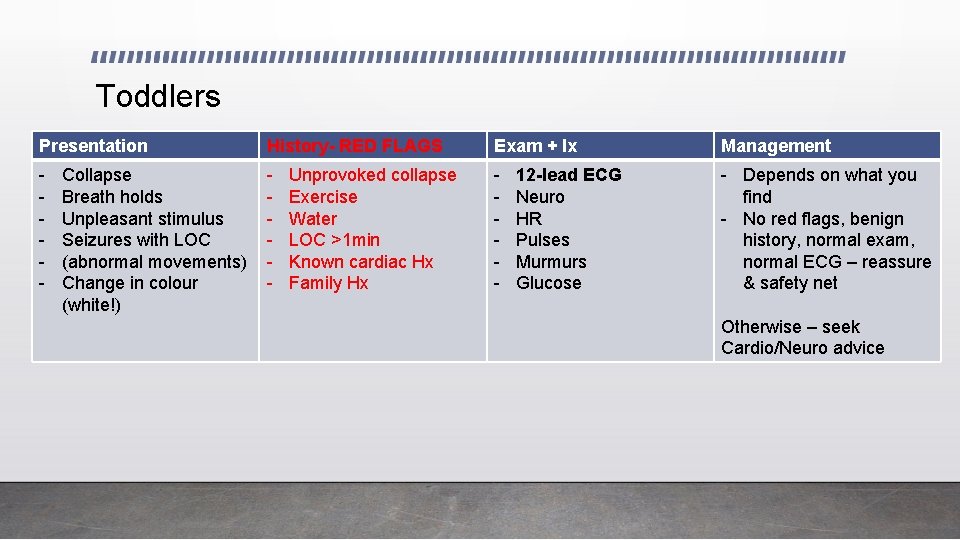
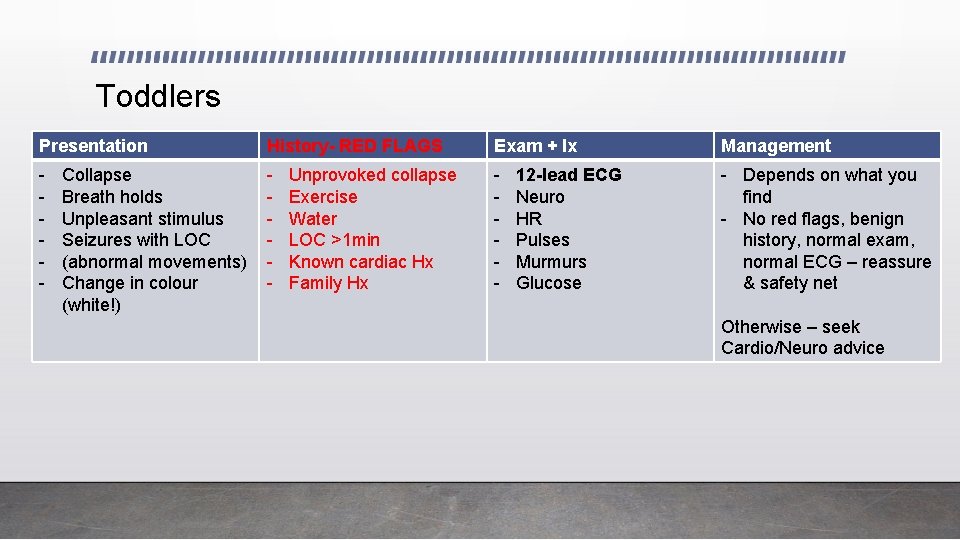
Toddlers Presentation History- RED FLAGS Exam + Ix Management - - Depends on what you find - No red flags, benign history, normal exam, normal ECG – reassure & safety net Collapse Breath holds Unpleasant stimulus Seizures with LOC (abnormal movements) Change in colour (white!) Unprovoked collapse Exercise Water LOC >1 min Known cardiac Hx Family Hx 12 -lead ECG Neuro HR Pulses Murmurs Glucose Otherwise – seek Cardio/Neuro advice
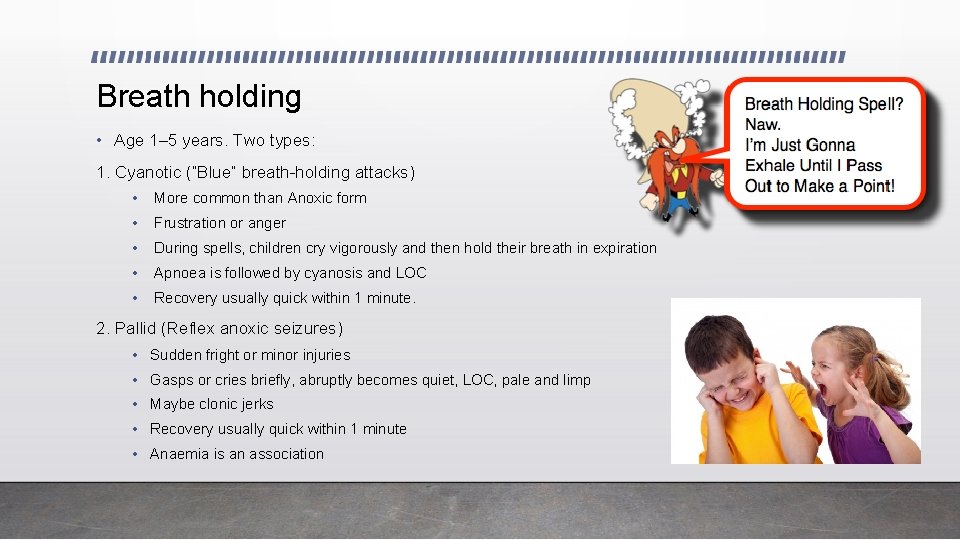
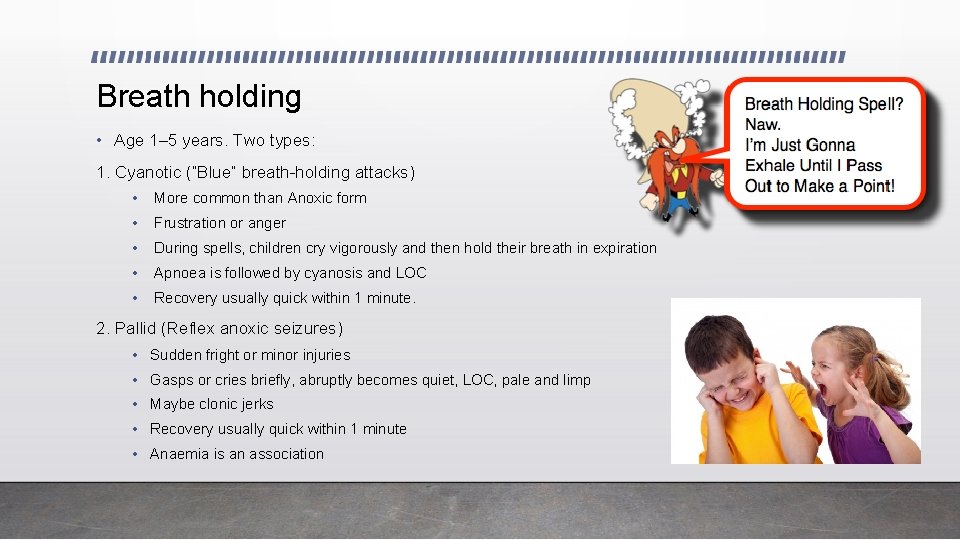
Breath holding • Age 1– 5 years. Two types: 1. Cyanotic (“Blue” breath-holding attacks) • More common than Anoxic form • Frustration or anger • During spells, children cry vigorously and then hold their breath in expiration • Apnoea is followed by cyanosis and LOC • Recovery usually quick within 1 minute. 2. Pallid (Reflex anoxic seizures) • Sudden fright or minor injuries • Gasps or cries briefly, abruptly becomes quiet, LOC, pale and limp • Maybe clonic jerks • Recovery usually quick within 1 minute • Anaemia is an association
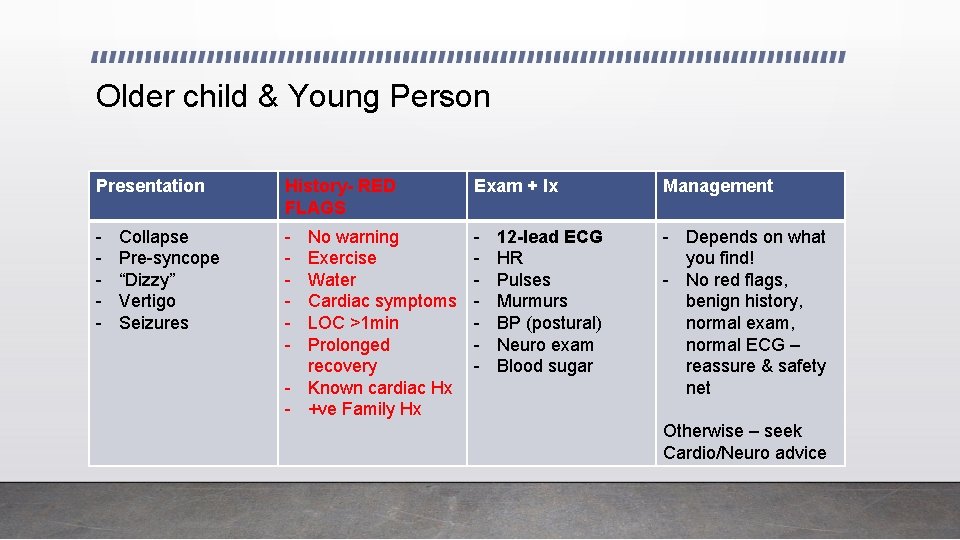
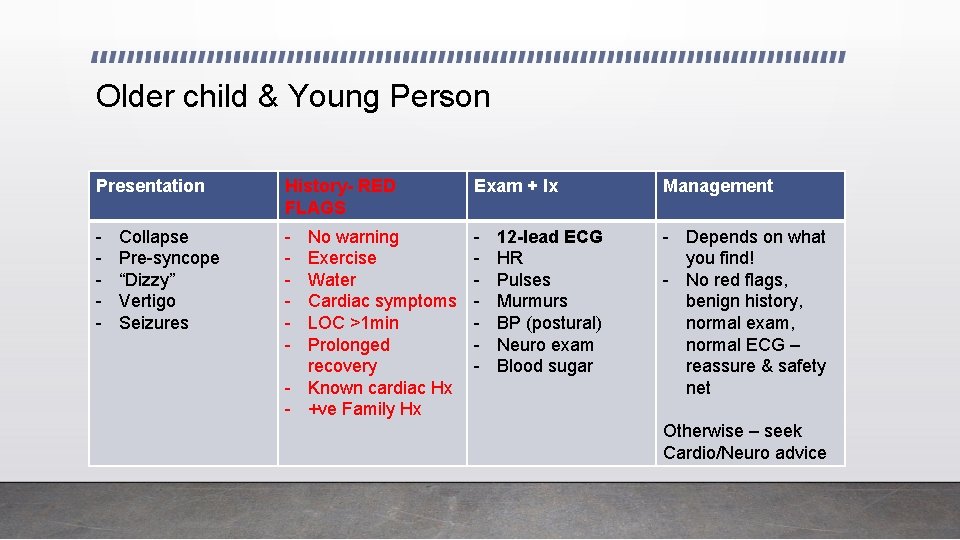
Older child & Young Person Presentation History- RED FLAGS Exam + Ix Management - - Depends on what you find! - No red flags, benign history, normal exam, normal ECG – reassure & safety net Collapse Pre-syncope “Dizzy” Vertigo Seizures No warning Exercise Water Cardiac symptoms LOC >1 min Prolonged recovery - Known cardiac Hx - +ve Family Hx 12 -lead ECG HR Pulses Murmurs BP (postural) Neuro exam Blood sugar Otherwise – seek Cardio/Neuro advice
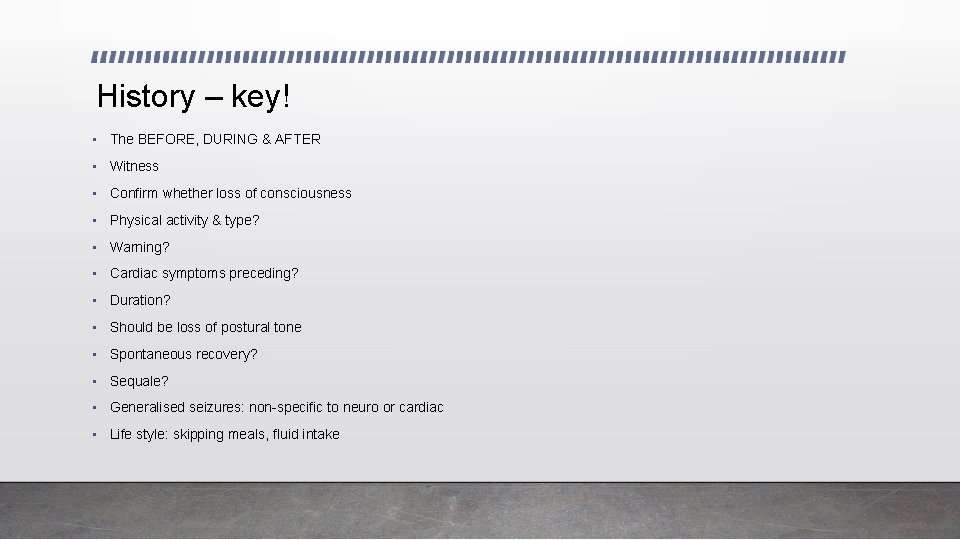
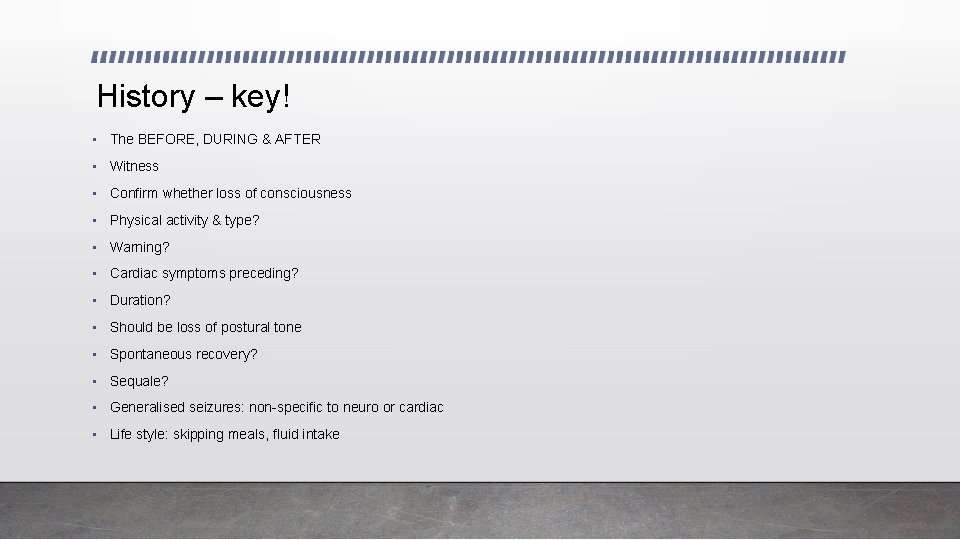
History – key! • The BEFORE, DURING & AFTER • Witness • Confirm whether loss of consciousness • Physical activity & type? • Warning? • Cardiac symptoms preceding? • Duration? • Should be loss of postural tone • Spontaneous recovery? • Sequale? • Generalised seizures: non-specific to neuro or cardiac • Life style: skipping meals, fluid intake
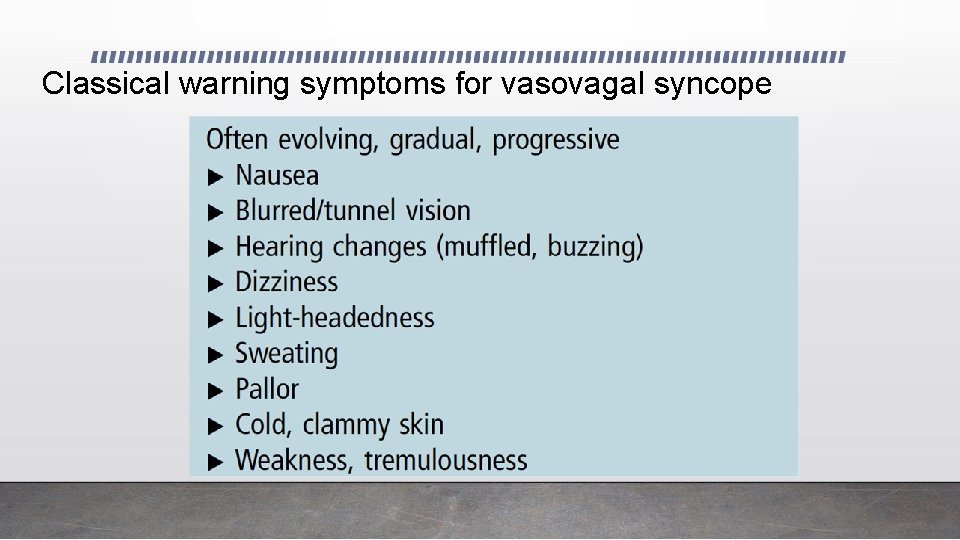
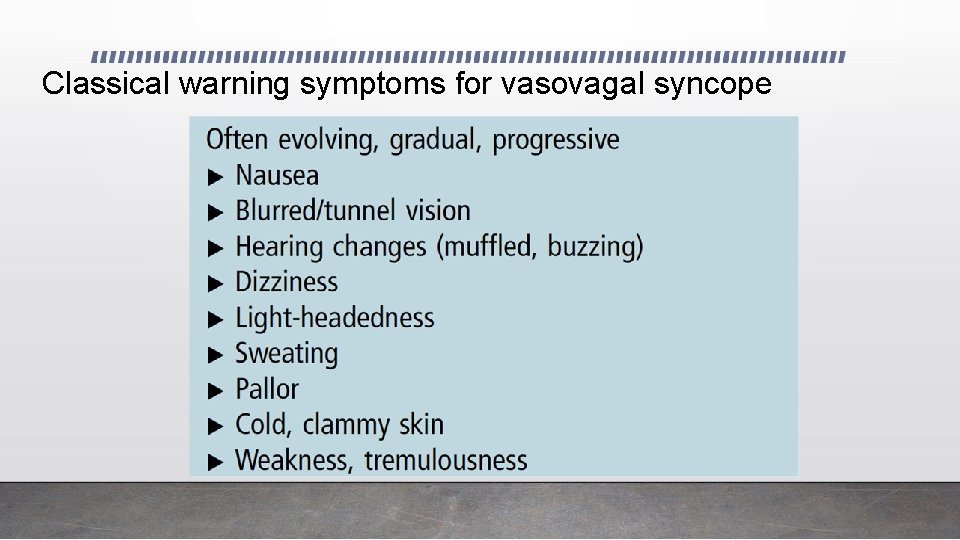
Classical warning symptoms for vasovagal syncope
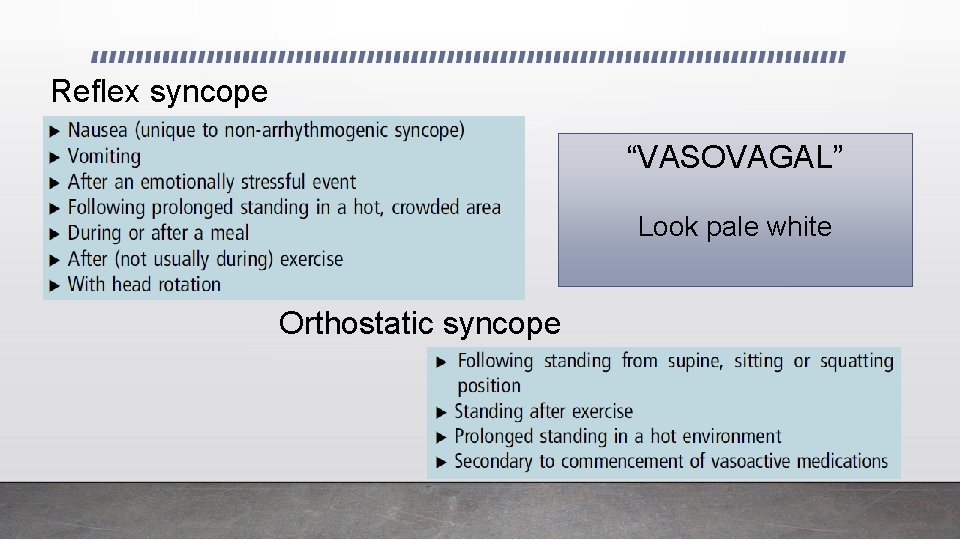
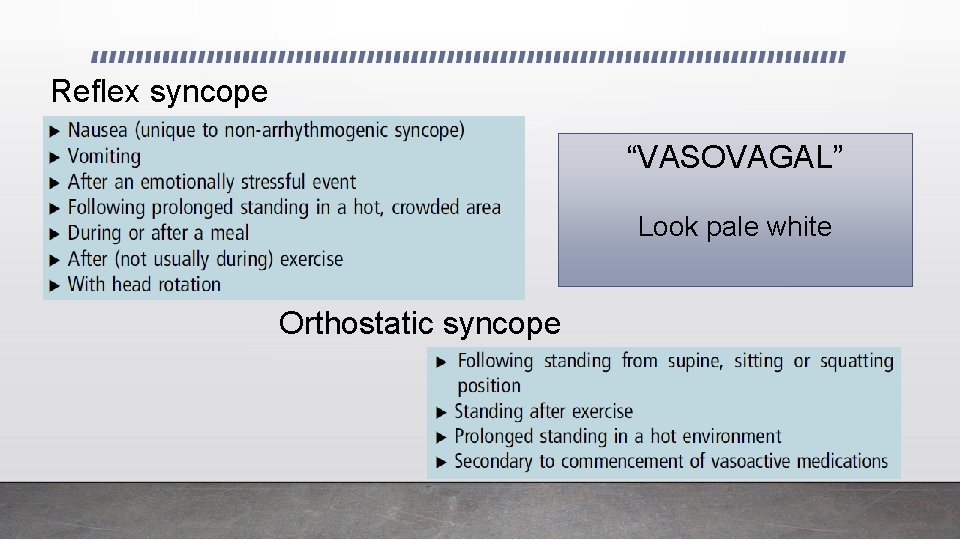
Reflex syncope “VASOVAGAL” Look pale white Orthostatic syncope

Cardiac red-flags - under age of 40 yrs Non-cardiac syncope can coexist with cardiac, so investigate if suspicious
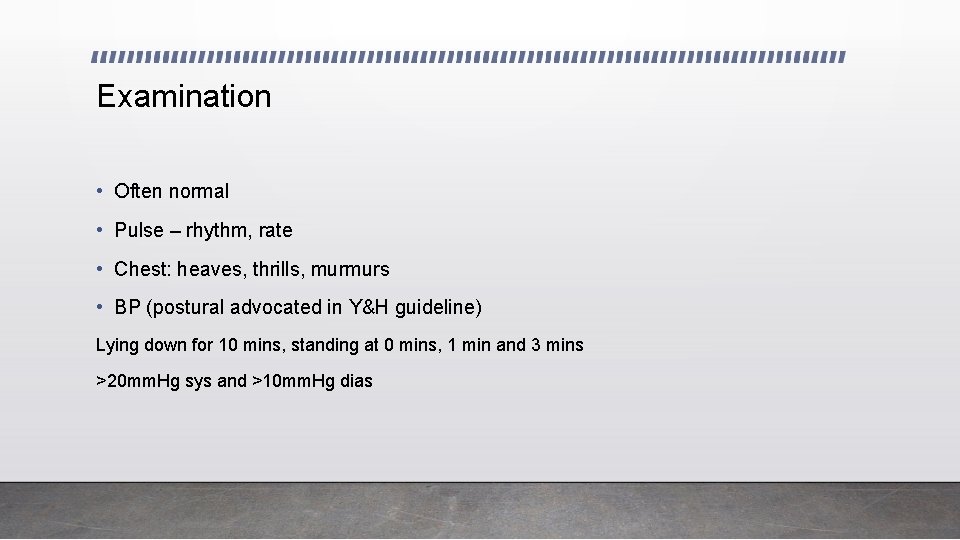
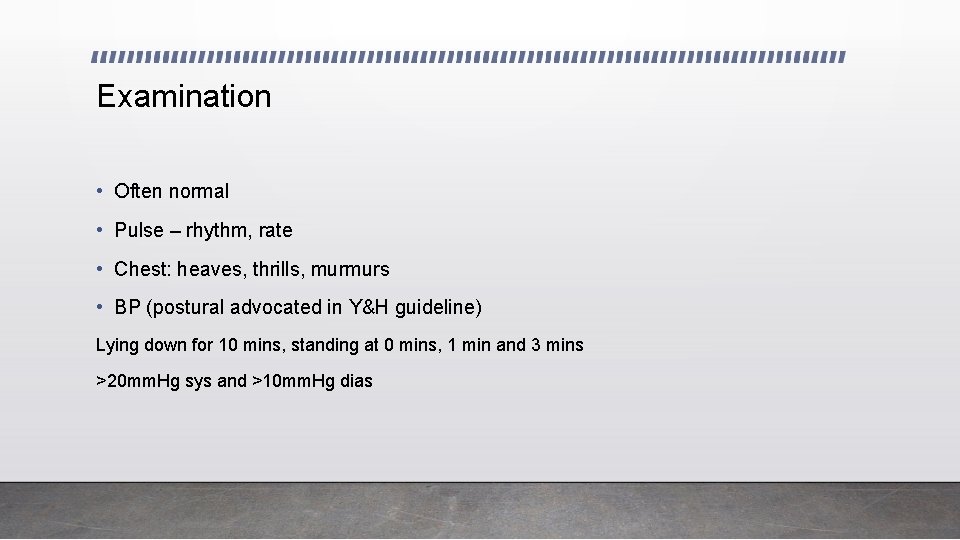
Examination • Often normal • Pulse – rhythm, rate • Chest: heaves, thrills, murmurs • BP (postural advocated in Y&H guideline) Lying down for 10 mins, standing at 0 mins, 1 min and 3 mins >20 mm. Hg sys and >10 mm. Hg dias
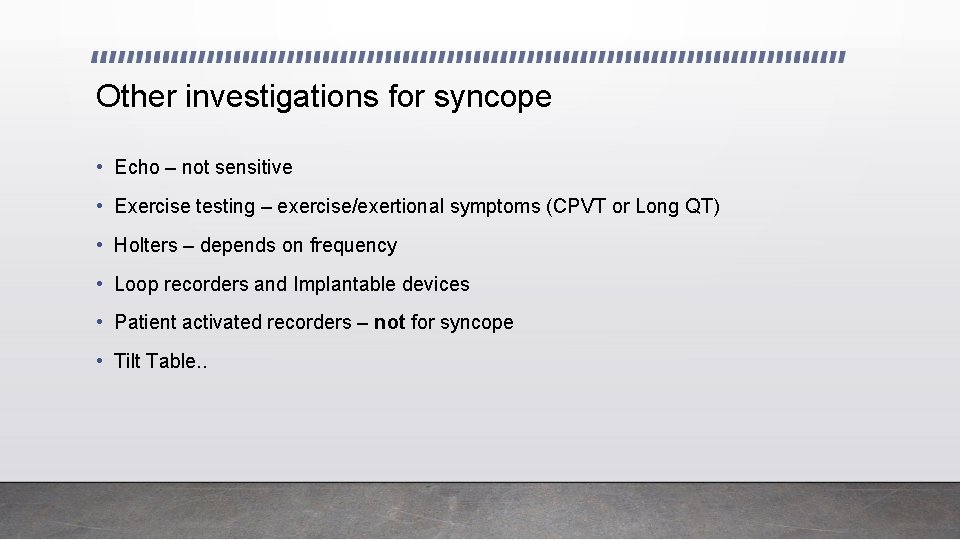
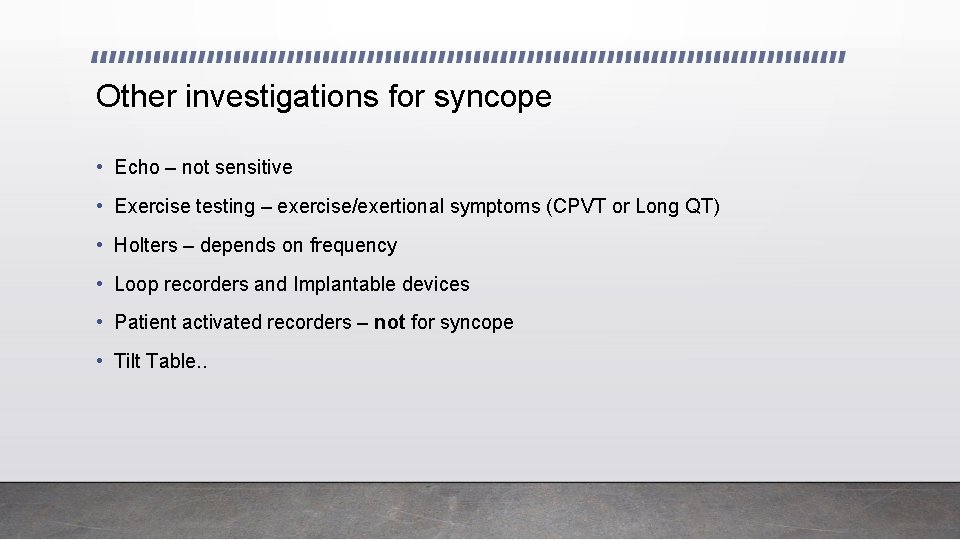
Other investigations for syncope • Echo – not sensitive • Exercise testing – exercise/exertional symptoms (CPVT or Long QT) • Holters – depends on frequency • Loop recorders and Implantable devices • Patient activated recorders – not for syncope • Tilt Table. .
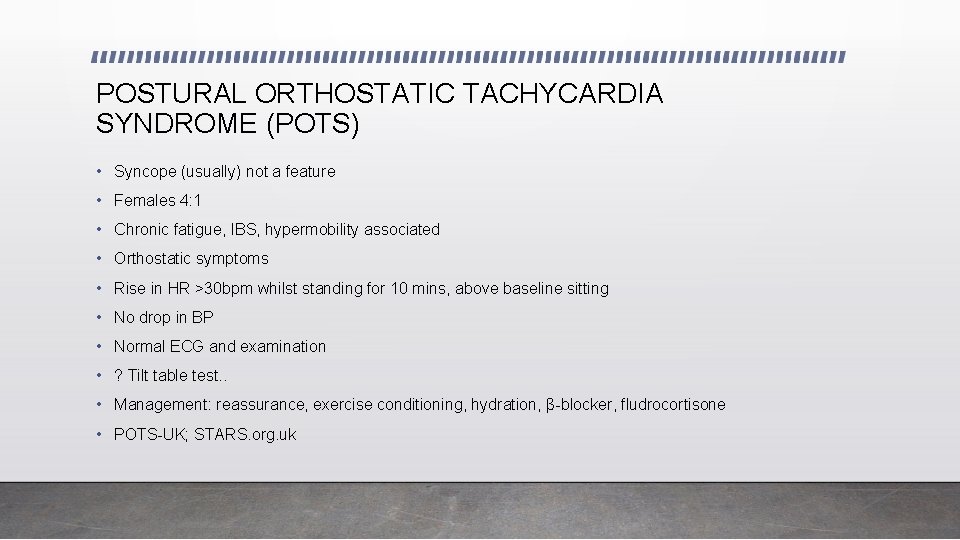
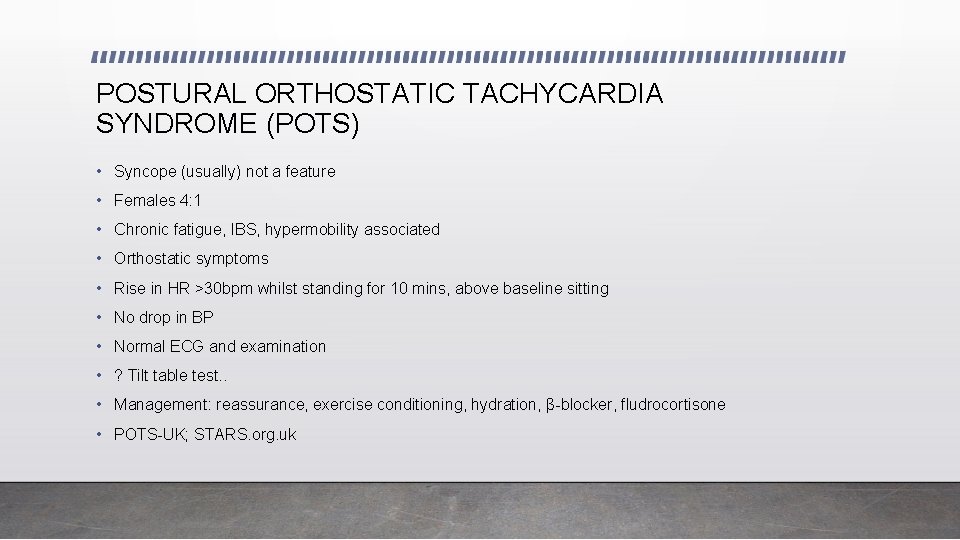
POSTURAL ORTHOSTATIC TACHYCARDIA SYNDROME (POTS) • Syncope (usually) not a feature • Females 4: 1 • Chronic fatigue, IBS, hypermobility associated • Orthostatic symptoms • Rise in HR >30 bpm whilst standing for 10 mins, above baseline sitting • No drop in BP • Normal ECG and examination • ? Tilt table test. . • Management: reassurance, exercise conditioning, hydration, β-blocker, fludrocortisone • POTS-UK; STARS. org. uk
Management for Orthostatic symptoms • Lifestyle (hydration, meals, add salt in diet) • Postural exercises • Muscle pump exercises • Head down, lie down, legs up
Summary: When to reassure or refer • History typical of non-cardiac (non-neuro-metabolic) • No cardiac red flags in history or family history • Normal CVS examination • Normal ECG - Reassure • Non-typical history for benign causes or suggests neurological • Red-flags for cardiac in history/family history • Abnormal examination • Abnormal ECG - Refer https: //www. networks. nhs. uk/nhs-networks/yorkshire-and-humber-congenital-cardiac-network
 Syncope vs seizure
Syncope vs seizure Nursing diagnosis for pulmonary embolism
Nursing diagnosis for pulmonary embolism Syncopale def
Syncopale def Syncope
Syncope Syncope in the older patient is
Syncope in the older patient is Complications of local anesthesia in dentistry
Complications of local anesthesia in dentistry Syncope
Syncope Syncope vs seizure
Syncope vs seizure Snycope
Snycope Syncope
Syncope When parking at an angle the motorist should position
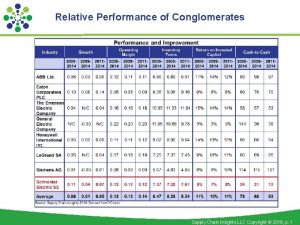
When parking at an angle the motorist should position Inventory turns
Inventory turns Lever image
Lever image One year old marcus turns away in disgust of a bitter
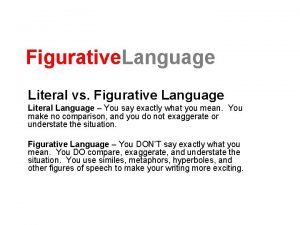
One year old marcus turns away in disgust of a bitter Literal and figurative language
Literal and figurative language A car on a level road turns a quarter circle ccw
A car on a level road turns a quarter circle ccw Wrist turns
Wrist turns Which shaft will turn most slowly
Which shaft will turn most slowly Cultural and ideological turns
Cultural and ideological turns Jesus turns water into wine lesson
Jesus turns water into wine lesson Inspector of turns
Inspector of turns During the time interval
During the time interval Inventory turns
Inventory turns Grant always turns in his homework
Grant always turns in his homework The zebras cried when the wise old elephant died
The zebras cried when the wise old elephant died H3po4 + mg(oh)2 balanced equation
H3po4 + mg(oh)2 balanced equation An archaeological dig turns up large numbers
An archaeological dig turns up large numbers I was in that state when a chap easily turns nasty analysis
I was in that state when a chap easily turns nasty analysis Robert pushes the box to the left
Robert pushes the box to the left