Confirmed VTE Treatment Pathway excludes VTE in pregnancy
- Slides: 1
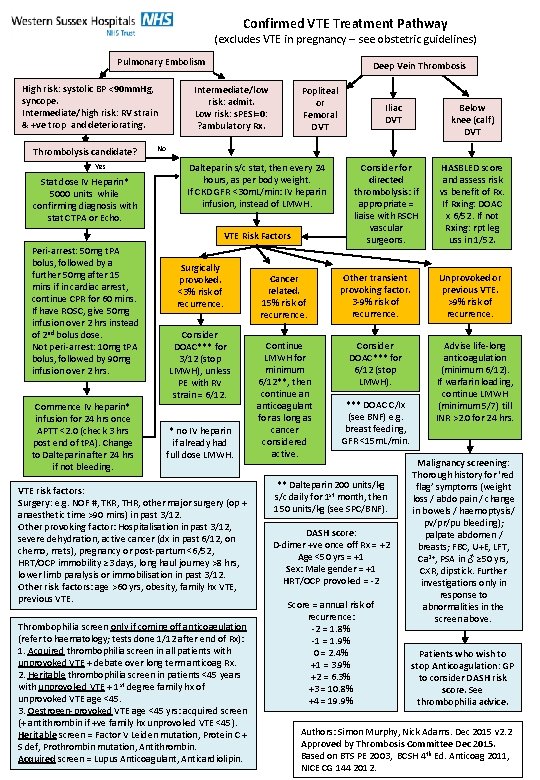
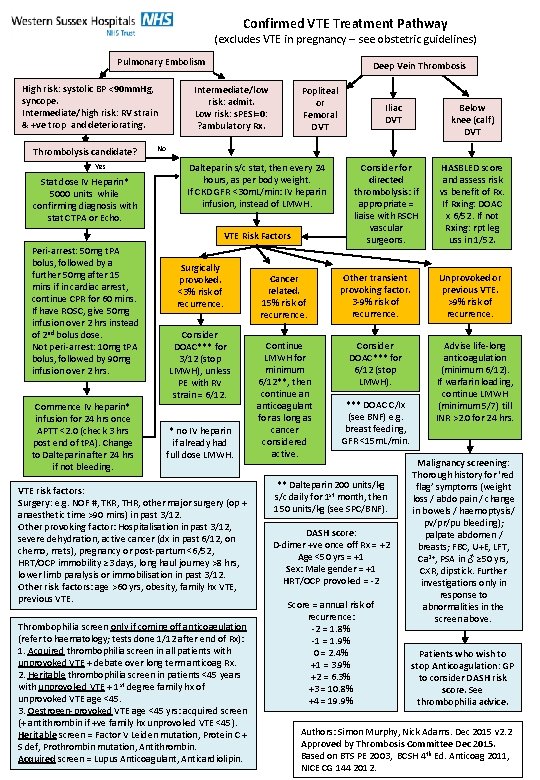
Confirmed VTE Treatment Pathway (excludes VTE in pregnancy – see obstetric guidelines) Pulmonary Embolism High risk: systolic BP <90 mm. Hg, syncope. Intermediate/high risk: RV strain & +ve trop and deteriorating. Thrombolysis candidate? Yes Stat dose IV Heparin* 5000 units while confirming diagnosis with stat CTPA or Echo. Deep Vein Thrombosis Intermediate/low risk: admit. Low risk: s. PESI=0: ? ambulatory Rx. Popliteal or Femoral DVT Commence IV heparin* infusion for 24 hrs once APTT <2. 0 (check 3 hrs post end of t. PA). Change to Dalteparin after 24 hrs if not bleeding. Below knee (calf) DVT No Dalteparin s/c stat, then every 24 hours, as per body weight. If CKD GFR <30 m. L/min: IV heparin infusion, instead of LMWH. VTE Risk Factors Peri-arrest: 50 mg t. PA bolus, followed by a further 50 mg after 15 mins if in cardiac arrest, continue CPR for 60 mins. If have ROSC, give 50 mg infusion over 2 hrs instead of 2 nd bolus dose. Not peri-arrest: 10 mg t. PA bolus, followed by 90 mg infusion over 2 hrs. Iliac DVT Surgically provoked. <3% risk of recurrence. Consider DOAC*** for 3/12 (stop LMWH), unless PE with RV strain = 6/12. * no IV heparin if already had full dose LMWH. VTE risk factors: Surgery: e. g. NOF #, TKR, THR, other major surgery (op + anaesthetic time >90 mins) in past 3/12. Other provoking factor: Hospitalisation in past 3/12, severe dehydration, active cancer (dx in past 6/12, on chemo, mets), pregnancy or post-partum <6/52, HRT/OCP immobility ≥ 3 days, long haul journey >8 hrs, lower limb paralysis or immobilisation in past 3/12. Other risk factors: age >60 yrs, obesity, family hx VTE, previous VTE. Thrombophilia screen only if coming off anticoagulation (refer to haematology; tests done 1/12 after end of Rx): 1. Acquired thrombophilia screen in all patients with unprovoked VTE + debate over long term anticoag Rx. 2. Heritable thrombophilia screen in patients <45 years with unprovoked VTE + 1 st degree family hx of unprovoked VTE age <45. 3. Oestrogen-provoked VTE age <45 yrs: acquired screen (+ antithrombin if +ve family hx unprovoked VTE <45). Heritable screen = Factor V Leiden mutation, Protein C + S def, Prothrombin mutation, Antithrombin. Acquired screen = Lupus Anticoagulant, Anticardiolipin. Consider for directed thrombolysis: if appropriate = liaise with RSCH vascular surgeons. Cancer related. 15% risk of recurrence. Other transient provoking factor. 3 -9% risk of recurrence. Continue LMWH for minimum 6/12**, then continue an anticoagulant for as long as cancer considered active. Consider DOAC*** for 6/12 (stop LMWH). *** DOAC C/Ix (see BNF) e. g. breast feeding, GFR <15 m. L/min. ** Dalteparin 200 units/kg s/c daily for 1 st month, then 150 units/kg (see SPC/BNF). DASH score: D-dimer +ve once off Rx = +2 Age <50 yrs = +1 Sex: Male gender = +1 HRT/OCP provoked = -2 Score = annual risk of recurrence: -2 = 1. 8% -1 = 1. 9% 0 = 2. 4% +1 = 3. 9% +2 = 6. 3% +3 = 10. 8% +4 = 19. 9% HASBLED score and assess risk vs benefit of Rx. If Rxing: DOAC x 6/52. If not Rxing: rpt leg uss in 1/52. Unprovoked or previous VTE. >9% risk of recurrence. Advise life-long anticoagulation (minimum 6/12). If warfarin loading, continue LMWH (minimum 5/7) till INR >2. 0 for 24 hrs. Malignancy screening: Thorough history for ‘red flag’ symptoms (weight loss / abdo pain / change in bowels / haemoptysis/ pv/pr/pu bleeding); palpate abdomen / breasts; FBC, U+E, LFT, Ca 2+, PSA in ♂ ≥ 50 yrs, CXR, dipstick. Further investigations only in response to abnormalities in the screen above. Patients who wish to stop Anticoagulation: GP to consider DASH risk score. See thrombophilia advice. Authors: Simon Murphy, Nick Adams. Dec 2015 v 2. 2 Approved by Thrombosis Committee Dec 2015. Based on BTS PE 2003, BCSH 4 th Ed. Anticoag 2011, NICE CG 144 2012.