Thyroid Physiology Seretion of thyroid hormones T 3









- Slides: 111
Thyroid
Physiology Seretion of thyroid hormones – T 3, T 4, calcitonine Iodine: 100 microgrames; 30% absorbed in digestive tract Capture in thyroid gland – oxidation (peroxidaze) – transportation in coloid (thyroglobuline) – iodisation of thirozine – MIT, DIT –T 3, T 4 – blood stream
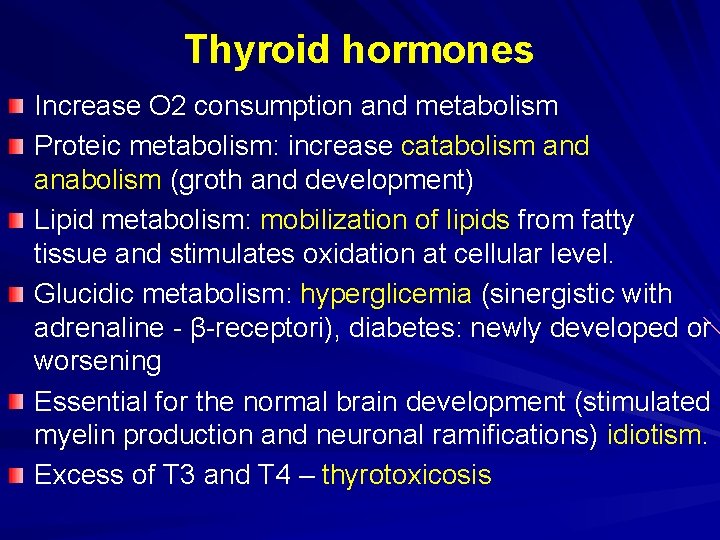
Thyroid hormones Increase O 2 consumption and metabolism Proteic metabolism: increase catabolism and anabolism (groth and development) Lipid metabolism: mobilization of lipids from fatty tissue and stimulates oxidation at cellular level. Glucidic metabolism: hyperglicemia (sinergistic with adrenaline - β-receptori), diabetes: newly developed or worsening Essential for the normal brain development (stimulated myelin production and neuronal ramifications) idiotism. Excess of T 3 and T 4 – thyrotoxicosis
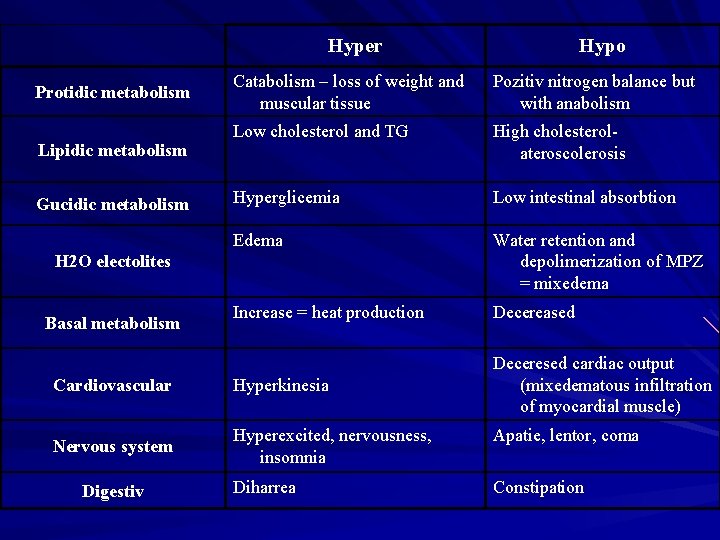
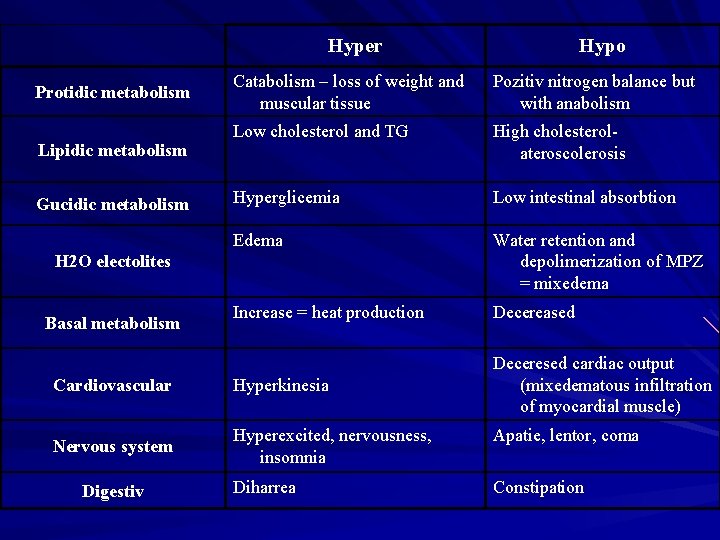
Hyper Hypo Catabolism – loss of weight and muscular tissue Pozitiv nitrogen balance but with anabolism Low cholesterol and TG High cholesterolateroscolerosis Hyperglicemia Low intestinal absorbtion Edema Water retention and depolimerization of MPZ = mixedema Increase = heat production Decereased Cardiovascular Hyperkinesia Deceresed cardiac output (mixedematous infiltration of myocardial muscle) Nervous system Hyperexcited, nervousness, insomnia Apatie, lentor, coma Diharrea Constipation Protidic metabolism Lipidic metabolism Gucidic metabolism H 2 O electolites Basal metabolism Digestiv
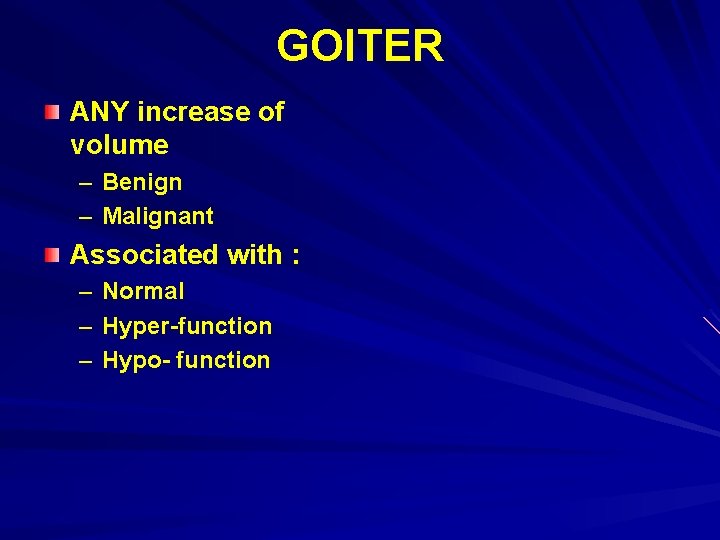
GOITER ANY increase of volume – Benign – Malignant Associated with : – – – Normal Hyper-function Hypo- function
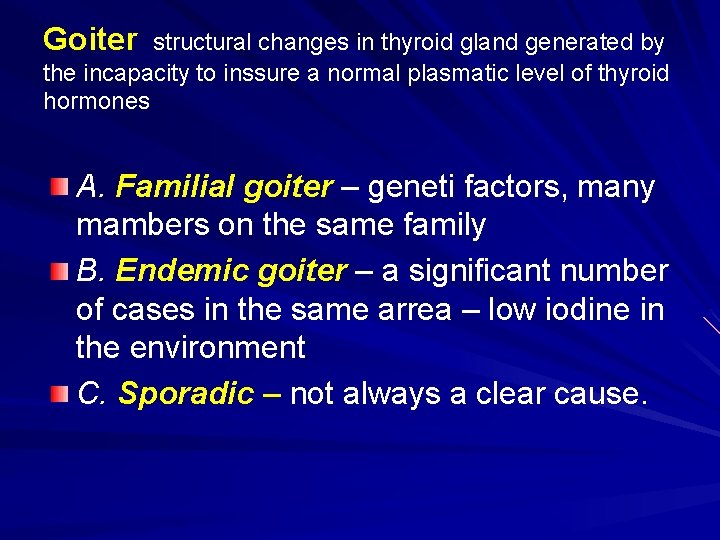
Goiter structural changes in thyroid gland generated by the incapacity to inssure a normal plasmatic level of thyroid hormones A. Familial goiter – geneti factors, many mambers on the same family B. Endemic goiter – a significant number of cases in the same arrea – low iodine in the environment C. Sporadic – not always a clear cause.
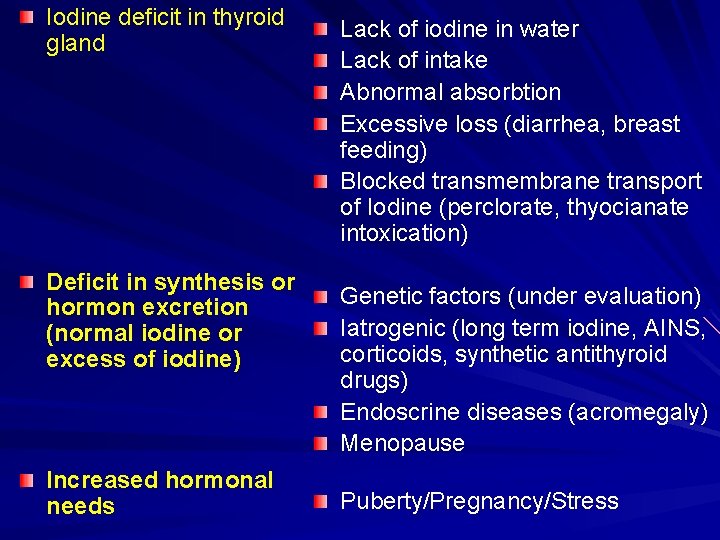
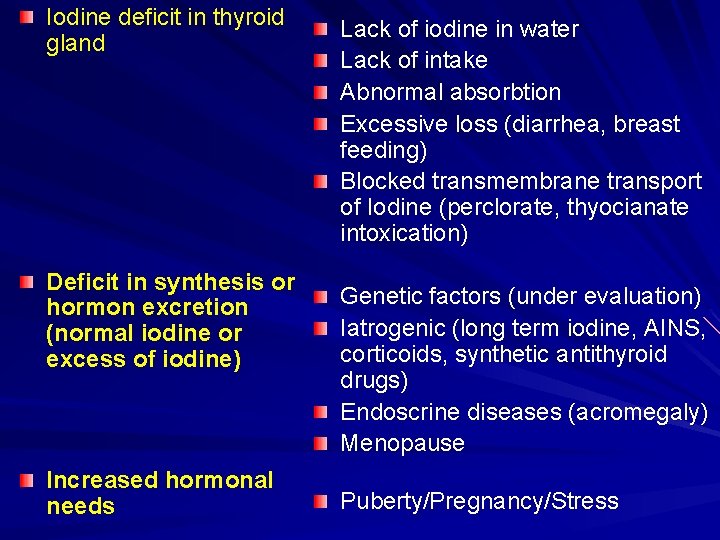
Iodine deficit in thyroid gland Deficit in synthesis or hormon excretion (normal iodine or excess of iodine) Increased hormonal needs Lack of iodine in water Lack of intake Abnormal absorbtion Excessive loss (diarrhea, breast feeding) Blocked transmembrane transport of Iodine (perclorate, thyocianate intoxication) Genetic factors (under evaluation) Iatrogenic (long term iodine, AINS, corticoids, synthetic antithyroid drugs) Endoscrine diseases (acromegaly) Menopause Puberty/Pregnancy/Stress

Pathology Difuse goiter Nodular goiter Adenomatous goiter Coloidal goiter Cystic goiter Vascular goiter Fibrotic goiter Calcified goiter
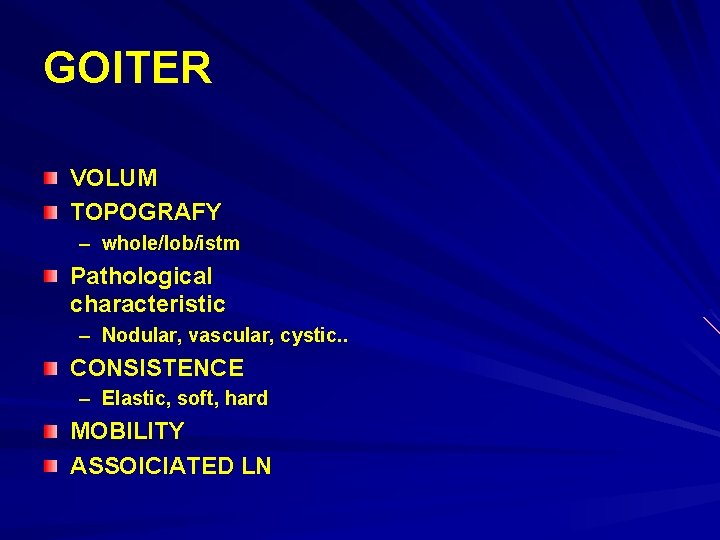
GOITER VOLUM TOPOGRAFY – whole/lob/istm Pathological characteristic – Nodular, vascular, cystic. . CONSISTENCE – Elastic, soft, hard MOBILITY ASSOICIATED LN
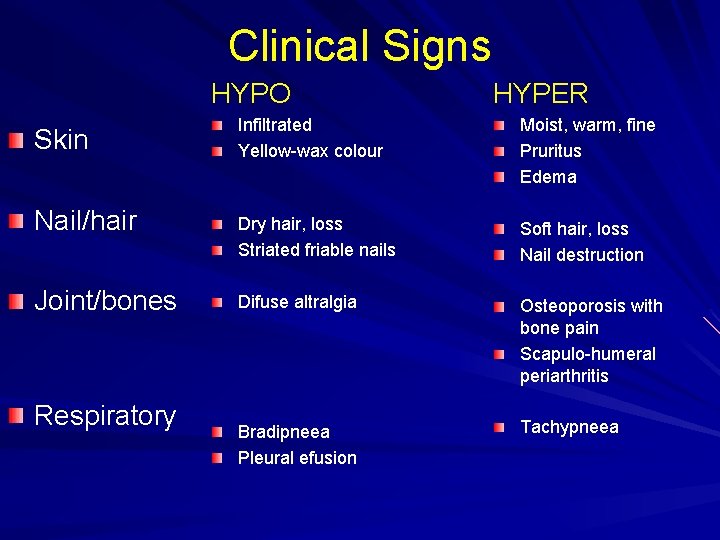
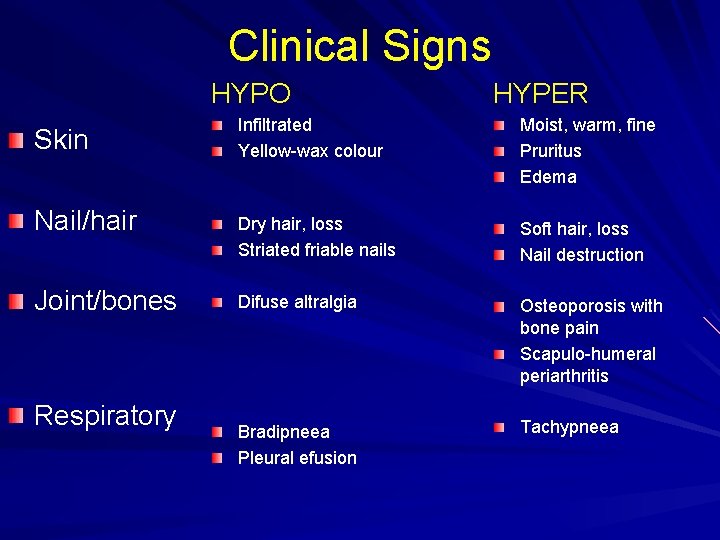
Clinical Signs HYPO Skin Nail/hair Joint/bones Respiratory HYPER Infiltrated Yellow-wax colour Moist, warm, fine Pruritus Edema Dry hair, loss Striated friable nails Soft hair, loss Nail destruction Difuse altralgia Osteoporosis with bone pain Scapulo-humeral periarthritis Bradipneea Pleural efusion Tachypneea
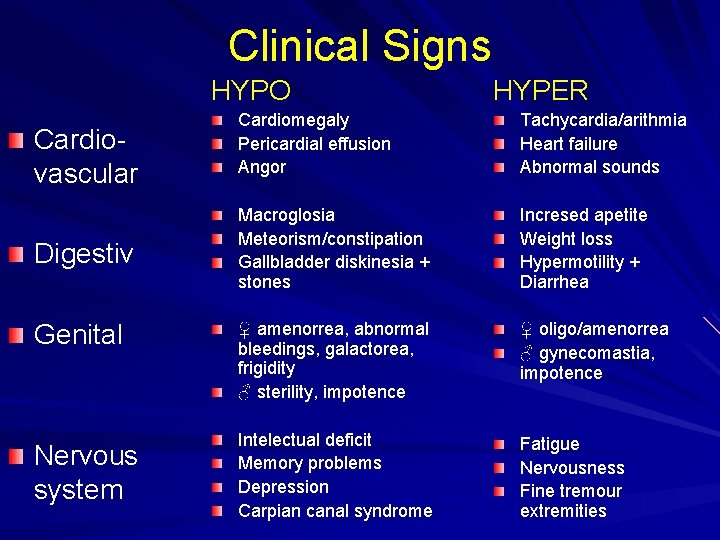
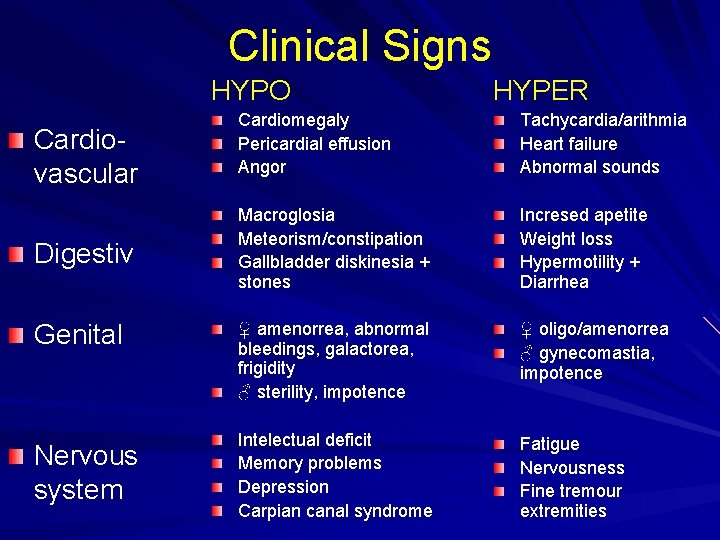
Clinical Signs HYPO Cardiovascular Digestiv Genital Nervous system HYPER Cardiomegaly Pericardial effusion Angor Tachycardia/arithmia Heart failure Abnormal sounds Macroglosia Meteorism/constipation Gallbladder diskinesia + stones Incresed apetite Weight loss Hypermotility + Diarrhea ♀ amenorrea, abnormal bleedings, galactorea, frigidity ♂ sterility, impotence ♀ oligo/amenorrea ♂ gynecomastia, impotence Intelectual deficit Memory problems Depression Carpian canal syndrome Fatigue Nervousness Fine tremour extremities
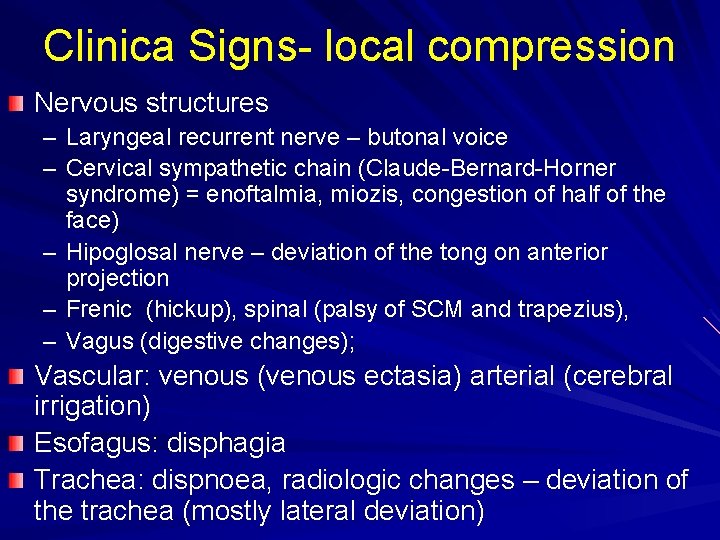
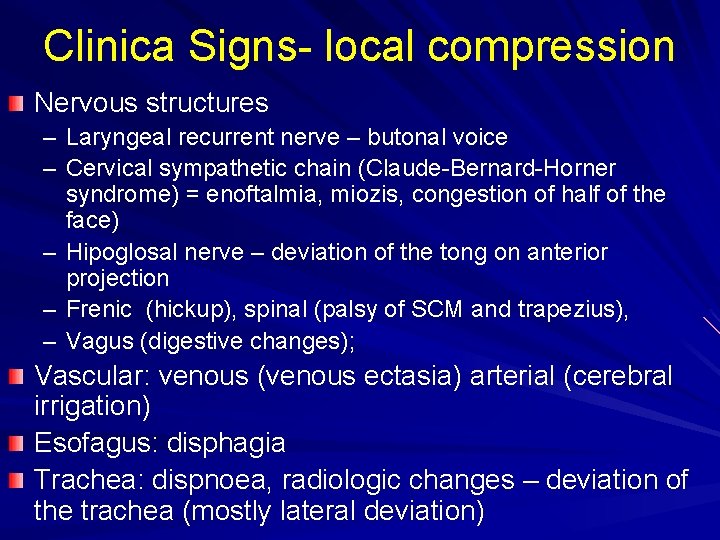
Clinica Signs- local compression Nervous structures – Laryngeal recurrent nerve – butonal voice – Cervical sympathetic chain (Claude-Bernard-Horner syndrome) = enoftalmia, miozis, congestion of half of the face) – Hipoglosal nerve – deviation of the tong on anterior projection – Frenic (hickup), spinal (palsy of SCM and trapezius), – Vagus (digestive changes); Vascular: venous (venous ectasia) arterial (cerebral irrigation) Esofagus: disphagia Trachea: dispnoea, radiologic changes – deviation of the trachea (mostly lateral deviation)
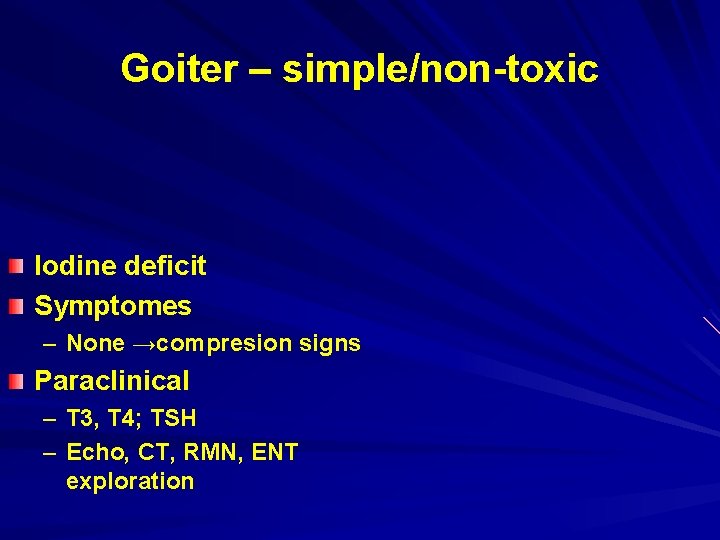
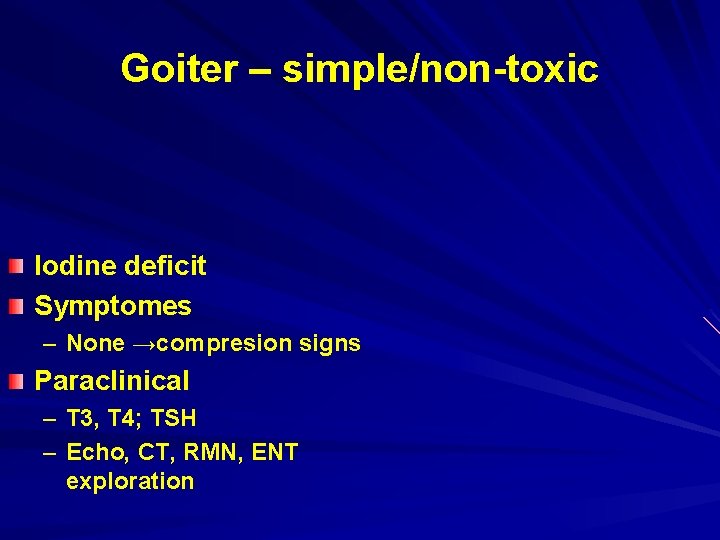
Goiter – simple/non-toxic Iodine deficit Symptomes – None →compresion signs Paraclinical – T 3, T 4; TSH – Echo, CT, RMN, ENT exploration

Goiter - simple SCINTIGRAM
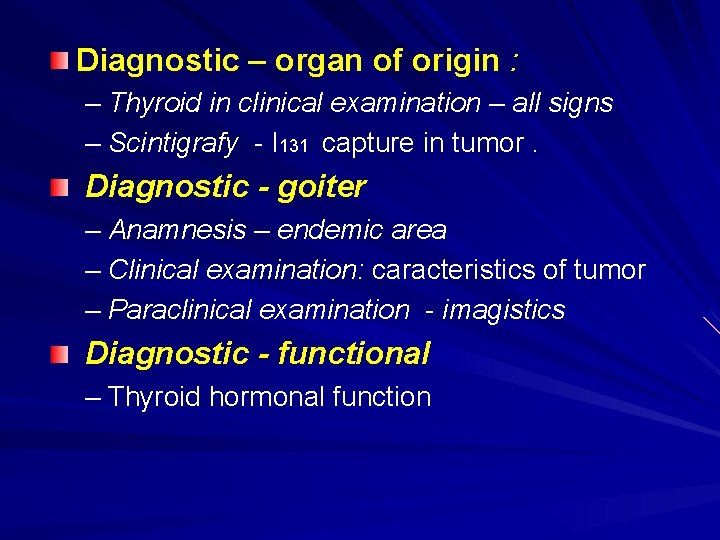
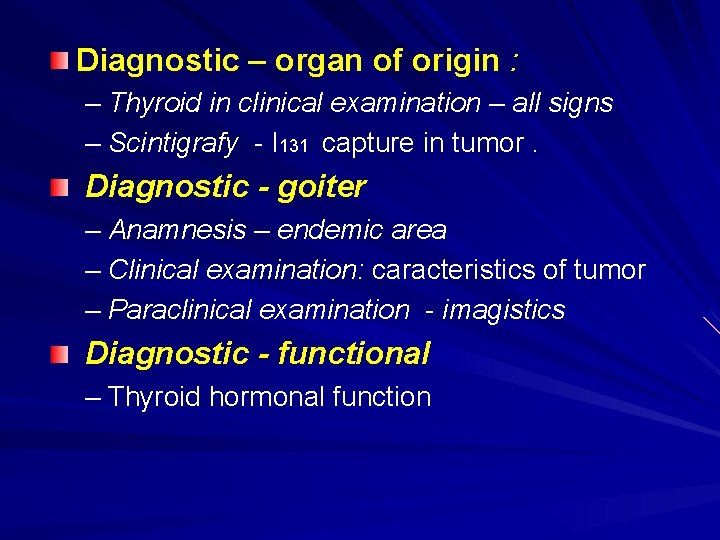
Diagnostic – organ of origin : – Thyroid in clinical examination – all signs – Scintigrafy - I 131 capture in tumor. Diagnostic - goiter – Anamnesis – endemic area – Clinical examination: caracteristics of tumor – Paraclinical examination - imagistics Diagnostic - functional – Thyroid hormonal function
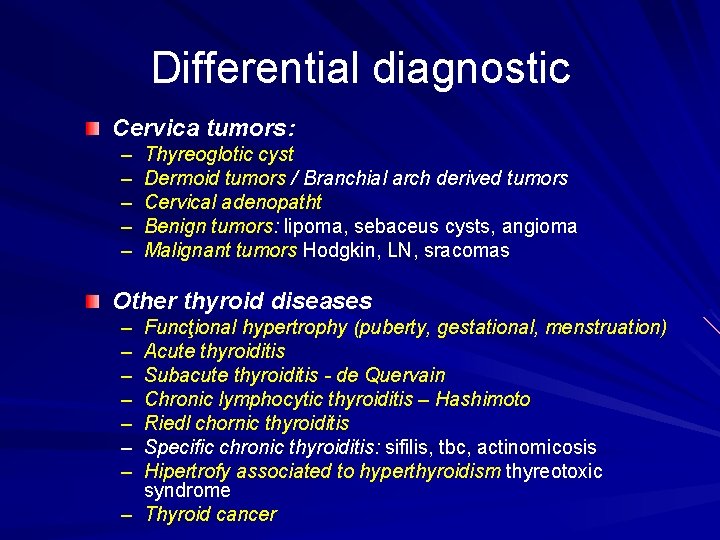
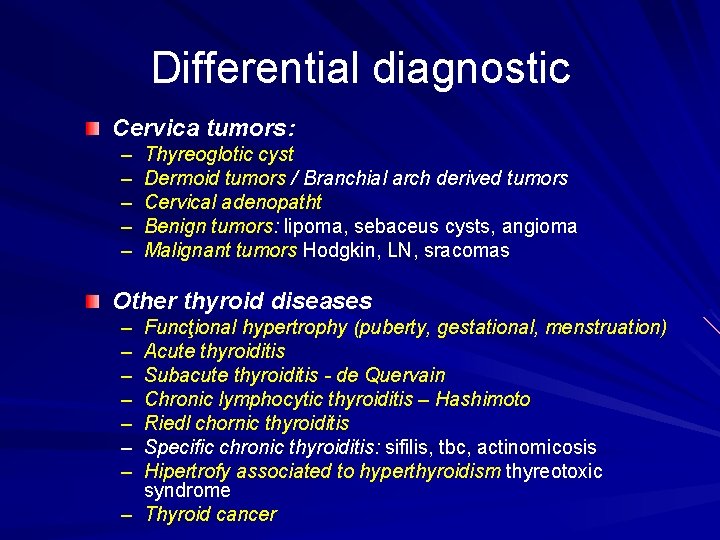
Differential diagnostic Cervica tumors: – – – Thyreoglotic cyst Dermoid tumors / Branchial arch derived tumors Cervical adenopatht Benign tumors: lipoma, sebaceus cysts, angioma Malignant tumors Hodgkin, LN, sracomas Other thyroid diseases – – – – Funcţional hypertrophy (puberty, gestational, menstruation) Acute thyroiditis Subacute thyroiditis - de Quervain Chronic lymphocytic thyroiditis – Hashimoto Riedl chornic thyroiditis Specific chronic thyroiditis: sifilis, tbc, actinomicosis Hipertrofy associated to hyperthyroidism thyreotoxic syndrome – Thyroid cancer
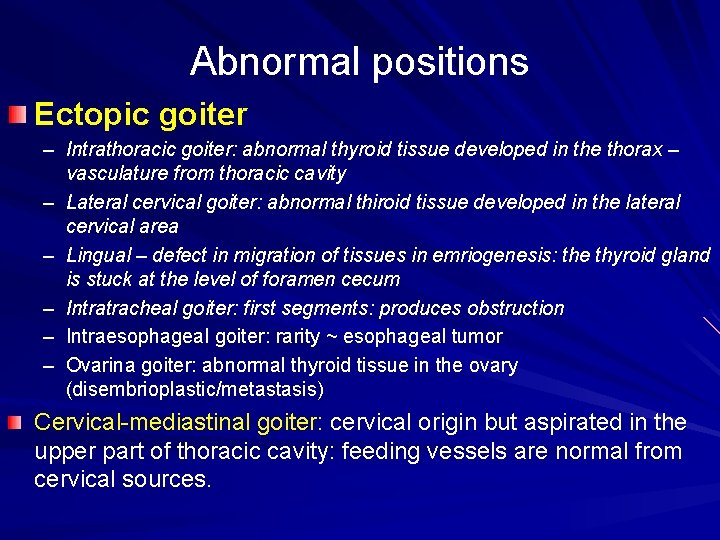
Abnormal positions Ectopic goiter – Intrathoracic goiter: abnormal thyroid tissue developed in the thorax – vasculature from thoracic cavity – Lateral cervical goiter: abnormal thiroid tissue developed in the lateral cervical area – Lingual – defect in migration of tissues in emriogenesis: the thyroid gland is stuck at the level of foramen cecum – Intratracheal goiter: first segments: produces obstruction – Intraesophageal goiter: rarity ~ esophageal tumor – Ovarina goiter: abnormal thyroid tissue in the ovary (disembrioplastic/metastasis) Cervical-mediastinal goiter: cervical origin but aspirated in the upper part of thoracic cavity: feeding vessels are normal from cervical sources.
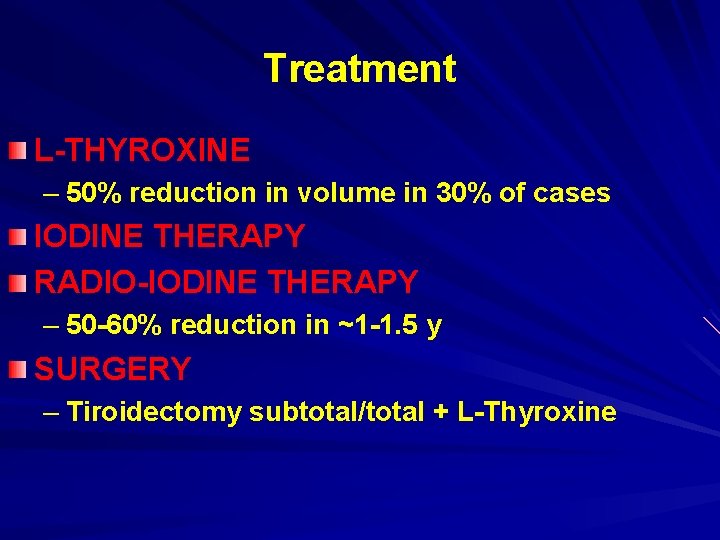
Treatment L-THYROXINE – 50% reduction in volume in 30% of cases IODINE THERAPY RADIO-IODINE THERAPY – 50 -60% reduction in ~1 -1. 5 y SURGERY – Tiroidectomy subtotal/total + L-Thyroxine
Surgical treatment – WHEN? Failure of other modalities Multinodular goiter or cold nodules on scintigrafy Goiter with lesions which are most probably irreversible: fibrosis, recurrent cysts) Complicated goiter: hyperthyroidism, inflammation, intracystic bleeding, compression syndrome Esthetic indications
THYROTOXICOSIS Hypermetabolic condition characterised by increased levels of FT 3 and/or FT 4 – Hyperthyroidism – Subacute thyroiditis – Exogenous administration of thyroid hormones
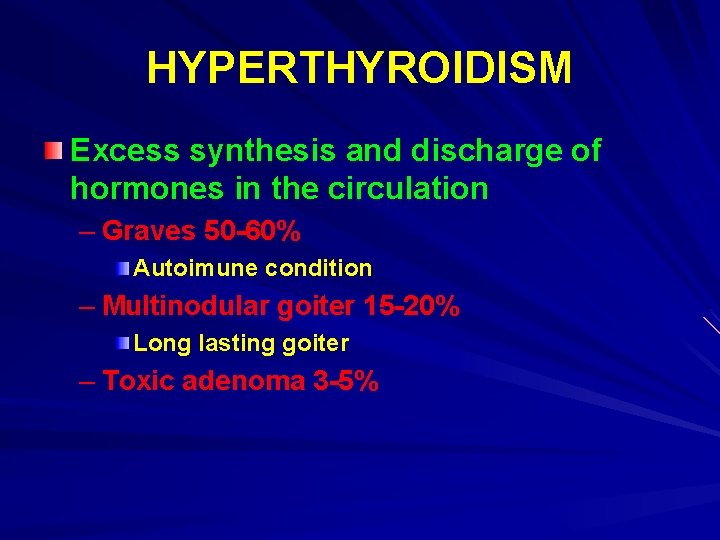
HYPERTHYROIDISM Excess synthesis and discharge of hormones in the circulation – Graves 50 -60% Autoimune condition – Multinodular goiter 15 -20% Long lasting goiter – Toxic adenoma 3 -5%
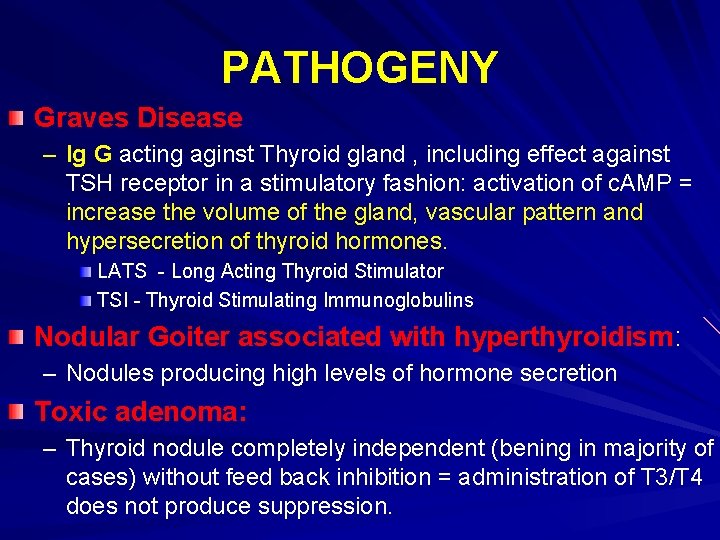
PATHOGENY Graves Disease – Ig G acting aginst Thyroid gland , including effect against TSH receptor in a stimulatory fashion: activation of c. AMP = increase the volume of the gland, vascular pattern and hypersecretion of thyroid hormones. LATS - Long Acting Thyroid Stimulator TSI - Thyroid Stimulating Immunoglobulins Nodular Goiter associated with hyperthyroidism: – Nodules producing high levels of hormone secretion Toxic adenoma: – Thyroid nodule completely independent (bening in majority of cases) without feed back inhibition = administration of T 3/T 4 does not produce suppression.
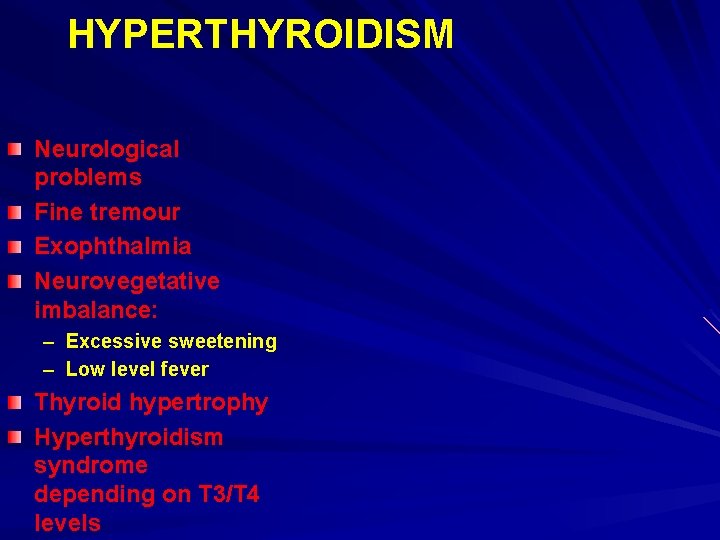
HYPERTHYROIDISM Neurological problems Fine tremour Exophthalmia Neurovegetative imbalance: – Excessive sweetening – Low level fever Thyroid hypertrophy Hyperthyroidism syndrome depending on T 3/T 4 levels
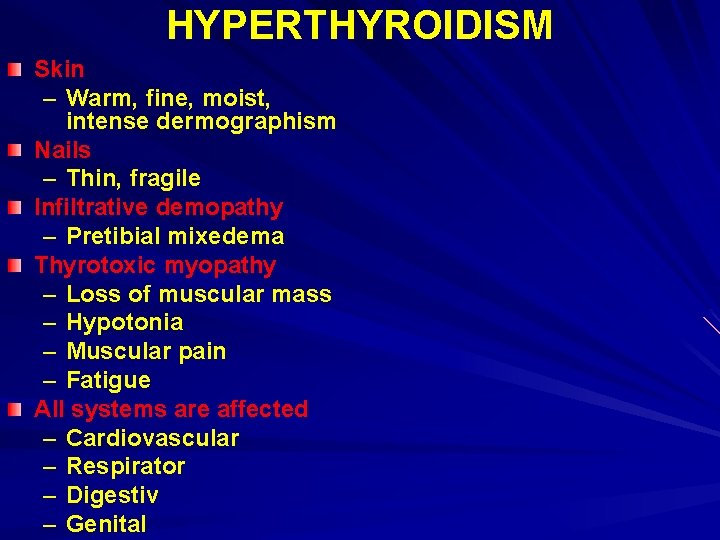
HYPERTHYROIDISM Skin – Warm, fine, moist, intense dermographism Nails – Thin, fragile Infiltrative demopathy – Pretibial mixedema Thyrotoxic myopathy – Loss of muscular mass – Hypotonia – Muscular pain – Fatigue All systems are affected – Cardiovascular – Respirator – Digestiv – Genital
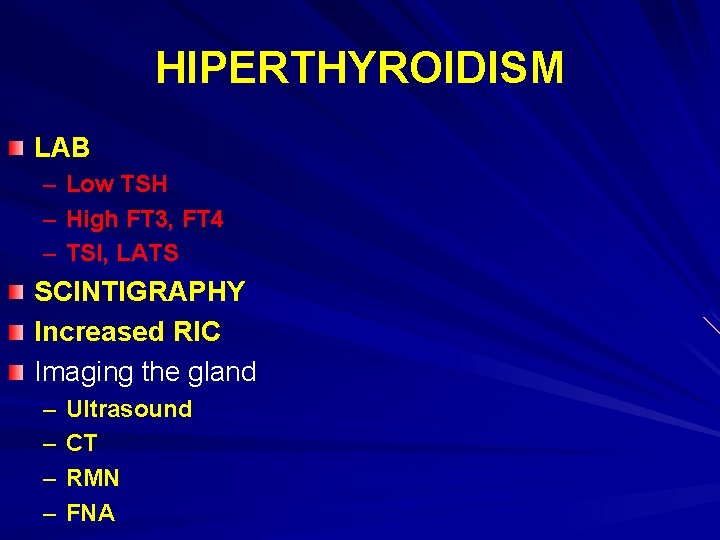
HIPERTHYROIDISM LAB – Low TSH – High FT 3, FT 4 – TSI, LATS SCINTIGRAPHY Increased RIC Imaging the gland – – Ultrasound CT RMN FNA
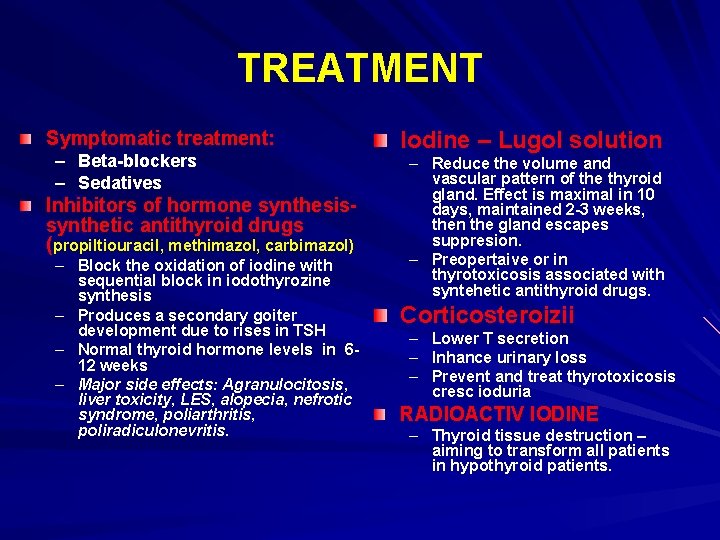
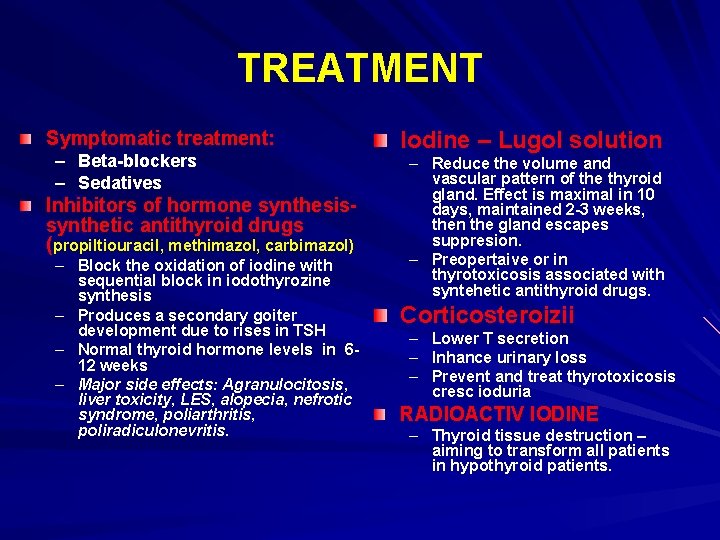
TREATMENT Symptomatic treatment: – Beta-blockers – Sedatives Inhibitors of hormone synthesissynthetic antithyroid drugs (propiltiouracil, methimazol, carbimazol) – Block the oxidation of iodine with sequential block in iodothyrozine synthesis – Produces a secondary goiter development due to rises in TSH – Normal thyroid hormone levels in 612 weeks – Major side effects: Agranulocitosis, liver toxicity, LES, alopecia, nefrotic syndrome, poliarthritis, poliradiculonevritis. Iodine – Lugol solution – Reduce the volume and vascular pattern of the thyroid gland. Effect is maximal in 10 days, maintained 2 -3 weeks, then the gland escapes suppresion. – Preopertaive or in thyrotoxicosis associated with syntehetic antithyroid drugs. Corticosteroizii – – – Lower T secretion Inhance urinary loss Prevent and treat thyrotoxicosis cresc ioduria RADIOACTIV IODINE – Thyroid tissue destruction – aiming to transform all patients in hypothyroid patients.
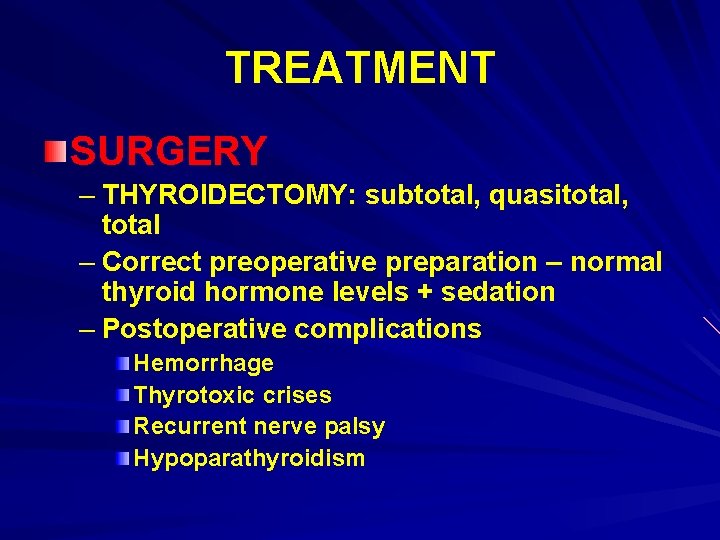
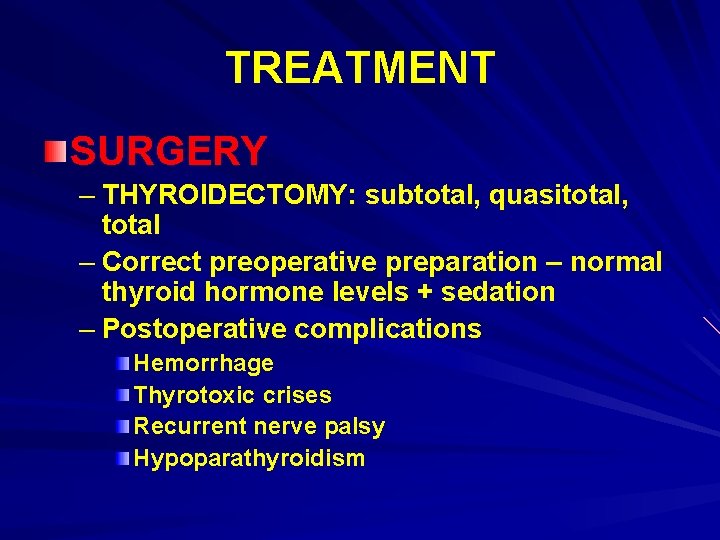
TREATMENT SURGERY – THYROIDECTOMY: subtotal, quasitotal, total – Correct preoperative preparation – normal thyroid hormone levels + sedation – Postoperative complications Hemorrhage Thyrotoxic crises Recurrent nerve palsy Hypoparathyroidism
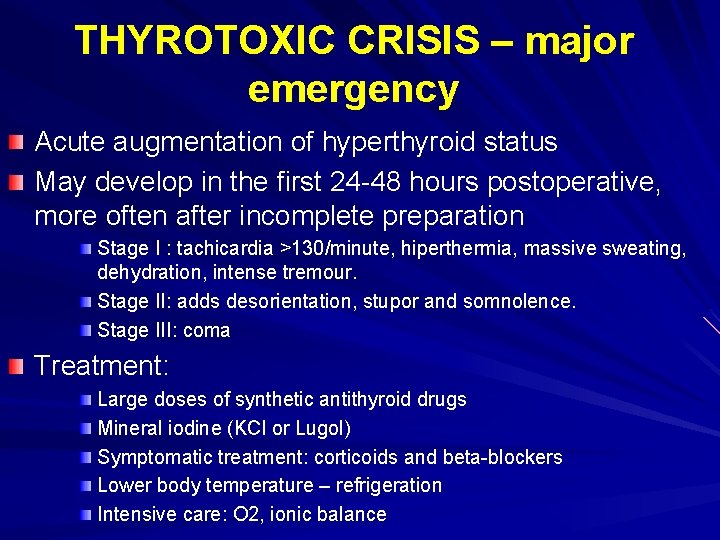
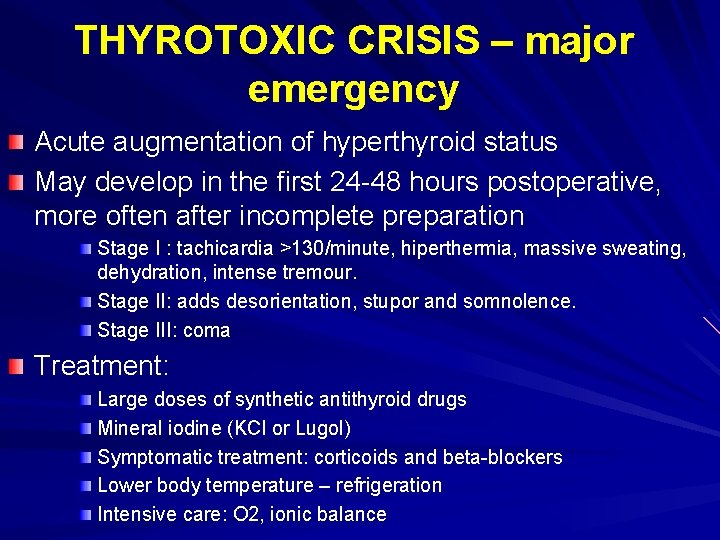
THYROTOXIC CRISIS – major emergency Acute augmentation of hyperthyroid status May develop in the first 24 -48 hours postoperative, more often after incomplete preparation Stage I : tachicardia >130/minute, hiperthermia, massive sweating, dehydration, intense tremour. Stage II: adds desorientation, stupor and somnolence. Stage III: coma Treatment: Large doses of synthetic antithyroid drugs Mineral iodine (KCl or Lugol) Symptomatic treatment: corticoids and beta-blockers Lower body temperature – refrigeration Intensive care: O 2, ionic balance
INFLAMMATORY DISEASES = THYROIDITIS
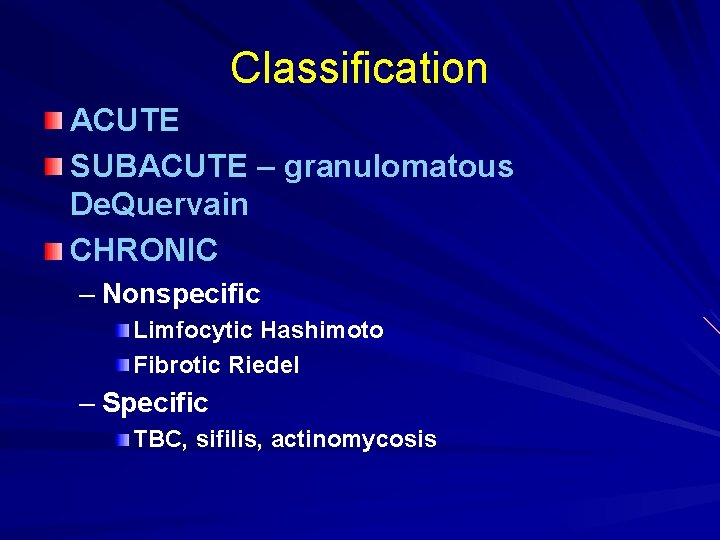
Classification ACUTE SUBACUTE – granulomatous De. Quervain CHRONIC – Nonspecific Limfocytic Hashimoto Fibrotic Riedel – Specific TBC, sifilis, actinomycosis
ACUTE THYROIDITIS <1% of all thyroid pathology, frequently preexisting goiter PATHOGENY Germes – abscess formation (aggressive germs + low immunity) – – Bacteria – streptococcus, stafilococcus, pneumococcus, G-bacili Viruses – influenza, Fungs: – Candida Parazitic Contamination: – Hematogenous, lymfatic, direct Source – Close contact – Distant source with hematogenic circulation
CLINICAL EXAMINATION Anamnesis – – – Sudden onset Local inflammatory signs Fever high (38. 5 -40), chills and tachicardia – Anterior cervical pain Pressure sensation Radiating: mandible, ear Intensifies with swallowing Antalgic position – – Dysphagia Dyspnoea Dysphonia Irritative coughing Clinical examination – T gland enlarged (whoe or part) and very painful – All inflammatory signs in the anterior cervical area (skin) – Abscess formation can produce fluctuence. – Inflammatory LN in the laterocervical area
LAB EVALUATION High WBC with % PMN Vey high ESR Thyroid scintigram: a cold difuse area (no iodine capture) US: hypoecoic i the begining, transsonic if absecess is formed. Blood cultures – isolation of bacteria RIC may be normal/lower then normal. In cases of abscess: puncture and culture of pathogenic germ
TREATMENT Prognostic: very good if rapidly diagnosed and treatment is adequate Complications without proper treatment: – Septic: local (mediastinitis, fistula formation – skin, esophagus, trachea), or metastatic. – Mechanic: large abscess behaves like a tumor – Vascular: thrombosis of adjacent veins – Endocrine: very unusual
TREATMENT - early Medical – Antibiotics: empirical + cultures – NSAID – Antialgic medication Surgical – Abscess – drainage – Partial thyroidectomy +/-
SUBACUTE THYROIDITIS Granulomatous thyroiditis De. Quervain thyroiditis
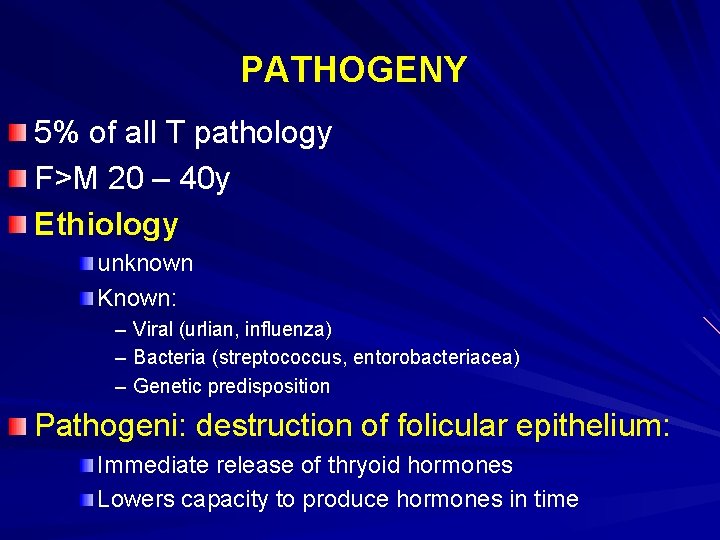
PATHOGENY 5% of all T pathology F>M 20 – 40 y Ethiology unknown Known: – Viral (urlian, influenza) – Bacteria (streptococcus, entorobacteriacea) – Genetic predisposition Pathogeni: destruction of folicular epithelium: Immediate release of thryoid hormones Lowers capacity to produce hormones in time

Pathological changes Macroscopic – T is increased in size (2 -3 x), harder, yelowish Mycroscopic – Multifocal granulomatous inflammatory reaction, limfocityc and plasma cells infiltration + interstitial
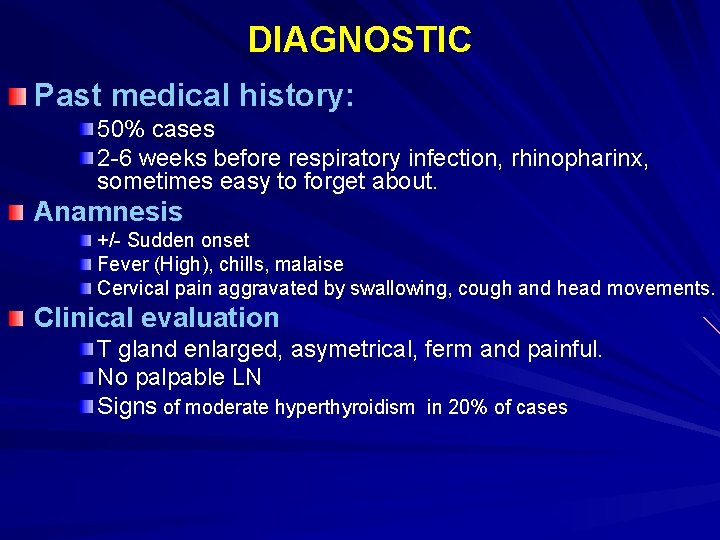
DIAGNOSTIC Past medical history: 50% cases 2 -6 weeks before respiratory infection, rhinopharinx, sometimes easy to forget about. Anamnesis +/- Sudden onset Fever (High), chills, malaise Cervical pain aggravated by swallowing, cough and head movements. Clinical evaluation T gland enlarged, asymetrical, ferm and painful. No palpable LN Signs of moderate hyperthyroidism in 20% of cases
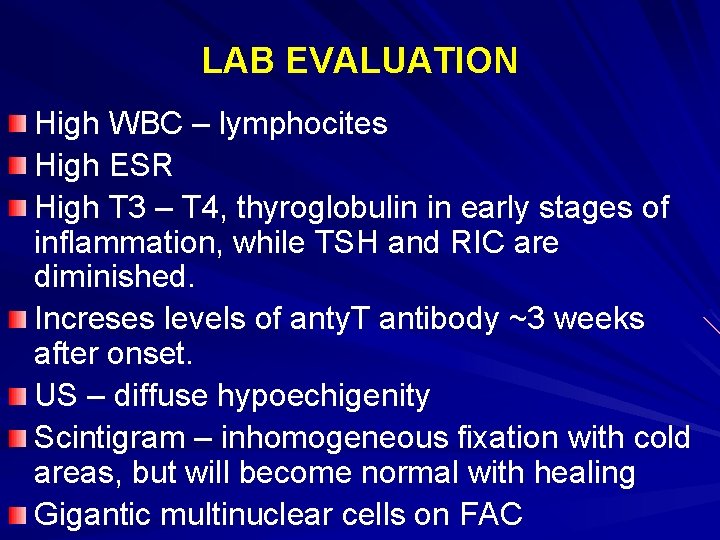
LAB EVALUATION High WBC – lymphocites High ESR High T 3 – T 4, thyroglobulin in early stages of inflammation, while TSH and RIC are diminished. Increses levels of anty. T antibody ~3 weeks after onset. US – diffuse hypoechigenity Scintigram – inhomogeneous fixation with cold areas, but will become normal with healing Gigantic multinuclear cells on FAC
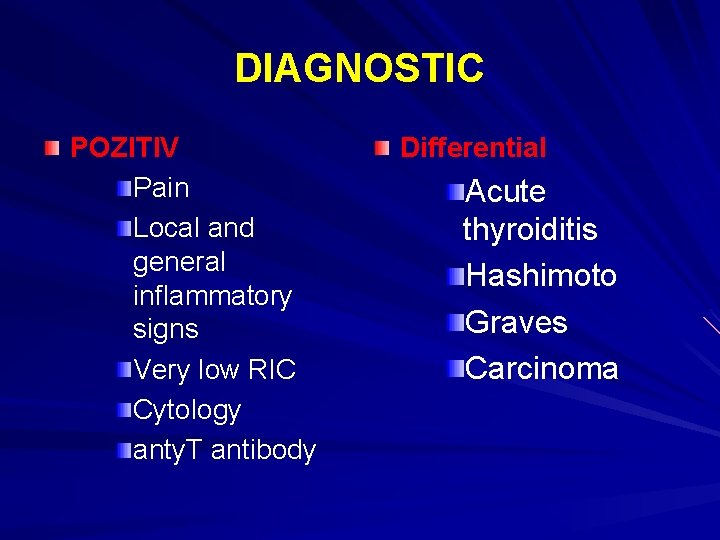
DIAGNOSTIC POZITIV Pain Local and general inflammatory signs Very low RIC Cytology anty. T antibody Differential Acute thyroiditis Hashimoto Graves Carcinoma
PROGRESSION Self healing condition – 1 -3 months – No sequels Transform in chronic inflammation – Riedel/ Hashimoto Hipothiroidism - 10% Recurrent condition – very rare
TREATMENT NSAID/ CORTICOSTEROIDS Hormonal – hyper or hypo function Surgical – an exception – Lobectomy, thyroidectomy – When a nodular hypertrophy persists
CRONIC LYMPHOCYTIC THYROIDITIS Hashimoto thyroiditis
PATHOGENY The most common type of inflammatory disease of T gland The most common cause of hypothyroidism F>B; 40 -50 y CAUSE – Autoimmune aggression: ATB against Thyroglubuline, Mycrosomes.
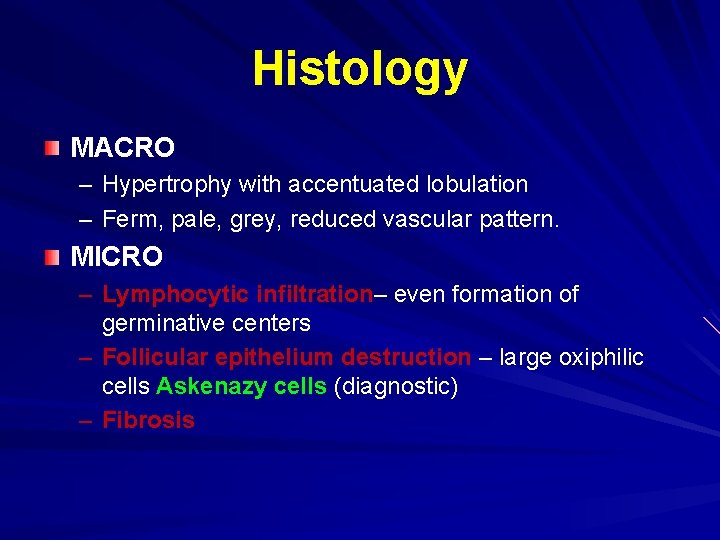
Histology MACRO – Hypertrophy with accentuated lobulation – Ferm, pale, grey, reduced vascular pattern. MICRO – Lymphocytic infiltration– even formation of germinative centers – Follicular epithelium destruction – large oxiphilic cells Askenazy cells (diagnostic) – Fibrosis
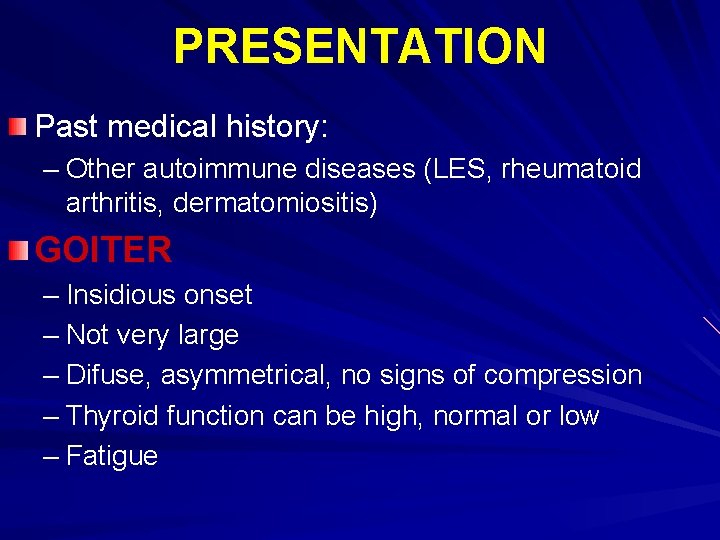
PRESENTATION Past medical history: – Other autoimmune diseases (LES, rheumatoid arthritis, dermatomiositis) GOITER – Insidious onset – Not very large – Difuse, asymmetrical, no signs of compression – Thyroid function can be high, normal or low – Fatigue
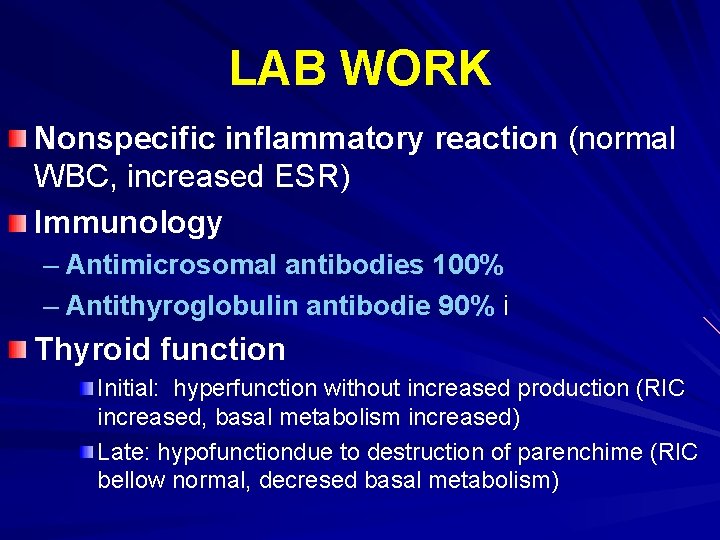
LAB WORK Nonspecific inflammatory reaction (normal WBC, increased ESR) Immunology – Antimicrosomal antibodies 100% – Antithyroglobulin antibodie 90% i Thyroid function Initial: hyperfunction without increased production (RIC increased, basal metabolism increased) Late: hypofunctiondue to destruction of parenchime (RIC bellow normal, decresed basal metabolism)
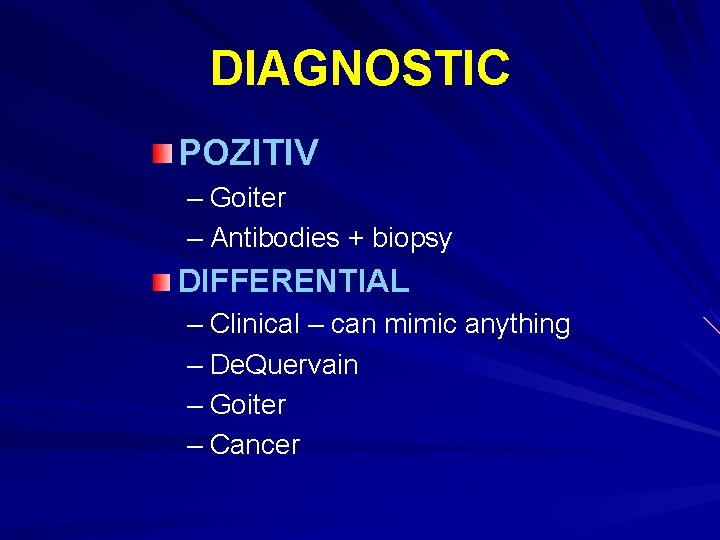
DIAGNOSTIC POZITIV – Goiter – Antibodies + biopsy DIFFERENTIAL – Clinical – can mimic anything – De. Quervain – Goiter – Cancer
COMPLICATIONS – Hypothyroidism – 50 -80% PROGNOSTIC – Slow progression with periods of long stagnation (years) followed y progression – Rapid progression - unusual
TREATMENT Hormonal – Hormonal replacement Surgical – Compression – Questionable diagnostic (Lymphoma/Cancer)
FIBROTIC THYROIDITIS Riedel wood-hard thyroiditis
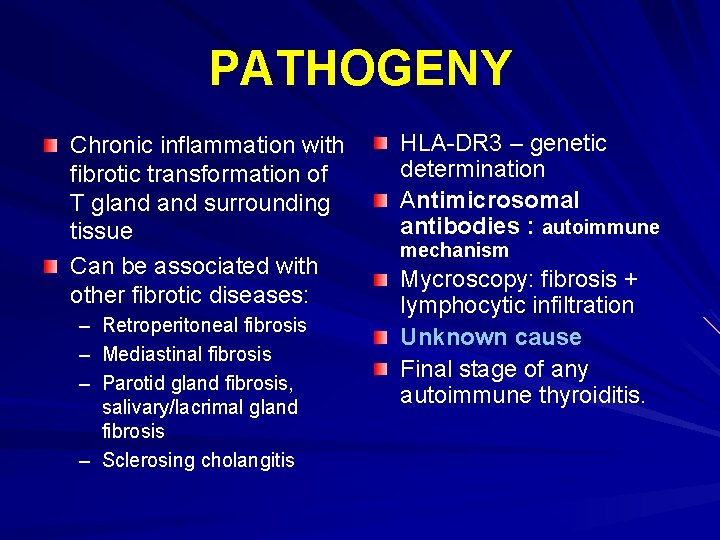
PATHOGENY Chronic inflammation with fibrotic transformation of T gland surrounding tissue Can be associated with other fibrotic diseases: – Retroperitoneal fibrosis – Mediastinal fibrosis – Parotid gland fibrosis, salivary/lacrimal gland fibrosis – Sclerosing cholangitis HLA-DR 3 – genetic determination Antimicrosomal antibodies : autoimmune mechanism Mycroscopy: fibrosis + lymphocytic infiltration Unknown cause Final stage of any autoimmune thyroiditis.
PATHOLOGY One lobe or whole gland Fibrotic, white tissue Fibrosis extends outside T gland: there are no cleavage plans and structures can not be identified
CLINICAL PRESENTATION Females: 30 -60 y age Anamnesis – signs of diffuse hypertrophy + compression of adjacent organs Clinical examination – – wood-hard consistency Tender T gland fixed to all plans T gland does not invade skin Hormonal status: normal (most cases) or hypo
LAB WORK Slight inflammatory response Normal or low T hormones Sometimes: low levels of anty. Thyroid antibodies US: hypoechoic + invasion in adjacent structures Scintigram: inhomogenous fixation with areas with non-fixation of iodine

DIAGNOSTIC Pozitiv: pathologic examination Differential – cancer – Hashimoto – De. Quervain COMPLICATIONS – Compression Progression – Very slow: years until compression is significant
TREATMENT Hormonal – Replacement for hypothyroidism – May reduce progression to fibrosis Surgical – Thyroidectomy – Limited excision for decompression
THYROID CANCER
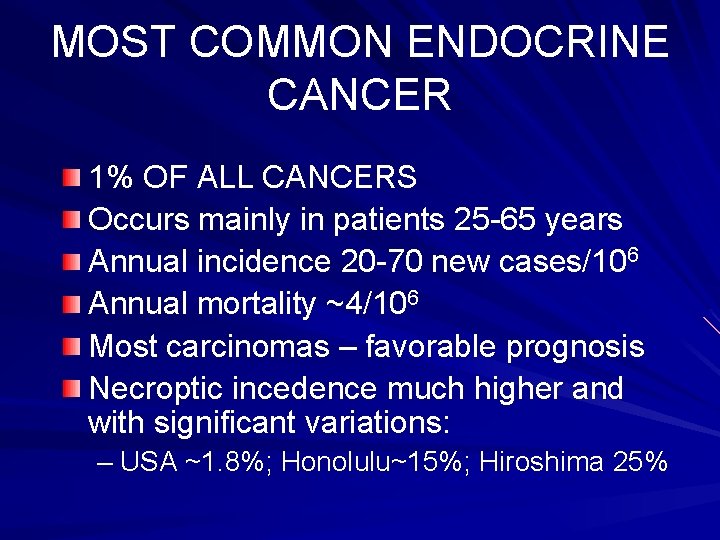
MOST COMMON ENDOCRINE CANCER 1% OF ALL CANCERS Occurs mainly in patients 25 -65 years Annual incidence 20 -70 new cases/106 Annual mortality ~4/106 Most carcinomas – favorable prognosis Necroptic incedence much higher and with significant variations: – USA ~1. 8%; Honolulu~15%; Hiroshima 25%
RISK FACTORS Iodine supplements increase the incidence of papillary carcinoma (<T, well differentiated, overall increases survival) External irradiation – in human the only proven carcinogenic factor for thyroid carcinoma – children with neck irradiation develop papillary carcinoma
RISK FACTORS – 1986 Cernobil effect- steady increase (Pacini 1997) Peak 3 x in 1992 -1994 ; ~80% children <14 years of age
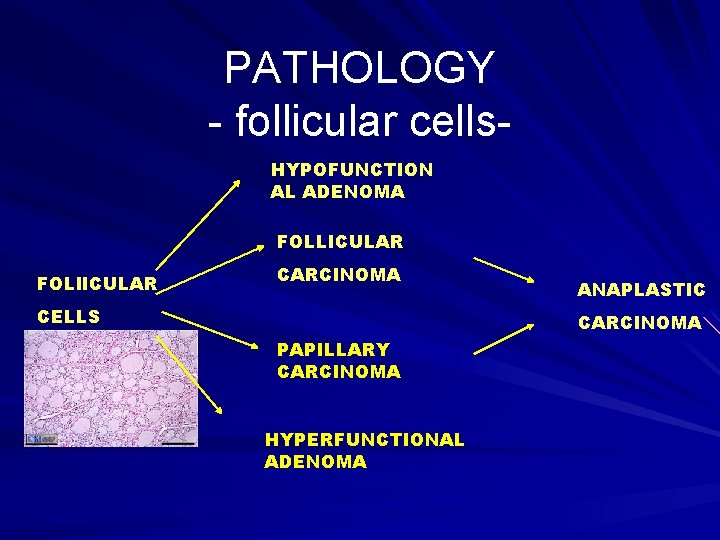
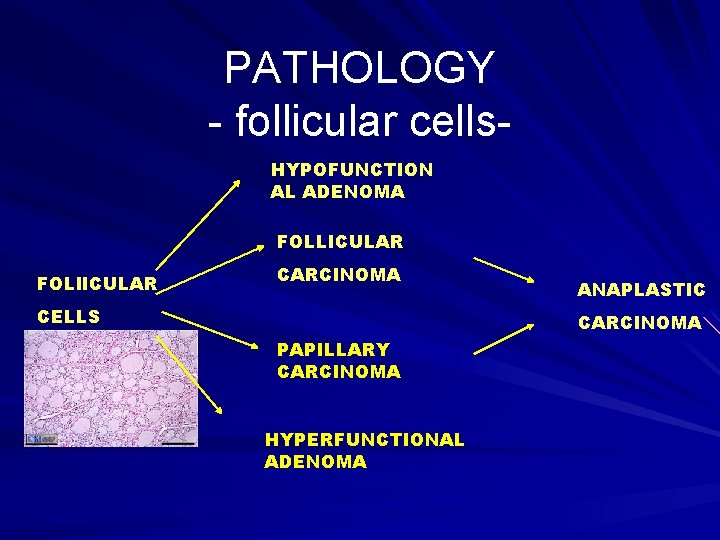
PATHOLOGY - follicular cells. HYPOFUNCTION AL ADENOMA FOLLICULAR FOLl. ICULAR CARCINOMA CELLS ANAPLASTIC CARCINOMA PAPILLARY CARCINOMA HYPERFUNCTIONAL ADENOMA
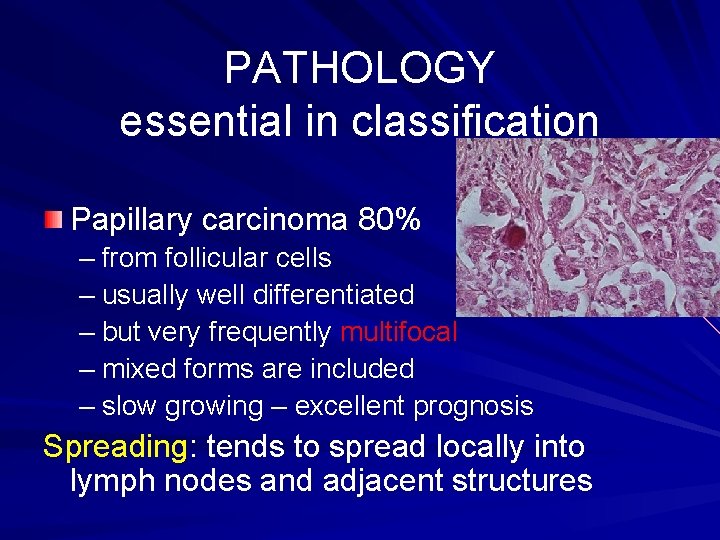
PATHOLOGY essential in classification Papillary carcinoma 80% – from follicular cells – usually well differentiated – but very frequently multifocal – mixed forms are included – slow growing – excellent prognosis Spreading: tends to spread locally into lymph nodes and adjacent structures
PATHOLOGY Invasion in the local lymph nodes is not associated with a worse prognosis Poor prognosis: – – – Male gender – >50 years – Less differentiated Tumors larger then 4 cm Local invasion or distant metastases Metastases: lungs, rarely to bones
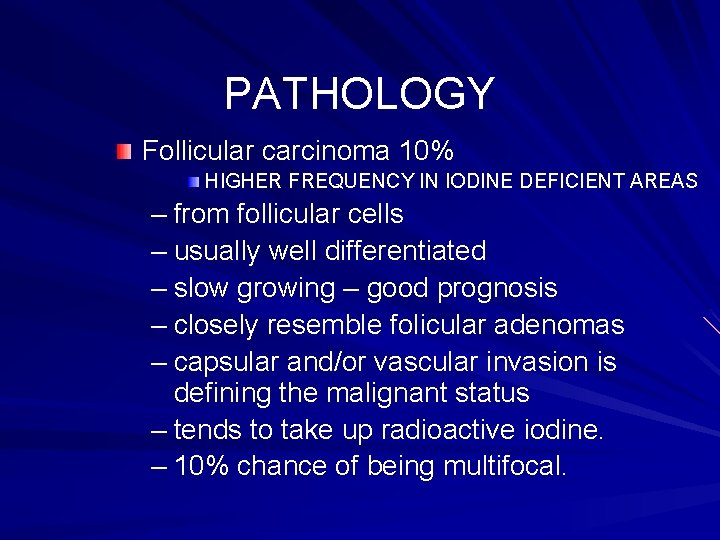
PATHOLOGY Follicular carcinoma 10% HIGHER FREQUENCY IN IODINE DEFICIENT AREAS – from follicular cells – usually well differentiated – slow growing – good prognosis – closely resemble folicular adenomas – capsular and/or vascular invasion is defining the malignant status – tends to take up radioactive iodine. – 10% chance of being multifocal.
PATHOLOGY Spreading: tends to spread through the blood stream making it more difficult to control and also grows into adjacent structures. Metastases – lung and bone – usually concentrate iodine Poor prognosis associated with: – Age >45 years – Local extracapsular invasion – Distant metastases
PATHOLOGY Hürthle Cell carcinoma 3. 6% – composed of "modified follicular cells" – very similar to follicular carcinoma – 25% chance of being multifocal – does not tend to take up radioactive iodine – has a prognosis similar to that of follicular carcinoma.

PATHOLOGY Medullary carcinoma 2. 7% – from the parafollicular C cells – There are two types Genetic disposition – AD MUTATIONSrepresents about 20% of all patients with medullary carcinoma USUALLY PRESENT IN BOTH LOBES Sporadic – occurs randomly and represents 80% of medullary carcinoma USUALLY PRESENTS UNILATERAL
PATHOLOGY - CMT Worse prognosis compared with previous forms: 50% survive at 10 years Occult tumors discovered in families at risk – 95% cure rate – Detection by screening for calcitonin basal and/or pentagastrin infusion test TUMOR PRESUMED – 95% cure TUMOR PALPABLE – 17% cure SPREADING: blood born metastases and lymphnodes
PATHOLOGY Anaplastic carcinoma 1. 7% – develops from follicular cells – poorly differentiated – aggressive and rapidly growing. – poor prognosis <2 years Spreading: rapidly in the adjacent structures and also sends blood born metastasis – STAGE IV Others rare tumors that may develop in the thyroid gland are – – – Lymphoma Sarcoma – originating in the connective tissue Carcinosarcoma - composed of both malignant thyroid cells and connective tissue Metastatic tumors
SIGNIFICANT MICROSCOPIC FEATURES 1. Differentiation level 2. Capsular or vascular invasion (in follicular and Hürthle cell carcinomas invasion is needed to prove the tumor malignant 3. Regional lymph node involvement 4. Invasion of adjacent structures (extracapsular invasion)
DIAGNOSTIC clinical examination Evaluation of the neck NODULE Assesment of nodules – – – Firmness Mobility Multiple Evaluation of typical metastatic sites – Cervical nodes – Bones – Lungs
DIAGNOSTIC anatomical evaluation ULTRASOUND SCAN – Confirm - thyroid gland – Solid/cystic – Unic/multicentric – Lymphnodes – Guides FNB – Doppler NON INVASIVE - SCREENING
DIAGNOSTIC anatomical test Scintiscan: – Evaluate the capacity to concentrate iodine – Cold nodules – 15 -20% are malignant – Essential in postoperative followup Estimate the remnant thyroid tissue Diagnose iodine concentrating metastatic tumor WBS - Diagnose bone metastases
DIAGNOSTIC anatomical test CAT scan and chest X-Ray – Lung metastases – Restrosternal goiters
FUNCTIONAL EVALUATION Is mostly used in the follow-up Thyroglobuline – >5 ng/ml after total thyroidectomy – >10 ng/ml after total thyroidectomy Calcitonine (Pg-CT) – marker for the diagnosis of MTC in high risk populations (nodule + CT(+) the most significant association) – Marker for postoperative follow-up
CYTOLOGIC DIAGNOSIS Fine needle aspiration cytology – most important study in evaluating thyroid nodules Core biopsy – larger sample but higher risk – – HISTOLOGIC DIAGNOSIS Preoperative diagnosis of most thyroid cancers Help to plan the extent of surgical resection Selection of cases which will not benefit from surgical management
CYTOLOGIC DIAGNOSIS Results – Nondiagnostic – Indeterminate – Malignant
GENETIC STUDIES Numerous mutations are associated with thyroid cancer MTC – Germinal cells RET mutations associated with early onset and multicentric tumors – MEN II (A and B) – Profilactic thyroidectomy

TREATMENT SURGICAL RESECTION IS THE STANDARD THERAPY
EXTENT OF SURGICAL RESECTION Depends primarily on HISTOLOGICAL type ESSENTIAL – PREOPERATIVE ACCURATE DIAGNOSIS – FNB AND INTRAOPERATIVE FROZEN SECTIONS Age Capsular/extracapsular invasion Invasion in adjacent structures
SURGICAL TREATMENT PAPILLARY CARCINOMA CONSERVATIVE – – – Lobectomy +/- istmusectomy Macroscopic - unic nodule Permanent TSH supression is essential – Acceptable if poor prognostic factors ar absent – 5 -10% will develop recurrences

SURGICAL TREATMENT PAPILLARY CARCINOMA AGGRESSIVE APPROACH – Near total/total thyroidectomy – For macroscopic multifocal + lymph-nodes involvement – Lymph-node dissection – primary drainage arrea
SURGICAL TREATMENT FOLLICULAR CARCINOMA Dg. suspected on FNB and CONFIRMED on frozen section Total/near total thyroidectomy Total thyroidectomy – makes metastases visible – 5 -10% recur in residual tissue

SURGICAL TREATMENT ANAPLASTIC TUMORS – Old age patients– usually is of no benefit – Middle age – total thyoidectomy may be tried, but little benefit – Istmusectomy – pressure on the trachea (similar results with radiotherapy) – 1 year survival rate ~0
SURGICAL TREATMENT MEDULLARY CARCINOMA – Total thyroidectomy Frequent multicentric (both forms) Lymphadenectomy in the primary drainage area – essential. 75% of cases demonstrate MTS in nodes from the central compartment Nodes in the secondary drainage area should be sampled - if involved RADICAL NECK DISSECTION Pheocromocytoma and parathyroid tumors should be checked and solved prior to total thyroidectomy
COMPLICATIONS recurrent laryngeal nerve damage 2 -8% permanent hypoparathyroidism 1 -3% ; 5 -10% in difficult resections hematoma formation wound infection keloid formation in the scar airway compromise (anaplastic carcinoma)
POSTOPERATIVE TREATMENT radioactive iodine thyroid suppression external radiotherapy (exceptional) – – locally advanced papillary carcinoma and metastatic sites external beam radiotherapy cytotoxic chemotherapy
FOLLOW-UP Differentiated carcinomas thyroglobulin measurement + WBS Medullary carcinoma calcitonin
PROGNOSIS OVERALL PROGNOSIS IS GOOD WITH > 94% LONG TERM SURVIVAL

PARATHYROID GLANDS
Disorders of the Parathyroid Glands Maintenance of calcium, phosphate and magnesium homeostasis is under the influence of two polypeptide hormones; * parathyroid hormone(PTH) * calcitonin (CT), * sterol hormone, 1, 25 dihydroxy cholecalciferol (1, 25 (OH)2 D 3.
Parathyroid Glands These hormones regulate the flow of minerals in and out of the extracellular fluid compartments through their actions on intestine, kidneys, and bones.
Normal function The PTH acts directly on the bones and kidneys and indirectly on the intestine through its effect on the synthesis of 1, 25 (OH)2 D 3. Its production is regulated by the concentration of serum ionized calcium. Lowering of the serum calcium levels will induce an increased rate of parathyroid hormone secretion
Normal function Calcitonin is released by the “C” cells (parafollicular cells in the thyroid gland) Secretion in response to small increases in plasma ionic calcium. It acts on the kidney and bones to restore the level of calcium PTH and calcitonin are antagonistic
Disorders of the Parathyroid Function Primary Hyperparathyroidism Excessive PTH from one/more glands which are hyperfunctional. Hyper. Ca that fails to inhibit in normal feedback loop. Cause? – possible genetic (multiple adenomas are frequent). Carcinoma<1%
Clinical Features Kidneys: renal stones or nephrocalcinosis (diffuse deposition of Ca. PO 4. Skeleton: osteitis fibrosa cystica Massive subperiostal resorbtion of bone Bone cysts and brown tumors of long bones Other: muscle weakness, easy fatigability, peptic ulcer disease, pancreatitis, hypertension, gout and pseudogout as well as anemia and depression 90% cases diagnosed before that on screening for calcium
Diagnosis hypercalcaemia in more than one serum measuremen elevated immunoreactive PTH is characteristic (i. PTH)
LAB Work Serum phosphate is usually low but may be normal. Hypercalcaemia is common alkaline phosphatase (of bone origin)- high urinary hydroxyproline concentrations are commonly elevated when the bones are involved. Negative glucocoticoid supression test (supression indicates no adenoma)
RADIOLOGY subperiosteal bone resorption usually on the radial surfacy of the distal phalanx with distal phalangeal tufting cysts formation and generalized osteopenia.
Pre-operative localization of the abnormal parathyroid gland(s): Ultrasonography MRI CT Thallium 201 – Tehcnichum 99 m scan (subtraction study)
Treatment Very often “biochemical” hyper. PTH. Resection of the parathyroid lesion is curative with recurrences observed mainly in the multiple glandular disease. Tumor 31/2 of all hyperplastic tissue Medical management of hypercalcemia – – Glucocorticoids Mithramycin Bisphonates Estrogen - Diuresis - Calcitonin - Phosphates
Secondary hyperparathyroidism chronic stimulation of the parathyroid glands by a chronic decrease in the ionic calcium level in the blood
Major causes Dietary deficiency of vitamin D or calcium Decreased intestinal absorption of vitamin D or calcium due to primary small bowel disease, short bowel syndrome, and postgastrectomy syndrome. Drugs that cause rickets or osteomalacia such as phenytoin, phenobarbital, cholestyramine, and laxative.
Major causes of chronic hypocalcemia States of tissue resistance to vitamin D Excessive intake of inorganic phosphate compunds Psudohypoparathyroidism Severe hypomagnesemia Chronic renal failure
Hypoparathyroidism Deficient secretion of PTH which manifests itself biochemically by hypocalcemia, hyperphospatemia diminished or absent circulating i. PTH and clinically the symptoms of neuromuscular hyperactivity.
Hypoparathyroidism Causes: Surgical hypoparathyroidism – the commonest Idiopathic hypoparathyroidism – Genetic – Autoimmune – Functional (associated with hypo. Mg – PTH can not be released in this condition)
Clinical features Neuromuscular: Cardiovascular Cataract Dental problems Malabsorbtion – – – Paresthesia Tetany Hyperventilation Adrenergic symptoms Convulsion Signs of latent tetany - Prolonged QT interval in the ECG - Resistance to digitalis - Hypotension - Refractory heart failure
Diagnosis In the absence of renal failure hypocalcaemia with hyperphosphataemia is virtually diagnostic of hypoparathyroidism. Undetectable serum i. PTH confirms the diagnosis or it can be detectable if the assay is very sensitive.
TREATMENT Prevention – surgical trauma Oral calcium with pharmacological doses of vitamin D or its potent analogues. Phosphate restriction in diet may also be useful with or without aluminum hydroxide gel to lower serum phosphate level.