ENDOCRINE SYSTEM THYROID GLAND Thyroid hormones affect nearly

- Slides: 61
ENDOCRINE SYSTEM
THYROID GLAND Thyroid hormones affect nearly all body tissues u Dysfunctions cause profound effects u Three hormones: u – T 3 ; T 4 ; calcitonin Thyroid hormone’s main component is iodine u Minimum daily requirement of I= 80 mcg; more like 500 mcg (contained in bread, water, and iodized salt) u
THYROID u Thyroid gland can store large quantities for months u S/S may not appear for months u Works on negative feedback system; TRH signals TSH which stimulates thyroid gland u Most hormone is bound to protein
THYROID u Functions: – Metabolism: increase rate, accelerate food utilization for energy, excites mental processes – Growth: in children accelerates growth – Carbohydrate: stimulates metabolism, including insulin secretion – Fat: enhances fat metabolism – Body wt: production relates inversely to body wt (does not stimulate appetite) – CV: causes vasodilation, increased cardiac output and heart rate, increased systolic B/P by 10 -20 mm but diastolic may drop the same – Respiration: increases O 2 use, rate, and depth – GI: increases appetitie, absorption, motility – CNS: speeds mental processes
THYROID u Assessments: – – – – Swallowing Skin changes Tolerance to heat or cold Weight changes Palpitations Drugs Radiation to neck or surgery Head trauma Alcohol Growth rate Appetite Menstrual periods BEGIN WITH INSPECTION, LOOKING FOR LUMPS, PUFFINESS, FACIAL EXPRESSIONS, ENLARGED TONGUE, VOICE, HAIR, VISION, NAILS, AND MUSCLE ACHES.
THYROID u Diagnostic tests: – Thyroid panel: T 3 & T 4; free and bound; – RAIU: radioactive iodine uptake; uses radioactive iodine and scan thyroid as it uses iodine. Given PO, IV, or liquid; only use small amt. no risk, do before scan with contrast – Stimulation tests – Scans – Ultasound – Biopsy
THYROID u Hyperthyroidism: – Involves excessive hormone production – Leads to hypermetabolism – Signs and symptoms: thyrotoxicosis – Stimulates heart, protein synthesis, breakdown>buildup leading to negative nitrogen balance (degradation); hyperglycemia; increased fat metabolism – Caused by two etiologies: u Increased iodine uptake (Grave’s, goiter, adenoma u Low iodine uptake (subacute and silent)
THYROID Grave’s disease: toxic diffuse goiter u Most common u Strikes women, 20 -30. u Multisystem syndrome, affecting eyes, skin, bones u Increased thyroid hormone as well as goiter u No sure cause: autoimmune disorder u Generally emotional upset precedes symptoms u Has heredity component u
THYROID u Assessment: – – – – Increase appetite but slight wt loss Dyspnea Decreased heat tolerance Menstruation may decrease or stop Increased bowel movements or diarrhea Nervous, irritable, restless Speak rapidly; laugh inappropriately Exopthalamus (BUG-EYE) Moist skin, thinning hair, elbows red; clubbing of nails (Plummer’s nails), hyperpigmentation (vitiligo- milk-white patches) Tremors, weakness Tachycardia, atrial fibrillation; widened pulse pressure Fine, soft hair; moist skin Hyperactive deep tendon reflexes
THYROID u Diagnostic tests: – Elevated T 3, T 4 – RAIU – No response to TRH – Below normal TSH – Thyroid scan
THYROID u Interventions: – Record vital signs – Rest, frequent linen changes, cool environment – Drugs to reduce hormone: can cause thyroid storm PTU u Tapezole u Iodine-radioactive; cells are destroyed u Lithium u Inderal: not used on clients with asthma or heart disease u – Watch for agranulocytosis: fever, sore throat, rash – Treatment does not correct infiltrative opthalopathy; use tears, elevate head, diuretics for edema; prednisone
THYROID u u u Surgical intervention: May perform total or subtotal Treat with drugs to return to near normal thyroid function prior to surgery – Give Lugol’s solution or SSKI (saturated solution of potassium iodide) prior to OR to firm thyroid, reduce vascularity which can reduce bleeding – Give in milk, OJ, sip thru straw so as not to discolor teeth – Watch for toxicity: buccal mucosal swelling, excessive salivation, skin reactions – May receive Inderal to reduce cardiac problems – Teach T, C, & DB; support head, explain about risk for hoarseness and soreness
THYROID u After surgical assess: – – – – – Vital signs Voice-may be hoarse; usually temporary Neuromuscular functioning Expect moderate drainage; check back of neck Respiratory distress- use humidified air Laryngeal stridor, paralysis, tetany Keep in semi-Fowler’s Avoid strain on suture line- avoid neck extension Keep emergency drugs: O 2, suction, trach tray, calcium gluconate u Monitor for transient hypothyroidism, damage to voice, nerves, hypocalcemia, and tetany u
THYROID u Thyroid storm: – Crisis situation- usually caused by Grave’s – Life-threatening – Uncontrolled hyperthyroidism – Develops quickly and triggered by stress; overpalpation of gland – Fever, tachycardia, systolic hypertension, GI, restlessness, confused, psychotic – Even with treatment, 25% mortality rate
THYROID u Hypothyroidism: – Deficiency in thyroid hormone – Leads to low metabolism with build-up of metabolites – Metabolites with water accumulate within cells, cause edema, called myxedema – Myxedema coma: rare but can occur; heart becomes flabby, chambers increase in size, CO decreases; life threatening; high mortality rate
THYROID u 3 TYPES: – HYPOTHYROIDISM: adult onset; tissue destruction is most probable cause – CRETINISM: u Profound hypothyroidism in infants u All developmental aspects are retarded u Severe brain damage can occur u If caught early, can prevent retardation – JUVENILE HYPOTHYROIDISM: u Begins during childhood, Hashimoto’s disease, caused by drugs, autoimmune u Affects growth and sexual maturation
THYROID u Assessments: – – – – Changed sleeping habits (increased) Lethargy, HA, wt gain Cold intolerance Dyspnea Constipation Menorrhagia Muscle aches Anorexia Lack of expression Cool, dry, skin, yellow tint, rough, thick, scaly Dry hair, coarse, lusterless Enlarged tongue Speech slow and deliberate with hoarse voice Impotence and infertility Decreased blood pressure; bradycardia; dysrhythmias; decreased urinary output
THYROID u Diagnostic tests: – Below-normal T 3 & T 4 – Above-normal TSH – Above-normal TRF – Above-normal creatinine phosphokinase – Anemia
THYROID u Interventions: – Requires life-long replacement hormone – Synthetic usually used T 4 (Levothyroid, Synthroid, Noroxine) – Start with lowest dose possible and work way up every 1 -3 weeks – With known cardiac problems, always use lowest dose possible – T 3 (Cytomel) has more rapid effect. – Euthroid (Liotrix)– combined T 3 & T 4 – Make sure client knows to continue with meds even if he feels better – Avoid sedation if possible
THYROIDITIS Inflammation of thyroid u Three types: u – Acute: bacterial; pain, malaise, fever, dysphagia; treat with antibiotics – Subacute: viral infection; fever, chills, dysphagia, pain, hard & enlarged gland; treat symptoms; antivirals – Chronic: (Hashimoto’s)- auto immune, invade thyroid with antibodies and lymphocytes causing tissue destruction; treat with thyroid hormone u Administer thyroid hormones; surgery; promote comfort and teaching
THYROID CANCER u 4 types u Surgery is treatment- total u Suppressive doses of thyroid for 3 months after surgery u Ablation- laser destruction of tissue u chemotherapy
PARATHYROIDS u u u u Parathyroid hormone corrects calcium deficiency by promoting calcium conservation by kidneys, stimulating calcium release by bone, enhance calcium absorption from GI, & reduce serum phosphate levels. Works on negative feedback control In kidneys, causes calcium to be reabsorbed with release of phosphorus Stimulates kidneys to convert Vit D to a metabolite that allows for PTH to work on bone In bone, helps convert osteoblasts to osteoclasts, promoting bone breakdown and release of calcium. Acts on GI to stimulate absorption of calcium (must have calcitriol). Calcitonin from thyroid causes inhibition of Ca++ release from bones
PARATHYROID u Hyperparathyroidism: – Primary: u Faulty PTH regulation; adenoma, genetics, CA, radiation, hyperplasia; occurs more commonly in women, 35 -65 – Secondary: u Compensatory response to defective homeostasis, chronic renal failure, malabsorption disorders – Tertiary: u Compensates for secondary malfunction to primary, leading to overgrowth of gland overproduction and secretion
PARATHYROID u All three lead to increased calcium and decreased phosphorus
PARATHYROID u Assessments: – Urine calcium increase and kidneys fail to concentrate urine – Phosphorus excretion increases – Enhances sodium, potassium, amino acids, bicarbonate (acidosis leading to excretion of Ca++ – Polyuria – Renal calculi – Bone demineralization (breakdown): u Bone pain u Pathologic fractures u Cystic bone disease
PARATHYROID u Other assessments: – – – Weakness, wt. loss, fatigue HA, depression Renal colic pain, back pain, Hematuria, renal calculi, cholelithiasis Anorexia, vomiting, constipation Peptic ulcer (stimulates gastric HCL) Increase heart contractility; decreased automaticity Increased sensitivity to digitalis Hypertension Depressed reflexes- hyporeflexia Confusion, irritability, mood swings
PARATHYROID u Diagnostic tests: – Serum PTH: elevated – Calcium: elevated (>10. 5 mg/dl; 5. 2 m. Eq/L – Kidney stones – Phosphorus: decreased – X-rays; CT; MRI: look at bone density and demineralization – PTH infusion test: (Ellsworth-Howard excretion test); give IV PTH, hourly urine samples looking for phosphorus – Calcitonin stimulation test: if cancer suspected; use calcium gluconate
PARATHYROID u Interventions: – Surgery (usually remove only three) – Stabilize calcium levels prior to surgery u Hemorrhage u Laryngeal paralysis u Difficulty swallowing u Respiratory distress u Transient hypoparathyroidism u Tetany u Muscle cramps u Hyperactive tendon reflexes u Prolonged QT on EKG u Positive Chvostek’s and Trousseau’s signs
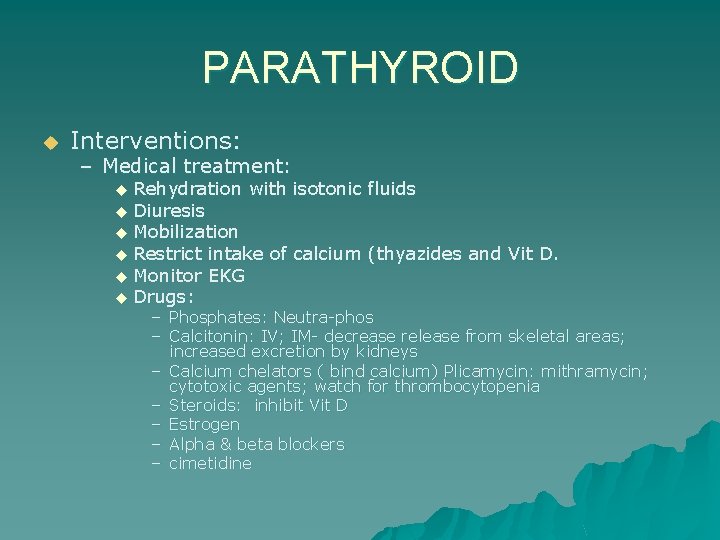
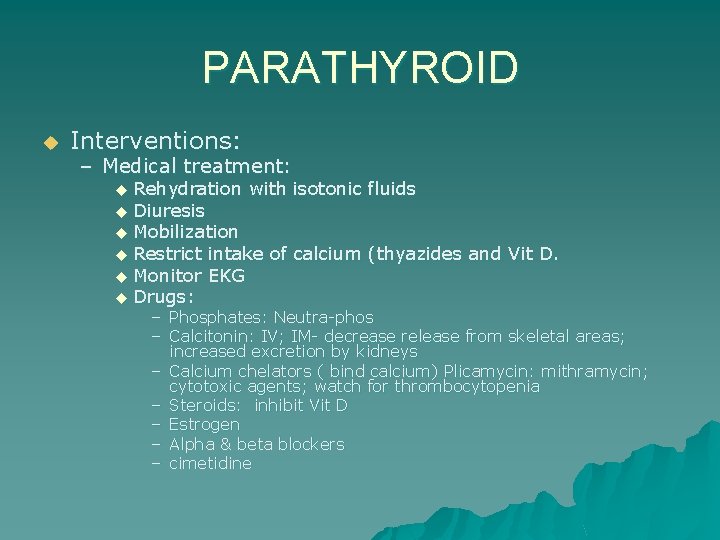
PARATHYROID u Interventions: – Medical treatment: Rehydration with isotonic fluids u Diuresis u Mobilization u Restrict intake of calcium (thyazides and Vit D. u Monitor EKG u Drugs: u – Phosphates: Neutra-phos – Calcitonin: IV; IM- decrease release from skeletal areas; increased excretion by kidneys – Calcium chelators ( bind calcium) Plicamycin: mithramycin; cytotoxic agents; watch for thrombocytopenia – Steroids: inhibit Vit D – Estrogen – Alpha & beta blockers – cimetidine
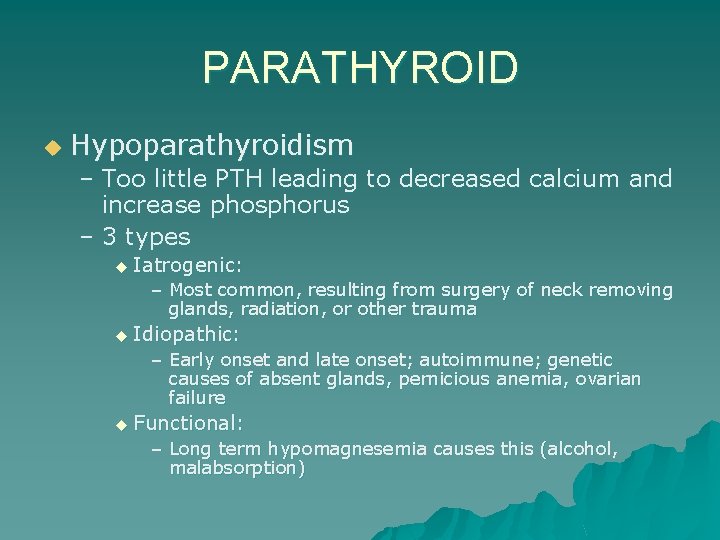
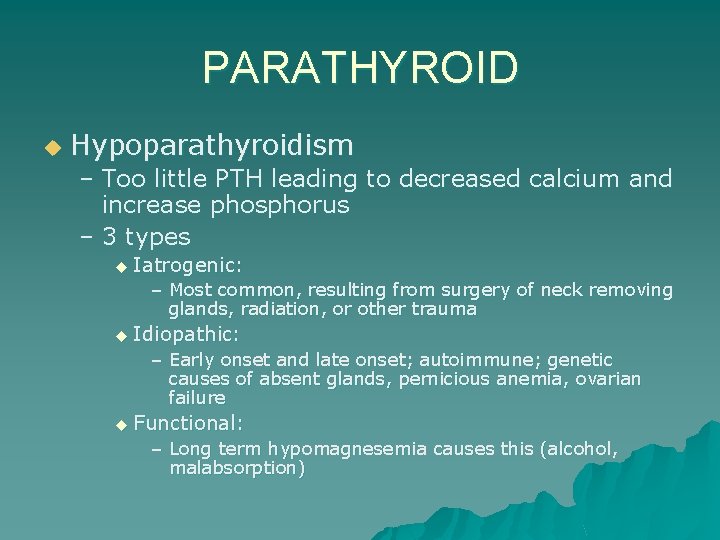
PARATHYROID u Hypoparathyroidism – Too little PTH leading to decreased calcium and increase phosphorus – 3 types u Iatrogenic: – Most common, resulting from surgery of neck removing glands, radiation, or other trauma u Idiopathic: – Early onset and late onset; autoimmune; genetic causes of absent glands, pernicious anemia, ovarian failure u Functional: – Long term hypomagnesemia causes this (alcohol, malabsorption)
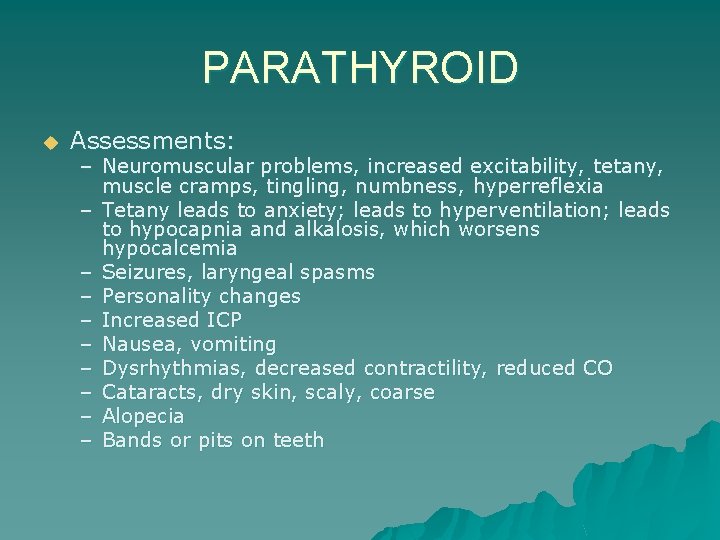
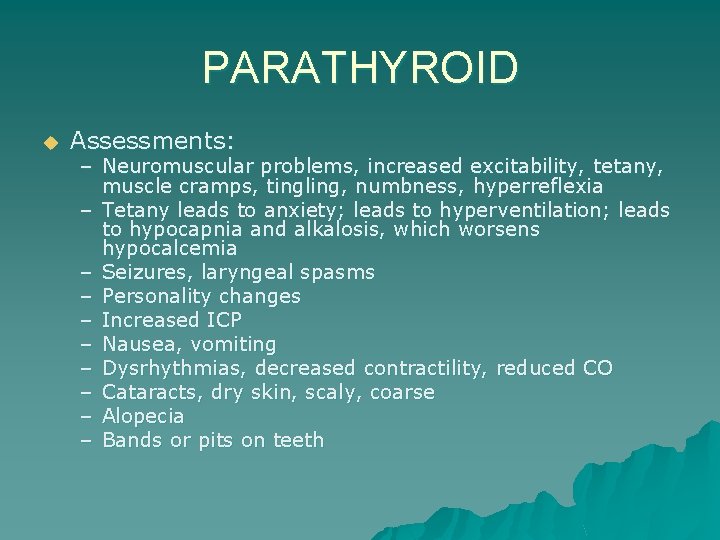
PARATHYROID u Assessments: – Neuromuscular problems, increased excitability, tetany, muscle cramps, tingling, numbness, hyperreflexia – Tetany leads to anxiety; leads to hyperventilation; leads to hypocapnia and alkalosis, which worsens hypocalcemia – Seizures, laryngeal spasms – Personality changes – Increased ICP – Nausea, vomiting – Dysrhythmias, decreased contractility, reduced CO – Cataracts, dry skin, scaly, coarse – Alopecia – Bands or pits on teeth
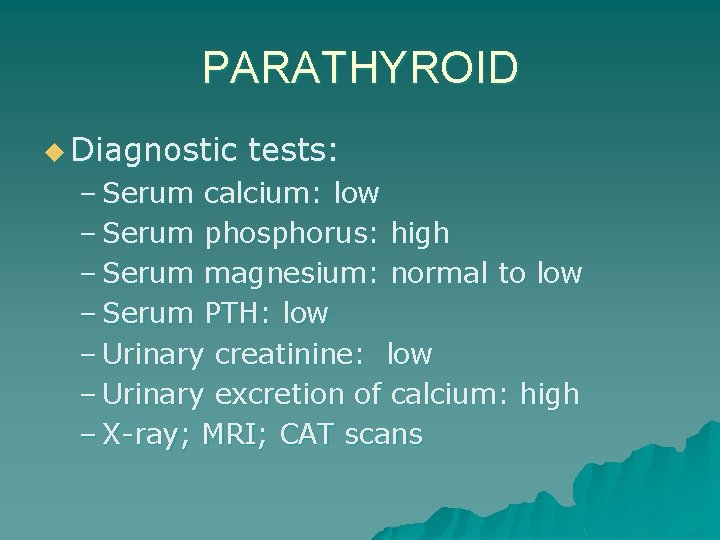
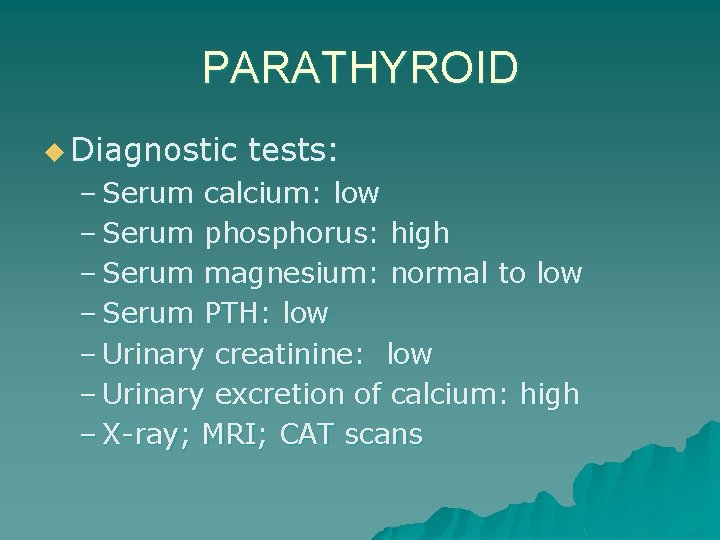
PARATHYROID u Diagnostic tests: – Serum calcium: low – Serum phosphorus: high – Serum magnesium: normal to low – Serum PTH: low – Urinary creatinine: low – Urinary excretion of calcium: high – X-ray; MRI; CAT scans
PARATHYROID u Interventions: – Treatment focuses on preventing tetany and correcting hypocalcemia u IV calcium gluconate or calcium gluconate – Do not use saline, promotes calcium and sodium excretion – Avoid bicarbonate, cause precipitation u Vit D and calcium supplements – Ergocalciferol (Vit D 2 ); Rocaltrol; may use combined therapy of oral and IV initially – Need 1 gram of calcium daily if using Vit D – Life-long therapy – Emergency airway if laryngeal spasms occur – Foods high in calcium but low in phosphorus- milk, yogurt, processed cheese.
ADRENAL GLANDS u Widespread effects, confusing clinical picture u S/S mimic many other disorders u Survival depends upon prompt diagnosis and treatment
ADRENAL GLANDS u u u Cortex secretes glucocorticoids and mineralocorticoids ACTH from anterior pituitary is controlled by CRF Other factors controlling release include stress, circadian rhythms ACTH peaks at 6 am, Cortisol at 8 am; lowest level at midnight With decreasing cortisol, ACTH is stimulated and released Stress prompts release of glucocorticoids to promote metabolism of proteins, amino acids, fatty acids, and glucose
ADRENAL GLANDS u u u Mineralocorticoids, aldosterone, is controlled by renin-agiontension system Renin is increased by blood volume, blood pressure, and Na+ Renin lead to angiotension II production and aldosterone formation K+ & Na+ directly affect aldosterone release Increased K+ increases aldosterone and Na+ decreases aldosterone Epinephrine and norephinephrine are produced, but because brain produces we can survive without adrenal medulla
ADRENAL GLAND u Assessments: – Most disorders have slow, gradual onset and progression – Changes early are subtle, hard to detect – Weight changes – Fatigue – Apathy – Depressed or neurotic – Worsens with increased stress – Physical appearance may be a clue
ADRENAL GLAND u Physical assessment: – Responds appropriately, but facial expressions do not match – Normal weight – Increased secondary sex characteristics – Fat distribution abnormal – Poor skin turgor – Purplish striae on abdomen – Pitting edema – Hyperpigmentation – Hair distribution is abnormal – Muscle weakness
ADRENAL GLANDS u Diagnostic tests: – Secreted in minute amounts, therefore most sensitive tests are RAI – Remember: if anxious, will affect results of some tests – Samples must be timed!!
ADRENAL GLANDS u Cushing’s syndrome: hypercortisolism Cortisol excess Affects more women than men Primary: u Secondary: u Iatrogenic: u u u – Usually a neoplasm – Pituitary or hypothalamus disorder causing increased ACTH; adrenal hyperplasia – Excessive use of steroids (prednisone) – Artifically increases cortisol, suppresses ACTH, causing adrenal atropy – S/S are of hyperfunction
ADRENAL GLAND Cushing’s u Assessments: – – – Fatigue, muscle wasting Frequent infections, slow wound healing Suppressed immune response ( can mask S/S); kill lymphocytes Truncal obesity, buffalo hump, moon-shaped face, scrawny arms and legs (PICKLE WITH LEGS) Fragile skin, purplish striae on abdomen, buttocks, breasts, bruises Masculinization in women, hirsutism (increased hair growth), acne Hypertension Osteoporosis Labile emotions Abnormal sleep patterns Nitrogen, carbohydrate, and mineral metabolism Elevated blood glucose
ADRENAL GLANDS CUSHING’S u Diagnostic tests: – Cortisol: high with no circadian variation – Urinary levels of steroid metabolites: high – RBC and granulocytes: high – X-rays, MRI, CAT scans – Dexamethasone suppression test: give 1 mg at night, test at 8 am; high level
ADRENAL GLAND CUSHING’S u Interventions: – Treat underlying cause; stop steroids – Remove tumors of pituitary or adrenalectomy ( uni or bi lateral) – Drugs: u Mitotane to inhibit cortisol synthesis ( watch for adrenal crisis!! u Cyproheptadine: ACTH inhibitor u Aldactone: mineralocorticoid antagonist to relieve hypertension and hypokalemia
ADRENAL GLAND CUSHING’S u Complications: – Fluid and e-lyte imbalances – Hypertension: Na+ and water retention – CHF: excess volume in compromised heart – Hypokalemia – Ventricular dysrhythmias: due to CHF and hypokalemia – Increased risk for infections & fractures – Skin breakdown
ADRENAL GLAND INSUFFICIENCY: ADDISON’S u u u Suppressed adrenocortical function and hormones May precipitate “adrenal crisis”: life-threatening Primary: – Addison’s- rare, chronic disorder – 90% gland usually destroyed before symptoms appear u Secondary: – Reduced ACTH secretion caused by pituitary disease or exogenous steroid administration; more common u Impairs stress response by reducing cortisol, aldosterone, androgens
ADRENAL GLAND ADDISON’S u Assessments: – – – – Muscle weakness and fatigue (especially during stress) Nausea, vomiting, diarrhea, abdominal pain Salt craving Anxiety, restlessness, irritability, and confusion Orthostatic hypotension HYPOGLYCEMIA & HYPERKALEMIA Hyperpigmentation (ONLY PRIMARY DISEASE HAS THIS) Knees, elbows, nipples, palm creases, scars( bronzed, “dirty tan”) u Small black freckles on neck, face; bluish splotches on mucous membranes u
ADRENAL GLANDS ADDISON’S u Diagnostic tests: – Serum cortisol: low – Urinary metabolites: low – ACTH: – ACTH stimulation: elevated cortisol=Addision’s; low cortisol=secondary disease – Hyperkalemia – Hyponatremia – Hpochloremia – Fasting hypoglycemia – BUN elevated; hematocrit HCT elevated

ADRENAL GLANDS ADDISON’S u Interventions: – Lifelong therapy with replacement – Drugs: Cortisone: twice daily, increase dose for stressful times u Florinef: aldosterone replacement u – – – – Salt food liberally Avoid fasting Eat high carbs and proteins Always wear medic alert identification Carry emergency kit with 100 mg hydrocortisone for injection Prevent acute exacerbations Avoid salt and fluid restriction with diuretics; may lead to crisis
ADRENAL GLANDS u Complications: – Adrenal crisis: due to insufficiency; can occur gradually or abruptly (acute adrenal insufficiency) – Potentially lethal – Occurs in individuals who don’t respond to therapy; increased stress without increased meds; abrupt corticosteroid withdrawal – ALWAYS WITHDRAW STEROIDS THERAPY GRADUALLY
ADRENAL GLANDS ADRENAL CRISIS u Treatment: – Restore volume with D 5 NS – Be sure to assess fluid status frequently – Cortisol q 6 hr. (Solu-Cortef IV): if given with saline, proves adequate to replace Aldosterone – Do not give methyleprednisolone (Solu. Medrol: lack mineralocorticoid effects) – Reduce anxiety
ADRENAL GLANDS PHEOCHROMOCYTOMA u Rare, benign tumor; arises in medulla u Results in hypersecretion of epinephrine and norepinephrine u Tumors appear more commonly on right side; middle-aged women u Can occur with thyroidal cancer and hyperparathyroidism-Sipple’s syndrome
PHEOCHROMOCYTOMA u Assessment: – Exaggerated flight or fight reaction – High blood pressure (Hallmark sign) 200/150 – End-organ damage; CVA, heart disease, kidney damage – Orthostatic hypotension – Attack occurs with sporadic release of catecholamines – Pounding heart beat, deep breathing, HA – Peripheral vasoconstriction – Hyperglycemia – anxiety
PHEOCHROMOCYTOMA u Attacks may occur frequently or seldom u May last minutes to hours u May result from exercise, lifting, emotional distress, exposure to cold, food, alcohol, sex, etc.
PHEOCHROMOCYTOMA u Diagnostic tests: – Must rule out all other disorders – Hyperglycemia – Elevated hematocrit – 240 urine for catecholamines and their metabolites (metanephrine(catecholamine) is more conclusive than vanillylmandelic acid(epinephrine) – EKG changes – CAT scan shows tumor – Diagnostic tests may precipitate a crisis!!!
PHEOCHROMOCYTOMA u Interventions: – Surgical removal – Prior to surgery, drugs to reduce the excessive adrenergic action (2 weeks) – Receive plasma volume expanders – During surgery, receive Regitine, alpha-adrenergic blocker to prevent hypertensive crisis – If unable to have surgery, may order drug, Demser, inhibits an enzyme promoting norepinephrine synthesis – Avoid drugs like opiates, histamines, OTC cold medications – During attack, maintain bedrest, HOB elevated to at 300 to reduce orthostatic hypotension
PHEOCHROMOCYTOMA u Complications: – Severe hypotension – CVA – Heart problems – If left untreated, always leads to death
ALDOSTERONISM Excessive secretion of mineralocorticoids, especially aldosterone u Primary: u – Called Conn’s syndrome, usually benign Aldosterone producing adenoma u Secondary: – Excess renin-angiotension stimulation; stimulation occurs with conditions involving low circulating blood volume: pregnancy, hypvolemia, CHF, cirrhosis, oral contraceptives, chronic renal failure
ALDOSTERONISM u Assessment: – Sodium and water retention, increased fluid volume, hypertension – HA, visual disturbances – Hypokalemia – Metabolic alkalosis: finger tingling and paresthesia – Increased urine output
ALDOSTERONISM u Diagnostic tests: – Decreased potassium – Elevated aldosterone – Urinary potassium elevated >30 m. Eq/L – X-rays, CAT scans, MRI
ALDOSTERONISM u Interventions: – Reduce B/P, correct hypokalemia – Surgical removal of tumor – Administer Aldactone – Potassium supplements – Sodium restriction
ALDOSTERONISM u Complications: – Hypertension and hypokalemia possibly leading to neurologic impairment – CHF – Lethal dysrhythmias – Profound muscle weakness