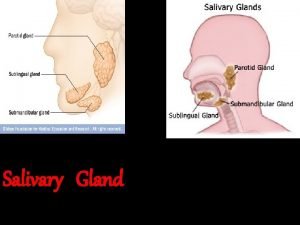
Thyroid and Parathyroid Glands Thyroid Gland This gland










- Slides: 36
Thyroid and Parathyroid Glands
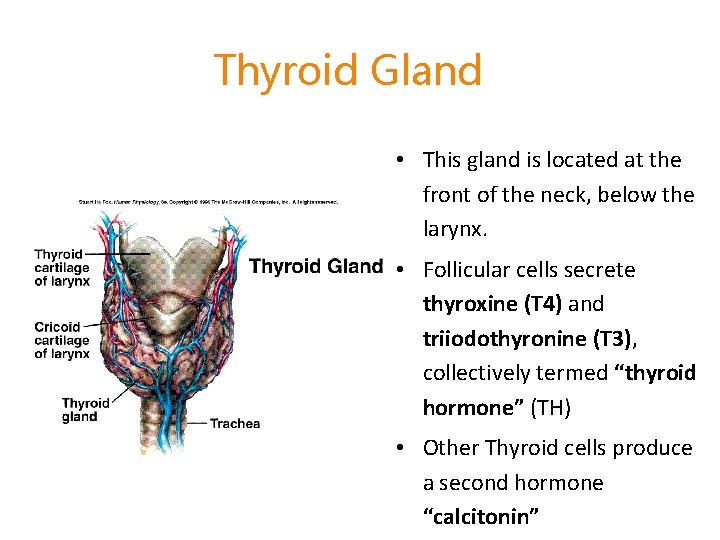
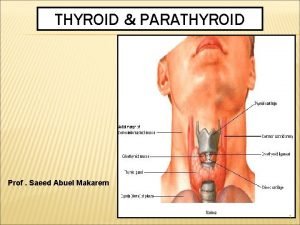
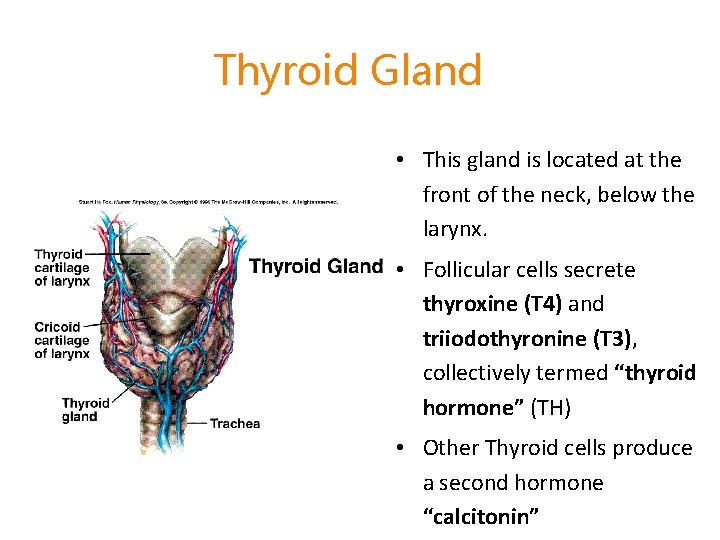
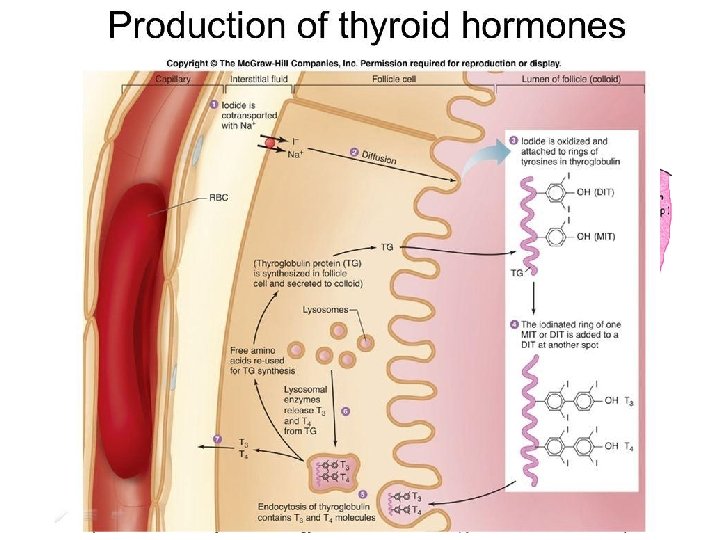
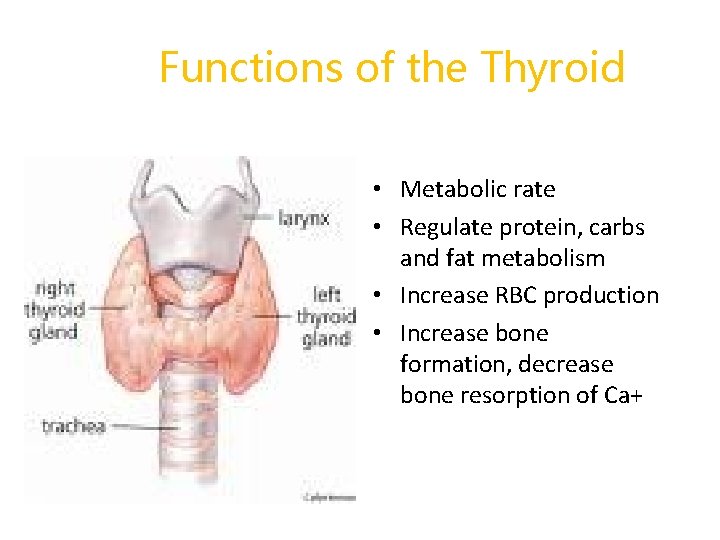
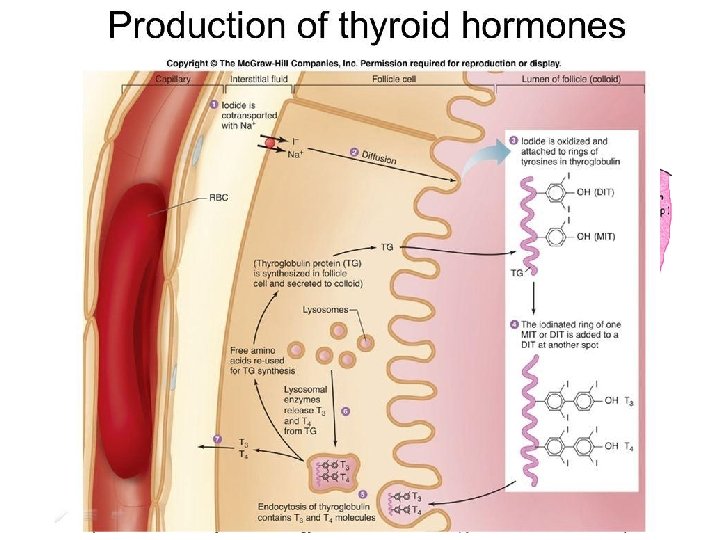
Thyroid Gland • This gland is located at the front of the neck, below the larynx. • Follicular cells secrete thyroxine (T 4) and triiodothyronine (T 3), collectively termed “thyroid hormone” (TH) • Other Thyroid cells produce a second hormone “calcitonin”
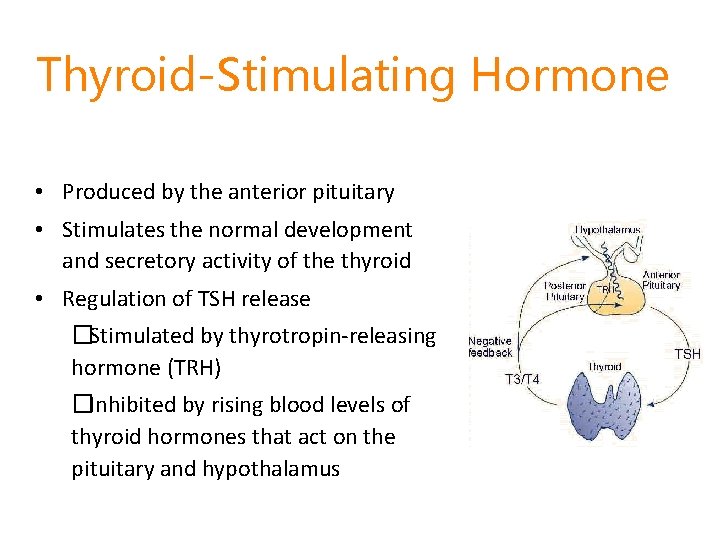
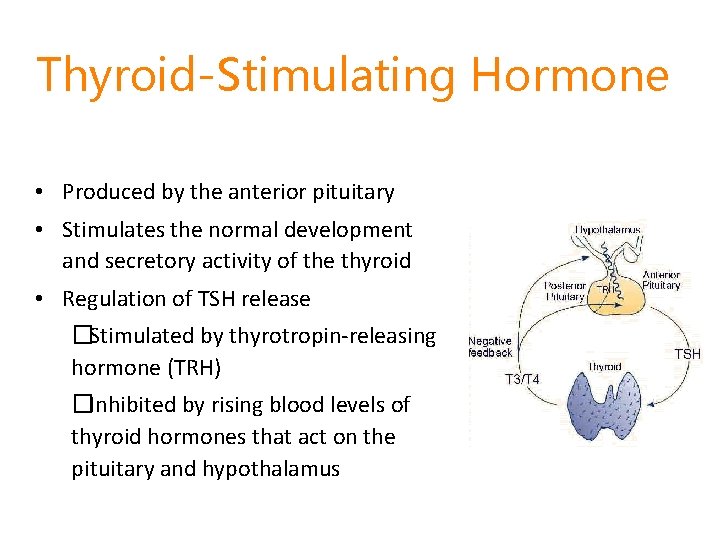
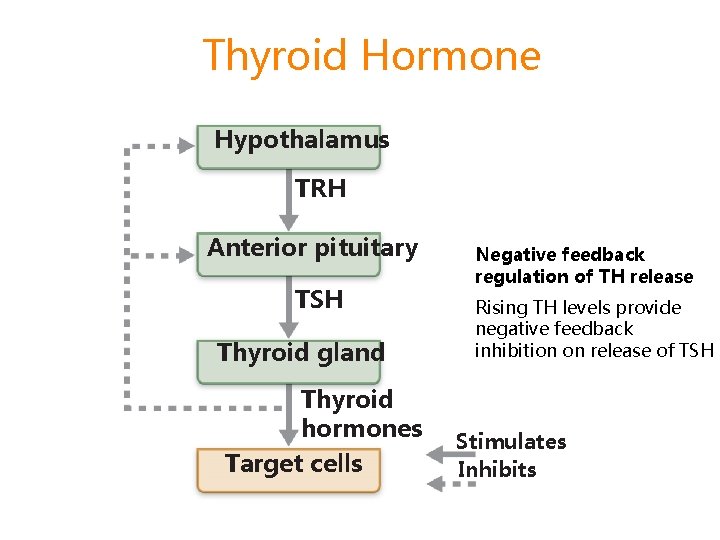
Thyroid-Stimulating Hormone • Produced by the anterior pituitary • Stimulates the normal development and secretory activity of the thyroid • Regulation of TSH release �Stimulated by thyrotropin-releasing hormone (TRH) �Inhibited by rising blood levels of thyroid hormones that act on the pituitary and hypothalamus
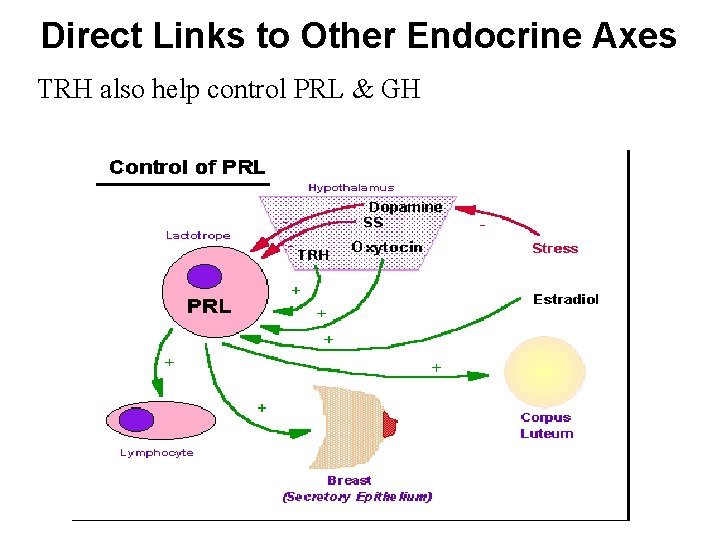
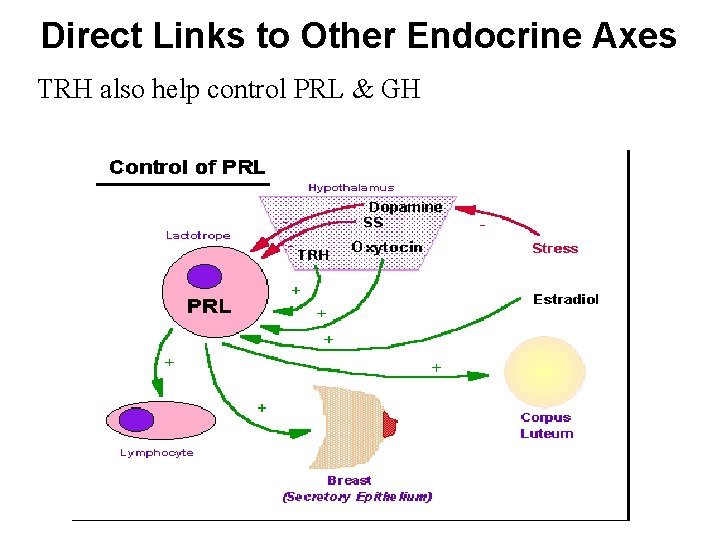
Direct Links to Other Endocrine Axes TRH also help control PRL & GH
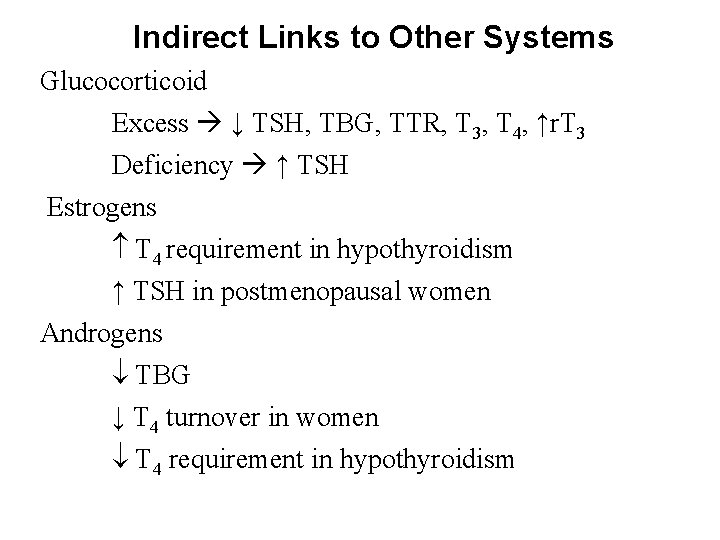
Indirect Links to Other Systems Glucocorticoid Excess ↓ TSH, TBG, TTR, T 3, T 4, ↑r. T 3 Deficiency ↑ TSH Estrogens T 4 requirement in hypothyroidism ↑ TSH in postmenopausal women Androgens TBG ↓ T 4 turnover in women T 4 requirement in hypothyroidism


Functions of the Thyroid • Metabolic rate • Regulate protein, carbs and fat metabolism • Increase RBC production • Increase bone formation, decrease bone resorption of Ca+
Regulation of Metabolism • Hormones T 3 & T 4 increase BMR • Secretion controlled by hypothalamic-pituitarythyroid gland axis • TRH » TSH » T 3 & T 4 (neg feedback) • Protein and Iodine very important for T 3 & T 4 production
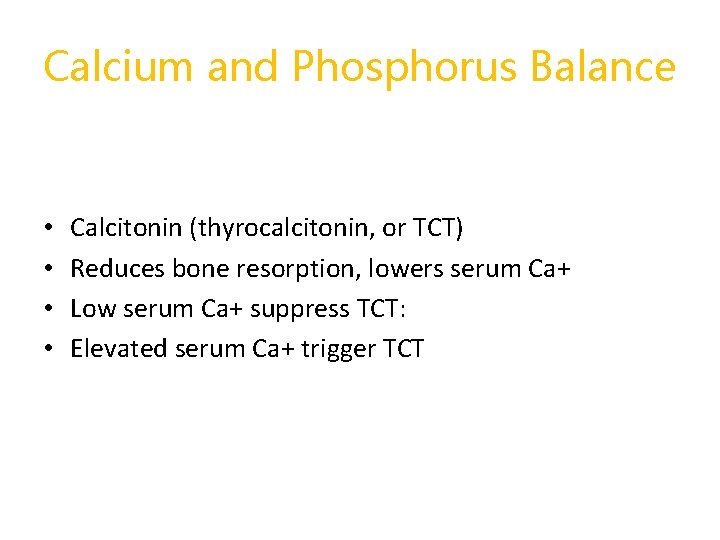
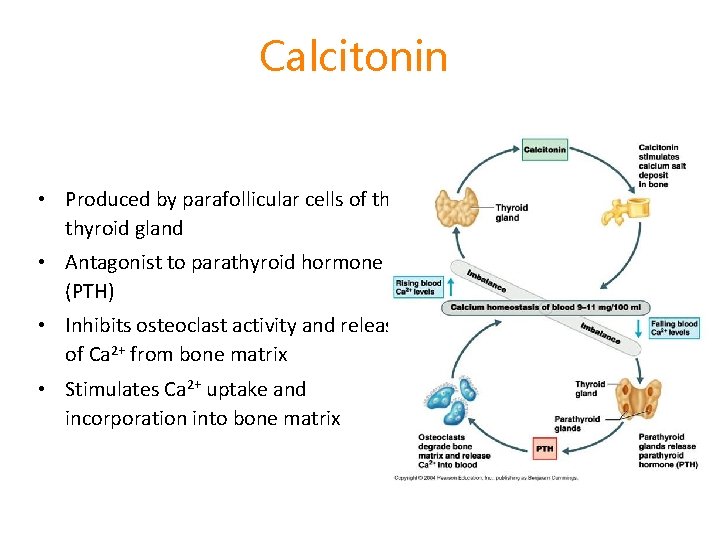
Calcium and Phosphorus Balance • • Calcitonin (thyrocalcitonin, or TCT) Reduces bone resorption, lowers serum Ca+ Low serum Ca+ suppress TCT: Elevated serum Ca+ trigger TCT
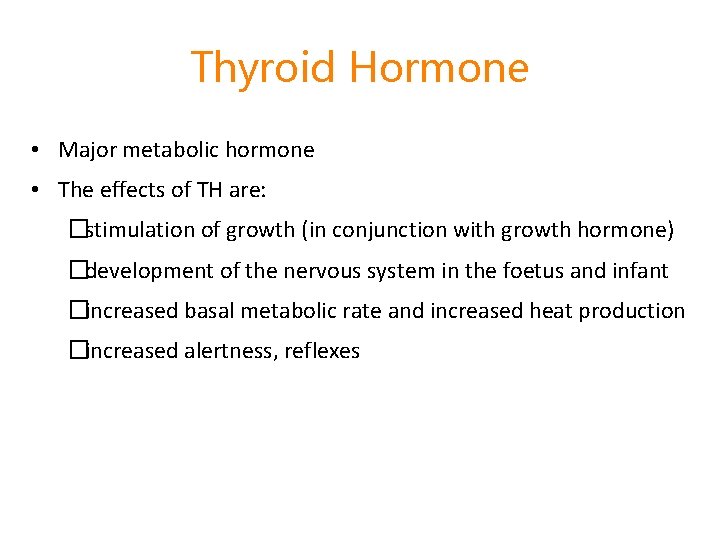
Thyroid Hormone • Major metabolic hormone • The effects of TH are: �stimulation of growth (in conjunction with growth hormone) �development of the nervous system in the foetus and infant �increased basal metabolic rate and increased heat production �increased alertness, reflexes
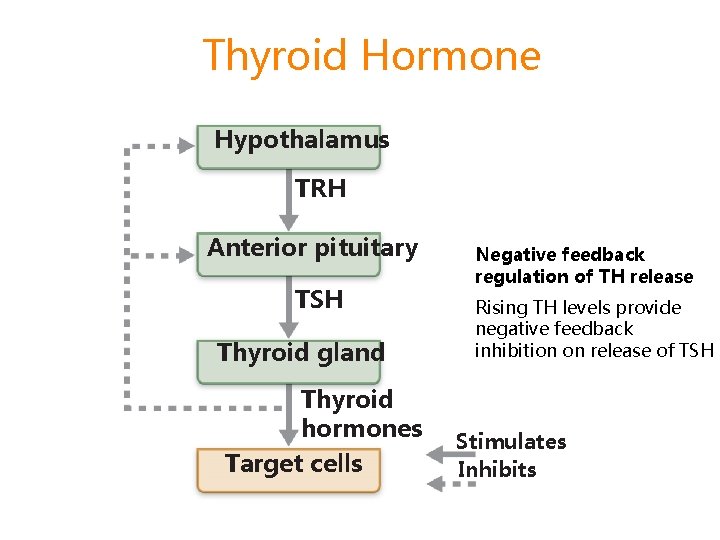
Thyroid Hormone Hypothalamus TRH Anterior pituitary TSH Thyroid gland Thyroid hormones Target cells Negative feedback regulation of TH release Rising TH levels provide negative feedback inhibition on release of TSH Stimulates Inhibits
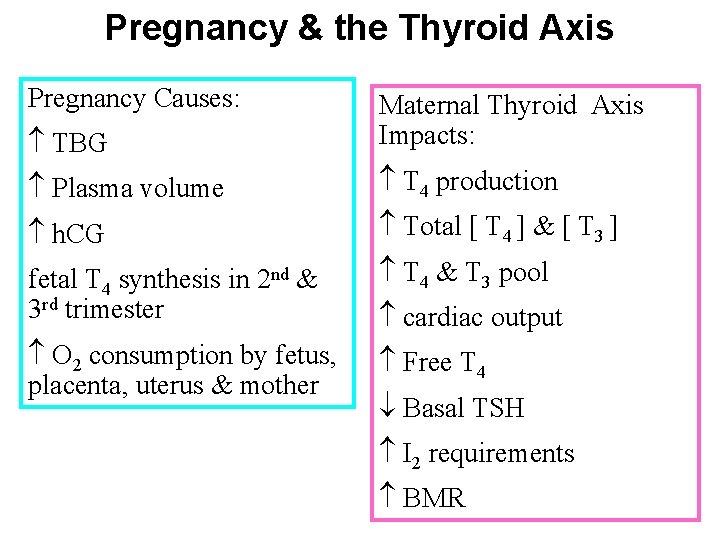
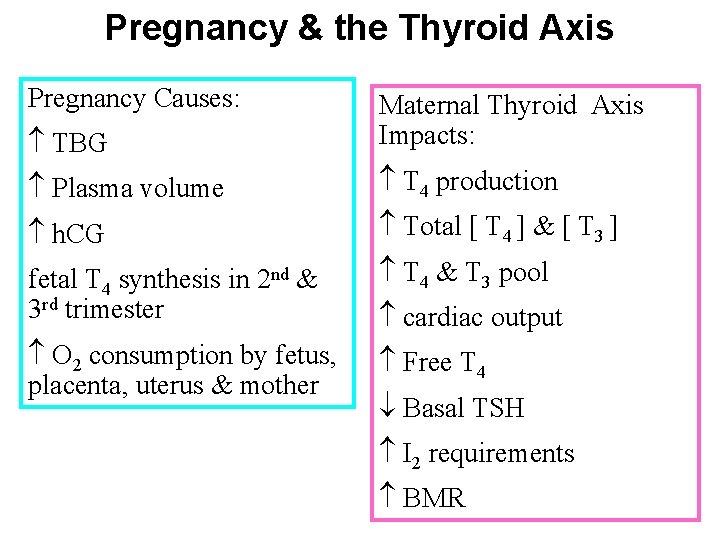
Pregnancy & the Thyroid Axis Pregnancy Causes: TBG Maternal Thyroid Axis Impacts: Plasma volume T 4 production h. CG Total [ T 4 ] & [ T 3 ] fetal T 4 synthesis in 2 nd & 3 rd trimester T 4 & T 3 pool O 2 consumption by fetus, placenta, uterus & mother Free T 4 cardiac output Basal TSH I 2 requirements BMR
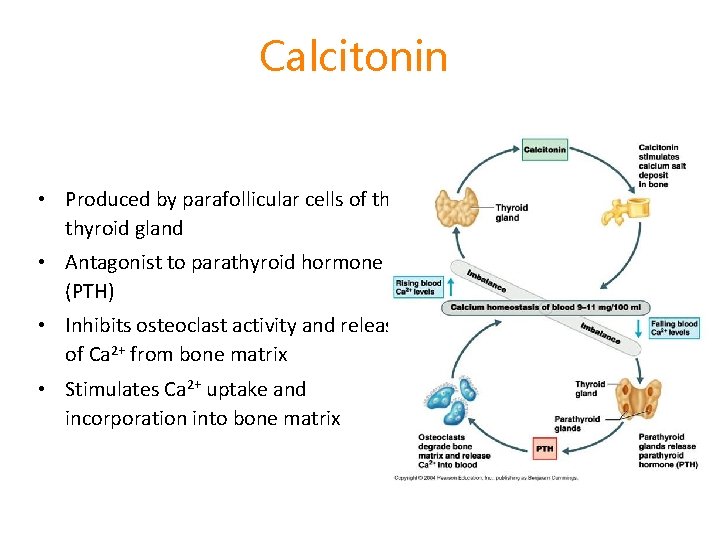
Calcitonin • Produced by parafollicular cells of the thyroid gland • Antagonist to parathyroid hormone (PTH) • Inhibits osteoclast activity and release of Ca 2+ from bone matrix • Stimulates Ca 2+ uptake and incorporation into bone matrix

Remember: Thyroid also secretes Calcitonin • Calcitonin helps--> • keep Calcium in bones • maintain balance of Calcium and Phosphorus Calcium -- 8. 8 - 10. 5 Phosphorus - 3 - 4. 5

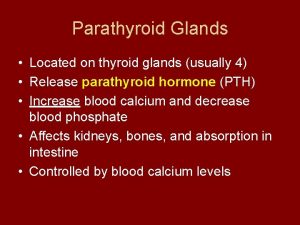
Parathyroid Glands • Four to eight tiny glands embedded in the posterior aspect of the thyroid gland • secrete parathyroid hormone (PTH), a peptide hormone • PTH—most important hormone in Ca 2+ homeostasis • Functions �Stimulates osteoclasts to digest bone matrix �Enhances reabsorption of Ca 2+ and secretion of phosphate by the kidneys �Promotes activation of vitamin D (by the kidneys); increases absorption of Ca 2+ by intestinal mucosa
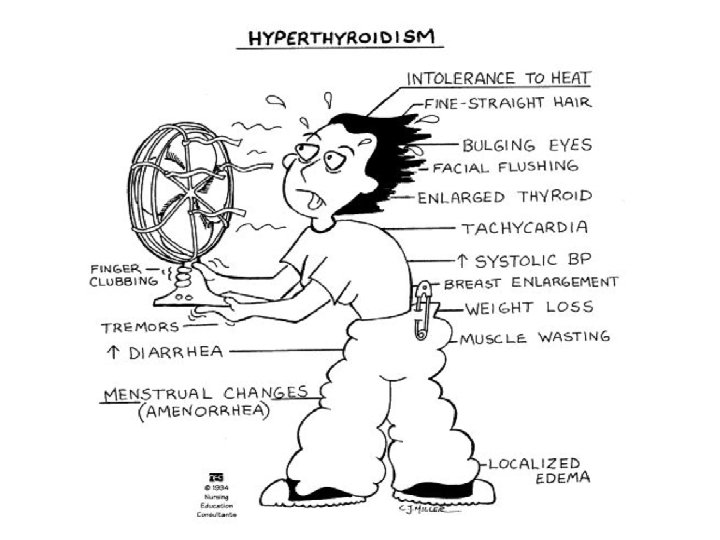
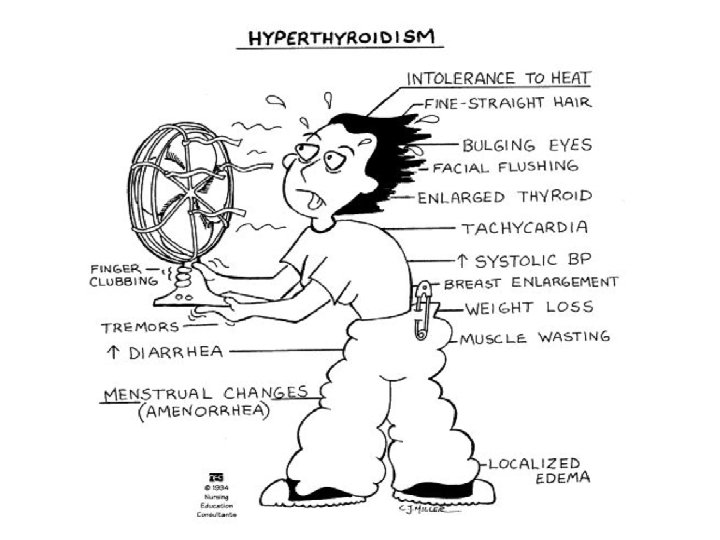
Causes of Hyperthyroidism • • • Graves’ disease (Autoimmune) Toxic multinodular goiter Thyroid adenoma (benign tumor) Pituitary hyperthyroidism Excessive use of thyroid hormone
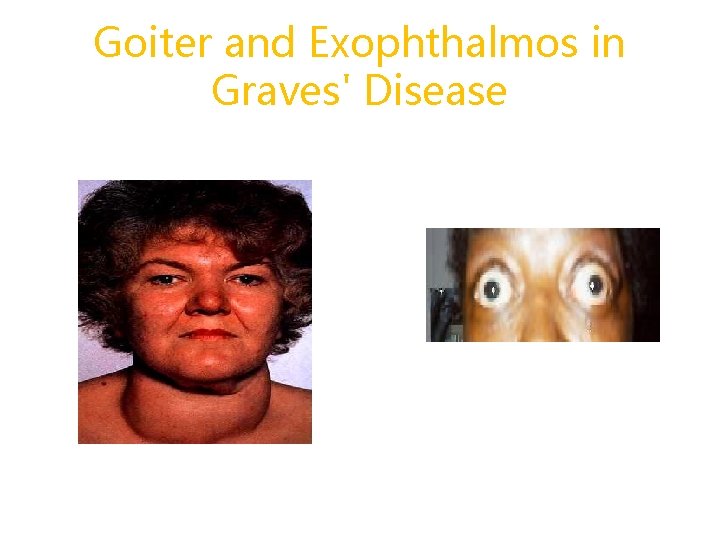
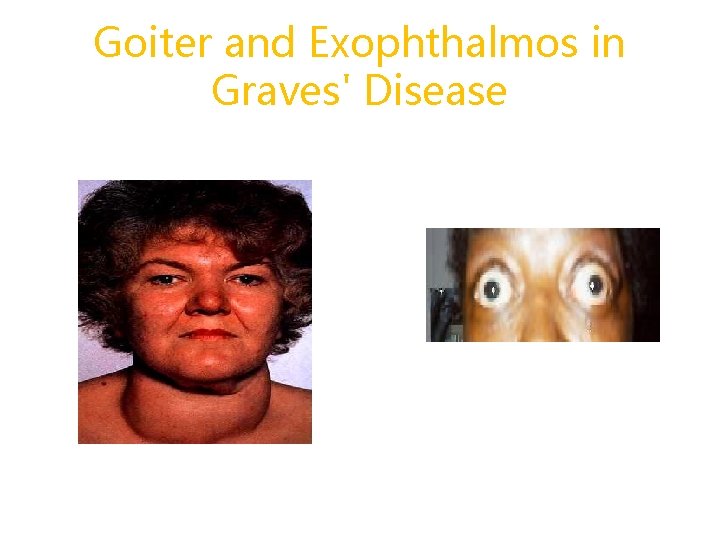
Goiter and Exophthalmos in Graves' Disease

Hyperthyroidism • • More common in women Lab assessment p. 1485: T 3, T 4 TSH (Graves’) Thyroid Scan (RAIU) = increased
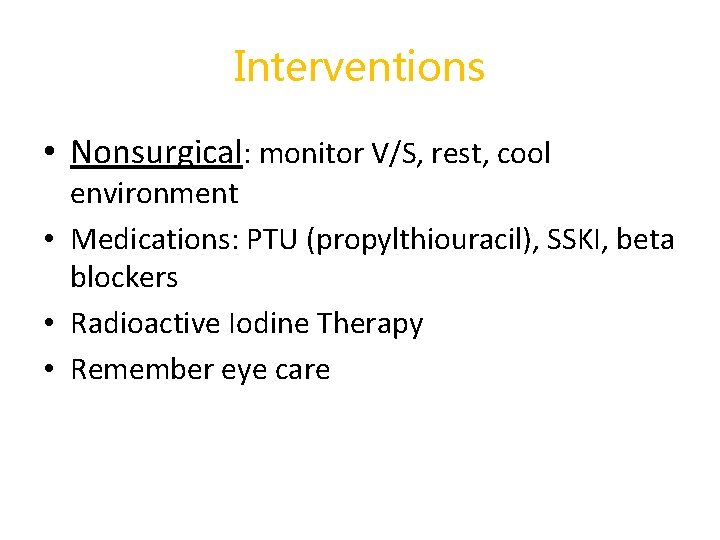
Interventions • Nonsurgical: monitor V/S, rest, cool environment • Medications: PTU (propylthiouracil), SSKI, beta blockers • Radioactive Iodine Therapy • Remember eye care
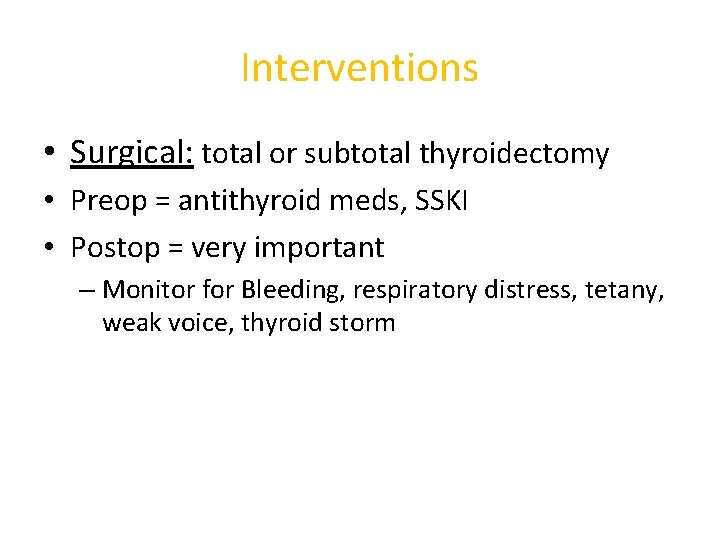
Interventions • Surgical: total or subtotal thyroidectomy • Preop = antithyroid meds, SSKI • Postop = very important – Monitor for Bleeding, respiratory distress, tetany, weak voice, thyroid storm
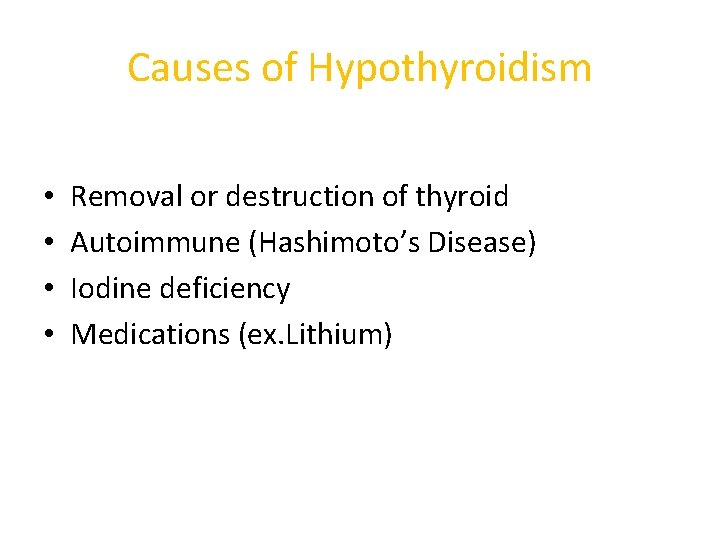
Causes of Hypothyroidism • • Removal or destruction of thyroid Autoimmune (Hashimoto’s Disease) Iodine deficiency Medications (ex. Lithium)
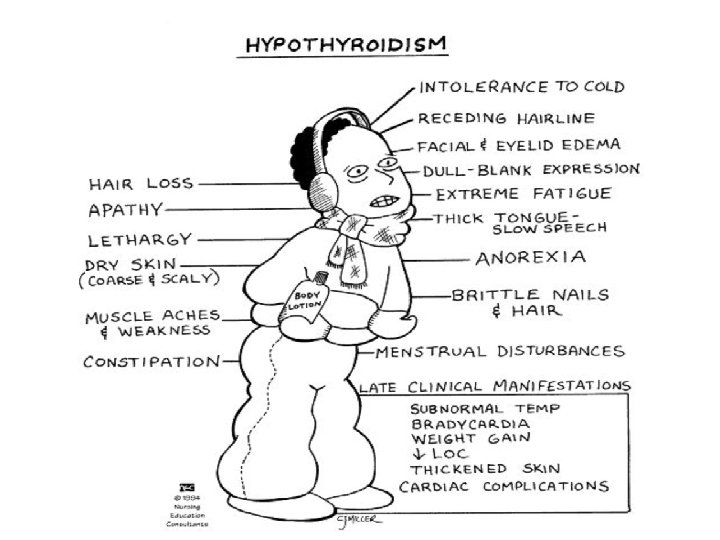

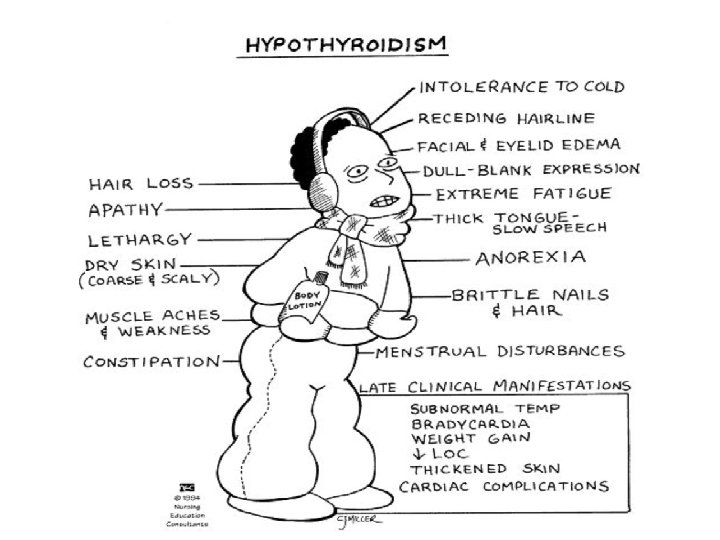
Hypothyroidism • • More common in women Lab assessment: T 3, T 4 TSH Monitor for depression

Interventions • • • Levothyroxine sodium (Synthroid) Avoid sedatives & narcotics Monitor vital signs Monitor for S&S of hyperthyroidism Family teaching re: mental status

Myxedema Coma • Hypothyroid Crisis --> rare but serious • Etiology: – acute illness/ trauma – * rapid withdrawal of thyroid meds. – use of sedatives / narcotics – surgery – exposure to cold

Myxedema Coma • • • temp / BP Na+ blood glucose Lactic acidosis Coma
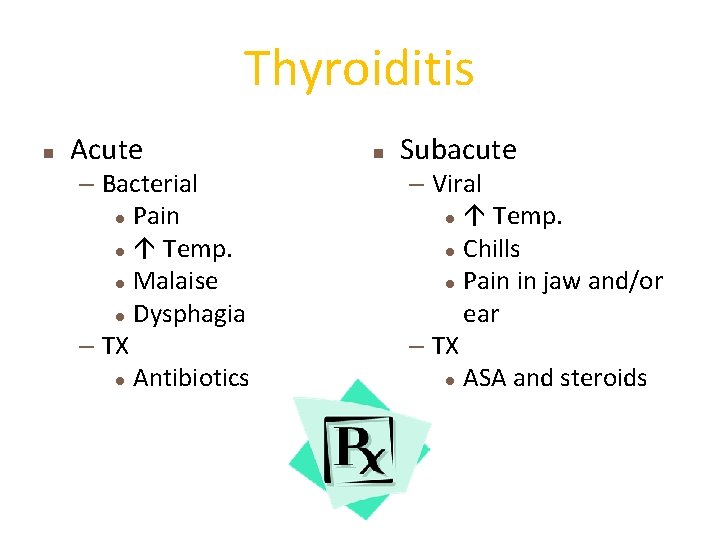
Thyroiditis n Acute – Bacterial l Pain l Temp. l Malaise l Dysphagia – TX l Antibiotics n Subacute – Viral l Temp. l Chills l Pain in jaw and/or ear – TX l ASA and steroids
Thyroid Cancer • Painless nodule in thyroid • Treatment : –RAI –Surgery
Hyperparathyroidism Pathophysiology • PTH secretion = Ca+ Phos – increased reabsorption of calcium by kidneys = • increased excretion of Phosphate • Causes – tumors – hyperplasia of parathyroid gland

Data Collection : • PTH – renal calculi – nephrocalcinosis – bone decalcification • serum Ca – GI: anorexia, N&V, epigastric pain, constipation, – M/S: fatigue & lethargy – [serum Ca] > 12 mg/dl = mental status
Complications: • Renal Failure • Fractures • Collapse of vertebra
Collaborative Management : focuses to decrease serum calcium • Diuretic & Fluid Therapy – Lasix /0. 9% Na Cl • Drug therapy – Phosphates – Calcitonin -miacalin spray Skel. Release Renal clearance – Calcium Chelators - binds with Ca. -< dec. Levels of free calcium • Parathyroidectomy
Hypoparathyroidism • PTH • Etiology (rare) – thyroid / parathyroid surgery – Hypomagnesemia – Idiopathic
 Kocher vein
Kocher vein Thyroid and parathyroid glands histology
Thyroid and parathyroid glands histology Parathyroid glands
Parathyroid glands Pseudostratified columnar epithelium in trachea
Pseudostratified columnar epithelium in trachea Thyroid scan
Thyroid scan Parathyroid hormone and calcitonin
Parathyroid hormone and calcitonin Zona glomerulosa produces
Zona glomerulosa produces Parathyroid gland chief cell
Parathyroid gland chief cell Pharyngeal arch pouch and cleft
Pharyngeal arch pouch and cleft Pituitary gland and pineal gland spiritual
Pituitary gland and pineal gland spiritual Enlarged thyroid gland
Enlarged thyroid gland Graves disease
Graves disease Enlarged thyroid gland
Enlarged thyroid gland Principal cells location
Principal cells location Follicular cells of thyroid gland
Follicular cells of thyroid gland Pineal gland
Pineal gland Cretinism diagram
Cretinism diagram Is thyroid a lymphatic organ
Is thyroid a lymphatic organ Histology thyroid gland
Histology thyroid gland Hashitoxicosis
Hashitoxicosis Swollen thyroid
Swollen thyroid Hyperparathyrodism
Hyperparathyrodism Thyroid symptoms
Thyroid symptoms Four oval masses on posterior thyroid gland
Four oval masses on posterior thyroid gland Thyoid gland
Thyoid gland Vitamin d and calcitonin
Vitamin d and calcitonin Cytoclast
Cytoclast Superior thyroid artery is a branch of
Superior thyroid artery is a branch of Parathyroid hormone pathway
Parathyroid hormone pathway Adenohypophsis
Adenohypophsis Major endocrine glands male and female
Major endocrine glands male and female Chapter 16 matching questions 20-24
Chapter 16 matching questions 20-24 Difference between endocrine and exocrine glands
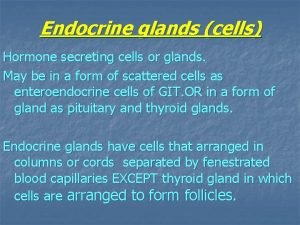
Difference between endocrine and exocrine glands It has fur and mammary glands
It has fur and mammary glands Whats the difference between endocrine and exocrine glands
Whats the difference between endocrine and exocrine glands Dopamine agonists
Dopamine agonists Pineal and pancreas glands
Pineal and pancreas glands