The Thunderclap Headache Amy Yu PGY3 July 14



- Slides: 50
The Thunderclap Headache Amy Yu, PGY-3 July 14 2010 Mc. Gill University
Outline l Subarachnoid hemorrhage l l Why do we care? How do we diagnose it? Then what? Migraine l l Evaluation Treatment
SAH – Why do we care? l l Because it can kill your patient Average case fatality rate 51% l l l 10% die before reaching the hospital 25% die within 24 hours of SAH onset 45% percent die within 30 days Because you can do something about it 30 -50% have sentinel bleed or "warning leak“ l Sudden and severe headache preceding SAH by 6 -20 days
SAH – Etiology l Most SAHs are caused by ruptured saccular aneurysms l l l 15 -20% negative angiography 24% will have lesion on 2 nd angiography Other etiologies l Trauma, AVM, vasculitides, intracranial arterial dissections, amyloid angiopathy, bleeding diatheses, and illicit drug use (cocaine and amphetamines)
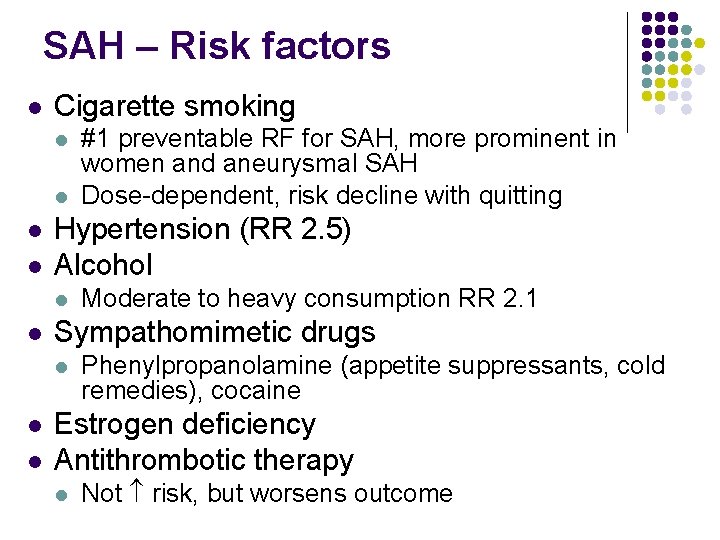
SAH – Risk factors l Cigarette smoking l l Hypertension (RR 2. 5) Alcohol l Moderate to heavy consumption RR 2. 1 Sympathomimetic drugs l l #1 preventable RF for SAH, more prominent in women and aneurysmal SAH Dose-dependent, risk decline with quitting Phenylpropanolamine (appetite suppressants, cold remedies), cocaine Estrogen deficiency Antithrombotic therapy l Not risk, but worsens outcome
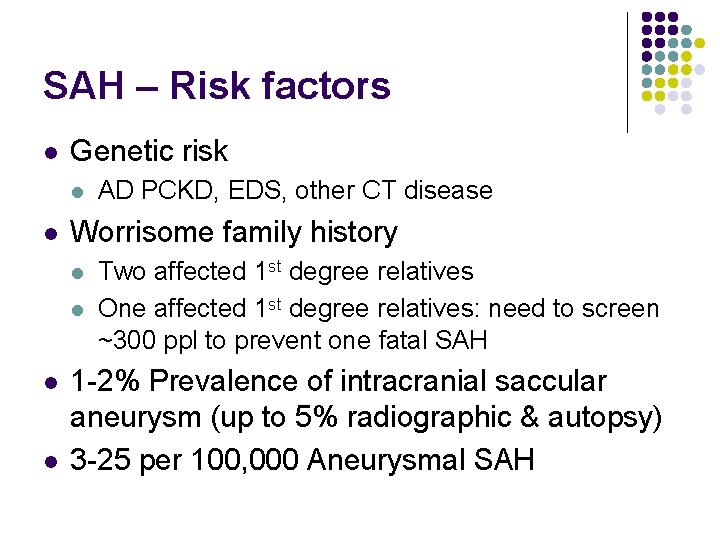
SAH – Risk factors l Genetic risk l l Worrisome family history l l AD PCKD, EDS, other CT disease Two affected 1 st degree relatives One affected 1 st degree relatives: need to screen ~300 ppl to prevent one fatal SAH 1 -2% Prevalence of intracranial saccular aneurysm (up to 5% radiographic & autopsy) 3 -25 per 100, 000 Aneurysmal SAH
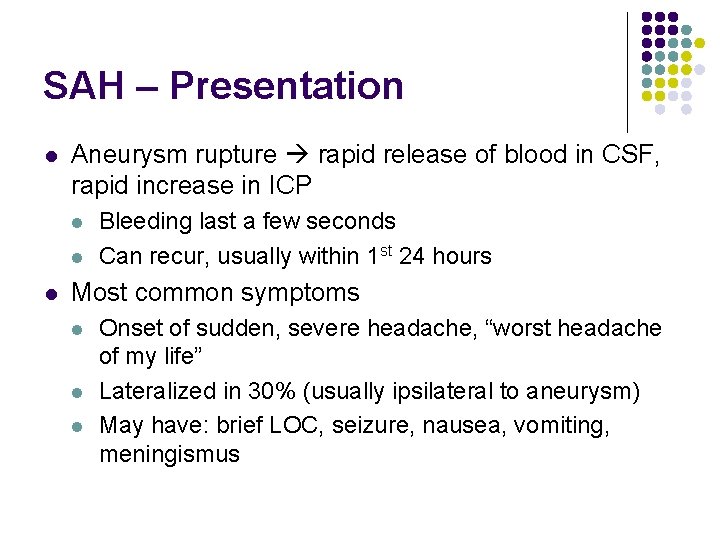
SAH – Presentation l Aneurysm rupture rapid release of blood in CSF, rapid increase in ICP l l l Bleeding last a few seconds Can recur, usually within 1 st 24 hours Most common symptoms l l l Onset of sudden, severe headache, “worst headache of my life” Lateralized in 30% (usually ipsilateral to aneurysm) May have: brief LOC, seizure, nausea, vomiting, meningismus
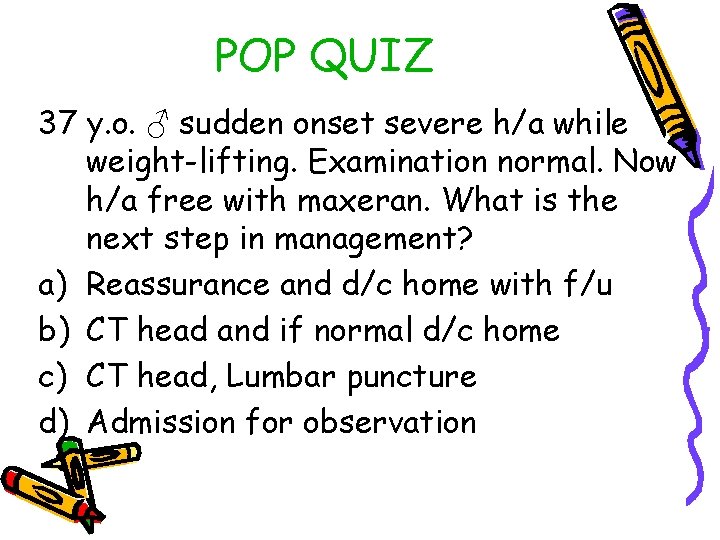
POP QUIZ 37 y. o. ♂ sudden onset severe h/a while weight-lifting. Examination normal. Now h/a free with maxeran. What is the next step in management? a) Reassurance and d/c home with f/u b) CT head and if normal d/c home c) CT head, Lumbar puncture d) Admission for observation
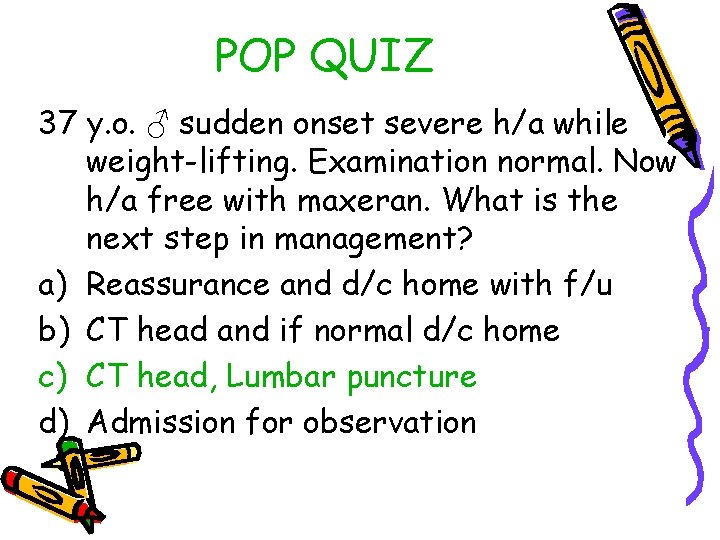
POP QUIZ 37 y. o. ♂ sudden onset severe h/a while weight-lifting. Examination normal. Now h/a free with maxeran. What is the next step in management? a) Reassurance and d/c home with f/u b) CT head and if normal d/c home c) CT head, Lumbar puncture d) Admission for observation
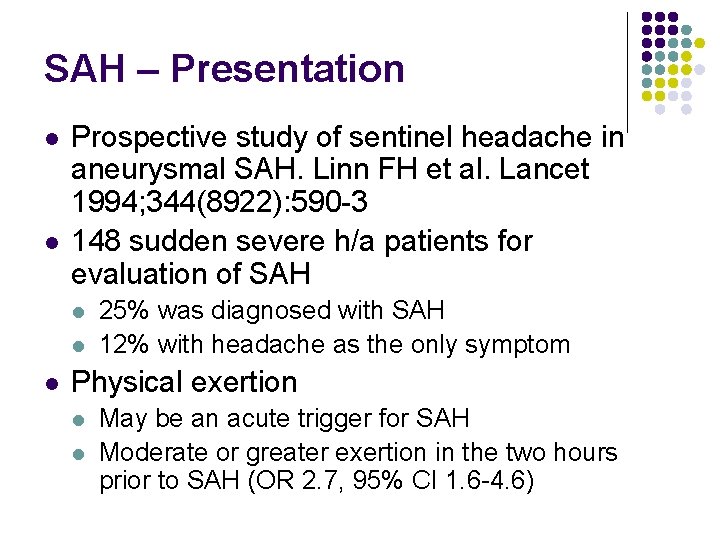
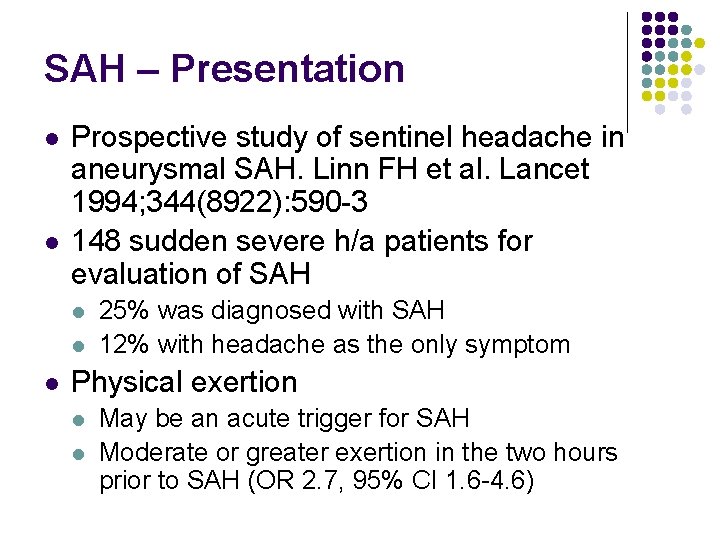
SAH – Presentation l l Prospective study of sentinel headache in aneurysmal SAH. Linn FH et al. Lancet 1994; 344(8922): 590 -3 148 sudden severe h/a patients for evaluation of SAH l l l 25% was diagnosed with SAH 12% with headache as the only symptom Physical exertion l l May be an acute trigger for SAH Moderate or greater exertion in the two hours prior to SAH (OR 2. 7, 95% CI 1. 6 -4. 6)

SAH – Physical examination l l l Retinal hemorrhage Vitreous hemorrhage (Terson’s syndrome) Meningismus Decreased level of consciousness Focal neuro signs (CN III palsy, CN VI palsy, bilateral leg weakness)
POP QUIZ Why are the following signs seen in aneurysmal SAH? a) CN III palsy b) CN VI palsy c) Bilateral leg weakness
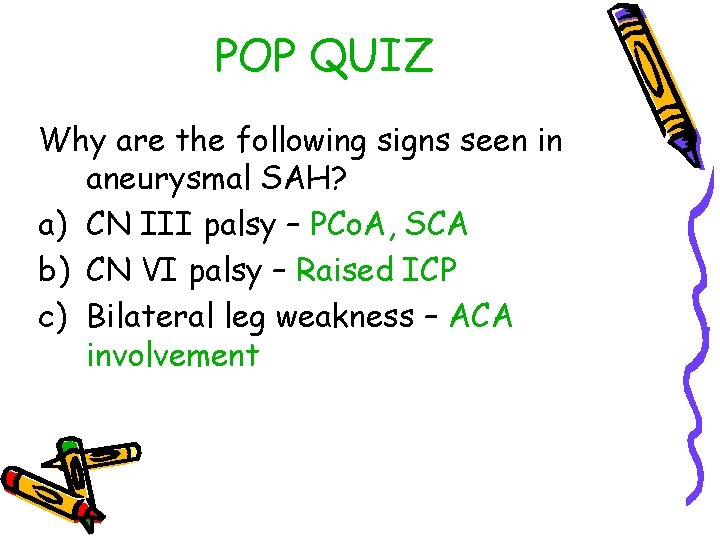
POP QUIZ Why are the following signs seen in aneurysmal SAH? a) CN III palsy – PCo. A, SCA b) CN VI palsy – Raised ICP c) Bilateral leg weakness – ACA involvement
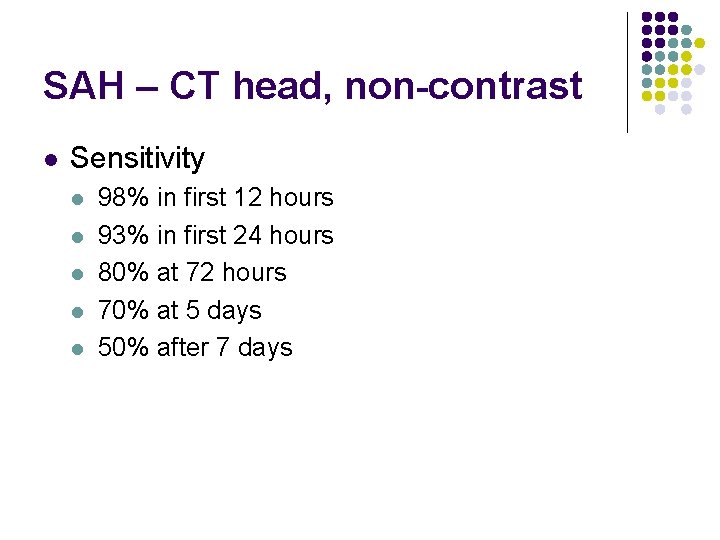
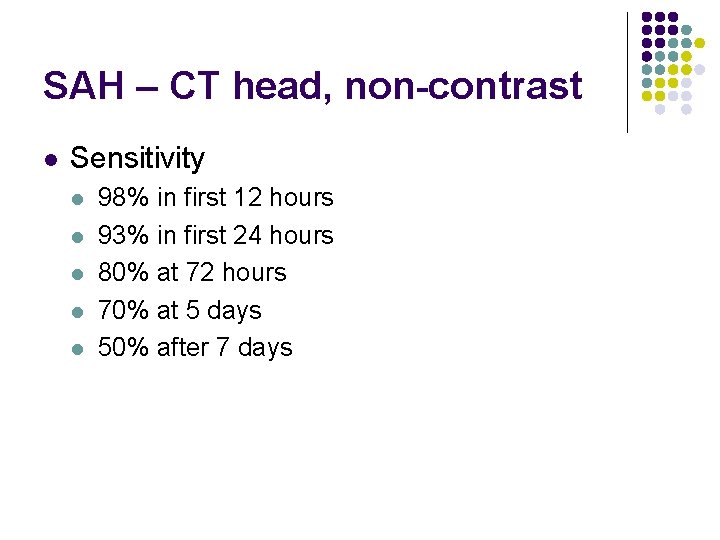
SAH – CT head, non-contrast l Sensitivity l l l 98% in first 12 hours 93% in first 24 hours 80% at 72 hours 70% at 5 days 50% after 7 days
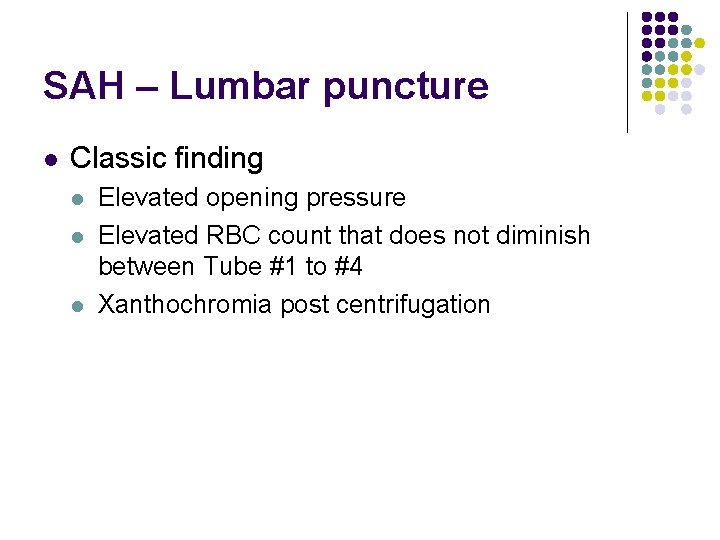
SAH – Lumbar puncture l Classic finding l l l Elevated opening pressure Elevated RBC count that does not diminish between Tube #1 to #4 Xanthochromia post centrifugation
POP QUIZ LP done for first thunderclap headache, CT head normal Tube #1 132 RBC, Tube #4 19 RBC a) What is your diagnosis? b) What further information would you like? c) What is the next step?
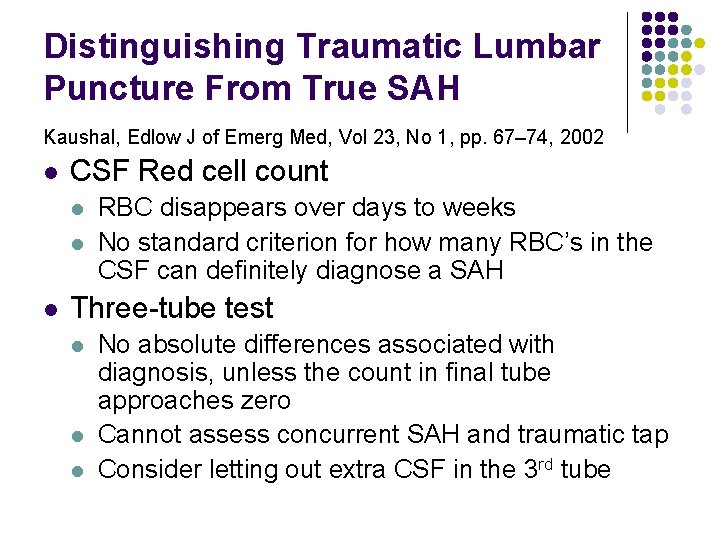
Distinguishing Traumatic Lumbar Puncture From True SAH Kaushal, Edlow J of Emerg Med, Vol 23, No 1, pp. 67– 74, 2002 l CSF Red cell count l l l RBC disappears over days to weeks No standard criterion for how many RBC’s in the CSF can definitely diagnose a SAH Three-tube test l l l No absolute differences associated with diagnosis, unless the count in final tube approaches zero Cannot assess concurrent SAH and traumatic tap Consider letting out extra CSF in the 3 rd tube
SAH vs. Traumatic tap l Xanthochromia l l l Hemoglobin degradation appears 4 -10 hours from bleed, may last for > 2 weeks Needs immediate centrifugation and analysis Visual inspection very poor specificity Need spectrophotometry, but unavailable at most centres Sensitive, but non-specific
SAH vs. Traumatic tap l Differential of xanthochromia l l l High CSF protein Jaundice Carotene addiction Meningitis Severe degenerative disc disease
SAH vs. Traumatic tap l Opening pressure l l l Other tests l l l Can help R/O other conditions (IIH, CSVT) Not elevated in traumatic tap, is elevated in 60% of SAH Abbrescia KL, The effect of lower-extremity position on cerebrospinal fluid pressures, Acad Emerg Med. 2001 Jan; 8(1): 8 -12. Positioning of the legs lead to 1 cm. H 2 O difference CSF D-dimer CSF Bilirubin Requires further validation Repeat LP at higher interspace Clot formation
You diagnose SAH, now what? l l Consult neurosurgery and neuroradiology CTA and MRA l l Non-invasive Useful for screening and surgical planning Sensitive at identifying aneurysms >3 -5 mm CTA 83 -98%
Pitfalls in SAH evaluation l l Be alert and think about SAH when faced with acute, severe headache Understand the limitations of CT head If you think about doing an LP, you should probably do it CTA or MRA are not diagnostic tests for SAH l Remember that 2 -5% of the population may have an unruptured aneurysm
DDx of thunderclap headache l l l l Other vascular disease (AVM, dissection) Intracerebral hemorrhage Migraine headache Tension headache CVST Pituitary apoplexy CSF hypovolemia syndrome Syncope
Part II: Migraine management
Migraine epidemiology l Migraine prevalence l l 18% female 6% male Highest among 25 -55 year olds International classification of headache disorders (2004)
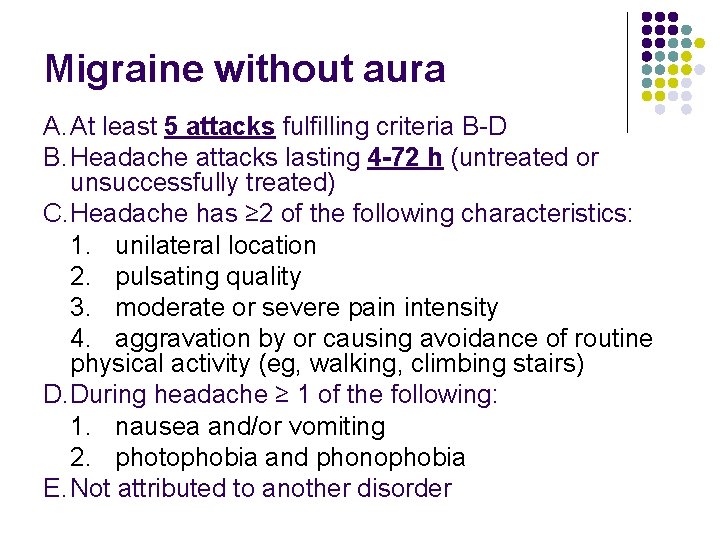
Migraine without aura A. At least 5 attacks fulfilling criteria B-D B. Headache attacks lasting 4 -72 h (untreated or unsuccessfully treated) C. Headache has ≥ 2 of the following characteristics: 1. unilateral location 2. pulsating quality 3. moderate or severe pain intensity 4. aggravation by or causing avoidance of routine physical activity (eg, walking, climbing stairs) D. During headache ≥ 1 of the following: 1. nausea and/or vomiting 2. photophobia and phonophobia E. Not attributed to another disorder
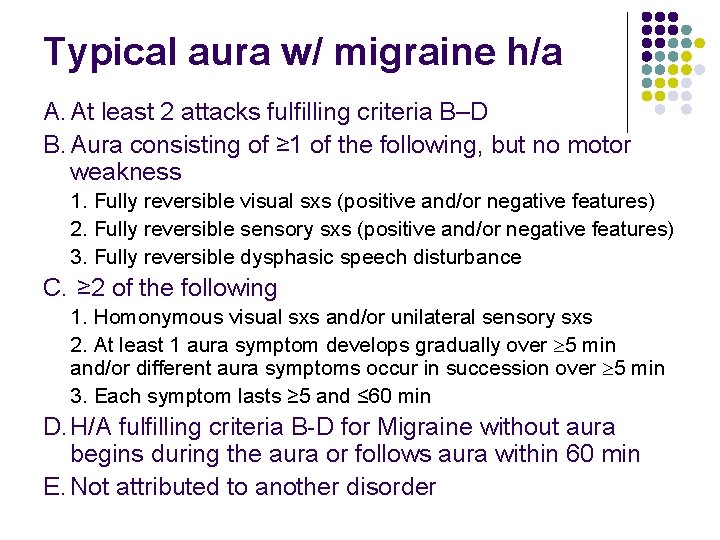
Typical aura w/ migraine h/a A. At least 2 attacks fulfilling criteria B–D B. Aura consisting of ≥ 1 of the following, but no motor weakness 1. Fully reversible visual sxs (positive and/or negative features) 2. Fully reversible sensory sxs (positive and/or negative features) 3. Fully reversible dysphasic speech disturbance C. ≥ 2 of the following 1. Homonymous visual sxs and/or unilateral sensory sxs 2. At least 1 aura symptom develops gradually over 5 min and/or different aura symptoms occur in succession over 5 min 3. Each symptom lasts ≥ 5 and ≤ 60 min D. H/A fulfilling criteria B-D for Migraine without aura begins during the aura or follows aura within 60 min E. Not attributed to another disorder
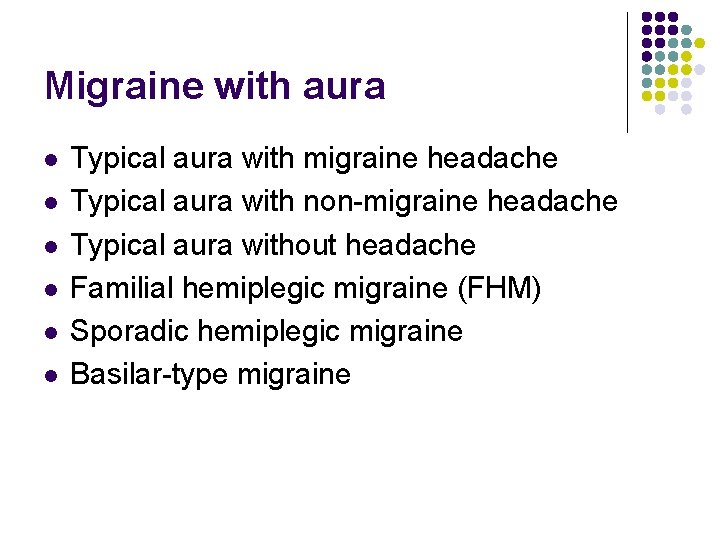
Migraine with aura l l l Typical aura with migraine headache Typical aura with non-migraine headache Typical aura without headache Familial hemiplegic migraine (FHM) Sporadic hemiplegic migraine Basilar-type migraine
The rational clinical examination series l l l Does This Patient With Headache Have a Migraine or Need Neuroimaging? Michael E. Detsky et al. JAMA, September 13, 2006, Vol 296, No. 10
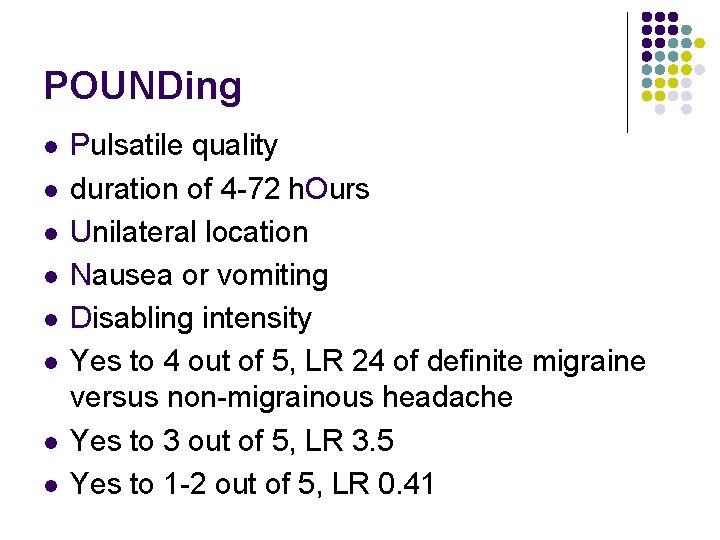
POUNDing l l l l Pulsatile quality duration of 4 -72 h. Ours Unilateral location Nausea or vomiting Disabling intensity Yes to 4 out of 5, LR 24 of definite migraine versus non-migrainous headache Yes to 3 out of 5, LR 3. 5 Yes to 1 -2 out of 5, LR 0. 41
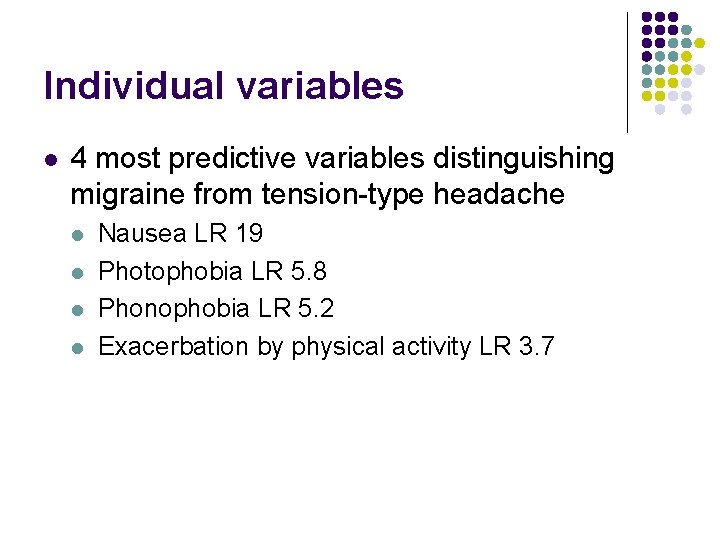
Individual variables l 4 most predictive variables distinguishing migraine from tension-type headache l l Nausea LR 19 Photophobia LR 5. 8 Phonophobia LR 5. 2 Exacerbation by physical activity LR 3. 7
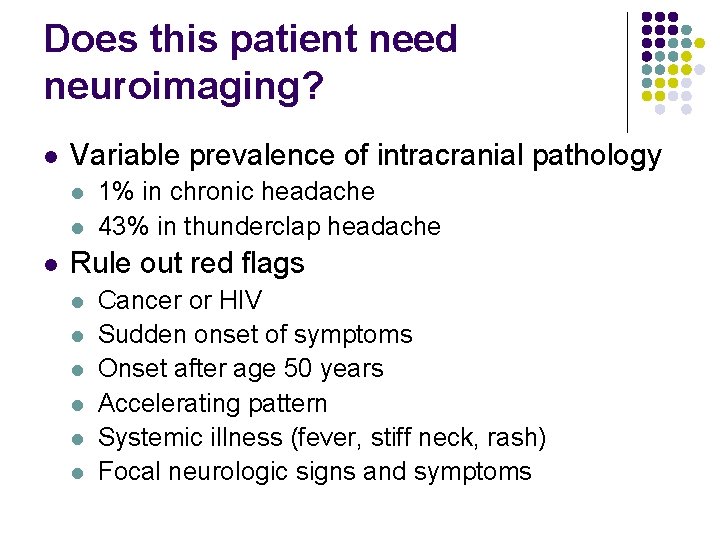
Does this patient need neuroimaging? l Variable prevalence of intracranial pathology l l l 1% in chronic headache 43% in thunderclap headache Rule out red flags l l l Cancer or HIV Sudden onset of symptoms Onset after age 50 years Accelerating pattern Systemic illness (fever, stiff neck, rash) Focal neurologic signs and symptoms
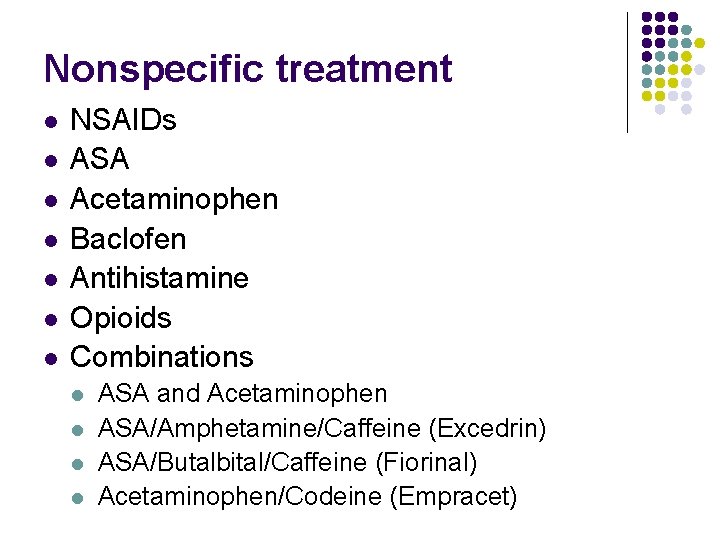
Nonspecific treatment l l l l NSAIDs ASA Acetaminophen Baclofen Antihistamine Opioids Combinations l l ASA and Acetaminophen ASA/Amphetamine/Caffeine (Excedrin) ASA/Butalbital/Caffeine (Fiorinal) Acetaminophen/Codeine (Empracet)
Nonspecific treatment l NSAIDs l l l ASA 1 gm IV is used in Europe for acute migraine l l 1 gm effervescent ASA (Alka-Seltzer) Avoid Opioids l l l Ensure adequate trial, e. g. Advil Gel caps 600 mg at onset of headache May reverse central sensitization in migraine Significant side effect (nausea, sedation, etc. ) May worsen central sensitization Avoid Butalbital (Fiorinal) l l No benefit shown High risk of habituation and dependency
Aspirin with or w/o antiemetic for acute migraine h/a in adults Kirthi V et al. Cochrane Database Syst Rev. 2010 Apr 14; 4: CD 008041 l ASA 900 mg or 1000 mg superior to placebo l l l NNTs 8. 1 (2 -hr pain-free), 4. 9 (2 -hr h/a relief), 6. 6 (24 -hr h/a relief) ASA reduces N/V, photo-, phonophobia Metoclopramide significantly further reduces N/V Sumatriptan 100 mg was better only for 2 -hour pain-free Adverse events with ASA l l l Mostly mild and transient Slightly more often than placebo Less common than Sumatriptan 100 mg
Specific Tx – Triptans l 3 main mechanisms of action l l l Cranial vasoconstriction Peripheral trigeminal inhibition Inhibition of transmission through second order neurons of the trigeminocervical complex
Oral triptans in acute migraine treatment: a meta-analysis of 53 trials Michel D Ferrari et al. Lancet 2001; 358: 1668– 75 l l l Collected raw patient data of 53 double-blind, randomised, controlled, clinical trials of oral triptans in migraine (12 unpublished) Summarized estimates across studies for important efficacy and tolerability parameters Rizatriptan, Eletriptan, and Almotriptan provide the highest likelihood of consistent success

Oral triptans in acute migraine treatment: a meta-analysis of 53 trials l l l l Rizatriptan 10 mg (Maxalt) l Consistent and rapid freedom from pain is desired Eletriptan 80 mg (Relpax) l High efficacy and low recurrence, lower tolerability Almotriptan 12. 5 mg (Axert, Almogran) l High tolerability and good efficacy Sumatriptan 50 mg and 100 mg (Imitrex, Imigran) l Good efficacy and tolerability l Longest clinical experience Zolmitriptan 2. 5 mg and 5 mg (Zomig, Asco. Top, Zomigon) l No specific advantages nor flaws Naratriptan 2. 5 mg (Amerge, Naramig) l Good tolerability l Slower onset of improvement (useful in mild or moderate migraine) Frovatriptan (Frova) l Lack of data

Triptans l l l Should be used if >10 days 50% disability in 3 mths Administered as early as possible after onset of h/a Safe medications in patients without cardiovascular disease or major vascular RF No clinically important differences in coronary vasoconstriction effects No triptan is demonstrably safer than the others Choice dependent on patient characteristics and preferences Individual responses to a triptan cannot be predicted
Specifc Tx – Ergots l Vasoconstriction by stimulating l l Adrenergic receptors 5 -HT receptors Norepinephrine receptors (venoconstrictors) Two main Ergots l Ergotamine (ET), more potent vasoconstrictor l l Superior to placebo, inferior to PO Sumatriptan 100 mg Dihydroergotamine (DHE) l Also inferior to Sumatriptan, but recurrence rate lower
Ergotamine l Oral bioavailability is <1% l l l Oral ET is appropriate for slowly evolving migraine without early-onset nausea l l l 1 st pass hepatic metabolism Rectal suppository: better plasma level, less nausea One 1 -mg tablet at the start of an attack Maximum total dose of 6 mg per attack Maximum 2 days per week with an interval of at least 4 days l Avoiding habituation, rebound, and daily headache
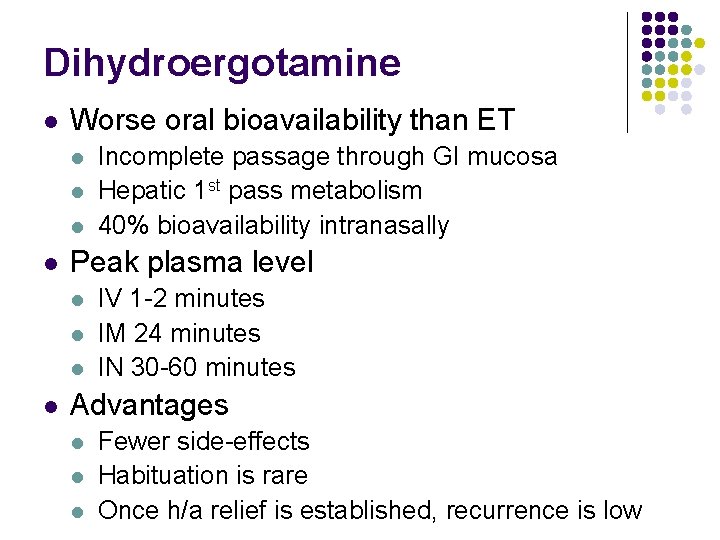
Dihydroergotamine l Worse oral bioavailability than ET l l Peak plasma level l l Incomplete passage through GI mucosa Hepatic 1 st pass metabolism 40% bioavailability intranasally IV 1 -2 minutes IM 24 minutes IN 30 -60 minutes Advantages l l l Fewer side-effects Habituation is rare Once h/a relief is established, recurrence is low
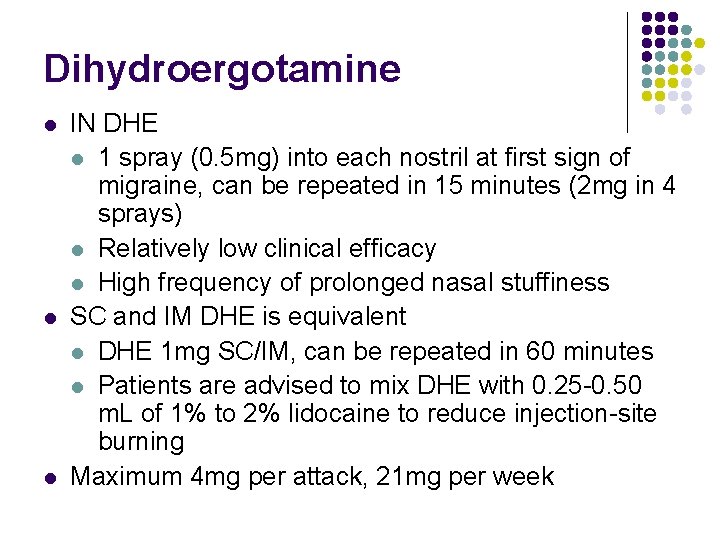
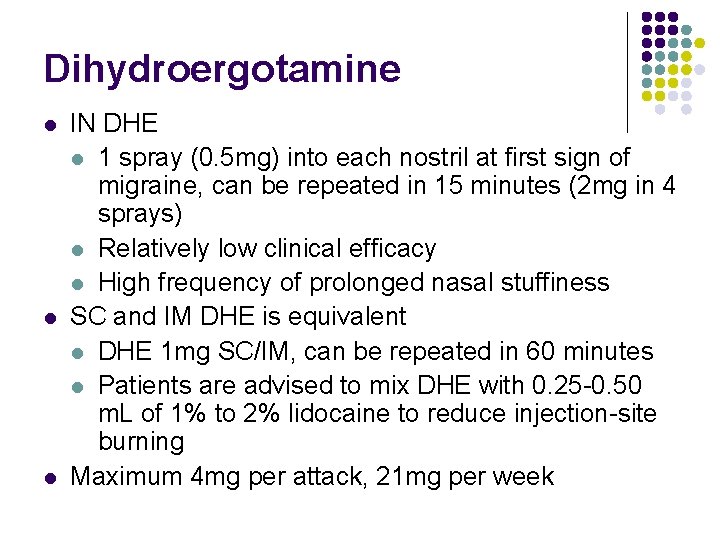
Dihydroergotamine l l l IN DHE l 1 spray (0. 5 mg) into each nostril at first sign of migraine, can be repeated in 15 minutes (2 mg in 4 sprays) l Relatively low clinical efficacy l High frequency of prolonged nasal stuffiness SC and IM DHE is equivalent l DHE 1 mg SC/IM, can be repeated in 60 minutes l Patients are advised to mix DHE with 0. 25 -0. 50 m. L of 1% to 2% lidocaine to reduce injection-site burning Maximum 4 mg per attack, 21 mg per week
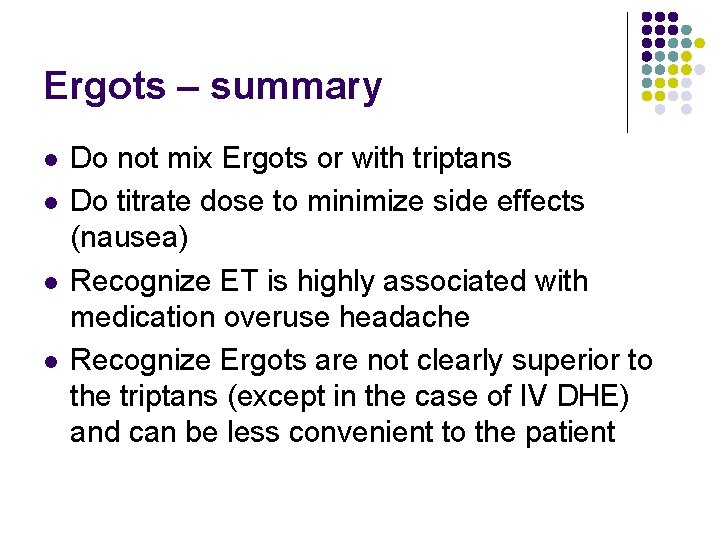
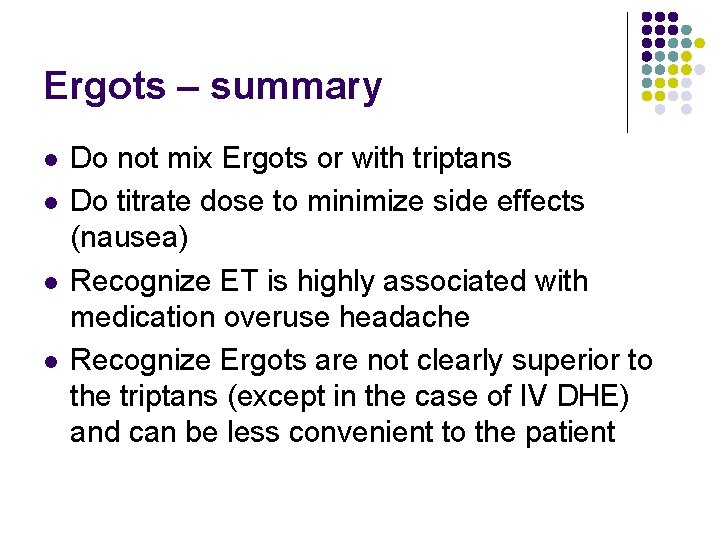
Ergots – summary l l Do not mix Ergots or with triptans Do titrate dose to minimize side effects (nausea) Recognize ET is highly associated with medication overuse headache Recognize Ergots are not clearly superior to the triptans (except in the case of IV DHE) and can be less convenient to the patient
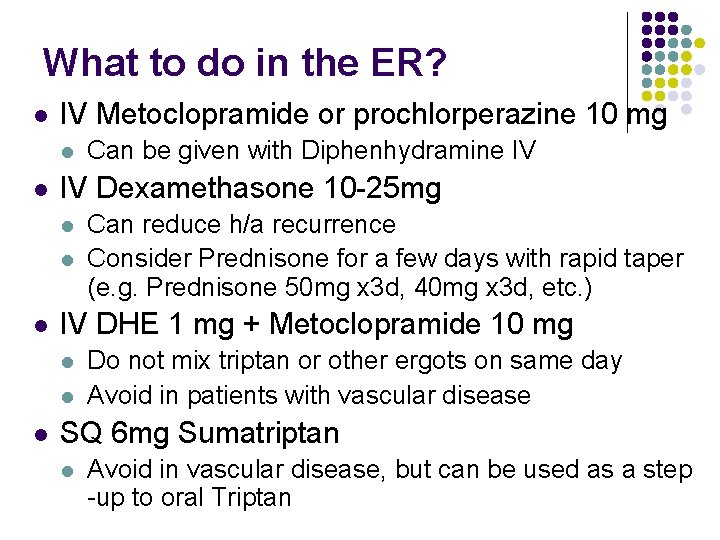
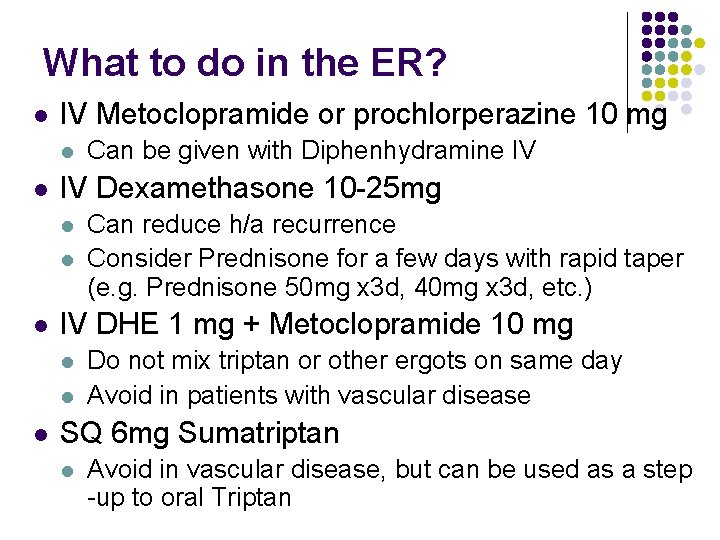
What to do in the ER? l IV Metoclopramide or prochlorperazine 10 mg l l IV Dexamethasone 10 -25 mg l l l Can reduce h/a recurrence Consider Prednisone for a few days with rapid taper (e. g. Prednisone 50 mg x 3 d, 40 mg x 3 d, etc. ) IV DHE 1 mg + Metoclopramide 10 mg l l l Can be given with Diphenhydramine IV Do not mix triptan or other ergots on same day Avoid in patients with vascular disease SQ 6 mg Sumatriptan l Avoid in vascular disease, but can be used as a step -up to oral Triptan
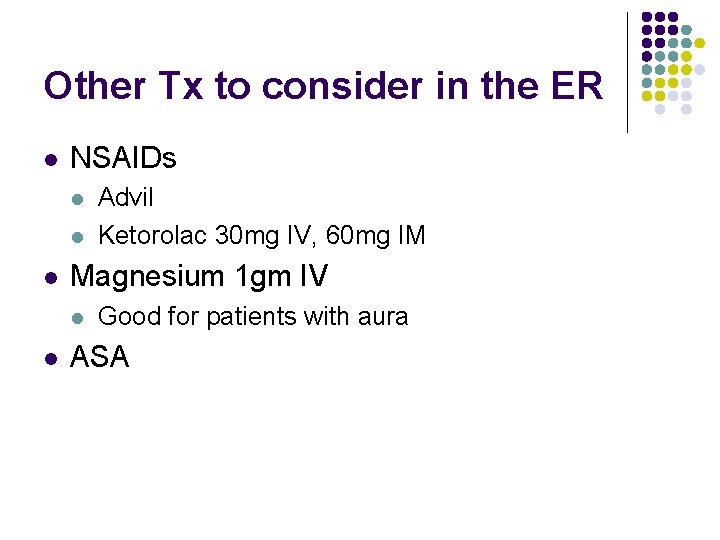
Other Tx to consider in the ER l NSAIDs l l l Magnesium 1 gm IV l l Advil Ketorolac 30 mg IV, 60 mg IM Good for patients with aura ASA
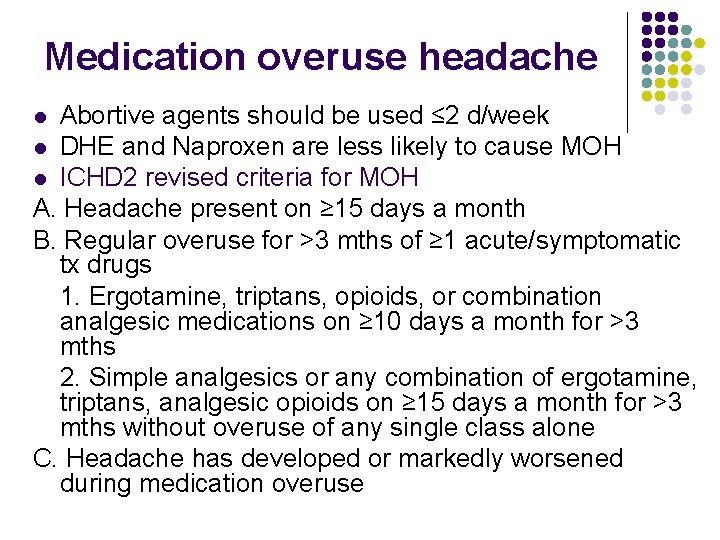
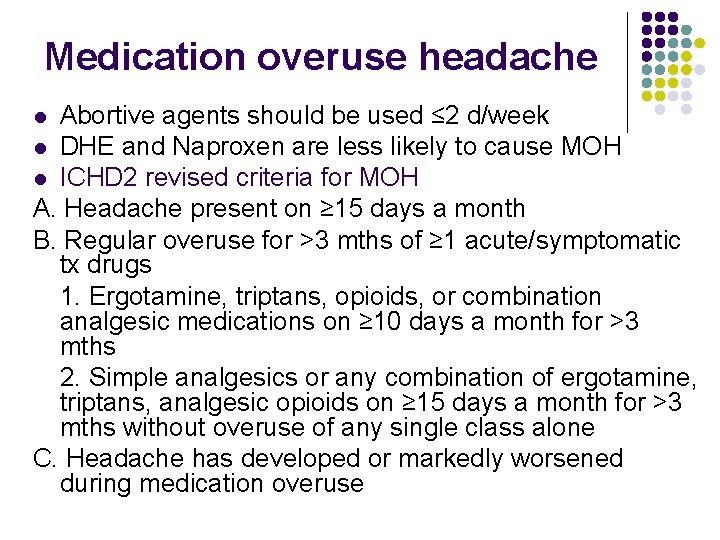
Medication overuse headache Abortive agents should be used ≤ 2 d/week l DHE and Naproxen are less likely to cause MOH l ICHD 2 revised criteria for MOH A. Headache present on ≥ 15 days a month B. Regular overuse for >3 mths of ≥ 1 acute/symptomatic tx drugs 1. Ergotamine, triptans, opioids, or combination analgesic medications on ≥ 10 days a month for >3 mths 2. Simple analgesics or any combination of ergotamine, triptans, analgesic opioids on ≥ 15 days a month for >3 mths without overuse of any single class alone C. Headache has developed or markedly worsened during medication overuse l
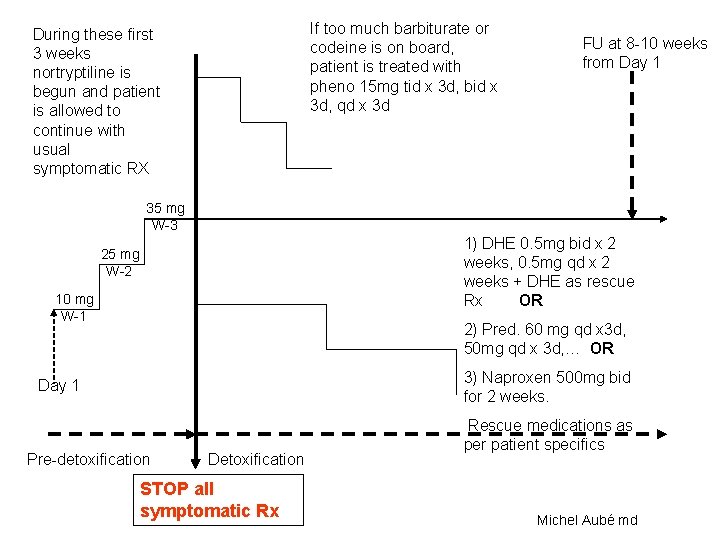
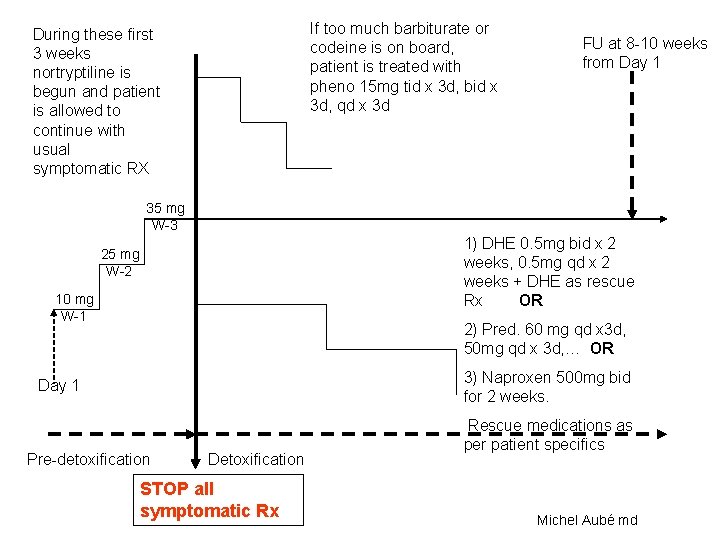
If too much barbiturate or codeine is on board, patient is treated with pheno 15 mg tid x 3 d, bid x 3 d, qd x 3 d During these first 3 weeks nortryptiline is begun and patient is allowed to continue with usual symptomatic RX FU at 8 -10 weeks from Day 1 35 mg W-3 1) DHE 0. 5 mg bid x 2 weeks, 0. 5 mg qd x 2 weeks + DHE as rescue Rx OR 25 mg W-2 10 mg W-1 2) Pred. 60 mg qd x 3 d, 50 mg qd x 3 d, … OR 3) Naproxen 500 mg bid for 2 weeks. Day 1 Pre-detoxification Detoxification STOP all symptomatic Rx Rescue medications as per patient specifics Michel Aubé md
Thank you for your attention!
 Red flag sign headache
Red flag sign headache Spina bifida occulta
Spina bifida occulta Post dural puncture headache
Post dural puncture headache Headache
Headache Headache
Headache Headache nursing management
Headache nursing management Vayu mudra image
Vayu mudra image Headache
Headache Improved
Improved European headache federation
European headache federation Anish bahra
Anish bahra Severe anxiety
Severe anxiety Headache red flags
Headache red flags Rasmussen syndrome
Rasmussen syndrome ı have a headache song
ı have a headache song Postdrome symptoms
Postdrome symptoms Pediatric headache red flags
Pediatric headache red flags Baep
Baep Postical
Postical Right side headache
Right side headache Dr alexander mauskop
Dr alexander mauskop Headache chart
Headache chart Medical leave in infosys
Medical leave in infosys Catawba indian nation bingo
Catawba indian nation bingo Sergei korolev
Sergei korolev Sources nso frenchhowell neill mit technology...
Sources nso frenchhowell neill mit technology... 2001 july 15
2001 july 15 Why are leaf yeasts more plentiful in july
Why are leaf yeasts more plentiful in july June 22 to july 22
June 22 to july 22 July 4 sermon
July 4 sermon Poppies in july imagery
Poppies in july imagery July 1-4 1863
July 1-4 1863 March april june july august
March april june july august Slidetodoc.com
Slidetodoc.com 2003 july 17
2003 july 17 What is the significance of july 4 1776 brainpop
What is the significance of july 4 1776 brainpop July 26 1953
July 26 1953 July 12 1776
July 12 1776 June too soon july stand by
June too soon july stand by Gdje se rodio nikola tesla
Gdje se rodio nikola tesla Tender definition
Tender definition July 14 1789
July 14 1789 Monday 13th july
Monday 13th july Sylvia plath poppies in july
Sylvia plath poppies in july Harris burdick pictures captain tory
Harris burdick pictures captain tory July 16 1776
July 16 1776 July 2 1937 amelia earhart
July 2 1937 amelia earhart Sensory language definition
Sensory language definition Ctdssmap payment schedule july 2021
Ctdssmap payment schedule july 2021 July 30 2009 nasa
July 30 2009 nasa Criciúma ec
Criciúma ec