Neurology Case Presentation Scott M Shorten MD PGY3



- Slides: 26
Neurology Case Presentation Scott M. Shorten, MD PGY-3
37 y. o. Right-handed Caucasian man CC: right facial droop, right arm and leg tingling and weakness
HPI • recurrent drooping of the right face • started 1. 5 yrs ago without clear precipitant • multiple times per day and while asleep, no warning, no trigger • Average 30 minutes (5 min-2 hours), with complete recovery between • Sometimes associated hand/arm numbness, no other consistent symptoms • This episode concerning due to ‘stabbing’ mid-frontal headache with photo/phonophobia, left arm and leg weakness, and lasted over 2 hours. Onset while out in the heat gardening. • ROS: fatigue, chest discomfort, neck pain
PMHx/Surg. Hx • • COPD Hyperlipidemia Depression Septic thrombophlebitis, R Cephalic vein • Appendectomy • Hemorrhoidectomy
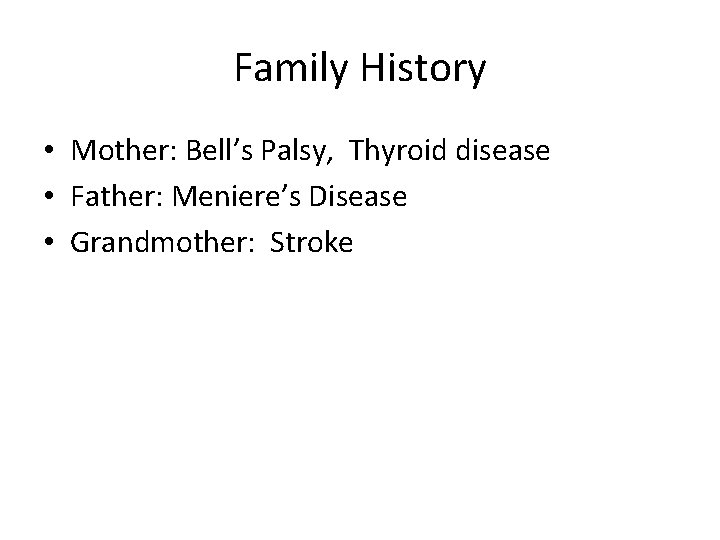
Family History • Mother: Bell’s Palsy, Thyroid disease • Father: Meniere’s Disease • Grandmother: Stroke
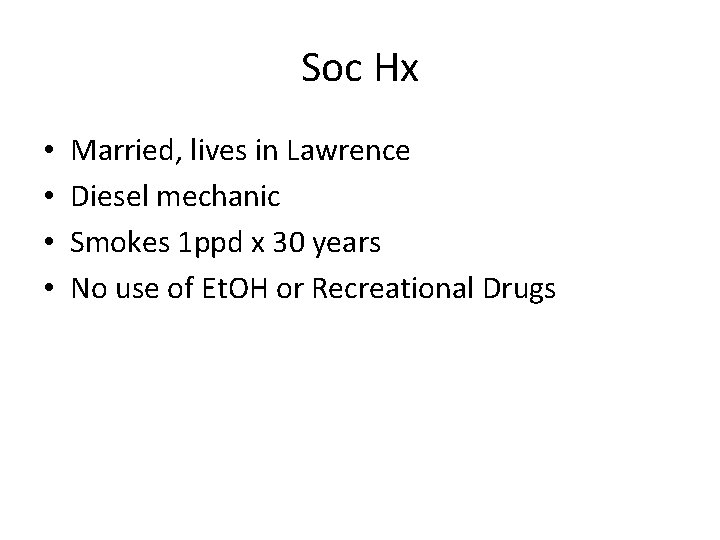
Soc Hx • • Married, lives in Lawrence Diesel mechanic Smokes 1 ppd x 30 years No use of Et. OH or Recreational Drugs
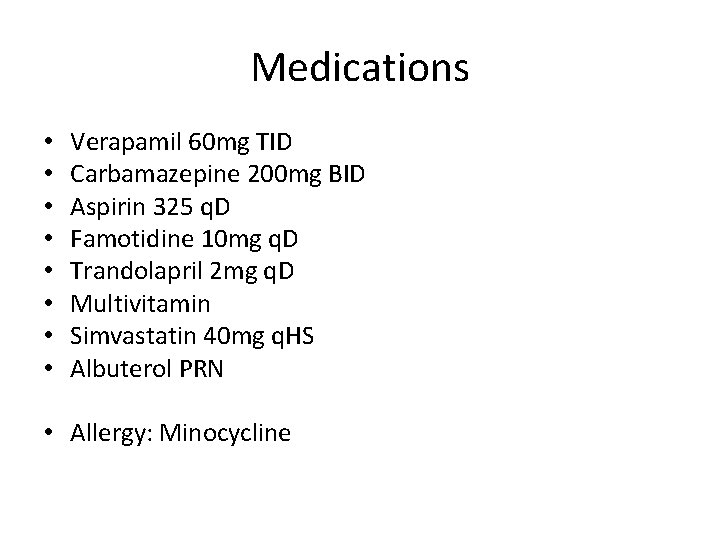
Medications • • Verapamil 60 mg TID Carbamazepine 200 mg BID Aspirin 325 q. D Famotidine 10 mg q. D Trandolapril 2 mg q. D Multivitamin Simvastatin 40 mg q. HS Albuterol PRN • Allergy: Minocycline
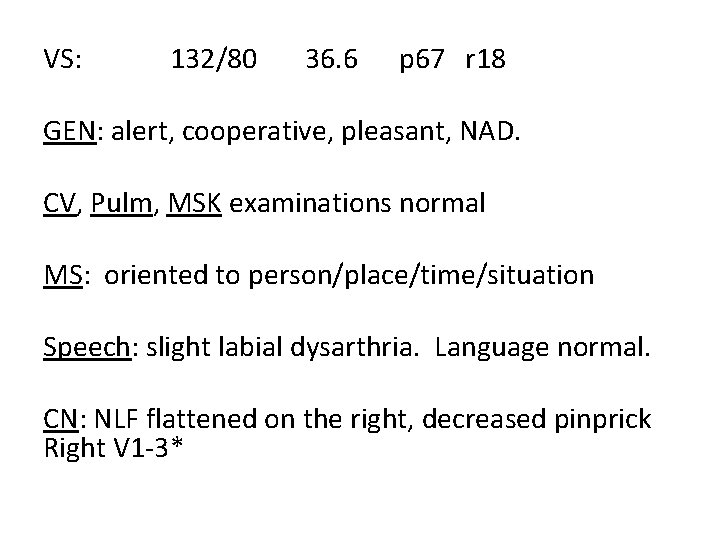
VS: 132/80 36. 6 p 67 r 18 GEN: alert, cooperative, pleasant, NAD. CV, Pulm, MSK examinations normal MS: oriented to person/place/time/situation Speech: slight labial dysarthria. Language normal. CN: NLF flattened on the right, decreased pinprick Right V 1 -3*
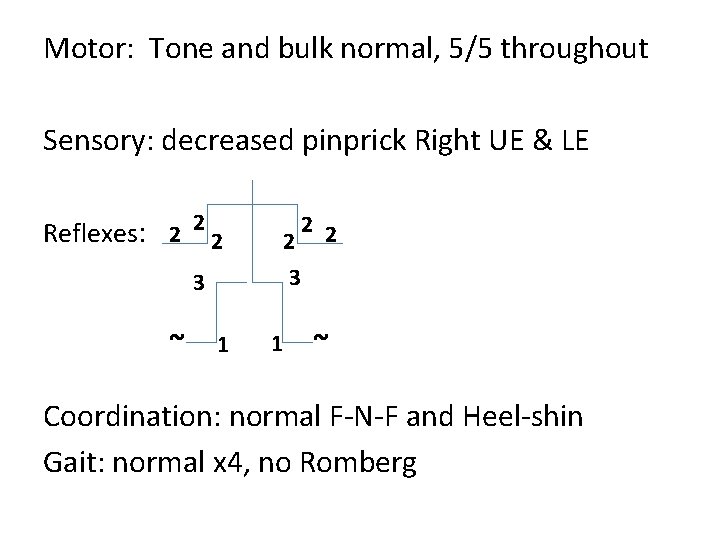
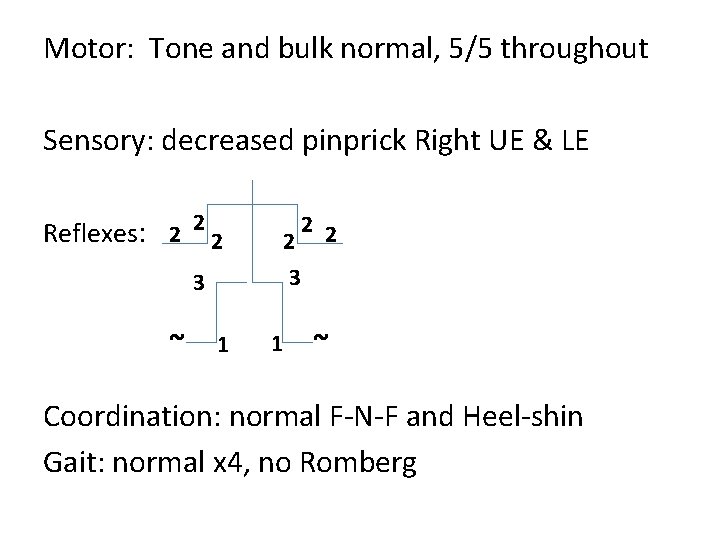
Motor: Tone and bulk normal, 5/5 throughout Sensory: decreased pinprick Right UE & LE Reflexes: 2 2 2 3 3 ~ 1 1 ~ Coordination: normal F-N-F and Heel-shin Gait: normal x 4, no Romberg

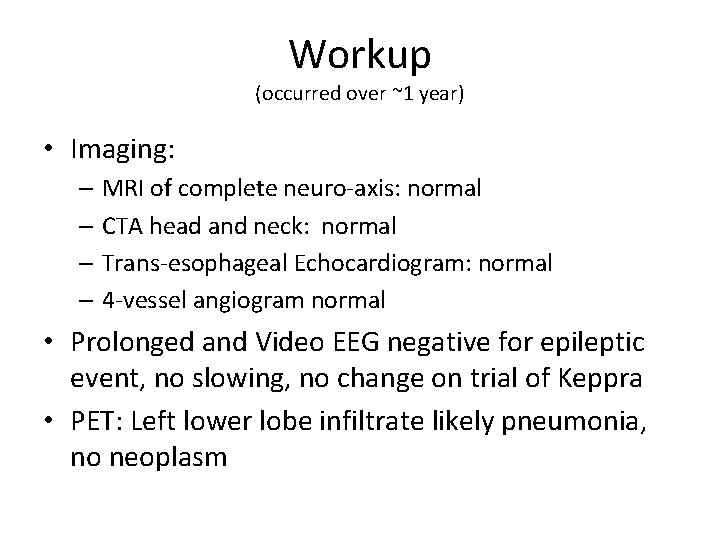
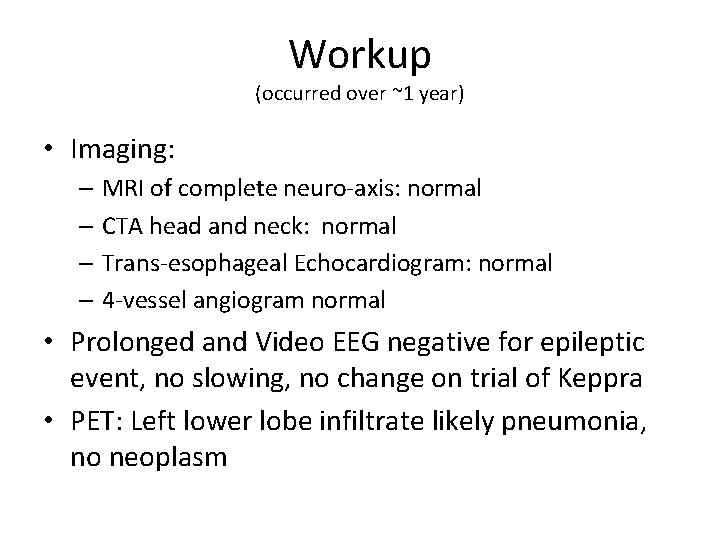
Workup (occurred over ~1 year) • Imaging: – MRI of complete neuro-axis: normal – CTA head and neck: normal – Trans-esophageal Echocardiogram: normal – 4 -vessel angiogram normal • Prolonged and Video EEG negative for epileptic event, no slowing, no change on trial of Keppra • PET: Left lower lobe infiltrate likely pneumonia, no neoplasm

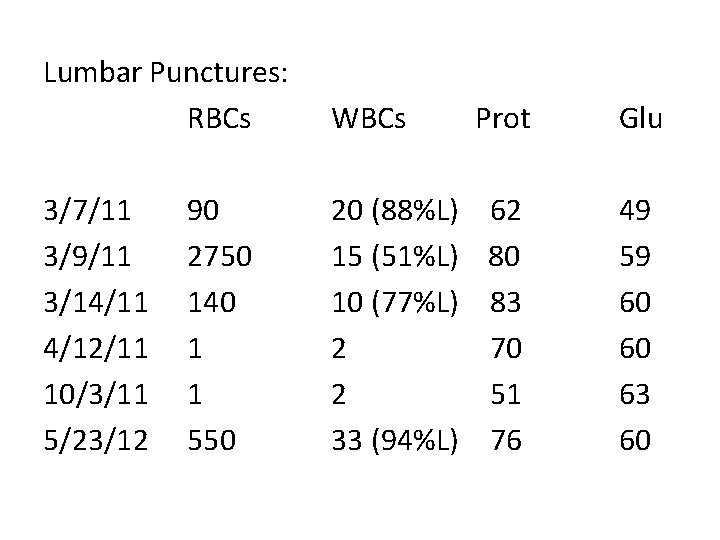
Lumbar Punctures: RBCs WBCs 3/7/11 3/9/11 3/14/11 4/12/11 10/3/11 5/23/12 20 (88%L) 15 (51%L) 10 (77%L) 2 2 33 (94%L) 90 2750 140 1 1 550 Prot Glu 62 80 83 70 51 76 49 59 60 60 63 60
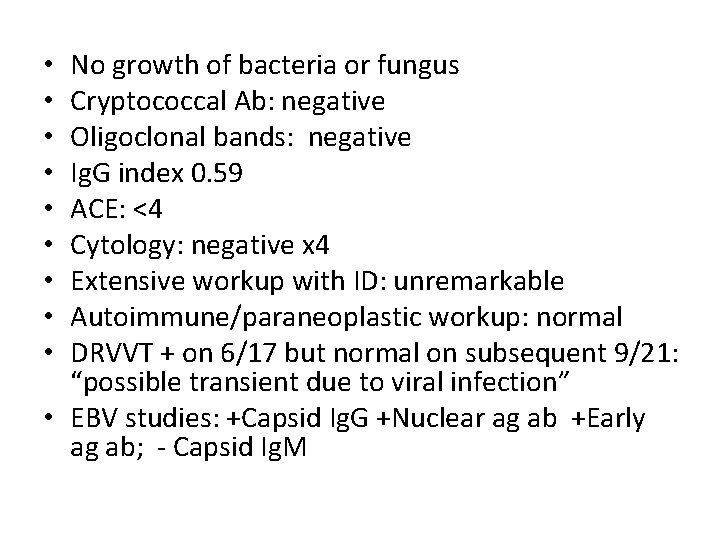
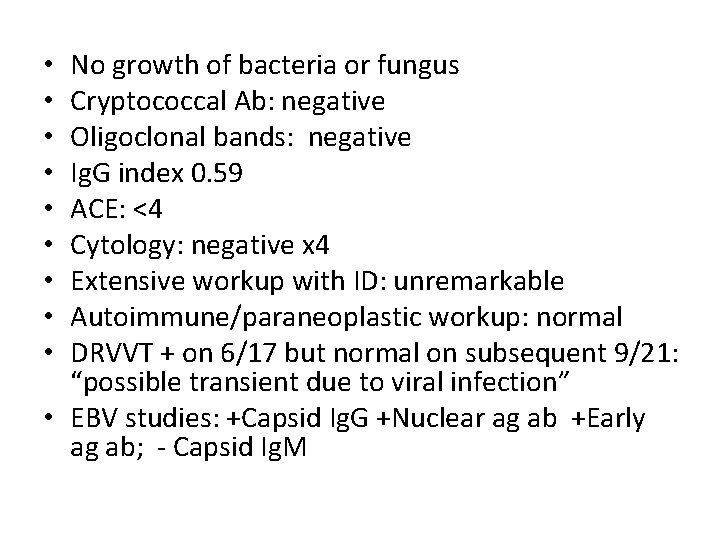
No growth of bacteria or fungus Cryptococcal Ab: negative Oligoclonal bands: negative Ig. G index 0. 59 ACE: <4 Cytology: negative x 4 Extensive workup with ID: unremarkable Autoimmune/paraneoplastic workup: normal DRVVT + on 6/17 but normal on subsequent 9/21: “possible transient due to viral infection” • EBV studies: +Capsid Ig. G +Nuclear ag ab +Early ag ab; - Capsid Ig. M • • •

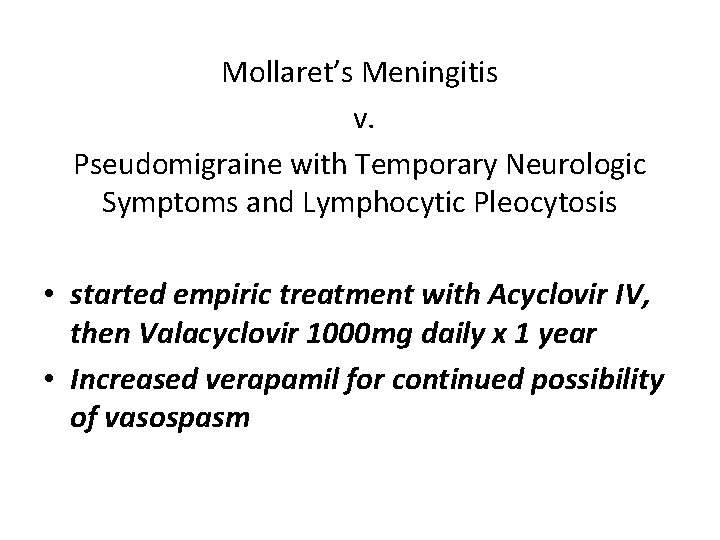
Mollaret’s Meningitis v. Pseudomigraine with Temporary Neurologic Symptoms and Lymphocytic Pleocytosis • started empiric treatment with Acyclovir IV, then Valacyclovir 1000 mg daily x 1 year • Increased verapamil for continued possibility of vasospasm
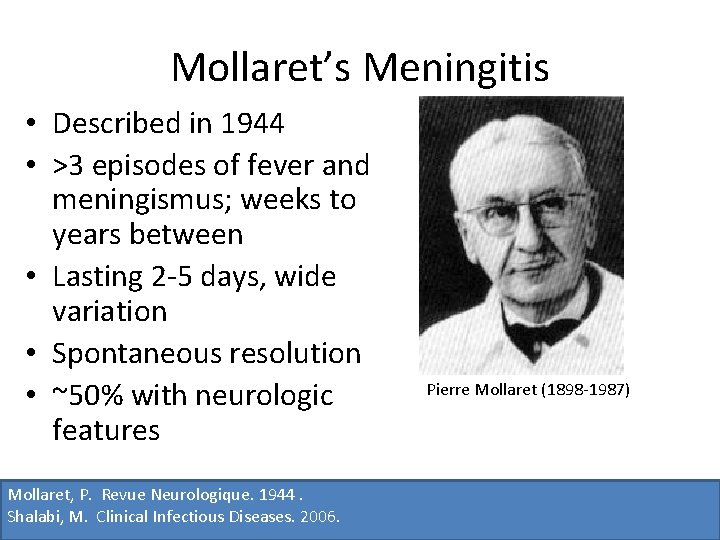
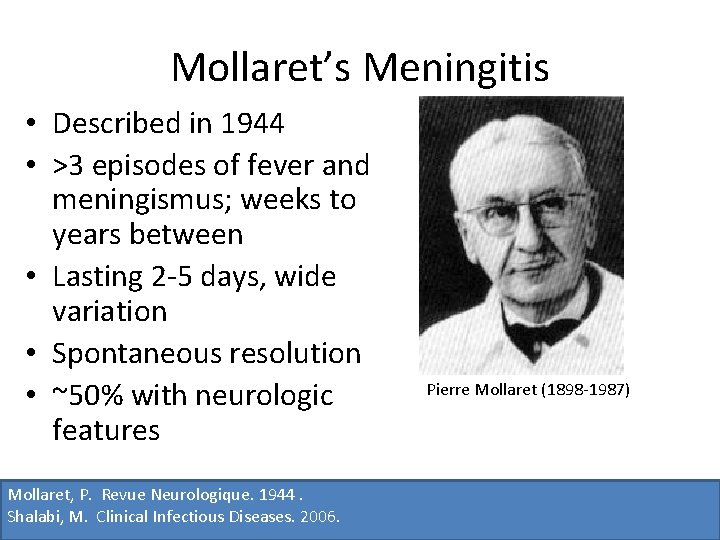
Mollaret’s Meningitis • Described in 1944 • >3 episodes of fever and meningismus; weeks to years between • Lasting 2 -5 days, wide variation • Spontaneous resolution • ~50% with neurologic features Mollaret, P. Revue Neurologique. 1944. Shalabi, M. Clinical Infectious Diseases. 2006. Pierre Mollaret (1898 -1987)
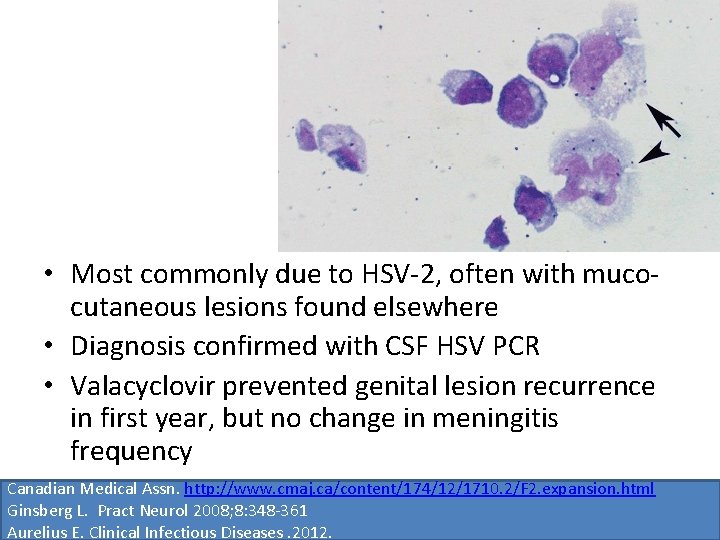
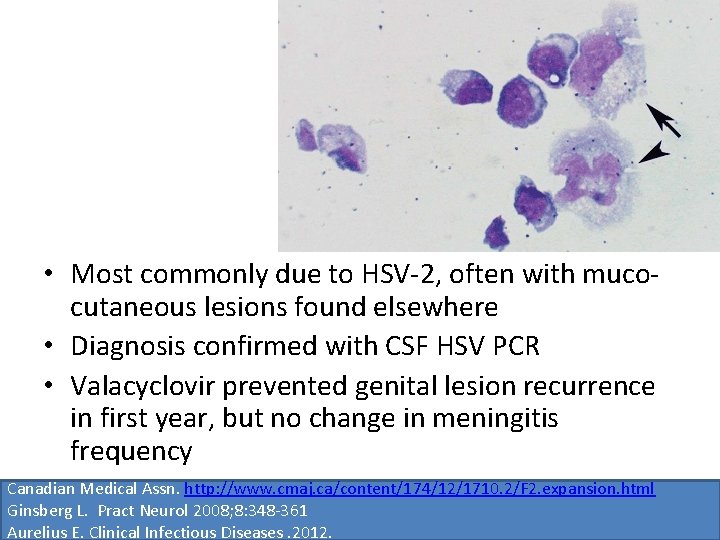
• Most commonly due to HSV-2, often with mucocutaneous lesions found elsewhere • Diagnosis confirmed with CSF HSV PCR • Valacyclovir prevented genital lesion recurrence in first year, but no change in meningitis frequency Canadian Medical Assn. http: //www. cmaj. ca/content/174/12/1710. 2/F 2. expansion. html Ginsberg L. Pract Neurol 2008; 8: 348 -361 Aurelius E. Clinical Infectious Diseases. 2012.
Pseudomigraine with Temporary Neurologic Symptoms and Lymphocytic Pleocytosis = Migrainous Syndrome with CSF Pleocytosis = Syndrome of Transient Headache and Neurologic Deficits with CSF Pleocytosis (Ha. NDL)
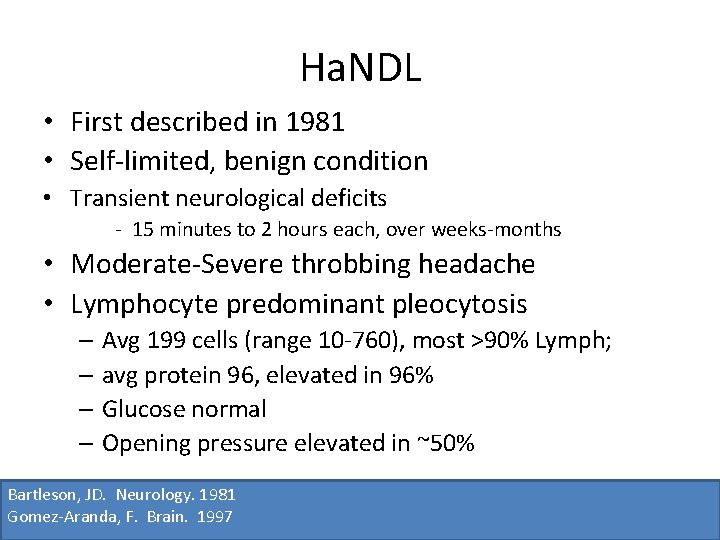
Ha. NDL • First described in 1981 • Self-limited, benign condition • Transient neurological deficits - 15 minutes to 2 hours each, over weeks-months • Moderate-Severe throbbing headache • Lymphocyte predominant pleocytosis – Avg 199 cells (range 10 -760), most >90% Lymph; – avg protein 96, elevated in 96% – Glucose normal – Opening pressure elevated in ~50% Bartleson, JD. Neurology. 1981 Gomez-Aranda, F. Brain. 1997
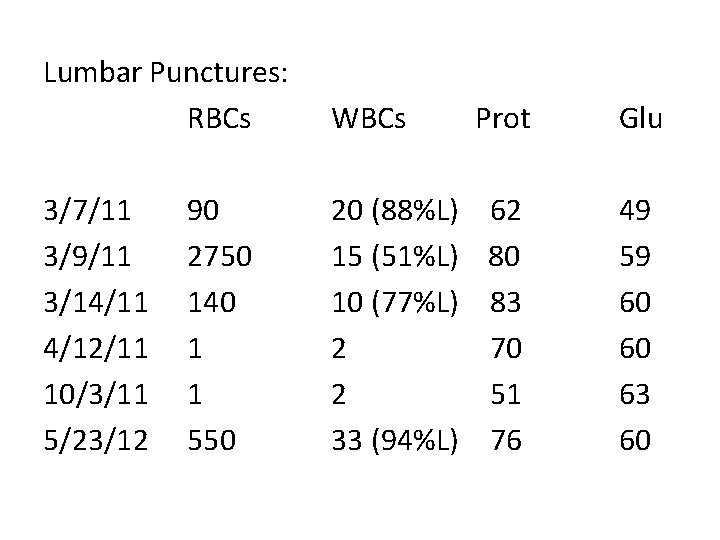
Lumbar Punctures: RBCs WBCs 3/7/11 3/9/11 3/14/11 4/12/11 10/3/11 5/23/12 20 (88%L) 15 (51%L) 10 (77%L) 2 2 33 (94%L) 90 2750 140 1 1 550 Prot Glu 62 80 83 70 51 76 49 59 60 60 63 60
• Usually in 30 s-40 s (range 7 -52 yrs) • 25 -40% had preceding cough/rhinitis/fatigue/diarrhea • No consistent gender predominance
Other Studies • Neuroimaging is usually normal – Leptomeningeal enhancement – Hypoperfusion on CT perfusion • EEG generally shows slowing in the corresponding region
Ha. NDL Etiology • Inflammatory/Infectious? – Few reports; Echovirus, HHV-6. • Migrainous? – SPECT imaging with decreased blood flow at sites corresponding to neurologic deficit – spreading cortical depression phenomenon • Infectious, triggering cortical depression? Castels-van Daele, M. Lancet. 1981. Emond, H. Cephalalgia. 2009. Caminero, AB. Headache. 1997
Diagnosis / Tx • Must first exclude more sinister causes • CSF with >15 cells/m. L of lymphocyte predominance • Episodes of moderate-severe headache occurring with or shortly following symptoms • Episodes recurring within 3 months • Symptomatic treatment only, if needed The International Classification of Headache Disorders: Cephalalgia. 2004
Our Patient • frequency of attacks 3 -4 per day (from up to 20). • Mostly affecting only his right face • Usually associated with moderate headache • Happy with improvement
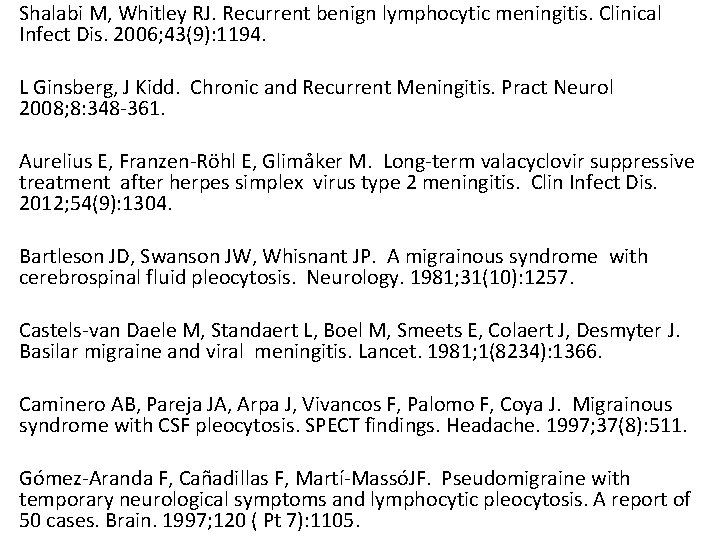
Shalabi M, Whitley RJ. Recurrent benign lymphocytic meningitis. Clinical Infect Dis. 2006; 43(9): 1194. L Ginsberg, J Kidd. Chronic and Recurrent Meningitis. Pract Neurol 2008; 8: 348 -361. Aurelius E, Franzen-Röhl E, Glimåker M. Long-term valacyclovir suppressive treatment after herpes simplex virus type 2 meningitis. Clin Infect Dis. 2012; 54(9): 1304. Bartleson JD, Swanson JW, Whisnant JP. A migrainous syndrome with cerebrospinal fluid pleocytosis. Neurology. 1981; 31(10): 1257. Castels-van Daele M, Standaert L, Boel M, Smeets E, Colaert J, Desmyter J. Basilar migraine and viral meningitis. Lancet. 1981; 1(8234): 1366. Caminero AB, Pareja JA, Arpa J, Vivancos F, Palomo F, Coya J. Migrainous syndrome with CSF pleocytosis. SPECT findings. Headache. 1997; 37(8): 511. Gómez-Aranda F, Cañadillas F, Martí-MassóJF. Pseudomigraine with temporary neurological symptoms and lymphocytic pleocytosis. A report of 50 cases. Brain. 1997; 120 ( Pt 7): 1105.