The Optimal Timing of Stage2 Palliation after the







- Slides: 66
The Optimal Timing of Stage-2 -Palliation after the Norwood Operation: A Multi-Institutional Analysis from the CHSS Fall Work Weekend November 19, 2016 James M. Meza, MD and Jake Jaquiss, MD (Study PI), for the Optimal Timing of Stage 2 Working Group
Overview • Background, Rationale, Hypothesis • Study Population and Characteristics • Outcomes and Risk Factors • Determinants of Timing of Stage-2 -Palliation • Optimal Timing – Methods and Results • Effect of interval procedures – Methods and Results • Interpretation and Clinical Implications
Mortality during Staged Palliation • Survival through single ventricle palliation = 50 -70% • Mortality after Norwood and before Stage-2 -Palliation (S 2 P) remains high • Timing of S 2 P is physician modifiable • Effect of timing not well understood
Timing of S 2 P is a Complex Decision Earlier S 2 P • • • Reduce volume load on systemic ventricle Eliminate shunt-associated risks Normalize coronary blood flow in those with BT shunt Normalize pulmonary vascular flow and pressure Underdevelopment of pulmonary vasculature Failure of PVR to decrease Later S 2 P • Growth of infant and pulmonary vasculature • Potentially decreased resource utilization • Increased exposure to risks of Norwood-associated physiology
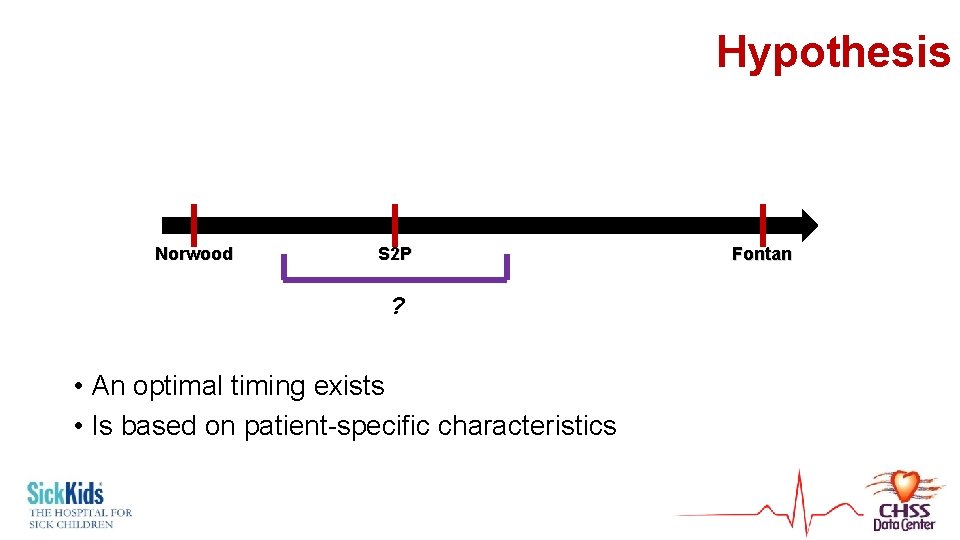
Hypothesis Norwood S 2 P ? • An optimal timing exists • Is based on patient-specific characteristics Fontan
Study Population & Characteristics
Patient Data Source = CHSS Critical Left Ventricular Outflow Tract Obstruction Registry • • Neonate ≤ age 30 days at admission to a CHSS institution 2005 onward AV & VA concordance Precludes an adequate systemic cardiac output through the aortic valve Study inclusion criteria • Initial Norwood operation
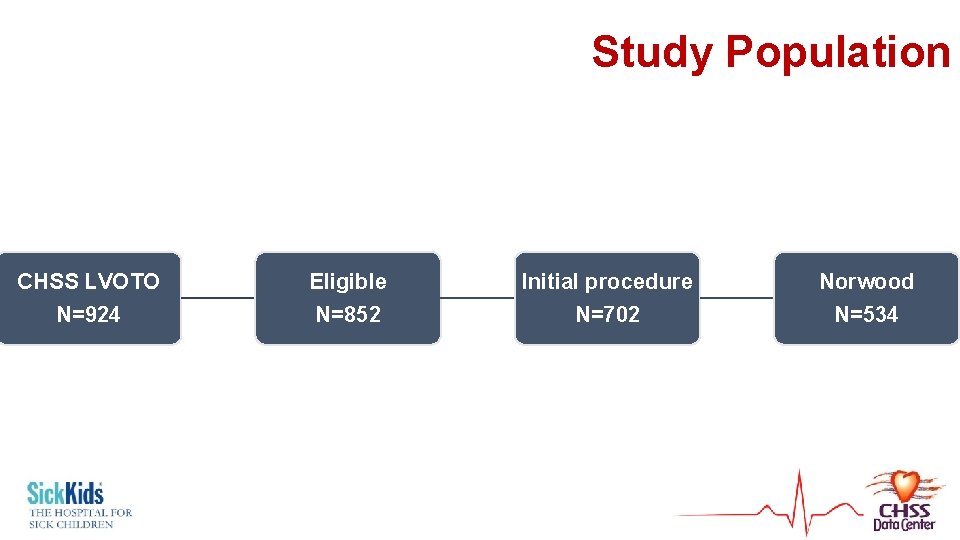
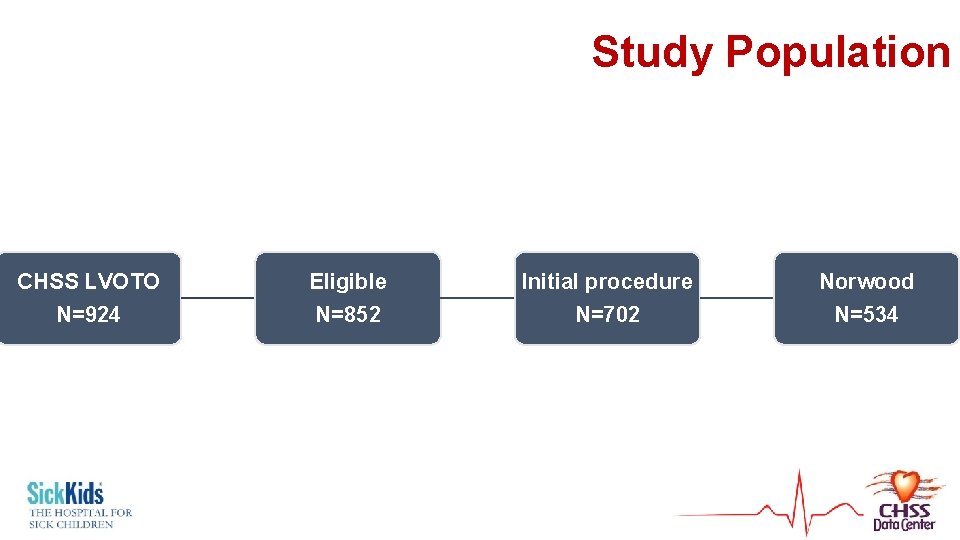
Study Population CHSS LVOTO N=924 Eligible N=852 Initial procedure N=702 Norwood N=534
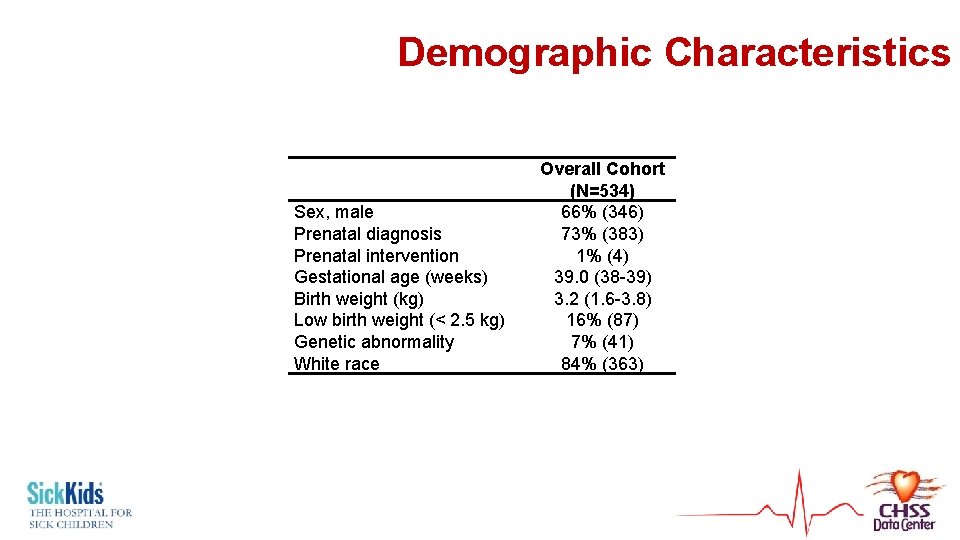
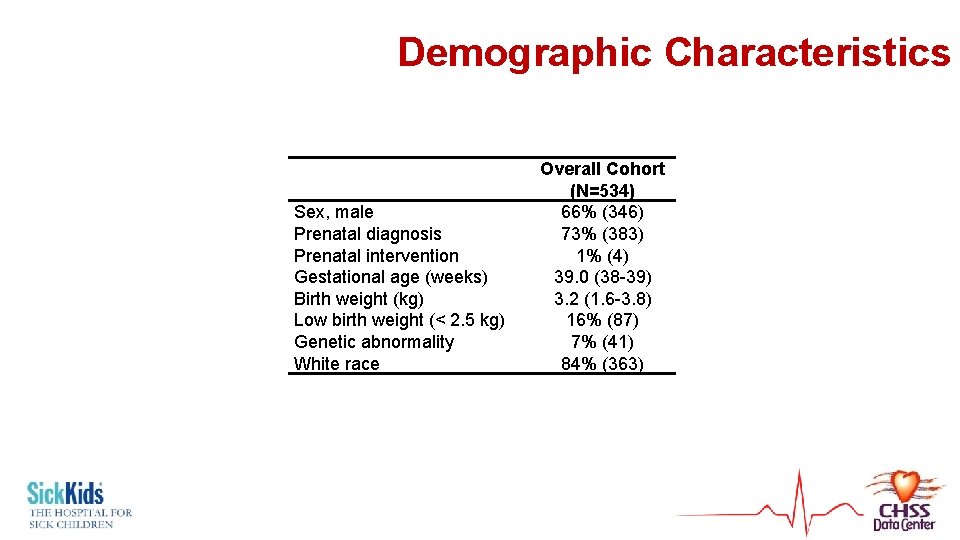
Demographic Characteristics Sex, male Prenatal diagnosis Prenatal intervention Gestational age (weeks) Birth weight (kg) Low birth weight (< 2. 5 kg) Genetic abnormality White race Overall Cohort (N=534) 66% (346) 73% (383) 1% (4) 39. 0 (38 -39) 3. 2 (1. 6 -3. 8) 16% (87) 7% (41) 84% (363)
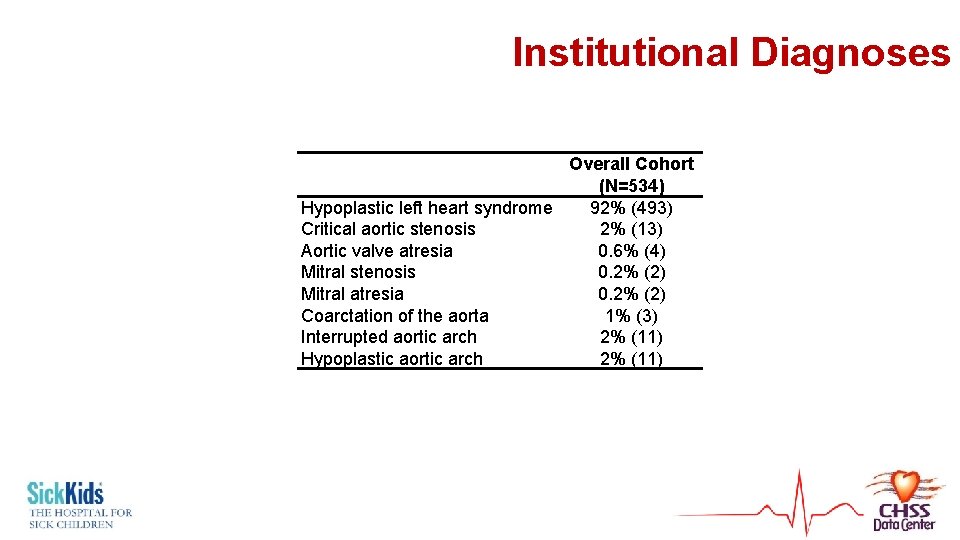
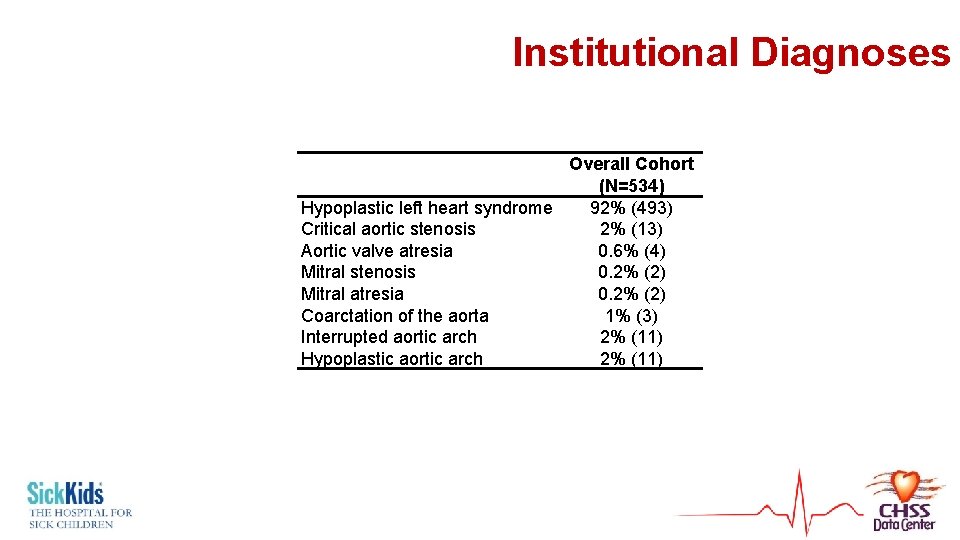
Institutional Diagnoses Overall Cohort (N=534) Hypoplastic left heart syndrome 92% (493) Critical aortic stenosis 2% (13) Aortic valve atresia 0. 6% (4) Mitral stenosis 0. 2% (2) Mitral atresia 0. 2% (2) Coarctation of the aorta 1% (3) Interrupted aortic arch 2% (11) Hypoplastic aortic arch 2% (11)
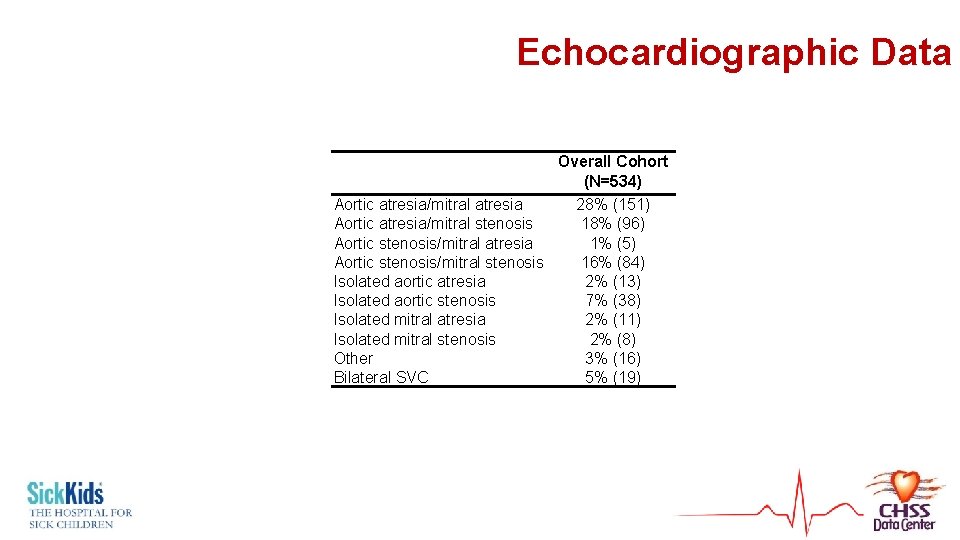
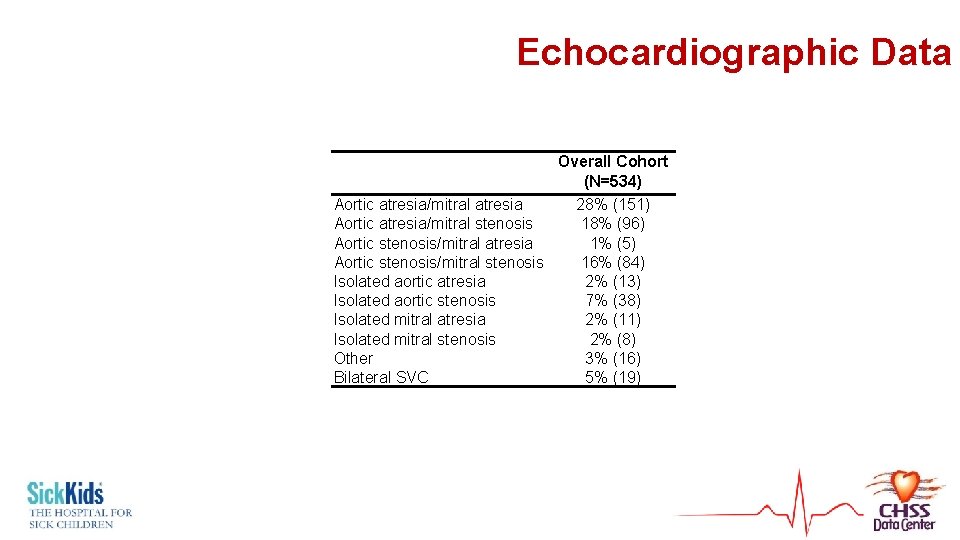
Echocardiographic Data Overall Cohort (N=534) Aortic atresia/mitral atresia 28% (151) Aortic atresia/mitral stenosis 18% (96) Aortic stenosis/mitral atresia 1% (5) Aortic stenosis/mitral stenosis 16% (84) Isolated aortic atresia 2% (13) Isolated aortic stenosis 7% (38) Isolated mitral atresia 2% (11) Isolated mitral stenosis 2% (8) Other 3% (16) Bilateral SVC 5% (19)

Outcomes and Risk Factors
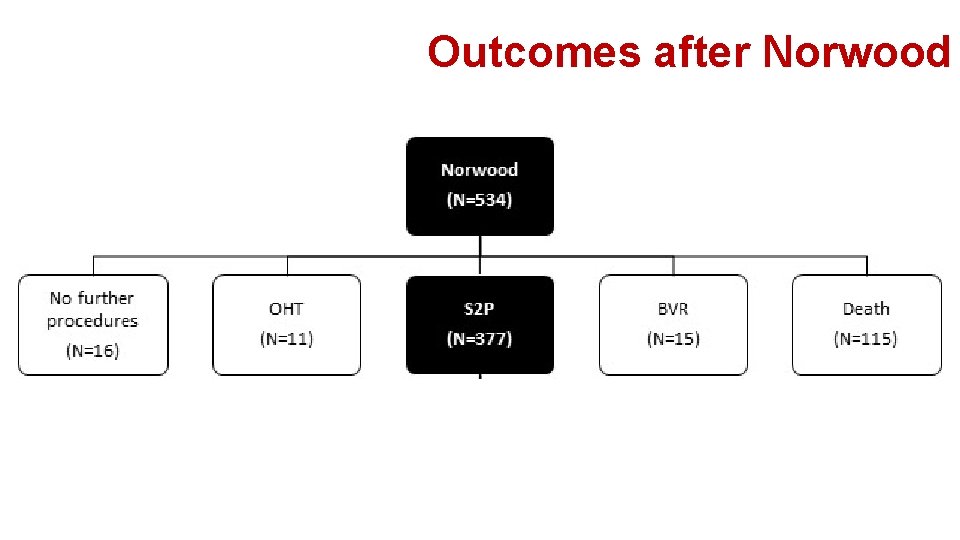
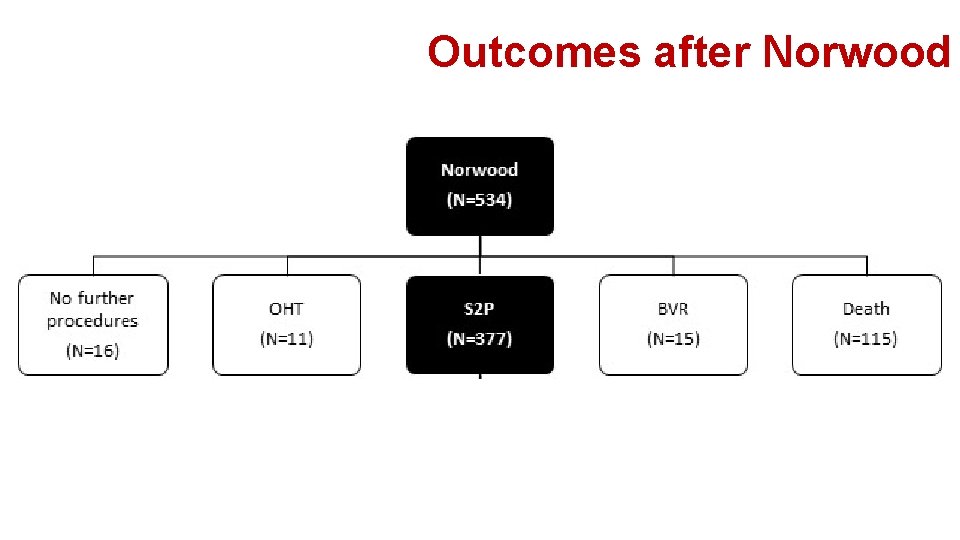
Outcomes after Norwood
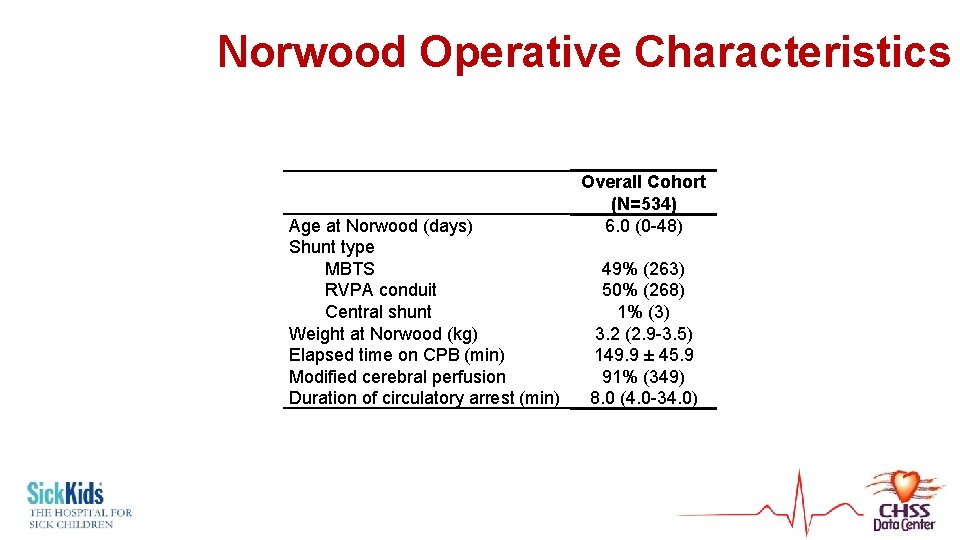
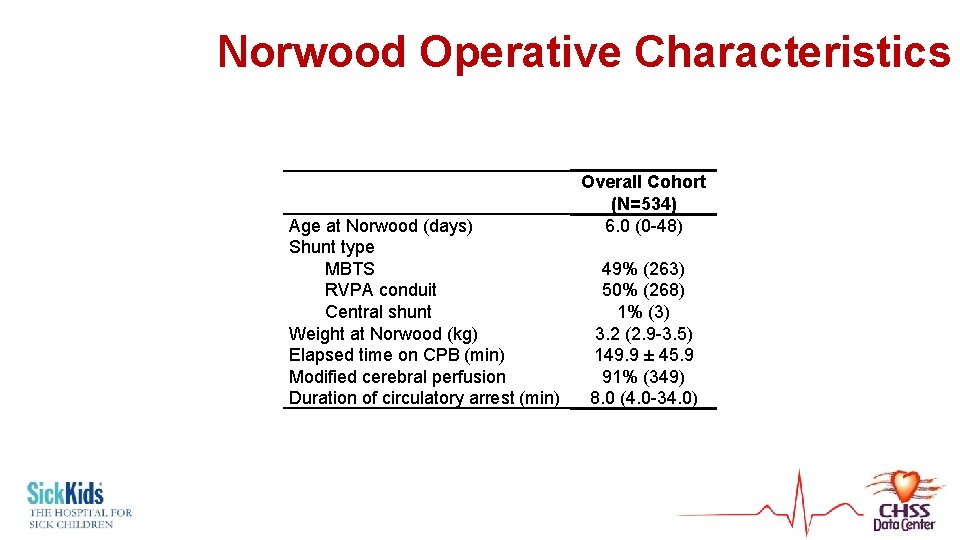
Norwood Operative Characteristics Age at Norwood (days) Shunt type MBTS RVPA conduit Central shunt Weight at Norwood (kg) Elapsed time on CPB (min) Modified cerebral perfusion Duration of circulatory arrest (min) Overall Cohort (N=534) 6. 0 (0 -48) 49% (263) 50% (268) 1% (3) 3. 2 (2. 9 -3. 5) 149. 9 ± 45. 9 91% (349) 8. 0 (4. 0 -34. 0)
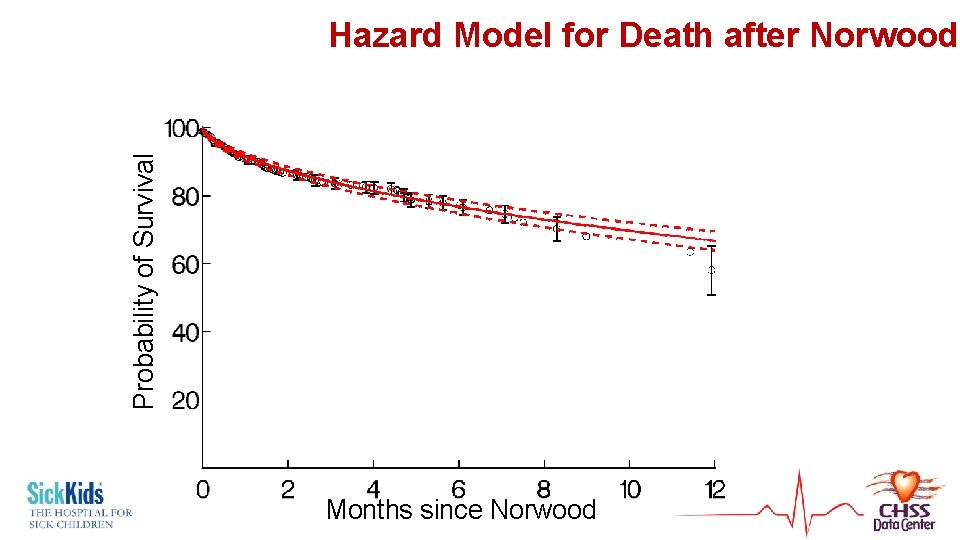
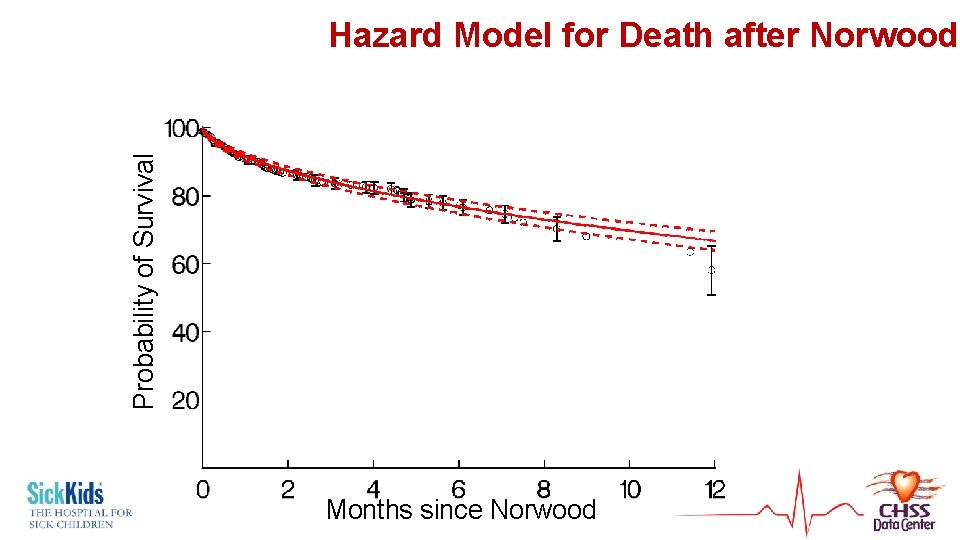
Probability of Survival Hazard Model for Death after Norwood Months since Norwood
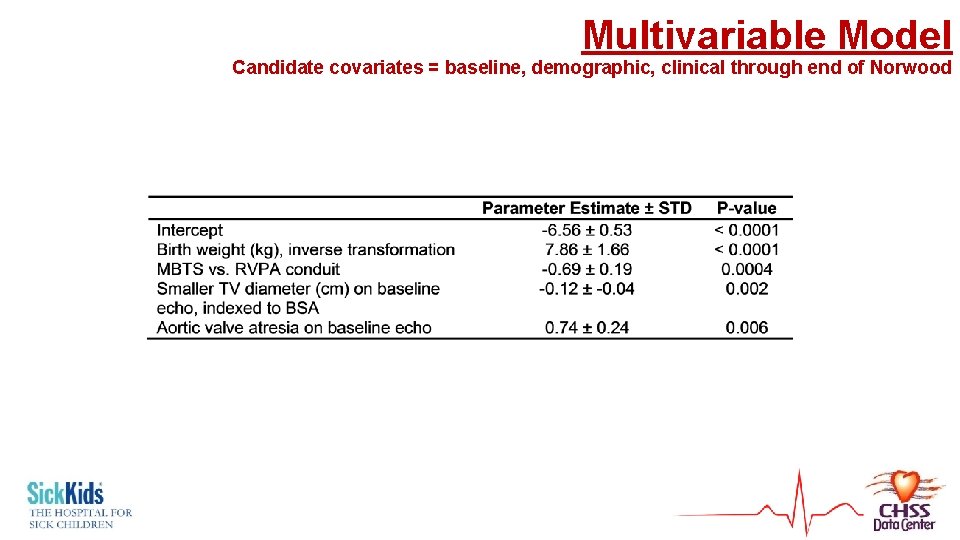
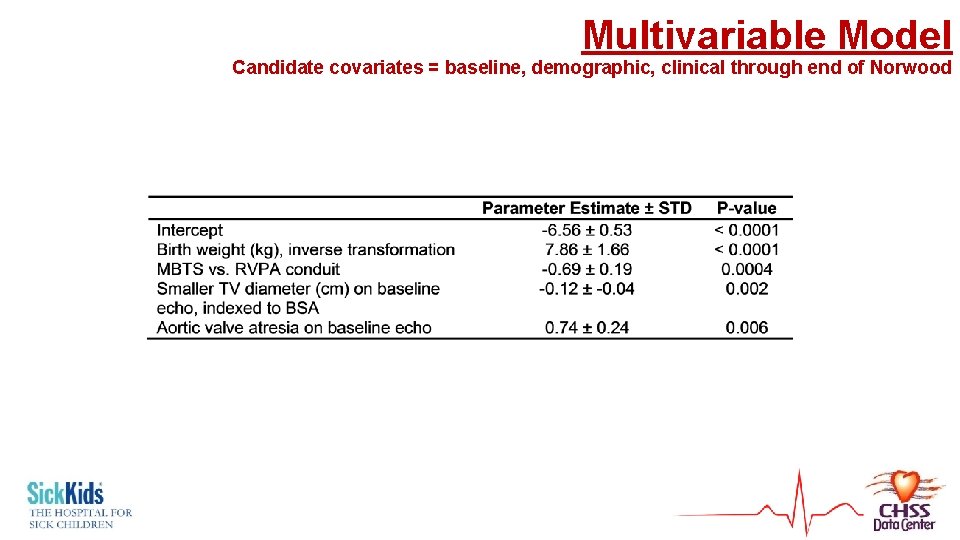
Multivariable Model Candidate covariates = baseline, demographic, clinical through end of Norwood
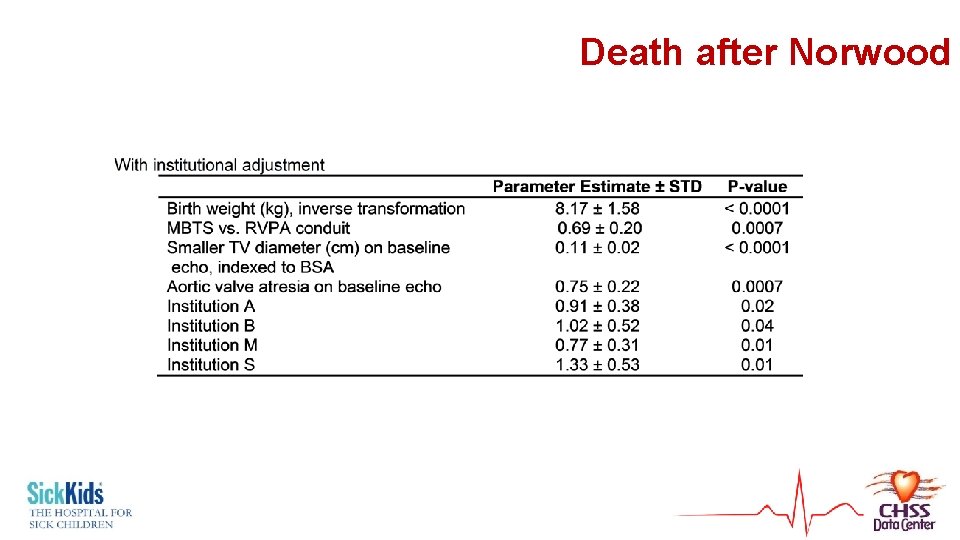
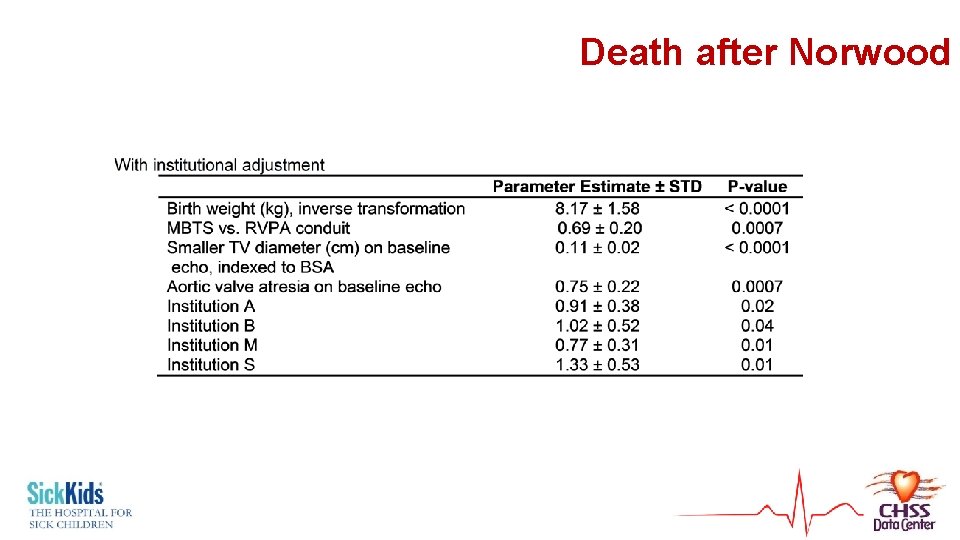
Death after Norwood
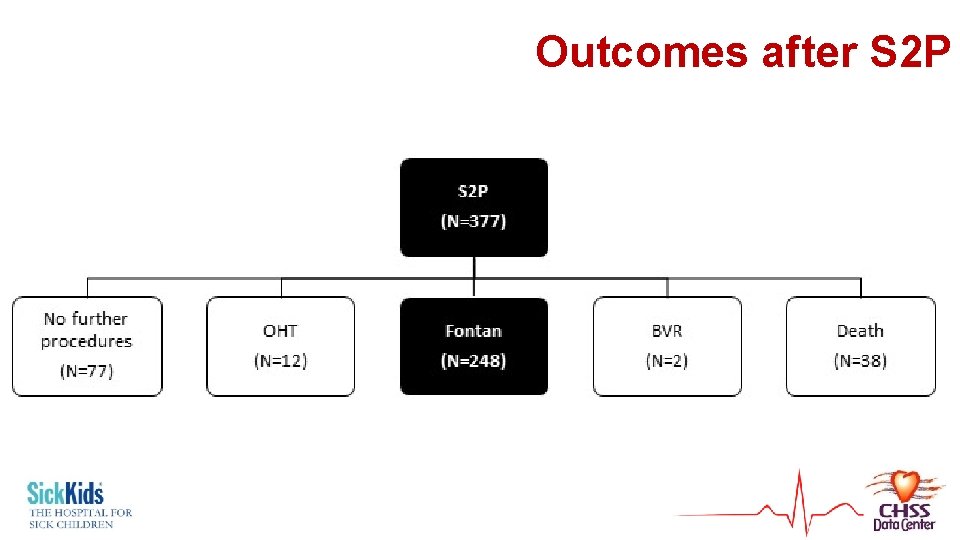
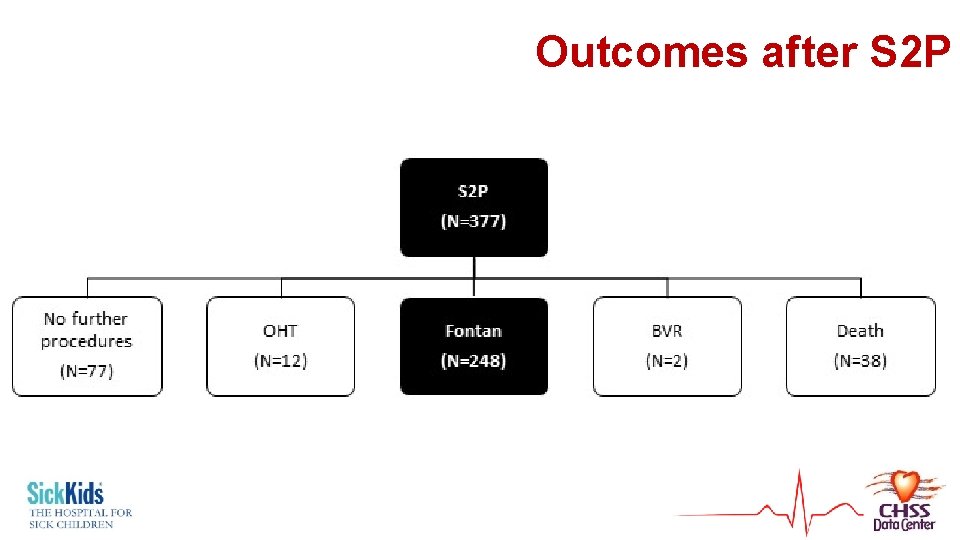
Outcomes after S 2 P
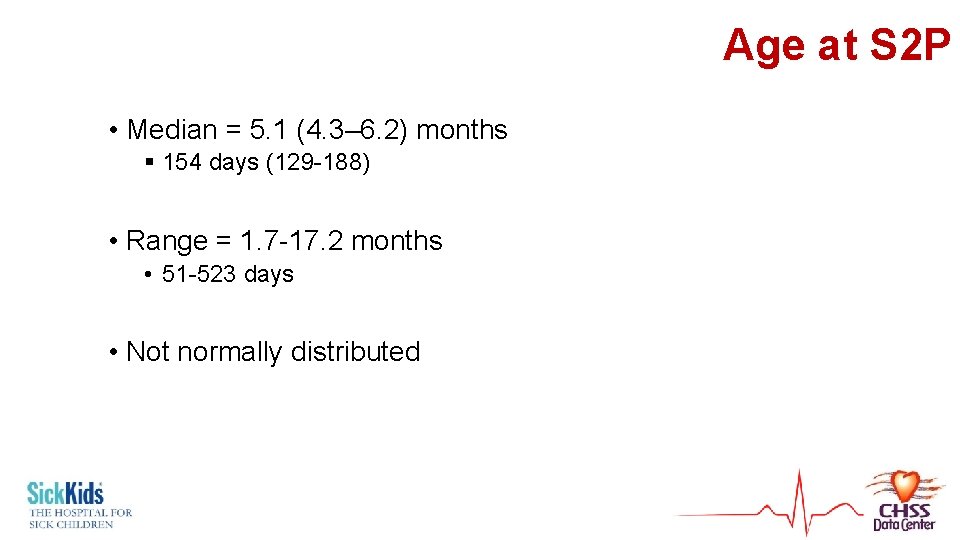
Age at S 2 P • Median = 5. 1 (4. 3– 6. 2) months § 154 days (129 -188) • Range = 1. 7 -17. 2 months • 51 -523 days • Not normally distributed

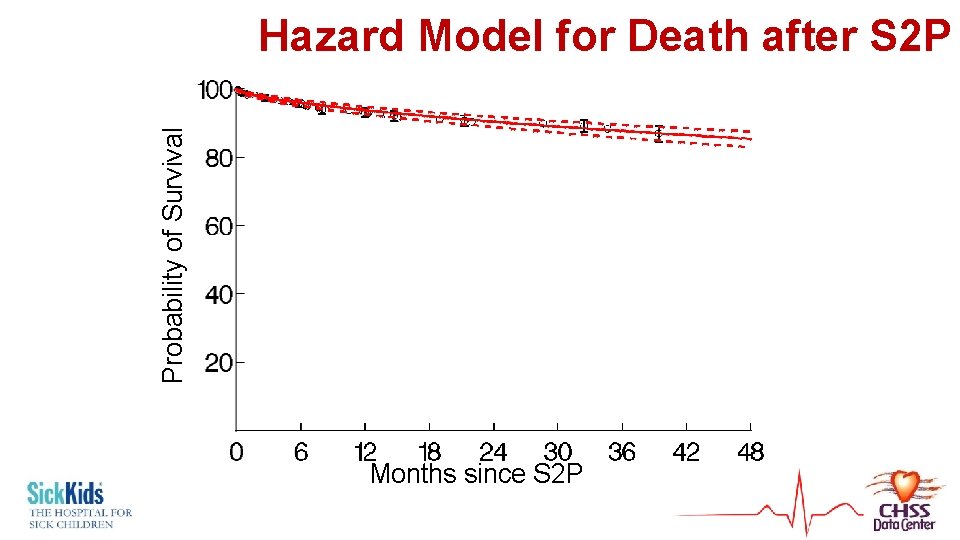
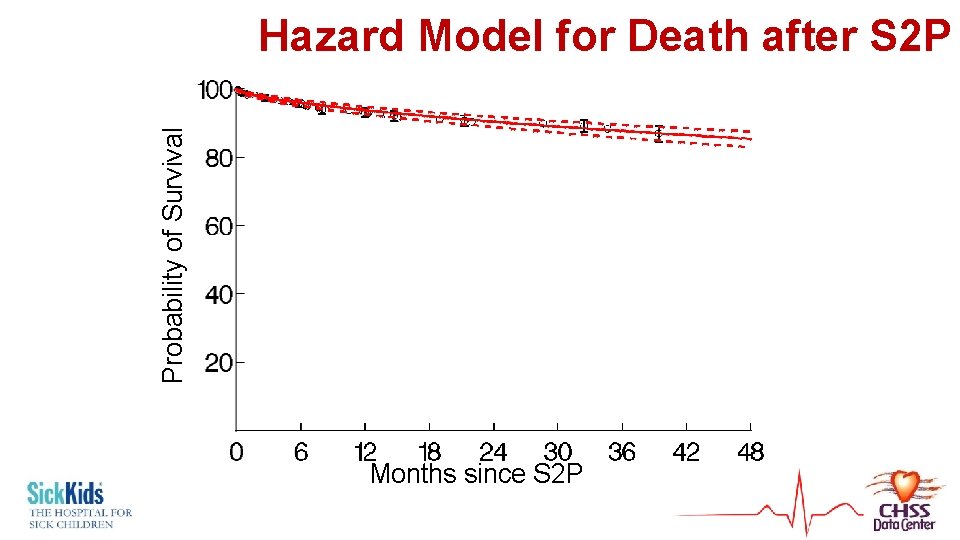
Probability of Survival Hazard Model for Death after S 2 P Months since S 2 P
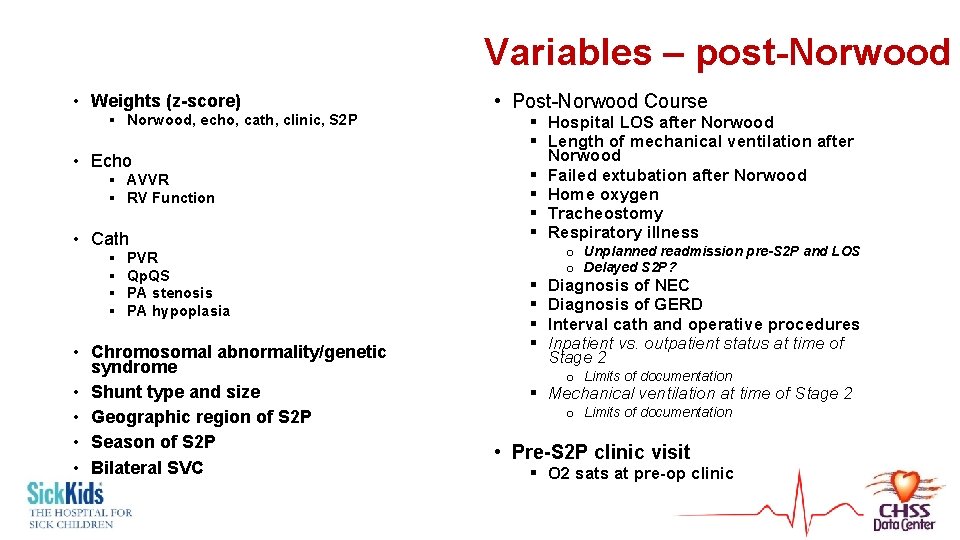
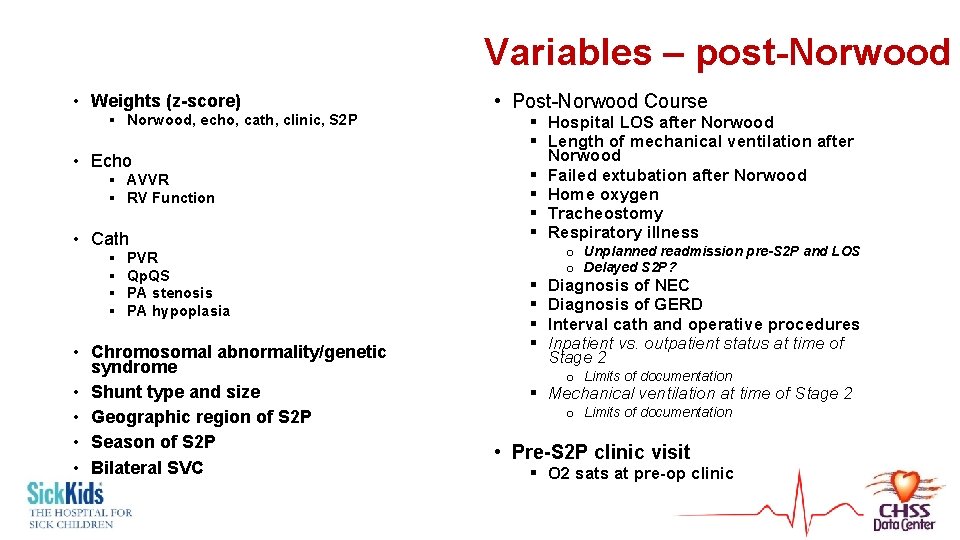
Variables – post-Norwood • Weights (z-score) § Norwood, echo, cath, clinic, S 2 P • Echo § AVVR § RV Function • Cath § § PVR Qp. QS PA stenosis PA hypoplasia • Chromosomal abnormality/genetic syndrome • Shunt type and size • Geographic region of S 2 P • Season of S 2 P • Bilateral SVC • Post-Norwood Course § Hospital LOS after Norwood § Length of mechanical ventilation after Norwood § Failed extubation after Norwood § Home oxygen § Tracheostomy § Respiratory illness § § o Unplanned readmission pre-S 2 P and LOS o Delayed S 2 P? Diagnosis of NEC Diagnosis of GERD Interval cath and operative procedures Inpatient vs. outpatient status at time of Stage 2 o Limits of documentation § Mechanical ventilation at time of Stage 2 o Limits of documentation • Pre-S 2 P clinic visit § O 2 sats at pre-op clinic
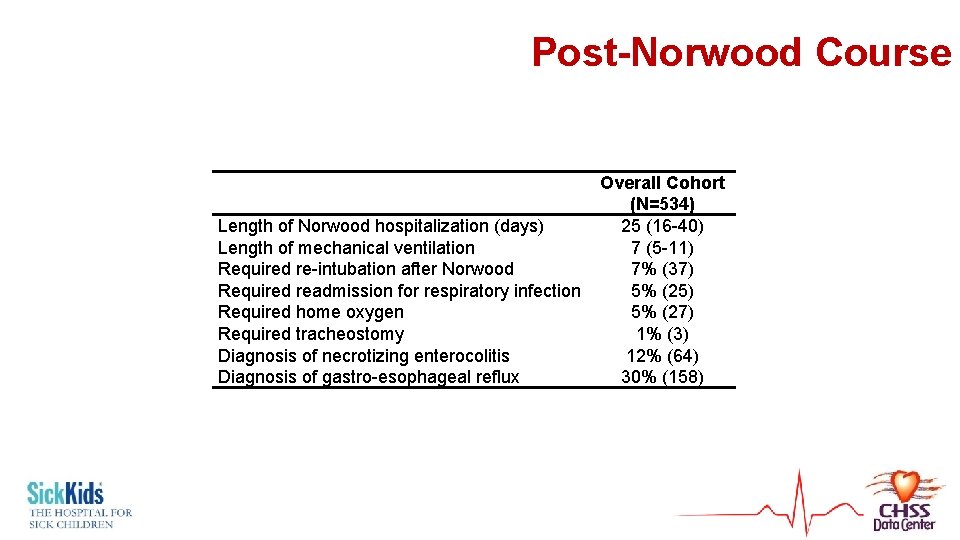
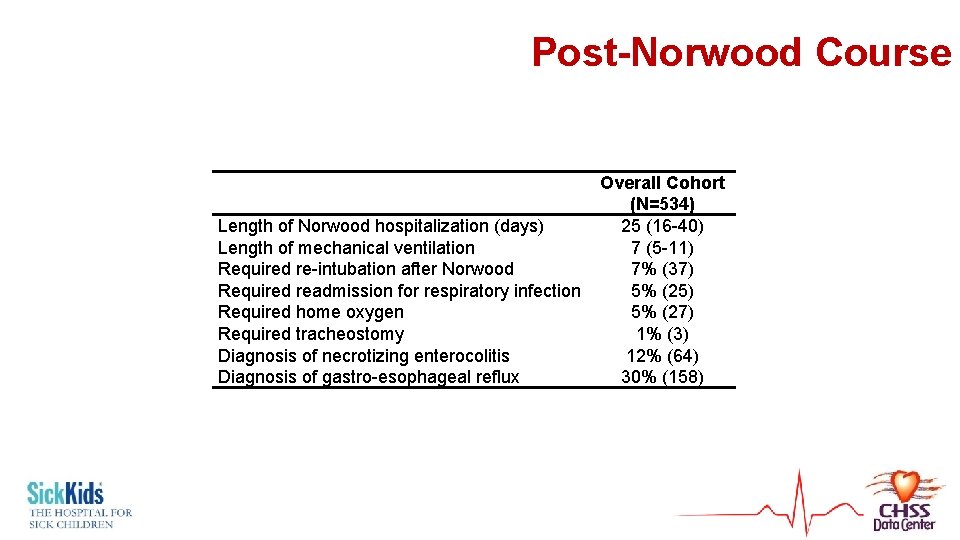
Post-Norwood Course Length of Norwood hospitalization (days) Length of mechanical ventilation Required re-intubation after Norwood Required readmission for respiratory infection Required home oxygen Required tracheostomy Diagnosis of necrotizing enterocolitis Diagnosis of gastro-esophageal reflux Overall Cohort (N=534) 25 (16 -40) 7 (5 -11) 7% (37) 5% (25) 5% (27) 1% (3) 12% (64) 30% (158)
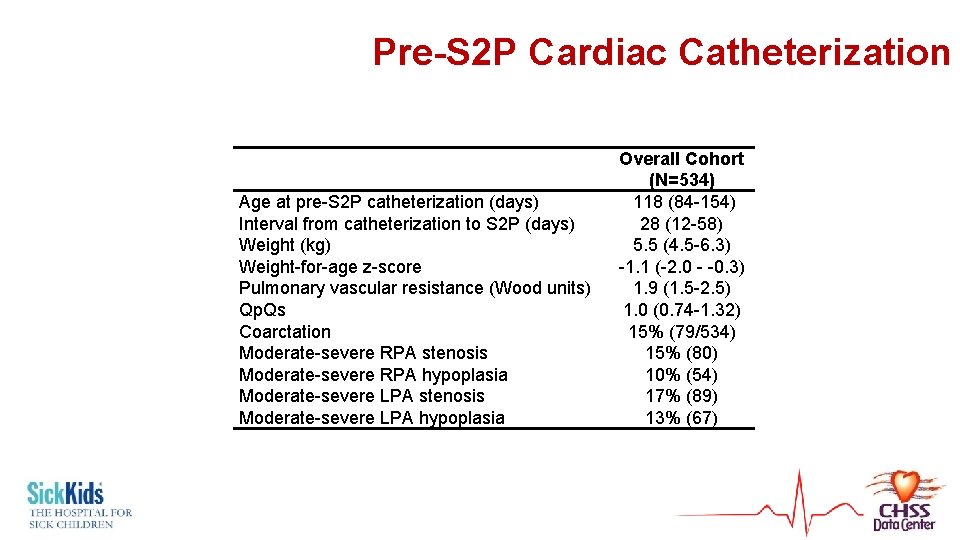
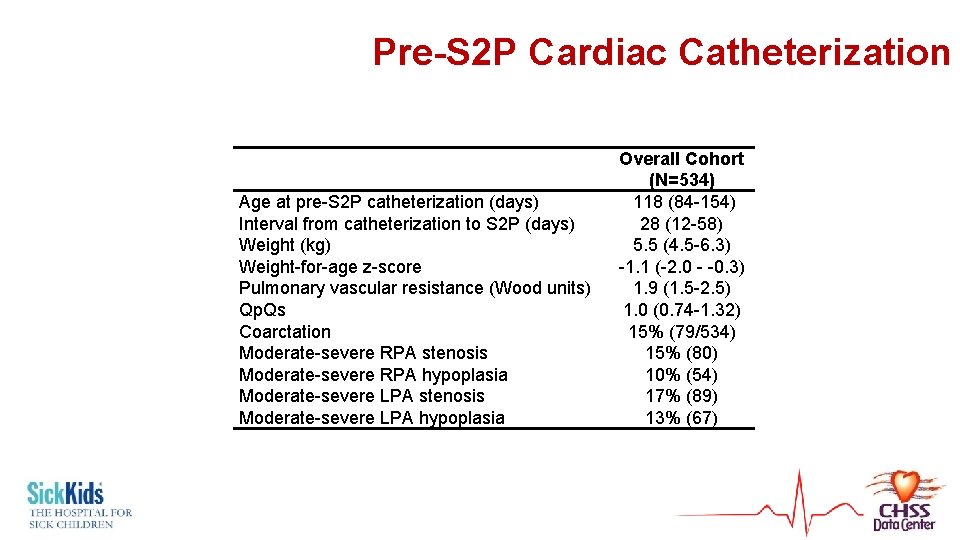
Pre-S 2 P Cardiac Catheterization Age at pre-S 2 P catheterization (days) Interval from catheterization to S 2 P (days) Weight (kg) Weight-for-age z-score Pulmonary vascular resistance (Wood units) Qp. Qs Coarctation Moderate-severe RPA stenosis Moderate-severe RPA hypoplasia Moderate-severe LPA stenosis Moderate-severe LPA hypoplasia Overall Cohort (N=534) 118 (84 -154) 28 (12 -58) 5. 5 (4. 5 -6. 3) -1. 1 (-2. 0 - -0. 3) 1. 9 (1. 5 -2. 5) 1. 0 (0. 74 -1. 32) 15% (79/534) 15% (80) 10% (54) 17% (89) 13% (67)
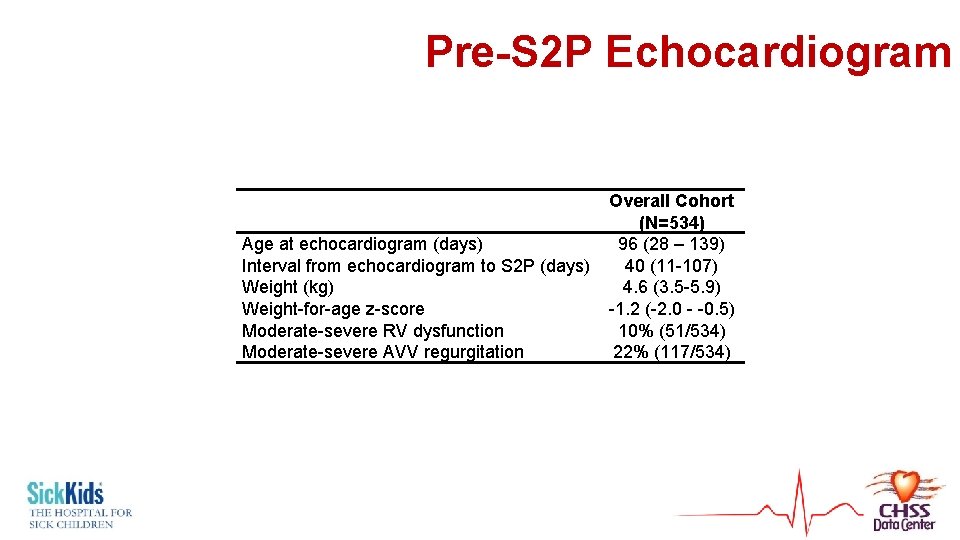
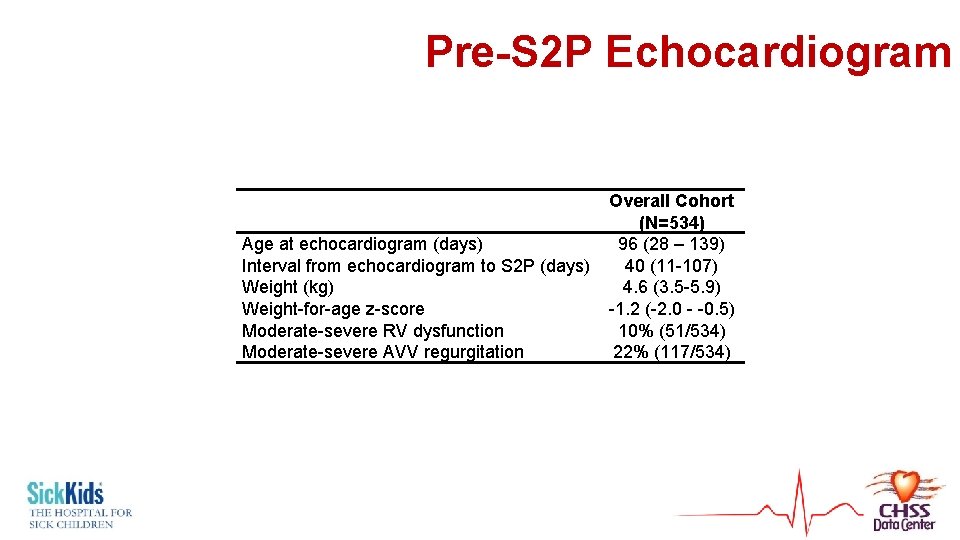
Pre-S 2 P Echocardiogram Age at echocardiogram (days) Interval from echocardiogram to S 2 P (days) Weight (kg) Weight-for-age z-score Moderate-severe RV dysfunction Moderate-severe AVV regurgitation Overall Cohort (N=534) 96 (28 – 139) 40 (11 -107) 4. 6 (3. 5 -5. 9) -1. 2 (-2. 0 - -0. 5) 10% (51/534) 22% (117/534)
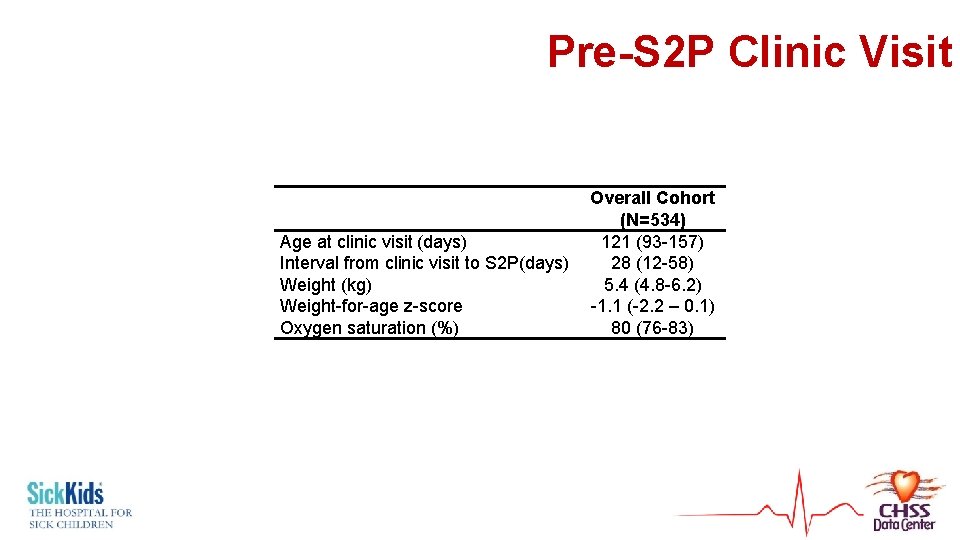
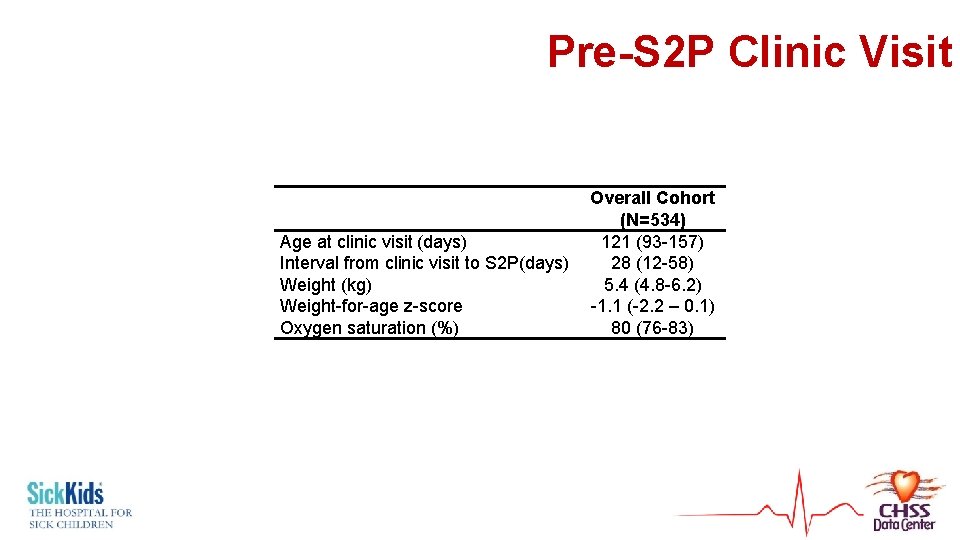
Pre-S 2 P Clinic Visit Age at clinic visit (days) Interval from clinic visit to S 2 P(days) Weight (kg) Weight-for-age z-score Oxygen saturation (%) Overall Cohort (N=534) 121 (93 -157) 28 (12 -58) 5. 4 (4. 8 -6. 2) -1. 1 (-2. 2 – 0. 1) 80 (76 -83)
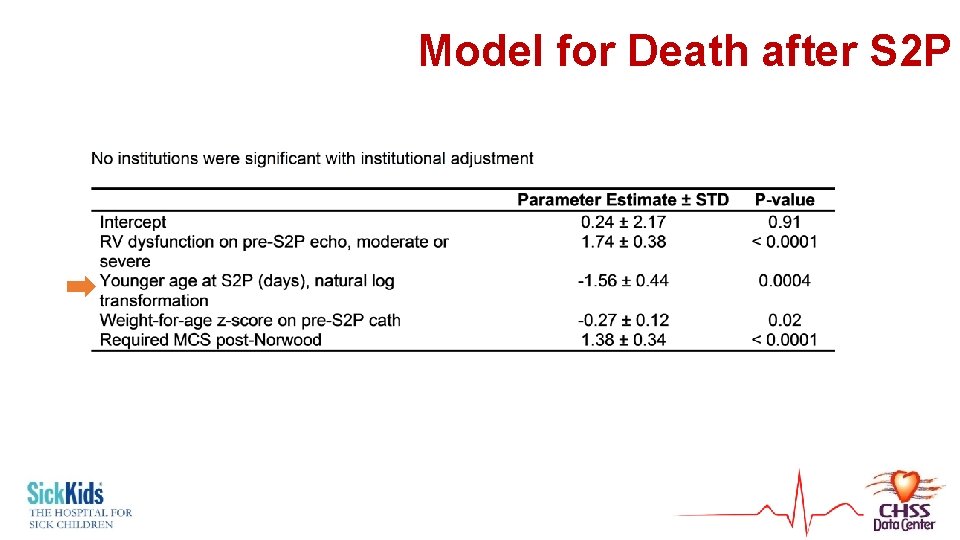
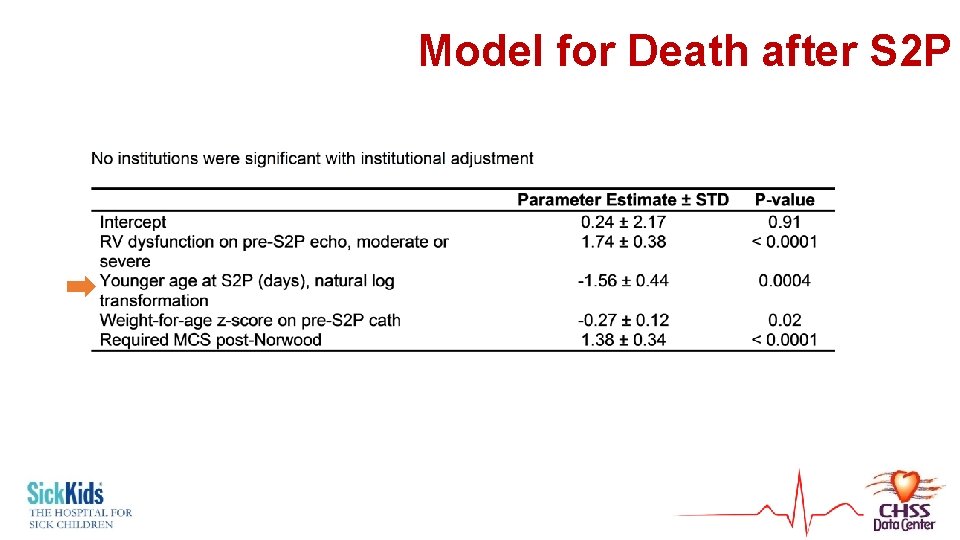
Model for Death after S 2 P
Determinants of Timing of S 2 P
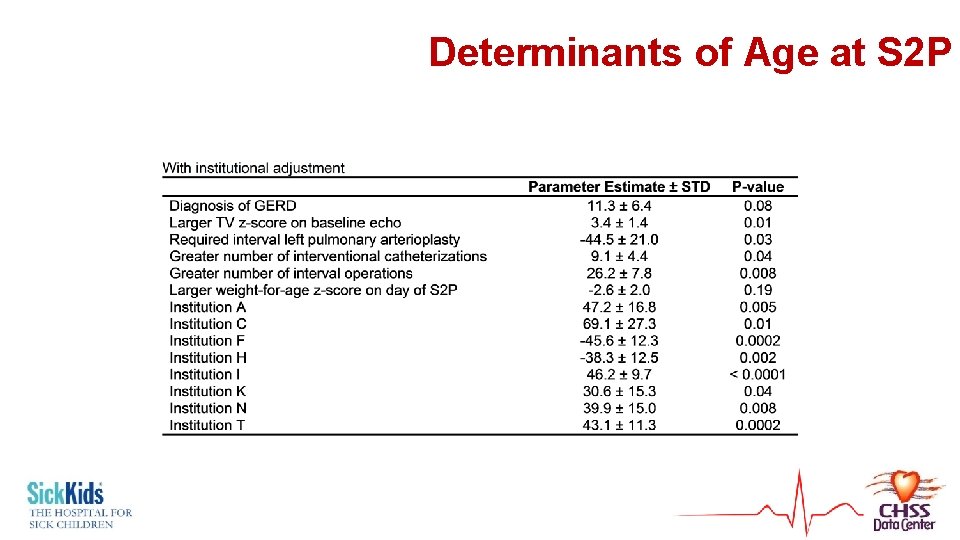
Determinants of Timing • Linear regression • Outcome = age at S 2 P • Candidate covariables – all from 1 st two models
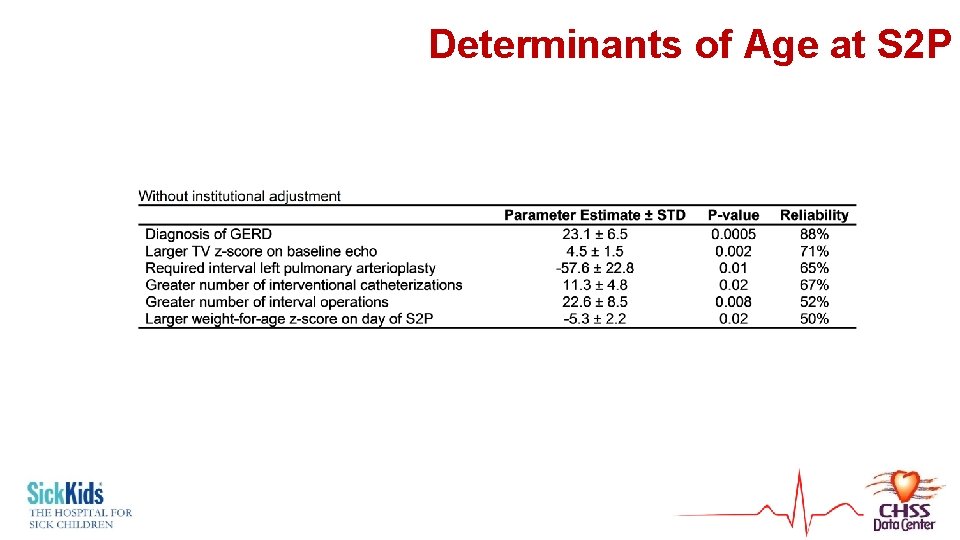
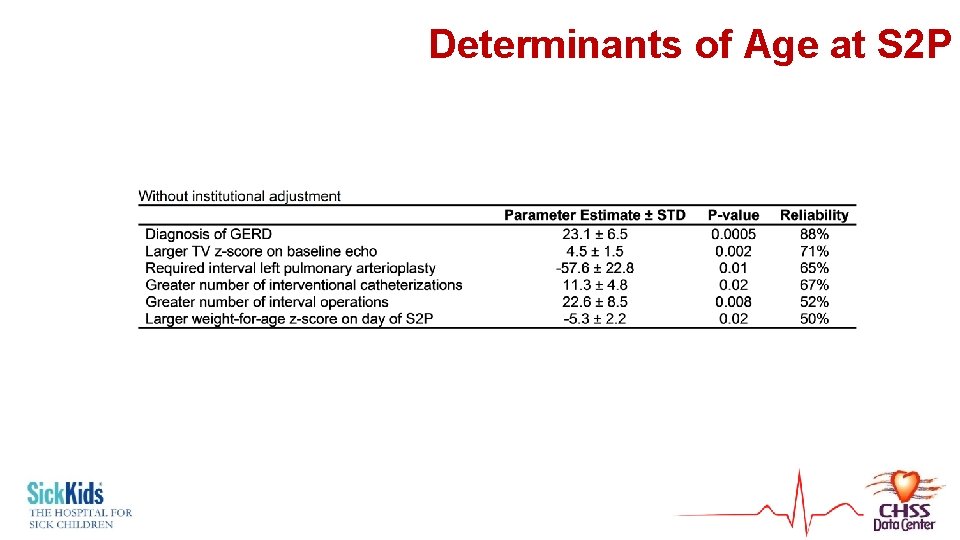
Determinants of Age at S 2 P
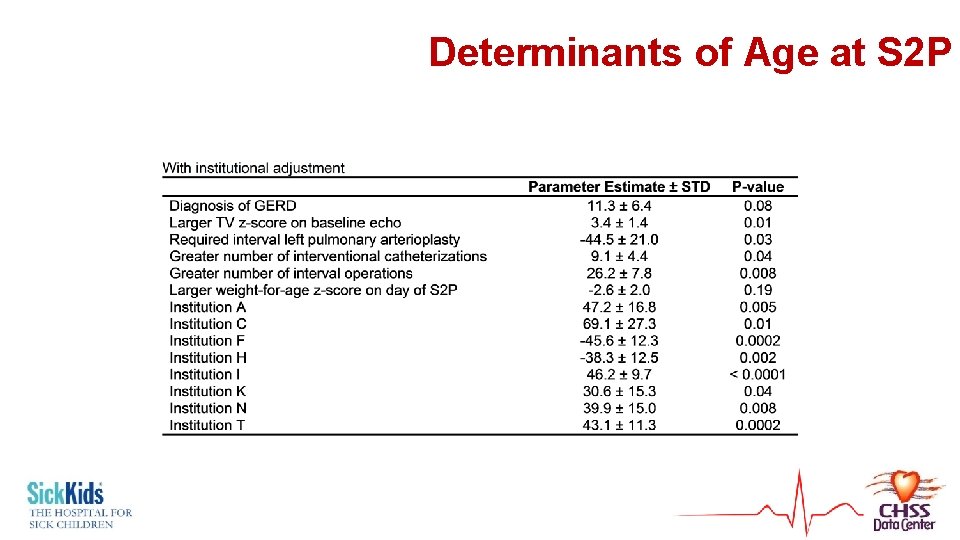
Determinants of Age at S 2 P
Analyzing Staged Procedures and Optimal Timing
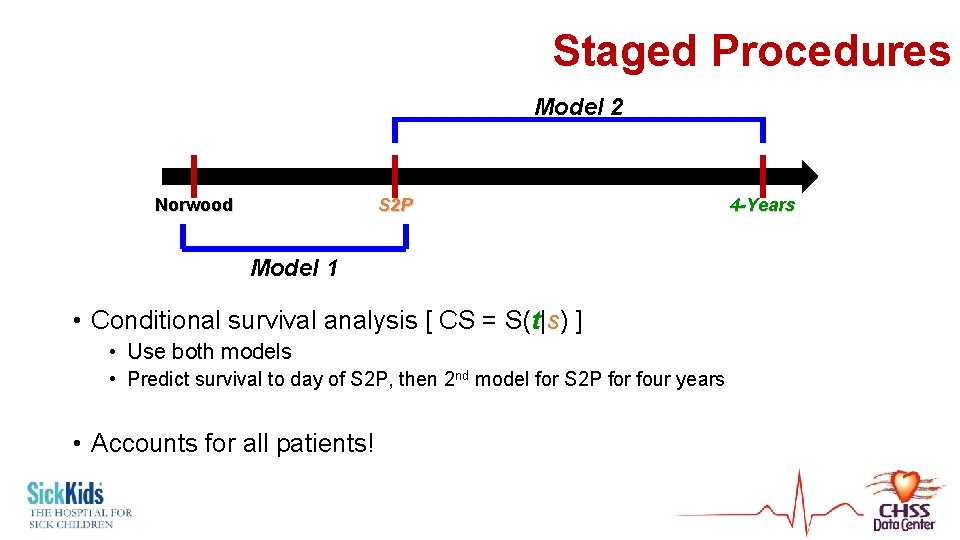
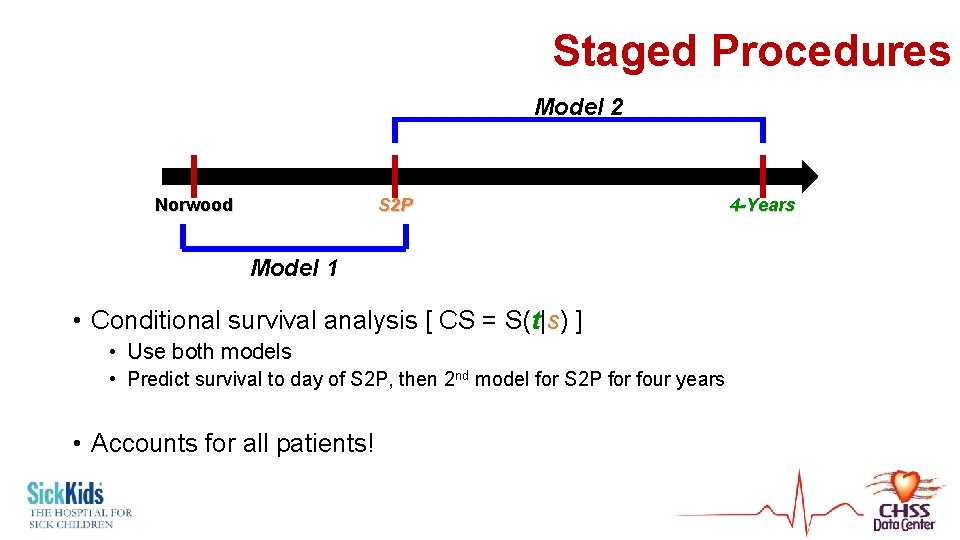
Staged Procedures Model 2 Norwood S 2 P 4 -Years Model 1 • Conditional survival analysis [ CS = S(t|s) ] • Use both models • Predict survival to day of S 2 P, then 2 nd model for S 2 P for four years • Accounts for all patients!
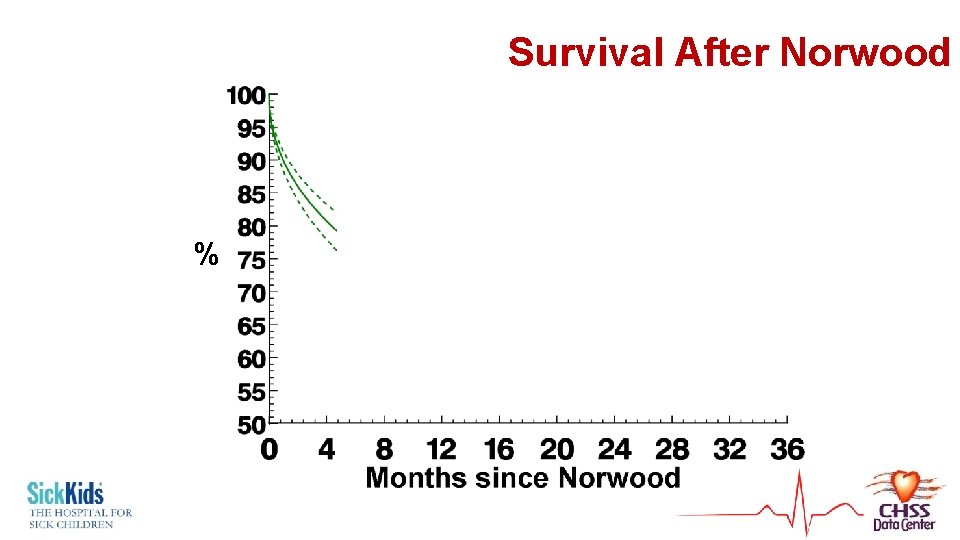
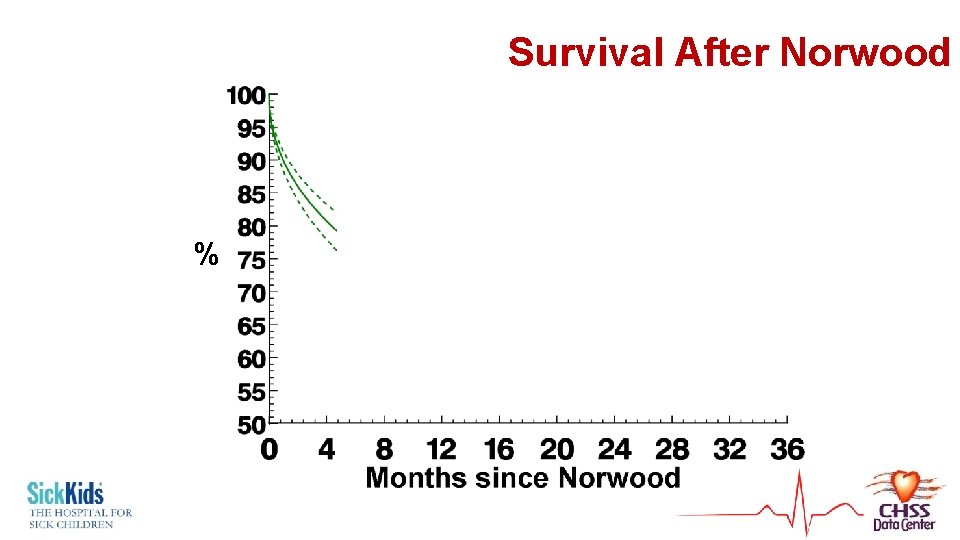
Survival After Norwood %
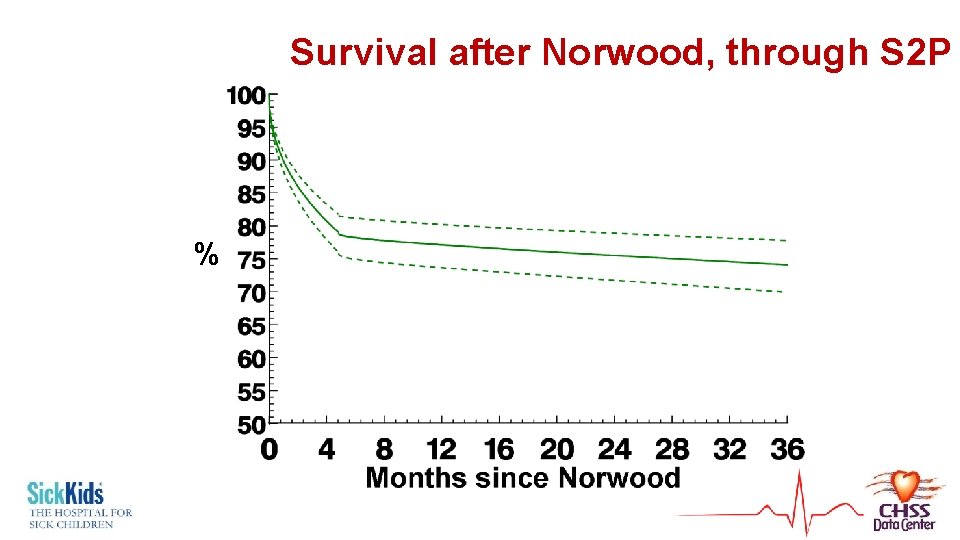
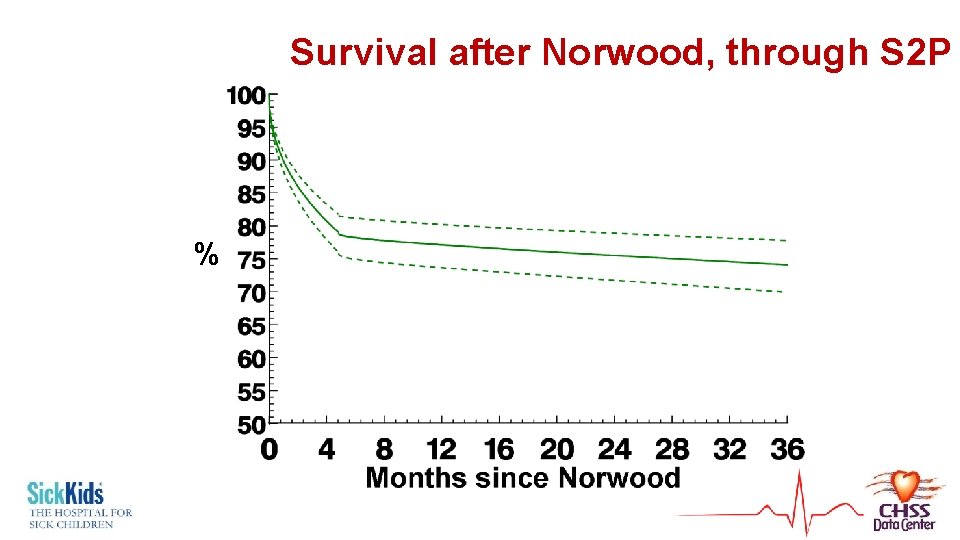
Survival after Norwood, through S 2 P %

Probability of Survival through S 2 P Survival at 4 years = 71± 5% Months since Norwood
Analyzing Timing • Age at S 2 P identified as risk factor • Parametric model = mathematical equation • Nomogram of survival vs. Age at S 2 P
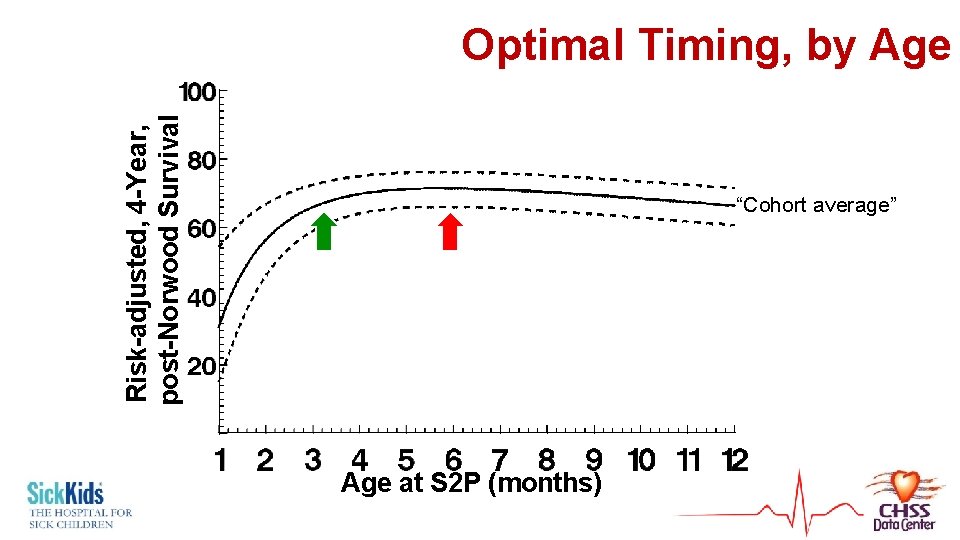
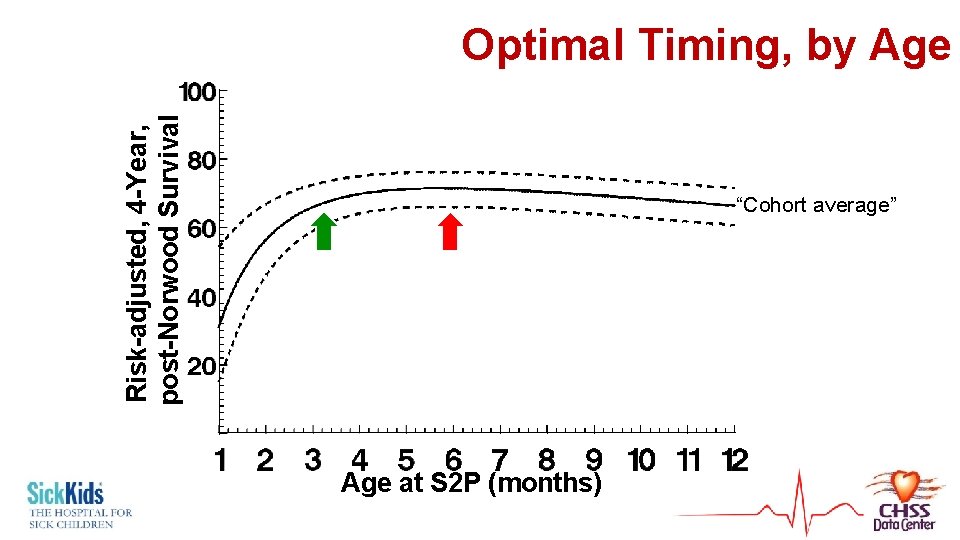
Risk-adjusted, 4 -Year, post-Norwood Survival Optimal Timing, by Age “Cohort average” Age at S 2 P (months)
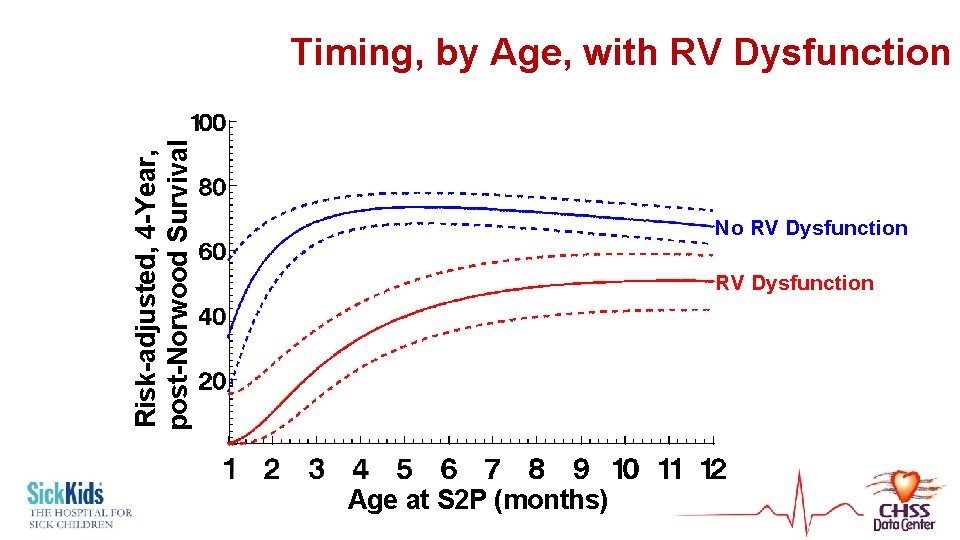
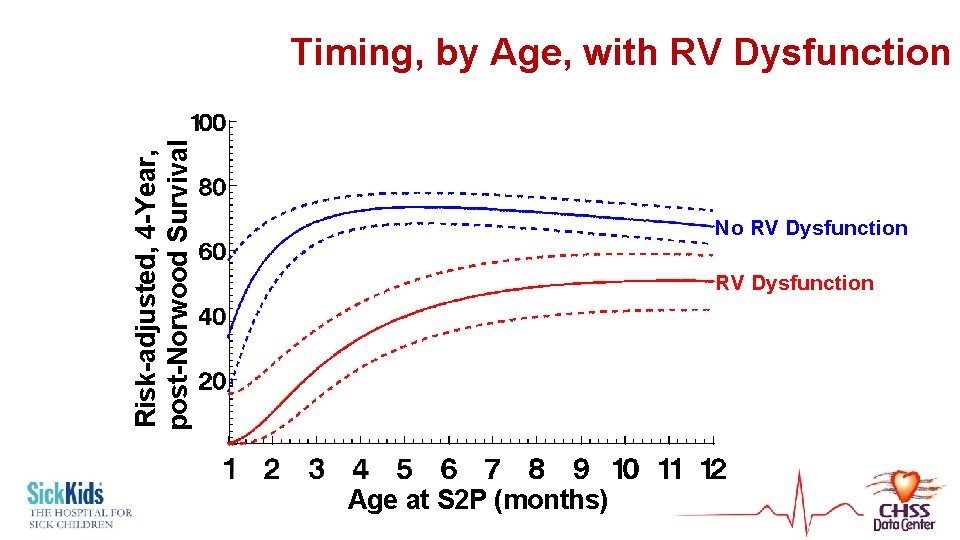
Risk-adjusted, 4 -Year, post-Norwood Survival Timing, by Age, with RV Dysfunction No RV Dysfunction Age at S 2 P (months)
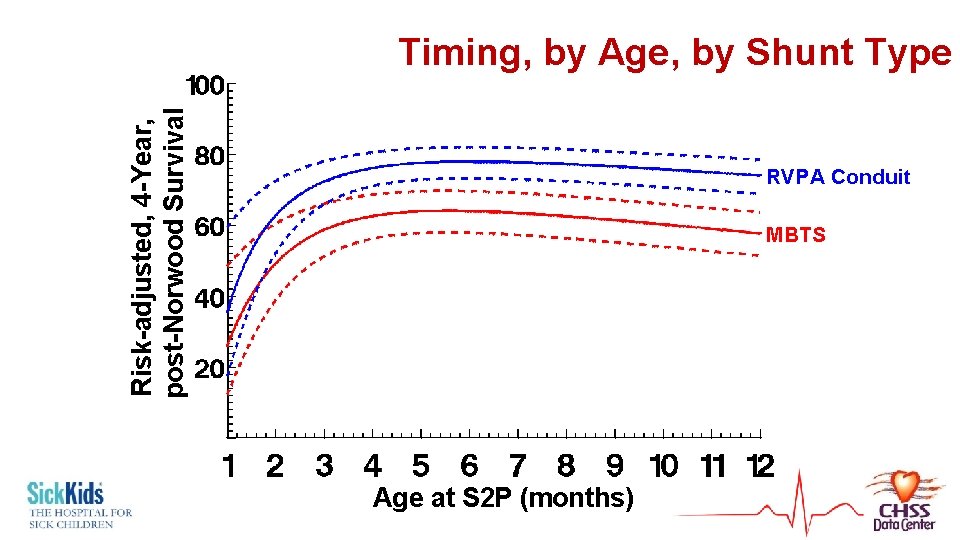
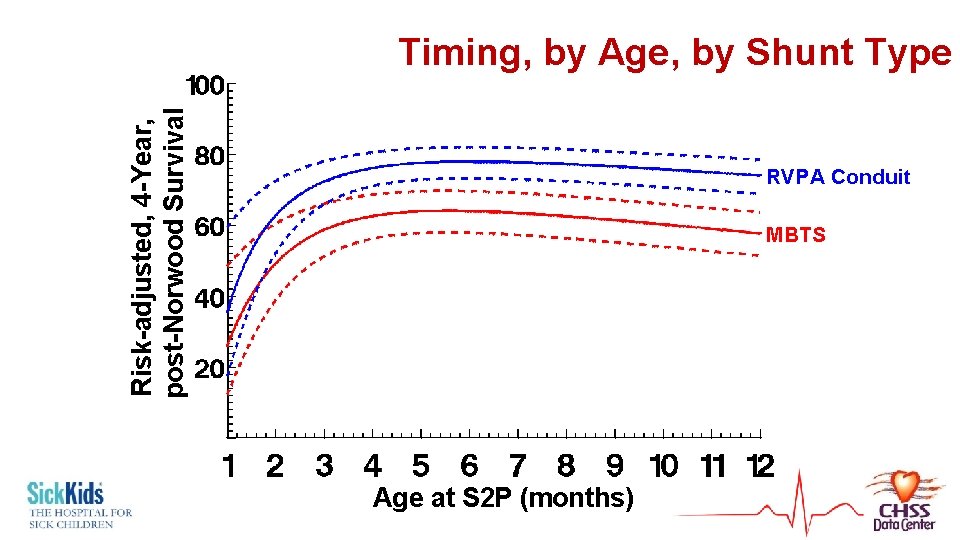
Risk-adjusted, 4 -Year, post-Norwood Survival Timing, by Age, by Shunt Type RVPA Conduit MBTS Age at S 2 P (months)
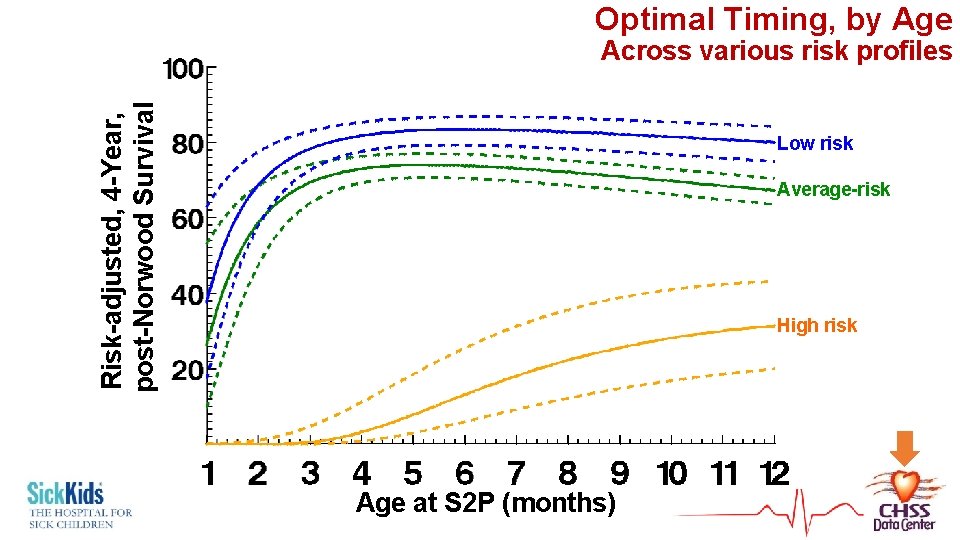
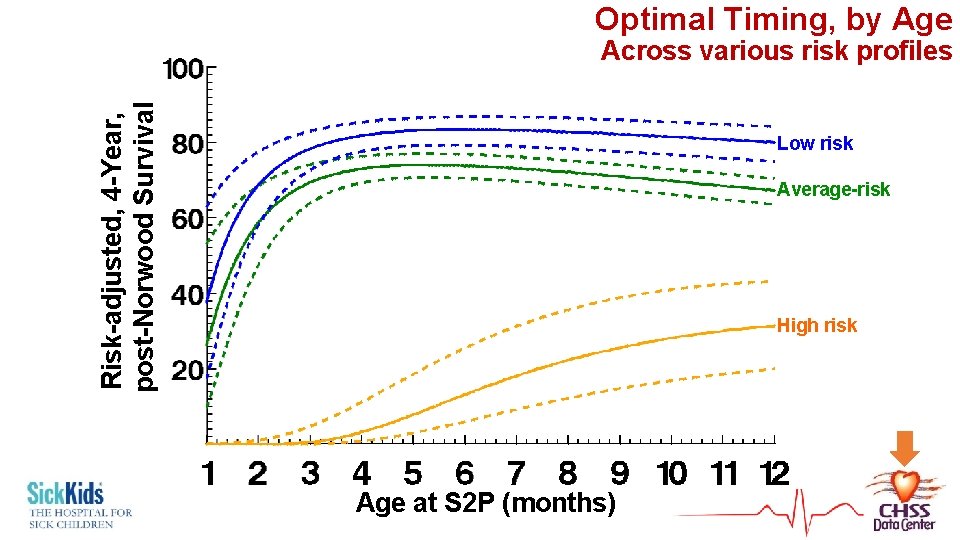
Optimal Timing, by Age Risk-adjusted, 4 -Year, post-Norwood Survival Across various risk profiles Low risk Average-risk High risk Age at S 2 P (months)
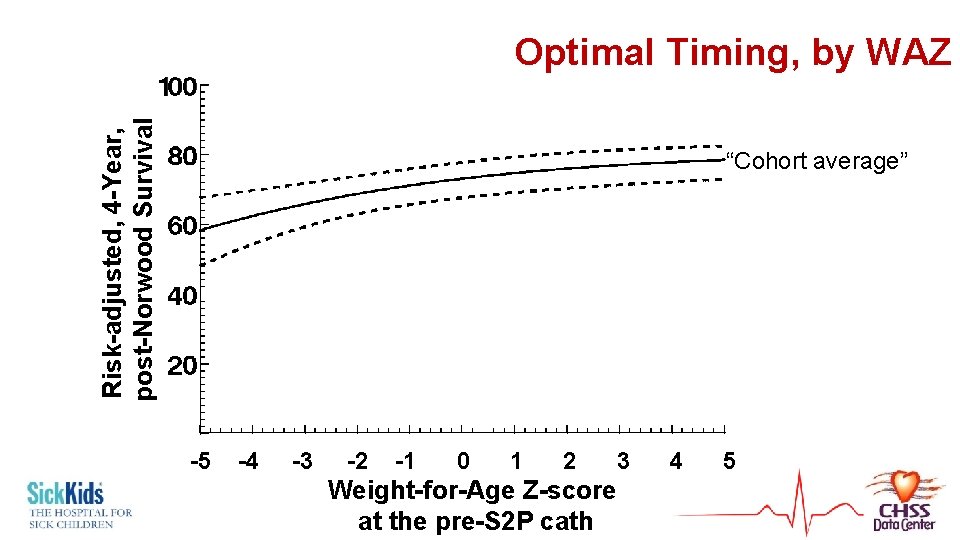
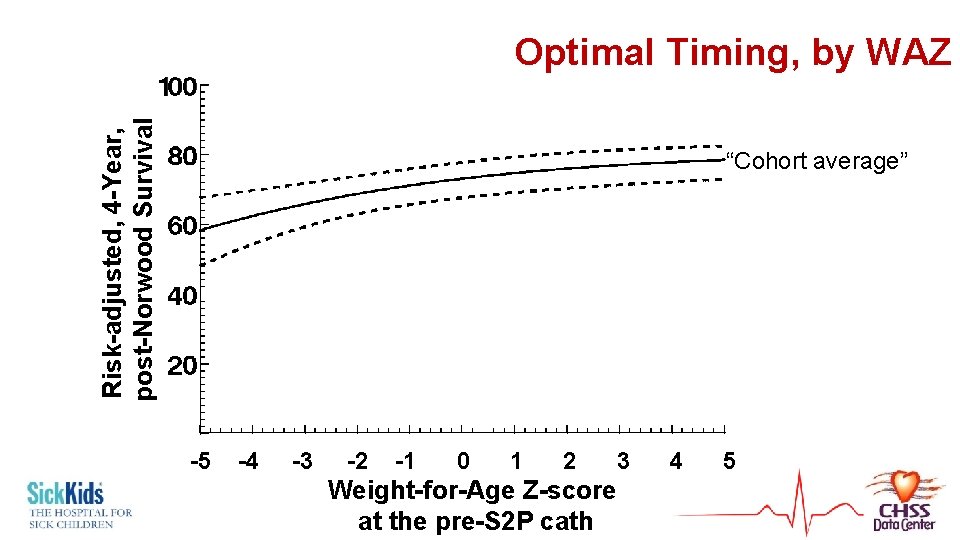
Risk-adjusted, 4 -Year, post-Norwood Survival Optimal Timing, by WAZ “Cohort average” -5 -4 -3 -2 -1 0 1 2 3 4 5 Weight-for-Age Z-score at the pre-S 2 P cath
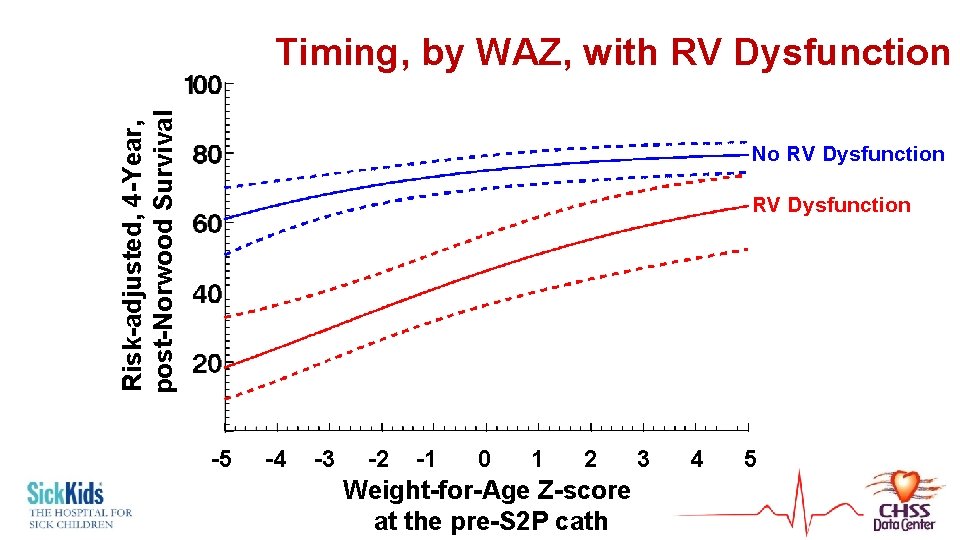
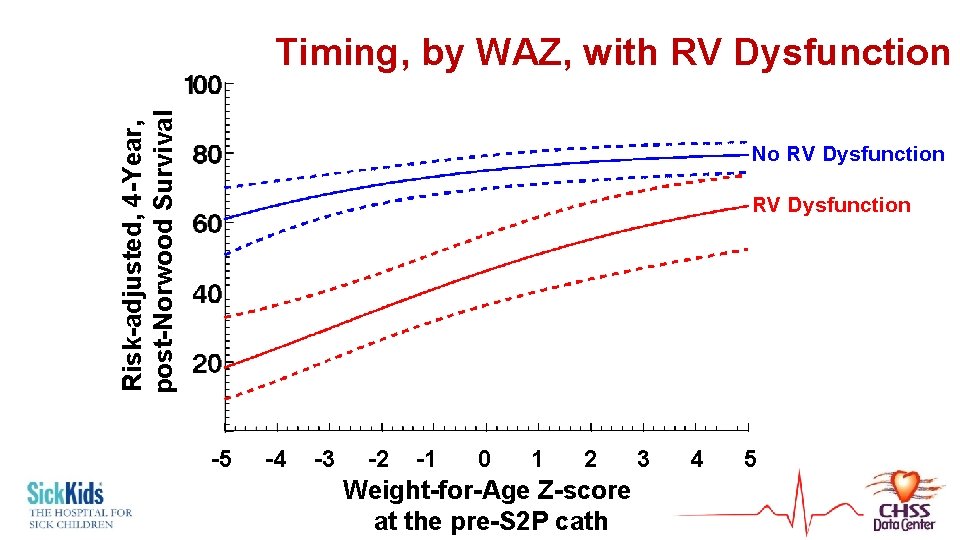
Risk-adjusted, 4 -Year, post-Norwood Survival Timing, by WAZ, with RV Dysfunction No RV Dysfunction -5 -4 -3 -2 -1 0 1 2 3 4 5 Weight-for-Age Z-score at the pre-S 2 P cath
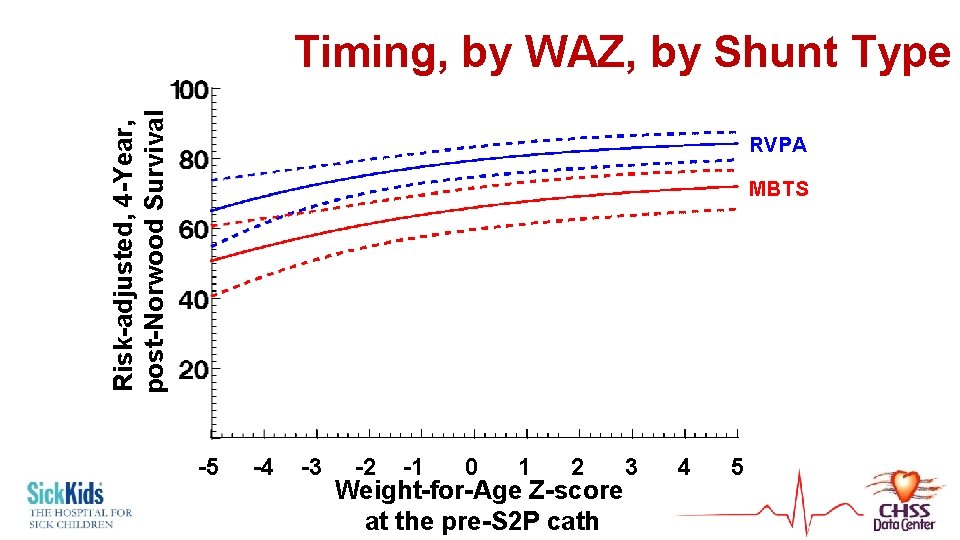
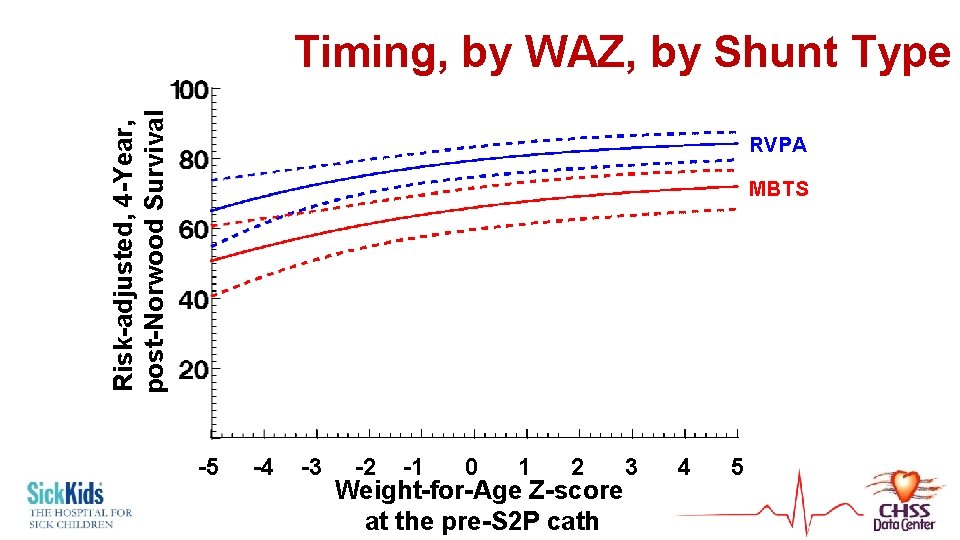
Risk-adjusted, 4 -Year, post-Norwood Survival Timing, by WAZ, by Shunt Type RVPA MBTS -5 -4 -3 -2 -1 0 1 2 3 4 5 Weight-for-Age Z-score at the pre-S 2 P cath
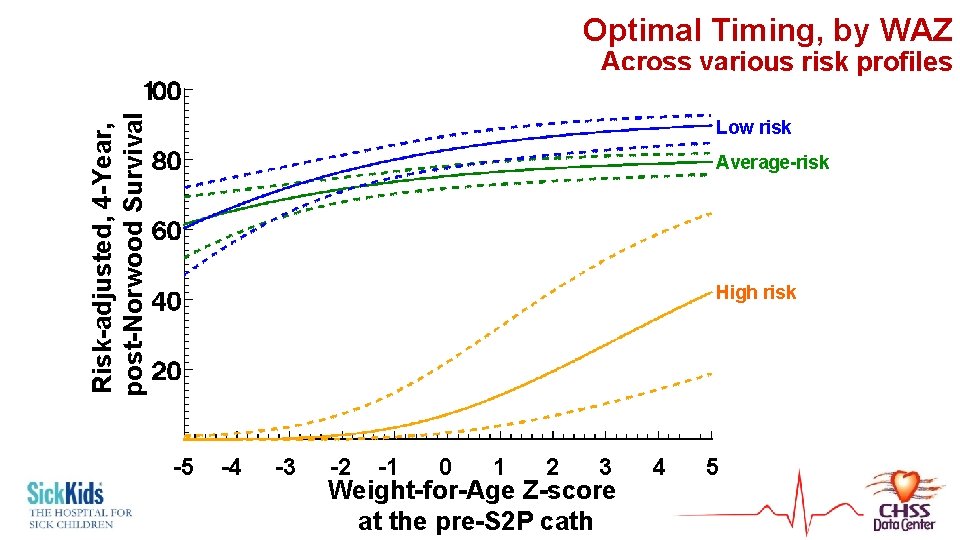
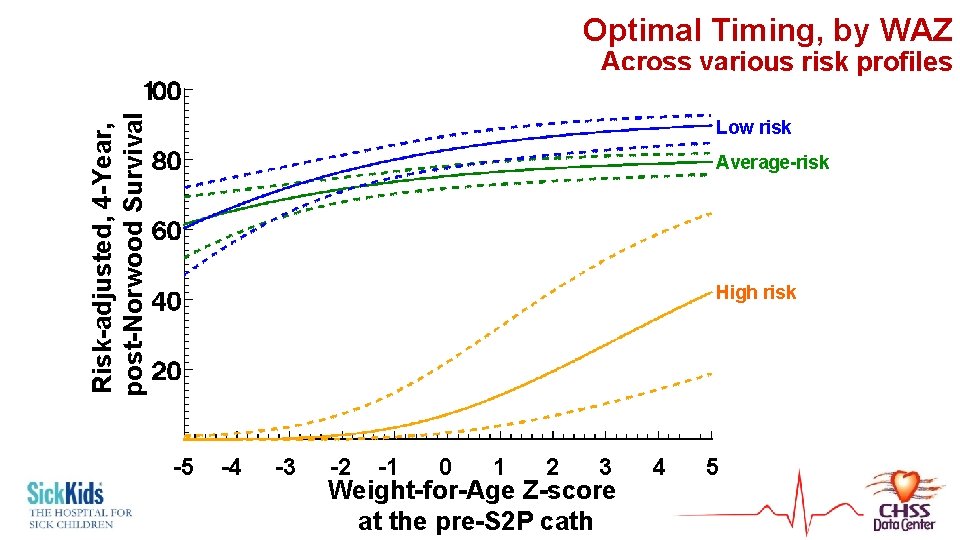
Optimal Timing, by WAZ Risk-adjusted, 4 -Year, post-Norwood Survival Across various risk profiles Low risk Average-risk High risk -5 -4 -3 -2 -1 0 1 2 3 4 5 Weight-for-Age Z-score at the pre-S 2 P cath
Elective S 2 P
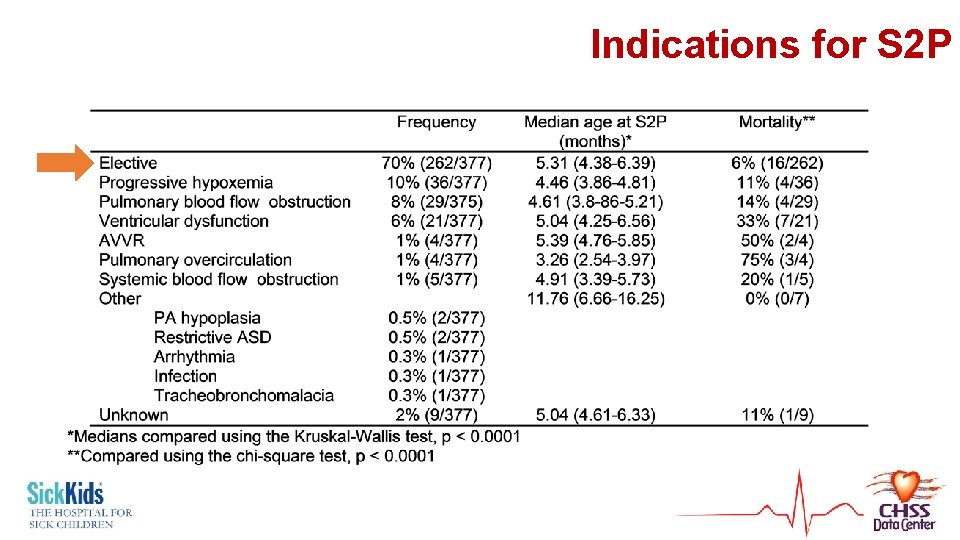
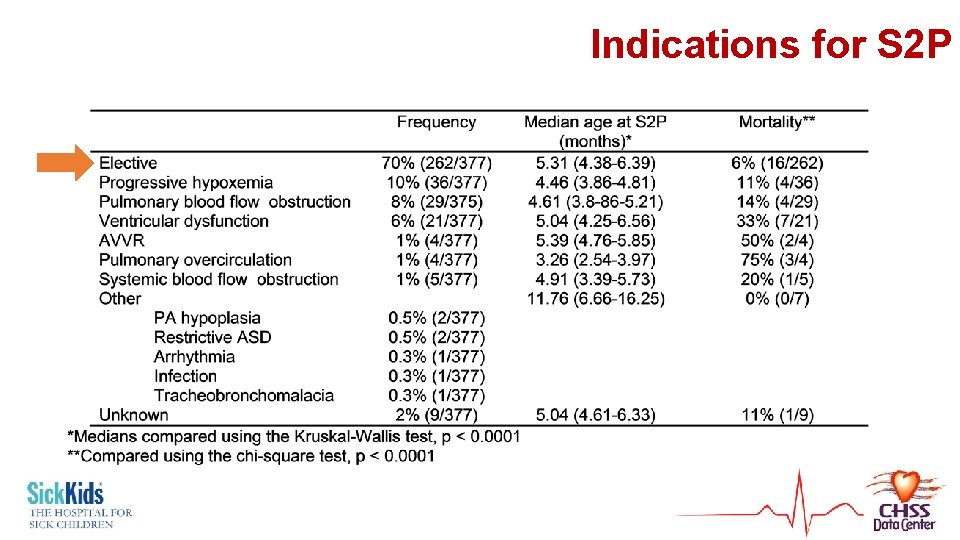
Indications for S 2 P
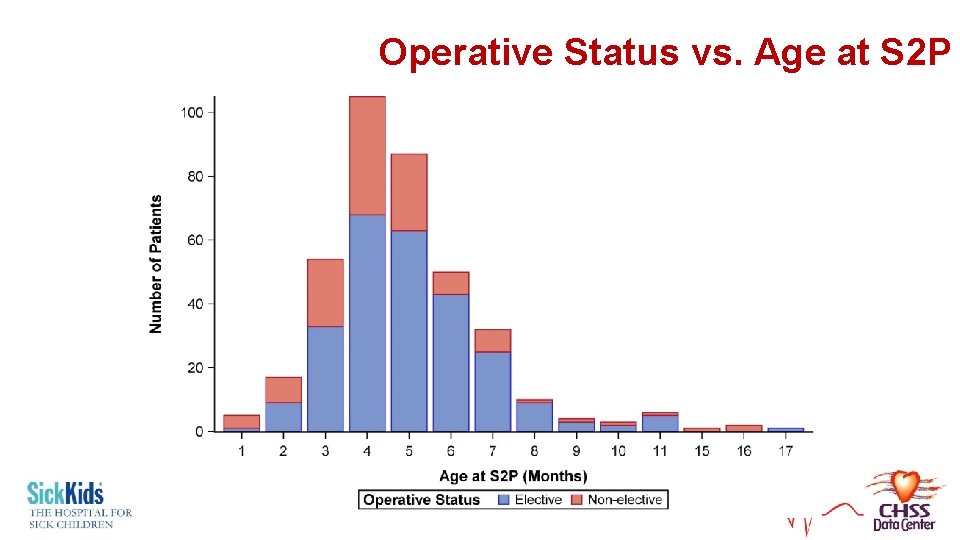
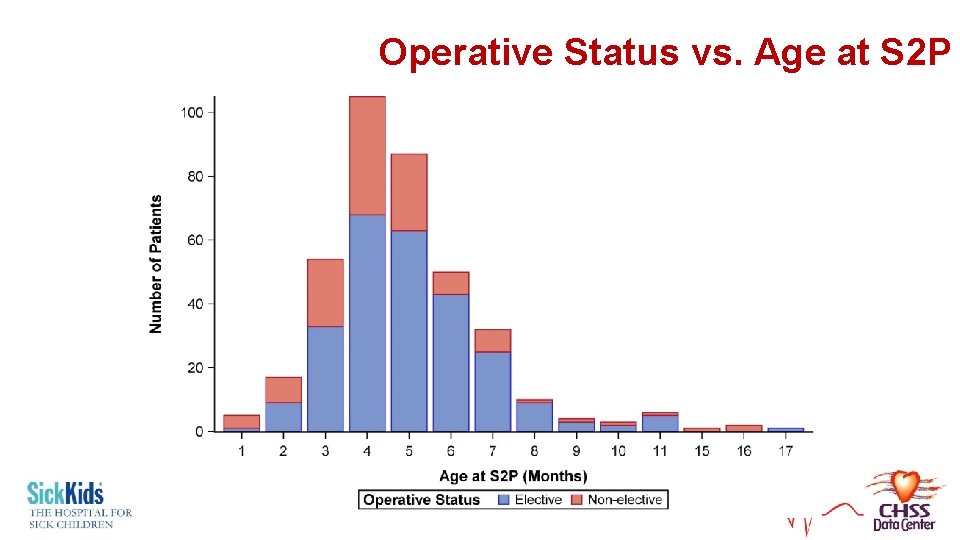
Operative Status vs. Age at S 2 P
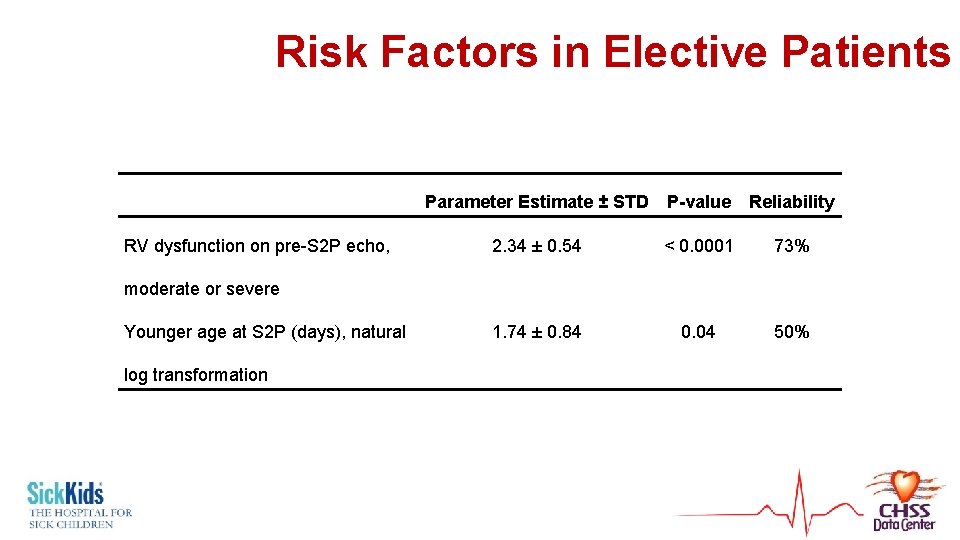
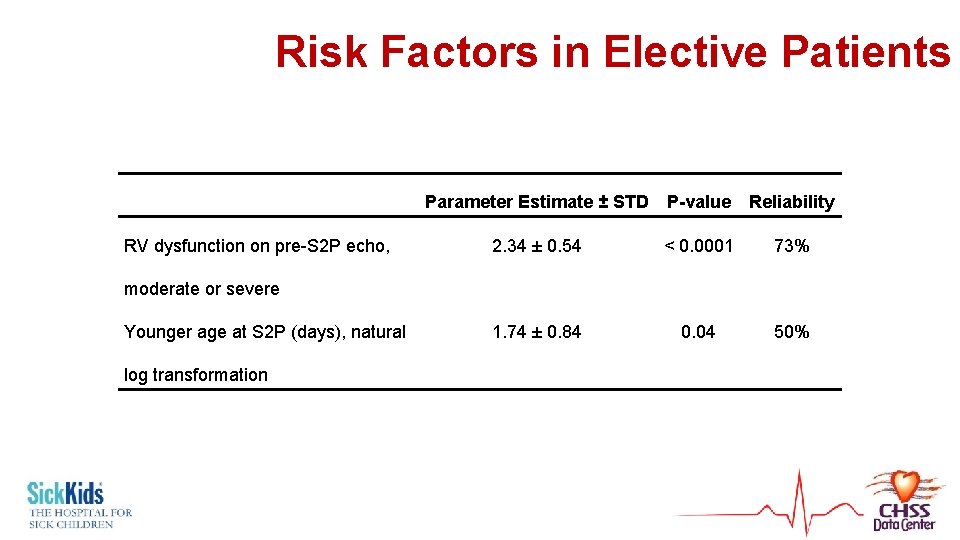
Risk Factors in Elective Patients RV dysfunction on pre-S 2 P echo, Parameter Estimate ± STD P-value Reliability 2. 34 ± 0. 54 < 0. 0001 73% 1. 74 ± 0. 84 0. 04 50% moderate or severe Younger age at S 2 P (days), natural log transformation
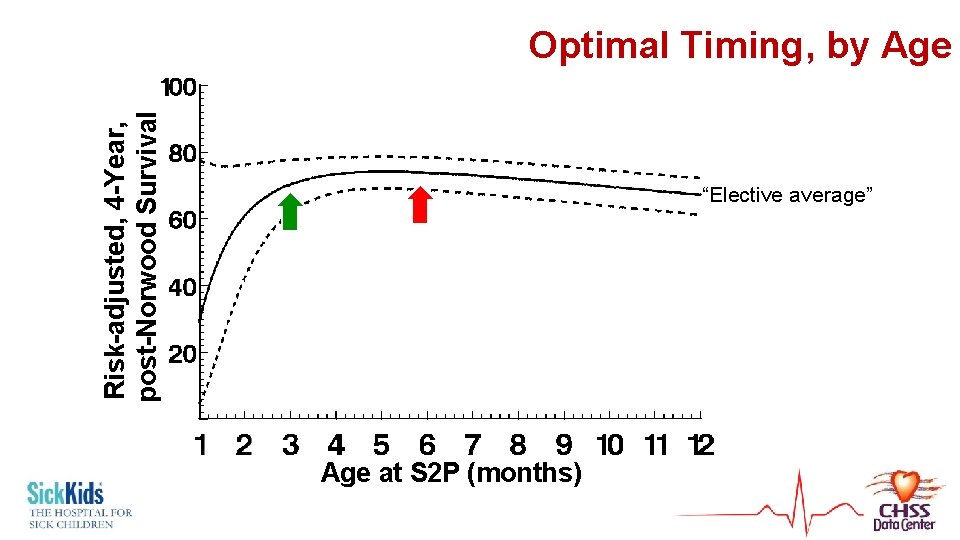
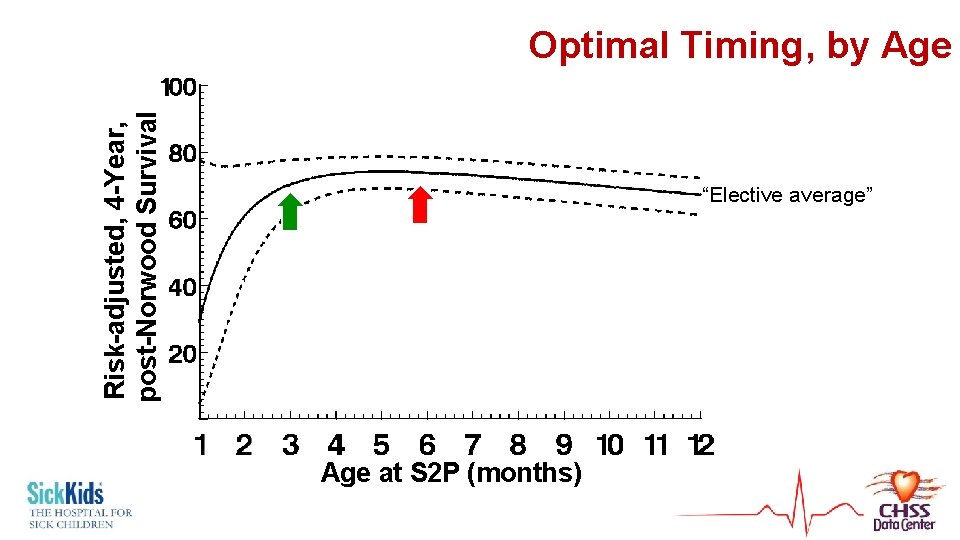
Risk-adjusted, 4 -Year, post-Norwood Survival Optimal Timing, by Age “Elective average” Age at S 2 P (months)
High-Risk Patients
Why does it appear that high-risk appear to do better with later S 2 P? • Regardless of age or WAZ – survival poor • Especially with early S 2 P • Cannot advocate non-intervention in the deteriorating “high-risk” infant • “Length time bias” • Highest risk patients die earlier – push down survival § Less high risk – survive longer to undergo later S 2 P
“High-Risk S 2 P” vs. Transplantation? • 11 patients underwent heart transplantation after Norwood • All currently still alive • Can’t make a model, can only suggest this from descriptive statistics

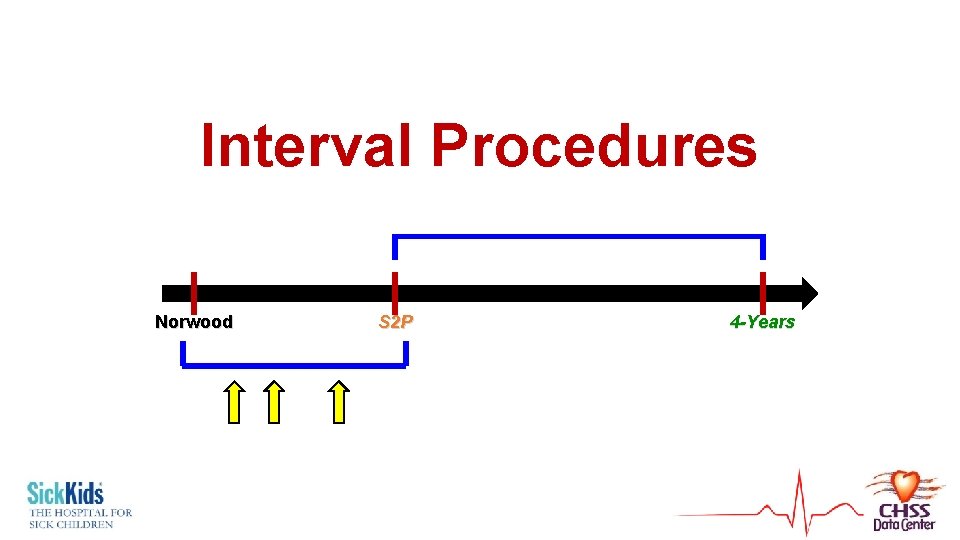
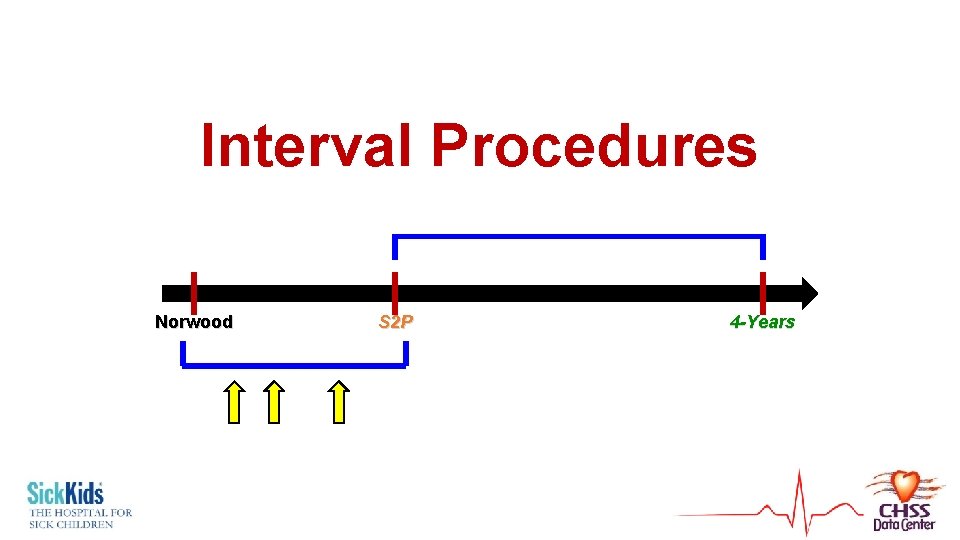
Interval Procedures Norwood S 2 P 4 -Years

Prevalence of Interval Procedures Interval cardiac catheterization procedure Interval operation Patients Total procedures # of Procedures Survival after Norwood 178 275 0 -5 97% 68 86 0 -3 68%
Methodology • First analyzed for development of 2 nd model • But occur during Norwood – S 2 P interval • Time-varying covariables • Modulated Renewal
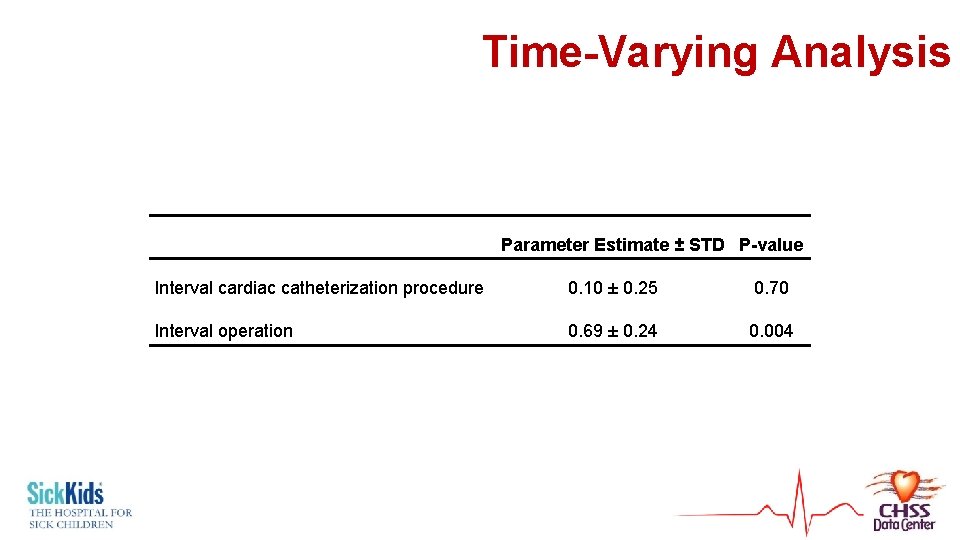
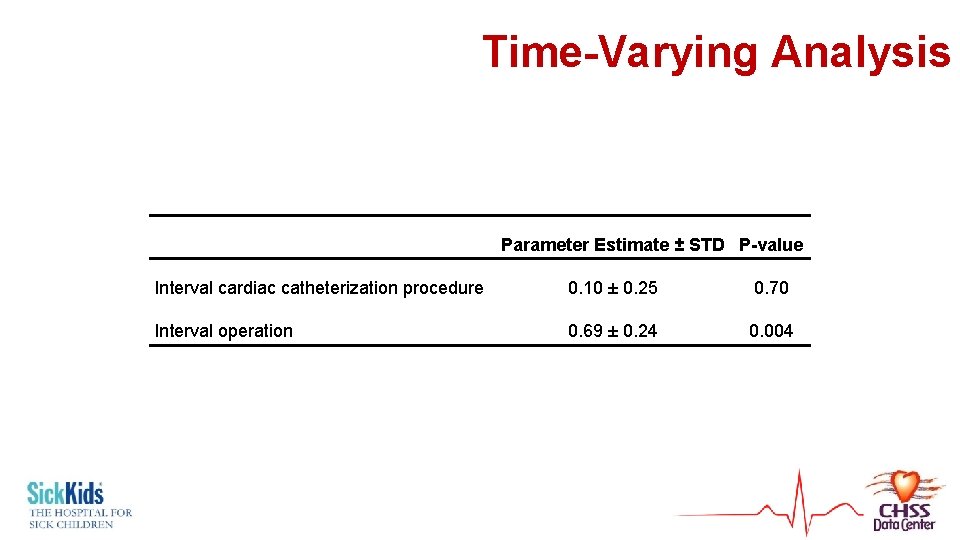
Time-Varying Analysis Parameter Estimate ± STD P-value Interval cardiac catheterization procedure 0. 10 ± 0. 25 0. 70 Interval operation 0. 69 ± 0. 24 0. 004
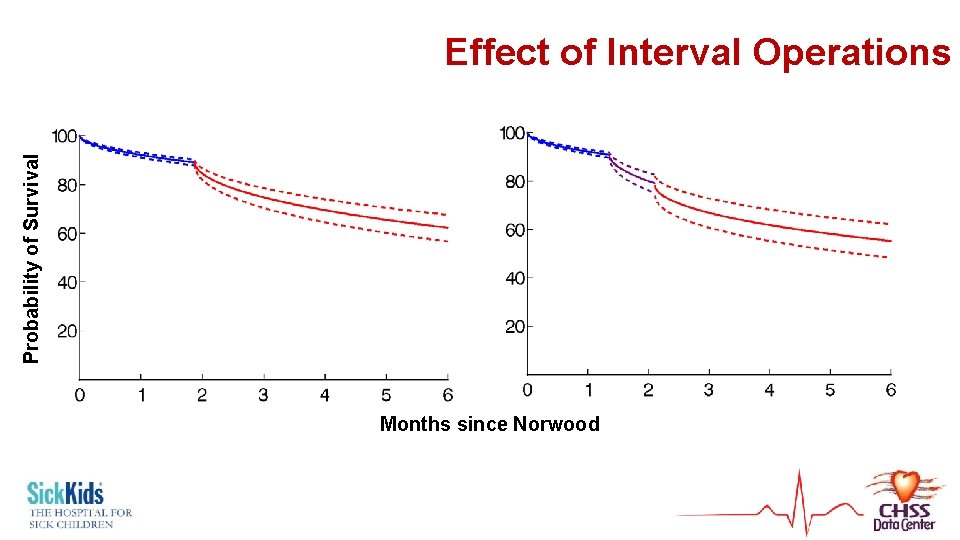
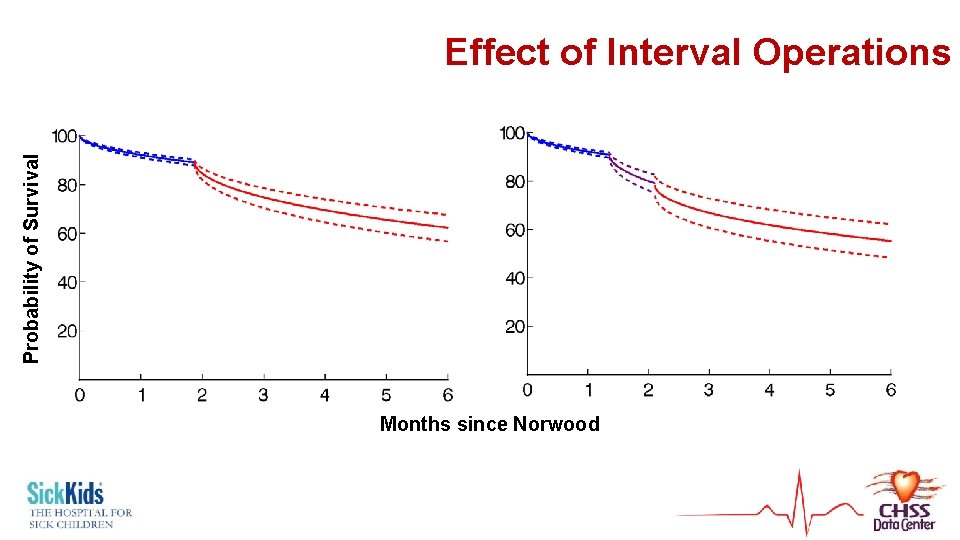
Probability of Survival Effect of Interval Operations Months since Norwood
Discussion, Implications, Conclusions
Low- and Average-Risk Patients • After 3 -4 months and z-score > -2 for low and average risk patients • “Elective” • Patients are progressing early/being delayed for no reason § Younger age – risk factor § Converting some from elective non-elective? § Outgrowing shunts? Waiting for shunt complications
High-Risk Patients • Survival is substantially reduced • A high risk patient at Norwood doesn’t become a better candidate after S 2 P (survival cost still seen) • Very poor survival with “early” S 2 P or low WAZ • No weight-for-age z-score, just like no age “maximizes” survival in these patients • Heart transplantation may maximize survival
Interval Procedures • Low threshold for catheter-based procedures • If facing a non-elective S 2 P with intervenable pathology (e. g. shunt stenosis), try to bridge to a later, elective S 2 P • Operative procedures confer greater risk • Don’t avoid doing • Marker of more severe pathology and higher risk

Implications • Survival through staged procedures should be considered across all, not as individual discrete intervals • Active plan can be developed or modified for planning timing of S 2 P • This info can help with prioritization of rare hearts from transplantation – have an idea of who will fail staged palliation

THANK YOU james. meza@sickkids. ca
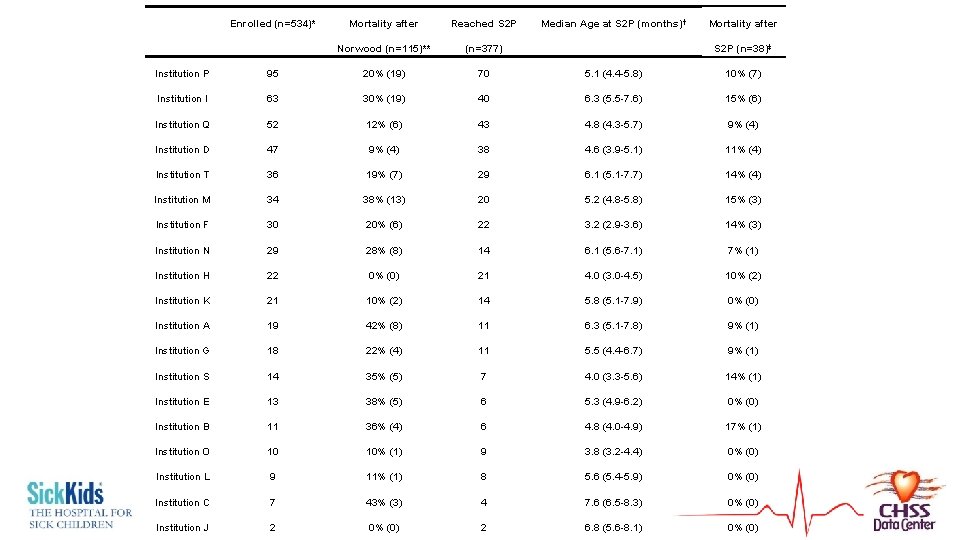
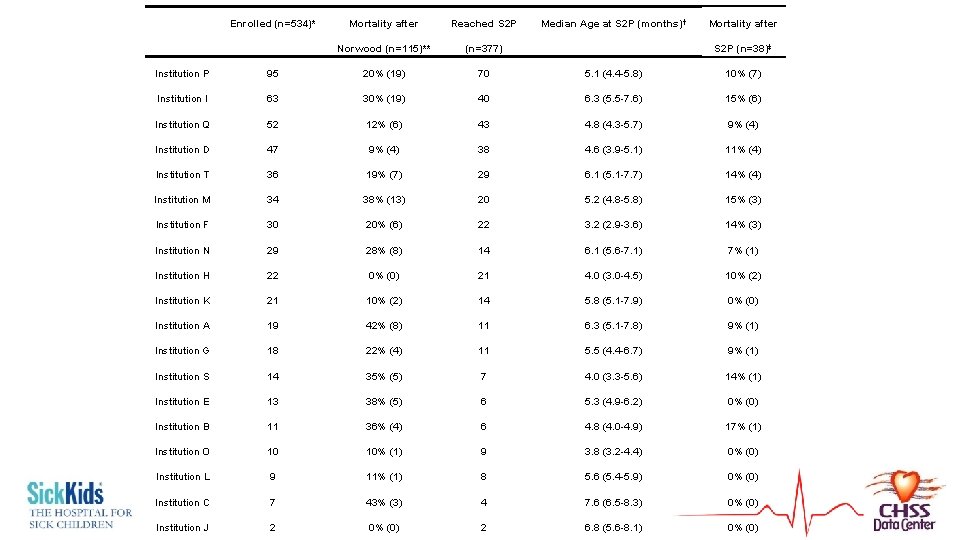
Enrolled (n=534)* Mortality after Reached S 2 P Norwood (n=115)** (n=377) Median Age at S 2 P (months)† Mortality after S 2 P (n=38)‡ Institution P 95 20% (19) 70 5. 1 (4. 4 -5. 8) 10% (7) Institution I 63 30% (19) 40 6. 3 (5. 5 -7. 6) 15% (6) Institution Q 52 12% (6) 43 4. 8 (4. 3 -5. 7) 9% (4) Institution D 47 9% (4) 38 4. 6 (3. 9 -5. 1) 11% (4) Institution T 36 19% (7) 29 6. 1 (5. 1 -7. 7) 14% (4) Institution M 34 38% (13) 20 5. 2 (4. 8 -5. 8) 15% (3) Institution F 30 20% (6) 22 3. 2 (2. 9 -3. 6) 14% (3) Institution N 29 28% (8) 14 6. 1 (5. 6 -7. 1) 7% (1) Institution H 22 0% (0) 21 4. 0 (3. 0 -4. 5) 10% (2) Institution K 21 10% (2) 14 5. 8 (5. 1 -7. 9) 0% (0) Institution A 19 42% (8) 11 6. 3 (5. 1 -7. 8) 9% (1) Institution G 18 22% (4) 11 5. 5 (4. 4 -6. 7) 9% (1) Institution S 14 35% (5) 7 4. 0 (3. 3 -5. 6) 14% (1) Institution E 13 38% (5) 6 5. 3 (4. 9 -6. 2) 0% (0) Institution B 11 36% (4) 6 4. 8 (4. 0 -4. 9) 17% (1) Institution O 10 10% (1) 9 3. 8 (3. 2 -4. 4) 0% (0) Institution L 9 11% (1) 8 5. 6 (5. 4 -5. 9) 0% (0) Institution C 7 43% (3) 4 7. 6 (6. 5 -8. 3) 0% (0) Institution J 2 0% (0) 2 6. 8 (5. 6 -8. 1) 0% (0)
 Landskursus palliation
Landskursus palliation Stage2 marketing
Stage2 marketing After me after me after me
After me after me after me John 14 1-3
John 14 1-3 Cost minimization formula
Cost minimization formula Optimal portfolio formula
Optimal portfolio formula Determining the optimal level of product availability
Determining the optimal level of product availability Optimal capital structure
Optimal capital structure Optimal driver launch angle and spin rate chart
Optimal driver launch angle and spin rate chart Optimal arousal theory
Optimal arousal theory Optimal theory
Optimal theory Servo pressure on jet ventilator
Servo pressure on jet ventilator Rumus miller orr
Rumus miller orr How about now
How about now An algorithm that returns near optimal solution is called
An algorithm that returns near optimal solution is called Optimal faktorkombinasjon
Optimal faktorkombinasjon Optimal temperature for enzymes
Optimal temperature for enzymes Optimal lung cancer pathway
Optimal lung cancer pathway Optimal challenge definition
Optimal challenge definition Optimal theory
Optimal theory Fifo page replacement calculator
Fifo page replacement calculator Corrective tax
Corrective tax Optimal receiver
Optimal receiver Social optimum quantity
Social optimum quantity Penguin ppt
Penguin ppt Optimal health in each of the six components of health
Optimal health in each of the six components of health How to achieve optimal health and wellness
How to achieve optimal health and wellness Bayes optimal classifier python
Bayes optimal classifier python Optimal sim m
Optimal sim m Chapter 11 nutrition and diets
Chapter 11 nutrition and diets Linear quadratic regulator example
Linear quadratic regulator example Performance-optimal read-only transactions
Performance-optimal read-only transactions Optimal auctions through deep learning
Optimal auctions through deep learning Optimal binary search tree java
Optimal binary search tree java Optimal boshqarish
Optimal boshqarish Optimal financing mix
Optimal financing mix Socially optimal level
Socially optimal level Contoh soal analisis sensitivitas program linear
Contoh soal analisis sensitivitas program linear Optimal confidence
Optimal confidence Production units have an optimal rate of output where
Production units have an optimal rate of output where Eurobond market structure
Eurobond market structure Optimal inventory level
Optimal inventory level Channel capacity planning
Channel capacity planning American career college optimal resume
American career college optimal resume Enzyme molecule
Enzyme molecule Optimal transport
Optimal transport Kriteria greedy
Kriteria greedy Optimal binary search tree
Optimal binary search tree Fredrik rusek
Fredrik rusek Contoh portofolio optimal
Contoh portofolio optimal What is optimal policy in reinforcement learning
What is optimal policy in reinforcement learning Panier optimal
Panier optimal Optimum arousal theory
Optimum arousal theory Ioslides
Ioslides Ordreomkostninger eksempler
Ordreomkostninger eksempler Difference between short hedge and long hedge
Difference between short hedge and long hedge Analisis post optimal
Analisis post optimal Optimal financing mix
Optimal financing mix Evolutionary theory of motivation
Evolutionary theory of motivation Optimal decisions in games in artificial intelligence
Optimal decisions in games in artificial intelligence Pareto optimal outcome
Pareto optimal outcome Optimal capital structure
Optimal capital structure Xxxyes
Xxxyes Optimal theory
Optimal theory Optimal choice
Optimal choice Product availability is a measure of
Product availability is a measure of How to calculate optimal capital structure
How to calculate optimal capital structure