The Integumentary System The Integumentary System The Skin
- Slides: 56
The Integumentary System
The Integumentary System The Skin 1. Name the tissue types composing the epidermis and dermis. 2. List the major layers of each and describe the functions of each layer. 3. Describe the factors that normally contribute to skin color. 4. Briefly describe how changes in skin color may be used as clinical signs of certain disease states.
The Integumentary System Appendages of the Skin 1. Compare the structure and locations of sweat and oil glands. Also compare the composition and functions of their secretions. 2. Compare and contrast eccrine and apocrine glands. 3. List the parts of a hair follicle and explain the function of each part. Also describe the functional relationship of arrector pili muscles to the hair follicle. 4. Name the regions of a hair and explain the basis of hair color. Describe the distribution, growth, replacement, and changing nature of hair during the life span. 5. Describe the structure of nails.
The Integumentary System Functions of the Integumentary System 1. Describe how the skin accomplishes at least five different functions. Homeostatic Imbalances of Skin 1. Summarize the characteristics of the three major types of skin cancers. 2. Explain why serious burns are life threatening. Describe how to determine the extent of a burn and differentiate first-, second-, and third -degree burns. Developmental Aspects of the Integumentary System 1. Describe and attempt to explain the causes of changes that occur in the skin from birth to old age.
• The skin and its derivatives (sweat and oil glands, hairs, and nails) make up a complex set of organs that serves several functions, mostly protective. Together, these organs form the integumentary system (in-teg″u-men′tar-e). The Skin • The skin covers the entire body, has a surface area of 1. 2 to 2. 2 square meters, weighs 4 to 5 kilograms (4– 5 kg = 9– 11 lb), and accounts for about 7% of total body weight in the average adult. • Also called the integument, which simply means “covering, ” the skin’s functions go well beyond serving as a large, opaque bag for the body contents. It is pliable yet tough, allowing it to take constant punishment from external agents. • Without our skin, we would quickly fall prey to bacteria and perish from water and heat loss.
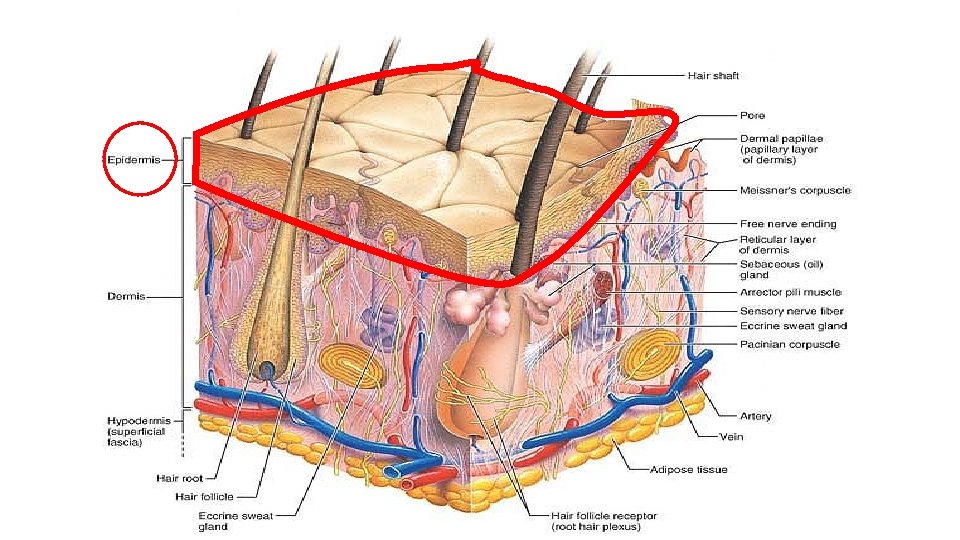
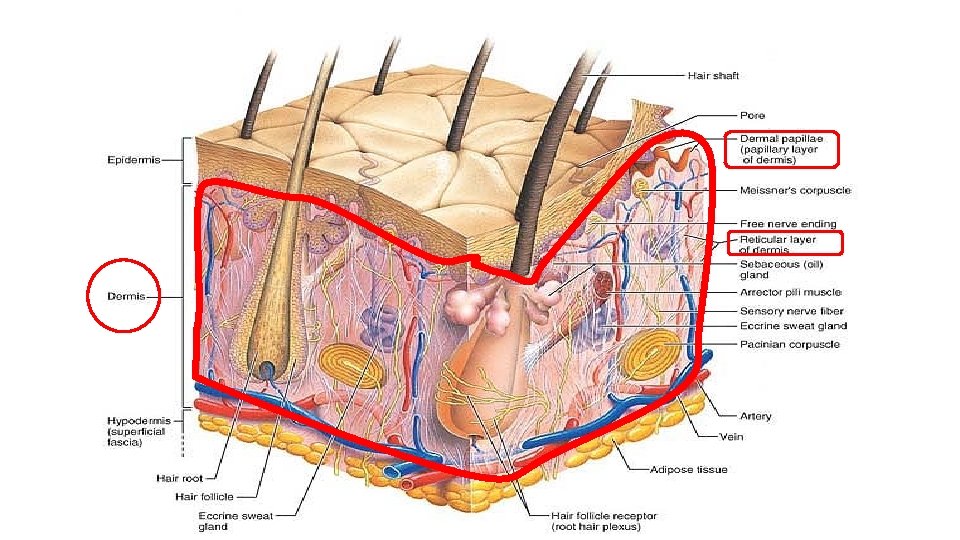
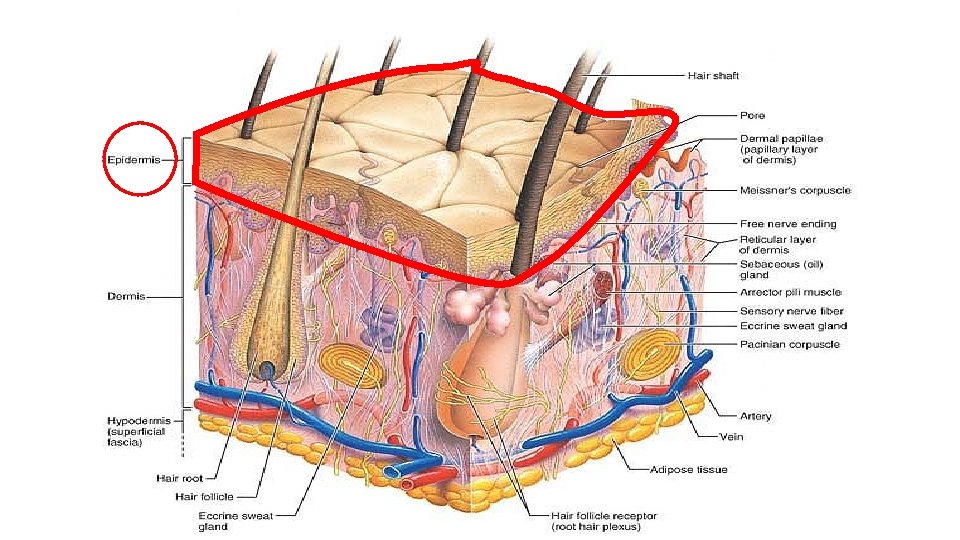
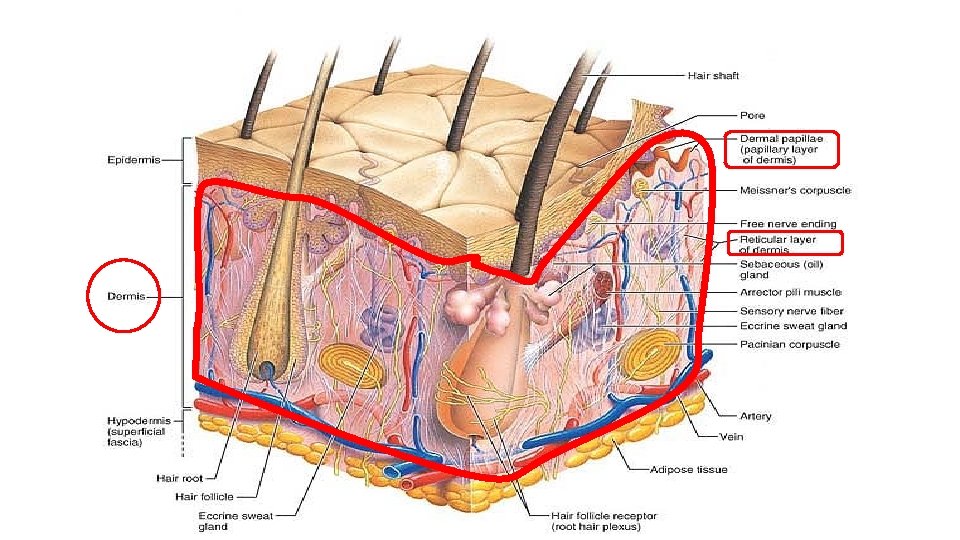
The Skin • The skin, which varies in thickness from 1. 5 to 4. 0 millimeters (mm) or more in different parts of the body, is composed of two distinct regions, the epidermis (ep″ ĭ-der′mis) and the dermis. • The epidermis (epi = upon), composed of epithelial cells, is the outermost protective shield of the body. • The underlying dermis, making up the bulk of the skin, is a tough, leathery layer composed of fibrous connective tissue. • Only the dermis is vascularized. • Nutrients reach the epidermis by diffusing through the tissue fluid from blood vessels in the dermis.
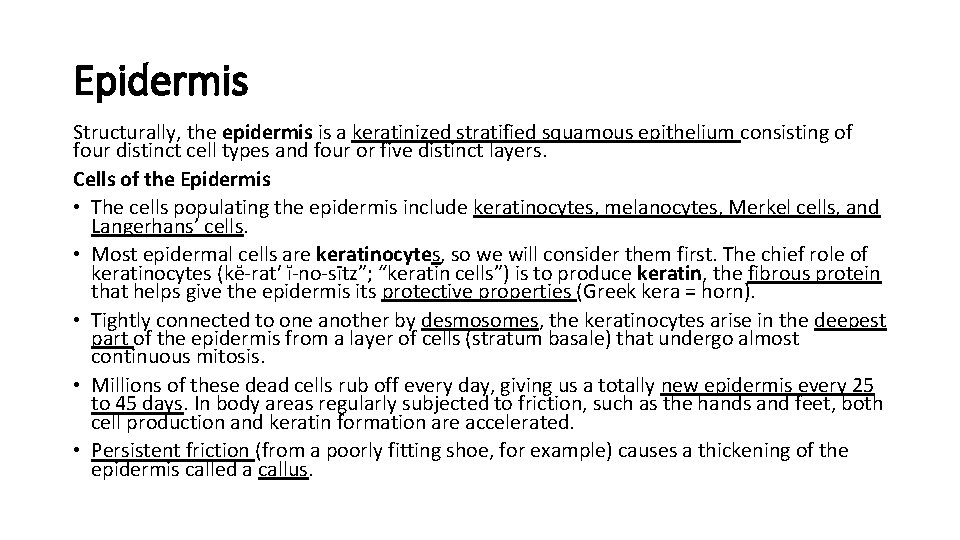
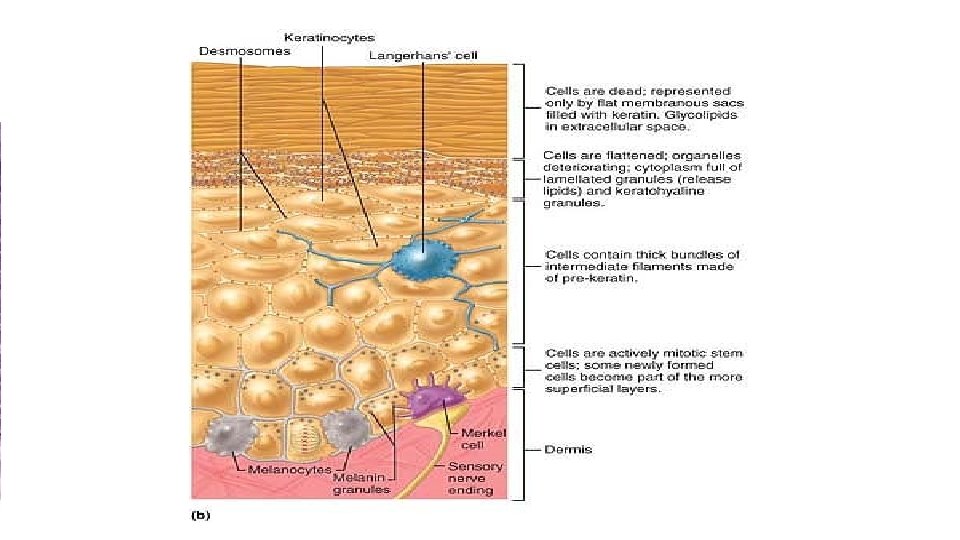
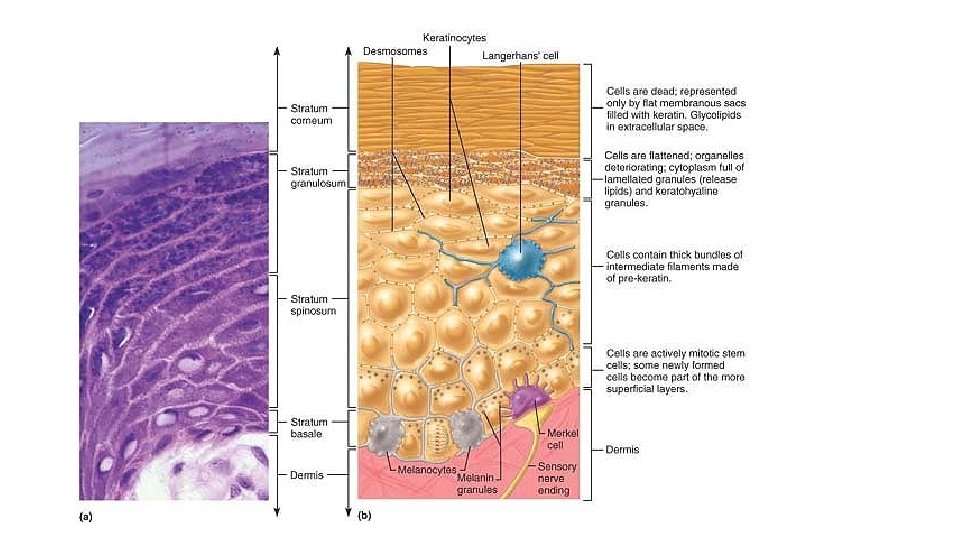
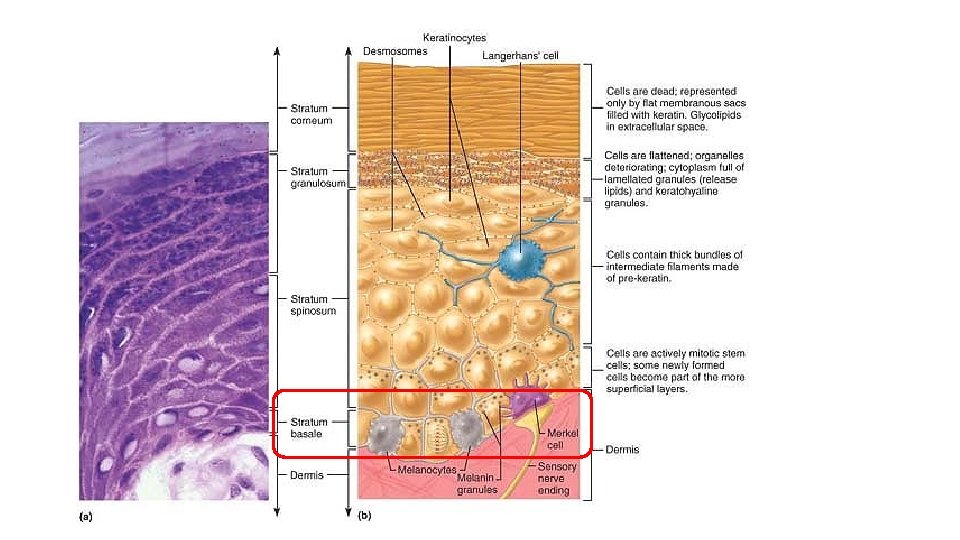
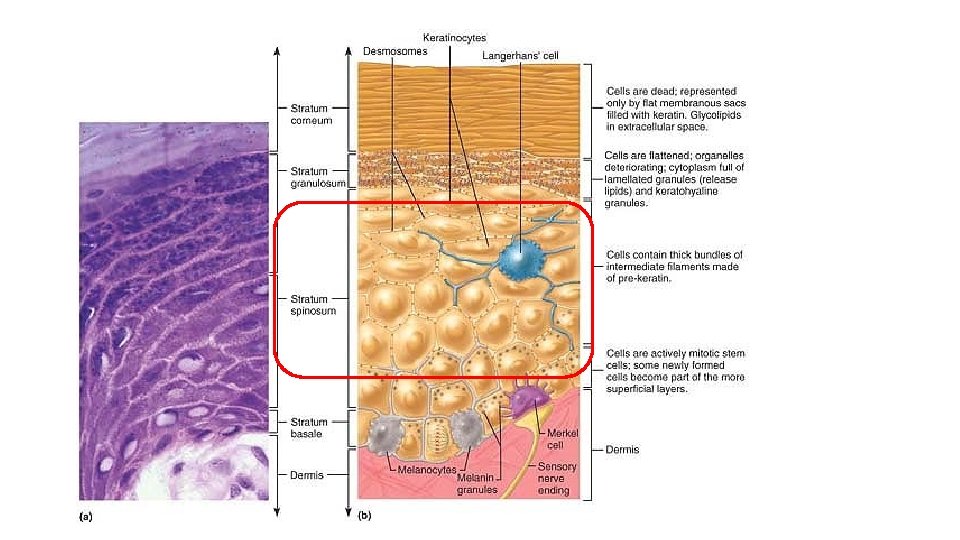
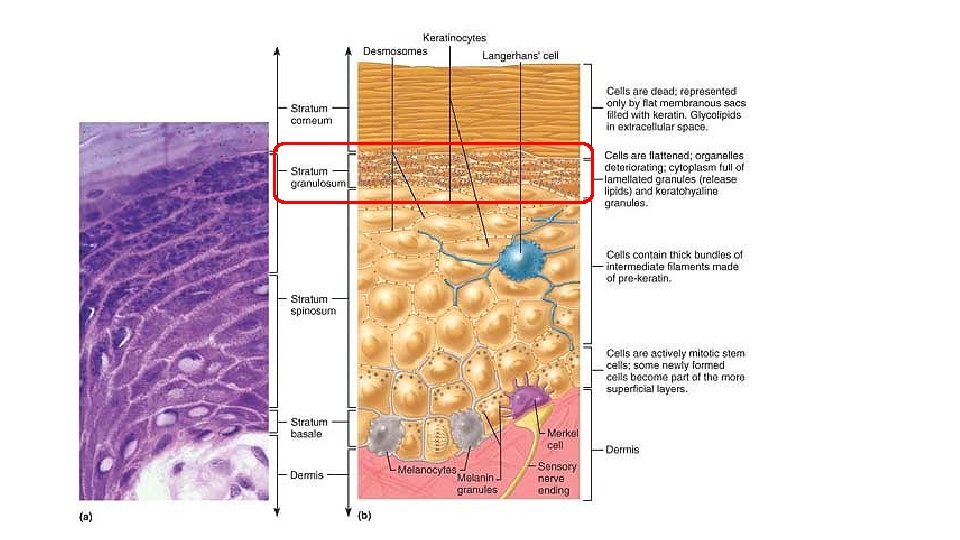
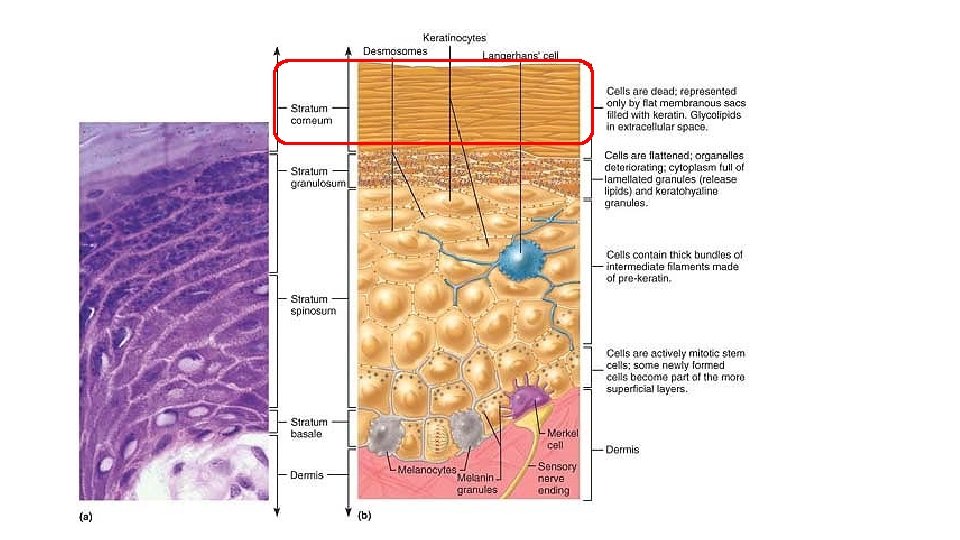
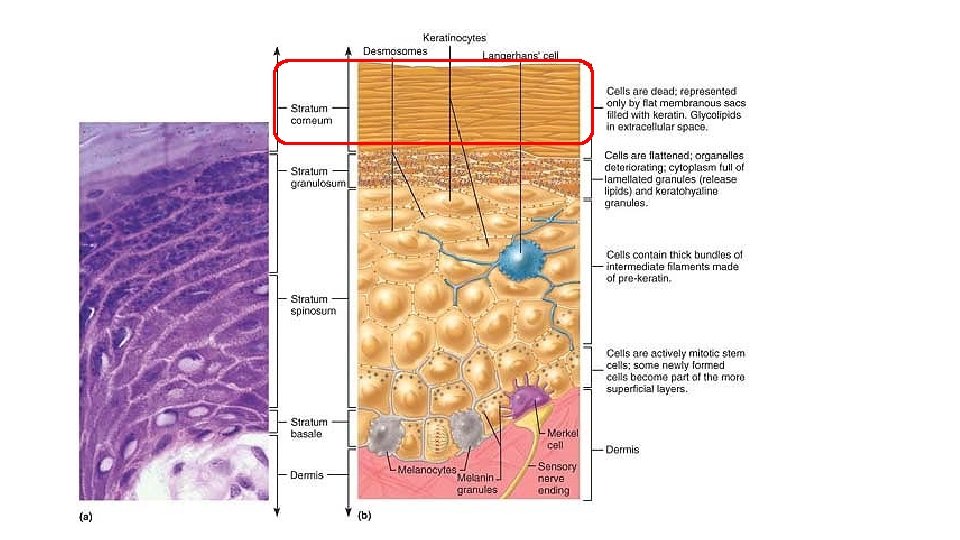
Epidermis Structurally, the epidermis is a keratinized stratified squamous epithelium consisting of four distinct cell types and four or five distinct layers. Cells of the Epidermis • The cells populating the epidermis include keratinocytes, melanocytes, Merkel cells, and Langerhans’ cells. • Most epidermal cells are keratinocytes, so we will consider them first. The chief role of keratinocytes (kĕ-rat′ ĭ-no-sītz”; “keratin cells”) is to produce keratin, the fibrous protein that helps give the epidermis its protective properties (Greek kera = horn). • Tightly connected to one another by desmosomes, the keratinocytes arise in the deepest part of the epidermis from a layer of cells (stratum basale) that undergo almost continuous mitosis. • Millions of these dead cells rub off every day, giving us a totally new epidermis every 25 to 45 days. In body areas regularly subjected to friction, such as the hands and feet, both cell production and keratin formation are accelerated. • Persistent friction (from a poorly fitting shoe, for example) causes a thickening of the epidermis called a callus.
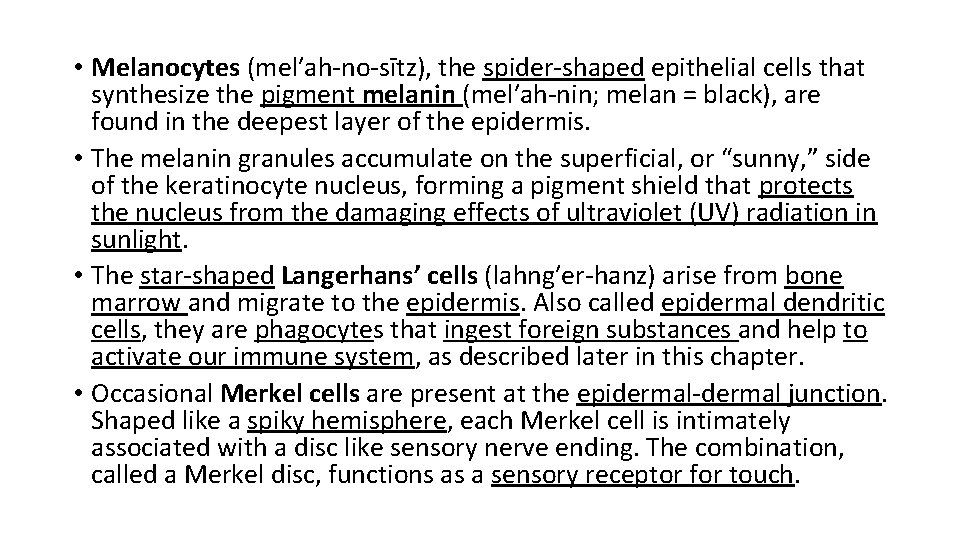
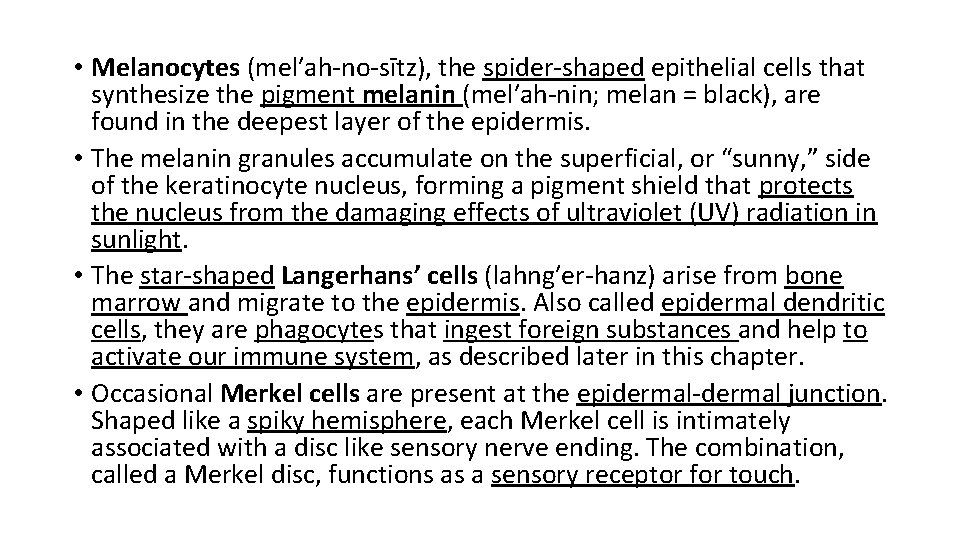
• Melanocytes (mel′ah-no-sītz), the spider-shaped epithelial cells that synthesize the pigment melanin (mel′ah-nin; melan = black), are found in the deepest layer of the epidermis. • The melanin granules accumulate on the superficial, or “sunny, ” side of the keratinocyte nucleus, forming a pigment shield that protects the nucleus from the damaging effects of ultraviolet (UV) radiation in sunlight. • The star-shaped Langerhans’ cells (lahng′er-hanz) arise from bone marrow and migrate to the epidermis. Also called epidermal dendritic cells, they are phagocytes that ingest foreign substances and help to activate our immune system, as described later in this chapter. • Occasional Merkel cells are present at the epidermal-dermal junction. Shaped like a spiky hemisphere, each Merkel cell is intimately associated with a disc like sensory nerve ending. The combination, called a Merkel disc, functions as a sensory receptor for touch.
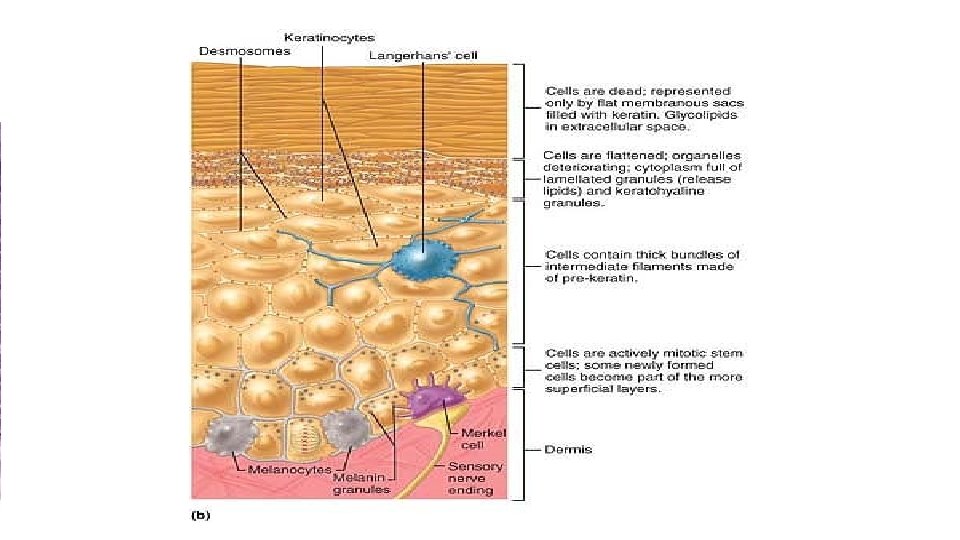
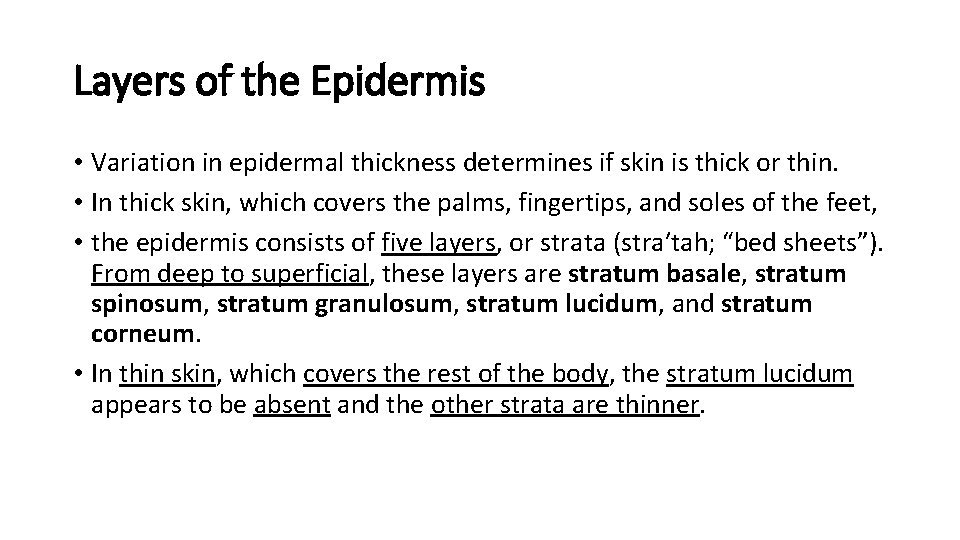
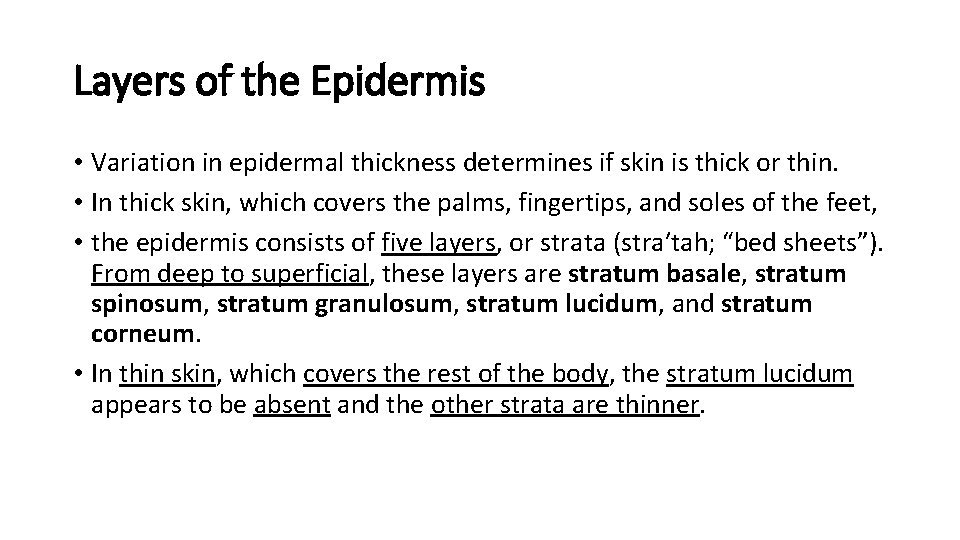
Layers of the Epidermis • Variation in epidermal thickness determines if skin is thick or thin. • In thick skin, which covers the palms, fingertips, and soles of the feet, • the epidermis consists of five layers, or strata (stra′tah; “bed sheets”). From deep to superficial, these layers are stratum basale, stratum spinosum, stratum granulosum, stratum lucidum, and stratum corneum. • In thin skin, which covers the rest of the body, the stratum lucidum appears to be absent and the other strata are thinner.
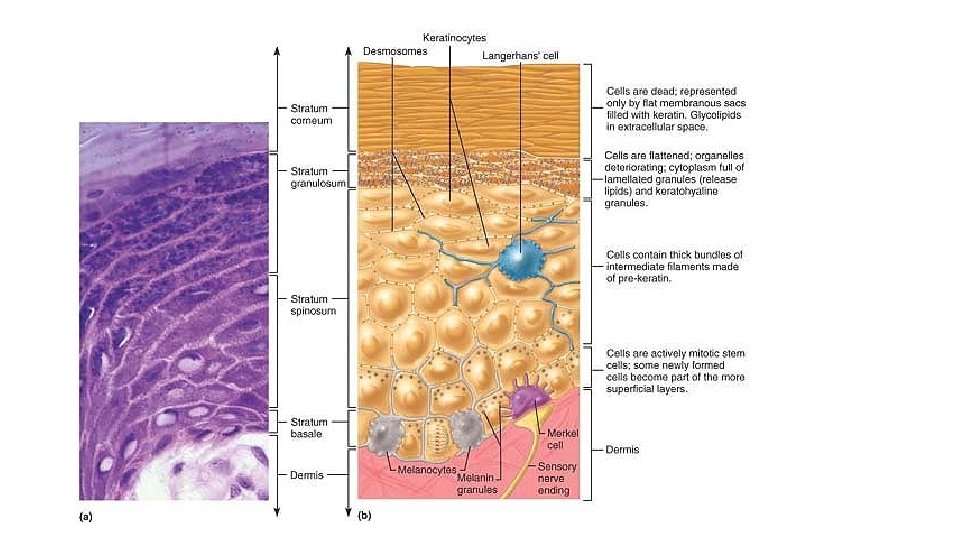
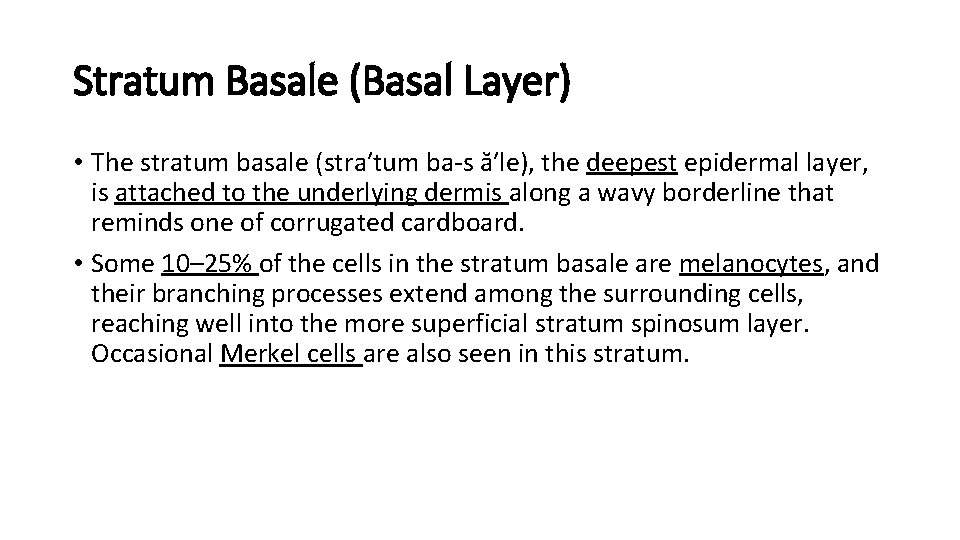
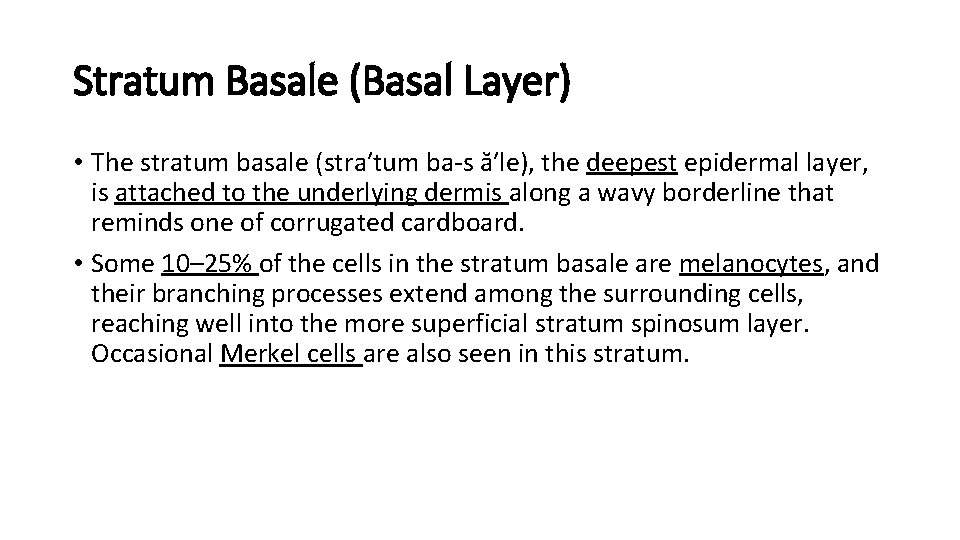
Stratum Basale (Basal Layer) • The stratum basale (stra′tum ba-s ă′le), the deepest epidermal layer, is attached to the underlying dermis along a wavy borderline that reminds one of corrugated cardboard. • Some 10– 25% of the cells in the stratum basale are melanocytes, and their branching processes extend among the surrounding cells, reaching well into the more superficial stratum spinosum layer. Occasional Merkel cells are also seen in this stratum.
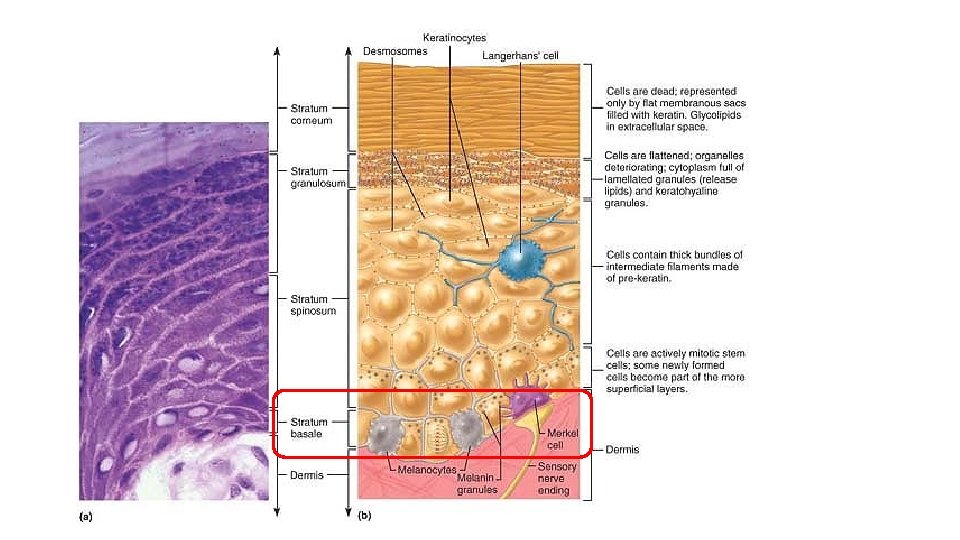
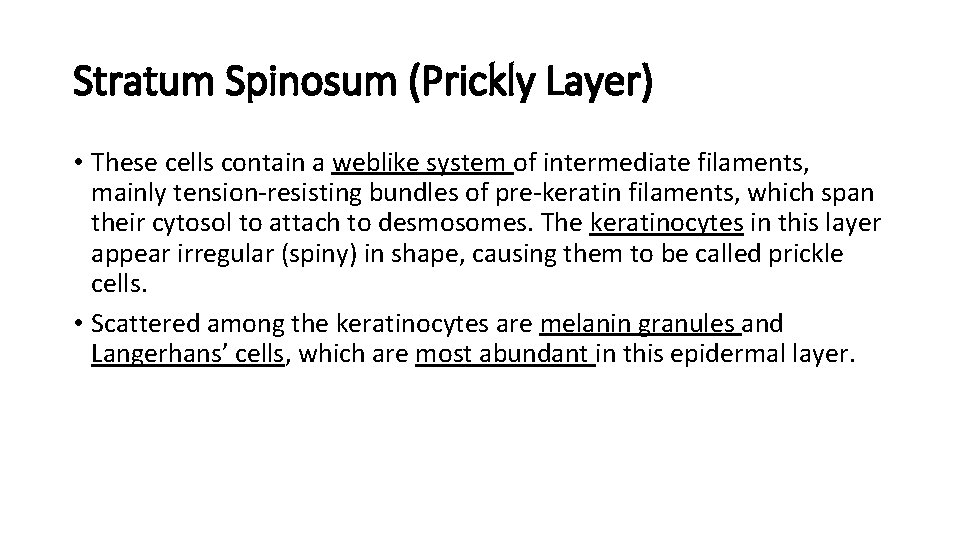
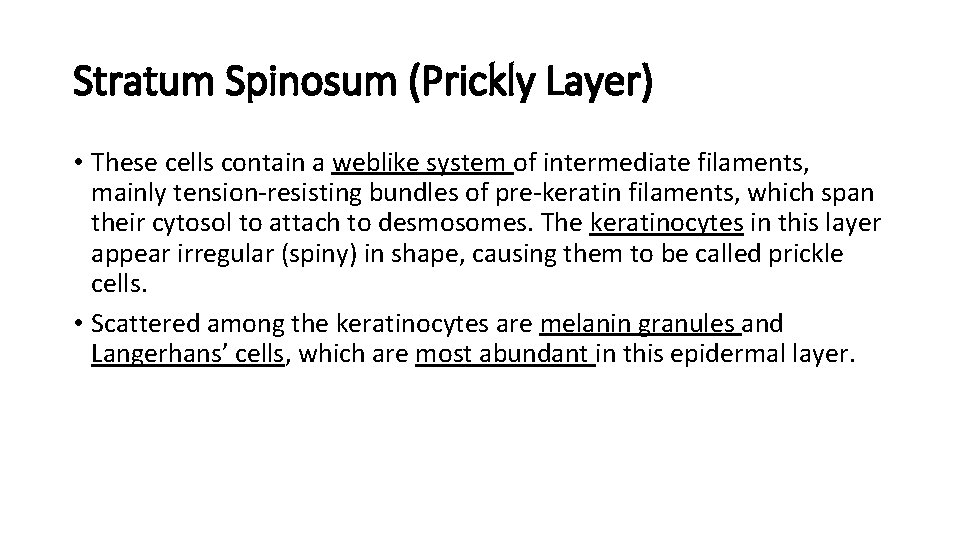
Stratum Spinosum (Prickly Layer) • These cells contain a weblike system of intermediate filaments, mainly tension-resisting bundles of pre-keratin filaments, which span their cytosol to attach to desmosomes. The keratinocytes in this layer appear irregular (spiny) in shape, causing them to be called prickle cells. • Scattered among the keratinocytes are melanin granules and Langerhans’ cells, which are most abundant in this epidermal layer.
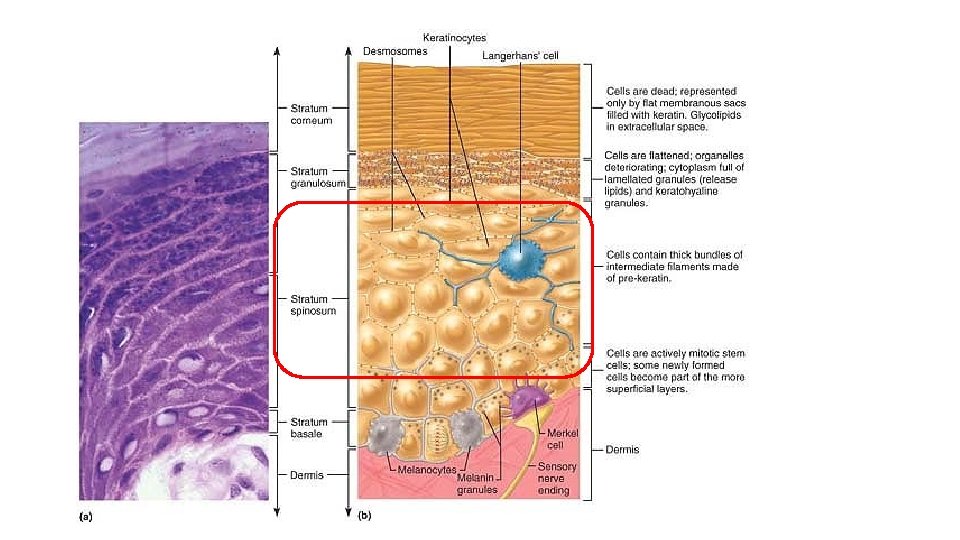
Stratum Granulosum (Granular Layer) • The thin stratum granulosum (gran″u-lo′sum) consists of three to five cell layers in which keratinocyte appearance changes drastically. • This makes them more resistant to destruction, so you might say that the keratinocytes are “toughening up” to make the outer strata the strongest skin region.
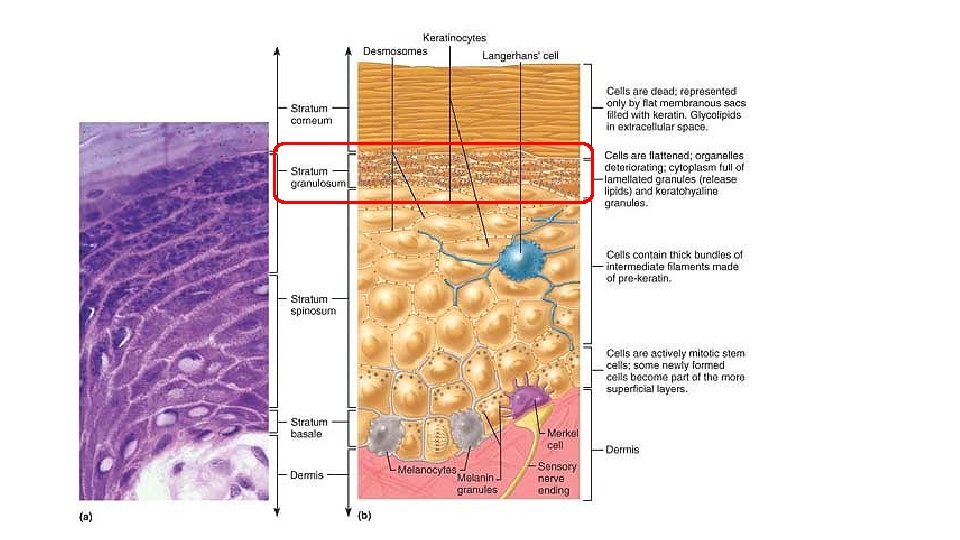
Stratum Lucidum (Clear Layer) • Through the light microscope, the stratum lucidum (loo′sid-um; “light”) appears as a thin translucent band just above the stratum granulosum. • As mentioned before, the stratum lucidum is visible only in thick skin.
Stratum Corneum (Horny Layer) • The outermost stratum corneum (kor′ne-um). • Keratin and the thickened plasma membranes of cells in this stratum protect the skin against abrasion and penetration, and the glycolipid between its cells waterproofs this layer. • Hence, the stratum corneum provides a durable “overcoat” for the body, protecting deeper cells from the hostile external environment (air) and from water loss, and rendering the body relatively insensitive to biological, chemical, and physical assaults. • It is amazing that a layer of dead cells can still play so many roles. • The shingle-like cell remnants of the stratum corneum are referred to as cornified, or horny, cells (cornu = horn). They are familiar to everyone as the dandruff shed from the scalp and the flakes that slough off dry skin.
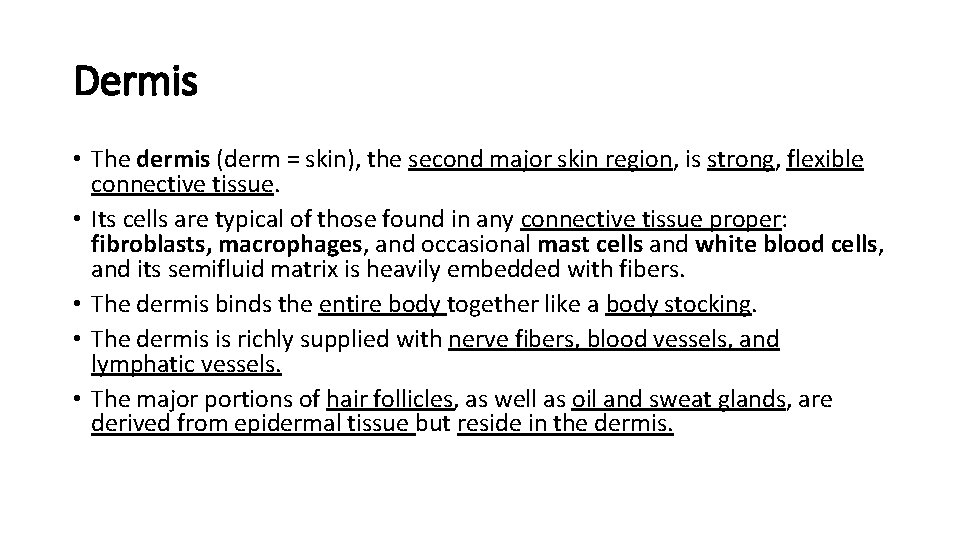
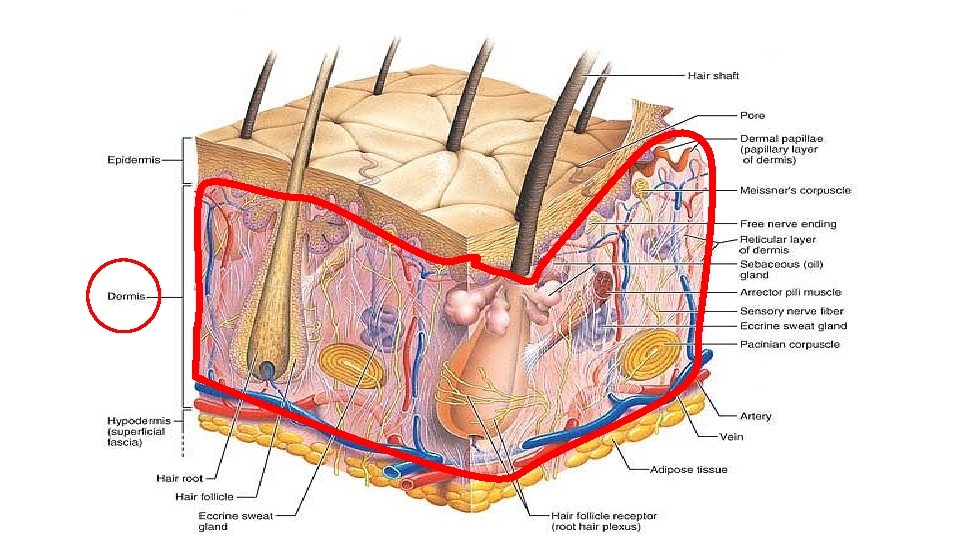
Dermis • The dermis (derm = skin), the second major skin region, is strong, flexible connective tissue. • Its cells are typical of those found in any connective tissue proper: fibroblasts, macrophages, and occasional mast cells and white blood cells, and its semifluid matrix is heavily embedded with fibers. • The dermis binds the entire body together like a body stocking. • The dermis is richly supplied with nerve fibers, blood vessels, and lymphatic vessels. • The major portions of hair follicles, as well as oil and sweat glands, are derived from epidermal tissue but reside in the dermis.
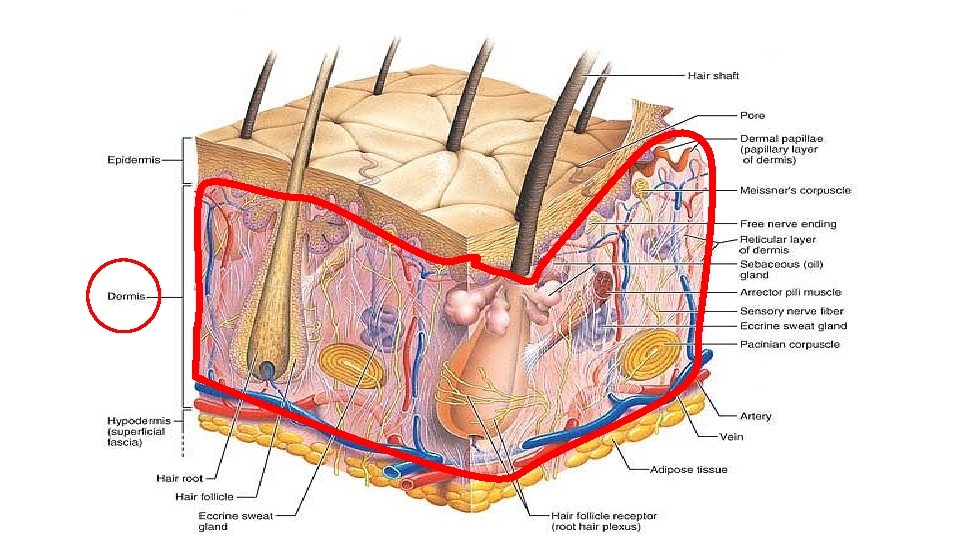
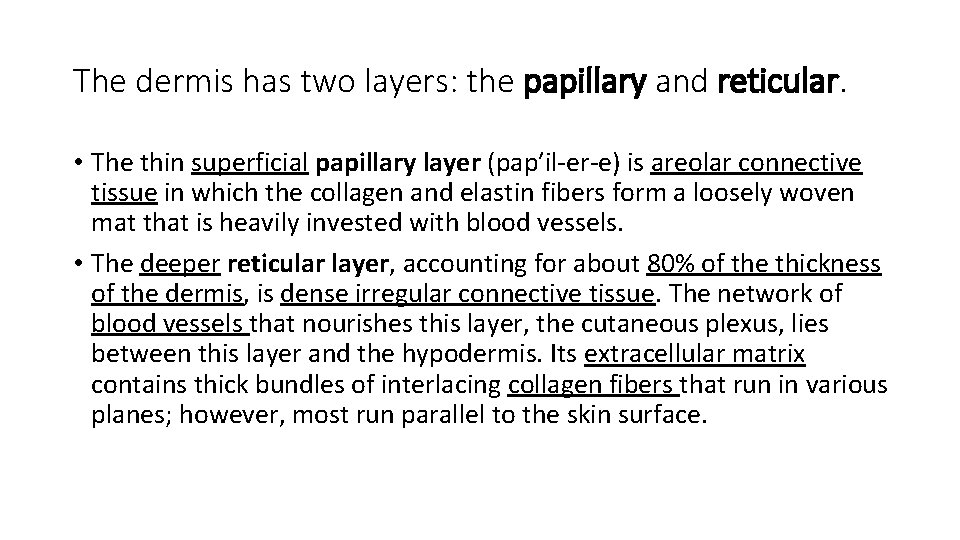
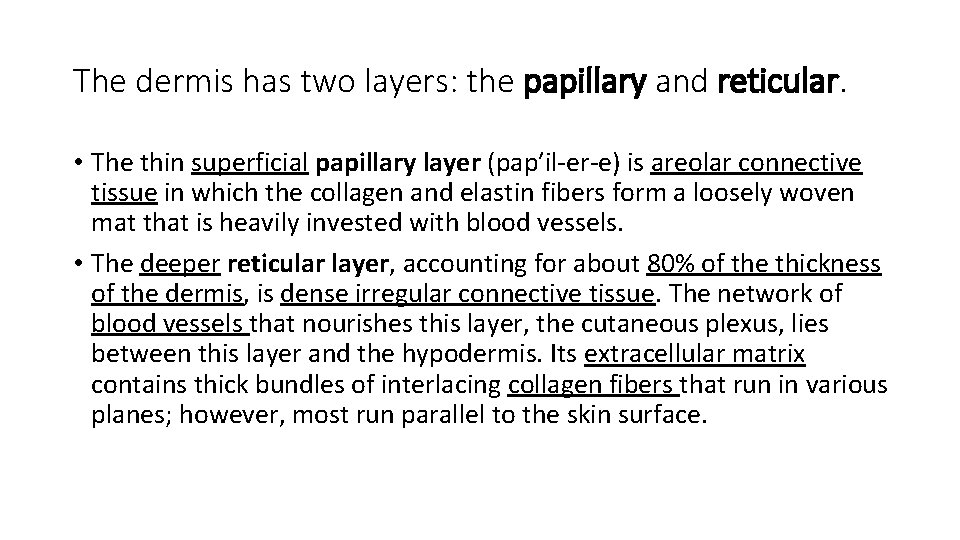
The dermis has two layers: the papillary and reticular. • The thin superficial papillary layer (pap′il-er-e) is areolar connective tissue in which the collagen and elastin fibers form a loosely woven mat that is heavily invested with blood vessels. • The deeper reticular layer, accounting for about 80% of the thickness of the dermis, is dense irregular connective tissue. The network of blood vessels that nourishes this layer, the cutaneous plexus, lies between this layer and the hypodermis. Its extracellular matrix contains thick bundles of interlacing collagen fibers that run in various planes; however, most run parallel to the skin surface.
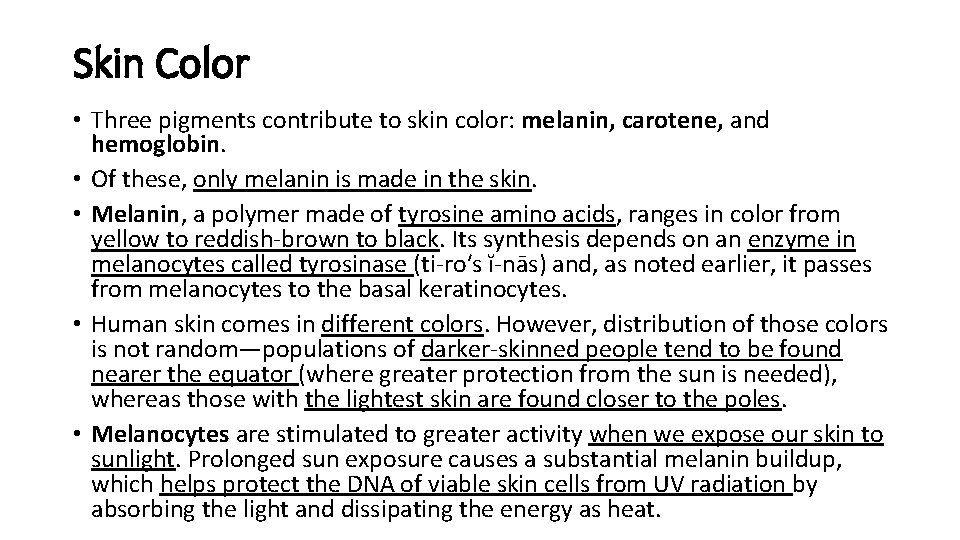
Skin Color • Three pigments contribute to skin color: melanin, carotene, and hemoglobin. • Of these, only melanin is made in the skin. • Melanin, a polymer made of tyrosine amino acids, ranges in color from yellow to reddish-brown to black. Its synthesis depends on an enzyme in melanocytes called tyrosinase (ti-ro′s ĭ-nās) and, as noted earlier, it passes from melanocytes to the basal keratinocytes. • Human skin comes in different colors. However, distribution of those colors is not random—populations of darker-skinned people tend to be found nearer the equator (where greater protection from the sun is needed), whereas those with the lightest skin are found closer to the poles. • Melanocytes are stimulated to greater activity when we expose our skin to sunlight. Prolonged sun exposure causes a substantial melanin buildup, which helps protect the DNA of viable skin cells from UV radiation by absorbing the light and dissipating the energy as heat.
Sub-Chapter Test
Appendages of the Skin • Along with the skin itself, the integumentary system includes several derivatives of the epidermis. • These skin appendages include the nails, sweat glands, sebaceous (oil) glands, and hair follicles and hair. • Each of these plays a unique role in maintaining body homeostasis.
Sweat (Sudoriferous) Glands • Sweat glands, also called sudoriferous glands (su″do-rif′er-us; sudor = sweat), are distributed over the entire skin surface except the nipples and parts of the external genitalia. • Their number is staggering — up to 3 million of them person. There are two types of sweat glands: eccrine and apocrine.
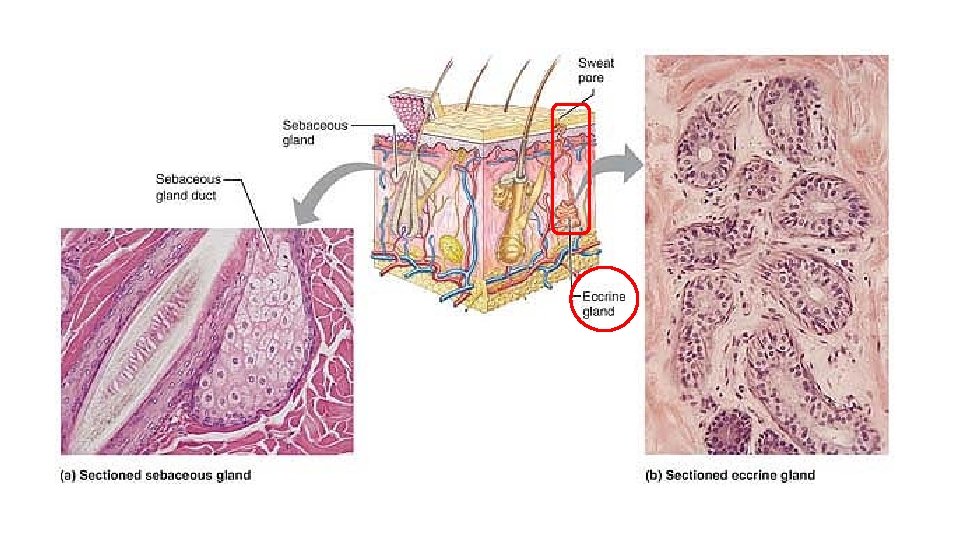
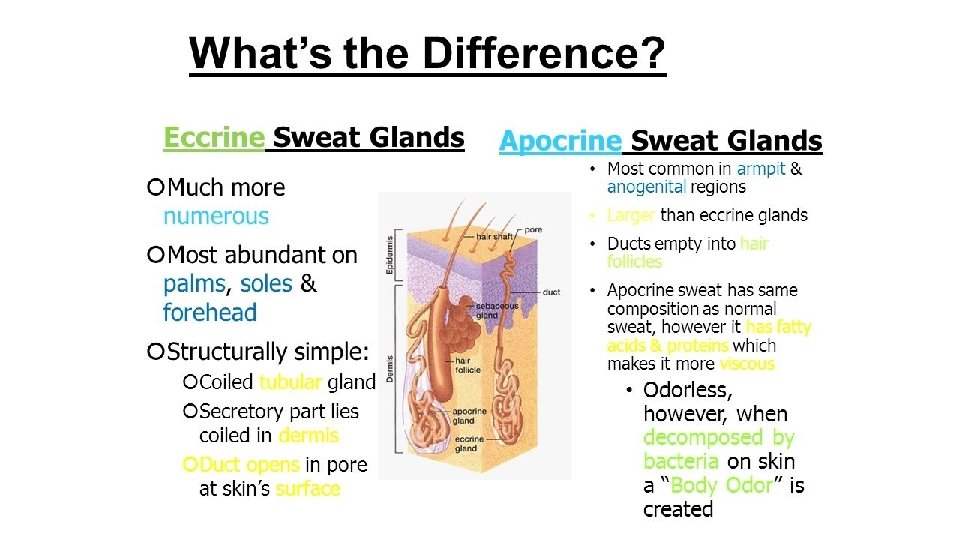
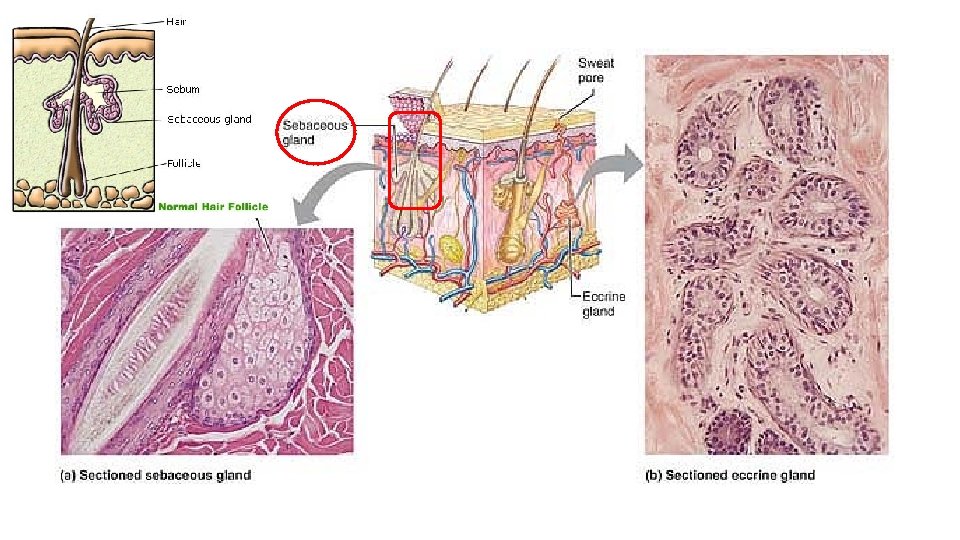
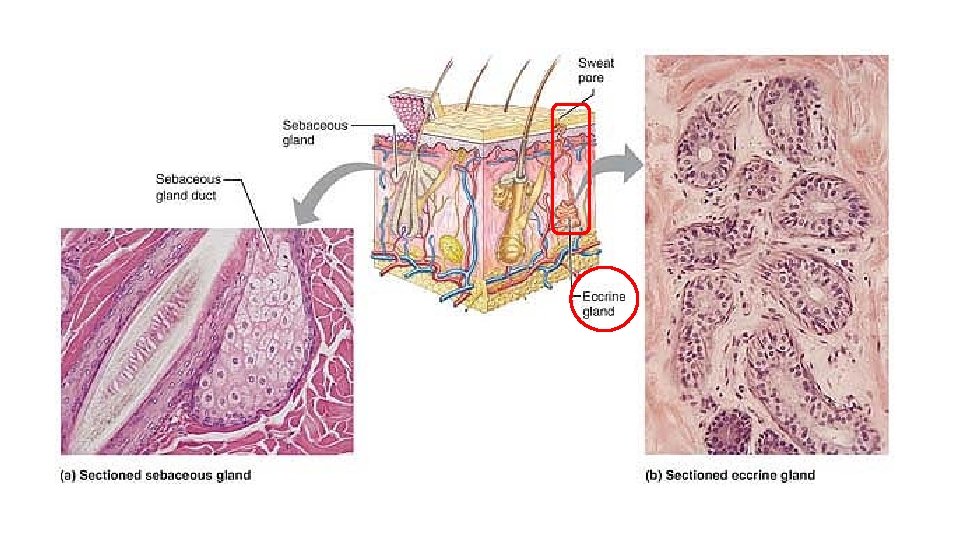
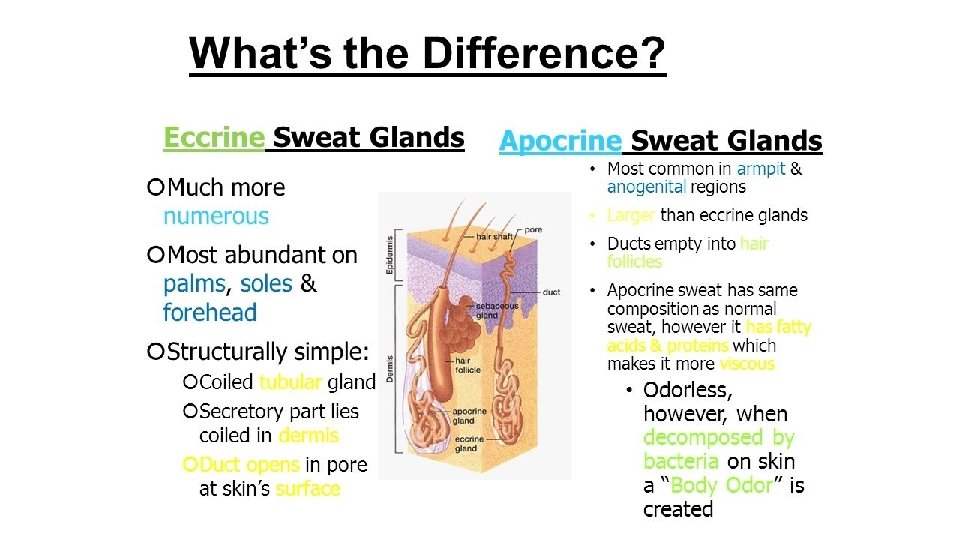
• Eccrine sweat glands (ek′rin; “secreting”), also called merocrine sweat glands, are far more numerous and are particularly abundant on the palms, soles of the feet, and forehead. • Each is a simple, coiled, tubular gland. The secretory part lies coiled in the dermis; the duct extends to open in a funnel-shaped pore (por = channel) at the skin surface. • Eccrine gland secretion, commonly called sweat, is a hypotonic filtrate of the blood that passes through the secretory cells of the sweat glands and is released by exocytosis. It is 99% water, with some salts (mostly sodium chloride), vitamin C, antibodies, a microbe-killing peptide dubbed dermicidin, and traces of metabolic wastes (urea, uric acid, and ammonia). • The exact composition depends on heredity and diet. Small amounts of ingested drugs may also be excreted by this route. Normally, sweat is acidic with a p. H between 4 and 6.
• Sweating is regulated by the sympathetic division of the autonomic nervous system, over which we have little control. • Its major role is to prevent overheating of the body. Heat-induced sweating begins on the forehead and then spreads inferiorly over the remainder of the body. • Emotionally induced sweating—the so-called “cold sweat” brought on by fright, embarrassment, or nervousness—begins on the palms, soles, and axillae (armpits) and then spreads to other body areas.
• Apocrine sweat glands * (ap′o-krin), approximately 2000 of them, are largely confined to the axillary and anogenital areas. • They are larger than eccrine glands, and their ducts empty into hair follicles. • Apocrine secretion contains the same basic components as true sweat, plus fatty substances and proteins. Consequently, it is quite viscous and sometimes has a milky or yellowish color. • The secretion is odorless, but when its organic molecules are decomposed by bacteria on the skin, it takes on a musky and generally unpleasant odor, the basis of body odor.
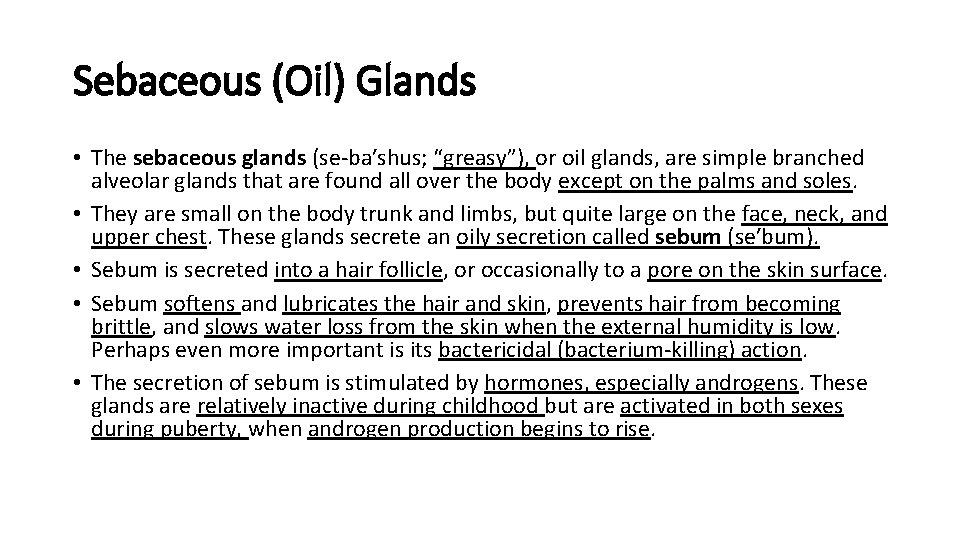
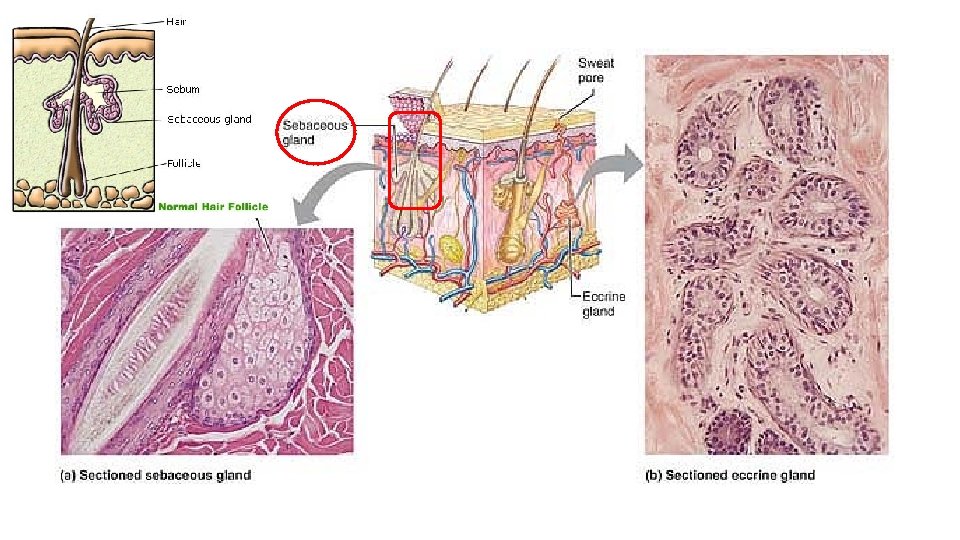
Sebaceous (Oil) Glands • The sebaceous glands (se-ba′shus; “greasy”), or oil glands, are simple branched alveolar glands that are found all over the body except on the palms and soles. • They are small on the body trunk and limbs, but quite large on the face, neck, and upper chest. These glands secrete an oily secretion called sebum (se′bum). • Sebum is secreted into a hair follicle, or occasionally to a pore on the skin surface. • Sebum softens and lubricates the hair and skin, prevents hair from becoming brittle, and slows water loss from the skin when the external humidity is low. Perhaps even more important is its bactericidal (bacterium-killing) action. • The secretion of sebum is stimulated by hormones, especially androgens. These glands are relatively inactive during childhood but are activated in both sexes during puberty, when androgen production begins to rise.
Hairs and Hair Follicles • Hair is an important part of our body image—consider, for example, the spiky hair style of punk rockers and the flowing, glossy manes of some high -fashion models. • Millions of hairs are distributed over our entire skin surface except our palms, soles, lips, nipples, and parts of the external genitalia (the head of the penis, for instance). • Although hair helps to keep other mammals warm, our sparse body hair is far less luxuriant and useful. Its main function in humans is to sense insects on the skin before they bite or sting us. • Hair on the scalp guards the head against physical trauma, heat loss, and sunlight. Eyelashes shield the eyes, and nose hairs filter large particles like lint and insects from the air we inhale.
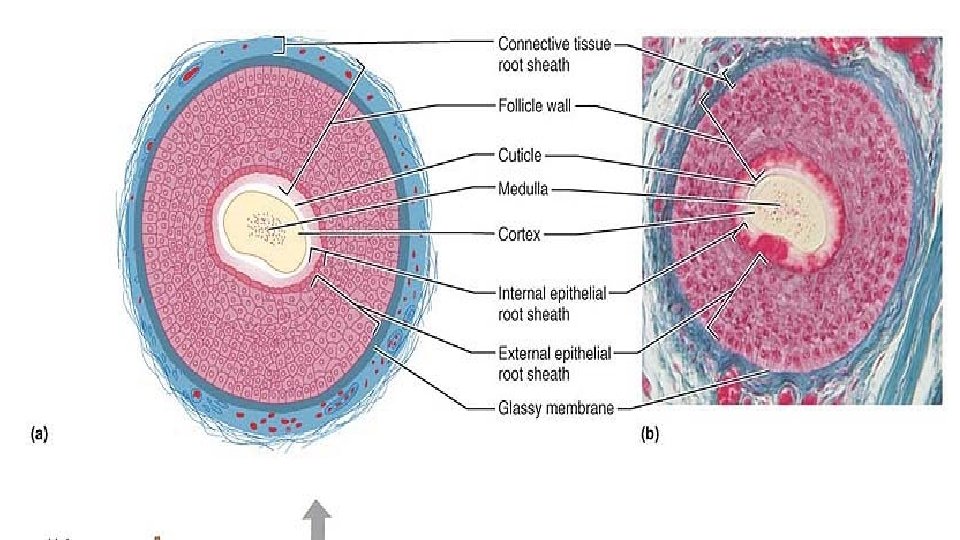
Structure of a Hair • Hairs, or pili (pi′li), are flexible strands produced by hair follicles and consist largely of dead, keratinized cells. • The hard keratin that dominates hairs and nails has two advantages over the soft keratin found in typical epidermal cells: (1) It is tougher and more durable, and (2) its individual cells do not flake off.
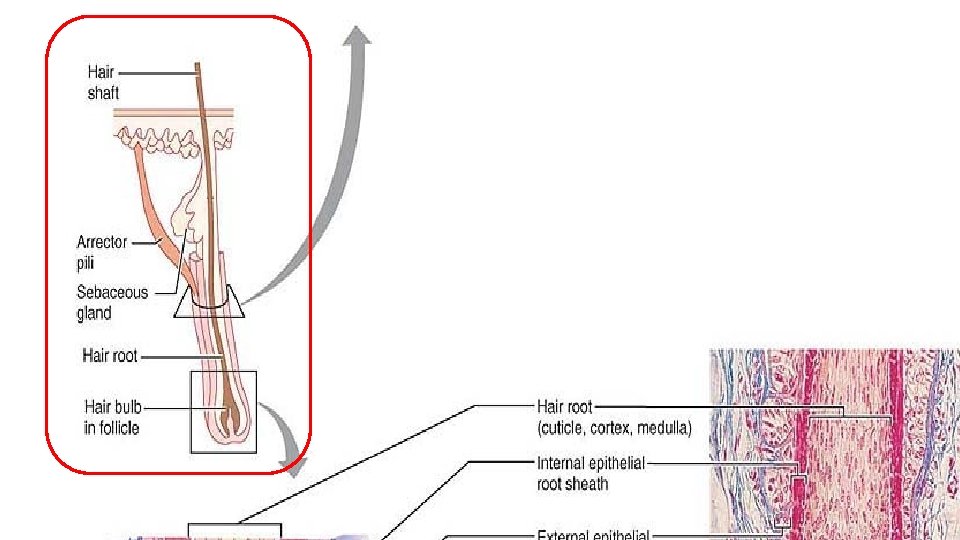
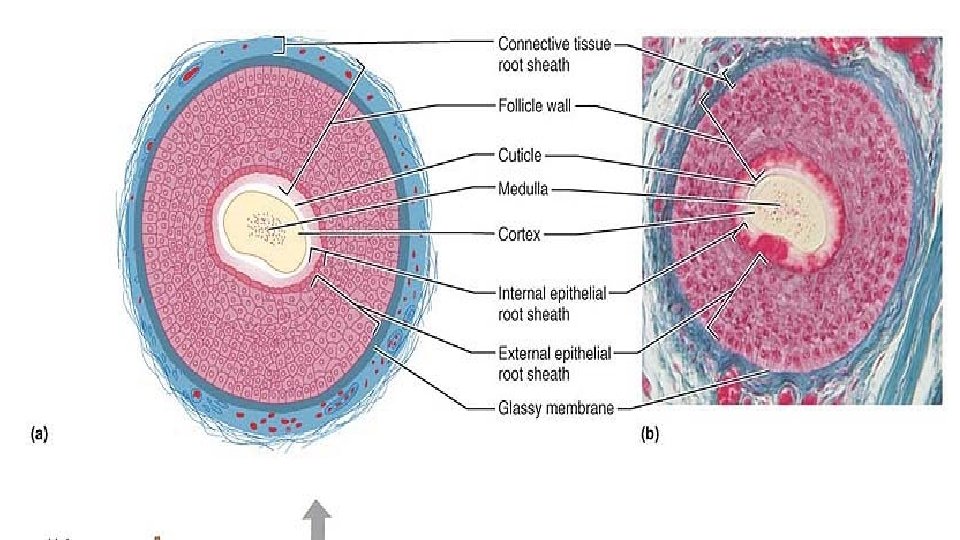
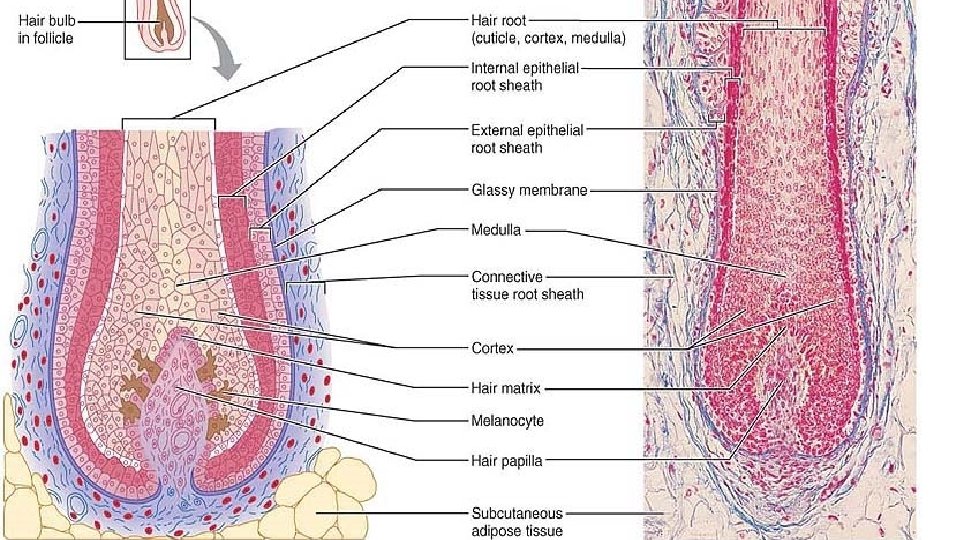
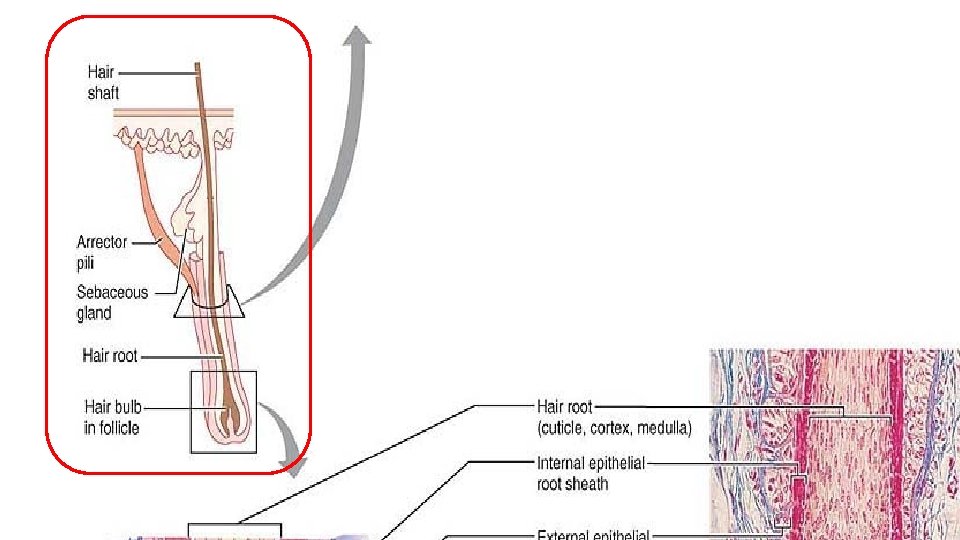
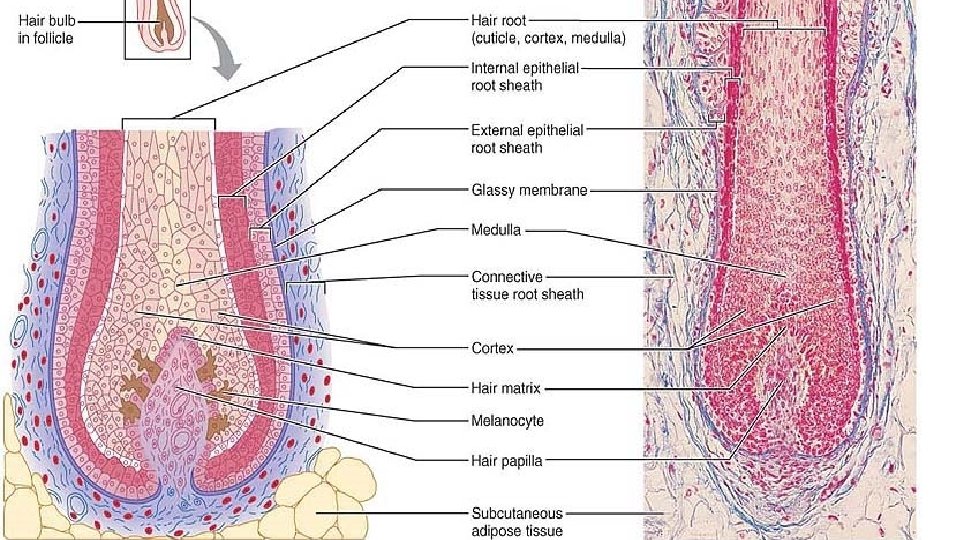
Structure of a Hair Follicle • Hair follicles (folli = bag) fold down from the epidermal surface into the dermis. In the scalp, they may even extend into the hypodermis. • The deep end of the follicle, located about 4 mm (1/6 in. ) below the skin surface, is expanded, forming a hair bulb. A knot of sensory nerve endings called a hair follicle receptor, or root hair plexus, wraps around each hair bulb, and bending the hair stimulates these endings. Consequently, our hairs act as sensitive touch receptors.
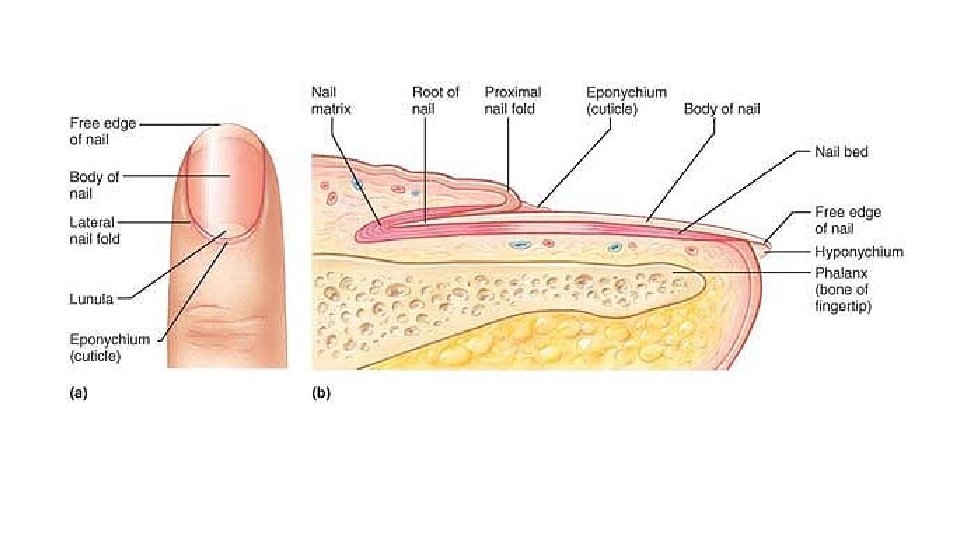
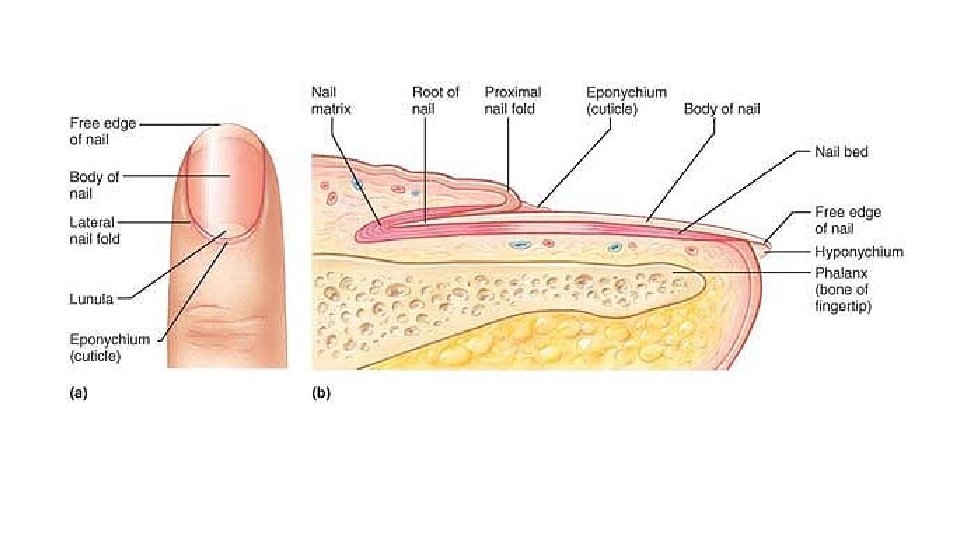
Nails • A nail is a scalelike modification of the epidermis that forms a clear protective covering on the dorsal surface of the distal part of a finger or toe. • Nails, which correspond to the hooves or claws of other animals, are particularly useful as “tools” to help pick up small objects and to scratch an itch. As noted, in contrast to soft keratin of the epidermis, nails contain hard keratin. • Each nail has a free edge, a body (visible attached portion), and a proximal root (embedded in the skin). The deeper layers of the epidermis extend beneath the nail as the nail bed; the nail itself corresponds to the superficial keratinized layers. • The thickened proximal portion of the nail bed, called the nail matrix, is responsible for nail growth.
• Nails normally appear pink because of the rich bed of capillaries in the underlying dermis. However, the region that lies over the thick nail matrix appears as a white crescent called the lunula (lu′nu-lah; “little moon”). • The proximal and lateral borders of the nail are overlapped by skin folds, called nail folds. The proximal nail fold projects onto the nail body as the cuticle or eponychium (ep″o-nik′e-um; “on the nail”). • The region beneath the free edge of the nail where dirt and debris tend to accumulate is the hyponychium (“below nail”), informally called the quick.
Sub-Chapter Test
Functions of the Integumentary System • The skin and its derivatives perform a variety of functions that affect body metabolism and prevent external factors from upsetting body homeostasis. • Given its superficial location it is our most vulnerable organ system, exposed to bacteria, abrasion, temperature extremes, and harmful chemicals.
Protection The skin constitutes at least three types of barriers: chemical, physical, and biological. üChemical Barriers • The chemical barriers include skin secretions and melanin. Although the skin’s surface teems with bacteria, the low p. H of skin secretions, or the so-called acid mantle, retards their multiplication. In addition, many bacteria are killed outright by bactericidal substances in sebum. • Skin cells also secrete a natural antibiotic called human defensin that literally punches holes in bacteria, making them look like sieves. • Wounded skin releases large quantities of protective peptides called cathelicidins that are particularly effective in preventing infection by group A streptococcus bacteria. • As discussed earlier, melanin provides a chemical pigment shield to prevent UV damage to the viable skin cells.
ü Physical/Mechanical Barriers • Physical, or mechanical, barriers are provided by the continuity of skin and the hardness of its keratinized cells. • As a physical barrier, the skin is a remarkable compromise. A thicker epidermis would be more impenetrable, but we would pay the price in loss of suppleness and agility. • The waterproofing glycolipids of the epidermis block the diffusion of water and water-soluble substances between cells, preventing both their loss from and entry into the body through the skin.
ü Biological Barriers • Biological barriers include the Langerhans’ (dendritic) cells of the epidermis, macrophages in the dermis, and DNA itself. • Langerhans’ cells are active elements of the immune system. For the immune response to be activated, the foreign substances, or antigens, must be presented to specialized white blood cells called lymphocytes. In the epidermis, it is the Langerhans’ cells that play this role. • Dermal macrophages constitute a second line of defense to dispose of viruses and bacteria that have managed to penetrate the epidermis. They, too, act as antigen “presenters. ” • Although melanin provides a fairly good chemical sunscreen, DNA itself is a remarkably effective biologically based sunscreen. Electrons in DNA molecules absorb UV radiation and transfer it to the atomic nuclei, which heat up and vibrate vigorously. However, since the heat dissipates to surrounding water molecules instantaneously, the DNA converts potentially destructive radiation into harmless heat.
Body Temperature Regulation • The body works best when its temperature remains within homeostatic limits. As long as the external temperature is lower than body temperature, the skin surface loses heat to the air and to cooler objects in its environment. • When body temperature rises, dermal blood vessels dilate and the sweat glands are stimulated into vigorous secretory activity. Evaporation of sweat from the skin surface dissipates body heat and efficiently cools the body, thus preventing overheating. • When the external environment is cold, dermal blood vessels constrict. This causes the warm blood to bypass the skin temporarily and allows skin temperature to drop to that of the external environment. Once this happened, passive heat loss from the body is slowed, thus conserving body heat.
Cutaneous Sensation • The skin is richly supplied with cutaneous sensory receptors, which are actually part of the nervous system. • The cutaneous receptors are classified as exteroceptors (ek″ster-osep′torz) because they respond to stimuli arising outside the body. • For example, Meissner’s corpuscles (in the dermal papillae) and Merkel discs allow us to become aware of a caress or the feel of our clothing against our skin, whereas Pacinian corpuscles (in the deeper dermis or hypodermis) alert us to bumps or contacts involving deep pressure. Hair follicle receptors report on wind blowing through our hair and a playful tug on a pigtail. • Painful stimuli (irritating chemicals, extreme heat or cold, and others) are sensed by free nerve endings that meander throughout the skin.
Metabolic Functions • When sunlight bombards the skin, modified cholesterol molecules circulating through dermal blood vessels are converted to a vitamin D precursor, and transported via the blood to other body areas to play various roles in calcium metabolism. For example, calcium cannot be absorbed from the digestive tract without vitamin D. • Besides synthesizing the vitamin D precursor, the epidermis has a host of other metabolic functions. • It makes chemical conversions that supplement those of the liver—for example, keratinocyte enzymes can “disarm” many cancer-causing chemicals that penetrate the epidermis; convert some harmless chemicals carcinogens, for instance, they can transform cortisone applied to irritated skin into hydrocortisone, a potent anti-inflammatory drug. • Skin cells also make several biologically important proteins, including collagenase, an enzyme that aids the natural turnover of collagen (and deters wrinkles).
Blood Reservoir • The dermal vascular supply is extensive and can hold large volumes of blood (about 5% of the body’s entire blood volume). • When other body organs, such as vigorously working muscles, need a greater blood supply, the nervous system constricts the dermal blood vessels. This shunts more blood into the general circulation, making it available to the muscles and other body organs.
Excretion • Limited amounts of nitrogen-containing wastes (ammonia, urea, and uric acid) are eliminated from the body in sweat, although most such wastes are excreted in urine. • Profuse sweating is an important avenue for water and salt (sodium chloride) loss.
Sub-Chapter Test