SYNCOPE Duka Glava Department of Cardiology University Hospital





- Slides: 36
SYNCOPE Duška Glavaš Department of Cardiology University Hospital Split
SYNCOPE • syncope (gr. sinkoptein-fall unconscious, fainting, passing out, . ) • Affected 3 -6/1000 people every year • 1 -3% of visitis to emergency unit • 1/3 medical students • More common in older and females
SYNCOPE-Differential diagnosis • Central nervous system ischaemia-inadequate supply of oxygenated blood in the brain, verebro-basilar insuff. • Vasovagal-response to “triggers” • Blood pressure-Orthostatic hypotension (movement from lying to standing position) • Cardiac • Other reasons
Disorders of consciousness: • a) b) c) There are three basic disorders: syncope nonsyncopal disorders of consciousness disorders that imitate disorders of consciousness
a) Syncopa • Syncope develope because of abrupt lowering of cardiac output, with cerebral ishaemia • Appearance is abrupt, duration short (~20 s), with complete recovery. Syncope is followed with hypotensia • Prodromal signs: dizziness, weakness, difficulties with vision, nausea, sweating, . • After syncope possibly is amnesia, cramps, incontinence • PRESINKOPA: existing of prodromal signs, without loss of consciousness
b) Nonsyncopal loss of consciousness • Cause is not general cerebral hypoperfusion • There are other mechanisms: epilepsy, hypoglicaemia, hypoxia, intoxication, .
c) Disorders that imitate loss of consciousness • Basically it is not loss of consciousness • Cardiovascular collapse: abrupt loss of circulation bacause of heart or peripheral vascular reasons; spondaneus recovery • Psychiatric disorders: hyperventilation syndrome, hysteria, catalepsy, drop attacks, .
Reflex syncope • VASOVAGAL: trigger is orthostatic reason • Ofen when somebody longer stay (in warm enviroment, . ) • Because of gravitation and filtration of fluid, 15 -20% volume is moved below diaphragm, results in ↓ vein inflow and stroke volume, with activation of reflex
Reflex syncope - SITUATIONAL: afferent arm of reflex is located in different organs (bladder, bowels, bronchi, central nerve system, during deglutition); painfull unpleasant stimulus - baroreceptor of sinus caroticus (carotid sinus syncope) - “triggers” shaving, moving of head, .
Carotid synus syncope • In healthy persons, pressure of sinus caroticus leads to ↓ heart rate and blood pressure • In older, sinus could be hypersensitive and develop bradicardia and hypotension • Term “Carotis synus syncope” we used for patients with abnormal replay to massage, and when patients have often symptoms (syncope, dizziness) provoked with “triggers” (tight collar)

Ortostatic syncope • Consequence of primary or secundary dysfunction of autonomic nerve system • Primary dysfunction-conseguence of degenerative neurologic disorders (Shy-Dragerov sy, Bradbury. Eglestonov sy), synkope without compensation mechanisms (as ↑puls), often progressive course, of disease, , . • Secundary-consequence of diabetic, alc, and other neuropathy, multiple sclerosis, drugs, .
Ortostatic hypotension • Hypovolemia have different reasons: • Ortostatic hypotension could be consequence of bleeding, diarrhae, vomitting, diuretics, sweating, . • Often after longer standing, after weight loss, in older and weaker persons, after sympatectomia, . • “Triggered” with endocrine disorders: hypoglicaemia, feocromocytoma, .

Cardiac syncope • Morgagni-Adams-Stokes syndrome: abrupt loss of consciousness because of interruption of circulation in the brain; block, seizures, distrubance of pulse and reapiration • asystolia of 10 s-unconsciousness; • 10 -40 s-cramps with apnea and cyanosis; • >5 min could be fattaly outcome
Cardiac syncope • Sick sinus syndrome (sy tachycardiabradicardia)-a synus node dysfunction, • Causing alternating tachycardia-bradycardia • Often there is a long pause asystole between heart beat
Cardiac syncope • Subclavian steal syndrome, arises from retrograde flow of blood in the vertebral artery or the internal thoracic artery, due to a proximal stenosis of subclavian artery • Various medications, such as beta-blockers may couse bradicardia and syncope
Cardiac syncope • Cardiac syncope are usually sudden (without prodromal sign) • Between attacks, patients usually fiiling good • the mean reasons of cardial syncopa are: arrhythmias and conduction disturbances (ventricular asystolia, AV block, VT, . )
Cardiac syncope • ARRHYTHMIAE (brady/tahy): sick sinus syndrome, AV block II/III degree, VT, PSVT, Sy WPW, longer/ shorter QT, Sy Brugade, drugs • HR<30/min, compansation is not enough for cerebral perfusion • HR>180/min diastole is to short for filling of ventricul • Other “triggers”: anaemia, ishaemua, valve disorders, CV insufficiency
Cardiac syncope • ARRHYTHMIAE (brady/tahy): sick sinus syndrome, AV block II/III degree, VT, PSVT, longer/ shorter QT, Sy Brugade, drugs • HR<30/min, compansation is not enough for cerebral perfusion • HR>180/min diastole is to short for filling of ventricul • Other “triggers”: anaemia, ishaemua, valve disorders, CV insufficiency

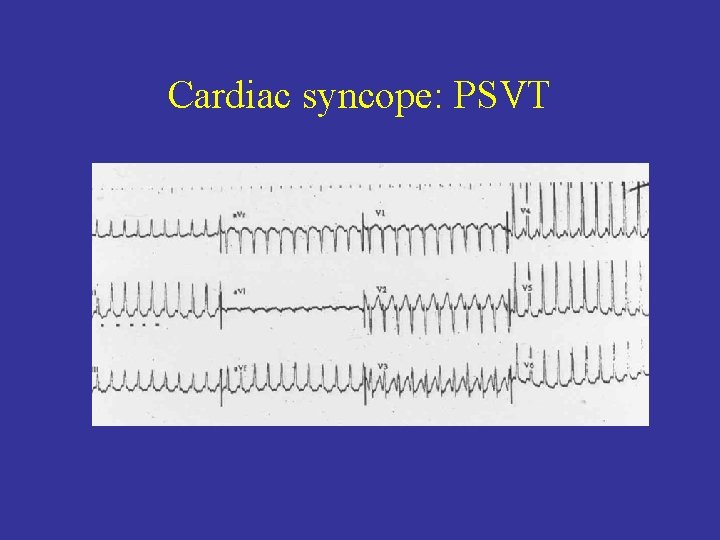
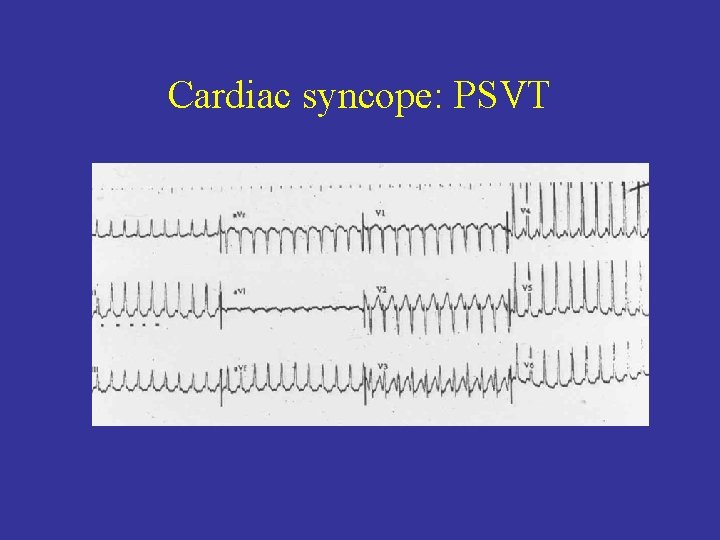
Cardiac syncope: PSVT
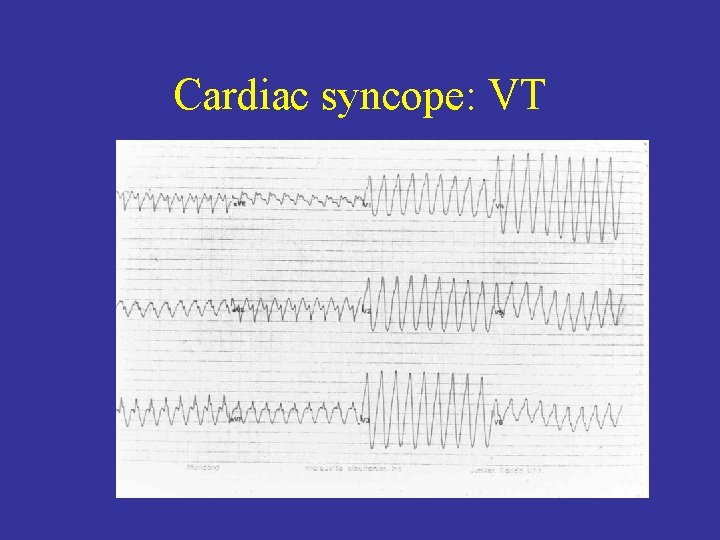
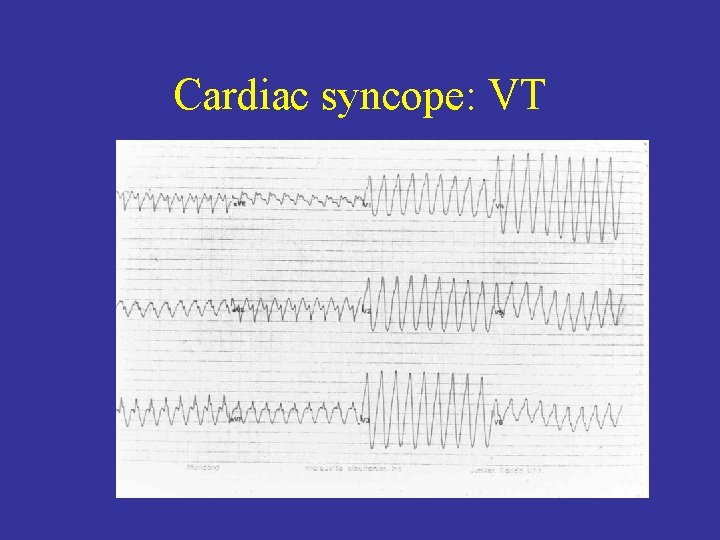
Cardiac syncope: VT
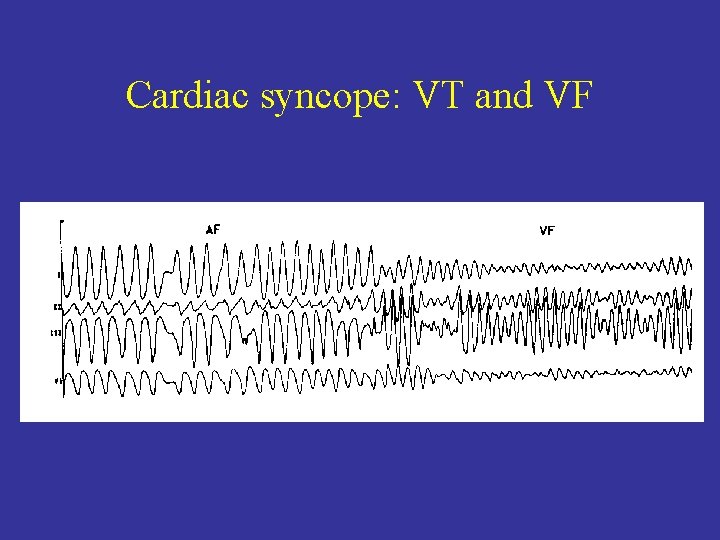
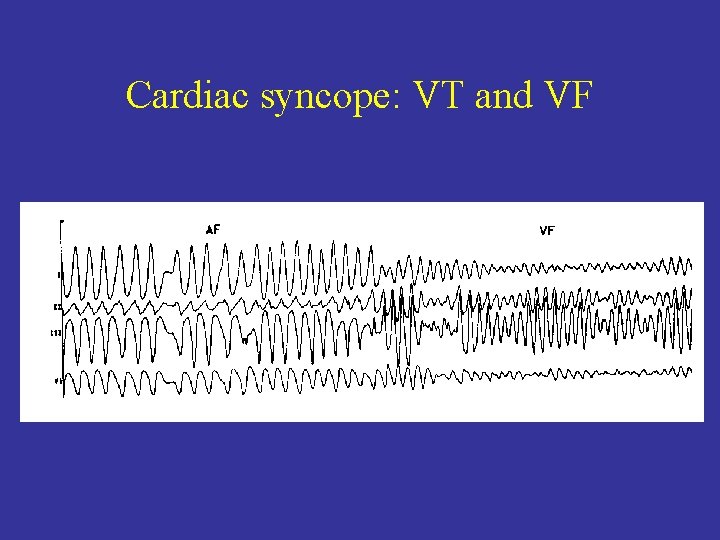
Cardiac syncope: VT and VF
Cardiac syncope • Structural heart disease: -stenotic valve disorders -opstructive cardiomyopathy, -acute coronary syndrome, -aortic dissection, pulmonary embolism, myxoma, tamponade, heart failure, .
Syncope-heart failure
Syncope-Aortic dissection
Cardiac syncope • Aortic stenosis is related with strain • Reasons: lower vascular resistance and lower stroke and minute volumen • Transient tachyarrhytmiae are often reasons for syncope in aortic stenosis • Ventricular asystolia is consequence of hypersensitive baroreceptors (aorta, LV)
Cardiac syncope • Aortic stenosis is related with strain • Reasons: lower vascular resistance and lower stroke and minute volumen • Transient tachyarrhytmiae are often reasons for syncope in aortic stenosis • Ventricular asystolia is consequence of hypersensitive baroreceptors (aorta, LV)
Cardiac syncope • intracardial formation could, dependent of moving of the body, stimulate syncope (myxoma) • syncope in mitral stenosis-related to embolism and tachyarrhythmiae • In primary pulmonary hypertension, mechanism is the same as in aortic stenosis • Syncope in Falloth tetralogy is related to strain (↑ R-L shant and artery hypoxia, with ↓ vascular resistance)
Diagnostic approach • Lab. tests: Hemoglobin count may indicate anemia; potassium, troponin, . • ECG: a. fibrillation, blocks, infraction, VT, . • For people with uncomplicated syncope with normal neurological exam, CT or MRI in not indicated • Carotid artery problems are unlikely to cause syncopa (ev. carotid ultrasound)
Diagnostic approach • Holter (24 h ECG monitoring)-portable ECG detect heart rhythms, arrhytmiae • Tilt table test: performed to elict orthostatic syncope secondary to auton. Dysfunction • Insertable cardiac monitor (loope recorder), to 28 -36 months, device continously monitors the rate and rhythm • San Francisco syncope rule-people with higher risk of serious reason(dilatative HF, .

Tretament: Vasovagal, orthostatic (hypotension) syncope • for returning blood to the brain-positioning the person on the ground, with legs elevated • or leaning forward and the head between the knees for at least 10 -15 min • cool and quiet place
Tretament: Cardiac syncope • • depends of reasons tachyarrhytmiae-PSVT/a. fibrill=β-blockers, bradyarrtyhmiae-a. fibrill, blocks=pacemaker VT/VF=amiodarone, implantable cardioverter-defibrillators (ICD)

Thank you!
 Syncope in the older patient is
Syncope in the older patient is Syncope vs seizure
Syncope vs seizure Migraine vs epilepsy
Migraine vs epilepsy Convulsieve syncope
Convulsieve syncope Chess score syncope
Chess score syncope Snycope
Snycope Nursing care for pulmonary embolism
Nursing care for pulmonary embolism Syncope
Syncope Syncope
Syncope Syncope
Syncope Vjetar uvećanica
Vjetar uvećanica Kabelska glava
Kabelska glava Extensiv lagtolkning
Extensiv lagtolkning Asirska umetnost
Asirska umetnost Kranjska kobasica od svinjskih glava
Kranjska kobasica od svinjskih glava Adina glava
Adina glava Alisa u zemlji cuda analiza
Alisa u zemlji cuda analiza Westcliffe cardiology service
Westcliffe cardiology service Clinical documentation improvement for cardiology
Clinical documentation improvement for cardiology Cardiology procedures chapter 47
Cardiology procedures chapter 47 Accp cardiology prn
Accp cardiology prn Acc sports cardiology
Acc sports cardiology Service line strategy
Service line strategy Egsys
Egsys Muse cardiology
Muse cardiology Ecg hanna
Ecg hanna Craig ainsworth cardiology
Craig ainsworth cardiology Hall-garcia cardiology associates
Hall-garcia cardiology associates Enloe cardiology
Enloe cardiology Justin davies md
Justin davies md Cardiology structured reporting
Cardiology structured reporting Accp cardiology prn journal club
Accp cardiology prn journal club Gaudium et spes art 49
Gaudium et spes art 49 Mafunzo ya umiliki wa duka la dawa muhimu
Mafunzo ya umiliki wa duka la dawa muhimu Kegembiraan dan harapan duka dan kecemasan
Kegembiraan dan harapan duka dan kecemasan Puisi kontemporer tragedi winka dan sihka
Puisi kontemporer tragedi winka dan sihka Kesedihan dan duka cita masa nifas
Kesedihan dan duka cita masa nifas