PEDIATRIC CARDIOLOGY PALS AND OEMS DAN MUSE MD
- Slides: 28
PEDIATRIC CARDIOLOGY PALS AND OEMS DAN MUSE MD
PEDIATRIC ASSESSMENT PRIMARY ASSESSMENT �Rapid assessment: � Respiratory � Cardiac � Neurologic
PEDIATRIC ASSESSMENT PRIMARY ASSESSMENT �Airway �Breathing �Circulation �AVPU: Alert, Voice, Pain, Unresponsive
PEDIATRIC ASSESSMENT CARDIOPULMONARY ASSESSMENT �In infants and children cardiopulmonary collapse is due primarily to: � Respiratory failure � Shock
PEDIATRIC ASSESSMENT CARDIOPULMONARY ASSESSMENT �As the kids grow up cardiac issues may present �They are predominantly arrhythmias. �Ischemia is not one of them!
PEDIATRIC ASSESSMENT CARDIOPULMONARY ASSESSMENT �Congenital � Tetrology of Fallot � Brugada’s Syndrome � Prolonged QT
PEDIATRIC ASSESSMENT CARDIOPULMONARY ASSESSMENT �Developmental � WPW/Svt’s � Idiopathic Hypertrophic Cardiomyopathy � Cardiomyopathy
PEDIATRIC ASSESSMENT CARDIOPULMONARY ASSESSMENT �Accidental � Commodio Cordis � Drugs
PEDIATRIC ASSESSMENT CARDIAC ARRHYTHMIAS �Defined as � Bradyarrhythmias � Tachyarrhythmias � Pulseless arrest
BRADYARRHYTHMIAS �Defined as � Slow heart rate based on normal rate for age. � Primary Bradycardia: Due to congenital or acquired heart conditions. � Secondary Bradycardia: Due to underlying conditions such as hypoxia, sepsis, acidosis, hypotension, drugs…
BRADYARRHYTHMIAS ARE FREQUENTLY PREARREST RHYTHMNS IN CHILDREN AND OFTENTIMES DUE TO HYPOXIA
BRADYARRHYTHMIAS OEMS PROTOCOLS EMT/EMT-INTERMEDIATE/ADVANCED EMT STANDING ORDERS �Routine Patient Care �If pulse is less than 60 in a child, AND the patient is severely symptomatic, consider starting Cardiopulmonary Resuscitation (CPR).
BRADYARRHYTHMIAS OEMS PROTOCOLS PARAMEDIC STANDING ORDERS IF PATIENT IS SEVERELY SYMPTOMATIC: �Epinephrine 1: 10, 000, 0. 01 mg/kg IV/IO (max. dose 0. 5 mg) OR, �Atropine 0. 02 mg/kg IV/IO (min. single dose 0. 1 mg, max. single dose 1 mg). If increased vagal tone or AV block suspected.
BRADYARRHYTHMIAS OEMS PROTOCOLS MEDICAL CONTROL MAY ORDER �Additional doses of above medications �Additional fluid boluses (10 -20 m. L/kg) �Transcutaneous pacing, if available.
BRADYARRHYTHMIAS OEMS PROTOCOLS MEDICAL CONTROL MAY ORDER �Epinephrine 1: 10, 000 – 0. 01 -0. 03 mg/kg IV/IO (max. single dose of 0. 5 mg) �Epinephrine Infusion 1: 1, 000, 0. 1 -1 mcg/kg/min IV/IO. For example, mix 1 mg of Epinephrine 1: 1000 in 250 m. L of Normal Saline, (15 micro drops/minute = 1 mcg / min. ) �Treat other conditions according to specific protocols.
TACHYARRHYTHMIAS �Abnormally rapid rates that originate in the atria or the ventricles �Certain arrhythmias such as SVT’s and Ventricular Tachycardia can lead to shock and death.
TACHYARRHYTHMIAS SVT �Heart rate : �Infants greater than 220 �Children greater than 180 �P waves are abnormal or hidden: NOT SINUS �PR interval may be absent or short �R-R interval is constant �Complex's are usually narrow. �SVT with aberrency
TACHYARRHYTHMIAS OEMS PROTOCOLS EMT/EMT-INTERMEDIATE/ADVANCED EMT STANDING ORDERS �Routine Patient Care �If tachycardia is related to acute injury or volume loss, see 2. 16 P Shock.
TACHYARRHYTHMIAS OEMS PROTOCOLS PARAMEDIC STANDING ORDERS �IV Normal Saline (KVO). If hypovolemic component is suspected, administer 20 m. L/kg IV Bolus of Normal Saline.
TACHYARRHYTHMIAS OEMS PROTOCOLS MEDICAL CONTROL MAY ORDER � Additional doses of above medications � Synchronized cardioversion 0. 5 joules/kg for symptomatic patients. * Subsequent cardioversion may be done at up to 1 joule/kg. If cardioversion is warranted, consider administration of 7. 6 Sedation for Electrical Therapy, per protocol. � See A 2 Pediatric Color Coded Medication Reference for dosing. � Adenosine 0. 1 mg/kg rapid IV/IO. If no effect, repeat Adenosine 0. 2 mg/kg Rapid IV push. MAXIMUM single dose of Adenosine must not exceed 12 mg. � Consider Vagal maneuvers (see Reminder below). � Treat other conditions according to specific protocols
TACHYARRHYTHMIAS OEMS PROTOCOLS OEMS WARNING Synchronized cardioversion should be considered for only those children whose heart rate is in excess of 220, and who demonstrate one or more of the following signs of hypoperfusion: Decreased level of consciousness, weak and thready pulses, capillary refill time of more than 4 seconds, or no palpable BLOOD PRESSURE.
TACHYARRHYTHMIAS OEMS PROTOCOLS OEMS WARNING REMINDER: Vagal maneuvers may precipitate asystole and therefore should be employed with caution in the field and only in a cardiac-monitored child with IV access.
VENTRICULAR TACHYCARDIA WITH PULSES OEMS PROTOCOLS EMT/EMT-INTERMEDIATE/ADVANCED EMT STANDING ORDERS �Routine Patient Care
VENTRICULAR TACHYCARDIA WITH PULSES PARAMEDIC STANDING ORDER �Unstable pediatric patients, synchronized cardioversion per Pediatric Color-Coded Appendix. �If cardioversion is warranted, see 7. 6 Sedation for Electrical Therapy �Stable pediatric patient administer Amiodarone dose per Pediatric Color-Coded Appendix
CARDIAC ARREST OEMS PROTOCOLS EMT / EMT-INTERMEDIATE / ADVANCED EMT STANDING ORDERS � Routine Patient Care—with focus on high quality CPR � Apply AED and use as soon as possible (with minimum interruption of chest compressions). From birth to age 8 years use pediatric AED pads. � If pediatric AED pads are unavailable, providers may use adult AED pads, provided the pads do not overlap.
CARDIAC ARREST OEMS PROTOCOLS EMT / EMT-INTERMEDIATE / ADVANCED EMT STANDING ORDERS �If unable to ventilate child after repositioning of airway, assume upper airway obstruction and follow Pediatric Upper Airway Obstruction Protocol. �Consider treatable causes
CARDIAC ARREST OEMS PROTOCOLS PARAMEDIC STANDING ORDERS �Defibrillate once at 2 -4 J/kg. �Epinephrine: 0. 01 mg/kg IV/IO (1: 10, 000, 0. 1 m. L/kg); repeat every 3 -5 minutes. �Defibrillate 4 -10 J/kg (do not exceed 10 J/kg) every 2 minutes. �Amiodarone 5 mg/kg IV/IO �Defibrillate 4 J/kg 30 -60 seconds after each medication.
CARDIAC ARREST OEMS PROTOCOLS MEDICAL CONTROL MAY ORDER �Additional doses of above medications �Sodium Bicarbonate 1 m. Eq/kg IV/IO. �All other treatment modalities based upon suspected cause of VT/FT. �Treat other conditions according to specific protocols.
 Muse cardiology
Muse cardiology Beta-blocker overdose treatment glucagon
Beta-blocker overdose treatment glucagon Dan muse
Dan muse Westcliffe medical centre
Westcliffe medical centre Clinical documentation improvement for cardiology
Clinical documentation improvement for cardiology Cardiology procedures chapter 47
Cardiology procedures chapter 47 Accp cardiology prn
Accp cardiology prn Acc sports cardiology
Acc sports cardiology Cardiology service line management
Cardiology service line management Dr nick gall cardiologist
Dr nick gall cardiologist Ecg hanna
Ecg hanna Craig ainsworth cardiology
Craig ainsworth cardiology Hall-garcia cardiology associates
Hall-garcia cardiology associates Enloe cardiology
Enloe cardiology Inculprate
Inculprate Cath lab report example
Cath lab report example Accp cardiology prn journal club
Accp cardiology prn journal club Spencer muse
Spencer muse Susan elizabeth blow
Susan elizabeth blow Pizzolato muse prosecco
Pizzolato muse prosecco Virgen maria muse
Virgen maria muse The endless column
The endless column Thalia muse
Thalia muse Muse soumaya
Muse soumaya Marine couverchel
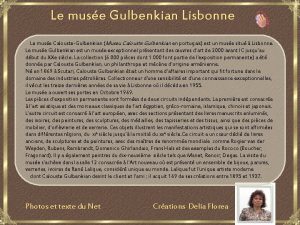
Marine couverchel Muse lisbonne
Muse lisbonne Benigni inferno canto 5
Benigni inferno canto 5 Le muse de louvre
Le muse de louvre Hotel muse bangkok
Hotel muse bangkok