Assisting in Cardiology Chapter 47 Copyright 2011 2007
- Slides: 58
Assisting in Cardiology Chapter 47 Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 1
Learning Objectives Define, spell, and pronounce the terms listed in the vocabulary. Apply critical thinking skills in performing patient assessment and care. Illustrate the anatomy and physiology of the heart and its significant structures. Summarize risk factors for the development of cardiovascular disease. Describe the signs, symptoms, and medical procedures employed in the diagnosis and treatment of coronary artery disease and myocardial infarction. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 2
Learning Objectives Compare and contrast the treatment protocols for hypertension. Outline the causes and results of congestive heart failure. Illustrate the effects of inflammation and valvular disorders on cardiac function. Describe the anatomy and physiology of the vascular system. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 3
Learning Objectives Differentiate among the various types of shock. Summarize the characteristics of common vascular disorders. Outline typical cardiovascular diagnostic procedures. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 4
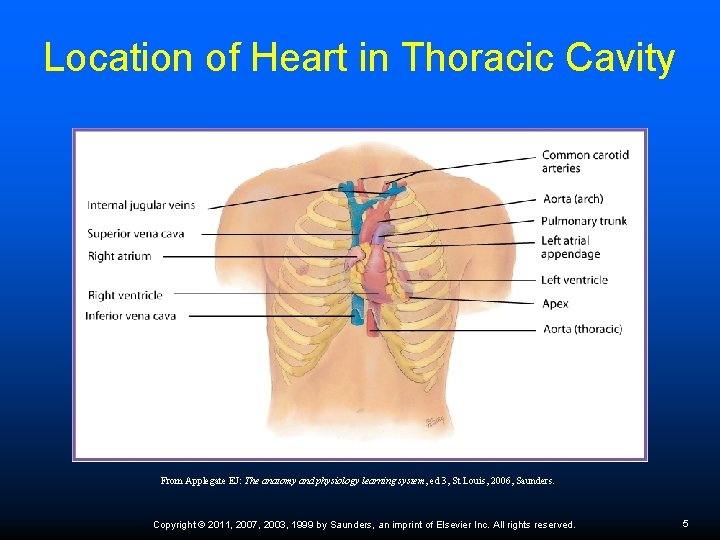
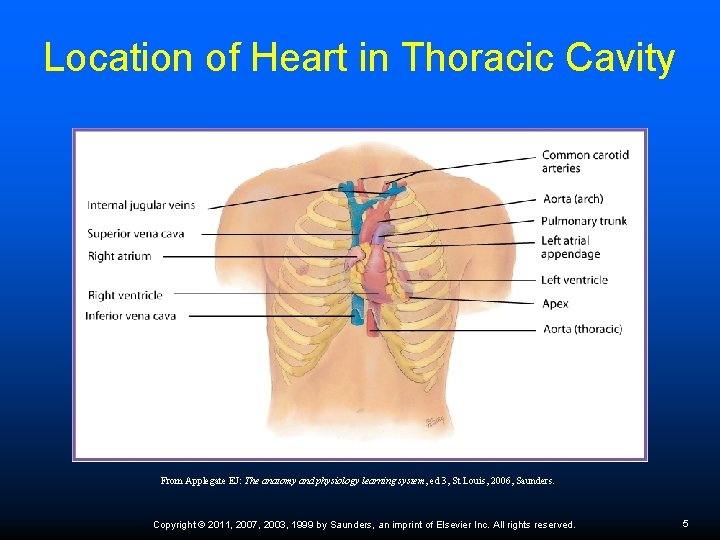
Location of Heart in Thoracic Cavity From Applegate EJ: The anatomy and physiology learning system, ed 3, St Louis, 2006, Saunders. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 5
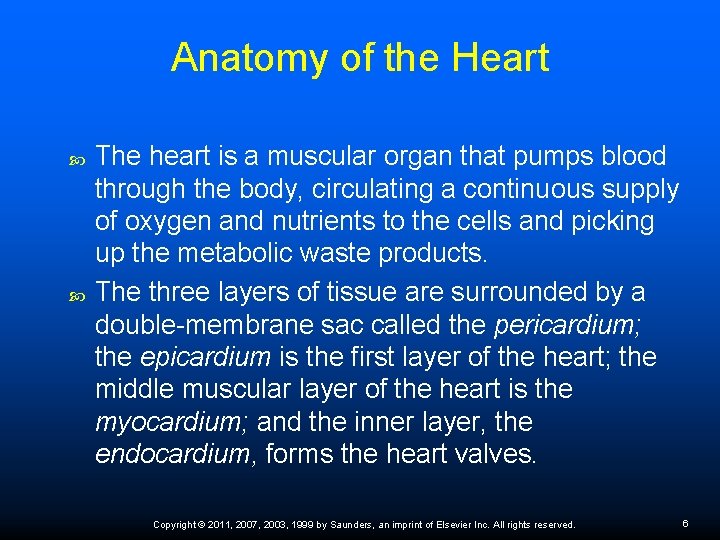
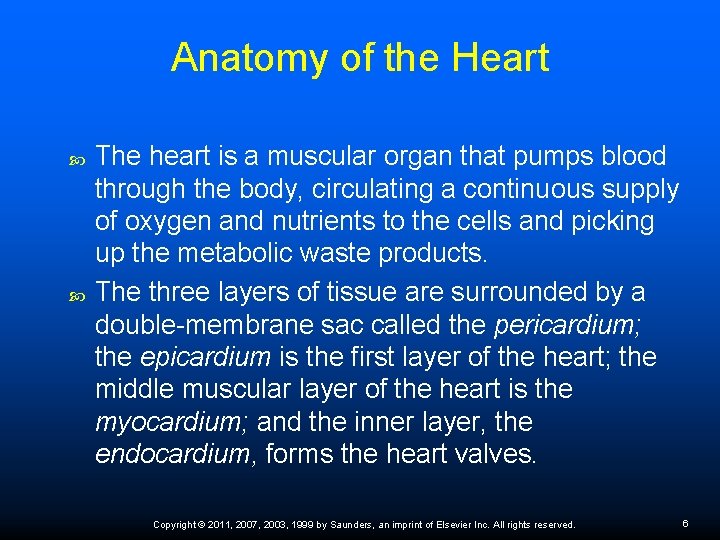
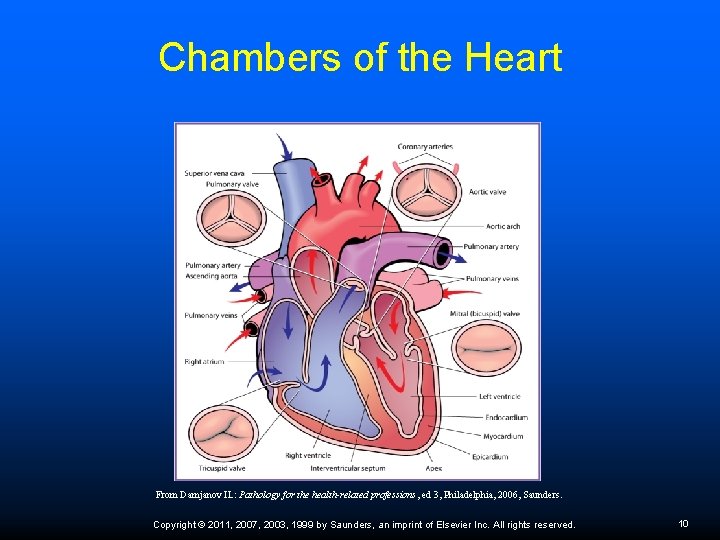
Anatomy of the Heart The heart is a muscular organ that pumps blood through the body, circulating a continuous supply of oxygen and nutrients to the cells and picking up the metabolic waste products. The three layers of tissue are surrounded by a double-membrane sac called the pericardium; the epicardium is the first layer of the heart; the middle muscular layer of the heart is the myocardium; and the inner layer, the endocardium, forms the heart valves. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 6
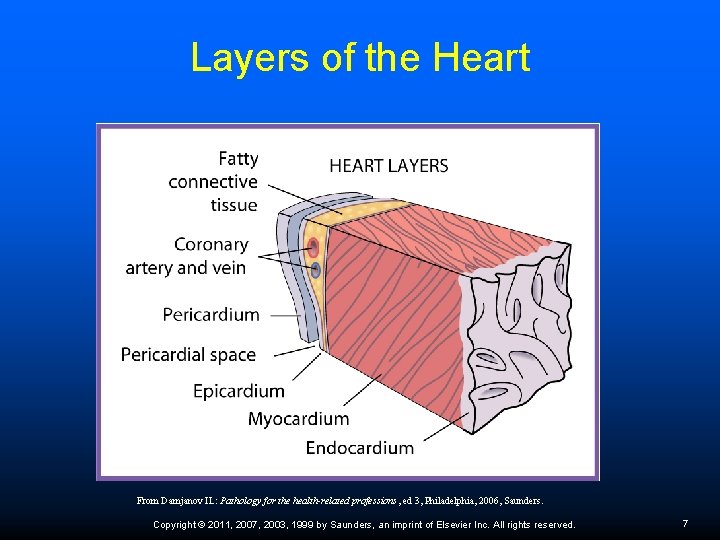
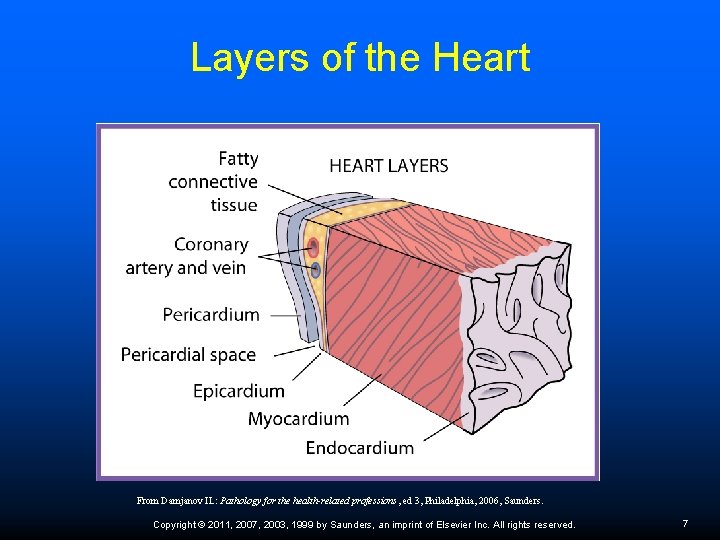
Layers of the Heart From Damjanov IL: Pathology for the health-related professions, ed 3, Philadelphia, 2006, Saunders. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 7
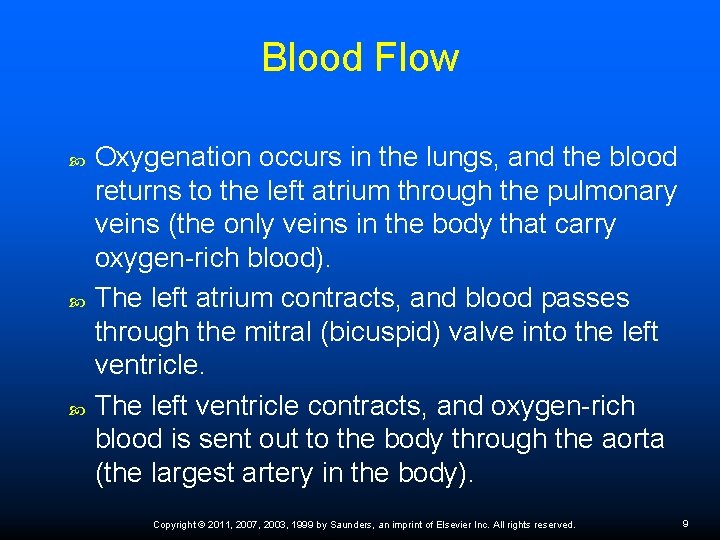
Blood Flow Blood flow through the heart begins in the right atrium, which receives deoxygenated blood from the inferior and superior vena cava. The right atrium contracts, and blood passes through the tricuspid valve into the right ventricle. The right ventricle contracts, and blood passes from the right ventricle to the lungs via the pulmonary artery (the only artery in the body that carries deoxygenated blood). Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 8
Blood Flow Oxygenation occurs in the lungs, and the blood returns to the left atrium through the pulmonary veins (the only veins in the body that carry oxygen-rich blood). The left atrium contracts, and blood passes through the mitral (bicuspid) valve into the left ventricle. The left ventricle contracts, and oxygen-rich blood is sent out to the body through the aorta (the largest artery in the body). Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 9
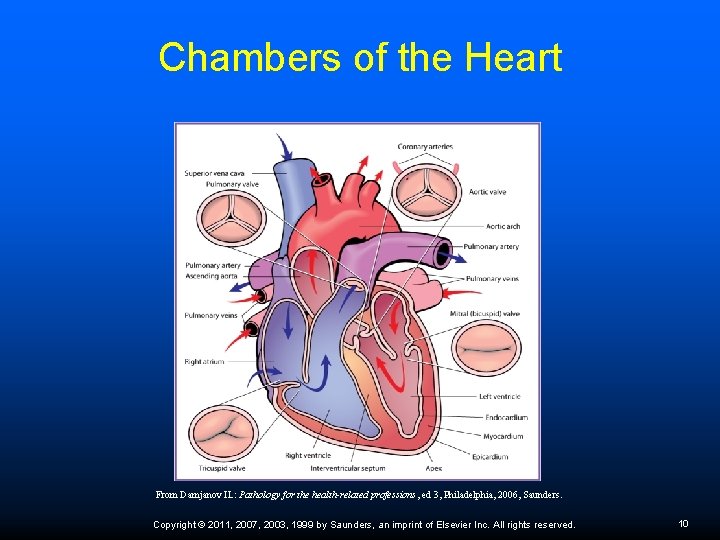
Chambers of the Heart From Damjanov IL: Pathology for the health-related professions, ed 3, Philadelphia, 2006, Saunders. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 10
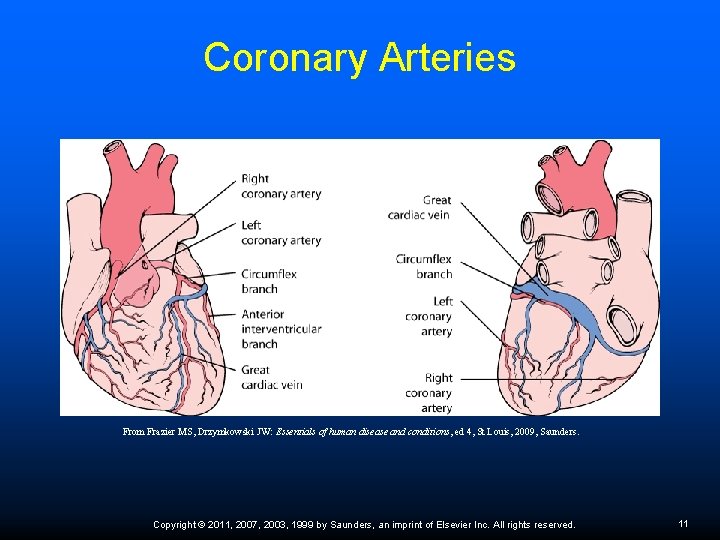
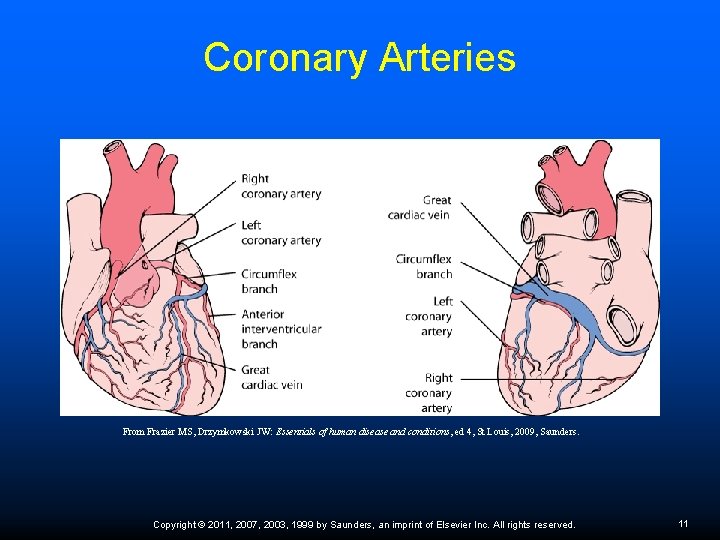
Coronary Arteries From Frazier MS, Drzymkowski JW: Essentials of human disease and conditions, ed 4, St Louis, 2009, Saunders. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 11
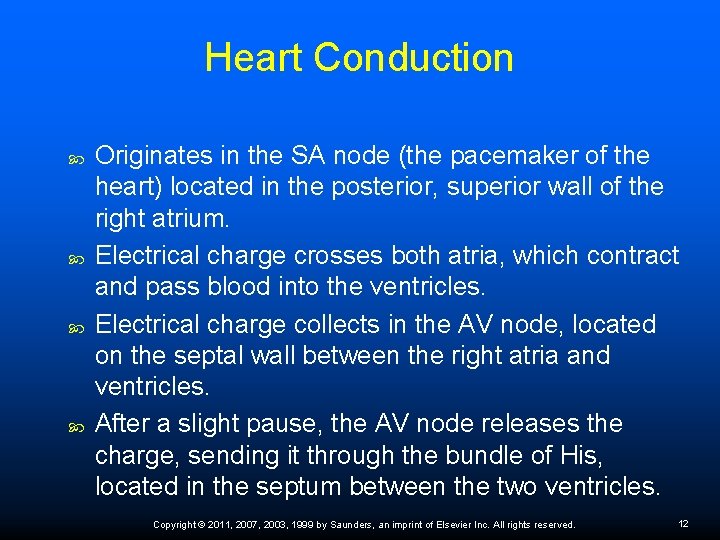
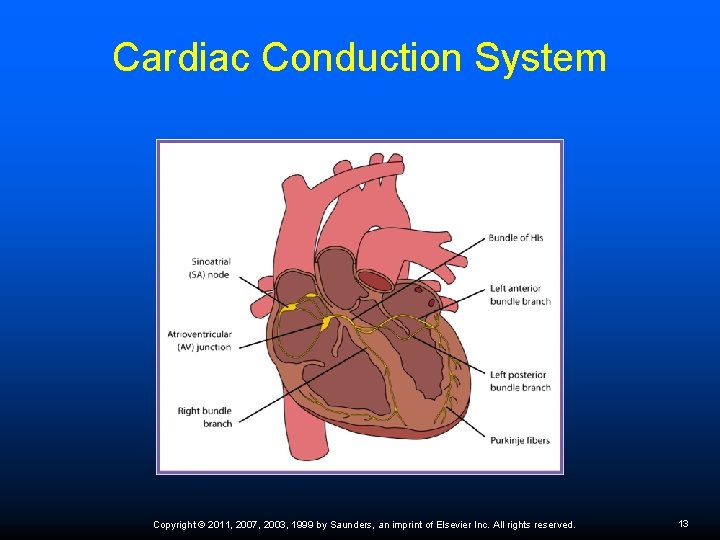
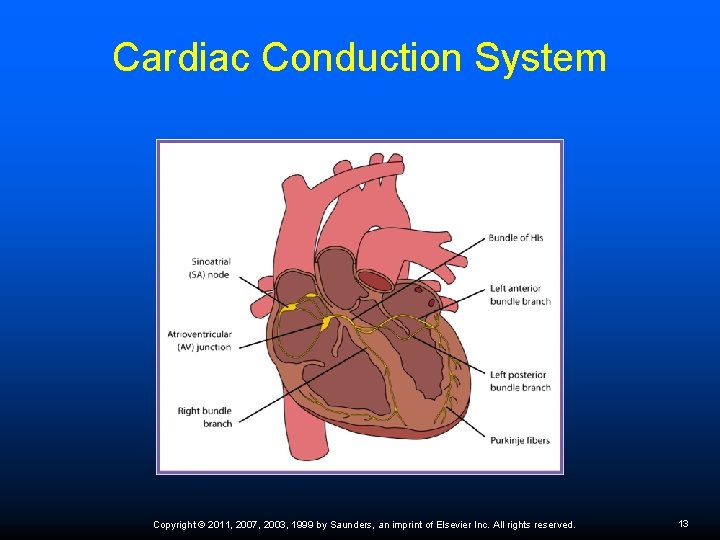
Heart Conduction Originates in the SA node (the pacemaker of the heart) located in the posterior, superior wall of the right atrium. Electrical charge crosses both atria, which contract and pass blood into the ventricles. Electrical charge collects in the AV node, located on the septal wall between the right atria and ventricles. After a slight pause, the AV node releases the charge, sending it through the bundle of His, located in the septum between the two ventricles. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 12
Cardiac Conduction System Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 13
Heart Conduction The bundle of His divides into the left and right bundle branches, which surround the left and right ventricles. Electrical charge continues through the Purkinje fibers, the most distal part of the heart’s conduction system. The Purkinje fibers complete ventricular stimulation, and the ventricles contract. Contraction of the heart chambers is depolarization. After contraction, repolarization or electrical recovery occurs. Polarization is the heart at rest. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 14
Diseases and Disorders of the Heart Multiple risk factors for cardiac disease include: genetic predisposition and family history Ø hypertension Ø age Ø gender Ø diabetes Ø elevated blood cholesterol levels Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 15
Cardiac Disease Risk Factors Lifestyle factors include: High-fat, high-caloric diets Ø Obesity Ø Smoking Ø Lack of exercise Ø Hypertension Ø Stress Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 16
Heart Disease Risk in Women are at greater risk with the following factors: Metabolic syndrome Ø combination of hypertension, elevated insulin levels, excess body fat around the waist, and high blood cholesterol levels Increased levels of stress and/or depression Female smokers are at much greater risk than male smokers Decreased estrogen production before menopause Difference in female risks and symptoms is associated with the method of plaque buildup in women Ø develop an evenly spread layer of plaque along the entire lumen of blood vessels rather than localized plaque buildup Ø have diffuse atheroma buildup in smaller vessels, which causes more subtle symptoms Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 17
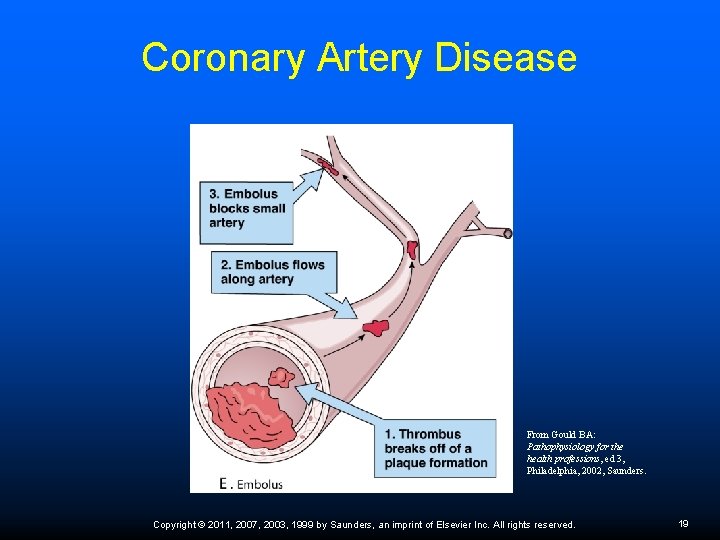
Coronary Artery Disease Arteries supplying the myocardium become narrowed by atherosclerotic plaques. Platelets stick to the plaque deposits, forming thrombi, and lipids continue to build up at the site. The process causes narrowing of the lumen of the arteries and inhibits normal blood flow, depriving the myocardium of adequate blood. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 18
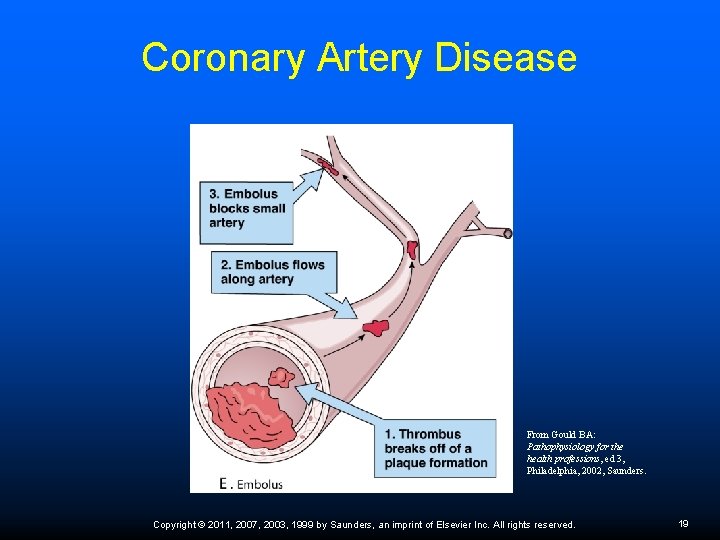
Coronary Artery Disease From Gould BA: Pathophysiology for the health professions, ed 3, Philadelphia, 2002, Saunders. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 19
Coronary Artery Disease Myocardial ischemia signs and symptoms: angina pectoris (pain behind the sternum that can be relieved by rest or nitroglycerin) followed by pressure or fullness in the chest, syncope, edema, unexplained coughing spells, and fatigue. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 20
Myocardial Infarction Symptoms of myocardial infarction (MI) are very similar to those of angina, but myocardial infarction pain lasts longer than 30 minutes and is unrelieved by rest or nitroglycerin tablets. An MI is diagnosed by ECG changes and elevated cardiac enzymes 6 to 12 hours after the episode. Enzymes are released by the necrotic myocardium and continue to increase for 24 to 49 hours after the MI. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 21
Myocardial Infarction Symptoms in Women Ischemia over a prolonged period leads to necrosis of a portion of the myocardium, resulting in a myocardial infarction. Women may exhibit a different clinical picture from that in men. Abdominal or midback pain Ø Jaw pain Ø Indigestion Ø Extreme fatigue Ø Aching in both arms Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 22
Critical Thinking Application A patient who is scheduled for an appointment in 2 days calls the office and reports that she is not feeling well. She complains that she has a feeling of fullness in the chest, her arms ache, and she is very tired. Although this patient does not have a history of myocardial infarction, what should Adam do? Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 23
Telephone Screening for Chest Pain Activate EMS if: Chest pain is crushing and radiating Ø Diaphoresis, dyspnea, nausea, indigestions, vertigo Ø History of CAD, MI, or angina Ø Change in pattern of angina Ø Chest pain occurs at rest or with minimal exertion Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 24
MI Diagnosis ECG changes and elevated cardiac enzymes Blood tests Creatinine kinase (CK) levels – start increasing 6 hours after initial MI and reach a peak in 18 hours with a return to normal in 24 to 36 hours; the more severe the cardiac damage the longer it takes for CK levels to peak and return to normal Ø Troponin levels – can detect minor myocardial damage not evident with CK levels; levels increase 4 – 6 hours after initial MI and peak in 10 to 24 hours; with minor myocardial damage, levels are elevated up to 10 to 14 days Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 25
MI Treatment Thrombolytic medications (Activase, Retavase) to dissolve the coronary artery blockage, but must be started within 12 hours of initial symptoms Aspirin Beta-blockers (Tenormin, Lopressor, Inderal) Anticoagulants (Coumadin) Anticholesterol agents (Lipitor, Zocor, Mevacor) Percutaneous transluminal coronary angioplasty or open-heart surgery may be indicated Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 26
Hypertensive Heart Disease Secondary hypertension occurs because of a disease process in another body system. Primary hypertension is idiopathic. MA responsibility—two BP readings, 2 minutes apart, with patient sitting in chair; if elevated, check BP in the other arm. Chronic elevated blood pressure can result in left ventricular hypertrophy, angina, MI, heart failure, stroke, or nephropathy. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 27
Classification of Blood Pressure Normal BP: SBP <120 and DBP <80 Prehypertension: 120– 139 or 80– 89 Hypertension stage 1: 140– 159 or 90– 99 Hypertension stage 2: ≥ 160 or ≥ 100 Hypertension treatment: treat BP <140– 90 mm Hg or <130/80 in patients with diabetes or chronic kidney disease Most patients require two medications to reach BP goal (diuretic and hypertensive medication) Refer to Table 47 -2 for hypertensive medications Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 28
Lifestyle Modifications Weight reduction: BMI from 19 to 25 will lower SBP 5– 20 mm Hg/10 kg DASH diet (rich in fruit and vegetables, low-fat dairy products, reduce saturated and total fat): SBP reduction of 8– 14 mm Hg Decrease sodium (2. 4 g/day): SBP drops 2– 8 mm Hg Aerobic exercise (30 min/day): drops 4– 9 mm Hg Moderate alcohol intake (men, no more than two drinks/day; women, one): drops 2– 4 mm Hg Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 29
Risk Factors Risk factors for developing hypertension include: family history of hypertension or stroke Ø hypercholesterolemia Ø smoking Ø high sodium intake Ø diabetes Ø excessive alcohol intake Ø aging Ø prolonged stress Ø race Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 30
Critical Thinking Application Essential hypertension is a common problem for patients seen in the cardiology department where Adam works. What could Adam do to help patients with primary hypertension? What informational materials or community resources would be helpful in gaining patient compliance with treatment? Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 31
Congestive Heart Failure Congestive heart failure occurs when the myocardium is unable to pump enough blood to meet the needs of the body. Develops over time because of weakness in the left ventricle from chronic hypertension or MI of the ventricular wall; valvular heart disease; or pulmonary complications. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 32
Heart Failure Typically, heart failure initially occurs on one side of the heart followed by the other side. Treatment: Limiting physical activity Ø Sodium restriction Ø Weight control Ø Diuretics Ø ACE inhibitors and digoxin Ø Routine monitoring of serum electrolytes to monitor potassium levels Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 33
Left-Sided Heart Failure Left-sided heart failure is usually caused by essential hypertension or left ventricle disease. Causes a backup of blood in the lungs, resulting in pulmonary edema. Signs and symptoms Dyspnea Ø Orthopnea Ø Nonproductive cough Ø Rales Ø Tachycardia Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 34
Right-Sided Heart Failure Right-sided heart failure causes a backup of blood in the right atrium, which prevents complete emptying of the vena cava, resulting in systemic edema, especially in the legs and feet. Right-sided heart failure can develop from lung disease. Cor pulmonale—right-sided heart failure caused by pulmonary hypertension resulting from COPD. Both types of heart failure cause fatigue, weakness, exercise intolerance, dyspnea, and sensitivity to cold temperatures. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 35
Treatment for CHF Nonmedication treatment – limit physical activity, restrict salt, no smoking, reduce stress, and control weight Patient education – stress monitoring weight gain; sudden increase in weight may indicate fluid retention Drug therapy – diuretics; ACE inhibitor (Vasotec, Prinivil, Zestril, Capoten); Digoxin; beta-blockers (Coreg, Lopressor); potassium supplement. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 36
Critical Thinking Application Kate Glasgow, a 76 -year-old patient with a history of CHF, is in the office today for a checkup. Miss Glasgow does not understand why she needs to stop using salt and does not weigh herself regularly at home. What can Adam do to help this patient understand the importance of her treatment regimen? Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 37
Hypotension Orthostatic or postural hypotension. Common problem in elderly. May contribute to falls and related injuries. Patients need to be evaluated for secondary causes and encouraged to adjust from a prone position by sitting at the side of the bed before standing. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 38
Rheumatic Heart Disease Develops because of unusual immune reaction that occurs approximately 2 weeks after an untreated beta-hemolytic streptococcal infection Antibodies cause inflammation in the layers of the heart Pericarditis—decreases cardiac activity and causes pericardial effusion Endocarditis—most common heart complication Vegetations form along the outer edges of the valve cusps, causing scarring and stenosis Ø Treatment: penicillin and antiinflammatory agents; prophylactic antibiotics before all invasive procedures Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 39
Valvular Disorders of the valves of the heart may be caused by a congenital defect or an infection, such as endocarditis or rheumatic heart disease. Two specific problems can occur with valve disease. The valve can be stenosed, restricting the forward flow of blood, or it can be incompetent, so blood can leak backward. The most common valve defect is mitral valve prolapse (MVP), an incompetence caused by a congenital defect or vegetation and scarring from endocarditis. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 40
Arteries and Veins Blood vessels are divided into two systems that begin and end with the heart. Arteries carry oxygenated blood away from the heart. Ø Capillaries are microscopic vessels responsible for the exchange of oxygen and carbon dioxide in the tissue. Ø Veins carry deoxygenated blood back to the heart. Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 41
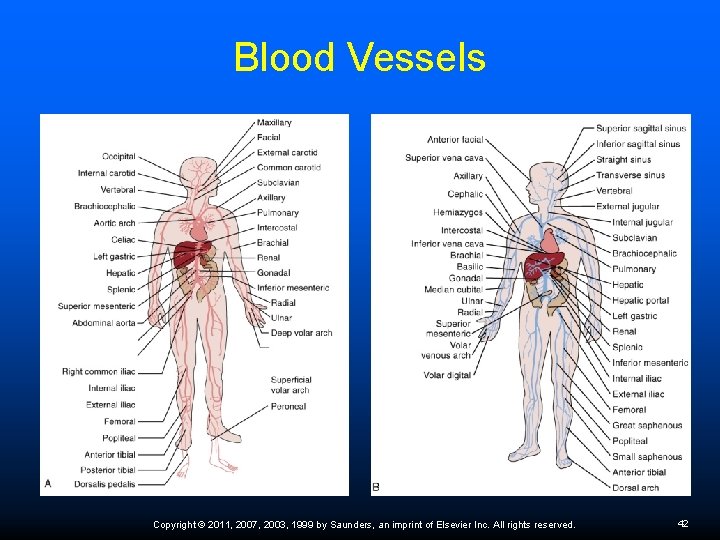
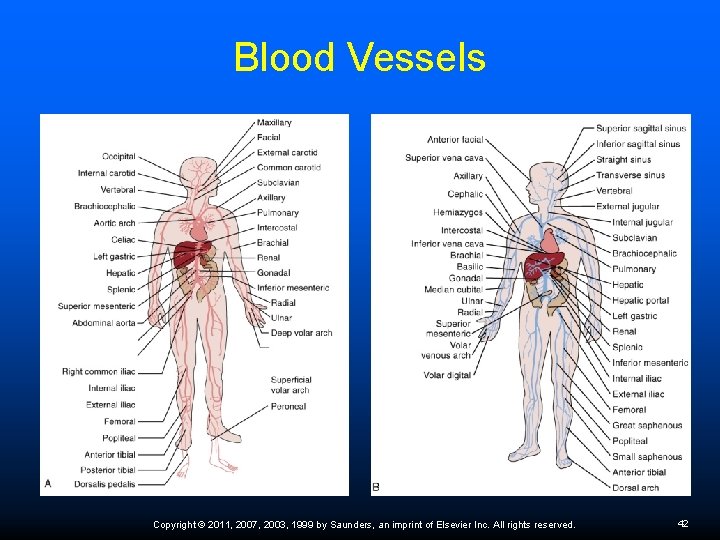
Blood Vessels Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 42
Shock Shock—general collapse of the circulatory system; includes decreased cardiac output, hypotension, and hypoxemia. Initial signs—extreme thirstiness, restlessness, and irritability. Body attempts to compensate with vasoconstriction of peripheral blood vessels, causing cool, clammy skin; pallor; tachycardia; and decreased urinary output. Signs and symptoms progress to a rapid, weak, and thready pulse; tachypnea; altered levels of consciousness. If the process is not reversed, the CNS becomes depressed and acute renal failure may occur. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 43
Types of Shock Cardiogenic—MI, pulmonary embolism, CHF Hypovolemic—hemorrhage, burns Neurogenic—spinal cord injury, stress, drug reaction Anaphylactic—allergic reaction Septic—systemic infection Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 44
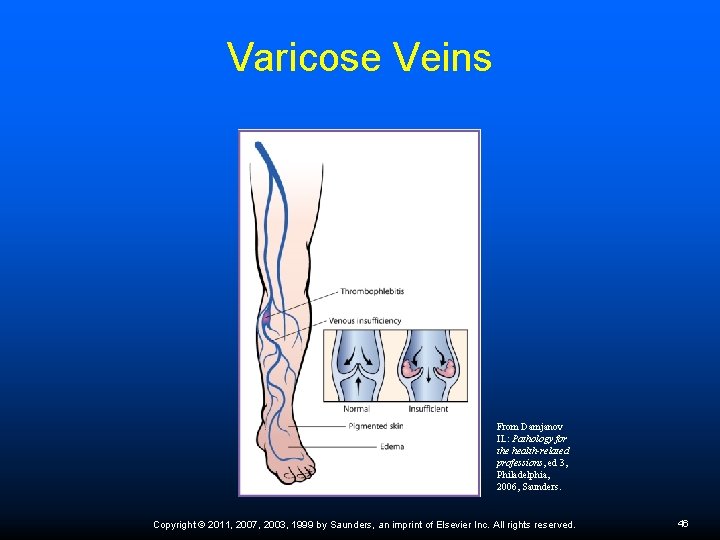
Varicose Veins Varicose veins are dilated, tortuous, superficial veins that develop because the valves do not completely close, allowing blood to flow backward. Causes the vein to distend from the increased pressure. Caused by congenitally defective valves, pregnancy, obesity, prolonged standing or sitting, heavy lifting. Treatment: Ø Ø Ø Aerobic exercise Limit heavy lifting Elevate legs when possible Wear support stockings Possible surgical intervention Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 45
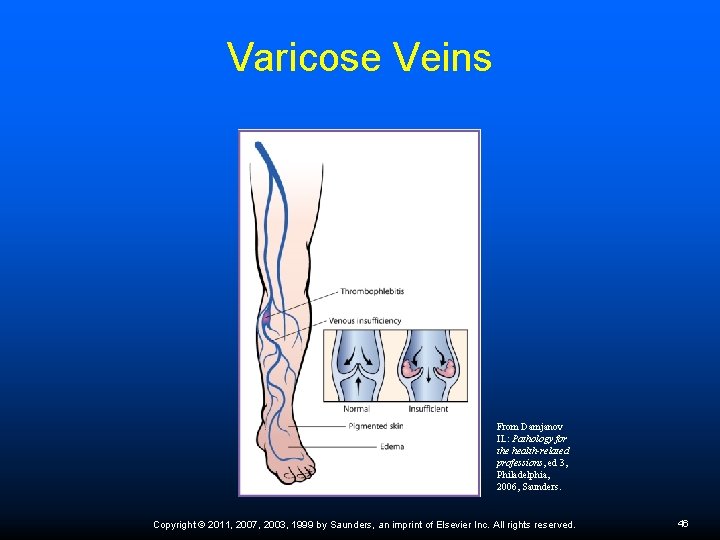
Varicose Veins From Damjanov IL: Pathology for the health-related professions, ed 3, Philadelphia, 2006, Saunders. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 46
Deep Vein Thrombosis DVT—thrombus with inflammatory changes that has attached to the deep venous system of the lower legs Causes partial or complete obstruction of vessel Symptoms— 50% asymptomatic at first; calf pain; swelling, warmth, edema, erythema at site Embolus—thrombus becomes dislodged and begins to circulate through the general circulation; pulmonary embolism is most serious Diagnosis: Doppler—measures rate of RBC flow; venography Treatment: IV heparin, oral coumadin; bed rest Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 47
Prevention of Deep Vein Thrombosis Take prescribed medications as directed. If prescribed anticoagulants, foods high in vitamin K (dark green leafy vegetables, canola and soy oils) should be eaten in small amounts. Avoid sitting still for long periods of time; periodically walk around or move legs frequently. Alter lifestyle factors such as obesity, smoking, and hypertension since they increase DVT risk. Wear compression stockings as ordered by the physician. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 48
Critical Thinking Application Alitza Lincoln is a 43 -year-old patient who has large varicose veins in both legs and a history of phlebitis. She is a checkout clerk at the local Wal-Mart, so she stands for extended periods of time. The physician is concerned about the development of a DVT and instructs Ms. Lincoln on the prevention, signs, and symptoms of a thrombus. Alitza asks Adam what she can do to prevent further problems with the veins in her legs. Adam uses a picture to illustrate the valves in the leg veins and explains preventive measures. What measures should Adam include? Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 49
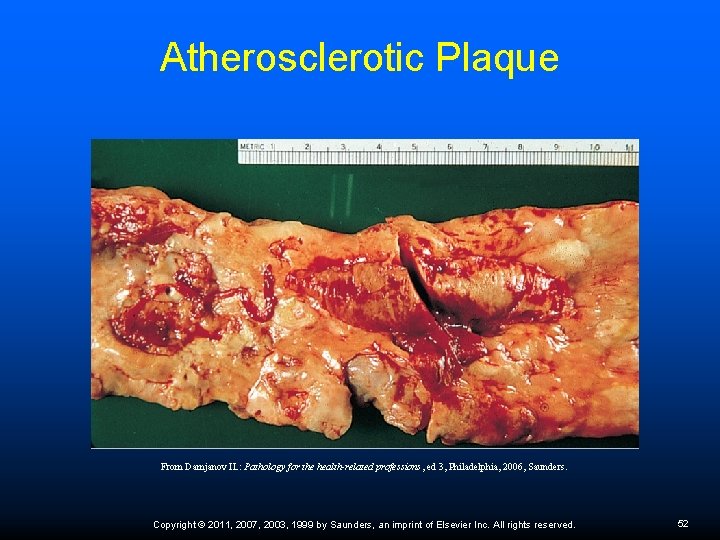
Arterial Disorders Arteriosclerosis—thickening and loss of elasticity of arterial walls associated with aging; can occur in arteries throughout the body and cause systemic ischemia and necrosis Atherosclerosis (form of arteriosclerosis)— formation of an atheroma (a buildup of cholesterol, cellular debris, and platelets along the inside vessel wall) Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 50
Treatment for Hypercholesterolemia Diet – reduce saturated fats and foods high in cholesterol Aerobic exercise to elevate HDL levels Stop smoking Statin drugs – Lipitor and Zocor Patient education about risk factors and promoting alterations in lifestyle Referral to dietitian Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 51
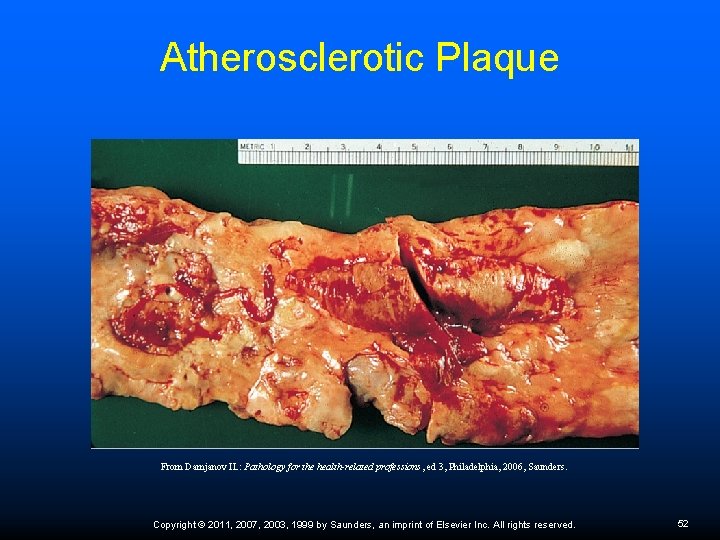
Atherosclerotic Plaque From Damjanov IL: Pathology for the health-related professions, ed 3, Philadelphia, 2006, Saunders. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 52
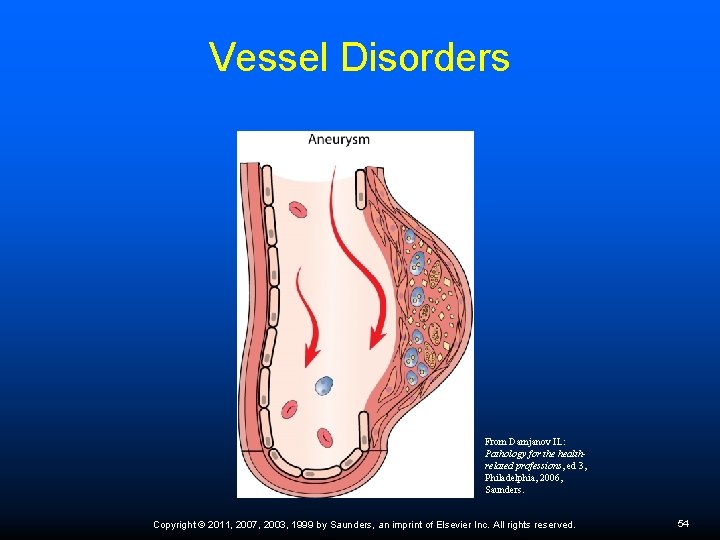
Vessel Disorders Aneurysm—dilation of vessel wall Caused by Marfan’s syndrome; atherosclerosis Ø Diagnosis: bruit; arteriograms; sonography; CT scan Ø Treatment: surgical repair Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 53
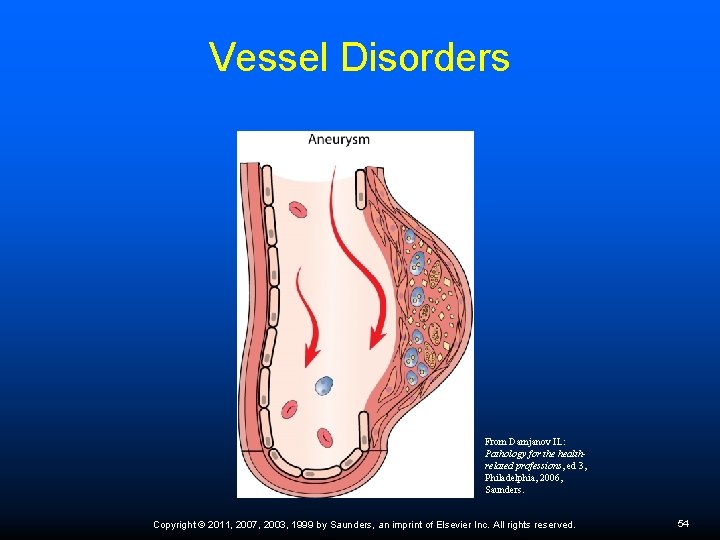
Vessel Disorders From Damjanov IL: Pathology for the healthrelated professions, ed 3, Philadelphia, 2006, Saunders. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 54
Peripheral Artery Disease Due to widespread atherosclerotic plaque buildup in the arteries outside of the heart, especially in the legs Plaque deposits decrease the lumen size and amount of oxygenated blood delivered to tissues Symptoms – intermittent claudications; leg numbness or weakness; persistently cold extremities; sores of the feet or legs that do not heal; and hair loss on the extremities Most effective treatments – regular exercise to promote new vessel growth and smoking cessation Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 55
Diagnostic Procedures Cardiovascular diagnostic procedures include: Doppler studies of the patency of blood vessels Ø Angiography to visualize arterial pathways Ø Echocardiography to assess the structure and movement of the parts of the heart, especially the valves Ø Cardiac catheterization to visualize the heart chambers, valves, and coronary arteries; may be followed with angioplasty and placement of stent Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 56
Cardiac Treatment Procedures Pacemaker – small battery-powered device implanted in the chest wall to generate an electrical impulse that is sent to the heart along flexible lead wires; can monitor BP, temperature, and breathing rate to determine whether the heart needs to be stimulated to contract more frequently; must be replaced when battery pack wears out Implantable cardioverter-defibrillator (ICD) – pager-size device implanted in the chest under the skin and attached to the heart with small wires; continuously monitors heart rhythm and delivers electric shock to correct life-threatening arrhythmias Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 57
Patient Education The medical assistant can help patients by encouraging and supporting them by using community resources. Patients learn best through visuals aids. Document educational interventions. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 58