Clinical Documentation Update Cardiology Service Line The Challenge
- Slides: 11
Clinical Documentation Update Cardiology Service Line
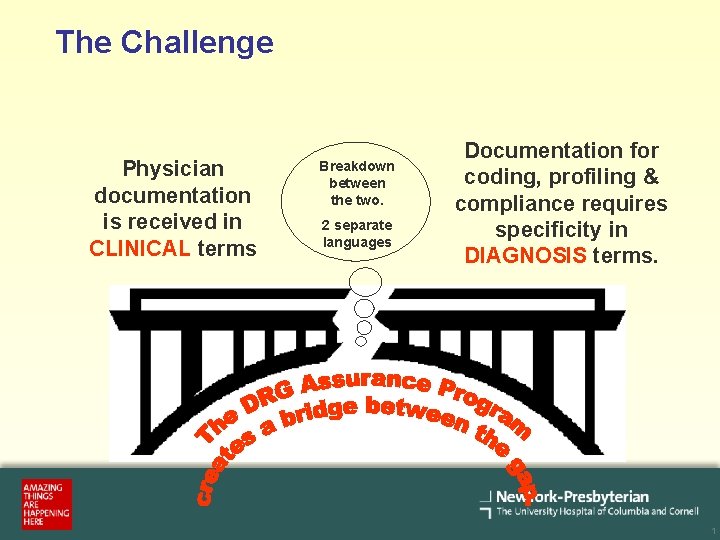
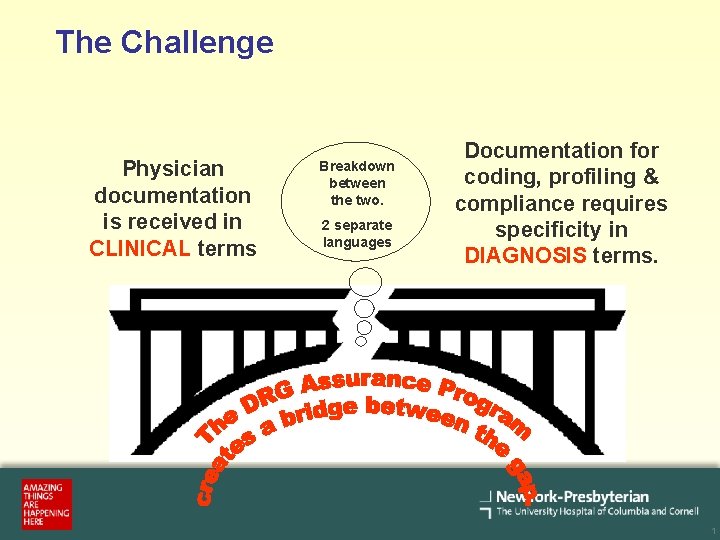
The Challenge Physician documentation is received in CLINICAL terms Breakdown between the two. 2 separate languages Documentation for coding, profiling & compliance requires specificity in DIAGNOSIS terms. 1
Our Goal § Clarify documentation in the medical record to reflect the true severity of the patient’s illness. § Achieve and maintain an administrative database that: – Accurately reflects the high quality of care provided – Ensures compliance with regulatory guidelines – Accurately reflects the complexity of our patient population – Provides a complete medical record for communication among providers 2
Case Mix Index (CMI) – Used for resource allocation such as nursing, PA/NP staffing levels – Compare peer hospitals – Calculate Medicare reimbursements – Designate length of stay allowances – A low CMI may result from DRG assignments that underestimate the patient acuity and the actual resources used in treatment 3
CMS Present on Admission Reporting Requirements § CMS defines POA: present at the time of order for inpatient admission § Conditions that develop during an outpatient encounter, including ED, observation, or outpatient surgery, are considered present on admission § POA indicator is assigned to the principal and secondary diagnoses § Provider must resolve inconsistent, missing, conflicting or unclear documentation § Conditions that occur during the inpatient stay are called “hospital Acquired Conditions” (HACs) Source: CMS Manual System Transmittal 1240, May 11, 2007 Subject: Present on Admission Indicator 4
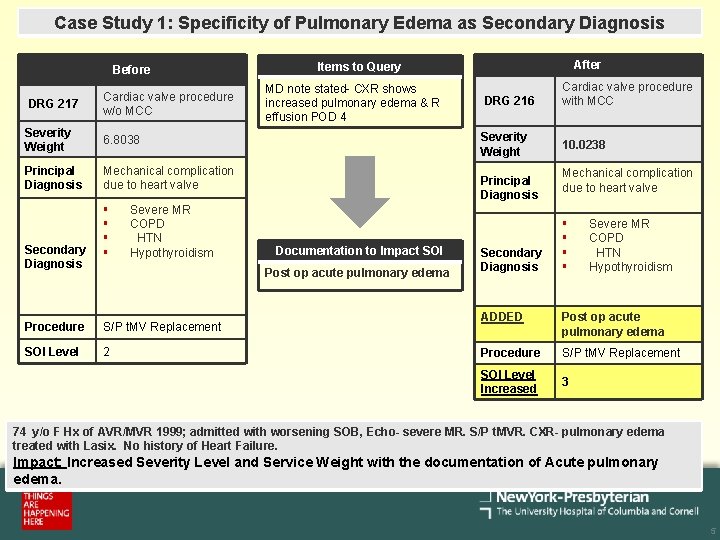
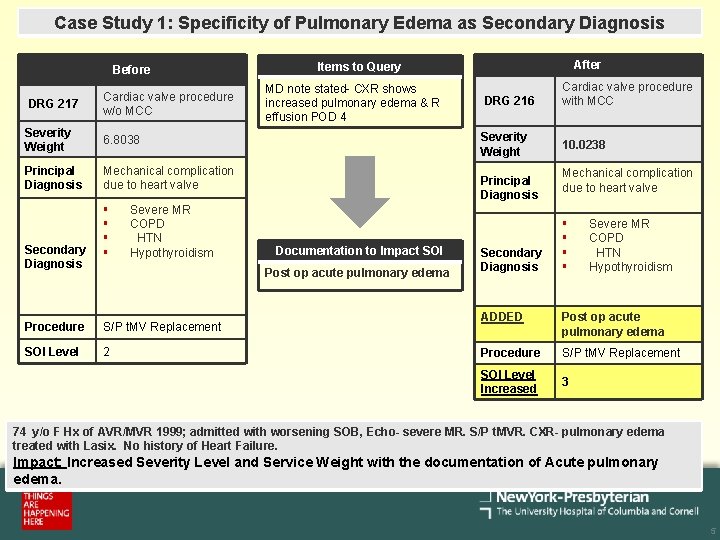
Case Study 1: Specificity of Pulmonary Edema as Secondary Diagnosis Before DRG 217 Cardiac valve procedure w/o MCC Severity Weight 6. 8038 Principal Diagnosis Mechanical complication due to heart valve Secondary Diagnosis § § Severe MR COPD HTN Hypothyroidism MD note stated- CXR shows increased pulmonary edema & R effusion POD 4 S/P t. MV Replacement SOI Level 2 DRG 216 Severity Weight Principal Diagnosis Documentation to Impact SOI Post op acute pulmonary edema Procedure After Items to Query Secondary Diagnosis Cardiac valve procedure with MCC 10. 0238 Mechanical complication due to heart valve § § Severe MR COPD HTN Hypothyroidism ADDED Post op acute pulmonary edema Procedure S/P t. MV Replacement SOI Level Increased 3 74 y/o F Hx of AVR/MVR 1999; admitted with worsening SOB, Echo- severe MR. S/P t. MVR. CXR- pulmonary edema treated with Lasix. No history of Heart Failure. Impact: Increased Severity Level and Service Weight with the documentation of Acute pulmonary edema. 5
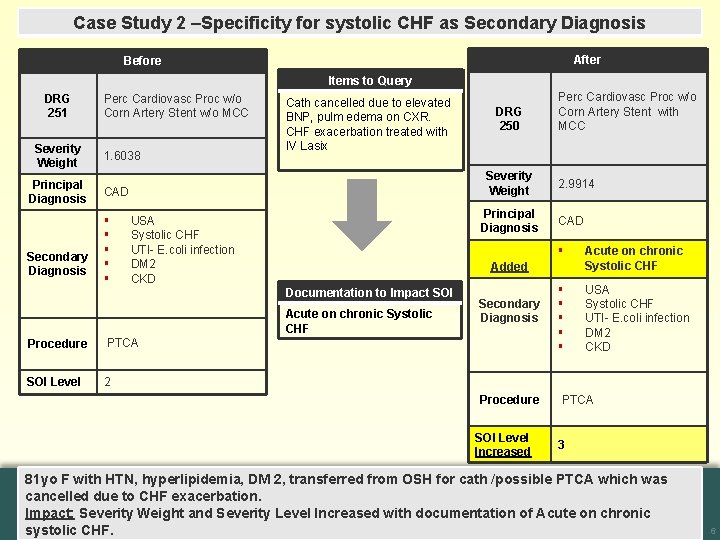
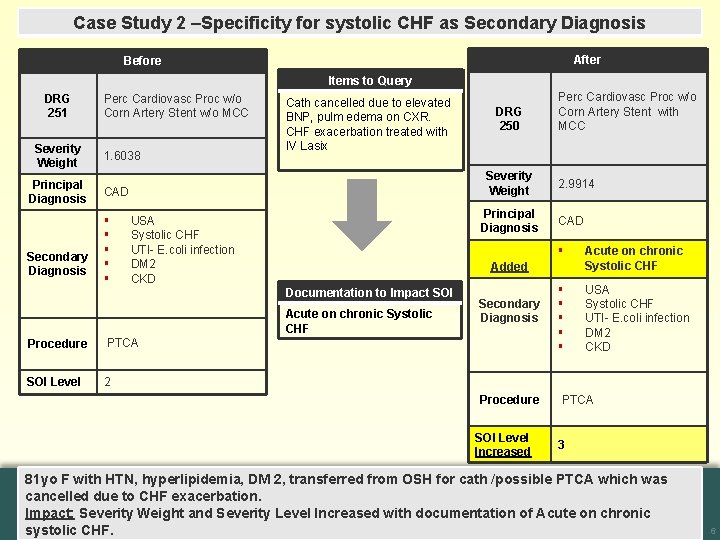
Case Study 2 –Specificity for systolic CHF as Secondary Diagnosis After Before Items to Query DRG 251 Severity Weight Principal Diagnosis Secondary Diagnosis Perc Cardiovasc Proc w/o Corn Artery Stent w/o MCC 1. 6038 Cath cancelled due to elevated BNP, pulm edema on CXR. CHF exacerbation treated with IV Lasix Severity Weight CAD § § § DRG 250 Principal Diagnosis USA Systolic CHF UTI- E. coli infection DM 2 CKD Acute on chronic Systolic CHF PTCA SOI Level 2 2. 9914 CAD § Acute on chronic Systolic CHF § § § USA Systolic CHF UTI- E. coli infection DM 2 CKD Added Documentation to Impact SOI Procedure Perc Cardiovasc Proc w/o Corn Artery Stent with MCC Secondary Diagnosis Procedure SOI Level Increased PTCA 3 81 yo F with HTN, hyperlipidemia, DM 2, transferred from OSH for cath /possible PTCA which was cancelled due to CHF exacerbation. Impact: Severity Weight and Severity Level Increased with documentation of Acute on chronic systolic CHF. 6
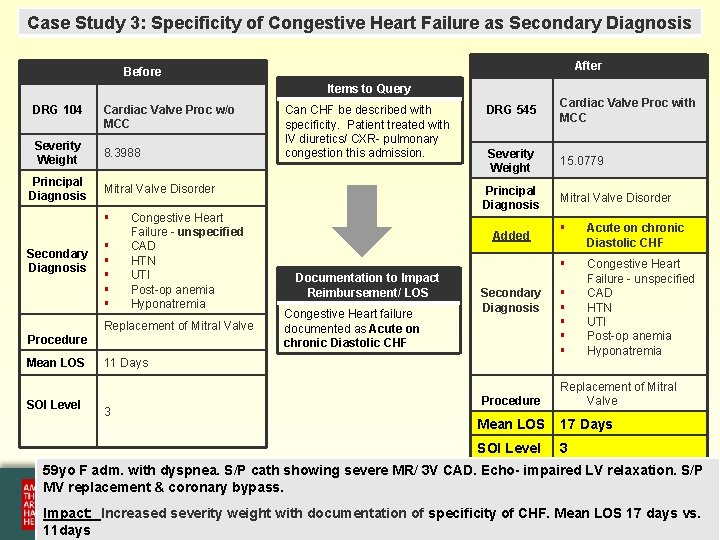
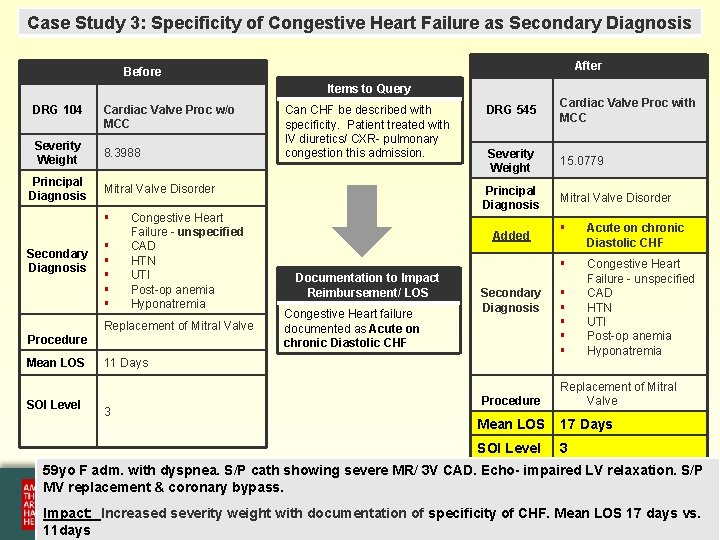
Case Study 3: Specificity of Congestive Heart Failure as Secondary Diagnosis After Before Items to Query DRG 104 Severity Weight Principal Diagnosis Cardiac Valve Proc w/o MCC 8. 3988 Mitral Valve Disorder § Secondary Diagnosis § § § Congestive Heart Failure - unspecified CAD HTN UTI Post-op anemia Hyponatremia Replacement of Mitral Valve Procedure Mean LOS SOI Level Can CHF be described with specificity. Patient treated with IV diuretics/ CXR- pulmonary congestion this admission. DRG 545 Cardiac Valve Proc with MCC Severity Weight 15. 0779 Principal Diagnosis Added Documentation to Impact Reimbursement/ LOS Congestive Heart failure documented as Acute on chronic Diastolic CHF Secondary Diagnosis 11 Days 3 Procedure Mitral Valve Disorder § Acute on chronic Diastolic CHF § Congestive Heart Failure - unspecified CAD HTN UTI Post-op anemia Hyponatremia § § § Replacement of Mitral Valve Mean LOS 17 Days SOI Level 3 59 yo F adm. with dyspnea. S/P cath showing severe MR/ 3 V CAD. Echo- impaired LV relaxation. S/P MV replacement & coronary bypass. Impact: Increased severity weight with documentation of specificity of CHF. Mean LOS 17 days vs. 11 days 7
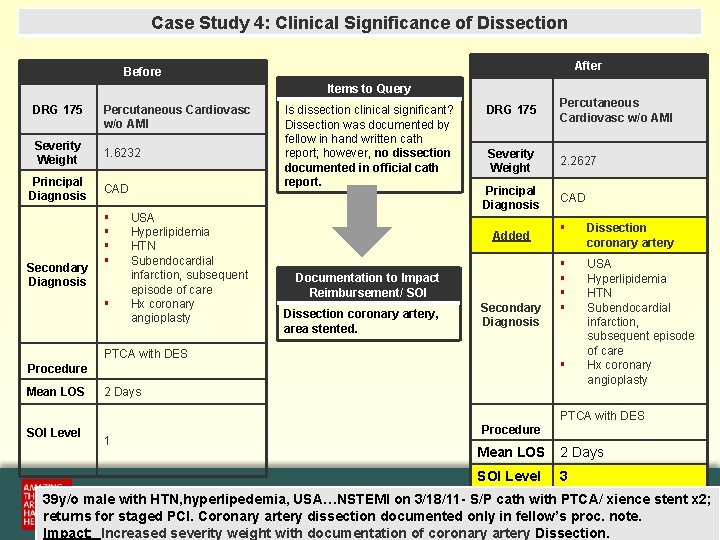
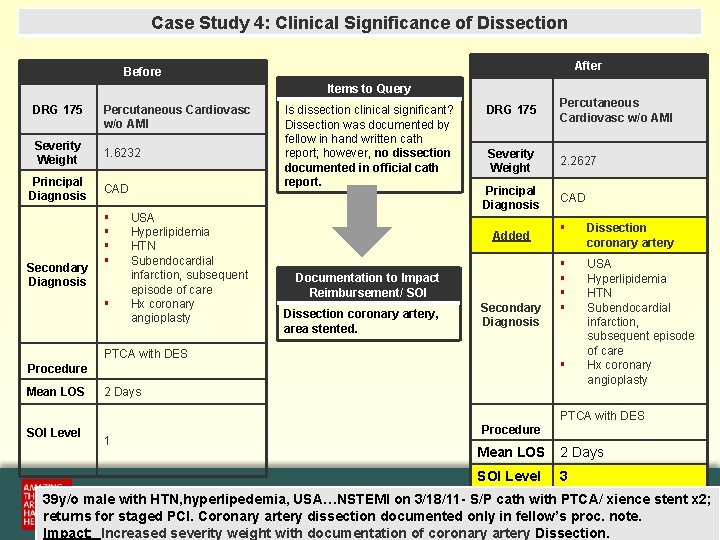
Case Study 4: Clinical Significance of Dissection After Before Items to Query DRG 175 Severity Weight Principal Diagnosis Secondary Diagnosis Percutaneous Cardiovasc w/o AMI 1. 6232 CAD § § § USA Hyperlipidemia HTN Subendocardial infarction, subsequent episode of care Hx coronary angioplasty Is dissection clinical significant? Dissection was documented by fellow in hand written cath report; however, no dissection documented in official cath report. DRG 175 Percutaneous Cardiovasc w/o AMI Severity Weight 2. 2627 Principal Diagnosis Added Documentation to Impact Reimbursement/ SOI Dissection coronary artery, area stented. Secondary Diagnosis PTCA with DES § Dissection coronary artery § § USA Hyperlipidemia HTN Subendocardial infarction, subsequent episode of care Hx coronary angioplasty § Procedure Mean LOS CAD 2 Days PTCA with DES SOI Level 1 Procedure Mean LOS 2 Days SOI Level 3 39 y/o male with HTN, hyperlipedemia, USA…NSTEMI on 3/18/11 - S/P cath with PTCA/ xience stent x 2; returns for staged PCI. Coronary artery dissection documented only in fellow’s proc. note. 8 Impact: Increased severity weight with documentation of coronary artery Dissection.
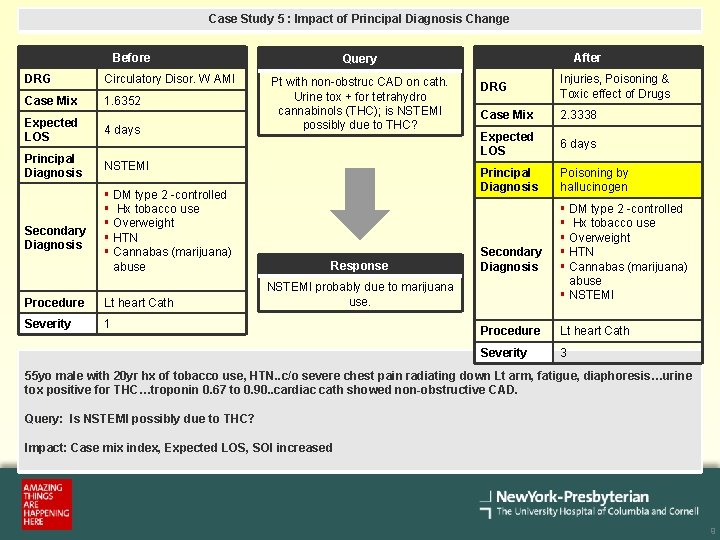
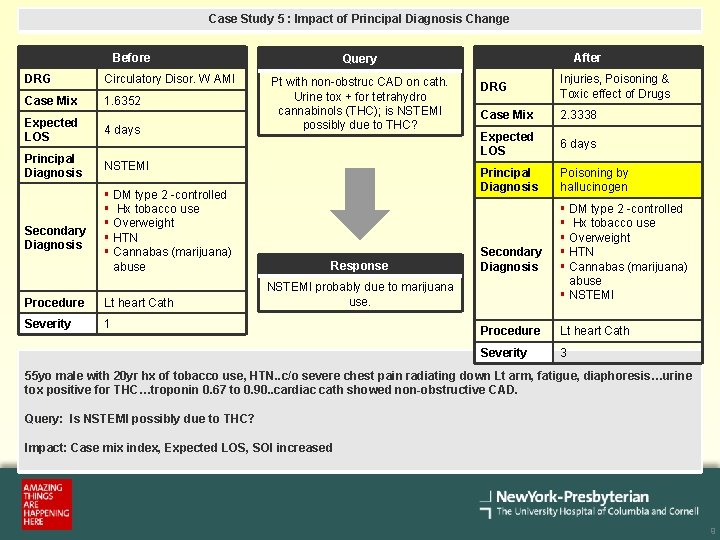
Case Study 5 : Impact of Principal Diagnosis Change Before DRG Circulatory Disor. W AMI Case Mix 1. 6352 Expected LOS 4 days Principal Diagnosis NSTEMI Secondary Diagnosis § DM type 2 -controlled § Hx tobacco use § Overweight § HTN § Cannabas (marijuana) abuse Procedure Lt heart Cath Severity 1 After Query Pt with non-obstruc CAD on cath. Urine tox + for tetrahydro cannabinols (THC); is NSTEMI possibly due to THC? Response DRG Injuries, Poisoning & Toxic effect of Drugs Case Mix 2. 3338 Expected LOS 6 days Principal Diagnosis Poisoning by hallucinogen Secondary Diagnosis NSTEMI probably due to marijuana use. § DM type 2 -controlled § Hx tobacco use § Overweight § HTN § Cannabas (marijuana) abuse § NSTEMI Procedure Lt heart Cath Severity 3 55 yo male with 20 yr hx of tobacco use, HTN. . c/o severe chest pain radiating down Lt arm, fatigue, diaphoresis…urine tox positive for THC…troponin 0. 67 to 0. 90. . cardiac cath showed non-obstructive CAD. Query: Is NSTEMI possibly due to THC? Impact: Case mix index, Expected LOS, SOI increased 9
Clinical Documentation Update Questions about this presentation? Please contact: § Thenia Nesbeth-Blades, RN, MSN Documentation Improvement Specialist thn 9003@nyp. org (212) 305 -0337 10
 Clinical documentation improvement for cardiology
Clinical documentation improvement for cardiology Healthcare service line management
Healthcare service line management Westcliffe cardiology service
Westcliffe cardiology service ........ is an alternative of log based recovery.
........ is an alternative of log based recovery. Outpatient clinical documentation improvement
Outpatient clinical documentation improvement Alcoac
Alcoac Golden thread clinical documentation
Golden thread clinical documentation Functional quadriplegia query examples
Functional quadriplegia query examples Clinical documentation challenges
Clinical documentation challenges Welcome to teen challenge uk - teen challenge uk
Welcome to teen challenge uk - teen challenge uk Cardiology procedures chapter 47
Cardiology procedures chapter 47 Accp cardiology prn
Accp cardiology prn