SURGERY OF THE PENIS AND URETHRA Congenital Anomaly








- Slides: 80
SURGERY OF THE PENIS AND URETHRA

Congenital Anomaly : §Agenesis Penis § Micropenis/Microphallus § Buried Penis (Concealed/Hidden/Trapped) § Phimosis § Paraphimosis § Hypospadias § Epispadias
Infection of the penis : balanopostitis Penile Cancer Urethritis Urethral Stone Urethral Strictures
Phimosis Description § inability to retract the foreskin § phimosis at the first few years is physiologic § the foreskin cannot be retracted after it has previously been retractable pathologic phimosis § by age 3. 5 years, most foreskins can be retracted
Epidemiology § 10 % of boys have non retractile foreskin § 1 % at puberty Signs and symptoms § discharge, soiling of undergarment § irritation, cracking, bleeding from foreskin Pathophysiology Physiologic phimosis § the glans penis is adherent to the prepuce in infants § glandular secretions and smegma facilitate separation
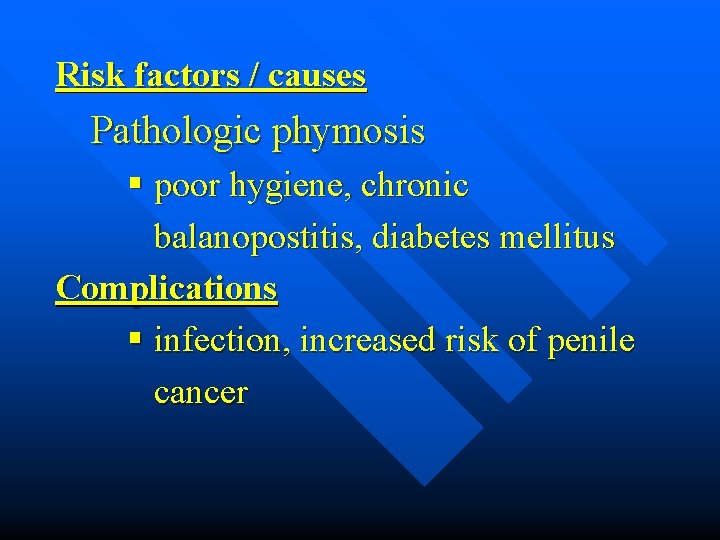
Pathologic phimosis § cicatricial preputial ring (from irritation result in inflammation and scarring) : poor local hygiene, chronic balanitis (Diabetes Mellitus), early forceful retraction of foreskin § balloon during voiding
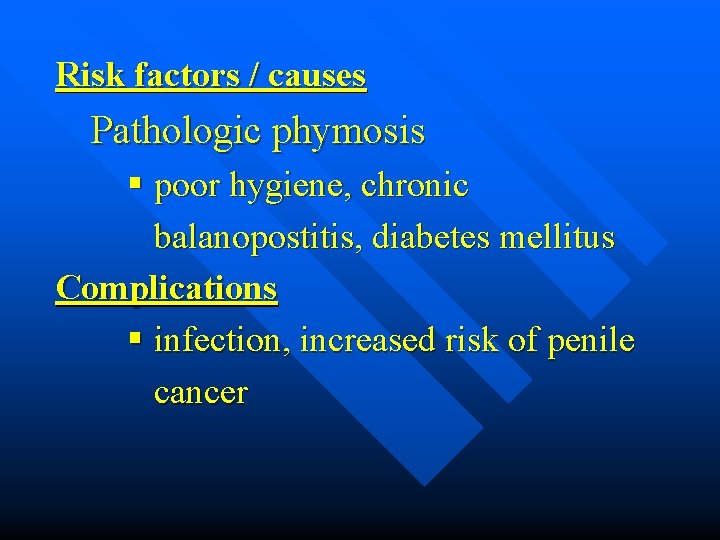
Risk factors / causes Pathologic phymosis § poor hygiene, chronic balanopostitis, diabetes mellitus Complications § infection, increased risk of penile cancer
Defferential Diagnosis § physiologic phimosis § pathologic phimosis § post circumcision phimosis
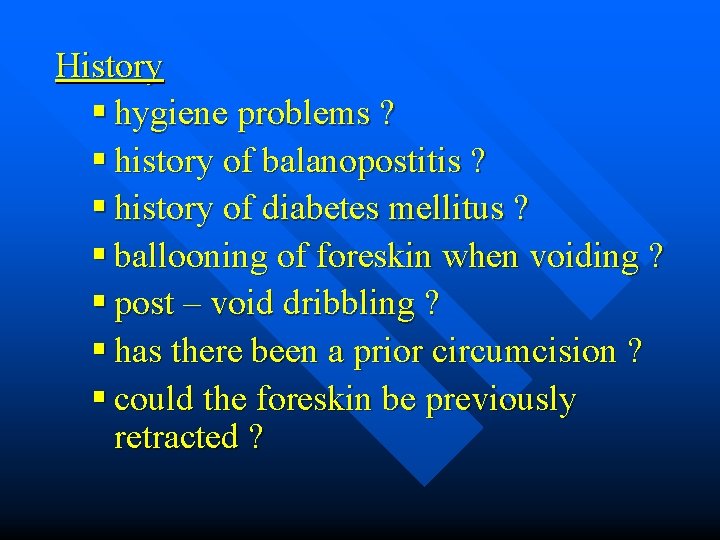
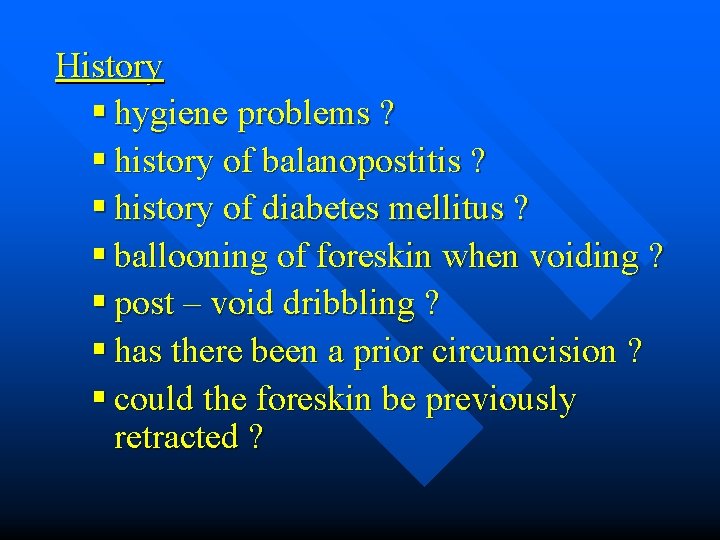
History § hygiene problems ? § history of balanopostitis ? § history of diabetes mellitus ? § ballooning of foreskin when voiding ? § post – void dribbling ? § has there been a prior circumcision ? § could the foreskin be previously retracted ?
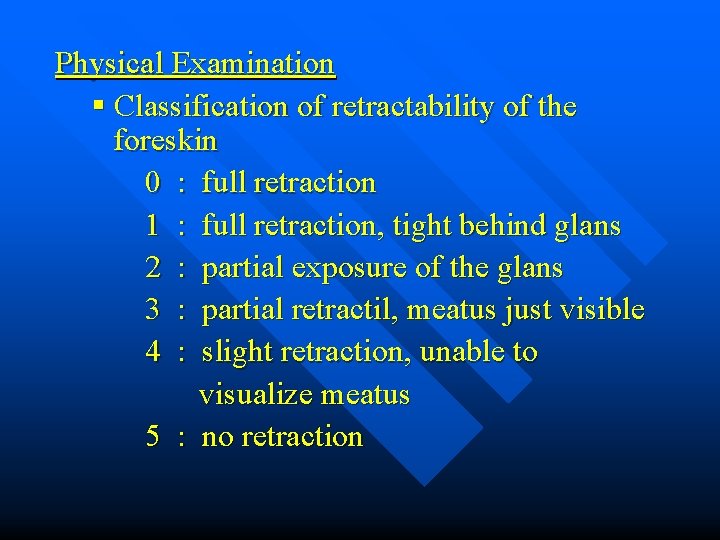
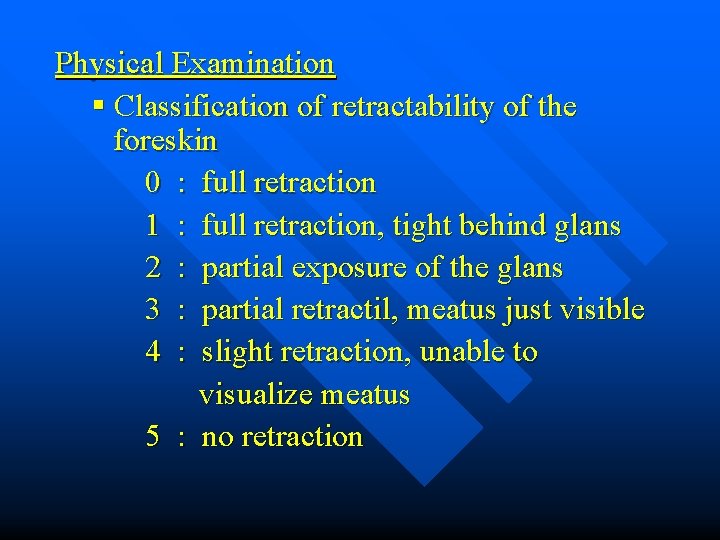
Physical Examination § Classification of retractability of the foreskin 0 : full retraction 1 : full retraction, tight behind glans 2 : partial exposure of the glans 3 : partial retractil, meatus just visible 4 : slight retraction, unable to visualize meatus 5 : no retraction


§ § § frenular lacerations preputial fissure cicatricial band inflammation or active infection “foreskins pearl” / smegma collection evidens of malignancy
Laboratory testing § serum glucose to evaluate for diabetes § culture and sensitivity of the subpreputial space Imaging : none Special studies : none
Physiologic phimosis § encourage good hygiene § gentle cleaning of smegma § instruct parents in gentle and gradual retraction of prepuce § never circumcise in patient with hipospadias, prepuce may needed for reconstruction
Pathologic phimosis § good hygiene § steroid ointment § infection ------ antibiotics systemic or topical
Treatment Medical § local steroid application ( topical vs injection ) § nonsteroidal drug application ( cream ) Surgical Phisiologic phimosis § circumcision ( not absolutely indicated ) § surgical correction of phimosis with preservation of the foreskin
Pathologic phimosis § circumcision ---- standard of care § preputial dilatation § dorsal / ventral slit § surgical correction with preservation of foreskin
Alternative therapies : none Patient education : none Monitoring post circumcision n Post circumcision phimosis ü inadequate primary procedure, post procedure scarring ü may occure with Gomco clamp, Guillotin techniques ü requires surgical revision ü glandular hyperaesthesias ( take several month after circumcision / epithelium develops squameus keratinized layer
n Complication ü ü ü of circumcision is low ( 0, 2 % - 0, 6 % ) hemorrhage infection avascular necrosis meatal stenosis fibrous bridge
ü urethrocutaneus fistula ü concealed penis ü penile denudation ü lymphedema penile • Prevention : none • Associated condition : diabetes mellitus
Paraphimosis Discription Painful swelling of the foreskin distal to a phimotic ring after retraction of the foreskin for a prolonged period.
Pathophysiology In children § § § A congenital narrowed preputial opening is present The foreskin is retracted behind the glans penis and not promptly reduced Entrapment in the coronal sulcus occurs secondary to swelling of the glans This lead to venous congestion, edema, and enlargement of the glans, followed by arterial occlusion and necrosis of the glans
In adults § Typically occurs in elderly men and may be associated with poor hygiene and/or chronic balanoposthitis § This iflamation leads to a contraction of the opening prepuce and forms a fibrotic ring of tissue
This in turn leads to constriction when the foreskin is retracted behind the glans § Result in venous congestion with edema § Failure to promptly reduce the paraphimosis can result in arterial occlusion and necrosis of the glans penis. This constitutes a urologic emergency §
Cause/risk factor § § § Phimosis Chronic balanoposthitis Chronic indwelling Foley catheterization and catheter changes § Patients requiring clean intermittent catheterization Complication § Necrosis of glans and distal urethra
Differential diagnosis § Balanitis § Balanoposthitis § Angioneurotic edema § Anasarca edema
Hystory § Has the patient been circumcised ? § Recurrent bouts of chronic balanitis ? § Chronic indwelling Foley catheterization ? § Clean intermittent catheterization ? § Diabetes mellitus : may be risk factor for phimosis § Phimosis ?
Physical examination § Edema and swelling of penile shaft proximal to the glans and corona § Thick phimotic ring proximal to corona § Late finding : swelling of the glans, venous congestion, necrosis of the glans penis.
Laboratory Testing § Not usually necessary § If surgery planned, preoperative laboratory studies, including coagulation factors Imaging: Chest film, if surgery planned General Measures § Considered urologic emergency § Delay in reducing paraphimosis can result necrosis of the glans
Medical § Gentle steady pressure to foreskin to decrease swelling (May use elastic wrap or Kerlix bandage) § Push the glans with thumbs, pulling the foreskin forward over the glans with the fingers ( Use the gauze pad to facilitate traction on the foreskin )

As an adjunct to simple reduction, a 25 – gauge needle is used to make multiple stab wounds in the edematous foreskin to help remove edema fluid May use 2 % lidocaine gel for local anesthetic § Hyaluronidase 1 cc ( 150 U/cc Wydase ) injected into the one or more sites in the edematous prepuce §
Surgical § Dorsal or ventral slit using 1 % lidocaine penile block § Convert to normal circumcision
Follow – Up § Circumcision should be performed when the edema/inflammation resolves § If there is no definitive treatment, paraphimosis tends to recur § Debridement of necrotic tissue is rarely indicated

Prevention When inserting or changing Foley catheters or performing clean intermittent catheterization, reduce the foreskin after the procedure is completed
Hypospadias Description § Common urogenital malformation in males, characterized by incompletely formed urethra wherein the misplaces meatus variably opens on the ventral aspect of the penis, scrotum, or perineum.
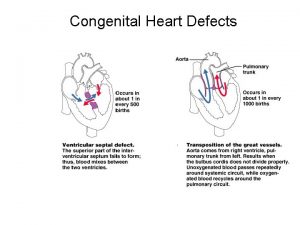
Malformation varies greatly in severity, ranging from the extreme form of perineal hypospadias with genital ambiguity to mild distal glans hypospadias. Commonly associated with chorde (abnormal curvature of the penis) in 50 % of the cases and/or meatal stenosis 30 % of cases.
Epidemiology § Incidence 1 in 300 live male births § More common in Whites than in Blacks, and in Italians and Jews than in other ethnic groups Genetics § Familial tendency 8 % of fathers of affected children have hypospadias, § 14 % of male siblings affected
Staging Classification § Based on location of meatus : glans, subcoronal, penile, penoscrotal, perineal § Distal hypospadias (subcoronal or penile) comprises 60 % of cases
Sign and Symptoms Associated anomalies § Undescended testicle: 9 % § Inguinal hernias: 9 % § Clinically significant upper tract anomalies ; rare Chordee § Chordee can occur without hypospadias, but is rare ( 0, 6 % )
Pathophysiology § Unknown, but several factors involves § Alterations of urethral fold closure result in hypospadias § Testosterone biosynthetic defects occur in half proximal hypospadias
§ Exposure to synthetic “ endocrine disrupters” that block the effect of testosterone is critical from 9 to 12 weeks gestation § Related to low birth rate in discordant monozygotic twins
Cause/Risk Factors § Unknown, some suggestion of familial risk Complications § Infertility § Psychological trauma ( Cosmetic )
Differential Diagnosis § Glandular § Subcoronal § Penile § Penoscrotal § Scrotal § Perineal

History : any family history ? Physical Examination § The urethral opening may be anywhere along the shaft of the penis or into the perineum, 62 % of the openings subcoronal or penile, 22 % penoscrotal angle, and 16 % scrotum or perineum § Severe proximal hypospadias may be confused with intersex disorders § The more proximal meatus, the more the ventral curvature (chordee) will be seen § Undescended testes and inguinal hernia
Laboratory testing § If surgery planned Imaging § Incidens of upper urinary tract abnormalities is rare. With more severe ( proximal ) cases of hypospadias, some recommended screening the upper tract
Treatment General measures § With any suspicion hypospadias, neonatal circumcision should not be perfomed § Many consider severe hypospadias to be a type of intersex disorder
Surgery Treatment of the hypospadias is surgical repair and the timing of repair is best § between 6 and 18 months § Current techniques are superior than the older techniques § Short – term follow – up examinations for development of fistulas/stricture Alternative therapies is psychosocial support as part of overall care
Epispadias Description § Development abnormality wherein the urethra opens on the dorsum of the penis.
Epidemiology § 1 in 117. 000 newborn boys § 1 in 484. 000 newborn girls § Male – to – Female ratio : 5 : 1
Signs and symptoms Male § Urethra opens anywhere from under pubic to the tip of penis § The complete or penopubic epispadias is most common
Female § Urethra opens from bladder neck to tip of urethra § Most severe and common type § Labia may obscure the epispadias in female
Pathophysiology § Absence of urinary sphincters in complete type(penopubc) in males and type III in female § Short, widened penis with dorsal chordee
§ Urethra most commonly as base of penis under pubic, opening can be on shaft or also on glans § Bifid clitoris, separated and rudimentary labia minora § Wide pubic diastasis; usually not as wide as in bladder exstrophy

Cause/Risk Factor § Unknown Complication § Urinary incontinence § Upper tract damage § Infertility
Differential diagnosis § Classic bladder exstrophy § Lesser degrees of epispadias History § Family history of epispadias
Physical examination § Pubic diastasis § Position of testes § Present of any degree of bladder prolapse or exstrophy
Laboratory testing § CBC, serum electrolytes Imaging § Plain X – Ray of pelvis to determine pubic diastasis § Renal ultrasound to assess presence of two kidneys and presence/absence hydronephrosis
Treatment General measure : Careful, overall examination of infant Surgical Objectives § Preservation of upper urinary tract § Reconstruction of functional and cosmetically acceptable external genitalia § Achievement of urinary continence
Female § Repair of urethra and genital reconstruction at around 12 months of age § Bladder neck repair
Male § Epispadias repair at 6 – 12 months of age after testosterone stimulation ( 3 mg/kg IM 2 weeks before surgery ) § Bladder neck repair at 4 to 5 years of age when bladder capacity is adequate § and child is participate in postoperative voiding program
Follow - up after epispadias repair § Urethral stent removed 10 – 12 days after surgery § Renal and bladder ultrasound at 4 months after surgery § Urine cultures at three monthly interval § Yearly cytoscopies and bladder capacity measurement under anesthesia until bladder capacity adequate for bladder neck repair
Follow - up for bladder neck repair § Clamp the suprapubic tube at 3 weeks after surgery and begin voiding trial § Removal of suprapubic tube when urine residuals are lees than 15 cc and child is voiding well § Cytoscopy and placement of small (8 Fr) urethral catheter if child cannot voiding well
§ Renal and bladder ultrasound prior to removal of suprapubic tube and again a 3 and 12 month after surgery § Antibiotic prophylaxis until follow – up shows nonreflux and child is voiding well
Urethral Stricture Description § narrowing of the urethral lumen / a scar within the urethra § 60 – 70 %, in the bulbar urethra

Etiology 1. Congenital : rare, soft, often without spongiofibrosis 2. Infection / inflammation : § Urethritis ( GO, TBC and Clamydial ) § may involve long segment, include bulbar urethra.
3. Traumatic § the most common type § blunt perineal “ straddel injury “ where urethra is trapped against the symphysis pubis § usually partial tear
4. Iatrogenic : instrumentation ( urethrocystoscopy, transurethral resection prostatectomy, catheterization ), usually found at meatus or penoscrotal junction.
n pelvic fracture : traffic accidents or industrial injuries ü 10 %, pelvic fracture will have urethral injury, which may vary from simple contusion through partial tear to complete transection with separation of the urethral end.
n penetrating : gunshot wounds ü degree of tissue injury according to projectile and velocity
Symptoms and Signs § decrease urinary stream ----more common § spraying, double stream § postvoiding dribbling § mild dysuria § hematuria § urinary tract infection § urethral bleeding
§ § § § epididymitis chronic prostatitis cystitis urethrocutaneus fistula induration in the area of the stricture periurethral absces palpable bladder ( urinary retention )
Physical examination § usually no specific findings § evidence of epididymitis § palpable bladder § small meatal
Imaging § retrograde urethrography § urethrogaphy bipolar/voiding urethrocystography § IVU ( upper urinary tract evaluation and pelvic bone)
Special studies § Endoscopy : urethroscopy allows direct visualization of the stricture § Uroflowmetry : may indicate obstructive pattern
Laboratory testing § nothing special, except as indicated ( urine culture / infection ) § blood analysis for preoperative care
Treatment § Conservative : urethral dilatation ( cause false passages ) § Surgical ü Endoscopy : Internal urethotomy (Sachse) or blind Otis ü Conventional (open surgical) : • meatal stricture : meatotomy, meatoplasty • long urethral strictures : two and multiple stage repairs
 Mcgovern nipple
Mcgovern nipple Craneosquisis
Craneosquisis Epithelium of urethra
Epithelium of urethra Length of male urethra
Length of male urethra Male urethra anatomy
Male urethra anatomy Curiculum vital
Curiculum vital Hypospedious
Hypospedious Membranous urethra
Membranous urethra Vaskularisasi ginjal
Vaskularisasi ginjal What does sperm contain
What does sperm contain Urethra
Urethra Stricture treatment in pune
Stricture treatment in pune Indications for prostatectomy
Indications for prostatectomy Puberty age
Puberty age Where does meiosis occur? *
Where does meiosis occur? * Vesicourethral canal
Vesicourethral canal Urogenital sinus
Urogenital sinus Mesosalpinx
Mesosalpinx Renal columns
Renal columns Q tip test urethra
Q tip test urethra Karunkula uretra
Karunkula uretra Urine formation
Urine formation Urethra pars bulbosa
Urethra pars bulbosa Pg
Pg Membranous urethra
Membranous urethra How does hiv get into the urethra
How does hiv get into the urethra Trabecula
Trabecula Male accessory glands
Male accessory glands Ostium urethra externum nereye açılır
Ostium urethra externum nereye açılır Aa. helicinae
Aa. helicinae Anterior urethra
Anterior urethra Male reproductive organ
Male reproductive organ Urethrorhagia
Urethrorhagia N
N кагами-огата
кагами-огата Congenital pneumonia
Congenital pneumonia Piciorul stramb congenital
Piciorul stramb congenital Glaucoma management
Glaucoma management Differential cyanosis
Differential cyanosis Congenital rubella syndrome
Congenital rubella syndrome Congenital malformations
Congenital malformations Congenital voice disorders
Congenital voice disorders Hormone type 4
Hormone type 4 Cyanotic vs acyanotic
Cyanotic vs acyanotic Juxtaductal position
Juxtaductal position Congenital fibrosis of the extraocular muscles
Congenital fibrosis of the extraocular muscles Most common congenital anomalies
Most common congenital anomalies Non classical adrenal hyperplasia
Non classical adrenal hyperplasia Congenital rubella syndrome triad
Congenital rubella syndrome triad Endocardial cushion defects
Endocardial cushion defects Congenital rubella syndrome triad
Congenital rubella syndrome triad Congenital adrenal hyperplasia characteristics
Congenital adrenal hyperplasia characteristics Potter face oligohydramnios
Potter face oligohydramnios Congenital hydronephrosis
Congenital hydronephrosis Congenital
Congenital Virilisation in females
Virilisation in females Congenital toxoplasmosis
Congenital toxoplasmosis Icd 10 multiple congenital anomalies
Icd 10 multiple congenital anomalies Congenital toxoplasmosis
Congenital toxoplasmosis Canadian congenital heart alliance
Canadian congenital heart alliance Congenital glaucoma triad
Congenital glaucoma triad Vulvodynia
Vulvodynia Vaginal agensis
Vaginal agensis Farah garmany
Farah garmany Congenital diaphragmatic hernia
Congenital diaphragmatic hernia Congenital heart
Congenital heart Mononucleosis
Mononucleosis Causes of congenital anomalies
Causes of congenital anomalies Spina bifida
Spina bifida Surgical neck
Surgical neck Mineralocorticoid function
Mineralocorticoid function Thyrotoxicosis mnemonic
Thyrotoxicosis mnemonic Barlow y ortolani
Barlow y ortolani Klisic test
Klisic test Congenital heart defect
Congenital heart defect Congenital
Congenital Congenital amusia
Congenital amusia Hutchinson triad
Hutchinson triad Anal advancement flap
Anal advancement flap Erythroplasia
Erythroplasia Congenital
Congenital