Mullerians Anomaly Congenital anomalies of the vagina Congenital





- Slides: 75

Mullerians Anomaly �Congenital anomalies of the vagina �Congenital cervical anomalies �Congenital anomalies of the uterus 2
Case 1 � 16 y virgin �Amenorrhea and chronic Cyclic pain from 1 years ago �V/S stable �Abd. Exam: Large uterus to umbilicus without tenderness �Rectal exam: palpation of cervix �Sono: normal adnexa & Large uterus : hematocolpus �Perineal Exam: Imperforated hymen 3
congenital anomalies of the vagina �The sinovaginal bulbs are two solid evaginations originating in the urogenital sinus at the distal aspect of the müllerian tubercle. �The sinovaginal bulbs proliferate into the caudal end of the uterovaginal canal to become a solid vaginal plate. �The lumen of the lower vagina is then formed by degeneration of the central cells of this vaginal plate, which occurs in a cephalad direction. � Canalization is complete by 20 weeks. 4
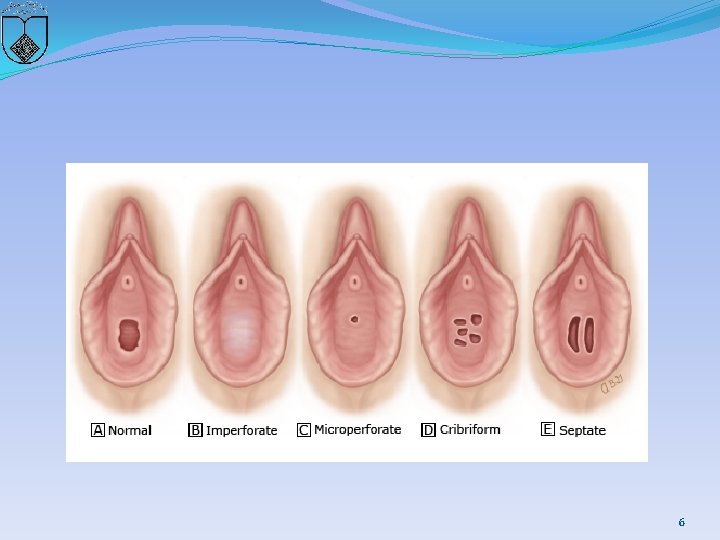
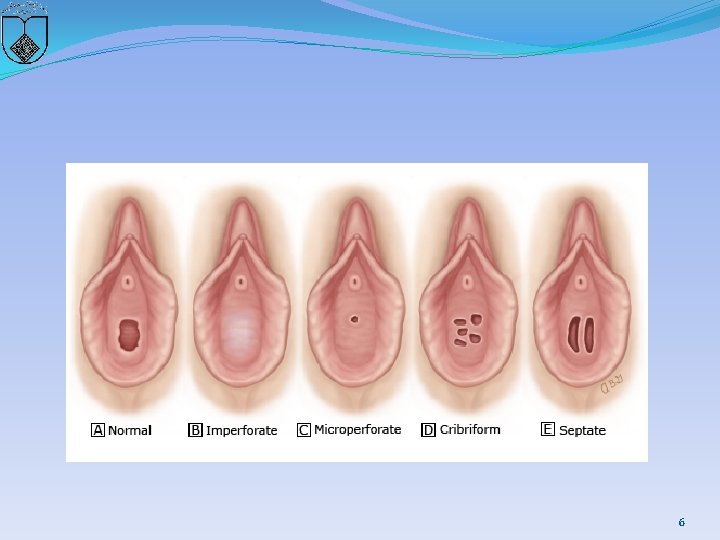
�Hymen � The vaginal lumen is separated from the urogenital sinus by the hymenal membrane. � The hymen usually ruptures before birth due to degeneration of the central epithelial cells. �However, a thin fold of mucous membrane persists around the vaginal introitus. �The hymenal membrane consists of fibrous connective tissue attached to the vaginal wall. �Hymenal anomalies are derived from incomplete degeneration of the central portion of the hymen. � These anatomic variants include imperforate, microperforate, septate, and cribriform hymens 5
6
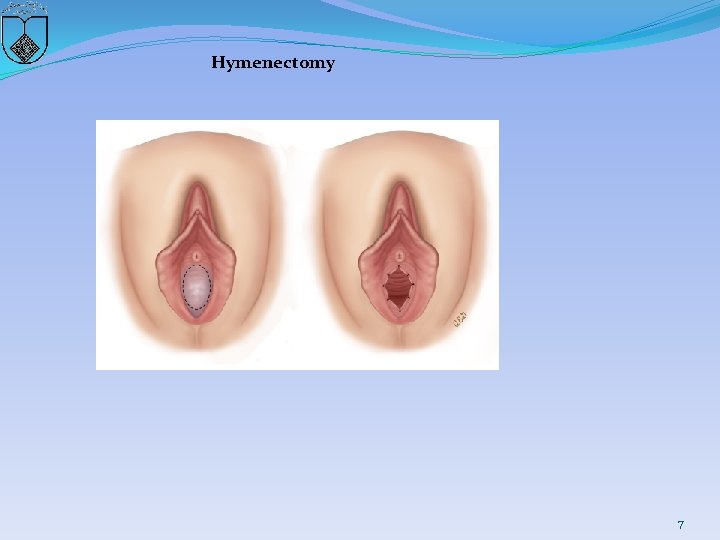
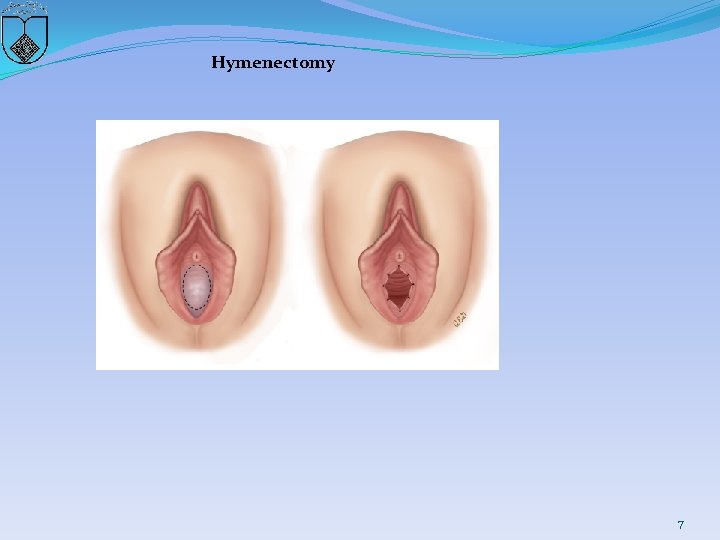
Hymenectomy 7
ANOMALIES OF THE VAGINA �Transverse vaginal septum �Longitudinal vaginal septum � Obstructed hemi-vagina �Vaginal agenesis �Agenesis of the lower vagina �Vaginal cysts 8
Transverse vaginal septum � 1 in 30, 000 to 1 in 80, 000 women � 46 % in the upper vagina � 35 to 40 % in the middle portion � 15 to 20 % in the lower vagina �less than 1 centimeter in thickness �have a fenestration and are thus not completely obstructed. �Children may present with mucocolpos, whereas adolescents can develop hematocolpos 9
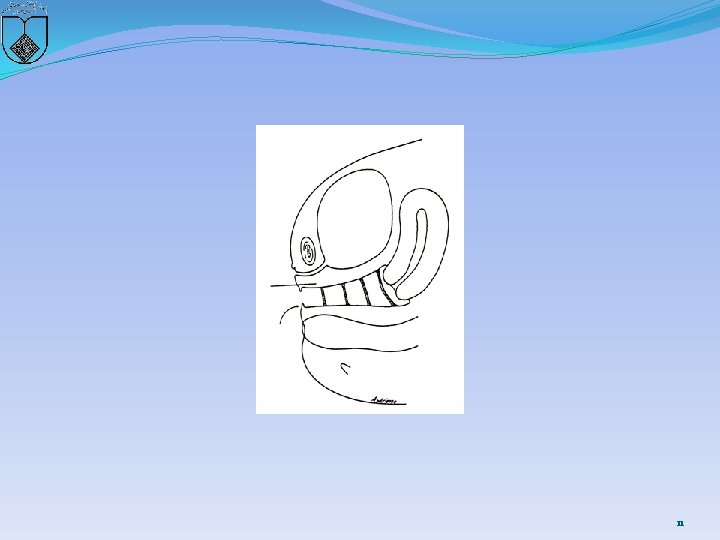
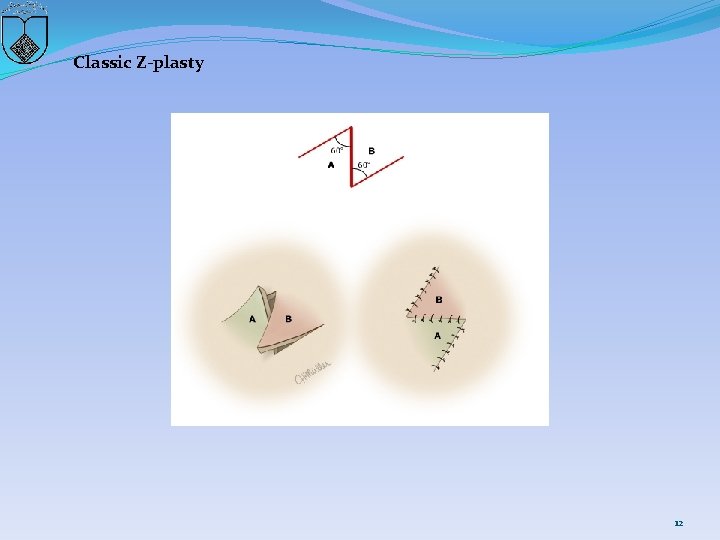
Ultrasonographic or magnetic resonance imaging � helps to define the location and thickness of the septum and to differentiate between a high septum and congenital absence of the cervix � A septum : excise and repair � Reanastomosis is easier if the upper vagina has been distended with menstrual blood products, as this acts as a natural tissue expander to increase the amount of upper vaginal tissue available for the reanastomosis. � preoperative use of vaginal dilators may thin the septum and facilitate reanastomosis. � A Z-plasty technique � Approximately 36 pregnancies have been reported in women with transverse septa. One-half had planned cesarean delivery, most of the rest had incision or instrumental dilation during labor, and a few underwent incision before pregnancy. Outcomes were generally good. 10
11
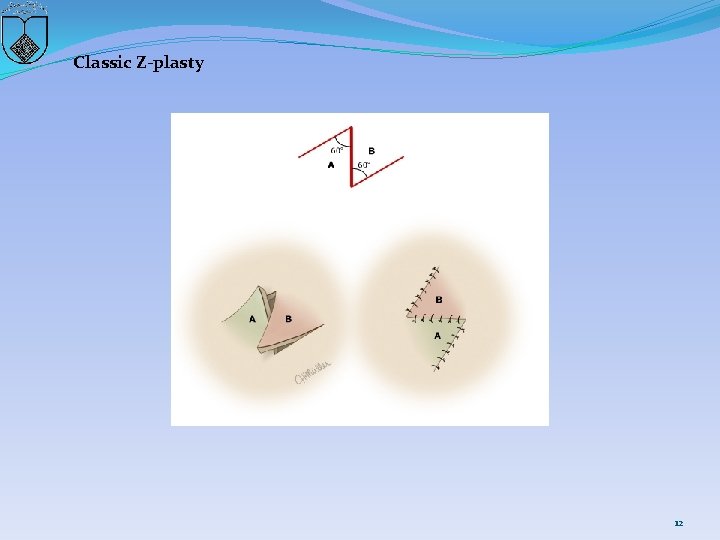
Classic Z-plasty 12
Longitudinal vaginal septum �associated with uterine anomalies, such as septate uterus and uterus didelphys �septum partial or complete � Symptom: dyspareunia or asymptomatic. �imaging of the upper reproductive tract �septal tissue should be excised �Surgery is not required in asymptomatic women with a longitudinal vaginal septum, but will facilitate vaginal delivery. 13
obstructed hemi-vagina �associated with ipsilateral renal agenesis. �pain, pus from microcommunication from the obstructed side to the non-obstructed vagina, and rarely cyclic peritonitis �surgical correction due to pain, increased risk of infection, and retrograde menses. �The obstructed vagina is entered, the fluid is drained, and then the vaginal tissue between the two vaginas is resected. �Great care is taken to avoid the bladder, rectum and the cervixes. � The two cervixes may be at different levels; therefore, the tissue between them should be left in place so as not to compromise their blood supply. 14
Vaginal agenesis �müllerian aplasia or Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome, refers to congenital absence of the vagina with variable uterine development � incidence 1 in 5000 (range 1 per 4000 to 10, 000 females) �usually accompanied by cervical and uterine agenesis � however, 7 to 10 percent of women have functional endometriu � 25 to 50 percent urologic anomalies � 10 to 15 percent skeletal anomalies 15
�normal ovaries and ovarian function, thus they develop normal secondary sexual characteristics �primary amenorrhea at 15 to 17 years of age �second most common cause of primary amenorrhea, after gonadal dysgenesis �Most patients have a rudimentary nonfunctioning uterus, but 2 to 7 percent have a uterus with functioning endometrium and may present with cyclic or chronic abdominopelvic pain secondary to hematocolpos, hematometra, hematosalpinx, or endometriosis 16
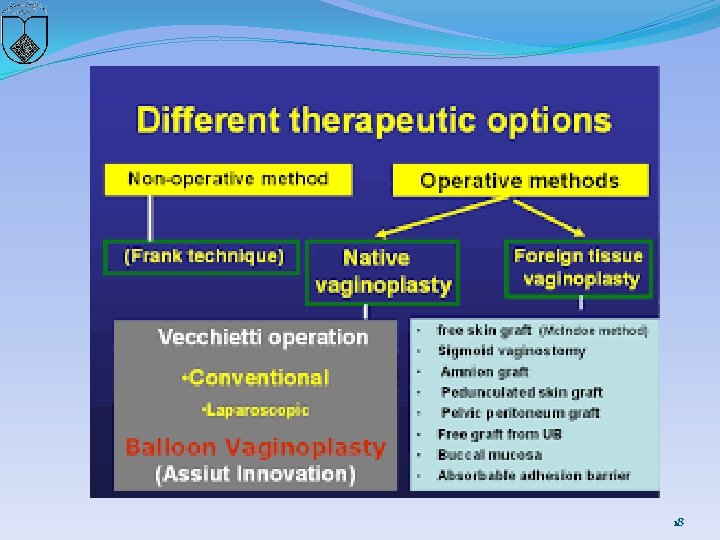
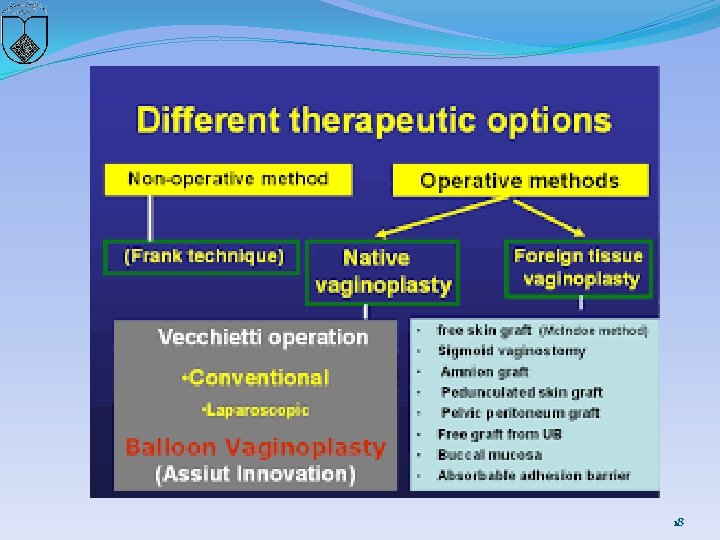
�first line for therapy : Nonsurgical treatment with selfdilatation �Surgery: if nonsurgical therapy fails or, if after extensive counseling, a patient elects a surgical approach �Mc. Indoe procedure �Williams vaginoplasty �Sigmoid vaginoplasty �Vecchietti procedure �Davydov procedure 17
18
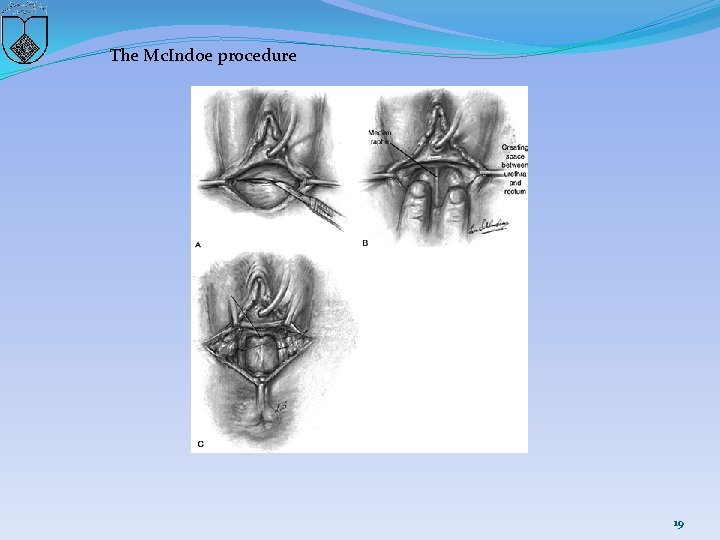
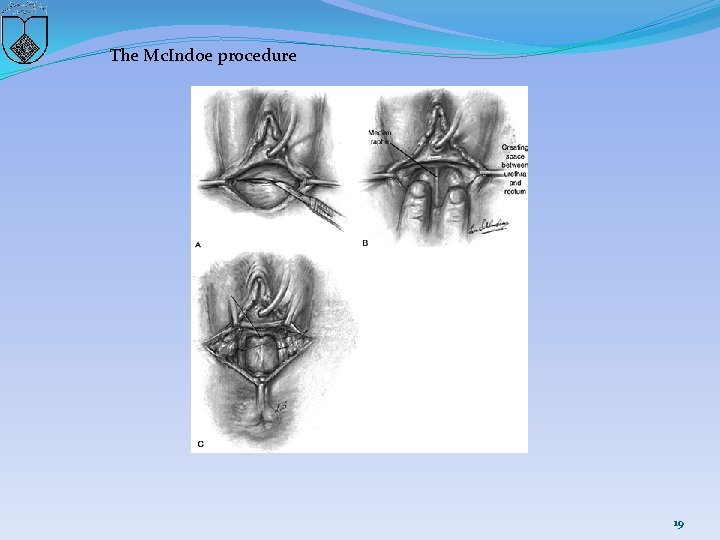
The Mc. Indoe procedure 19
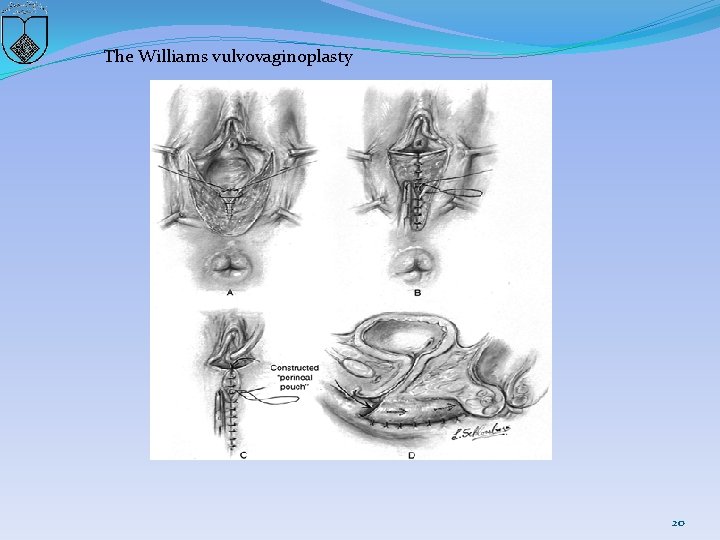
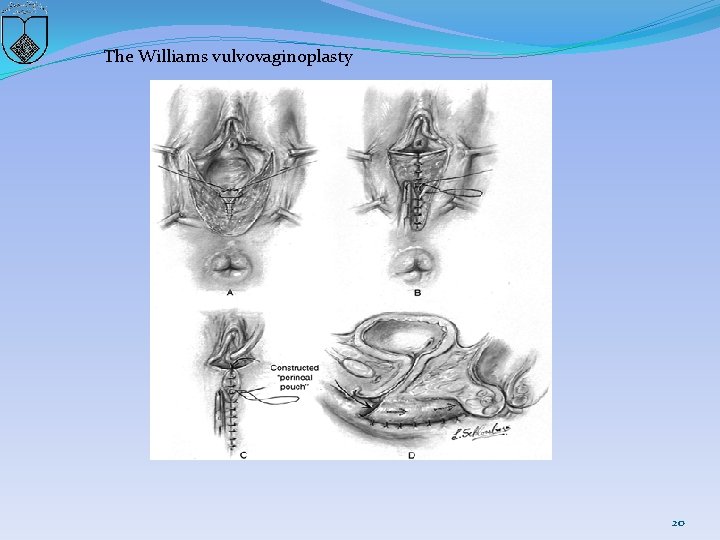
The Williams vulvovaginoplasty 20

21
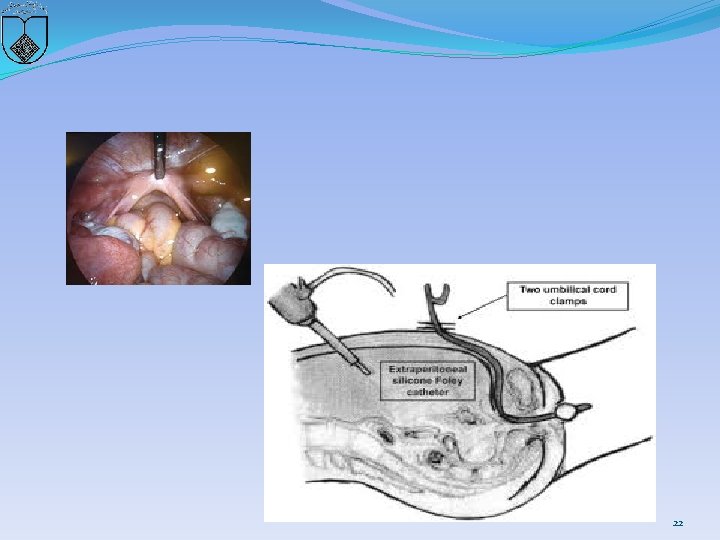
22
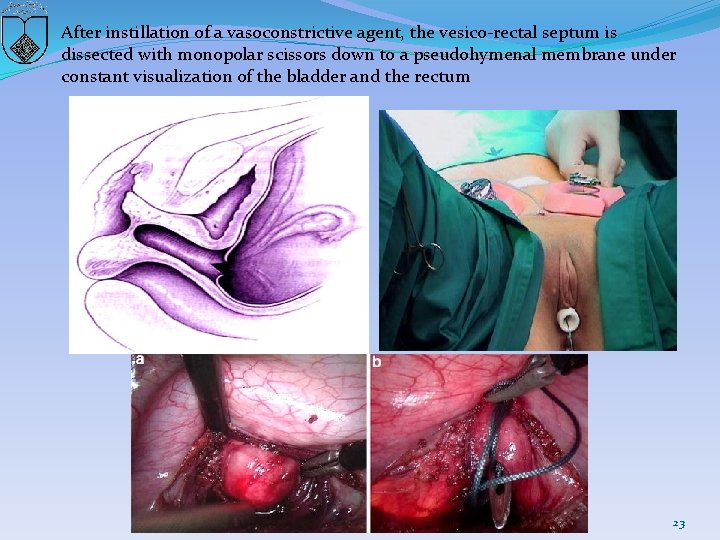
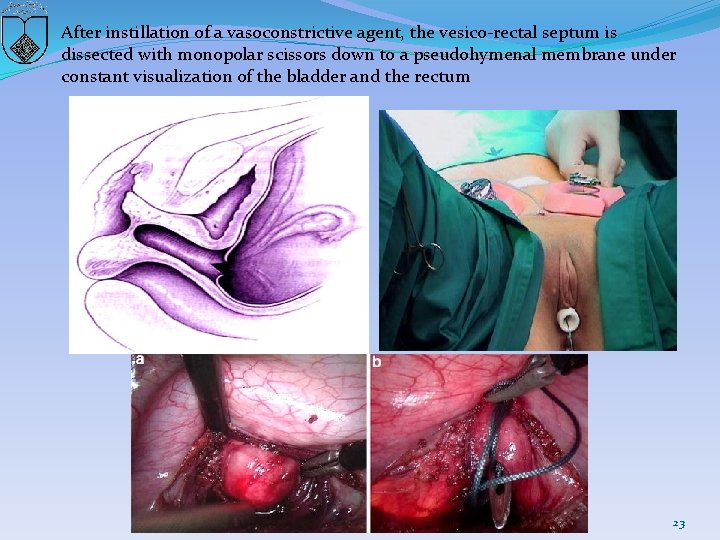
After instillation of a vasoconstrictive agent, the vesico-rectal septum is dissected with monopolar scissors down to a pseudohymenal membrane under constant visualization of the bladder and the rectum 23
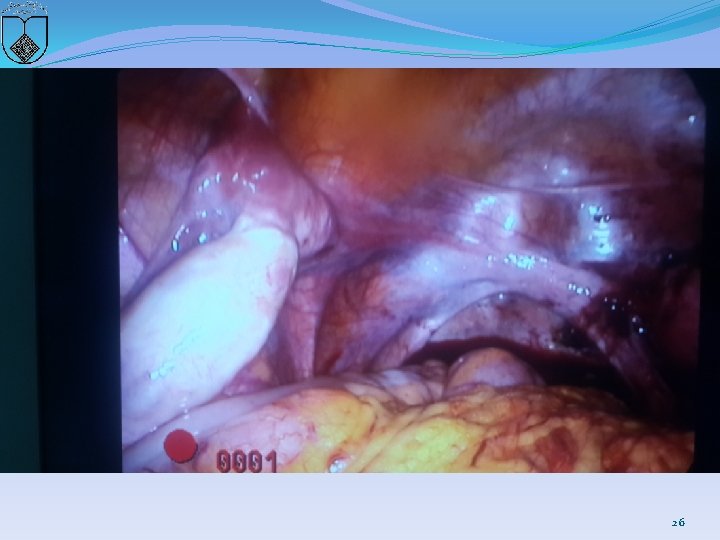
Case 2 � 19 y Married without coitus �C. C: Primary amenorrhea and chronic pelvic pain �Lab test and karyotype was normal �Rectovaginal exam: 3 -4 cm vaginal pouch & don’t touch cervix �Sono: unilateral Rudimentary horn without endometrial line and NL ovaries �MRI: …Cervix was not seen, NL Kidny �Diag Laparoscopy 24

25
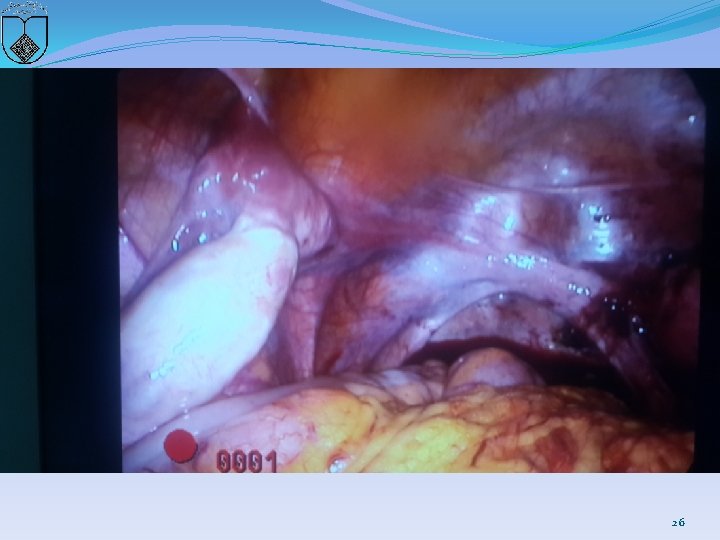
26
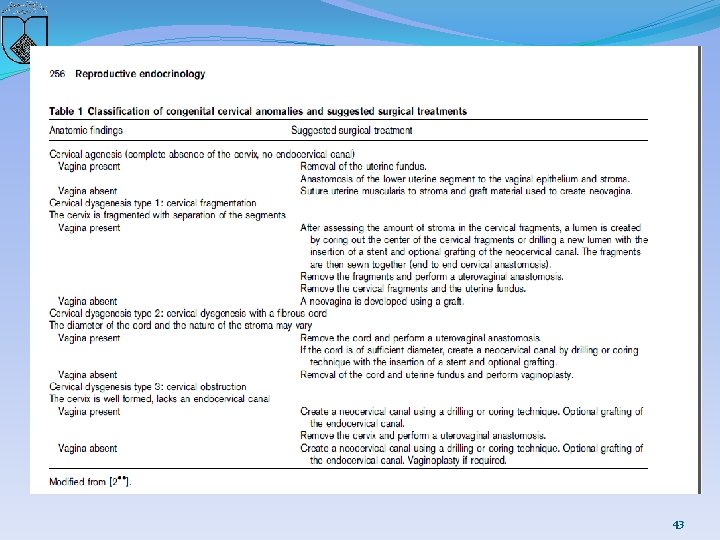
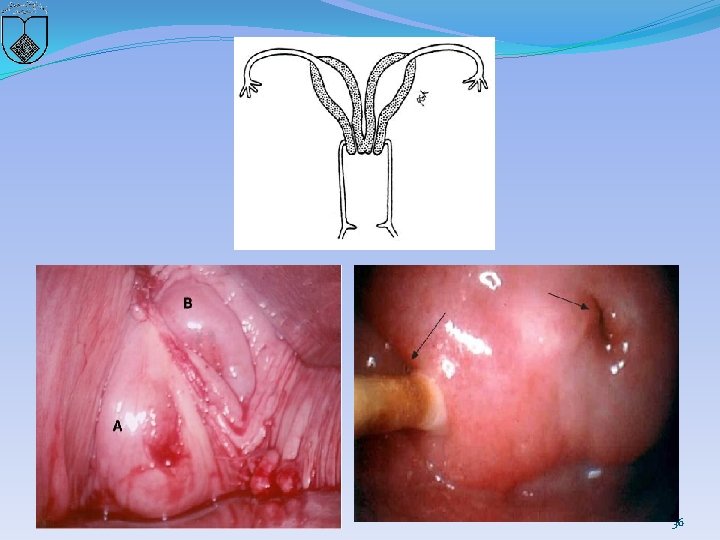
Congenital cervical anomalies �If one or both müllerian ducts fail to fuse, or if development of one or both ducts does not occur, or is incomplete, duplication or agenesis of the cervix can occur. � Coexistent anomalies of the vagina, uterus, and urinary tract are common since anomalies of the mesometanephric duct frequently occur in association with those of the müllerian ducts 27
Duplication of the cervix �Two distinct cervices or two fused cervices �It may be difficult to differentiate and determine if there are two separate cervices or if there is a single cervix with a septum. �Nonobstructive duplication of the cervix is usually asymptomatic and does not require intervention. �Obstructive lesions require surgical intervention (described below) if hematometra or pyometra occurs. � In cases of cervical duplication with a longitudinal vaginal septum or an obstructed hemivagina, great care should be taken when removing the septum so as not to compromise the blood supply to the individual cervices 28
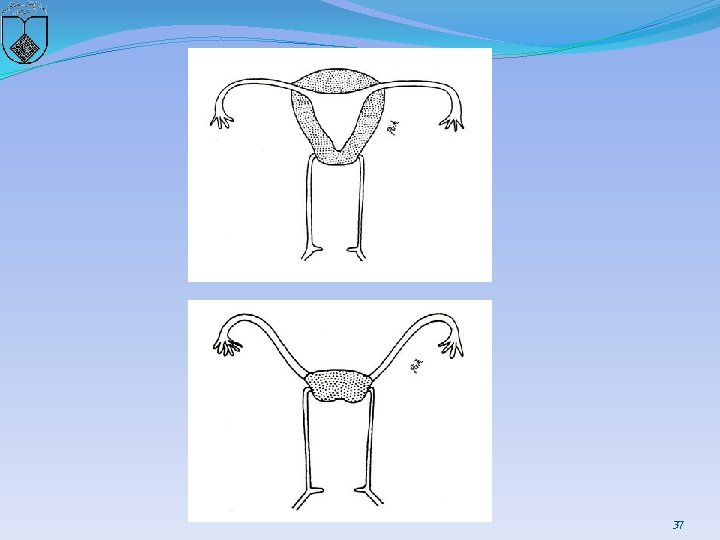
Agenesis/hypoplasia �Cervical agenesis and hypoplasia are rare. �With complete agenesis, both the cervix and the upper vagina must be absent, as the proximal portion of the vagina does not form in the absence of a cervix during embryonic development �When the cervix is present, but hypoplastic, the vagina can be normal �Cervical hypoplasia is typically recognized at menarche �Adolescents may present with primary amenorrhea, cyclic or chronic abdominopelvic pain, or a pelvic mass (from hematometra). �Imaging with ultrasound and magnetic resonance are helpful in defining the anatomy 29
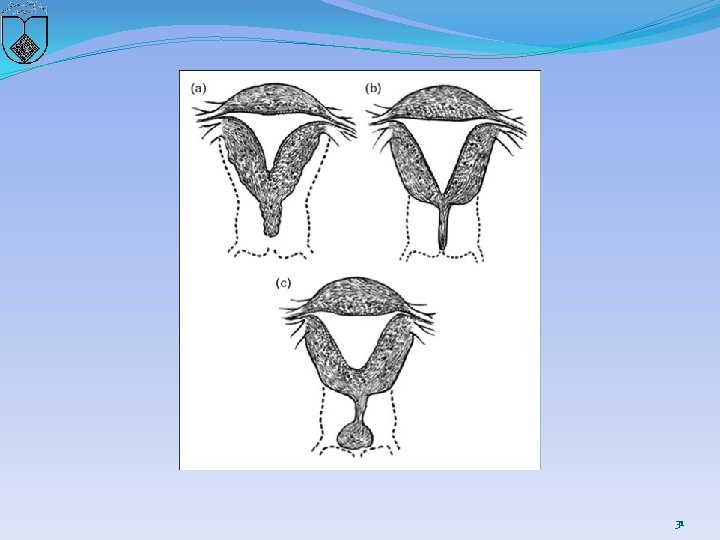
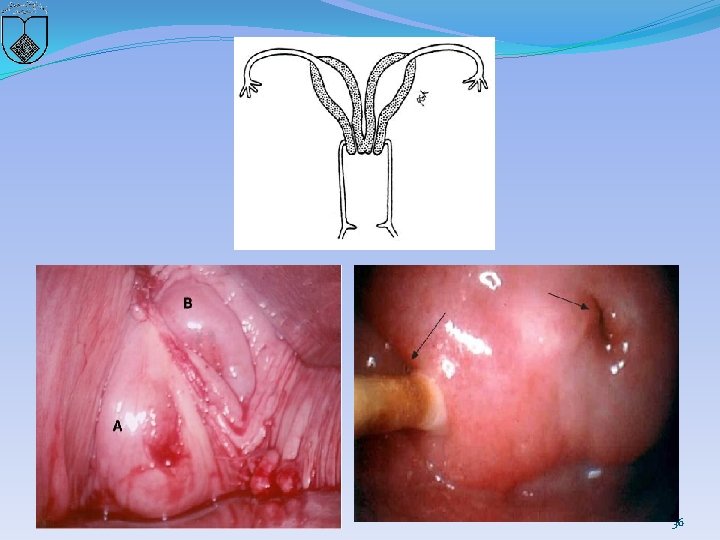
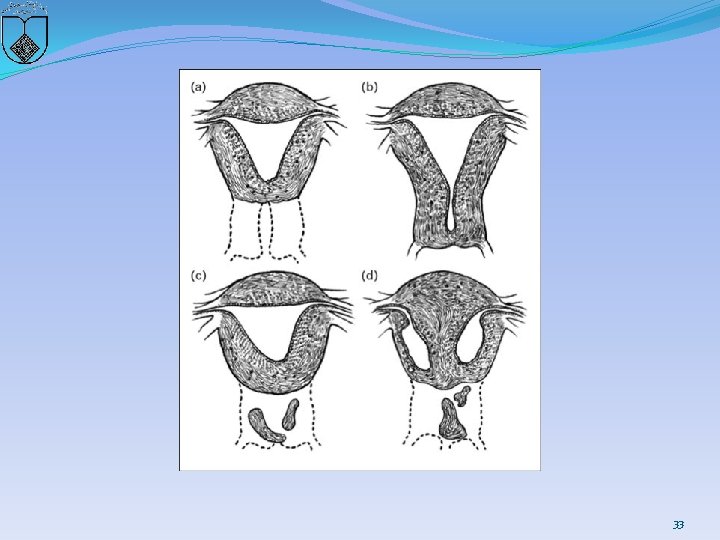
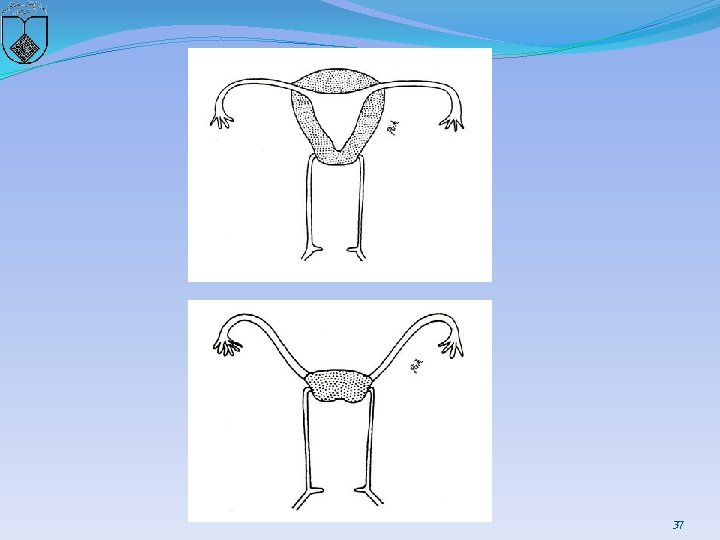
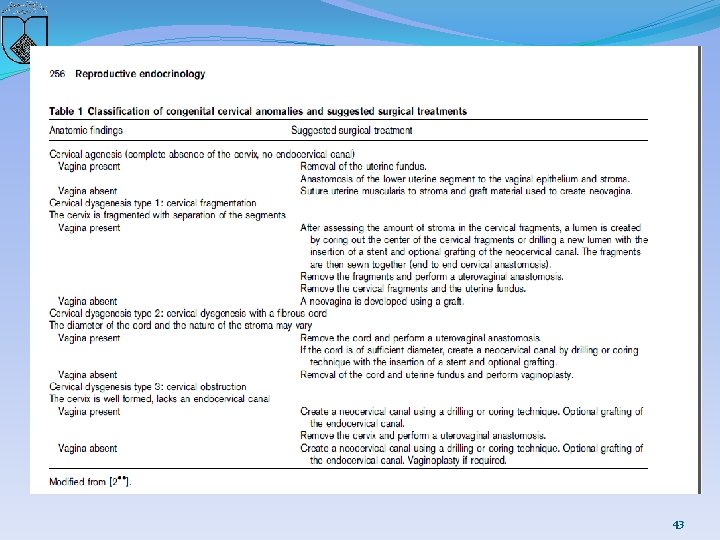
Two basic categories of cervical anomalies �first type: � cervical aplasia, lack a uterine cervix �lower uterine segment narrows: terminate in a peritoneal sleeve at a point well above the normal communication with the vaginal apex 30
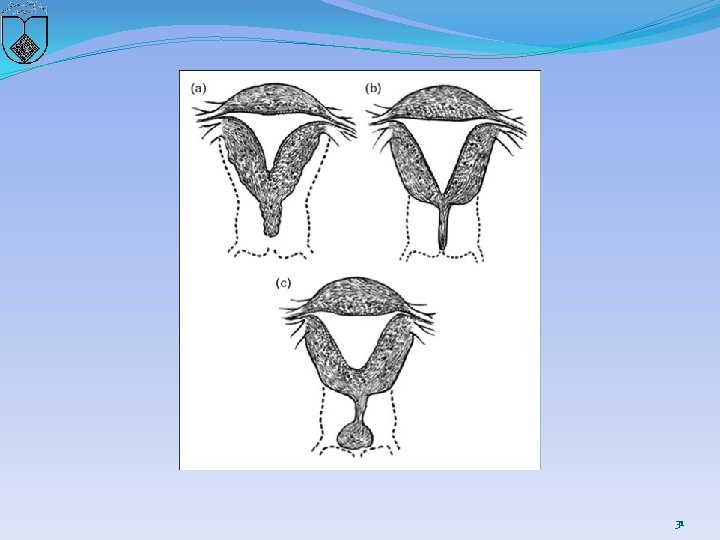
31
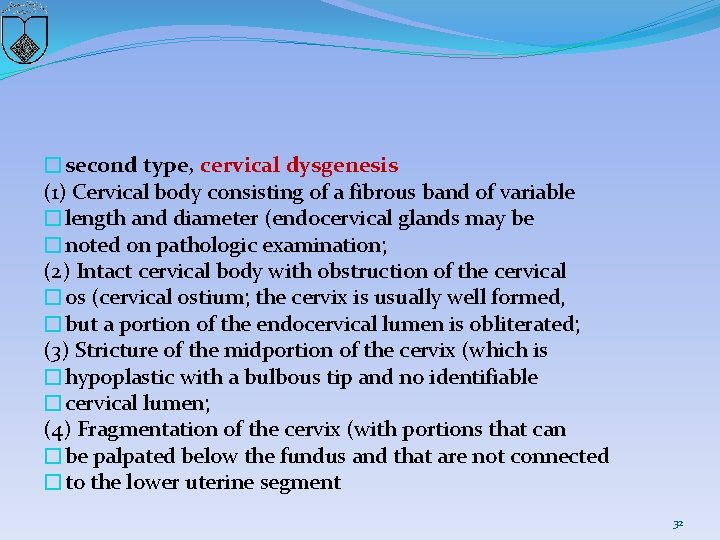
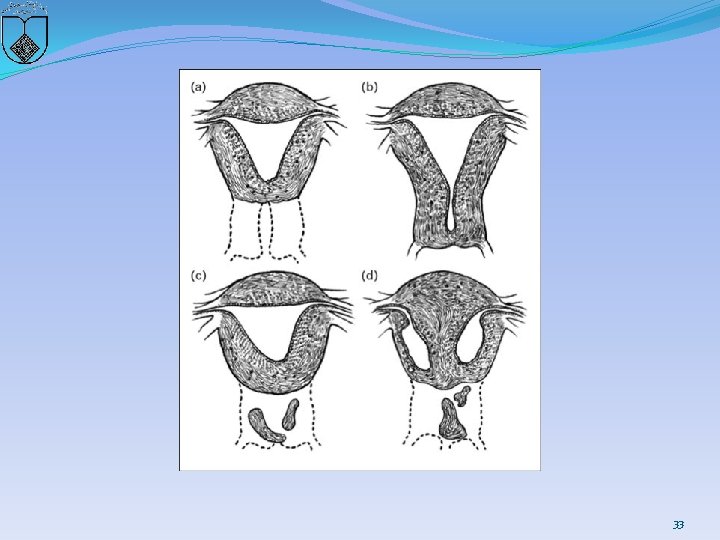
�second type, cervical dysgenesis (1) Cervical body consisting of a fibrous band of variable �length and diameter (endocervical glands may be �noted on pathologic examination; (2) Intact cervical body with obstruction of the cervical �os (cervical ostium; the cervix is usually well formed, �but a portion of the endocervical lumen is obliterated; (3) Stricture of the midportion of the cervix (which is �hypoplastic with a bulbous tip and no identifiable �cervical lumen; (4) Fragmentation of the cervix (with portions that can �be palpated below the fundus and that are not connected �to the lower uterine segment 32
33
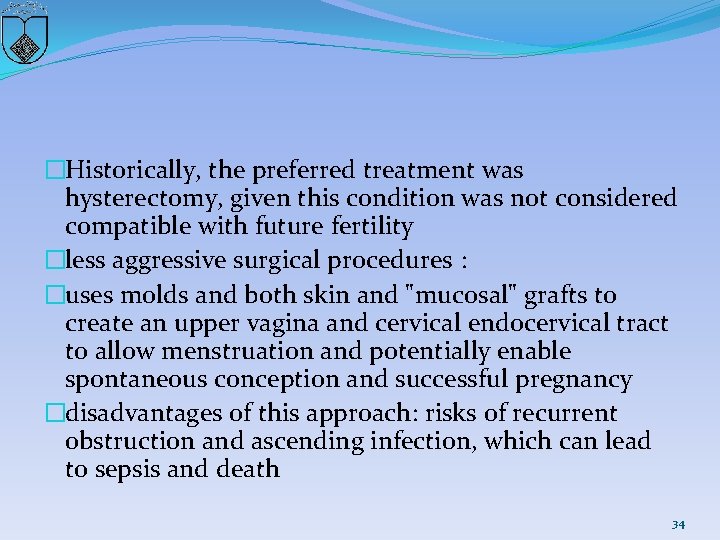
�Historically, the preferred treatment was hysterectomy, given this condition was not considered compatible with future fertility �less aggressive surgical procedures : �uses molds and both skin and "mucosal" grafts to create an upper vagina and cervical endocervical tract to allow menstruation and potentially enable spontaneous conception and successful pregnancy �disadvantages of this approach: risks of recurrent obstruction and ascending infection, which can lead to sepsis and death 34
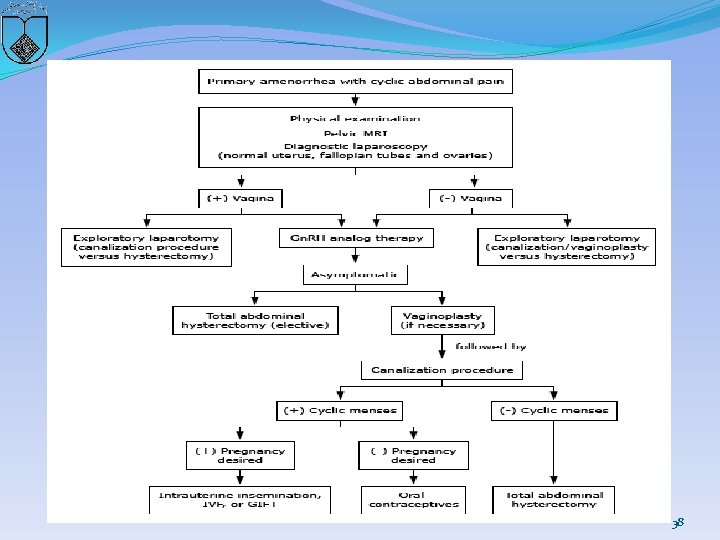
�A treatment algorithm �clinicians should select a surgical procedure carefully and be certain of the diagnosis (eg, differentiate between a high transverse vaginal septum and cervical agenesis) �A safe, successful surgical procedure is more likely when there is normal cervical tissue that just lacks a patent cervical canal than when there is significant cervical agenesis. 35
36
37
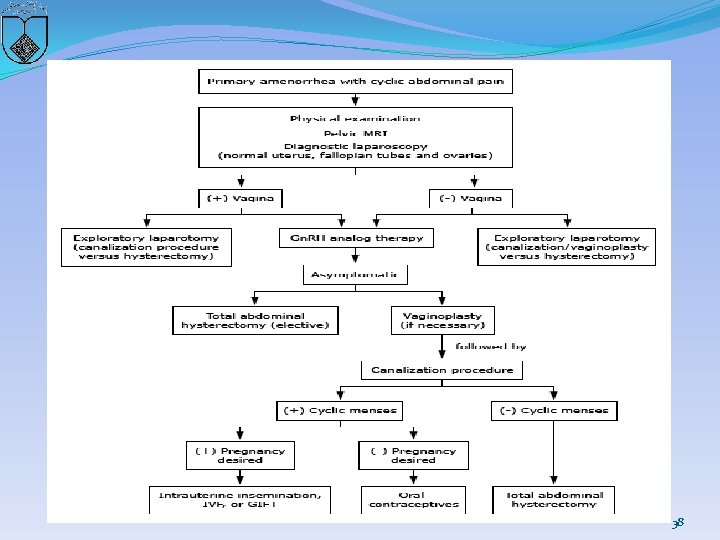
38
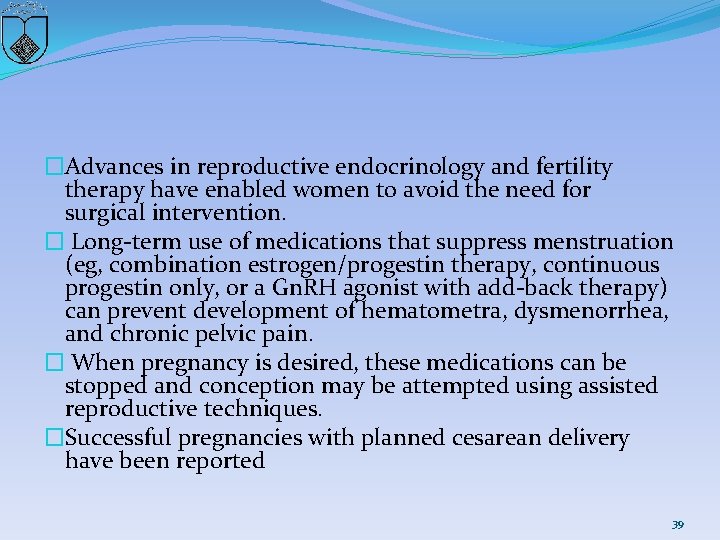
�Advances in reproductive endocrinology and fertility therapy have enabled women to avoid the need for surgical intervention. � Long-term use of medications that suppress menstruation (eg, combination estrogen/progestin therapy, continuous progestin only, or a Gn. RH agonist with add-back therapy) can prevent development of hematometra, dysmenorrhea, and chronic pelvic pain. � When pregnancy is desired, these medications can be stopped and conception may be attempted using assisted reproductive techniques. �Successful pregnancies with planned cesarean delivery have been reported 39
40
recommended approach �The first step : defining the anatomy prior to performing any reconstructive procedure �cervix is a thin cord or the uterine cavity is hypoplastic �or absent, the uterus and cervical remnants are removed �If a reconstructive procedure is performed, epithelialization with a suitable graft of neocervical canal is recommended 41
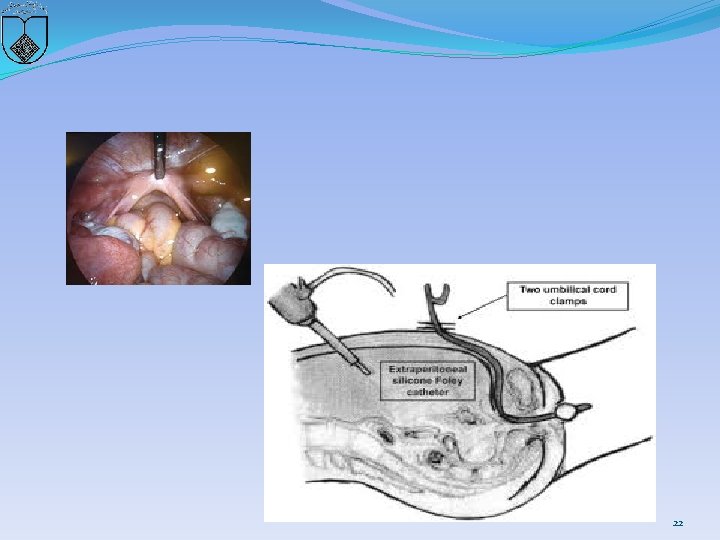
uterovaginal anastomosis �complete dissection of the rectouterine and vesicouterine space to expose the vagina or neovaginal canal, �allowing circumferential anastomosis of the vagina and stroma to the lower uterine segment. The uterus is pulled down and sutured to the vagina or vestibular mucosa A stent (16 French Foleycatheter) is placed with or without a mold, depending on surgeon preference or the need to graft the newly createdneovagina. �The patient is given a broad-spectrum antibiotic for 15 days. 42
43
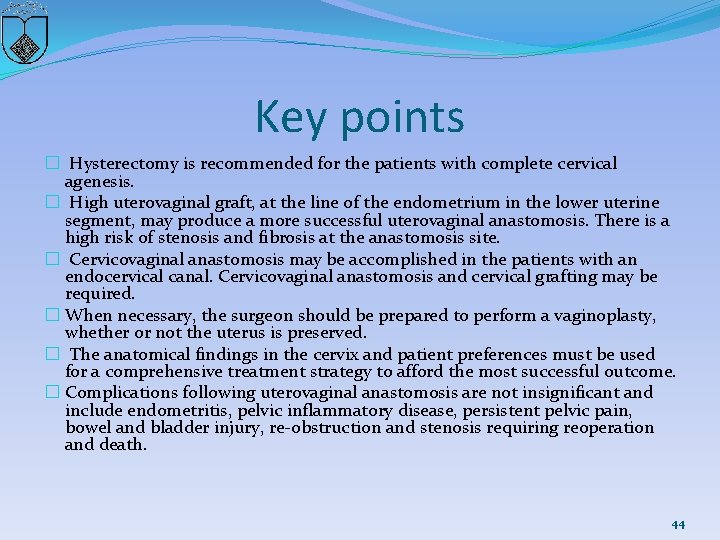
Key points � Hysterectomy is recommended for the patients with complete cervical agenesis. � High uterovaginal graft, at the line of the endometrium in the lower uterine segment, may produce a more successful uterovaginal anastomosis. There is a high risk of stenosis and fibrosis at the anastomosis site. � Cervicovaginal anastomosis may be accomplished in the patients with an endocervical canal. Cervicovaginal anastomosis and cervical grafting may be required. � When necessary, the surgeon should be prepared to perform a vaginoplasty, whether or not the uterus is preserved. � The anatomical findings in the cervix and patient preferences must be used for a comprehensive treatment strategy to afford the most successful outcome. � Complications following uterovaginal anastomosis are not insignificant and include endometritis, pelvic inflammatory disease, persistent pelvic pain, bowel and bladder injury, re-obstruction and stenosis requiring reoperation and death. 44
Uterine septum: a guideline American Society for Reproductive Medicine, Birmingham, Alabama 2016 45
�There are three common developmental defects of the müllerian system to consider: �Agenesis �Lateral fusion defects �Vertical fusion defects 46
Agenesis � The Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome refers to congenital absence of the vagina with variable uterine development; it is the result of müllerian agenesis. �Variable uterine development may result in lateral hemi-uteri or uterine horns, a midline uterus without a cervix, or no uterine structures at all. 47
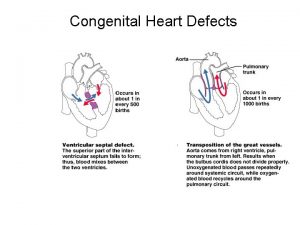
Lateral fusion defects �Lateral fusion defects are the most common type of müllerian defect. �The resulting organs are either symmetric or asymmetric, and obstructed or nonobstructed. �These fusion defects result from failure of formation of one müllerian duct, migration of a duct, fusion of the müllerian ducts, or absorption of the intervening septum. �Defective resorption of the tissue between the fused müllerian ducts results in a uterine septum, which may extend either partially down the uterus or the full length to the cervix. � A septum is the most common type of uterine defect 48
Vertical fusion defects �Vertical fusion defects are due to either defective fusion of the caudal end of the müllerian duct and urogenital sinus or problems with vaginal canalization. � The resulting vaginal septum or cervical agenesis or dysgenesis may be obstructed or nonobstructed. �The amount of obstruction will determine symptomatology, including obstetric outcomes. 49
Lateral fusion defects �Septate/arcuate uterus �Unicornuate uterus �Bicornuate uterus �Uterine didelphys 50
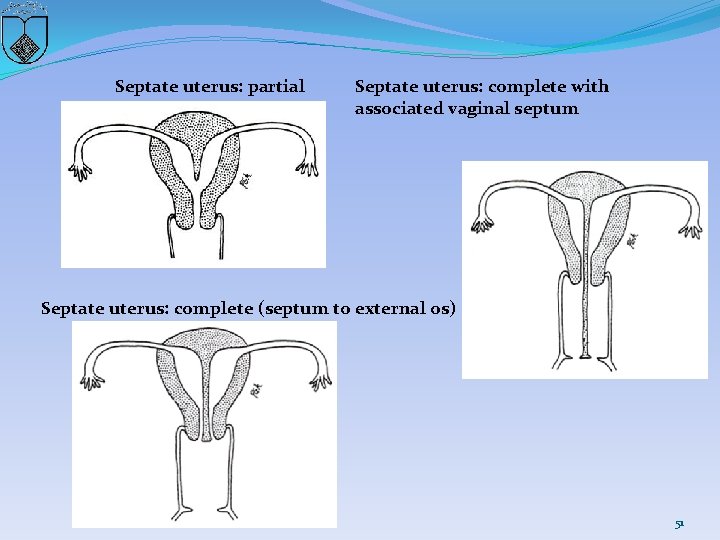
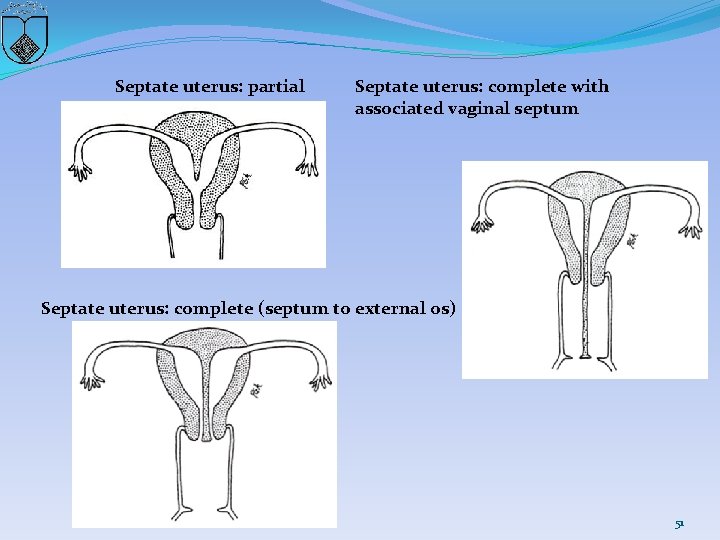
Septate uterus: partial Septate uterus: complete with associated vaginal septum Septate uterus: complete (septum to external os) 51
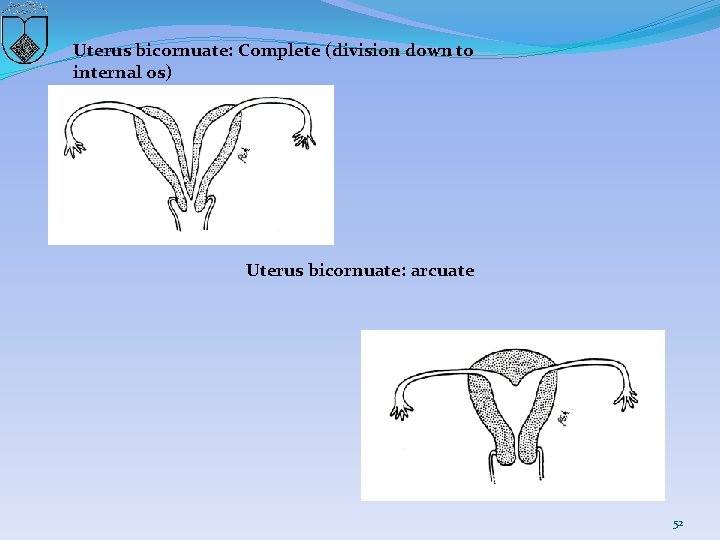
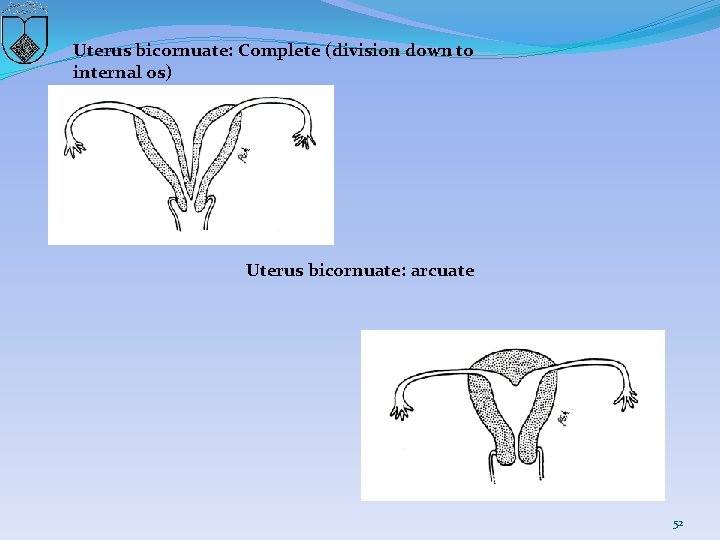
Uterus bicornuate: Complete (division down to internal os) Uterus bicornuate: arcuate 52

53
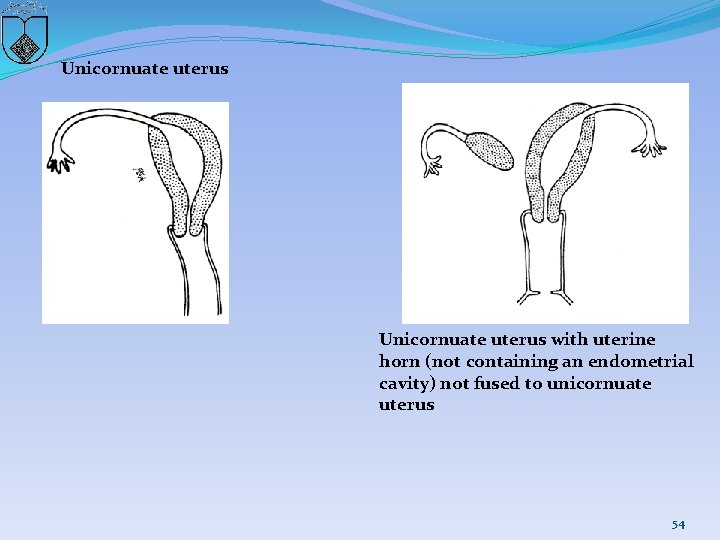
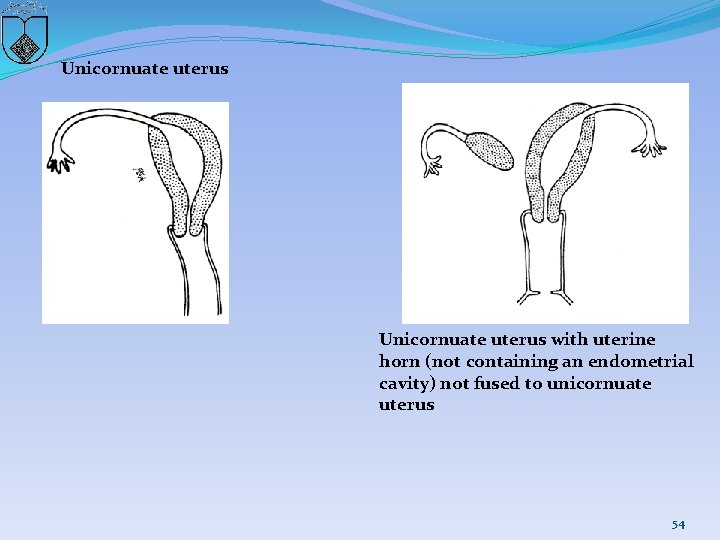
Unicornuate uterus with uterine horn (not containing an endometrial cavity) not fused to unicornuate uterus 54
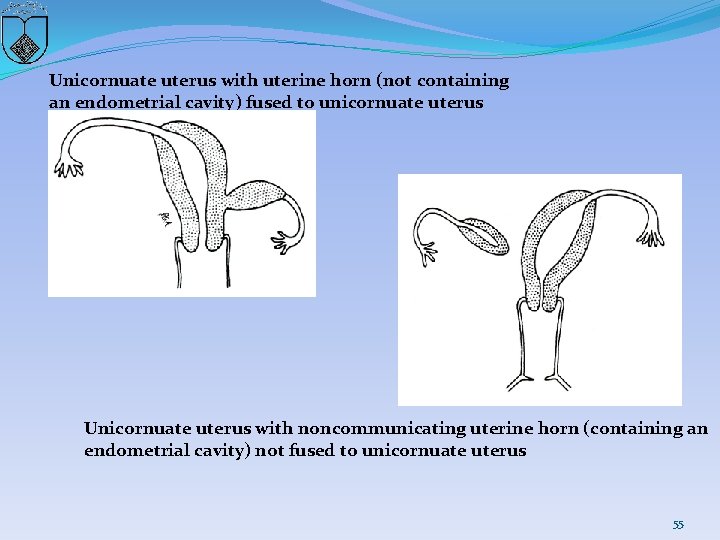
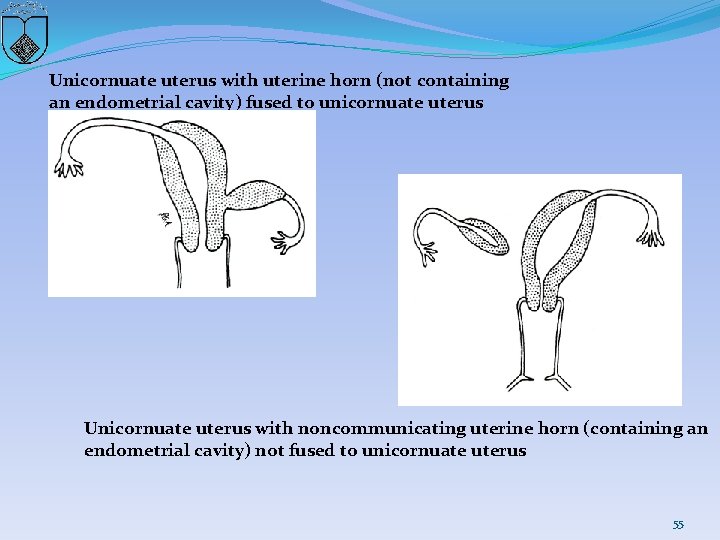
Unicornuate uterus with uterine horn (not containing an endometrial cavity) fused to unicornuate uterus Unicornuate uterus with noncommunicating uterine horn (containing an endometrial cavity) not fused to unicornuate uterus 55
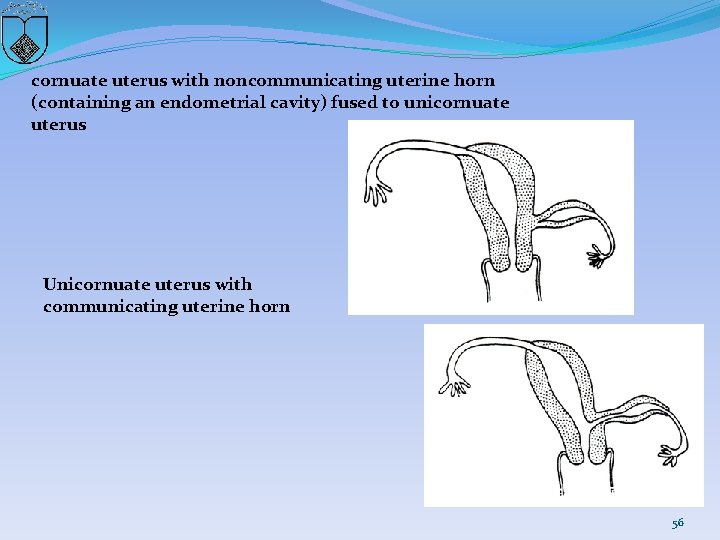
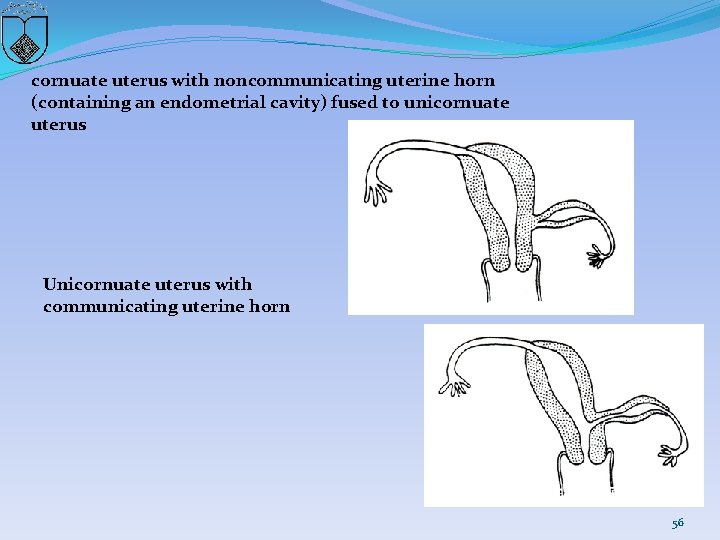
cornuate uterus with noncommunicating uterine horn (containing an endometrial cavity) fused to unicornuate uterus Unicornuate uterus with communicating uterine horn 56
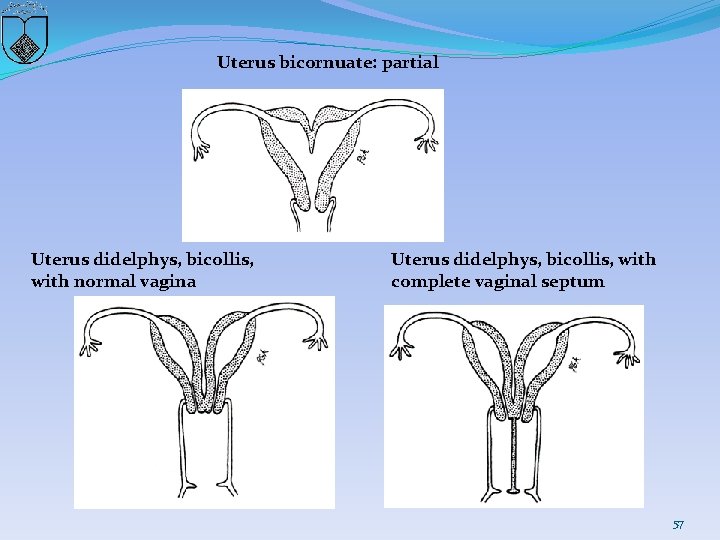
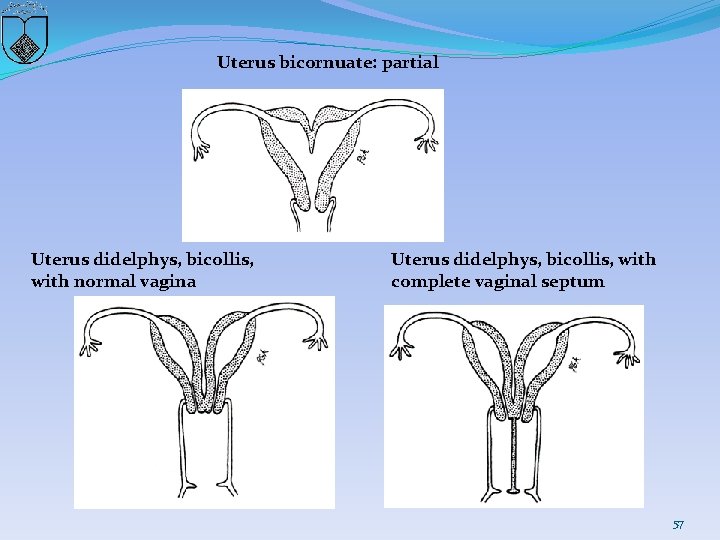
Uterus bicornuate: partial Uterus didelphys, bicollis, with normal vagina Uterus didelphys, bicollis, with complete vaginal septum 57
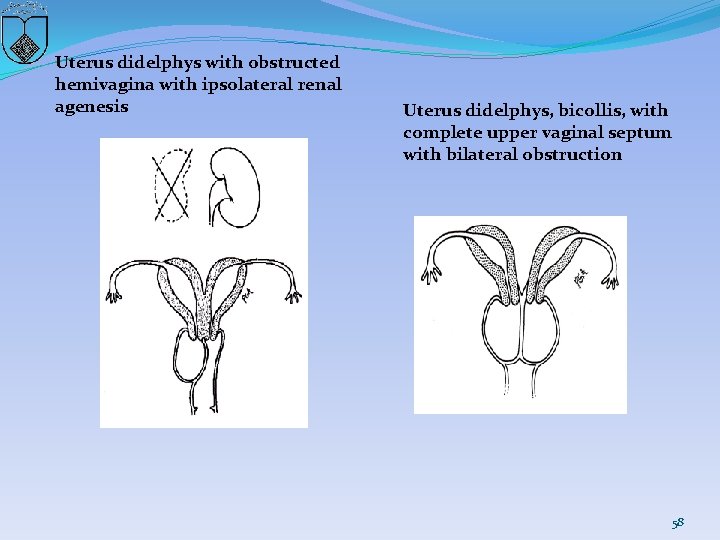
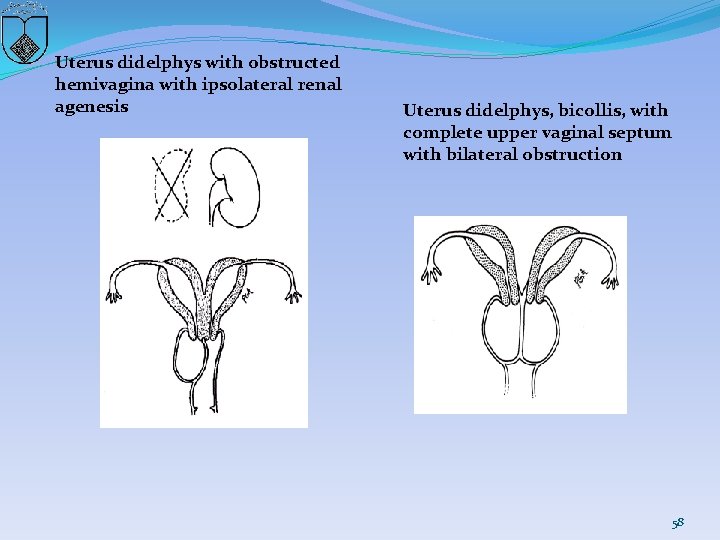
Uterus didelphys with obstructed hemivagina with ipsolateral renal agenesis Uterus didelphys, bicollis, with complete upper vaginal septum with bilateral obstruction 58
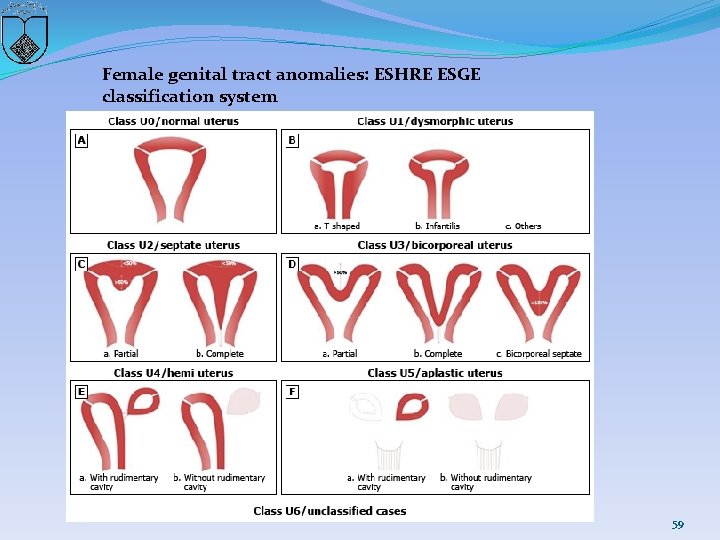
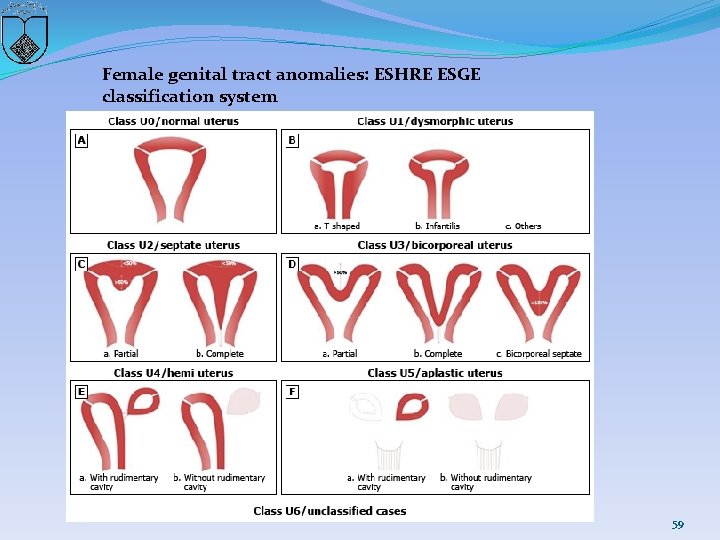
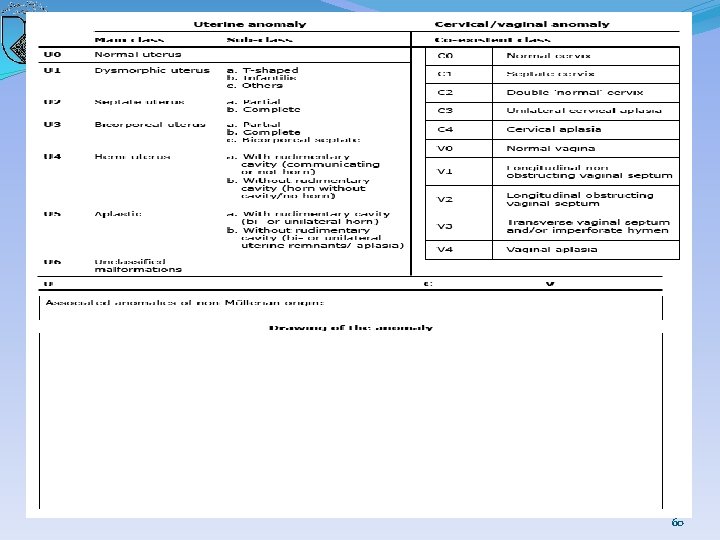
Female genital tract anomalies: ESHRE ESGE classification system 59
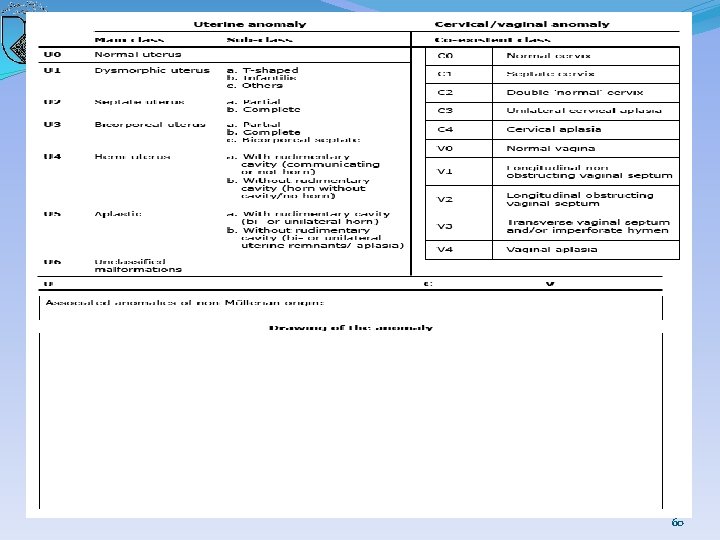
60
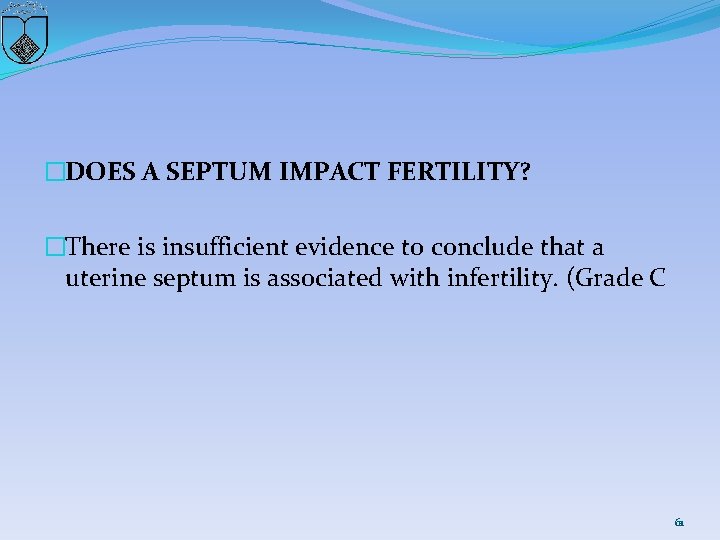
�DOES A SEPTUM IMPACT FERTILITY? �There is insufficient evidence to conclude that a uterine septum is associated with infertility. (Grade C 61
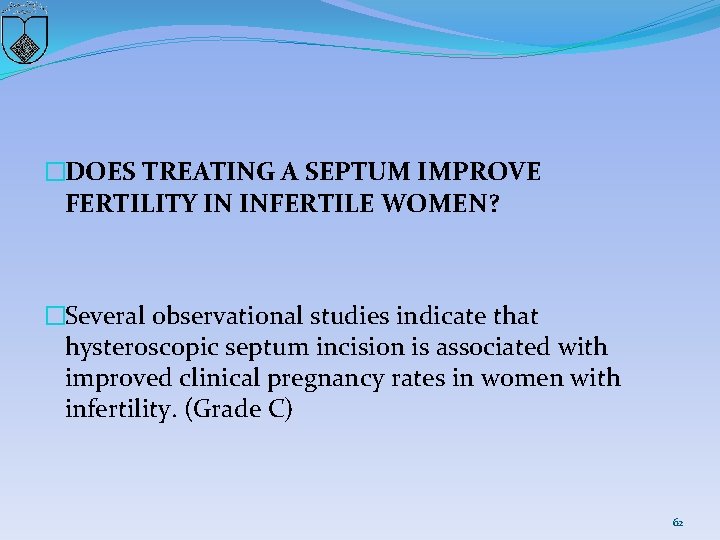
�DOES TREATING A SEPTUM IMPROVE FERTILITY IN INFERTILE WOMEN? �Several observational studies indicate that hysteroscopic septum incision is associated with improved clinical pregnancy rates in women with infertility. (Grade C) 62
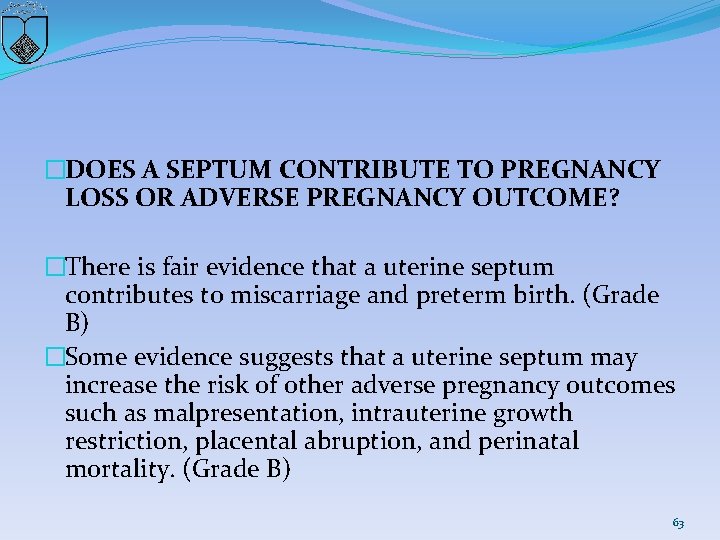
�DOES A SEPTUM CONTRIBUTE TO PREGNANCY LOSS OR ADVERSE PREGNANCY OUTCOME? �There is fair evidence that a uterine septum contributes to miscarriage and preterm birth. (Grade B) �Some evidence suggests that a uterine septum may increase the risk of other adverse pregnancy outcomes such as malpresentation, intrauterine growth restriction, placental abruption, and perinatal mortality. (Grade B) 63
�DOES TREATING A SEPTUM IMPROVE OBSTETRICAL OUTCOMES? �Some limited studies indicate that hysteroscopic septum incision is associated with a reduction in subsequent miscarriage rates and improvement in live -birth rates in patients with a history of recurrent pregnancy loss. (Grade C) �Some limited studies indicate that hysteroscopic septum incision is associated with an improvement in live-birth rate in women with infertility or prior pregnancy loss. (Grade C) 64
�ARE SEPTUM CHARACTERISTICS ASSOCIATED WITH WORSE REPRODUCTIVE OUTCOMES? �There is insufficient evidence to conclude that obstetric outcomes are different when comparing the size as defined by length or width of uterine septa. (Grade C) 65
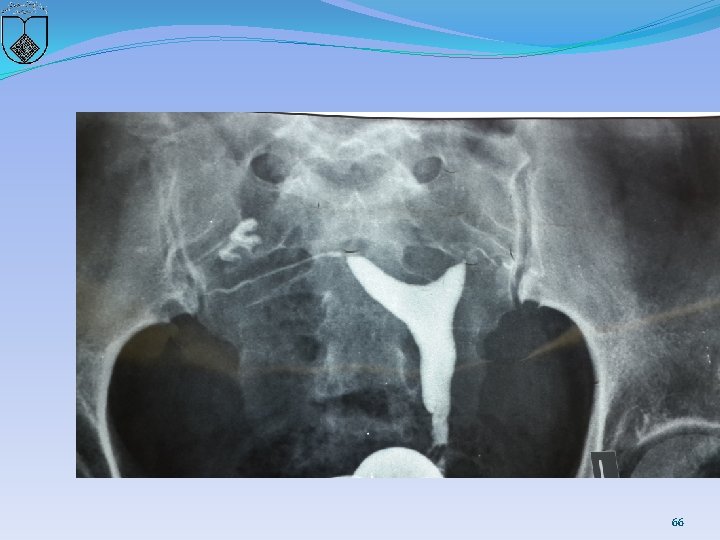
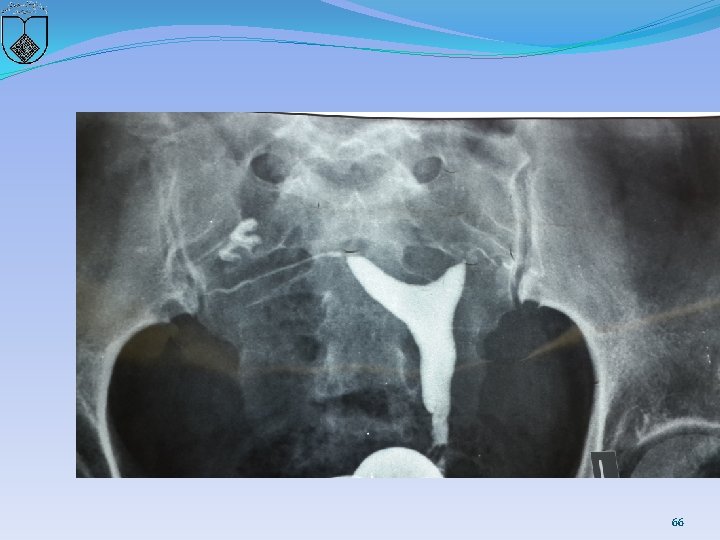
66
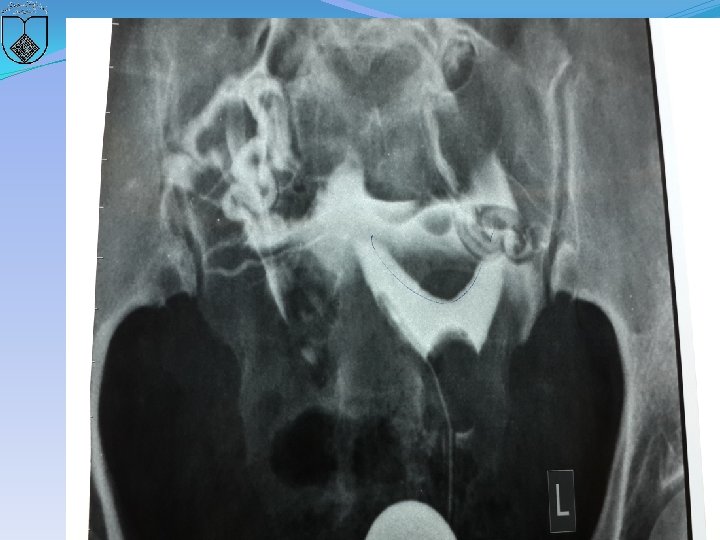
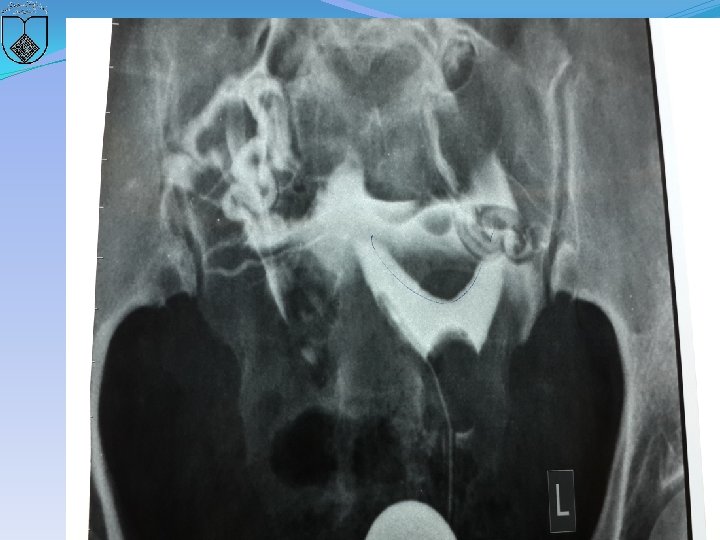
67

68
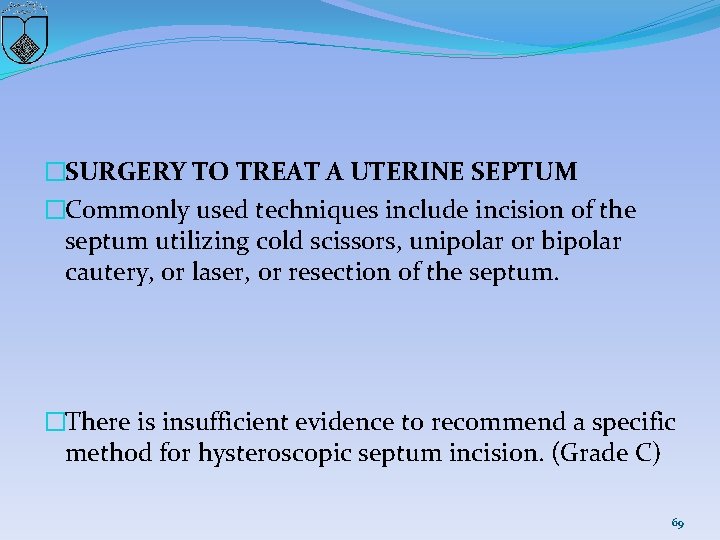
�SURGERY TO TREAT A UTERINE SEPTUM �Commonly used techniques include incision of the septum utilizing cold scissors, unipolar or bipolar cautery, or laser, or resection of the septum. �There is insufficient evidence to recommend a specific method for hysteroscopic septum incision. (Grade C) 69
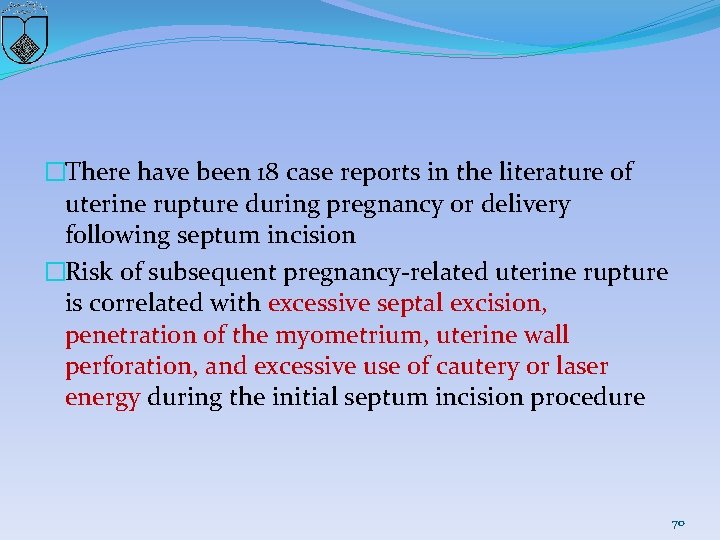
�There have been 18 case reports in the literature of uterine rupture during pregnancy or delivery following septum incision �Risk of subsequent pregnancy-related uterine rupture is correlated with excessive septal excision, penetration of the myometrium, uterine wall perforation, and excessive use of cautery or laser energy during the initial septum incision procedure 70
�HOW LONG AFTER SURGICAL TREATMENT OF A UTERINE SEPTUM SHOULD A WOMAN WAIT TO CONCEIVE? �Although the available evidence suggests that the uterine cavity is healed by 2 months postoperatively, there is insufficient evidence to advocate a specific length of time before a woman should conceive. (Grade C) 71
�SHOULD PREOPERATIVE MANAGEMENT TO THIN THE ENDOMETRIUM BE USED? �There is insufficient evidence for or against recommending danazol or Gn. RH agonists to thin the endometrium prior to hysteroscopic septum incision. (Grade C) 72
IS ADHESION PREVENTION NEEDED? �Intrauterine adhesion formation following hysteroscopic uterine septum incision can have significant consequences. � Although the risk is believed to be low � treatment options include : � Antibiotics � postoperative estrogen therapy � placement of an intrauterine balloon or device � to separate the endometrial walls in the postoperative period 73
�IS ADHESION PREVENTION NEEDED? �There is insufficient evidence to recommend for or against adhesion prevention treatment, or any specific method following hysteroscopic septum incision. (Grade C) 74
RECOMMENDATIONS �In a patient with infertility, prior pregnancy loss, or poor obstetrical outcome it is reasonable to consider septum incision. (Grade C) �In a patient without infertility or prior pregnancy loss, it may be reasonable to consider septum incision following counseling regarding potential risks and benefits of the procedure. (Grade C) 75
 Erythroplasia
Erythroplasia Kode icd 10 malformasi anorektal
Kode icd 10 malformasi anorektal Causes of congenital anomalies
Causes of congenital anomalies Mcgovern nipple
Mcgovern nipple Spina bifida
Spina bifida Congenial
Congenial Choledocolithaisis
Choledocolithaisis Data redundancy and update anomalies
Data redundancy and update anomalies Anomali refraksi
Anomali refraksi The criminal man
The criminal man Modification anomalies
Modification anomalies Cfsv2 monthly prec anomalies
Cfsv2 monthly prec anomalies Convex population pyramid
Convex population pyramid Défauts et anomalies du bois
Défauts et anomalies du bois Attention anomalies finance
Attention anomalies finance Aiha pbs
Aiha pbs Anomalies du rcf pendant le travail
Anomalies du rcf pendant le travail Database anomalies
Database anomalies Andrea frazzini
Andrea frazzini Ralentissement variable atypique
Ralentissement variable atypique Oddball: spotting anomalies in weighted graphs
Oddball: spotting anomalies in weighted graphs Enterocystoma
Enterocystoma Processus ciliaris
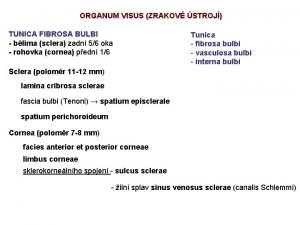
Processus ciliaris Hymen utuh
Hymen utuh Gonnorhoe
Gonnorhoe Auxonograma
Auxonograma Musculo transverso del perineo
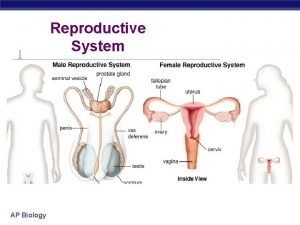
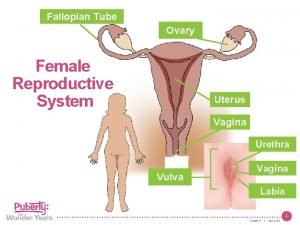
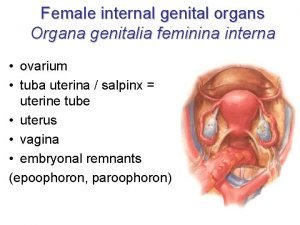
Musculo transverso del perineo Female reproductive system definition
Female reproductive system definition Mm. levatores costarum
Mm. levatores costarum Vagina diagram labeled
Vagina diagram labeled Bruchova membrána
Bruchova membrána Epididymitis
Epididymitis Vagina
Vagina Wee foal
Wee foal Female anatomy cervix
Female anatomy cervix Narrow neck which projects into the vagina inferiorly
Narrow neck which projects into the vagina inferiorly The female anatomy
The female anatomy Perineal cavity
Perineal cavity Vagina tongue
Vagina tongue Kaya dengan tenunan parenchyme
Kaya dengan tenunan parenchyme Franja ovarica
Franja ovarica Oppqrst
Oppqrst Ligaments of vagina
Ligaments of vagina Cat epididymis
Cat epididymis Shigeko kubota
Shigeko kubota Sistema reprodutor feminino
Sistema reprodutor feminino Cervix
Cervix Diafragma
Diafragma Arbour vitae uteri
Arbour vitae uteri Vaginal vault prolapse
Vaginal vault prolapse Anatomi vagina
Anatomi vagina Fungsi labium majora
Fungsi labium majora Bell stage
Bell stage Tendo prepubicus
Tendo prepubicus Corpus luteum in female reproductive system
Corpus luteum in female reproductive system Dr. wulan m. soemardji spog
Dr. wulan m. soemardji spog M deltoidea
M deltoidea Regio deltoidea
Regio deltoidea Loss of heart muscle
Loss of heart muscle Vagina prolapse
Vagina prolapse Longitud vagina
Longitud vagina Feminina organa genitalia
Feminina organa genitalia Function of cervix
Function of cervix Anatomi vagina
Anatomi vagina Organ reproduksi pria tampak depan
Organ reproduksi pria tampak depan Axillary nerve
Axillary nerve Jnjnl
Jnjnl Ventriculus cordis dexter
Ventriculus cordis dexter Physiology of cervix
Physiology of cervix Cupula pericardii
Cupula pericardii C 2 =121
C 2 =121 Ararat anomaly google earth
Ararat anomaly google earth Types of anomaly in semantics
Types of anomaly in semantics Belady's anomaly example
Belady's anomaly example Transaction flow testing
Transaction flow testing Signature based vs anomaly based
Signature based vs anomaly based