STI HIV DR V S DORAIRAJ DIRECTOR IC





















- Slides: 81

STI & HIV DR. V. S. DORAIRAJ. DIRECTOR I/C & PROFESSOR INSTITUTE OF VENEREOLOGY MADRAS MEDICAL COLLEGE
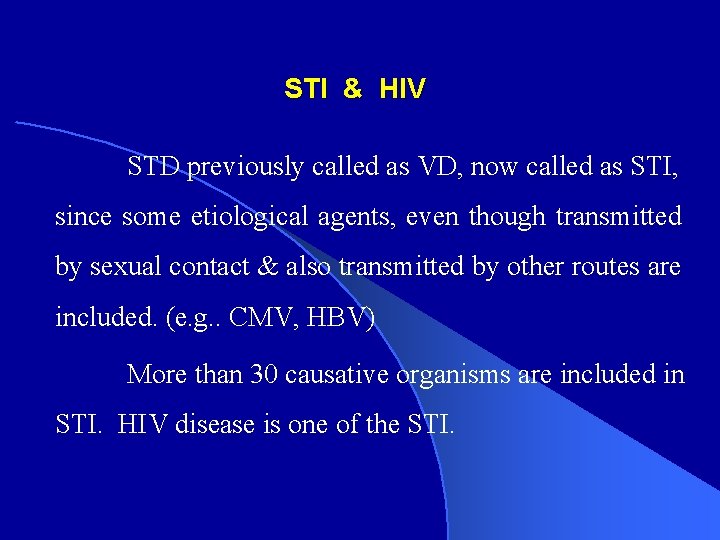
STI & HIV STD previously called as VD, now called as STI, since some etiological agents, even though transmitted by sexual contact & also transmitted by other routes are included. (e. g. . CMV, HBV) More than 30 causative organisms are included in STI. HIV disease is one of the STI.

· According to WHO, 330 million cases are reported every year, all over the world as STD. · India has high incidence of STD; and the annual incidence rate is 5% among the infectious diseases.
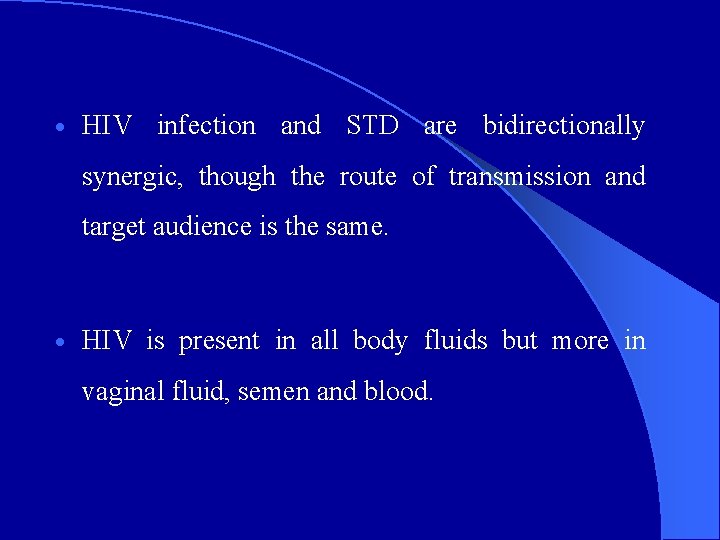
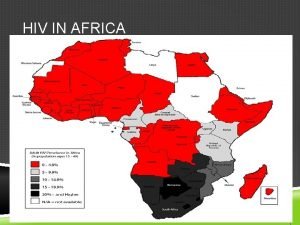
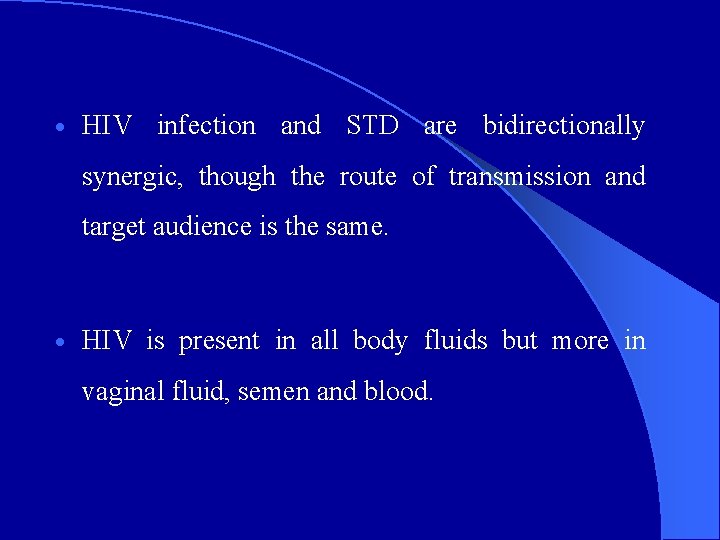
· HIV infection and STD are bidirectionally synergic, though the route of transmission and target audience is the same. · HIV is present in all body fluids but more in vaginal fluid, semen and blood.

INTERACTION BETWEEN HIV INFECTION AND OTHER STD · 1. Potential for STD to increase the rate of both HIV Acquisition and Transmission – In patients with genital ulcers, the acquisition and transmission is increased by 10 folds due to raw area. – In patients with genital discharge it will be increased by 5 folds due to micro ulceration of mucosa.
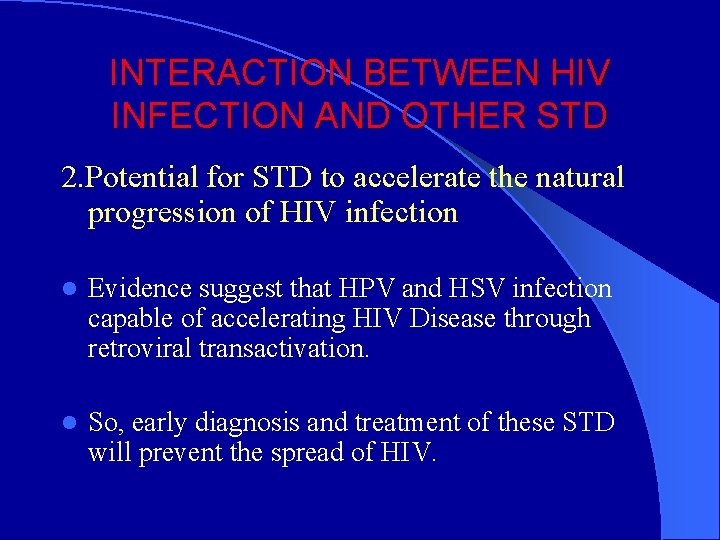
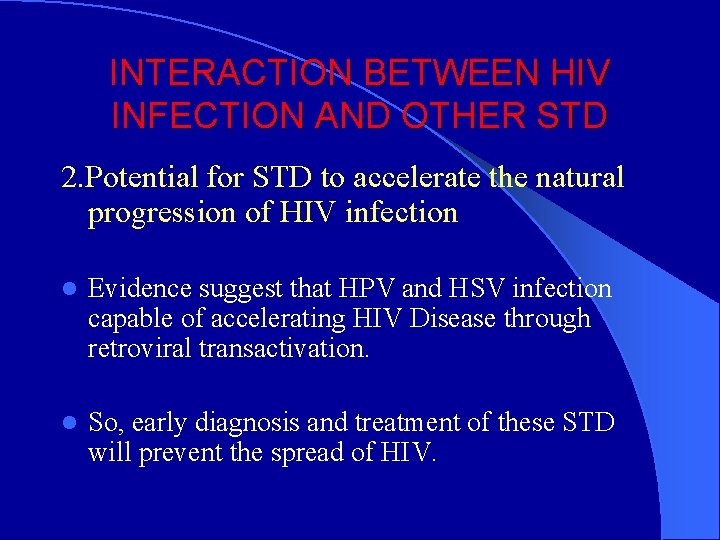
INTERACTION BETWEEN HIV INFECTION AND OTHER STD 2. Potential for STD to accelerate the natural progression of HIV infection l Evidence suggest that HPV and HSV infection capable of accelerating HIV Disease through retroviral transactivation. l So, early diagnosis and treatment of these STD will prevent the spread of HIV.

STD in HIV Infection In HIV patients, STD will have, 1. Shorter incubation period 2. Clinical Features altered – Atypical and Florid 3. Serological parameters altered-in Secondary Syphilis 4. Complications will be preponed. 5. Refractory to treatment.

SEXUALLY TRANSMITTED DISEASES AND ASSOCIATED PATHOGENS 1. BACTERIAL a. Syphilis Treponema pallidum b. Gonorrhea Neisseria gonorrhoeae c. Chancroid Haemophilus ducreyi d. Granuloma inguinale Calymmatobacterium granulomatis e. Lymphogranuloma venereum Chlamydia trachomatis (L 1, L 2, L 3) f. Bacterial vaginosis Gardnerella vaginalis, Mobiluncus, Mycoplasma, Ureaplasma, Bacteroides, Peptococcus g. Non-gonococcal urethritis Chlamydia trachomatis (D to K) Mycoplasma, Ureaplasma, etc. h. Pelvic inflammatory disease N. gonorrhoeae, C. trachomatis, Mycoplasma, Ureaplasma, etc. i. Enteric disease Salmonella, Shigella, Campylobacter fetus, Branhamella catarrhalis.
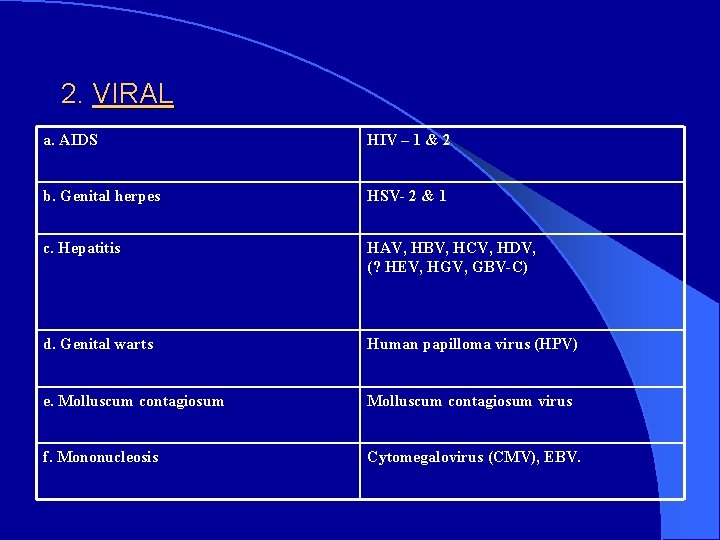
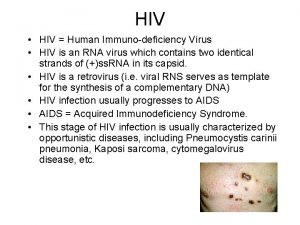
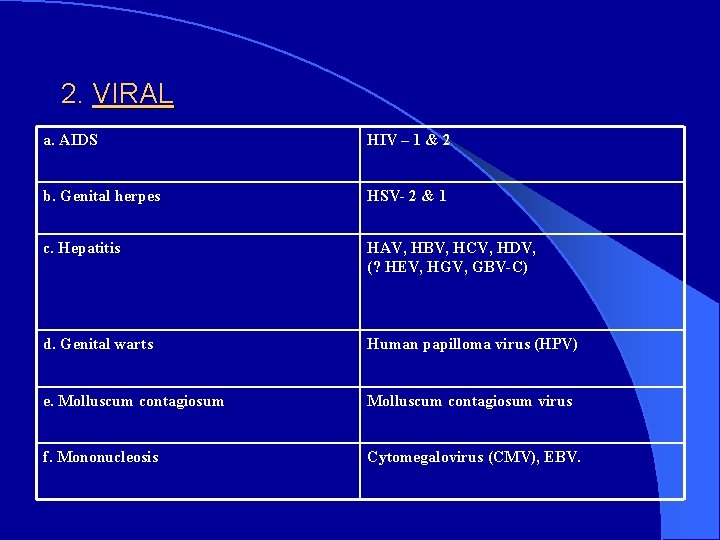
2. VIRAL a. AIDS HIV – 1 & 2 b. Genital herpes HSV- 2 & 1 c. Hepatitis HAV, HBV, HCV, HDV, (? HEV, HGV, GBV-C) d. Genital warts Human papilloma virus (HPV) e. Molluscum contagiosum virus f. Mononucleosis Cytomegalovirus (CMV), EBV.
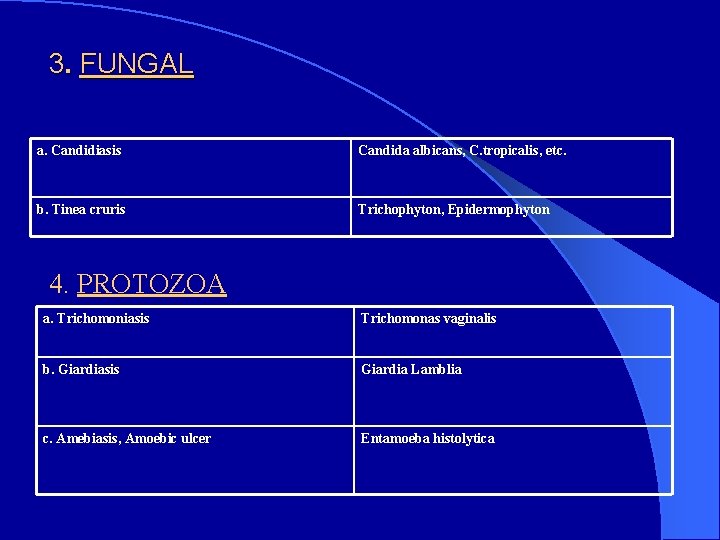
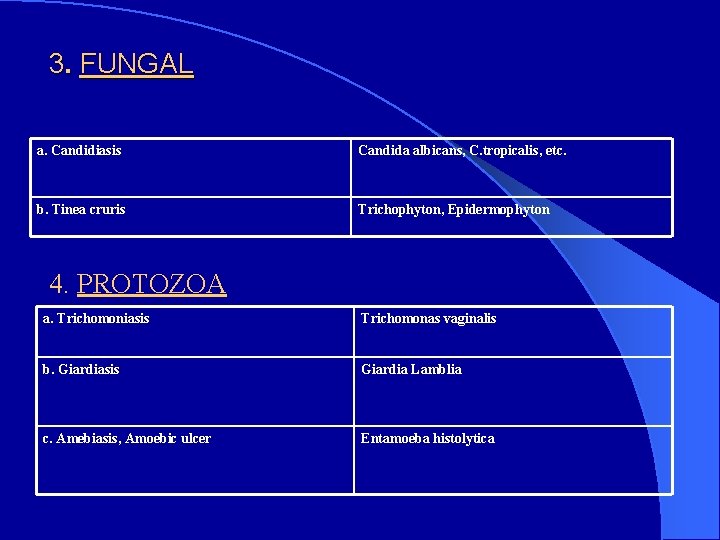
3. FUNGAL a. Candidiasis Candida albicans, C. tropicalis, etc. b. Tinea cruris Trichophyton, Epidermophyton 4. PROTOZOA a. Trichomoniasis Trichomonas vaginalis b. Giardiasis Giardia Lamblia c. Amebiasis, Amoebic ulcer Entamoeba histolytica
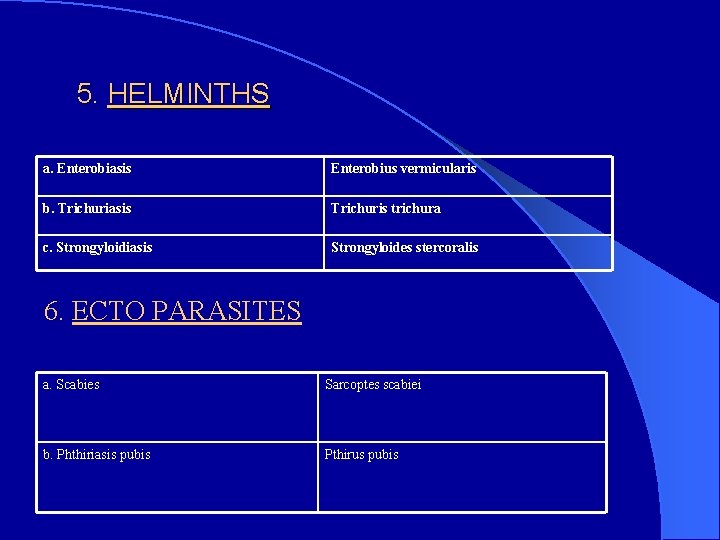
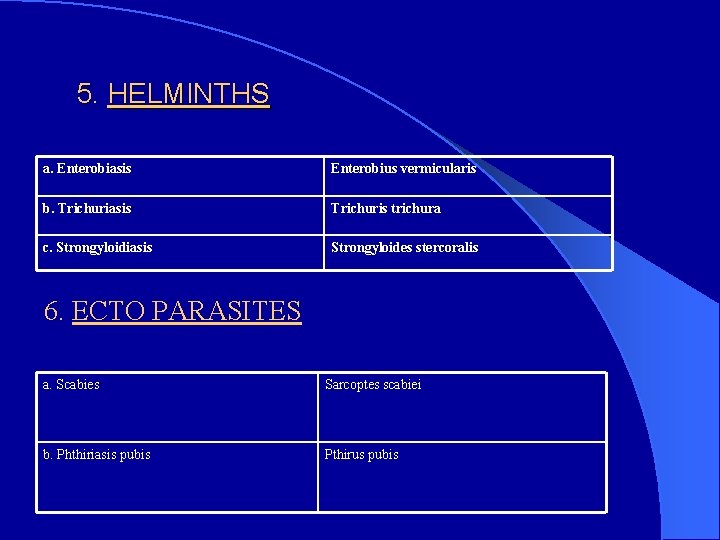
5. HELMINTHS a. Enterobiasis Enterobius vermicularis b. Trichuriasis Trichuris trichura c. Strongyloidiasis Strongyloides stercoralis 6. ECTO PARASITES a. Scabies Sarcoptes scabiei b. Phthiriasis pubis Pthirus pubis

l After the emergence of HIV disease , the incidence of syphilis , viral infections like Herpes, genital warts , protozoal infection like trichomoniasis & fungal infections like candidiasis are increased.

Genital Ulcer Diseases l Syphilis l Chancroid l Venereal Granuloma l Lymphogranuloma Venereum (LGV) l Herpes Genitalis

SYPHILIS HIV disease and Syphilis involves all system. Only difference is in syphilis, the causative organism, Treponema pallidum itself affects all system; whereas in HIV disease; because of immunedeficiency, the opportunistic organisms affect all the systems. Syphilis affects head to foot, hair to nail, does not spare any part of the body. Syphilologist – Stokes, says “ One who knows syphilis – knows medicine”. Incubation period : 9 - 90 days

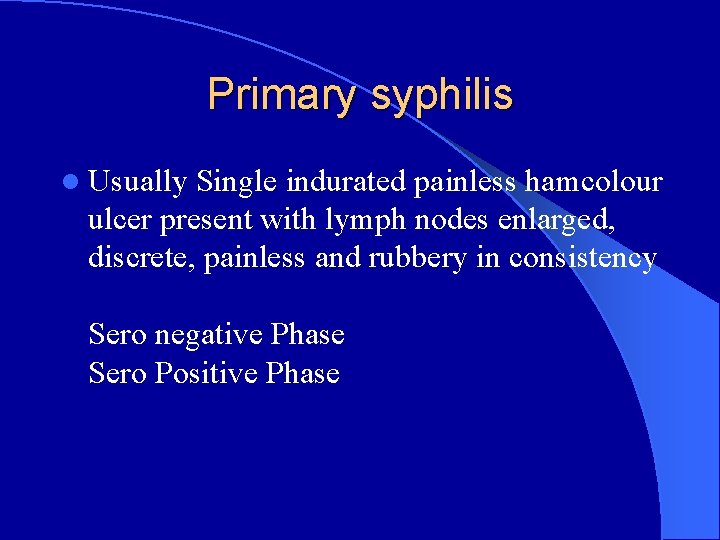
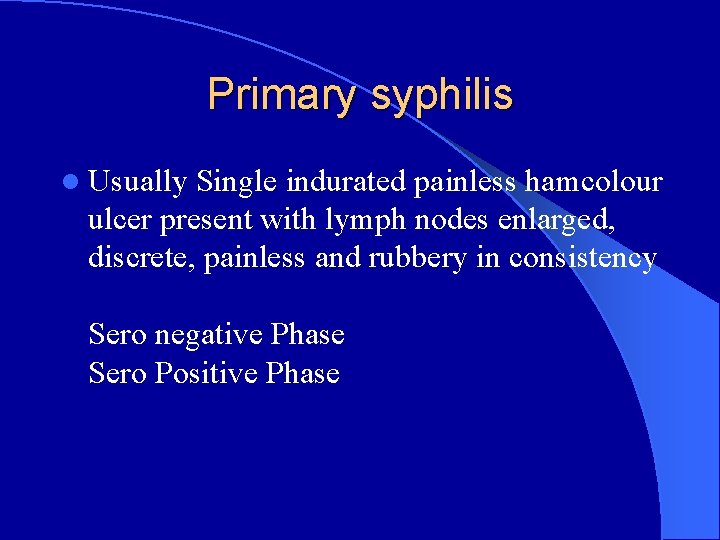
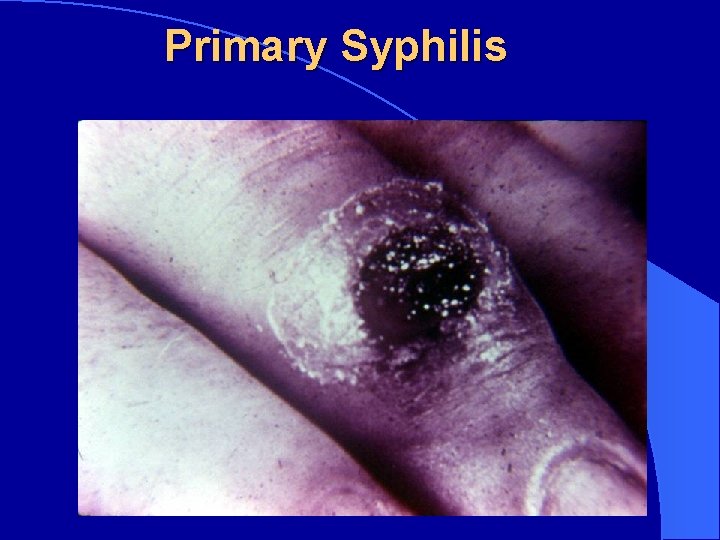
Primary syphilis l Usually Single indurated painless hamcolour ulcer present with lymph nodes enlarged, discrete, painless and rubbery in consistency Sero negative Phase Sero Positive Phase
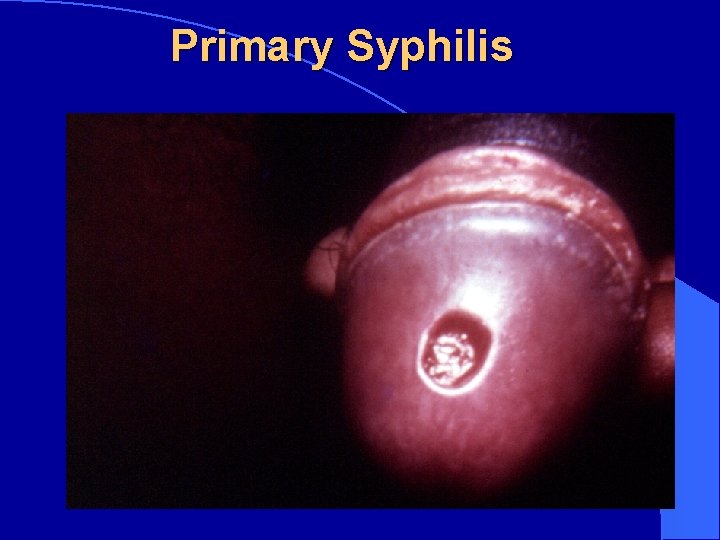
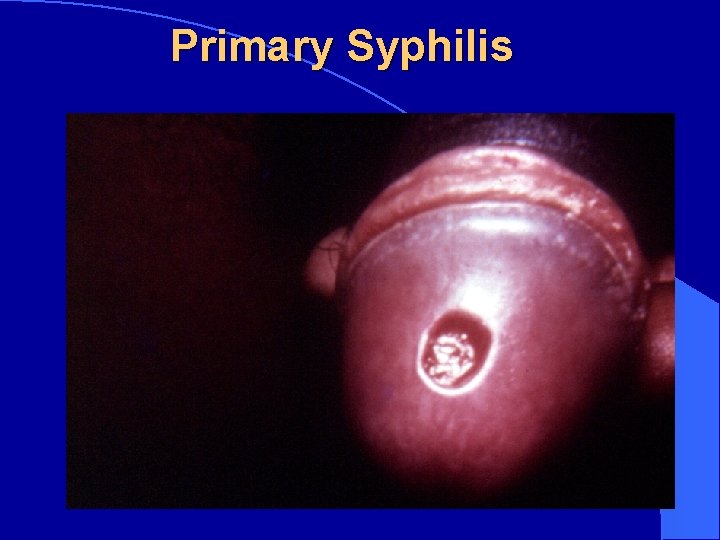
Primary Syphilis
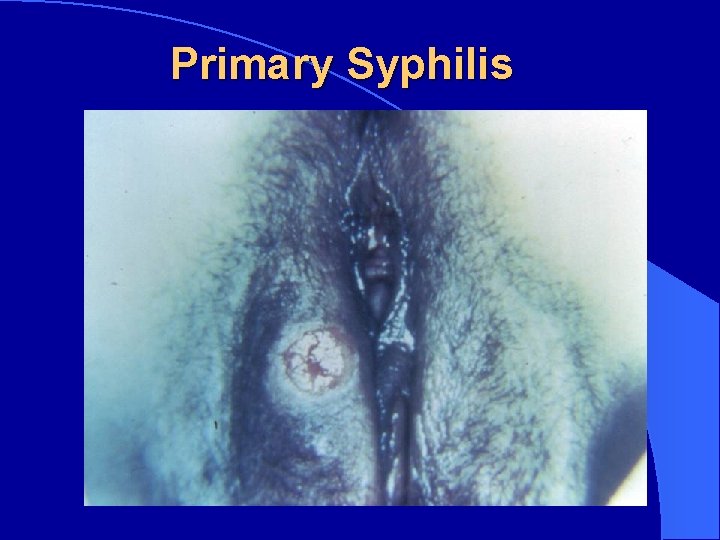
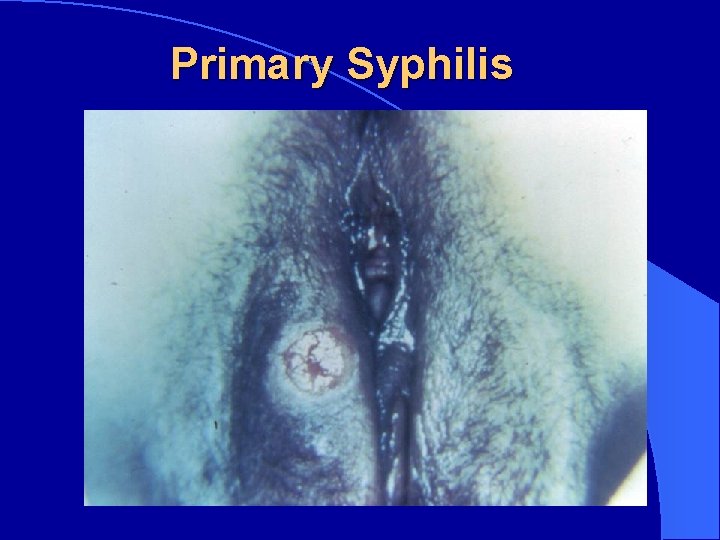
Primary Syphilis
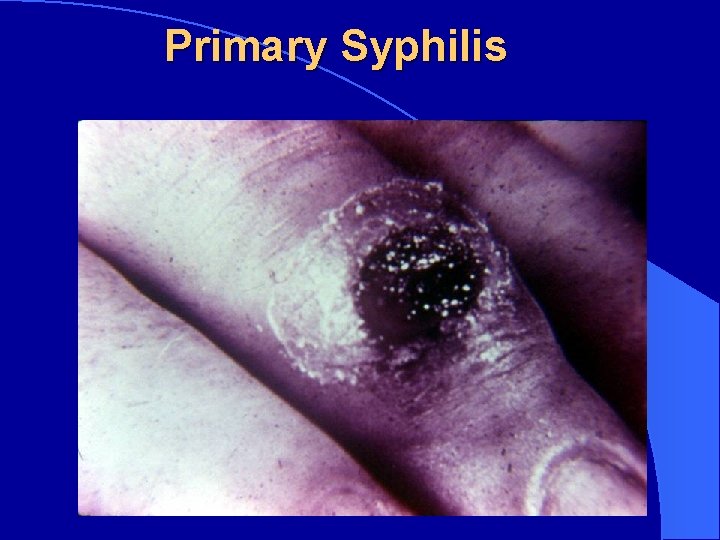
Primary Syphilis
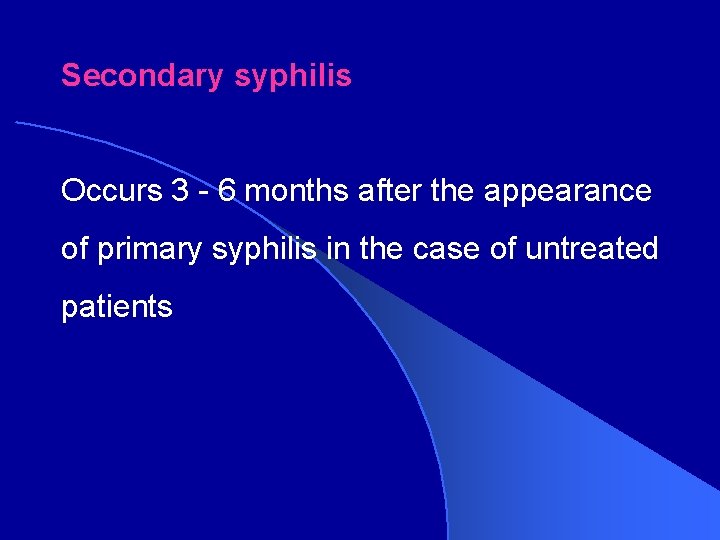
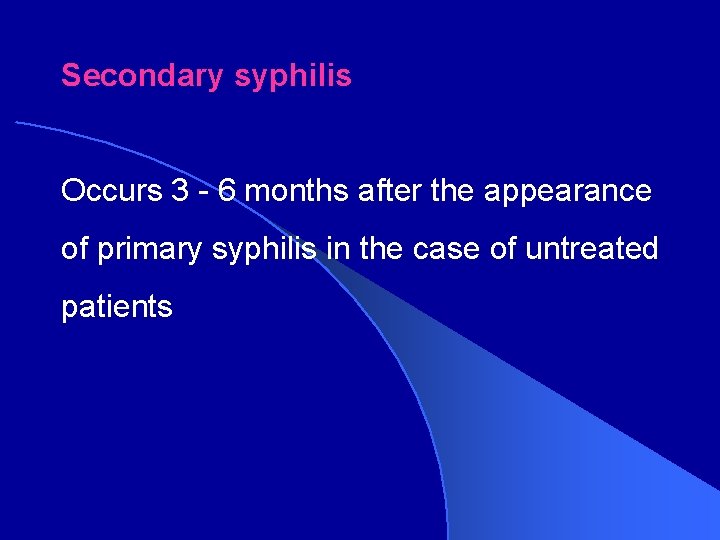
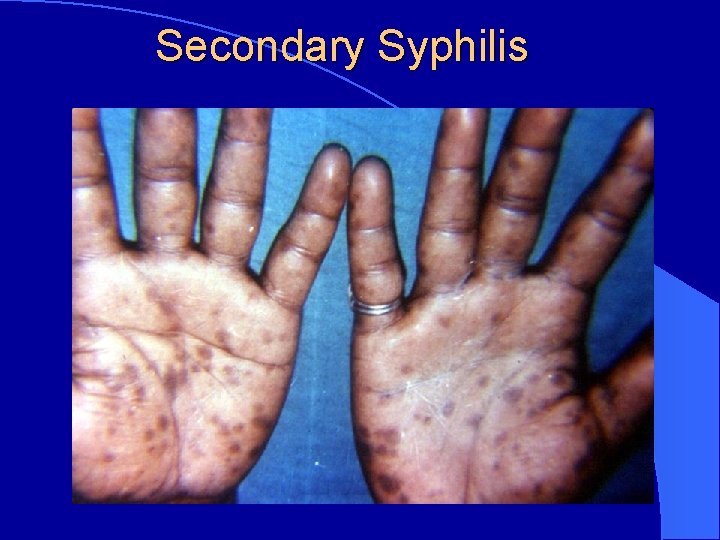
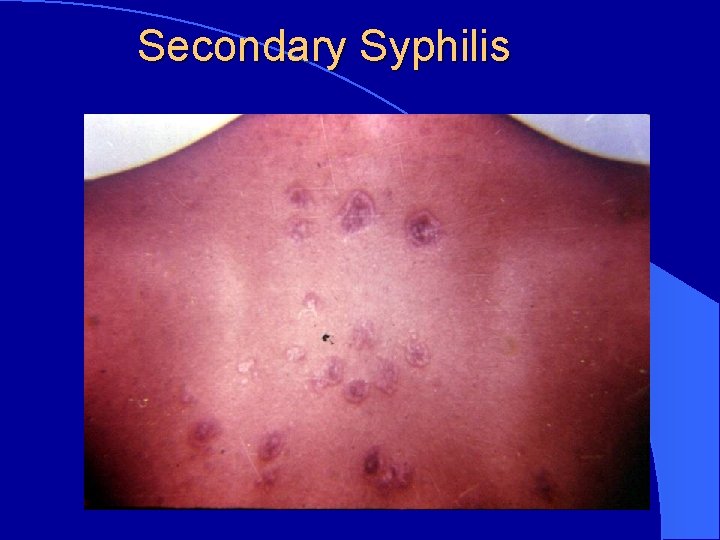
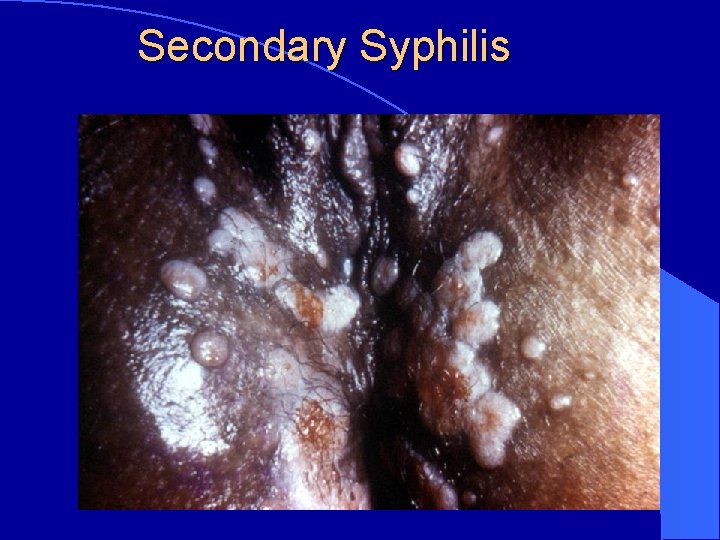
Secondary syphilis Occurs 3 - 6 months after the appearance of primary syphilis in the case of untreated patients
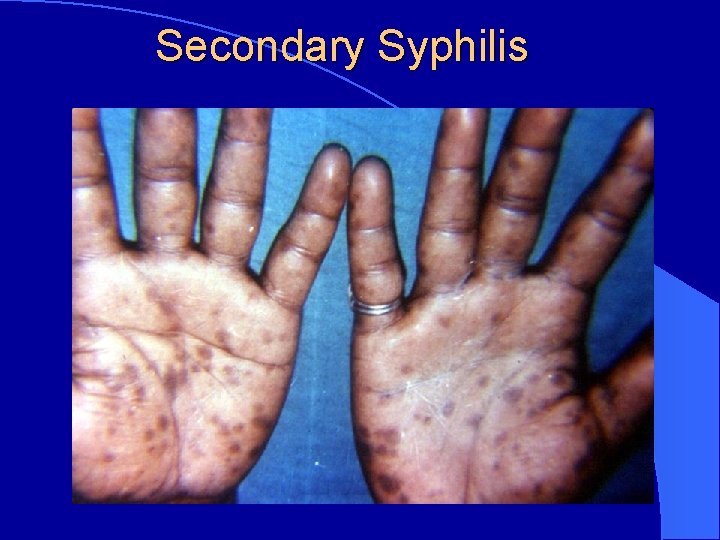
Secondary Syphilis
Secondary Syphilis
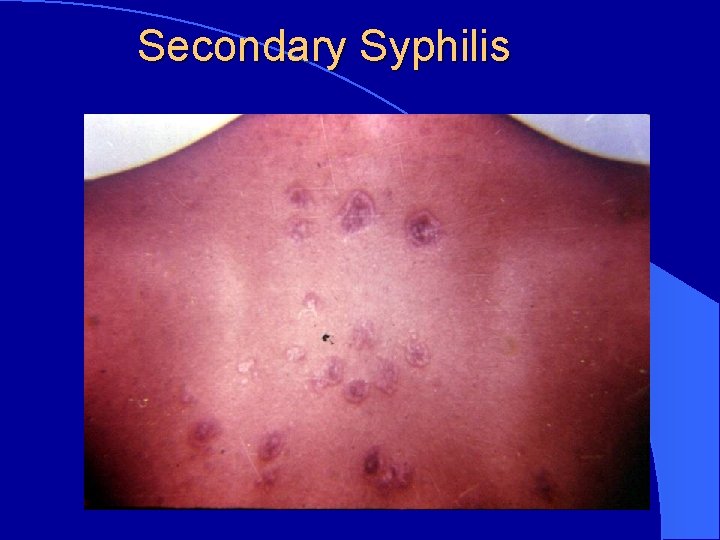
Secondary Syphilis
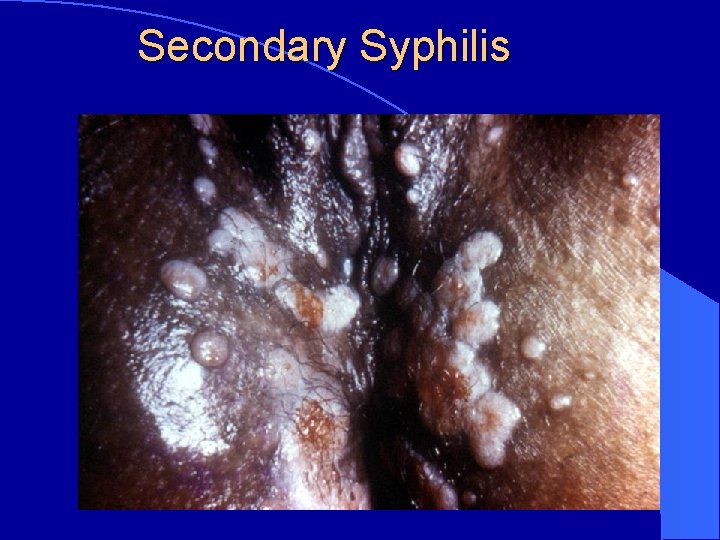
Secondary Syphilis
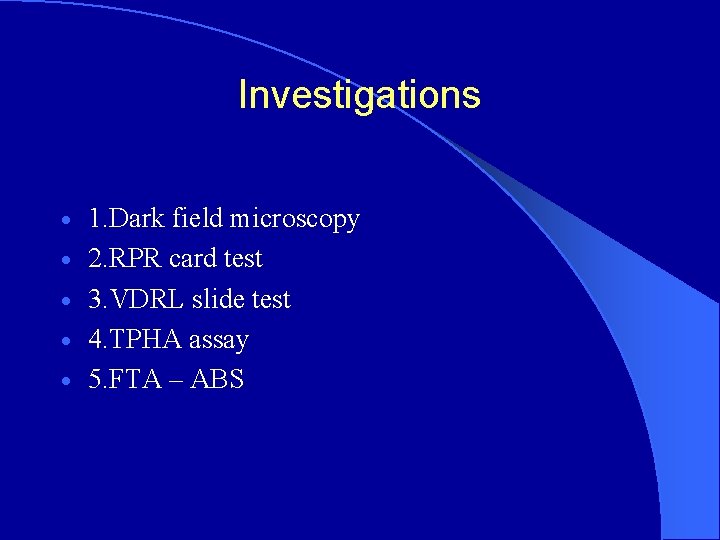
Investigations · · · 1. Dark field microscopy 2. RPR card test 3. VDRL slide test 4. TPHA assay 5. FTA – ABS

Treatment Early Acquired Syphilis ( <2 years from the date of contact · (Primary / Secondary / Early latent syphilis) · Inj. Benzathine Penicillin 24 Lakhs I. U I. M single dose (or) · Inj. Procaine Penicillin 12 Lakhs I. U I. M daily for 10 days ·
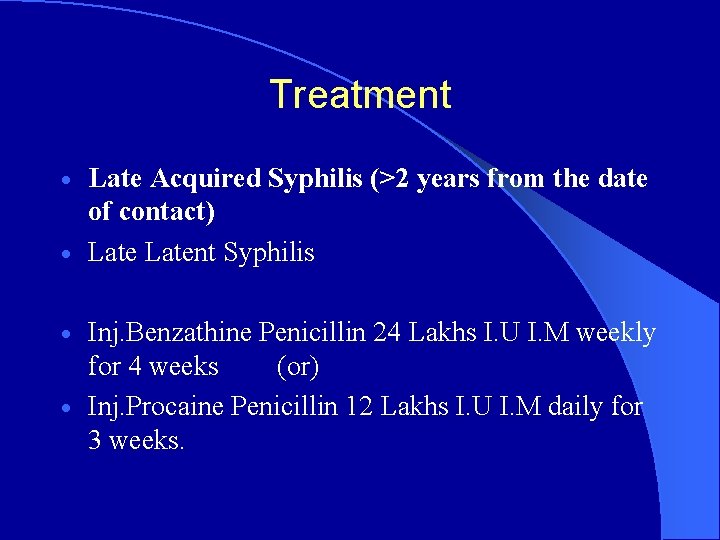
Treatment Late Acquired Syphilis (>2 years from the date of contact) · Latent Syphilis · Inj. Benzathine Penicillin 24 Lakhs I. U I. M weekly for 4 weeks (or) · Inj. Procaine Penicillin 12 Lakhs I. U I. M daily for 3 weeks. ·
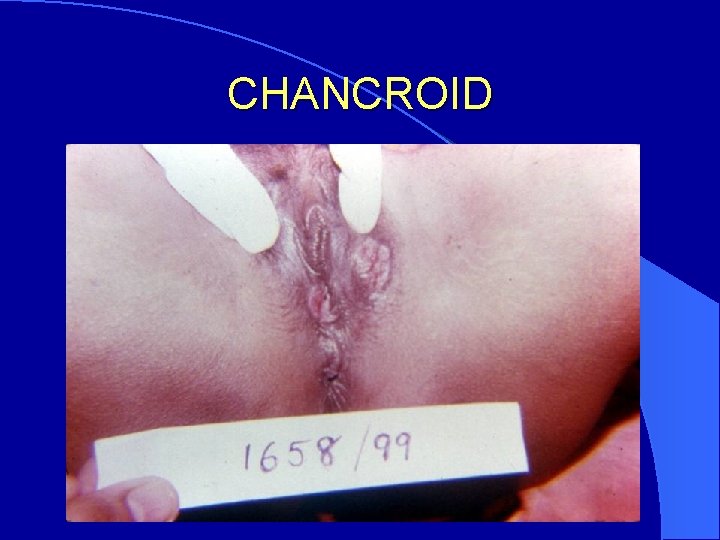
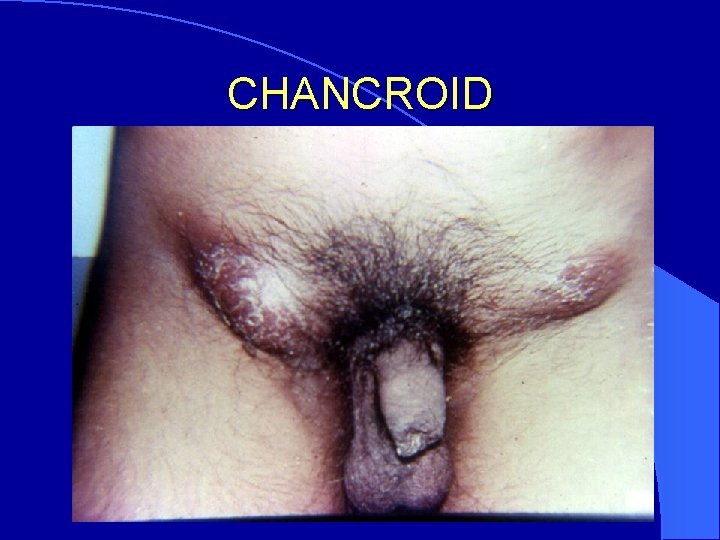
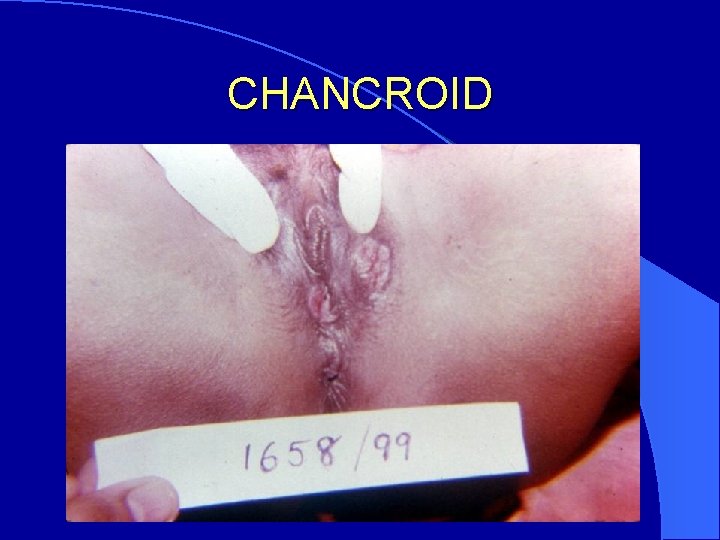
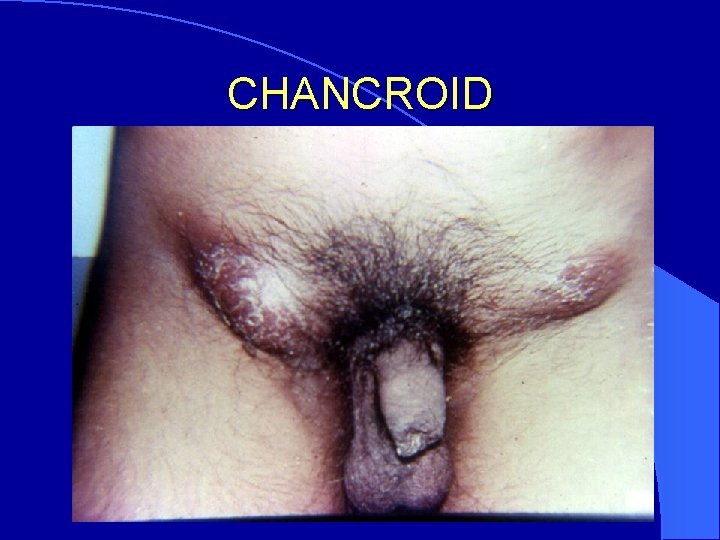
CHANCROID Causative agent : Haemophilus ducreyi Incubation period : 5 -7 days Multiple Soft Painful easily bleeding ulcers with Bubo (Uni locular)

CHANCROID
CHANCROID
CHANCROID
Investigations 1. Smear – Grams stain 2. Culture –Blood enriched media Treatment T. Cotrimoxazole S. S 2 b. d for 10 – 15 days (or) T. Erythromycin 500 m. g q. i. d for 10 – 15 days

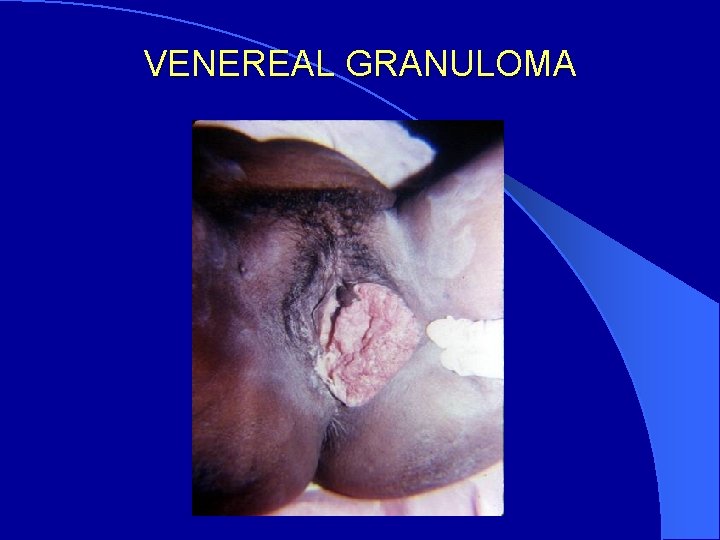
VENEREAL GRANULOMA Causative agent : granulomatis Calymmatobacterium Granulomatous Ulcer with Velvety appearance and wavy margin. Inguinal Lymph nodes not involved

VENEREAL GRANULOMA
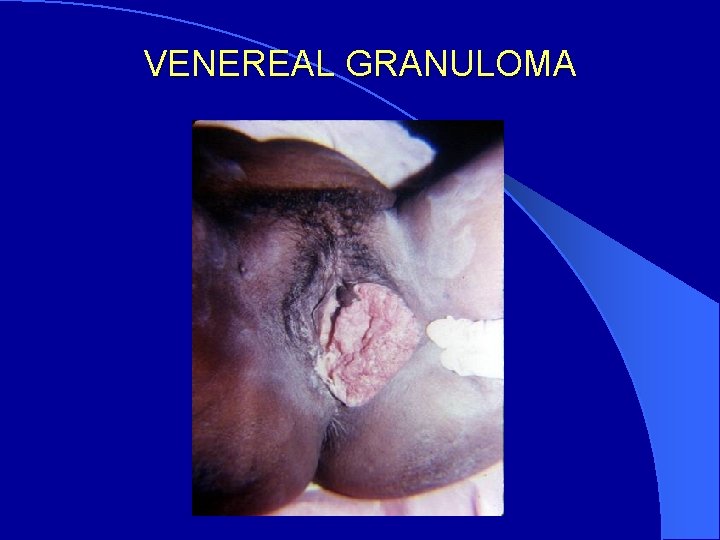
VENEREAL GRANULOMA
Investigations Tissue smear – Leishman’s stain Giemsa stain Treatment T. Erythromycin 500 m. g q. i. d for 10 – 14 days (or) C. Doxycycline 100 m. g b. d for 10 – 14 days (or) C. Tetracycline 500 m. g q. i. d for 10 – 14 days
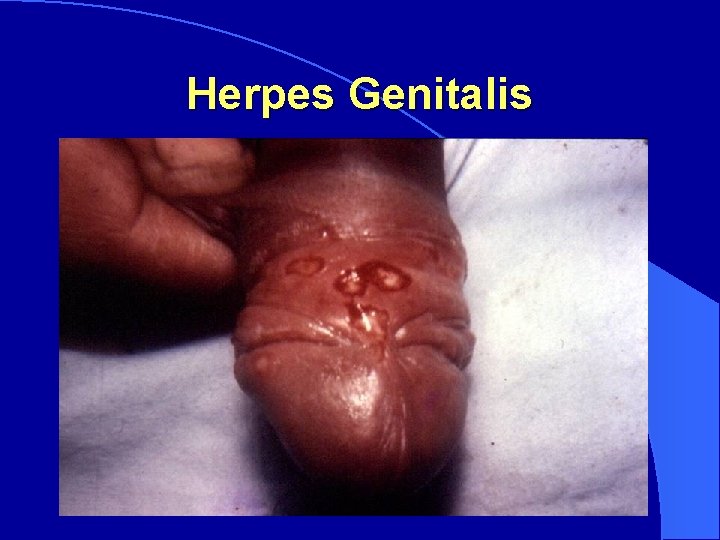
Herpes Genitalis Causative agent : Herpes simplex virus – 2&1 Incubation period : 2 -7 days Grouped Vesicles Rupture and form Superficial, Erosive Ulcer with polycyclic border

Herpes Genitalis
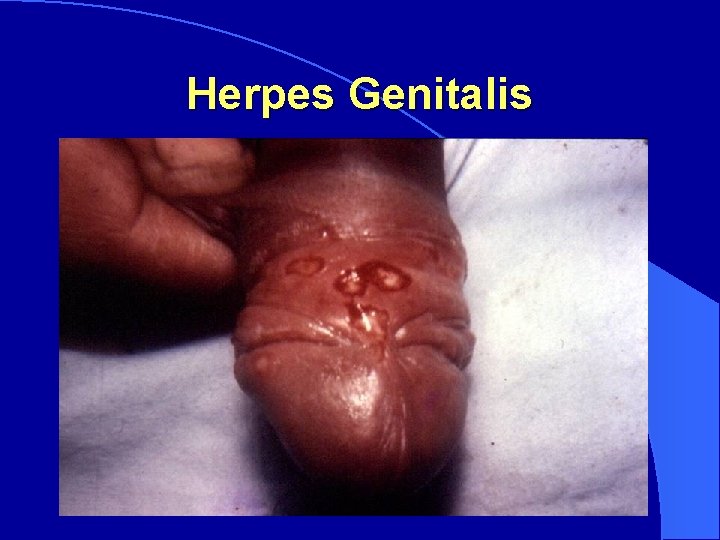
Herpes Genitalis

Investigations Smear – Leishmans stain – multinucleated giant epithelial cells Treatment First clinical episode - T. Acyclovir 200 m. g 5 times daily for 7 days Recurrence - T. Acyclovir 200 m. g 5 times daily for 5 days Acyclovir topical application
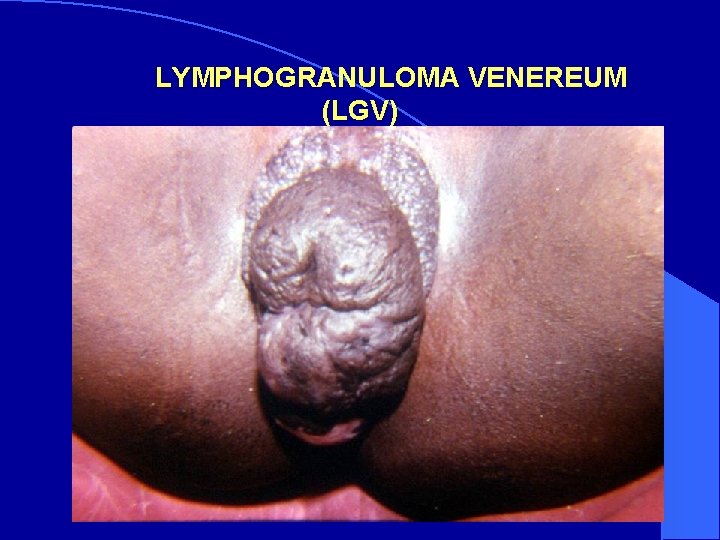
LYMPHOGRANULOMA VENEREUM (LGV) Causative agents : Chlamydia trachomatis (L 1, L 2, L 3) Incubation period : 3 – 21 days Superficial, erosive, transient Ulcer. Usually patient may notice the Ulcer, he will land in the stage of Bubo. (Multi Lacular)

LYMPHOGRANULOMA VENEREUM (LGV)
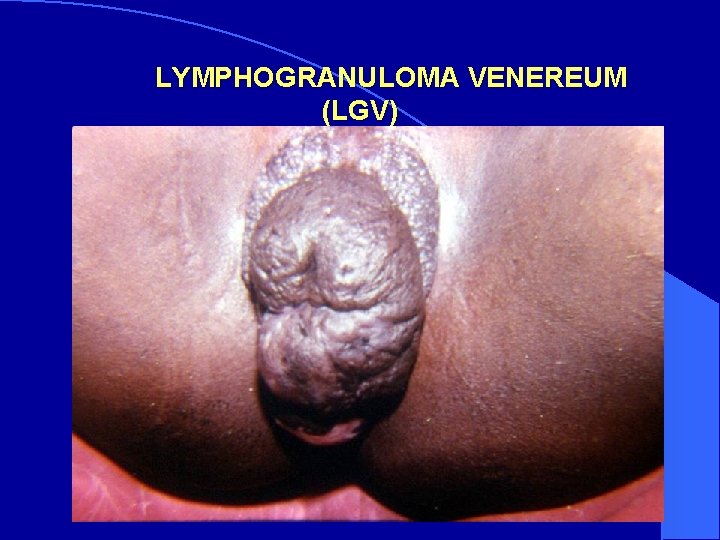
LYMPHOGRANULOMA VENEREUM (LGV)
Investigations 1. Antigen detection –a)Direct Fluorescent Antibody Technique b)ELISA 2. Antibody detection-a)Micro Immuno Fluorescence b)ELISA Treatment C. Doxycycline 100 m. g b. d for 10 – 14 days (or) C. Tetracycline 500 m. g q. i. d for 10 – 14 days Bubo must be aspirated through the normal skin
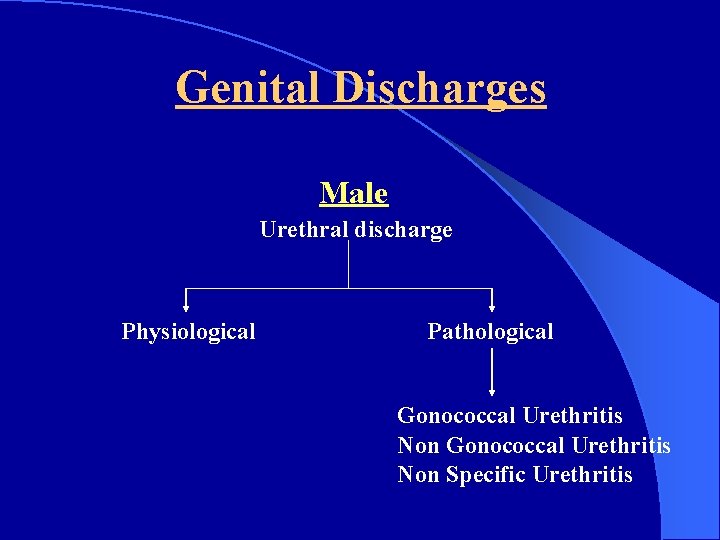
Genital Discharges Male Urethral discharge Physiological Pathological Gonococcal Urethritis Non Specific Urethritis
Genital Discharges Female Vaginal Discharge Physiological Pathological Gonococcal Trichomoniasis Candidiasis Bacterial Vaginosis

GONOCOCCAL INFECTION Causative agent : Neisseria gonorrhoeae Incubation period : 2 – 5 days Sites : Can infect any columnar epithelium urethra, cervix, rectum, pharynx, conjunctiva ( NOT vagina)
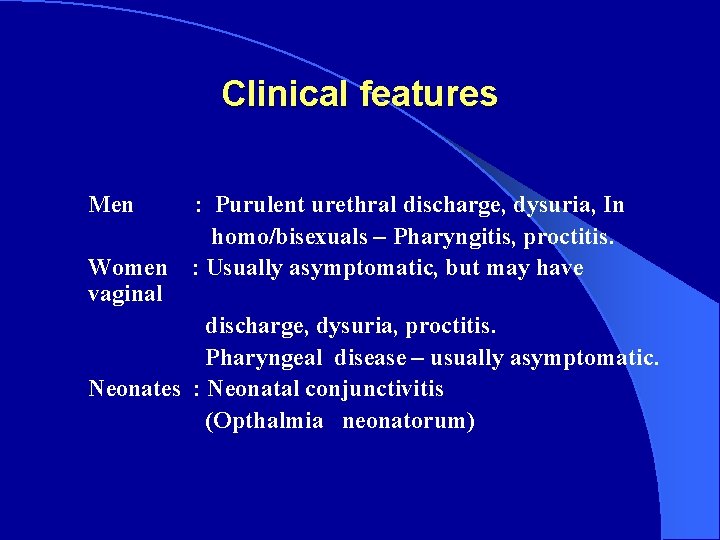
Clinical features Men Women vaginal : Purulent urethral discharge, dysuria, In homo/bisexuals – Pharyngitis, proctitis. : Usually asymptomatic, but may have discharge, dysuria, proctitis. Pharyngeal disease – usually asymptomatic. Neonates : Neonatal conjunctivitis (Opthalmia neonatorum)
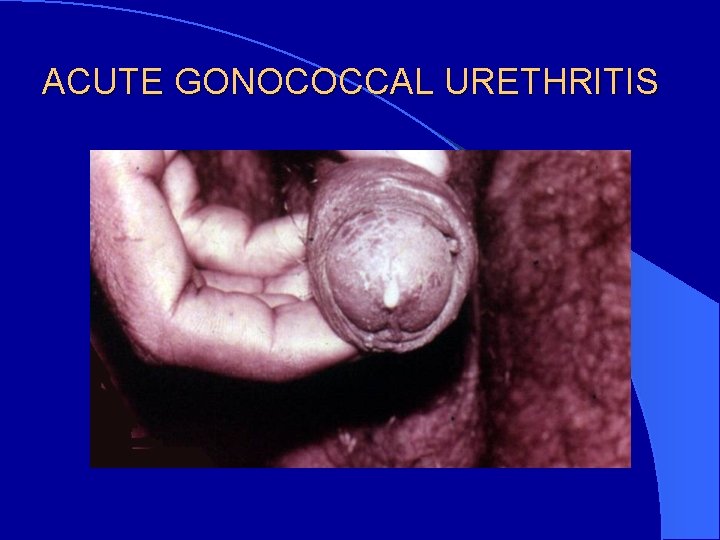
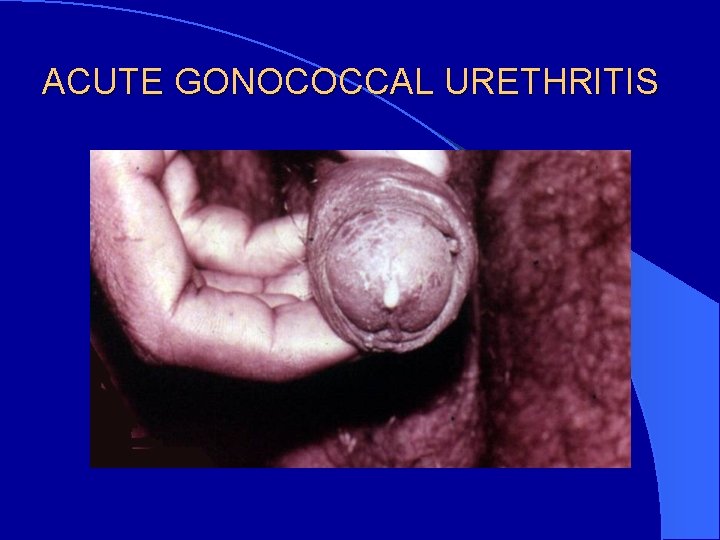
ACUTE GONOCOCCAL URETHRITIS

Investigations 1. Smear – Grams stain 2. Culture – Modified Thayer Martin medium Treatment Inj. Procaine penicillin 48 lakhs I. U I. M single dose after test dose (or) Inj. Kanamycin 2 gram I. M single dose (or) Inj. Gentamycin 240 m. g I. M single dose(or) Inj. Ceftriaxone 250 m. g I. M single dose(or) T. Azithromycin 2 gram orally single dose
NON - GONOCOCCAL URETHRITIS (NGU) Causative agent : Known causes like Trichomonas vaginalis & other microorganisms Incubation period : Variable (1 - 5 weeks) Clinical features: Men : Urethral discharge - slight, mucoid or watery, dysuria or urethral itching. Women : usually asymptomatic, but if associated with cervicitis or salpingitis – Abdominal pain, fever and infertility can occur.
Investigations a)Wet mount – Saline preparation for T. V b) Urine culture & sensitivity Treatment Depending on the cause & sensitivity
TRICHOMONIASIS Causative agent : Trichomonas vaginalis Incubation period : 5 – 28 days Clinical features: About 50 -90% of women asymptomatic, vaginal discharge – usually copious, often greenish yellow, can be frothy, malodor. Erythema of vagina and vulva can present, colpitis macularis (Strawberry cervix) – in a smaller proportion of patients.
Investigations a)Wet mount – Saline preparation b)Culture –Modified Diamond’s medium Treatment T. Metronidazole 200 m. g t. d. s for 7 days (or) T. Metronidazole 2 grams single dose
CANDIDIASIS Causative agent : Candida albicans Clinical features : Discharge – thick white curd like vaginal discharge. Counter part in men : Candidal balanoposthitis
Investigations a)Wet mount – KOH preparation b)Smear – Gram’s stain c)Culture –Sabouraud’s medium Treatment T. Fluconazole 150 m. g single dose (or) Clotrimazole 200 m. g intra vaginally daily for 3 days
Bacterial Vaginosis (BV) Causative agents : G. vaginalis, Mobiluncus, Bacteroides. Clinical features Thin homogenous white adherent discharge.
Investigations 1. Saline wet mount – Clue cells 2. Whiff test Treatment T. Metronidazole 400 m. g t. d. s for 7 days (or) T. Clindamycin 300 m. g b. d for 7 days
NON – SPECIFIC URETHRITIS (NSU) Causative agent : C. Trachomatis (D to K), Ureaplasma, Mycoplasma, etc. Incubation period : Variable (1 - 5 weeks) Clinical features: Men : Urethral discharge - slight, mucoid or watery, dysuria or urethral itching. Women : usually asymptomatic, but if associated with cervicitis or salpingitis - pain, fever and infertility can occur. Treatment C. Doxycycline 100 m. g b. d for 7 days

Pelvic Inflammatory disease (PID) Causative agents : N. gonorrhoeae, C. trachomatis, Prevotella, Mobiluncus, M. hominis, Ureaplasma etc. Incubation Period : Variable Clinical features Lower abdominal tenderness, bilateral adnexal tenderness Cervical motion tenderness, Negative pregnancy test.
Investigations 1. Smear for G. C 2. Culture for G. C 3. Wet film for T. V 4. USG abdomen Treatment 1) C. Doxycycline 100 m. g b. d for 10 – 14 days & T. Metronidazole 400 m. g t. d. s for 10 days (or) 2) Inj. Ceftriaxone 250 m. g i. m single dose & C. Doxycycline 100 m. g b. d for 10 – 14 days& T. Metronidazole 400 m. g t. d. s for 10 days
Genital Warts Causative agents : Human papilloma virus (HPV-6, 11, 18…) Incubation period : 1 to 6 months.
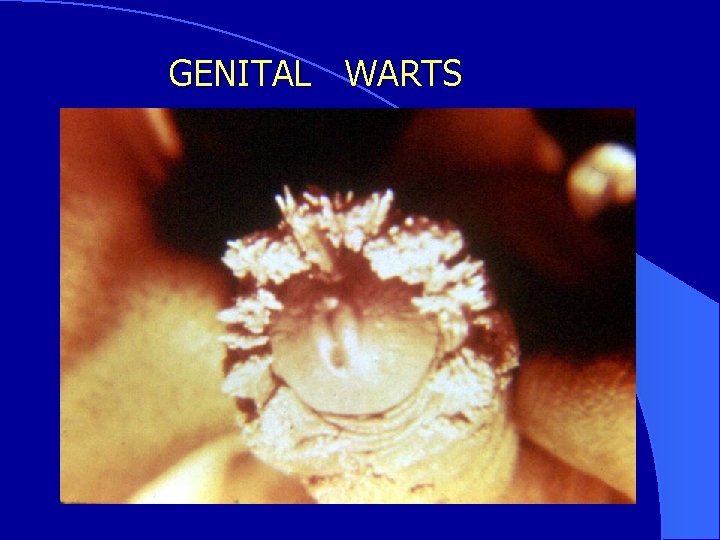
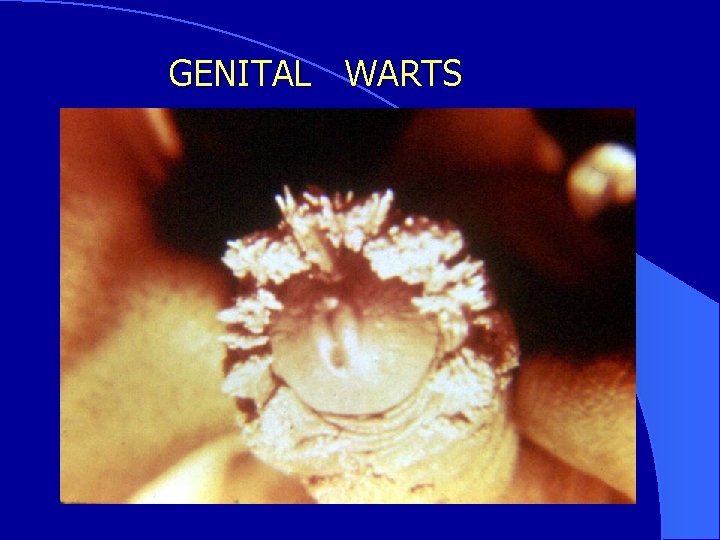
GENITAL WARTS

Investigations Histo pathology Treatment 1. Chemical cautery – application of podophyllum 2. Cryotherapy 3. Electrocautery 4. Excision
SYNDROMIC MANAGEMENT OF STD l The syndromic approach is an approach where the health care providers diagnose and treat patients on the basis of groups of symptoms or signs rather than for specific STD.
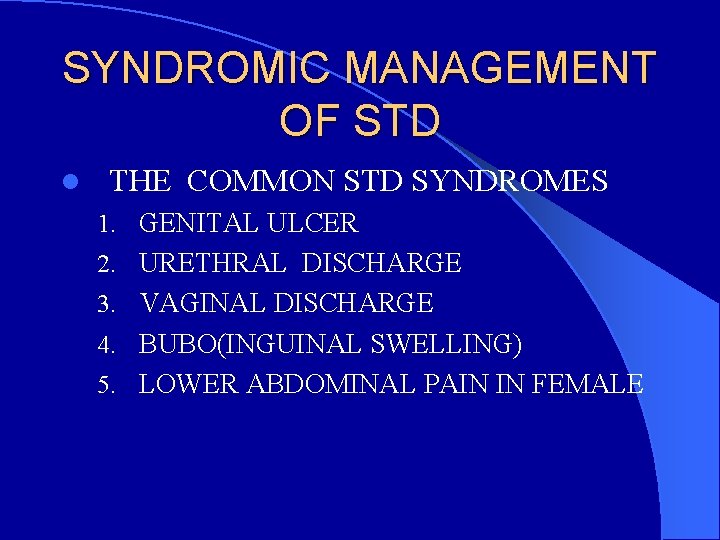
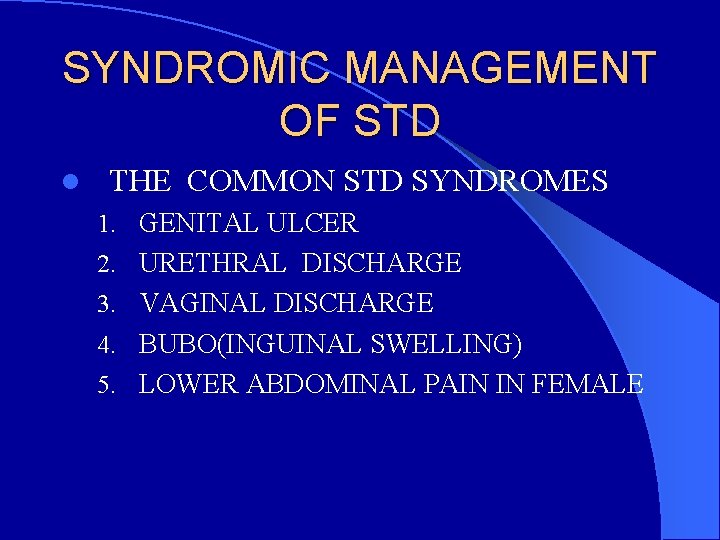
SYNDROMIC MANAGEMENT OF STD l THE COMMON STD SYNDROMES 1. GENITAL ULCER 2. URETHRAL DISCHARGE 3. VAGINAL DISCHARGE 4. BUBO(INGUINAL SWELLING) 5. LOWER ABDOMINAL PAIN IN FEMALE
BENEFITS OF SYNDROMIC MANAGEMENT – SIMPLE IN ITS APPROACH – MISDIAGNOSIS & INAPPROPRIATE TREATMENT ARE REDUCED. – IMMEDIATE TREATMENT CAN BE PROVIDED-NO WAITING TIME FOR INVESTIGATIONS – HELPS IN PREVENTION OF TRANSMISSION OF HIV – SINGLE VISIT - COST EFFECTIVE.
DISADVANTAGES-LIMITATIONS OF SYNDROMIC MANAGEMENT l SINCE THE TREATMENT IS ON A SINGLE VISIT, FOLLOW UP IS DIFFICULT l OVERDOSING MAY RESULT l WASTAGE OF DRUGS l CHANCES OF DEVELOPMENT OF RESISTANT STRAINS
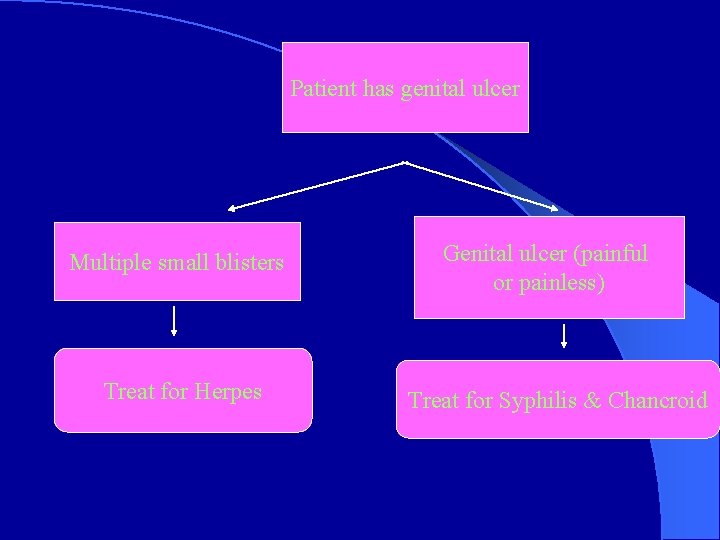
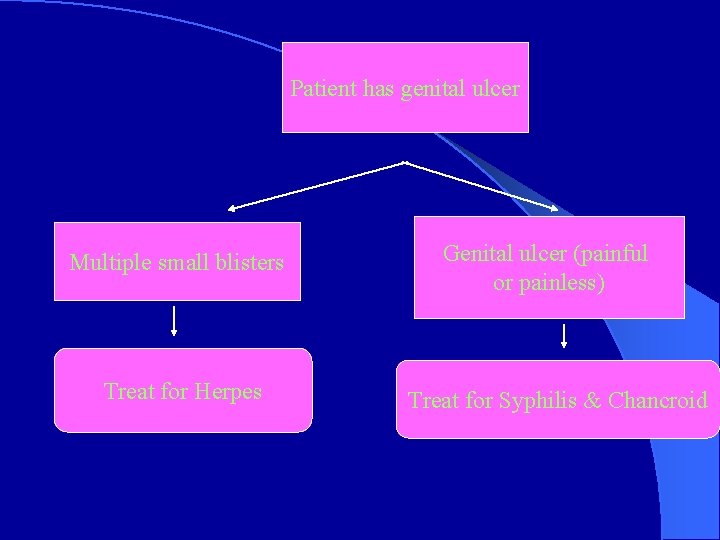
Patient has genital ulcer Multiple small blisters Treat for Herpes Genital ulcer (painful or painless) Treat for Syphilis & Chancroid
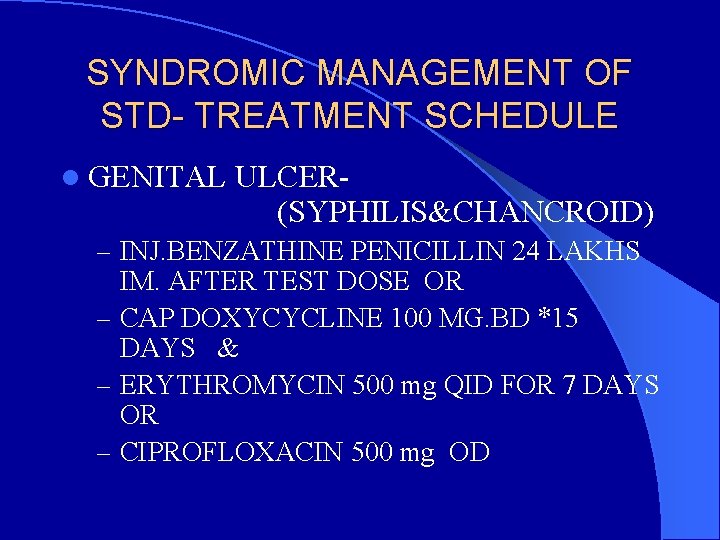
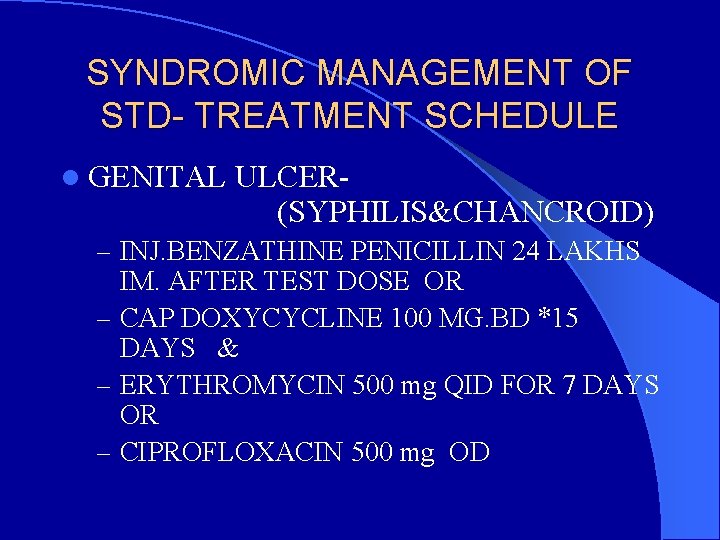
SYNDROMIC MANAGEMENT OF STD- TREATMENT SCHEDULE l GENITAL ULCER(SYPHILIS&CHANCROID) – INJ. BENZATHINE PENICILLIN 24 LAKHS IM. AFTER TEST DOSE OR – CAP DOXYCYCLINE 100 MG. BD *15 DAYS & – ERYTHROMYCIN 500 mg QID FOR 7 DAYS OR – CIPROFLOXACIN 500 mg OD
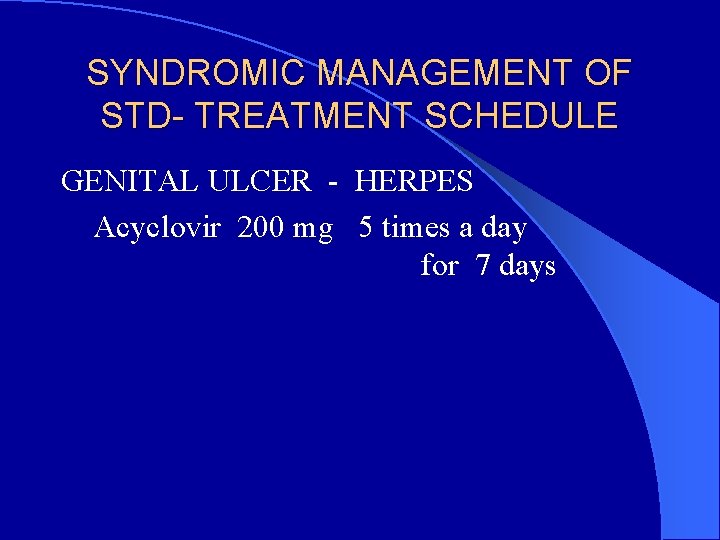
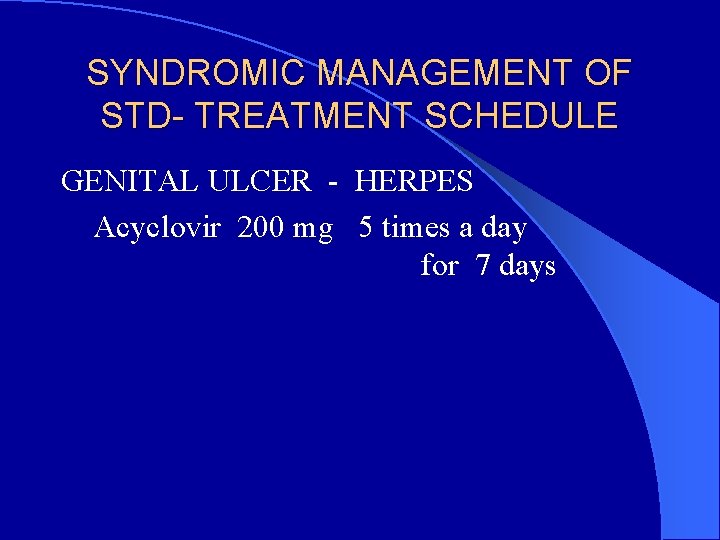
SYNDROMIC MANAGEMENT OF STD- TREATMENT SCHEDULE GENITAL ULCER - HERPES Acyclovir 200 mg 5 times a day for 7 days
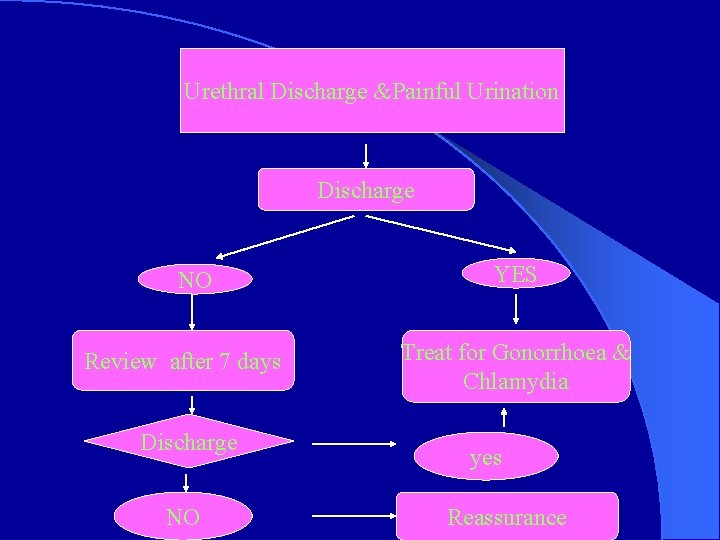
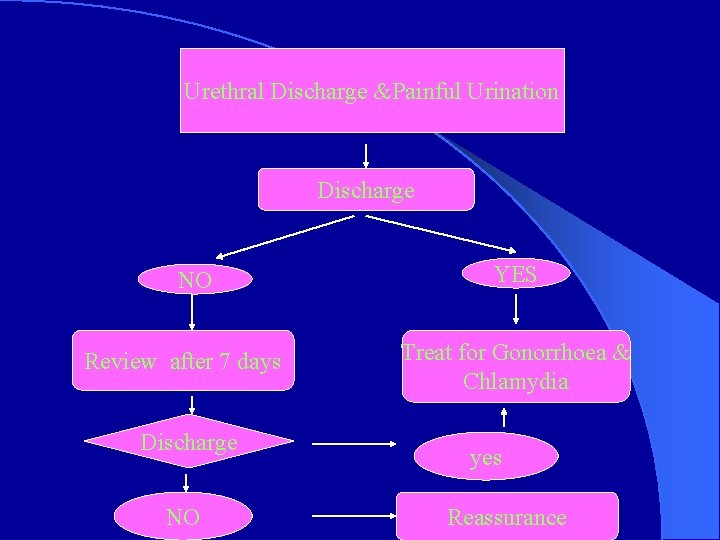
Urethral Discharge &Painful Urination Discharge NO Review after 7 days Discharge NO YES Treat for Gonorrhoea & Chlamydia yes Reassurance
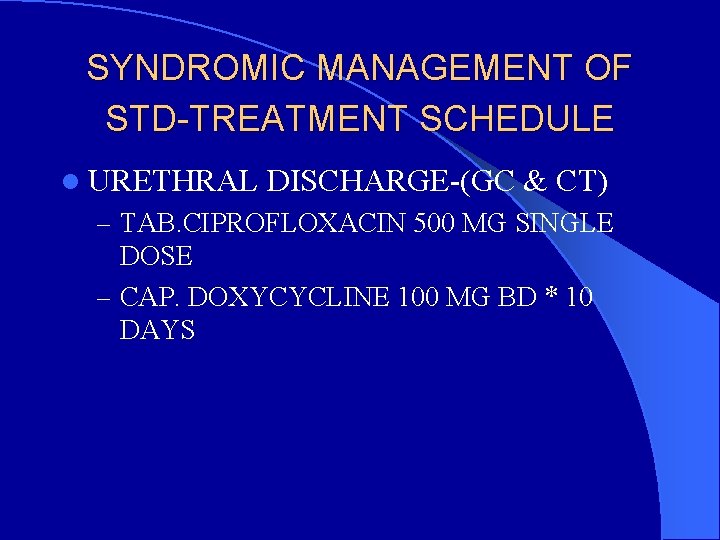
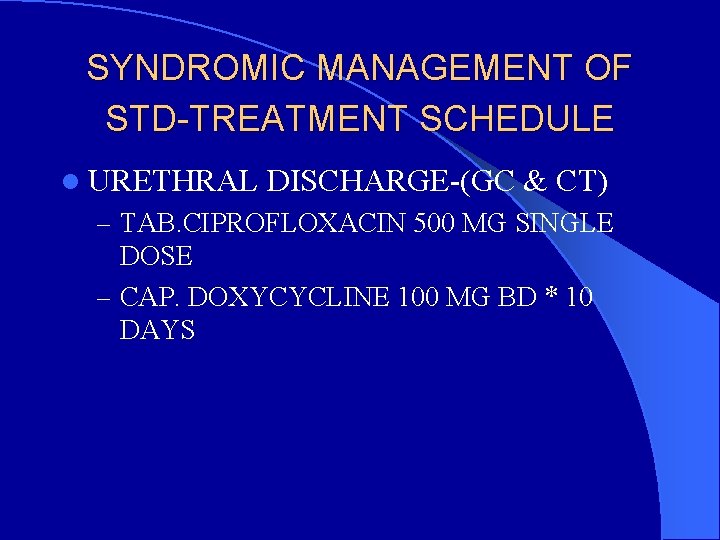
SYNDROMIC MANAGEMENT OF STD-TREATMENT SCHEDULE l URETHRAL DISCHARGE-(GC & CT) – TAB. CIPROFLOXACIN 500 MG SINGLE DOSE – CAP. DOXYCYCLINE 100 MG BD * 10 DAYS
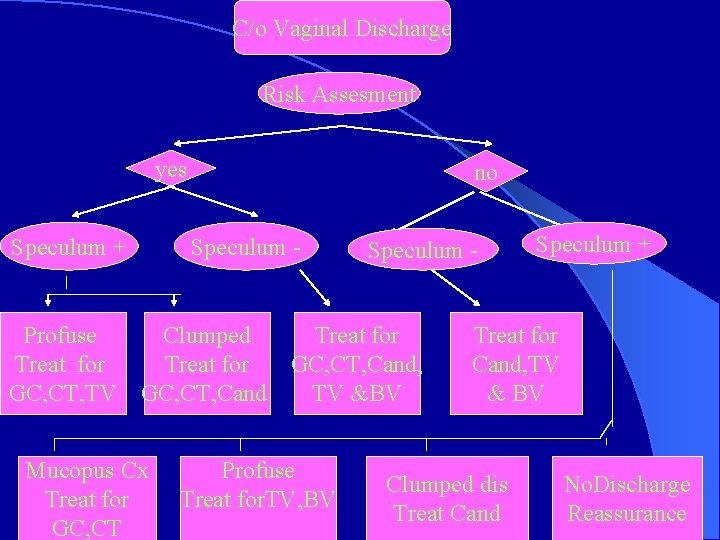
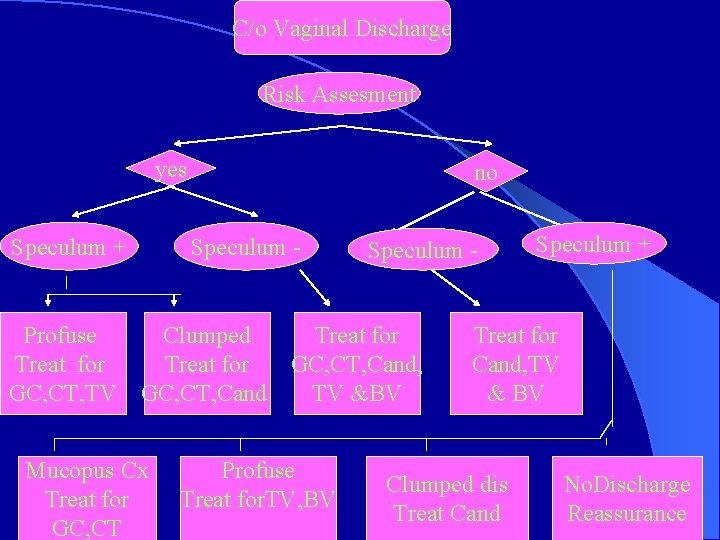
C/o Vaginal Discharge Risk Assesment yes Speculum + no Speculum - Profuse Clumped Treat for GC, CT, Cand, GC, CT, TV GC, CT, Cand TV &BV Mucopus Cx Treat for GC, CT Profuse Treat for. TV, BV Speculum + Treat for Cand, TV & BV Clumped dis Treat Cand No. Discharge Reassurance
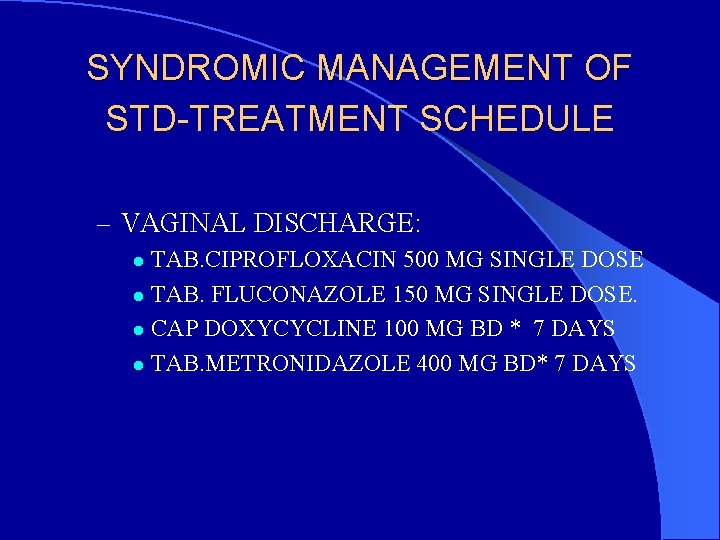
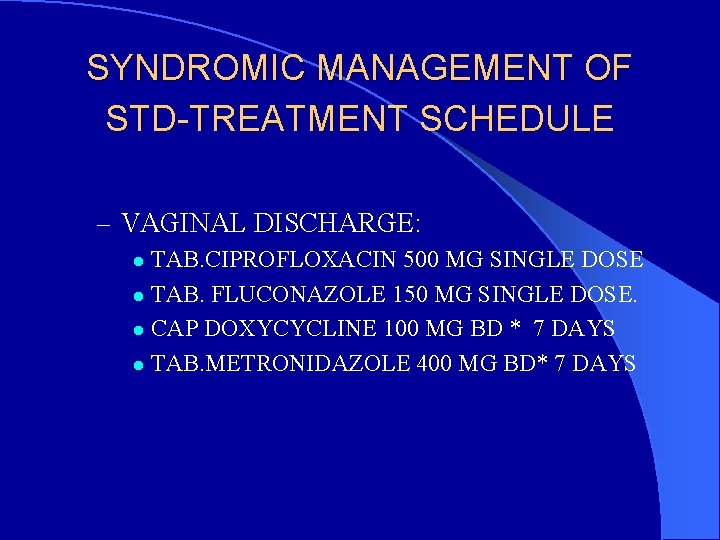
SYNDROMIC MANAGEMENT OF STD-TREATMENT SCHEDULE – VAGINAL DISCHARGE: TAB. CIPROFLOXACIN 500 MG SINGLE DOSE l TAB. FLUCONAZOLE 150 MG SINGLE DOSE. l CAP DOXYCYCLINE 100 MG BD * 7 DAYS l TAB. METRONIDAZOLE 400 MG BD* 7 DAYS l
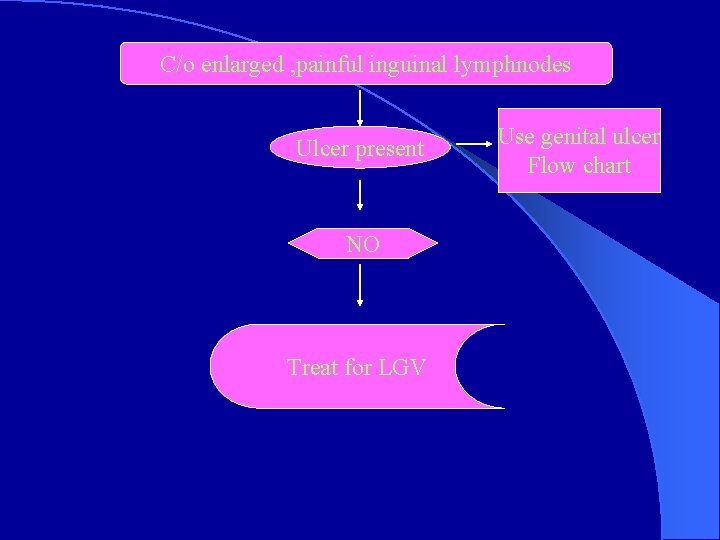
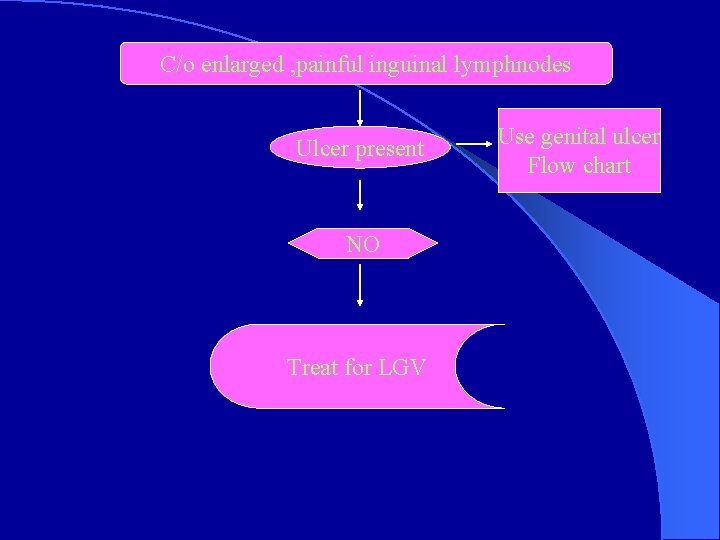
C/o enlarged , painful inguinal lymphnodes Ulcer present NO Treat for LGV Use genital ulcer Flow chart
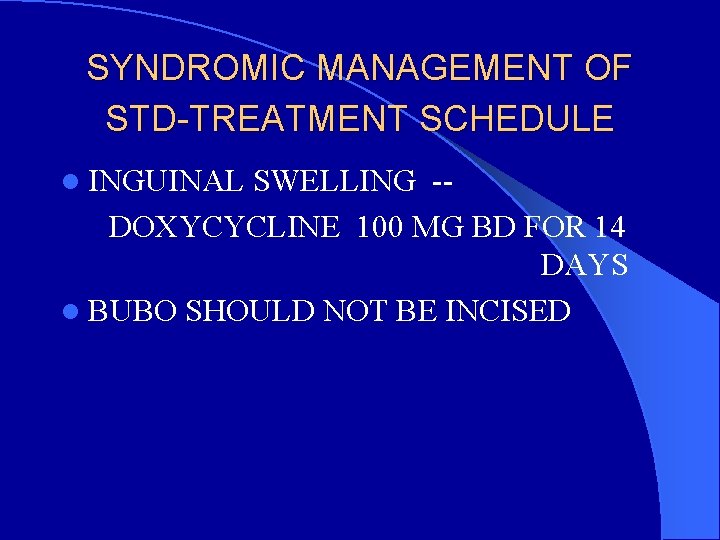
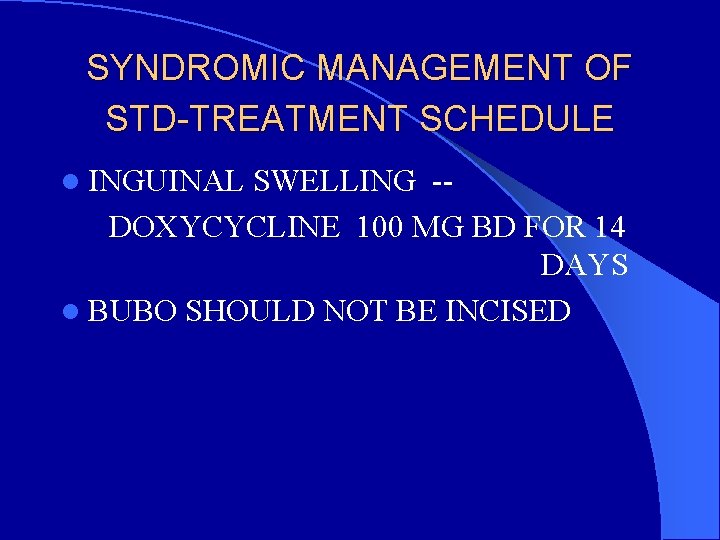
SYNDROMIC MANAGEMENT OF STD-TREATMENT SCHEDULE l INGUINAL SWELLING -DOXYCYCLINE 100 MG BD FOR 14 DAYS l BUBO SHOULD NOT BE INCISED
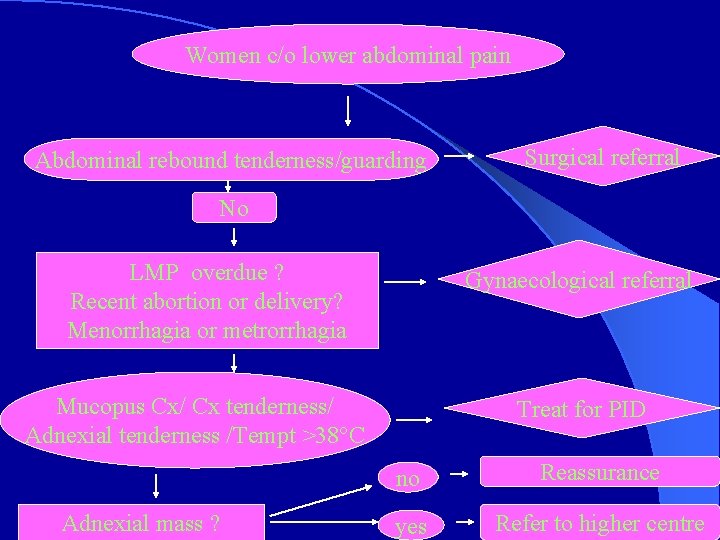
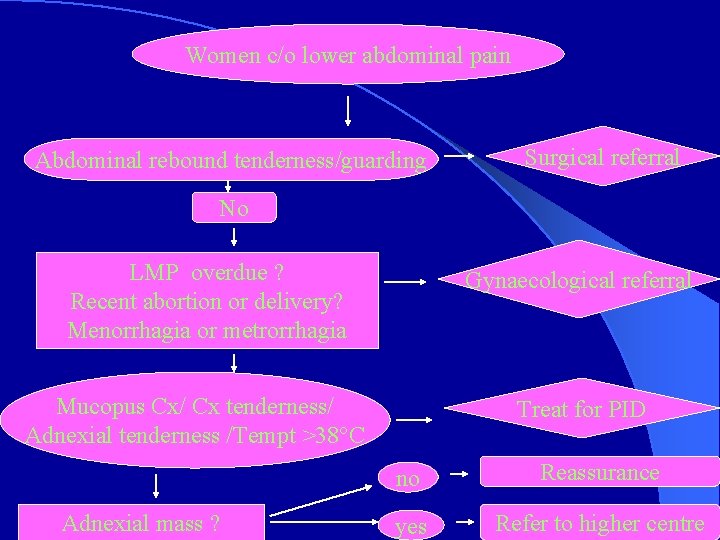
Women c/o lower abdominal pain Abdominal rebound tenderness/guarding Surgical referral No LMP overdue ? Recent abortion or delivery? Menorrhagia or metrorrhagia Gynaecological referral Mucopus Cx/ Cx tenderness/ Adnexial tenderness /Tempt >38°C Adnexial mass ? Treat for PID no Reassurance yes Refer to higher centre
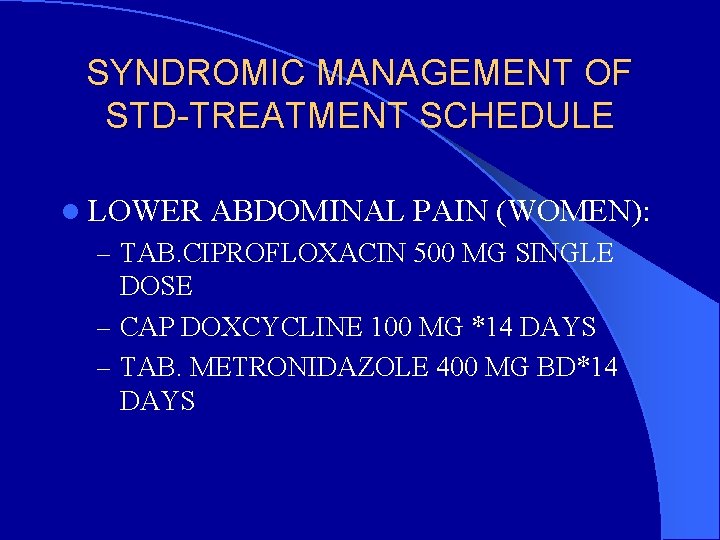
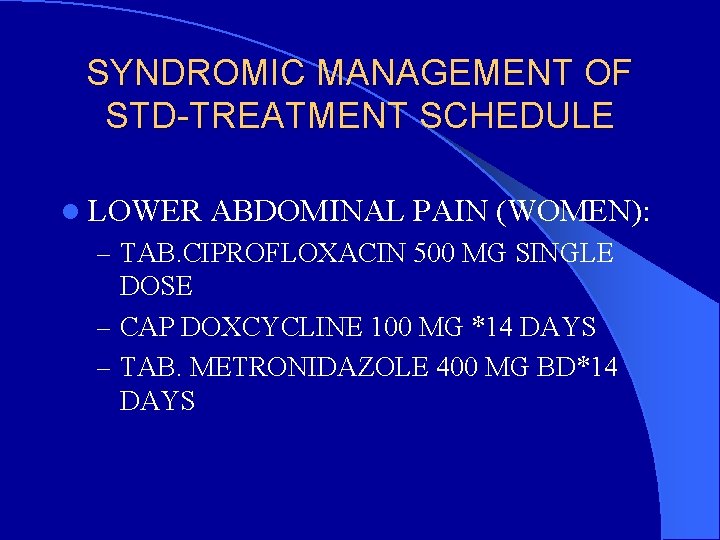
SYNDROMIC MANAGEMENT OF STD-TREATMENT SCHEDULE l LOWER ABDOMINAL PAIN (WOMEN): – TAB. CIPROFLOXACIN 500 MG SINGLE DOSE – CAP DOXCYCLINE 100 MG *14 DAYS – TAB. METRONIDAZOLE 400 MG BD*14 DAYS
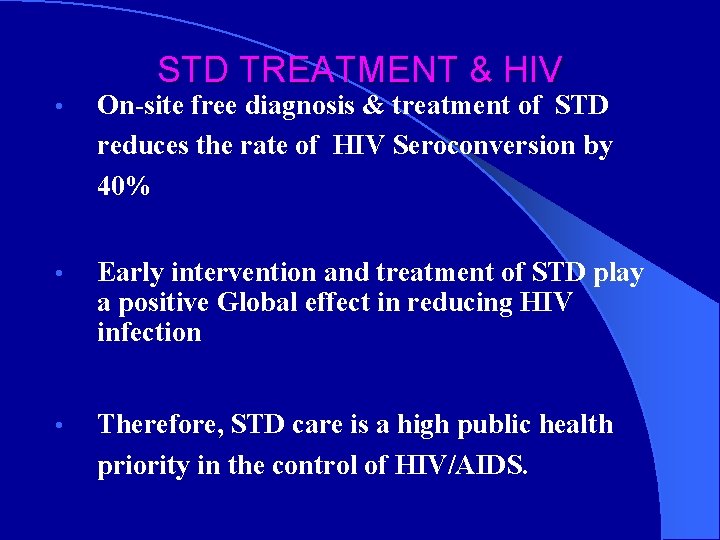
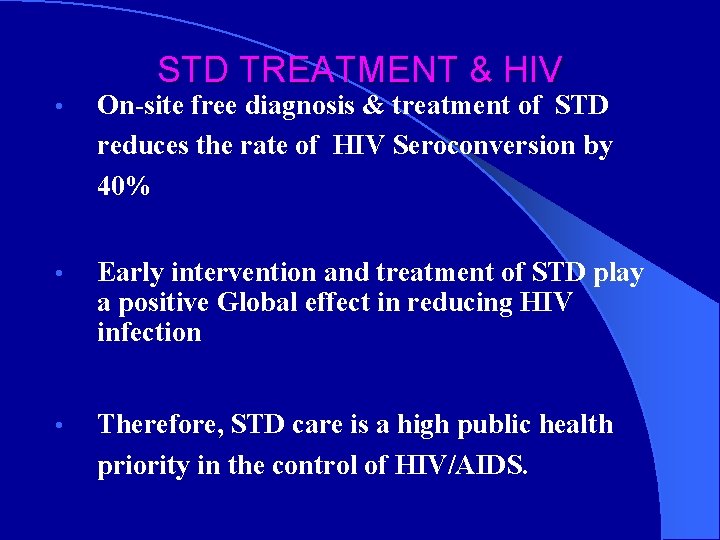
STD TREATMENT & HIV • On-site free diagnosis & treatment of STD reduces the rate of HIV Seroconversion by 40% • Early intervention and treatment of STD play a positive Global effect in reducing HIV infection • Therefore, STD care is a high public health priority in the control of HIV/AIDS.

 Peran manajer sti
Peran manajer sti What does the root sta/sti mean
What does the root sta/sti mean Rails sti vs polymorphic
Rails sti vs polymorphic Ceri evans
Ceri evans Sti
Sti Kit 1 std
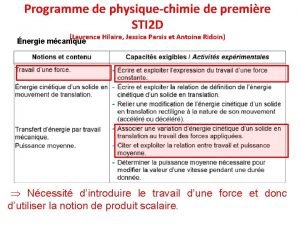
Kit 1 std Sti 2 d
Sti 2 d Peran manajer sti
Peran manajer sti Salpingitits
Salpingitits I sti
I sti Identify the meaning of the root sta/sti.
Identify the meaning of the root sta/sti. Sti stands for
Sti stands for Pemtic
Pemtic Dca to sti
Dca to sti Cpro sti portfolio
Cpro sti portfolio Sti university moscow
Sti university moscow 17 year old penis
17 year old penis Portail sti
Portail sti Diomed biyoteknoloji san.tic.ltd.şti
Diomed biyoteknoloji san.tic.ltd.şti What stds are curable
What stds are curable Stif competencies
Stif competencies Max leonardo
Max leonardo Sti 2 d
Sti 2 d Direktorat sti upi
Direktorat sti upi Sti
Sti Hycode sti
Hycode sti Wpe effect in layout
Wpe effect in layout Std vs sti
Std vs sti Sexually transmitted diseases
Sexually transmitted diseases Fiebig hiv
Fiebig hiv Hora de agora
Hora de agora Chapter 25 sexually transmitted infections and hiv/aids
Chapter 25 sexually transmitted infections and hiv/aids Procentowe ryzyko zakażenia hiv
Procentowe ryzyko zakażenia hiv Hiv diagnostics conference
Hiv diagnostics conference Chii chinonzi hiv
Chii chinonzi hiv Hiv
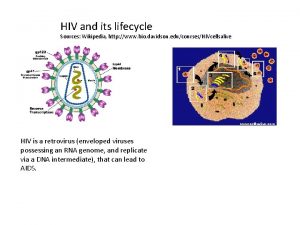
Hiv Hiv life cycle
Hiv life cycle Hiv cure
Hiv cure Főember az úton kocsi rázza
Főember az úton kocsi rázza Hiv diagnosis algorithm
Hiv diagnosis algorithm Hiv adalah
Hiv adalah Hiv
Hiv Hiv treatments
Hiv treatments Hiv test results
Hiv test results Types of hiv counselling
Types of hiv counselling Ibase hiv
Ibase hiv Hiv stays alive in dried blood
Hiv stays alive in dried blood Itil wikipedia fr
Itil wikipedia fr Where did hiv come from
Where did hiv come from Syntom på klamydia
Syntom på klamydia Triệu chứng nhiễm hiv
Triệu chứng nhiễm hiv Hiv transmissions
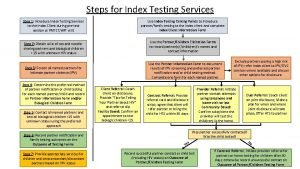
Hiv transmissions 10 steps of index testing
10 steps of index testing Vertical resposta
Vertical resposta Hiv in adults
Hiv in adults Alur pelayanan hiv di puskesmas
Alur pelayanan hiv di puskesmas Hiv test window period
Hiv test window period Hiv
Hiv Ephi ethiopia
Ephi ethiopia Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Ciclo do hiv
Ciclo do hiv Hiv vaccinr
Hiv vaccinr Window period hiv
Window period hiv Hiv
Hiv Patogenesis hiv
Patogenesis hiv Tabela perímetro cefálico por idade
Tabela perímetro cefálico por idade Most common malignancy in hiv
Most common malignancy in hiv Hiv lifecycle
Hiv lifecycle Hiv
Hiv Received oral from hiv positive
Received oral from hiv positive Causative organism of hiv/aids
Causative organism of hiv/aids Objawy hiv
Objawy hiv Hiv retrovirus
Hiv retrovirus Hiv in adults
Hiv in adults Global hiv prevention coalition
Global hiv prevention coalition Hiv risk factors
Hiv risk factors Prognas adalah
Prognas adalah Burkitt lymphoma
Burkitt lymphoma Hiv
Hiv Yu1u
Yu1u Vidas hiv duo ultra package insert
Vidas hiv duo ultra package insert Hiv virus
Hiv virus