Scoring system in ICU Sedation in ICU Dr

- Slides: 49
Scoring system in ICU & Sedation in ICU Dr. Ashton D'Souza Moderator : Dr. Sudesh Rao
v The practice of critical care medicine, which originated in the 1940 s with anesthesiologists providing life support to patients with polio, has undergone revolutionary changes. v The development of new equipment, procedures, and medications has enabled intensivists to treat critically ill patients and support them through increasingly invasive procedures.
v Scoring systems for ICU allow an assessment of the severity of disease and provide an estimate of in-hospital mortality v A weighting is applied to each variable, and the sum of the weighted individual scores produces the severity score. v Physiology based scoring system is better than diagnosis based scoring systems
Parts of Scoring system : 1. Severity Score 2. Calculated probablity of mortality The Ideal Scoring System : 1. simple, reliable, easily obtainable 2. wide patient applicabilty: different diagnosis all age groups all levels or types of ICU 3. high sensitivity and specificity 4. stimulates improvement in outcome 5. independent of treatment 6. ability to predict functional status or quality of life after ICU discharge
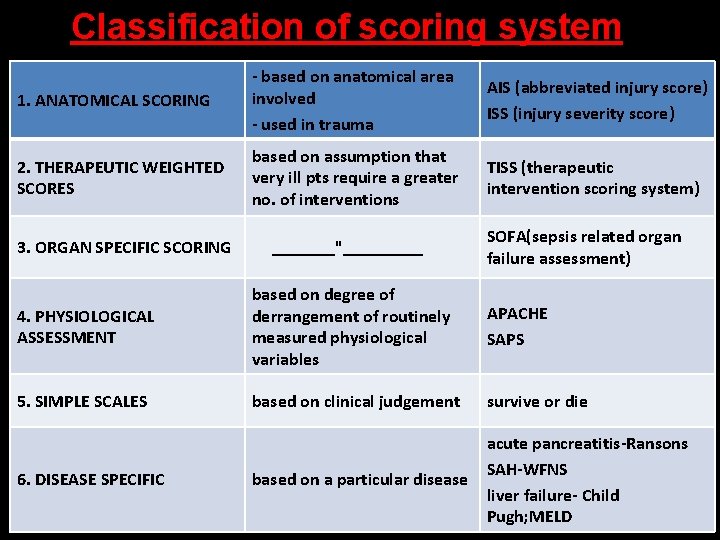
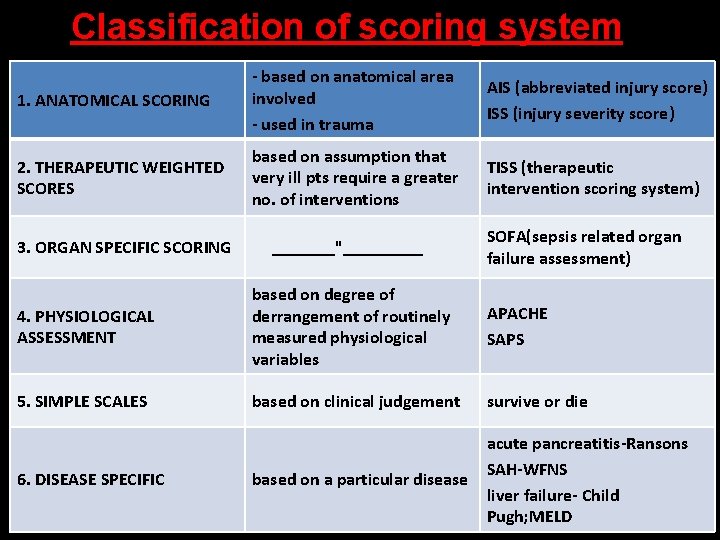
Classification of scoring system 1. ANATOMICAL SCORING - based on anatomical area involved - used in trauma AIS (abbreviated injury score) ISS (injury severity score) 2. THERAPEUTIC WEIGHTED SCORES based on assumption that very ill pts require a greater no. of interventions TISS (therapeutic intervention scoring system) 3. ORGAN SPECIFIC SCORING _______"_____ SOFA(sepsis related organ failure assessment) 4. PHYSIOLOGICAL ASSESSMENT based on degree of derrangement of routinely measured physiological variables APACHE SAPS 5. SIMPLE SCALES based on clinical judgement survive or die based on a particular disease acute pancreatitis-Ransons SAH-WFNS liver failure- Child Pugh; MELD 6. DISEASE SPECIFIC
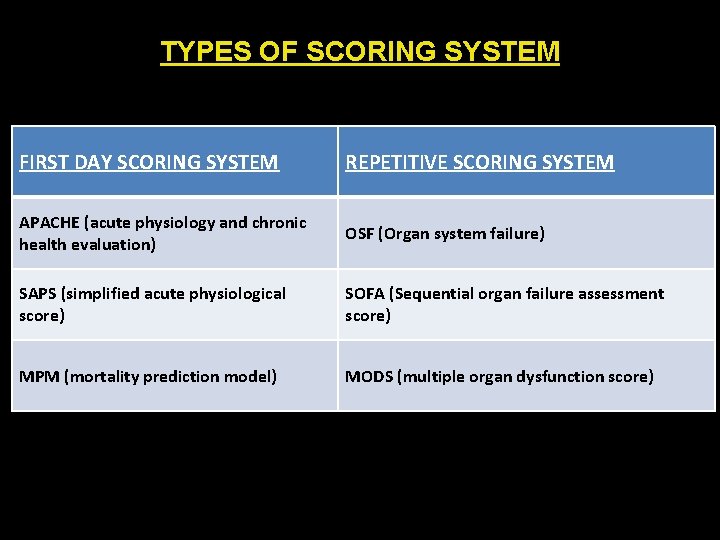
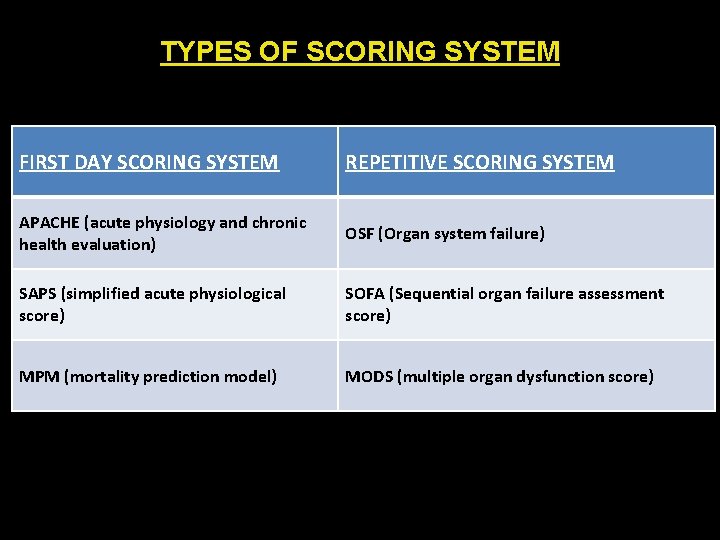
TYPES OF SCORING SYSTEM FIRST DAY SCORING SYSTEM REPETITIVE SCORING SYSTEM APACHE (acute physiology and chronic health evaluation) OSF (Organ system failure) SAPS (simplified acute physiological score) SOFA (Sequential organ failure assessment score) MPM (mortality prediction model) MODS (multiple organ dysfunction score)
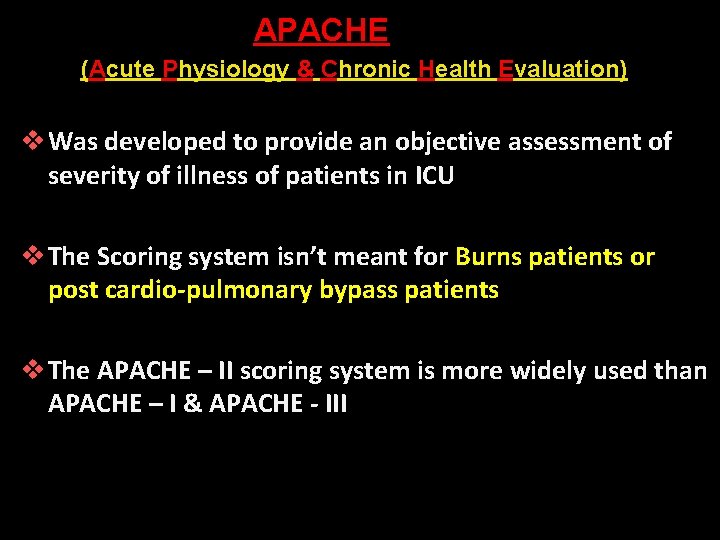
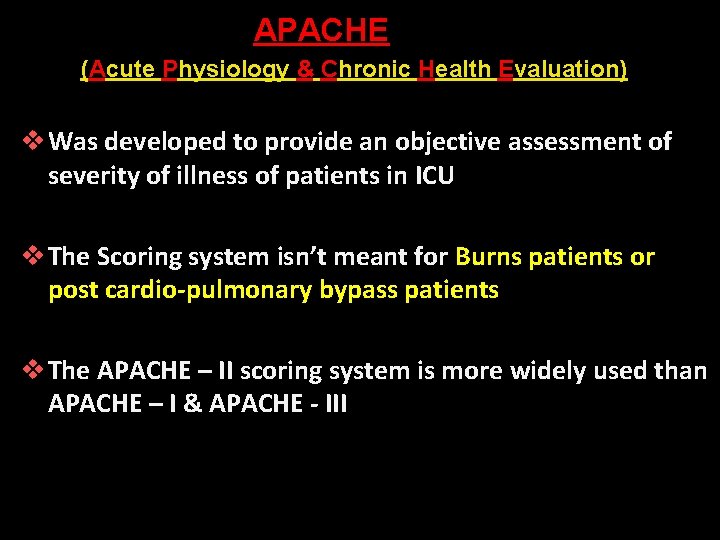
APACHE (Acute Physiology & Chronic Health Evaluation) v Was developed to provide an objective assessment of severity of illness of patients in ICU v The Scoring system isn’t meant for Burns patients or post cardio-pulmonary bypass patients v The APACHE – II scoring system is more widely used than APACHE – I & APACHE - III
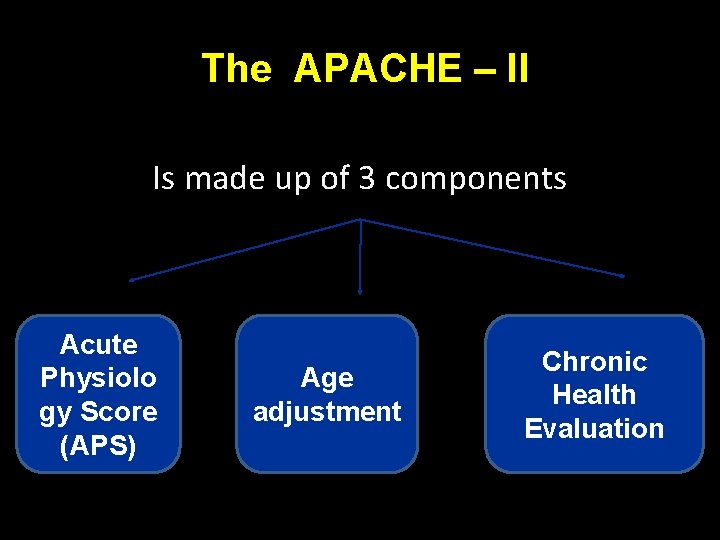
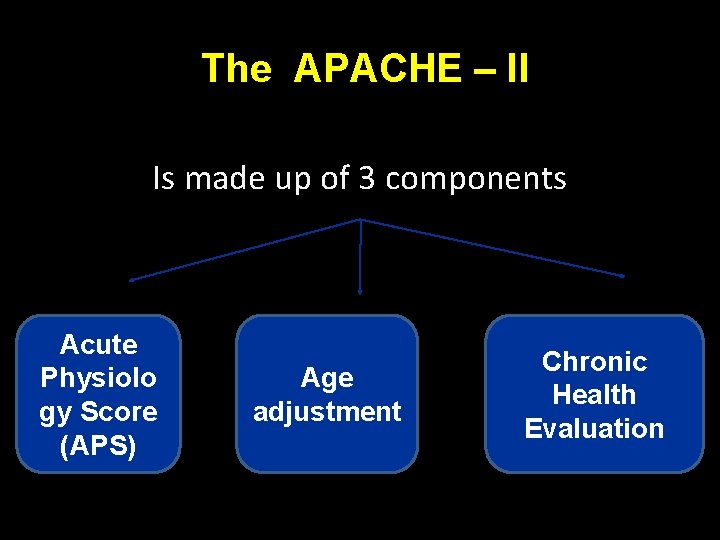
The APACHE – II Is made up of 3 components Acute Physiolo gy Score (APS) Age adjustment Chronic Health Evaluation
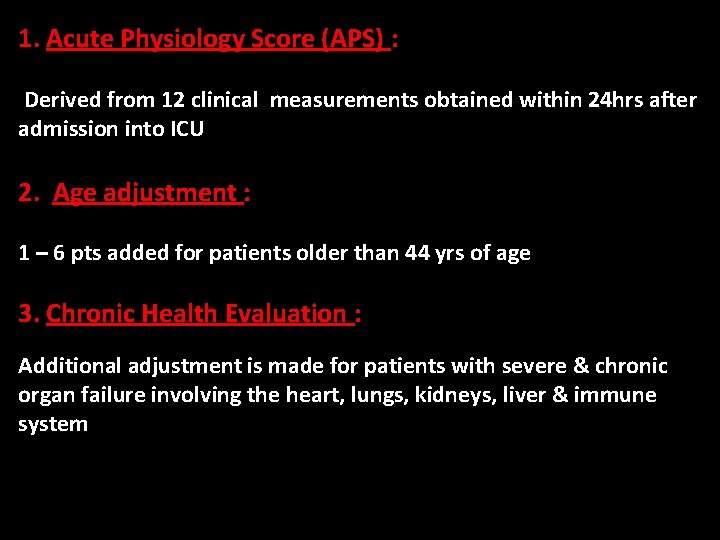
1. Acute Physiology Score (APS) : Derived from 12 clinical measurements obtained within 24 hrs after admission into ICU A variable is assigned 0 pts if its not measured 2. Age adjustment : 1 – 6 pts added for patients older than 44 yrs of age 3. Chronic Health Evaluation : Additional adjustment is made for patients with severe & chronic organ failure involving the heart, lungs, kidneys, liver & immune system
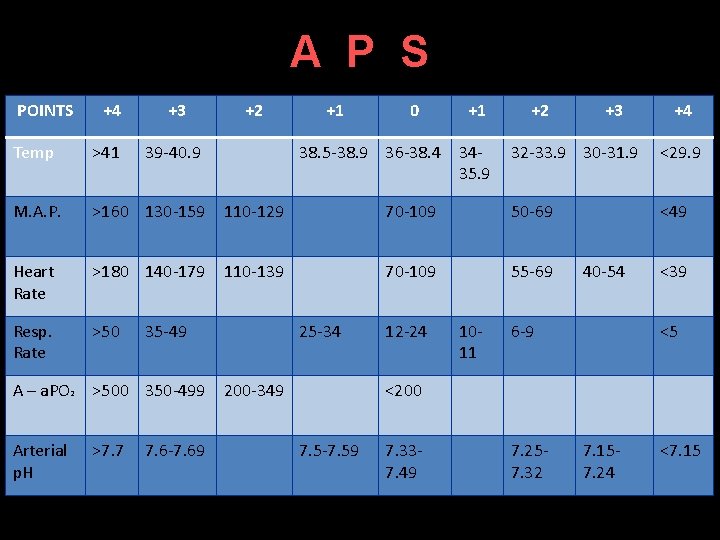
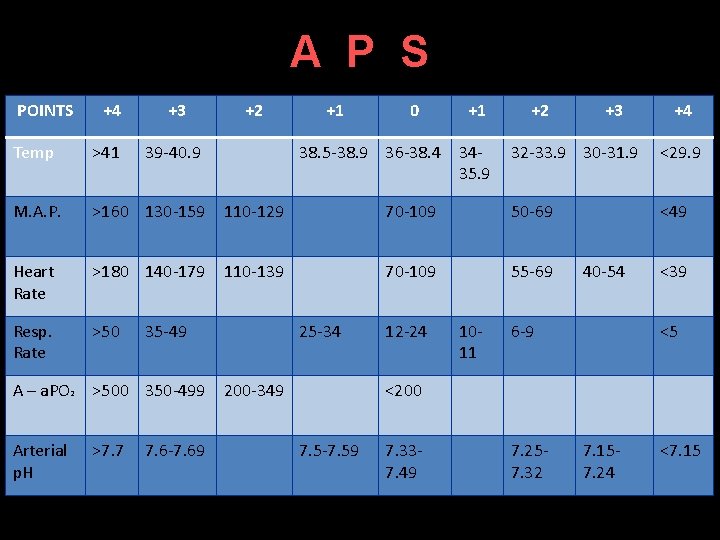
A P S POINTS +4 +3 +2 Temp >41 39 -40. 9 M. A. P. >160 130 -159 110 -129 Heart Rate >180 140 -179 110 -139 Resp. Rate >50 Arterial p. H >7. 7 7. 6 -7. 69 0 +1 38. 5 -38. 9 36 -38. 4 3435. 9 35 -49 A – a. PO 2 >500 350 -499 +1 25 -34 200 -349 +2 +3 +4 32 -33. 9 30 -31. 9 <29. 9 70 -109 50 -69 <49 70 -109 55 -69 12 -24 1011 40 -54 6 -9 <39 <5 <200 7. 5 -7. 59 7. 337. 49 7. 257. 32 7. 157. 24 <7. 15
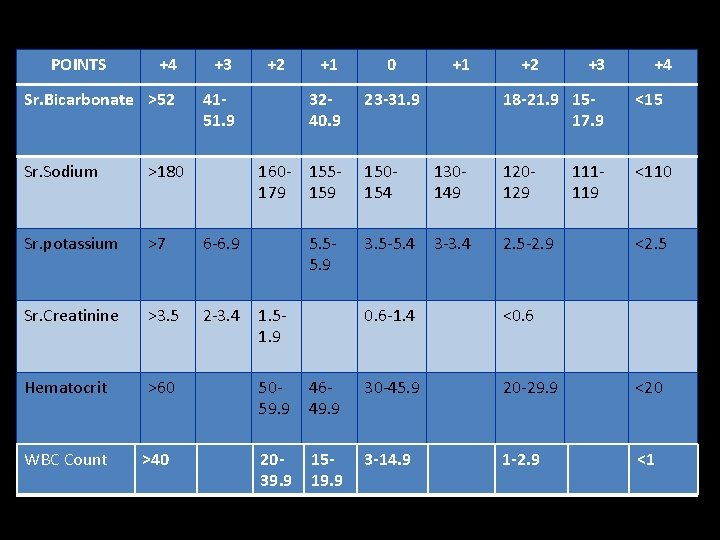
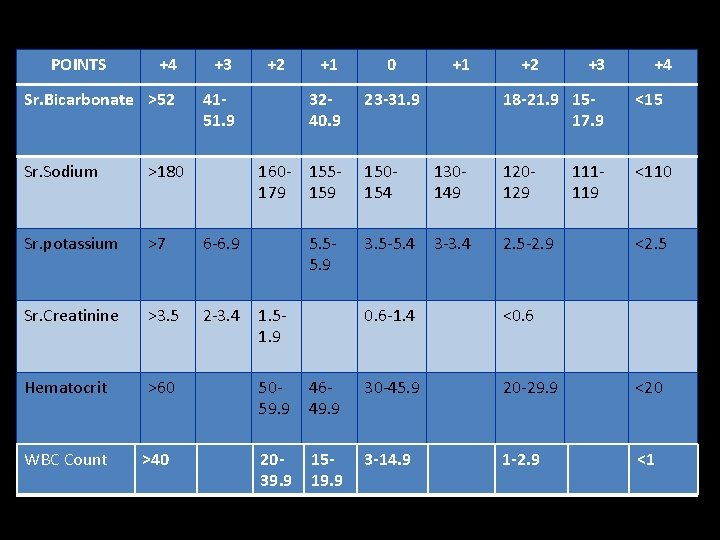
POINTS +4 +3 Sr. Bicarbonate >52 4151. 9 Sr. Sodium >180 Sr. potassium >7 6 -6. 9 Sr. Creatinine >3. 5 2 -3. 4 Hematocrit >60 WBC Count >40 +2 +1 0 3240. 9 23 -31. 9 160 - 155179 159 5. 55. 9 1. 51. 9 +1 +2 +3 +4 18 -21. 9 1517. 9 <15 <110 150154 130149 120129 3. 5 -5. 4 3 -3. 4 2. 5 -2. 9 0. 6 -1. 4 <0. 6 111119 <2. 5 5059. 9 4649. 9 30 -45. 9 20 -29. 9 <20 2039. 9 1519. 9 3 -14. 9 1 -2. 9 <1
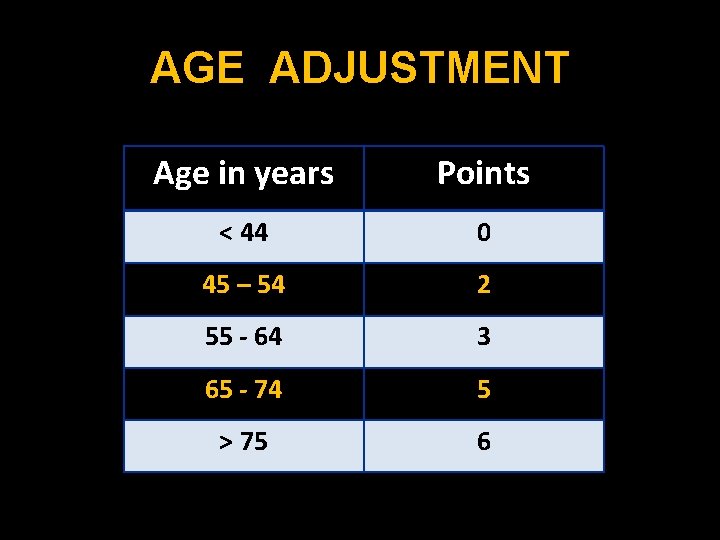
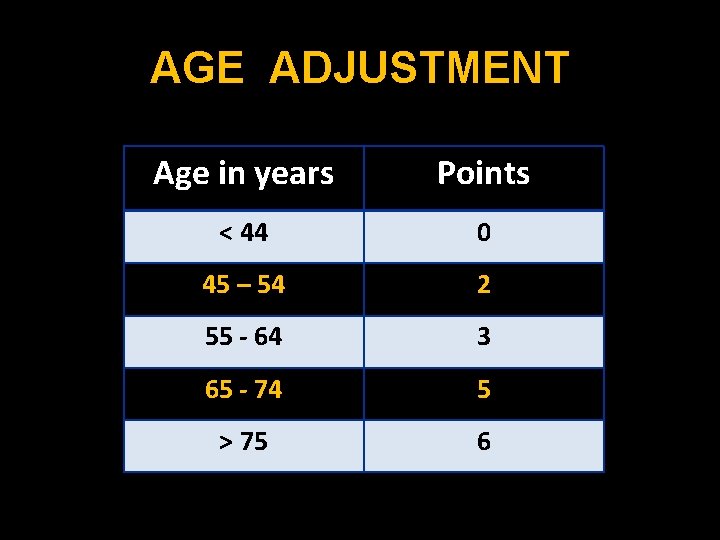
AGE ADJUSTMENT Age in years Points < 44 0 45 – 54 2 55 - 64 3 65 - 74 5 > 75 6
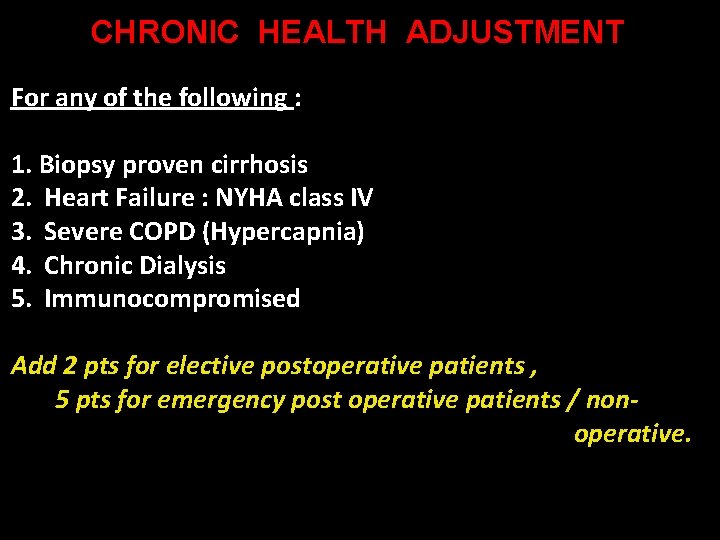
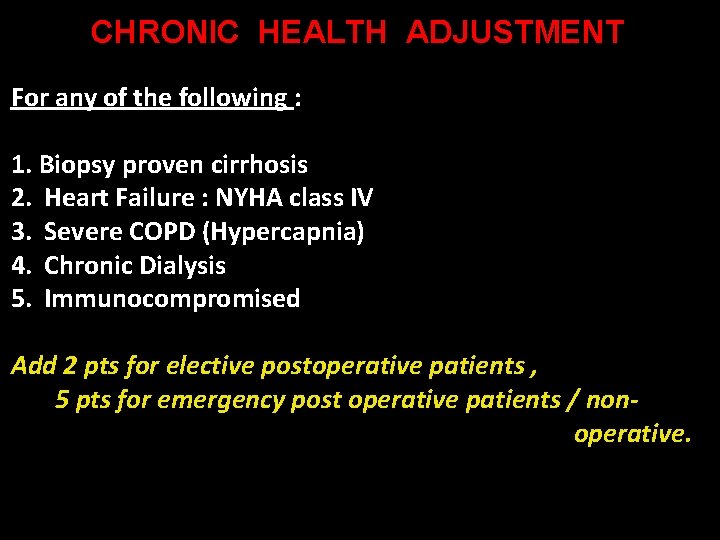
CHRONIC HEALTH ADJUSTMENT For any of the following : 1. Biopsy proven cirrhosis 2. Heart Failure : NYHA class IV 3. Severe COPD (Hypercapnia) 4. Chronic Dialysis 5. Immunocompromised Add 2 pts for elective postoperative patients , 5 pts for emergency post operative patients / nonoperative.
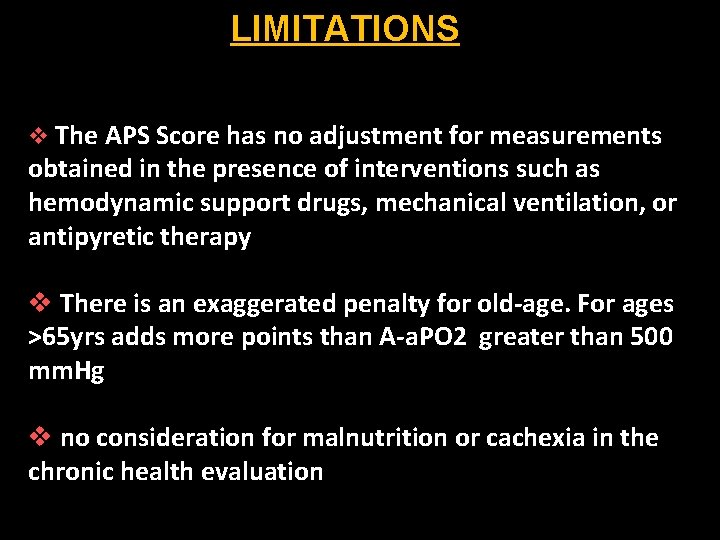
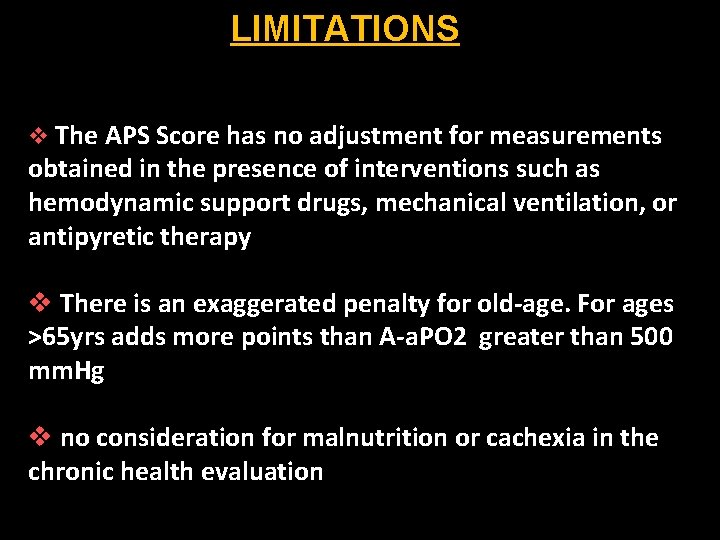
LIMITATIONS v The APS Score has no adjustment for measurements obtained in the presence of interventions such as hemodynamic support drugs, mechanical ventilation, or antipyretic therapy v There is an exaggerated penalty for old-age. For ages >65 yrs adds more points than A-a. PO 2 greater than 500 mm. Hg v no consideration for malnutrition or cachexia in the chronic health evaluation
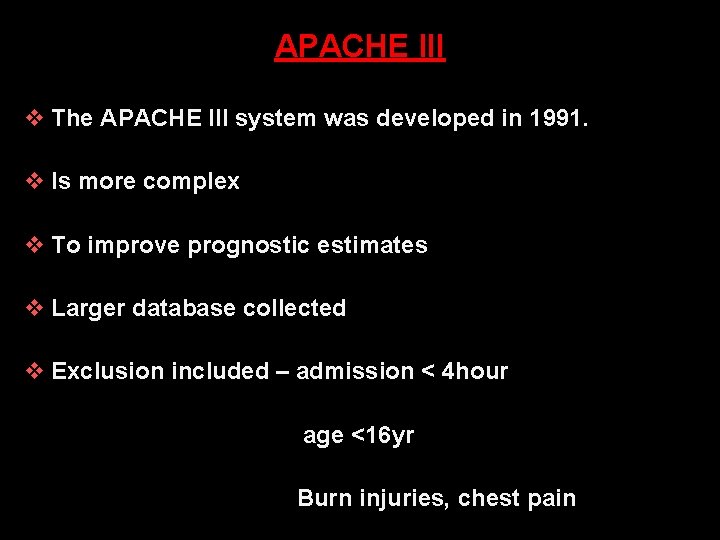
APACHE III v The APACHE III system was developed in 1991. v Is more complex v To improve prognostic estimates v Larger database collected v Exclusion included – admission < 4 hour age <16 yr Burn injuries, chest pain
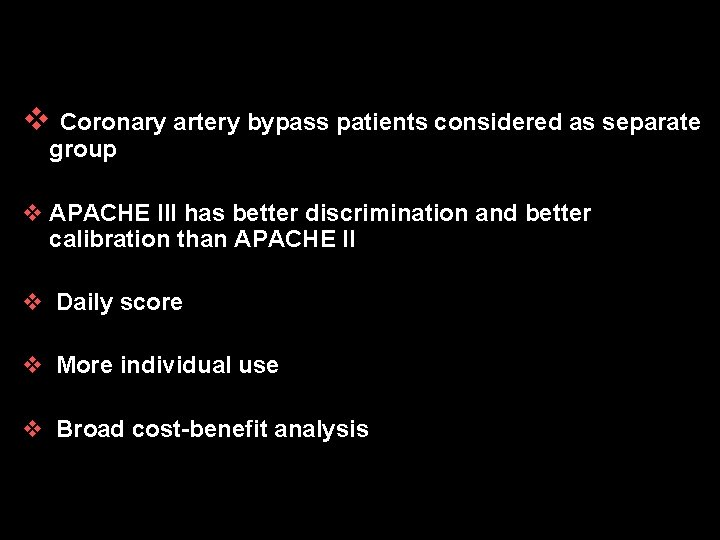
v Coronary artery bypass patients considered as separate group v APACHE III has better discrimination and better calibration than APACHE II v Daily score v More individual use v Broad cost-benefit analysis
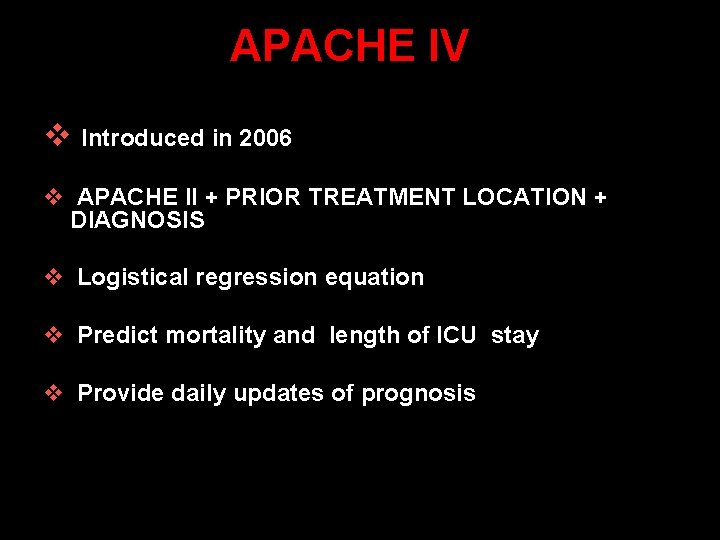
APACHE IV v Introduced in 2006 v APACHE II + PRIOR TREATMENT LOCATION + DIAGNOSIS v Logistical regression equation v Predict mortality and length of ICU stay v Provide daily updates of prognosis
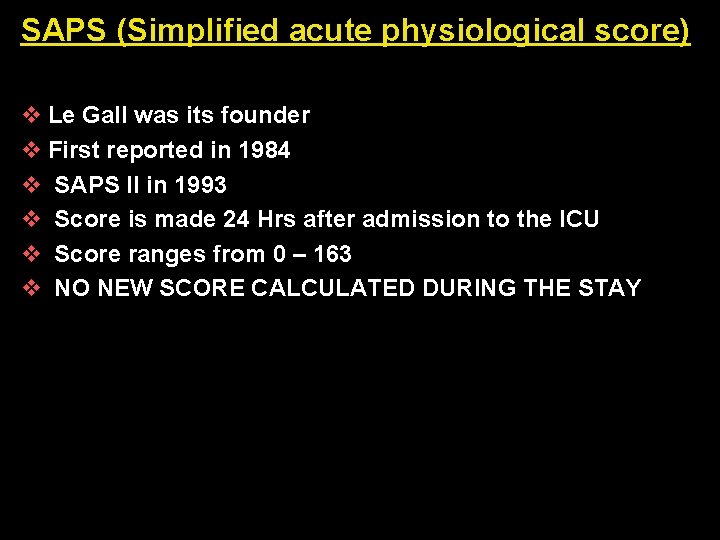
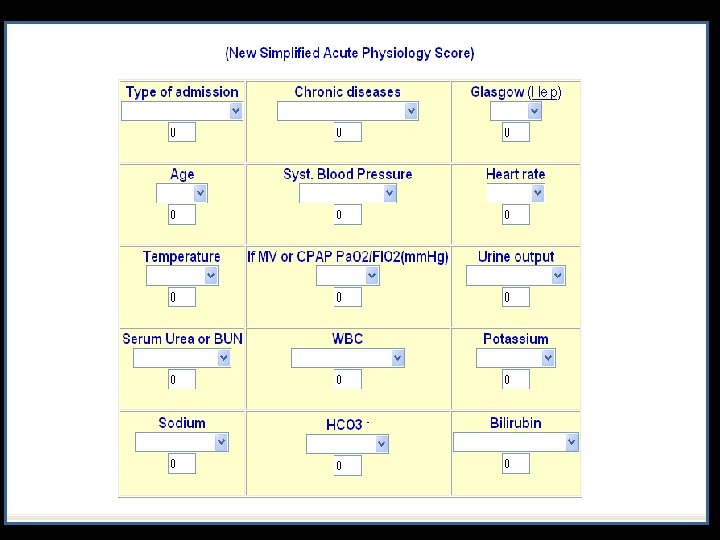
SAPS (Simplified acute physiological score) v Le Gall was its founder v First reported in 1984 v SAPS II in 1993 v Score is made 24 Hrs after admission to the ICU v Score ranges from 0 – 163 v NO NEW SCORE CALCULATED DURING THE STAY
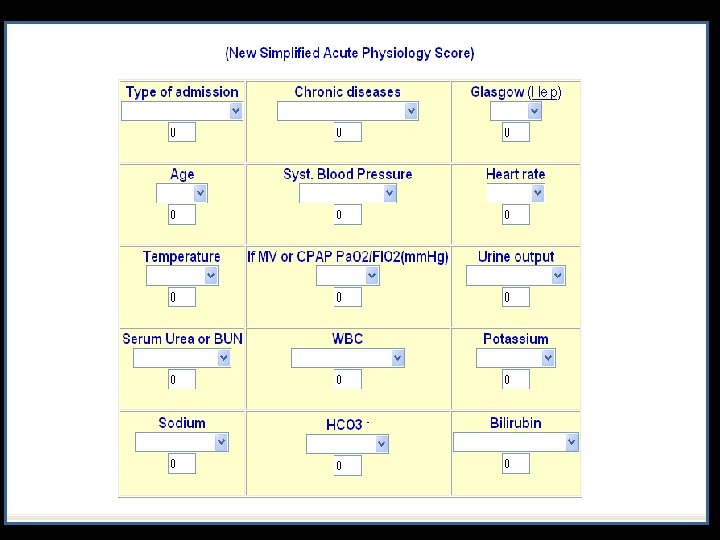
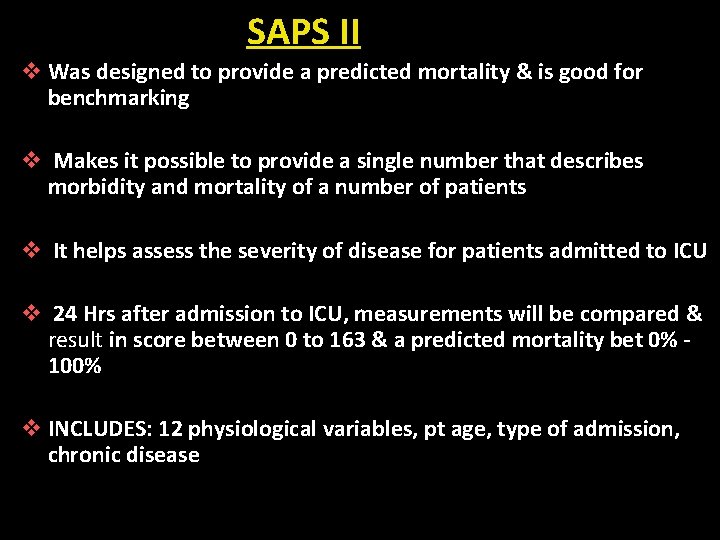
SAPS II v Was designed to provide a predicted mortality & is good for benchmarking v Makes it possible to provide a single number that describes morbidity and mortality of a number of patients v It helps assess the severity of disease for patients admitted to ICU v 24 Hrs after admission to ICU, measurements will be compared & result in score between 0 to 163 & a predicted mortality bet 0% 100% v INCLUDES: 12 physiological variables, pt age, type of admission, chronic disease
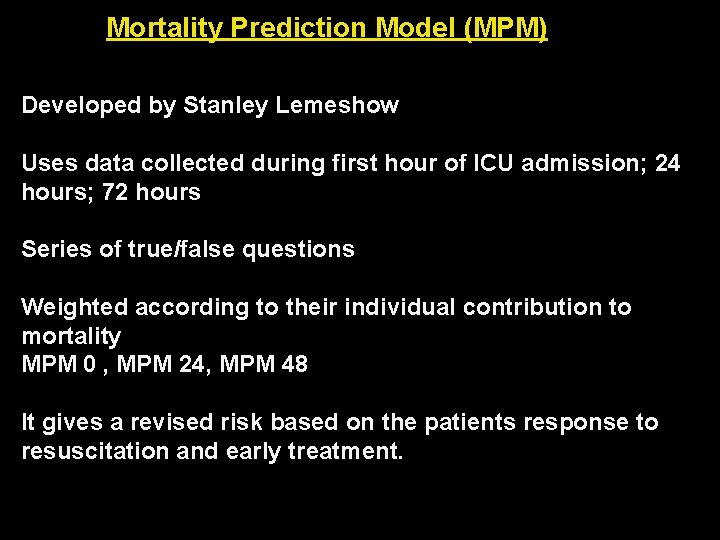
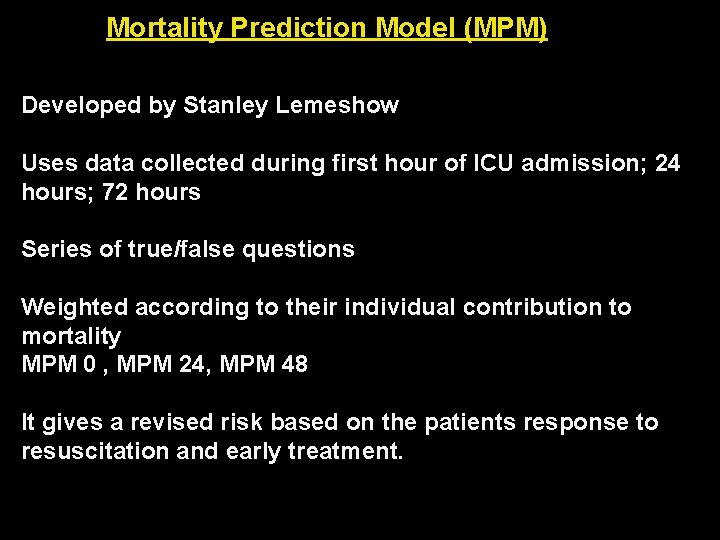
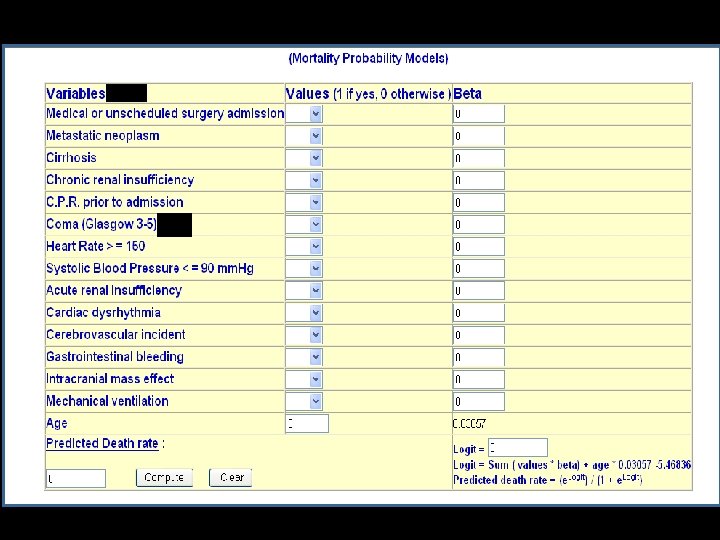
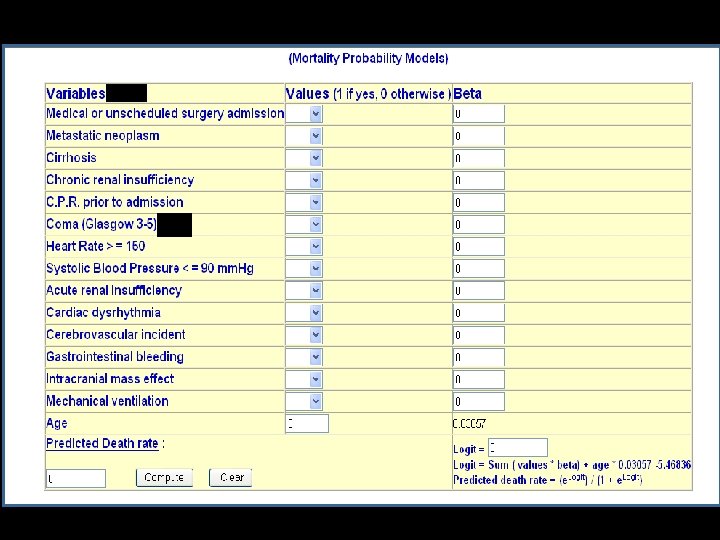
Mortality Prediction Model (MPM) Developed by Stanley Lemeshow Uses data collected during first hour of ICU admission; 24 hours; 72 hours Series of true/false questions Weighted according to their individual contribution to mortality MPM 0 , MPM 24, MPM 48 It gives a revised risk based on the patients response to resuscitation and early treatment.
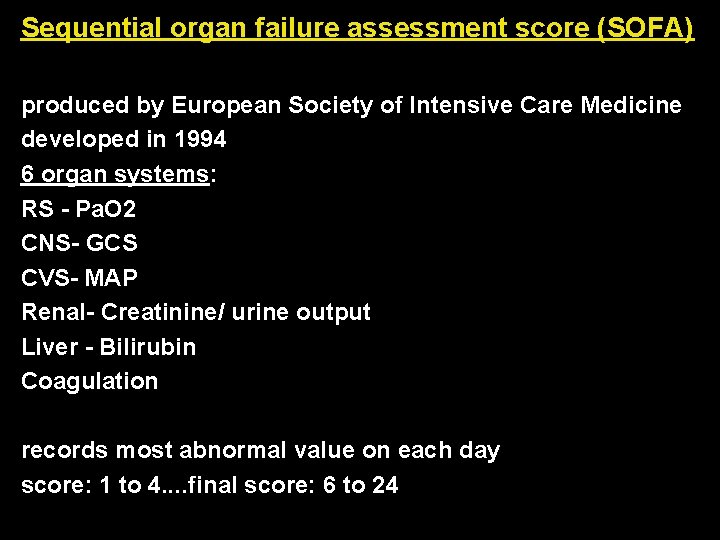
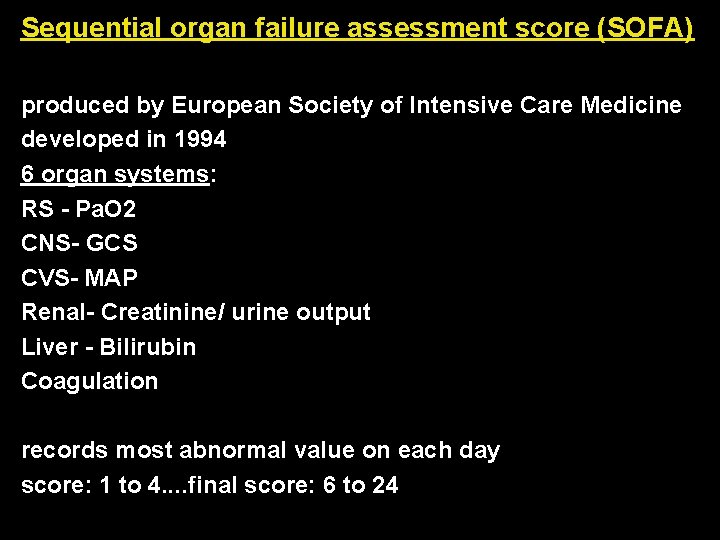
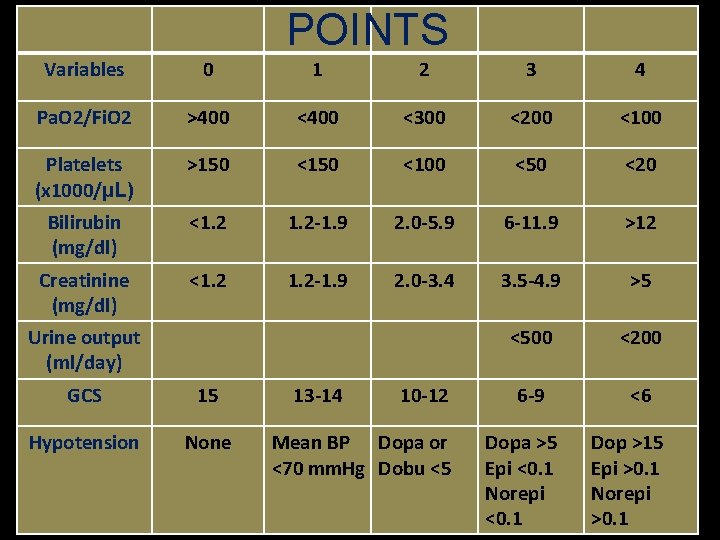
Sequential organ failure assessment score (SOFA) produced by European Society of Intensive Care Medicine developed in 1994 6 organ systems: RS - Pa. O 2 CNS- GCS CVS- MAP Renal- Creatinine/ urine output Liver - Bilirubin Coagulation records most abnormal value on each day score: 1 to 4. . final score: 6 to 24
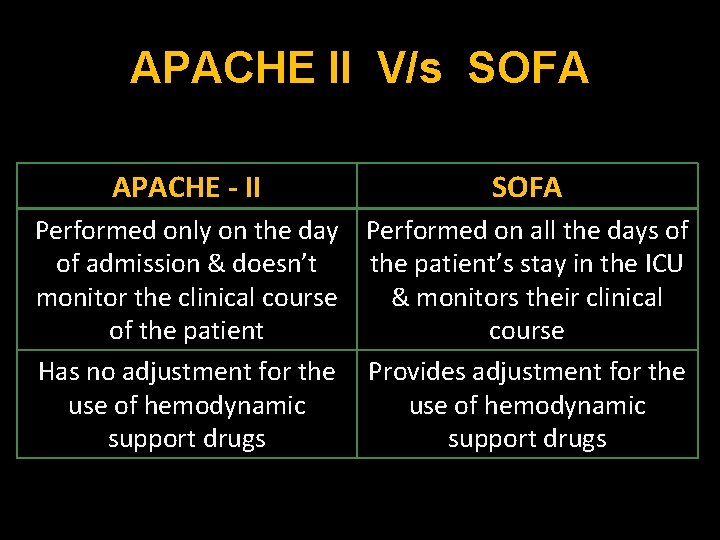
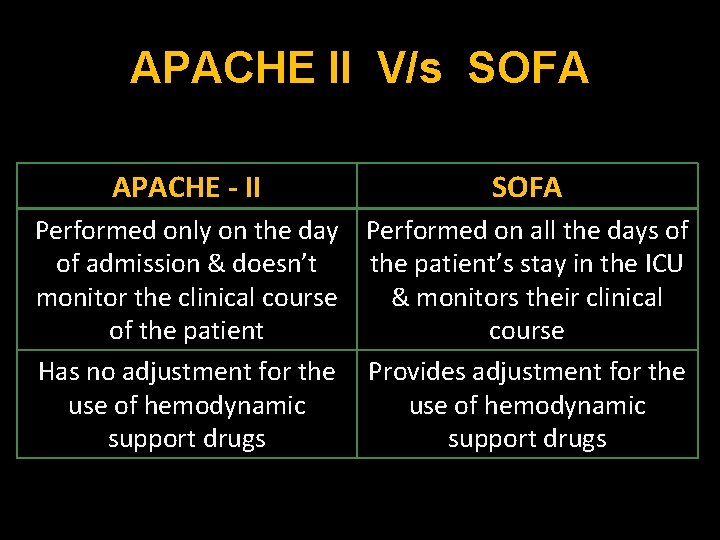
APACHE II V/s SOFA APACHE - II SOFA Performed only on the day Performed on all the days of of admission & doesn’t the patient’s stay in the ICU monitor the clinical course & monitors their clinical of the patient course Has no adjustment for the Provides adjustment for the use of hemodynamic support drugs
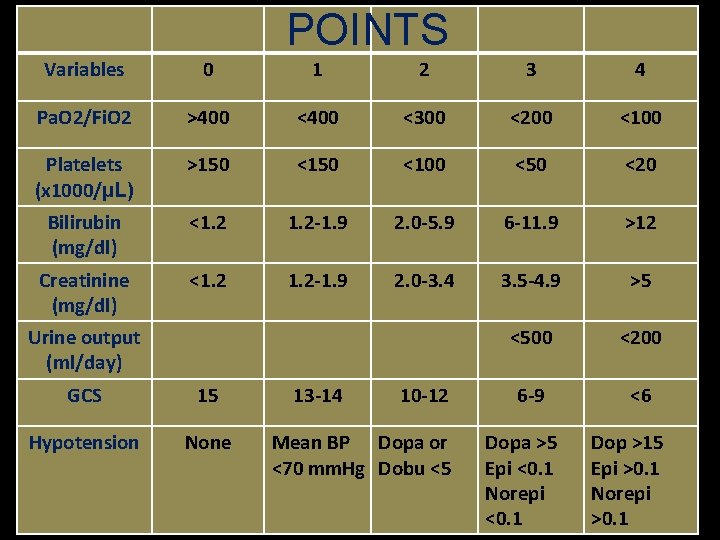
POINTS Variables 0 1 2 3 4 Pa. O 2/Fi. O 2 >400 <300 <200 <100 Platelets (x 1000/µL) >150 <100 <50 <20 Bilirubin (mg/dl) <1. 2 -1. 9 2. 0 -5. 9 6 -11. 9 >12 Creatinine (mg/dl) <1. 2 -1. 9 2. 0 -3. 4 3. 5 -4. 9 >5 <500 <200 6 -9 <6 Urine output (ml/day) GCS 15 Hypotension None 13 -14 10 -12 Mean BP Dopa or <70 mm. Hg Dobu <5 Dopa >5 Epi <0. 1 Norepi <0. 1 Dop >15 Epi >0. 1 Norepi >0. 1
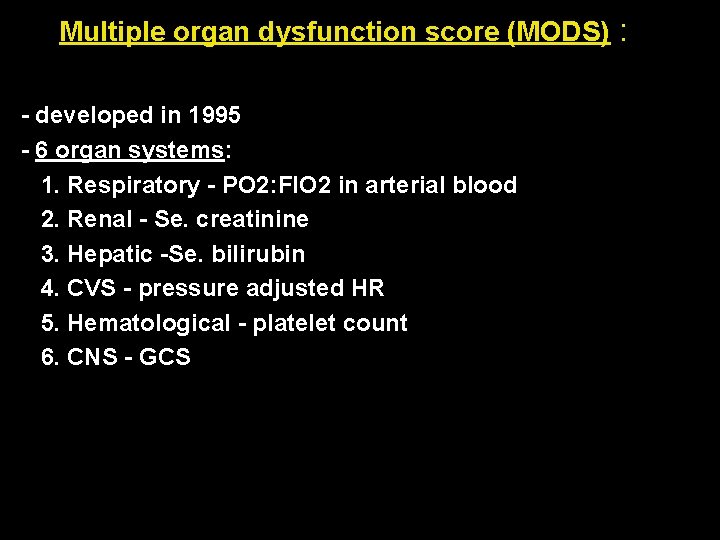
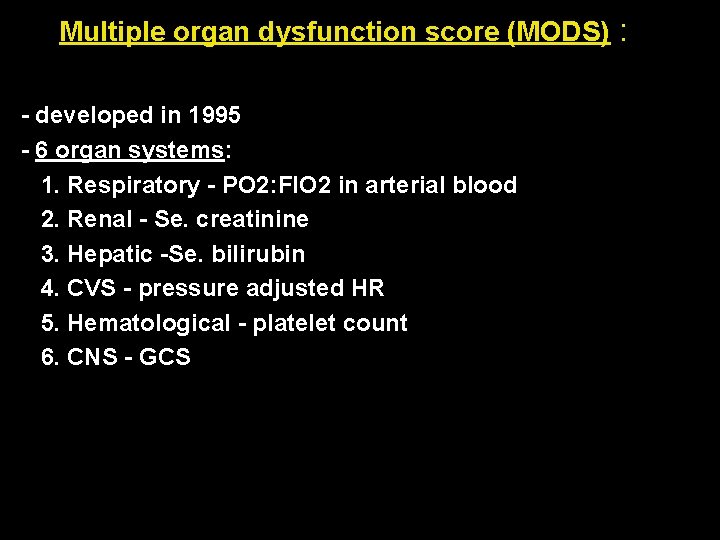
Multiple organ dysfunction score (MODS) : - developed in 1995 - 6 organ systems: 1. Respiratory - PO 2: FIO 2 in arterial blood 2. Renal - Se. creatinine 3. Hepatic -Se. bilirubin 4. CVS - pressure adjusted HR 5. Hematological - platelet count 6. CNS - GCS
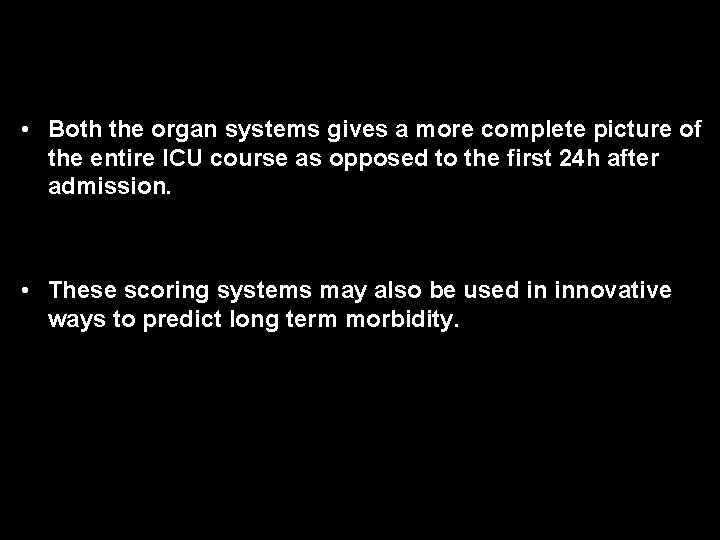
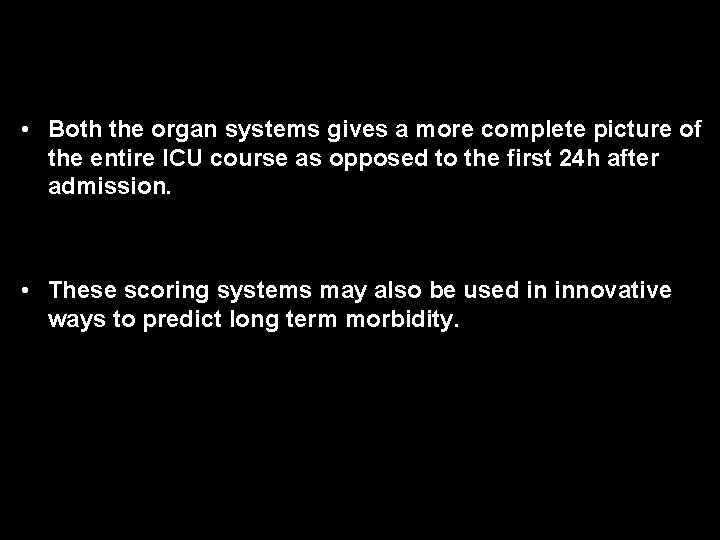
• Both the organ systems gives a more complete picture of the entire ICU course as opposed to the first 24 h after admission. • These scoring systems may also be used in innovative ways to predict long term morbidity.
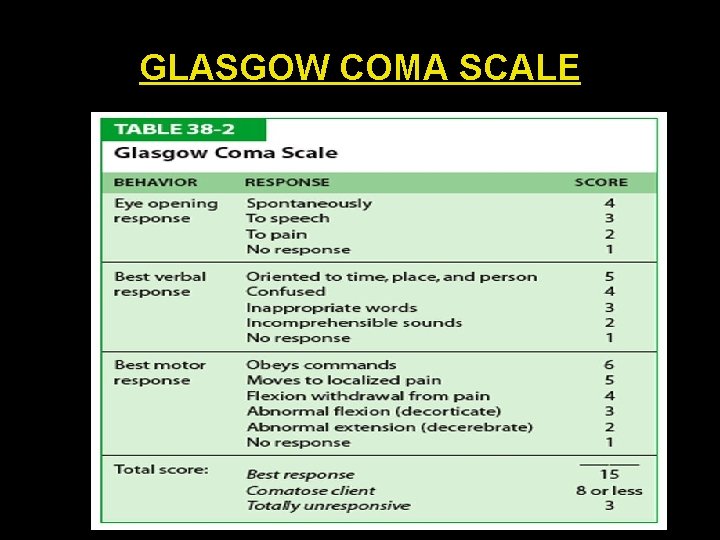
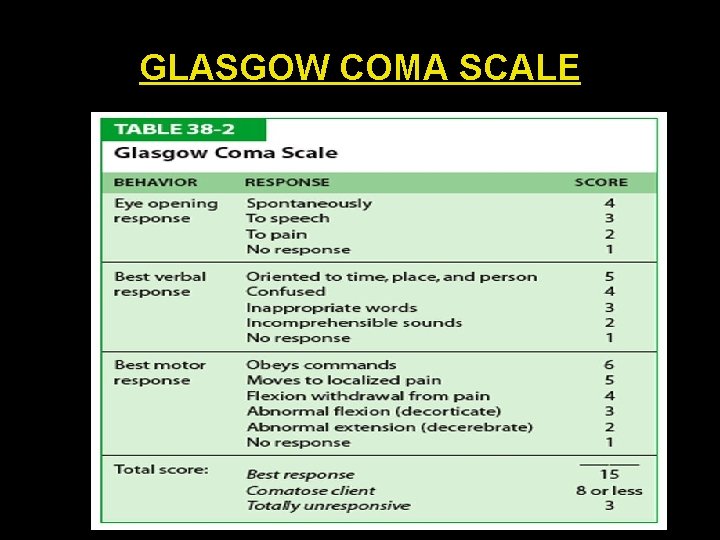
GLASGOW COMA SCALE
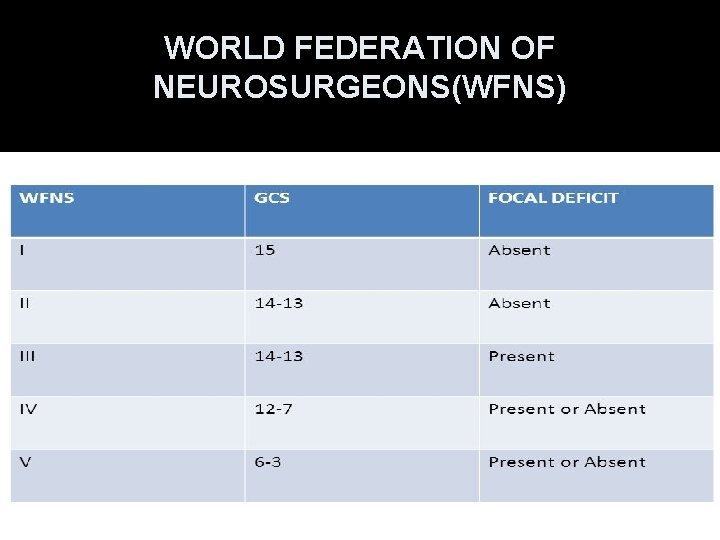
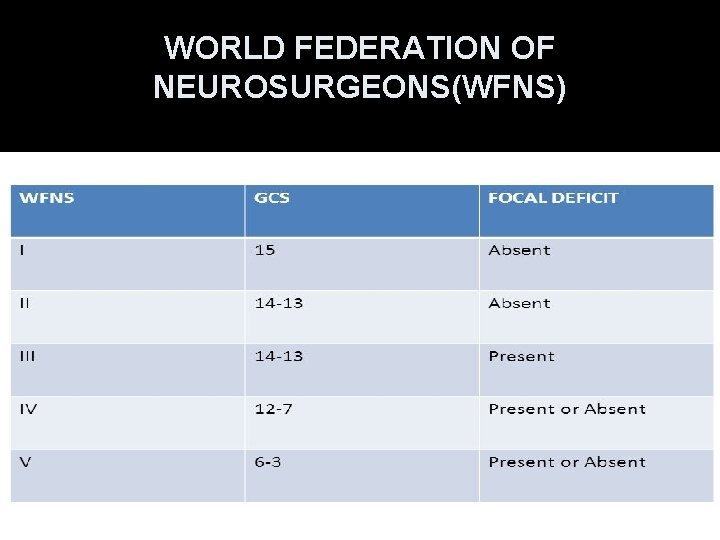
WORLD FEDERATION OF NEUROSURGEONS(WFNS)
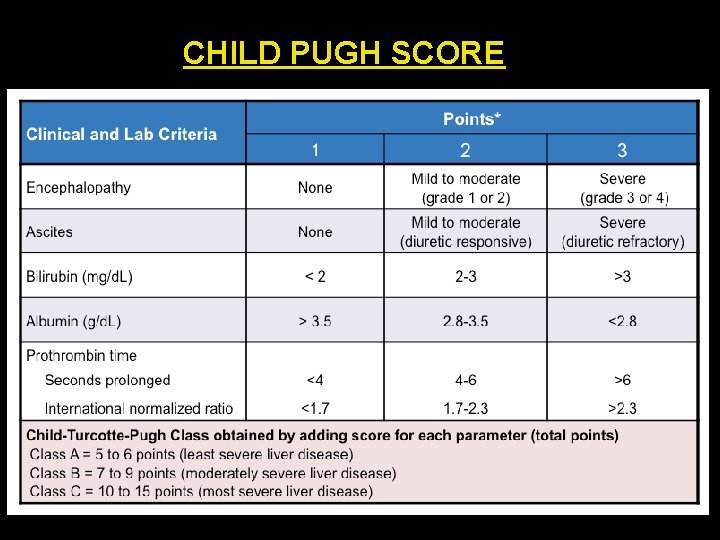
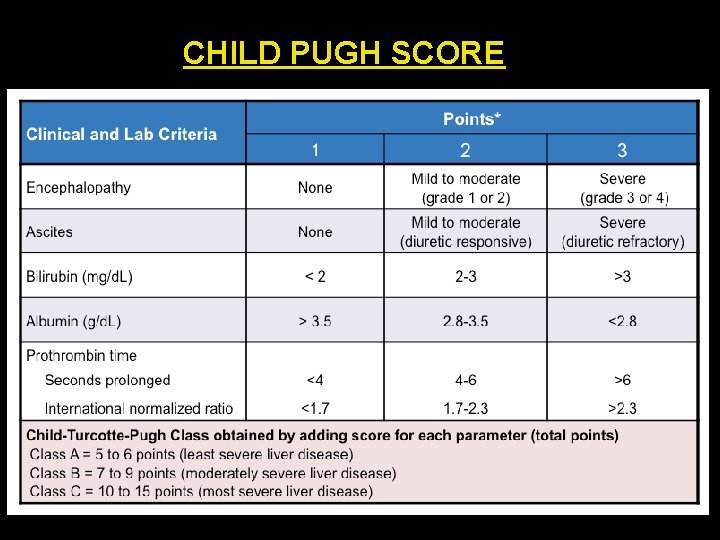
CHILD PUGH SCORE
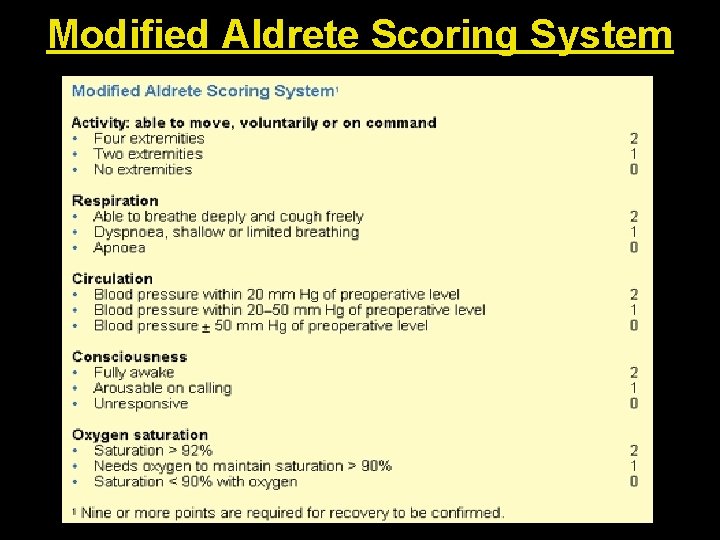
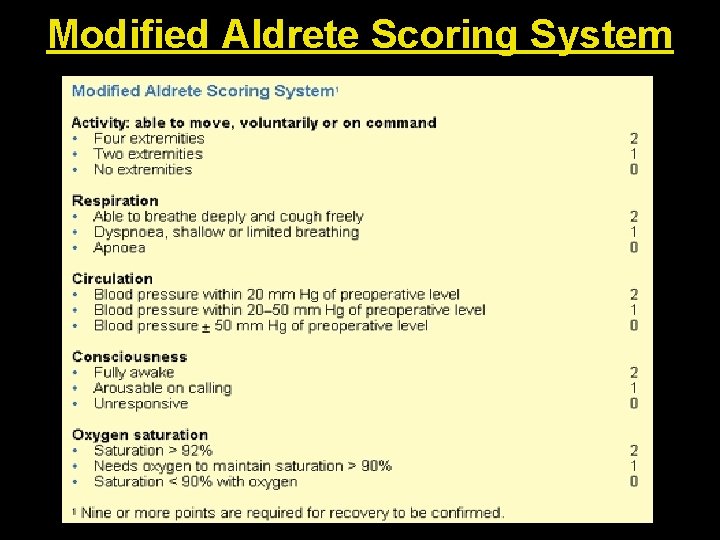
Modified Aldrete Scoring System
SEDATION IN ICU
v Sedation allows the depression of patients’ awareness of the environment and reduction of their response to external stimulation. v The effective management of pain, anxiety and sleep (hypnosis) are the major aims of a sedation therapy regimen.
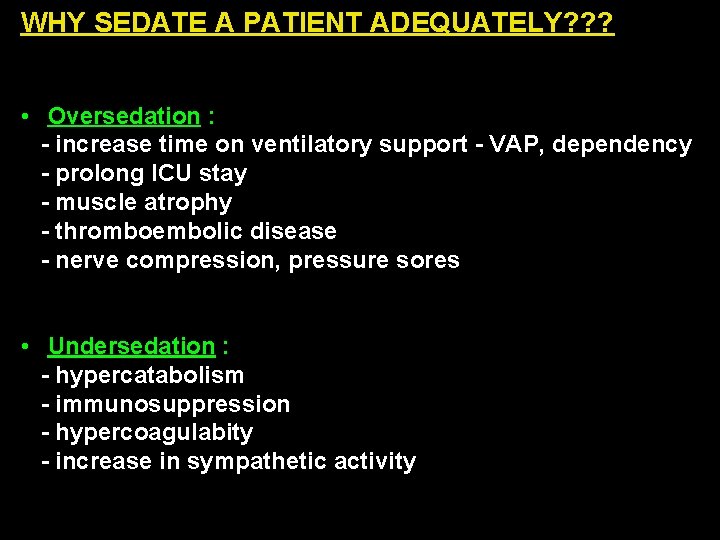
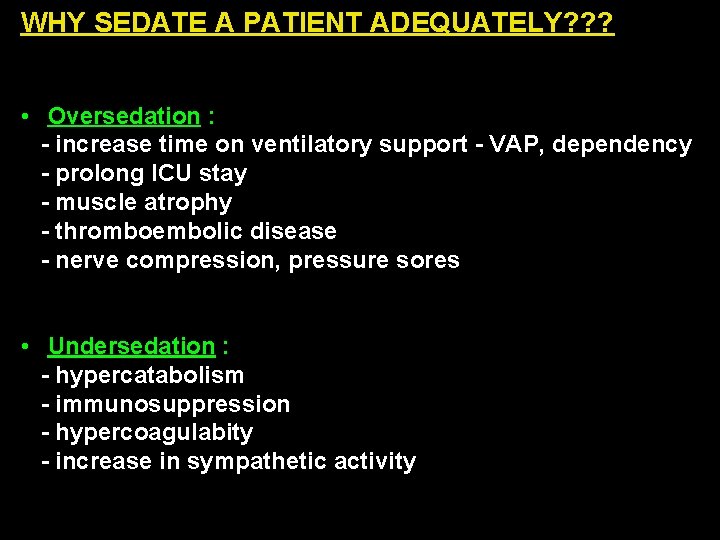
WHY SEDATE A PATIENT ADEQUATELY? ? ? • Oversedation : - increase time on ventilatory support - VAP, dependency - prolong ICU stay - muscle atrophy - thromboembolic disease - nerve compression, pressure sores • Undersedation : - hypercatabolism - immunosuppression - hypercoagulabity - increase in sympathetic activity
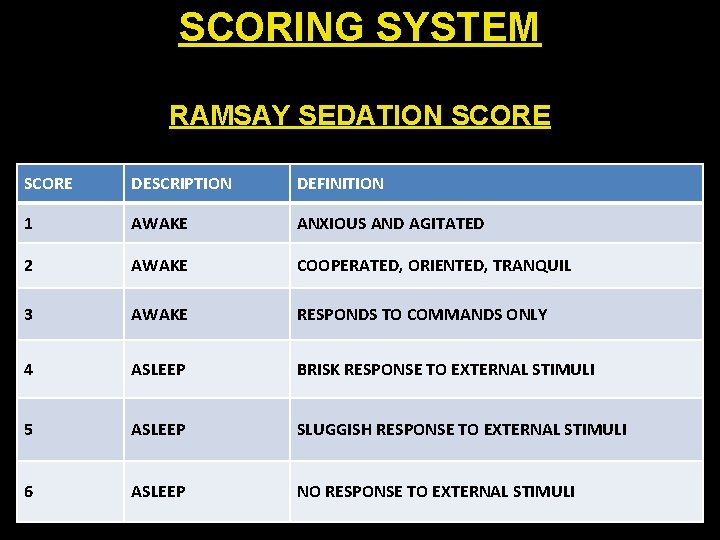
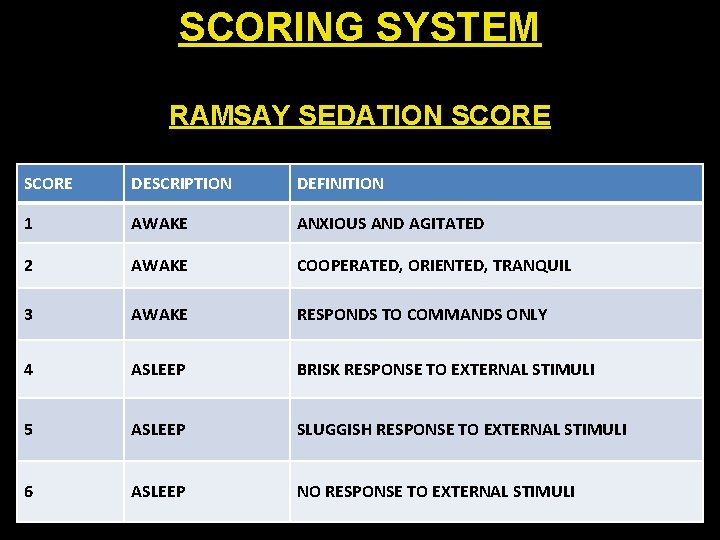
SCORING SYSTEM RAMSAY SEDATION SCORE DESCRIPTION DEFINITION 1 AWAKE ANXIOUS AND AGITATED 2 AWAKE COOPERATED, ORIENTED, TRANQUIL 3 AWAKE RESPONDS TO COMMANDS ONLY 4 ASLEEP BRISK RESPONSE TO EXTERNAL STIMULI 5 ASLEEP SLUGGISH RESPONSE TO EXTERNAL STIMULI 6 ASLEEP NO RESPONSE TO EXTERNAL STIMULI
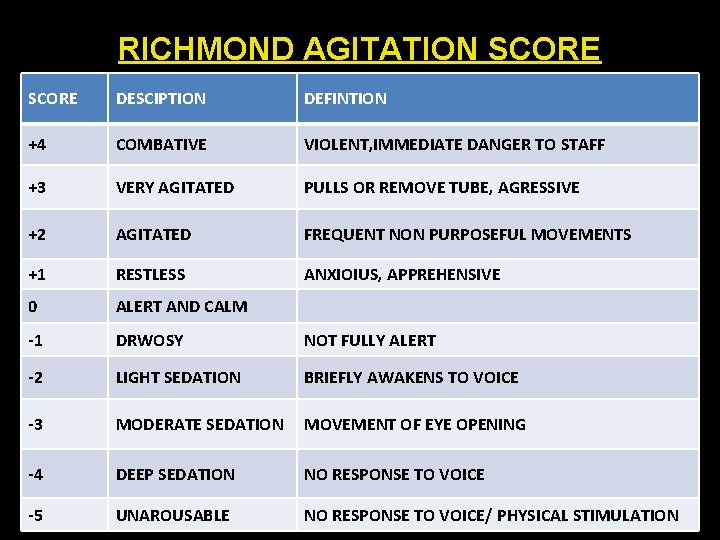
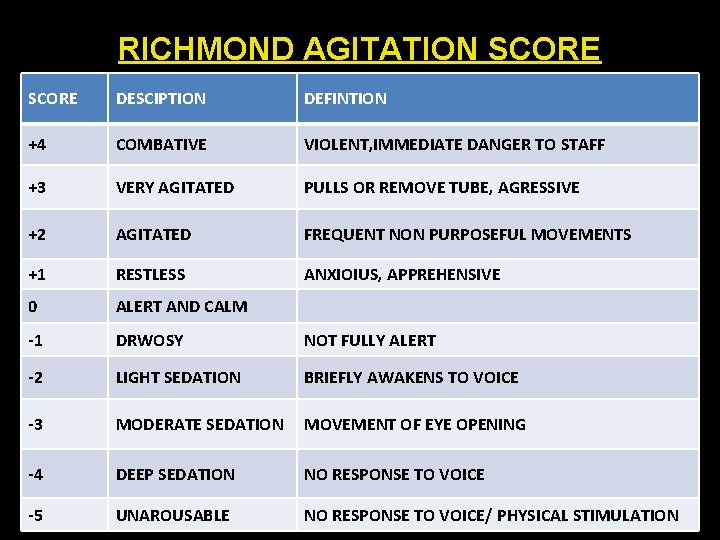
RICHMOND AGITATION SCORE DESCIPTION DEFINTION +4 COMBATIVE VIOLENT, IMMEDIATE DANGER TO STAFF +3 VERY AGITATED PULLS OR REMOVE TUBE, AGRESSIVE +2 AGITATED FREQUENT NON PURPOSEFUL MOVEMENTS +1 RESTLESS ANXIOIUS, APPREHENSIVE 0 ALERT AND CALM -1 DRWOSY NOT FULLY ALERT -2 LIGHT SEDATION BRIEFLY AWAKENS TO VOICE -3 MODERATE SEDATION MOVEMENT OF EYE OPENING -4 DEEP SEDATION NO RESPONSE TO VOICE -5 UNAROUSABLE NO RESPONSE TO VOICE/ PHYSICAL STIMULATION
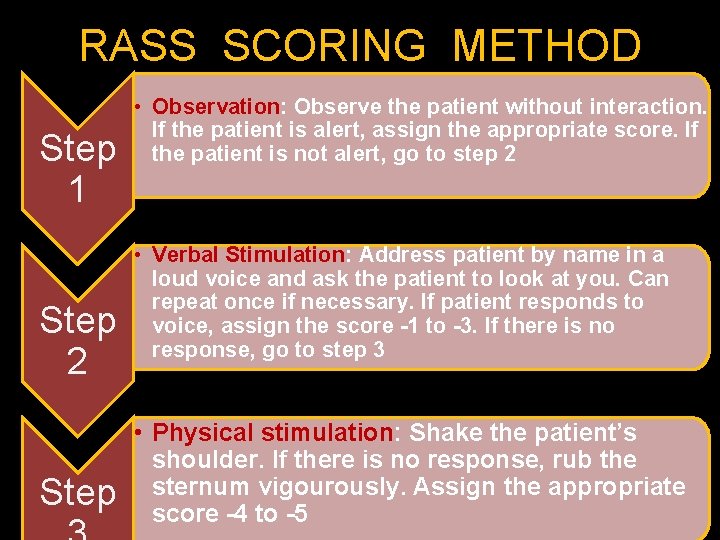
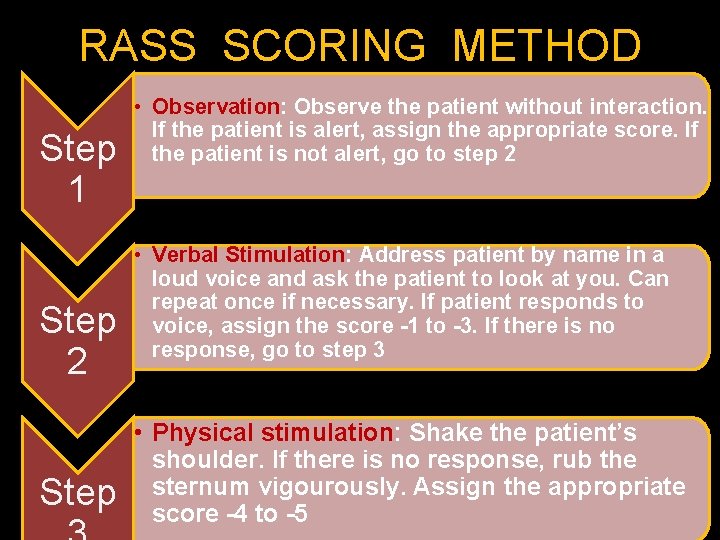
RASS SCORING METHOD Step 1 Step 2 Step • Observation: Observe the patient without interaction. If the patient is alert, assign the appropriate score. If the patient is not alert, go to step 2 • Verbal Stimulation: Address patient by name in a loud voice and ask the patient to look at you. Can repeat once if necessary. If patient responds to voice, assign the score -1 to -3. If there is no response, go to step 3 • Physical stimulation: Shake the patient’s shoulder. If there is no response, rub the sternum vigourously. Assign the appropriate score -4 to -5
Prompt identification and treatment of possible underlying causes of agitation: - pain - delirium - hypoxia - hypoglycemia - hypotension - withdrawal from alcohol or other drugs
MEASURES OF SEDATION 1. EEG 2. BIS
NON PHARMACOLOGICAL METHODS OF SEDATION - music therapy - reduce noise : sleep occurs best <35 d. B - lighting of the bed space to mimic day-night orientation

PHARMACOLOGICAL TREATMENT FOR SEDATION
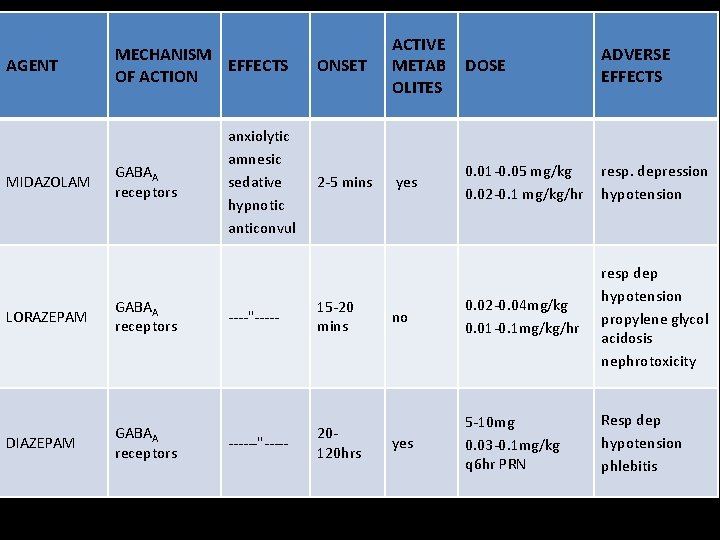
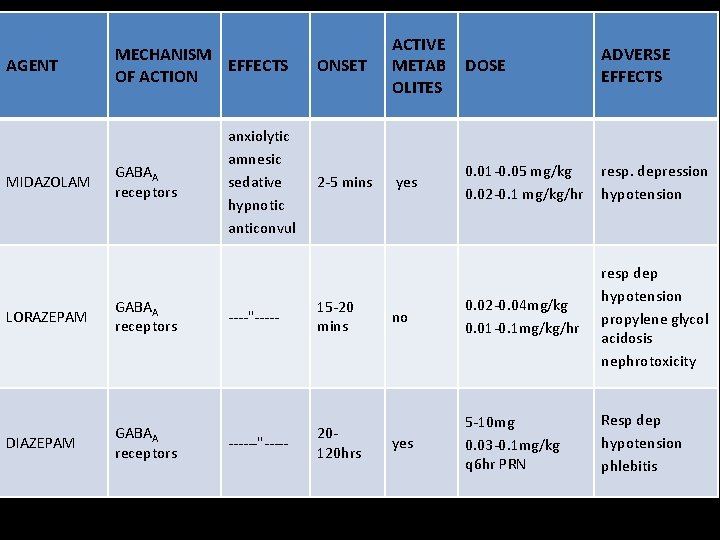
AGENT MIDAZOLAM MECHANISM EFFECTS OF ACTION GABAA receptors LORAZEPAM GABAA receptors DIAZEPAM GABAA receptors anxiolytic amnesic sedative hypnotic anticonvul ONSET ACTIVE METAB OLITES DOSE ADVERSE EFFECTS 2 -5 mins yes 0. 01 -0. 05 mg/kg 0. 02 -0. 1 mg/kg/hr resp. depression hypotension no 0. 02 -0. 04 mg/kg 0. 01 -0. 1 mg/kg/hr resp dep hypotension propylene glycol acidosis nephrotoxicity yes 5 -10 mg 0. 03 -0. 1 mg/kg q 6 hr PRN Resp dep hypotension phlebitis ----"----- 15 -20 mins ------"----- 20120 hrs
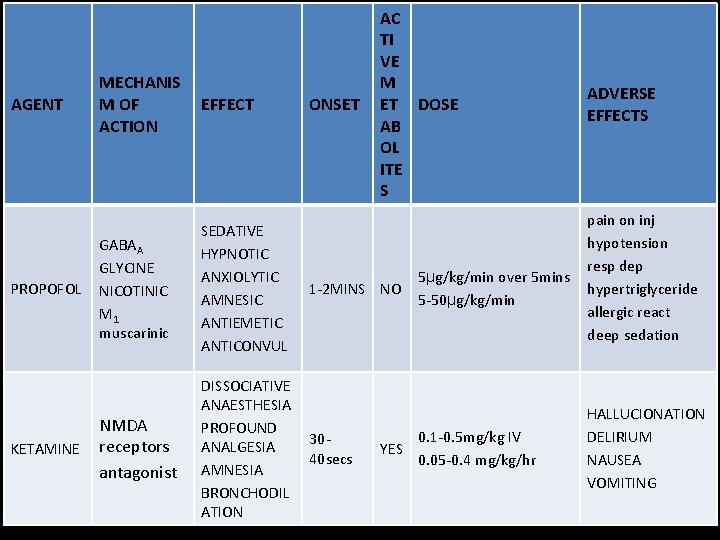
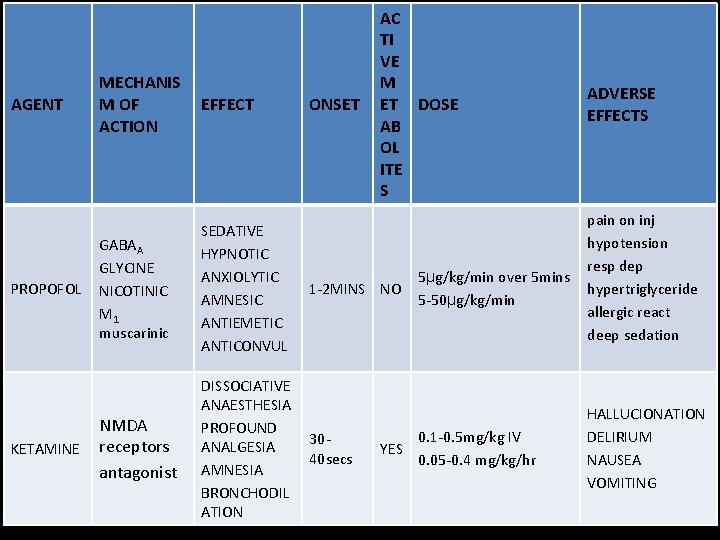
AGENT PROPOFOL KETAMINE MECHANIS M OF ACTION EFFECT GABAA GLYCINE NICOTINIC M 1 muscarinic SEDATIVE HYPNOTIC ANXIOLYTIC AMNESIC ANTIEMETIC ANTICONVUL NMDA receptors antagonist DISSOCIATIVE ANAESTHESIA PROFOUND ANALGESIA AMNESIA BRONCHODIL ATION ONSET AC TI VE M ET DOSE AB OL ITE S 1 -2 MINS NO 3040 secs YES 5µg/kg/min over 5 mins 5 -50µg/kg/min 0. 1 -0. 5 mg/kg IV 0. 05 -0. 4 mg/kg/hr ADVERSE EFFECTS pain on inj hypotension resp dep hypertriglyceride allergic react deep sedation HALLUCIONATION DELIRIUM NAUSEA VOMITING
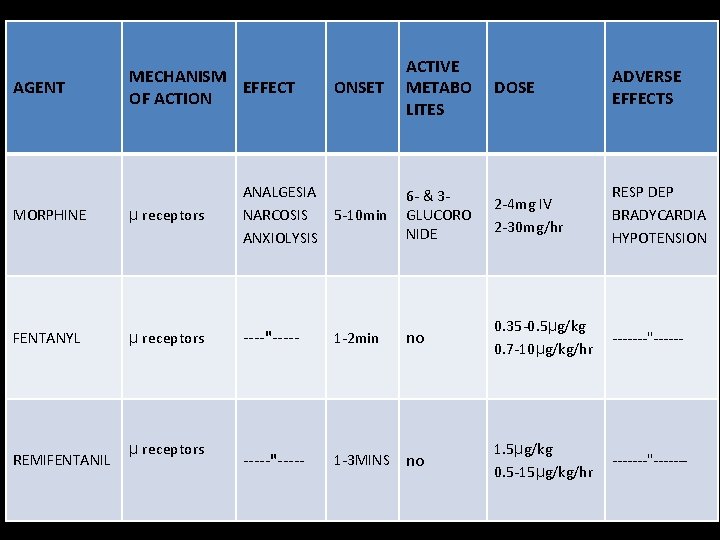
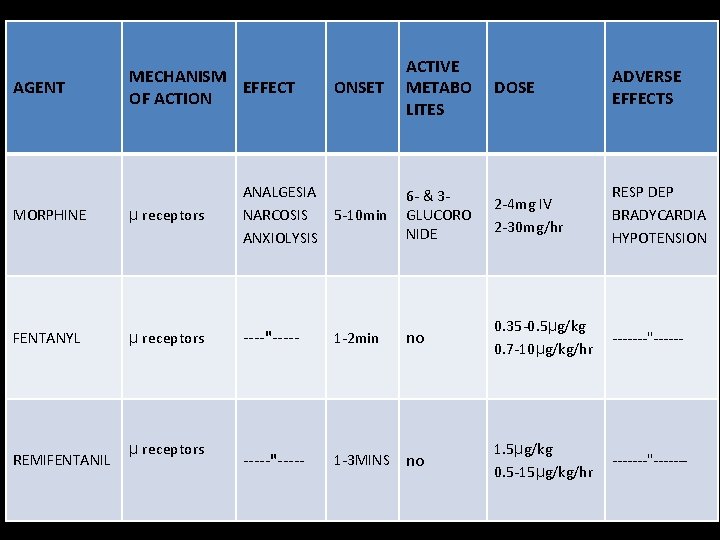
AGENT MECHANISM EFFECT OF ACTION ONSET ACTIVE METABO LITES DOSE ADVERSE EFFECTS 6 - & 3 GLUCORO NIDE 2 -4 mg IV 2 -30 mg/hr RESP DEP BRADYCARDIA HYPOTENSION MORPHINE µ receptors ANALGESIA NARCOSIS 5 -10 min ANXIOLYSIS FENTANYL µ receptors ----"----- 1 -2 min no 0. 35 -0. 5µg/kg 0. 7 -10µg/kg/hr -------"------"----- 1 -3 MINS no 1. 5µg/kg 0. 5 -15µg/kg/hr -------"------- REMIFENTANIL µ receptors
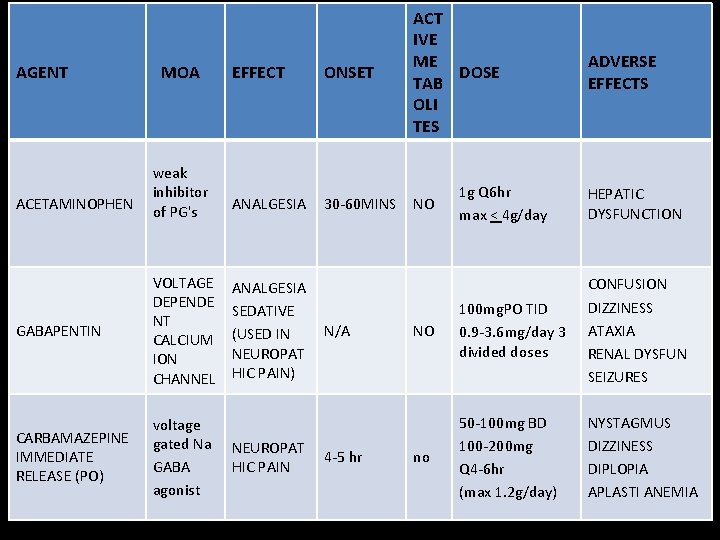
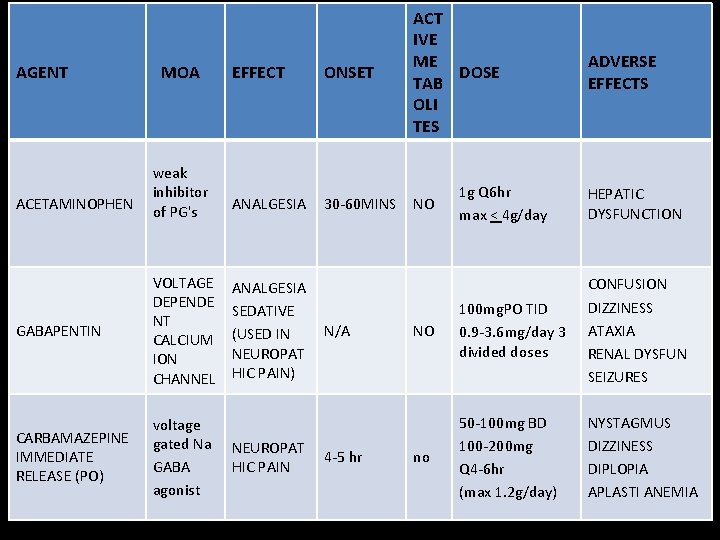
EFFECT ONSET ACT IVE ME DOSE TAB OLI TES weak inhibitor of PG's ANALGESIA 30 -60 MINS NO GABAPENTIN VOLTAGE DEPENDE NT CALCIUM ION CHANNEL ANALGESIA SEDATIVE (USED IN NEUROPAT HIC PAIN) CARBAMAZEPINE IMMEDIATE RELEASE (PO) voltage gated Na GABA agonist AGENT ACETAMINOPHEN MOA NEUROPAT HIC PAIN N/A 4 -5 hr ADVERSE EFFECTS 1 g Q 6 hr max < 4 g/day HEPATIC DYSFUNCTION NO 100 mg. PO TID 0. 9 -3. 6 mg/day 3 divided doses CONFUSION DIZZINESS ATAXIA RENAL DYSFUN SEIZURES no 50 -100 mg BD 100 -200 mg Q 4 -6 hr (max 1. 2 g/day) NYSTAGMUS DIZZINESS DIPLOPIA APLASTI ANEMIA
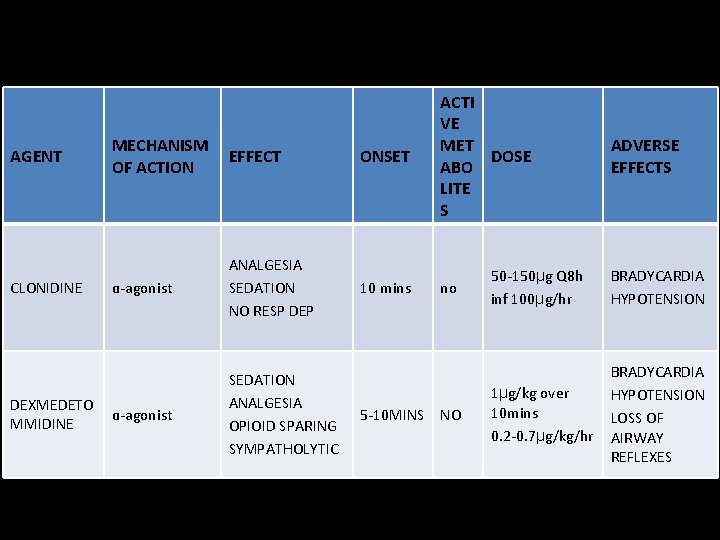
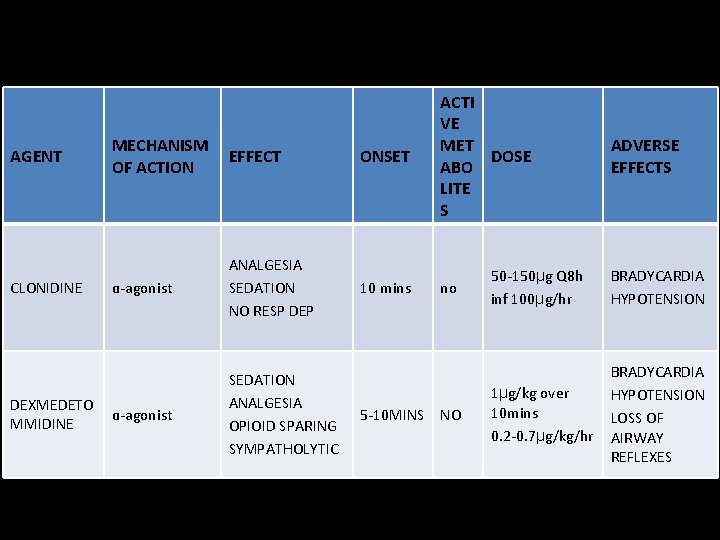
AGENT CLONIDINE DEXMEDETO MMIDINE MECHANISM OF ACTION EFFECT ONSET ACTI VE MET DOSE ABO LITE S ɑ-agonist ANALGESIA SEDATION NO RESP DEP 10 mins no ɑ-agonist SEDATION ANALGESIA OPIOID SPARING SYMPATHOLYTIC 5 -10 MINS NO ADVERSE EFFECTS 50 -150µg Q 8 h inf 100µg/hr BRADYCARDIA HYPOTENSION 1µg/kg over 10 mins 0. 2 -0. 7µg/kg/hr BRADYCARDIA HYPOTENSION LOSS OF AIRWAY REFLEXES
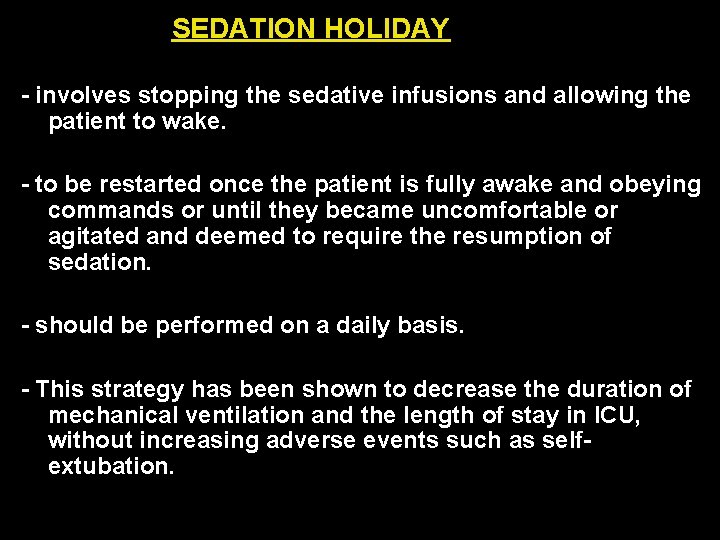
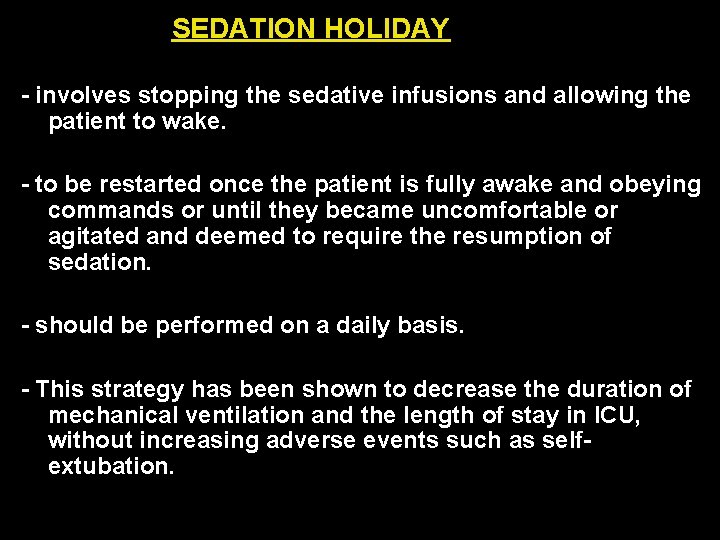
SEDATION HOLIDAY - involves stopping the sedative infusions and allowing the patient to wake. - to be restarted once the patient is fully awake and obeying commands or until they became uncomfortable or agitated and deemed to require the resumption of sedation. - should be performed on a daily basis. - This strategy has been shown to decrease the duration of mechanical ventilation and the length of stay in ICU, without increasing adverse events such as selfextubation.
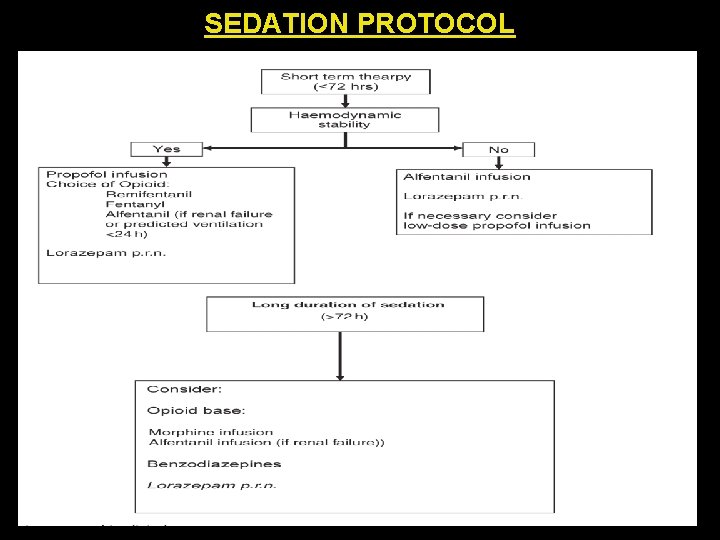
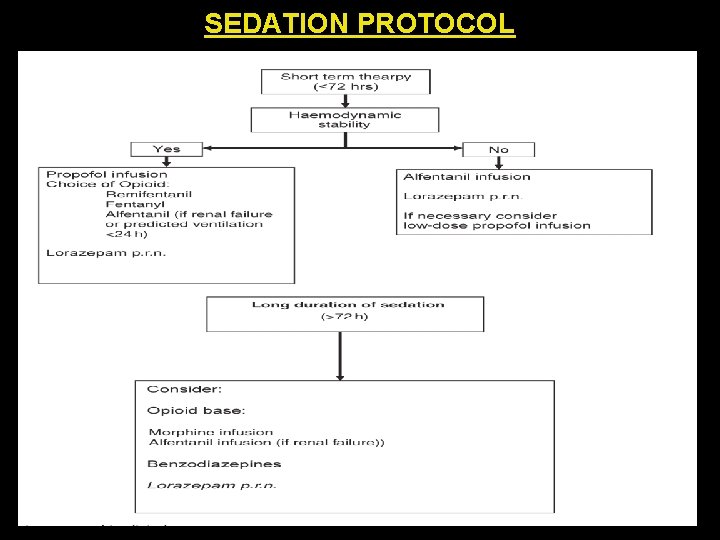
SEDATION PROTOCOL
THANK YOU