PROCEDURAL SEDATION ANALGESIA ADULT Provider Program PRODECURAL SEDATION


- Slides: 55
PROCEDURAL SEDATION & ANALGESIA ADULT Provider Program
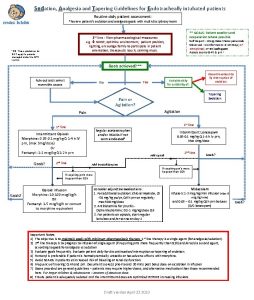
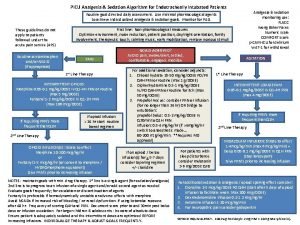
PRODECURAL SEDATION AND ANALGESIA Sedation and analgesia produced by administration of amnesiac, analgesic, and sedative medications Also known as moderate sedation Level of sedation achieved can be unpredictable due to a number of patient variables including, but not limited to: Age Weight Medical conditions Drugs administered/patient response to drugs Amounts administered
DEFINITIONS Minimal sedation/anxiolysis: drug induced state, patients respond normally to verbal commands; impaired cognitive and coordination possible; ventilatory and CV functions unaffected Moderate sedation(procedural): depressed level of consciousness with purposeful response to verbal commands/light tactile stimulation; ability to maintain patent airway and spontaneous ventilation Deep Sedation: not easily roused; respond purposefully to repeated or painful stimulation; may require assistance in maintaining patent airway and spontaneous ventilation may be inadequate Anesthesia: loss of consciousness, no response even to painful stimuli; impaired airway patency and ventilation; CV function may be impaired
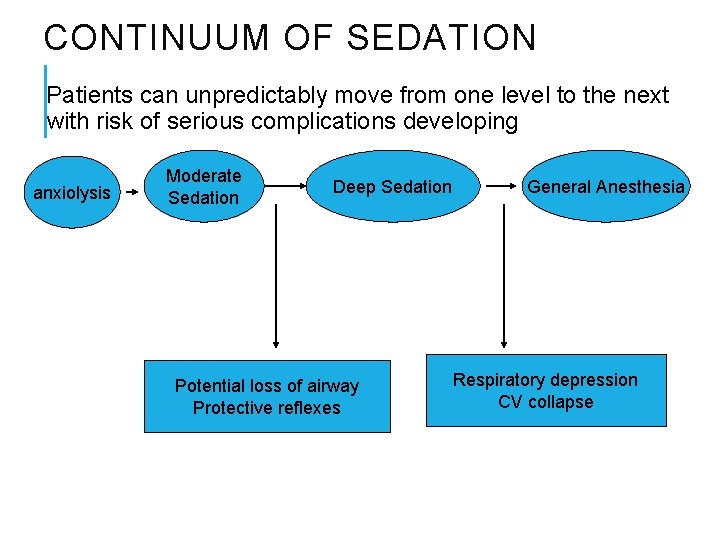
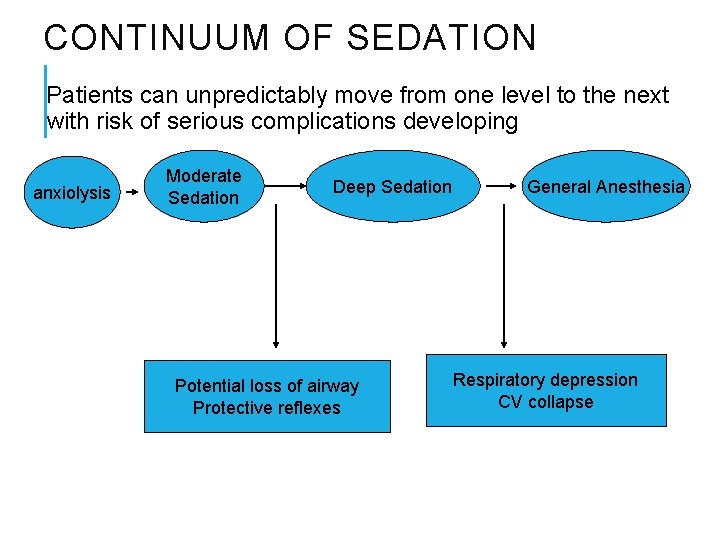
CONTINUUM OF SEDATION Patients can unpredictably move from one level to the next with risk of serious complications developing anxiolysis Moderate Sedation Deep Sedation Potential loss of airway Protective reflexes General Anesthesia Respiratory depression CV collapse
OBJECTIVES OF SEDATION/ANALGESIA Mood alteration Enhanced patient cooperation Management of pain* Stable vital signs Amnesia* Rapid recovery *Not always achieved/cannot be guaranteed to a patient
OVERSHOOTING THE TARGET Total doses of medication administered and individual patient response may lead patient to a deeper level of sedation Deep sedation/general anesthesia increases the risk for: Respiratory depression Hypoventilation Decreased response to hypoxic drive Cardiovascular depression Loss of consciousness/responsiveness Loss of airway patency
HOW TO AVOID OVERSEDATING… Be aware of the clinical endpoints for medication administration: Thick, slurred, slow speech and/or nystagmus Patient expresses he/she is comfortable Have a thorough knowledge of medications administered Onset, peak, duration Actions Side effects Method & rate of administration Know the sedation definitions Perform adequate pre-assessment of patient Provide careful monitoring of patient intra and postprocedure
GOALS OF PRE-SEDATION ASSESSMENT Identification of risk factors for sedation Reduction of patient anxiety through education and communication Obtain informed consent Optimize patient care, comfort and satisfaction Evaluate patient’s health status to determine if any pre-procedure consultations, testing are required Communicate patient issues among the health team assisting with the procedure
COMPONENTS OF PRESEDATION ASSESSMENT Includes the following: ASA (by provider) Airway evaluation (by provider) Weight Allergies Current medications NPO status Medical history Pay particular attention to respiratory issues such as COPD, sleep apnea, morbid obesity Surgical history Social history: smoking, drinking, drug use Informed consent and patient education
PRE-SEDATION ASSESSMENT: THE JOINT AND SNHMC POLICY Reassessment of Patient Immediately Prior to Procedure Performed by the provider: “The patient is reevaluated immediately prior to procedural sedation and analgesia administration. Included in this reassessment are cardiopulmonary status, review of vital signs, airway evaluation, and risk for sedation. ”
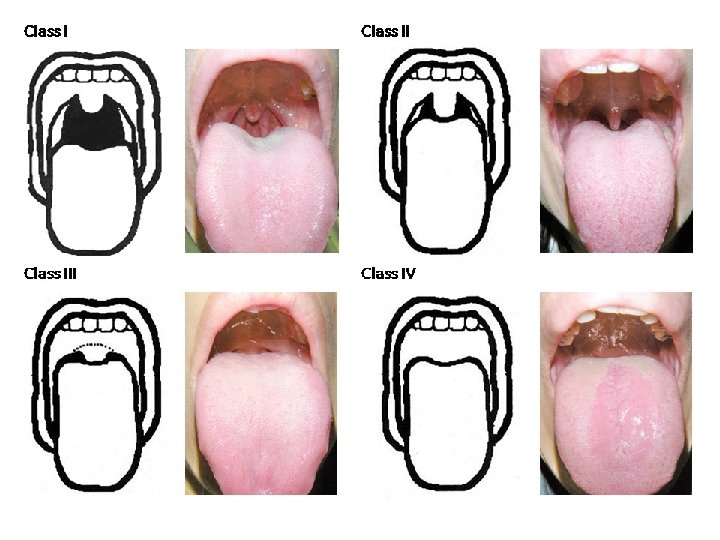
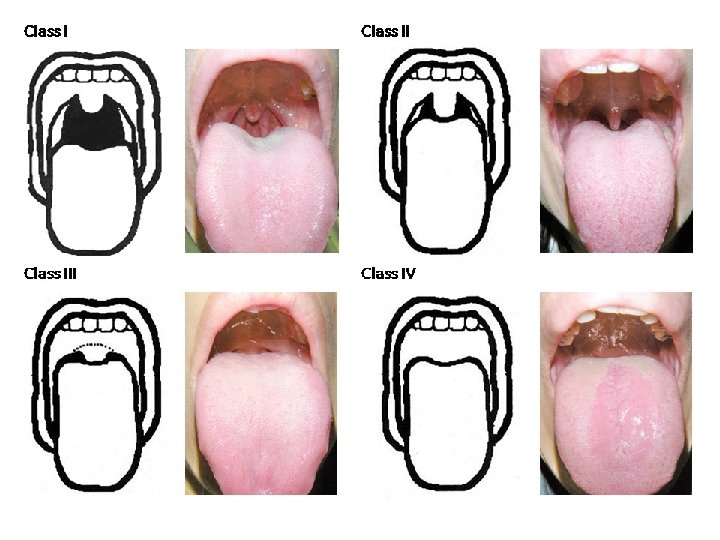
AIRWAY ASSESSMENT Mallampati Airway Classification Attempts to grade the degree of difficulty of endotracheal intubation Ranges from grade I to IV Patient should be in sitting position for this assessment Head in neutral position and mouth opened as wide as possible Instruct the patient not to speak during exam as this may lift the soft palate and interfere with accurate classification
AMERICAN SOCIETY OF ANESTHESIOLOGISTS PATIENT CLASSIFICATION: RISK ASSESSMENT ASA 1 A normal, healthy patient. The pathological process for which surgery is to be performed is localized and does not entail a systemic disease. Example: An otherwise healthy patient scheduled for a screening colonscopy
AMERICAN SOCIETY OF ANESTHESIOLOGISTS PATIENT CLASSIFICATION ASA 2 A patient with systemic disease, caused either by the condition to be treated or other pathophysiological process, but which does not result in limitation of activity. Example: a patient with asthma or hypertension that is well controlled with medical therapy and has no systemic sequelae
AMERICAN SOCIETY OF ANESTHESIOLOGISTS PATIENT CLASSIFICATION ASA 3 A patient with moderate or severe systemic disease caused either by the condition to be treated surgically or other pathophysiological processes, which does limit activity. Example: a patient with uncontrolled asthma that limits activity, or poorly controlled COPD or diabetes; multiple co-morbidities
AMERICAN SOCIETY OF ANESTHESIOLOGISTS PATIENT CLASSIFICATION ASA 4 A patient with severe systemic disease that is a constant, potential threat to life. Example: a patient with heart failure, or a patient with renal failure requiring dialysis.
AMERICAN SOCIETY OF ANESTHESIOLOGISTS PATIENT CLASSIFICATION ASA 5 A patient who is at substantial risk of death within 24 hours, and is submitted to the procedure in desperation. Example: a patient with fixed and dilated pupils status post a head injury.
CONSIDER ANESTHESIA REFERRAL FOR THE FOLLOWING PATIENTS: ASA III or higher Morbid obesity Sleep apnea Pregnancy Cardiomyopathy History of difficult sedations Full stomach Significant cardiac, pulmonary, renal or CNS dysfunction
MEDICATIONS COMMONLY USED IN PROCEDURAL SEDATION
WHY ADMINISTER MULTIPLE MEDICATIONS FOR PROCEDURAL SEDATION? No one single drug produces all the desired effects of procedural sedation May be achieved through drug combination Desired effects are: Rapid onset of action Short duration of action Lack of cumulative effects Rapid recovery Minimal side effects Increased patient satisfaction
BENZODIAZEPINES Bind in CNS, particularly cerebral cortex Used to achieve Anxiolysis Sedation Hypnosis Skeletal muscle relaxation Midazolam (Versed)
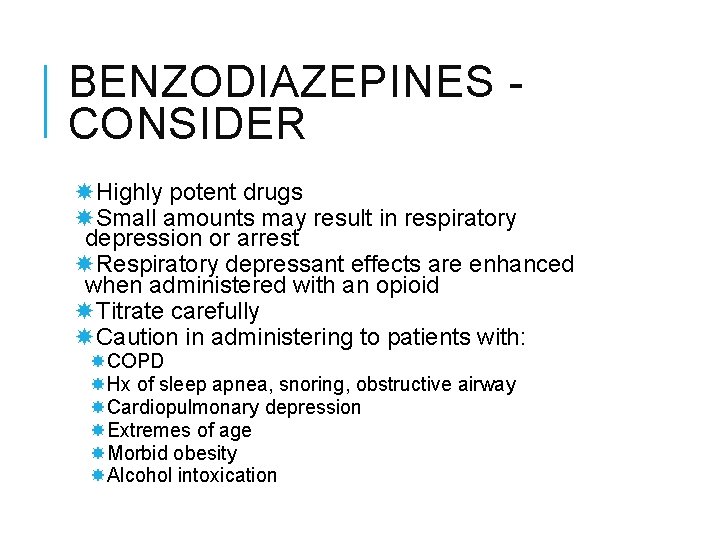
BENZODIAZEPINES CONSIDER Highly potent drugs Small amounts may result in respiratory depression or arrest Respiratory depressant effects are enhanced when administered with an opioid Titrate carefully Caution in administering to patients with: COPD Hx of sleep apnea, snoring, obstructive airway Cardiopulmonary depression Extremes of age Morbid obesity Alcohol intoxication
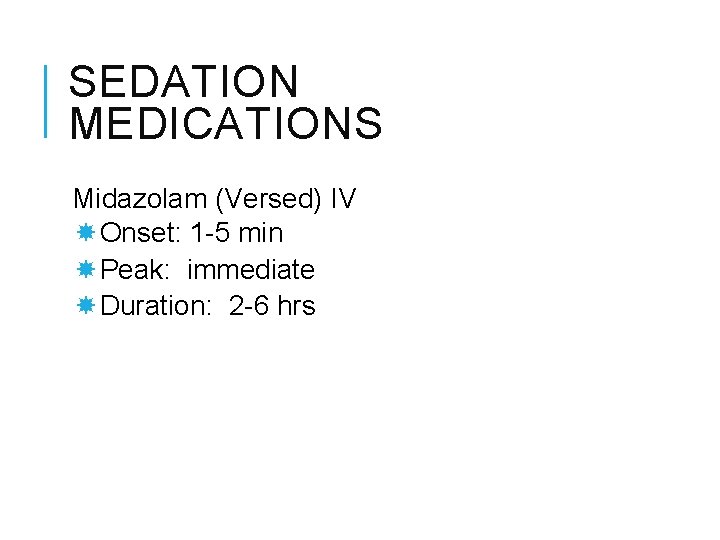
SEDATION MEDICATIONS Midazolam (Versed) IV Onset: 1 -5 min Peak: immediate Duration: 2 -6 hrs
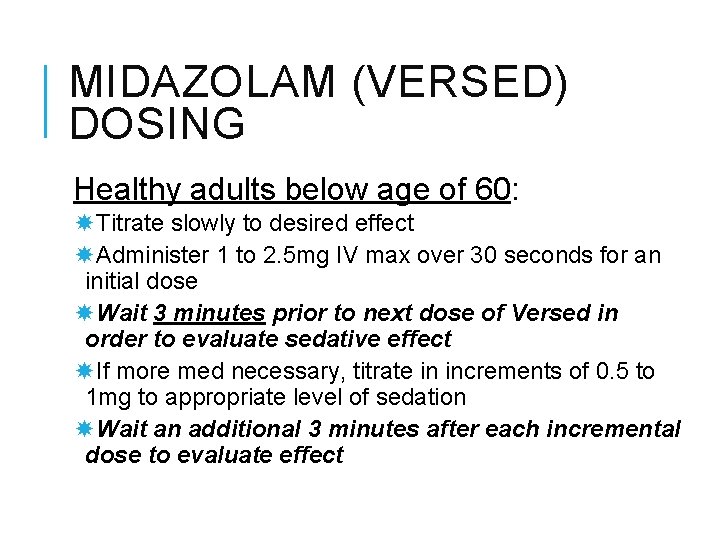
MIDAZOLAM (VERSED) DOSING Healthy adults below age of 60: Titrate slowly to desired effect Administer 1 to 2. 5 mg IV max over 30 seconds for an initial dose Wait 3 minutes prior to next dose of Versed in order to evaluate sedative effect If more med necessary, titrate in increments of 0. 5 to 1 mg to appropriate level of sedation Wait an additional 3 minutes after each incremental dose to evaluate effect
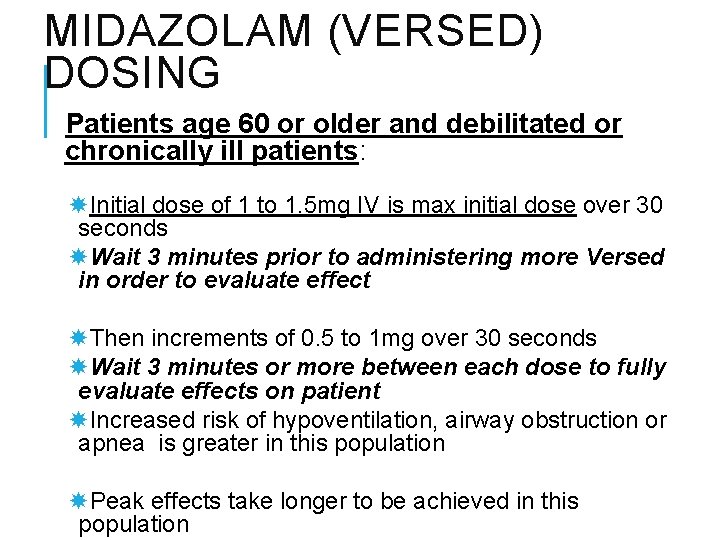
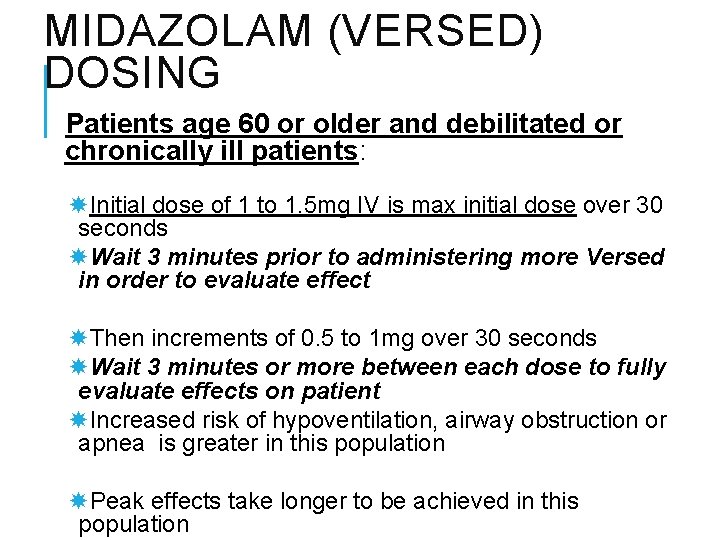
MIDAZOLAM (VERSED) DOSING Patients age 60 or older and debilitated or chronically ill patients: Initial dose of 1 to 1. 5 mg IV is max initial dose over 30 seconds Wait 3 minutes prior to administering more Versed in order to evaluate effect Then increments of 0. 5 to 1 mg over 30 seconds Wait 3 minutes or more between each dose to fully evaluate effects on patient Increased risk of hypoventilation, airway obstruction or apnea is greater in this population Peak effects take longer to be achieved in this population
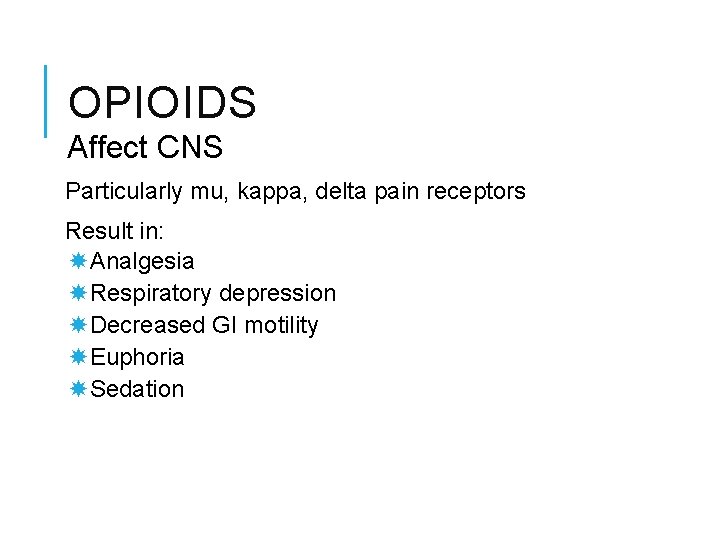
OPIOIDS Affect CNS Particularly mu, kappa, delta pain receptors Result in: Analgesia Respiratory depression Decreased GI motility Euphoria Sedation
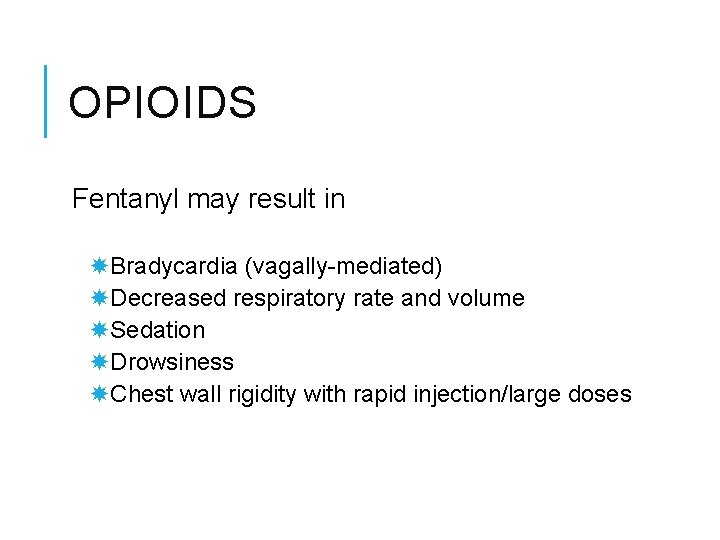
OPIOIDS Fentanyl may result in Bradycardia (vagally-mediated) Decreased respiratory rate and volume Sedation Drowsiness Chest wall rigidity with rapid injection/large doses
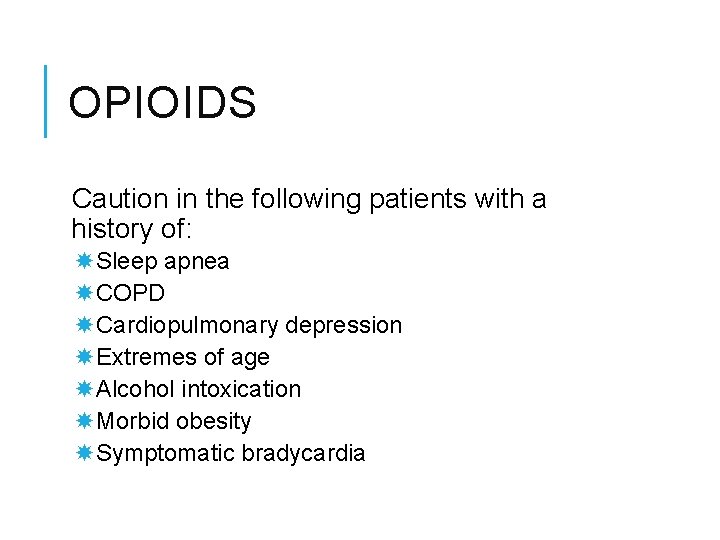
OPIOIDS Caution in the following patients with a history of: Sleep apnea COPD Cardiopulmonary depression Extremes of age Alcohol intoxication Morbid obesity Symptomatic bradycardia
FENTANYL About 75 -125 times more potent than morphine on a mg for mg basis Rapid onset IV 3 -5 min Short duration of action 30 -60 min Provides analgesia and may produce some sedation
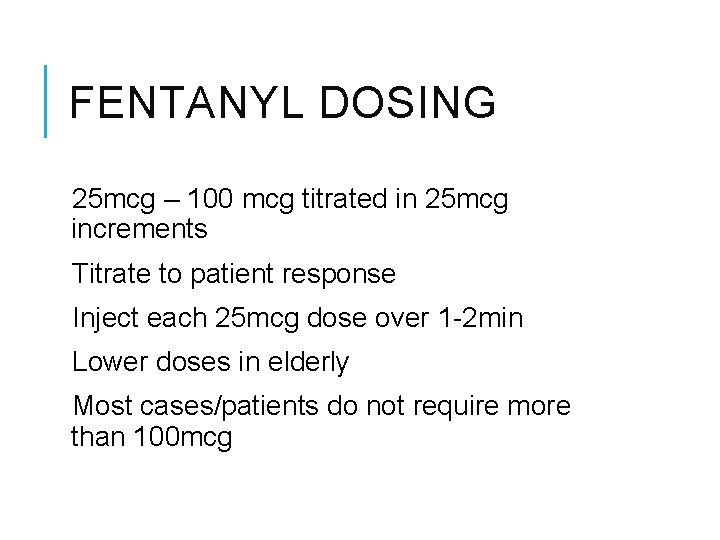
FENTANYL DOSING 25 mcg – 100 mcg titrated in 25 mcg increments Titrate to patient response Inject each 25 mcg dose over 1 -2 min Lower doses in elderly Most cases/patients do not require more than 100 mcg
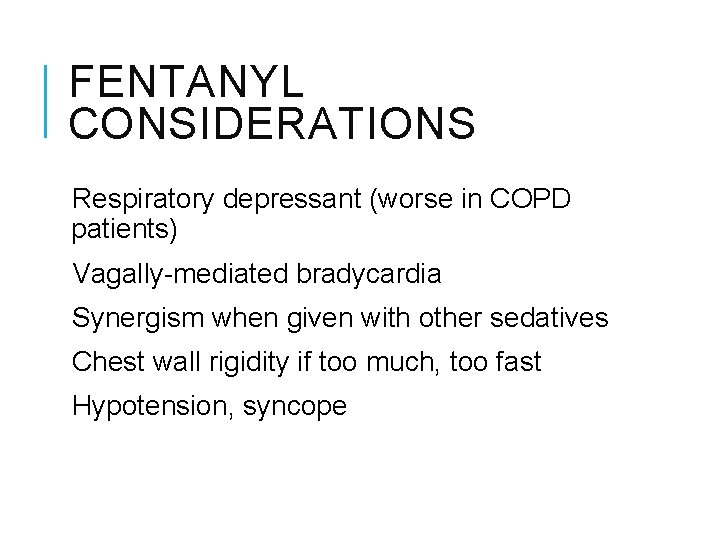
FENTANYL CONSIDERATIONS Respiratory depressant (worse in COPD patients) Vagally-mediated bradycardia Synergism when given with other sedatives Chest wall rigidity if too much, too fast Hypotension, syncope
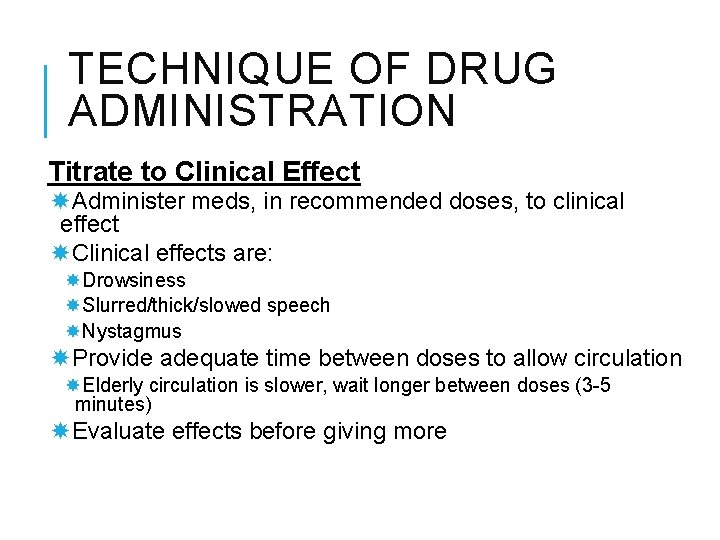
TECHNIQUE OF DRUG ADMINISTRATION Titrate to Clinical Effect Administer meds, in recommended doses, to clinical effect Clinical effects are: Drowsiness Slurred/thick/slowed speech Nystagmus Provide adequate time between doses to allow circulation Elderly circulation is slower, wait longer between doses (3 -5 minutes) Evaluate effects before giving more
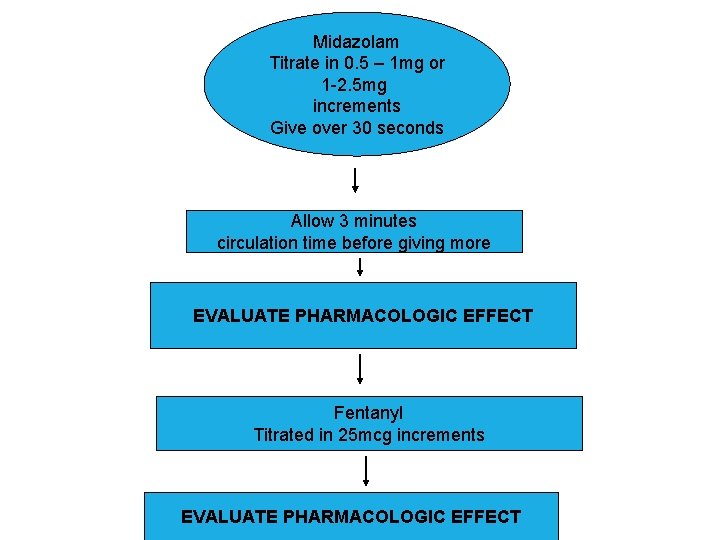
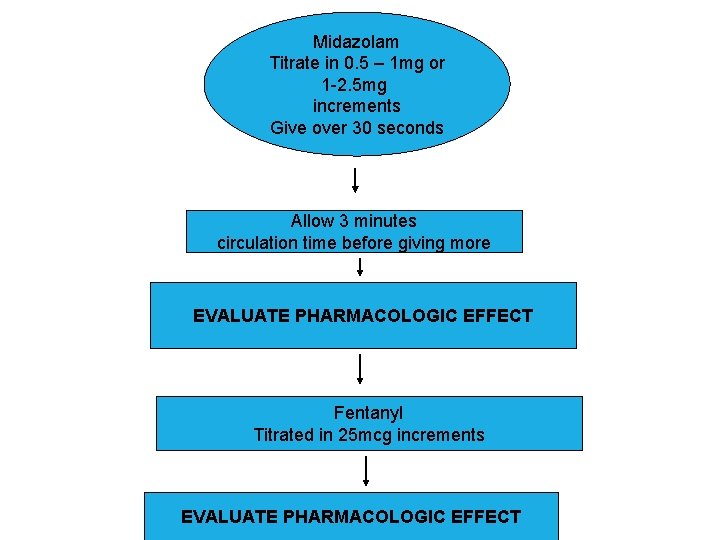
Midazolam Titrate in 0. 5 – 1 mg or 1 -2. 5 mg increments Give over 30 seconds Allow 3 minutes circulation time before giving more EVALUATE PHARMACOLOGIC EFFECT Fentanyl Titrated in 25 mcg increments EVALUATE PHARMACOLOGIC EFFECT
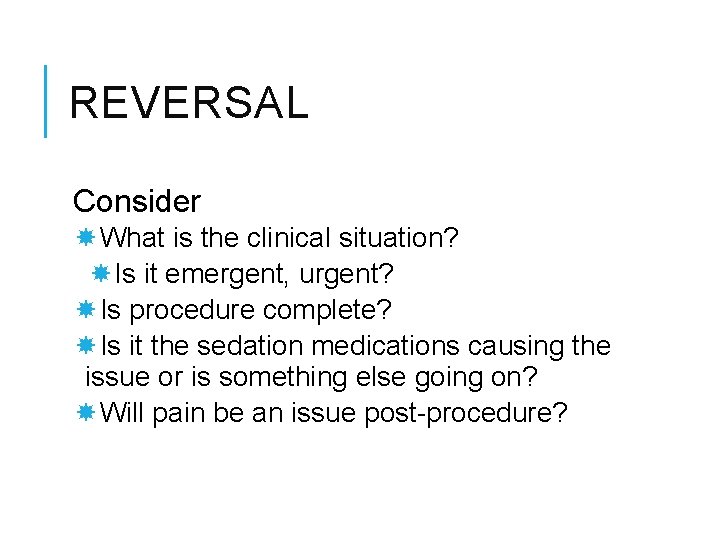
REVERSAL Consider What is the clinical situation? Is it emergent, urgent? Is procedure complete? Is it the sedation medications causing the issue or is something else going on? Will pain be an issue post-procedure?
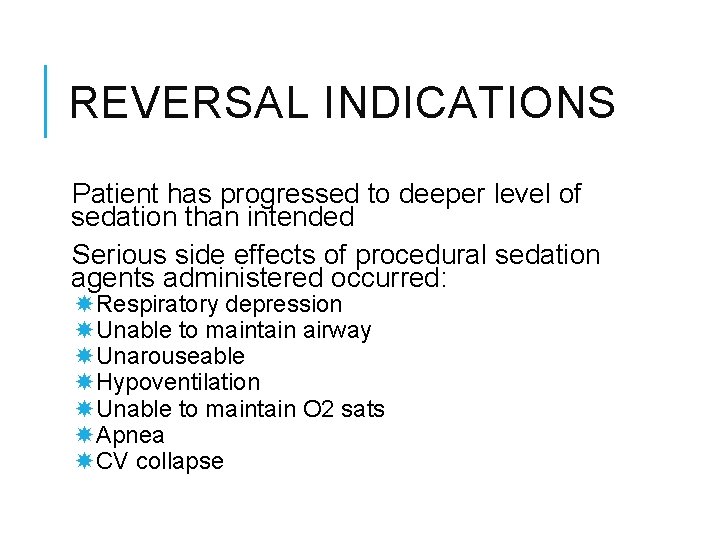
REVERSAL INDICATIONS Patient has progressed to deeper level of sedation than intended Serious side effects of procedural sedation agents administered occurred: Respiratory depression Unable to maintain airway Unarouseable Hypoventilation Unable to maintain O 2 sats Apnea CV collapse
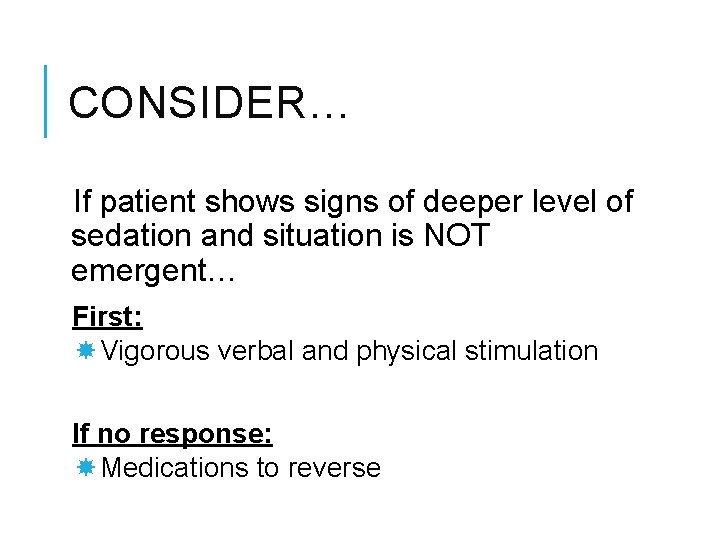
CONSIDER… If patient shows signs of deeper level of sedation and situation is NOT emergent… First: Vigorous verbal and physical stimulation If no response: Medications to reverse
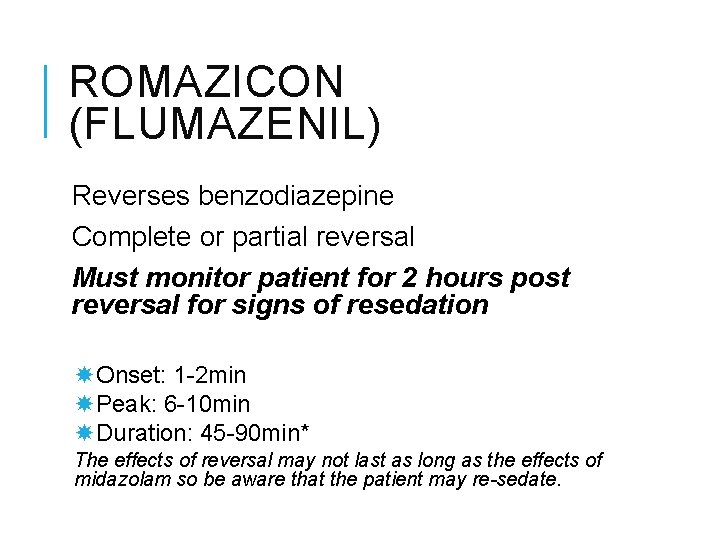
ROMAZICON (FLUMAZENIL) Reverses benzodiazepine Complete or partial reversal Must monitor patient for 2 hours post reversal for signs of resedation Onset: 1 -2 min Peak: 6 -10 min Duration: 45 -90 min* The effects of reversal may not last as long as the effects of midazolam so be aware that the patient may re-sedate.
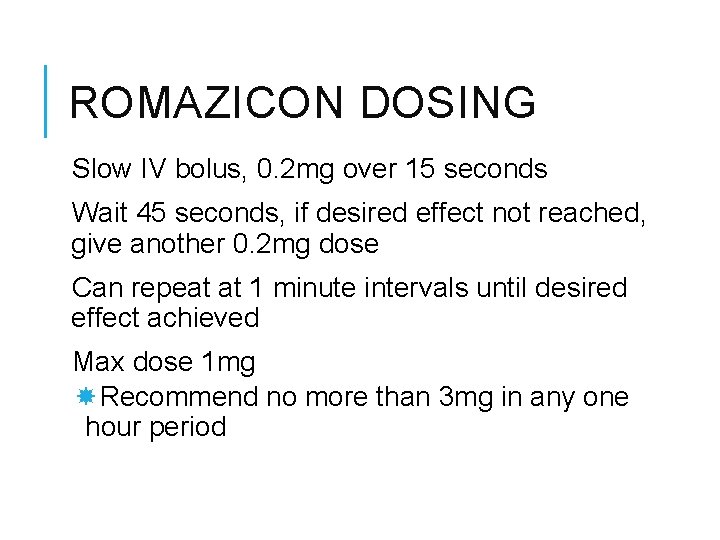
ROMAZICON DOSING Slow IV bolus, 0. 2 mg over 15 seconds Wait 45 seconds, if desired effect not reached, give another 0. 2 mg dose Can repeat at 1 minute intervals until desired effect achieved Max dose 1 mg Recommend no more than 3 mg in any one hour period
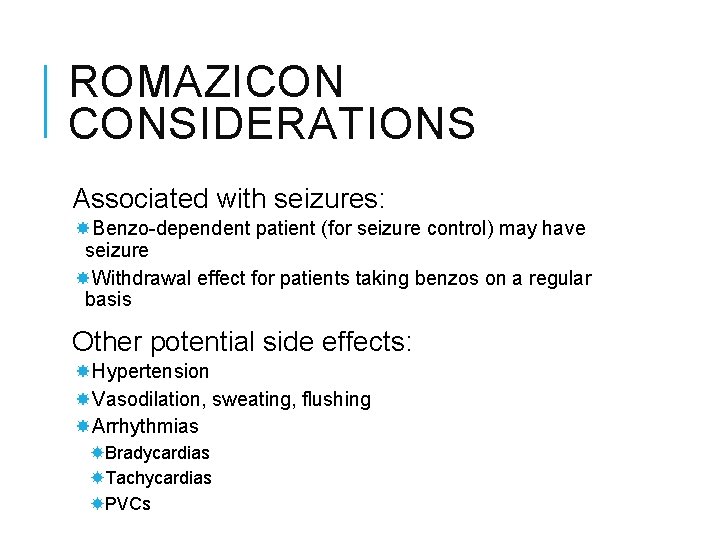
ROMAZICON CONSIDERATIONS Associated with seizures: Benzo-dependent patient (for seizure control) may have seizure Withdrawal effect for patients taking benzos on a regular basis Other potential side effects: Hypertension Vasodilation, sweating, flushing Arrhythmias Bradycardias Tachycardias PVCs
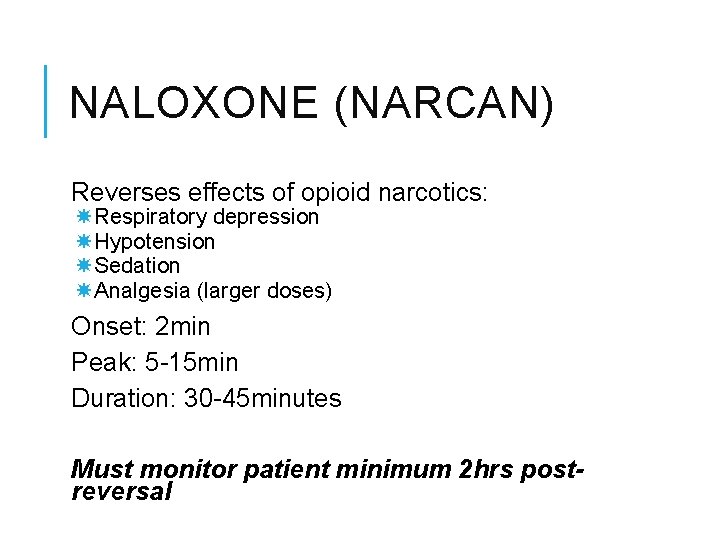
NALOXONE (NARCAN) Reverses effects of opioid narcotics: Respiratory depression Hypotension Sedation Analgesia (larger doses) Onset: 2 min Peak: 5 -15 min Duration: 30 -45 minutes Must monitor patient minimum 2 hrs postreversal
NALOXONE DOSING Administer titrated doses of 0. 1 mg increments May repeat every few minutes until desired effect(s) achieved
NALOXONE CONSIDERATIONS May cause: Hypertension Tachycardia Acute withdrawal in patients with narcotic dependence Agitation/combativeness Seizures Exaggerated if patient uses/misuses opioids
INTRA-PROCEDURE CARE Continuously monitor Level of consciousness/responsiveness Vital signs O 2 sat ETCO 2 ECG Monitor for complications

POST-PROCEDURE CARE Purpose: Return patient to pre-procedure physiologic function prior to discharge (home or inpatient unit) Expectation is that patient is discharged at the same baseline as he/she was pre-procedure Variables: These affect care and discharge time Include: Procedure performed & time in procedure Type and amounts of sedation Age of patient Presence of comorbidities Reversal agents administered
PROCEDURAL SEDATION & ANALGESIA DISCHARGE GUIDELINES The following 3 slides are taken directly from the SNHMC ICPC (policy) manual
DISCHARGE CRITERIA: The patient may be discharged to home or the inpatient unit when the discharge criteria have been met and sedation or narcotic analgesic has not been administered within 30 minutes. If a patient has received a reversal agent the patient will be monitored postprocedure for at least 2 (two) hours from the time the reversal agent was given. Patients who have received sedation or anesthesia in the outpatient setting will be discharged in the company of a responsible, designated adult. Definition: A responsible, designated adult is someone who can receive and understand instructions, stay with the patient, and call for assistance as instructed.
Written discharge instructions (for outpatients) that include information about expected behavior after sedation, instructions for eating and drinking, and the warning signs of complications will be provided. A 24 hour emergency contact number for complications will be given to the patient and the responsible, designated adult. Primary emergency contact should be the physician or allied health provider who performed the procedure or his/her coverage. A discharge order must be written by the physician or allied health provider. Outpatients cannot to drive themselves home. Patients will be cautioned against driving, operating machinery, or making important decisions for the next 24 hours.
COMPLICATIONS OF PROCEDURAL SEDATION Airway Obstruction Even when recognized immediately, can lead to respiratory insufficiency Can occur at any time intra or post-procedure Signs and symptoms Increased respiratory effort Snoring/snorting sounds Sternal retraction Rocking chest motion Inspiratory stridor Hypoxemia Hypercarbia Absence of breath sounds

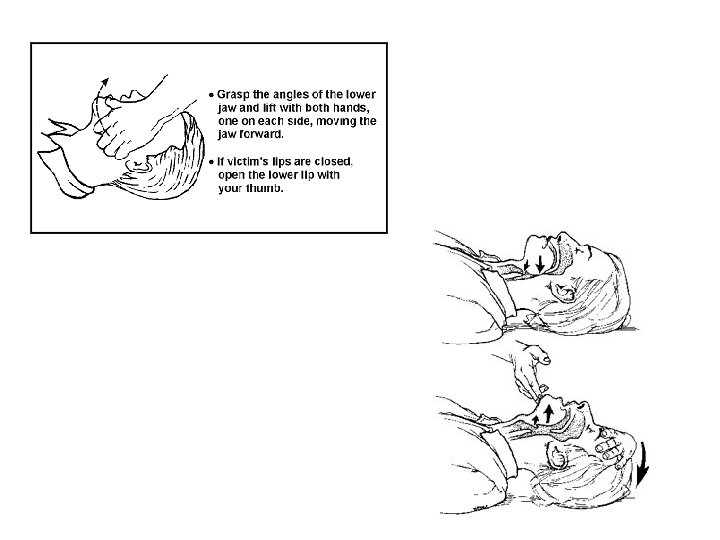
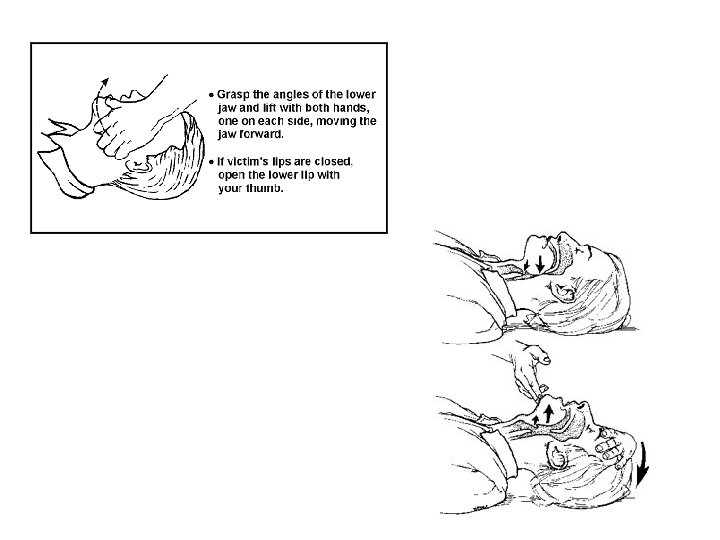
MANAGEMENT OF AIRWAY OBSTRUCTION Goals: Anterior displacement of mandible Elevation of base of tongue off of posterior pharyngeal wall to restore airflow Techniques: Verbal/physical stimulation Airway maneuver Nasal/oral airway insertion Consider pharmacological reversal Anesthesia stat?
HYPOXIA Evidence shows a reduction in adverse effects during procedural sedation when supplemental O 2 is delivered throughout the case All patients should receive O 2 unless there is a specific contraindication to its use* *A patient with a contraindication to O 2 probably needs anesthesia Administer at a rate to maintain O 2 sats at 95% or better, or at patient’s baseline
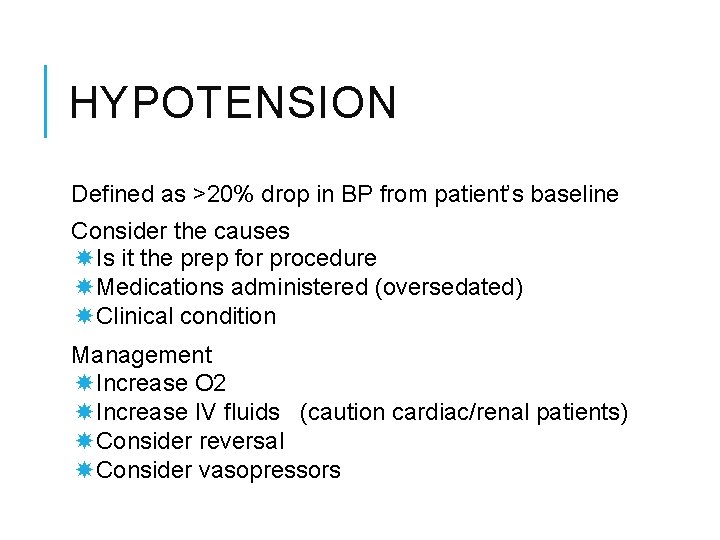
HYPOTENSION Defined as >20% drop in BP from patient’s baseline Consider the causes Is it the prep for procedure Medications administered (oversedated) Clinical condition Management Increase O 2 Increase IV fluids (caution cardiac/renal patients) Consider reversal Consider vasopressors
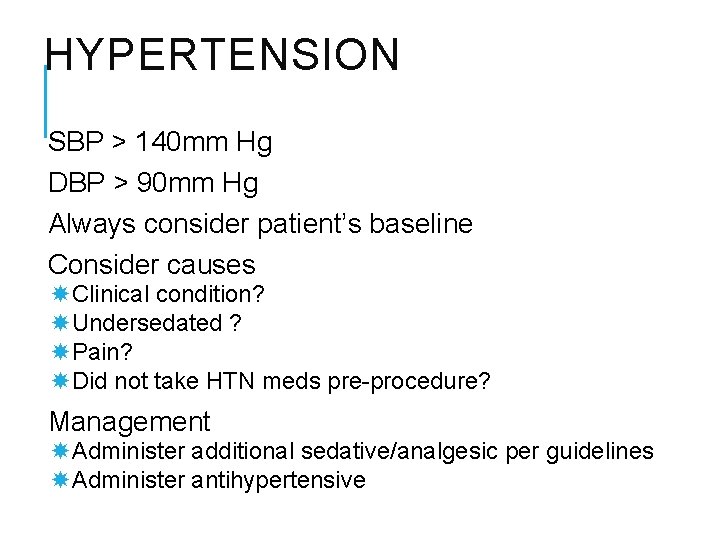
HYPERTENSION SBP > 140 mm Hg DBP > 90 mm Hg Always consider patient’s baseline Consider causes Clinical condition? Undersedated ? Pain? Did not take HTN meds pre-procedure? Management Administer additional sedative/analgesic per guidelines Administer antihypertensive
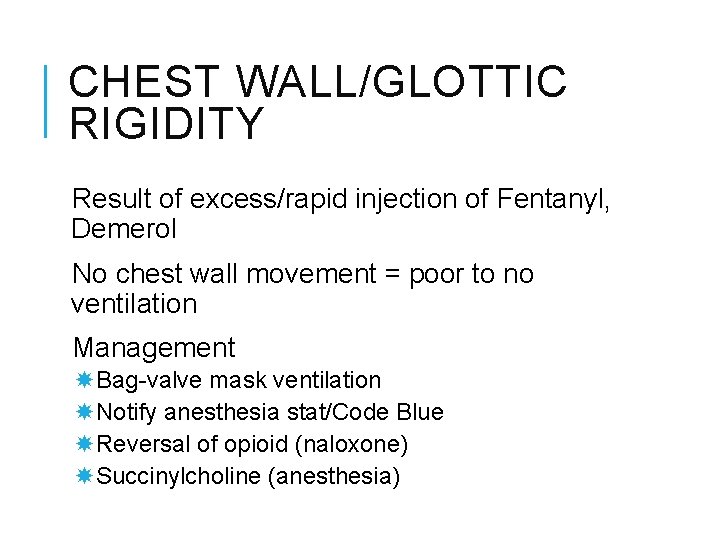
CHEST WALL/GLOTTIC RIGIDITY Result of excess/rapid injection of Fentanyl, Demerol No chest wall movement = poor to no ventilation Management Bag-valve mask ventilation Notify anesthesia stat/Code Blue Reversal of opioid (naloxone) Succinylcholine (anesthesia)
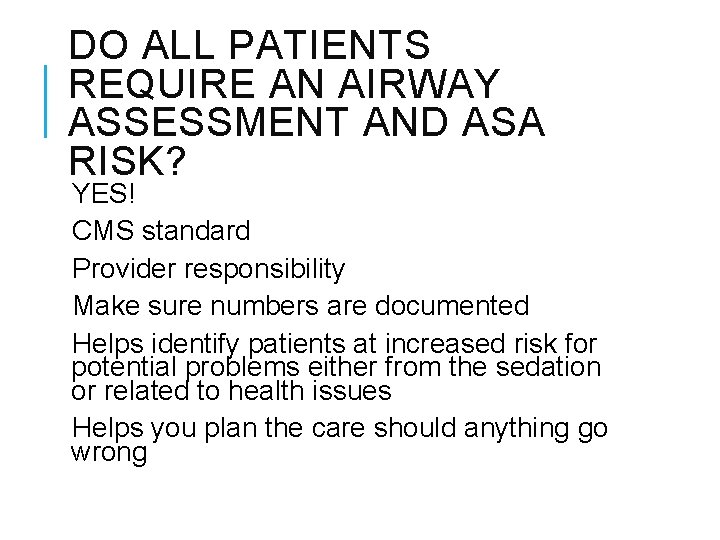
DO ALL PATIENTS REQUIRE AN AIRWAY ASSESSMENT AND ASA RISK? YES! CMS standard Provider responsibility Make sure numbers are documented Helps identify patients at increased risk for potential problems either from the sedation or related to health issues Helps you plan the care should anything go wrong
 Prodecural
Prodecural Analgesia sistemica
Analgesia sistemica Elastomero morfina effetti collaterali
Elastomero morfina effetti collaterali Poss sedation scale
Poss sedation scale Dexmedetomidine dose
Dexmedetomidine dose Richmond agitation sedation scale
Richmond agitation sedation scale Over-sedation
Over-sedation Rikers sedation scale
Rikers sedation scale Sédation
Sédation Sccm pad guidelines
Sccm pad guidelines Vmware service provider program
Vmware service provider program Gitlow v new york constitutional question
Gitlow v new york constitutional question Procedural justice
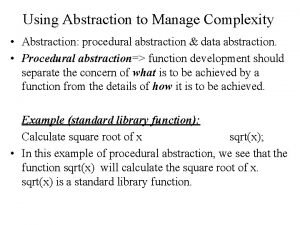
Procedural justice Procedural abstraction computer science
Procedural abstraction computer science Preference for specific design control for procedural bias
Preference for specific design control for procedural bias Functional programming vs object oriented
Functional programming vs object oriented Oracle procedural language extensions to sql
Oracle procedural language extensions to sql A purpose of procedural writing is
A purpose of procedural writing is Features of a procedural text
Features of a procedural text Procedural modeling in blender with python
Procedural modeling in blender with python Procedural analysis
Procedural analysis Types of knowledge
Types of knowledge Isa-95
Isa-95 Procedural hukommelse
Procedural hukommelse Substantive vs procedural due process
Substantive vs procedural due process Mdcps dpgt
Mdcps dpgt Python procedural language
Python procedural language Joey paquet
Joey paquet Substantive vs procedural due process
Substantive vs procedural due process Substantive vs procedural due process
Substantive vs procedural due process Each e/m code description identifies the
Each e/m code description identifies the Liberty chapter 20
Liberty chapter 20 Substantive vs procedural due process
Substantive vs procedural due process Declarative self vs procedural self
Declarative self vs procedural self Chapter 19 procedural coding
Chapter 19 procedural coding What is procedural programming
What is procedural programming Computable functions and predicates in ai
Computable functions and predicates in ai Explain the basis of procedures
Explain the basis of procedures Define dental public health
Define dental public health Compare procedural semantics and declarative semantics.
Compare procedural semantics and declarative semantics. Procedural sound generation
Procedural sound generation Procedural constructs
Procedural constructs Superpipeline
Superpipeline Procedural unconscionability
Procedural unconscionability Procedural knowledge examples in math
Procedural knowledge examples in math The procedural view of democracy is most concerned with
The procedural view of democracy is most concerned with Misattribution psychology
Misattribution psychology Physical and procedural barriers of cross contamination
Physical and procedural barriers of cross contamination Relational query languages
Relational query languages Apa pengertian dari procedural dependency?
Apa pengertian dari procedural dependency? Antecedent procedural questions
Antecedent procedural questions Blender procedural road
Blender procedural road Verilog vpi
Verilog vpi Statement terminator
Statement terminator Module coupling
Module coupling Sequential cohesion example
Sequential cohesion example