Chapter 28 Procedural and Diagnostic Coding Lecture Notes
- Slides: 19
Chapter 28 Procedural and Diagnostic Coding Lecture Notes Medical Assisting Administrative & Clinical Competencies, 8 th edition, Michelle Blesi
Healthcare Common Procedure Coding System (HCPCS) The Healthcare Common Procedure Coding system (HCPCS) is comprised of two levels (subsystems): Level I: Current Procedural Terminology (CPT) codes, published by the American Medical Association (AMA). Level II: Codes that identify products, supplies, and services not included in CPT, produced by the Centers for Medicare and Medicaid Services (CMS). The term procedure code refers to a code that represents a medical procedure such as surgery or diagnostic tests, and medical services such as evaluating a patients condition by physical examination. This term is often used interchangeably with “CPT”.
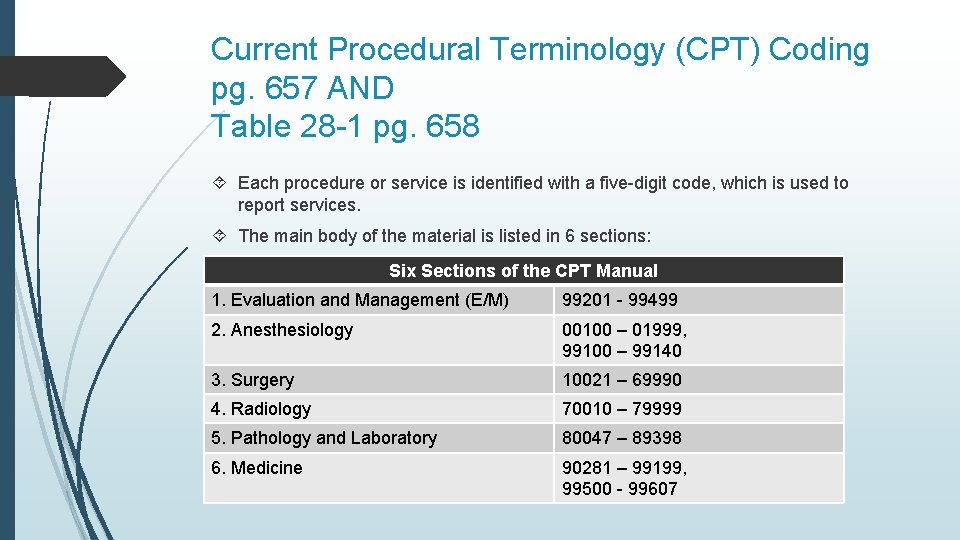
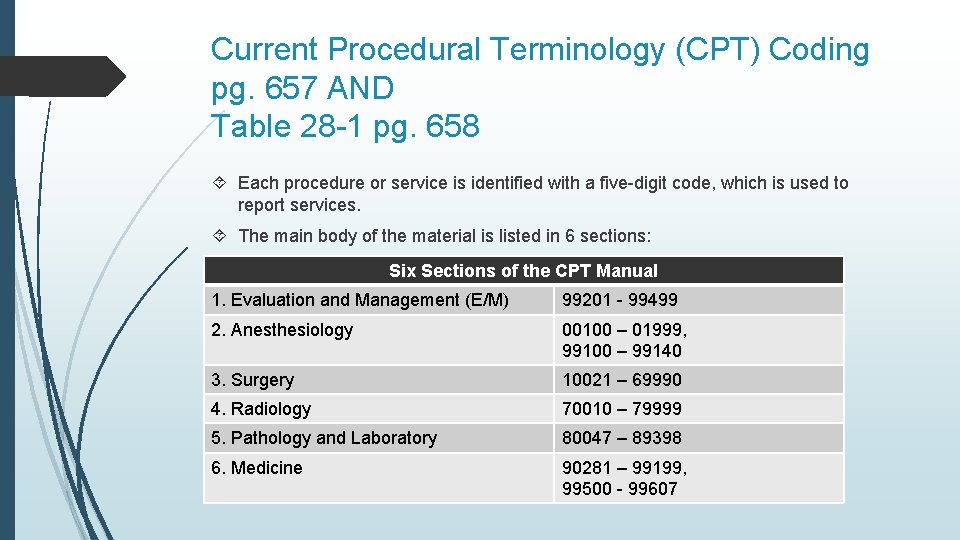
Current Procedural Terminology (CPT) Coding pg. 657 AND Table 28 -1 pg. 658 Each procedure or service is identified with a five-digit code, which is used to report services. The main body of the material is listed in 6 sections: Six Sections of the CPT Manual 1. Evaluation and Management (E/M) 99201 - 99499 2. Anesthesiology 00100 – 01999, 99100 – 99140 3. Surgery 10021 – 69990 4. Radiology 70010 – 79999 5. Pathology and Laboratory 80047 – 89398 6. Medicine 90281 – 99199, 99500 - 99607
Add-on Codes pg. 658 Add-on codes are ALWAY performed in addition to the primary procedure or service. Add-on codes are designated with the + symbol and are found in Appendix D of the CPT code book. Add-on codes are NEVER reported as a stand-alone code.
CPT Symbols pg. 658 Conventions are a list of abbreviations, punctuations, symbols, typefaces, and instructional notes. Conventions provide guidelines for using the code set.
Modifiers pg. 659 In some instances, a specific procedure or service might need to be slightly altered, and if this is the case, instructions and Appendix A explain the use of modifiers. Modifiers inform third-party payers that circumstances for that particular code have been altered.
Coding Terminology pg. 660 Any code that includes more than one procedure in its description is a bundled code. Code descriptions must be read carefully as it can be considered fraudulent coding to unbundle codes. Unbundling of codes refers to using several CPT codes for a service when one inclusive code is available. Upcoding: When a facility coder assigns a procedure code that does NOT match patient documentation, with the intention of increasing reimbursement to the facility or practice, serious penalties and fines will be levied against the facility or practice for submitting fraudulent claims. Downcoding is another practice in which a reported Evaluation and Management service is reduced to a lower level based strictly on the diagnosis code reported.
Evaluation and Management Services Guidelines pg. 661 A new patient for CPT purposes is a patient who has not received services from a provider of the exact same specialty and subspecialty within the past three years. An established patient is one who has received professional services from a provider of the exact same specialty and subspecialty who belongs to the same group practice, within the past three years.
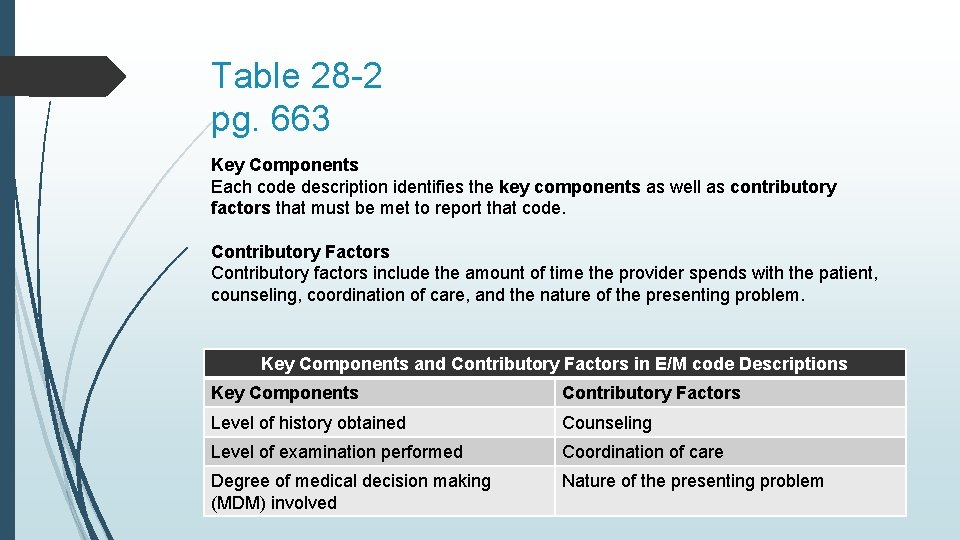
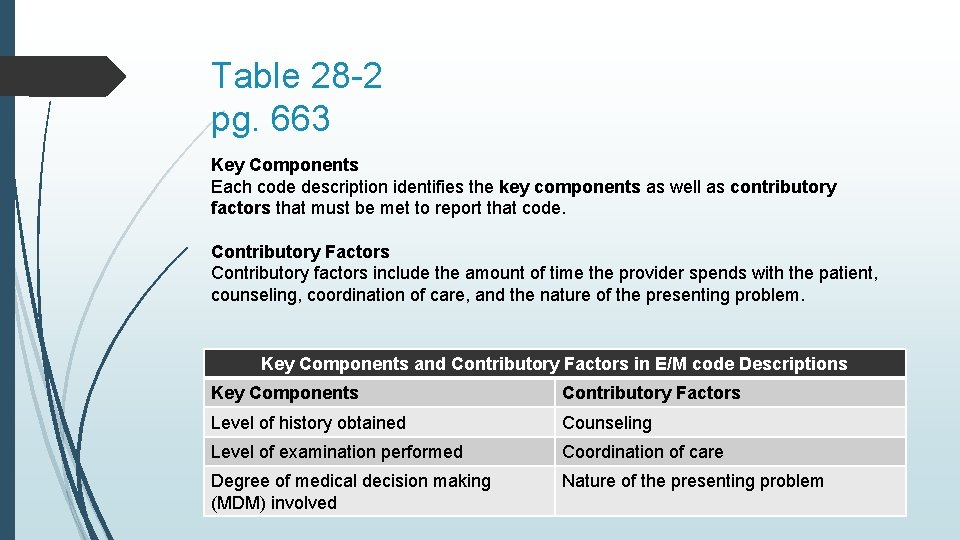
Table 28 -2 pg. 663 Key Components Each code description identifies the key components as well as contributory factors that must be met to report that code. Contributory Factors Contributory factors include the amount of time the provider spends with the patient, counseling, coordination of care, and the nature of the presenting problem. Key Components and Contributory Factors in E/M code Descriptions Key Components Contributory Factors Level of history obtained Counseling Level of examination performed Coordination of care Degree of medical decision making (MDM) involved Nature of the presenting problem
Surgical Coding pg. 664 Surgical procedures found in CPT are often part of a surgical package. A surgical package generally includes: The preoperative exam and testing The surgical procedure itself (including local or regional anesthesia if used) The routine follow-up care for a set period of time The payer assigns a fee to each of the surgical packages. The global period refers to the period of time that is covered for follow-up care.
CPT Coding Rules pg. 667 Generally, services performed in the office are marked on the patient’s encounter form by the provider. Any service or procedure that is coded must be adequately documented in the medical record. If clarification is needed because the documentation is unclear about what procedure or service was performed, seek assistance from the provider Remember, if a service is not documented, it should not be coded; payers regard undocumented services as never having been performed.
CPT Coding Rules pg. 667 General rules for assigning CPT codes are as follows: 1. Analyze the provider’s statement or description for the service provided and isolate the main term. 2. Identify the main term in the index. 3. Check for any relevant subterms under the main term. 4. Note the code(s) found in the index for the main term or subterm(s). 5. After locating the term and the code in the index, verify each code in the respective section of the manual to be sure the description matches the procedure or service performed. 6. NEVER CODE DIRECTLY FROM THE INDEX. ALWAYS, crossreference with the code or codes found in the index with the actual code descriptions in the tabular list. 7. Many times, one specific code is provided; the description should be reviewed and compared to the procedure or service provided. In other cases, there will be multiple codes or code ranges, all of which will need to be reviewed to locate the correct code. Verify the descriptions to select the correct code. 8. In all cases, it is necessary to review all descriptions of codes listed for main terms and subterms to be sure the correct code is selected.
HCPCS Level II Codes pg. 670 HCPCS Level II codes were developed to identify products and supplies for which there are no CPT codes, including items such as durable medical equipment (DME), drugs, and injectables. HCPCS Level II codes are composed of five characters (alphanumeric – letters and numbers) and published annually. The HCPCS Level II manual has two sections, the index and the tabular list of codes. The search for the correct HCPCS code begins in the index which has services and supplies listed in alphabetic order. When appropriate, the correct HCPCS modifier should be appended to provide additional information about the circumstances surrounding the service. It is also possible to report both CPT codes and HCPCS Level II codes on the same claim. HCPCS Level II G codes are temporary codes for procedures and or professional services.
ICD-10 -CM Code Structure pg. 673 ICD-10 -CM codes vary from three to seven characters. The first three characters designate the category of the diagnosis. The next three characters (four through six) correspond to the related etiology (the cause of a disease or condition), anatomic site, severity, or other vital clinical details. The seventh character applies to certain categories noted with the Tabular List of codes. If a code that requires seven characters has fewer than six characters, use the placeholder “X” to fill in all of the empty character spaces. Seventh character extentions for injuries include for example: A - initial encounter D – subsequent encounter S – sequela (a pathological condition resulting from prior injury, disease, or attack) ICD-10 -CM codes describe the disease or condition presented by the patient.
Medical Necessity Guidelines pg. 674 The AMA defines medical necessity as services or procedures that a prudent physician would provide to a patient in order to prevent, diagnose, or treat an illness, injury, or disease or the associated symptoms in a manner that is: In accordance with the generally accepted standard of medical practice. Clinically appropriate in terms of frequency, type, extent, site, and duration. Not for the intended economic benefit of the health plan or purchaser or the convenience of the patient, physician, or other health care provider (AMA, 2017).
Overview of ICD-10 -CM Official Conventions pg. 674 - 675 The Alphabetic Index contains the Index to Diseases and Injuries (main index) and the Index to External Causes of Injury. In addition, the main index includes the Neoplasm Table and a Table of Drugs and Chemicals. The Tabular List contains categories, subcategories, and valid codes. The Tabular List is an alphanumeric classification system.
ICD-10 -CM Official Guidelines for Coding and Reporting pg. 676 In addition to the specifics of the guideline, general ICD-10 -CM coding rules to follow are: 1. Code correctly and completely any diagnosis or procedure that affects the care, influences the health status, or is a reason for treatment on that visit. 2. Code the minimum number of diagnoses that fully describe the patient’s care received on that visit. The diagnosis must reflect the patient’s need for treatment, x -rays, diagnostic procedures, or medications. 3. Code each problem to the highest level of specificity (fourth through seventh character) available in the classification. Sequence codes correctly so that it is possible to understand the chronology of events (e. g. the reason for the visit and care). 4. The main rule to remember is that the reason for the patient visit (encounter) is coded first. This is the primary diagnosis.
Procedure 28 -3 pg. 685 Perform Diagnostic Coding 1. Review the narrative diagnostic finding(s) indicated on the encounter form (Progress Note/A&P) and either underline or highlight them. 2. Identify the main terms in the diagnostic statement(s). 3. Using the Alphabetic Index of the ICD-10 -CM manual locate the correct main term. Never code directly from the Alphabetic Index! 4. Turn to the Tabular List of the ICD-10 -CM manual and locate the code of the main term you identified from the Alphabetic Index. 5. After locating the main term in the Tabular List, review any subterms listed to identify the most accurate code. Carefully reading the main term and subterms helps locate the correct code. 6. Read the description of the code and any coding conventions related to it. Continue the process until you have found the correct code. Be sure to pick the most specific code available. 7. On the encounter form, write down the code you have determined best describes the diagnosis(es) reported. If reporting electronically, select the correct ICD-10 -CM code(s) in the EMR.
Medicare Audit pg. 689 Effective November 2, 2015, anyone knowingly submitting a false claim or creating a false record or statement to receive payment from the federal government will be fined a minimum per-claim civil penalty of $10, 781 and a maximum per-claim civil penalty of $21, 563 per false claim submitted. Violations of the Federal False Claims Act can also include imprisonment and other penalities.