ICU Curriculum Sedation and Analgesia in the ICU
- Slides: 33
ICU Curriculum Sedation and Analgesia in the ICU
Clinical Case 68 year old female with COPD presented to the emergency department with 3 days of cough, dyspnea and fevers. Over the prior 12 hours, she was acting more somnolent requiring presentation to the emergency department. Temp: 39. 4 HR: 124 BP: 111/73 RR: 28 Sp. O 2: 78% on 6 L Somnolent and unarousable Emergently intubated in the ED with propofol and ketamine.
Clinical question What initial sedation would you choose? A. Fentanyl B. Midazolam C. Propofol D. Dexmedetomidine E. None
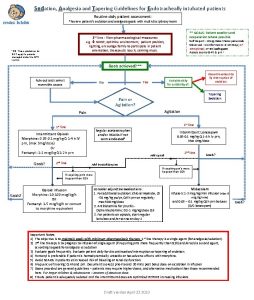
Approach to ICU sedation Multiple reasons for appearing uncomfortable Recent guidelines support an “analgo-sedation” approach Assessment should address in order: Pain Agitation Delirium
Management of Analgesia Pain may be caused by: Underlying condition Monitoring and therapeutic devices Routine nursing care Prolonged immobility Goals of pain control: Optimizing patient comfort Avoiding self harm Avoiding physiologic responses to pain such as hypermetabolism and increased oxygen consumption
ICU Pain Assessment No superior tool, but a protocolized, frequent assessment is essential Behavioral Pain Scale (BPS): Evaluates: Facial expression (ex: relaxed, grimacing) Body movement (ex: no movement, limbs retracted) Ventilator Compliance (ex: tolerating, unable to control) Critical Care Pain Observation Tool (CPOT) Evaluates: Facial expression Body movement Body posture Verbal response (in non-intubated patients) or ventilator compliance (in intubated patients)
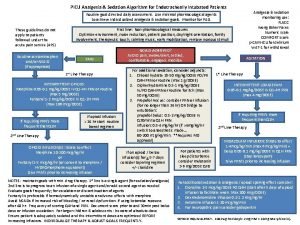
Analgesia Therapy Opioids – the mainstay of pain treatment in the ICU Selection of specific agent depends on each agent’s pharmacology and side effect profile Guidelines recommend the use of fentanyl, hydromorphone, or morphine if an IV opioid analgesic is required
Fentanyl First line opioid for ICU analgesia Synthetic derivative of morphine, approximately 100 times more potent No histamine-releasing properties Rapid onset and short duration of action But…prolonged administration will lead to slower elimination (and possibly prolonged sedation) because of mobilization of drug from fat and muscle stores Metabolized to inactive compounds in the liver, so renal failure does not alter its pharmacokinetics
Assessment of Agitation Multiple sedation assessment scales have been developed for clinical use Ramsay Sedation Scale Richmond Agitation-Sedation Scale (RASS) Minnesota Sedation Assessment Tool (MSAT) Most scales rate the patient’s response to increasing levels of stimulation Sedation scales allow more uniform assessment of sedation and easier titration of sedatives according to sedation protocols
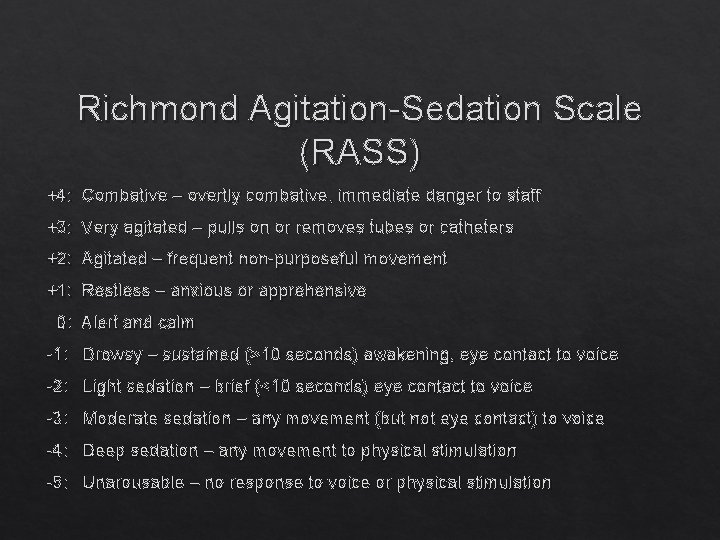
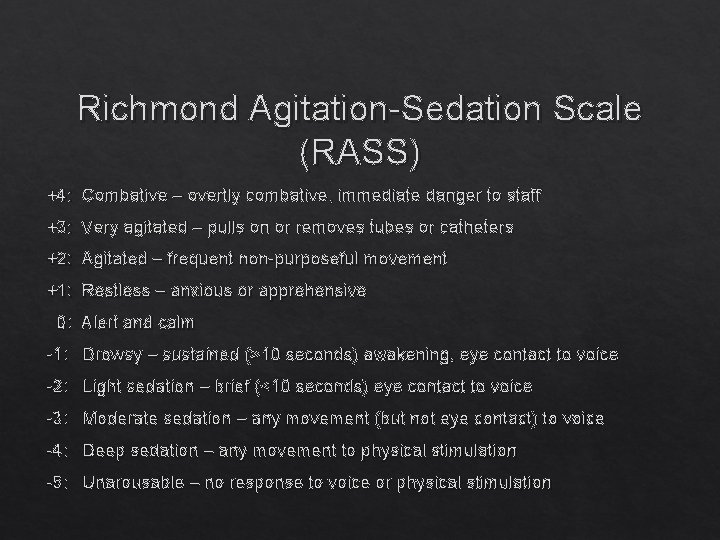
Richmond Agitation-Sedation Scale (RASS) +4: Combative – overtly combative, immediate danger to staff +3: Very agitated – pulls on or removes tubes or catheters +2: Agitated – frequent non-purposeful movement +1: Restless – anxious or apprehensive 0: Alert and calm -1: Drowsy – sustained (>10 seconds) awakening, eye contact to voice -2: Light sedation – brief (<10 seconds) eye contact to voice -3: Moderate sedation – any movement (but not eye contact) to voice -4: Deep sedation – any movement to physical stimulation -5: Unarousable – no response to voice or physical stimulation
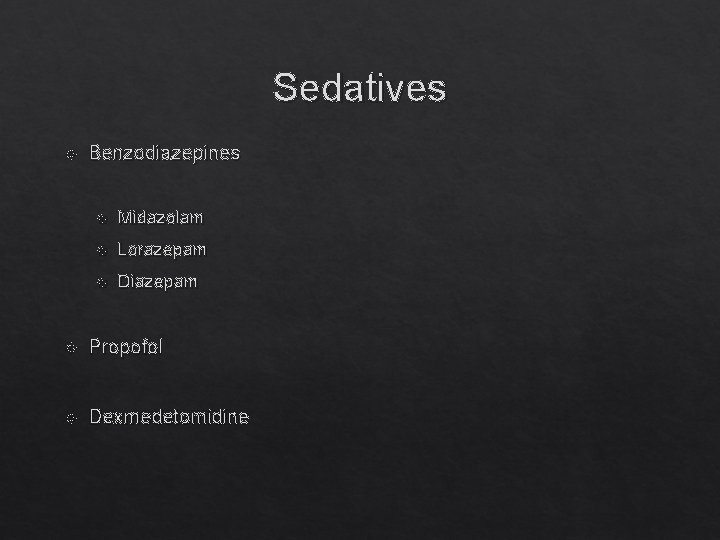
Sedatives Benzodiazepines Midazolam Lorazepam Diazepam Propofol Dexmedetomidine
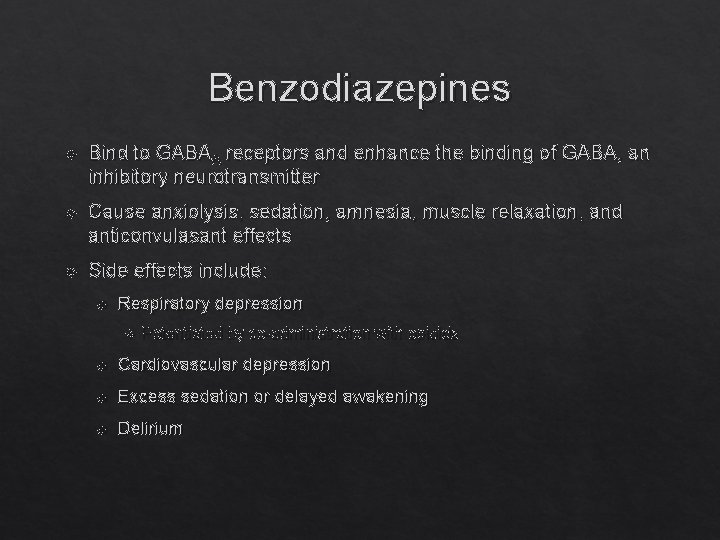
Benzodiazepines Bind to GABAA receptors and enhance the binding of GABA, an inhibitory neurotransmitter Cause anxiolysis, sedation, amnesia, muscle relaxation, and anticonvulasant effects Side effects include: Respiratory depression Potentiated by co-administration with opioids Cardiovascular depression Excess sedation or delayed awakening Delirium
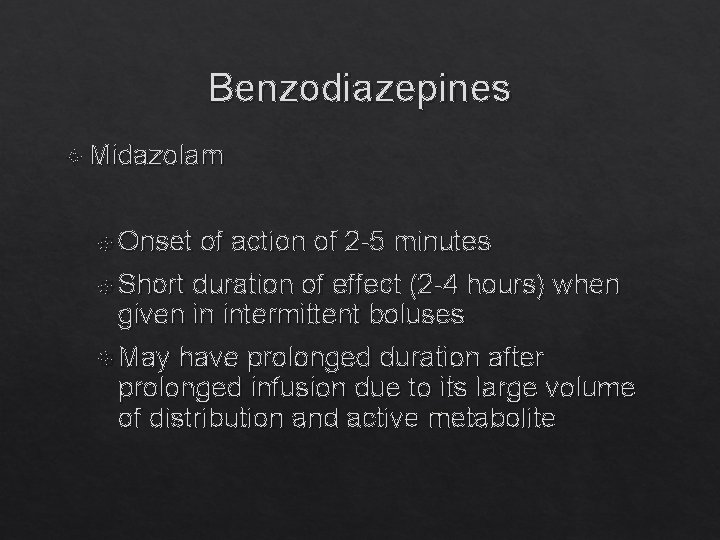
Benzodiazepines Midazolam Onset of action of 2 -5 minutes Short duration of effect (2 -4 hours) when given in intermittent boluses May have prolonged duration after prolonged infusion due to its large volume of distribution and active metabolite
Benzodiazepines Lorazepam Slower onset of action (5 -20 minutes) because it’s less lipophilic Moderate duration of effect (6 -8 hours) when given in intermittent boluses Metabolism does not form active metabolites Propylene glycol is the carrier and may lead to toxicity (hyperosmolarity, anion gap metabolic acidosis, and kidney injury)
Propofol Mechanism of action not completely understood, but likely acts via interaction with GABA receptors Has amnestic, anxiolytic, anticonvulsant, and muscle relaxant effects No analgesic effect Duration of action is 3 -10 minutes when given in intermittent boluses (due to rapid redistribution from effector sites); slightly longer duration of action when given as an infusion Useful when rapid awakening is desired
Propofol Elimination is not impaired by hepatic or renal dysfunction Most common side effects: dose- and rate-dependent hypotension, bradycardia, arrhythmias, neuroexcitatory effects Prolonged infusions can lead to pancreatitis, increased carbon dioxide production, hypertriglyceridemia, and excessive caloric load (1. 1 kcal/ml)
Propofol Infusion Sydrome A rare complication of propofol infusions of greater than 4 mg/kg/hr for >48 hours Associated with refractory bradycardia, severe metabolic acidosis, rhabdomyolysis, cardiovascular collapse, hyperlipidemia, renal failure, and hepatomegaly Treatment includes discontinuation of propofol and supportive care Associated with high mortality
Dexmedetomidine Centrally acting alpha-2 agonist Has sedative, anxiolytic, and analgesic properties Does not cause significant respiratory depression Adverse effects include hypotension and bradycardia
Which sedative is best?
Propofol versus midazolam Ostermann and colleagues (JAMA, 2000) reviewed 20 randomized trials comparing propofol with midazolam and concluded that: Propofol was at least as effective as midazolam in providing sedation Propofol resulted in a faster time to extubation Propofol was associated with an increased risk of hypotension (although it was unclear if this was clinically significant) There was insufficient data to determine if sedation with propofol decreased ICU length of stay compared to midazolam
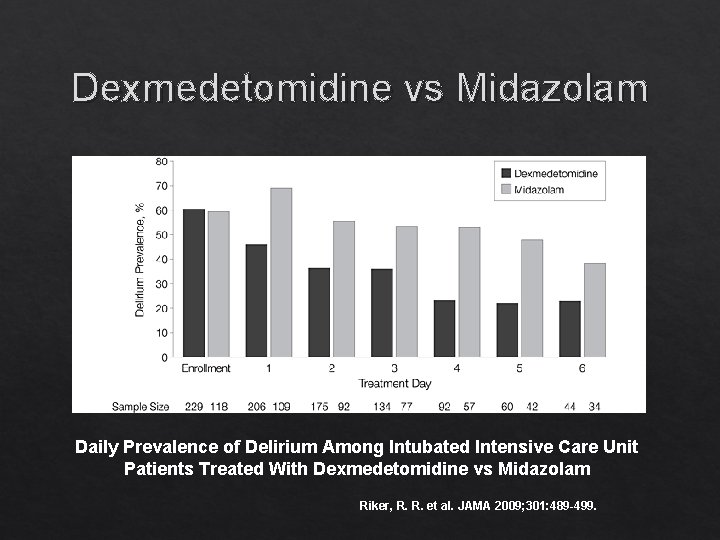
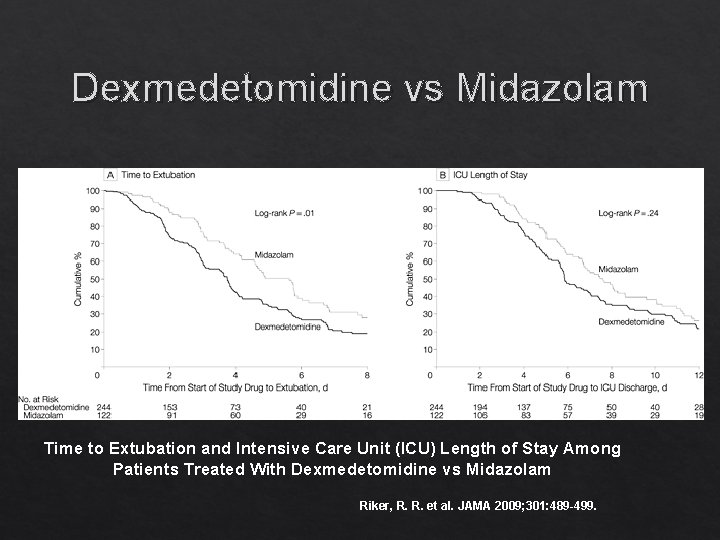
Dexmedetomidine versus Propofol: A randomized trial of 89 postop patients (Corbett, 2005) demonstrated that patients who received dexmedetomidine were less deeply sedated and had a shorter duration of intubation Midazolam: Multicenter randomized trial of 375 patients (Riker, 2009) showed that the dexmedetomidine group had a significantly lower prevalence of delirium and a shorter duration of intubation
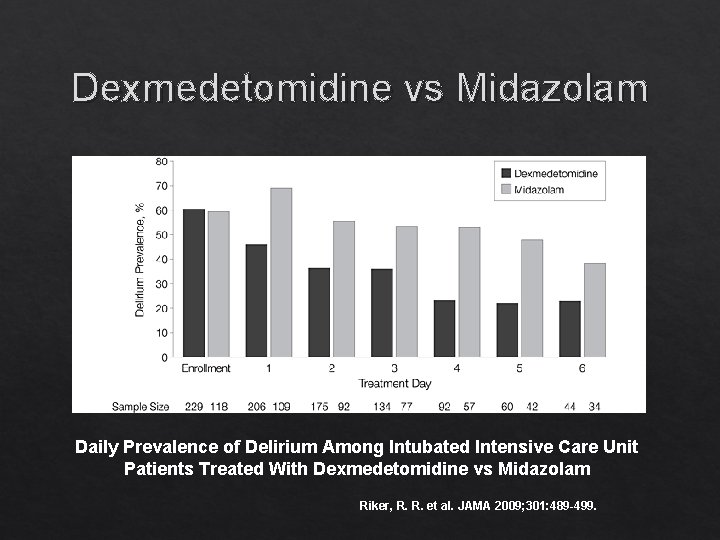
Dexmedetomidine vs Midazolam Daily Prevalence of Delirium Among Intubated Intensive Care Unit Patients Treated With Dexmedetomidine vs Midazolam Riker, R. R. et al. JAMA 2009; 301: 489 -499.
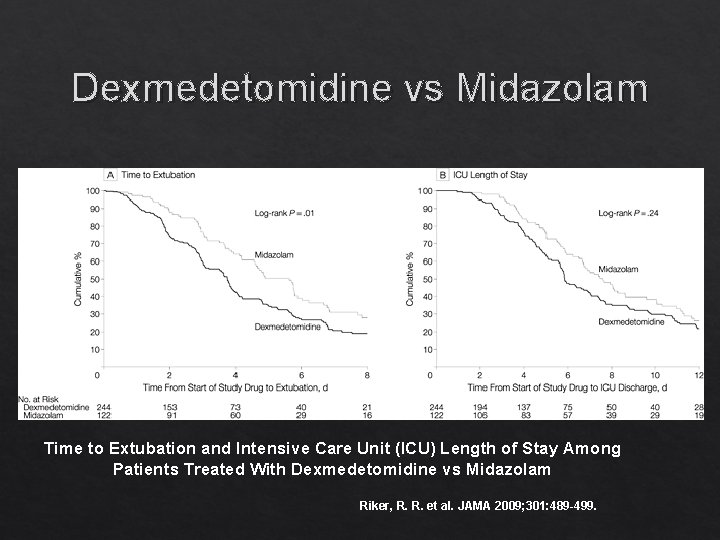
Dexmedetomidine vs Midazolam Time to Extubation and Intensive Care Unit (ICU) Length of Stay Among Patients Treated With Dexmedetomidine vs Midazolam Riker, R. R. et al. JAMA 2009; 301: 489 -499.
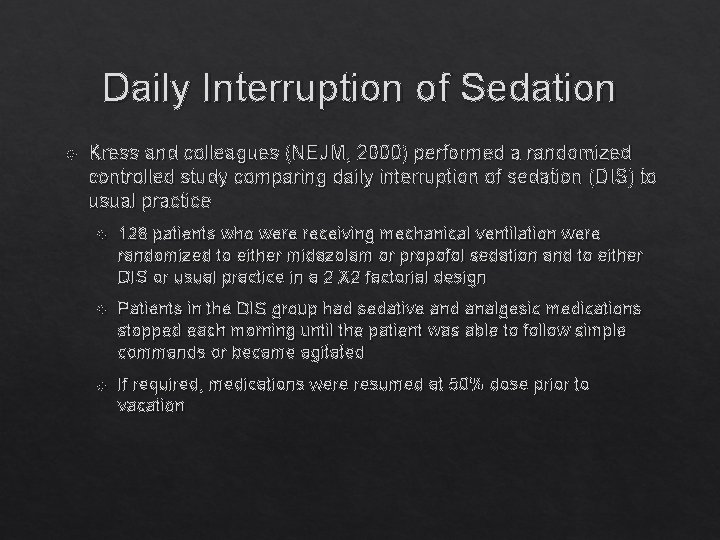
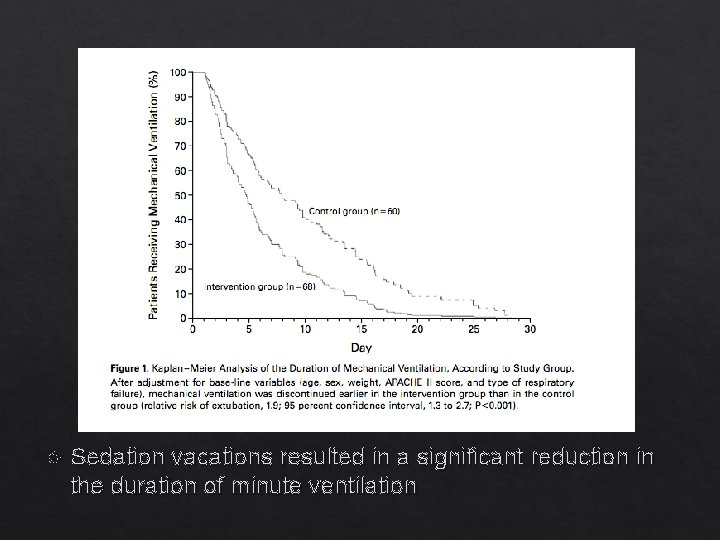
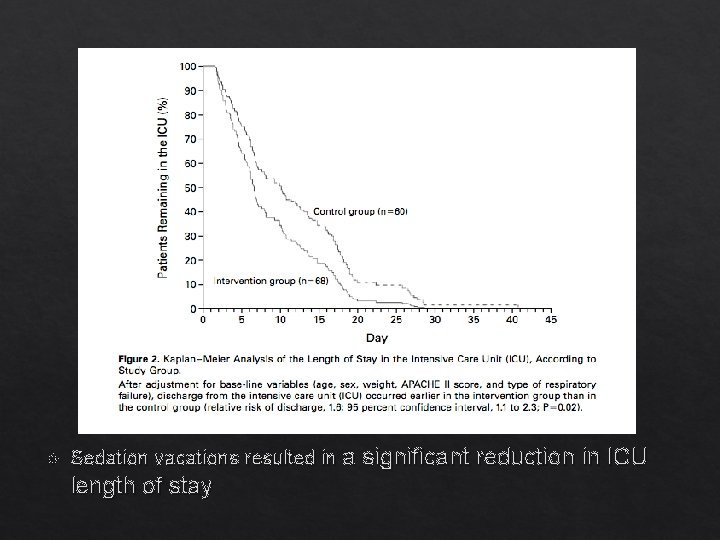
Daily Interruption of Sedation Kress and colleagues (NEJM, 2000) performed a randomized controlled study comparing daily interruption of sedation (DIS) to usual practice 128 patients who were receiving mechanical ventilation were randomized to either midazolam or propofol sedation and to either DIS or usual practice in a 2 X 2 factorial design Patients in the DIS group had sedative and analgesic medications stopped each morning until the patient was able to follow simple commands or became agitated If required, medications were resumed at 50% dose prior to vacation
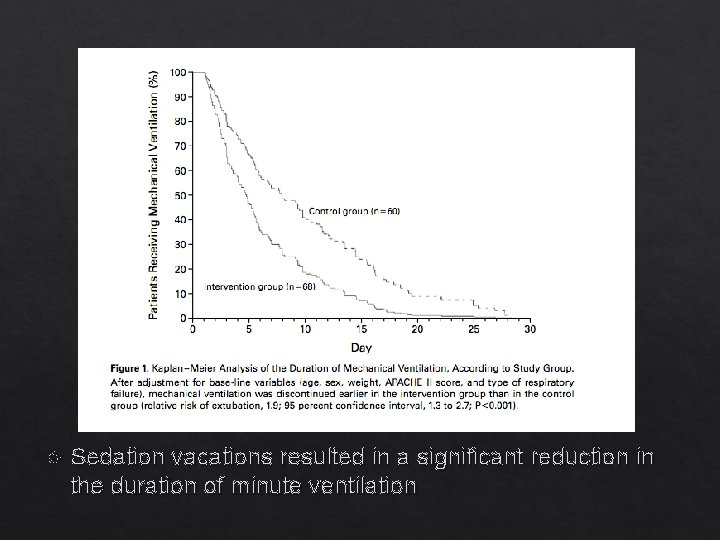
Sedation vacations resulted in a significant reduction in the duration of minute ventilation
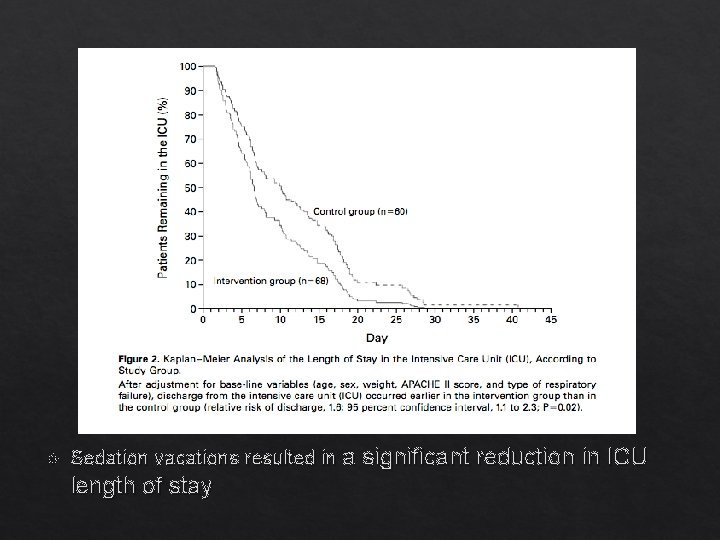
Sedation vacations resulted in a significant reduction in ICU length of stay
Assessment of Delirium Validated tools that screen for delirium Confusion Assessment Method for the ICU (CAM-ICU) Intensive Care Delirium Screening Checklist (ICDSC) Risk increased with Severity of Illness Underlying dementia or alcoholism Coma Benzodiazepines
Treatment of Delirium Prophylaxis No pharmacologic prophylaxis recommended Minimize depth of sedation Non-pharmacologic interventions Frequent re-orientation Early mobilization Maintain sleep-wake cycle Minimize patient care at night Treatment Atypical antipsychotics likely beneficial Transition to dexmedetomidine Non-pharmacologic interventions as above
Take-Home Points Approach in a pain, agitation, delirium algorithm Not every patient requires a sedative Monitor patients with assessment tools Keep patients comfortable while allowing them to remain interactive Avoid benzodiazepines if possible, given their greater association with delirium compared to other agents Incorporate strategies to reduce excessive medication, such as daily sedation vacations
Clinical Case 68 year old female with COPD presented to the emergency department with 3 days of cough, dyspnea and fevers. Over the prior 12 hours, she was acting more somnolent requiring presentation to the emergency department. Temp: 39. 4 HR: 124 BP: 111/73 RR: 28 Sp. O 2: 78% on 6 L. 66 inches. 70 kg. Somnolent and unarousable. Emergently intubated in the ED with propofol and ketamine.
Clinical Question What initial sedation would you choose? A. Fentanyl B. Midazolam C. Propofol D. Dexmedetomidine E. None
Clinical Question What initial sedation would you choose? A. Fentanyl B. Midazolam C. Propofol D. Dexmedetomidine E. None
 Analgesia sistemica
Analgesia sistemica Elastomero morfina effetti collaterali
Elastomero morfina effetti collaterali Poss score medical
Poss score medical Richmond agitation sedation scale
Richmond agitation sedation scale Richmond agitation sedation scale
Richmond agitation sedation scale Over-sedation
Over-sedation Rikers sedation scale
Rikers sedation scale Sédation
Sédation Sccm sedation guidelines
Sccm sedation guidelines Icu layout and design
Icu layout and design Perencanaan kebutuhan tenaga keperawatan
Perencanaan kebutuhan tenaga keperawatan Escala rass
Escala rass Icu localization
Icu localization Icu tersier adalah
Icu tersier adalah Information and communications university zambia
Information and communications university zambia 5hs and 5ts
5hs and 5ts Sean forsythe
Sean forsythe Escala consciencia
Escala consciencia Language
Language Cam icu escala
Cam icu escala Cheetah nicom monitor
Cheetah nicom monitor Abcde methode ehbo
Abcde methode ehbo Intensive care unit definition
Intensive care unit definition Icu orientation
Icu orientation Icu for dummies
Icu for dummies List of lecturers at icu zambia
List of lecturers at icu zambia Patient acuity tool
Patient acuity tool Icu library
Icu library Icu case presentation
Icu case presentation Icu case presentation
Icu case presentation Icu transliterator
Icu transliterator Icu medical b3108
Icu medical b3108 Kp icu jpm
Kp icu jpm Ideal icu setup
Ideal icu setup