Indications of ICU admission and ICU management of
- Slides: 27
Indications of ICU admission and ICU management of critically ill COVID 19 patients DR AVINASH AGRAWAL Prof & HOD Dept. Of critical Care Medicine, King George’s Medical University, UP, Lucknow
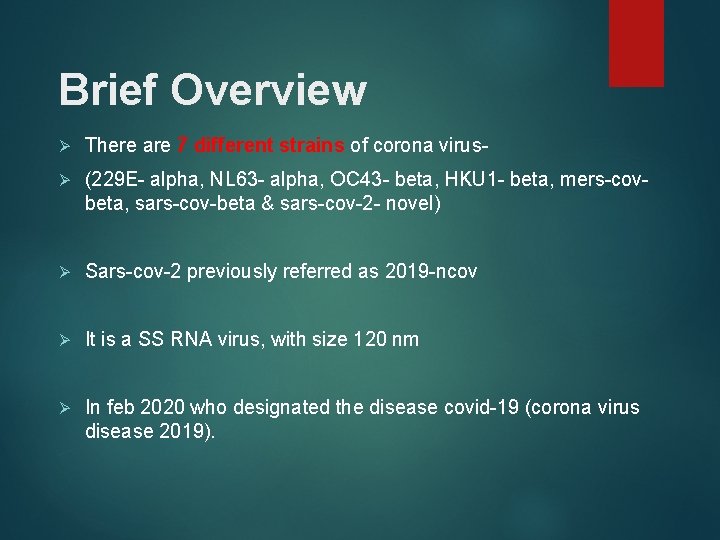
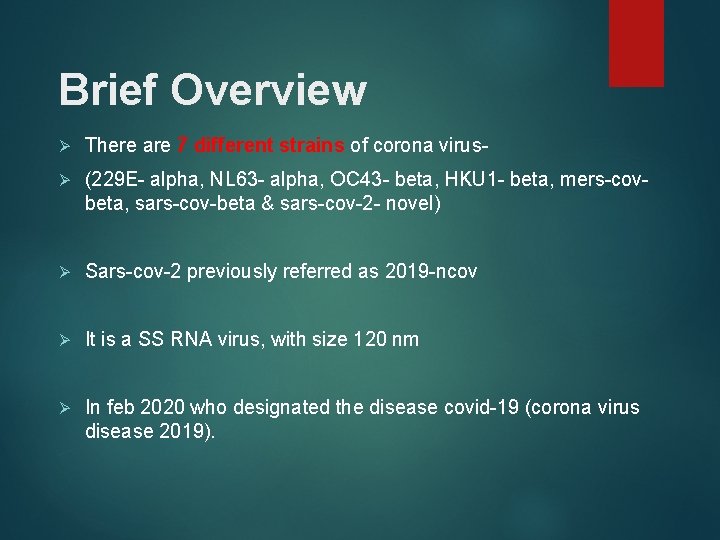
Brief Overview Ø There are 7 different strains of corona virus- Ø (229 E- alpha, NL 63 - alpha, OC 43 - beta, HKU 1 - beta, mers-covbeta, sars-cov-beta & sars-cov-2 - novel) Ø Sars-cov-2 previously referred as 2019 -ncov Ø It is a SS RNA virus, with size 120 nm Ø In feb 2020 who designated the disease covid-19 (corona virus disease 2019).
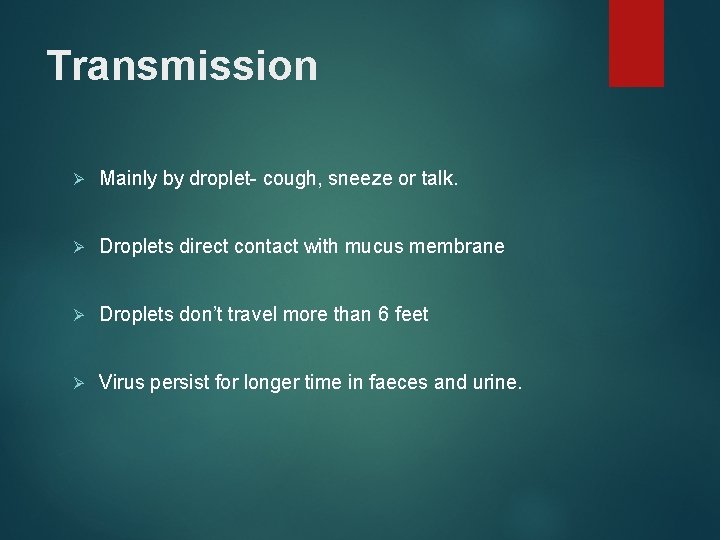
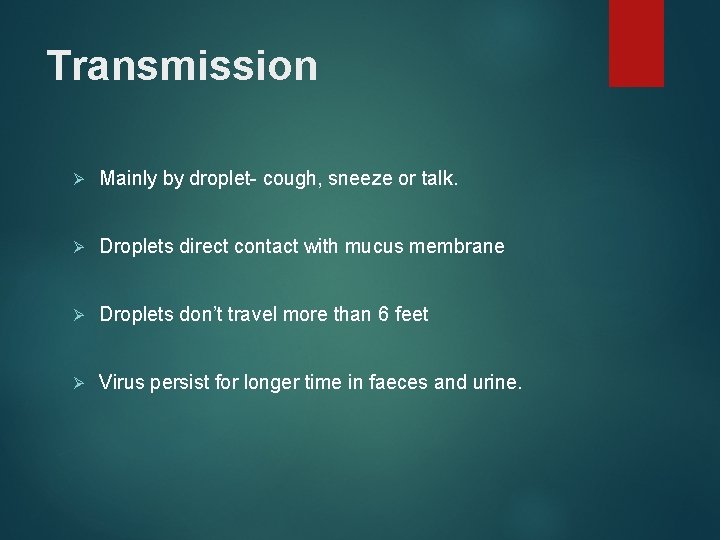
Transmission Ø Mainly by droplet- cough, sneeze or talk. Ø Droplets direct contact with mucus membrane Ø Droplets don’t travel more than 6 feet Ø Virus persist for longer time in faeces and urine.
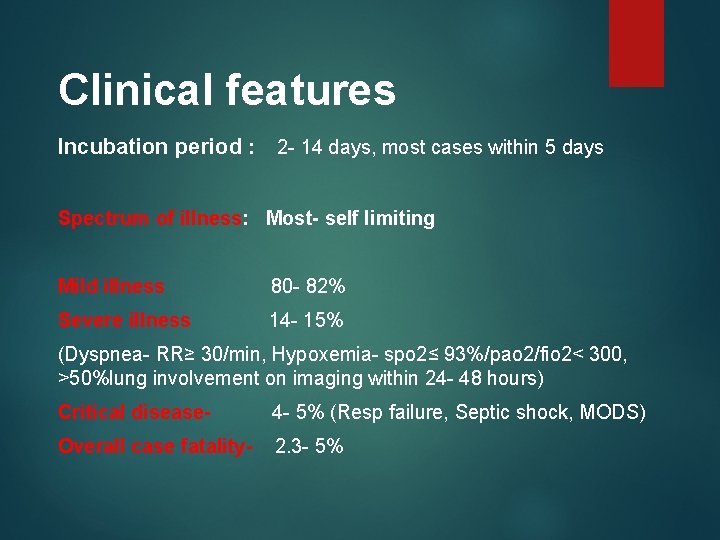
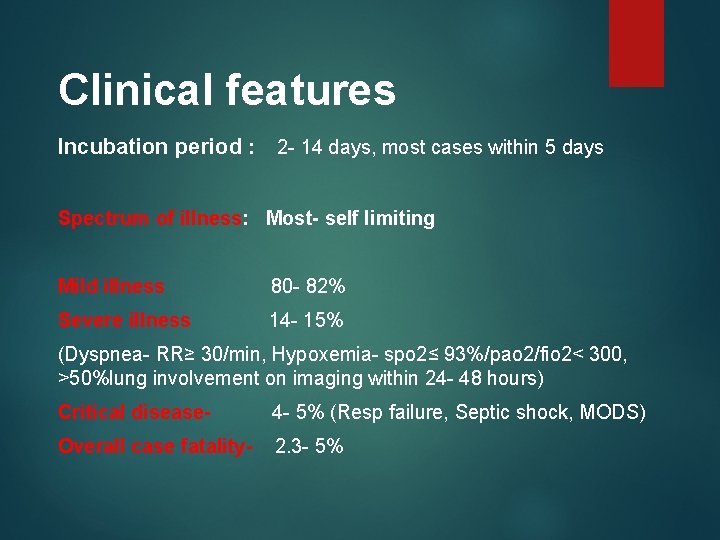
Clinical features Incubation period : 2 - 14 days, most cases within 5 days Spectrum of illness: Most- self limiting Mild illness 80 - 82% Severe illness 14 - 15% (Dyspnea- RR≥ 30/min, Hypoxemia- spo 2≤ 93%/pao 2/fio 2< 300, >50%lung involvement on imaging within 24 - 48 hours) Critical disease- 4 - 5% (Resp failure, Septic shock, MODS) Overall case fatality- 2. 3 - 5%
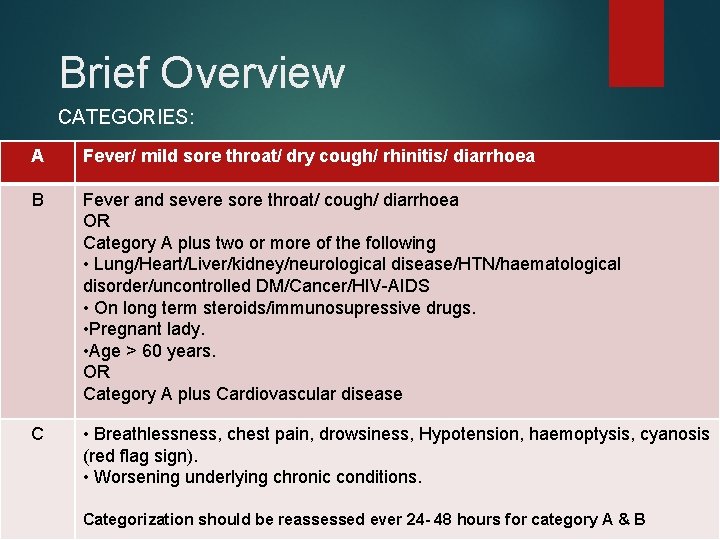
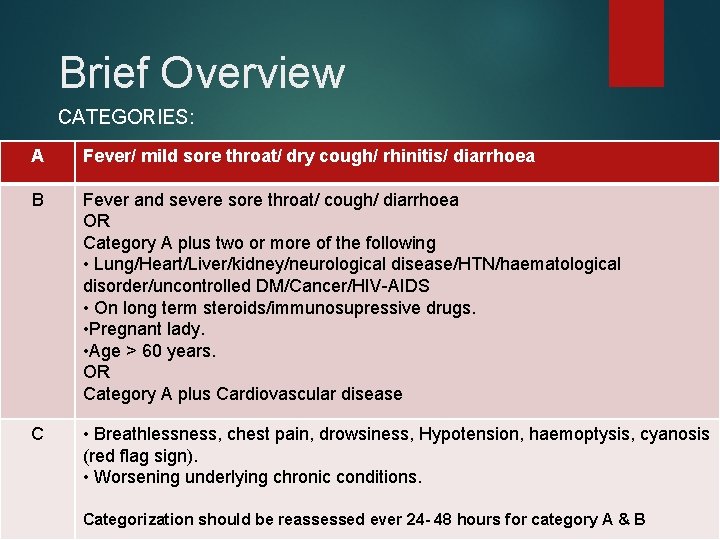
Brief Overview CATEGORIES: A Fever/ mild sore throat/ dry cough/ rhinitis/ diarrhoea B Fever and severe sore throat/ cough/ diarrhoea OR Category A plus two or more of the following • Lung/Heart/Liver/kidney/neurological disease/HTN/haematological disorder/uncontrolled DM/Cancer/HIV-AIDS • On long term steroids/immunosupressive drugs. • Pregnant lady. • Age > 60 years. OR Category A plus Cardiovascular disease C • Breathlessness, chest pain, drowsiness, Hypotension, haemoptysis, cyanosis (red flag sign). • Worsening underlying chronic conditions. Categorization should be reassessed ever 24 - 48 hours for category A & B
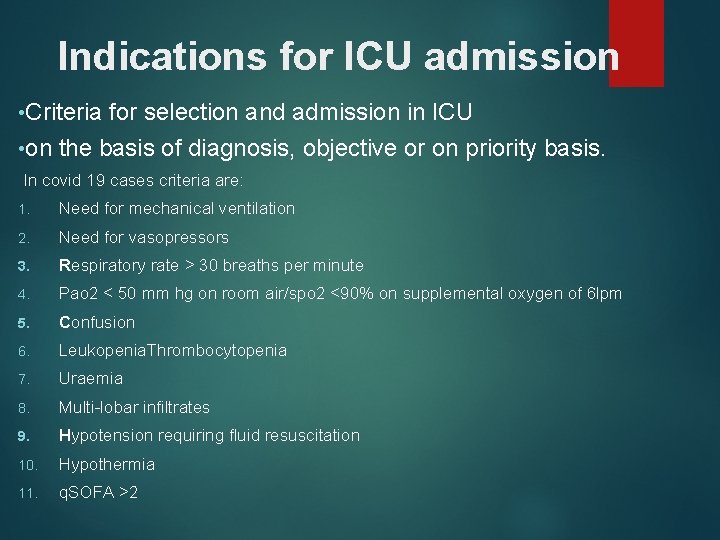
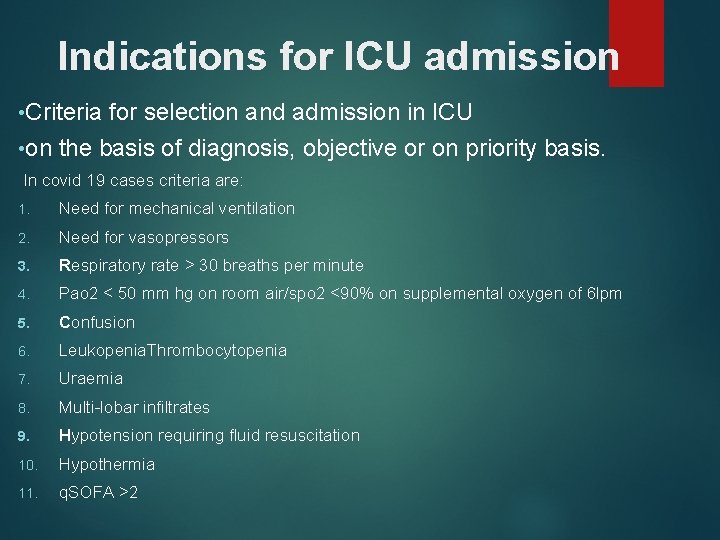
Indications for ICU admission • Criteria for selection and admission in ICU • on the basis of diagnosis, objective or on priority basis. In covid 19 cases criteria are: 1. Need for mechanical ventilation 2. Need for vasopressors 3. Respiratory rate > 30 breaths per minute 4. Pao 2 < 50 mm hg on room air/spo 2 <90% on supplemental oxygen of 6 lpm 5. Confusion 6. Leukopenia. Thrombocytopenia 7. Uraemia 8. Multi-lobar infiltrates 9. Hypotension requiring fluid resuscitation 10. Hypothermia 11. q. SOFA >2
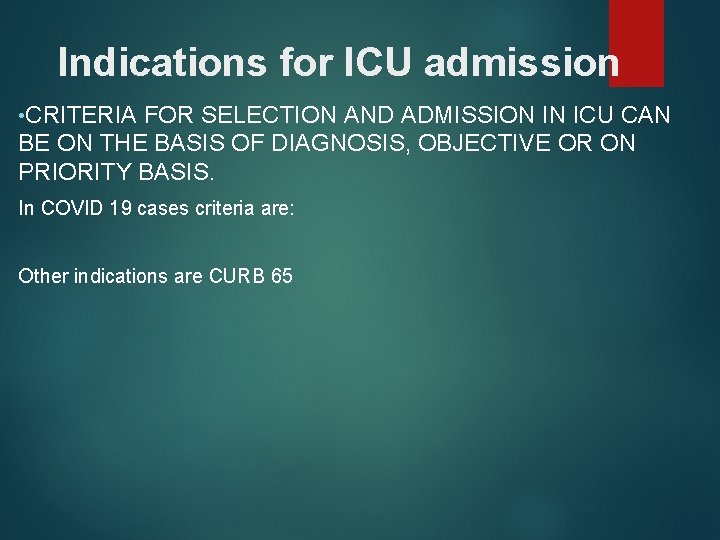
Indications for ICU admission • CRITERIA FOR SELECTION AND ADMISSION IN ICU CAN BE ON THE BASIS OF DIAGNOSIS, OBJECTIVE OR ON PRIORITY BASIS. In COVID 19 cases criteria are: Other indications are CURB 65
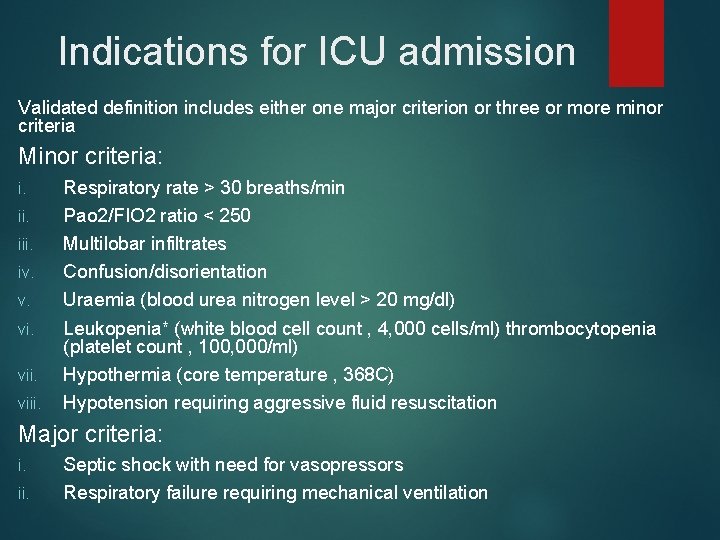
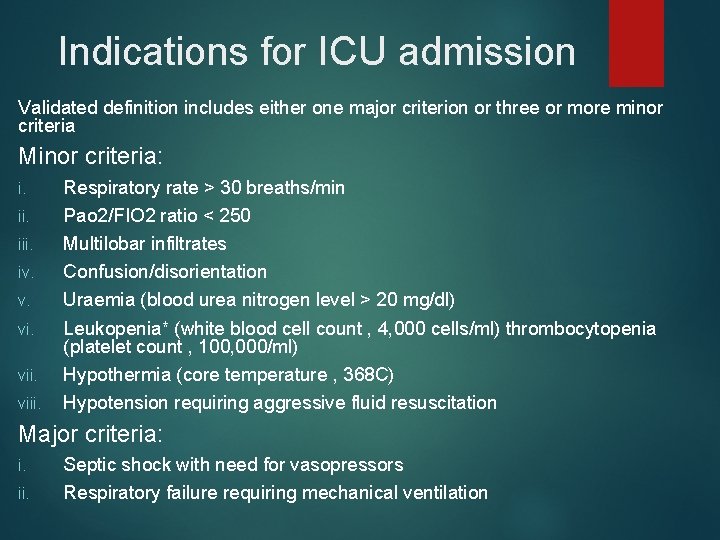
Indications for ICU admission Validated definition includes either one major criterion or three or more minor criteria Minor criteria: i. iii. iv. v. viii. Respiratory rate > 30 breaths/min Pao 2/FIO 2 ratio < 250 Multilobar infiltrates Confusion/disorientation Uraemia (blood urea nitrogen level > 20 mg/dl) Leukopenia* (white blood cell count , 4, 000 cells/ml) thrombocytopenia (platelet count , 100, 000/ml) Hypothermia (core temperature , 368 C) Hypotension requiring aggressive fluid resuscitation Major criteria: i. ii. Septic shock with need for vasopressors Respiratory failure requiring mechanical ventilation
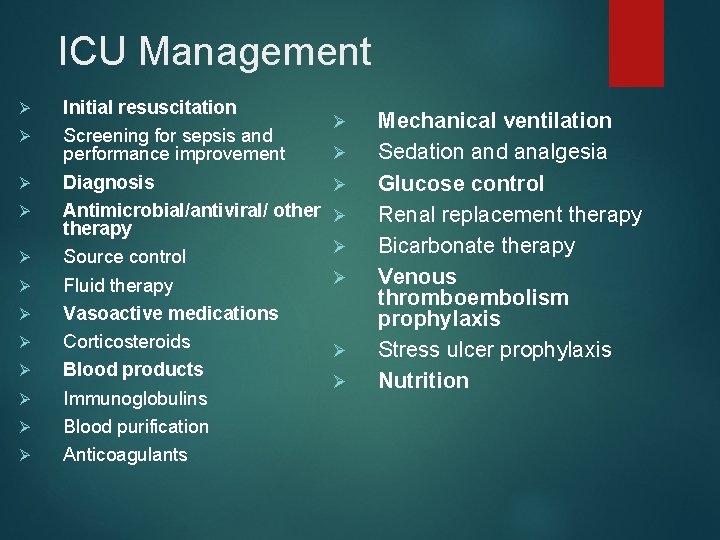
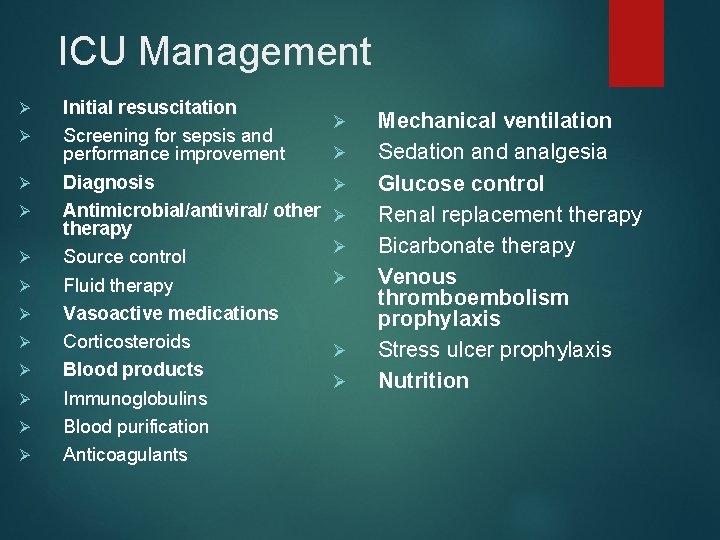
ICU Management Ø Ø Ø Initial resuscitation Screening for sepsis and performance improvement Diagnosis Antimicrobial/antiviral/ otherapy Source control Fluid therapy Vasoactive medications Corticosteroids Blood products Immunoglobulins Blood purification Anticoagulants Ø Ø Ø Ø Mechanical ventilation Sedation and analgesia Glucose control Renal replacement therapy Bicarbonate therapy Venous thromboembolism prophylaxis Stress ulcer prophylaxis Nutrition
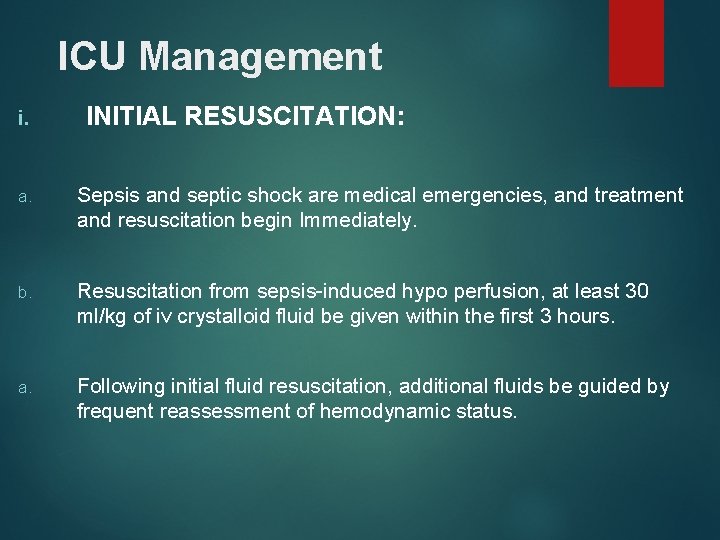
ICU Management i. INITIAL RESUSCITATION: a. Sepsis and septic shock are medical emergencies, and treatment and resuscitation begin Immediately. b. Resuscitation from sepsis-induced hypo perfusion, at least 30 ml/kg of iv crystalloid fluid be given within the first 3 hours. a. Following initial fluid resuscitation, additional fluids be guided by frequent reassessment of hemodynamic status.
a. Further hemodynamic assessment (such as assessing cardiac function) to determine the type of shock if the clinical examination does not lead to a clear diagnosis. a. Dynamic over static variables be used to predict fluid responsiveness, where available. a. Initial target mean arterial pressure of 65 mm hg in patients with septic shock requiring vasopressors. a. Guiding resuscitation to normalize lactate in patients with elevated lactate levels as a marker of tissue hypo perfusion.
ICU Management VII. VASOACTIVE MEDICATIONS: 1. Nor epinephrine as the first-choice vasopressor 2. Vasopressin or Epinephrine to Nor epinephrine with the intent of raising mean arterial pressure to target or decraese dose of noradrenaline 3. dopamine as an alternative vasopressor agent to nor epinephrine only in highly selected patients (e. g. Patients with low risk of tachyarrhythmia and absolute or relative bradycardia). 4. . Against using low-dose dopamine for renal protection.
5. Using dobutamine in patients who show evidence of persistent hypo perfusion despite adequate fluid loading and the use of vasopressor agents 6. All patients requiring vasopressors have an arterial catheter placed as soon as practical if resources are available
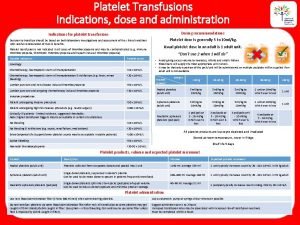
ICU Management IX. BLOOD PRODUCTS: 1. RBC transfusion when Hb decreases to < 7. 0 g/dl in adults except in myocardial ischemia, severe hypoxemia, or acute hemorrhage. 2. Against the use of erythropoietin for treatment of anaemia associated with sepsis. 3. Against the use of fresh frozen plasma to correct clotting abnormalities in the absence of bleeding or planned invasive procedures.
Prophylactic platelet transfusion when counts are < 10, 000/mm 3 (10 × 109/L) in the absence of apparent bleeding When counts are < 20, 000/mm 3 (20 × 109/L) if the patient has a significant risk of bleeding. Higher platelet counts (≥ 50, 000/mm 3 [50 × 109/L]) are advised for active bleeding, surgery, or invasive procedures.
ICU Management XIII. MECHANICAL VENTILATION: Ø Patients on HFNC and NIV should be thoroughly monitored Ø If worsening of respiratory conditions and need of intubation, intubation should not be delayed in such cases Invasive mechanical ventilation Ø Initaite Mechanical ventilationuse using lung protective strategy (tidal volume 48 ml/kg predicted body weight). Ø Plateau pressure goal: ≤ 30 cm h 2 o Ø Check pplat (0. 5 second inspiratory pause), at least every 4 h and after each change in PEEP or VT. Ø If pplat > 30 cm h 2 o: decrease vt by 1 ml/kg steps (minimum = 4 ml/kg). Ø Consider use of incremental fio 2/peep combinations such as shown below to achieve goal
ICU Management XV. GLUCOSE CONTROL: A protocolized approach to blood glucose management in ICU patients with sepsis, commencing insulin dosing when two consecutive blood glucose levels are > 180 mg/ dl Target an upper blood glucose level ≤ 180 mg/dl rather than an upper target blood glucose level ≤ 110 mg/dl. Blood glucose values be monitored every 1 to 2 hours until glucose values and insulin infusion rates are stable, then every 4 hours thereafter in patients receiving insulin infusions. That glucose levels obtained with point-of-care testing of capillary blood be interpreted with caution because such measurements may not accurately estimate arterial blood or plasma glucose values. Use of arterial blood rather than capillary blood for point-of-care testing using glucose meters if patients have arterial catheters.
ICU Management XVIII. VENOUS THROMBOEMBOLISM PROPHYLAXIS : Pharmacologic prophylaxis against venous thromboembolism (VTE) in the Absence contraindications to the use of these agents LMWH rather than UFH for VTE prophylaxis In the absence of contraindications to the use of LMWH Combination pharmacologic VTE prophylaxis And mechanical prophylaxis, whenever possible Mechanical VTE prophylaxis when pharmacologic VTE is contraindicated.
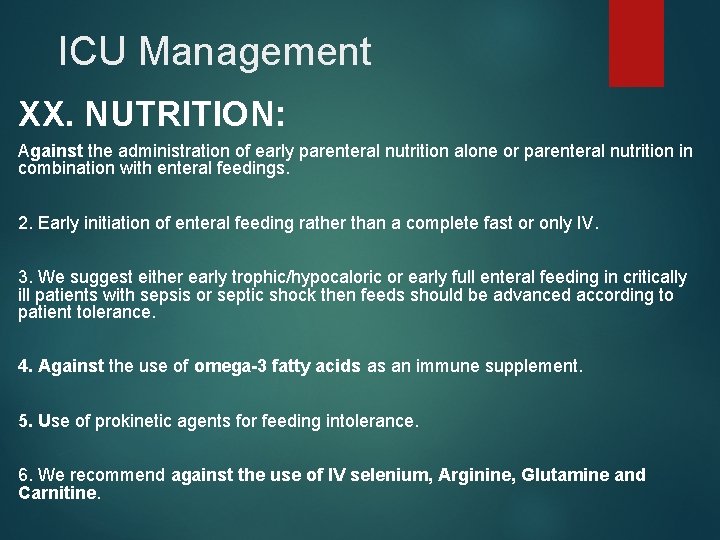
ICU Management XX. NUTRITION: Against the administration of early parenteral nutrition alone or parenteral nutrition in combination with enteral feedings. 2. Early initiation of enteral feeding rather than a complete fast or only IV. 3. We suggest either early trophic/hypocaloric or early full enteral feeding in critically ill patients with sepsis or septic shock then feeds should be advanced according to patient tolerance. 4. Against the use of omega-3 fatty acids as an immune supplement. 5. Use of prokinetic agents for feeding intolerance. 6. We recommend against the use of IV selenium, Arginine, Glutamine and Carnitine.
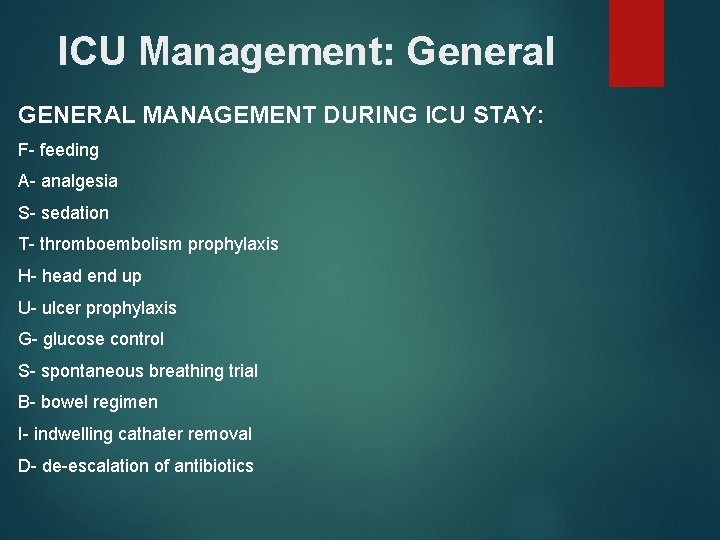
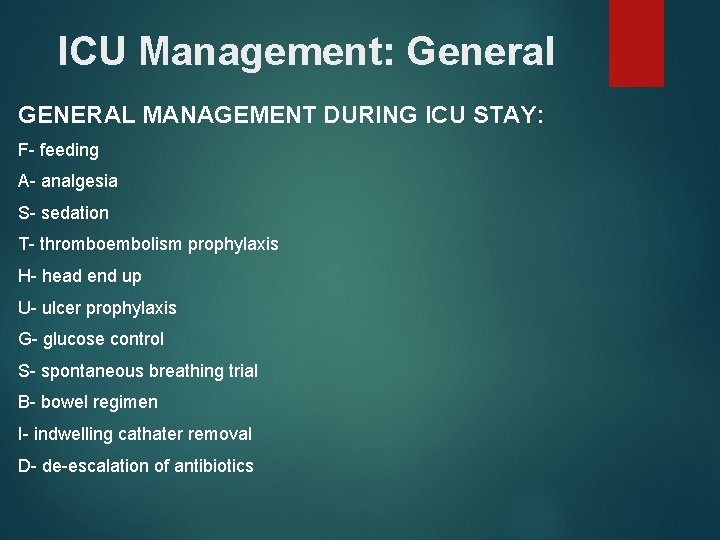
ICU Management: General GENERAL MANAGEMENT DURING ICU STAY: F- feeding A- analgesia S- sedation T- thromboembolism prophylaxis H- head end up U- ulcer prophylaxis G- glucose control S- spontaneous breathing trial B- bowel regimen I- indwelling cathater removal D- de-escalation of antibiotics
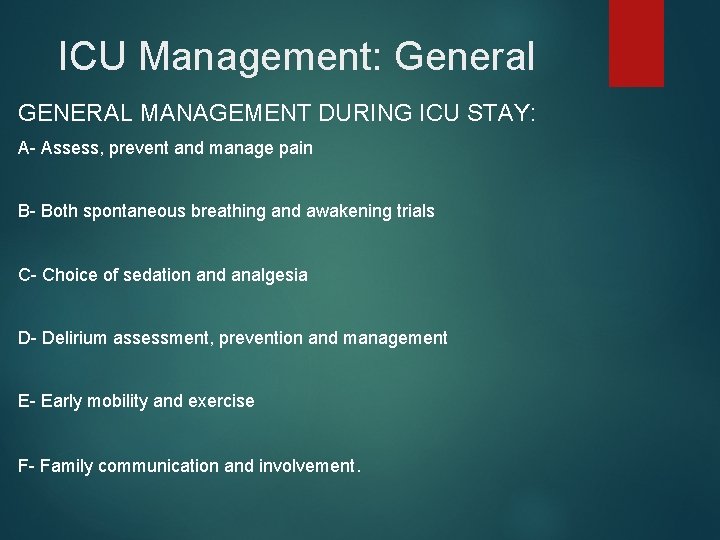
ICU Management: General GENERAL MANAGEMENT DURING ICU STAY: A- Assess, prevent and manage pain B- Both spontaneous breathing and awakening trials C- Choice of sedation and analgesia D- Delirium assessment, prevention and management E- Early mobility and exercise F- Family communication and involvement.
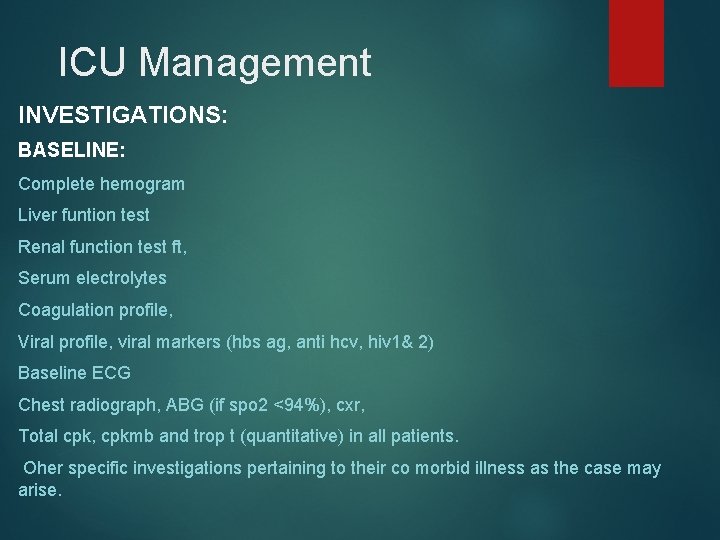
ICU Management INVESTIGATIONS: BASELINE: Complete hemogram Liver funtion test Renal function test ft, Serum electrolytes Coagulation profile, Viral profile, viral markers (hbs ag, anti hcv, hiv 1& 2) Baseline ECG Chest radiograph, ABG (if spo 2 <94%), cxr, Total cpk, cpkmb and trop t (quantitative) in all patients. Oher specific investigations pertaining to their co morbid illness as the case may arise.
ICU Management RISK FACTORS AND PROGNOSTIC DETERMINANTS: History of co morbidities (Htn, DM, COPD, Asthma, Hemato-lymphoid cancer, Solid organ cancer, CLD, CKD, CHF, IHD, Stroke, Dementia etc. ). • Higher body temperatures were associated with more severe disease and higher fatality. • In the wuhan cohort, the following laboratory cut offs appeared to indicate a poor prognosis • lymphopenia < 2000/cu. mm • Neutrophil / lymphocyte ratio >2 • LDH > 245 u/l • hs-cardiac troponin > 28 ng/ml • Prothrombin time > 16 s • Serum ferritin > 300 μg/l • D dimer •
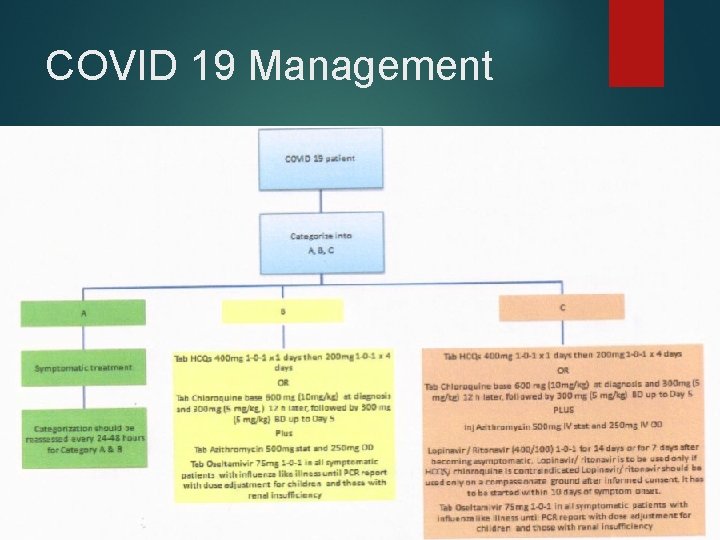
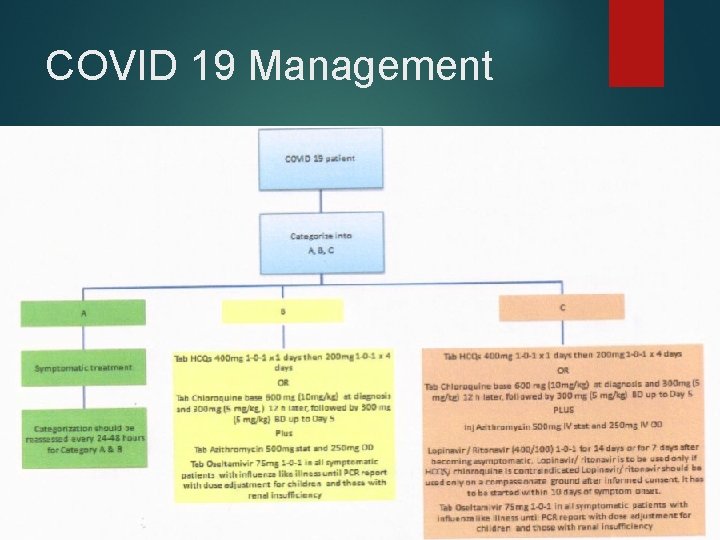
COVID 19 Management
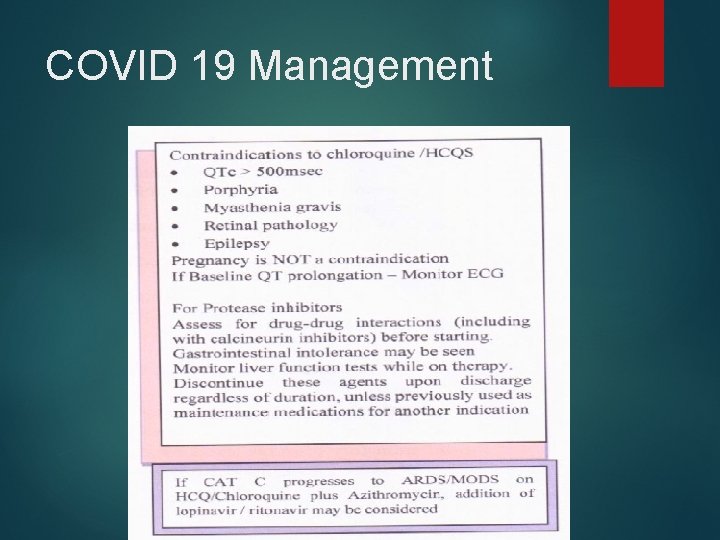
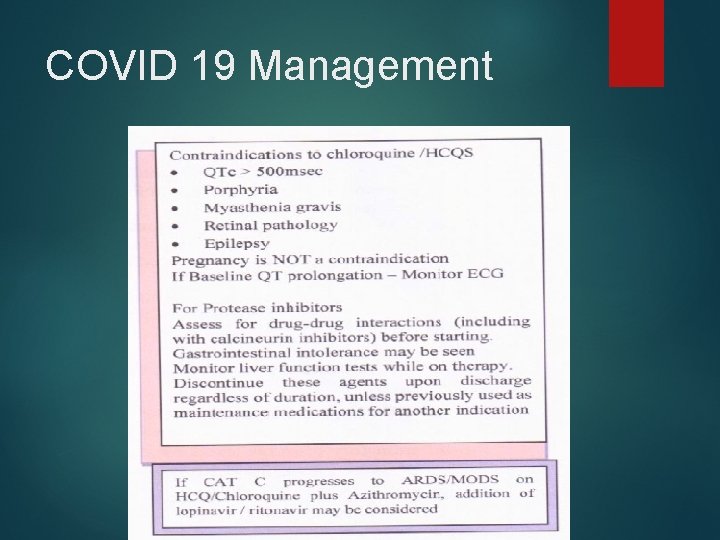
COVID 19 Management
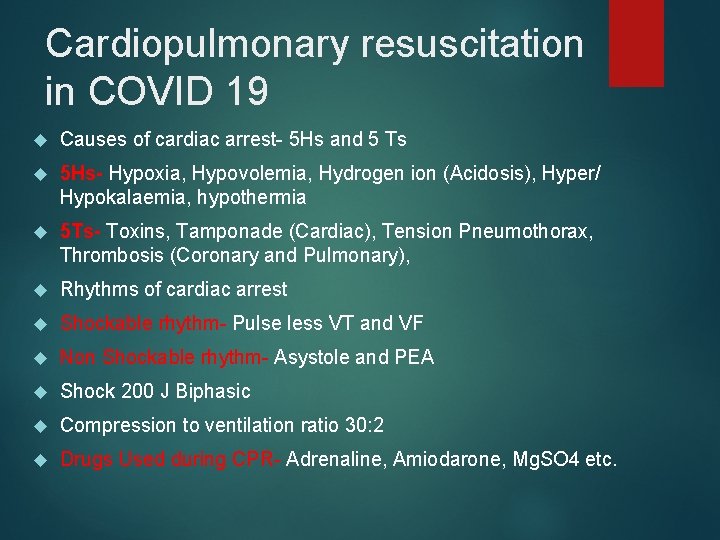
Cardiopulmonary resuscitation in COVID 19 Causes of cardiac arrest- 5 Hs and 5 Ts 5 Hs- Hypoxia, Hypovolemia, Hydrogen ion (Acidosis), Hyper/ Hypokalaemia, hypothermia 5 Ts- Toxins, Tamponade (Cardiac), Tension Pneumothorax, Thrombosis (Coronary and Pulmonary), Rhythms of cardiac arrest Shockable rhythm- Pulse less VT and VF Non Shockable rhythm- Asystole and PEA Shock 200 J Biphasic Compression to ventilation ratio 30: 2 Drugs Used during CPR- Adrenaline, Amiodarone, Mg. SO 4 etc.
References: COVID 19 Guidelines- WHO COVID 19 Guidelines- Position statement ISCCM COVID 19 Guidelines- International Pulmonologist’s Concensus COVID 19 Guidelines- Government of Kerala Surviving Sepsis Campaign 2016 guidelines
 Icu layout and design
Icu layout and design Dental sealant definition
Dental sealant definition Rumus depkes menghitung tenaga perawat
Rumus depkes menghitung tenaga perawat Escala de sedacion agitacion sas
Escala de sedacion agitacion sas Icu localization
Icu localization Icu primer sekunder tersier
Icu primer sekunder tersier Emphancy
Emphancy 5hs and 5ts
5hs and 5ts Sean forsythe
Sean forsythe Cam icu escala
Cam icu escala Cam icu
Cam icu Cam icu escala
Cam icu escala Cheetah challenge icu
Cheetah challenge icu Abcde methode ehbo
Abcde methode ehbo Concept of intensive care unit
Concept of intensive care unit Icu orientation
Icu orientation Icu for dummies
Icu for dummies Information and communications university
Information and communications university Patient acuity tool
Patient acuity tool Icu library
Icu library Icu case presentation
Icu case presentation Icu case presentation
Icu case presentation Icu transliterator
Icu transliterator Icu medical b3108
Icu medical b3108 Kp icu jpm
Kp icu jpm Alaeg
Alaeg Chatecholamine
Chatecholamine Shanks algorithm example
Shanks algorithm example