Admission procedures Dr F Mostajeran MD Admission procedures





















- Slides: 65


Admission procedures Dr. F Mostajeran MD
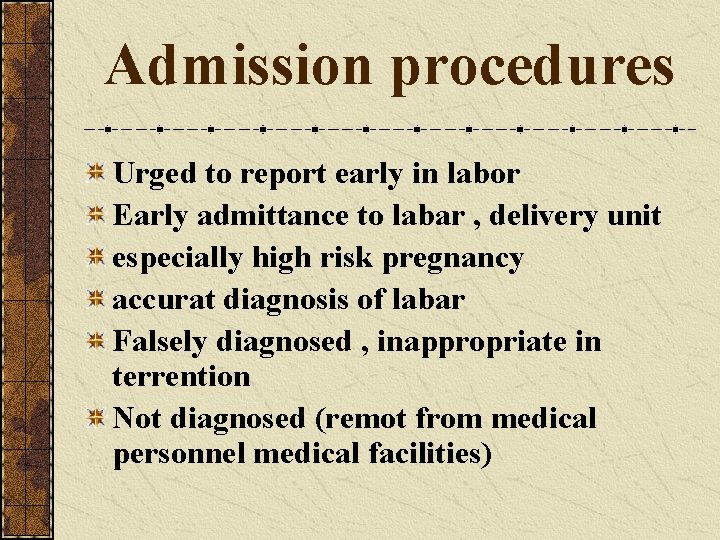
Admission procedures Urged to report early in labor Early admittance to labar , delivery unit especially high risk pregnancy accurat diagnosis of labar Falsely diagnosed , inappropriate in terrention Not diagnosed (remot from medical personnel medical facilities)
Definition of labor Uterine contractions that bring effacement and dilatation of cervix. Painful contractions become regular onset of labor as beginning at the time of admission to the labor unit Admission for labor based on dilatations accompanied by painful contractions.
D. Diagnasis between false and true labor is difficult Contractions of true labor Regular intervals Intervals gradually shorten Intensity gradually increases Discomfort back , abdomen Cervix dilates Discomfort is not stopped by sedation
Contractions of false labor Irregular intervals Intervals long Intensity unchanged Discomfort lawer abdomen Cervix not dilate Relieved by sedation

Pregnant woman who is having Cantractions Emergency condition Labor is defined as process of childbirth beginning Latent phase delivery placenta
Electronic admission testing Recommend NST or CST on all patient (labar – delivery unit) Fetal admission test identify unsuspected cases
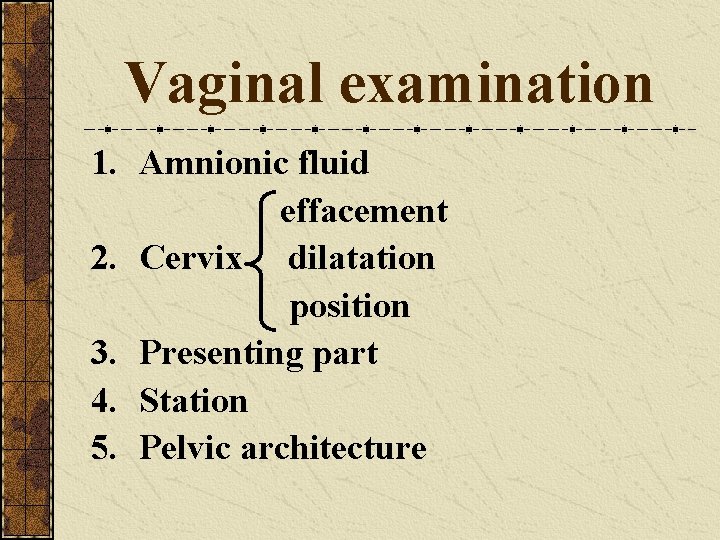
Vaginal examination 1. Amnionic fluid effacement 2. Cervix dilatation position 3. Presenting part 4. Station 5. Pelvic architecture
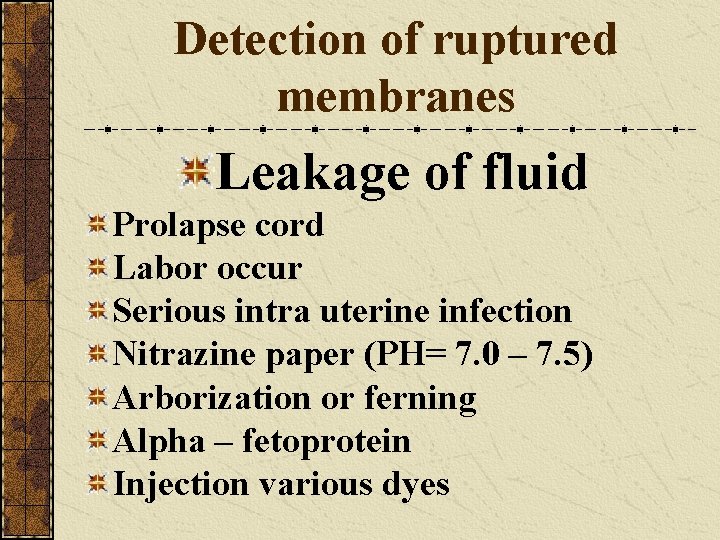
Detection of ruptured membranes Leakage of fluid Prolapse cord Labor occur Serious intra uterine infection Nitrazine paper (PH= 7. 0 – 7. 5) Arborization or ferning Alpha – fetoprotein Injection various dyes

Vital signs and review of pregnancy record Physical examination Preparation of vulva and perineum Inspection and cleaning of the vulva , perineum , mini – shave - enema
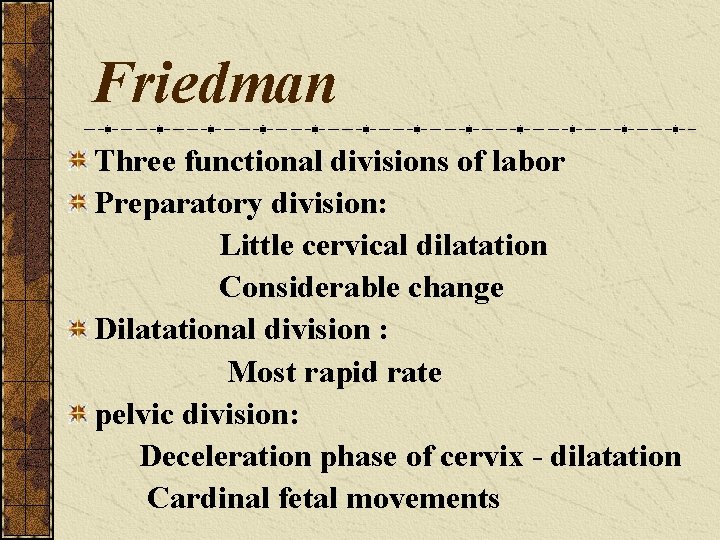
Friedman Three functional divisions of labor Preparatory division: Little cervical dilatation Considerable change Dilatational division : Most rapid rate pelvic division: Deceleration phase of cervix - dilatation Cardinal fetal movements
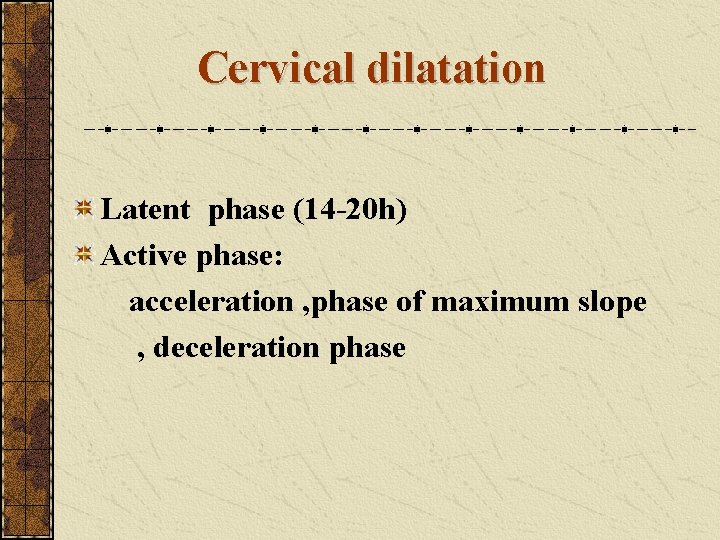
Cervical dilatation Latent phase (14 -20 h) Active phase: acceleration , phase of maximum slope , deceleration phase


Management first stage of labor Remainder of general physical exam is completed HCT HB protein - glocose average duration first stage of labor 7 hours in nulliparous w 4 hours in parous w

Fetal monitoring during labar Contractions and response FH Suitable stethoscopc , doppler ultrasonic devices FH should be checked after contractions every 30 minutes (15) Second stage every 15 minutes (5) Cantinous electronic monitoring
MATERNAL MONITORING Vital signs T , pulse , BP every 4/h PROM temprature every 1/h 18 h of PROM antimicrobial
Subsequent vaginal examinations When membrans rupture if head was not Defenetly engaged fetal H immediately and during the next uterine contraction (occult umbilical cord compression) periodic examinations at 2 -3 hours interval

Oral intake Gastric emptying time prolanged (food – medication remain in the stomach – not absorbed may be vomited) Food should be withheld Intravenous fluids Infusion system routine early labar (IV line) Longer labors glucose sodium water 60 -120 ml/hr

Maternal position during labor normal laboring woman Not be confined to bed Comfortable chair In bed position most comfortabl (lateral recumbend)

Analgesia Is initiated on the basis of maternal discomfort vaginal examination befor administration of analgesia (delivering a depressed infant) Timing , method and size of initial and subsequent dose , interval of time until delivery
Amniotomy There is a great temptation Benefits: rapid labor detection of meconium staining Internal fetal M Aseptic technique Head must be well applied to the cerxin
Urinary bladder function Bladder distention avoid Abstracted labor Subsequent bladdes hypotonia, infection Suprapubic region shauld be visualized , palpated detect filling bladder If could not void on a bedpan Intermittent catheterization
Management of second stage labor Full dilatation of the cervix Begins to bear dawn 50 minutos in nulliparous 20 minutos in multiparous
Higher parity 2 -3 expulsive efforts may suffice Complete the delivery of the infant FHR Low – risk 15 H. risk 5
Fetal H. R Contraction – maternal expulsive efforts FHR are not consequence of head compression Descent fetus and reduction in uterine volume some degree of premature separation placenta

tighten a loop or loops of umbilical cord Around the fetus umbilical blood flow Prolonged uninterrupted maternal expulsive efforts dangerous to the fetus
Preparation for delivery Variety of positions Dorsal lithotomy position For beter exposure legholders stirrups Cramps in the legs (brief massage – changing position) Preparation for delivery entails vulvar and perineal cleansing
Spontaneous delivery Delivery of the head Contraction perineum bulges Vulvovaginal opening becomes more dilated Gradually circular opening This encirclement of the largest head By the vulvar ring is known as crowning
Perineum is extremely thin Episiotomy , laceration Episiotomy risk tear external anal – rectum Episiotomy - anterior tear urethra , labia
Ritgen manover Vaginal introitus 5 cm Towel – draped , gloved hand forward pressure on the chin of the fetus other hand exerts pressure superiorly against occiput
Cleaning the nasopharynx Minimize aspiration AF – debris , blood once thorax is delivered face quickly wiped nause , mouth are aspirated
Following delivery of anterior shoulder Finger should be passed to the neck Nuchal cords 25% + Drawn down , loose – slipped over the head Clamping the cord 4 -5 cm , 2 -3 cm fetal abdomen two clamps Plastic cord clamp

Timing of cord clamping Infant is placed at or below vaginal interoitus 3 , 80 ml of blood shifted from placenta to infant 80 ml 50 mg Iron , Iron deficiency anemia Maternal alloimmunization our policy after cleaning airway 30" cord clamp
Management of the third stage After delivery of the infant Height uterine fundus Uterus firm , no unusual bleeding Waiting until placentac separat – no massage Hand rest on the fundus (atonic – filled with blood)
Signs of placental separation 1. uterus becames globular firm 2. Sudden gush of blood 3. Uterus rises (placenta separated , passes dawn to lower u-segment 4. Its balk pushes uterus upward 5. Umbilical cord protrudes forther out

delivery of the placenta Traction on the umbilical cord must not be used inversion Manaol removal of placenta occasionally placenta will not separat At any time brisk bleeding and , placenta can not be delivered Active management of the third stage 5 units oxytocin +0. 5 ergometrine reductian in the length of third stage
Fourth stage of labor Exam placenta , membranes , umbilical cord Completeness , anomalies Hour immediately fallowing delivery Critical fourth stage of labor uterine atony , BP , pulse every 15
Oxytocic Agents Oxytocin (pitocin , syntocinon) Methylergo novine maleat (methergine) Reduce blood loss by stimuloting myometrial contraction Iml 10 IU half – lifc IV 3 Inapropriate dose kill the fetus , rupture uterus
Cardiovascular effects Deleterious effects follow IV bolus Antidiuresis rare maternal convulsion antidiuretic action Water intoxication (20, 40 mu/minut ) Concentration should be increared rather than rate of flow Normal saline are lactated ringer solution
Ergonovine and methylergonavine IV – IM – orally no differenc in actions Sensitivity of pregnant uterus is very great In pregnancy 0. 1 my IV , 0. 25 my oral tetanic Uterine contraction Tetanic effect prerention , control PPH IV administration sometimes tram sient , severe hypertension
Prostaglandins Not used routinely Manage ment PPH PG F 2 x 250 ng IM (15 -90" ) 8 does 88% successful 20% side effects diarrhea , hypertension vomiting , Fever , flushing , tachycandia PG E 2 20 -mg suppositories
Lacerat ons of the Birth canal Classified First fourchette , perineal skin vaginal mucous Second fascia and muscles of perineal body Third anal sphincter Fourth retal mucosa
Episiotomy and repair Incision of pudenda Perineotomy incision of perineu Episiotamy synonymously with penineotomy Begin in midline : Directed laterally mediolateral Directed down ward midline
Timing of episiotomy Perform when head is visible during contraction 3 -4 After application of blades Timing of repair Most common practice repair until placenta delivered Technique Hemostasis Anatomical restoration without excessive suturing Chromic catgut 3 -0
Fourth – degree laceration Various techniques remcommend Esential approximat torn edges rectal mucosa With muscularis sutures 0. 5 cm apart Muscular layer covered with a layer of fascia

Labor with occiput presentations 95% fetus occiput or vertex presentation Most commonly ascertained ab – exam Confirmed V. Examination before or at the onset of labor Sagitlal suture in the transrevse pelvic diameter LOT , ROT , LOA , ROA ROP , LOP (narrow forepelvis , anterior placentation


OCCCIPUT ANTERIOR PRESENTATION Irregular shape pelvic canal Large dimensions fetal head Adoptation or accommodation of suitable Portions of head to the varius segment of the pelvis is required
Cardinal movements of labar Engagement Descent Flexion Internal rotation Extension External rotation expulsion
Concomitantly , uterine cantractions Important modifications in fetal attitude straightening of the fetus loss dorsal convexity , closer application of the extremities to the body , fetal ovoid cylinder

Engagement Biparietal diameter – greatest transverse diameter F. Head passes thraugh the pelvic inlet Lost few weeks of pregnancy Until after cammencement of labor In many multiparous , some nulliparous At onset of labor head freely movable above inlet Referred “floating”
Asynclitism Sagittal suture remaining parallel to transverse axis may not lie exactly midway Between symphysis and sacral promontory Sagitlal suture deflected posteriorly or anteriorly
Asynclitism anteror or posterior Moderat degree of asynclitism are the rule in normal labor Severe asynclitism may lead to cephalopelvic disproportion even with an normal – sized pelvis
DESCENT First requisit for birth infant In nulli parus take place befor the onset of labor Further descent until onset of the second stage In multiparous descent usually begins with engagement

1. 2. 3. 4. Descent is brought by one or more of four forces Pressure of amnionic fluid Direct pressure of fondus with cont ractions Bearing down efforts abdominal muscles Extension and straightening of fetal body
FLEXION As soon as descending head meets resistance Cervix , walls of the pelvis , pelvic floor The chin is braught into more intimate contact Fetal thorox suboccipitobreg matic occipitafrontal
Internal rotation occiput gradually moves from original position toward symphysis pubis Less commonly posteriorly Internal rotation essential completion of labor It always associated with descent and acomplished after engagement
Extension After in-rotation sharply flexed head reaches the vulva Undergoes extension which essential to birth Vulvar outlet directed upward , for ward Extension must occur before head can pass through it

Head born by further extension occiput , bregma , fore head , nose mouth Finally chin pass Head drops down ward chin lies over anal region

External rotation delivered head under goes restitution occiput toward the left rotates left ischial tuberosity occiput toward the right rotates right ischial tuberosity Bisacromial diameter in to relation anteroposterior diameter of the pelbic outlet shoulders (anteriar – posterior)
Expulsion Immediatly after external rotation Anterior shoulder under symphysis pubis Posterior shoulder distended perineum After delivery of the shoulders Rest of body quickly extruded

 Admission bed making procedure
Admission bed making procedure Admission enquiry letter
Admission enquiry letter Kgs admission
Kgs admission Mednax baby steps
Mednax baby steps Norton scale
Norton scale Admission transfer discharge and physical exams
Admission transfer discharge and physical exams Ung dual enrollment deadline
Ung dual enrollment deadline Fort wayne zoo admission
Fort wayne zoo admission Intake-admission interview
Intake-admission interview Kgs nursery admission
Kgs nursery admission Poly u e admission
Poly u e admission Ucla nursing application
Ucla nursing application Uway apply
Uway apply Plmar vision and mission
Plmar vision and mission Uci admissions office
Uci admissions office Temple university ielp
Temple university ielp Suny canton vet tech
Suny canton vet tech Chapter 11 admission transfer and discharge
Chapter 11 admission transfer and discharge Joint admission portal
Joint admission portal Chapter 11 admission transfer and discharge
Chapter 11 admission transfer and discharge Chattahoochee tech gpa requirements
Chattahoochee tech gpa requirements Www.parcoursup.fr gestion
Www.parcoursup.fr gestion Usf admission portal
Usf admission portal Tarrant county college admission requirements
Tarrant county college admission requirements Purpose of admission in hospital
Purpose of admission in hospital Hajee karutha rowther howdia college admission
Hajee karutha rowther howdia college admission Esireims
Esireims Nacac admission trends survey
Nacac admission trends survey Ucla gpa requirements
Ucla gpa requirements Admission maastricht university
Admission maastricht university Hospital environment for sick child
Hospital environment for sick child Admission by investment
Admission by investment Denmark admission
Denmark admission Nursing ubc
Nursing ubc Admission control
Admission control Adcvandismal
Adcvandismal Admission under reception order
Admission under reception order Swing bed admission checklist
Swing bed admission checklist Direct school admission
Direct school admission Sfu admission
Sfu admission Admission guide 2019-2020
Admission guide 2019-2020 Ncku international student
Ncku international student Chapter 9 admission transfer discharge and physical exams
Chapter 9 admission transfer discharge and physical exams Classroom procedures and expectations
Classroom procedures and expectations Substantive procedures
Substantive procedures Safe rigging
Safe rigging Telephone answering procedures
Telephone answering procedures Analytical procedures examples
Analytical procedures examples Lending policies and procedures managing credit risk
Lending policies and procedures managing credit risk Functional check flight procedures
Functional check flight procedures Antecedent control procedures
Antecedent control procedures Isa 315 changes
Isa 315 changes Computer aided medical procedures
Computer aided medical procedures 1. 13-1 work together, p. 381
1. 13-1 work together, p. 381 Hold procedure
Hold procedure The office procedures and technology
The office procedures and technology Chapter 47 laboratory materials and procedures
Chapter 47 laboratory materials and procedures Frame rail sectioning procedures
Frame rail sectioning procedures Skl comsec
Skl comsec Exploratory research quantitative
Exploratory research quantitative Gwisnet
Gwisnet Types of analytical procedures
Types of analytical procedures Biochemical data, medical tests, and procedures (bd)
Biochemical data, medical tests, and procedures (bd) Rnav procedures
Rnav procedures Investigation procedures
Investigation procedures Safe lab procedures
Safe lab procedures