RENAL DISEASE AND KIDNEY TRANSPLANTATION Dr Masood Entezari




- Slides: 63

RENAL DISEASE AND KIDNEY TRANSPLANTATION Dr Masood Entezari Asl
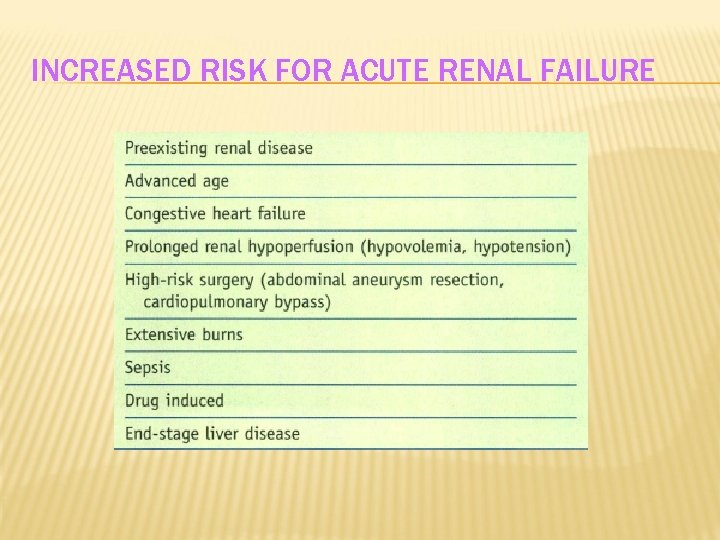
RENAL DISEASE The kidney has an important role in the excretion of all xenobiotics and is crucial in adjusting the composition and volume of the extracellular fluid compartment, maintaining acid -base balance, and regulating hemoglobin levels Preoperatively, the three risk factors that most accurately predict the likelihood of acute renal failure in the postoperative period are: (1) preexisting renal disease (2) congestive heart failure (3) advanced age
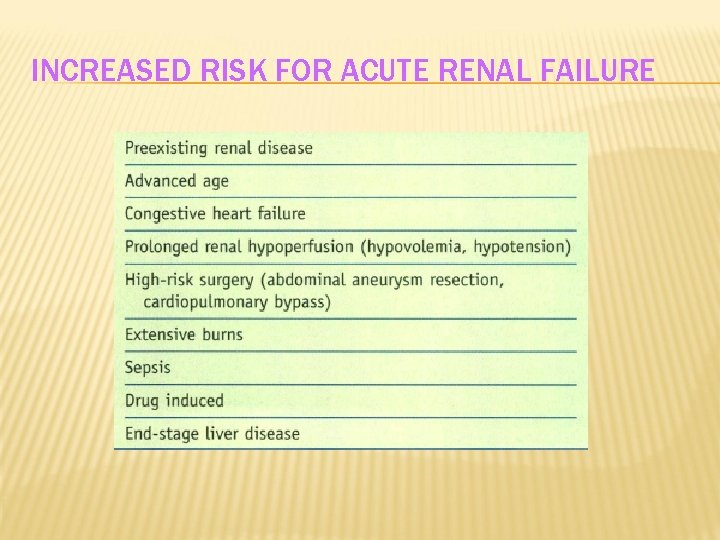
INCREASED RISK FOR ACUTE RENAL FAILURE
RENAL BLOOD FLOW Although the kidneys represent only 0. 5% of total body weight, their blood flow is equivalent to about 20% of cardiac output Approximately two thirds of renal blood flow is distributed to the renal cortex Renal blood flow and the glomerular filtration rate (GFR) remain relatively constant at mean arterial pressures in the range of 60 to I 5 O mm Hg This ability to maintain renal blood flow at a constant rate despite changes in perfusion pressure is known as auto regulation It is achieved by adjustment of afferent arteriolar tone, which alters the resistance to blood flow Auto regulation is important because it acts to protect the glomerular capillaries from high systemic blood pressure during acute hypertensive episodes and maintains GFR and renal tubule function during modest decreases in systemic blood pressure
RENAL BLOOD FLOW When mean arterial pressure is outside the auto regulatory range, renal blood flow becomes pressure dependent. Renal blood flow is strongly influenced by the activity of the sympathetic nervous system and by release of renin and other hormones Sympathetic nervous system stimulation can produce renal vasoconstriction and a marked decrease in renal blood flow even if systemic blood pressure is within the auto regulatory range Any decrease in renal blood flow will initiate the release of renin, which can further decrease renal blood flow

GLOMERULAR FILTRATION RATE Hydrostatic pressure within the glomerular capillaries is about 50 mm. Hg This pressure acts to force water and other low-molecular-weight substances such as electrolytes through the glomerular capillaries into Bowman's space Plasma oncotic pressure is about 25 mm Hg at the afferent arteriole and with filtration increases to about 35 mm Hg at the efferent arteriole
GLOMERULAR FILTRATION RATE Despite a relatively low net filtration pressure, the glomerular capillaries are able to filter plasma at a rate equivalent to about 125 ml/min GFR is reduced by decreased mean arterial pressure or decreased renal blood flow Ultimately, about 90% of the fluid filtered at the glomeruli is reabsorbed from renal tubules into peri tubular capillaries and thus returned to the circulation
HUMORAL SUBSTANCES RENIN Renin is a proteolytic enzyme secreted by the juxtaglomerular apparatus of the kidneys in response to: (1) sympathetic nervous system stimulation (2) decreased renal perfusion pressure (3) decreases in the delivery of sodium to the distal convoluted renal tubules Renin acts on a circulating globulin in plasma (angiotensinogen) to form angiotensin I Angiotensin I is split in the lungs by a converting enzyme to form angiotensin II Angiotensin II is a potent vasoconstrictor and an important stimulus for the release of aldosterone from the adrenal cortex
PROSTAG LANDINS Prostaglandins are produced in the renal medulla and released in response to sympathetic nervous system stimulation and increased levels of angiotensin II During periods of hemodynamic instability, prostaglandins act intrarenally to modulate the vasoconstrictive actions of catecholamines
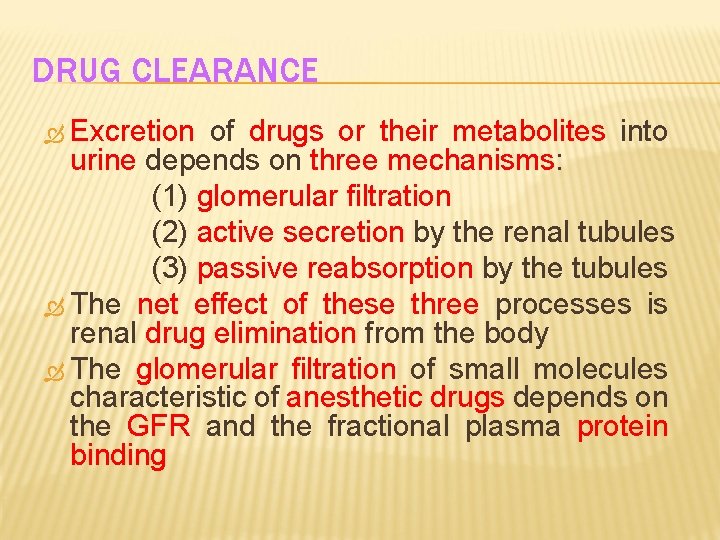
DRUG CLEARANCE Excretion of drugs or their metabolites into urine depends on three mechanisms: (1) glomerular filtration (2) active secretion by the renal tubules (3) passive reabsorption by the tubules The net effect of these three processes is renal drug elimination from the body The glomerular filtration of small molecules characteristic of anesthetic drugs depends on the GFR and the fractional plasma protein binding
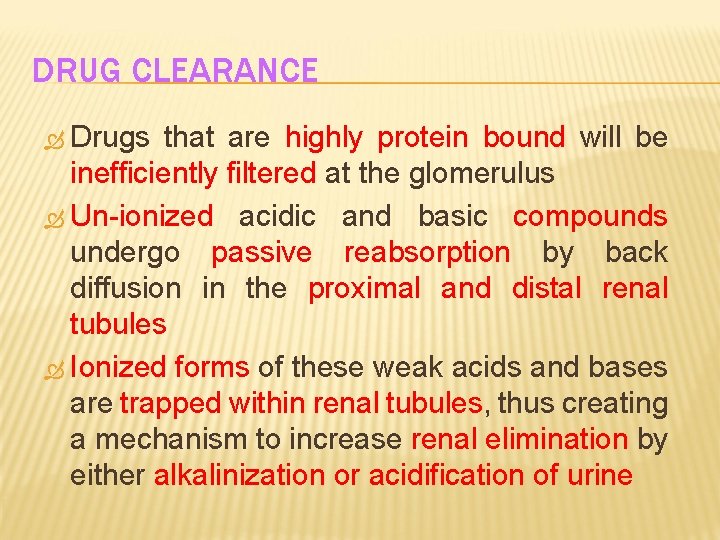
DRUG CLEARANCE Drugs that are highly protein bound will be inefficiently filtered at the glomerulus Un-ionized acidic and basic compounds undergo passive reabsorption by back diffusion in the proximal and distal renal tubules Ionized forms of these weak acids and bases are trapped within renal tubules, thus creating a mechanism to increase renal elimination by either alkalinization or acidification of urine
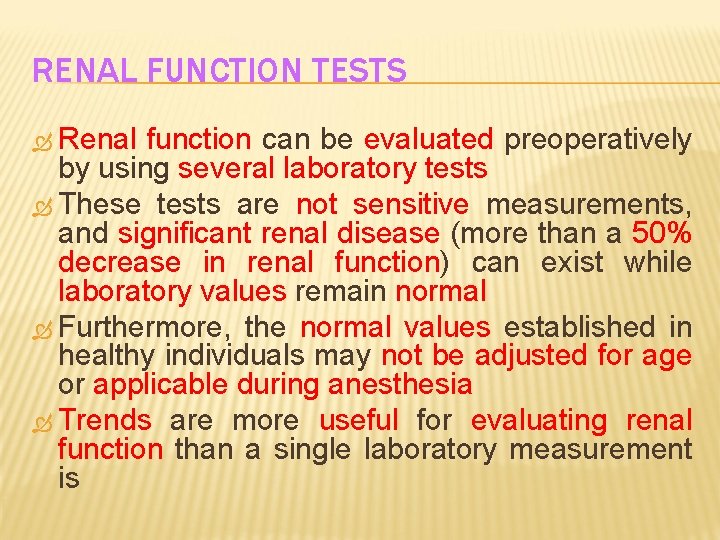
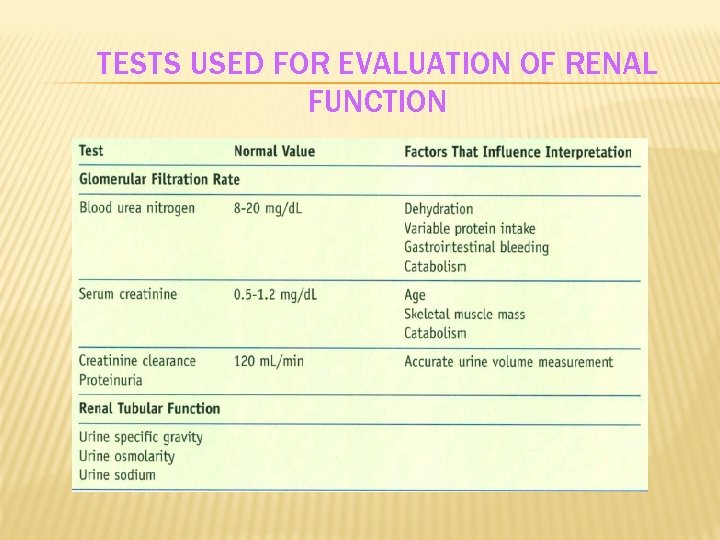
RENAL FUNCTION TESTS Renal function can be evaluated preoperatively by using several laboratory tests These tests are not sensitive measurements, and significant renal disease (more than a 50% decrease in renal function) can exist while laboratory values remain normal Furthermore, the normal values established in healthy individuals may not be adjusted for age or applicable during anesthesia Trends are more useful for evaluating renal function than a single laboratory measurement is
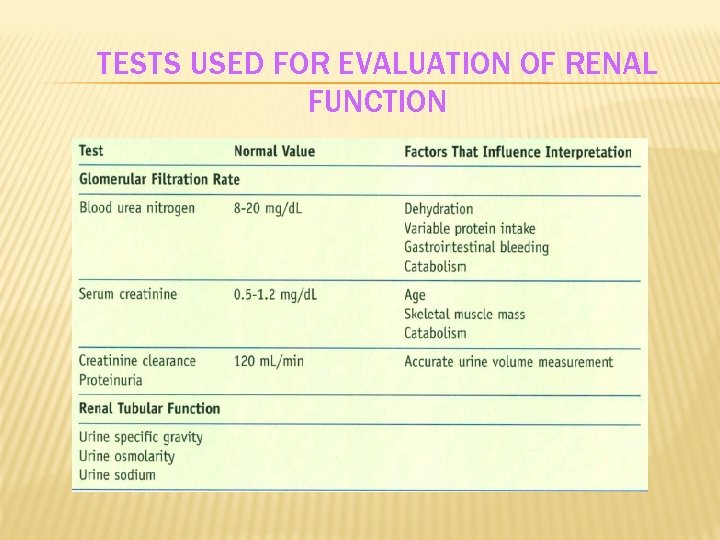
TESTS USED FOR EVALUATION OF RENAL FUNCTION
SERUM CREATININE Serum creatinine concentrations are often used to indicate the GFR In contrast to blood urea nitrogen (BUN) concentrations, serum creatinine levels are not influenced by protein metabolism or the rate of fluid flow through renal tubules Serum creatinine concentrations are, however, influenced by skeletal muscle mass Maintenance of normal serum creatinine concentrations in elderly patients with known decreases in GFR reflects decreased creatinine production because of the decreased skeletal muscle mass that frequently accompanies aging
SERUM CREATININE Indeed, mild increases in the serum creatinine concentration in elderly patients may suggest significant renal disease Likewise, in patients with chronic renal failure, serum creatinine concentrations may not accurately reflect the GFR because of : (1) decreased creatinine production (2) the presence of decreased skeletal muscle mass (3) nonrenal (gastrointestinal tract) excretion of creatinine
BLOOD UREA NITROGEN (BUN) BUN concentrations, which are normally 10 to 20 mg/dl, vary with changes in GFR The BUN concentration is a potentially misleading test of renal function because of the influence of dietary intake, coexisting illnesses, and intravascular fluid volume. For example, high-protein diets or gastrointestinal bleeding can increase the production of urea and thereby result in increased BUN concentrations (azotemia) despite a normal GFR Other causes of increased BUN concentrations despite a normal GFR are increased catabolism during febrile illnesses and dehydration
BLOOD UREA NITROGEN Increased BUN concentrations in the presence of dehydration most likely reflect increased urea absorption because of the slow movement of fluid through the renal tubules, which results in a BUN-to -Creatinine ratio greater than 20 When slow movement of fluid through the renal tubules is responsible for increased BUN concentrations, serum creatinine levels remain normal BUN concentrations can remain normal in the presence of low-protein diets despite decreases in GFR Aside from these extraneous influences, BUN concentrations greater than 50 mg/dl almost always reflect a decreased GFR
CREATININE CLEARANCE Creatinine clearance (normal, 110 to 150 ml/min) is a measurement of the ability of the glomeruli to excrete creatinine into urine for a given serum creatinine concentration Because creatinine clearance does not depend on corrections for age or the presence of a steady state, it is the most reliable measurement of GFR The principal disadvantage of this test is the need for timed (2 hours may be as acceptable as 24 hours) urine collections
PROTEINURIA Small amounts of protein are normally filtered through glomerular capillaries and then reabsorbed in the proximal convoluted tubules Proteinuria (excretion of more than 150 mg of protein per day) is most likely due to abnormally high filtration rather than impaired reabsorption by the renal tubules Intermittent proteinuria occasionally occurs in healthy individuals when standing and disappears when supine Other nonrenal causes of proteinuria include exercise, fever, and congestive heart failure
URINE INDICES Measurement of urine osmolality and urinary sodium and calculation of the fractional excretion of sodium can help differentiate between prerenal and renal tubular (intrarenal) causes of azotemia
OTHER LABORATORY MEASUREMENTS Measurement of serum calcium, uric acid, and creatinine kinase concentrations and serum osmolality may be useful in the differential diagnosis of acute renal failure secondary to conditions such as rhabdomyolysis, nephrotoxic drugs, or malignancy
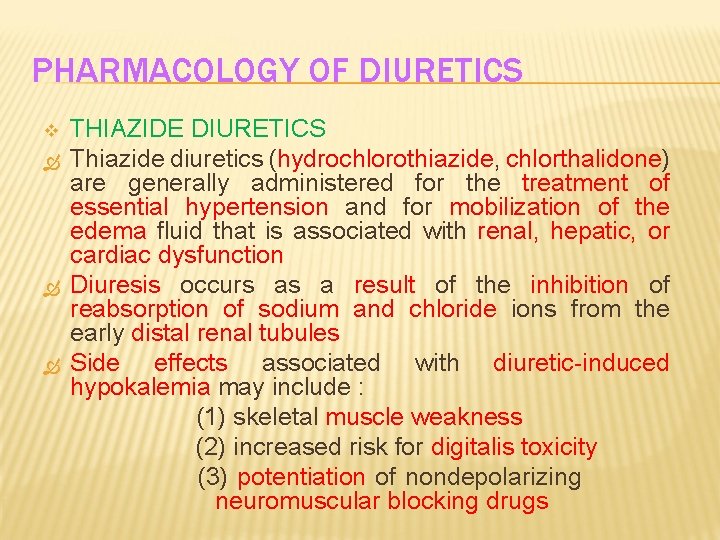
PHARMACOLOGY OF DIURETICS v THIAZIDE DIURETICS Thiazide diuretics (hydrochlorothiazide, chlorthalidone) are generally administered for the treatment of essential hypertension and for mobilization of the edema fluid that is associated with renal, hepatic, or cardiac dysfunction Diuresis occurs as a result of the inhibition of reabsorption of sodium and chloride ions from the early distal renal tubules Side effects associated with diuretic-induced hypokalemia may include : (1) skeletal muscle weakness (2) increased risk for digitalis toxicity (3) potentiation of nondepolarizing neuromuscular blocking drugs
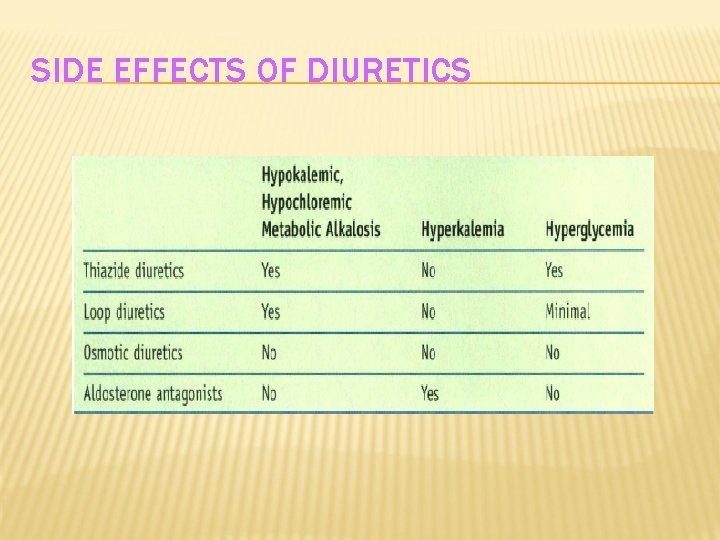
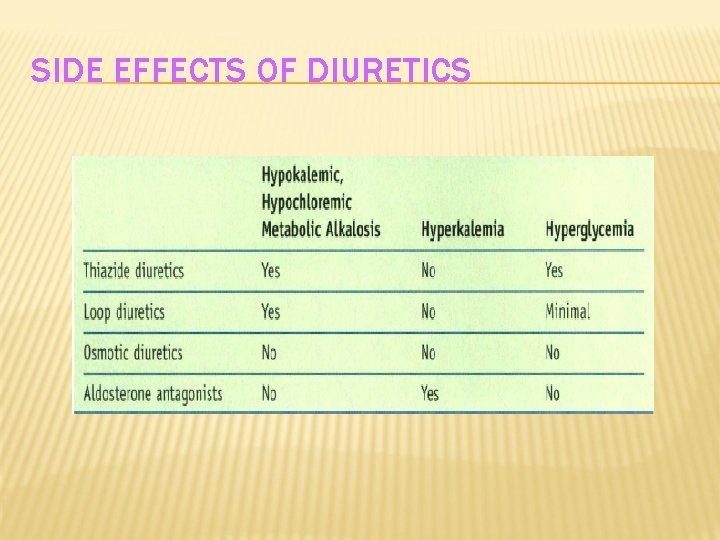
SIDE EFFECTS OF DIURETICS
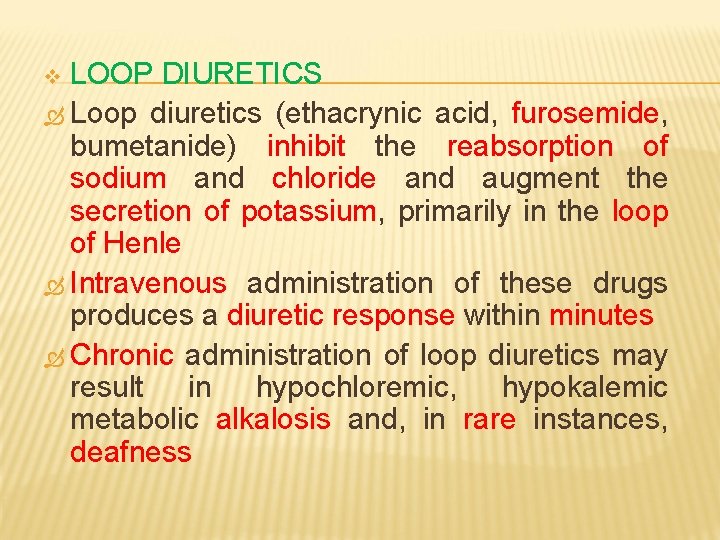
LOOP DIURETICS Loop diuretics (ethacrynic acid, furosemide, bumetanide) inhibit the reabsorption of sodium and chloride and augment the secretion of potassium, primarily in the loop of Henle Intravenous administration of these drugs produces a diuretic response within minutes Chronic administration of loop diuretics may result in hypochloremic, hypokalemic metabolic alkalosis and, in rare instances, deafness v
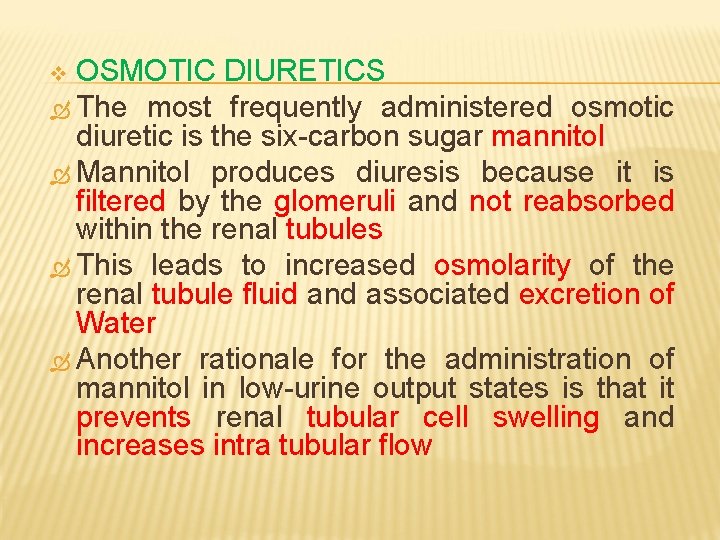
OSMOTIC DIURETICS The most frequently administered osmotic diuretic is the six-carbon sugar mannitol Mannitol produces diuresis because it is filtered by the glomeruli and not reabsorbed within the renal tubules This leads to increased osmolarity of the renal tubule fluid and associated excretion of Water Another rationale for the administration of mannitol in low-urine output states is that it prevents renal tubular cell swelling and increases intra tubular flow v
Mannitol increases fluid movement from intracellular spaces into extracellular spaces such that intravascular fluid volume expands acutely This redistribution of fluid from intracellular to extracellular compartments decreases brain size and intracranial pressure Mannitol may further diminish intracranial pressure by decreasing the rate of cerebrospinal fluid formation
ALDOSTERONE ANTAGONISTS Spironolactone blocks the renal tubular effects of aldosterone and offsets the loss of potassium that is associated with the administration of thiazide diuretics. Fluid overload secondary to cirrhosis of the liver is often treated with spironolactone The most serious toxic effect of spironolactone is hyperkalemia Preoperative measurement of the serum potassium concentration is indicated for patients taking spironolactone v
RENAL-DOSE DOPAMINE Dopamine dilates renal arterioles, which increases renal blood flow and the GFR Treatment with low-dose dopamine (0. 5 to 3 чg/kg/min) may augment urine output but does not appear to alter the course of acute renal failure Dose-dependent side effects of dopamine include tachydysrhythmias, pulmonary shunting, and tissue ischemia (gastrointestinal tract, digits) v
PATHOPHYSIOLOGY OF END-STAGE RENAL DISEASE End-stage renal disease (ESRD) causes profound physiologic changes that affect several organs
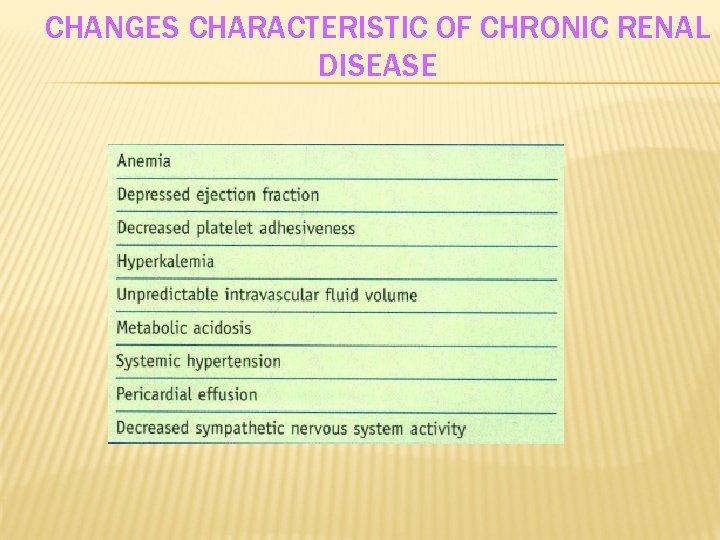
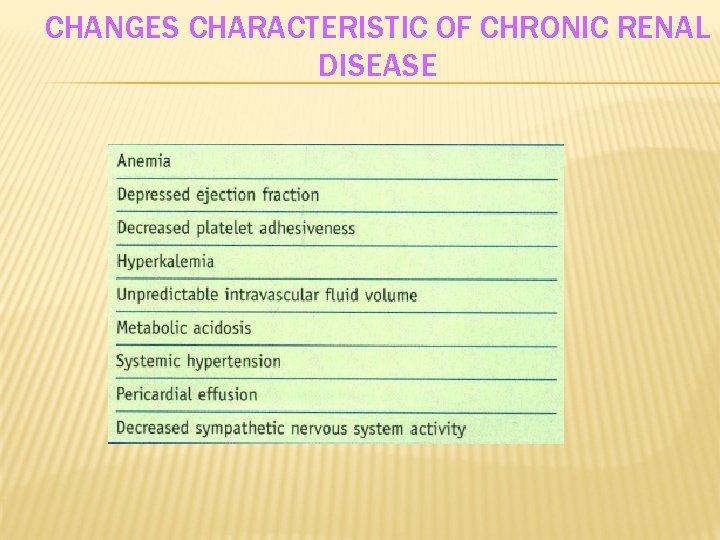
CHANGES CHARACTERISTIC OF CHRONIC RENAL DISEASE
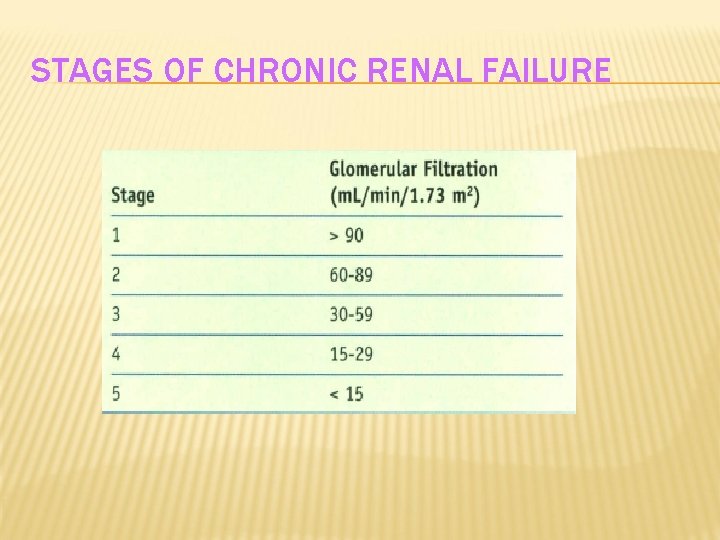
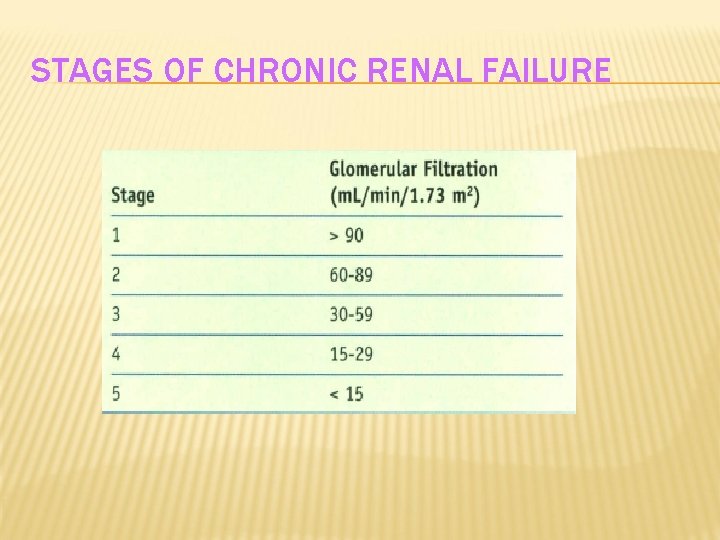
STAGES OF CHRONIC RENAL FAILURE
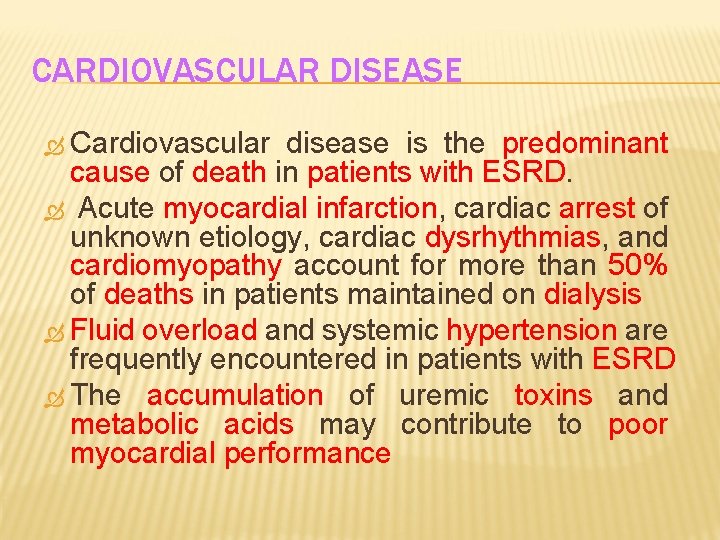
CARDIOVASCULAR DISEASE Cardiovascular disease is the predominant cause of death in patients with ESRD. Acute myocardial infarction, cardiac arrest of unknown etiology, cardiac dysrhythmias, and cardiomyopathy account for more than 50% of deaths in patients maintained on dialysis Fluid overload and systemic hypertension are frequently encountered in patients with ESRD The accumulation of uremic toxins and metabolic acids may contribute to poor myocardial performance
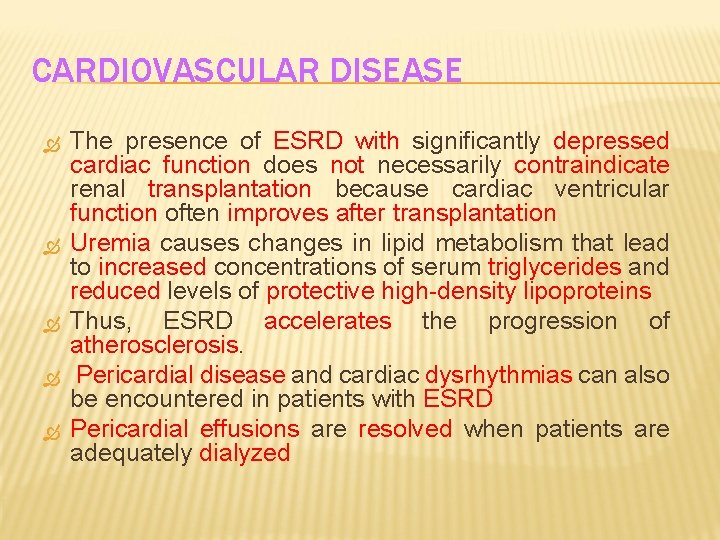
CARDIOVASCULAR DISEASE The presence of ESRD with significantly depressed cardiac function does not necessarily contraindicate renal transplantation because cardiac ventricular function often improves after transplantation Uremia causes changes in lipid metabolism that lead to increased concentrations of serum triglycerides and reduced levels of protective high-density lipoproteins Thus, ESRD accelerates the progression of atherosclerosis. Pericardial disease and cardiac dysrhythmias can also be encountered in patients with ESRD Pericardial effusions are resolved when patients are adequately dialyzed
METABOLIC DISEASE A large number of patients with ESRD manifest diabetes mellitus Kidney failure as a result of diabetes develops in nearly 30% to 40% of patients with ESRD, and these patients account for 30% of those on the waiting list for kidney transplantation In fact, nephropathy develops in nearly 60% of insulindependent diabetic patients Patients with ESRD and diabetes have a higher cardiovascular risk than do patients with renal failure alone Once patients are unable to excrete their dietary fluid and electrolyte loads, abnormalities in plasma electrolyte concentrations (sodium, potassium, calcium, magnesium, and phosphate) can develop The most life-threatening electrolyte abnormality is hyperkalemia
ANEMIA AND ABNORMAL COAGULATION Patients with renal failure generally display a normochromic, normocytic anemia because of decreased erythropoiesis and retained toxins that are secondary to renal failure Treatment with recombinant erythropoietin can frequently raise hemoglobin levels to 10 to 14 g/dl, which reduces symptoms of fatigue and improves both cerebral and cardiac function Occasionally, recombinant erythropoietin therapy may exacerbate preexisting essential hypertension Renal failure patients may also display uremiainduced defects in platelet function
MANAGEMENT OF ANESTHESIA IN PATIENTS WITH END-STAGE RENAL DISEASE General endotracheal anesthesia provides acceptable hemodynamics, excellent skeletal muscle relaxation, and a predictable depth of anesthesia in patients with ESRD who are undergoing major operations Patients with advanced stages of comorbid conditions may require more extensive monitoring, such as continuous monitoring of systemic blood pressure and perhaps central venous pressure Large swings in blood pressure may occur with hypotension being more likely than hypertension during maintenance of anesthesia Those with the most severe comorbid conditions, such as symptomatic coronary artery disease or a history of congestive heart failure, may benefit from monitoring with a pulmonary artery catheter or transesophageal echocardiography
The status of hemodialysis shunts or fistulas should be monitored (presence of a thrill) during positioning and intraoperatively to confirm continued potency Patients with uremia and other comorbid conditions (diabetes mellitus) should be considered to be at risk for aspiration during induction of anesthesia and treated as though they have a "full stomach" The use of succinylcholine is not contraindicated in patients with ESRD. The increase in serum potassium concentration after an intubating dose of succinylcholine is approximately 0. 6 m. Eq/L for patients both with and without ESRD This increase can be tolerated without imposing a significant cardiac risk, even in the presence of an initial serum potassium concentration higher than 5 m. Eq/L
Several strategies have been successfully used to achieve adequate heart rate and blood pressure control during induction of anesthesia. Moderate to large doses of opioids such as fentanyl can blunt the response to laryngoscopy However, systemic blood pressure is frequently more difficult to maintain after induction of anesthesia, and hypotension may require treatment with vasoconstrictors The short-acting β-adrenergic blocker esmolol may be used to blunt the hemodynamic response to tracheal intubation and is ideally suited for patients with an adequate ejection fraction Drugs or their metabolites that depend on renal elimination (pancuronium, morphine, meperidine) should be used cautiously or avoided
Atracurium and cisatracurium are metabolized by spontaneous Hoffman degradation and plasma cholinesterase, which makes their duration of action independent of liver or kidney function Similarly, fentanyl, sufentanil, alfentanil, and remifentanil are alternatives to morphine Choices of inhaled anesthetics include desflurane, isoflurane, and sevoflurane The metabolism of sevoflurane to inorganic fluoride has been implicated in experimental studies of renal toxicity, although no controlled human studies are available to indicate either safety concerns or danger when using sevoflurane in the setting of ESRD
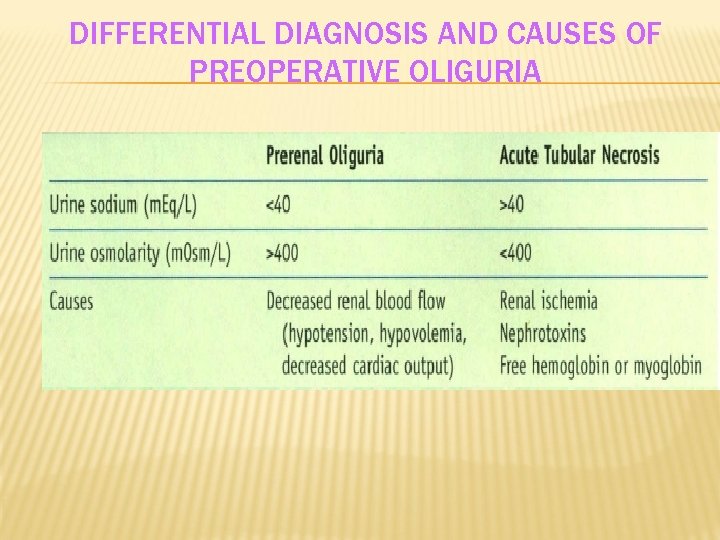
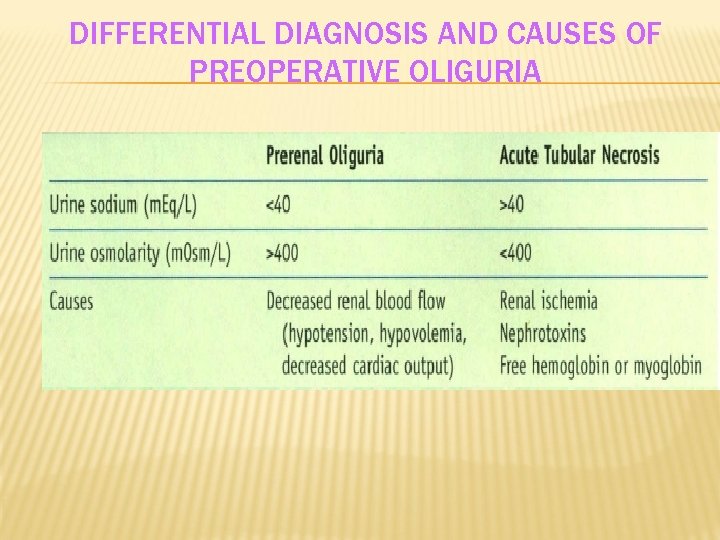
DIFFERENTIAL DIAGNOSIS OF PERI OPERATIVE OLIGURIA PRE RENAL OLIGURIA Prerenal oliguria is characterized by the excretion of concentrated urine that contains minimal amounts of sodium (Table) Excretion of highly concentrated and sodium -poor urine confirms that renal tubular function is intact and reflects an attempt by the kidneys to conserve sodium and restore intravascular fluid volume in response to decreased renal blood flow
DIFFERENTIAL DIAGNOSIS AND CAUSES OF PREOPERATIVE OLIGURIA
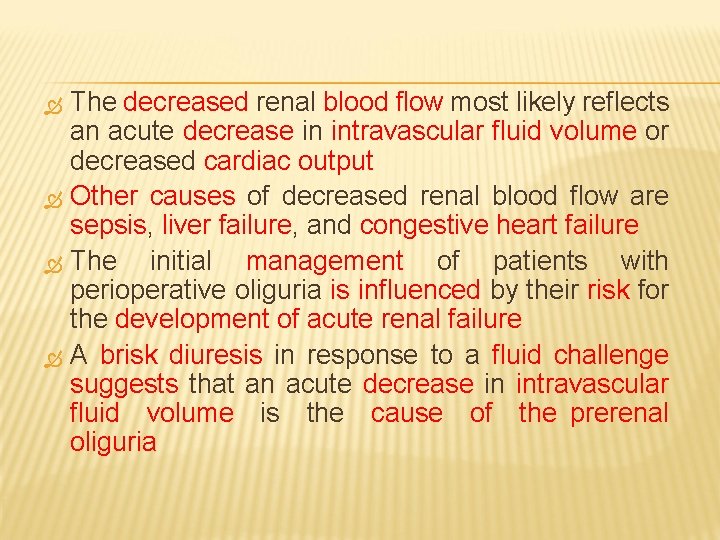
The decreased renal blood flow most likely reflects an acute decrease in intravascular fluid volume or decreased cardiac output Other causes of decreased renal blood flow are sepsis, liver failure, and congestive heart failure The initial management of patients with perioperative oliguria is influenced by their risk for the development of acute renal failure A brisk diuresis in response to a fluid challenge suggests that an acute decrease in intravascular fluid volume is the cause of the prerenal oliguria
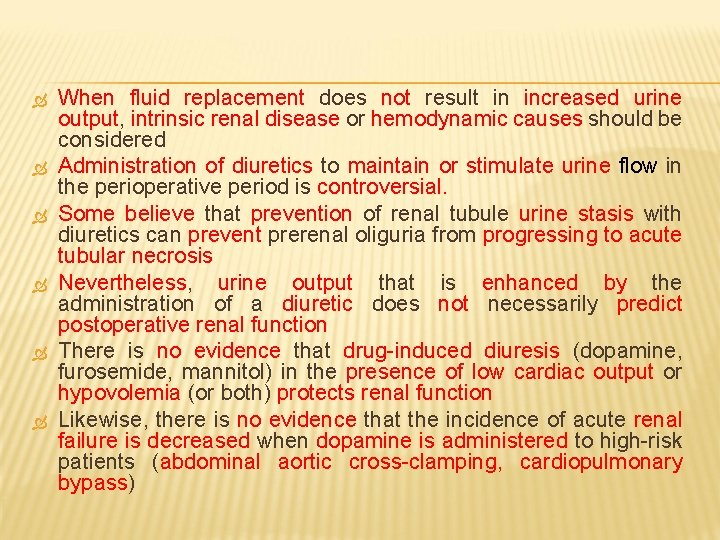
When fluid replacement does not result in increased urine output, intrinsic renal disease or hemodynamic causes should be considered Administration of diuretics to maintain or stimulate urine flow in the perioperative period is controversial. Some believe that prevention of renal tubule urine stasis with diuretics can prevent prerenal oliguria from progressing to acute tubular necrosis Nevertheless, urine output that is enhanced by the administration of a diuretic does not necessarily predict postoperative renal function There is no evidence that drug-induced diuresis (dopamine, furosemide, mannitol) in the presence of low cardiac output or hypovolemia (or both) protects renal function Likewise, there is no evidence that the incidence of acute renal failure is decreased when dopamine is administered to high-risk patients (abdominal aortic cross-clamping, cardiopulmonary bypass)
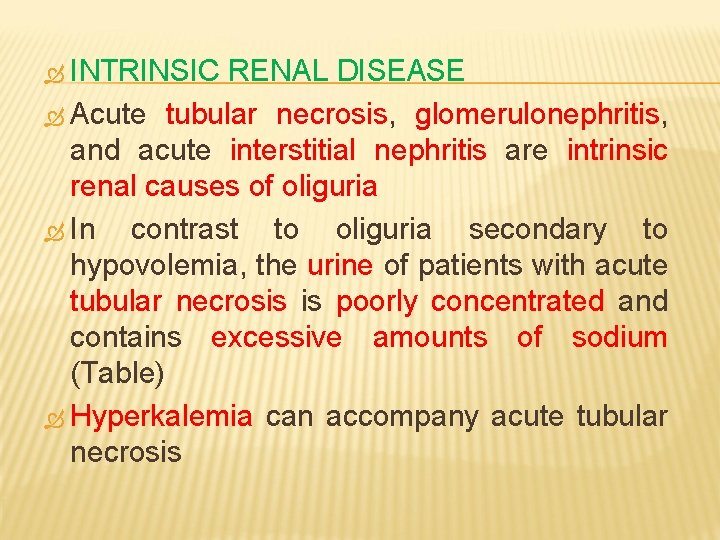
INTRINSIC RENAL DISEASE Acute tubular necrosis, glomerulonephritis, and acute interstitial nephritis are intrinsic renal causes of oliguria In contrast to oliguria secondary to hypovolemia, the urine of patients with acute tubular necrosis is poorly concentrated and contains excessive amounts of sodium (Table) Hyperkalemia can accompany acute tubular necrosis
POSTRENAL OLIGURIA An obstruction that is distal to the renal collecting system usually involves a mechanical problem such as a blood clot in the ureter, bladder, or urethra Surgical ligation and renal calculi are other postrenal causes of low urine output Another common postrenal cause is bladder catheter obstruction
KIDNEY TRANSPLANTATION
INTRODUCTION Solid organ transplantation has become a wellaccepted treatment modality for patients with end-stage organ disease The role of the anesthesiologist in organ transplantation may involve caring for organ donors, prospective recipients, or patients who have already received transplants but require further surgery Organs that are most frequently transplanted are the kidneys and the liver An extensive preoperative workup with an emphasis on the cardiopulmonary system and conditions related to the failing organ is required for all potential transplant candidates
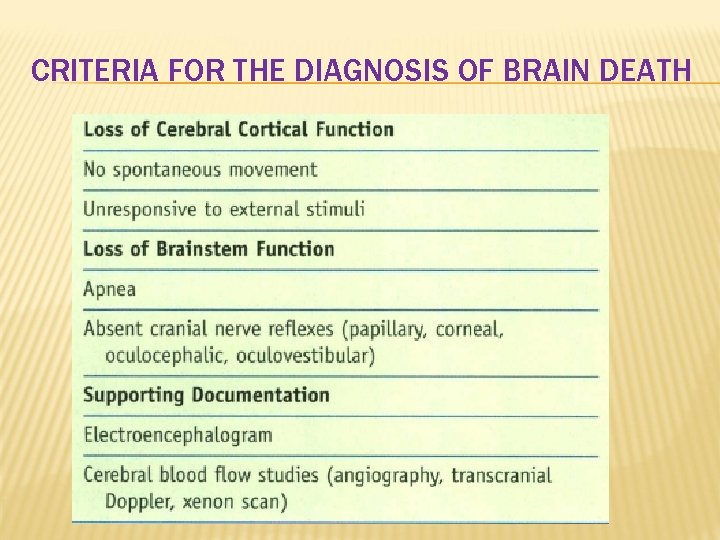
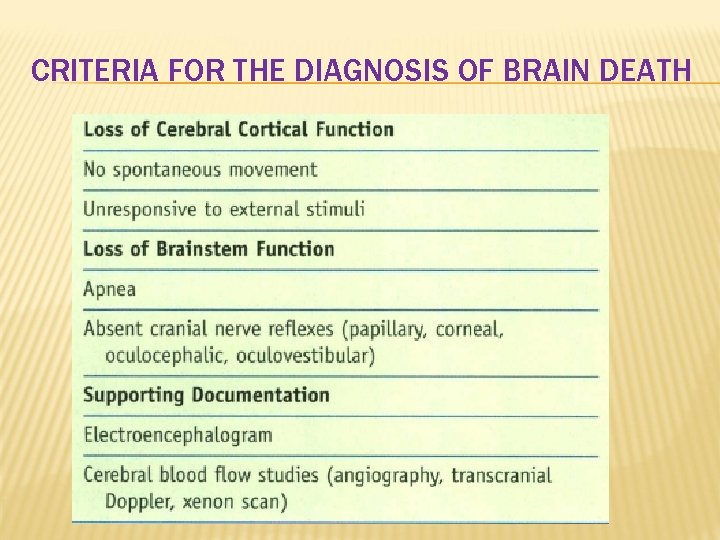
CRITERIA FOR THE DIAGNOSIS OF BRAIN DEATH
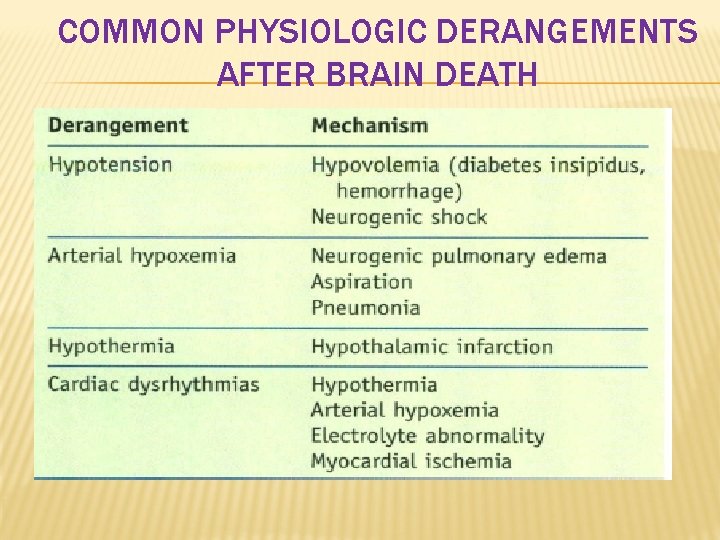
UNIQUE CONSIDERATIONS FOR ORGAN TRANSPLANTATION Death is always certified before the donor procedure Anesthetic care for organ procurement requires a focus on maintenance of donor organ perfusion and oxygenation and recognition of common physiologic derangements associated with brain death (Table) Organ preservation after removal from the donor includes hypothermia to decrease metabolism with preservative solutions of specific additives to maintain cellular integrity and decrease hypothermiamediated injury Refinement of perioperative care plus improved management of patients after transplantation has resulted in a dramatic improvement in both 1 - and 5 year graft survival
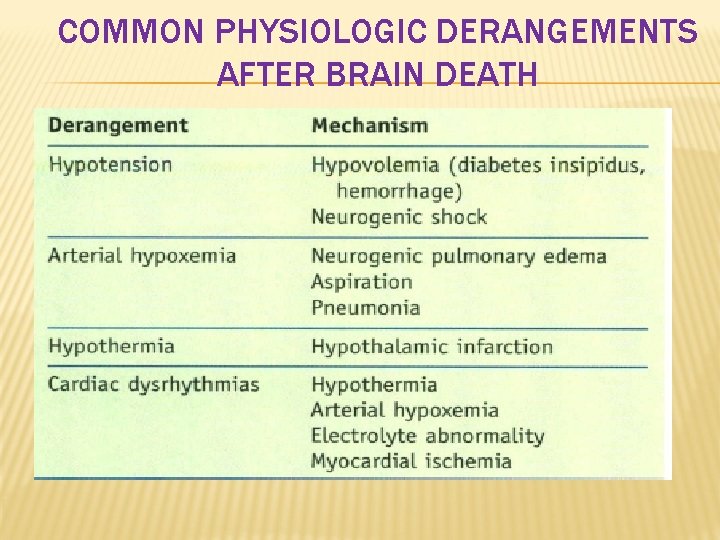
COMMON PHYSIOLOGIC DERANGEMENTS AFTER BRAIN DEATH
Postoperative organ function after transplantation depends on multiple factors, including donor demographics, organ ischemia time, mechanism of death of the donor, and medical condition of the recipient Improvement in immunosuppressive regimens and better tissue typing have contributed to the increasing success of organ transplantation Infection (bacterial, fungal, viral) attributable to chronic immunosuppression is the most common cause of death in transplant recipients, thus emphasizing the importance of strict asepsis during the management of anesthesia The frequency of cancer (especially skin and Iymphoproliferative) is increased in transplant patients, perhaps reflecting loss of the protective effects of an active immune system

CONTRAINDICATIONS TO SOLID ORGAN TRANSPLANTATION Absolute and relative contraindications to solid organ transplantation have diminished over recent years For instance, candidates for kidney transplantation are increasingly older and have more complex medical problems. Evidence of malignancy is not a contraindication For example, hepatocellular carcinoma with underlying cirrhosis is considered to be an indication for liver transplantation as long as the tumor has not reached a certain size Active infection is an absolute contraindication until it has been treated and the infection has resolved Severe irreversible pulmonary hypertension is a contraindication to heart transplantation, but these patients may be candidates for combined heart-lung transplantation
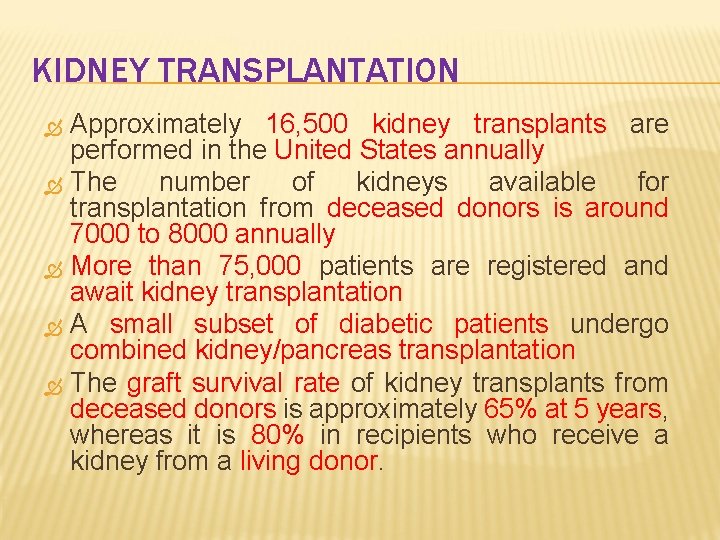
KIDNEY TRANSPLANTATION Approximately 16, 500 kidney transplants are performed in the United States annually The number of kidneys available for transplantation from deceased donors is around 7000 to 8000 annually More than 75, 000 patients are registered and await kidney transplantation A small subset of diabetic patients undergo combined kidney/pancreas transplantation The graft survival rate of kidney transplants from deceased donors is approximately 65% at 5 years, whereas it is 80% in recipients who receive a kidney from a living donor.
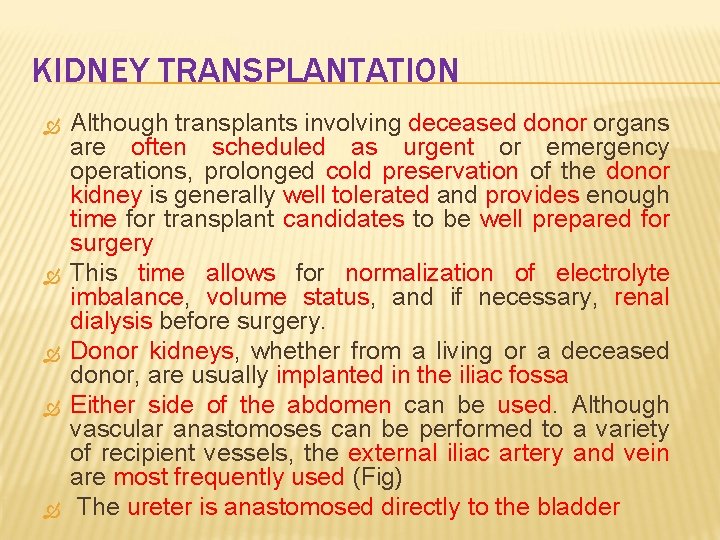
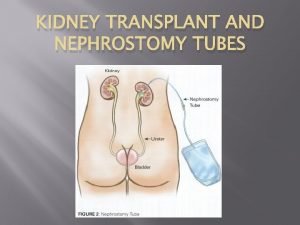
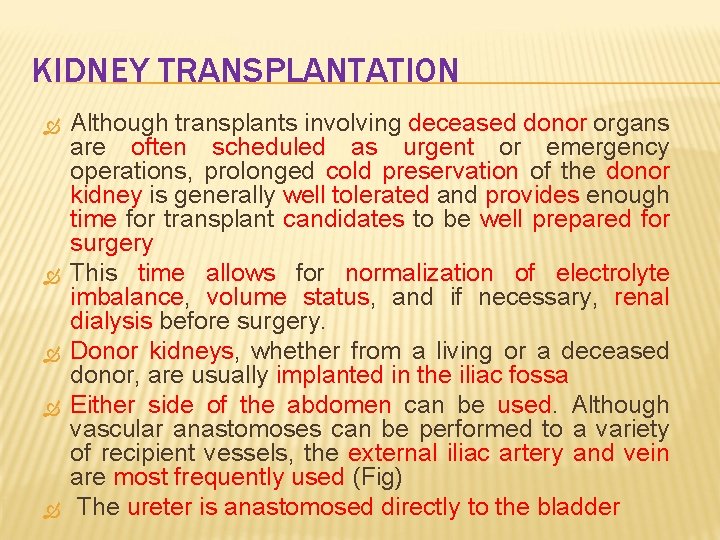
KIDNEY TRANSPLANTATION Although transplants involving deceased donor organs are often scheduled as urgent or emergency operations, prolonged cold preservation of the donor kidney is generally well tolerated and provides enough time for transplant candidates to be well prepared for surgery This time allows for normalization of electrolyte imbalance, volume status, and if necessary, renal dialysis before surgery. Donor kidneys, whether from a living or a deceased donor, are usually implanted in the iliac fossa Either side of the abdomen can be used. Although vascular anastomoses can be performed to a variety of recipient vessels, the external iliac artery and vein are most frequently used (Fig) The ureter is anastomosed directly to the bladder
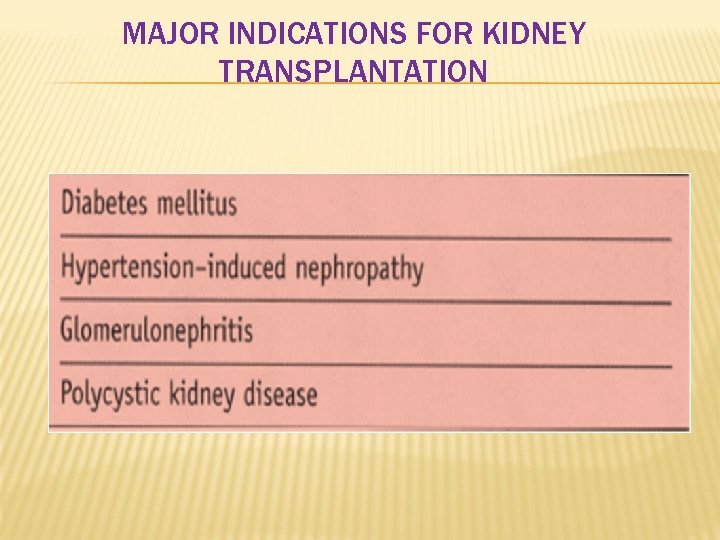
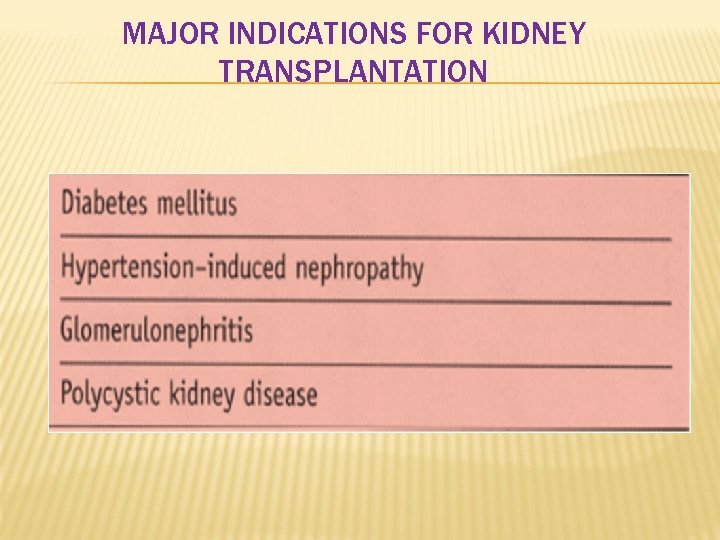
MAJOR INDICATIONS FOR KIDNEY TRANSPLANTATION

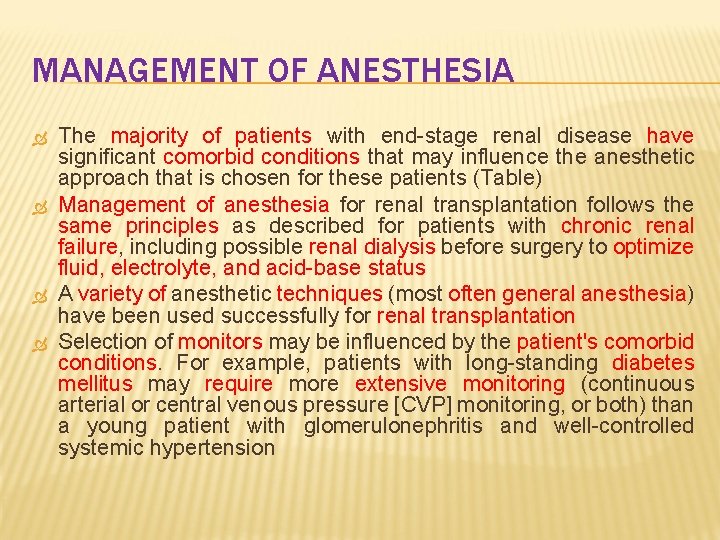
MANAGEMENT OF ANESTHESIA The majority of patients with end-stage renal disease have significant comorbid conditions that may influence the anesthetic approach that is chosen for these patients (Table) Management of anesthesia for renal transplantation follows the same principles as described for patients with chronic renal failure, including possible renal dialysis before surgery to optimize fluid, electrolyte, and acid-base status A variety of anesthetic techniques (most often general anesthesia) have been used successfully for renal transplantation Selection of monitors may be influenced by the patient's comorbid conditions. For example, patients with long-standing diabetes mellitus may require more extensive monitoring (continuous arterial or central venous pressure [CVP] monitoring, or both) than a young patient with glomerulonephritis and well-controlled systemic hypertension
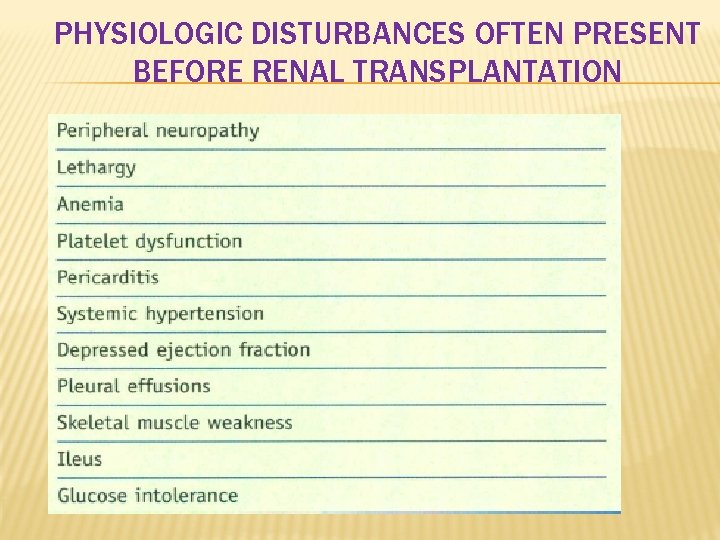
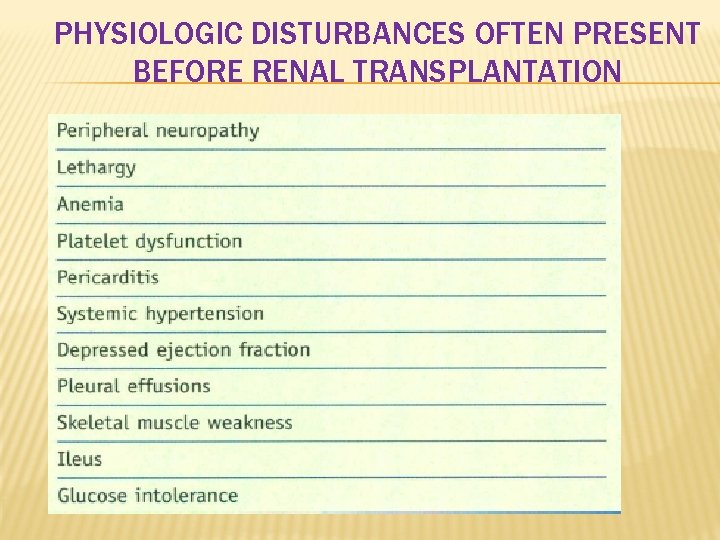
PHYSIOLOGIC DISTURBANCES OFTEN PRESENT BEFORE RENAL TRANSPLANTATION
When CVP monitoring is used, the goal is to maintain CVP in the 10 - to I 5 -mm Hg range to optimize fluid status and renal perfusion Surgical stimulation after dissection of the fascia for placement of the donor kidney is minimal, and systemic hypotension may ensue as a result of the effects of anesthetic drugs Effort should be made to avoid episodes of hypotension after reperfusion because renal graft function is critically dependent on perfusion pressure Excessive opioid administration coupled with minimal surgical stimulation may contribute to hypotension. Intravenous administration of α-adrenergic drugs such as phenylephrine may be avoided In as much as animal models have demonstrated that vessels in the transplanted kidney are sensitive to sympathomimetics, which can compromise blood flow to the transplanted organ Of note, convincing scientific data in humans are not available
Mannitol, loop diuretics, and dopamine may be used intraoperatively to improve renal perfusion pressure and enhance urine production Low dose mannitol (12. 5 to 25 g IV) and loop diuretics are usually administered before unclamping the vascular supply to the transplanted kidney The role of dopamine in kidney transplantation remains controversial Prompt urine production is seen in more than 90% of living donor kidney transplants and in 40% to 70% of deceased donor transplants During the latter stages of closure of the surgical wound, a decrease in urine output suggests mechanical impingement of the graft, vessel, or ureter
If impingement occurs, the Foley catheter should be irrigated and checked for patency If intraoperative ultrasound is immediately available, it can be used to examine flow through the arterial and venous anastomoses Moderate to severe systemic hypertension can accompany emergence from anesthesia after renal transplantation Antihypertensive therapy may be initiated in the operating room and continued during the recovery period Postoperative pain is generally mild to moderate and can be well controlled with intravenous opioids Epidural catheters are not usually placed in this patient population
 Ira pré renal renal e pós renal
Ira pré renal renal e pós renal Ira pré renal renal e pós renal
Ira pré renal renal e pós renal Insertion sort pseudocode
Insertion sort pseudocode Peritubular capillaries and vasa recta difference
Peritubular capillaries and vasa recta difference Detrusal
Detrusal Masood sepehrimanesh
Masood sepehrimanesh Chris chien
Chris chien Cybr373
Cybr373 Loading dose formula in pharmacology
Loading dose formula in pharmacology Bone marrow transplantation sri lanka
Bone marrow transplantation sri lanka Law of transplantation
Law of transplantation Patrick evrard transplantation
Patrick evrard transplantation Cultural transposition
Cultural transposition Transplant
Transplant Stem cell or bone marrow transplantation thailand
Stem cell or bone marrow transplantation thailand Ersd
Ersd Nemo dialysis
Nemo dialysis Nih scale
Nih scale Kara potter
Kara potter Choronic kidney disease
Choronic kidney disease Albumin kidney disease
Albumin kidney disease Albumin kidney disease
Albumin kidney disease Symptomatic polycystic kidney disease
Symptomatic polycystic kidney disease Uremia pathogenesis
Uremia pathogenesis Communicable disease and non communicable disease
Communicable disease and non communicable disease Kidney organ system
Kidney organ system Medulla kidney
Medulla kidney Claire gibbons
Claire gibbons Kidney failure urine color chart
Kidney failure urine color chart Urineferous
Urineferous Urine infection symptoms
Urine infection symptoms Tubular secretion
Tubular secretion Gross features
Gross features Pathophysiology of kidney stones
Pathophysiology of kidney stones Juxtaglomerular apparatus
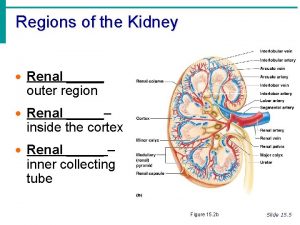
Juxtaglomerular apparatus What are the three regions of the kidney
What are the three regions of the kidney Kidney infection
Kidney infection 3 layers of the kidney
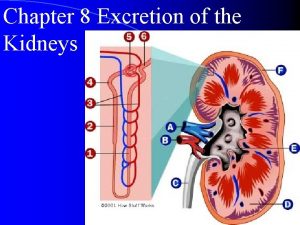
3 layers of the kidney Internal anatomy of the kidney
Internal anatomy of the kidney Macula densa function
Macula densa function Figure 15-2 is a longitudinal section of a kidney
Figure 15-2 is a longitudinal section of a kidney Medulla kidney
Medulla kidney Slk criteria
Slk criteria Acute tubular necrosis
Acute tubular necrosis Tubuloglomerular feedback mechanism
Tubuloglomerular feedback mechanism Urinary tract obstruction
Urinary tract obstruction Coverings of kidney
Coverings of kidney Kaarlo hinkkala
Kaarlo hinkkala Pylonephrite
Pylonephrite Flea bitten kidney seen in
Flea bitten kidney seen in Hyperplastic arteriolitis
Hyperplastic arteriolitis Hypoplasia
Hypoplasia Nursing management of hydronephrosis
Nursing management of hydronephrosis Oviduct frog
Oviduct frog Excretory system organs and functions
Excretory system organs and functions Kidney epithelial tissue
Kidney epithelial tissue Lig hepatoduodenal
Lig hepatoduodenal Hydrogen secretion in kidney
Hydrogen secretion in kidney Basinlike area of the kidney continuous with the ureter
Basinlike area of the kidney continuous with the ureter Vertebrocostal angle
Vertebrocostal angle Kidney epithelial tissue
Kidney epithelial tissue Retroperitoneal organs
Retroperitoneal organs Endive oxalate
Endive oxalate Topper learning.com
Topper learning.com