Fall Prevention Fareen Ahmed Chris Chien Zaira Masood





- Slides: 35
Fall Prevention Fareen Ahmed Chris Chien Zaira Masood Mary Randolph Tiani Tuiolosega
• An incident that results in a person coming to rest inadvertently on the ground or floor or other lower level. • Patient falls, defined as the rate at which patients fall during their hospital stays per 1, 000 patient days, are a nursing-sensitive quality indicator in the delivery of inpatient services. • Patient fall rates are perceived as the indicator that could be most improved through nurse-led safety strategies or interventions. • In other words, nurses assume the primary responsibility and are somewhat liable when a patient falls in the inpatient care unit. Definition of a Fall

• According to reports published by the Centers for Disease Control and Prevention Injury Center (2007), patient falls are the: • Third most common cause of unintentional injury death across all age groups. • First leading cause among people 65 years and older. Background
• Sun Coast Regional Hospital is a 500 bed, full service, acute care facility with a medical staff of approximately 1, 100 and employee base of 1, 500. Facility Information
• Number of Patient Falls / Number of Patient Days x 1, 000 = Fall Rate per 1, 000 patients. • Currently, the risk of inpatient falls is 50% per 1, 000 patients annually. Problem
• We are a quality improvement team which has been brought in by Sun Coast Regional Hospital to help reduce the risk of inpatient falls within their facility. • Our goal is to reduce the risk by 90%, resulting in 10% risk of inpatient falls per 1, 000 patients annually. Aim
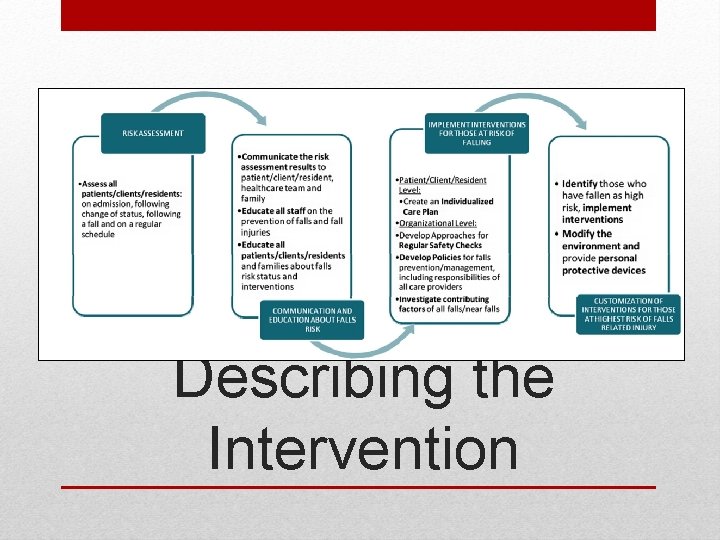
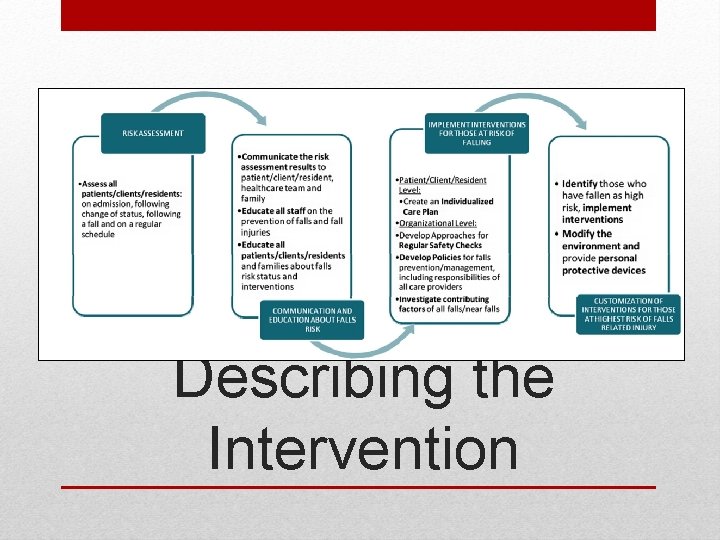
Describing the Intervention
• All patients aged 65 and over. • Younger patients at increased risk of falling, such as those with: • • History of falls Neurological conditions Cognitive problems Visual impairment Patients to be Targeted for this Initiative
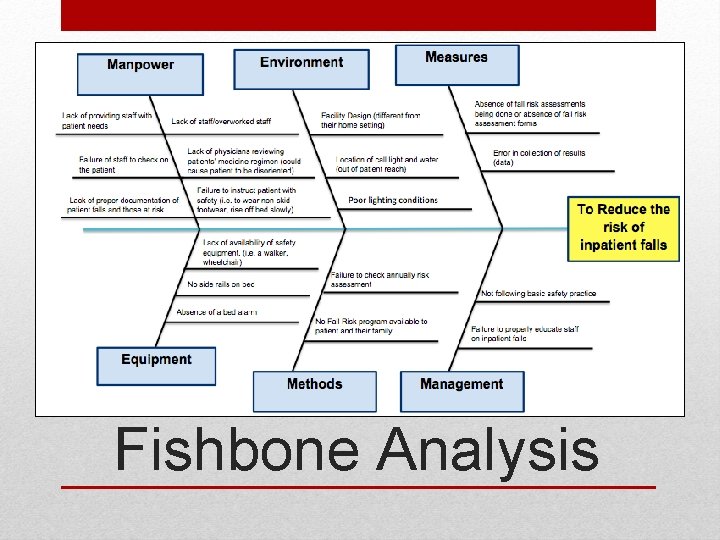
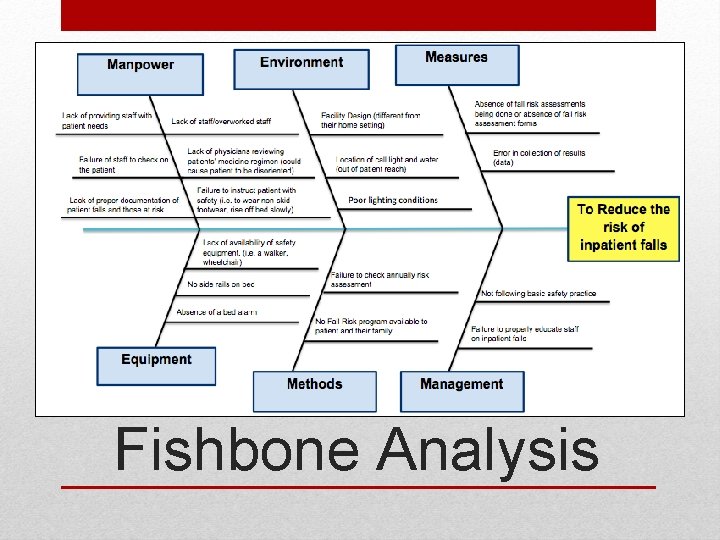
Fishbone Analysis
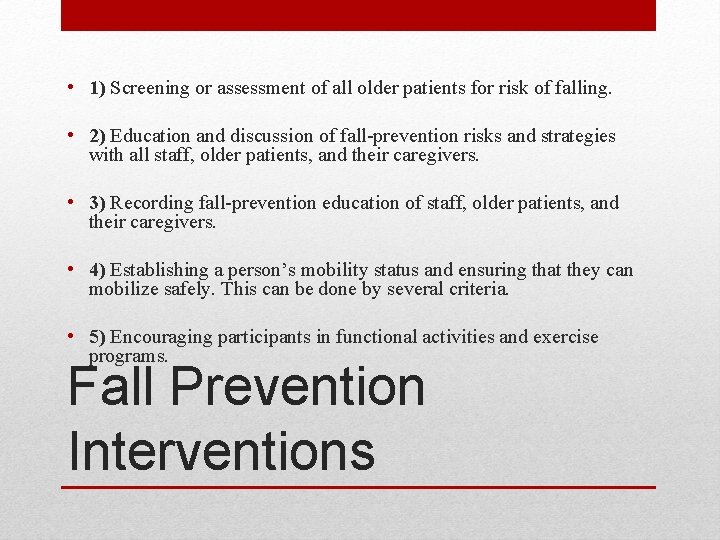
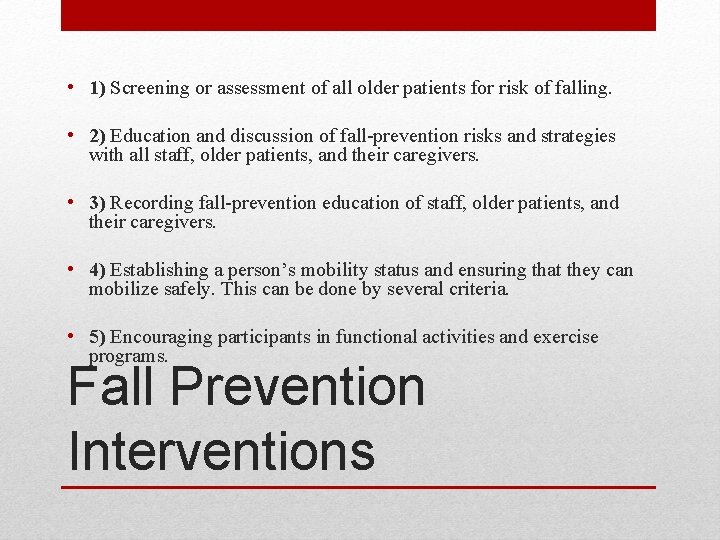
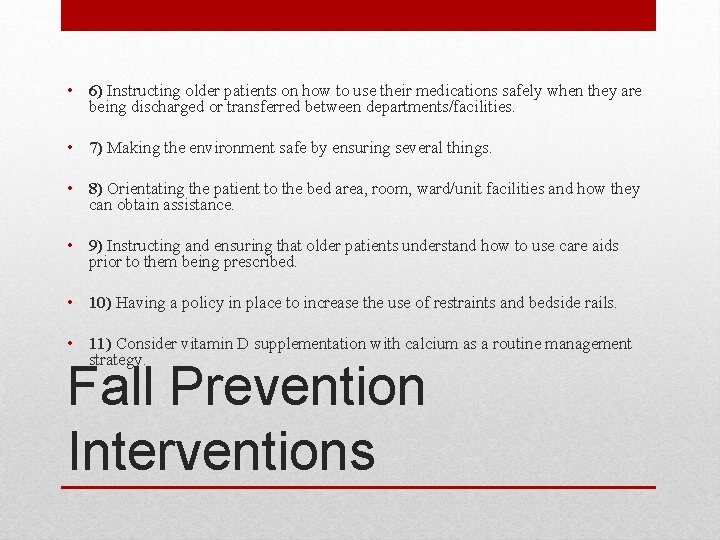
• 1) Screening or assessment of all older patients for risk of falling. • 2) Education and discussion of fall-prevention risks and strategies with all staff, older patients, and their caregivers. • 3) Recording fall-prevention education of staff, older patients, and their caregivers. • 4) Establishing a person’s mobility status and ensuring that they can mobilize safely. This can be done by several criteria. • 5) Encouraging participants in functional activities and exercise programs. Fall Prevention Interventions
• 6) Instructing older patients on how to use their medications safely when they are being discharged or transferred between departments/facilities. • 7) Making the environment safe by ensuring several things. • 8) Orientating the patient to the bed area, room, ward/unit facilities and how they can obtain assistance. • 9) Instructing and ensuring that older patients understand how to use care aids prior to them being prescribed. • 10) Having a policy in place to increase the use of restraints and bedside rails. • 11) Consider vitamin D supplementation with calcium as a routine management strategy. Fall Prevention Interventions

• A hospital can be a dangerous and erratic place for inpatients because: • Unfamiliar physical environment (different from that of their home setting). • Changes in patients' medical conditions as related to their physical and psychological health and sensory systems (e. g. , pain). Facility Design
• A better physical facility design may lead to better health care outcomes, such as fewer patient falls in acute care hospitals. • A patient-centered facility design should promote patient safety. • A safety-driven design with a goal to prevent inpatient fall related injuries should be a hospital design principle. Facility Design

• Increase patient to provider ratio. • Adding information regarding falls onto patients’ charts. Workforce
Patients Staff • Educate about how falls can impact health. • How and where to get assistance when being mobile. • Steps to prevent falls as a patient. • Educate and train in the use of various mobility aids. • Educate about how falls can impact health of patients. • How to assess patients’ risk regarding various diagnoses. • Steps to prevent patient falls. • Steps to take when patients do fall. Educating Patients & Staff
• Find an opportunity to improve • Organize a team • Clarify current understanding of process • Understanding the causes • Select an intervention(s) FOCUS
• Sun Coast Regional Hospital is faced with a large risk of patients falling in the facility each year. Currently, the fall rate is 50% per 1, 000 patients annually. • Falls can be devastating, especially for seniors. Fallrelated injuries may ensue and cause further negative health outcomes. • As the QI team, our plan is to reduce this number significantly by incorporating strategies that will help reduce the risk of patients falling. Find an Opportunity to Improve
• The QI team will consist of: • Team Leader: Oversees QI process and directs the team. • Nursing Staff: Assesses patients’ risk of falling, supervise and assist them with their mobility needs. • Data Technician: Records and updates information and continuously ensures team and patients are up-to-date with intervention strategies. • Facilities Manager: Oversees improvement of hospital design for patient safety and facility maintenance. • Compliance Officer: Ensures the team is complying within safe practices for patients when implementing interventions. Organize a
• The current process at Sun Coast is very poor and is often a reactive step which only takes place once patients have already suffered from a fall. • Falls are recorded any fall-related injuries are then treated promptly. • There are minimal preventative practices and procedures along with an insufficient amount of patient to provider ratio. • With such a poor process, the number of falls will continue to increase and no improvements will be made. Clarify current Understanding
• There are multiple causes that may trigger patients to fall during their stay in the hospital, and without proper oversight and preventative practices, falls will likely occur often. • As the quality improvement team, we have identified three (3) sources that contribute highly to the annual fall rate and which we shall address with interventions. • Materials (education of patients & staff) • Physical environment (facility design) • Workforce (staff increase) Understanding the Causes
Materials • Education and discussion of fall-prevention risks and strategies with all staff, patients, and their caregivers. Physical Environment • Making the environment safe by ensuring several things (i. e. , install more hand rails, clean and hazard-free floors, well-lit rooms, etc. ). Workforce • Orientating the patient to the bed area, room, or ward/unit facilities and how they can obtain assistance. Selecting the Intervention(s)

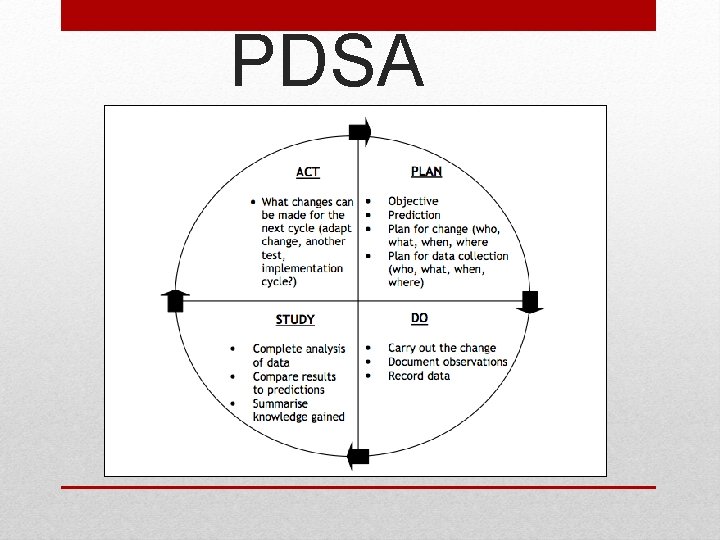
PDSA Cycle
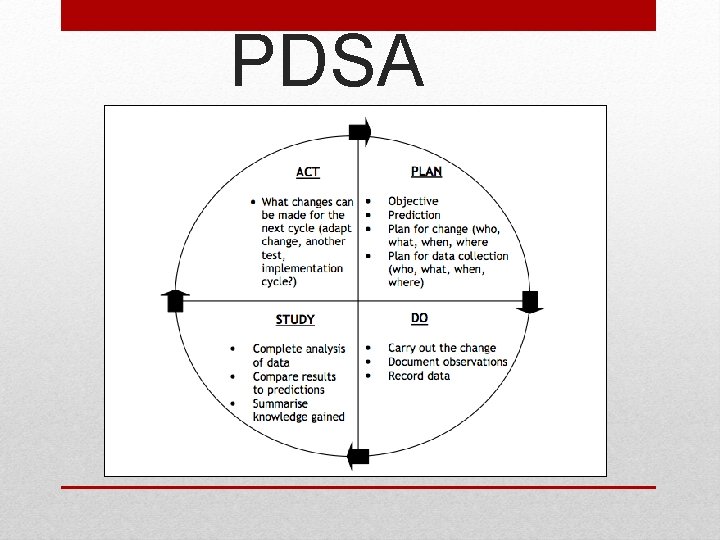
PDSA
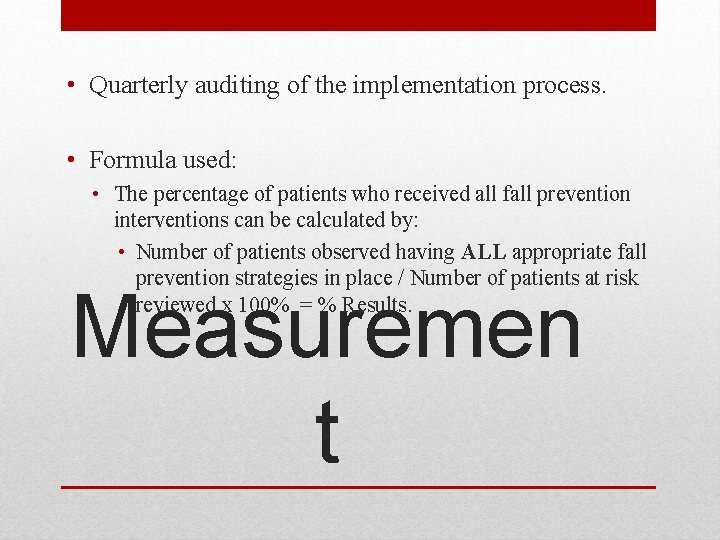
• Quarterly auditing of the implementation process. • Formula used: • The percentage of patients who received all fall prevention interventions can be calculated by: • Number of patients observed having ALL appropriate fall prevention strategies in place / Number of patients at risk reviewed x 100% = % Results. Measuremen t
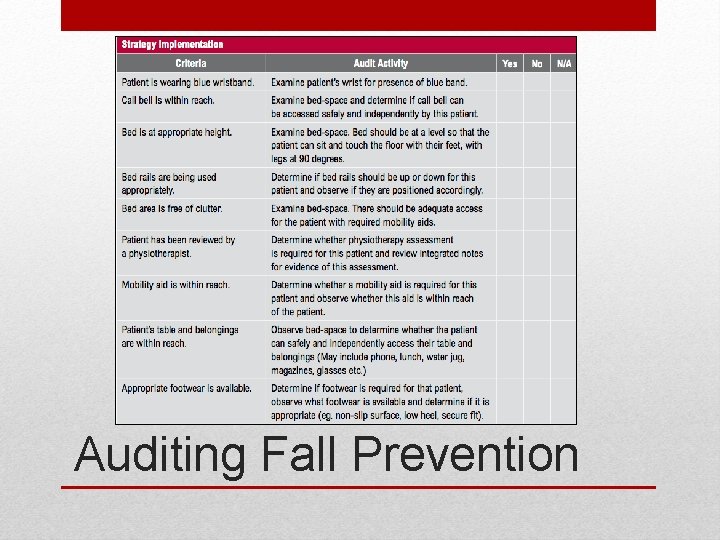
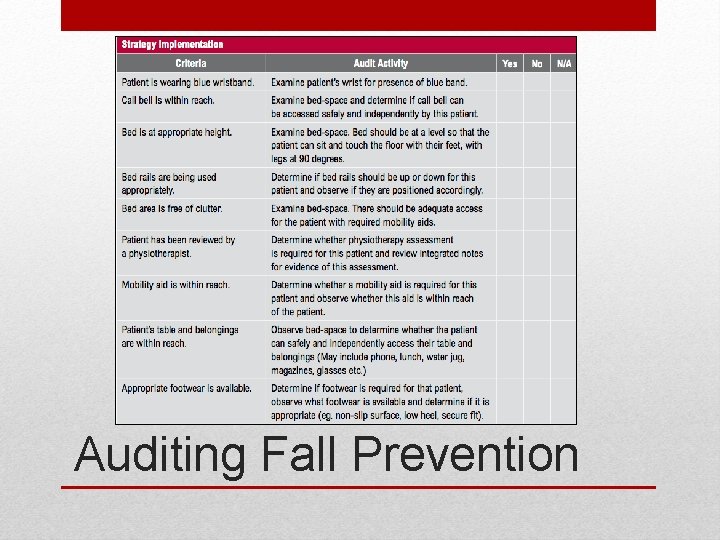
Auditing Fall Prevention
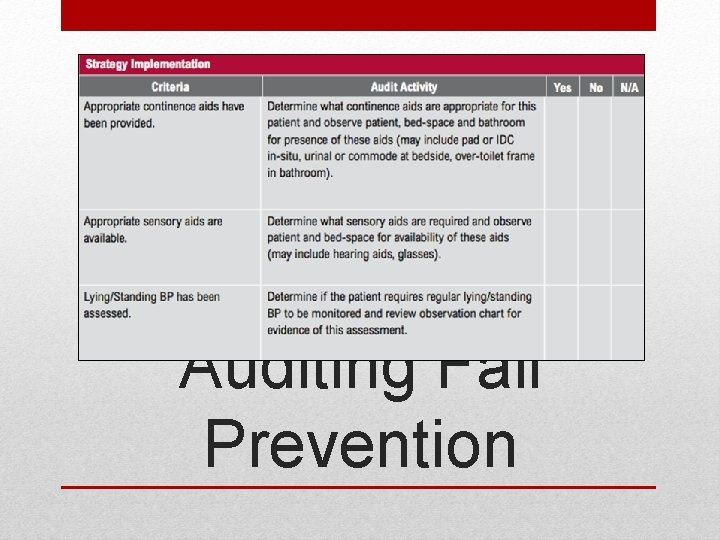
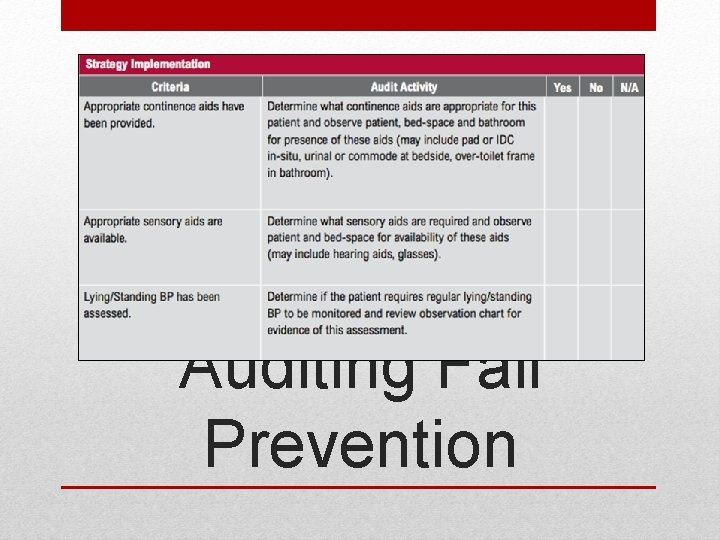
Auditing Fall Prevention
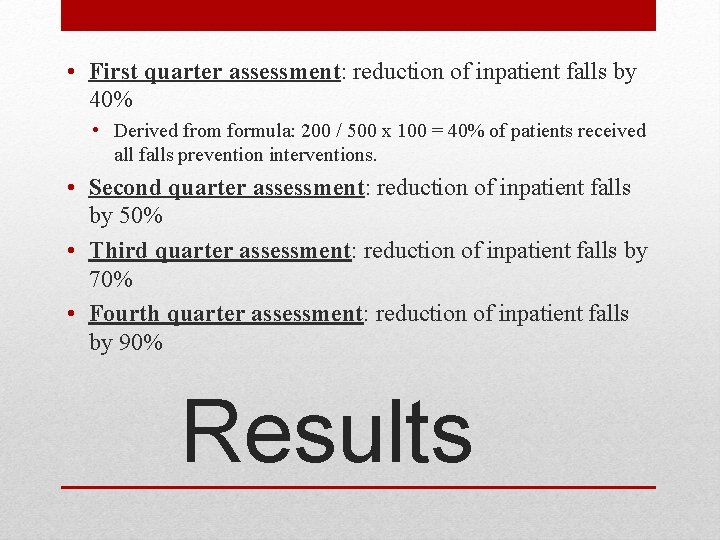
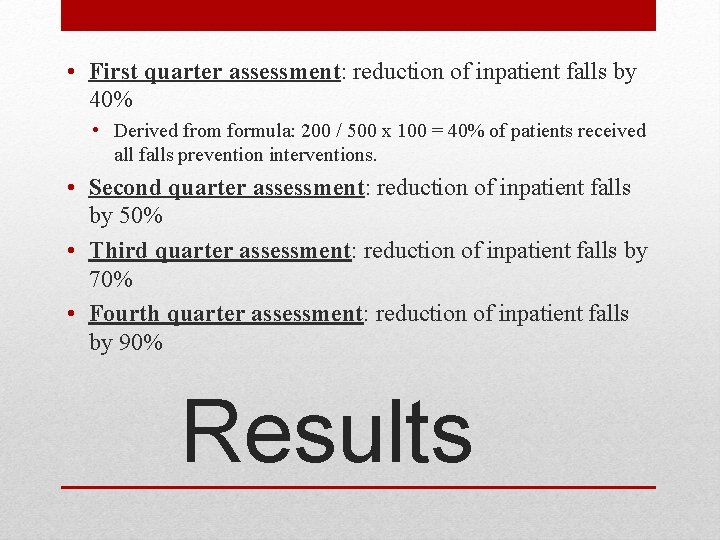
• First quarter assessment: reduction of inpatient falls by 40% • Derived from formula: 200 / 500 x 100 = 40% of patients received all falls prevention interventions. • Second quarter assessment: reduction of inpatient falls by 50% • Third quarter assessment: reduction of inpatient falls by 70% • Fourth quarter assessment: reduction of inpatient falls by 90% Results
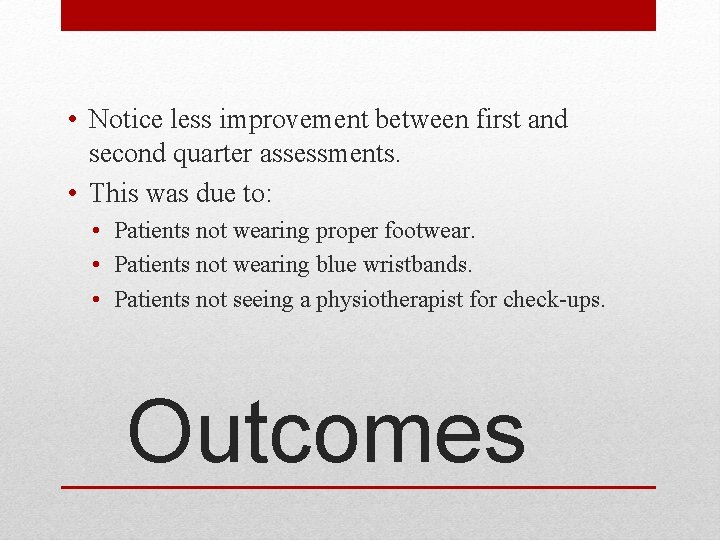
• Notice less improvement between first and second quarter assessments. • This was due to: • Patients not wearing proper footwear. • Patients not wearing blue wristbands. • Patients not seeing a physiotherapist for check-ups. Outcomes
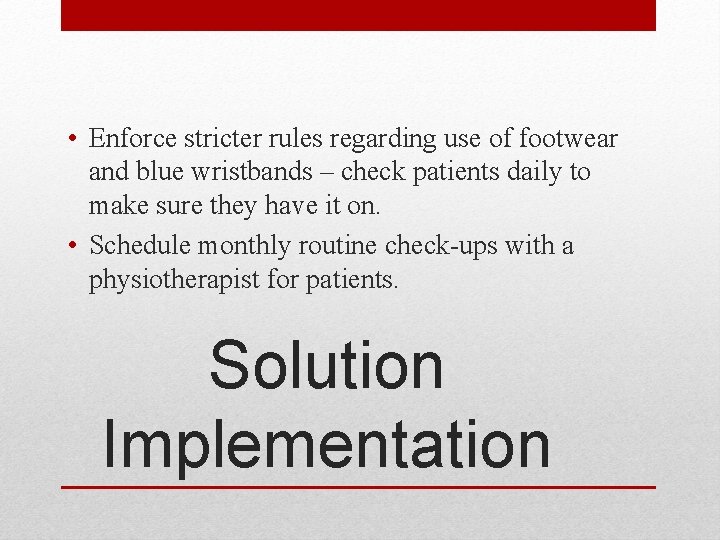
• Enforce stricter rules regarding use of footwear and blue wristbands – check patients daily to make sure they have it on. • Schedule monthly routine check-ups with a physiotherapist for patients. Solution Implementation
• Failure Mode and Effects Analysis (FMEA) • Proactive risk assessment • Prevents an adverse event • Close examination of a process • To help determine where improvements are needed • Reduces likelihood of adverse affects • Process in terms of: • What could go wrong? • If something does go wrong, what will be the result? • What needs to be done to prevent a bad outcome when something does go wrong? • Hospitals and nursing facilities that are accredited by The Joint Commission are required to periodically conduct a prospective risk assessment for patient safety improvement. Risk Assessment

• Narrowed focus to three (3) main areas: • Materials: • Education for patients about falls • Education for employees • Physical environment: • Keeping the beds low under a certain degree • Open floor plan in bedrooms • Workforce: • Patient to provider ratio • Adding information to charts regarding falls • Annually conduct risk assessment with every department: • Set goals: • Current: Reduction of 90% • Ultimate: No falls • Audit charts Process
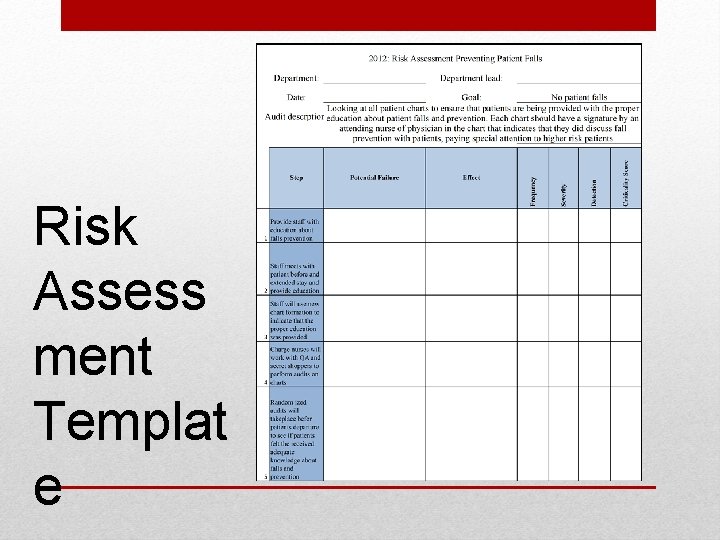
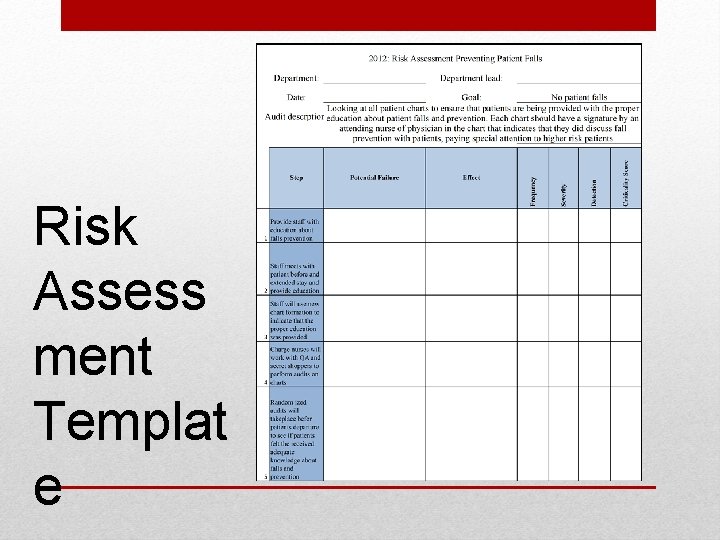
Risk Assess ment Templat e
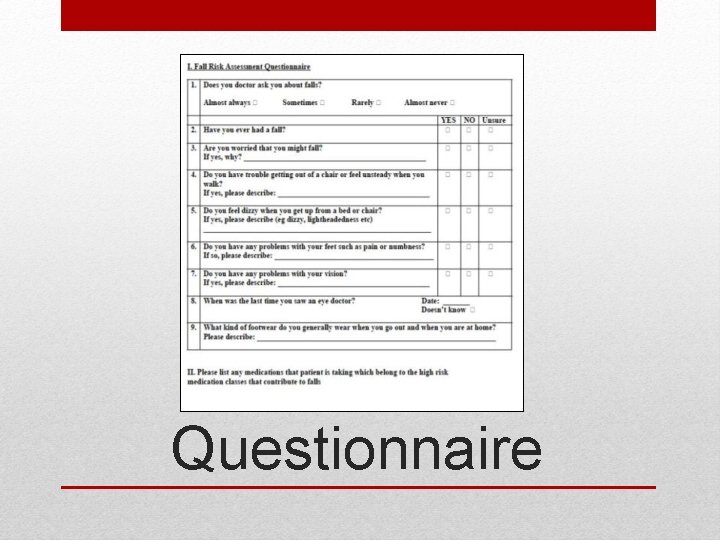
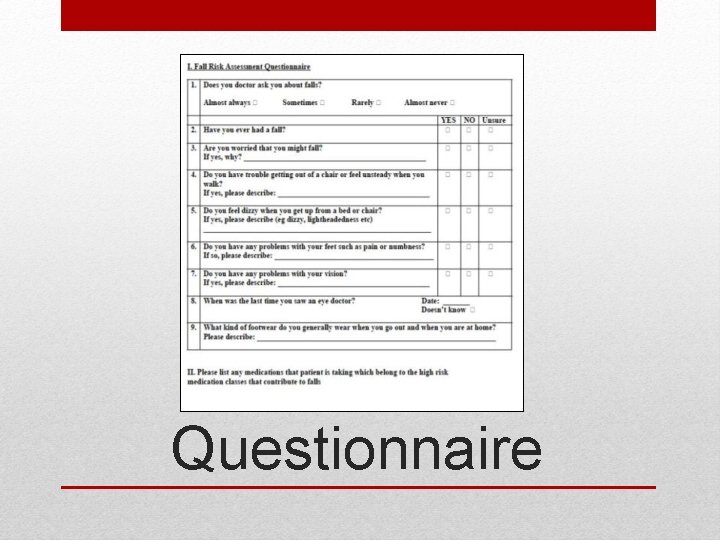
Audit Tool: Questionnaire
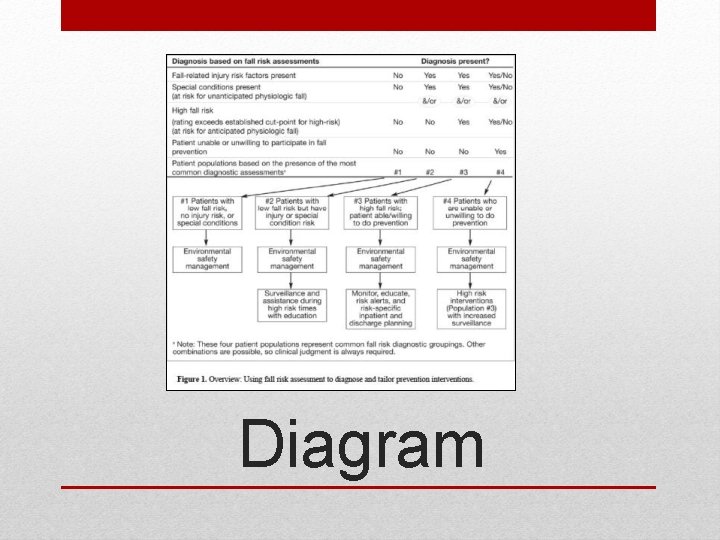
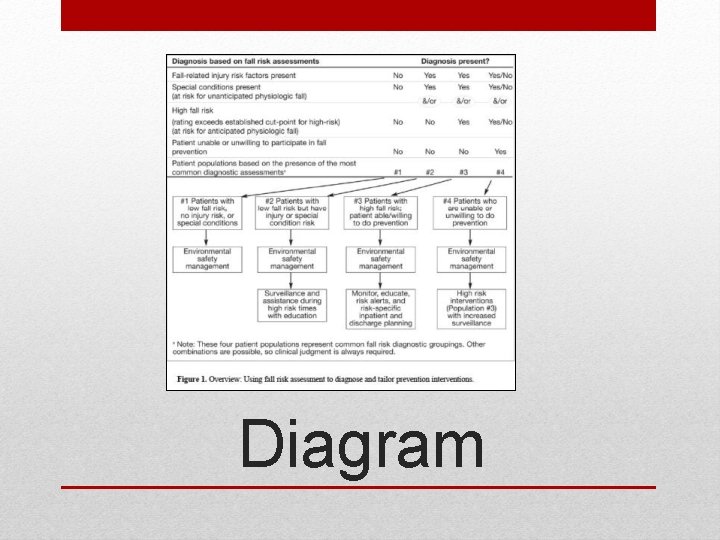
Audit Tool: Diagram
• Sun Coast RH faces a high risk of patient fall rate of 50% per 1, 000 patients annually. • The QI team aims to reduce the risk by 90%. • Conduct a fishbone analysis to find multiple causes and settled on three (3) that were of great significance. • Completed the FOCUS-PDSA model. • Conduct a risk assessment of patients. • Measured results using a formula and obtained outcomes of the interventions. • Reinforce interventions for patient falls and continued with QI process. Conclusion
 Zaira masood
Zaira masood Chris chien
Chris chien Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention Ahmed muhudiin ahmed
Ahmed muhudiin ahmed Masood mansoori
Masood mansoori Solving equations project
Solving equations project Examples of smart goals for fall prevention
Examples of smart goals for fall prevention Mullinure health and wellbeing centre
Mullinure health and wellbeing centre Chapter 14 fall prevention
Chapter 14 fall prevention Fallsafe care bundle
Fallsafe care bundle Fall prevention quiz
Fall prevention quiz Splatt falls history
Splatt falls history Fall prevention occupational therapy
Fall prevention occupational therapy Fall prevention interventions
Fall prevention interventions 5 ps of fall prevention
5 ps of fall prevention Post fall management guidelines
Post fall management guidelines Position chien de fusil
Position chien de fusil Máu chiên bò chúa không ưng
Máu chiên bò chúa không ưng Chien-chung shen
Chien-chung shen Andy chien
Andy chien Chien de garde chapter 4
Chien de garde chapter 4 Chiến thắng biên giới thu đông 1950 violet
Chiến thắng biên giới thu đông 1950 violet Dyssocialisation primaire
Dyssocialisation primaire Programmes tlvision ce soir
Programmes tlvision ce soir Harry potter mythologie
Harry potter mythologie Jai un chien
Jai un chien Chiến lược xuyên quốc gia của ikea
Chiến lược xuyên quốc gia của ikea Chiến lược marketing của lg
Chiến lược marketing của lg Máu chiên bò chúa không ưng
Máu chiên bò chúa không ưng Narcoleptsy
Narcoleptsy Minotaur surrealism
Minotaur surrealism Chiến thắng mtao mxây
Chiến thắng mtao mxây Joseph pasteur
Joseph pasteur Eric chien symantec
Eric chien symantec Sơ đồ chiến dịch điện biên phủ
Sơ đồ chiến dịch điện biên phủ Germaine berton
Germaine berton