PRIMI WITH MITRAL STENOSIS POSTED FOR ELECTIVE L
- Slides: 45
PRIMI WITH MITRAL STENOSIS POSTED FOR ELECTIVE L. S. C. S- CASE DISCUSSION BY DR. B. V. MAHESH BABU M. D. DESIGNATED PROFESSOR OF ANAESTHESIOLOGY, RANGARAYA MEDICAL COLLEGE, KAKINADA
WHAT ARE THE CARDIO VASCULAR CHANGES DURING PREGNANCY?
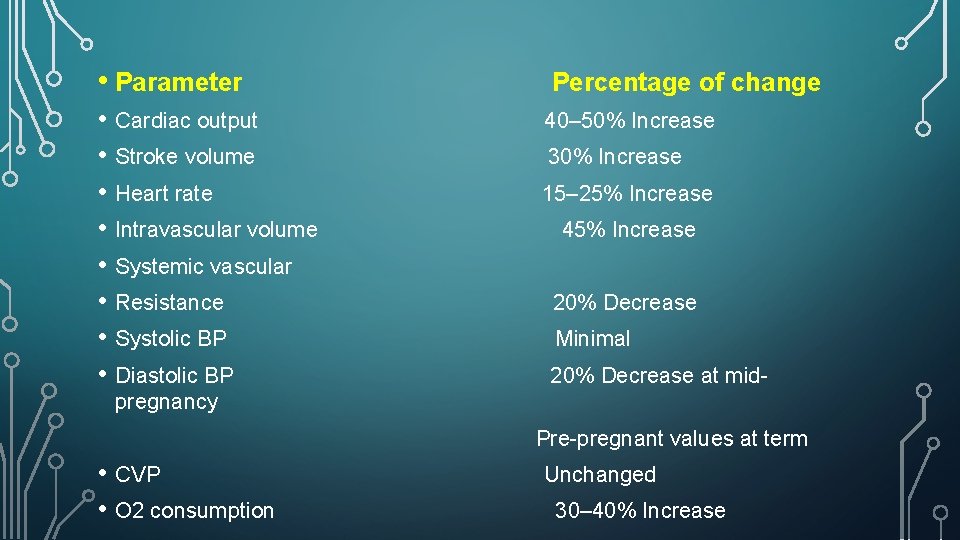
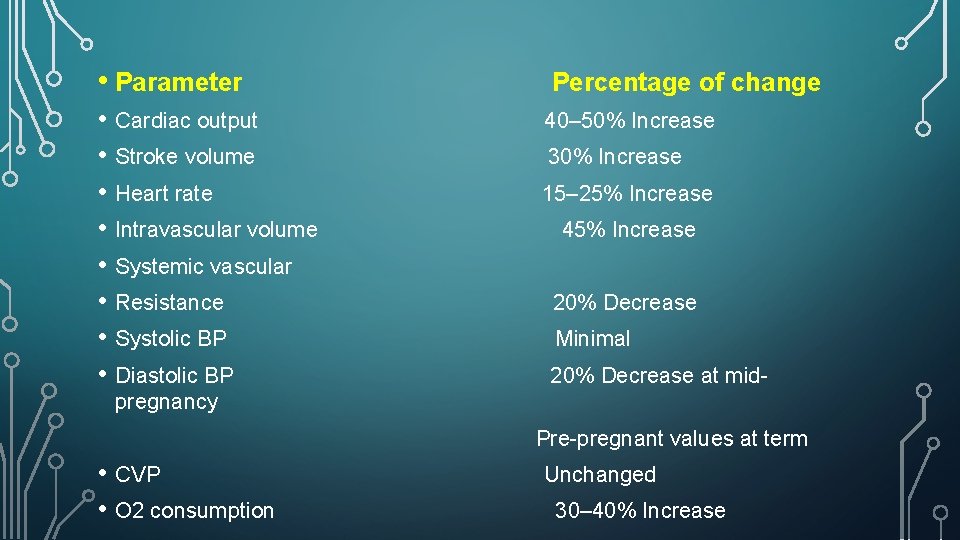
• Parameter • Cardiac output • Stroke volume • Heart rate • Intravascular volume • Systemic vascular • Resistance • Systolic BP • Diastolic BP Percentage of change 40– 50% Increase 30% Increase 15– 25% Increase 45% Increase 20% Decrease Minimal 20% Decrease at mid- pregnancy Pre-pregnant values at term • CVP • O 2 consumption Unchanged 30– 40% Increase
WHAT ARE THE COMMON CAUSES OF MITRAL STENOSIS ?
• Rheumatic fever is the most common cause of mitral stenosis (MS). • It is four times more common in women than men. • Only 50% of patients have a history of clinical evidence of acute rheumatic fever. • The other causes are Congenital ( Lutembacher syndrome-A. S. D with M. S) or calcification, SLE, Carcinoid , infiltrative disorders and Rheumatioid arthritis.
WHAT IS THE NORMAL COURSE OF A CASE OF MITRAL STENOSIS ?
• Thickened leaflets and fused commissures develop within 2 years after an acute attack. • Then, after an asymptomatic period lasting up to 20 years, acute congestive heart failure (CHF) may occur, brought on by an increase in either heart rate or cardiac output. • Approximately, 25% of women with mitral stenosis first experience symptoms during pregnancy.
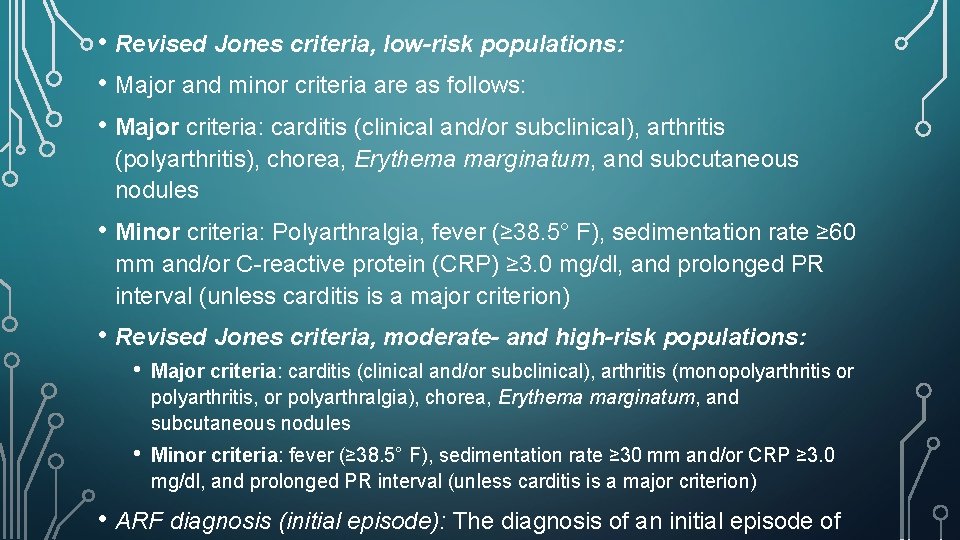
WHAT ARE REVISED JONES’ CRITERIA?
• Revised Jones criteria, low-risk populations: • Major and minor criteria are as follows: • Major criteria: carditis (clinical and/or subclinical), arthritis (polyarthritis), chorea, Erythema marginatum, and subcutaneous nodules • Minor criteria: Polyarthralgia, fever (≥ 38. 5° F), sedimentation rate ≥ 60 mm and/or C-reactive protein (CRP) ≥ 3. 0 mg/dl, and prolonged PR interval (unless carditis is a major criterion) • Revised Jones criteria, moderate- and high-risk populations: • Major criteria: carditis (clinical and/or subclinical), arthritis (monopolyarthritis or polyarthritis, or polyarthralgia), chorea, Erythema marginatum, and subcutaneous nodules • Minor criteria: fever (≥ 38. 5° F), sedimentation rate ≥ 30 mm and/or CRP ≥ 3. 0 mg/dl, and prolonged PR interval (unless carditis is a major criterion) • ARF diagnosis (initial episode): The diagnosis of an initial episode of
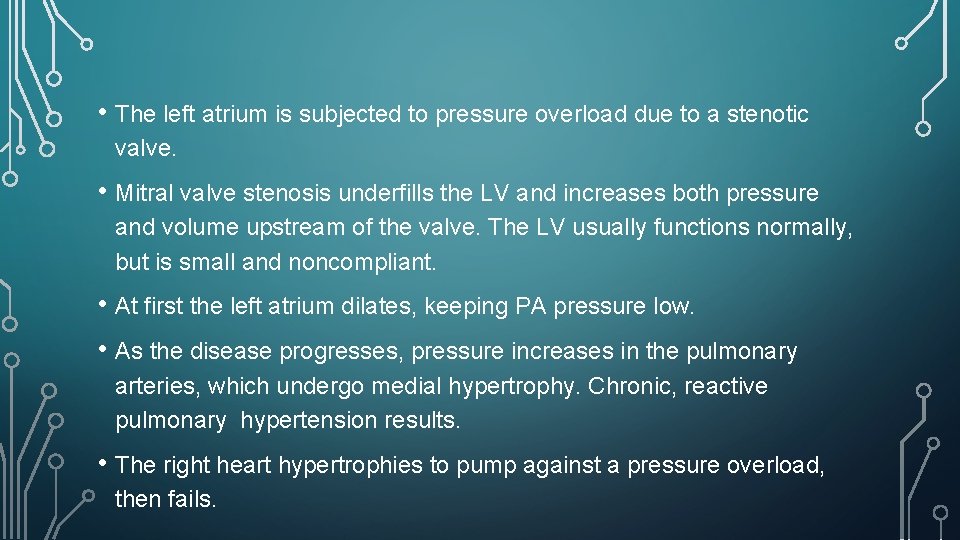
WHAT IS THE PATHOPHYSIOLOGY OF MITRAL STENOSIS ?
• The left atrium is subjected to pressure overload due to a stenotic valve. • Mitral valve stenosis underfills the LV and increases both pressure and volume upstream of the valve. The LV usually functions normally, but is small and noncompliant. • At first the left atrium dilates, keeping PA pressure low. • As the disease progresses, pressure increases in the pulmonary arteries, which undergo medial hypertrophy. Chronic, reactive pulmonary hypertension results. • The right heart hypertrophies to pump against a pressure overload, then fails.
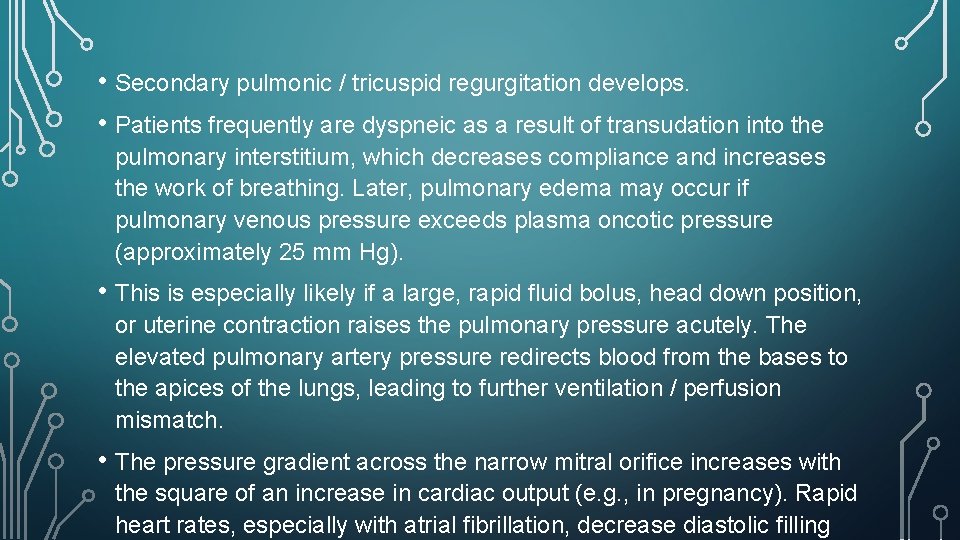
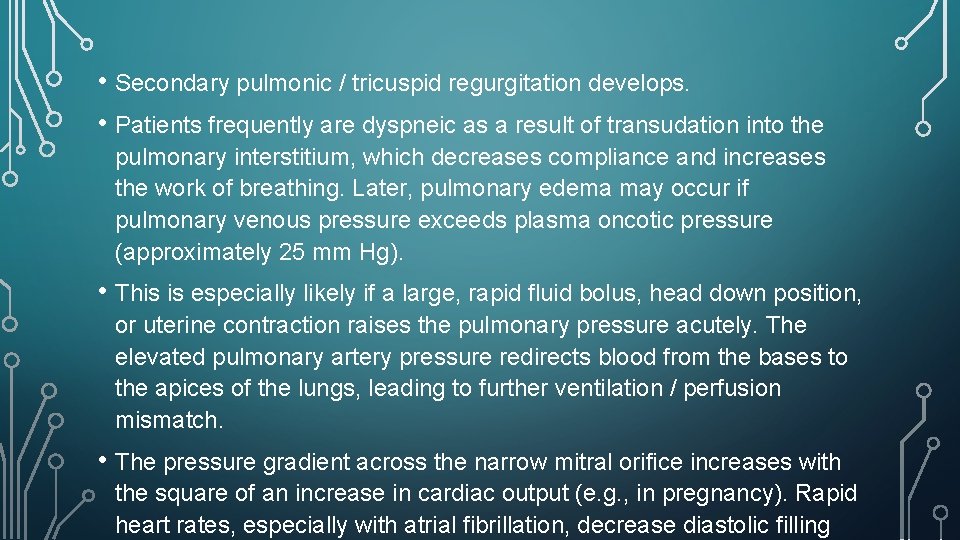
• Secondary pulmonic / tricuspid regurgitation develops. • Patients frequently are dyspneic as a result of transudation into the pulmonary interstitium, which decreases compliance and increases the work of breathing. Later, pulmonary edema may occur if pulmonary venous pressure exceeds plasma oncotic pressure (approximately 25 mm Hg). • This is especially likely if a large, rapid fluid bolus, head down position, or uterine contraction raises the pulmonary pressure acutely. The elevated pulmonary artery pressure redirects blood from the bases to the apices of the lungs, leading to further ventilation / perfusion mismatch. • The pressure gradient across the narrow mitral orifice increases with the square of an increase in cardiac output (e. g. , in pregnancy). Rapid heart rates, especially with atrial fibrillation, decrease diastolic filling
HOW IS THE RISK STRATIFICATION DONE IN THESE CASES( PREGNANT WOMEN WITH M. S) ?
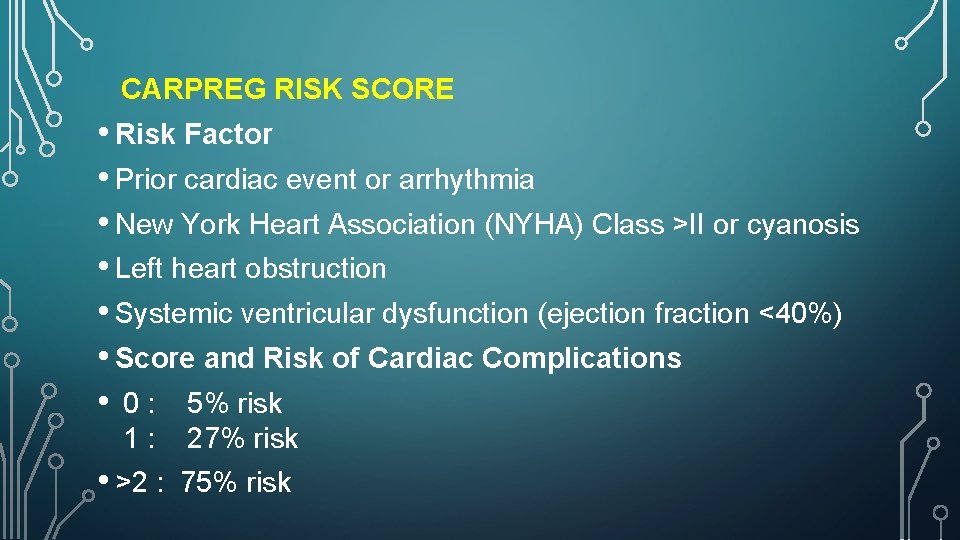
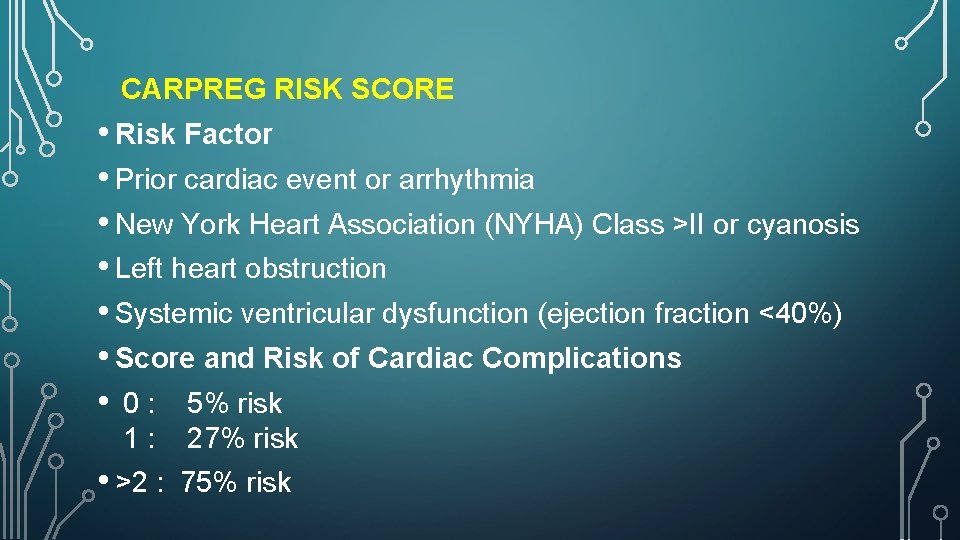
CARPREG RISK SCORE • Risk Factor • Prior cardiac event or arrhythmia • New York Heart Association (NYHA) Class >II or cyanosis • Left heart obstruction • Systemic ventricular dysfunction (ejection fraction <40%) • Score and Risk of Cardiac Complications • 0 : 5% risk 1: 27% risk • >2 : 75% risk
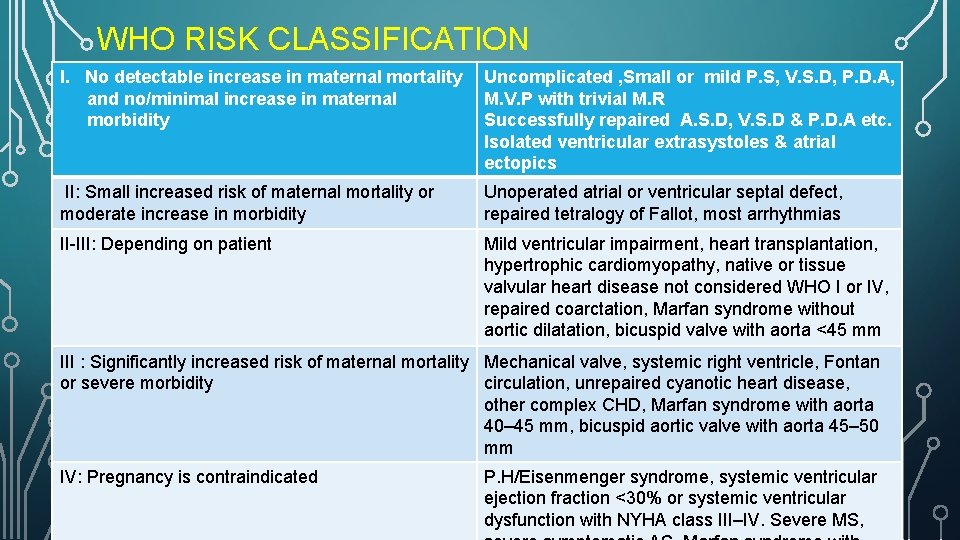
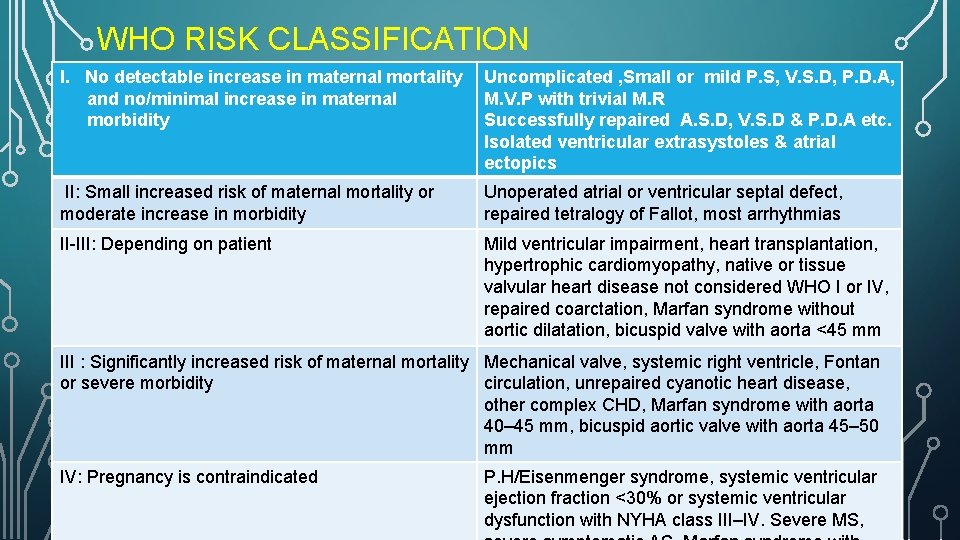
WHO RISK CLASSIFICATION I. No detectable increase in maternal mortality and no/minimal increase in maternal morbidity Uncomplicated , Small or mild P. S, V. S. D, P. D. A, M. V. P with trivial M. R Successfully repaired A. S. D, V. S. D & P. D. A etc. Isolated ventricular extrasystoles & atrial ectopics II: Small increased risk of maternal mortality or moderate increase in morbidity Unoperated atrial or ventricular septal defect, repaired tetralogy of Fallot, most arrhythmias II-III: Depending on patient Mild ventricular impairment, heart transplantation, hypertrophic cardiomyopathy, native or tissue valvular heart disease not considered WHO I or IV, repaired coarctation, Marfan syndrome without aortic dilatation, bicuspid valve with aorta <45 mm III : Significantly increased risk of maternal mortality Mechanical valve, systemic right ventricle, Fontan or severe morbidity circulation, unrepaired cyanotic heart disease, other complex CHD, Marfan syndrome with aorta 40– 45 mm, bicuspid aortic valve with aorta 45– 50 mm IV: Pregnancy is contraindicated P. H/Eisenmenger syndrome, systemic ventricular ejection fraction <30% or systemic ventricular dysfunction with NYHA class III–IV. Severe MS,
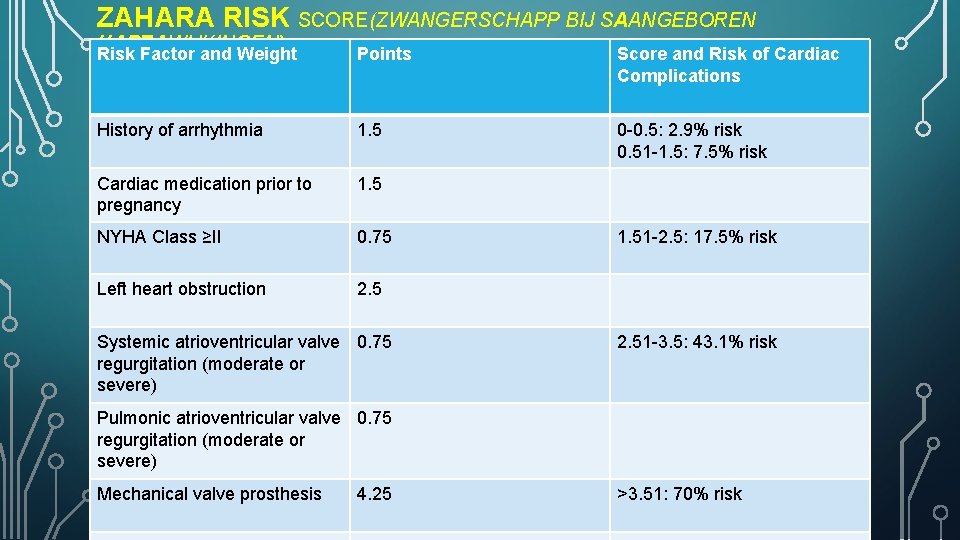
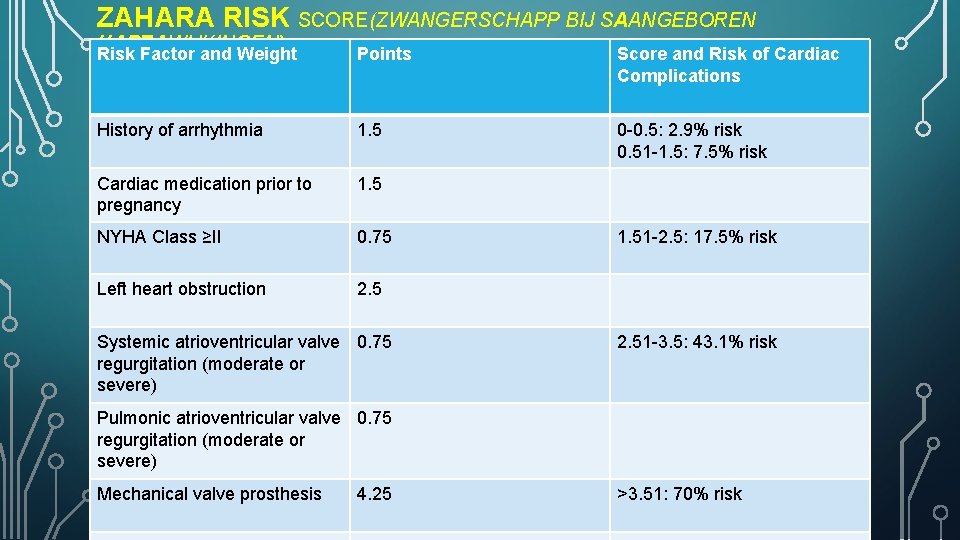
ZAHARA RISK SCORE(ZWANGERSCHAPP BIJ SAANGEBOREN HARTAWIJKINGEN) Risk Factor and Weight Points Score and Risk of Cardiac Complications History of arrhythmia 1. 5 0 -0. 5: 2. 9% risk 0. 51 -1. 5: 7. 5% risk Cardiac medication prior to pregnancy 1. 5 NYHA Class ≥II 0. 75 Left heart obstruction 2. 5 Systemic atrioventricular valve 0. 75 regurgitation (moderate or severe) 1. 51 -2. 5: 17. 5% risk 2. 51 -3. 5: 43. 1% risk Pulmonic atrioventricular valve 0. 75 regurgitation (moderate or severe) Mechanical valve prosthesis 4. 25 >3. 51: 70% risk
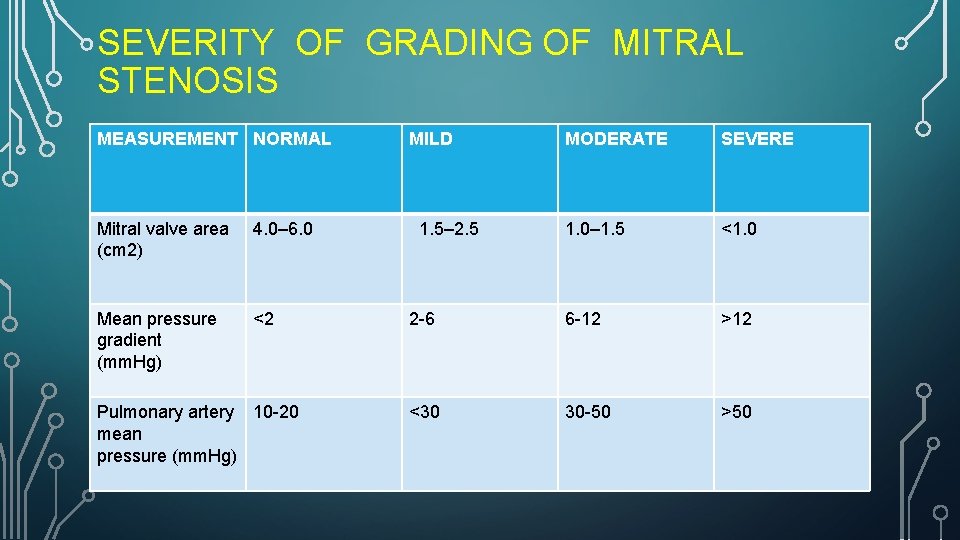
HOW DO YOU CLASSIFY THE SEVERITY OF MITRAL STENOSIS?
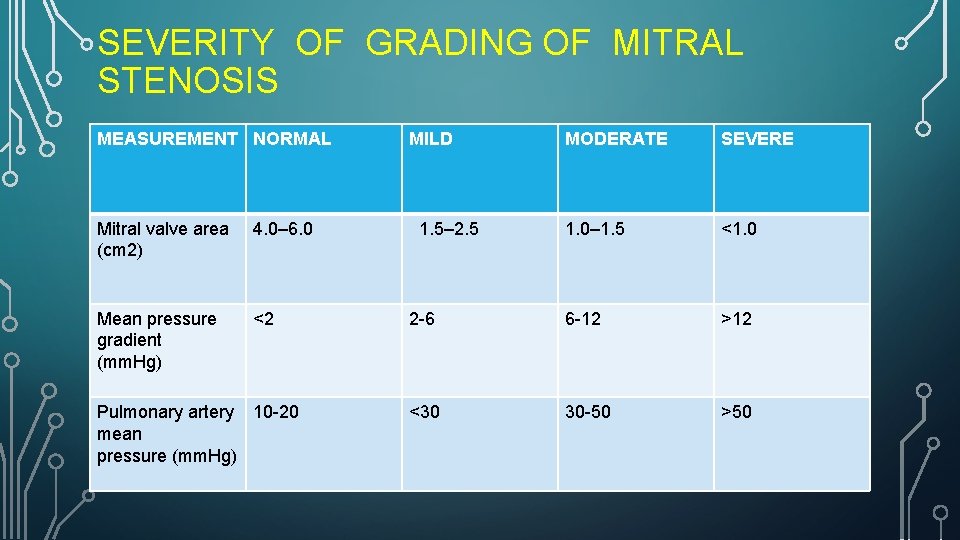
SEVERITY OF GRADING OF MITRAL STENOSIS MEASUREMENT NORMAL Mitral valve area (cm 2) 4. 0– 6. 0 Mean pressure gradient (mm. Hg) <2 Pulmonary artery 10 -20 mean pressure (mm. Hg) MILD MODERATE SEVERE 1. 0– 1. 5 <1. 0 2 -6 6 -12 >12 <30 30 -50 >50 1. 5– 2. 5
WHAT IS AHA/ ACC STAGING OF MITRAL STENOSIS?
AHA / ACC STAGING OF M. S
WHAT ARE THE CLINICAL SYMPTOMS & SIGNS OF M. S?
• Symptoms include breathlessness, orthopnea, Paroxysmal nocturnal dyspnea, hemoptysis, chest pain and palpitations. Breathlessness is due to fluid transudation into the lungs, decreasing lung compliance and increasing the work of breathing. A mitral valve area > 1. 5 cm 2 usually does not cause symptoms at rest. As severity of stenosis increases, patients develop decreased exercise tolerance and breathlessness. • Signs include reduced pulse pressure, raised jugular venous pressure, right parasternal heave, mid-diastolic murmur with presystolic accentuation, loud S 1, opening snap, crepitations, tricuspid murmur, hepatomegaly, ascites and pedal edema. • In pregnancy , disproportionate or unexplained dyspnea with pathological murmur , Paroxysmal nocturnal dyspnea, hemoptysis and syncope –are not physiological and suggestive of some valvular
WHAT INVESTIGATIONS YOU ORDER IN THIS CASE?
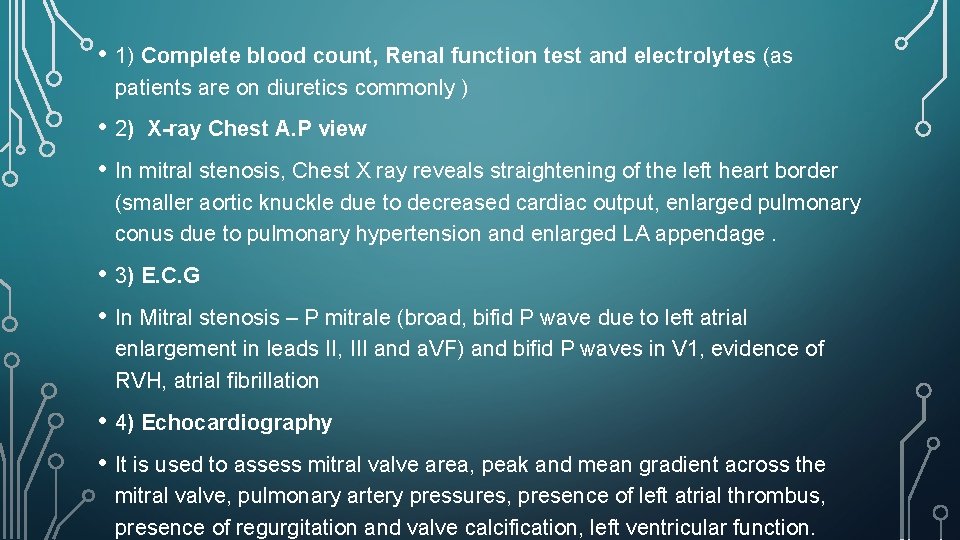
• 1) Complete blood count, Renal function test and electrolytes (as patients are on diuretics commonly ) • 2) X-ray Chest A. P view • In mitral stenosis, Chest X ray reveals straightening of the left heart border (smaller aortic knuckle due to decreased cardiac output, enlarged pulmonary conus due to pulmonary hypertension and enlarged LA appendage. • 3) E. C. G • In Mitral stenosis – P mitrale (broad, bifid P wave due to left atrial enlargement in leads II, III and a. VF) and bifid P waves in V 1, evidence of RVH, atrial fibrillation • 4) Echocardiography • It is used to assess mitral valve area, peak and mean gradient across the mitral valve, pulmonary artery pressures, presence of left atrial thrombus, presence of regurgitation and valve calcification, left ventricular function.
WHAT IS WILKINS SCORE?
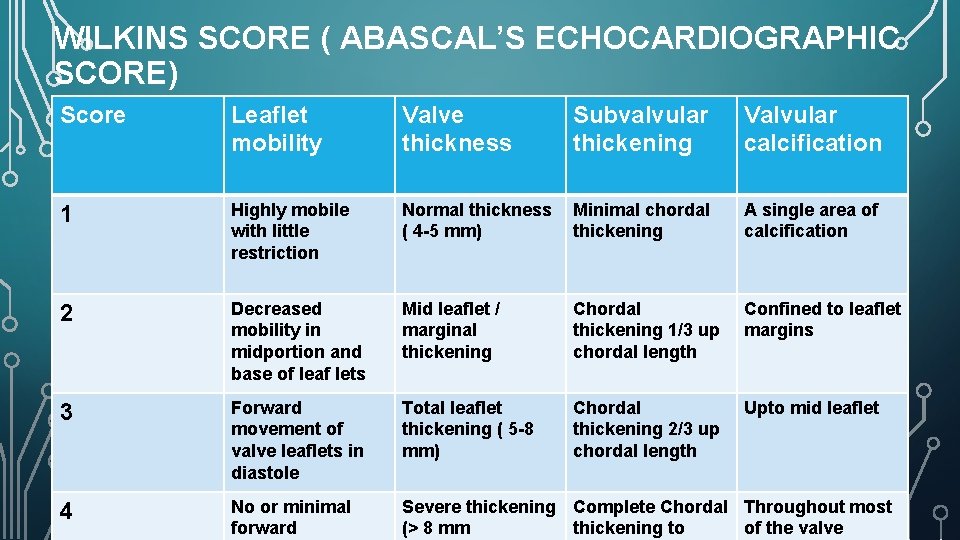
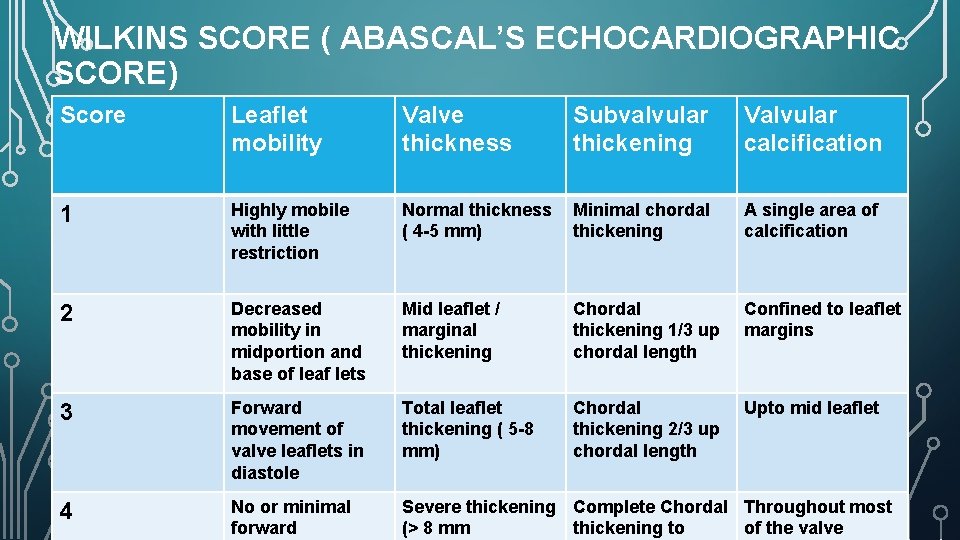
WILKINS SCORE ( ABASCAL’S ECHOCARDIOGRAPHIC SCORE) Score Leaflet mobility Valve thickness Subvalvular thickening Valvular calcification 1 Highly mobile with little restriction Normal thickness ( 4 -5 mm) Minimal chordal thickening A single area of calcification 2 Decreased mobility in midportion and base of leaf lets Mid leaflet / marginal thickening Chordal thickening 1/3 up chordal length Confined to leaflet margins 3 Forward movement of valve leaflets in diastole Total leaflet thickening ( 5 -8 mm) Chordal thickening 2/3 up chordal length Upto mid leaflet 4 No or minimal forward Severe thickening Complete Chordal Throughout most (> 8 mm thickening to of the valve
HOW DO YOU OPTIMIZE THIS PATIENT PRE -OPERATIVELY?
• Many patients with moderate or severe mitral stenosis can be managed successfully with medical therapy, which includes strict control of heart rate, volume status and frequent monitoring. The two goals of medical therapy are to reduce the heart rate and reduce the left atrial pressure. • Heart rate reduction can be achieved with beta blockers -Metoprolol or bisoprolol are preferred. • Digoxin can be used in patients with atrial fibrillation for control of ventricular rate and is generally considered safer, well tolerated and has few adverse fetal effects. Amiodarone is contraindicated during pregnancy and should not be used for control of ventricular rate. • Reduction in left atrial pressure is achieved by the use of diuretics. (avoid uteroplacental hypoperfusion ) • Prophylactic anticoagulation with UFH, LMWH, or Vitamin K antagonist (VKA)
WHAT ARE THE GOALS TO AIM FOR IN ANAESTHETIC MANAGEMENT OF PREGNANT WOMAN WITH M. S?
• Prevent rapid ventricular rates • Sinus tachycardia should be corrected immediately by reversing the precipitating event (pain, anxiety, light general anesthesia, hypovolemia, hypercarbia, acidosis) or by administering beta blockers intravenously. • Minimize increase in central blood volume • Over transfusion, Trendelenburg position, or autotransfusion via uterine contraction can precipitate pulmonary edema, right ventricular failure or atrial fibrillation. • • Avoid marked decreases in SVR Marked decrease in SVR is not well tolerated. Decreases in SVR are compensated by increases in heart rate (as stroke volume is fixed). • Prevent increases in pulmonary artery pressure Hypercarbia, hypoxia, acidosis, lung hyperinflation or increased lung water can increase PVR.
WHAT IS THE SURGICAL MANAGEMENT FOR MITRAL VALVULAR DISEASE IN PREGNANCY?
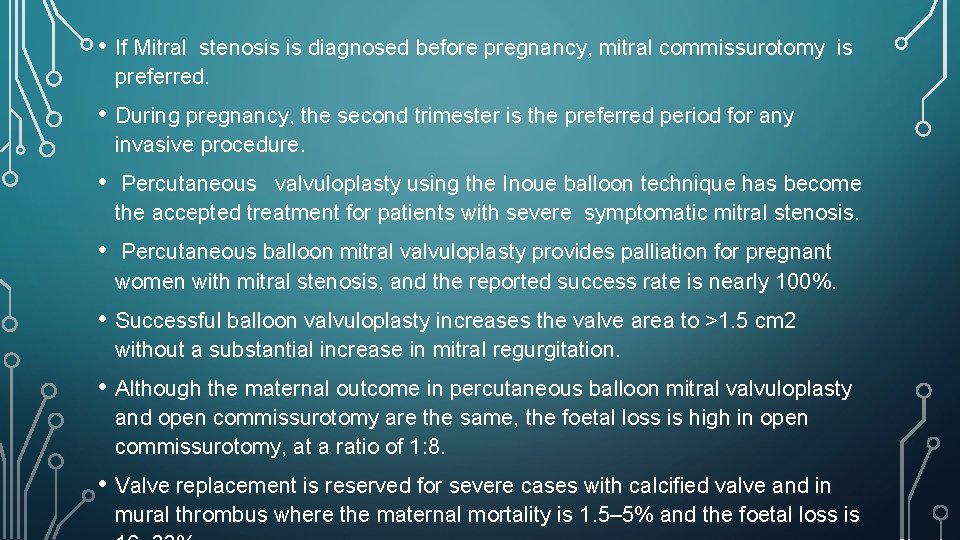
• If Mitral stenosis is diagnosed before pregnancy, mitral commissurotomy is preferred. • During pregnancy, the second trimester is the preferred period for any invasive procedure. • Percutaneous valvuloplasty using the Inoue balloon technique has become the accepted treatment for patients with severe symptomatic mitral stenosis. • Percutaneous balloon mitral valvuloplasty provides palliation for pregnant women with mitral stenosis, and the reported success rate is nearly 100%. • Successful balloon valvuloplasty increases the valve area to >1. 5 cm 2 without a substantial increase in mitral regurgitation. • Although the maternal outcome in percutaneous balloon mitral valvuloplasty and open commissurotomy are the same, the foetal loss is high in open commissurotomy, at a ratio of 1: 8. • Valve replacement is reserved for severe cases with calcified valve and in mural thrombus where the maternal mortality is 1. 5– 5% and the foetal loss is
HOW DO YOU PLAN FOR LABOUR ANALGESIA FOR THIS PATIENT?
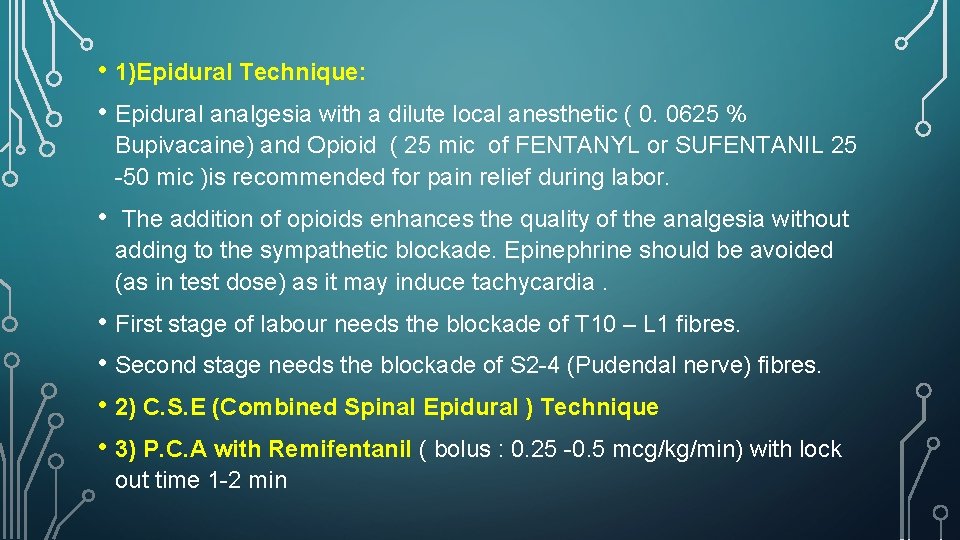
• 1)Epidural Technique: • Epidural analgesia with a dilute local anesthetic ( 0. 0625 % Bupivacaine) and Opioid ( 25 mic of FENTANYL or SUFENTANIL 25 -50 mic )is recommended for pain relief during labor. • The addition of opioids enhances the quality of the analgesia without adding to the sympathetic blockade. Epinephrine should be avoided (as in test dose) as it may induce tachycardia. • First stage of labour needs the blockade of T 10 – L 1 fibres. • Second stage needs the blockade of S 2 -4 (Pudendal nerve) fibres. • 2) C. S. E (Combined Spinal Epidural ) Technique • 3) P. C. A with Remifentanil ( bolus : 0. 25 -0. 5 mcg/kg/min) with lock out time 1 -2 min
WHAT IS THE PLAN OF ANAESTHESIA FOR THIS PATIENT COMING FOR AN ELECTIVE CAESAREAN SECTION?
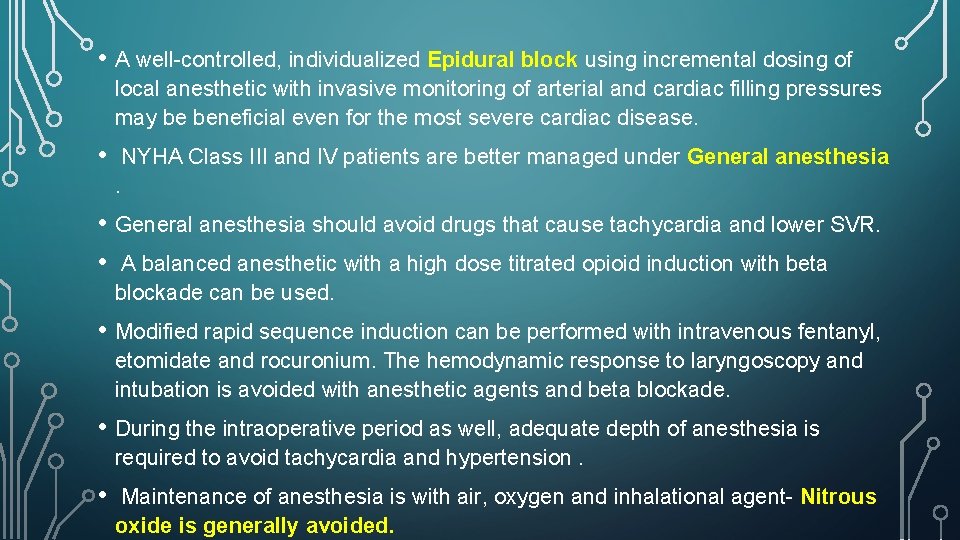
• A well-controlled, individualized Epidural block using incremental dosing of local anesthetic with invasive monitoring of arterial and cardiac filling pressures may be beneficial even for the most severe cardiac disease. • NYHA Class III and IV patients are better managed under General anesthesia. • General anesthesia should avoid drugs that cause tachycardia and lower SVR. • A balanced anesthetic with a high dose titrated opioid induction with beta blockade can be used. • Modified rapid sequence induction can be performed with intravenous fentanyl, etomidate and rocuronium. The hemodynamic response to laryngoscopy and intubation is avoided with anesthetic agents and beta blockade. • During the intraoperative period as well, adequate depth of anesthesia is required to avoid tachycardia and hypertension. • Maintenance of anesthesia is with air, oxygen and inhalational agent- Nitrous oxide is generally avoided.
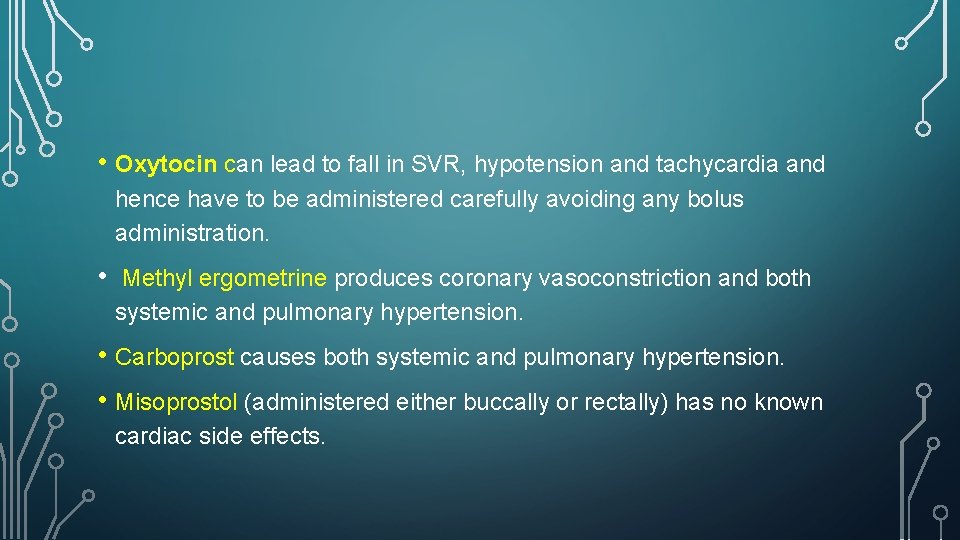
WHAT ARE THE EFFECTS OF THE UTEROTONIC DRUGS IN THIS PATIENT WITH M. S ?
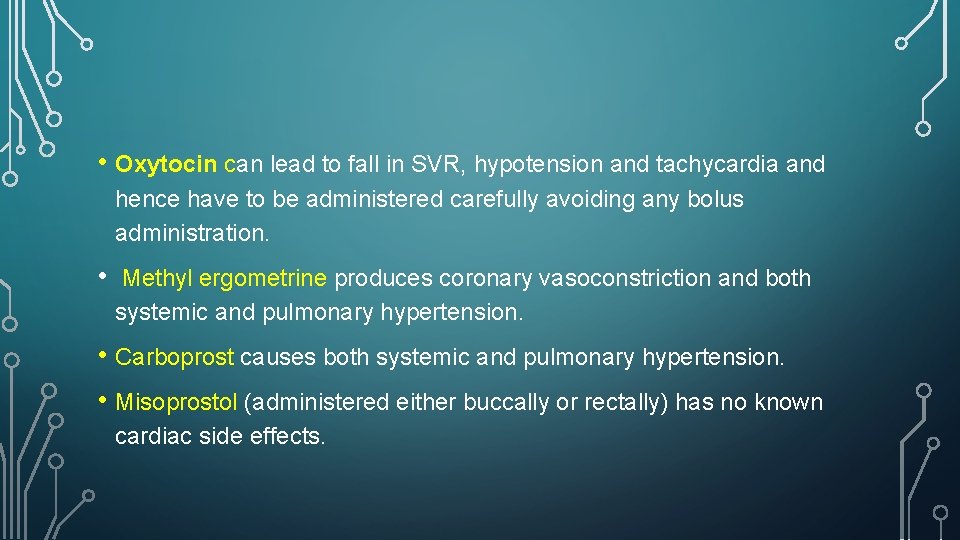
• Oxytocin can lead to fall in SVR, hypotension and tachycardia and hence have to be administered carefully avoiding any bolus administration. • Methyl ergometrine produces coronary vasoconstriction and both systemic and pulmonary hypertension. • Carboprost causes both systemic and pulmonary hypertension. • Misoprostol (administered either buccally or rectally) has no known cardiac side effects.
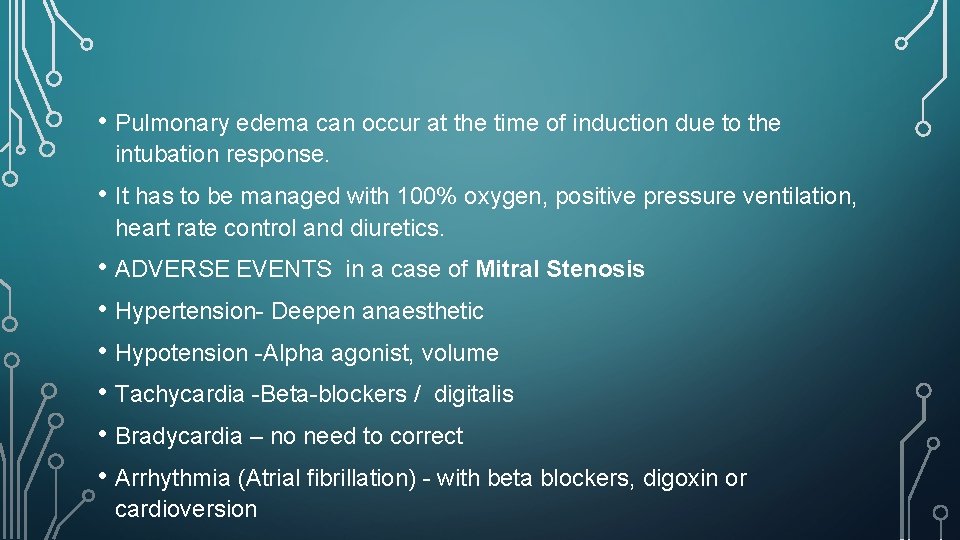
WHAT ARE THE COMMON INTRA OPERATIVE COMPLICATIONS & HOW DO YOU MANAGE THEM ?
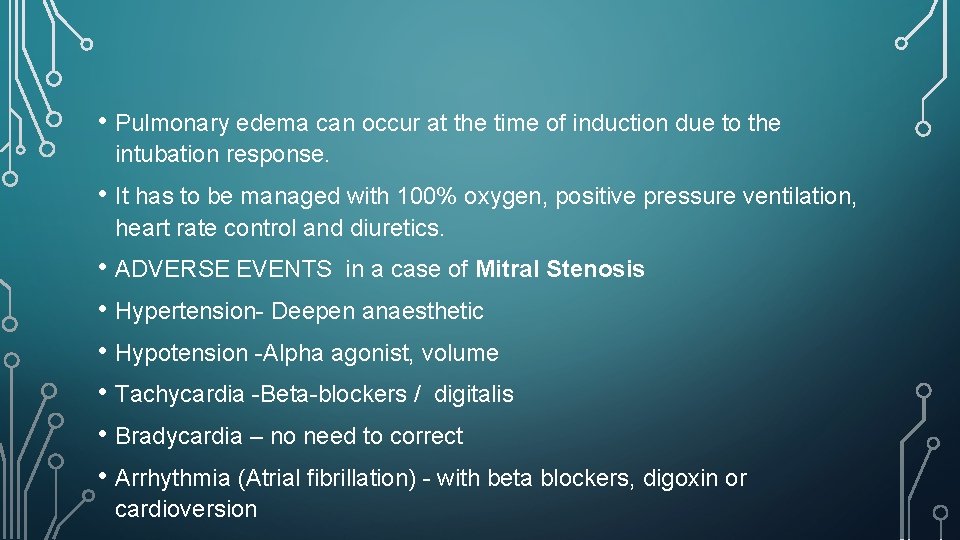
• Pulmonary edema can occur at the time of induction due to the intubation response. • It has to be managed with 100% oxygen, positive pressure ventilation, heart rate control and diuretics. • ADVERSE EVENTS in a case of Mitral Stenosis • Hypertension- Deepen anaesthetic • Hypotension -Alpha agonist, volume • Tachycardia -Beta-blockers / digitalis • Bradycardia – no need to correct • Arrhythmia (Atrial fibrillation) - with beta blockers, digoxin or cardioversion
HOW DO YOU MANAGE ANTICOAGULANTS DURING PREGNANCY?
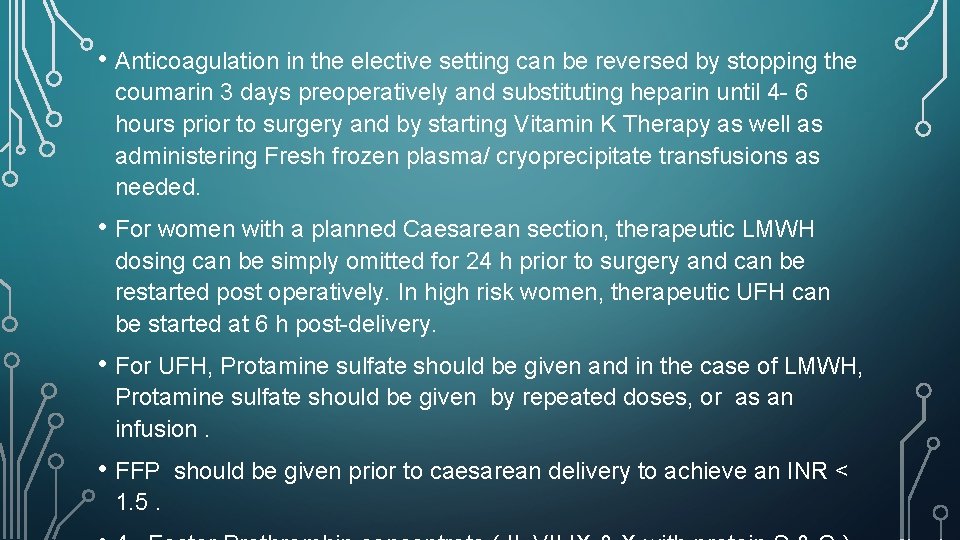
• Anticoagulation in the elective setting can be reversed by stopping the coumarin 3 days preoperatively and substituting heparin until 4 - 6 hours prior to surgery and by starting Vitamin K Therapy as well as administering Fresh frozen plasma/ cryoprecipitate transfusions as needed. • For women with a planned Caesarean section, therapeutic LMWH dosing can be simply omitted for 24 h prior to surgery and can be restarted post operatively. In high risk women, therapeutic UFH can be started at 6 h post-delivery. • For UFH, Protamine sulfate should be given and in the case of LMWH, Protamine sulfate should be given by repeated doses, or as an infusion. • FFP 1. 5. should be given prior to caesarean delivery to achieve an INR <
HOW DO YOU MANAGE THIS PATIENT POST OPERATIVELY?
• Patients with moderate to severe mitral stenosis need to be monitored post-operatively in an intensive care unit. • Those who were taken up for Caesarean with NYHA Class III-IV symptoms benefit from postoperative mechanical ventilation. • Analgesia, restricted fluid administration and hemodynamic monitoring should continue in the postoperative period. • Epidural analgesia is preferred, provided coagulation profile is good.
THANK YOU FOR YOUR ATTENTION ! WISH YOU ALL THE BEST