PLEURAL DISEASE Sevda zdoan MD Chest Diseases Pleural






- Slides: 47
PLEURAL DISEASE Sevda Özdoğan MD, Chest Diseases
Ø Pleural effusions Ø Emphyema Ø Pleural malignancy Ø Hemothorax Ø Pneumothorax
Pleural Anatomy and Physiology Ø Pleura is a serous membrane formed from mesenchyme that separates the lung paranchym, mediastinum, diaphragm and thoracic cage Ø It is composed of 2 layers as: l l Parietal pleura Visceral pleura
Pleural Cavity Ø It is the space between the visseral and parietal pleura Ø Normally contains a small amount of fluid (10 -20 ml in each pleural cavity) Ø This pleural fluid is mainly produced by the parietal pleural surface and reabsorbed by the two layers (Mainly parietal pleura)
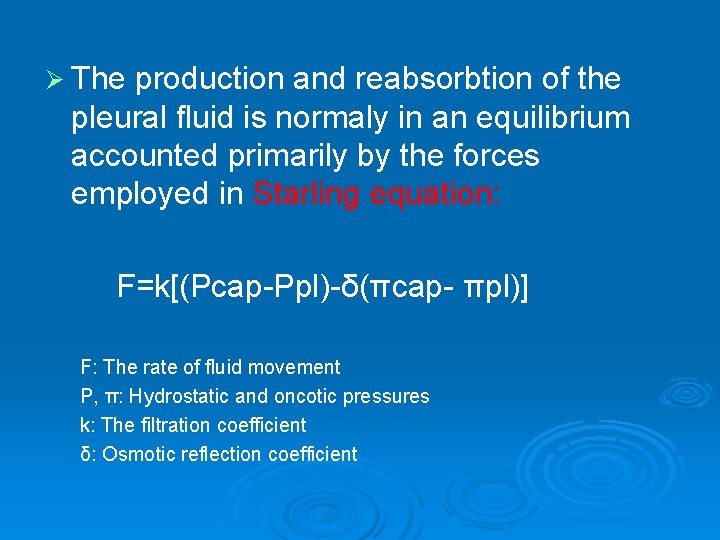
Ø The production and reabsorbtion of the pleural fluid is normaly in an equilibrium accounted primarily by the forces employed in Starling equation: F=k[(Pcap-Ppl)-δ(πcap- πpl)] F: The rate of fluid movement P, π: Hydrostatic and oncotic pressures k: The filtration coefficient δ: Osmotic reflection coefficient
Pleural Effusion Ø If the physiologic balance between the filtration and the drainage of the pleural fluid is disturbed, pleural effusion accumulate. Ø Fluid may accumulate in the pleural space in response to the disease of the pleural membranes or as a manifestation of a systemic illness
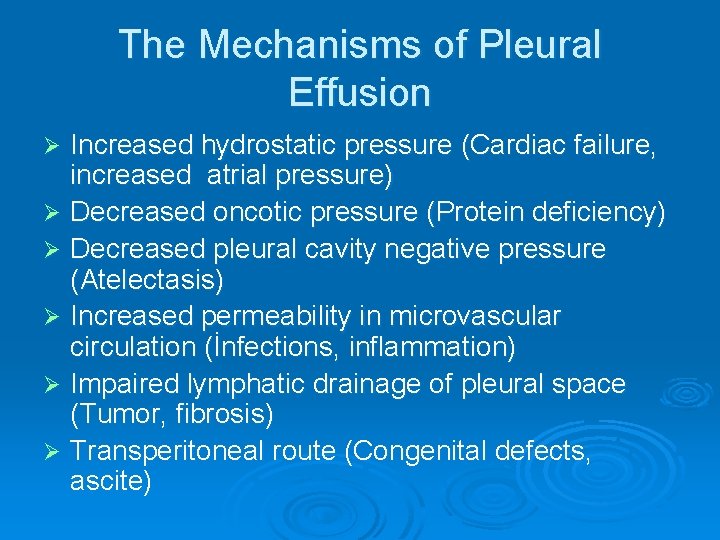
The Mechanisms of Pleural Effusion Increased hydrostatic pressure (Cardiac failure, increased atrial pressure) Ø Decreased oncotic pressure (Protein deficiency) Ø Decreased pleural cavity negative pressure (Atelectasis) Ø Increased permeability in microvascular circulation (İnfections, inflammation) Ø Impaired lymphatic drainage of pleural space (Tumor, fibrosis) Ø Transperitoneal route (Congenital defects, ascite) Ø
Symptoms Ø Chest pain (inspiratory) l Decreases when the fluid increases Ø Dyspnea Ø Cough Ø Symptoms of the underlying disease l l Fever Hemoptysis Weight loss. . .
Physical Examination Ø No physical signs can be detected when the fluid is less than 300 ml Ø İnspection l l İncreased size of the affected hemithorax Trachea is deviated away from the diseased side
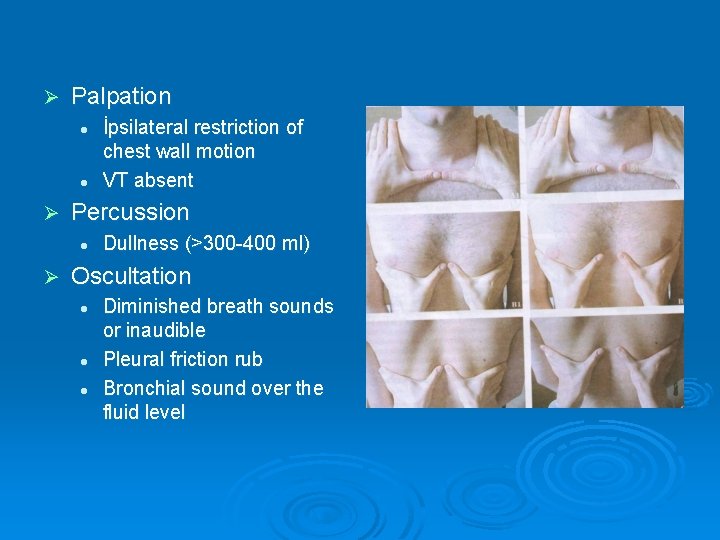
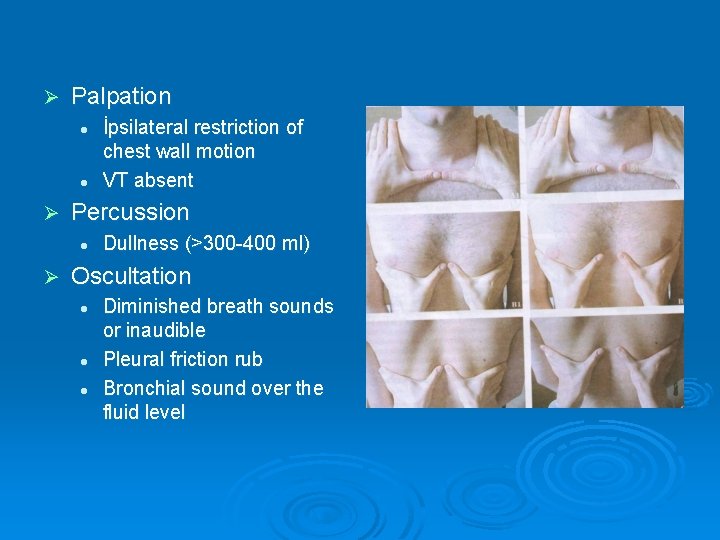
Ø Palpation l l Ø Percussion l Ø İpsilateral restriction of chest wall motion VT absent Dullness (>300 -400 ml) Oscultation l l l Diminished breath sounds or inaudible Pleural friction rub Bronchial sound over the fluid level
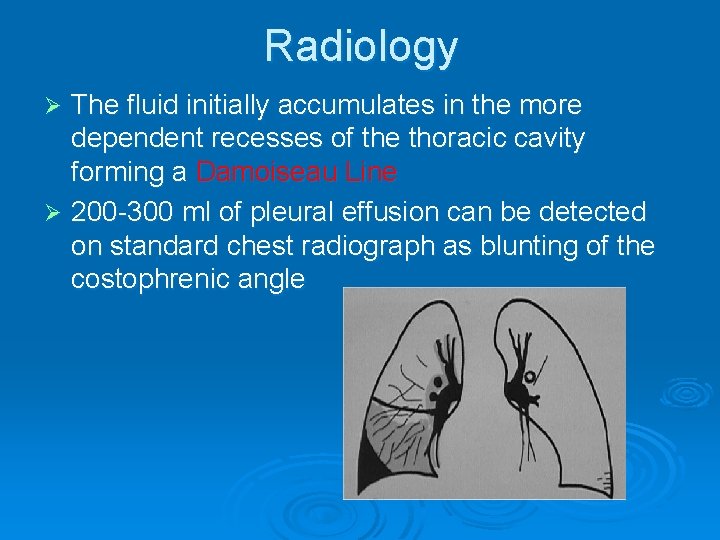
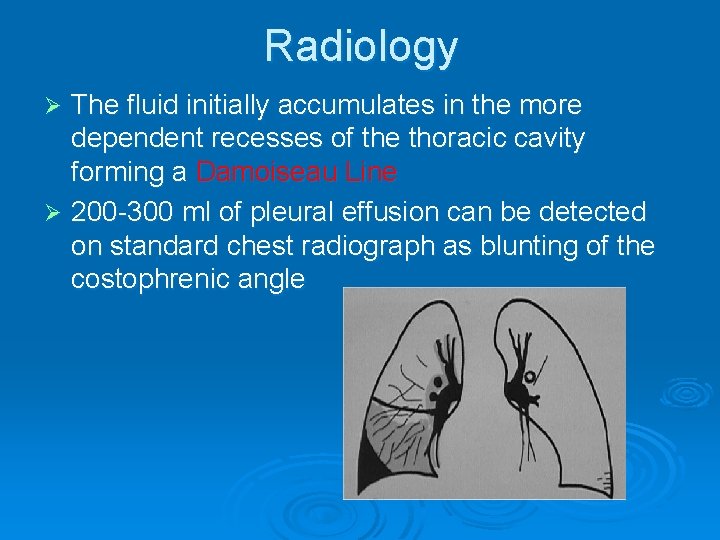
Radiology The fluid initially accumulates in the more dependent recesses of the thoracic cavity forming a Damoiseau Line Ø 200 -300 ml of pleural effusion can be detected on standard chest radiograph as blunting of the costophrenic angle Ø


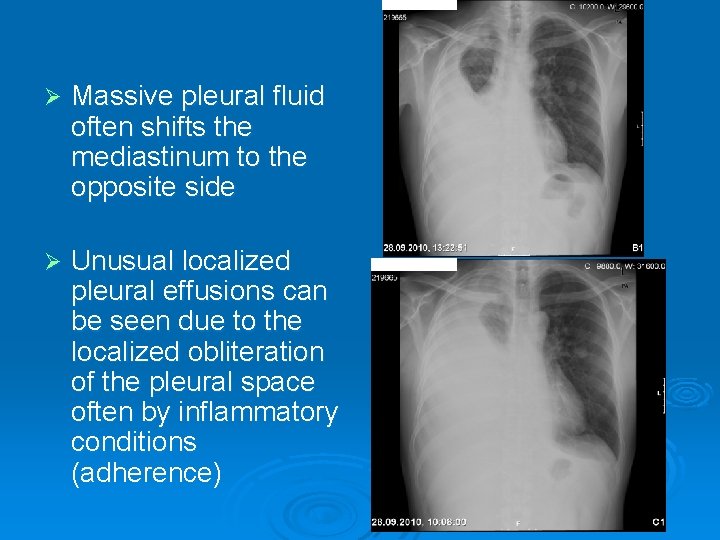
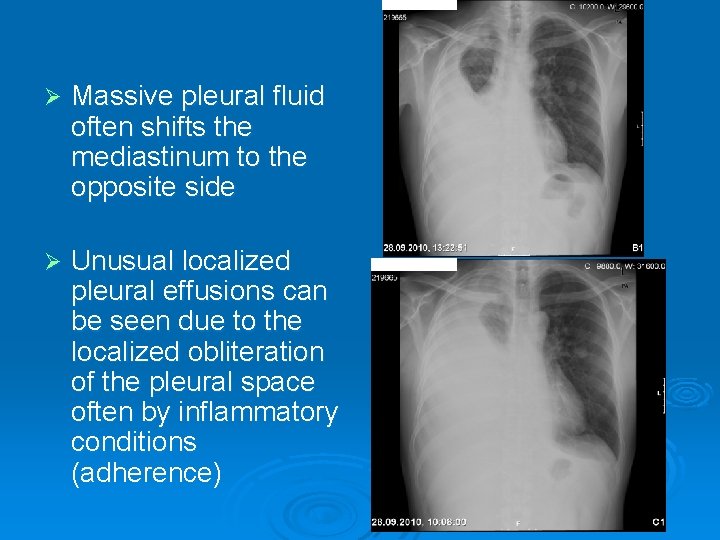
Ø Massive pleural fluid often shifts the mediastinum to the opposite side Ø Unusual localized pleural effusions can be seen due to the localized obliteration of the pleural space often by inflammatory conditions (adherence)
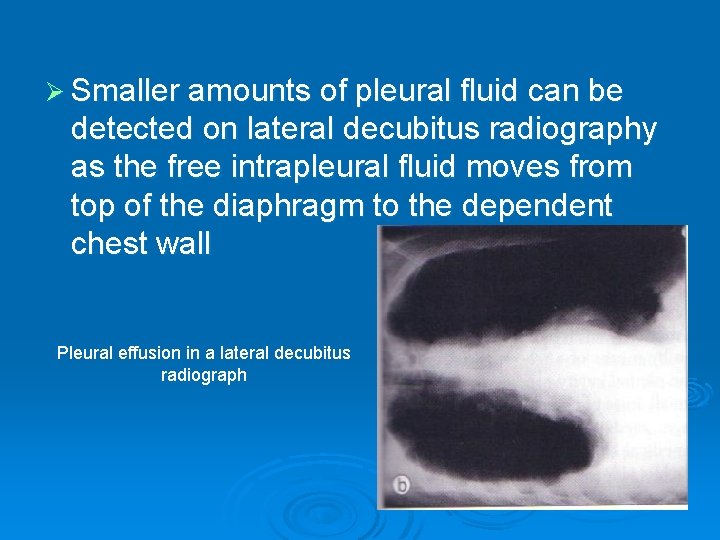
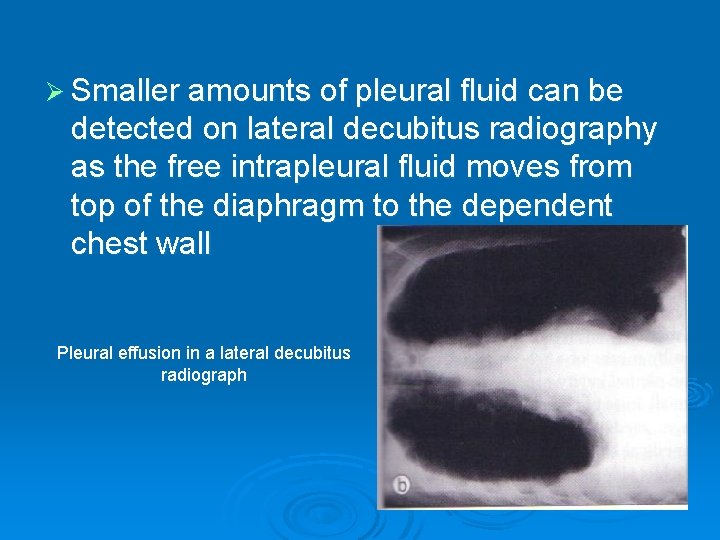
Ø Smaller amounts of pleural fluid can be detected on lateral decubitus radiography as the free intrapleural fluid moves from top of the diaphragm to the dependent chest wall Pleural effusion in a lateral decubitus radiograph
Ø Ultrasound is able to demonstrate smaller amounts of fluid as 100 ml Ø CT has similar sensitivity to ultrasound, not routine but can be performed to evaluate concomitant paranchymal lesions Ø CT is sensitive in identifying pleural thickening and calcification

Thoracenthesis and Pleural Fluid analysis Ø Appereance l l l Serous (light to dark yellow, clear) Serosangineous (Blood tinged can be due to thoracentesis itself) Hemorrhagic (hemothorax if hct>50% of blood hct) Purulent (fetid odor in unaerobic infections) Chylous (milky)
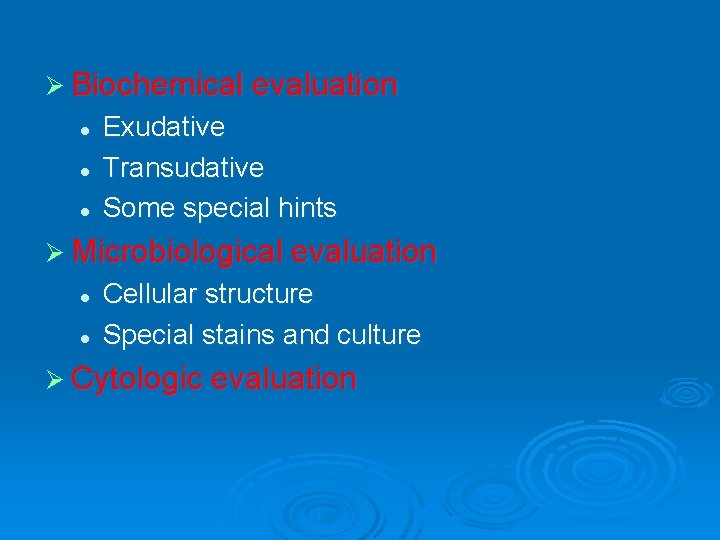
Ø Biochemical evaluation l l l Exudative Transudative Some special hints Ø Microbiological evaluation l l Cellular structure Special stains and culture Ø Cytologic evaluation
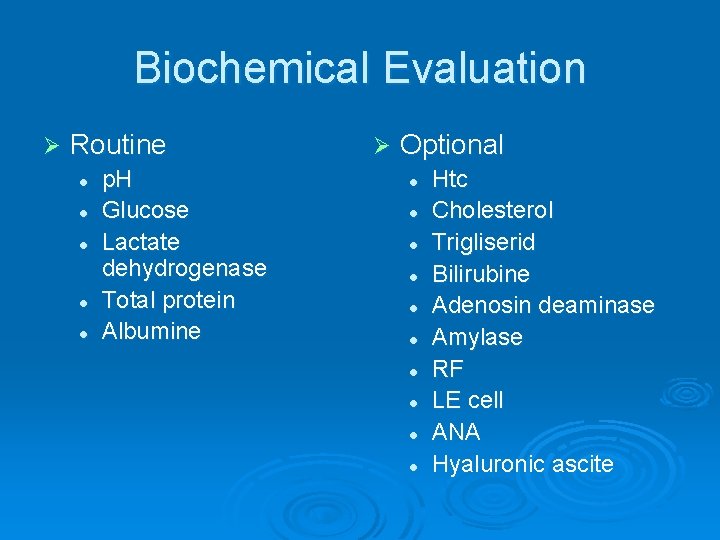
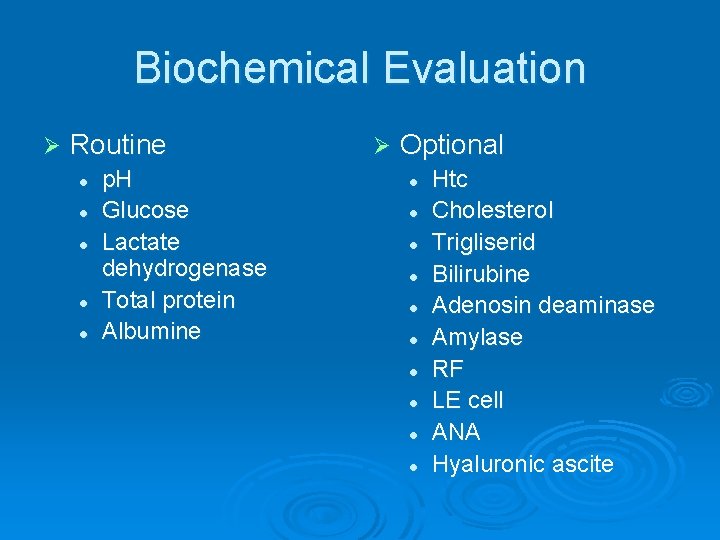
Biochemical Evaluation Ø Routine l l l p. H Glucose Lactate dehydrogenase Total protein Albumine Ø Optional l l Htc Cholesterol Trigliserid Bilirubine Adenosin deaminase Amylase RF LE cell ANA Hyaluronic ascite
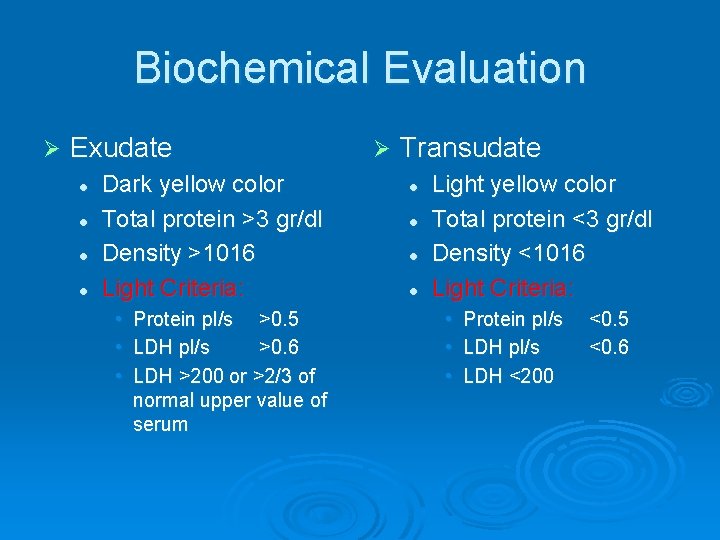
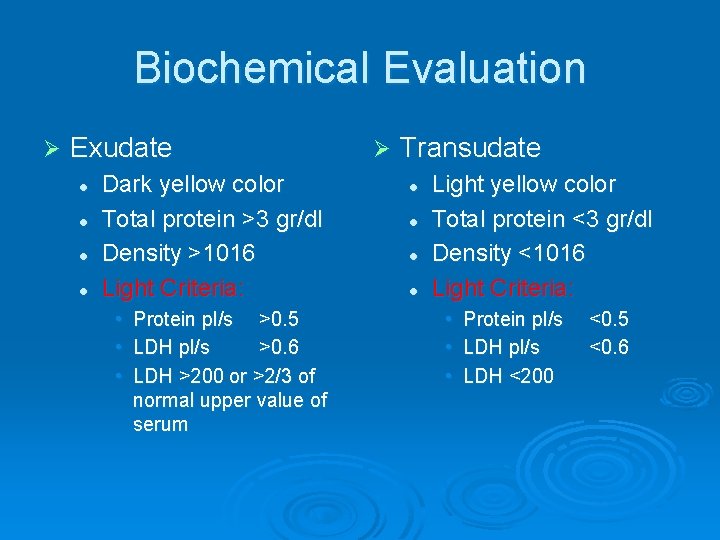
Biochemical Evaluation Ø Exudate l l Dark yellow color Total protein >3 gr/dl Density >1016 Light Criteria: • • • Protein pl/s >0. 5 LDH pl/s >0. 6 LDH >200 or >2/3 of normal upper value of serum Ø Transudate l l Light yellow color Total protein <3 gr/dl Density <1016 Light Criteria: • • • Protein pl/s LDH <200 <0. 5 <0. 6
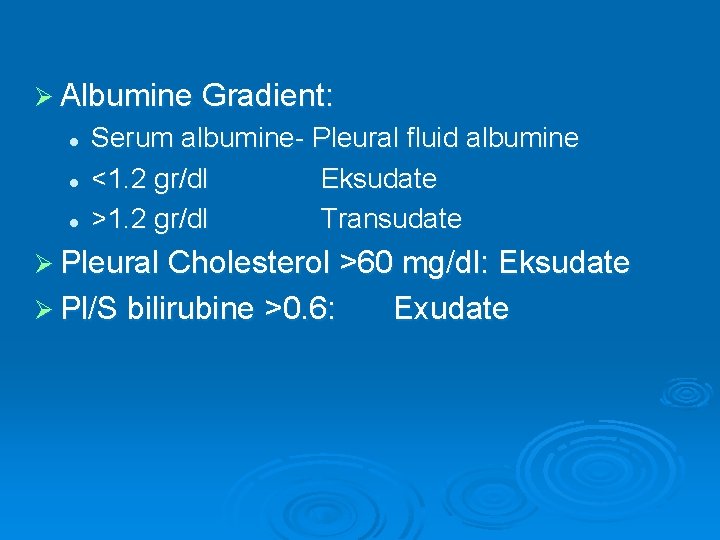
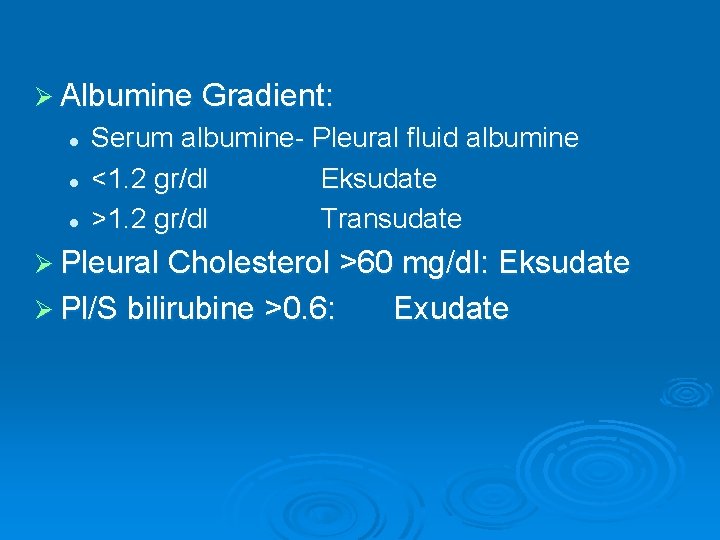
Ø Albumine Gradient: l l l Serum albumine- Pleural fluid albumine <1. 2 gr/dl Eksudate >1. 2 gr/dl Transudate Ø Pleural Cholesterol >60 mg/dl: Eksudate Ø Pl/S bilirubine >0. 6: Exudate
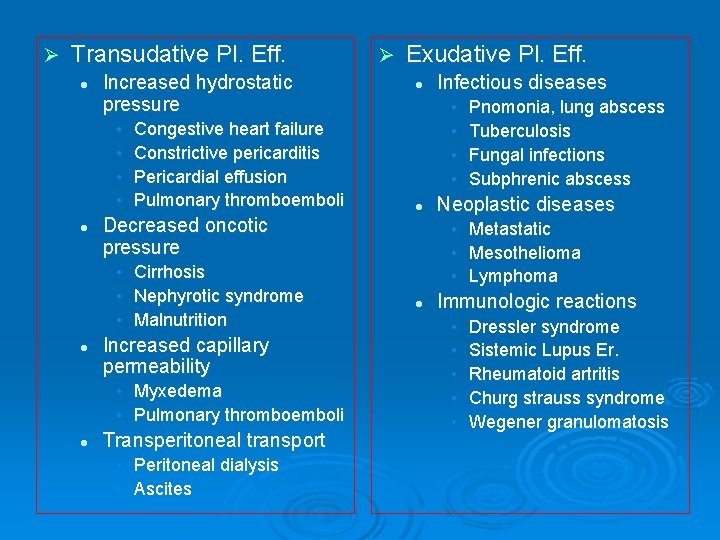
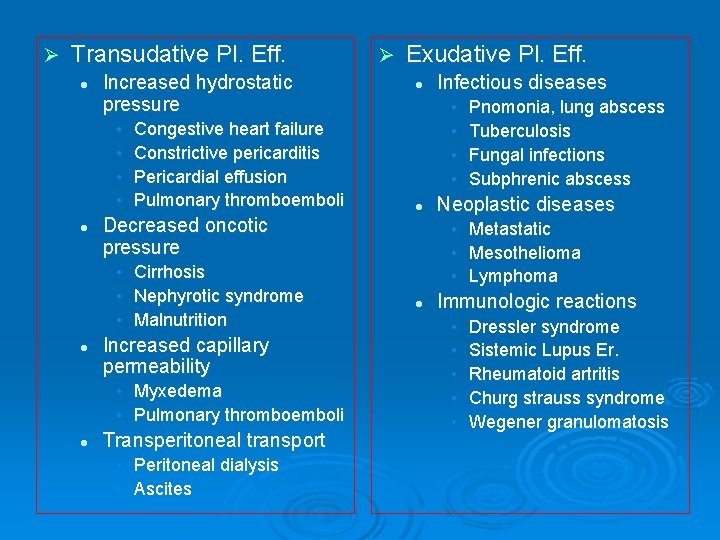
Ø Transudative Pl. Eff. l Increased hydrostatic pressure • • l Congestive heart failure Constrictive pericarditis Pericardial effusion Pulmonary thromboemboli Increased capillary permeability • Myxedema • Pulmonary thromboemboli l Exudative Pl. Eff. l Transperitoneal transport • Peritoneal dialysis • Ascites Infectious diseases • • l Decreased oncotic pressure • Cirrhosis • Nephyrotic syndrome • Malnutrition l Ø Pnomonia, lung abscess Tuberculosis Fungal infections Subphrenic abscess Neoplastic diseases • Metastatic • Mesothelioma • Lymphoma l Immunologic reactions • • • Dressler syndrome Sistemic Lupus Er. Rheumatoid artritis Churg strauss syndrome Wegener granulomatosis
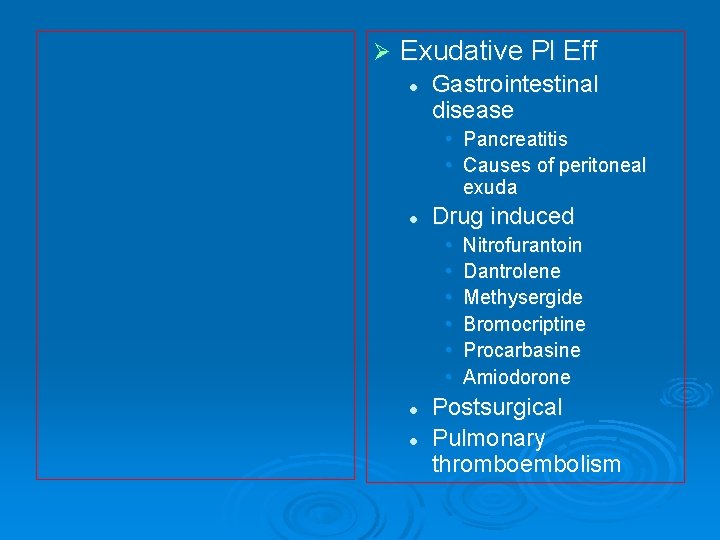
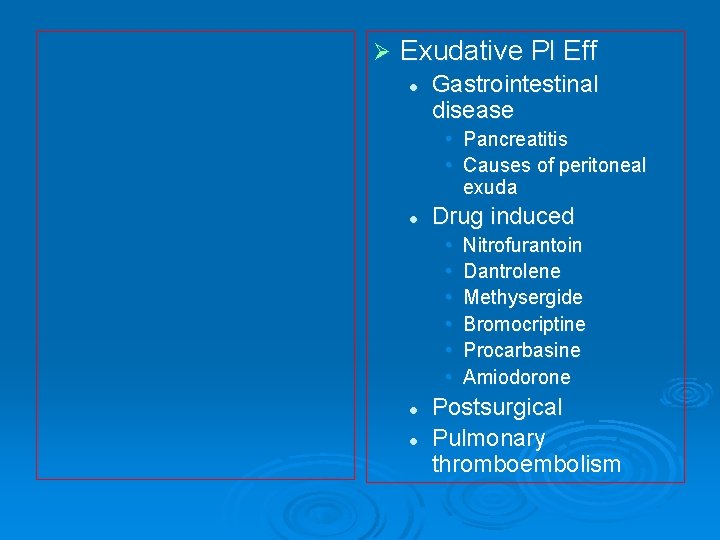
Ø Exudative Pl Eff l Gastrointestinal disease • Pancreatitis • Causes of peritoneal exuda l Drug induced • • • l l Nitrofurantoin Dantrolene Methysergide Bromocriptine Procarbasine Amiodorone Postsurgical Pulmonary thromboembolism
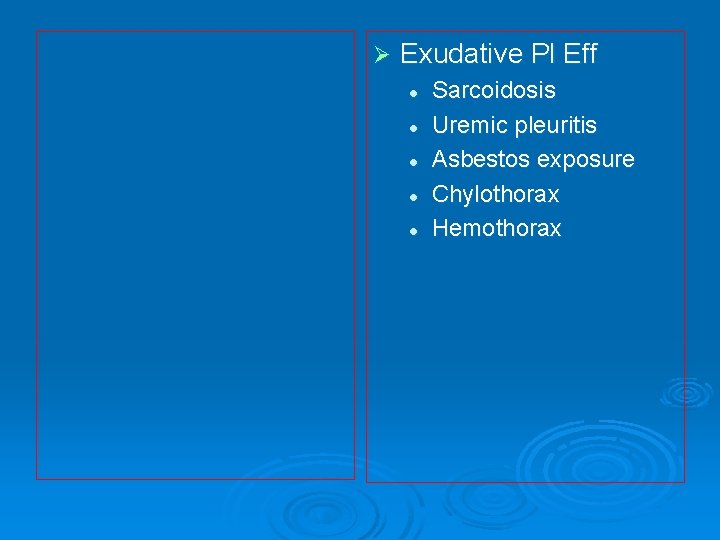
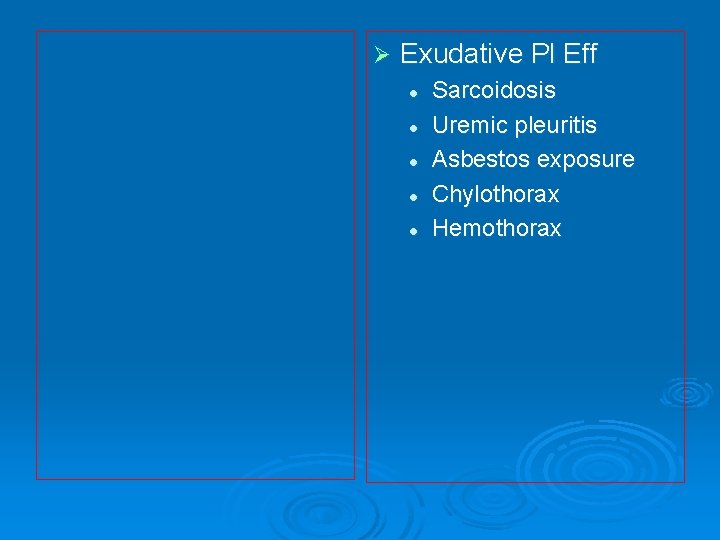
Ø Exudative Pl Eff l l l Sarcoidosis Uremic pleuritis Asbestos exposure Chylothorax Hemothorax
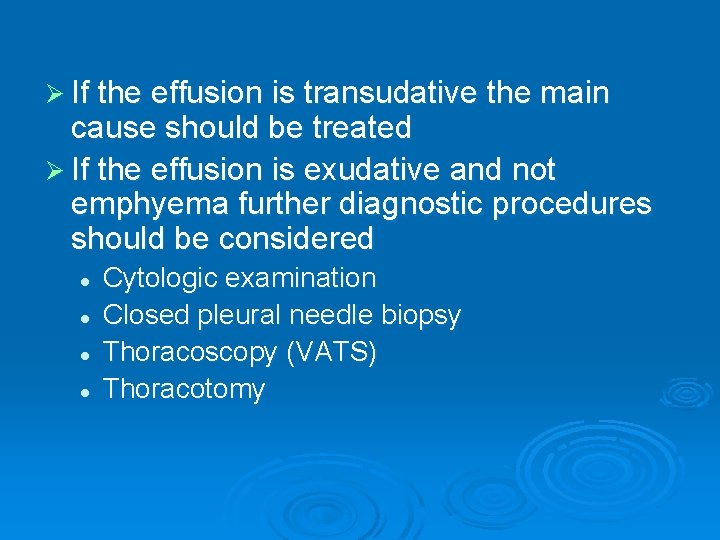
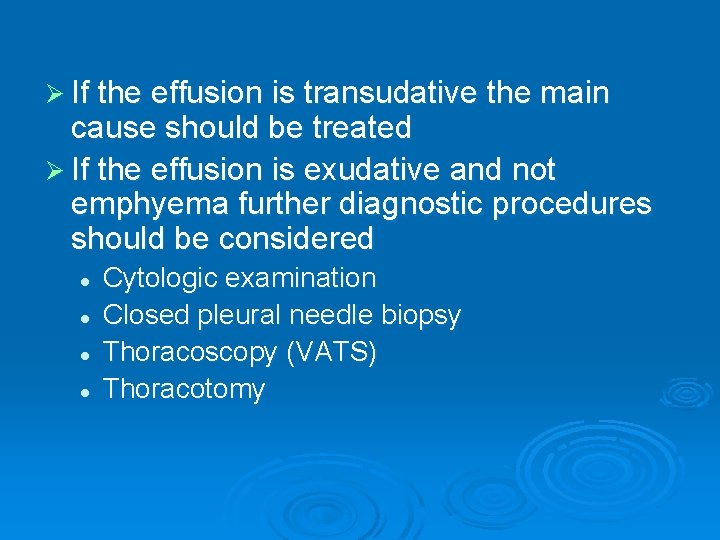
Ø If the effusion is transudative the main cause should be treated Ø If the effusion is exudative and not emphyema further diagnostic procedures should be considered l l Cytologic examination Closed pleural needle biopsy Thoracoscopy (VATS) Thoracotomy
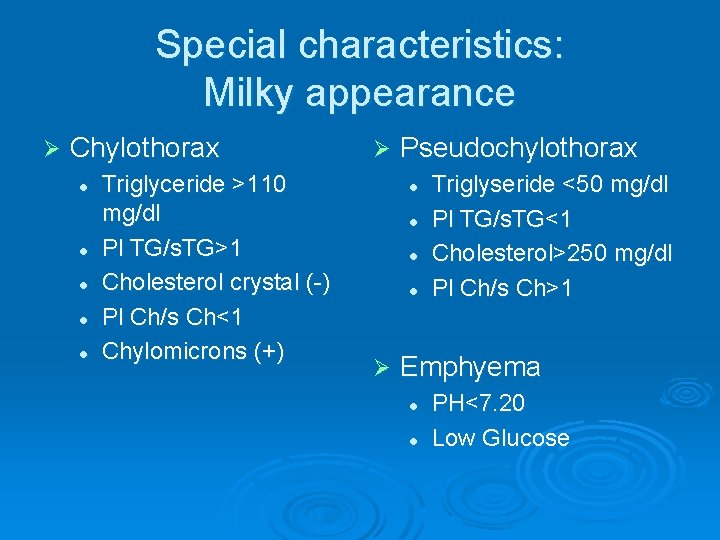
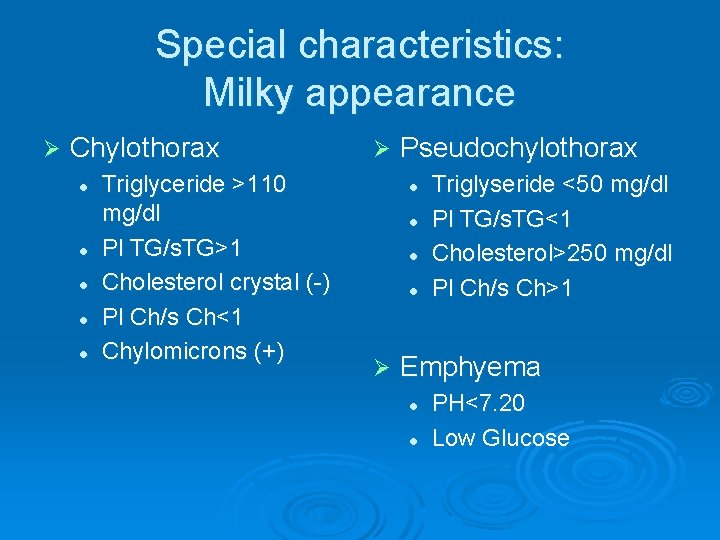
Special characteristics: Milky appearance Ø Chylothorax l l l Triglyceride >110 mg/dl Pl TG/s. TG>1 Cholesterol crystal (-) Pl Ch/s Ch<1 Chylomicrons (+) Ø Pseudochylothorax l l Ø Triglyseride <50 mg/dl Pl TG/s. TG<1 Cholesterol>250 mg/dl Pl Ch/s Ch>1 Emphyema l l PH<7. 20 Low Glucose
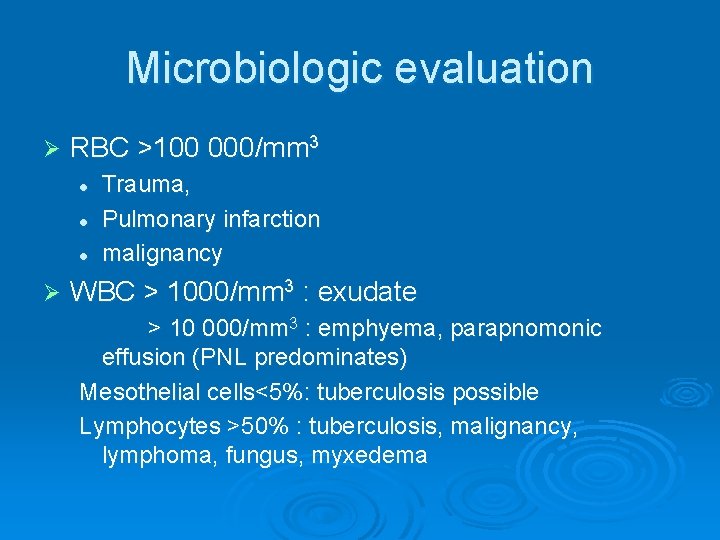
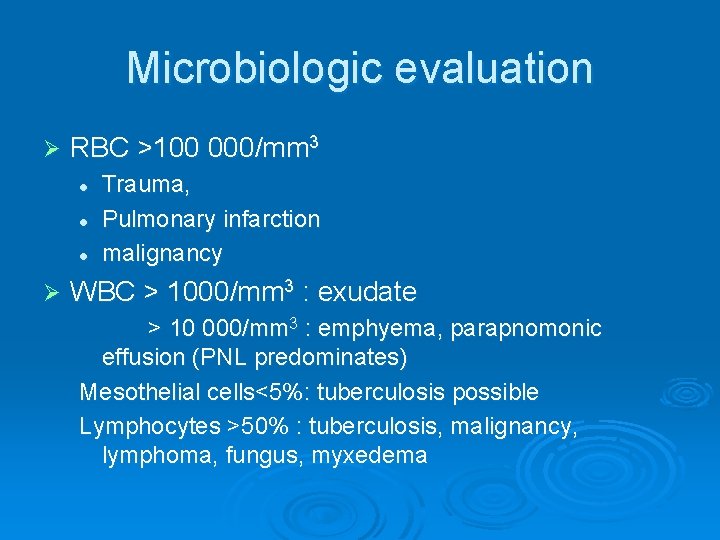
Microbiologic evaluation Ø RBC >100 000/mm 3 l l l Ø Trauma, Pulmonary infarction malignancy WBC > 1000/mm 3 : exudate > 10 000/mm 3 : emphyema, parapnomonic effusion (PNL predominates) Mesothelial cells<5%: tuberculosis possible Lymphocytes >50% : tuberculosis, malignancy, lymphoma, fungus, myxedema
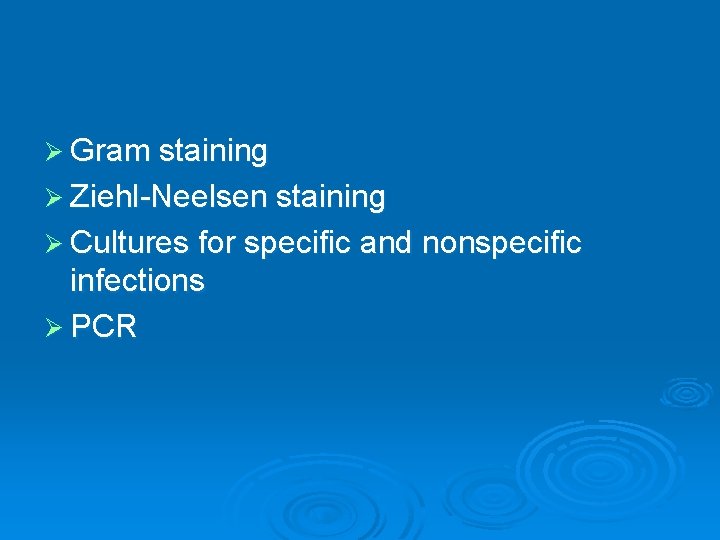
Ø Gram staining Ø Ziehl-Neelsen staining Ø Cultures for specific and nonspecific infections Ø PCR
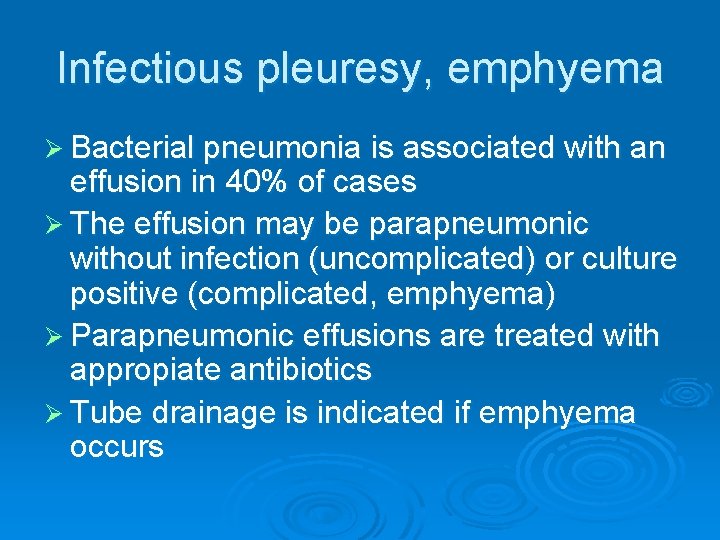
Infectious pleuresy, emphyema Ø Bacterial pneumonia is associated with an effusion in 40% of cases Ø The effusion may be parapneumonic without infection (uncomplicated) or culture positive (complicated, emphyema) Ø Parapneumonic effusions are treated with appropiate antibiotics Ø Tube drainage is indicated if emphyema occurs
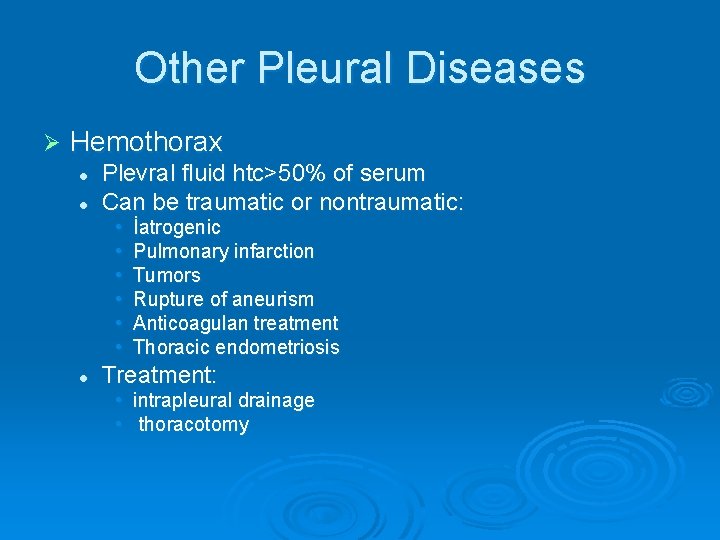
Other Pleural Diseases Ø Hemothorax l l Plevral fluid htc>50% of serum Can be traumatic or nontraumatic: • • • l İatrogenic Pulmonary infarction Tumors Rupture of aneurism Anticoagulan treatment Thoracic endometriosis Treatment: • • intrapleural drainage thoracotomy
Ø Fibrothorax l l A thick fibrous tissue formed on visceral pleura Cause: • • • l Empyema Tuberculosis Hemothorax Treatment: Decortication
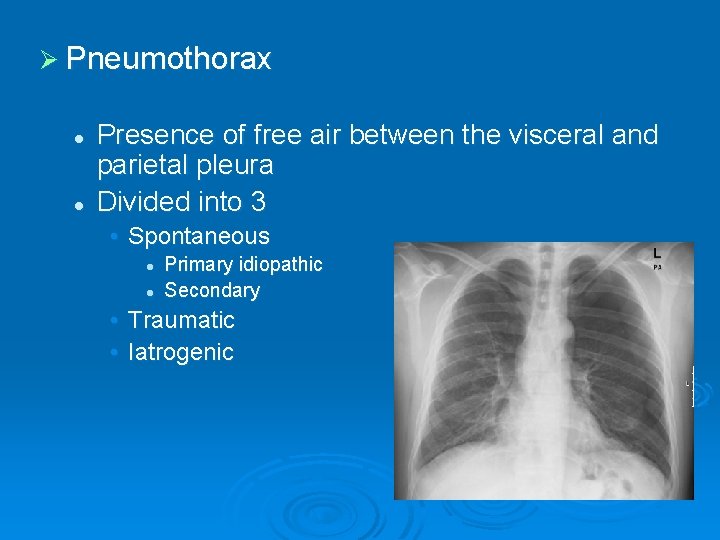
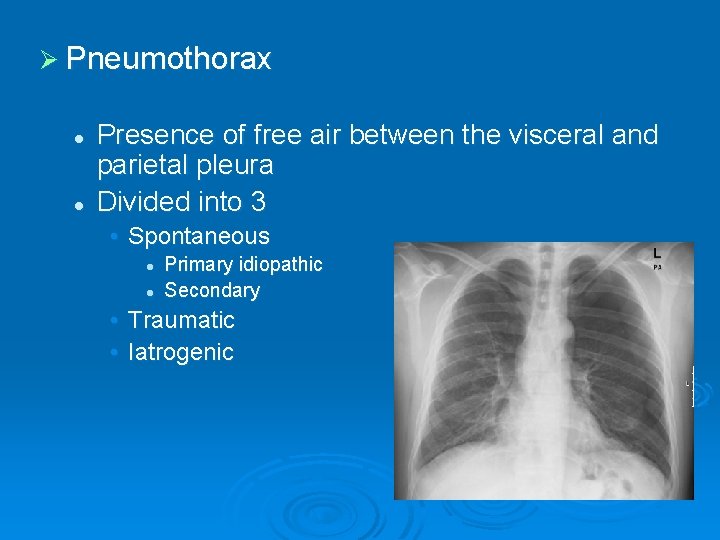
Ø Pneumothorax l l Presence of free air between the visceral and parietal pleura Divided into 3 • Spontaneous l l Primary idiopathic Secondary • Traumatic • Iatrogenic
Primary Spontaneous Pneumothorax Ø Mostly occurs in young, male, smokers Ø There is no obvious underlying pulmonary disease Ø Subpleural blebs and bullae probably play a role in pathogenesis Ø Symptoms can be an acute unset of dyspnea and unilateral chest pain but can be absent also depending on the size of the pneumothorax
Ø Physical examination: l l l Ø Hypersonority on percusion Reduced breath sounds, reduced VT, enlarged hemithorax Hypotension and cardiac tamponade may occur depending on the size of the pneumothorax Radiology: l l Pleural line Hyperlucency at the periphery Mediastinal shift Expiration film can be used when the lesion is not apparent


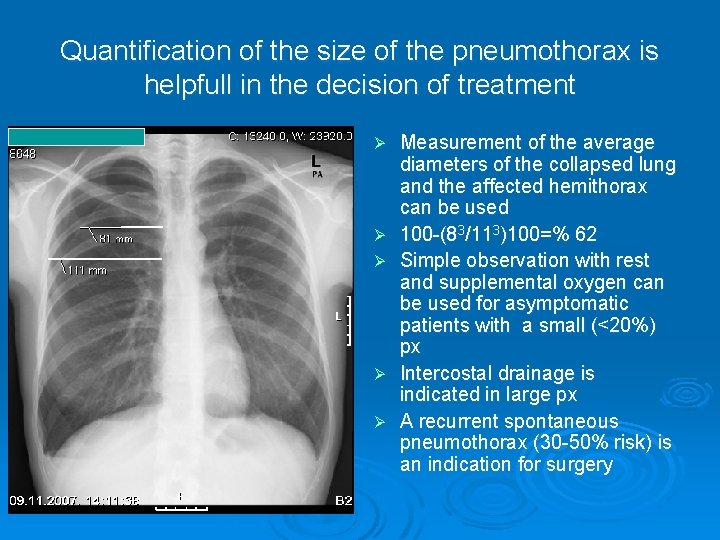
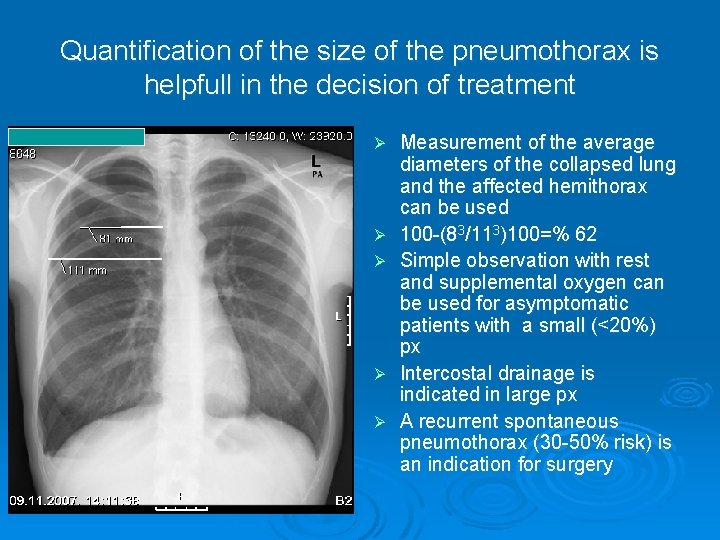
Quantification of the size of the pneumothorax is helpfull in the decision of treatment Ø Ø Ø Measurement of the average diameters of the collapsed lung and the affected hemithorax can be used 100 -(83/113)100=% 62 Simple observation with rest and supplemental oxygen can be used for asymptomatic patients with a small (<20%) px Intercostal drainage is indicated in large px A recurrent spontaneous pneumothorax (30 -50% risk) is an indication for surgery
Secondary Spontaneous Pneumothorax Ø Patients have an underlying pulmonary disease: l l l COPD Asthma Congenital cysts and bullae Interstitial lung fibrosing diseases Cystic fibrosis Hystiocytosis X Whooping cough Lymphangiomyomatosis Pleural endometriosis, catamenial pneumothorax Pleural malignancy Sarcoidosis Bacterial pneumonia and Pneumocystis Pneumonia
Traumatic and Iatrogenic Pneumothorax Ø Iatrogenic pneumothorax can be seen during: l l l l Thorasentesis Pleural needle biopsy Transthoracic lung aspiration biopsy Mechanical ventilation Central venous catheterization Tracheostomy Cardiopulmonary resusitation
Pleural Neoplasms Ø Benign: l l Pleural lipoma Local pleural fibroma (Fibrous mesothelioma) Ø Malign: l Diffuse malign mesothelioma
Malign Pleural effusions Ø Diffuse Malign Mesothelioma Ø Bronchial carcinoma (adenocarcinoma) Ø Lymphoma Ø Breast carcinoma Ø Other adenocarcinomas
Malignant Mesothelioma Primary tumour of pleural, pericardial, peritonial mesothelium Ø Etiology: 70 -90% asbest exposure: Ø l l Occupational: asbest is resistant to heat and friction so used in building, water pipes, brakes, isolation systems, textile Environmental: Eskişehir, Kütahya, Bilecik, Yozgat, Sivas, Diyarbakır Latent period is 30 -40 years in occupational exposure Ø Smoking dramaticaly increase the risk of cancer in asbest exposure Ø
Erionite is another fibrous zeolite found in soil, high in Nevşehir: Tuzköy, Karain, Sarıhıdır area in Turkey. It is more carcinogenic than asbest. 49% of total deaths in the villages of Ürgüp are due to DMM
Ø The most common clinical presentations are dyspnea, chest pain, unilateral decreased volume of the affected hemithorax (frozen chest) (inspite of fluid accumilation) Ø Nodular thickening of the pleura, irregular thickening of the interlobar fissure, absence of mediastinal shift with massive pleural effusion (frozen chest) Diagnosis by histologic examination Ø Treatment oncologic and surgical if possible, prognosis is poor Ø

-END-
 Anlamlı maniler
Anlamlı maniler Sevda ibrahimova sülh marşı
Sevda ibrahimova sülh marşı Bharathi viswanathan
Bharathi viswanathan Icd 10 morbus hansen
Icd 10 morbus hansen Periradicular disease definition
Periradicular disease definition Cardiovascular system diseases and disorders chapter 8
Cardiovascular system diseases and disorders chapter 8 Epidemiological triad
Epidemiological triad Non communicable diseases
Non communicable diseases What are deficiency
What are deficiency Modern lifestyle and hypokinetic diseases
Modern lifestyle and hypokinetic diseases Milady chapter 10 nail disorders and diseases
Milady chapter 10 nail disorders and diseases Difference between communicable and noncommunicable
Difference between communicable and noncommunicable Chapter 32 childhood communicable diseases bioterrorism
Chapter 32 childhood communicable diseases bioterrorism Diseases in civil war
Diseases in civil war Diseases of the musculoskeletal system
Diseases of the musculoskeletal system Human diseases a systemic approach
Human diseases a systemic approach Waterwashed diseases
Waterwashed diseases Diseases spread by columbian exchange
Diseases spread by columbian exchange Introduction of nutrients
Introduction of nutrients Quality gurus
Quality gurus Ascaris lumbricoides
Ascaris lumbricoides Nutritional diseases
Nutritional diseases Tronsmo plant pathology and plant diseases download
Tronsmo plant pathology and plant diseases download Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Section 19-3 diseases caused by bacteria and viruses
Section 19-3 diseases caused by bacteria and viruses Diseases caused by dust
Diseases caused by dust Nursing management of reproductive tract infection
Nursing management of reproductive tract infection Pulpitis classification
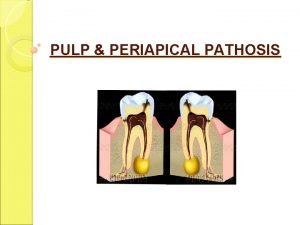
Pulpitis classification Phytomastigophora characteristics
Phytomastigophora characteristics Columbian exchange restaurant names
Columbian exchange restaurant names Infection or disease that originates within the body
Infection or disease that originates within the body Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Chapter 10 lymphatic system diseases and disorders
Chapter 10 lymphatic system diseases and disorders Vitamins sources functions and deficiency chart
Vitamins sources functions and deficiency chart Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Non communicable diseases infographic
Non communicable diseases infographic Purulent diseases of lungs and pleura
Purulent diseases of lungs and pleura Microbes
Microbes Sexually transmitted diseases
Sexually transmitted diseases Communicable and noncommunicable diseases venn diagram
Communicable and noncommunicable diseases venn diagram Chapter 23 lesson 1 understanding communicable diseases
Chapter 23 lesson 1 understanding communicable diseases King of diseases
King of diseases Myths and fallacies about non communicable diseases
Myths and fallacies about non communicable diseases Protein deficiency diseases
Protein deficiency diseases Albugo eye
Albugo eye Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Vagninitis
Vagninitis Chapter 8 skin disorders and diseases
Chapter 8 skin disorders and diseases